EVALUATION
• Patient will identify whether blood pressure reading is within normal limits for age.
• Patient with vascular insufficiency will describe precautions to take to avoid further circulatory deficiency.
• Patient will demonstrate self-monitoring of blood pressure.
To examine the peripheral vascular system, first assess the adequacy of blood flow to the extremities by measuring arterial pulses and inspecting the condition of the skin and nails. A systematic technique is useful, starting with the carotid arteries in the neck and moving down to the arteries in the upper and lower extremities. The wall of an artery is normally elastic, making it easily palpable. After the artery is depressed, it will spring back to shape when pressure is released. The arterial pulses to be palpated include the temporal, carotid, brachial, radial, femoral, popliteal, posterior tibial and dorsalis pedis. These pulses are palpated for rate, rhythm, strength and symmetry. An inequality may indicate localised obstruction or an abnormally positioned artery.
Each peripheral artery is examined using the distal pads of the second and third fingers. The thumb may help anchor the brachial and femoral artery. Firm pressure is applied without occluding the pulse. When it is difficult to find a pulse, it is helpful to vary pressure and feel all around the pulse site.
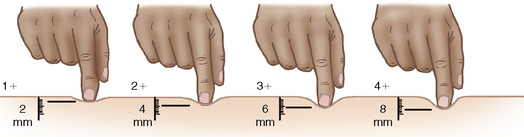
The strength of a pulse is a measurement of the force at which blood is ejected against the arterial wall. Some examiners use a scale rating from 0 to 4 for the strength of a pulse (Seidel and others, 2011):
0. Absent, not palpable
1. Pulse diminished, barely palpable
2. Easily palpable, normal pulse
3. Full pulse, increased
4. Strong, bounding pulse, cannot be obliterated.
CAROTID PULSES
When the left ventricle pumps blood into the aorta, pressure waves transmitted through the arterial system manifest as pulses palpable in arteries close to the skin or lying over bone. The pressure in carotid arteries provides a more accurate reflection of heart function than that in peripheral arteries because of the closeness to the aorta.
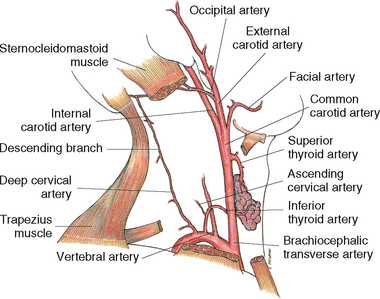
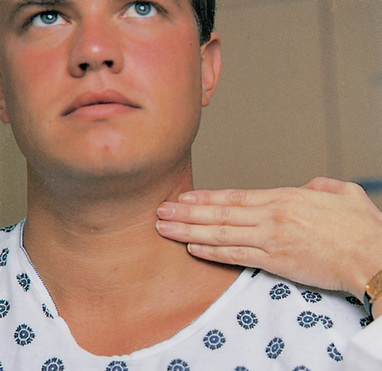
The carotid arteries supply oxygenated blood to the head and neck (Figure 27-24) and are protected by the overlying sternocleidomastoid muscle. To examine the carotid arteries, have the patient sit or lie supine with the head of the bed elevated 30 degrees. One carotid artery is examined at a time (Figure 27-25), as occlusion of both arteries could result in loss of consciousness due to inadequate cerebral circulation. In addition, vigorous palpation or massage is contraindicated because it stimulates the carotid sinus. The carotid sinus, located at the bifurcation of the common carotid arteries in the upper third of the neck, sends impulses along the vagus nerve. Carotid sinus stimulation can cause a reflex drop in heart rate and blood pressure, which causes syncope or circulatory arrest.
The neck is first inspected for obvious pulsation of the artery. The patient turns the head slightly away from the artery being examined. For palpation of the pulse, the patient turns the head slightly towards the side being examined. This manoeuvre relaxes the neck muscles for easier palpation. Slide the tips of your index and middle fingers around the medial edge of the sternocleidomastoid muscle.
The normal carotid pulse is localised rather than diffuse. A strong pulse, the carotid has a thrusting quality. No change occurs during inspiration or expiration. Rotation of the neck or a shift from a sitting to a supine position does not change the quality of the carotid artery pulsation. Both carotid arteries should be equal in pulse rate, rhythm and strength, and should be equally elastic. An abnormal artery may be described as hard, inelastic or calcified.
The carotid is one of the most commonly auscultated pulses. Auscultation is especially important for middle-aged adults, older adults or people suspected of having cerebrovascular disease manifested by carotid artery obstruction. When the lumen of a blood vessel is narrowed, its blood flow is disturbed causing a bruit to be heard using the bell of the stethoscope.
OTHER PULSES
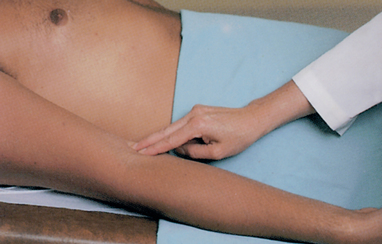
In the upper extremities the main artery is the brachial artery, which channels blood to the radial and ulnar arteries of the forearm and hand. To palpate the brachial pulse, find the groove between the biceps and triceps muscles above the elbow at the antecubital fossa (Figure 27-26). The artery runs along the medial side of the extended arm. Palpate the artery with the fingertips of the first three fingers in the muscle groove. If circulation in this artery becomes blocked, the circulation in the radial or ulnar arteries will be impaired and the hands will not receive adequate blood flow.
To locate pulses in the arm and hand, have the patient sit or lie down. The radial pulse is found along the radial side of the forearm, at the wrist. In a thin person, a groove is formed lateral to the flexor tendon of the wrist. The radial pulse can be felt with light palpation in the groove (Figure 27-27). The ulnar pulse is on the opposite side of the wrist and tends to feel less prominent than the radial pulse (Figure 27-28).
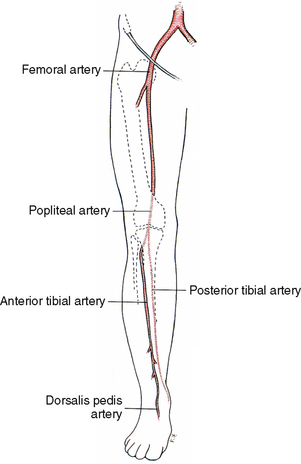
The femoral artery is the main artery in the leg, delivering blood to the popliteal, posterior tibial and dorsalis pedis arteries (Figure 27-29). It is one of the strongest arteries in an infant or small child. An interconnection between the posterior tibial and dorsalis pedis arteries guards against local arterial occlusion.
The femoral pulse is best found during deep palpation with the patient lying down with the inguinal area exposed (Figure 27-30). The femoral artery runs below the inguinal ligament, midway between the symphysis pubis and the anterosuperior iliac spine. Bimanual palpation is effective in obese patients. This technique differs from the previous description of bimanual palpation. Place the fingertips of both hands on opposite sides of the pulse site. A pulsatile sensation can be felt as the fingertips are pushed apart by arterial pulsation.
The popliteal pulse is found behind the knee and is difficult to locate. The patient should slightly flex the knee, with the foot resting on the bed, or assume a prone position with the knee slightly flexed and leg muscles relaxed (Figure 27-31). With the fingers of both hands, palpate deeply into the popliteal fossa, just lateral to the midline.
With the patient’s foot relaxed, locate the dorsalis pedis pulse. The artery runs along the top of the foot in line with the groove between the extensor tendons of the great toe and first toe (Figure 27-32). Locate the pulse by placing the fingertips between the great and first toe and slowly inching up the foot. This pulse may be congenitally absent.
The posterior tibial pulse is found on the inner side of each ankle (Figure 27-33). Place the fingers behind and below the medial malleolus. The artery is easily located with the foot relaxed and slightly extended.
DOPPLER ULTRASOUND STETHOSCOPES
Factors influencing the ability to assess a pulse include obesity, reduction in the heart’s stroke volume, diminished blood volume or arterial obstruction. An ultrasound stethoscope can amplify the sounds of a pulse wave. A thin layer of transmission gel is applied to the patient’s skin at the pulse site or directly onto the transducer tip of the probe. The volume control is then turned to ‘on’ and the tip of the probe placed at an angle of 45–90 degrees on the skin (Figure 27-34). The probe is moved until a pulsating ‘whooshing’ sound is heard, indicating the presence of arterial blood flow.
LOWER EXTREMITIES
During examination of the lower extremities, inspect skin and nail texture; hair distribution on the lower legs, feet and toes; the venous pattern; and scars, pigmentation or ulcers. Normally the lower limbs are symmetrical, warm and pink with presence of hair and intact skin. There is normally no evidence of oedema or tenderness on palpation. The absence of hair growth over the legs may indicate circulatory insufficiency, shaven lower legs, or in males from wearing tight-fitting socks.
PERIPHERAL VEINS
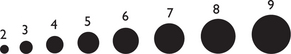
The status of the peripheral veins is assessed by asking the patient to assume sitting and standing positions. Assessment includes inspection and palpation for varicosities, peripheral oedema and phlebitis. Varicosities are superficial veins that become dilated, especially when the legs are in a dependent position. They are common in older adults and people who spend a lot of time standing (e.g. restaurant staff, nurses) because the veins normally fibrose, dilate and stretch. To assess for pitting oedema, use a thumb to press firmly for 5 seconds and then release over the medial malleolus or the shins. A depression left in the skin indicates oedema with the severity characterised by grading 1+ to 4+ (Figure 27-35).
Abnormal findings of the vascular system
Venous congestion causes tissue oedema, indicating an inadequate circulatory flow back to the heart. Dependent oedema of the feet and ankles can be a sign of venous insufficiency and right-sided heart failure. Chronic recurring ulcers of the feet or lower legs are a serious sign of circulatory insufficiency and require medical intervention. If an arterial occlusion is present, the patient has signs resulting from an absence of blood flow (Table 27-19). The six Ps—pain, pallor, pulselessness, polar (cold temperature), paraesthesias and paralysis—characterise an occlusion (Sieggreen, 2006). Signs such as these require urgent medical intervention.
TABLE 27-19 SIGNS OF VENOUS AND ARTERIAL INSUFFICIENCY
| ASSESSMENT CRITERION |
VENOUS |
ARTERIAL |
| Colour |
Normal or cyanotic |
Pale; worsened by elevation of extremity; dusky red when extremity is lowered |
| Temperature |
Normal |
Cool (blood flow blocked to extremity) |
| Pulse |
Normal |
Decreased or absent |
| Oedema |
Often marked |
Absent or mild |
| Skin changes |
Brown pigmentation around ankles |
Thin, shiny skin; decreased hair growth; thickened nails |
Varicosities in the anterior or medial part of the thigh and the posterolateral part of the calf are abnormal. Diminished or unequal carotid pulsations can indicate atherosclerosis or aortic arch disease.
Phlebitis is an inflammation of a vein that occurs commonly after trauma to the vessel wall, infection, prolonged immobilisation and prolonged insertion of intravenous catheters. To assess for phlebitis, inspect the calves for localised redness, tenderness and swelling over vein sites.
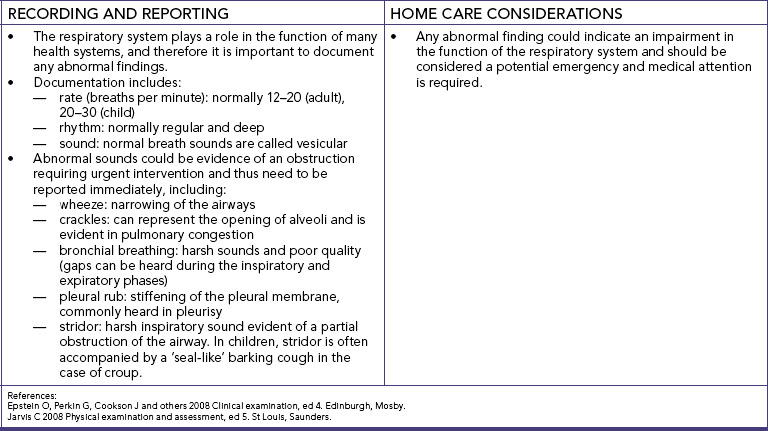
Respiratory system
Respiratory assessment
GENERAL INSPECTION
Once again, note general appearance of the patient and observe general responses to activity. The condition of the skin, mucosa, nail beds, lips, nose, throat and tracheal position offers useful data about the patient’s respiratory status. First examine the face, looking at the colour of the skin and mucosa. Inspect the nose for symmetry of nares, presence of discharge and evidence of nasal flaring. Inspect the lips for colour and symmetry. Inspect the nails for shape and colour.
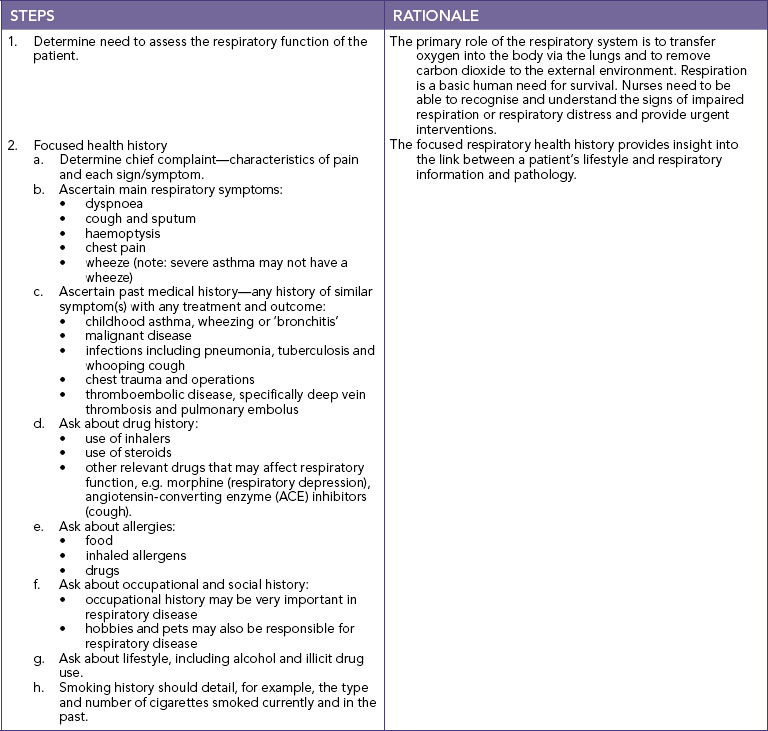
SKILL 27-4 Assessment of the respiratory system
DELEGATION CONSIDERATIONS
Assessment of the respiratory system may be undertaken by enrolled nurses under the guidance of the registered nurse.
• Ensure review of the anatomy and physiology of the respiratory system for risk factors.
• Ensure review of the anatomical landmarks of the chest wall.
• Ensure hand hygiene is performed and personal protective equipment worn when appropriate.
EQUIPMENT
• Stethoscope
• Pen
• Documentation
• Watch (with a second hand)
• Portable pulse oximeter
NOSE, SINUSES AND OROPHARYNX
Inspection and palpation are used to assess the nose and sinuses. The patient sits during the examination. When inspecting the external nose, observe for shape, size, skin, colour and the presence of deformity or inflammation. The nose is normally smooth and symmetrical and the same colour as the face. Note any tenderness, masses or underlying deviations. Nasal structures are usually firm and stable. Air normally passes freely through the nose as a person breathes. To assess patency of the nares, place a finger on the side of the patient’s nose and occlude one naris. The patient is asked to breathe with the mouth closed. The examination is repeated for the other naris.
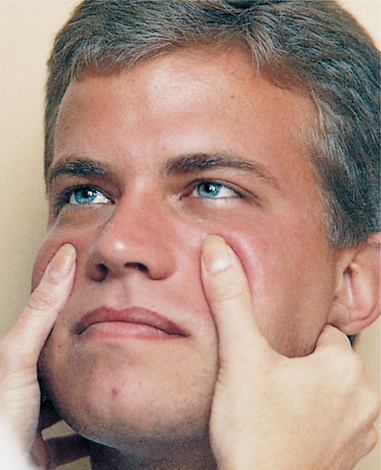
Examination of the sinuses involves palpation. The most effective way to assess for tenderness is by externally palpating the frontal and maxillary facial areas (Figure 27-36). The frontal sinus is palpated by exerting pressure with the thumb up and under the patient’s eye. Gentle, upward pressure elicits tenderness easily if sinus irritation is present and reveals the severity of sinus irritation. Pressure should not be applied to the eyes. Box 27-17 describes teaching guidelines during nose and sinus assessment. The presence of a nasogastric or nasopharyngeal tube entails routine checking for naris skin breakdown (excoriation), characterised by redness and sloughing of the skin. Table 27-20 lists components of the nursing history.
