References
1. Couto, CG. Oncology. In: Sherding RG, ed. The cat: diseases and clinical management. New York: Churchill Livingstone, 1989.
2. Hardy, WD, Jr. Hematopoietic tumors of cats. J Am Anim Hosp Assoc. 1981;17:921–940.
3. Essex, M, Francis, DP. The risk to humans from malignant diseases of their pets: An unsettled issue. J Am Anim Hosp Assoc. 1976;12:386–390.
4. Theilen, GH, Madewell, BR. Feline hematopoietic neoplasms. In Theilen GH, Madewell BR, eds.: Veterinary cancer medicine, ed 2, Philadelphia: Lea & Febiger, 1987.
5. Vail, DM, Moore, AS, Ogilvie, GK, et al. Feline lymphoma (145 cases): Proliferation indices, CD3 immunoreactivity and their association with prognosis in 90 cats receiving therapy. J Vet Intern Med. 1998;12:349–354.
6. Cotter, SM. Feline viral neoplasia. In Greene CE, ed.: Infectious diseases of the dog and cat, ed 3, Philadelphia: WB Saunders, 1998.
7. Louwerens, M, London, CA, Pedersen, NC, et al. Feline lymphoma in the post-feline leukemia virus era. J Vet Intern Med. 2005;19:329–335.
8. Rissetto, K, Villamil, JA, Selting, KA, et al. Recent trends in feline intestinal neoplasia: an epidemiologic study of 1,129 cases in the veterinary medical database from 1964 to 2004. J Am Anim Hosp Assoc. 2011;47:28–36.
9. Schmidt, JM, North, SM, Freeman, KP, et al. Feline paediatric oncology: retrospective assessment of 233 tumours from cats up to one year (1993 to 2008). J Small Anim Pract. 2010;51:306–311.
10. Gabor, LJ, Malik, R, Canfield, PJ. Clinical and anatomical features of lymphosarcoma in 118 cats. Aust Vet J. 1998;76:725–732.
11. Gabor, LJ, Canfield, PJ, Malik, R. Immunophenotypic and histological characterization of 109 cases of feline lymphosarcoma. Aust Vet J. 1999;77:436–441.
12. Stutzer, B, Simon, K, Lutz, H, et al. Incidence of persistent viraemia and latent feline leukaemia virus infection in cats with lymphoma. J Feline Med Surg. 2011;13:81–87.
13. Weiss, AT, Klopfleisch, R, Gruber, AD. Prevalence of feline leukaemia provirus DNA in feline lymphomas. J Feline Med Surg. 2010;12:929–935.
14. Ahmad, S, Levy, LS. The frequency of occurrence and nature of recombinant feline leukemia viruses in the induction of multicentric lymphoma by infection of the domestic cat with FeLV-945. Virology. 2010;403:103–111.
15. Fuhino, Y, Satoh, H, Ohno, K, et al. Molecular cytogenetic analysis of feline leukemia virus insertions in cat lymphoid tumor cells. J Virol Methods. 2010;163:344–352.
16. Fujino, Y, Liao, CP, Zhao, YS, et al. Identification of a novel common proviral integration site, flit-1, in feline leukemia virus induced thymic lymphoma. Virology. 2009;30:16–22.
17. Fujino, Y, Ohno, K, Tsujimoto, H. Molecular pathogenesis of feline leukemia virus-induced malignancies: insertional mutagenesis. Vet Immunol Immunopathol. 2008;123:138–143.
18. Shelton, GH, Grant, CK, Cotter, SM, et al. Feline immunodeficiency virus (FIV) and feline leukemia virus (FeLV) infections and their relationship to lymphoid malignancies in cats: a retrospective study (1968-1988). J Acquir Immune Def Synd. 1990;3:623–630.
19. Hutson, CA, Rideout, BA, Pederson, NC. Neoplasia associated with feline immunodeficiency virus infection in cats of southern California. J Am Vet Med Assoc. 1991;199:1357–1362.
20. Endo, Y, Cho, KW, Nishigaki, K, et al. Molecular characteristics of malignant lymphomas in cats naturally infected feline immunodeficiency virus. Vet Immun Immunopath. 1997;57:153–167.
21. Terry, A, Callanan, JJ, Fulton, R, et al. Molecular analysis of tumours from feline immunodeficiency virus (FIV)-infected cats: an indirect role for FIV. Int J Cancer. 1995;61:227–232.
22. Wang, J, Kyaw-Tanner, M, Lee, C, et al. Characterisation of lymphosarcomas in Australian cats using polymerase chain reaction and immunohistochemical examination. Aust Vet J. 2001;79:41–46.
23. Beatty, JA, Lawrence, CE, Callanan, JJ, et al. Feline immunodeficiency virus (FIV)-associated lymphoma: a potential role for immune dysfunction in tumourigenesis. Vet Immunol Immunopathol. 1998;23:309–322.
24. Gabor, LJ, Love, DN, Malik, R, et al. Feline immunodeficiency virus status of Australian cats with lymphosarcoma. Aust Vet J. 2001;79:540–545.
25. Beatty, J, Terry, A, MacDonald, J, et al. Feline immunodeficiency virus integration in B-cell lymphoma identifies a candidate tumor suppressor gene on human chromosome 15q15. Cancer Res. 2002;62:7175–7180.
26. Poli, A, Abramo, F, Baldinotti, F, et al. Malignant lymphoma associated with experimentally induced feline immunodeficiency virus infection. J Comp Pathol. 1994;110:319–328.
27. Callanan, JJ, McCandlish, IA, O’Neil, B, et al. Lymphosarcoma in experimentally induced feline immunodeficiency virus infection. Vet Rec. 1992;130:293–295.
28. Rosenberg, MP, Hohenhaus, AE, Matus, RE. Monoclonal gammopathy and lymphoma in a cat infected with feline immunodeficiency virus. J Am Anim Hosp Assoc. 1991;27:335–337.
29. Buracco, P, Guglielmino, R, Abate, O, et al. Large granular lymphoma in a FIV-positive and FeLV-negative cat. J Small Anim Pract. 1992;33:279–284.
30. Zwahlen, CH, Lucroy, MD, Kraegel, SA, et al. Results of chemotherapy for cats with alimentary malignant lymphoma: 21 cases (1993-1997). J Am Vet Med Assoc. 1998;213:1144–1149.
31. Mahony, OM, Moore, AS, Cotter, SM, et al. Alimentary lymphoma in cats: 28 cases (1988-1993). J Am Vet Med Assoc. 1995;207:1593–1598.
32. Rassnick, KM, Mauldin, GN, Moroff, SD, et al. Prognostic value of argyrophilic nucleolar organizer region (AgNOR) staining in feline intestinal lymphoma. J Vet Intern Med. 1999;13:187–190.
33. Slawienski, MJ, Mauldin, GE, Mauldin, GN, et al. Malignant colonic neoplasia in cats: 46 cases (1990-1996). J Am Vet Med Assoc. 1997;211:878–881.
34. Mayr, B, Winkler, G, Schaffner, G, et al. N-ras mutations in a feline lymphoma: Low frequency of N-ras mutations in a series of feline, canine and bovine lymphomas. Vet J. 2002;163:326–328.
35. Cadile, CD, Kitchell, BE, Biller, BJ, et al. Telomerase activity as a marker for malignancy in feline tissues. Am J Vet Res. 2001;62:1578–1581.
36. Yazawa, M, Okuda, M, Uyama, R, et al. Molecular cloning of the feline telomerase reverse transcriptase (TERT) gene and its expression in cell lines and normal tissues. J Vet Med Sci. 2003;65:573–577.
37. Kano, R, Sato, E, Okamura, T, et al. Expression of Bcl-2 in feline lymphoma cell lines. Vet Clin Pathol. 2008;37:57–60.
38. Madewell, B, Griffey, S, Walls, J, et al. Reduced expression of cyclin-dependent kinase inhibitor p27Kip1 in feline lymphoma. Vet Pathol. 2001;38:698–702.
39. Dank, G, Lucroy, MD, Griffey, SM, et al. Bcl-2 and MIB-1 labeling indexes in cats with lymphoma. J Vet Intern Med. 2002;16:720–725.
40. Bertone, ER, Snyder, LA, Moore, AS. Environmental tobacco smoke and risk of malignant lymphoma in pet cats. Am J Epidemiol. 2002;156:268–273.
41. Marconato, L, Leo, C, Girelli, R, et al. Association between waste management and cancer in companion animals. J Vet Intern Med. 2009;23:564–569.
42. Schmiedt, CW, Grimes, JA, Holzman, G, et al. Incidence and risk factors for development of malignant neoplasia after feline renal transplantation and cyclosporine-based immunosuppression. Vet Comp Oncol. 2009;7:45–53.
43. Wooldridge, JD, Gregory, CR, Mathews, KG, et al. The prevalence of malignant neoplasia in feline renal-transplant recipients. Vet Surg. 2002;31:94–97.
44. Carreas, JK, Goldschmidt, M, Lamb, M, et al. Feline epitheliotropic intestinal malignant lymphoma: 10 cases(1997-2000). J Vet Intern Med. 2003;17:326–331.
45. Ragaini, L, Aste, G, Cavicchioli, L, et al. Inflammatory bowel disease mimicking alimentary lymphosarcoma in a cat. Vet Res Commun. 2003;27(Suppl 1):791–793.
46. Tams, TR. Inflammatory bowel disease. Philadelphia: WB Saunders; 1991. [pp 409–414].
47. Hart, JF, Shaker, E, Patnaik, AK, et al. Lymphocytic-plasmacytic enterocolitis in cats: 60 cases (1988-1990). J Am Anim Hosp Assoc. 1994;30:505–514.
47a. Bridgeford, ED, Marini, RP, Feng, Y, et al. Gastric helicobacter species as a cause of feline gastric lymphoma: a viable hypothesis. Vet Immunol Immunopathol. 2008;1123:106–113.
48. Valli, VE, Jacobs, RM, Norris, A, et al. The histologic classification of 602 cases of feline lymphoproliferative disease using the National Cancer Institute working formulation. J Vet Diagn Invest. 2000;12:295–306.
49. Valli, VE, Jacobs, RM, Parodi, AL, et al. Histological classification of hematopoietic tumors of domestic animals. Washington, DC: Armed Forces Institute of Pathology and The World Health Organization; 2002.
50. Gieger, T. Alimentary lymphoma in cats and dogs. Vet Clin North Am Small Anim Pract. 2011;41:419–432.
51. Moore, PF, Rodriguez-Bertos, A, Kass, PH. Feline gastrointestinal lymphoma: Mucosal architecture, immunophenotype and molecular clonality. Vet Pathol. 2011. [[Epub ahead of print]].
52. Lingard, AE, Briscoe, K, Beatty, JA, et al. Low-grade alimentary lymphoma: clinicopathological findings and response to treatment in 17 cases. J Feline Med Surg. 2009;11:692–700.
53. Pohlman, LM, Higginbotham, ML, Welles, EG, et al. Immunophenotypic and histologic classification of 50 cases of feline gastrointestinal lymphoma. Vet Pathol. 2009;46:259–268.
54. Kiupel, M, Scedley, RC, Pfent, C, et al. Diagnostic algorithm to differentiate lymphoma from inflammation in feline small intestinal biopsy samples. Vet Pathol. 2011;48:212–222.
55. Vezzali, E, Parodi, AL, Marcato, PS, et al. Histopathologic classification of 171 cases of canine and feline non-Hodgkin lymphoma according to the WHO. Vet Comp Oncol. 2010;8:38–49.
56. Swerdlow, SH, Campo, E, Harris, NL, et al. WHO classification of tumors of the haematopoietic and lymphoid tissues, ed 4. Lyon, France: International Agency for Research on Cancer (IARC); 2008.
57. Briscoe, KA, Krockenberger, M, Beatty, JA, et al. Histopathological and immunohistochemical evaluation of 53 cases of feline lymphoplasmacytic enteritis and low-grade alimentary lymphoma. J Comp Pathol. 2011;145:187–198.
58. Warren, A, Center, S, McDonough, S, et al. Histopathologic features, immunophenotyping, clonality, and eubacterial fluorescence in situ hybridization in cats with lymphocytic cholangitis/cholangiohepatitis. Vet Pathol. 2011;48:627–641.
59. Krick, EL, Little, L, Patel, R, et al. Description of clinical and pathological findings, treatment and outcome of feline large granular lymphocyte lymphoma (1996-2004). Vet Comp Oncol. 2008;6:102–111.
60. Roccabianca, P, Vernau, W, Caniatti, M, et al. Feline large granular lymphocyte (LGL) lymphoma with secondary leukemia: primary intestinal origin with predominance of a CD3/CD8(alpha)(alpha) phenotype. Vet Pathol. 2006;43:15–28.
61. Ezura, K, Nomura, I, Takahashi, T, et al. Natural killer-like T cell lymphoma in a cat. Vet Rec. 2004;28:268–270.
62. Day, MJ. Review of thymic pathology in 30 cats and 36 dogs. J Small Anim Prac. 1997;38:393–403.
63. Davies, C, Forrester, SD. Pleural effusion in cats: 82 cases (1987 to 1995). J Small Anim Prac. 1996;37:217–224.
64. Teske, E, Sraten, GV, van Noort, R, et al. Chemotherapy with cyclophosphamide, vincristine and prednisolone (COP) in cats with malignant lymphoma: New results with an old protocol. J Vet Intern Med. 2002;16:179–186.
65. Day, MJ, Kyaw-Tanner, M, Silkstone, MA, et al. T-cell-rich B-cell lymphoma in the cat. J Comp Pathol. 1999;120:155–167.
66. Walton, RM, Hendrick, MJ. Feline Hodgkin’s-like lymphoma: 20 cases (1992-1999). Vet Pathol. 2001;38:504–511.
67. Holt, E, Goldschmidt, MH, Skorupski, K. Extranodal conjunctival Hodgkin’s-like lymphoma in a cat. Vet Ophthalmol. 2006;9:141–144.
68. Taylor, SS, Goodfellow, MR, Browne, WJ, et al. Feline extranodal lymphoma: response to chemotherapy and survival in 110 cats. J Small Anim Pract. 2009;50:584–592.
69. Little, L, Patel, R, Goldschmidt, M. Nasal and nasopharyngeal lymphoma in cats: 50 cases (1989-2005). Vet Pathol. 2007;44:885–892.
70. Henderson, SM, Bradley, K, Day, MJ, et al. Investigation of nasal disease in the cat- a retrospective study of 77 cases. J Feline Med Surg. 2004;6:245–257.
71. Mukaratirwa, S, van der Linde-Sipman, JS, Gruys, E, et al. Feline nasal and paranasal sinus tumours: clinicopathological study, histomorphological description and diagnostic immunohistochemistry of 123 cases. J Feline Med Surg. 2001;3:235–245.
72. Demko, JL, Cohn, LA. Chronic nasal discharge in cats: 75 cases (1993-2004). J Am Vet Med Assoc. 2007;230:1032–1037.
73. Haney, SM, Beaver, L, Turrel, J, et al. Survival analysis of 97 cats with nasal lymphoma: a multi-institutional retrospective study (1986-2006). J Vet Intern Med. 2009;23:287–294.
74. Mooney, SC, Hayes, AA, Matus, RE, et al. Renal lymphoma in cats: 28 cases (1977-1984). J Am Vet Med Assoc. 1987;191:1473–1477.
75. Tomek, A, Cizinauskas, S, Doherr, M, et al. Intracranial neoplasia in 61 cats: localization, tumour types and seizure patterns. J Feline Med Surg. 2006;8:243–253.
76. Troxel, MT, Vite, CH, Van Winkle, TJ, et al. Feline intracranial neoplasia: retrospective review of 160 cases (1985-2001). J Vet Intern Med. 2003;17:850–859.
77. Marioni-Henry, K, Van Winckle, TJ, Smith, SH, et al. Tumors affecting the spinal cord of cats: 85 cases (1980-2005). J Am Vet Med Assoc. 2008;232:237–243.
78. Marioni-Henry, K, Vite, CH, Newton, AL, et al. Prevalence of diseases of the spinal cord of cats. J Vet Intern Med. 2004;18:851–858.
79. Taylor, SS, Harvey, AM, Bar, FJ, et al. Laryngeal disease in cats: a retrospective study of 35 cases. J Feline Med Surg. 2009;11:954–962.
80. Fontaine, J, Heimann, M, Day, MJ. Cutaneous epitheliotropic T-cell lymphoma in the cat: a review of the literature and five new cases. Vet Dermatol. 2011;22:454–461.
81. Caciolo, PL, Nesbitt, GH, Patnaik, AK, et al. Cutaneous lymphosarcoma in the cat: a report of nine cases. J Am Anim Hosp Assoc. 1984;20:491–496.
82. May, MJ. Immunophenotypic characterization of cutaneous lymphoid neoplasia in the dog and cat. J Comp Pathol. 1995;112:79–96.
83. Gilbert, S, Affolter, VK, Gross, TL, et al. Clinical, morphological and immunohistochemical characterization of cutaneous lymphocytosis in 23 cats. Vet Dermatol. 2004;15:3–12.
84. Wood, C, Almes, K, Bagladi-Swanson, M, et al. Sézary syndrome in a cat. J Am Anim Hosp Assoc. 2008;44:144–148.
85. Schick, RO, Murphy, GF, Goldschmidt, MH. Cutaneous lymphosarcoma and leukemia in a cat. J Am Vet Med Assoc. 1993;203:1155–1158.
86. Grahn, BH, Peiffer, RL, Cullen, CL, et al. Classification of feline intraocular neoplasms based on morphology, histochemical staining and immunohistochemical labeling. Vet Ophthalmol. 2006;9:395–403.
