General anaesthetics
General anaesthetics work in the brain to induce reversible unconsciousness with amnesia, akinesia and varying degrees of analgesia. This allows surgical or other painful procedures to be undertaken without the person being aware. General anaesthesia was introduced into clinical practice in the 19th century, with the inhalation of vapours such as diethyl ether and chloroform. Major drawbacks with such compounds included the time taken to cause loss of consciousness, slow recovery, unpleasant taste, irritant properties and their potential to explode. Cardiac and hepatic toxicity also limited the usefulness of chloroform. The perfect general anaesthetic would possess the properties shown in Box 17.1, but no single anaesthetic agent has all of these. Therefore, to produce general anaesthesia it is usual to use a combination of several drugs that have different desirable and unwanted effects. Each contributes in different degrees to sedation, analgesia and muscle relaxation, an approach known as ‘balanced anaesthesia’ (Table 17.1). Full general anaesthesia produces not only loss of consciousness, but also depresses brainstem reflexes with loss of spontaneous respiration and depression of heart rate and blood pressure, a state that is comparable to coma.
Table 17.1
The concept of ‘balanced anaesthesia’
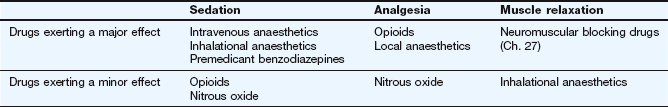
Drugs are used in combination to produce the appropriate balance of sedation, analgesia and muscle relaxation while minimising unwanted effects; at particular doses and concentrations, each contributes minor or major effects to achieve this balance. Excessive or inadequate doses of any one agent could disturb the balance.
General anaesthesia for surgical procedures involves several steps, although not all are essential for successful anaesthesia:
Premedication is given to adults to reduce anxiety and produce amnesia, usually with a benzodiazepine such as diazepam (Ch. 20). In addition, an antiemetic such as metoclopramide (Ch. 32) may be used.
Anaesthesia was originally induced and maintained solely by inhalation of a volatile agent, when several stages of general anaesthesia are observed during induction in adults (Table 17.2). The stage of excitation with struggling can be overcome by using a bolus of intravenous anaesthetic for rapid induction, followed by an inhalational anaesthetic for maintenance. For short surgical procedures in adults, both induction and maintenance can be achieved with an intravenous anaesthetic alone (total intravenous anaesthesia). In children, excitation is less of a problem, and anaesthesia is often both induced and maintained with an inhalational anaesthetic agent. Full general anaesthesia produces depression of spontaneous respiration and blood pressure, requiring artificial ventilation and perhaps circulatory support. Some short procedures do not need full general anaesthesia, and can be carried out under sedation by an anaesthetic with preserved respiratory and cardiovascular function. The adequacy of general anaesthesia is assessed by monitoring the heart rate, blood pressure and other physiological functions. For example, it can be inferred that the level of anaesthesia is inadequate and that pain is being experienced if the heart rate rises, or the person develops perspiration, tears, return of muscle tone, movement or change in pupil size.
Table 17.2
| Stage | Description | Effects produced |
| I | Analgesia | Analgesia without amnesia or loss of touch sensation; consciousness retained |
| II | Excitation | Excitation and delirium with struggling; respiration rapid and irregular; frequent eye movements with increased pupil diameter; amnesia |
| III | Surgical anaesthesia | Loss of consciousness; subdivided into four levels or planes of increasing depth Plane I: decrease in eye movements and some pupillary constriction Plane II: loss of corneal reflex Planes III and IV: increasing loss of pharyngeal reflex, and progressive decrease in thoracic breathing and general muscle tone |
| IV | Medullary depression | Loss of spontaneous respiration and progressive depression of cardiovascular reflexes, no eye movements; requires respiratory and circulatory support |
For abdominal and thoracic surgery, and for long operations, full skeletal muscle paralysis is produced by giving neuromuscular blocking drugs (Ch. 27), in which case endotracheal intubation and mechanical ventilation are essential. Analgesia can be provided by an intravenous opioid for systemic analgesia, or by a local anaesthetic (Ch. 18) to provide regional analgesia, such as into the epidural space (epidural analgesia) or around peripheral nerves.
At the end of an operation, resumption of consciousness (reversal of anaesthesia) occurs when intravenous anaesthetics are redistributed or metabolised, or when inhalational anaesthetics are redistributed or exhaled. Residual neuromuscular blockade by competitive blocking agents may need reversal with an anticholinesterase such as neostigmine (Ch. 27). Attentiveness, and therefore the ability to drive safely, may be impaired for up to 24 h after general anaesthesia.
Mechanisms of action of general anaesthetics
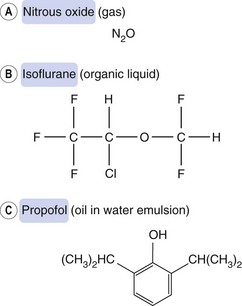
General anaesthesia can be produced by compounds of widely differing chemical structure: simple gases such as nitrous oxide, volatile liquids such as isoflurane and non-volatile solids such as propofol (Fig. 17.1). They act at several sites in the brain, but particularly the brainstem arousal centres, frontal cortex and thalamus to produce unconsciousness, and the spinal cord, pons and medulla to produce muscle relaxation.