BOX 27-17 CLIENT TEACHING DURING NOSE AND SINUS ASSESSMENT
OBJECTIVES
• Patient will safely use over-the-counter nasal sprays.
• Parents will take proper measures to stop a child’s nosebleed.
• Older adult will take safety precautions with loss of olfaction.
TEACHING STRATEGIES
• Caution patient against overuse of over-the-counter nasal sprays, which can lead to ‘rebound’ effect, causing excess nasal congestion.
• Instruct parents on care of a child with nosebleeds: have child sit up and lean forward to avoid aspiration of blood, apply pressure to the anterior nose with the thumb and forefinger as the child breathes through the mouth, and apply ice or a cold cloth to the bridge of the nose if pressure fails to stop bleeding.
• Instruct older adults to install smoke detectors on each floor of their home.
• Instruct older adults to always check dated labels on food to ensure against spoilage.
EVALUATION
• Patient will explain appropriate use of over-the-counter nasal sprays.
• Parents will demonstrate and describe technique for stopping a child’s nosebleed.
TABLE 27-20 NURSING HISTORY FOR NOSE AND SINUS ASSESSMENT
| ASSESSMENT QUESTIONS |
RATIONALE |
| Have you experienced a knock to your nose? |
Trauma can cause septal deviation and asymmetry of external nose |
| Do you have a history of allergies, nasal discharge, epistaxis (nose bleeds) or postnasal drip? |
History is useful in determining source or nature of nasal and sinus drainage |
| Have you experienced nasal discharge in the past? Can you describe the colour, amount, odour, duration of the discharge? Did you have any associated symptoms (e.g. sneezing, nasal congestion, obstruction or mouth-breathing)? |
Can help to rule out presence of infection, allergy or drug use |
| Have you experienced nosebleeds? Describe the frequency, amount of bleeding, treatment. Was there any difficulty stopping the bleeding? |
Characteristics may reveal trauma, medication use or excessive dryness as causative factors |
| Do you use nasal spray or drops? |
Overuse of over-the-counter nasal preparations can cause physical change in mucosa |
| Do you snore at night? Do you have difficulty breathing? |
Difficulty with breathing or snoring may indicate septal deviation or obstruction |
THORAX AND LUNGS
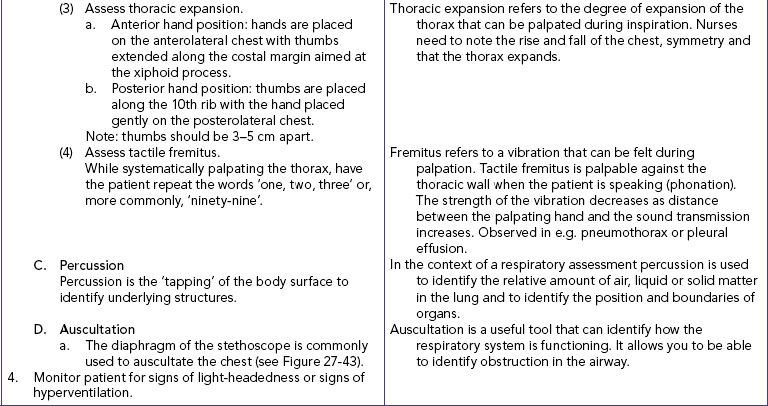
Examination of the lungs and thorax requires the patient to be in an upright or semi-Fowler’s position and to be undressed to the waist. Good lighting is essential. The trachea is palpated to identify if it is in the midline position.
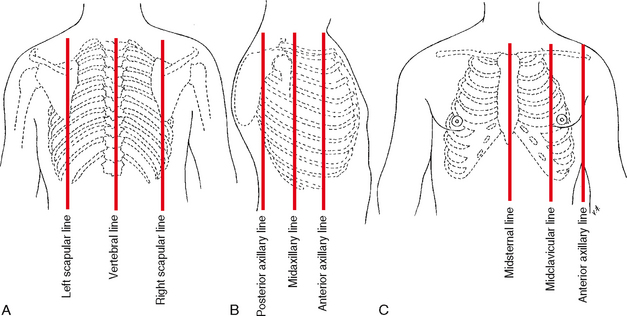
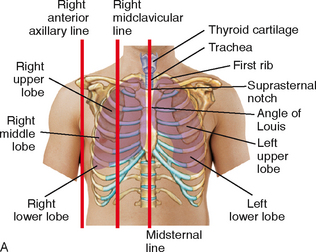
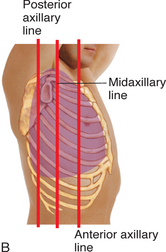
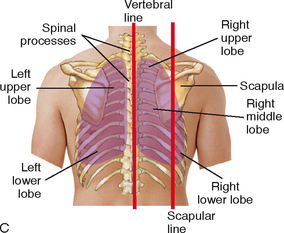
RESPIRATORY ASSESSMENT LANDMARKS
Before assessing the thorax and lungs, identify the landmarks of the chest (Figure 27-37). By knowing the position of underlying organs in relation to the landmarks, you can anticipate where to palpate or auscultate the chest wall. To begin, locate the angle of Louis at the manubriosternal junction. The angle is a visible and palpable angulation of the sternum and is the point at which the second rib articulates with the sternum. Count the ribs and intercostal spaces (between the ribs) from this point. The number of each intercostal space corresponds with that of the rib just above it. The spinous process of the third thoracic vertebra and the fourth, fifth and sixth ribs help to locate the lung’s lobes laterally. The lower lobes project laterally and anteriorly (Figure 27-38). Posteriorly, the tip or inferior margin of the scapula lies approximately at the level of the seventh rib (Figure 27-39). After identifying the seventh rib, count upwards to locate the third thoracic vertebra and align it with the inner borders of the scapula to locate the posterior lobes. During the examination keep a mental image of the location of the lobes of the lung and the position of each rib (Figure 27-40). Locating the position of each rib is critical to identifying the lobe of the lung being assessed.
POSTERIOR THORAX
First inspect the shape and symmetry of the patient’s chest from the back and front. The anteroposterior (AP) diameter is noted. Normally the chest contour is symmetrical, with the AP diameter a third to a half of the transverse, or side-to-side, diameter. Infants have an almost round shape. Ageing and chronic lung disease are characterised by a barrel-shaped chest (AP diameter equals transverse diameter).
Standing at a midline position behind the patient, examine the skin and characteristics of the chest wall; position of the spine (straight without lateral deviation), position of the scapulae (symmetrical and closely attached to the thoracic wall), the slope of the ribs (across and down). Note the movement of the thorax as a whole (regular expansion and relaxation with equality of movement). Assess for abnormalities such as retraction of the intercostal spaces during inspiration, and bulging of the intercostal spaces during expiration.
The thoracic muscles and skeleton are palpated for lumps, masses, pulsations and unusual movement. Note pain or tenderness. If a suspicious mass or swollen area is detected, it is lightly palpated for size, shape and the typical qualities of a lesion. Care with palpation is important because fractured rib fragments could be displaced against vital organs. Normally there is no pain or tenderness on palpation, the scapulae are symmetrical and the chest wall is stable.
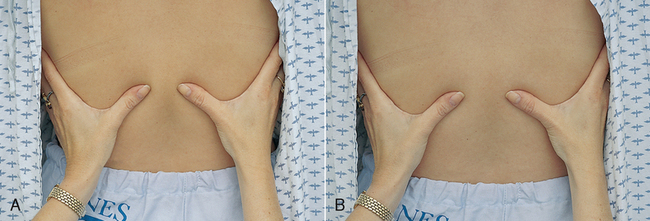
To measure chest excursion or depth of breathing, stand behind the patient and place the thumbs along the spinal processes at the 10th rib, with the palms lightly contacting the posterolateral surfaces. The thumbs should be about 5 cm apart pointing towards the spine, with fingers pointing laterally (Figure 27-41). The hands are pressed towards the spine so that a small skin fold appears between the thumbs. The patient is instructed to take a deep breath after exhaling. Note the movement of your thumbs. Chest excursion should be symmetrical, separating the thumbs 3–5 cm. Normally breathing is pain-free and does not produce a cough.
Auscultation assesses the movement of air through the tracheobronchial tree and detects mucus or obstructed airways. The diaphragm of the stethoscope is placed firmly on the skin, over the posterior chest wall between the ribs (Figure 27-42). The patient sits upright (if possible), folds the arms in front of the chest and keeps the head bent forwards while taking slow, deep breaths with the mouth slightly open. Listen to an entire inspiration and expiration at each position of the stethoscope. If sounds are faint, as in the obese patient, the patient should be asked to breathe harder and faster. Breath sounds are much louder in children because of the thinness of the chest wall. In children, the bell works best because the chest is small.
Auscultate for normal breath sounds and abnormal or adventitious sounds. Normal breath sounds differ in character, depending on the area of the lungs being auscultated. Sounds normally heard over the posterior thorax include bronchovesicular and vesicular sounds (Figure 27-43 and Table 27-21). The location and characteristics of the sounds should be noted, as should the absence of breath sounds (found in patients with collapsed or surgically removed lobes).
TABLE 27-21 NORMAL BREATH SOUNDS
| DESCRIPTION |
LOCATION |
ORIGIN |
| VESICULAR |
| Vesicular sounds are soft, breezy and low-pitched. Inspiratory phase is three times longer than expiratory phase |
Best heard over lung’s periphery (except over scapula) |
Created by air moving through smaller airways |
| BRONCHOVESICULAR |
| Bronchovesicular sounds are blowing sounds that are medium-pitched and of medium intensity. Inspiratory phase is equal to expiratory phase |
Best heard posteriorly between scapulae and anteriorly over bronchioles lateral to sternum at first and second intercostal spaces |
Created by air moving through large airways |
| BRONCHIAL |
| Bronchial sounds are loud and high-pitched with hollow quality. Expiration lasts longer than inspiration (2 : 1 ratio) |
Best heard over trachea |
Created by air moving through trachea close to chest wall |
LATERAL THORAX
Extend the assessment of the posterior thorax to the lateral sides of the chest. The patient is asked to raise the arms, which improves access to lateral thoracic structures. Inspection, palpation and auscultation skills are used to methodically examine the lateral thorax (see Figure 27-43). Excursion cannot be assessed laterally. Normally, breath sounds in the lateral thorax are vesicular.
ANTERIOR THORAX
The anterior thorax is inspected for the same features as the posterior thorax. The patient sits or lies down with the head elevated. Observe the accessory muscles of breathing: sternocleidomastoid, trapezius and abdominal muscles. The accessory muscles move little with normal passive breathing. When a patient requires effort to breathe as a result of strenuous exercise or disease (e.g. chronic obstructive pulmonary disease), the accessory muscles and abdominal muscles contract. Some patients produce a grunting sound.
Observe the width of the costal angle, which is usually larger than 90 degrees between the two costal margins. Observe the breathing pattern. Normal breathing is quiet and barely audible near the open mouth. Respiratory rate and rhythm are more often assessed anteriorly.
Palpate the anterior thoracic muscles and skeleton for lumps, masses, tenderness or unusual movement. The sternum and xiphoid are relatively inflexible. To measure chest excursion anteriorly, place the hands over each lateral rib cage, with the thumbs approximately 2.5 cm apart and angled along each costal margin (Figure 27-44). The thumbs are pushed towards the midline to create a fold of skin between the thumbs. As the patient inhales deeply, the thumbs should normally separate approximately 2.5–5 cm, with each side expanding equally (Figure 27-44).
Special attention should be paid to the lower lobes, where mucus commonly gathers. Bronchovesicular and vesicular sounds are heard above and below the clavicles and along the lung periphery. An additional normal breath sound, the bronchial sound, can be heard over the trachea. It is loud, high-pitched and hollow-sounding, with expiration lasting longer than inspiration (2 : 1 ratio).
Abnormal findings of the respiratory system
Recent trauma may have caused oedema and discolouration of the skin of the nose. If swelling or deformities exist, gently palpate the ridge and soft tissue of the nose by placing one finger on each side of the nasal arch and moving the fingers from the nasal bridge to the tip.
A sinus infection results in yellowish or greenish discharge from the nose. Habitual use of intranasal cocaine and opioids can cause puffiness and increased vascularity of the nasal mucosa (Brand and others, 2008).
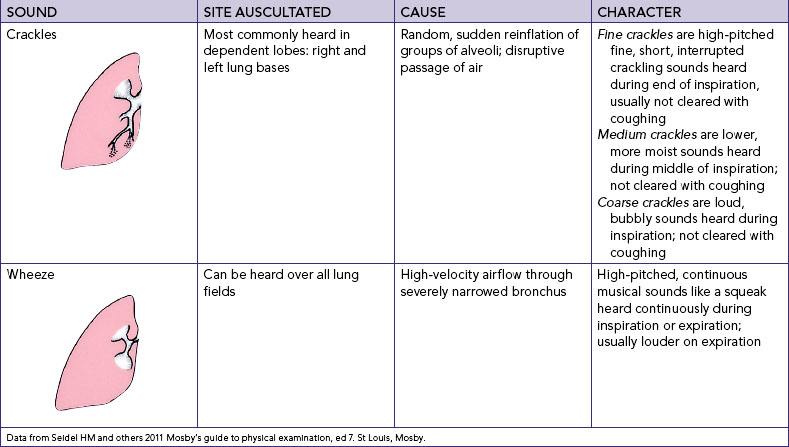
Patients with respiratory diseases, at risk of respiratory complications or with chest pain who cannot fully expand the lungs suffer symptoms such as cough, increased sputum production and dyspnoea. These patients require accurate physical assessment of the thorax and lungs to identify appropriate nursing interventions (Box 27-18). This assessment requires review of the ventilatory and respiratory functions of the lungs and an analysis of the nursing history for lung assessment (see Table 27-22). Reduced chest excursion may be caused by pain, postural deformity or fatigue. In the older adult, chest movement declines because of costal cartilage calcification and respiratory muscle atrophy. Abnormal sounds result from air passing through moisture, mucus or narrowed airways; from alveoli suddenly re-inflating; or from an inflammation between the lung’s pleural linings. Adventitious or added sounds often occur superimposed over normal sounds. The two types of adventitious sounds which beginning nurses should be able to detect are crackles and wheezes. Each sound is caused by a specific entity and is characterised by typical auditory features (Table 27-23).
BOX 27-18 CLIENT TEACHING DURING LUNG ASSESSMENT
OBJECTIVES
• Patient will describe warning signs of lung disease.
• Older adult will receive influenza and pneumonia vaccines annually.
• Patient with chronic obstructive pulmonary disease (COPD) will clear airways more effectively and report less shortness of breath.
TEACHING STRATEGIES
• Explain risk factors for chronic lung disease and lung cancer, including cigarette smoking, history of smoking for over 20 years, exposure to environmental pollution and radiation exposure from occupational, medical and environmental sources. Residential radon exposure may also increase risk, especially in cigarette smokers. Exposure to sidestream cigarette smoke increases risk for non-smokers.
• Discuss warning signs of lung cancer, such as a persistent cough, sputum streaked with blood, chest pains and recurrent attacks of pneumonia or bronchitis.
• Counsel older adult on benefits of receiving annual influenza and pneumonia vaccinations because of a greater susceptibility to respiratory infection.
• Teach patient with COPD coughing and pursed-lip breathing exercises.
• Persons at risk of tuberculosis who visit clinics or healthcare centres should be referred for skin testing.
EVALUATION
• Patient will describe risk factors for lung disease and cancer.
• Patient will identify any known risks for cancer.
• Patient will name warning signs for cancer.
• Elderly patients and those with chronic lung conditions will have received influenza and pneumonia immunisation.
• Patient will accurately perform breathing and coughing exercises.