87. Kiselow, MA, Rassnick, KM, McDonough, SP, et al. Outcome of cats with low-grade lymphocytic lymphoma: 41 cases (1995-2005). J Am Vet Med Assoc. 2008;232:405–410.
88. Fondacaro, JV, Richter, KP, Carpenter, JL, et al. Feline gastrointestinal lymphoma:67 cases (1988-1996). Eur J Comp Gastroenterol. 4, 1999.
89. Court, EA, Watson, ADJ, Peaston, AE. Retrospective study of 60 cases of feline lymphosarcoma. Aust Vet J. 1997;75:424–427.
90. Forrester, SD, Fossum, TW, Rogers, KS, et al. Diagnosis and treatment of chylothorax associated with lymphoblastic lymphosarcoma in four cats. J Am Vet Med Assoc. 1991;198:291–294.
91. Spodnick, GJ, Berg, J, Moore, FM, et al. Spinal lymphoma in cats: 21 cases (1976-1989). J Am Vet Med Assoc. 1992;200:373–376.
92. Lane, SB, Kornegay, JN, Duncan, JR, et al. Feline spinal lymphosarcoma: a retrospective evaluation of 23 cats. J Vet Intern Med. 1994;8:99–104.
93. Savary, KCM, Price, GS, Vaden, SL. Hypercalcemia in cats: A retrospective study of 71 cases (1991-1997). J Vet Intern Med. 2000;14:184–189.
94. Gabor, LJ, Canfield, PJ, Malik, R. Haematological and biochemical findings in cats in Australia with lymphosarcoma. Aust Vet J. 2000;78:456–461.
95. Gerou-Ferriani, M, McBrearty, AR, Burchmore, RJ, et al. Agarose gel serum protein electophoresis in cats with and without lymphoma and preliminary results of tandem mass fingerprinting analysis. Vet Clin Pathol. 2011;40:159–173.
96. Avery, A. Molecular diagnostics of hematologic malignancies. Top Companion Anim Med. 2009;24:144–150.
97. Werner, JA, Woo, JC, Vernau, W, et al. Characterization of feline immunoglobulin heavy chain variable region genes for the molecular diagnosis of B-cell neoplasia. Vet Pathol. 2005;42:596–607.
98. Moore, PF, Woo, JC, Vernau, W, et al. Characterization of feline T cell receptor gamma (TCRG) variable region genes for the molecular diagnosis of feline intestinal T cell lymphoma. Vet Immunol Immunopathol. 2005;106:167–178.
99. Weiss, AT, Klopfleisch, R, Gruber, AD. T-cell receptor γ chain variable and joining region genes of subgroup 1 are clonally rearranged in feline B- and T-cell lymphoma. J Comp Pathol. 2011;144:123–134.
100. Henrich, M, Hecht, W, Weiss, AT, et al. A new subgroup of immunoglobulin heavy chain variable region genes for the assessment of clonality in feline B-cell lymphomas. Vet Immunol Immunopathol. 2009;130:59–69.
101. Mooney, SC, Hayes, AA. Lymphoma in the cat: An approach to diagnosis and management. Sem Vet Med Surg (Small Anim). 1986;1:51–57.
102. Zwingenberger, AL, Marks, SL, Baker, TW, et al. Ultrasonographic evaluation of the muscularis propria in cats with diffuse small intestinal lymphoma or inflammatory bowel disease. J Vet Intern Med. 2010;24:289–292.
103. Evans, SE, Bonczynski, JJ, Broussard, JD, et al. Comparison of endoscopic and full-thickness biopsy specimens for diagnosis of inflammatory bowel disease and alimentary tract lymphoma in cats. J Am Vet Med Assoc. 2006;229:1447–1450.
104. Kleinschmidt, S, Harder, J, Nolte, I, et al. Chronic inflammatory and non-inflammatory diseases of the gastrointestinal tract in cats: diagnostic advantage of full-thickness intestinal and extraintestinal biopsies. J Feline Med Surg. 2010;12:97–103.
105. Fossum, TW, Jacobs, RM, Birchard, SJ. Evaluation of cholesterol and triglyceride concentrations in differentiating chylous and nonchylous pleural effusions in dogs and cats. J Am Vet Med Assoc. 1986;188:49–51.
106. Tromblee, TC, Jones, JC, Etue, AE, et al. Association between clinical characteristics, computed tomography characteristics, and histologic diagnosis for cats with sinonasal disease. Vet Radiol Ultrasound. 2006;47:241–248.
107. Detweiler, DA, Johnson, LR, Kass, PH, et al. Computed tomographic evidence of bulla effusions in cats with sinonasal diseases: 2001-2004. J Vet Intern Med. 2006;20:1080–1084.
108. Valdes-Martinez, A, Cianciolo, R, Mai, W. Association between renal hypoechoic subcapsular thickening and lymphosarcoma in cats. Vet Radiol Ultrasound. 2007;48:357–360.
109. Tzannes, S, Hammond, MF, Murphy, S, et al. Owners’ perception of their cats’ quality of life during COP chemotherapy for lymphoma. J Feline Med Surg. 2008;10:73–81.
110. Malik, R, Gabor, LJ, Foster, SF, et al. Therapy for Australian cats with lymphosarcoma. Aust Vet J. 2001;79:808–817.
111. Hadden, AG, Cotter, SM, Rand, W, et al. Efficacy and toxicosis of VECAP-C treatment of lymphoma in cats. J Vet Intern Med. 2008;22:153–157.
112. Simon, D, Eberle, N, Laacke-Singer, L, et al. Combination chemotherapy in feline lymphoma: Treatment, outcome, tolerability and duration in 23 cats. J Vet Intern Med. 2008;22:394–400.
113. Milner, RJ, Peyton, J, Cooke, K, et al. Response rates and survival times for cats with lymphoma treated with the University of Wisconsin-Madison chemotherapy protocol: 38 cases (1996-2003). J Am Vet Med Assoc. 2005;227:1118–1122.
114. Moore, AS, Cotter, SM, Frimberger, AE, et al. A comparison of doxorubicin and COP for maintenance of remission in cats with lymphoma. J Vet Intern Med. 1996;10:372–375.
115. Mooney, SC, Hayes, AA, MacEwen, EG, et al. Treatment and prognostic factors in lymphoma in cats: 103 cases (1977-1981). J Am Vet Med Assoc. 1989;194:696–699.
116. Jeglum, KA, Whereat, A, Young, K. Chemotherapy of lymphoma in 75 cats. J Am Vet Med Assoc. 1987;190:174–178.
117. Poirier, VJ, Thamm, DH, Kurzman, ID, et al. Liposome-encapsulated doxorubicin (Doxil) and doxorubicin in the treatment of vaccine-associated sarcoma in cats. J Vet Intern Med. 2002;16:726–731.
118. Peaston, AE, Maddison, JE. Efficacy of doxorubicin as an induction agent for cats with lymphosarcoma. Aust Vet J. 1999;77:442–444.
119. Kristal, O, Lana, SE, Ogilvie, GK, et al. Single agent chemotherapy with doxorubicin for feline lymphoma: a retrospective study of 19 cases (1994-1997). J Vet Intern Med. 2001;15:125–130.
120. Oberthaler, KT, Mauldin, E, McManus, PM, et al. Rescue therapy with doxorubicin-based chemotherapy for relapsing or refractory feline lymphoma: a retrospective study of 23 cases. J Feline Med Surg. 2009;11:259–265.
121. Fan, TM, Kitchell, BE, Dhaliwal, RS, et al. Hematological toxicity and therapeutic efficacy of lomustine in 20 tumor-bearing cats: critical assessment of a practical dosing regimen. J Am Anim Hosp Assoc. 2002;38:357–363.
122. Rassnick, KM, Gieger, TL, Williams, LE, et al. Phase I evaluation of CCNU (lomustine) in tumor-bearing cats. J Vet Intern Med. 2001;15:196–199.
123. LeBlanc, AK, Cox, SK, Kirk, CA, et al. Effects of L-asparaginase on plasma amino acid profiles and tumor burden in cats with lymphoma. J Vet Intern Med. 2007;21:760–763.
124. Cotter, SM. Treatment of lymphoma and leukemia with cyclophosphamide, vincristine, and prednisone: II. Treatment of cats. J Am Anim Hosp Assoc. 1983;19:166–172.
125. Stein, TJ, Pellin, M, Steinberg, H, et al. Treatment of feline gastrointestinal small-cell lymphoma with chlorambucil and glucocorticoids. J Am Anim Hosp Assoc. 2010;46:413–417.
126. Williams, LE, Pruitt, AF, Thrall, DE. Chemotherapy followed by abdominal cavity irradiation for feline lymphoblastic lymphoma. Vet Radiol Ultrasound. 2010;51:681–687.
127. Parshley, DL, LaRue, SM, Kitchell, B, et al. Abdominal irradiation as a rescue therapy for feline gastrointestinal lymphoma: a retrospective study of 11 cats (2001-2008). J Feline Med Surg. 2011;13:63–68.
128. Sfiligoi, GA, Theon, AP, Kent, MS. Response of 19 cats with nasal lymphoma to radiation therapy and chemotherapy. Vet Rad Ultrasound. 2007;48:388–392.
129. Elmslie, RE, Ogilvie, GK, Gillette, EL, et al. Radiotherapy with and without chemotherapy for localized lymphoma in 10 cats. Vet Radiol. 1991;32:277–280.
130. Komori, S, Nakamura, S, Takahashi, K, et al. Use of lomustine to treat cutaneous nonepitheliotropic lymphoma in a cat. J Am Vet Med Assoc. 2005;226:237–239.
131. Grindem, CB. Ultrastructural morphology of leukemia cells in the cat. Vet Pathol. 1988;22(2):147–155.
132. Gorman, NT, Evans, RJ. Myeloproliferative disease in the dog and cat: clinical presentations, diagnosis and treatment. Vet Rec. 1987;121:490–496.
133. Grindem, CB, Perman, V, Stevens, JB. Morphological and clinical and pathological characteristics of spontaneous leukemia in 10 cats. J Am Anim Hosp Assoc. 1985;21:227.
134. Blue, JT, French, TW, Scarlett-Kranz, J. Non-lymphoid hematopoietic neoplasia in cats: a retrospective study of 60 cases. Cornell Vet. 1988;78:21–42.
135. Facklam, NR, Kociba, GJ. Cytochemical characterization of feline leukemic cells. Vet Pathol. 1986;23:155–161.
136. Weiss, DJ. Differentiating benign and malignant causes of lymphocytosis in feline bone marrow. J Vet Intern Med. 2005;19:855–859.
137. Hisasue, M, Okayama, H, Okayama, T, et al. Hematologic abnormalities and outcome of 16 cats with myelodysplastic syndromes. J Vet Intern Med. 2001;15:471–477.
138. Essex, ME. Feline leukemia: a naturally occurring cancer of infectious origin. Epidemiol Rev. 1982;4:189–203.
139. Workman, HC, Vernau, W. Chronic lymphocytic leukemia in dogs and cats: the veterinary perspective. Vet Clin North Am Small Anim Pract. 2003;33:1379–1399.
140. Tebb, A, Cave, T, Barron, R, et al. Diagnosis and management of B cell chronic lymphocytic leukaemia in a cat. Vet Rec. 2004;154:430–433.
 Section C
Section C
Canine Acute Myeloid Leukemia, Myeloproliferative Neoplasms, and Myelodysplasia
Karen M. Young and David M. Vail
Myeloproliferative disorders (MPDs) are a group of neoplastic diseases of bone marrow in which there are clonal disorders of hematopoietic stem cells.1 Aberrant proliferation of cells with defective maturation and function leads to reduction of normal hematopoiesis and invasion of other tissues. These disorders have been classified based on biologic behavior, degree of cellular differentiation, and lineage of the neoplastic cells (granulocytic, monocytic, erythroid, megakaryocytic, or mixed). Newer classification systems in humans have incorporated genetics and molecular genetic analysis; these are currently areas of active investigation in the study of animal leukemias.2 In 1991 the Animal Leukemia Study Group made recommendations for classifying nonlymphoid leukemias in dogs and cats.3 More recently, the Oncology Committee of the American College of Veterinary Pathologists (ACVP) has been reexamining criteria for a classification system and spearheading large multiinstitutional studies to validate the criteria. Long-term objectives of these studies are to define molecular lesions, establish prognostic markers, and target effective therapeutic approaches.4
Incidence and Risk Factors
Myeloid neoplasms are uncommon or rare in the dog and occur 10 times less frequently than lymphoproliferative disorders.5 Accurate information about incidence and other epidemiologic information await consistent use of a uniform classification system (see later discussion). There is no known age, breed, or sex predisposition, although in some retrospective studies, large-breed dogs have been overrepresented.6-14 In dogs, the etiology of spontaneously occurring leukemia is unknown. It is likely that genetic and environmental factors (including exposure to radiation, drugs, or toxic chemicals) play a role. In humans, acquired chromosomal derangements lead to clonal overgrowth with arrested development.15 At the end of the last century, chromosomal abnormalities were reported in dogs with AML, chronic myelogenous leukemia (CML), and lymphoid leukemia.16,17 However, because karyotyping is difficult to perform in dogs because of the large number and morphologic similarity of their chromosomes and their resistance to banding, defining genetic factors in canine myeloid neoplasms has awaited application of molecular technologies and use of the canine genome map.2,18-21 Certain forms of leukemia in dogs have been produced experimentally following irradiation.22-24 In contrast to MPDs in cats, no causative viral agent has been demonstrated in dogs, although retrovirus-like budding particles were observed in the neoplastic cells of a dog with granulocytic leukemia.25
Pathology and Natural Behavior
A review of normal hematopoiesis will aid in understanding the various manifestations of MPDs. Hematopoiesis is the process of proliferation, differentiation, and maturation of stem cells into terminally differentiated blood cells. A simplified scheme is presented in Figure 32-17. Pluripotent stem cells differentiate into either lymphopoietic or hematopoietic multipotent stem cells.26 Under the influence of specific regulatory and microenvironmental factors, multipotent stem cells in bone marrow differentiate into progenitor cells committed to a specific hematopoietic cell line, for example, erythroid, granulocytic-monocytic, or megakaryocytic. Maturation results in the production of terminally differentiated blood cells—erythrocytes, granulocytes, monocytes, and platelets—that are delivered to the circulation. In some cases, as in the maturation of reticulocytes to erythrocytes, final development may occur in the spleen.
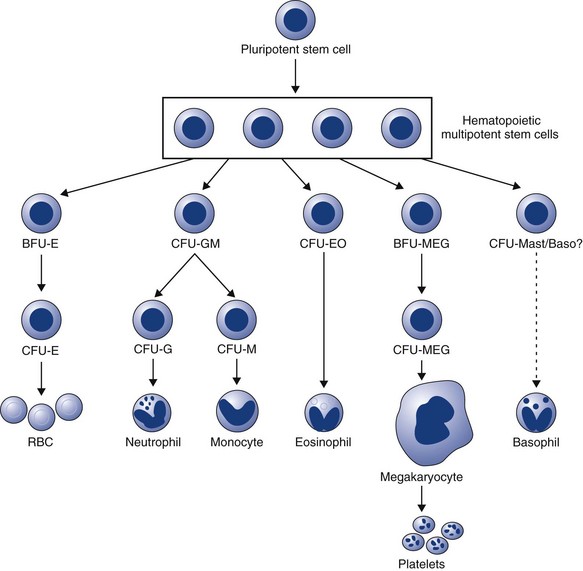
Figure 32-17 A simplified scheme of hematopoiesis. BFU, Blast-forming units; CFU, colony-forming units; E, erythroid; GM, granulocytic-monocytic; EO, eosinophil; MEG, megakaryocyte.
Proliferation and differentiation of hematopoietic cells are controlled by a group of regulatory growth factors.26,27 Of these, erythropoietin is the best characterized; it regulates erythroid proliferation and differentiation and is produced in the kidney, where changes in oxygen tension are detected. The myeloid compartment depends on a group of factors, collectively referred to as colony-stimulating factors (CSFs). These factors act at the level of the committed progenitor cells but also influence the functional capabilities of mature cells. Some of these factors have a broad spectrum of activity; others are more restricted in their target cells and actions. CSFs are produced in vitro by a multitude of cell types, including monocytes, macrophages, lymphocytes, and endothelial cells, and these cells likely play a role in the production and regulation of these factors in vivo. The gene for thrombopoietin also has been cloned, and it appears that this hormone alone can induce differentiation of megakaryocytes and platelet production.28 Recombinant forms of many of these hormones are increasingly available.
Clonal disorders of bone marrow include myeloaplasia (usually referred to as aplastic anemia), myelodysplasia, and myeloproliferation. A preleukemic syndrome, characterized by peripheral pancytopenia and bone marrow hyperplasia with maturation arrest, is more correctly termed myelodysplasia because the syndrome does not always progress to overt leukemia. This syndrome has been described in cats, usually in association with FeLV infection but has only rarely been recognized in dogs.29-32 These clonal disorders may be manifested by abnormalities in any or all lineages because hematopoietic cells share a common stem cell. In addition, transformation from one form to another may occur.33
Myeloid neoplasms are classified in several ways. The terms acute and chronic refer to the degree of cellular differentiation of the leukemic cells, but these terms also correlate with the biologic behavior of the neoplasm.34 Disorders resulting from uncontrolled proliferation or decreased apoptosis of cells incapable of maturation lead to the accumulation of poorly differentiated or “blast” cells. These disorders are included under the umbrella term, acute myeloid leukemia (AML). Disorders resulting from unregulated proliferation of cells that exhibit progressive, albeit incomplete and defective, maturation lead to the accumulation of differentiated cells. These disorders are termed myeloproliferative neoplasms (MPN) and include polycythemia vera, CML and its variants, essential thrombocythemia, and possibly primary myelofibrosis. Myeloid neoplasms are further classified by the lineage of the dominant cell type(s), defined by Romanowsky stains, special cytochemical stains, ultrastructural features, flow cytometric analysis, and immunologic cell markers, and they have been classified into subtypes (see later discussion).