General anaesthetics act at cell membranes, and the relationship between lipid solubility and potency led to the Meyer–Overton hypothesis that their incorporation into lipids altered the properties and function of neuronal cell membranes. However, this does not account for many of the properties of general anaesthetics, including the differing anaesthetic potencies of the stereoisomers of some anaesthetic agents which suggests stereospecific interaction with target receptors. The general relationship between lipid solubility and anaesthetic potency is probably more important for determining the pharmacokinetic properties of the drug than for explaining its mode of action.
Although it is not known precisely how general anaesthetics work, there is increasing evidence that implicates actions at ligand-gated ion channels (Table 17.3). Individual intravenous or inhalational anaesthetic agents have diverse abilities to inhibit or enhance the functions of a number of ion channels, thus explaining the differences in their capacities to produce unconsciousness, amnesia, analgesia and muscle relaxation. This may be achieved by direct interaction with the ion channel or by modulation of the receptors that control these channels. In particular, their actions are to inhibit the functions of excitatory receptors (such as those for acetylcholine [nicotinic] and for glutamate (N-methyl-D-aspartate [NMDA] receptors) and to enhance the functions of inhibitory receptors (such as those for γ-aminobutyric acid [GABAA] and possibly glycine), or to activate K+ channels that are widely expressed in inhibitory GABA interneurons.
Table 17.3
Possible sites of action of inhalation and intravenous general anaestheticsa
| Drug group | Properties of group | Receptor and channel targets |
| Etodimate, propofol, thiopental | Potent amnesics Potent sedatives Weak muscle relaxants |
Enhance activity at GABAA receptors |
| Nitrous oxide, ketamine | Potent analgesics Weak sedatives Weak muscle relaxants |
Inhibit glutamate NMDA receptors Inhibit ACh nicotinic receptors Open two-pore K+ channels |
| Sevoflurane, isoflurane, desflurane | Potent amnesics Potent sedatives Potent muscle relaxants |
Enhance activity at GABAA receptors Enhance activity at glycine receptors Inhibit glutamate NMDA receptors Inhibit ACh nicotinic receptors Open two-pore K+ channels |
ACh, acetylcholine; GABA, γ-aminobutyric acid; NMDA, N-methyl-D-aspartate.
aInformation for this table is derived mainly from Solt and Forman (2007) and is based on data from in vitro studies and in vivo studies in transgenic animals.
Receptor binding sites for general anaesthetics have not been fully characterised, but are probably on proteins associated with the receptors and ion channels. General anaesthetics may compete with endogenous ligands or modulate the effect of these ligands at the receptor. As a result, they inhibit both local and long-range (such as thalamocortical) neural circuits.
The various stages of anaesthesia (Table 17.2) probably arise as a result of the different sizes of neurons affected by anaesthetics and their accessibility to the anaesthetic agent. A rapid action on small neurons in the dorsal horn of the spinal cord (nociceptive impulses; Ch. 19) and inhibitory cells in the brain (see effects of alcohol; Ch. 54) explain the early analgesic and excitation phases. By contrast, neurons of the medullary centres are less sensitive.
Drugs used in anaesthesia
General anaesthetics can be grouped according to their route of administration, which is either intravenous or inhalational.
Intravenous anaesthetics
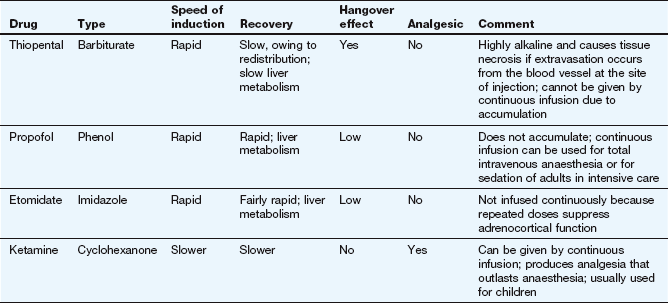
Intravenous anaesthetics can be given by slow intravenous injection for rapid induction of anaesthesia and then replaced by inhalational anaesthetics for longer-term maintenance of anaesthesia. Both propofol and ketamine (but not etomidate or thiopental) can also be given by continuous infusion without inhalational anaesthesia for short operations (total intravenous anaesthesia) or for prolonged sedation. Ketamine is analgesic, unlike all other available intravenous anaesthetics, but it does not reliably suppress laryngeal reflexes, which can make endotracheal intubation more difficult. It is now rarely used, except for paediatric anaesthesia. Some properties of commonly used intravenous anaesthetics are shown in Table 17.4.