TABLE 27-22 NURSING HISTORY FOR LUNG ASSESSMENT
| ASSESSMENT QUESTIONS |
RATIONALE |
| Do you have a persistent cough (productive or non-productive)? Have you had any chest pain, shortness of breath, shortness of breath at night, difficulty breathing during activity or at rest, poor activity tolerance or recurrent attacks of pneumonia or bronchitis? How much sputum do you cough up? |
Symptoms of respiratory alterations may help nurse localise objective physical findings. (Warning signals for lung cancer are in italic type) |
| Has there been any blood in your sputum? Have you had any unexplained weight loss, fatigue, night sweats or fever? |
These are risk factors for both tuberculosis and HIV infection |
| Are you allergic to pollens, dust or other airborne irritants or to foods, drugs or chemical substances? |
Symptoms such as choking feeling, bronchospasm with respiratory stridor, wheezes on auscultation, and dyspnoea may be caused by allergic response |
| Assess history of tobacco or marijuana use, including type of tobacco, duration and amount (pack years = number of years smoking × number of packets per day), age started and efforts to quit |
Smoking is a risk factor for lung cancer, heart disease and emphysema or bronchitis. Cigarette smoking accounts for a significant percentage of all cancer deaths. The medical practitioner will diagnose the disease |
| Does patient have history of chronic hoarseness? |
Hoarseness may indicate laryngeal disorder or abuse of cocaine or opioids (sniffing) |
| Review family history for cancer, tuberculosis, allergies or chronic obstructive pulmonary disease |
These conditions place patient at risk of lung disease |
| Review history for known or suspected HIV infection, substance abuse, proximity to a patient with infectious tuberculosis (TB), in a household setting, being homeless, being in prison or working in a hospital |
These are risk factors for tuberculosis (WHO, 2011) |
| Determine whether patient works in environment containing pollutants (e.g. asbestos, arsenic, coal dust) or requiring exposure to radiation. Does patient have exposure to sidestream cigarette smoke? |
These risk factors increase chance of various lung diseases. Knowledge of environmental factors will assist you to focus health teaching |
• CRITICAL THINKING
Part of Mrs Marsaja’s treatment for chest pain requires her to rest in bed. She commences ambulation again, under supervision. You note that she becomes breathless easily with exertion and she tells you she does not feel very well.
What subjective and objective cardiac and respiratory data will you collect in this situation?
Cognitive–perceptual pattern
The neurological system is responsible for many functions, including initiation and coordination of movement, reception and perception of sensory stimuli, organisation of thought processes, control of speech, and storage of memory. The cerebral cortex controls and integrates intellectual and emotional functioning. A close relationship exists between the neurological system and all other body systems. An assessment of cognition and perception will provide you with information about your patient’s capacity to think, sense, perceive and move.
An assessment of cognition and perception includes mental state, sensation and perception, and motor function to detect any changes that may interfere with the person’s ability to meet functional needs. Subjective assessment includes the patient’s description of the adequacy of the special senses (vision, hearing, touch, taste and smell), motor function and any specific symptoms such as visual or auditory hallucinations or illusions, headaches or tremors. Questions are also asked about medication and medical diagnoses (e.g. hypertension, diabetes, epilepsy, liver or renal disease). Physical assessment is focused on examination of the person’s mental state, special-sense organs to detect any dysfunction and ability to move voluntarily, deliberately and in a smooth and coordinated way.
To make good use of your time, it is wise to integrate assessment of cognition and perception with other parts of the physical examination. For example, conscious state and mental and emotional status is observed as the nursing history is collected. Many variables must be considered when deciding the extent of the examination, including a review of nursing history findings (Table 27-24). A patient’s level of consciousness influences the ability to follow directions. A person’s general physical status influences tolerance to assessment. For example, an inability to walk makes a detailed assessment of coordination impossible. The patient’s chief symptom(s) also help determine the need for a thorough neurological assessment. If the patient reports headache or a recent loss of function in an extremity, a complete neurological assessment is required. If a patient demonstrates a change in conscious state, this could indicate a medical emergency requiring prompt intervention.
TABLE 27-24 NURSING HISTORY FOR NEUROLOGICAL ASSESSMENT
| ASSESSMENT QUESTIONS |
RATIONALE |
Have you experienced seizures/convulsions?
Can you describe the sequence of events (aura, fall to ground, motor activity, loss of consciousness)?
What treatment have you received for the seizures?
|
Seizure activity often originates from central nervous system alteration. Characteristics of seizure help determine its origin |
| Do you have headaches, tremors, dizziness, vertigo, numbness or tingling of body part, visual changes, weakness, pain or changes in speech? |
These symptoms frequently originate from alterations in central nervous system or peripheral nervous system function. Identification of specific patterns may help diagnose pathological condition |
| Discuss with spouse, family members or friends any recent changes in patient’s behaviour (e.g. increased irritability, mood swings, memory loss, change in energy level) |
Behavioural changes may result from intracranial pathological states |
| What medications are you taking? Are you taking any non-prescription drugs? |
Analgesics, antipsychotics, antidepressants or nervous system stimulants can alter level of consciousness or cause behavioural changes |
| Assess patient’s use of alcohol, sedative-hypnotics or recreational drugs |
Abuse can cause tremors, ataxia and changes in peripheral nerve function |
| If an older patient displays sudden acute confusion (delirium), review history for drug toxicity (anticholinergics, diuretics, digoxin, cimetidine, sedatives, antihypertensives, antiarrhythmics), serious infections, metabolic disturbances, heart failure and severe anaemia |
One of the most common mental disorders in older persons.
Condition is always potentially reversible
|
| Review past history for head or spinal cord injury, hypertension or psychiatric disorders |
Factors may cause neurological symptoms or behavioural changes to develop, focusing assessment on possible cause |
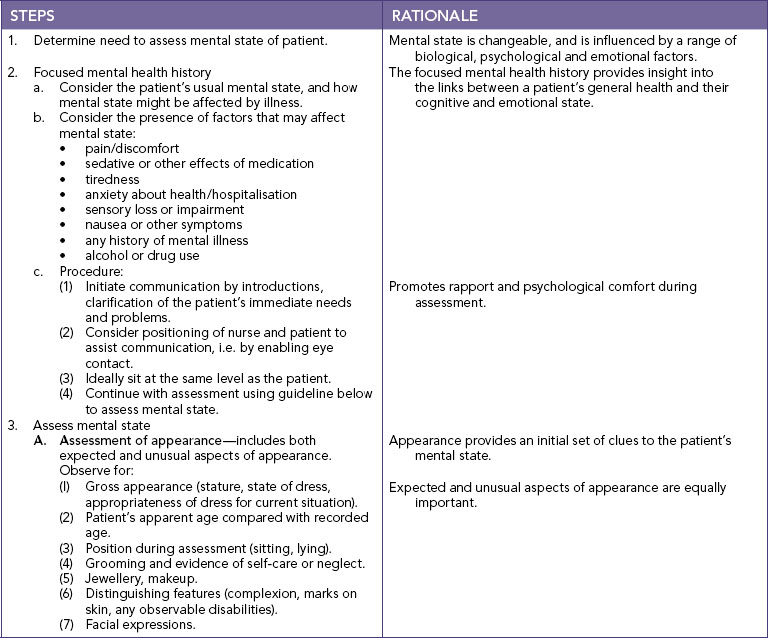
Mental and emotional status
To ensure an objective cognitive assessment, find out about the patient’s cultural and educational background, values, beliefs and previous experiences. Such factors influence the patient’s response to questions. A great deal can be learned about mental capacities and emotional state by simply interacting with the patient. Throughout your nursing care activities you will be gathering information about the way your patient behaves and thinks, and the appropriateness of emotions and ideas. Assessment of mental and emotional status includes collecting information to determine the ability to think, understand and interact with the environment. A mental status assessment is usually divided into four main areas: appearance, behaviour, cognition and thought processes. In children the mental status assessment covers behavioural, cognitive and psychosocial development and how the child is coping with their environment.
Ask questions about the patient’s educational level, their perception of memory, ability to read and write and ability to learn. Ask whether there is a history of anxiety, depression or changes in mood. When assessing a child’s mental and emotional status, it is important to ask the parent(s) about the health of the mother in pregnancy, the process of birth and achievement of developmental milestones. It is also important to hear the parent’s perception of the child’s behaviour. An alteration in mental or emotional status may reflect a disturbance in cerebral functioning. Primary brain disorders, medication and metabolic changes are examples of factors that may change cerebral function.
Behaviour and appearance
Behaviour, moods, hygiene, grooming and choice of dress and level of consciousness reveal pertinent information about mental status. It is important to note mannerisms and actions during the entire physical assessment, including non-verbal and verbal behaviour. Does the patient respond appropriately to directions? Does the patient’s mood vary with no apparent cause? Does the patient show concern about appearance? Is the patient’s hair clean and neatly groomed, and are the nails trim and clean? The patient should behave in a manner expressing concern and interest in the examination. The patient’s facial appearance and mood should be appropriate to the situation. The patient should make eye contact with you and express appropriate feelings that correspond to the situation. Choice and fit of clothing may reflect socioeconomic background or personal taste rather than deficiency in self-concept or self-care, however. Avoid making hasty judgments and consider the appropriateness of clothing for the weather. Older adults may neglect their appearance because of a lack of energy or finances, or physical incapacity or reduced vision.
SKILL 27-5 Mental state assessment
Mental state assessment is a key nursing skill and provides a structured set of observations about the patient’s cognitive and emotional state at a specific point in time.
DELEGATION CONSIDERATIONS
The mental state assessment can be conducted without supervision. Most aspects of the mental state assessment can be carried out as part of routine nursing care, i.e. they can be integrated into other nursing procedures.
Before proceeding:
• review the categories of mental state assessment, and communication skills
• revise the structured format for mental state assessment (BATOMI) (see Box 44-4)
EQUIPMENT
• Mental health assessment uses communication skills and therapeutic use of self
• Consider privacy and appropriateness of setting
Use of language, vocabulary and non-verbal communication should be appropriate to the occasion. The ability to understand spoken or written words and to express the self through writing, words or gestures is a function of the cerebral cortex. The patient’s voice is assessed for inflection, tone and manner of speech. The patient’s voice should have inflections, be clear and strong and increase in volume appropriately. Speech should be fluent. Ineffective communication (e.g. omission or addition of letters and words, misuse of words, hesitations) is indicative of aphasia, possibly resulting from an injury to the cerebral cortex. Normally a patient names objects correctly, follows commands and reads sentences correctly.
Cognition and thought processes
The level of consciousness exists along a continuum from full waking, alertness and cooperation through to unresponsiveness to any form of external stimuli. A fully conscious patient responds to questions spontaneously. As consciousness lowers, a patient may show irritability, a shortened attention span or an unwillingness to cooperate. To avoid ambiguity in the assessment of the level of consciousness, the Glasgow Coma Scale (GCS) measures consciousness using an objective numerical scale (Table 27-25). Caution is needed in using the scale with patients who have sensory losses (e.g. vision or hearing or where English is a second language). As consciousness deteriorates, a patient becomes disoriented to name, time and place. Ask short, to-the-point questions regarding information that the patient knows (e.g. ‘Tell me your name’, ‘What’s the name of this place?’ and ‘What day is this?’). The patient’s ability to understand and answer questions has a direct effect on your ability to perform a complete examination.
TABLE 27-25 GLASGOW COMA SCALE
| ACTION |
RESPONSE |
SCORE |
| Eye opening |
Spontaneously |
4 |
| To speech |
3 |
| To pain |
2 |
| No response |
1 |
| Best verbal response |
Oriented |
5 |
| Confused |
4 |
| Inappropriate words |
3 |
| Incomprehensible sounds |
2 |
| No response |
1 |
| Best motor response |
Obeys commands |
6 |
| Localises to pain |
5 |
| Flexion withdrawal |
4 |
| Abnormal flexion |
3 |
| Abnormal extension |
2 |
| No response |
1 |
| Total score |
|
15 |
A patient may be unable to follow simple commands, such as ‘Squeeze my finger’. At this lowered level of consciousness the patient is often responsive only to painful stimuli. Test the patient by using a painful stimulus such as the trapezium squeeze. A patient with serious neurological impairment exhibits abnormal posturing in response to such stimuli. A flaccid response indicates the absence of muscle tone in the extremities and severe brain injury. The GCS allows an evaluation of a patient’s neurological status over time. The higher the score, the more normal or improved the level of functioning.
For the conscious and alert patient, testing of intellectual function includes memory (recent, immediate and past), knowledge, abstract thinking, association and judgment. Each aspect of intellectual function is tested through a specific technique. As cultural and educational background influences the ability to respond to test questions, do not ask questions related to concepts or ideas with which the patient is unfamiliar. Any hearing loss should be recognised in the interpretation of findings. Good communication techniques are necessary throughout the examination to ensure the patient clearly understands all directions and testing.
A problem with memory becomes apparent during the nursing history. To assess past memory, the patient is asked to recall mother’s maiden name, a birthday or a special date. It is best to ask open-ended questions rather than simple yes/no questions. A patient should have immediate recall of such information. To assess immediate recall, the patient repeats a series of numbers (e.g. 7, 4, 1) in order presented or in reverse order. Gradually increase the number of digits (e.g. 7, 4, 1, 8, 6) until the patient fails to repeat the digits correctly. Normally an individual is able to repeat a series of 5 to 8 digits forwards and 4 to 6 digits backwards. To test recent memory, say clearly and slowly the name of three unrelated objects. After saying all three ask the patient to repeat them. This is continued until the patient is successful. Then, later in the assessment, ask the patient to say the three words again. The patient should be able to identify the three words. Another test for recent memory involves asking the patient to recall events occurring during the same day (e.g. what was eaten for breakfast). Information may need to be validated with a family member. Confabulation will be evidence of the patient compensating for memory loss by using fictional information.
Knowledge can be assessed by asking patients what they know about their illnesses or the reason for seeking healthcare. By assessing knowledge, you can determine the patient’s ability to learn or understand.
Interpreting abstract ideas or concepts reflects the capacity for abstract thinking. A higher level of intellectual functioning is required for an individual to explain such phrases as ‘A stitch in time saves nine’ or ‘Don’t count your chickens before they’re hatched’. Note whether the patient’s explanations are relevant and concrete. The patient with altered mental ability is likely to interpret the phrase literally or merely rephrase the words.
Another higher level of intellectual functioning involves finding similarities or associations between concepts: a dog is to a beagle as a cat is to a Siamese. Name related concepts and ask the patient to identify their associations. Questions should be appropriate to the patient’s level of intelligence. It is sufficient to use simple concepts.
Judgment requires a comparison and evaluation of facts and ideas to understand their relationships and to form appropriate conclusions. Try to measure the ability to make logical decisions. By assessing judgment, you can also measure the ability to organise thought processes. This can be determined by asking the patient why they decided to seek healthcare or how they plan to adjust to limitations after returning home. A simpler test involves asking what patients would do if placed in a situation such as being locked out of their home or suddenly becoming ill when alone at home.
There are special assessment tools designed to assess a patient’s mental status. Kahn and Goldfarb’s mental status questionnaire (MSQ) (Kahn and others, 1960) is a 10-item instrument and a widely used tool. Folstein and others (1975) developed the Mini Mental State Examination (MMSE) method to measure orientation and cognitive function (Box 27-19). A maximum score on the MMSE is 30. Patients with scores of 21 or lower generally reveal cognitive impairment requiring further assessment.
BOX 27-19 MINI-MENTAL STATE EXAMINATION (MMSE)
MMSE sample items:
• Orientation to time—‘What is the date?’
• Registration—‘Listen carefully. I am going to say three words. You say them back after I stop. Ready? Here they are … APPLE (pause), PENNY (pause), TABLE (pause). Now repeat those words back to me.’ [Repeat up to 5 times, but score only the first trial.]
• Naming—‘What is this?’ [Point to a pencil or pen.]
• Reading—‘Please read this and do what it says.’ [Show examinee the words on the stimulus form: CLOSE YOUR EYES]
Reproduced by special permission of the publisher, Psychological Assessment Resources, Inc., 16204 North Florida Avenue, Lutz, Florida 33549, from the Mini Mental State Examination by Marshal Folstein and Susan Folstein, Copyright 1975, 1998, 2001 by Mini Mental LLC, Inc. Published 2001 by Psychological Assessment Resources, Inc. Further reproduction is prohibited without permission of PAR, Inc. The MMSE can be purchased from PAR, Inc. by calling +1 (813) 968-3003.