AML has a more sudden onset and is more aggressive. In both acute and chronic disorders, however, abnormalities in proliferation, maturation, and functional characteristics can occur in any hematopoietic cell line.1 In addition, normal hematopoiesis is adversely affected. Animals with leukemia usually have decreased numbers of circulating normal cells. The pathogenesis of the cytopenias is complex and may result in part from production of inhibitory factors. Eventually, neoplastic cells displace normal hematopoietic cells, and this is termed myelophthisis. Anemia and thrombocytopenia are particularly common. Neutropenia and thrombocytopenia result in infection and hemorrhage, which may be more deleterious to the animal than the primary disease process.
Acute Myeloid Leukemia
AML is rare and is characterized by aberrant proliferation and/or decreased apoptosis of a clone of cells without maturation. This results in accumulation of immature blast cells in bone marrow and peripheral blood (Figure 32-18, A to E). The WBC count is variable and ranges from leukopenia to counts up to 150,000/µL. Spleen, liver, and lymph nodes are frequently involved, and other tissues, including tonsils, kidney, heart, and the CNS, may be infiltrated as well. There is no characteristic age, and even very young dogs may be affected.35 The clinical course of these disorders tends to be rapid. Production of normal peripheral blood cells is usually diminished or absent, and anemia, neutropenia, and thrombocytopenia are common with infection and hemorrhage occurring as frequent sequelae. Occasionally, neoplastic blasts are present in bone marrow but not in peripheral blood. This is termed aleukemic leukemia, whereas subleukemic suggests a normal or decreased WBC count with some neoplastic cells in circulation.
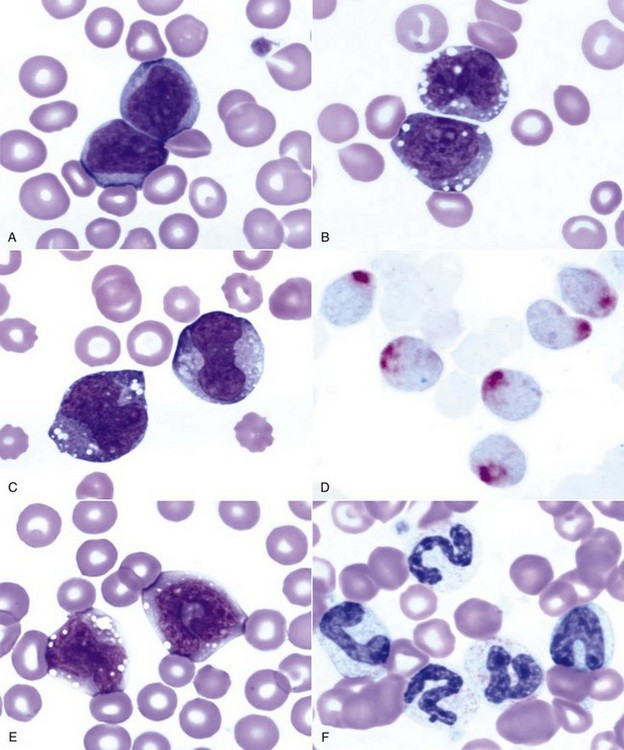
Figure 32-18 Peripheral blood from dogs with myeloid neoplasms. All diagnoses were confirmed by cytochemical staining. Note how similar the blast cells appear in A to C. A, Acute myeloblastic leukemia (M1). (Wright’s stain, ×100 objective.) B, Acute myelomonocytic leukemia (M4). (Wright’s stain, ×100 objective.) C, Acute monocytic leukemia (M5a); Wright’s stain. D, Acute monocytic leukemia (M5a). (Cytochemical stain: a-naphthyl butyrate esterase [nonspecific esterase] with red reaction product.) E, Acute monocytic leukemia with some differentiation (M5b). (Wright’s stain, ×100 objective.) F, Chronic myelogenous leukemia (CML). (Wright’s stain, ×100 objective.)
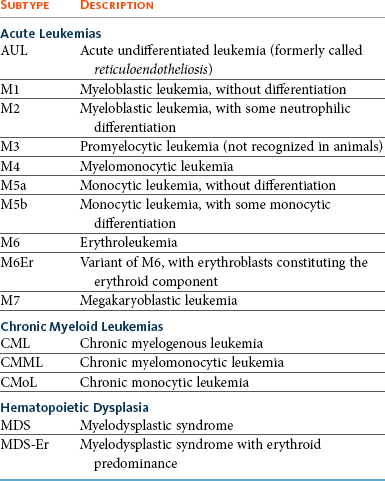
In 1985 the Animal Leukemia Study Group was formed under the auspices of the American Society for Veterinary Clinical Pathology to develop specific morphologic and cytochemical criteria for classifying acute nonlymphocytic leukemias. Recognition of specific subtypes of leukemia is required to compile accurate and useful information about prognosis and response to treatment, as well as to compare studies from different sites. In 1991, this group proposed a classification system following adaptation of the French-American-British (FAB) system and criteria established by the NCI Workshop.3 Group members examined blood and bone marrow from 49 dogs and cats with myeloid neoplasms. Romanowsky-stained specimens were examined first to identify blast cells and their percentages. Lineage specificity was then determined using cytochemical markers. The percentage of blasts and the information about lineage specificity were used in combination to classify disorders as acute undifferentiated leukemia (AUL), acute myeloid leukemia (AML, subtypes M1 to M5 and M7), and erythroleukemia with or without erythroid predominance (M6 and M6Er). A description of these subtypes is presented in Table 32-12.
Canine karyotyping is difficult, but with advancements in molecular cytogenetic analysis, chromosome painting, and genomic hybridization, AML in dogs can now be analyzed at the base-pair level,18,19 and missense mutations in FLT3, C-KIT, and RAS sequences have been identified in dogs with AML, similar to what has been found for human AML.36 In addition to serving as diagnostic and prognostic markers, cytogenetic lesions may be therapeutic targets. As cytogenetic abnormalities continue to be identified, this information will need to be incorporated into classification schemes.
With the exception of acute promyelocytic leukemia or M3, all of these subtypes have been described in dogs. However, because this modified FAB system has been adopted only recently, the names given to these disorders in the literature vary considerably. In addition, in the absence of cytochemical staining, immunophenotyping, or electron microscopic evaluation, the specific subtype of leukemia has often been uncertain, making retrospective analysis of epidemiologic information, prognosis, and response to therapy confusing at best. Although defining specific subtypes may seem to be an academic exercise owing to the uniformly poor prognosis of acute leukemias, this information is critical to improving the management of these diseases. Because of the low incidence of AML, national and international cooperative efforts will be required to accumulate information on the pathogenesis and response to different treatment modalities of specific subtypes. Utilization of a uniform classification system is an essential first step.
Different forms of AML are demonstrated in Figure 32-18, A to E. The most frequently reported forms of AML in the dog are acute myeloblastic leukemia (M1 and M2) and acute myelomonocytic leukemia (M4).* Megakaryoblastic leukemia (M7) also is well recognized in dogs10,47-58 and may be associated with platelet dysfunction.51 Monocytic leukemias have likely included those with and without monocytic differentiation (M5a and M5b),11,59 but in some cases the diagnosis may have been chronic myelomonocytic or chronic monocytic leukemia (see later discussion). There are few reports in dogs of spontaneously occurring erythroleukemia (M6) in which the leukemic cells include myeloblasts, monoblasts, and erythroid elements.60-62 AULs have uncertain lineages because they are negative for all cytochemical markers. These leukemias should be distinguished from lymphoid leukemias by flow cytometric analysis of the leukemic cells for cellular antigens that identify their lineage.63 In addition, examination of blast cells by electron microscopy may reveal characteristic ultrastructural features.
Myeloproliferative Neoplasms
MPNs, previously termed chronic myeloproliferative disorders, are characterized by excessive production of differentiated bone marrow cells, resulting in the accumulation of erythrocytes (polycythemia vera), granulocytes and/or monocytes (CML and its variants), or platelets (essential thrombocythemia). Primary myelofibrosis as a clonal disorder of marrow stromal cells, characterized by proliferation of megakaryocytes and granulocytic precursors with accumulation of collagen in bone marrow, has been recognized only rarely in animals. Myelofibrosis is considered a response to injury and may occur secondary to other neoplasms, systemic inflammation, drug exposure, or FeLV infection in cats.
Polycythemia Vera
Polycythemia vera (PV) is a clonal disorder of stem cells, although whether the defect is in the pluripotent stem cell or the hematopoietic multipotent stem cell is still not clear. In humans, progenitor cells have an increased sensitivity to insulin-like growth factor 1, which stimulates hematopoiesis.64 It is not known whether this hypersensitivity is the primary defect or is secondary to another gene mutation. In any case, the result is overproduction of red blood cells (RBCs). The disease is rare and must be distinguished from more common causes of polycythemia, including relative and secondary absolute polycythemia (see later discussion). In PV, there is neoplastic proliferation of the erythroid series with terminal differentiation to RBCs. The disease has been reported in dogs that tend to be middle-aged with no breed or sex predilection65-73 and is characterized by an increased RBC mass evidenced by an increased packed cell volume (PCV), RBC count, and hemoglobin concentration. The PCV is typically in the range of 65% to 85%. The bone marrow is hyperplastic, although the myeloid : erythroid (M : E) ratio tends to be normal. In contrast to the disease in humans, other cell lines do not appear to be involved, and transformation to other MPNs has not been reported. The disease in dogs may be more appropriately termed primary erythrocytosis. In humans, acquired JAK2 gene mutations are identified in 90% of patients with primary polycythemia, and recently an identical mutation in the JAK2 gene of one of five dogs with primary polycythemia was reported.74
Chronic Myelogenous Leukemia
In dogs, CML is more similar to chronic neutrophilic leukemia, a rare form of MPN in humans, than to CML in humans because it is a neoplastic proliferation of the neutrophil series, although concurrent eosinophilic and basophilic differentiation can occur. CML can occur in dogs of any age.35,75-79 Neutrophils and neutrophilic precursors accumulate in bone marrow and peripheral blood as well as in other organs. The peripheral WBC count is usually, but not always, greater than 100,000/µL. Both immature and mature neutrophils are present, as demonstrated in Figure 32-18, F. Mature forms are usually more numerous, but sometimes an “uneven” left shift is present. Signs of dysplasia may be evident, including hypersegmentation, ringed nuclei, and giant forms. Eosinophils and basophils may also be increased. The bone marrow is characterized by granulocytic hyperplasia, and morphologic abnormalities may not be present. Erythroid and megakaryocytic lines may be affected, resulting in anemia, thrombocytopenia, or less commonly, thrombocytosis. This disorder must be distinguished from severe neutrophilic leukocytosis and “leukemoid reactions” caused by inflammation or immune-mediated diseases. Leukemoid reactions can also occur as a paraneoplastic syndrome. In humans with CML, characteristic cytogenetic abnormalities are present in all bone marrow cells, signifying a lesion at the level of an early multipotent stem cell. Typically, these individuals have a chromosomal translocation, resulting in the Philadelphia chromosome or BCR-ABL translocation between chromosomes 9 and 22.80 The analogous chromosomes in dogs are chromosomes 9 and 26, and BCR-ABL mutations have now been reported in three cases of CML in dogs.2 Variants of CML are chronic myelomonocytic leukemia (CMML) and chronic monocytic leukemia (CMoL).81-83 These diagnoses are made based on the percentage of monocytes in the leukemic cell population. BCR-ABL translocation has also been reported in a dog with CMoL.45
In addition to accumulating in bone marrow and peripheral blood, leukemic cells also are found in the red pulp of the spleen, the periportal and sinusoidal areas of the liver, and sometimes lymph nodes. Other organs such as the kidney, heart, and lung are less commonly affected. In addition, extramedullary hematopoiesis may be present in the liver and spleen. Death is usually due to complications of infection or hemorrhage secondary to neutrophil dysfunction and thrombocytopenia. In some cases, CML may terminate in “blast crisis,” in which there is a transformation from a predominance of well-differentiated granulocytes to excessive numbers of poorly differentiated blast cells in peripheral blood and bone marrow. This phenomenon is well documented in the dog.75,76,78
Basophilic and Eosinophilic Leukemia
Basophilic leukemia, although rare, has been reported in dogs and is characterized by an increased WBC count with a high proportion of basophils in peripheral blood and bone marrow.84-86 Hepatosplenomegaly, lymphadenopathy, and thrombocytosis may be present. All the dogs have been anemic. Basophilic leukemia should be distinguished from mast cell leukemia (mastocytosis). Whether dogs develop eosinophilic leukemia remains in question. Reported cases have had high blood eosinophil counts and eosinophilic infiltrates in organs.87,88 One dog responded well to treatment with corticosteroids. The distinction between neoplastic proliferation of eosinophils and idiopathic hypereosinophilic syndrome remains elusive. Disorders associated with eosinophilia such as parasitism, skin diseases, or diseases of the respiratory and GI tracts should be considered first in an animal with eosinophilia. One distinguishing feature should be clonality, with reactive eosinophilia comprising polyclonal cells and the neoplastic condition arising from a single clone. As clonality assays become more available, this discrepancy may be resolved.
Essential Thrombocythemia
In humans, essential thrombocythemia, or primary thrombocytosis, is characterized by platelet counts that are persistently greater than 600,000/µL. There are no blast cells in circulation, and marked megakaryocytic hyperplasia of the bone marrow without myelofibrosis is present. Thrombosis and bleeding are the most common sequelae, and most patients have splenomegaly. Other MPDs, especially PV, should be ruled out, and importantly, there should be no primary disorders associated with reactive thrombocytosis.89 These include inflammation, hemolytic anemia, iron deficiency anemia, malignancies, recovery from severe hemorrhage, rebound from immune-mediated thrombocytopenia, and splenectomy. In addition, certain drugs such as vincristine can induce thrombocytosis. Essential thrombocythemia has been recognized in dogs.33,90-93 In one dog, the platelet count exceeded 4 million/µL and bizarre giant forms with abnormal granulation were present. The bone marrow contained increased numbers of megakaryocytes and megakaryoblasts, but circulating blast cells were not seen. Other findings included splenomegaly, GI bleeding, and increased numbers of circulating basophils. Causes of secondary or reactive thrombocytosis were ruled out.90 Basophilia was also reported in a more recent case.92 In another dog, primary thrombocytosis was diagnosed and then progressed to CML.33 In some cases reported in the literature as essential thrombocythemia, the dogs had microcytic hypochromic anemias. Because iron deficiency anemia is associated with reactive or secondary thrombocytosis, care must be taken to rule out this disorder. However, spurious microcytosis may be reported if a dog has many giant platelets that are counted by an analyzer as small RBCs.93 Microscopic review of the blood film may be helpful in these cases.
Other Bone Marrow Disorders
Primary myelofibrosis has been reported only rarely in dogs and is usually a secondary, or reactive, process.94,95 In humans, myelofibrosis is characterized by collagen deposition in bone marrow and increased numbers of megakaryocytes and granulocytic precursors, many of which exhibit morphologic abnormalities. In fact, breakdown of intramedullary megakaryocytes and subsequent release of factors that promote fibroblast proliferation or inhibit collagen breakdown may be the underlying pathogenesis of the fibrosis.96 Focal osteosclerosis is sometimes present. Anemia, thrombocytopenia, splenomegaly, and myeloid metaplasia (production of hematopoietic cells outside the bone marrow) are consistent features.
In dogs, myelofibrosis occurs secondary to MPDs, radiation damage, and congenital hemolytic anemias.97-100 In some cases, the inciting cause is unknown (idiopathic myelofibrosis). There may be concurrent marrow necrosis in cases of ehrlichiosis, septicemia, or drug toxicity (estrogens, cephalosporins), and there is speculation that fibroblasts proliferate in response to release of inflammatory mediators associated with the necrosis.94 Myeloid metaplasia has been reported to occur in the liver, spleen, and lung.100 Extramedullary hematopoiesis is ineffective in preventing or correcting the pancytopenia that eventually develops.
Myelodysplastic Syndrome
Dysfunction of the hematopoietic system can be manifested by a variety of abnormalities that constitute myelodysplastic syndrome (MDS). In dogs, in which the syndrome is rare, there usually are cytopenias in two or three lines in the peripheral blood (anemia, neutropenia, and/or thrombocytopenia). Other blood abnormalities can include macrocytic erythrocytes and metarubricytosis. The bone marrow is typically normocellular or hypercellular, and dysplastic changes are evident in several cell lines. If blast cells are present, they make up less than 30% of all nucleated cells,2 although this threshold is being changed to less than 20%.4,20 Myelodysplasia is sometimes referred to as preleukemia because, in some cases, it may progress to acute leukemia.29-31 Based on reported cases, poor prognostic indices include increased percentage of blast cells, cytopenias involving more than one lineage, and cellular atypia. Primary MDSs are clonal disorders and are considered neoplastic. Complex classification schemes for human MDS, based on percentages of blasts in bone marrow, cytogenetic analysis, cytopenias, need for transfusions, and other variables, comprise at least nine subtypes; their applicability to veterinary medicine is unknown.5 Three subtypes are proposed for dogs and cats and include MDS with excessive blasts (MDS-EB), in which blast percentages are greater than 5% and less than 20%, and progression to AML may occur; MDS with refractory cytopenia (MDS-RC) with blast percentages less than 5% and cytopenias in one or more lineages; and MDS with erythroid predominance (MDS-ER) in which the M : E ratio is less than 1 and prognosis is poor.4 Larger studies are needed to determine the utility of this classification scheme and other potential prognostic indices, such as sex, age, and FeLV positivity. In addition to accumulating enough cases, another confounding factor to studying and classifying MDS is the presence of reversible MDSs that occur secondary to immune-mediated, infectious, and other diseases in both dogs and cats.