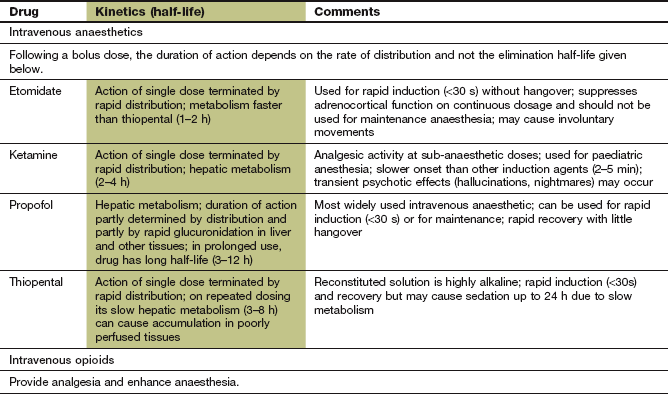
Pharmacokinetics
Thiopental is a thiobarbiturate that has a very rapid onset of action (within 30 s) owing to its high lipid solubility and ease of passage across the blood–brain barrier. The duration of action after a bolus dose is very short (about 2–5 min). Blood concentrations fall rapidly, initially because of distribution into tissues with greatest blood flow; distribution then occurs more slowly into the major muscle groups and into adipose tissue, which is lipid-rich but has poor blood flow (Fig. 17.2). With thiopental, total intravenous anaesthesia is not practicable, as during a lengthy procedure the brain and blood and slowly equilibrating tissues would reach equilibrium. Recovery from anaesthesia on cessation of anaesthetic administration would then depend on the elimination half-life (3–8 h for thiopental, related to hepatic metabolism) not the distribution half-life (about 3 min). Therefore, following induction of anaesthesia with thiopental, an inhalational agent is used for maintenance of anaesthesia.
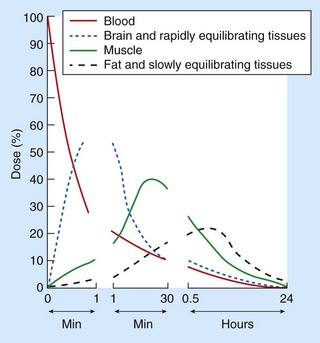
Fig. 17.2 The amounts of thiopental in blood, brain (and other rapidly equilibrating tissues), muscle, adipose tissue and other slowly equilibrating tissues after an intravenous infusion over 10 s.
Note: the time axis is not linear: the continued uptake into muscle between 1 and 30 min lowers the concentration in the blood and in all rapidly equilibrating tissues (including the brain); the terminal elimination slopes are parallel for all tissues; metabolism removes about 15% of the body load per hour.
Propofol has a slightly slower onset of action (about 30 s) compared with thiopental, but its duration of action is also limited by redistribution after a bolus dose. It can be given as an infusion for total intravenous anaesthesia (and for sedation in intensive care), but under these circumstances its duration of action is determined by a slower tissue distribution phase (half-life 0.5–1 h), whereas after prolonged use its duration of action is determined by hepatic clearance (half-life about 6 h). Propofol is particularly useful for day surgery, because of its rapid distribution and absence of hangover effects. It can also be used by intravenous infusion for up to 3 days for sedation in conscious adults requiring controlled ventilation in an intensive care unit.
Ketamine can be given by intramuscular injection or intravenously by bolus injection or infusion. When used for induction or for total intravenous anaesthesia the anaesthetic action is terminated largely by distribution (half-life about 15 min). With prolonged infusion it becomes dependent on hepatic metabolism (half-life 2–4 h).
Etomidate has a rapid onset of action after intravenous injection, and its action is terminated by rapid metabolism in plasma and the liver, so that the duration of action is about 6–10 min with minimal hangover. It is not used to maintain anaesthesia because prolonged infusion can suppress adrenocortical function.
Unwanted effects
 On the central nervous system (CNS): general depression of the CNS can produce respiratory and cardiovascular depression. Slow release of thiopental distributed into tissues may result in some sedation for up to 24 h after use. Hallucinations and vivid dreams are common during recovery from ketamine (emergence reactions), but are less frequent in children. They can be reduced by giving a benzodiazepine (Ch. 20).
On the central nervous system (CNS): general depression of the CNS can produce respiratory and cardiovascular depression. Slow release of thiopental distributed into tissues may result in some sedation for up to 24 h after use. Hallucinations and vivid dreams are common during recovery from ketamine (emergence reactions), but are less frequent in children. They can be reduced by giving a benzodiazepine (Ch. 20).
 On muscles: extraneous muscle movement is common with etomidate, and to a lesser degree with propofol. They can be reduced by a benzodiazepine or opioid analgesic given before induction. Ketamine increases muscle tone and can cause laryngospasm.
On muscles: extraneous muscle movement is common with etomidate, and to a lesser degree with propofol. They can be reduced by a benzodiazepine or opioid analgesic given before induction. Ketamine increases muscle tone and can cause laryngospasm.
 On the heart: thiopental, propofol and to a lesser extent etomidate depress the heart, producing bradycardia and reducing blood pressure. By contrast, ketamine more often produces tachycardia and an increase in blood pressure.
On the heart: thiopental, propofol and to a lesser extent etomidate depress the heart, producing bradycardia and reducing blood pressure. By contrast, ketamine more often produces tachycardia and an increase in blood pressure.
 Nausea and vomiting during recovery are experienced by up to 40% of people but rarely persist for more than 24 h. Propofol has an anti-emetic action.
Nausea and vomiting during recovery are experienced by up to 40% of people but rarely persist for more than 24 h. Propofol has an anti-emetic action.
 Convulsions have been reported after propofol. These can be delayed, indicating the need for special caution after day surgery.
Convulsions have been reported after propofol. These can be delayed, indicating the need for special caution after day surgery.