Abnormal findings of cognition and perception
A common mental disorder affecting older adults is delirium. This is an acute condition characterised by confusion, disorientation and restlessness (Box 27-20). The acute condition is often misdiagnosed as a form of dementia (e.g. Alzheimer’s disease). Thus the underlying cause of the condition is missed. Delirium is often overlooked in older adults because of a failure to adequately assess mental status, or discounted as common older adult behaviour (Flagg and others, 2010). Fortunately, the condition can be reversed when correctly assessed. Often, the delirium worsens at night. A history of patient’s behaviour before delirium developed is essential in early recognition of the condition.
BOX 27-20 CLINICAL CRITERIA FOR DELIRIUM
Definition—an acute disturbance of consciousness that is accompanied by a change in cognition. It cannot be accounted for by a pre-existing or evolving dementia. Delirium develops over a short period of time, usually hours to days, and tends to fluctuate during the course of the day. It is usually a direct physiological consequence of a general medical condition.
• There is reduced clarity of awareness of the environment.
• Ability to focus, sustain or shift attention is impaired (questions must be repeated).
• Person is easily distracted by irrelevant stimuli.
• There is an accompanying change in cognition (memory impairment, disorientation or language disturbance).
• Waxing and waning of orientation occurs through the day.
• Recent memory is most commonly affected.
• Disorientation is usually shown, with person disoriented to time or place.
• Language disturbance may involve impaired ability to name objects or ability to write; speech may be rambling.
• Perceptual disturbances may include misinterpretations, illusions or hallucinations.
Modified from American Psychiatric Association 1994 Diagnostic and statistical manual of mental disorders, ed 4 (DSM-IV). Washington DC, American Psychiatric Association; Monk T, Price C 2011 Postoperative cognitive disorders. Curr Opinion Crit Care 17:376–81.
• CRITICAL THINKING
While administering medication to Mrs Marsaja, you note that she is confused as to place and time and her speech is slightly slurred. What subjective and objective data related to cognition and perception will you collect?
There are different types of cerebrovascular disease: cerebral insufficiency, infarction, haemorrhage or arteriovenous malformation causing symptoms of infarction, haemorrhage or mass lesion. Syndromes accompanying either ischaemic or haemorrhagic lesions are commonly referred to as stroke. Both ischaemic and haemorrhagic strokes tend to develop abruptly and the signs and symptoms reflect the area of the brain damaged. Common symptoms include headache, altered conscious state, aphasia, dysphagia and impaired mobility (Cook and Clements, 2011). The two types of aphasia are sensory (receptive) and motor (expressive). With receptive aphasia, a person cannot understand written or verbal speech. With expressive aphasia, a person understands written and verbal speech but cannot write or speak appropriately when trying to communicate. A patient may suffer a combination of receptive and expressive aphasia, depending on the part of the cerebral cortex involved.
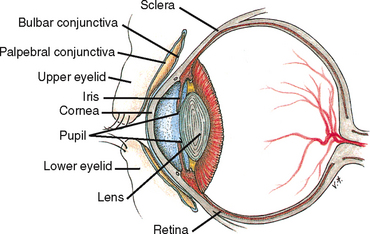
Eyes
Functional vision is important for independence in all aspects of our lives. Examination of the eyes includes assessment of visual acuity, visual fields, extraocular movements, and external and internal eye structures (Table 27-26). Figure 27-45 shows a cross-section of the eye. The assessment detects visual alterations (Box 27-21) and determines the level of assistance patients require. Patients with visual problems may also need special aids for reading educational materials or instructions (e.g. medication labels).
TABLE 27-26 NURSING HISTORY FOR EYE ASSESSMENT
| ASSESSMENT QUESTIONS |
RATIONALE |
| Determine problems that prompted patient to seek healthcare. Do you have any of the following: eye pain, photophobia (sensitivity to light), burning, itching, excess tearing or crusting, diplopia (double vision), blurred vision, awareness of a ‘film’ over field of vision, floaters (small black spots that seem to float across field of vision), flashing lights or halos around lights? |
Common symptoms of eye disease indicate need for referral to specialist |
| Do you have a history of eye disease, eye trauma, diabetes, hypertension or eye surgery? |
Some diseases or trauma can cause risk of partial or complete visual loss. Surgery may have been performed for a visual disorder |
| Is there a family history of eye disorders or diseases? |
Certain eye problems such as glaucoma or retinitis pigmentosa are inherited |
| What is your occupation? What are your hobbies? Do you wear safety glasses? |
Performance of close, intricate work can cause eye fatigue. Working with computers may cause eye strain. Certain occupational tasks (e.g. working with chemicals) and recreational activity (e.g. fencing or motorcycle riding) place people at risk of eye injury unless precautions are taken |
| Do you wear glasses or contact lenses? For what purpose? |
Glasses or contacts should be worn during certain portions of examination for accurate assessment |
| When did you last visit the ophthalmologist or optometrist? |
Date of last eye examination reveals level of preventive care taken by patient |
| What medications are you taking? Do you use eye drops or eye ointment? |
Determines need to assess patient’s knowledge of medications.
Certain medications can cause visual symptoms
|
BOX 27-21 COMMON EYE AND VISUAL PROBLEMS
Astigmatism—a condition in which parallel light rays do not focus on a single point on the retina. An uneven curvature of the cornea or lens causes light to be focused on different points.
Cataract—an increased opacity of the lens, which blocks light rays from entering the eye. Cataracts may develop slowly and progressively after age 35 or suddenly after trauma. Cataracts are one of the most common eye disorders. By age 70, most older adults have some evidence of visual impairment from cataracts.
Glaucoma—intraocular structural damage resulting from elevated intraocular pressure. It is caused by obstruction of the outflow of aqueous humour. Without treatment the disorder can cause blindness.
Hyperopia—farsightedness, a refractive error in which rays of light enter the eye and focus behind the retina. People are able to clearly see distant objects but not close objects.
Macular degeneration—blurred central vision often occurring suddenly, caused by a progressive degeneration of the centre of the retina. It is the most common visual impairment in people over age 50 and the most common cause of blindness in older adults. There is no cure.
Myopia—nearsightedness, a refractive error in which rays of light enter the eye and focus in front of the retina. People are able to clearly see close objects but not distant objects.
Presbyopia—impaired near vision in middle-aged and older adults, caused by loss of elasticity of the lens and associated with the ageing process.
Retinopathy—a non-inflammatory eye disorder resulting from changes in retinal blood vessels. It is a leading cause of blindness.
Strabismus—a congenital problem in which the eyes appear crossed. The muscles controlling movement of the eyes are not coordinated.
Hands should be washed before and after the examination, and gloves worn when palpating the eyelids.
Assessment of the eyes
VISUAL ACUITY
The assessment of visual acuity—the ability to see small details—tests central vision. If patients wear glasses, they should wear them during the examination. The language spoken and the ability to read should be assessed. Asking patients to read aloud can help determine literacy. If the patient has difficulty reading, move to the next step.
Assessment of distant vision is assessed very simply in clinical environments by asking the patient to identify objects in the distance. If patients cannot identify objects in the distance, their ability to count upraised fingers or distinguish light is assessed. A hand is held 30 cm from the patient’s face and they count the upraised fingers. Light perception is checked by shining a penlight into the eye and then turning the light off. If the patient notes when the light is turned on or off, light perception is intact. Near vision can be assessed by asking patients to read from a newspaper, wristwatch or similar item. Patients are instructed to hold the item a comfortable distance (5–6 cm) from the eyes, and to read the smallest line possible. Simple testing such as this is adequate for beginning nurses.
EXTRAOCULAR MOVEMENTS
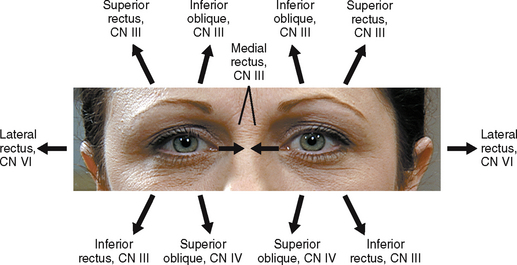
Six small muscles guide the movement of each eye and three cranial nerves are involved: the oculomotor nerve (cranial nerve [CN] III), the trochlear nerve (CN IV) and the abducens nerve (CN VI; see Table 27-27). Both eyes move parallel to each other in each of the six directions of gaze (Figure 27-46). The patient sits or stands 60 cm away facing you while you hold a finger at a comfortable distance (15–30 cm) from the patient’s eyes. The patient keeps the head in a fixed position facing you and follows the movement of the finger with the eyes only. The patient looks to the right, to the left, and diagonally up and down to the left and right. Move your finger smoothly and slowly within the normal field of vision. As the patient gazes in each direction, observe for parallel eye movement, the position of the upper eyelid in relation to the iris, and the presence of abnormal movements. As the eyes move through each direction of gaze, the upper eyelid covers the iris only slightly.
Assessing the corneal light reflex can check eye alignment. A weakness or imbalance of the extraocular muscles can cause misalignment. In a darkened room and with the patient looking straight ahead, a penlight is shone onto the bridge of the patient’s nose from a distance of 60–90 cm. Normally light reflects on the cornea in the same spot on both eyes. If an abnormality is present, the light shines on a different spot on each eye.
VISUAL FIELDS
As the patient looks straight ahead, all objects in the periphery can normally be seen. To assess visual fields, the patient stands or sits 60 cm away, facing you at eye level. The patient closes or covers one eye (e.g. the left) and looks at your eye directly opposite. Close your opposite eye (in this case the right) so that the field of vision is superimposed on that of the patient. Move a finger equidistant from yourself and the patient outside the field of vision, then slowly bring it back into the visual field. Ask the patient to tell you when they first see your finger. If you see the finger before the patient does, a portion of the patient’s visual field is reduced. The procedure is repeated for each field of vision for the other eye. Patients with visual field problems may be at risk of injury because they cannot see all objects in front of them.
EXTERNAL EYE STRUCTURES
To inspect external eye structures, stand directly in front of the patient at eye level and ask the patient to look at your face.
Assess the position of the eyes in relation to each other; they are normally parallel to each other.
EYEBROWS
Eyebrows are normally symmetrical. They are inspected for size, extension, texture of hair, alignment and movement. A loss or absence of hair may indicate a hormonal disturbance or be the result of waxing or plucking. Ageing causes loss of the lateral third of the eyebrows. The brows should rise and lower symmetrically.
EYELIDS
The eyelids are inspected for position, colour, condition of the surface, condition and direction of the eyelashes and the patient’s ability to open and close the eyes and to blink. When the eyes are open in a normal position, the lids do not cover the pupil and the sclera cannot be seen above the iris. The eyelashes are normally distributed evenly and curved outwards away from the eye. The eyelids are normally smooth and the same colour as the skin. The lids normally close symmetrically. Ask the patient to open their eyes for inspection of the lower lids. The same characteristics as for the upper lids are assessed. Normally a person blinks involuntarily and bilaterally up to 20 times a minute. The blink reflex helps lubricate the cornea. Note and report absent, infrequent, rapid or monocular (one-eyed) blinking.
LACRIMAL APPARATUS
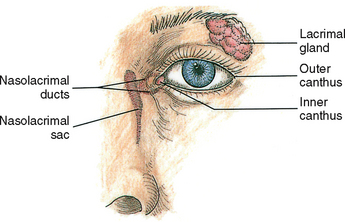
The anterior surface of the eye, made up of the sensitive cornea and conjunctivae, is moistened or lubricated by tears secreted from the lacrimal gland (Figure 27-47). The gland is located in the upper outer wall of the anterior part of the orbit. Tears flow from the gland across the eye’s surface to the lacrimal duct, which is located in the nasal corner or inner canthus of the eye. The lacrimal gland can be the site of tumours or infections. The area of the gland is inspected for oedema and redness, and it is palpated gently to detect tenderness. Normally the gland cannot be felt. Mild palpation of the duct at the lower eyelid just inside the lower orbital rim, not on the side of the nose, may cause a regurgitation of tears.
CONJUNCTIVAE AND SCLERAE
The bulbar conjunctiva covers the exposed surface of the eyeball up to the outer edge of the cornea, and the palpebral conjunctiva is the delicate membrane lining the eyelids. Normally the conjunctiva is transparent, enabling the examiner to view the tiny underlying blood vessels that give it a light-pink colour. The sclera is seen under the bulbar conjunctiva and normally is the colour of white porcelain in Caucasians and light-yellow in dark-skinned people.
CORNEAS
The cornea is the transparent, colourless portion of the eye covering the pupil and iris. As the patient looks straight ahead, inspect the cornea for clarity and texture while shining a penlight obliquely across the cornea’s entire surface. The cornea is normally shiny, transparent and smooth. However, in older adults the cornea loses its lustre. Any irregularity in the surface may indicate an abrasion or tear that warrants immediate examination by a specialist. The colour and details of the underlying iris should be easy to see. In older adults the iris becomes faded. A thin white ring along the margin of the iris, called an arcus senilis, is common with ageing but is abnormal in anyone aged under 40 years.
PUPILS AND IRISES
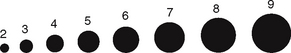
Observe the pupils for size, shape, equality, accommodation and reaction to light. The pupils are normally black, round, regular and equal in size (3–7 mm in diameter) (Figure 27-48). The iris should be clearly visible. Pupillary reflexes (to light and accommodation) are tested in a dimly lit room. As the patient looks straight ahead, bring a penlight from the side of the patient’s face, directing the light onto the pupil (Figure 27-49). If the patient looks at the light, there will be a false reaction to accommodation (adjustment). A directly illuminated pupil constricts, and the opposite pupil constricts involuntarily in correlation. Observe the quickness and equality of the reflex of both eyes.
To test for accommodation, the patient gazes at a distant object (the far wall) and then at a test object (finger or pencil) held approximately 10 cm from the bridge of the patient’s nose. The pupils normally converge and adjust by constricting when looking at close objects. The pupillary responses are equal. Testing for accommodation is important if the patient has a defect in the pupillary response to light (Seidel and others, 2011). If pupillary reaction is normal in all tests, the abbreviation PERRLA (pupils equal, round, reactive to light and accommodation) is recorded.
Abnormal findings of the eye
Hyperthyroidism, tumours or inflammation of the orbit usually cause bulging of the eyes (exophthalmos) (Holcomb, 2002). Crossing of eyes (strabismus) results from neuromuscular injury or inherited abnormalities. Paralysis of the facial nerve exists if a patient cannot move the eyebrows. Nystagmus, an involuntary, rhythmical oscillation of the eyes, reflects local injury to eye muscles and supporting structures or a disorder of the cranial nerves innervating the muscles (Fetzer, 2000). Nystagmus might be apparent in some patients when checking extraocular movements.
An abnormal drooping of the lid over the pupil is called ptosis (pronounced ‘toe-sis’) and is caused by oedema or impairment of the third cranial nerve. Defects in the position of the lid margins may also be observed. An older adult frequently has lid margins that turn out (ectropion) or in (entropion). An entropion may lead to the lid’s lashes irritating the conjunctiva and cornea, increasing the risk of infection. Failure of the lids to close exposes the cornea to drying. This condition is common in unconscious patients or in those with facial nerve paralysis. Lid oedema may be due to allergies or to heart or kidney failure.
An erythematous or yellow lump (hordeolum or stye) on the follicle of an eyelash indicates an acute suppurative inflammation. Redness indicates inflammation or infection. Lesions are inspected for typical characteristics and discomfort or drainage. Gloves should be worn if drainage is present. The nasolacrimal duct may become obstructed, blocking the flow of tears. If the patient complains of excessive eye-watering, look for evidence of oedema in the inner canthus.
CONJUNCTIVAE AND SCLERA
Sclerae may become pigmented and appear either yellow or green if liver disease is present (Tizzard and Davenport, 2007). The presence of redness may indicate an allergic or infectious conjunctivitis. Bright-red blood in a localised area surrounded by normal-appearing conjunctiva usually indicates subconjunctival haemorrhage. A pale conjunctiva results from anaemia, whereas a fiery red appearance is a result of inflammation (conjunctivitis). Conjunctivitis is a highly contagious infection. The crusty drainage that collects on eyelid margins can easily spread from one eye to the other.