History and Clinical Signs
Dogs with myeloid neoplasms have similar presentations regardless of the specific disease entity, although animals with AML have a more acute onset of illness and a more rapid clinical course. A history of lethargy, inappetence, and weight loss is common. Clinical signs include emaciation, persistent fever, pallor, petechiation, hepatosplenomegaly, and, less commonly, lymphadenopathy and enlarged tonsils. Shifting leg lameness, ocular lesions, and recurrent infections are also seen. Vomiting, diarrhea, dyspnea, and neurologic signs are variable features. Serum biochemical analytes may be within the reference intervals but can change if significant organ infiltration occurs. Animals with MDS may be lethargic and anorectic and have pallor, fever, and hepatosplenomegaly. In PV, dogs often have erythema of mucous membranes owing to the increase in RBC mass. Some dogs are polydipsic. In addition, neurologic signs such as disorientation, ataxia, or seizures may be present and are thought to be the result of hyperviscosity or hypervolemia.69 Hepatosplenomegaly is usually absent.
Peripheral blood abnormalities are consistently found. In addition to the presence of neoplastic cells, other abnormalities, including cytopenias of any lineage, may be present. Low numbers of nucleated RBCs are present in the blood of about half the dogs with acute nonlymphocytic leukemia.3 Nonregenerative anemia and thrombocytopenia are present in most cases. Anemia is usually normocytic and normochromic, although macrocytic anemia is sometimes present. Pathogenic mechanisms include effects of inhibitory factors leading to ineffective hematopoiesis, myelophthisis, immune-mediated anemia secondary to neoplasia, and hemorrhage secondary to thrombocytopenia, platelet dysfunction, or DIC. Anemia is most severe in AML, although both anemia and thrombocytopenia may be milder in animals with the M5 subtype (acute monocytic leukemia). In myelofibrosis, the anemia is characterized by anisocytosis and poikilocytosis. In addition, pancytopenia and leukoerythroblastosis, in which immature erythroid and myeloid cells are in circulation, may be present. These phenomena probably result from replacement of marrow by fibrous tissue with resultant shearing of red cells and escape of immature cells normally confined to bone marrow. In PV, the PCV is increased, usually in the range of 65% to 85%. The bone marrow is hyperplastic, and the M : E ratio is usually in the normal range.
Neoplastic cells are often defective functionally. Platelet dysfunction has been reported in a dog with acute megakaryoblastic leukemia (M7),51 and in CML, neutrophils have decreased phagocytic capacity and other abnormalities. One exception to this was a report of CML in a dog in which the neutrophils had enhanced phagocytic capacity and superoxide production.101 The authors hypothesized that increased synthesis of GM-CSF resulted from a lactoferrin deficiency in the neoplastic neutrophils and mediated the enhanced function of these cells.
Diagnostic Techniques and Work-Up
In all cases of myeloid neoplasms, diagnosis depends on examination of peripheral blood and bone marrow. AML is diagnosed on the basis of finding blast cells with clearly visible nucleoli in blood and bone marrow. Most dogs with acute leukemia have circulating blasts. These cells may be present in low numbers in peripheral blood, and a careful search of the smear, especially at the feathered edge, should be made. Even if blasts are not detected in circulation, indications of bone marrow disease such as nonregenerative anemia or thrombocytopenia are usually present. Occasionally, neoplastic cells can be found in cerebrospinal fluid in animals with invasion of the CNS. Smears of aspirates from tissues such as the lymph nodes, spleen, or liver may contain blasts but usually contribute little to the diagnostic work-up.
Examination of blasts stained with standard Romanowsky stains may give clues as to the lineage of the cells (Figure 32-18, A to C and E). In myelomonocytic leukemia, the nuclei of the blasts are usually pleomorphic, with round to lobulated forms. In some cells, the cytoplasm may contain large azurophilic granules or vacuoles. Blasts in megakaryocytic leukemia may contain vacuoles and have cytoplasmic blebs. In addition, bizarre macroplatelets may be present. Although these distinguishing morphologic features may suggest a definitive diagnosis, cytochemical staining or immunophenotyping are usually required to define the lineage of the blasts. Several investigators have reported modification of diagnoses following cytochemical staining.102,103 It is especially important to distinguish AML from lymphocytic leukemia in order to provide accurate prognostic information to the owner and institute appropriate therapy.
The Animal Leukemia Group has recommended the following diagnostic criteria, summarized in Figure 32-19.3 Using well-prepared Romanowsky-stained blood and bone marrow films, a minimum of 200 cells are counted to determine the leukocyte differential in blood and the percentage of blast cells in bone marrow and/or blood. In bone marrow, blast cells are calculated both as a percentage of all nucleated cells (ANC) and nonerythroid cells (NEC) and are further characterized using cytochemical markers.102-104 Neutrophil differentiation is identified by positive staining of blasts for peroxidase, Sudan Black B, and chloracetate esterase. Nonspecific esterases (alpha-naphthyl acetate esterase or alpha-naphthyl butyrate esterase), especially if they are inhibited by sodium fluoride, mark monocytes. Canine monocytes may also contain a few peroxidase-positive granules. Acetylcholinesterase is a marker for megakaryocytes in dogs and cats. In addition, positive immunostaining for von Willebrand’s factor (factor VIII-related antigen) and platelet glycoproteins on the surface of blasts identifies them as megakaryocyte precursors.10,49-53 Alkaline phosphatase (AP) only rarely marks normal cells in dogs and cats but is present in blasts cells in acute myeloblastic and myelomonocytic leukemias. However, owing to reports of AP activity in lymphoid leukemias in dogs, its specificity as a marker for myeloid cells is not certain. Omega exonuclease is a specific marker for basophils, which are also positive for chloracetate esterase activity.86
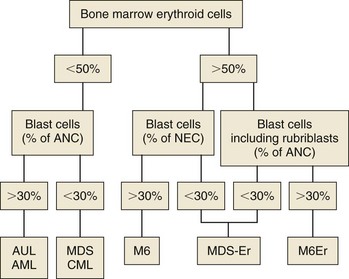
Figure 32-19 A scheme to classify myeloid neoplasms and myelodysplastic syndromes in dogs and cats. (Blast cells, Myeloblasts, monoblasts, and megakaryoblasts; ANC, all nucleated cells in bone marrow, including lymphocytes, plasma cells, macrophages, and mast cells; NEC, nonerythroid cells in bone marrow; AUL, acute undifferentiated leukemia; AML, acute myeloid leukemias M1 to M5 and M7; CML, chronic myeloid leukemias, including chronic myelogenous, chronic myelomonocytic, and chronic monocytic leukemias; MDS, myelodysplastic syndrome; MDS-Er, myelodysplastic syndrome with erythroid predominance; M6, erythroleukemia; M6Er, erythroleukemia with erythroid predominance.) (From Jain NC, Blue JT, Grindem CB, et al: Proposed criteria for classification of acute myeloid leukemia in dogs and cats, Vet Clin Pathol 20(3):63–82, 1991.)
Blood and bone marrow differential counts and cytochemical staining should be performed and interpreted by experienced veterinary cytopathologists. If erythroid cells are less than 50% of ANC and the blast cells are greater than 30%, a diagnosis of AML or AUL is made. If erythroid cells are greater than 50% of ANC and the blast cells are greater than 30%, a diagnosis of erythroleukemia (M6) is made. If rubriblasts are a significant proportion of the blast cells, a diagnosis of M6Er, or erythroleukemia with erythroid predominance, can be made. It should be noted that in the human AML classification system, the blast threshold has been lowered to 20% and similar recommendations are being made for AML in dogs and cats.
In some cases, electron microscopy is required to identify the lineage of the blast cells. For example, megakaryocyte precursors are positive for platelet peroxidase activity and contain demarcation membranes and alpha granules.49,53 Both of these features are detected at the ultrastructural level. Immunophenotyping, used to identify cell lineages in human patients, awaits development of appropriate markers for animal species (see later). Increasingly, cytogenetic abnormalities are being identified in animal leukemias; cytogenetic analysis may yield important diagnostic and prognostic information and become a valuable tool for identifying targeted therapeutic approaches.
Although morphologic and cytochemical analyses have formed the mainstay of cell identification, newer technologies now are routinely used to classify leukemias by using monoclonal antibodies to detect antigens associated with certain cell types. Cells can be immunophenotyped using flow cytometric analysis or immunocytochemistry.20,63,105-108 Cells from both acute lymphoid leukemia and AML are positive for CD34. Many lymphocyte markers, including CD3, CD4, CD8, CD18, CD21, CD45, CD79, and IgG, are available for dogs and can be used to rule out lymphoblastic leukemia in dogs with acute leukemias.63,105 Other markers include myeloperoxidase (MPO) and CD11b for myeloid cells and CD41 for megakaryoblasts. There is some overlap in expression of these cellular antigens. For example, canine (but not human) granulocytes express CD4. It is best to use a panel of antibodies (similar to using a battery of cytochemical stains) because antigens are often expressed on multiple lineages, and lineage infidelity can occur. These tests have become more valuable with the availability of canine reagents. Currently, the ACVP Oncology Committee recommends that the following immunophenotyping panel be done on bone marrow and/or blood smears to characterize animal leukemias: for B lymphocytes, CD79a; for T lymphocytes, CD3; for myeloid cells, MPO and CD11b; for megakaryoblasts, CD41; for dendritic cells, CD1c; and for acute leukemias, CD34.20
Because of the degree of differentiation of cells in MPN, these disorders must be distinguished from nonneoplastic causes of increases in these cell types. In order to make a diagnosis of PV, it must first be established that the polycythemia is absolute rather than relative. In relative polycythemias, plasma volume is decreased from hemoconcentration, dehydration, or hypovolemia, and the absolute RBC mass is not increased. Splenic contraction can also result in relative polycythemia. Absolute polycythemia, in which RBC mass is increased, is usually secondary to tissue hypoxia, causing appropriate increased production of erythropoietin. Rarely, erythropoietin may be produced inappropriately by a tumor (e.g., renal cell carcinoma) or in renal disease (pyelonephritis) or localized renal hypoxia.109-111 These causes of polycythemia should be eliminated by appropriate laboratory work, thoracic radiographs, arterial blood gas analysis, and renal ultrasonography. In humans with PV, plasma erythropoietin (EPO) levels are low. EPO levels in dogs with PV tend to be low or low-normal, whereas in animals with secondary absolute polycythemia, the levels are high.112,113 Samples for determination of EPO concentrations should be taken prior to therapeutic phlebotomy used to treat hyperviscosity and, owing to fluctuations in EPO levels, should be repeated if results are incongruous with other information.
There are no pathognomonic features of CML in dogs, and other common causes for marked leukocytosis with a left shift (“leukemoid reaction”) and granulocytic hyperplasia of bone marrow must be eliminated. These include infections, especially pyogenic ones; immune-mediated diseases; and other malignant neoplasms. In CML, maturation sometimes appears disorderly, and there may be variation in the size and shape of neutrophils at the same level of maturation. In addition, neoplastic leukocytes may disintegrate more rapidly and appear vacuolated.35 Because of the invasive nature of CML, biopsy of liver or spleen may also help to distinguish true leukemia from a leukemoid reaction, assuming the animal can tolerate the procedure. If characteristic cytogenetic abnormalities can be found in dogs with CML, this analysis may be helpful.
Basophilic leukemia is diagnosed by finding excessive numbers of basophils in circulation and in bone marrow. Basophilic leukemia must be differentiated from mastocytosis based on the morphology of the cell type present. Basophils have a segmented nucleus and variably sized granules, whereas mast cells have a round-to-oval nucleus that may be partially or totally obscured by small, round, metachromatic-staining granules. This distinction is usually easy to make; however, in basophilic leukemia, changes in the morphology of the nucleus and granules make the distinction less clear.85
Essential thrombocythemia has been diagnosed based on finding persistent and excessive thrombocytosis (>600,000/µL) without circulating blast cells and in the absence of another MPD (e.g., PV), myelofibrosis, or disorders known to cause secondary thrombocytosis.89 These include iron deficiency anemia, chronic inflammatory diseases, recovery from severe hemorrhage, rebound from immune-mediated thrombocytopenia, and absence of a spleen. Thrombocytosis is transient in these disorders or abates with resolution of the primary disease. In essential thrombocythemia, platelet morphology may be abnormal, with bizarre giant forms and abnormal granulation.90 In the bone marrow, megakaryocytic hyperplasia is a consistent feature, and dysplastic changes may be evident in megakaryocytes.93 Spurious hyperkalemia may be present in serum samples from dogs with thrombocytosis from any cause due to the release of potassium from platelets during clot formation.114 Measuring potassium in plasma is recommended in these cases and usually demonstrates a potassium concentration within reference interval. Platelet aggregability has been variably reported as impaired90 or enhanced.93 In the one dog in which it was measured, the plasma thrombopoietin (TPO) concentration was normal.92 It is unclear whether TPO plays a role in essential thrombocythemia or is suppressed by the high platelet mass. Elucidation of the pathogenesis of this disorder should be aided by the recent cloning of the genes for thrombopoietin and its receptor, the proto-oncogene mpl.115
In MDS, abnormalities in two or three cell lines are usually manifested in peripheral blood as neutropenia with or without a left shift, nonregenerative anemia, or thrombocytopenia. Other changes include macrocytosis and metarubricytosis. The bone marrow is typically normocellular or hypercellular with an increased M : E ratio, and blasts cells, although increased, constitute less than 20% of nucleated cells; in a report of 13 dogs with primary or secondary MDS, in all but one dog the blast cell percentage was less than 20%.116 Dysplastic changes can be detected in any cell line. Dyserythropoiesis is characterized by asynchronous maturation of erythroid cells typified by large hemoglobinized cells with immature nuclei (megaloblastic change). If the erythroid component is dominant, the MDS is called MDS-Er (see Table 32-12).3,32 In dysgranulopoiesis, giant neutrophil precursors and abnormalities in nuclear segmentation and cytoplasmic granulation can be seen. Finally, dysthrombopoiesis is characterized by giant platelets and micromegakaryocytes.
Myelofibrosis should be suspected in animals with nonregenerative anemia or pancytopenia, abnormalities in erythrocyte morphology (especially shape), and leukoerythroblastosis. Bone marrow aspiration is usually unsuccessful, resulting in a “dry tap.” This necessitates a bone marrow biopsy taken with a Jamshidi needle.117 The specimen is processed for routine histopathologic examination, and if necessary, special stains for fibrous tissue can be used. Because myelofibrosis occurs secondary to other diseases of bone marrow such as chronic hemolytic anemia or bone marrow necrosis, the clinician should look for a primary disease process.
Treatment
Acute Myeloid Leukemia
Treatment of acute nonlymphocytic leukemias has been unrewarding to date. However, we have little information on the response of specific subtypes of leukemia to uniform chemotherapeutic protocols, in part due to the rarity of these disease processes and the paucity of cases in the literature. The veterinarian is advised to contact a veterinary oncologist for advice on new protocols and appropriate management of these cases.
The therapeutic goal is to eradicate leukemic cells and reestablish normal hematopoiesis. Currently, this is best accomplished by cytoreductive chemotherapy, and the agents most commonly utilized include a combination of Ara-C plus an anthracycline, such as doxorubicin or cyclophosphamide, vincristine, and prednisone.* In humans, the introduction of cytosine arabinoside has been the single most important development in the therapy of acute nonlymphocytic leukemia.120 In dogs, Ara-C, 100 to 200 mg/m2, given by slow infusion (12 to 24 hrs) daily for 3 days and repeated weekly, has been used, as well as several other variations using subcutaneous injections of cytosine (see Chapter 11). Doxorubicin, 30 mg/m2 IV every 2 to 3 weeks, can be administered at intervals alternating with Ara-C. If remission is achieved, as evidenced by normalization of the hemogram, the COAP protocol (cyclophosphamide, vincristine (Oncovin), Ara-C, and prednisone), as described for canine lymphoma, could be used as maintenance therapy.9,118 Another protocol that has been used in treating acute myeloblastic leukemia is presented in Table 32-13.
Table 32-13
Protocol for the Treatment of Acute Myeloproliferative Disorders
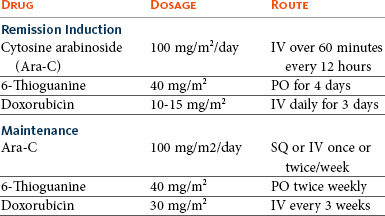
IV, Intravenous; PO, by mouth; SQ, subcutaneous.
Data from Mears EA, Raskin RE, Legendre AM: Basophilic leukemia in a dog, J Vet Intern Med 11(2):92–94, 1997.
Regardless of the chemotherapy protocol used, significant bone marrow suppression will develop, and intensive supportive care will be necessary. Transfusions of whole blood or platelet-rich plasma may be required to treat anemia and thrombocytopenia, and infection should be managed with aggressive antibiotic therapy. Because of the generally poor response, the major thrust of therapy may be to provide palliative supportive care.