 Pain on injection with etomidate and propofol: this can be reduced by injecting into a large vein or by giving an opioid analgesic just before induction with etomidate, or giving intravenous lignocaine with propofol. Thiopental is an alkaline solution that is irritant if it extravasates outside the vein, causing tissue necrosis.
Pain on injection with etomidate and propofol: this can be reduced by injecting into a large vein or by giving an opioid analgesic just before induction with etomidate, or giving intravenous lignocaine with propofol. Thiopental is an alkaline solution that is irritant if it extravasates outside the vein, causing tissue necrosis.
 Propofol is not used for continuous sedation in children because of the risk of propofol infusion syndrome, which includes metabolic acidosis, heart failure and rhabdomyolysis.
Propofol is not used for continuous sedation in children because of the risk of propofol infusion syndrome, which includes metabolic acidosis, heart failure and rhabdomyolysis.
Intravenous opioids
Intravenous opioids are usually given at induction for intraoperative analgesia, therefore reducing the dose requirement of anaesthetic agents. They can also be used for sedation and respiratory depression during assisted ventilation in intensive care. In high doses, opioids stimulate the vagus and produce bradycardia; this can be helpful to reduce the tachycardia and hypertension produced by sympathetic nervous system activation during surgery. Details of the mechanism of action of opioids can be found in Chapter 19.
Pharmacokinetics
After intravenous injection, fentanyl has a rapid onset of action within 1–2 min. After a single dose the drug is distributed rapidly into skeletal muscle and fat (half-life about 15 min) and its duration of action is about 30–60 min. The effect is maintained by repeated injections or infusion, but with prolonged use tissue stores are saturated and fentanyl then has a long duration of action determined by its hepatic metabolism (half-life about 4 h). After repeated injections respiratory depression may become apparent during recovery from the anaesthetic.
Remifentanil is an opioid ester that has a similar rapid onset to fentanyl but a very short half-life of about 5 min, due to metabolism by tissue and plasma esterases. After an initial bolus dose of remifentanil continuous intravenous infusion is used to maintain its effects.
Unwanted effects
 Muscle rigidity: this particularly affects the chest wall and jaw and can be prevented during surgery with neuromuscular junction blocking drugs (Ch. 27). Myoclonus and rigidity can persist after recovery, and require reversal with the opioid antagonist naloxone (Ch. 19)
Muscle rigidity: this particularly affects the chest wall and jaw and can be prevented during surgery with neuromuscular junction blocking drugs (Ch. 27). Myoclonus and rigidity can persist after recovery, and require reversal with the opioid antagonist naloxone (Ch. 19)
 Respiratory depression: this may be profound and means that assisted ventilation is usually necessary during surgery when large doses have been used.
Respiratory depression: this may be profound and means that assisted ventilation is usually necessary during surgery when large doses have been used.
Inhalational anaesthetics
Inhalational anaesthetics are either volatile liquids, which must be vaporised before administration, or gases. All inhalational anaesthetics must be given with adequate oxygen (usually a minimum 25% of the inspired gas mixture) to avoid hypoxia during anaesthesia.
Volatile liquid anaesthetics such as sevoflurane can be used for both induction and maintenance of anaesthesia, or for maintenance following induction with an intravenous anaesthetic. Sevoflurane is widely used for induction as well as maintenance in children as it has a pleasant odour. With some volatile liquid anaesthetics, such as desflurane and isoflurane, irritation of the mucous membranes makes them less suitable for induction. Recovery is rapid after sevoflurane, since it is eliminated more quickly than isoflurane, and therefore early postoperative analgesia may be necessary.
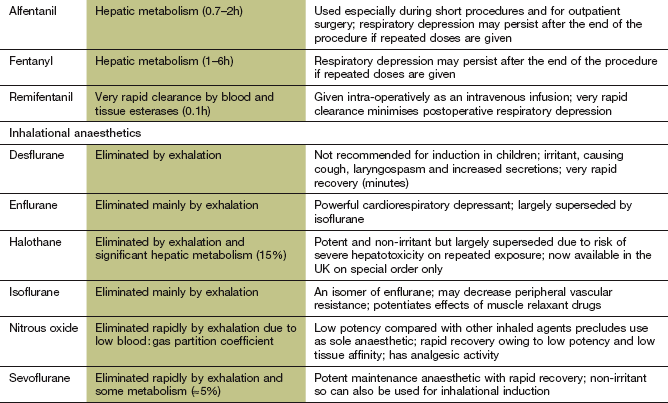
Nitrous oxide is a gaseous anaesthetic that is not sufficiently potent to be used alone (Table 17.5), but it has the advantage of producing analgesia (unlike the other inhalational anaesthetics). It is often used in combination with other anaesthetics, and reduces the required dose of the other agent. Nitrous oxide can only be used as the sole inhalational agent when combined with an intravenous opioid and a neuromuscular blocking drug (Ch. 27), but there is a risk of awareness during surgery. Nitrous oxide is also used in sub-anaesthetic doses for analgesia alone.