PUPILS
Cloudy pupils indicate cataracts. Dilated pupils can result from glaucoma, trauma, neurological disorders, eye medications (e.g. atropine) or withdrawal from opioids. Constricted pupils may be caused by inflammation of the iris or use of drugs (e.g. pilocarpine, morphine or cocaine). Pinpoint pupils are a common sign of opioid intoxication (Dixon, 2007). Examination with a beam of light aims to assess the afferent (optic nerve) and efferent (parasympathetic via third cranial nerve constricting and sympathetic dilating) pathways of the pupillary reflexes (Fuller and Manford, 2010). Any abnormality along the nerve pathways from the retina to the iris alters the ability of the pupils to react to light. Changes in intracranial pressure, lesions along the nerve pathways, locally applied ophthalmic medications and direct trauma to the eye may alter pupillary reaction.
Ears
Ear assessment is used to determine the integrity of ear structures and the condition of hearing. Nursing history data (Table 27-28) help identify risks of hearing disorders. Ear examination is focused on assessment of pain, discharge or presence of lumps or foreign objects. Internal and external examination of the ears will detect evidence of ear pressure, fullness, pain and excessive cerumen (ear wax).
TABLE 27-28 NURSING HISTORY FOR EAR ASSESSMENT
| ASSESSMENT QUESTIONS |
RATIONALE |
| Do you have any of the following: ear pain, itching, discharge, vertigo, tinnitus (ringing in ears) or change in hearing? |
These signs and symptoms indicate infection or hearing loss |
Assess risks of hearing problem:
Infants/children—hypoxia at birth, meningitis, birthweight less than 1500 g, family history of hearing loss, congenital anomalies of skull or face, non-bacterial intrauterine infections (rubella, herpes), maternal drug use, excessively high bilirubin, head trauma
Adults—exposure to industrial or recreational noise, genetic disease (Ménière’s disease), neurodegenerative disorder
|
Risk factors predispose patient to permanent hearing loss.
It may be difficult to assess infant’s hearing status with examination only
|
| Do you experience loud noises at work ? Are protective devices available? Do you wear them? |
Prolonged noise exposure can cause temporary or permanent hearing loss |
| Note behaviours indicative of hearing loss, such as failure to respond when spoken to, requests to repeat comments, leaning forward to hear and child’s inattentiveness or use of monotonous voice tone |
Persons with hearing loss cope with sensory deficit through a variety of behavioural cues |
| What medications do you take? |
Some medications are ototoxic, e.g. large doses of aspirin, aminoglycosides, furosemide, streptomycin, cisplatin, ethacrynic acid |
| Do you use a hearing aid? |
Determination allows nurse to assess effectiveness, ability to care for device and allows nurse to adjust voice tone to communicate |
| Have you had a recent hearing problem? Describe the onset, contributing factors, affected ear and effect on activities for daily living |
Nature and severity of hearing problem are determined |
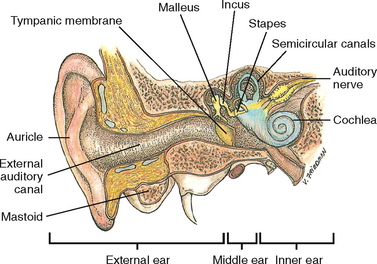
The ears are easy to examine because of their accessibility. The three parts of the ear are the external, middle and inner ear (Figure 27-50). The external ear includes the auricle and external auditory meatus (ear canal). The middle ear is an air-filled cavity containing the three bony ossicles (malleus, incus and stapes). The eustachian tube connects the middle ear to the nasopharynx. Pressure between the outer atmosphere and the middle ear is stabilised through the eustachian tube. The inner ear contains the cochlea, vestibule and semicircular canals. The inner ear consists of the bony labyrinth, the semicircular canals and the membranous labyrinth.
Understanding the mechanisms for sound transmission helps identify the nature of hearing disorders. Sound travels through the ear by air and bone conduction; the following explains the steps of hearing.
• Sound waves in the air enter the external ear, passing through the outer ear canal.
• The sound waves reach the tympanic membrane, causing it to vibrate.
• Vibrations are transmitted through the middle ear by the bony ossicular chain to the oval window at the opening of the inner ear.
• The cochlea receives the sound vibration.
• Nerve impulses from the cochlea travel to the auditory (eighth cranial) nerve and to the cerebral cortex.
Inspection of the ear
AURICLES
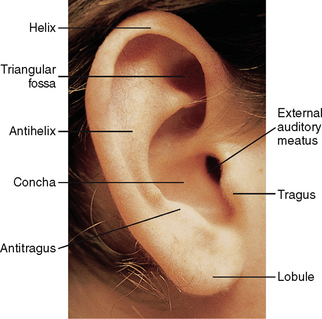
With the patient sitting comfortably, inspect and palpate the auricle’s size, shape, symmetry, landmarks, position and colour (Figure 27-51). The auricles are normally level with each other. The upper point of attachment is in a straight line with the lateral canthus, or corner of the eye. The position of the auricle should also be almost vertical. As you palpate the ears for tenderness and lesions, note the condition of the skin. The colour should be the same as that of the face, without moles, cysts, deformities or nodules. Palpate the auricles for texture, tenderness and skin lesions. The auricle is normally smooth, without lesions. If the patient reports pain, gently pull the auricle, press on the tragus and palpate behind the ear over the mastoid process.
Inspect the opening of the ear canal for size and discharge. Discharge may be accompanied by an odour. The meatus should not be swollen or occluded. Cerumen, a yellow, waxy substance, is common. The deeper structures of the external and middle ear can only be observed with an otoscope, which is usually only performed by advanced practice nurses.
HEARING ACUITY
Hearing loss can be determined from the patient’s response to conversation. The three types of hearing loss are conduction, sensorineural and mixed. A conduction loss interrupts sound waves as they travel from the outer ear to the cochlea of the inner ear because the sound waves are not transmitted through the outer and middle ear structures. Causes of a conduction loss include swelling of the auditory canal or tears in the tympanic membrane. A sensorineural loss involves the inner ear, auditory nerve or hearing centre of the brain. Sound is conducted through the outer and middle ear structures, but the continued transmission of sound becomes interrupted at some point beyond the bony ossicles. A mixed loss involves a combination of conduction and sensorineural loss.
Note the patient’s response to questions and any need to repeat questions. If hearing loss is suspected, the patient’s response to the whispered voice is assessed. One ear is tested at a time while the patient occludes the other ear with a finger. The patient is asked to gently move the finger in their ear up and down during the test. While standing 30–60 cm from the ear being tested, cover your mouth so that the patient is unable to read lips. After exhaling fully, the nurse first whispers softly towards the unoccluded ear, reciting random numbers with equally accented syllables, such as nine-four-ten. If necessary, voice intensity is gradually increased until the patient correctly repeats the numbers. The other ear is then tested for comparison.
People working or living around loud noises are at risk of hearing loss. Older adults experience an inability to hear high-frequency sounds and consonants (e.g. S, Z, T and G). Deterioration of the cochlea and a thickening of the tympanic membrane cause older adults to gradually lose hearing acuity. They are especially at risk of hearing loss due to ototoxicity (injury to auditory nerve) resulting from high-maintenance doses of antibiotics (e.g. aminoglycosides).
Abnormal findings of the ear
Disorders of the ear result from several types of problems, including mechanical dysfunction (blockage by ear wax or foreign body), trauma (foreign bodies or noise exposure), neurological disorders (auditory nerve damage), acute illnesses (viral infection) and toxic effects of medications.
If palpating the external ear increases pain, an external ear infection is likely. If palpation does not influence the pain, the patient may have a middle ear infection (Warren, 2008). Tenderness in the mastoid area can indicate mastoiditis. Yellow or green foul-smelling discharge may indicate infection or a foreign body.
Ears that are low-set or at an unusual angle are a sign of chromosome abnormality (e.g. Down syndrome) (Ranweiler, 2009). Redness is a sign of inflammation or fever. A reddened canal with discharge is a sign of inflammation or infection. Accumulated cerumen is a common problem and its build-up can create a mild hearing loss. During the examination, the examiner asks about methods that the patient uses to clean the ear canal (Box 27-22). A pink or red bulging tympanic membrane indicates inflammation. A white colour reveals pus behind it.
BOX 27-22 CLIENT TEACHING DURING EAR ASSESSMENT
OBJECTIVES
• Patient will use proper technique for cleaning the ears.
• Patient will follow preventive guidelines for screening of hearing loss.
• Patient with hearing loss will communicate effectively.
TEACHING STRATEGIES
• Instruct patient about the proper way to clean the outer ear (see Chapter 34), avoiding use of cotton-tipped applicators and sharp objects such as hairpins, which may cause impaction of cerumen deep in the ear canal.
• Encourage patients over age 65 to have regular hearing checks. Explain that a reduction in hearing is a normal part of ageing.
• Instruct family members of patient with hearing loss to avoid shouting, speaking instead in low tones, and to be sure the patient can see the speaker’s face.
EVALUATION
• Patient will use a safe technique for cleaning the ears.
• Patient will have frequent hearing checks.
If a hearing loss is present, referral is made to a specialist. If the patient has a known hearing loss, then encourage the use of hearing aids.
Sensory function
The sensory pathways of the central nervous system conduct information about pain, temperature, position, vibration, and crude and finely localised touch. Different pathways relay the sensations. For most patients, a quick screening of sensory function is sufficient unless there are symptoms of reduced sensation, motor impairment or paralysis.
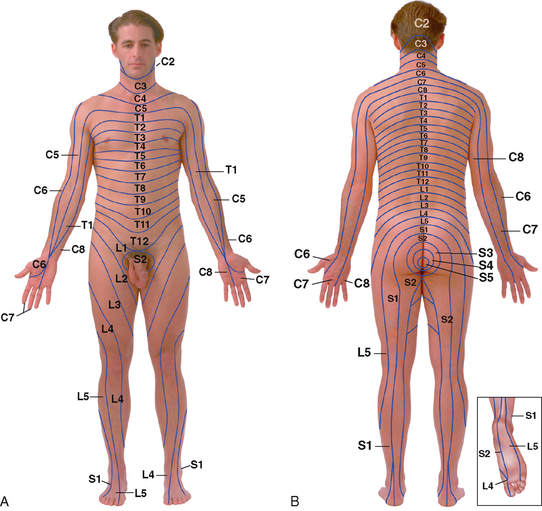
Normally a patient has sensory responses to all stimuli tested. Sensations along the body’s surface are felt equally on both sides of the face, trunk and extremities. A knowledge of the sensory dermatome zones (Figure 27-52) is essential. Some areas of the skin are innervated by specific dorsal-root cutaneous nerves. For example, if reduced sensation is noted when checking for light touch along an area of the skin (e.g. the lower neck), the existence of a neurological lesion can be determined (e.g. fourth cervical spinal cord segment).
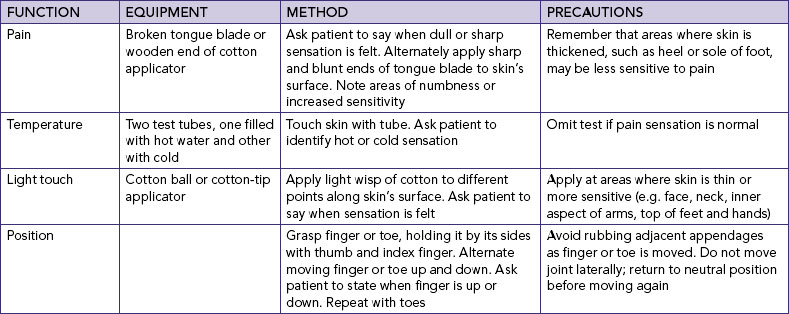
All sensory testing is performed with the patient’s eyes closed so that the patient is unable to see when or where a stimulus strikes the skin (Table 27-29). Stimuli are applied in a random, unpredictable order to maintain the patient’s attention and prevent detection of a predictable pattern. The patient is asked to tell the nurse when, what and where each stimulus is felt. Compare symmetrical areas of the body while applying stimuli to the patient’s arms, trunk and legs.
SKILL 27-6 Assessment of central nervous system and level of consciousness
DELEGATION CONSIDERATIONS
Assessment of the central nervous system (CNS) may be undertaken by enrolled nurses under the guidance of the registered nurse.
• Ensure review of the anatomy and physiology of the CNS for risk factors
• Ensure review of the Glasgow Coma Scale (GCS)
• Ensure hand hygiene is performed and personal protective equipment is worn when appropriate.
EQUIPMENT
• Penlight torch
• Neurological observation chart
• Pen
References: Forbes H, Watt E 2012 Jarvis’s Physical examination and health assessment. Sydney, Saunders Australia. National Stroke Foundation (NSF) 2012 Spread the word F.A.S.T. (blog). Melbourne, NSF. Online. Available at www.strokefoundation.com.au/blog/?tag=fast 27 Apr 2012.
| STEPS |
RATIONALE |
1. Determine need to assess neurological status of patient.
|
Certain conditions place patients at risk of neurological alterations (stroke, seizure, paralysis). Physical signs and symptoms such as confusion, drowsiness and limb weakness may indicate alterations in neurological function. As cognitive function deteriorates, the patient becomes disorientated to time, place and person and is unable to process and demonstrate higher order functioning. |
2. Focused health history
|
The focused neurological health history provides insight into the link between a patient’s lifestyle and neurological information and pathology. |
| |
a. Determine chief complaint—characteristics of pain and each sign/symptom using the PQRST approach (see Chapter 6).
|
|
| |
b. Ascertain presence of:
• seizure—location (i.e. body parts involved), quantity in time, quality (general or localised) • associated manifestations—incontinence, injury, memory loss and cyanosis • aggravating factors—bright/flashing lights, TV, sleep deprivation, stress, fever in children, alcohol.
|
|
| |
c. Ask about setting—warning aura, sequence of events, e.g. headache
|
|
| |
d. Ask about timing—first onset.
|
|
| |
e. Assess syncope—quality, i.e. total vs partial loss of consciousness; and quantity in time.
|
|
| |
f. Assess pain—location and quality
|
|
| |
g. Assess paraesthesia and associated manifestations, e.g. pain, stiffness, gait changes, poor peripheral pulses, injury
|
|
| |
h. Assess disturbances in gait: quality—ataxic, spastic, hemiplegic
|
|
| |
i. Assess visual changes: quality—blindness, in particular fields of vision, blurred vision, bright/flashing lights
|
|
| |
|
|
| |
k. Assess for memory disorders: quality—recent or remote memory loss
|
|
| |
l. Assess for dysphasia or dysphagia.
|
|
| |
m. Determine past history of neurological-specific conditions and surgery, and non-neurological-specific conditions.
|
|
| |
n. Ask about social history—alcohol use, work environment, recreation and leisure, sexual practice, stress.
|
|
3. Explain procedure to patient and clarify any concerns.
|
Promotes patient’s cooperation and comfort during the assessment. |
4. Ensure patient comfort and privacy.
|
|
5. Neurological assessment commences with a Glasgow Coma Scale (GCS) score to measure level of consciousness (see Table 27-25).
|
The GCS assesses the patient’s level of consciousness. It is able to evaluate the brain function as a whole, rather than assessing particular lobes of the brain.
The level of consciousness exists along a continuum from full waking, alertness and cooperation through to any form of external stimuli. A fully conscious patient responds to questions spontaneously. As consciousness lowers, a patient may show irritability, a shortened attention span or an unwillingness to cooperate.
|
| |
|
The patient’s eyes typically should be open (depending on time of day or presentation). Patient assessed in this level of consciousness should be recorded as ‘spontaneous’ (score 4). |
| |
|
(1)Observe the patient’s eyes when entering the room.
|
|
| |
|
(2)If the patient is not awake, give the patient a command such as: ‘Open your eyes.’
|
Positive patient response should be recorded as eye opening ‘to speech’ (score 3). |
| |
|
(3)If the patient does not respond to verbal stimuli, assess their response to a painful stimulus (see motor response below); progress from light to deep stimulus.
|
Positive patient response should be recorded as eye opening ‘to pain’ (score 2). |
| |
|
(4)There may be no response to speech or painful stimuli.
|
Patient assessed in this level of consciousness should be recorded as ‘no response’ (score 1). |
| |
|
|
| |
|
(1)Assess orientation by seeking the best verbal response from the patient to simple questions:
‘Where are you at the moment?’ ‘Do you know what month it is?’ ‘Do you know what year it is?’
|
|
| |
|
(2)Patients should be able to hold a conversation and answer the above questions correctly.
|
If answered correctly, patient response should be recorded as ‘orientated’ (score 5).