Polycythemia Vera
In treating PV, therapy is directed at reducing RBC mass. The PCV should be reduced to 50% to 60% or by one-sixth of its starting value; phlebotomies should be performed as needed, administering appropriate colloid and crystalloid solutions to replace lost electrolytes; 20 mL of whole blood/kg of body weight can be removed at regular intervals.67 In humans, phlebotomy continues to be the therapeutic approach used most frequently.
Radiophosphorus (32P) has been shown to provide long-term control but can only be used in specialized centers.121 The chemotherapeutic drug of choice is hydroxyurea, an inhibitor of DNA synthesis. This drug should be administered at an initial dose of 30 mg/kg for 10 days and then reduced to 15 mg/kg PO daily.69 The major goal of treatment is to maintain the PCV as close to normal as possible.
Chronic Myelogenous Leukemia
CML is best managed with chemotherapy to control the proliferation of the abnormal cell line and improve the quality of life. Hydroxyurea is the most effective agent for treating CML during the chronic phase.75,122 The initial dosage is 20 to 25 mg/kg twice daily. Treatment with hydroxyurea should continue until the leukocyte count falls to 15,000 to 20,000 cells/µL.75,79,84 Then the dosage of hydroxyurea can be reduced by 50% on a daily basis or to 50 mg/kg given biweekly or triweekly. In humans, the alkylating agent busulfan can be used as an alternative.123 An effective dosage has not been established in the dog, but following human protocols, 0.1 mg/kg/day PO is given until the leukocyte count is reduced to 15,000 to 20,000 cells/µL.
Despite response to chemotherapy and control for many months, most dogs with CML will eventually enter a terminal phase of their disease. In one study of seven dogs with CML, four underwent terminal phase blast crisis.75 In humans, blast crisis may be lymphoid or myeloid.124 In dogs, it is usually difficult to determine the cell of origin. These dogs have a poor prognosis, and the best treatment to consider, if any, would be that listed in Table 32-13.
It has now been documented that a subset of CML in dogs may be associated with a BCR-ABL chromosomal abnormality (the so-called “Raleigh chromosome”) similar to the “Philadelphia chromosome” translocation responsible for a large majority of CML in humans.2 While imatinib mesylate (Gleevec) is known to be an effective therapy for CML in humans, BCR-ABL kinase inhibitors have, as yet, not been investigated for this subset of CML in dogs.
Essential Thrombocythemia
Few cases have been reported, but one dog was treated successfully with a combination chemotherapy protocol that included vincristine, Ara-C, cyclophosphamide, and prednisone.91 Treatment is controversial in humans because of the lack of evidence that asymptomatic patients benefit from chemotherapy. Patients with thrombosis or bleeding are given cytoreductive therapy. Hydroxyurea is the drug of choice for initially controlling the thrombocytosis.89
Myelodysplastic Syndrome
There is no standard therapeutic regime for MDS. Often, humans receive no treatment if the cytopenias do not cause clinical signs. Transfusions are given when necessary, and patients with fever are evaluated aggressively to detect infections. Growth factors, such as EPO, GM-CSF, G-CSF, and IL-3, are sometimes used in patients who require frequent transfusions to increase their blood cell counts and enhance neutrophil function.125,126 In one case report, human EPO was administered (100 U/kg SQ, every 48 hours) to a dog with MDS because of profound anemia. The rationale for use of EPO was to promote terminal differentiation of dysplastic erythrocytes. The PCV increased from 12% to 34% by day 19 of EPO treatment. This dog remained in remission for more than 30 months.32 Other factors that induce differentiation of hematopoietic cells include retinoic acid analogs,127 1,25 dihydroxyvitamin D3,128 interferon-α, and conventional chemotherapeutic agents, such as 6-thioguanine and Ara-C.129 The propensity of these factors to enhance progression to leukemia is not known in many cases, but the potential risk exists.
Prognosis
In general, the prognosis for animals with MPN is better than for dogs with AML, in which it is grave. The prognosis for PV and CML is guarded, but significant remissions have been achieved with certain therapeutic regimes and careful monitoring. Animals commonly survive a year or more.75,84 Development of blast crisis portends a grave prognosis.
Comparative Aspects
The pathophysiology and therapy of nonlymphocytic leukemia in humans are being studied intensively. Myeloid neoplasms have been demonstrated to be clonal, with abnormalities evident in all hematopoietic cell lines. Leukemogenesis is likely caused by mutation or amplification of proto-oncogenes in a two-step process that initially involves a single cell and is followed by additional chromosomal alterations that may involve oncogenes.1,15 These alterations are manifested as cytogenetic abnormalities. Environmental factors known to cause leukemia are exposure to high-dose radiation, benzene (chronic exposure), and alkylating agents.130 New classification systems have incorporated genetic mutations, more accurately reflect prognoses, and facilitate use of consistent categorization among institutions.131
Therapeutic modalities under investigation or development include combination chemotherapy, immunotherapy, cytokine therapy, drug-resistance modulators, proapoptotic agents, antiangiogenic factors, signal transduction-active agents, and bone marrow transplantation. The prognosis for MPN is better than for AML. For acute nonlymphocytic leukemias, the prognosis is better for children than adults, with only 10% of adults receiving chemotherapy maintaining remissions for more than 5 years.130 The spontaneous canine diseases probably occur too infrequently to serve as useful models. Myeloid neoplasms have been induced experimentally in the dog by irradiation and transplantation in an attempt to create models for study. Many similarities between human and canine myeloid neoplasms exist, and veterinary medicine may benefit from any therapeutic advances made in the human field.
References
1. Lichtman, MA, Classification and clinical manifestations of the clonal myeloid disorders. Lichtman MA, Kipps TJ, Seligsohn U, et al, eds. Williams hematology ed 8. New York: McGraw-Hill; 2010 http://www.accessmedicine.com/content.aspx?aID=6121127 [Accessed December 23, 2011].
2. Breen, M, Modiano, JF. Evolutionarily conserved cytogenetic changes in hematologic malignancies of dogs and humans—man and his best friend share more than companionship. Chromosome Res. 2008;16(1):145–154.
3. Jain, NC, Blue, JT, Grindem, CB, et al. A report of the animal leukemia study group. Proposed criteria for classification of acute myeloid leukemia in dogs and cats. Vet Clin Pathol. 1991;20(3):63–82.
4. Juopperi, TA, Bienzle, D, Bernreuter, DC, et al. Prognostic markers for myeloid neoplasms: a comparative review of the literature and goals for future investigation. Vet Pathol. 2011;48(1):182–197.
5. Nielsen, SW. Myeloproliferative disorders in animals. In: Clarke WJ, Howard EB, Hackett PL, eds. Myeloproliferative disorders in animals and man. Oak Ridge, Tenn: USAEC Division of Technical Information Extension, 1970.
6. Christopher, MM, Metz, AL, Klausner, J, et al. Acute myelomonocytic leukemia with neurologic manifestations in the dog. Vet Pathol. 1986;23(2):140–147.
7. Keller, P, Sager, P, Freudiger, U, et al. Acute myeloblastic leukemia in a dog. J Comp Pathol. 1985;95(4):619–632.
8. Clark, P, Swenson, CL, Drenen, CM. A 6-year-old Rottweiler with weight loss. Aust Vet J. 1997;75(10):709. [714–715].
9. Graves, TK, Swenson, CL, Scott, MA. A potentially misleading presentation and course of acute myelomonocytic leukemia in a dog. J Am Anim Hosp Assoc. 1997;33:37–41.
10. Colbatzy, F, Hermanns, W. Acute megakaryoblastic leukemia in one cat and two dogs. Vet Pathol. 1993;30(2):186–194.
11. Latimer, KS, Dykstra, MJ. Acute monocytic leukemia in a dog. J Am Vet Med Assoc. 1984;184:852–854.
12. Hamlin, RH, Duncan, RC. Acute nonlymphocytic leukemia in a dog. J Am Vet Med Assoc. 1990;196:110–112.
13. Grindem, CB, Stevens, JB, Perman, V. Morphologic classification and clinical and pathological characteristics of spontaneous leukemia in 17 dogs. J Am Anim Hosp Assoc. 1985;21:219–226.
14. Modiano, JF, Smith, R, III., Wojcieszyn, J, et al. The use of cytochemistry, immunophenotyping, flow cytometry, and in vitro differentiation to determine the ontogeny of a canine monoblastic leukemia. Vet Clin Pathol. 1998;27:40–49.
15. Jandl, JH. Hematopoietic malignancies. In: Blood: pathophysiology. Boston: Blackwell Scientific Publications; 1991.
16. Grindem, CB, Buoen, LC. Cytogenetic analysis of leukemic cells in the dog: A report of 10 cases and a review of the literature. J Comp Pathol. 1986;96:623–635.
17. Reimann, N, Bartnitzke, S, Bullerdiek, J, et al. Trisomy 1 in a canine acute leukemia indicating the pathogenetic importance of polysomy 1 in leukemias of the dog. Cancer Genet Cytogenet. 1997;101:49–52.
18. Breen, M. Canine cytogenetics—from band to base pair. Cytogenet Genome Res. 2008;120(1-2):50–60.
19. Breen, M. Update on genomics in veterinary oncology. Top Companion Anim Med. 2009;24(3):113–121.
20. McManus, PM. Classification of myeloid neoplasms: a comparative review. Vet Clin Pathol. 2005;34:189–212.
21. Reimann, N, Bartnitzke, S, Nolte, I, et al. Working with canine chromosomes: current recommendations for karyotype description. J Hered. 1999;90:31–34.
22. Anderson, AC, Johnson, RM. Erythroblastic malignancy in a beagle. J Am Vet Med Assoc. 1962;141:944–946.
23. Seed, TM, Tolle, DV, Fritz, TE, et al. Irradiation-induced erythroleukemia and myelogenous leukemia in the beagle dog: Hematology and ultrastructure. Blood. 1977;50:1061–1079.
24. Tolle, DV, Seed, TM, Fritz, TE, et al. Acute monocytic leukemia in an irradiated beagle. Vet Pathol. 1979;16:243–254.
25. Sykes, GP, King, JM, Cooper, BC. Retrovirus-like particles associated with myeloproliferative disease in the dog. J Comp Pathol. 1985;95(4):559–564.
26. Quesenberry, PJ. Hemopoietic stem cells, progenitor cells, and cytokines. In Beutler E, Lichtman MA, Coller BS, et al, eds.: Williams hematology, ed 5, New York: McGraw-Hill, 1995.
27. Metcalf, D. The hemopoietic colony stimulating factors. New York: Elsevier; 1984.
28. Lok, S, Kaushansky, K, Holly, RD, et al. Cloning and expression of murine thrombopoietin cDNA and stimulation of platelet production in vivo. Nature. 1994;369:565–568.
29. Couto, CG, Kallet, AJ. Preleukemic syndrome in a dog. J Am Vet Med Assoc. 1984;184:1389–1392.
30. Couto, CG. Clinicopathologic aspects of acute leukemias in the dog. J Am Vet Med Assoc. 1985;186(7):681–685.
31. Weiss, DJ, Raskin, R, Zerbe, C. Myelodysplastic syndrome in two dogs. J Am Vet Med Assoc. 1985;187(10):1038–1040.
32. Boone, LI, Knauer, KW, Rapp, SW, et al. Use of human recombinant erythropoietin and prednisone for treatment of myelodysplastic syndrome with erythroid predominance in a dog. J Am Vet Med Assoc. 1998;213(7):999–1001.
33. Degen, MA, Feldman, BF, Turrel, JM, et al. Thrombocytosis associated with a myeloproliferative disorder in a dog. J Am Vet Med Assoc. 1989;194(10):1457–1459.
34. Evans, JR, Gorman, NT. Myeloproliferative disease in the dog and cat: Definition, aetiology and classification. Vet Rec. 1987;121:437–443.
35. Jain, NC, The leukemia complex. Schalm’s veterinary hematology ed 4. Philadelphia: Lea & Febiger; 1986.
36. Usher, SG, Radford, AD, Villiers, EJ, et al. RAS, FLT3, and C-KIT mutations in immunophenotyped canine leukemias. Exp Hematol. 2009;37(1):65–77.
37. Barthel, CH. Acute myelomonocytic leukemia in a dog. Vet Pathol. 1974;11:79–86.
38. Green, RA, Barton, CL. Acute myelomonocytic leukemia in a dog. J Am Anim Hosp Assoc. 1977;13:708–712.
39. Jain, NC, Madewell, BR, Weller, RE, et al. Clinical-pathological findings and cytochemical characterizations of myelomonocytic leukaemia in 5 dogs. J Comp Pathol. 1981;91:17–31.
40. Linnabary, RD, Holscher, MA, Glick, AD, et al. Acute myelomonocytic leukemia in a dog. J Am Anim Hosp Assoc. 1978;14:71–75.
41. Moulton, JE, Dungworth, DL. Tumors of the lymphoid and hemopoietic tissues. In Moulton JE, ed.: Tumors in domestic animals, ed 2, Berkeley: University of California Press, 1978.
42. Ragan, HA, Hackett, PL, Dagle, GE. Acute myelomonocytic leukemia manifested as myelophthistic anemia in a dog. J Am Vet Med Assoc. 1976;169:421–425.
43. Rohrig, KE. Acute myelomonocytic leukemia in a dog. J Am Vet Med Assoc. 1983;182:137–141.
44. Madewell, BR, Jain, NC, Munn, RJ. Unusual cytochemical reactivity in canine acute myeloblastic leukemia. Comp Haematol Int. 1991;1(2):117–120.
45. Hayashi, A, Tanaka, H, Kitamura, M, et al. Acute myelomonocytic leukemia (AML-M4) in a dog with the extradural lesion. J Vet Med Sci. 2011;73:419–422.
46. Hisasue, M, Nishimura, T, Neo, S, et al. A dog with acute myelomonocytic leukemia. J Vet Med Sci. 2008;70:619–621.
47. Holscher, MA, Collins, RD, Glick, AD, et al. Megakaryocytic leukemia in a dog. Vet Pathol. 1978;15:562–565.
48. Canfield, PJ, Church, DB, Russ, IG. Myeloproliferative disorder involving the megakaryocytic line. J Small Anim Pract. 1993;34(6):296–301.
49. Bolon, B, Buergelt, CD, Harvey, JW, et al. Megakaryoblastic leukemia in a dog. Vet Clin Pathol. 1989;18(3):69–72.
50. Shull, RM, DeNovo, RC, McCracken, MD. Megakaryoblastic leukemia in a dog. Vet Pathol. 1986;23(4):533–536.
51. Cain, GR, Feldman, BF, Kawakami, TG, et al. Platelet dysplasia associated with megakaryoblastic leukemia in a dog. J Am Vet Med Assoc. 1986;188(5):529–530.
52. Cain, GR, Kawakami, TG, Jain, NC. Radiation-induced megakaryoblastic leukemia in a dog. Vet Pathol. 1985;22(6):641–643.
53. Mesick, J, Carothers, M, Wellman, M. Identification and characterization of megakaryoblasts in acute megakaryoblastic leukemia in a dog. Vet Pathol. 1990;27(3):212–214.
54. Comazzi, S, Gelain, ME, Belfanti, U, et al. Acute megakaryoblastic leukemia in a dog : a report of 3 cases and review of the literature. J Am Anim Hosp Assoc. 2010;46:327–335.
55. Willan, M, Mulaire, L, Schwendenwein, I, et al. Chemotherapy in canine acute megakaryoblastic leukemia: a case report and review of the literature. In Vivo. 2009;23:911–918.
56. Ferreira, HM, Smith, SH, Schwartz, AM, et al. Myeloperoxidase-positive acute megakaryoblastic leukemia in a dog. Vet Clin Pathol. 2011;40:530–537.
57. Suter, SE, Vernau, W, Fry, MM, et al. CD34+, CD41+ acute megakaryoblastic leukemia in a dog. Vet Clin Pathol. 2007;36:288–292.
58. Park, HM, Doster, AR, Tashbaeva, RE, et al. Clinical, histopathological and immunohistochemical findings in a case of megakaryoblastic leukemia in a dog. J Vet Diagn Invest. 2006;18:287–291.
59. Mackey, LJ, Jarrett, WFH, Lauder, IM. Monocytic leukaemia in the dog. Vet Rec. 1975;96:27–30.
60. Capelli, JL. Erythroleukemia in a dog. Pratique Medicale and Chirurgicale de l’Animal de Compagnie. 1990;26(4):337–340.
61. Hejlasz, Z. Three cases of erythroleukemia in dogs. Medycyna Weterynaryjna. 1986;42(6):346–349.
62. Tomiyasu, H, Fujino, Y, Takahashi, M, et al. Spontaneous erythroblastic leukaemia (AML-M6Er) in a dog. J Small Anim Pract. 2011;52:445–457.
63. Grindem, CB. Blood cell markers. Vet Clin North Am. 1996;26(5):1043–1064.
64. Prchal, J. Primary polycythemias. In: Adamson JW, ed. Current opinion in hematology. Philadelphia: Current Science, 1995.
65. Bush, BM, Fankhauser, R. Polycythaemia vera in a bitch. J Small Anim Pract. 1972;13:75–89.
66. Carb, AV. Polycythemia vera in a dog. J Am Vet Med Assoc. 1969;154:289–297.
67. McGrath, CJ. Polycythemia vera in dogs. J Am Vet Med Assoc. 1974;164:1117–1122.
68. Miller, RM. Polycythemia vera in a dog. Vet Med/Small Anim Clin. 1968;63:222–223.
69. Peterson, ME, Randolph, JK. Diagnosis of canine primary polycythemia and management with hydroxy-urea. J Am Vet Med Assoc. 1982;180:415–418.