Table 17.5
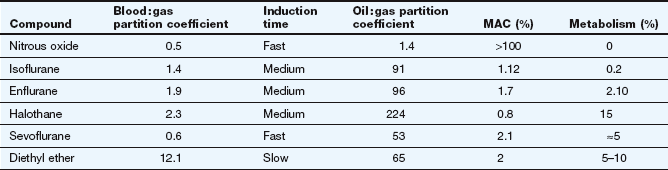
The blood : gas partition coefficient correlates closely with the time to induction when the drug is used as the sole anaesthetic. The oil : gas partition correlates with the potency of the anaesthetic, which correlates inversely with the minimum alveolar concentration (MAC) necessary for surgical anaesthesia. Nitrous oxide cannot produce anaesthesia alone so has a theoretical MAC of >100%. Metabolism is the percentage of drug eliminated as urinary metabolites, with the remainder eliminated mainly in the expired air. Halothane is no longer available in the UK, and diethyl ether is no longer used clinically but is included in the table for comparative purposes.
Pharmacokinetics
The concentration and duration of administration of inhaled anaesthetic required to give a sufficient concentration of the drug in the CNS for general anaesthesia will depend on the relationships shown in Figure 17.3 and Table 17.5. There are four factors to consider.
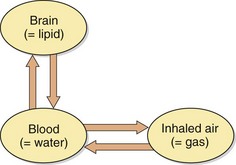
Fig. 17.3 Equilibration of inhalational general anaesthetics between air, blood and brain.
The concentration ratio between blood and air at equilibrium is estimated from in vivo studies of the blood : gas partition coefficient and correlates with the induction time of the drug (Table 17.5). The concentrations in brain and blood at equilibrium reflect the different affinities of the two body compartments for general anaesthetics. The brain : blood ratio is 1–3 : 1 for all commonly used anaesthetics. The concentration in the inspired air required to give the necessary concentration in brain membranes (minimum alveolar concentration; MAC) correlates inversely with the blood : gas partition coefficient which is an indication of the potency of the compound.
1. The rate of absorption across the alveolar membranes. This depends on both the concentration of drug in the inspired air and the rate of drug delivery; that is, the rate and depth of inspiration. These factors are most important if an inhaled agent is used for induction, but less significant once equilibrium has been established between the inhaled concentration and that in the brain. Lung conditions such as emphysema, which result in poor alveolar ventilation, will slow the induction of anaesthesia.
2. The rate at which the anaesthetic concentration in the blood reaches equilibrium with that in the inspired air, which is affected by the solubility of the anaesthetic in blood and in rapidly equilibrating tissues. A high solubility in blood compared with the brain will slow the attainment of equilibrium.
3. The cardiac output, which will determine circulation time and drug delivery to the brain. This is not usually a limiting factor.
4. The relative concentrations of the drug in the brain and blood at equilibrium. The rate of entry of drug into the brain is not limiting for lipid-soluble drugs such as anaesthetics. The rate-limiting step is the rate of delivery via the inhaled gas compared with the total amount in the body at equilibrium.
Anaesthetic potency of the volatile anaesthetics is measured as the minimum alveolar concentration (MAC) of an agent necessary to immobilise 50% of subjects exposed to a noxious stimulus (which in humans is a surgical skin incision). Therefore, MAC is the equivalent of the ED50 (the 50% effective dose) for other drugs (Ch. 1). The MAC for inhaled anaesthetics correlates inversely with the oil : gas partition coefficient, which reflects the ratio between the concentration in the lipid membranes of brain cells (oil) and the inhaled concentration (gas). A potent inhalational anaesthetic agent such as halothane has a high oil : gas ratio and this high lipid solubility means it has a low MAC (Table 17.5).
Another physicochemical property that affects the action of an inhaled anaesthetic agent is the blood : gas partition coefficient (or blood : gas ratio), which indicates the relative solubilities of the drug in blood and air. A high solubility in blood, and therefore in all rapidly equilibrating body tissues, means that a greater amount of the agent will need to be administered before its partial pressure in the blood equilibrates with that in the inspired air. The blood : gas ratio therefore correlates with the time to induction of anaesthesia. This conforms to the basic pharmacokinetic principle that compounds with a large apparent volume of distribution take longer to reach steady state during a constant rate of drug administration (Ch. 2). Table 17.5 shows that sevoflurane has a low blood : gas ratio and consequently a fast induction time, while induction with diethyl ether (which is no longer used clinically) is prolonged because of its high blood : gas ratio,
The major route of elimination of inhalational anaesthetics is via the airways in expired air. Factors that influence the duration of the induction phase, such as ventilation rate and the blood : gas partition coefficient, will also affect the time taken to eliminate the anaesthetic. Diethyl ether has a very long recovery time due its high blood : gas ratio (Table 17.5). The recovery time may also depend on the duration of inhalation, which can affect the extent to which the drug has entered slowly equilibrating tissues. Elimination from these tissues is also slow, which can maintain the plasma concentration of the drug and delay recovery. During recovery, the depth of anaesthesia reverses through the stages discussed above (Table 17.2) to consciousness; a rapid recovery which minimises stage II of anaesthesia (see Table 17.2) is beneficial.
General anaesthetics are also partly eliminated by metabolism, the extent of which depends on the time that the agent is retained in the body and is available to the metabolising enzymes. Thus, exhalation and metabolism can be regarded as alternative pathways of elimination, the proportions of which are determined largely by the volatility of the agent and its blood : gas partition coefficient (Table 17.5).