If answered incorrectly, patient response should be recorded as ‘confused’ (score 4).
|
| |
|
(3)Patient may respond with single words and answer does not match the question asked.
|
Patient response should be recorded as ‘inappropriate words’ (score 3). |
| |
|
(4)Patient may respond with incomprehensible sounds only (such as moans and groans).
|
Patient response should be recorded as ‘incomprehensible sounds’ (score 2). |
| |
|
(5)There may be no response to any stimuli.
|
Patient response should be recorded as ‘no response’ (score 1). |
| |
|
|
| |
|
(1)Assess the patient’s ability to follow two simple commands such as:
‘Squeeze and let go of my hands.’
|
Positive patient response should be recorded as ‘obeys commands’ (score 6). |
| |
|
(2)If patient is unable to perform the above activities, apply a central painful stimulus (e.g. trapezium squeeze) to determine the best arm response.
|
As neurological function deteriorates motor responses are reduced. A patient with serious neurological impairment exhibits abnormal posturing in response to pain. |
| |
|
|
a. The patient may demonstrate purposeful movement to remove the painful stimulus, bringing the hand up to at least chin level.
|
Patient response should be recorded as ‘localises to pain’ (score 5). |
| |
|
|
b. The patient may bend the arm at the elbows but fails to locate the pain.
|
Patient response should be recorded as ‘flexion withdrawal’ (score 4). |
| |
|
|
c. The patient may demonstrate abnormal flexion (decorticate posturing): flexion of the elbow, wrist and fingers, with adduction of the limb. Lower limbs may also be in extension, internal rotation and plantar flexion.
|
Patient response should be recorded as ‘abnormal flexion’ (score 3). |
| |
|
|
d. The patient may demonstrate abnormal extension (decerebrate posturing): elbow extension, adduction and internal rotation with palm pronated. Lower limbs may also be in extension and plantar flexion.-0
|
Patient response should be recorded as ‘abnormal extension’ (score 2). |
| |
|
|
e. There may be no response after the application of a central painful stimulus.
|
Patient response should be recorded as ‘no response’ (score 1). |
6. Total GCS scores out of 15 and document on neurological observation chart.
|
Overall score or change in score determines need to report to medical officer. |
7. Assess pupil reaction and gauge.
a. Check pupillary response for shape, size (mm) and reaction to light. b. Use a pen torch to elicit a response from the pupils— shine the light from the peripheries of the eye, to the centre. c. Note pupillary response for both eyes, which should be brisk constriction to light. d. Measure pupil size, which should be equal.
|
|
|
|
Response is recorded on a continuum from normal through mild weakness, severe weakness, flexion, extension to no response. |
| |
A. Bilateral upper limb muscle strength
|
|
| |
|
(1)Ask the patient to take your hands and squeeze.
|
|
| |
|
(2)Ask the patient to pull your hands towards them against resistance.
|
|
| |
|
(3)Ask the patient to push your hands away against resistance.
|
|
| |
B. Bilateral lower limb muscle strength
|
|
| |
|
(1)Ask the patient to push down with their foot onto your hands against resistance.
|
|
| |
|
(2)Ask the patient to lift up their foot against your hand with resistance.
|
|
| |
|
(3)Apply gently pressure to the shins and ask the patient to extend and flex their legs against resistance.
|
|
9. Continue to perform neurological assessment as required by presentation and hospital protocol.
|
The GCS allows the evaluation of a patient’s status over time. The higher the score, the more improved or normal the level of functioning. |
| RECORDING AND REPORTING |
HOME CARE CONSIDERATIONS |
• Record GCS scores with date and time of assessment. Report decrease in GCS by two or more points to medical officer immediately.
• Pupils’ response: document size of pupil (mm) and response to light.
• Limb movements’ response: document power of movements of arms and legs.
|
• Act FAST:
Face: check their face—has their mouth drooped? Arms: can they lift both arms? Speech: is their speech slurred? Do they understand you? Time: is critical. If you see any of these signs, call for emergency medical assistance (National Stroke Foundation, 2012).
|
Motor function
An assessment of motor function includes the same measurements made during the musculoskeletal examination. Muscles are assessed for size, strength and tone. In addition, cerebellar function is assessed. The cerebellum coordinates muscular activity by producing smooth, steady and efficient movements of muscle groups. The maintenance of balance and equilibrium is also a function of the cerebellum. Sensory impulses from the vestibular portion of the inner ear travel to the cerebellum, where impulses are relayed to proper motor nerves to maintain body equilibrium. The cerebellum also controls posture.
Coordination
As the tests used to measure coordination are difficult to explain, it is often necessary to demonstrate each manoeuvre and then have patients repeat it after determining that they are physically able to make the necessary movements. Observe the smoothness and balance of movements (Box 27-23).
BOX 27-23 CLIENT TEACHING DURING NEUROLOGICAL ASSESSMENT
OBJECTIVES
• Patient’s family will understand relationship of patient’s behavioural and mental changes to physical status.
• Patient with sensory or motor impairment will select safety measures for self-care.
• Older adult will routinely inspect skin for injuries.
TEACHING STRATEGIES
• Explain to family or friends the neurological implications of any behavioural or mental impairment shown by patient.
• If patient has sensory or motor impairments, explain measures to ensure safety (e.g. use of walking aids or safety bars in bathrooms or stairways).
• Teach older adult to plan enough time to complete tasks, because reaction time is slowed.
• Teach older adult to observe skin surfaces for areas of trauma, because perception of pain is reduced.
EVALUATION
• Patient will explain safety measures used to avoid injury from sensory and motor limitations.
• Patient will explain reason for inspecting skin surface routinely.
• Patient will perform self-care and mobility safely.
To assess fine motor function, have the patient extend the arms out to the sides and touch each forefinger alternately to the nose (first with eyes open, then with eyes closed). Normally the patient touches the nose smoothly. Performing rapid, rhythmical, alternating movements demonstrates coordination in the upper extremities. While sitting, the patient begins by patting the knees with both hands. Then the patient alternately turns up the palm and back of the hands while continuously patting. The manoeuvre should be done smoothly and regularly with increasing speed.
An additional manoeuvre for upper extremity coordination involves touching each finger with the thumb of the same hand in rapid sequence. The patient moves from the index finger to the little finger and back, with one hand tested at a time. The patient’s dominant hand is slightly less awkward when performing this movement. Movements should be smooth and in succession.
Lower-extremity coordination is tested with the patient lying supine, legs extended. Ask the patient to lift the heel up and put it on the opposite knee, and then run it accurately down the front of the shin. The nurse can also place a hand at the ball of the patient’s foot and ask the patient to tap this hand with the foot as quickly as possible. Each foot is tested for speed and smoothness. The feet do not move as rapidly or evenly as the hands.
Balance
You can use one or two of the following tests to assess balance and gross motor function.
• Have the patient perform a Romberg test by standing with feet together, arms at the sides, both with eyes open and with eyes closed. While standing at the side to protect the patient’s safety, observe swaying. Slight swaying is normal. The patient does not normally have to break the stance.
• Have the patient close the eyes, with arms held straight at the sides, and stand on one foot and then the other. Normally balance is maintained for 5 seconds with slight swaying.
• Ask the patient to walk a straight line by placing the heel of one foot directly in front of the toes of the other foot.
Abnormal findings related to sensory and motor function
Cognitive impairment, poor vision, muscular weakness and imbalance and lack of coordination are common consequences of neurological disorders. Patients with any of these changes are at risk of falling (Healey, 2010). Healthcare facilities use risk-assessment tools to predict the level of risk for falling for their patients. An example of such a tool is provided in the article by Lovallo and others (2010).
Sexuality–reproductive pattern
The general focus of this area of assessment is on the sexual-reproductive aspects of individuals during their lifespan. Assessment includes discussion of sex-role behaviour, gender identification, physiological and biological functioning, and the cultural and societal expectations of sexual behaviour. Reproductive patterns involve the capability to procreate, pregnancy and childbirth, and normal reproductive functioning. For most beginning nurses, asking questions about a person’s sexual health and inspection of external genitalia will be sufficient (see Chapter 24 for a guide to taking a sexual health history). However, it is important for beginning nurses to have knowledge of the developmental changes that occur across the life span and with this frame of reference evaluate the client in the areas considered to be relevant. Experienced nurses working in sexual health clinics, obstetrics or gynaecological settings and some urological settings will undertake a more comprehensive assessment of sexual and reproductive function.
An examination of the genitalia can be embarrassing for any person unless a calm and relaxed assessment approach is used. For women the gynaecological examination is one of the most difficult experiences. Some women may prefer to have the examination conducted by a female nurse; it is important to determine each woman’s preference prior to commencing the assessment. Specific consideration must be undertaken for adolescents, who may choose to have a parent present during the examination. A male examiner should always have a female attendant present during the examination. A female examiner may prefer to work alone, but should have a female attendant if the patient is particularly anxious or has a preference for a support person. The patient should be provided with very thorough explanations for procedures used in the examination. Privacy, respect and professional tact are extremely important when assessing the patient.
The individual client situation will determine the focus of the assessment in this area. Some of the possible areas for examination are outlined. The assessment of sexuality and reproductive function includes relevant subjective data, outlined in Box 27-24.
BOX 27-24 ASSESSMENT OF SEXUALITY AND REPRODUCTION
FEMALES:
• Menstrual history, pregnancy and birthing, miscarriages/abortions
• Contraception
• Menopause
• Additional information—bladder problems?
MALES:
• Assessment of prostate enlargement (over 50 years of age)
• Additional information—bladder problems?
• Contraception
GENERAL HEALTH HISTORY:
• History of sexually transmitted infections (STIs)/partner with STIs
• Surgery/chronic health problems
• Endocrine disorders (diabetes)
• Medications
COMMON SYMPTOMS:
• Infections, discharge, pain/discomfort/itching, history of abuse, impotence, lumps
KNOWLEDGE ABOUT SEXUALITY AND SEXUAL FUNCTIONING:
• Knowledge of normal anatomy and physiology, changes with age, contraception, STIs, illness
HEALTH MAINTENANCE FACTORS:
• Breast screening—mammogram, clinical examination
• Pap smear/testicular examination
• Prevention of STIs
CONCERNS ABOUT SEXUAL PERFORMANCE AND SATISFACTION:
• Sexual function—sexual drive, perceived satisfaction, effects of health/illness, medications
• Sexual behaviour—sexual preference, attitudes and values, religious beliefs, perception of women’s/men’s roles
Objective data relevant to the particular client situation are collected. Some of the possible areas for examination are outlined next. Review developmental changes across the life span, and with this frame of reference evaluate the client in the areas considered to be relevant. General observation for clients of both sexes includes inspection of the development of secondary sex characteristics.
Breasts
Breast cancer, while the most commonly diagnosed cancer in Australian women, is the second-highest cause of cancer-related deaths. The incidence of breast cancer has risen more than 20% from 1997 to 2007 while the mortality rate has remained constant over the same period. According to data from Cancer Australia (2011), 1 in 9 women will be diagnosed with cancer in their lifetime. In addition, 3 out of 4 women diagnosed with breast cancer are aged over 50 years. It is projected that by 2015, 15,409 women will be diagnosed with breast cancer in Australia. This represents a 22% increase compared with 2006.
Women of all ages are at risk of developing breast cancer, but the risk increases as they get older. A woman may be at higher risk of breast cancer if (National Breast and Ovarian Cancer Centre, 2009):
• her mother, sister or daughter has had breast cancer before the age of 50 years
• she has already had cancer in one breast
• she has never had a child or her first child was born after the age of 30.
The patient’s history (Table 27-30) will alert you to any signs of breast disease and normal developmental changes. Because of its glandular structure, the breast undergoes changes during a woman’s life. Knowledge of these changes (Box 27-25) will help you to complete an accurate assessment.
TABLE 27-30 NURSING HISTORY FOR BREAST ASSESSMENT
| ASSESSMENT QUESTIONS |
RATIONALE |
Do you have a personal or family history of breast cancer? Have you had children? How old were you when you gave birth to your first child? How long have you breastfed your babies (total time)?
When was your first period? What age were you when you reached menopause? Do you take hormone replacement therapy?
|
Risk factors for breast cancer include: women aged 40 and over; mother or sister diagnosed with breast cancer before the age of 50 years; early puberty (before age 12 years); late menopause (after 55 years); overweight; high alcohol intake; gave birth to first child after age 30; less than 12 months total breastfeeding time |
| Have you noticed a lump, thickening, pain or tenderness of breast; discharge, distortion, retraction or scaling of nipple; or change in size of breast? |
Potential signs and symptoms of breast cancer allow nurse to focus on specific areas of breast during assessment |
| If patient reports a breast mass, ask about length of time since lump was first noticed. Does lump come and go, or is it always present? Have there been changes in the lump (e.g. size, relationship to menses), and are there associated symptoms? |
Helps to determine nature of mass |
| What medications are you taking? |
Some medications may cause nipple discharge. Hormones and caffeine may cause fibrocystic changes in breast |
| Do you know about breast awareness strategies? |
Nurse’s role is to educate patient about breast awareness strategies |
BOX 27-25 NORMAL CHANGES IN THE BREAST DURING A WOMAN’S LIFE SPAN
PUBERTY (8–20 YEARS)
Breasts mature in five stages. One breast may grow more rapidly than the other. The ages at which changes occur and rate of developmental progression vary.
STAGE 1 (PREADOLESCENT)
This stage involves elevation of the nipple only.
STAGE 2
The breast and nipple elevate as a small mound, and the areolar diameters enlarge.
STAGE 3
There is further enlargement and elevation of the breast and areola, with no separation of contour.
STAGE 4
The areola and nipple project into the secondary mound above the level of the breast. (May not occur in all girls.)
STAGE 5 (MATURE BREAST)
Only the nipple projects, and the areola recedes (may vary in some women).
YOUNG ADULTHOOD (20–30 YEARS)
Breasts reach full (non-pregnant) size. Shape is generally symmetrical. Breasts may be unequal in size.
PREGNANCY
Breast size gradually enlarges to 2–3 times the previous size. Nipples enlarge and may become erect. Areolae darken, and diameters increase. Superficial veins become prominent. A yellowish fluid (colostrum) may be expelled from the nipples.
MENOPAUSE
Breasts shrink. Tissue becomes softer, sometimes flabby.
OLDER ADULTHOOD
• Breasts become elongated, pendulous and flaccid as a result of glandular tissue atrophy. The skin of the breasts tends to wrinkle, appearing loose and flabby.
• Nipples become smaller, flatter and lose erectile ability. Nipples may invert because of shrinkage and fibrotic changes.
From Ebersole P, Hess P 2008 Toward healthy aging, ed 7. St Louis, Mosby.
Assessment of female breast
INSPECTION
The patient removes the top of her gown/drape to allow a simultaneous view of both breasts. The patient may stand or sit with arms hanging loosely at her sides. If possible, place a mirror in front of the patient so that she can see what to look for when inspecting her breasts (Figure 27-53). The breasts are inspected for size and symmetry. The breasts usually extend from the third to the sixth ribs, with the nipple at the level of the fourth intercostal space. One breast is commonly larger than the other. However, a difference in size may be caused by inflammation or a mass. As the woman becomes older, the ligaments supporting the breast tissue weaken, causing the breasts to sag and the nipples to lower.
Observe the contour or shape of the breasts and note masses, flattening, retraction or dimpling. Breasts vary in shape from convex to pendulous or conical. The overlying skin is inspected for colour and venous pattern. Venous patterns are more easily seen in thin patients or pregnant women. The presence of lesions, oedema or inflammation is also noted. Lift each breast when necessary to observe lower and lateral aspects for colour and texture changes. Redness and excoriation are common on the undersurface. The breasts are the colour of neighbouring skin, and venous patterns are the same bilaterally.