70. Quesnal, AD, Kruth, SA. Polycythemia vera and glomerulonephritis in a dog. Can Vet J. 1992;33(10):671–672.
71. Meyer, HP, Slappendel, RJ, Greydanus-van-der-Putten, SWM. Polycythaemia vera in a dog treated by repeated phlebotomies. Vet Q. 1993;15(3):108–111.
72. Wysoke, JM, Van Heerden, J. Polycythaemia vera in a dog. J S Afr Vet Assoc. 1990;61(4):182–183.
73. Holden, AR. Polycythaemia vera in a dog. Vet Rec. 1987;120(20):473–475.
74. Beurlet, S, Krief, P, Sansonetti, A, et al. identification of JAK2 mutations in canine primary polycythemia. Exp Hematol. 2011;39:542–545.
75. Leifer, CE, Matus, RE, Patnaik, AK, et al. Chronic myelogenous leukemia in the dog. J Am Vet Med Assoc. 1983;183:686–689.
76. Pollet, L, Van Hove, W, Matheeuws, D. Blastic crisis in chronic myelogenous leukaemia in a dog. J Small Anim Pract. 1978;19:469–475.
77. Grindem, CB, Stevens, JB, Brost, DR, et al. Chronic myelogenous leukaemia with meningeal infiltration in a dog. Comp Haematol Int. 1992;2(3):170–174.
78. Dunn, JK, Jeffries, AR, Evans, RJ, et al. Chronic granulocytic leukaemia in a dog with associated bacterial endocarditis, thrombocytopenia and preretinal and retinal hemorrhages. J Small Anim Pract. 1987;28(11):1079–1086.
79. Fine, DM, Tvedten, HW. Chronic granulocytic leukemia in a dog. J Am Vet Med Assoc. 1999;214(2):1809–1812.
80. Liesveld, JL, Lichtman, MA. Chronic myelogenous leukemia and related disorders. In Lichtman MA, Kipps TJ, Seligsohn U, et al, eds.: Williams hematology, ed 8, New York: McGraw-Hill, 2010.
81. Cruz Cardona, JA, Milner, R, Alleman, AR. BCR-ABL translocation in a dog with chronic monocytic leukemia. Vet Clin Pathol. 2011;40(1):40–47.
82. Rossi, G, Gelain, ME, Foroni, S, et al. Extreme monocytosis in a dog with chronic monocytic leukaemia. Vet Rec. 2009;165:54–56.
83. Hiraoka, H, Hisasue, M, Nagashima, N, et al. A dog with myelodysplastic syndrome: chronic myelomonocytic leukemia. J Vet Med Sci. 2007;69:665–668.
84. MacEwen, EG, Drazner, FH, McClellan, AJ, et al. Treatment of basophilic leukemia in a dog. J Am Vet Med Assoc. 1975;166:376–380.
85. Mahaffey, EA, Brown, TP, Duncan, JR, et al. Basophilic leukemia in a dog. J Comp Pathol. 1987;97(4):393–399.
86. Mears, EA, Raskin, RE, Legendre, AM. Basophilic leukemia in a dog. J Vet Intern Med. 1997;11(2):92–94.
87. Jensen, AL, Nielsen, OL. Eosinophilic leukemoid reaction in a dog. J Small Anim Pract. 1992;33(7):337–340.
88. Ndikuwera, J, Smith, DA, Obwolo, MJ, et al. Chronic granulocytic leukaemia/eosinophilic leukaemia in a dog. J Small Anim Pract. 1992;33(11):553–557.
89. Beer, PA, Green, AR, Essential thrombocythemia. Lichtman MA, Kipps TJ, Seligsohn U, et al, eds. Williams hematology ed 8. New York: McGraw-Hill; 2010 http://www.accessmedicine.com/content.aspx?aID=6136261 [Accessed December 23, 2011].
90. Hopper, PE, Mandell, CP, Turrel, JM, et al. Probable essential thrombocythemia in a dog. J Vet Intern Med. 1989;3(2):79–85.
91. Simpson, JW, Else, RW, Honeyman, P. Successful treatment of suspected essential thrombocythemia in the dog. J Small Anim Pract. 1990;31(7):345–348.
92. Bass, MC, Schultze, AE. Essential thrombocythemia in a dog: Case report and literature review. J Am Anim Hosp Assoc. 1998;34:197–203.
93. Dunn, JK, Heath, MF, Jeffries, AR, et al. Diagnostic and hematologic features of probable essential thrombocythemia in two dogs. Vet Clin Pathol. 1999;28(4):131–138.
94. Reagan, WJ. A review of myelofibrosis in dogs. Toxicol Pathol. 1993;21(2):164–169.
95. Weiss, DJ. A retrospective study of the incidence and the classification of bone marrow disorders in the dog at a veterinary teaching hospital (1996-2004). J Vet Intern Med. 2006;20(4):955–961.
96. Castro-Malaspina, H. Pathogenesis of myelofibrosis: Role of ineffective megakaryopoiesis and megakaryocyte components. In: Berk PD, Castro-Malaspina H, Wasserman LR, eds. Myelofibrosis and the biology of connective tissue. New York: Alan R. Liss, 1984.
97. Rudolph, R, Huebner, C. Megakaryozytenleukose beim hund. Kleintier-Praxis. 1972;17:9–13.
98. Dungworth, DL, Goldman, M, Switzer, JW, et al. Development of a myeloproliferative disorder in beagles continuously exposed to 90Sr. Blood. 1969;34:610–632.
99. Prasse, KW, Crouser, D, Beutler, E, et al. Pyruvate kinase deficiency anemia with terminal myelofibrosis and osteosclerosis in a beagle. J Am Vet Med Assoc. 1975;166:1170–1175.
100. Thompson, JC, Johnstone, AC. Myelofibrosis in the dog: Three case reports. J Small Anim Pract. 1983;24(9):589–601.
101. Thomsen, MK, Jensen, AL, Skak-Nielsen, T, et al. Enhanced granulocyte function in a case of chronic granulocytic leukemia in a dog. Vet Immunol Immunopathol. 1991;28(2):143–165.
102. Grindem, CB, Stevens, JB, Perman, V. Cytochemical reactions in cells from leukemic dogs. Vet Pathol. 1986;23:103–109.
103. Facklam, NR, Kociba, GJ. Cytochemical characterization of leukemic cells from 20 dogs. Vet Pathol. 1986;22:363–369.
104. Goldman, EE, Graham, JC. Clinical diagnosis and management of acute nonlymphoid leukemias and chronic myeloproliferative disorders. In Feldman BF, Zinkl JG, Jain NC, eds.: Schalm’s veterinary hematology, ed 5, Philadelphia: Lippincott Williams & Wilkins, 2000.
105. Cobbold, S, Metcalfe, S. Monoclonal antibodies that define canine homologues of human CD antigens: Summary of the First International Canine Leukocyte Antigen Workshop (CLAW). Tissue Antigens. 1994;43(3):137–154.
106. Tasca, S, Carli, E, Caldin, M, et al. Hematologic abnormalities and flow cytometric immunophenotyping results in dogs with hematopoietic neoplasia: 210 cases (2002-2006). Vet Clin Pathol. 2009;38:2–12.
107. Villiers, E, Baines, S, Law, AM, et al. Identification of acute myeloid leukemia in dogs using flow cytometry with myeloperoxidase, MAC387, and a canine neutrophil-specific antibody. Vet Clin Pathol. 2006;35:55–71.
108. Comazzi, S, Gelain, ME, Spagnolo, V, et al. Flow cytometric patterns in blood from dogs with non-neoplastic and neoplastic hematologic diseases using double labeling for CD18 and CD45. Vet Clin Pathol. 2006;35:47–54.
109. Peterson, ME, Zanjani, ED. Inappropriate erythropoietin production from a renal carcinoma in a dog with polycythemia. J Am Vet Med Assoc. 1981;179:995–996.
110. Scott, RC, Patnaik, AK. Renal carcinoma associated with secondary polycythemia in a dog. J Am Anim Hosp Assoc. 1972;8:275–283.
111. Waters, DJ, Prueter, JC. Secondary polycythemia associated with renal disease in the dog: Two case reports and review of literature. J Am Anim Hosp Assoc. 1988;24:109–114.
112. Cook, SM, Lothrop, CD. Serum erythropoietin concentrations measured by radioimmunoassay in normal, polycythemic, and anemic dogs and cats. J Vet Intern Med. 1994;8(1):18–25.
113. Giger, U, Serum erythropoietin concentrations in polycythemic and anemic dogs. Proceedings of the 9th Annual Vet Med Forum (ACVIM) 1991;143–145.
114. Reimann, KA, Knowlen, CG, Tvedten, HW. Factitious hyperkalemia in dogs with thrombocytosis. J Vet Intern Med. 1989;3:47–52.
115. Kaushansky, K. Thrombopoietin: The primary regulator of platelet production. Blood. 1995;86(2):419–431.
116. Weiss, DJ, Aird, B. Cytologic evaluation of primary and secondary myelodysplastic syndromes in the dog. Vet Clin Pathol. 2001;30:67–75.
117. Friedrichs, KR, Young, KM. How to collect diagnostic bone marrow samples. Vet Med. 2005;8:578–588.
118. Theilen, GH, Madewell, BR, Gardner, MB. Hematopoietic neoplasms, sarcomas and related conditions. In Theilen GH, Madewell BR, eds.: Veterinary cancer medicine, ed 2, Philadelphia: Lea & Febiger, 1987.
119. Gorman, NT, Evans, RJ. Myeloproliferative disease in the dog and cat: Clinical presentations, diagnosis and treatment. Vet Rec. 1987;121:490–496.
120. Mayer, RJ. Current chemotherapeutic treatment approaches to the management of previously untreated adults with de novo acute myelogenous leukemia. Semin Oncol. 1987;14:384–396.
121. Smith, M, Turrel, JM. Radiophosphorus (32P) treatment of bone marrow disorders in dogs: 11 cases (1970-1987). J Am Vet Med Assoc. 1982;194:98–102.
122. Lyss, AP. Enzymes and random synthetics. In: Perry MC, ed. The chemotherapy source book. Baltimore: Williams & Wilkins; 1992:398–412.
123. Bolin, RW, Robinson, WA, Sutherland, J, et al. Busulfan versus hydroxyurea in long-term therapy of chronic myelogenous leukemia. Cancer. 1982;50:1683–1686.
124. Rosenthal, S, Canellos, GP, Whang-Pang, J, et al. Blast crisis of chronic granulocytic leukemia: Morphologic variants and therapeutic implications. Am J Med. 1977;63:542–547.
125. Liesveld, JL, Lichtman, MA, Myelodysplastic syndromes (clonal cytopenias and oligoblastic myelogenous leukemia). Lichtman MA, Kipps TJ, Seligsohn U, et al, eds. Williams hematology ed 8. New York: McGraw-Hill; 2010 http://www.accessmedicine.com/content.aspx?aID=6139818 [Accessed December 23, 2011].
126. Ganser, A, Hoelzer, D. Treatment of myelodysplastic syndromes with hematopoietic growth factors. Hematol Oncol Clin North Am. 1992;6:633–653.
127. Ohno, R, Noe, T, Hirano, M, et al. Treatment of myelodysplastic syndromes with all-trans retinoic acid. Blood. 1993;81:1152–1154.
128. Kelsey, SM, Newland, AC, Cunningham, J, et al. Sustained haematological response to high dose oral alfacalcidol in patients with myelodysplastic syndrome [Letter]. Lancet. 1992;340:316.
129. Jacobs, A. Treatment for the myelodysplastic syndromes. Hematologica. 1987;72:477–480.
130. Liesveld, JL, Lichtman, MA, Acute myelogenous leukemia. Lichtman MA, Kipps TJ, Seligsohn U, et al, eds. Williams hematology ed 8. New York: McGraw-Hill; 2010 http://www.accessmedicine.com/content.aspx?aID=6140629 [Accessed December 23, 2011].
131. Vardiman, JW, Thiele, J, Arber, DA, et al. The 2008 revision of the World Health Organization (WHO) classification of the myeloid neoplasms and acute leukemia: rationale and important changes. Blood. 2009;114(5):937–951.
 Section D
Section D
Myeloma-Related Disorders
Myeloma-related disorders (MRDs) arise when a cell of the plasma cell or immunoglobulin-producing B-lymphocyte precursor lineage transforms and proliferates to form a neoplastic population of similar cells. This population is believed in most instances to be monoclonal (i.e., derived from a single cell) because they typically produce homogenous immunoglobulin, although some examples of biclonal and polyclonal MRD neoplasms exist. A wide variety of clinical syndromes are represented by MRDs, including multiple myeloma (MM), extramedullary plasmacytoma (EMP [both cutaneous and noncutaneous]), IgM (Waldenström’s) macroglobulinemia, solitary osseous plasmacytoma (SOP), and Ig-secreting lymphomas and leukemias (including plasma cell leukemia). MM is the most important MRD based on clinical incidence and severity. There appears to be some discordance and blurring of the distinction between MM and multicentric noncutaneous EMP in cats and these two MRDs will be discussed together in this species.
Multiple Myeloma
Although MM represents less than 1% of all malignant tumors in animals, it is responsible for approximately 8% of all hematopoietic tumors and 3.6% of all primary and secondary tumors affecting bone in dogs.1,2 In a compilation of bone marrow disorders in dogs (n = 717), MM represented 4.4% and 19.8% of all abnormal samples and neoplastic processes, respectively.3 Further, in a compilation of serum protein electrophoretic samples (n = 147 dogs), MM accounted for 4.3% of abnormal and 28.5% of neoplastic processes encountered, respectively.4 Early studies suggested a male predisposition,5 although subsequent reports have not supported this.1,6 Older dogs are affected with an average age of between 8 and 9 years.1,5,6 In one large case series, German shepherd dogs were overrepresented based on the hospital population.1 The true incidence of MM in the cat is unknown; however, it is a more rare diagnosis than in the dog, representing only 1 of 395 and 4 of 3248 tumors in two large compilations of feline malignancies and 0.9% of all malignancies and 1.9% of hematologic malignancies in another report.7-9 MM represented 1.4% and 14% of abnormal and malignant serum protein electrophoretic samples, respectively, in a compilation of 155 feline samples.10 MM occurs in aged cats (median age 12 to 14 years), most commonly in domestic short hairs and no sex predilection has been consistently reported, although a male preponderance may exist.6,9,11,12 MM has not been associated with corona virus or FeLV or FIV infections.
The etiology of MM is for the most part unknown. Genetic predispositions, molecular aberrations (e.g., c-Kit), viral infections, chronic immune stimulation, and exposure to carcinogen stimulation have all been suggested as contributing factors.6,13-18 Suggestion of a familial association in cats follows cases reported among siblings.12 Evidence exists that molecular mechanisms of cellular control, including overexpression of cell cycle control components like cyclin D1 (see Chapter 2) and receptor tyrosine kinase dysregulation may be involved in canine myeloma and plasma cell tumors.17,18 In rodent models, chronic immune stimulation and exposure to implanted silicone gel have been associated with development of MM,13,14 as have chronic infections and prolonged hyposensitization therapy in humans.15 Viral Aleutian disease of mink results in monoclonal gammopathies in a small percentage of cases.16 Exposure to the agricultural industry, petroleum products, and irradiation are known risk factors for development in humans.19-21 Additionally, progression of solitary plasma cell tumors to MM has been reported in both dogs and cats, and a single case of a B-cell lymphoma progressing to MM exists in the dog.22,23
Pathology and Natural Behavior
Multiple myeloma is a systemic proliferation of malignant plasma cells or their precursors arising as a clone of a single cell that usually involves multiple bone marrow sites in dogs. In cats, as previously stated, a blurring of the distinction of MM and multicentric noncutaneous EMP within the MRD occurs because widespread abdominal organ involvement without significant bone marrow infiltration has been described in a significant proportion of cases in European compilations.11,24 Because both MM and multicentric noncutaneous EMP have a similar clinical course and widespread systemic involvement with hyperglobulinemia in cats, they will be discussed as MM in this chapter. Malignant plasma cells can have a varied appearance on histologic sections and cytologic preparations. The degree of differentiation ranges from those resembling normal plasma cells in late stages of differentiation (Figure 32-20) to very large anaplastic round cells (often referred to as plasmablasts), with a high mitotic index representing early stages of differentiation.5,6,9,24,25 Binucleate and multinucleate cells are often present (see Figure 7-32, Chapter 7). In 16 cats with MM in a North American case series, the majority (83%) of plasma cells were immature and had marked atypia, including increased size, multiple nuclei, clefted nuclei, anisocytosis, anisokaryosis, variable N : C ratios, decreased chromatin density, and variable nucleoli; nearly one-quarter had “flame cell” morphology characterized by peripheral eosinophilic cytoplasmic processes.9 However, in a European compilation of feline multicentric noncutaneous MRD cases (n = 17), 78% had well-differentiated morphologies.24 The authors of this latter case series developed a grading system dependent on the percentage of plasmablasts within the neoplastic cells in which well-differentiated, intermediate-grade, and poorly differentiated have less than 15%, 15% to 49%, and 50% or more plasmablasts, respectively. Malignant plasma cells typically produce an overabundance of a single type of or component of immunoglobulin, which is referred to as the M component (Figure 32-21). The M component can be represented by any class of the entire immunoglobulin or only a portion of the molecule, such as the light chain (Bence Jones protein) or heavy chain (heavy chain disease) of the molecule. In the dog, the M component is usually represented by either IgA or IgG immunoglobulin types in nearly equal incidence, whereas the ratio of IgG : IgA in cats is approximately 5 : 1 in some reports and approximately 1 : 1 in others.1,5-9,24,26 That being said, in the author’s (DMV) experience, the vast majority of canine cases are of the IgA type. If the M component is the IgM type, the term macroglobulinemia (Waldenström’s) is often applied. Several cases of biclonal gammopathy in dogs and cats have been reported.9,11,12,27-32 Several cases of nonsecretory MM have been reported in dogs.33,34 Rarely, cryoglobulinemia occurs in dogs with MM and IgM macroglobulinemia and has been reported in a cat with IgG myeloma.6,35-37 Cryoglobulins are paraproteins that are insoluble at temperatures below 37° C and require blood collection and clotting to be performed at 37° C prior to serum separation. If whole blood is allowed to clot at temperatures below this, the protein precipitates in the clot and is lost. Pure light-chain M component is rare but has been reported in both dogs and cats.38,39
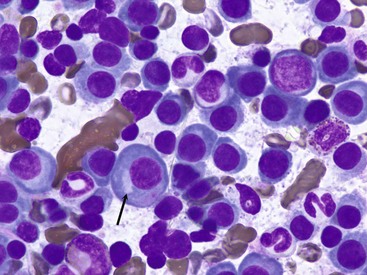
Figure 32-20 Bone marrow aspirate from a dog with multiple myeloma showing an overabundance of large neoplastic plasma cells with characteristic paranuclear clear zone representing the Golgi apparatus (arrow). (Dif-quick stain, ×100 objective.)