Unwanted effects
A number of unwanted effects are common to most clinically useful inhalational anaesthetics; however, each agent also has a unique profile of additional unwanted effects.
 Cardiovascular system. The volatile liquid anaesthetics depress myocardial contractility and predispose to bradycardia by interfering with transmembrane Ca2+ flux, with a resultant decrease in cardiac output and blood pressure. Isoflurane is less cardiodepressant, but may reduce blood pressure by arterial vasodilation. Nitrous oxide also has less depressant effect on the heart and circulation and its use in combination with other agents that depress the heart may permit reduction in their dosage. Inhalational anaesthetics often increase cerebral blood flow, which can exacerbate an elevated intracranial pressure. Arrhythmias occasionally occur with volatile liquid anaesthetics.
Cardiovascular system. The volatile liquid anaesthetics depress myocardial contractility and predispose to bradycardia by interfering with transmembrane Ca2+ flux, with a resultant decrease in cardiac output and blood pressure. Isoflurane is less cardiodepressant, but may reduce blood pressure by arterial vasodilation. Nitrous oxide also has less depressant effect on the heart and circulation and its use in combination with other agents that depress the heart may permit reduction in their dosage. Inhalational anaesthetics often increase cerebral blood flow, which can exacerbate an elevated intracranial pressure. Arrhythmias occasionally occur with volatile liquid anaesthetics.
 Respiratory system. All anaesthetic agents depress the response of the respiratory centre in the medulla to carbon dioxide and hypoxia. They also decrease tidal volume and increase respiratory rate. Desflurane and isoflurane are irritant to mucous membranes and can cause coughing, apnoea and laryngospasm if used for induction.
Respiratory system. All anaesthetic agents depress the response of the respiratory centre in the medulla to carbon dioxide and hypoxia. They also decrease tidal volume and increase respiratory rate. Desflurane and isoflurane are irritant to mucous membranes and can cause coughing, apnoea and laryngospasm if used for induction.
 Liver. Most agents decrease liver blood flow. Mild hepatic dysfunction, because of specific hepatic toxicity, is common after treatment with halothane. However, about 1 in 30 000 people will develop severe hepatic necrosis following the use of halothane, especially after repeat exposure within a short time interval. For this reason, halothane is only used after a careful anaesthetic history (especially in the preceding 3 months) and is avoided in those with a history of unexplained jaundice or pyrexia following exposure to halothane. Halothane is only available in the UK on special order. Hepatotoxicity is rare with other halogenated anaesthetics.
Liver. Most agents decrease liver blood flow. Mild hepatic dysfunction, because of specific hepatic toxicity, is common after treatment with halothane. However, about 1 in 30 000 people will develop severe hepatic necrosis following the use of halothane, especially after repeat exposure within a short time interval. For this reason, halothane is only used after a careful anaesthetic history (especially in the preceding 3 months) and is avoided in those with a history of unexplained jaundice or pyrexia following exposure to halothane. Halothane is only available in the UK on special order. Hepatotoxicity is rare with other halogenated anaesthetics.
 Uterus. Relaxation of the uterus may increase the risk of haemorrhage when anaesthesia is used in labour. Nitrous oxide has less effect on uterine muscle than the volatile liquid anaesthetics.
Uterus. Relaxation of the uterus may increase the risk of haemorrhage when anaesthesia is used in labour. Nitrous oxide has less effect on uterine muscle than the volatile liquid anaesthetics.
 Skeletal muscle. Most agents produce some muscle relaxation, which enhances the activity of neuromuscular blocking drugs (Ch. 27). With sevoflurane this may be sufficient to enable tracheal intubation without the use of a neuromuscular blocker.
Skeletal muscle. Most agents produce some muscle relaxation, which enhances the activity of neuromuscular blocking drugs (Ch. 27). With sevoflurane this may be sufficient to enable tracheal intubation without the use of a neuromuscular blocker.
 Chemoreceptor trigger zone. Inhalational anaesthetics trigger postoperative nausea and vomiting. This may be most pronounced with nitrous oxide.
Chemoreceptor trigger zone. Inhalational anaesthetics trigger postoperative nausea and vomiting. This may be most pronounced with nitrous oxide.
 Postoperative shivering. This occurs in up to 65% of those recovering from general anaesthesia. The aetiology is unclear.
Postoperative shivering. This occurs in up to 65% of those recovering from general anaesthesia. The aetiology is unclear.
 Malignant hyperthermia. This is a rare but potentially fatal complication of volatile liquid anaesthetics. It is genetically determined, and results from a defect in the ryanodine receptor (RyR1) that regulates release of Ca2+ from the sarcoplasmic reticulum in muscle cells (Ch. 5, Fig. 5.4). A sudden increase in intracellular Ca2+ produces tachycardia, unstable blood pressure, hypercapnoea, fever and hyperventilation, followed by hyperkalaemia and metabolic acidosis. Muscle rigidity may occur. Treatment is with dantrolene, which is an RyR1 receptor antagonist (Ch. 24).