Inspect the nipple and areola for size, colour, shape, discharge and the direction the nipples point. The normal areolae are round or oval and nearly equal bilaterally. Colour ranges from pink to brown. In light-skinned women the areola turns brown during pregnancy and remains dark. In dark-skinned women the areola is brown before pregnancy (Seidel and others, 2011). Normally the nipples point in symmetrical directions, the surface is smooth or wrinkled and they are everted with no drainage. If nipples are inverted, ask if this has been a lifetime history. Clear yellow discharge 2 days after childbirth is common. The characteristics of the inspection are explained to the patient to teach the significance of abnormal signs or symptoms.
PALPATION
Palpation allows determination of the condition of underlying breast tissue. Breast tissue consists of glandular tissue, fibrous supportive ligaments and fat. Glandular tissue is organised into lobes that end in ducts opening onto the nipple’s surface. The largest portion of glandular tissue is in the upper outer quadrant and tail of each breast. Suspensory ligaments connect to skin and fascia underlying the breast to support the breast and maintain its upright position. Fatty tissue is located superficially and to the sides of the breast.
The consistency of normal breast tissue varies widely. The breasts of a young woman are firm and elastic. In an older woman the tissue may feel stringy and nodular. If the patient reports a mass, examine the opposite breast to ensure an objective comparison of normal and abnormal tissue. Use the pads of the first three fingers to compress breast tissue gently against the chest wall, noting tissue consistency (Figure 27-54). Palpation is performed systematically in one of three ways (Figure 27-55):
1. a back-and-forth technique with the fingers moving up and down each quadrant
2. clockwise or counterclockwise, forming small circles with the fingers along each quadrant and the tail
3. palpating from the centre of the breast in a radial fashion, returning to the areola to begin each spoke.
Whatever approach is used, be sure to cover the entire breast and tail, directing attention to any areas of tenderness.
When palpating large, pendulous breasts, use a bimanual technique. The inferior portion of the breast is supported in one hand while the other hand is used to palpate breast tissue against the supporting hand.
During palpation, note the consistency of breast tissue. It normally feels dense, firm and elastic. In fibrocystic disease, a common problem in women, tissue feels lumpy but this is found bilaterally. With menopause, breast tissue shrinks and becomes softer. The lobular feel of glandular tissue is normal. The lower edge of each breast may feel firm and hard. This is the normal inframammary ridge and not a tumour. It may be helpful for the patient to feel normal tissue variations.
Special attention is given to gently palpating the nipple and areola. The thumb and index finger compress the nipple gently, noting any discharge. Examination of the nipple and areola may cause the nipple to become erect, with wrinkling of the areola. These changes are normal.
Male breasts
Examination of the male breast is relatively easy. Although breast cancer in men is relatively rare, all changes should be investigated. The nipple and areola are inspected for nodules, oedema and ulceration. An enlarged male breast may result from obesity or glandular enlargement. Breast enlargement in young males may be indicative of steroid use. Fatty tissue feels soft, whereas glandular tissue is firm. Any masses are palpated for the same characteristics as in the female breast.
Abnormal findings of the breast
Cancerous lesions are hard, fixed, non-tender and irregular in shape. A common benign condition of the breast is fibrocystic breast disease. This condition is characterised by lumpy, painful breasts and sometimes nipple discharge. Symptoms are more apparent during the menstrual period. When palpated, the cysts (lumps) are soft, well-differentiated and moveable. Deep cysts may feel hard. Retraction or dimpling results from invasion of underlying ligaments by tumours. The ligaments become fibrotic and pull the overlying skin inwards towards the tumour. Oedema also changes the breasts’ contours. To assess for retraction or changes in the shape of breasts, ask the patient to assume three positions: raise arms above the head, press hands against the hips and extend arms straight ahead while sitting. A recent inversion or inward turning of the nipple may indicate an underlying growth. Rashes or ulcerations are not normal on the breast or nipples. Bleeding or discharge from the nipple is noted. Each manoeuvre causes a contraction of the pectoral muscles, which will accentuate retraction (Foy and Blowers, 2009).
Abnormal masses are palpated to determine the following:
• location in relation to quadrants
• diameter in centimetres
• shape (e.g. round or discoid)
• consistency (soft, firm or hard)
• tenderness
• mobility
• discreteness (whether boundaries of mass are clear or unclear).
Until recently, breast self-examination was strongly promoted as an early detection strategy. However, there is no evidence that use of specific breast examination techniques make any difference to the detection of breast cancers. Instead, the following guidelines for the early detection of breast cancer are recommended (Cancer Council Australia, 2011):
• Develop breast awareness strategies, which include:
–
viewing breasts in the mirror when dressing and undressing.
–
feeling breasts while bathing or showering. It is recommended that the woman feels all of her breast from the collarbone to below the bra-line and in the armpits as well. The National Breast and Ovarian Cancer Centre (NBOCC) website provides a tool to assist women to develop breast awareness (see
www.cheekycheckup.com.au)
–
consulting a healthcare provider if any changes are noticed in the breasts.
• Have a mammogram every 2 years from the age of 50 years. The Breast Screen Australia program provides free 2-yearly mammographic screening and follow-up, aimed specifically at women aged 50–69 years (Cancer Council Australia, 2011). Women over 70 years qualify for free mammogram screening, but they do not receive reminders to attend appointments.
• Women in the high-risk categories should be frequently monitored and have regular mammograms. A breast cancer screening tool which is simple to use is available for women on the NBOCC website (see Online resources). This interactive tool is designed for women who have not had breast cancer to identify their level of risk for breast cancer compared with another woman of a similar age group.
External genitalia
Inspection of external genitalia
Opportunities for beginning nurses for examination of the external genitalia of male and female patients will occur during routine hygiene, toileting and dressing activities or urinary catheter care. When assisting the patient with any of these activities, you have the opportunity to inspect the distribution of pubic hair, colour of hair and presence of lesions in the pubic region as well as the genitalia. Furthermore, because the incidence of sexually transmitted infections (STIs) in adolescents and young adults is high, an assessment of the genitalia should be a routine part of any health maintenance examination for this age group, which are likely to be performed by nurses or medical practitioners working in specialist settings.
Sexual maturity is determined in part by the quantity and distribution of hair growth. A preadolescent has no pubic hair except for fine body hair like that on the abdomen; hair grows during adolescence. In the female, hair grows along the labia, becoming darker, coarser and curlier as it spreads over the pubic symphysis. Hair growth eventually forms a triangle over the female perineum and along the medial surfaces of the thighs. Hair growth should not spread up over the abdomen. In the male, the pubic hair extends from the base of the penis over the symphysis pubis and becomes coarse and curly. Hair should be free of nits and lice. The underlying skin should be free of inflammation, irritation or lesions.
THE FEMALE PATIENT
The surface characteristics of the labia majora are inspected. The skin of the perineum is smooth, clean and slightly darker than other skin. The mucous membranes appear dark-pink and moist. The usually symmetrical labia majora may be gaping or closed and appear dry or moist. After childbirth the labia majora are separated, causing the labia minora to become more prominent. When a woman reaches menopause, the labia majora become thinned, and with advancing age they become atrophied. The labia majora are normally without inflammation, oedema, lesions or lacerations.
The size of the clitoris is variable. However, it is normally about 2 cm or less in length and 0.5 cm in width. Look for atrophy, inflammation or adhesions. If inflamed, the clitoris will be a bright cherry-red. In young women it is a common site for syphilitic lesions, or chancres, which appear as small open ulcers draining serous material. Dry, scaly, nodular lesions in older women may signal malignant changes.
The urethral orifice is observed for colour and position. It is normally intact without inflammation. The urethral meatus is anterior to the vaginal orifice and is pink. At times it is difficult to locate. It may appear as a small slit or pinhole-opening just above the vaginal canal. In women who have had several vaginal childbirths, the opening to the vaginal canal often extends upwards, interfering with the view of the urethra. Note any discharge, polyps or fistulas.
When inspecting the vaginal orifice (introitus), inspect for inflammation, oedema, discolouration, discharge and lesions. Normally, the introitus is a thin, vertical slit or a large orifice with moist tissue. The hymen, just inside the introitus, may, in the virgin, restrict the opening of the vagina. Only remnants of the hymen remain after sexual intercourse.
You will also inspect the anus at this time, looking for lesions and haemorrhoids (see section below on rectal examination).
• CRITICAL THINKING
Mrs Marsaja asks you for advice on how to manage a rash that has started in her pubic area. What questions will you ask? What physical assessment will you undertake?
THE MALE PATIENT
The first sign of puberty, an increase in genital and pubic hair development, is variable but generally does not start before 9.5 years of age. The testes and penis develop, with the scrotal skin darkening and becoming thinner and more wrinkled in texture. The penis slowly lengthens, eventually reaching to the bottom of the scrotum.
Begin by assessing the sexual maturity of the patient, noting the size and shape of the penis and testes, the colour and texture of the scrotal skin and the character and distribution of pubic hair.
PENIS
Inspect the structures of the penis, including the shaft, corona, prepuce (foreskin), glans and urethral meatus. The dorsal vein should be apparent on inspection. In uncircumcised males, the foreskin is retracted to reveal the glans and urethral meatus; the foreskin should retract easily. A small amount of thick, white secretion between glans and foreskin is normal. If there is evidence of abnormal discharge, a culture is usually obtained. The urethral meatus is slit-like and should be positioned on the ventral surface just millimetres from the tip of the glans. In some congenital conditions, the meatus is displaced along the penile shaft. Gentle compression of the glans between thumb and index finger opens the urethral meatus to allow inspection for discharge. The opening should be glistening and pink. The meatus is also inspected for lesions, oedema and inflammation.
The glans is carefully checked around its entire circumference for lesions. The area between the foreskin and glans is a common site for venereal lesions. Any lesion is palpated gently to note tenderness, size, consistency and shape.
Continue to inspect the entire shaft of the penis, including the under-surface, looking for lesions, scars and oedema. The shaft is palpated between the thumb and first two fingers to detect any localised areas of tenderness. When inspection and palpation of the penis is completed, the foreskin is pulled down to its original position.
SCROTUM
Inspect the scrotum for swelling and lesions and palpate the testes for size, shape and smoothness. The ideal position for this part of the examination is with the patient in the standing position. Be particularly cautious when palpating the scrotum because the structures lying within the scrotal sac are very sensitive. The scrotum is a sac-like structure divided internally into two halves. Each half contains a testicle, epididymis and the ductus deferens, which travels upwards into the inguinal ring. Normally the left testicle is lower than the right. Inspect the scrotum’s size, shape and symmetry while observing for lesions or oedema. The scrotum is usually more deeply pigmented than the body skin, and the surface is coarse. It is gently lifted to view the posterior surface. The scrotal skin is usually loose. A tightening of the skin may reveal oedema. The scrotum’s size normally changes with temperature variations as the dartos muscle contracts in cold and relaxes in warm temperatures.
The underlying testicles are normally ovoid and approximately 2–4 cm in size. The testicles and epididymis are gently palpated between the thumb and first two fingers. They should be sensitive to gentle compression but not tender, and they should feel smooth, rubbery and free of nodules. The size, shape and consistency of the organs are noted. In the older man the testicles decrease in size and are less firm during palpation. The patient should be asked about any unusual tenderness.
Abnormal findings of the male reproductive system
The most common symptoms of testicular cancer are a painless enlargement of one testis and the appearance of a palpable, small, hard lump, about the size of a pea, on the front or side of the testicle.
TESTICULAR SELF-EXAMINATION
Testicular cancer is the most common cancer in young men aged between 18 and 39 years. While there is no evidence to show that self-examination improves patient outcomes, Cancer Council Australia recommends that getting to know your body in combination with healthy living are important health strategies. In getting to know his body, the patient can feel his testes after a shower when the scrotum and structures are relaxed and more easily felt (Box 27-26). Testes should be held between the thumb and fingers and gently rolled, feeling the entire surface. They should be similar in size, shape and consistency—firm but not hard with a smooth surface. Should any irregularity be felt, the person should consult his healthcare provider for a clinical examination (Cancer Council Australia, 2011).
BOX 27-26 MALE GENITAL SELF-EXAMINATION
Illustrations from Seidel HM and others 2011 Mosby’s guide to physical examination, ed 7. St Louis, Mosby.
All men 15 years and older should perform this examination monthly using the following steps.
GENITAL EXAMINATION
• Perform the examination after a warm bath or shower when the scrotal sac is relaxed.
• Stand naked in front of a mirror and hold the penis in your hand and examine the head. Pull back the foreskin if uncircumcised.
• Inspect and palpate the entire head of the penis in a clockwise motion, looking carefully for any bumps, sores or blisters.
• Look also for any bumpy warts.
• Look at the opening at the end of the penis for discharge (see illustration).
• Look along the entire shaft of the penis for the same signs.
• Be sure to separate pubic hair at the base of the penis and carefully examine the skin underneath.
TESTICULAR SELF-EXAMINATION
• Look for swelling or lumps in the skin of the scrotum while looking in the mirror.
• Use both hands, placing the index and middle fingers under the testicles and the thumb on top (see illustration).
• Gently roll the testicle, feeling for lumps, thickening or a change in consistency (hardening).
• Find the epididymis (a cordlike structure on the top and back of the testicle; it is not a lump).
• Feel for small, pea-sized lumps on the front and side of the testicle. The lumps are usually painless and are abnormal.
• Call your healthcare provider if you find a lump.
Inspection of the anus
Begin by inspecting the perianal and sacrococcygeal areas, where skin should be smooth and uninterrupted. Look for lumps, rashes, inflammation, excoriation and scars. Fungal infection can cause perianal irritation.
Using the non-dominant hand, gently draw the buttocks apart to inspect the anus. Anal tissues are normally moist and hairless compared with perianal skin. The tissue is coarser and more darkly pigmented. The anus is held closed by the voluntary external muscle sphincter. Inspect anal tissue for skin lesions, external haemorrhoids (dilated veins that appear as reddened protrusions), fissures and fistulas, inflammation, rashes or discolouration.
Value–belief pattern
The purpose of assessing a person’s values and beliefs is to understand the basis for the person’s health-related decisions and actions in order to plan and implement individualised nursing care. Contemporary healthcare places an emphasis on person-centred care by arguing that the person (including their family) should be at the centre of care. Person-centred care is defined as ‘treatment and care provided by health services [that] places the person at the centre of their own care and considers the needs of the older person’s carers’ (Department of Human Services, 2006). This means that the patient is included in the decision making about their treatment and any other health-related decisions. Health-related decisions and actions are determined by what the patient values, and by their goals and beliefs. Partnership between patient and the healthcare team can be achieved by developing a relationship with the person, providing care for the patient that is consistent with their values, careful and thorough assessment and focusing on the person’s abilities rather than disabilities (McCormack, 2001).
To gain a better understanding of your patient, ask if there are any perceived conflicts with values, beliefs or expectations that are health-related. You might also find out if religion is important to your patient and if it is helpful when difficulties arise. It is important to also find out whether being ill or in hospital will interfere with the patient’s religious practices. For some patients religious practices are significantly important, as are dietary considerations. For some patients, some health practices and their consent to some treatments might be influenced by their values and beliefs. For example, a person who follows the Jehovah Witness faith may not want to have a blood transfusion. You may need to find out if the patient or their family requires specific spiritual help, and put them in touch with the spiritual adviser available in the community or hospital.
Self perception–self concept pattern
Self-perception and self-concept involve the exploration of the person’s sense of personal identity, goals, emotional responses, the way they think about themselves, and feelings about self-image and worth (see Chapter 23 for a more comprehensive discussion). This includes their perceptions about their appearance, abilities and limitations. As well as including their view of themselves, their perceptions of how others view them are also sought. Illness and disability can have impacts on our views of self, our personal identity and our plans. When self-concept is threatened through losses related to health or employment, for example, self-perception and self-concept may be threatened.
Subjective data collection is focused on the person’s description of their social identity perceptions of self-worth, perceptions of body image, and actual or potential threats to their self-concept. Specific questions are focused on collecting information about demographic characteristics such as age, gender, family situation and group memberships. Asking the patient to describe themselves and to explore the factors that have contributed to their self-concept, such as what they like most/least about themself, how they feel about themself and what others think of them, helps to identify the person’s perception of self-worth. Finding out from the patient their perceptions of their main health concern and their body will assist you to identify how the patient perceives their body image. Finding out about the things that make the person feel anxious, fearful or distressed will assist you to identify the patient’s perception of actual or potential threats to self-concept.