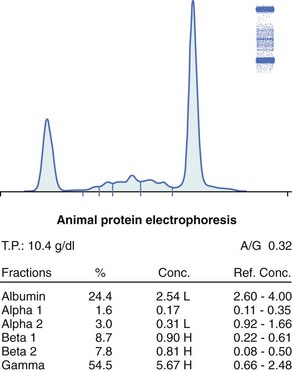
Figure 32-21 Serum protein electrophoresis from a cat with multiple myeloma. Stained cellulose acetate electrophoretic strip (upper right corner) with accompanying densitogram. Note large M-component spike (representing an IgG monoclonal gammopathy) present in the gamma region. (Courtesy Dr. Frances Moore, Marshfield Laboratories, Marshfield, WI.)
The pathology associated with MM is a result of either high levels of circulating M component, organ or bone infiltration with neoplastic cells, or both. Associated pathologic conditions include bone disease, bleeding diathesis, hyperviscosity syndrome, renal disease, hypercalcemia, immunodeficiency (and subsequent susceptibility to infections), cytopenias secondary to myelophthisis, and cardiac failure.
Bone lesions can be isolated, discrete osteolytic lesions (including pathologic fractures) (Figure 32-22, A) or diffuse osteopenias, or both (Figure 32-23). Approximately one-quarter to two-thirds of dogs with MM have radiographic evidence of bony lysis or diffuse osteoporosis.1,5,6 The incidence of radiographic skeletal lesions in cats varies tremendously within reports, from as few as 8% in European case series to as high as 65% in North American case series.8,9,11,12,26 Those bones engaged in active hematopoiesis are more commonly affected and include the vertebrae, ribs, pelvis, skull, and proximal or distal long bones. Skeletal lesions are rare with IgM (Waldenström’s) macrogammaglobulinemia, in which malignant cells often infiltrate the spleen, liver, and lymph tissue rather than bone.6,40-42
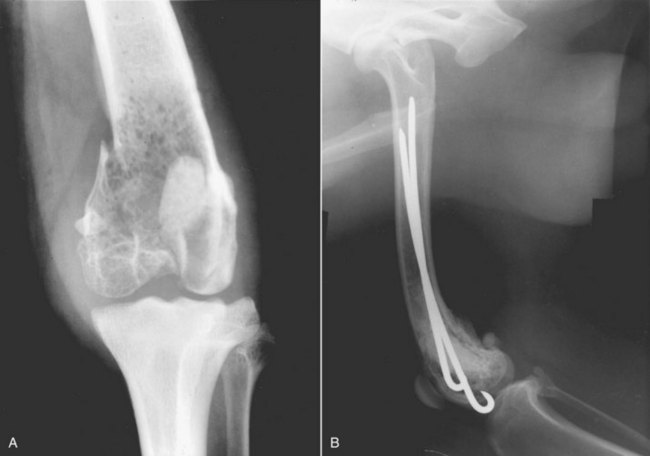
Figure 32-22 A, Radiograph of a distal femur in a dog demonstrating severe osteolysis and a pathologic fracture secondary to a plasma cell tumor. B, Radiograph of the same pathologic fracture after surgical repair with Rush rods and bone cement. Local site was treated with adjuvant radiation. The dog was continued on chemotherapy for 2 more years and did well.
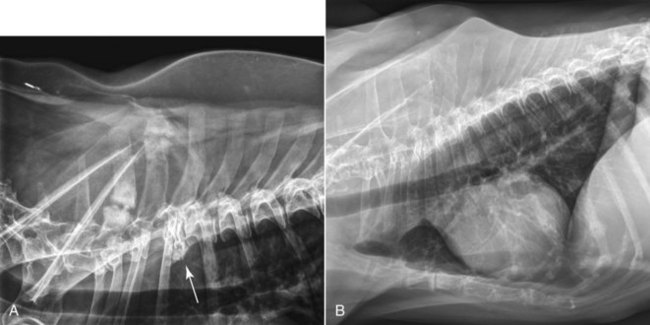
Figure 32-23 A, Lateral thoracic radiographs of a dog showing multiple expansile lytic lesions and pathologic fractures of the dorsal spinous processes and collapse fracture (arrow) of the third thoracic vertebral body. B, Lateral thoracic radiographs of a dog with diffuse osteopenia secondary to multiple myeloma. Note the overall decreased opacity of the lumbar vertebrae and dorsal spinous processes secondary to diffuse marrow involvement causing loss of bone trabeculae and thinning of the cortices.
Bleeding diathesis can result from one or a combination of events. M components may interfere with coagulation by (1) inhibiting platelet aggregation and the release of platelet factor-3; (2) causing adsorption of minor clotting proteins; (3) generating abnormal fibrin polymerization; and (4) producing a functional decrease in calcium.6,43,44 Approximately one-third of dogs and one-quarter of cats have clinical evidence of hemorrhage.1,9,11,12 In dogs, nearly half have abnormal prothrombin (PT) and partial thromboplastin (PTT) times. Thrombocytopenia may also play a role if bone marrow infiltration is significant (i.e., myelophthisis).
Hyperviscosity syndrome (HVS) represents one of a constellation of clinicopathologic abnormalities resulting from greatly increased serum viscosity. The magnitude of viscosity changes is related to the type, size, shape, and concentration of the M component in the blood. HVS is more common with IgM macroglobulinemias due to the high molecular weight of this class of immunoglobulin. IgA-secreting myelomas (usually present as a dimer in the dog), may undergo polymerization resulting in increased serum viscosity.1,6,45 IgG-associated HVS can also occur, albeit less frequently. High serum viscosity occurs in approximately 20% of dogs with MM and can result in bleeding diathesis, neurologic signs (e.g., dementia, depression, seizure activity, coma), ophthalmic abnormalities (e.g., dilated and tortuous retinal vessels, retinal hemorrhage [Figure 32-24], retinal detachment), and increased cardiac workload with the potential for subsequent development of cardiomyopathy.* These consequences are thought to be a result of sludging of blood in small vessels, ineffective delivery of oxygen and nutrients, and coagulation abnormalities. HVS has been reported in cats with IgG-, IgA-, and IgM-secreting tumors.6,8,49-53 In several of these cases, relative serum viscosity was increased above control ranges.
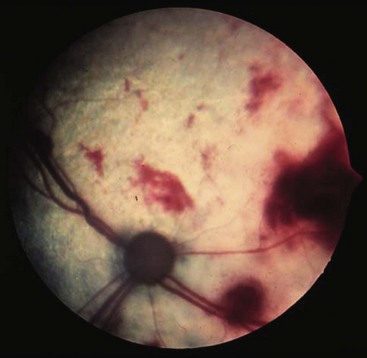
Figure 32-24 Multiple retinal hemorrhages on the fundus in a cat with hyperviscosity syndrome secondary to multiple myeloma.
Renal disease is present in approximately one-third to one-half of dogs with MM, and azotemia was observed in one-third of cats in one report.1,5,9,11 The pathogenesis of renal failure is often multifactorial and can ensue as a result of Bence Jones (light-chain) proteinuria, tumor infiltration into renal tissue, hypercalcemia, amyloidosis, diminished perfusion secondary to hyperviscosity syndrome, dehydration, or ascending urinary tract infections.1,6,43,44 Normally, heavy- and light-chain synthesis is well balanced in nonneoplastic immunoglobulin production. In the case of MM, an unbalanced excess of light-chain products may be produced. Light chains are of low molecular weight and are normally filtered by the renal glomerulus, and their presence in urine can result in protein precipitates and subsequent renal tubular injury. The presence of light chains in urine without a concomitant monoclonal spike in serum, although rare, is indicative of pure light-chain disease.38 Tubules become obstructed by large laminated casts containing albumin, immunoglobulin, and light chains.6,38,43,44 Bence Jones proteinuria occurs in approximately 25% to 40% of dogs with MM.1,5,6 Bence Jones proteinuria is reported to occur in approximately 40% of cats with MM/MRD.9,11 Hypercalcemia is reported in 15% to 20% of dogs with MM and is thought to result primarily from the production of osteoclast-activating factor by neoplastic cells.1,6,54 Other factors, including increased levels of various cytokines, TNF, IL-1, and IL-6 have been implicated in human MM. In two dogs with MM and hypercalcemia, serum elevations in circulating N-terminal PTHrP were noted.55 Hypercalcemia may also be exacerbated by associated renal disease. Hypercalcemia, initially thought to be a rare event in cats with MM, occurred in 10% to 25% of recently reported cases.9,11,12,56
Susceptibility to infection and immunodeficiency have long been associated with MM and are often the ultimate cause of death in affected animals.1,6,26 Infection rates in humans with MM are fifteen times higher than normal and usually represent pneumonia or urinary tract infections.57 Response to vaccination has also been shown to be suppressed in humans with MM.57 Immunoglobulin levels are often severely depressed in affected animals.6 In addition, leukopenias may be present secondary to myelophthisis.
Variable cytopenias may be observed in association with MM. A normocytic, normochromic, nonregenerative anemia is encountered in approximately two-thirds of dogs with MM.1,5,6 This can result from marrow infiltration (myelophthisis), blood loss from coagulation disorders, anemia of chronic disease, or increased erythrocyte destruction secondary to high serum viscosity. Rare erythrophagocytic forms of MM have also been reported in both dogs and cats and may contribute to anemia.58,59 Similar factors lead to thrombocytopenia and leukopenia in nearly one-third and one-quarter of dogs with MM, respectively. In cats, approximately two-thirds, half, and one-third will be anemic, thrombocytopenic, and neutropenic, respectively.9,11,12
Cardiac disease if present is usually a result of excessive cardiac workload and myocardial hypoxia secondary to hyperviscosity.43,45,53 Myocardial infiltration with amyloid and anemia may be complicating factors. Nearly half of cats with MM in one report presented with a cardiac murmur, the etiology of which was not established.9 Three cats with HVS presented with congestive heart failure, murmurs, and echocardiographic signs consistent with hypertrophic cardiomyopathy.53
History and Clinical Signs
Clinical signs of MM may be present up to a year prior to diagnosis with a median duration of one month reported in dogs.1,9 In one cat, M-component elevations were detected 9 years prior to clinical presentation. In this latter case, the M-component elevation was consistent with monoclonal gammopathy of unknown significance (MGUS). MGUS (i.e., benign, essential, or idiopathic monoclonal gammopathy) is a benign monoclonal gammopathy that is not associated with osteolysis, bone marrow infiltration, or Bence Jones proteinuria. MGUS has also been reported in dogs.60,61 Signs of MM can be variable based on the wide range of pathologic effects possible. Tables 32-14 and 32-15 list the relative frequencies of clinical signs observed in the dog and cat, respectively, based on a compilation of several reports.* Bleeding diathesis is usually represented by epistaxis and gingival bleeding. Funduscopic abnormalities may include retinal hemorrhage (see Figure 32-24), venous dilatation with sacculation and tortuosity, retinal detachment, and blindness.† CNS signs may include dementia, seizure activity, tremors, and deficiencies in midbrain or brain-stem localizing reflexes secondary to HVS or extreme hypercalcemia. Signs reflective of transverse myelopathies secondary to vertebral column infiltration, pathologic fracture, or extradural mass compression can also occur.1,6,35,62,63 One case of ataxia and seizure activity in a dog with EMP secondary to tumor-associated hypoglycemia has been reported.64 Additionally, paraneoplastic polyneuropathy has been reported in a dog with MM.65 A history of chronic respiratory infections and persistent fever may also be present in cats. Hepatosplenomegaly and renomegaly can occur due to organ infiltration. Bleeding diathesis due to HVS is less common in the cat; however, epistaxis, pleural and peritoneal hemorrhagic effusions, retinal hemorrhage, and central neurologic signs have been reported.6,8,49-53 Polydipsia and polyuria can occur secondary to renal disease or hypercalcemia, and dehydration may develop. Hindlimb paresis secondary to osteolysis of lumbar vertebral bodies or extradural compression has been reported in cats.12,66
Table 32-14
Frequency of Clinical Signs Reported for Dogs with Multiple Myeloma (n = 60)
| Clinical Sign | Frequency Reported (%) |
| Lethargy and weakness | 62 |
| Lameness | 47 |
| Bleeding diathesis | 37 |
| Funduscopic abnormalities | 35 |
| Polyuria/polydipsia | 25 |
| CNS deficits | 12 |
Data from Matus RE, Leifer CE, MacEwen EG, et al: Prognostic factors for multiple myeloma in the dog, J Am Vet Med Assoc 188:1288–1291, 1986.
Table 32-15
Approximate Frequency of Clinical Signs Reported for Cats with Myeloma-Related Disorders (n = 53)
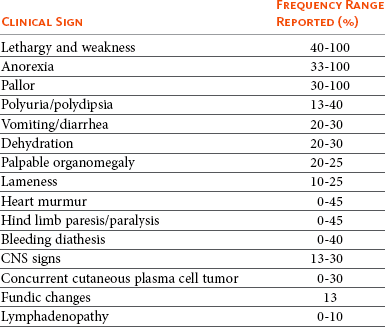
Data from MacEwen EG, Hurvitz AI: Diagnosis and management of monoclonal gammopathies, Vet Clin N Am Small Anim Pract 7:119–132, 1977; Patel RT, Caceres A, French AF, et al: Multiple myeloma in 16 cats: a retrospective study, Vet Clin Pathol 34:341–352, 2005; Mellor PJ, Haugland S, Murphy S, et al: Myeloma-related disorders in cats commonly present as extramedullary neoplasms in contrast to myeloma in human patients: 24 cases with clinical follow-up, J Vet Intern Med 20:1376–1383. 2006; Hanna F: Multiple myelomas in cats, J Feline Med Surg 7:275–287, 2005; and Drazner FH: Multiple myeloma in the cat, Comp Cont Ed Pract Vet 4:206–216, 1982.
Diagnosis and Staging
The diagnosis of MM in dogs usually follows the demonstration of bone marrow plasmacytosis (see Figure 32-20), the presence of osteolytic bone lesions (see Figures 32-22 and 32-23), and the demonstration of serum or urine myeloma proteins (M component) (see Figure 32-21). In the absence of osteolytic bone lesions, a diagnosis can also be made if marrow plasmacytosis is associated with a progressive increase in the M component. In the cat, because the degree of bone marrow infiltration may not be as marked, it has been suggested that consideration of plasma cell morphology and visceral organ infiltration (Figure 32-25) be given in cases with demonstrable M-component disease in the absence of marked (<20%) marrow plasmacytosis.9,11,24
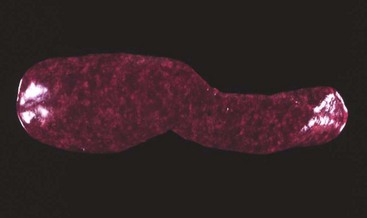
Figure 32-25 Necropsy specimen of a spleen from a cat with multiple myeloma showing diffuse plasma cell infiltration.
All animals suspected of plasma cell tumors should receive a minimal diagnostic evaluation including a CBC, platelet count, serum biochemistry profile, and urinalysis. Particular attention should be paid to renal function and serum calcium levels. If clinical hemorrhage is present, a coagulation assessment (e.g., platelet count, PT, PTT) and serum viscosity measurements are indicated. All animals should undergo a careful funduscopic examination. Serum electrophoresis and immunoelectrophoresis are performed to determine the presence of a monoclonal M component (see Figure 32-21) and to categorize the immunoglobulin class involved. Heat precipitation and electrophoresis of urine may be performed to determine presence of Bence Jones proteinuria because commercial urine dipstick methods are not capable of this determination. Definitive diagnosis usually follows the performance of a bone marrow aspiration in the dog. A bone marrow core biopsy or multiple aspirations may be necessary due to the possibility of uneven clustering or infiltration of plasma cells in the bone marrow. Normal marrow contains less than 5% plasma cells, whereas myelomatous marrow often greatly exceeds this level. Current recommendations require more than 20% marrow plasmacytosis to be present, although a 10% cutoff in cats has been recently recommended with special attention to cellular atypia.9 Even the 10% threshold is problematic in cats, and cellular atypia and visceral organ involvement (assessed through needle aspiration cytology or tissue biopsy) should be considered equally important in the species.9,11,24 Rarely, biopsy of osteolytic lesions (i.e., Jamshidi core biopsy; see Chapter 24) is necessary for diagnosis in the dog. In one case of MM in a dog, splenic aspirates were diagnostically helpful.67 Overall frequencies of clinical diagnostic abnormalities for dogs and cats with MM are compiled from published series having at least five cases each and are listed in Table 32-16.