Malignant hyperthermia. This is a rare but potentially fatal complication of volatile liquid anaesthetics. It is genetically determined, and results from a defect in the ryanodine receptor (RyR1) that regulates release of Ca2+ from the sarcoplasmic reticulum in muscle cells (Ch. 5, Fig. 5.4). A sudden increase in intracellular Ca2+ produces tachycardia, unstable blood pressure, hypercapnoea, fever and hyperventilation, followed by hyperkalaemia and metabolic acidosis. Muscle rigidity may occur. Treatment is with dantrolene, which is an RyR1 receptor antagonist (Ch. 24).
True/false questions
1. Inhalational anaesthetics may have their effect by interacting with specific receptors.
2. Inhalational anaesthetics are all gases.
3. Most inhalational anaesthetics are sulphur-containing compounds.
4. Halothane closely approaches the properties of an ideal inhalational anaesthetic.
5. The risk of hangover effects with inhalational anaesthetics increases if the operation is long.
6. The minimum alveolar concentration (MAC) of an inhalational anaesthetic required to produce surgical anaesthesia correlates inversely with the oil : gas partition coefficient of drug.
7. Nitrous oxide administered alone at a concentration of 50% in inspired air reaches the MAC necessary for surgical anaesthesia.
8. Nitrous oxide is frequently given with oxygen and a halogenated anaesthetic agent to produce effective surgical anaesthesia.
9. Isoflurane is metabolised as extensively as halothane.
10. The short duration of action of thiopental is due to its distribution into richly perfused tissues such as muscles.
11. The elimination half-life of thiopental is similar to the distribution half-life.
12. Propofol can be given alone by continuous intravenous infusion to maintain anaesthesia.
13. Accidental injection of thiopental into an artery can have serious consequences.
14. Ketamine is a sedative but is without analgesic action.
15. Fentanyl should not be administered concurrently with inhalational anaesthetics.
16. With modern anaesthetics the classical stages of anaesthesia induction are rarely seen.
17. When administering an inhalational anaesthetic, the excitement stage of anaesthesia may be prolonged if an intravenous anaesthetic is not given beforehand.
18. Most inhalational anaesthetics have a depressant effect on the cardiovascular system.
19. Inhalational anaesthetics increase the sensitivity of the respiratory centre to carbon dioxide and hypoxia.
20. Sevoflurane has the advantage of a fast onset of action and rapid elimination.
One-best-answer (OBA) question
1. Which the following is the most accurate statement concerning the pharmacology of agents used in anaesthesia?
A The respiratory medulla is particularly sensitive to the depressant action of general anaesthetics.
B The major route of elimination of most inhalational anaesthetics is via the liver.
C Metoclopramide is often given as a premedication before general anaesthesia.
D The intravenous opioid fentanyl should not be administered together with sevoflurane.
2. Which of the following is not an ideal property of an inhalational anaesthetic?
Case-based question
A 40-year-old woman is scheduled for a laparotomy because of an abdominal swelling. She has not had a previous operation and is otherwise healthy, with normal cardiovascular and respiratory function. She was premedicated with pethidine (meperidine) and atropine. The operation lasted 40 min. Refer to Ch.27 for information on neuromuscular junction blockers.
A Why is atropine little used nowadays as pre-anaesthetic medication in adults?
B Do the muscarinic receptor antagonists atropine and hyoscine have the same properties?
The woman was intubated after the administration of thiopental, fentanyl and suxamethonium (succinylcholine).
C Why has the routine use of suxamethonium to facilitate endotracheal intubation been reduced?
Following intubation, pancuronium and fentanyl were given and she was ventilated with nitrous oxide, enflurane and oxygen. An ovarian cyst was removed and the operation took 40 min.
D Is pancuronium the most suitable choice of muscle relaxant? What alternatives are available?
After the operation, she did not breathe spontaneously, despite the administration of neostigmine and glycopyrronium.
E What are the possible reasons for the apnoea and how could they be treated?
F Would mivacurium (a short-duration muscle relaxant) have been a preferable muscle relaxant to use in this patient?
G What is the reason for administering glycopyrronium with neostigmine at the end of the operation?
1. True. It is increasingly thought that general anaesthetics act at a number of excitatory and inhibitory receptors (Table 17.3).
2. False. Many inhalational anaesthetics are volatile liquids.
3. False. The main inhalational anaesthetics are halogenated compounds.
4. False. Halothane is potent but can cause cardiac arrhythmias, hepatotoxicity, hypotension and sensitisation of the heart to catecholamines.
5. True. In prolonged anaesthesia, lipid-soluble agents may accumulate in body fat stores and be slowly released after the operation.
6. True. The higher the oil : gas ratio, the lower the inhaled concentration of anaesthetic required to produce anaesthesia.
7. False. Even at concentrations higher than 50%, nitrous oxide is not potent enough to produce effective surgical anaesthesia on its own.
8. True. Nitrous oxide provides additional analgesic activity in combination with a fluorinated anaesthetic and oxygen.
9. False. Halothane undergoes substantial metabolism, but the other halogenated anaesthetics do not.
10. True. Rapid redistribution of thiopental from the CNS terminates its anaesthetic action.
11. False. The half-life of the thiopental redistribution is about 3 min, but its elimination from the body is much slower (half-life 3–8 h), partially accounting for the hangover effect seen with this drug.