When collecting objective data, observe the general appearance of the patient and their body language. For some patients it may be necessary to also use a specific assessment tool to measure anxiety, depression or body image. The person’s body language may indicate poor self-esteem, anxiety or nervousness.
Abnormal findings relating to self-concept
Abnormal findings include irritability, angry outbursts, withdrawal, poor eye-contact, drooping of head and shoulders, facial tension, speech inarticulate with rapid speech tremors or twitches, and use of body movements such as foot shuffling. See Chapter 23 for more information.
Role–relationships pattern
To assess roles and relationships requires examination of the way in which a person engages in relationships and assumes roles in life. The patient’s perception of relationships and satisfaction with their roles is the major focus of subjective data collection. The person’s satisfaction with relationships is an important component of this area. Objective assessment in this area is to describe the person’s pattern of family and social roles and associated responsibilities. Loss, threat or change may produce problems in this area.
When collecting the subjective data, your questioning will focus on the person’s description of their usual role–relationship functioning and any difficulties with roles and relationships. Ask the patient about their role in family, friendships, in the community and with co-workers. Some patients might be preparing for a new role, such as becoming a parent. Ask the patient to describe the relationships with individuals and family. This will include a description of the family structure. You could use a diagram to show the family structure. Find out about living arrangements and communication patterns used within the family. Inquire about the processes used to make decisions on important issues. It may be necessary to identify support structures, from either individuals or the family. In some cases it may be necessary to explore discipline patterns within the family. Your questions will depend on the patient’s situation.
• CRITICAL THINKING
Mrs Marsaja tells you that she is excited to be going to rehabilitation as she sees this as an important step in preparing for her return to her home. She tells you she misses her garden. She is very annoyed that her son insists on her going to a nursing home.
What questions will you ask Mrs Marsaja and her son?
Sleep–rest pattern
Assessment of sleep and rest requires examination of how the individual rates or judges the adequacy of his or her sleep, rest and relaxation in terms of quality and quantity. The amount of energy the person has in relation to the amount of sleep, rest and relaxation is examined.
Subjective data includes exploration of the person’s usual sleep patterns, usual sleep and bedtime rituals, sleeping environment, factors that influence sleep, and common problems with sleeping. In addition it is important to find out about how the person relaxes. For the detailed subjective data collection, ask the client about the number of hours, times, naps, changes in the pattern, time of retiring and time of awakening. Find out about the quality of the sleep environment, such as the number and type of pillows, bedcovers, noise and sleep position used. Explore the aids that the person may use, such as warm milk and medications. The person’s perception of sleep adequacy, performance capabilities for ADLs and psychological and physiological state on awakening should be sought. Information about how the person prepares for sleep is also useful. For example, you could explore whether there are difficulties with sleep onset, sleep interruptions or early morning awakening. The following will affect sleep quality to some degree: health problems, night-time voiding, medications, caffeine, alcohol, occurrence of dreaming and nightmares, leg cramps, snoring, sleepwalking and nocturnal enuresis (bedwetting). Explore the activities the person feels assist in achieving rest or relaxation. These may include naps, reading, television, exercise and yoga.
Common problems related to sleep and rest include daytime sleepiness, morning headache, difficulty initiating and maintaining sleep (insomnia), and uncontrolled falling asleep.
When doing a physical examination of a person who is experiencing difficulties with sleep and rest, observe the person’s general appearance. In particular, observe for signs of lack of sleep/rest. For example, the person may have a flat or expressionless facial affect, red eyes, dark circles, yawning, slurred speech, incorrect word use, mispronunciation or impaired coordination, and may appear to be restless. Further objective data can be collected by observation of the person while asleep. For further information, refer to Chapter 35.
• CRITICAL THINKING
Mrs Marsaja tells you that she normally likes to go to bed early but wakes during the middle of the night and cannot get back to sleep. What questions will you ask?
Coping–stress tolerance pattern
Stress is part of life, and the way in which we respond is variable. Illness and the surrounding uncertainties not only present a threat to self and how we see ourselves and our personal identity, but also cause the individual to respond to that threat or stress biologically, psychologically and behaviourally (Karademas, 2011). There can be physical responses such as elevated blood pressure, increased heart rate and palpitations, among others. Emotional responses to stress include demonstrations of fear, anxiety, restlessness and agitation. Finally, the individual’s coping mechanisms might be positive such as seeking support, talking to others and/or engaging in physical activity. Some individuals respond to stress negatively by taking drugs, abusing alcohol or avoiding confronting the stressor. Assessing a person’s coping and stress tolerance involves examination of the individual’s ability to handle life crises, resolve conflicts and access assistive resources.
Detailed subjective data collection includes determining the person’s views of the nature of stressors which the individual is currently coping with and has coped with in the past. The stressors may be physical, psychological or socioeconomic, or a combination of these. Ask your patient about the major changes/losses that may have occurred over the past year and the meaning of those changes. Ask your patient how these situations have affected them physically and emotionally. It is also important to identify how the person normally relieves and copes with stress. For example, the person may seek information, take direct action (fight or flight) or use social supports. Some people use defence mechanisms such as drinking, smoking, sleeping or using medications. Once you have identified the strategies the person uses to manage their stress, find out how successful these measures are perceived to be.
Gathering further evidence of coping ability and tolerance to stress can also be found in every other area of health assessment. An outcome of stress may be insomnia, weight loss or decreased concentration. There may be physical signs that include restlessness, irritability and nervousness. There may be an increased blood pressure and/or pulse. There may be evidence of increased perspiration.
• CRITICAL THINKING
While Mrs Marsaja is excited to be going to rehabilitation, she also tells you that she is frightened she may not be allowed to return to her home. She tells you that she and her son argued about this the previous evening and she feels very upset. What questions would you ask?
After the examination
You may choose to record findings from the health assessment during the interview and examination, or at the end. Most institutions have special forms that make it easy to record examination data (see Chapter 14). For example, on admission you will be required to complete specific paperwork which includes admission assessment data.
After completing the assessment, help the patient dress and provide an opportunity to wash face and hands and assume a comfortable position. The patient in the home may only need time to dress and join the nurse in the living room or kitchen. When the patient is comfortable, it helps to share a summary of the assessment findings. If the findings have revealed serious abnormalities, such as a mass or a highly irregular heart rate, the patient’s medical practitioner should be consulted before any findings are revealed. Significant findings are communicated to appropriate medical and nursing personnel, either verbally or in the written care plan. Some assessment data indicates a critical change in the patient’s condition, such as changes that may occur in the vital signs. It is imperative that such changes are reported urgently and action taken to keep the patient safe.
The patient often needs a number of ancillary examinations, such as X-ray examinations, laboratory tests or ultrasonography, after a physical examination. These tests provide additional screening information to rule out the presence of abnormalities and help in the diagnosis of specific abnormalities found during the examination. The nurse explains the purpose of these tests and the sensations that the patient can expect.
KEY CONCEPTS
• Baseline assessment findings reflect the patient’s functional abilities when the nurse first assesses the patient and serve as the basis for comparison with subsequent assessment findings.
• Ongoing focused assessment is used to monitor patient progress and response to treatments.
• Assessment data are used to determine the severity of patient symptoms and areas of risk and degree of function, select appropriate nursing interventions and evaluate the outcomes of nursing care.
• Physical assessment of a child or infant requires the nurse to apply principles of physical growth and development.
• The nurse recognises that the normal process of ageing affects physical findings collected from an older adult.
• Teaching should be integrated throughout the examination to help patients learn about health promotion and disease prevention.
• The nurse can use time more efficiently by integrating physical assessment with routine nursing care.
• Inspection requires good lighting, full exposure of the body part and a careful comparison of the part with its counterpart on the opposite side of the body.
• Palpation involves the use of parts of the hand to detect different types of physical characteristics.
• Percussion is the detection of differences in density of underlying tissues by listening to sounds produced while striking the body’s surface.
• A good stethoscope should have earpieces that fit snugly, flexible thick-walled tubing of the proper length and a chest-piece with a bell and diaphragm.
• Through auscultation, the nurse assesses the character of sounds created in various body organs.
• A physical examination should be performed only after proper preparation of the environment and equipment and after preparing the patient physically and psychologically.
• Throughout the examination the nurse should keep the patient warm, comfortable and informed of each step of the process.
• The patient assumes various positions during the physical examination to provide greater accessibility to body parts and to increase accuracy in assessment.
• The nurse uses a systematic approach when conducting a physical assessment.
• A competent examiner learns to combine assessments of different body systems simultaneously.
• Information from the nursing history helps the nurse to focus on examining body systems likely to be affected.
• When assessing a seriously ill patient, the nurse concentrates on the body systems most likely to be affected.
• Accuracy in assessing the thorax, heart and abdomen is enhanced by creating a mental image of internal organs in relation to external anatomical landmarks.
• When examining a woman’s breasts, the nurse explains the techniques for breast self-examination.
• The abdominal assessment differs from other parts of the examination in that auscultation follows inspection.
• During assessment of the genitalia, the nurse explains the techniques for self-examination.
• Assessment of musculoskeletal function can easily be conducted by observing the patient walking or participating in other active movements.
• The nurse assesses mental and emotional status by interacting with the patient throughout the examination.
• At the end of the examination, the nurse provides for the patient’s comfort, then completes a detailed review of physical assessment findings.
REFERENCES
Alfaro-LeFevre R. Applying nursing process: a tool for critical thinking, ed 7. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins, 2010.
Australian Institute of Health and Welfare (AIHW). Cancer in Australia: an overview. Canberra: AIHW, 2010.
Brand HS, Gonggrijp S, Blanksma CJ. Cocaine and oral health. Br Dent J. 2008;204:365–369.
Cancer Australia. Breast cancer statistics. Canberra: Australian Government, 2011. Online Available at http://canceraustralia.nbocc.org.au/breast-cancer/about-breast-cancer/breast-cancer-statistics 30 Apr 2012.
Cancer Council Australia. Early detection facts sheets. Sydney: Cancer Council Australia, 2011. Online Available at www.cancer.org.au/Healthprofessionals/patientfactsheets/Early_detection.htm
Cancer Society of New Zealand. Skin cancer facts and figures. Wellington: Cancer Society of New Zealand, 2008. Online Available at www.cancernz.org.nz/reducing-your-cancer-risk/sunsmart/about-skin-cancer/skin-cancer-facts-and-figures 4 Apr 2012.
Cant R. Investing in patients’ nutrition: nutrition risk screening in hospital. Austral J Adv Nurs. 2011;28(2):81–87.
Centers for Disease Control and Prevention (CDC). Overweight and obesity: obesity trends. Atlanta, GA: CDC, 2000. Online Available at www.cdc.gov/nccdphp/dnpa/obesity/trend/index.htm 5 Jun 2010.
Cook LK, Clements SL. Stroke recognition and management: early identification and treatment are the keys. Am J Nurs. 2011;111(5):64–69.
Department of Health and Ageing (DoHA). Body mass index, national Measure Up campaign. Canberra: DoHA, 2011. Online. Available at www.health.gov.au/internet/abhi/publishing.nsf/Content/Body+Mass+Index-lp 4 Apr 2012.
Department of Human Services (DHS). What is person-centred health care? A literature review. Melbourne: State of Victoria DHS, 2006. Online Available at www.mednwh.unimelb.edu.au/pchc/downloads/PCHC_literature_review.pdf 4 Apr 2012.
Dixon P. Managing acute heroin overdose. Emerg Nurse. 2007;15(2):30–35.
Douglas C, Stolic S. The nurse’s role in health assessment: collecting and analysing data. In: Lewis P, Foley D, eds. Weber & Kelley’s Health assessment in nursing. Sydney: Lippincott Williams & Wilkins, 2011.
Ebersole P, Hess P. Toward healthy aging: human needs and nursing response, ed 7. St Louis: Mosby, 2008.
Egan BA, Mentes JC. Benefits of physical activity for knee osteoarthritis. J Gerontol Nurs. 2010;36(9):9–14.
Fetzer SJ. Clinical insights and review. Nystagmus: benign or significant? J Perianesthes Nurs. 2000;15(1):53–59.
Flagg B, Cox L, McDowell S, et al. Nursing identification of delirium. Clin Nurse Spec. 2010;24(5):260–266.
Folstein MF, et al. Mini-mental state: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:82.
Forbes H, Watt E. Jarvis’s Physical examination and health assessment. Sydney: Saunders, 2012.
Foy F, Blowers E. Breast cancer overview: diagnosis and staging. Pract Nurs. 2009;20(6):276–281.
Fuller G, Manford M. Neurology: an illustrated colour text, ed 3. Edinburgh: Churchill Livingstone, 2010.
Green L. An overview and update of psoriasis. Nurs Stand. 2011;25(35):47–55.
Gordon M. Nursing diagnosis: process and application, ed 3. St Louis: Mosby, 1994.
Healey F. A guide on how to prevent falls and injury in hospitals. Nurs Older People. 2010;22(9):16–22.
Holcomb SS. Thyroid diseases: a primer for the critical care nurse. Dimensions Crit Care Nurs. 2002;21(4):127–133.
Kahn RL, et al. Brief objective measures for the determination of mental status of the aged. Am J Psychiatr. 1960;117:326–328.
Karademas E. Psychological well-being and the role of perceived primal threat: evidence from two studies in patient and health samples. Stress Health. 2011;27:e111–e119.
Lee L, Grap MJ. Care and management of the patient with ascites. Med Surg Nursing. 2008;17(6):376–381.
Loescher LI, Harris RB, Lim KH, et al. Thorough skin self-examination in patients with melanoma. Oncol Nurs Forum. 2006;33(3):633–637.
Lovallo C, et al. Accidental falls in hospital inpatients: evaluation of sensitivity and specificity of two risk assessment tools. J Adv Nurs. 2010;66(3):690–696.
McCormack B. Autonomy and the relationship between nurses and older people. Ageing Soc. 2001;21:417–446.
Meiner S. Gerontological nursing, ed 4. St Louis: Mosby, 2011.
National Breast and Ovarian Cancer Centre (NBOCC). Breast cancer risk factors—a review of the evidence. Sydney: NCOCC, 2009. Online Available at http://canceraustralia.nbocc.org.au/view-document-details/rfrw-breast-cancer-risk-factors-a-review-of-the-evidence 19 Apr 2012.
National Breast and Ovarian Cancer Centre (NBOCC). Hormone replacement therapy (HRT) and risk of breast cancer, NBOCC position statement. Sydney: Cancer Australia, 2010. Online Available at http://canceraustralia.nbocc.org.au/our-organisation/position-statements/hormone-replacement-therapy-hrt-and-risk-of-breast-cancer 4 Apr 2012.
National Breast and Ovarian Cancer Centre (NBOCC. Early detection of breast cancer. NBOCC Position statement. Sydney: Cancer Australia, 2010. Online Available at http://canceraustralia.nbocc.org.au/our-organisation/position-statements/early-detection-of-breast-cancer 4 Apr 2012.
Oliver S. Care of patients with rheumatoid arthritis. Prim Health Care. 2009;19(5):16–22.
Ranweiler R. Assessment and care of the newborn with Down syndrome. Adv Neonatal Care. 2009;9(1):17–26.
Roush K. Prevention and treatment of osteoporosis in postmenopausal women: a review. Am J Nurs. 2011;111(8):26–35.
Sieggreen M. A contemporary approach to peripheral arterial disease. Nurse Pract. 2006;31(7):14–18.
Seidel HM, et al. Mosby’s guide to physical examination, ed 7. St Louis: Mosby, 2011.
Tizzard S, Davenport M. Early identification and referral of liver disease. Community Pract. 2007;80(9):40–42.
Tough J. Assessment and treatment of chest pain. Nurs Stand. 2004;18(37):45–55.
Warren E. ENT in primary care: part 5: ear pain. Pract Nurse. 2008;35(12):35–37.
Walker J. The role of the nurse in the management of osteoporosis. Br J Nurs. 2010;19(19):1243–1247.
Webster J, Healy J. Continuing professional development. Nutrition in hospitalized patients. Nurs Older People. 2009;21(10):31–38.
World Health Organization(WHO). Risk factors for tuberculosis. Geneva: WHO, 2011. Online Available at http://apps.who.int/tb/surveillanceworkshop/status_analysis/risk_factors_for_tb.htm 4 Apr 2012.