12. True. Propofol is useful for short operations, but its rapid elimination and little hangover effect mean that it can also be given by continuous infusion for maintenance anaesthesia, such as in intensive care units.
13. True. Extravascular or intra-arterial injection of thiopental can be damaging due its high pH (approximately 9–10).
14. False. Ketamine does have analgesic action, unlike other available intravenous anaesthetics.
15. False. Fentanyl is short-acting with a rapid recovery and is increasingly used for intraoperative analgesia with inhalation anaesthetics.
16. True. The classical stages of anaesthetic induction were originally described following the use of slower-acting anaesthetics than those used today.
17. True. The intravenous agent is used to provide rapid induction of anaesthesia.
18. True. Most are negatively inotropic and they depress myocardial function by interfering with Ca2+ fluxes. Halothane also sensitises the heart to catecholamines and can lead to arrhythmias.
19. False. Inhalational anaesthetics reduce the ventilatory response to carbon dioxide and hypoxia and increase the arterial partial pressure of carbon dioxide.
20. True. Sevoflurane is rapid in onset and more rapidly eliminated than halothane or isoflurane.
OBA answers
1. Answer C is correct as an anti-emetic such as metoclopramide is often used to reduce the risk of vomiting caused by general anaesthetics and opioid analgesics. Medullary centres are relatively insensitive to anaesthetics (answer A). Inhalation anaesthetics are eliminated mainly by exhalation, not hepatic metabolism (answer B). Fentanyl is often used as an analgesic together with inhalational anaesthetics (answer D). With modern anaesthetic practice atropine is seldom needed to reduce bronchial and salivary secretions (answer E).
2. Answer E is correct as a high blood : gas ratio is associated with a long induction time, so it is not an ideal property of an inhalational anaesthetic. The other answers (A–D) are desirable properties of an ideal anaesthetic.
Case-based answers
A Atropine (and hyoscine) block muscarinic receptors, reducing bronchial and salivary secretions, but modern anaesthetics have less irritant effect, thus reducing this problem. Muscarinic antagonists can reduce the bradycardia caused by some inhalation anaesthetics and by suxamethonium.
B No. Atropine can cause CNS excitation, whereas hyoscine causes sedation and has anti-emetic properties.
C Relatively minor but frequent complications occur with suxamethonium, including bradycardia, postoperative myalgia, transient hyperkalaemia and raised intraocular, intracranial and intragastric pressures. A rare, but potentially fatal, complication is malignant hyperthermia. The competitive blocking drug rocuronium has a short duration of action and does not cause these problems.
D Pancuronium is probably not the ideal muscle relaxant to use as it can cause tachycardia and hypertension and is long-acting (Ch. 27). An alternative would be vecuronium, which has an intermediate duration of action and lacks cardiovascular effects. Rocuronium is more expensive but has a rapid onset and short duration of action and a low risk of cardiovascular effects.
E There are at least three possible reasons for the postoperative apnoea. (1) Opioid-induced apnoea caused by the use of pethidine followed by fentanyl, resulting in respiratory depression. The effect could be reversed by the opioid antagonist naloxone. (2) The dose of neostigmine given may have been insufficient to reverse the competitive blockade induced by long-acting pancuronium. (3) The woman could have a genetically determined deficiency of pseudocholinesterase (plasma cholinesterase, butyrylcholinesterase), found in about 1 in 2000 individuals, which would normally metabolise suxamethonium. Administration of neostigmine would exacerbate the respiratory suppression. Fresh frozen plasma (containing pseudocholinesterase) could be given.
F Although mivacurium is a short-acting muscle relaxant, it is metabolised by pseudocholinesterase and its effect would be greatly prolonged if the person has the genetic deficiency in this enzyme.
G Neostigmine inhibits acetylcholinesterase, increasing acetylcholine concentrations at cholinergic synapses. It partially or fully reverses the actions of competitive blockers of N2 receptors at the neuromuscular junction, but also enhances the activity of acetylcholine at muscarinic receptors, causing bradycardia and bronchoconstriction. Glycopyrronium is a selective muscarinic receptor antagonist used to prevent these muscarinic effects.
Brown, EN, Lydic, R, Schiff, ND. General anesthesia, sleep, and coma. N Engl J Med. 2010;363:2638–2650.
Campagna, JA, Miller, KW, Forman, SA. Mechanisms of actions of inhaled anaesthetics. N Engl J Med. 2003;348:2110–2124.
Chau, P-L. New insights into the molecular mechanisms of action of general anaesthetics. Br J Pharmacol. 2010;161:288–307.
Dodds, C. General anaesthesia: practical recommendations and recent advances. Drugs. 1999;58:453–467.
Fox, AJ, Rowbottam, DJ. Anaesthesia. BMJ. 1999;319:557–560.
Litman, RS, Rosenberg, H. Malignant hyperthermia. Update on susceptibility testing. JAMA. 2005;293:2918–2924.
Nathan, N, Odin, I. Induction of anaesthesia. A guide to drug choice. Drugs. 2007;67:701–723.
Solt, K, Forman, SA. Correlating the clinical actions and molecular mechanisms of general anesthetics. Curr Opin Anaesthesiol. 2007;20:300–306.