Table 32-16
Approximate Frequency of Clinical Diagnostic Abnormalities for Dogs and Cats* with Multiple Myeloma (n = 53 cats, 82 dogs)
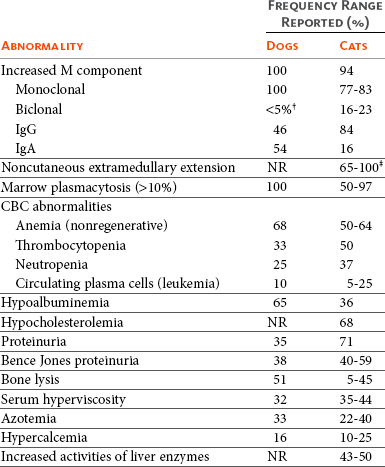
NR, Not reported; CBC, complete blood count.
*Includes noncutaneous extramedullary plasmacytoma (EMP) cases from Mellor.11
†Several single case reports exist for biclonal gammopathy in dogs with MM.
‡11 of 11 in one report had evidence of infiltration in either spleen, lymph node, or liver.
Data from Matus RE, Leifer CE, MacEwen EG, et al: Prognostic factors for multiple myeloma in the dog. J Am Vet Med Assoc 188:1288–1291, 1986; MacEwen EG, Hurvitz AI: Diagnosis and management of monoclonal gammopathies, Vet Clin N Am Small Anim Pract 7:119–132, 1977; Patel RT, Caceres A, French AF, et al: Multiple myeloma in 16 cats: a retrospective study, Vet Clin Pathol 34:341–352, 2005; Mellor PJ, Haugland S, Murphy S, et al: Myeloma-related disorders in cats commonly present as extramedullary neoplasms in contrast to myeloma in human patients: 24 cases with clinical follow-up, J Vet Intern Med 20:1376–1383, 2006; Hanna F: Multiple myelomas in cats, J Feline Med Surg 7:275–287, 2005; and Drazner FH: Multiple myeloma in the cat, Comp Cont Ed Pract Vet 4:206–216, 1982.
Immunohistochemical and Molecular Diagnostics
Histochemical and immunohistochemical analyses of cells or tissues suspected of MRD are more often applied in the case of solitary plasmacytomas or where EMP is suspected in the absence of marrow involvement and will be discussed in subsequent sections; however, they have been occasionally useful in the diagnosis of MM. Molecular diagnostic techniques for MM have received limited use thus far in veterinary oncology; however, determining clonality of the immunoglobulin heavy chain variable region gene has been performed in feline plasmacytoma and myeloma using PARR techniques (see Chapter 8),68 and use of this technology in cases where diagnosis is not straightforward awaits further investigation. The author has used PARR analysis both before treatment and after clinical remission in a small number of dogs with MM involved in clinical trials and documented its utility (1) for initial diagnosis and (2) to characterize molecular remission.
Imaging
Routine thoracic and abdominal radiographs are recommended in suspected cases. Occasionally, bony lesions can be observed in skeletal areas on these standard films, and organomegaly (liver, spleen, kidney) is observed in the majority of cats.9,11 Abdominal ultrasound is recommended in all cats suspected of MM because this modality reveals involvement of one or more abdominal organs in the majority of cases.9,11 These include splenomegaly with or without nodules, diffuse hyperechoic hepatomegaly with or without nodules, renomegaly, and iliac lymph node enlargement. In one case series in cats, 85% of organs with ultrasonographic abnormalities were subsequently confirmed to have plasma cell infiltration.11 Skeletal survey radiographs are recommended to determine presence and extent of osteolytic lesions, which may have diagnostic, prognostic, and therapeutic implications. Although nuclear scintigraphy (bone scan) for clinical staging of dogs with MM has been performed, due to the predominant osteolytic activity with osteoblastic inactivity present, scans seldom give positive results and are therefore not useful for routine diagnosis.69 In physician-based oncology, bone mineral density analysis (dual-energy x-ray absorptiometry [DEXA] scan) to document osteoporosis, MRI scan of bone marrow, and PET/CT are commonly used for staging; however, these modalities have not been applied consistently in the veterinary literature. A clinical staging system for canine MM has been suggested1; however, at present, no prognostic significance has been attributed to it.
Differential Diagnosis of MM
Disease syndromes other than plasma cell tumors can be associated with monoclonal gammopathies and should be considered in any list of differentials. These include other lymphoreticular tumors (B-cell lymphoma, extramedullary plasmacytoma, chronic and acute B-lymphocytic leukemia), chronic infections (e.g., ehrlichiosis, leishmaniasis, FIP), and MGUS.*
Treatment
Initial Therapy of Multiple Myeloma
Therapy for MM is directed at both the tumor cell mass and the secondary systemic effects they elicit. All diagnostic procedures should be completed before initiating primary therapy to ensure a diagnosis is complete and baseline values are procured for monitoring response. Chemotherapy is effective at reducing myeloma cell burden, relieving bone pain, allowing for skeletal healing, and reducing levels of serum immunoglobulins in the majority of dogs with MM and will greatly extend both the quality and quantity of most patients’ lives. MM in dogs is initially a gratifying disease to treat for both the clinician and the companion animal owner, although complete elimination of neoplastic myeloma cells is rarely achieved and eventual relapse is to be expected. Unlike dogs, only one-half of cats with MM will respond to chemotherapy and most responses will be short-lived; however, several long-term responses (i.e., >1 year) have been reported and treatment should be attempted when educated clients decide on a therapeutic option.*
Melphalan, an alkylating agent, is the chemotherapeutic of choice for the treatment of multiple myeloma.1,6 In the dog, an initial starting dose of 0.1 mg/kg PO, once daily for 10 days, is then reduced to 0.05 mg/kg PO, once daily continuously. The addition of prednisone therapy is thought to increase the efficacy of melphalan therapy. Prednisone is initiated at a dosage of 0.5 mg/kg PO, once daily for 10 days, then reduced to 0.5 mg/kg every other day prior to discontinuation after 60 days of therapy. Melphalan, however, is continued at 0.05 mg/kg/day until clinical relapse occurs or myelosuppression necessitates a dose reduction. The vast majority of dogs on melphalan and prednisone combination therapy tolerate the regimen well. The most clinically significant toxicity of melphalan is myelosuppression, in particular a delayed thrombocytopenia. CBCs, including platelet counts, should be performed biweekly for 2 months of therapy and monthly thereafter. If significant myelosuppression occurs (usually thrombocytopenia or neutropenia), reduction of the dosage or treatment frequency may be necessary. An alternative pulse-dosing regimen for melphalan (7 mg/m2 PO, daily for 5 consecutive days every 3 weeks) has been used successfully by the author in a small number of cases in which myelosuppression was limiting more conventional continuous low-dose therapy. This pulse-dose regimen is now being used first-line by the author with the caveat that long-term response data are currently lacking.
Melphalan and prednisone therapy can also be used in cats with multiple myeloma; however, it appears this protocol is more myelosuppressive than in the dog and careful monitoring is required. In the cat, a dosing schedule similar to the dog has been reported12,26; 0.1 mg/kg (approximately 0.5 mg, or one-quarter of a 2 mg tablet) once daily for 10 to 14 days, then every other day until clinical improvement or leukopenia develop. Long-term continuous maintenance (0.1 mg/kg, once every 7 days) has been advocated.12 An alternative protocol advocated in the cat uses melphalan at 2 mg/m2, once every 4 days continuously, and appears to be well tolerated.11
Cyclophosphamide has been used as an alternative alkylating agent or in combination with melphalan in dogs and cats with MM.1,6,11 There is no evidence to suggest it is superior to melphalan therapy. In the author’s practice, cyclophosphamide is limited to those cases presenting with severe hypercalcemia or with widespread systemic involvement in which a faster acting alkylating agent may more quickly alleviate systemic effects of the disease. Cyclophosphamide is initiated at a dosage of 200 mg/m2 IV, once, at the same time oral melphalan therapy is started. Because cyclophosphamide is less likely to affect thrombocytes, it may be substituted in those patients in which thrombocytopenia has developed secondary to long-term melphalan use.
Chlorambucil, another alkylating agent, has been used successfully for the treatment of IgM macroglobulinemia in dogs at a dosage of 0.2 mg/kg PO, once daily.6,40 Little or no clinical signs of toxicity result from this dosing schedule. Chlorambucil has also been used in cats with MRD.11
Lomustine (CCNU), yet another alkylating agent, has been used in a limited number of cats with MM and a partial response has been reported following dosing at 50 mg/m2 PO, every 21 days.74
Evaluation of Response to Therapy
Evaluation of response to systemic therapy for multiple myeloma is based on improvement in clinical signs, clinicopathologic parameters, and radiographic improvement of skeletal lesions or ultrasonographic improvement of organ involvement.1,6,11 Subjective improvement in clinical signs of bone pain, lameness, lethargy, and anorexia should be evident within 3 to 4 weeks following initiation of therapy. Objective laboratory improvement, including reduction in serum globulin, immunoglobulin, and calcium, along with normalization of the hemogram, is usually noted within 3 to 6 weeks (Figure 32-26). Radiographic improvement in osteolytic bone lesions may take months and resolution may only be partial. Ophthalmic complications (including long-standing retinal detachments) and paraneoplastic neuropathies can be expected to resolve along with tumor mass.48,65 In cats responding to chemotherapy, clinical improvement is noted in 2 to 4 weeks and serum protein and radiographic bone abnormalities were greatly improved by 8 weeks.11,12
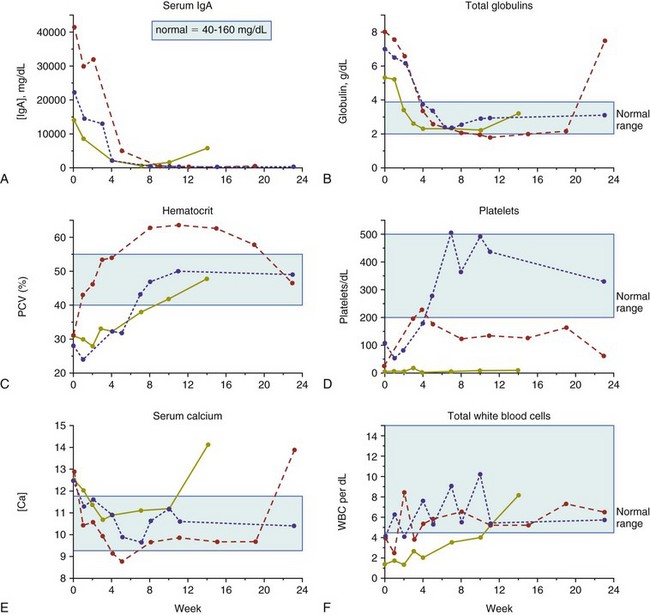
Figure 32-26 Clinicopathologic data changes over time (weeks) after initiation of cytotoxic chemotherapy in three dogs with IgA multiple myeloma. Light blue area, Normal reference range. A, Serum IgA (mg/dL); B, total globulins (g/dL); C, hematocrit (%); D, platelets/dL; E, serum calcium (mg/dL); F, total white blood cells/dL.
As previously discussed, complete resolution of MM does not generally occur and a good response is defined as a reduction in measured M component (i.e., immunoglobulin or Bence Jones proteins) of at least 50% of pretreatment values.6 Reduction in serum immunoglobulin levels may lag behind reductions in Bence Jones proteinuria because the half-lives are 15 to 20 days and 8 to 12 hours, respectively.75 For routine follow-up, quantification of the increased serum globulin, immunoglobulin, or urine Bence Jones protein is performed monthly until a good response is noted and then every 2 to 3 months thereafter. Repeat bone marrow aspiration or imaging (in the case of visceral disease) for evaluation of plasma cell infiltration may be occasionally necessary. Bone marrow reevaluation is particularly prudent when cytopenias develop during chemotherapy, and drug-induced myelosuppression must be differentiated from myelophthisis due to neoplastic marrow recurrence.
Therapy Directed at Complications of Multiple Myeloma
The long-term control of complications, including hypercalcemia, HVS, bleeding diathesis, renal disease, immunosuppression, ophthalmic complications, and pathologic skeletal fractures, depend on controlling the primary tumor mass. Therapy directed more specifically at these complications may, however, be indicated in the short term.
If hypercalcemia is marked and significant clinical signs exist, standard therapies, including fluid diureses, with or without pharmacologic agents (e.g., calcitonin), may be indicated (see Chapter 5). Moderate hypercalcemia will typically resolve within 2 to 3 days following initiation of melphalan/prednisone chemotherapy.
HVS is best treated in the short term by plasmapheresis.* Whole blood is collected from the patient and centrifuged to separate plasma from packed cells. Packed red cells are resuspended in normal saline or other crystalloid and reinfused into the patient. Bleeding diathesis will usually resolve along with HVS; however, platelet-rich plasma transfusions may be necessary in the face of thrombocytopenia.
Renal impairment may necessitate aggressive fluid therapy in the short term and maintenance of adequate hydration in the long term. Careful attention to secondary urinary tract infections and appropriate antimicrobial therapy is indicated. Ensuring adequate water intake at home is important, and occasionally, educating owners in subcutaneous fluid administration is indicated. Continued monitoring of renal function is recommended along with follow-up directed at tumor response.
Patients with MM can be thought of as immunologically impaired. Some have recommended prophylactic antibiotic therapy in dogs with MM6; however, in humans, no benefit for this approach over diligent monitoring and aggressive antimicrobial management when indicated has been observed.43 Cidal antimicrobials are preferred over static drugs, and avoidance of nephrotoxic antimicrobials is recommended.
Pathologic fractures of weight-bearing long bones and vertebrae resulting in spinal cord compression may require immediate surgical intervention in conjunction with systemic chemotherapy. Orthopedic stabilization of fractures should be undertaken and may be followed with external-beam RT (see Figure 32-22). Recently, inhibition of osteoclast activity by bisphosphonate drugs has been shown to reduce the incidence and severity of skeletal complications of MM in humans.69 This class of drugs may hold promise for use in dogs and cats with various skeletal tumors; however, they have not been adequately evaluated in MRD.78
Rescue Therapy
When MM eventually relapses in dogs and cats undergoing melphalan therapy or in the uncommon case that is initially resistant to alkylating agents, rescue therapy may be attempted. The author has had success with VAD, which is a combination of doxorubicin (30 mg/m2 IV, every 21 days), vincristine (0.7 mg/m2 IV, days 8 and 15), and dexamethasone sodium phosphate (1.0 mg/kg IV, once a week on days 1, 8, and 15), given in 21-day cycles. Whereas most dogs initially respond to this rescue protocol, the duration of response tends to be short, lasting only a few months. High-dose cyclophosphamide (300 mg/m2 IV, every 7 days) has also been used with limited success as a rescue agent. Liposomal doxorubicin has produced a long-term remission in a dog with MM previously resistant to native doxorubicin.79
Investigational Therapies
MM is ultimately a uniformly fatal disease in most species, including humans, and thus significant effort is being placed on investigational therapies for this disease. Currently, bone marrow ablative therapy and marrow or stem cell rescue, thalidomide (and other antiangiogenic therapies), bortezomib (a proteasome inhibitor), arsenic trioxide, the bisphosphonates, and several molecular targeting therapies are under investigation; however, their use in veterinary species is limited or completely absent at present. The promise of molecular targeted therapies is, however, foreshadowed by a case of a dog with MM that was resistant to melphalan, prednisone, and doxorubicin that subsequently achieved a partial response to tyrosine kinase inhibitor therapy (toceranib; see Chapter 14, Section B) that was maintained for 6 months.18
Prognosis
The prognosis for dogs with MM is good for initial control of tumor and a return to good quality of life. In a group of 60 dogs with MM, approximately 43% achieved a complete remission (i.e., serum immunoglobulins normalized), 49% achieved a partial remission (i.e., immunoglobulins <50% pretreatment values), and only 8% did not respond to melphalan and prednisone chemotherapy.1 Long-term survival is the norm, with a median of 540 days reported (Figure 32-27). The presence of hypercalcemia, Bence Jones proteinuria, and extensive bony lysis are known negative prognostic indices in the dog.1 The long-term prognosis for dogs with MM is poor because recurrence of tumor mass and associated clinical signs is expected. Eventually, the tumor is no longer responsive to available chemotherapeutics and death follows from renal failure, sepsis, or euthanasia for intractable bone or spinal pain.1,6
Figure 32-27 Survival curve of 37 dogs with multiple myeloma treated with chemotherapy. The median survival time (MST) is 540 days. Rights were not granted to include this figure in electronic media. Please refer to the printed book. (From Matus RE, Leifer CE, MacEwen EG, et al: Prognostic factors for multiple myeloma in the dog, J Am Vet Med Assoc 188:1288–1292, 1986.) J Am Vet Med Assoc
The prognosis for MM in the cat is not as favorable in the short term as it is in the dog.6,9,11,12,26 Whereas most cats (approximately 60%) transiently respond to melphalan/prednisone or COP-based protocols, most responses are partial and not durable. Typically, cats with MM succumb to their disease within 4 months.8,9,12,26 However, long-term survivors (>1 year) have been occasionally reported.* In one European case series, seven cats undergoing melphalan or COP-based therapy had a median survival of 9.5 months.11 One investigator grouped MM in cats into two prognostic categories (Table 32-17) based on criteria known to predict behavior in dogs.12 Although no rigorous statistical analysis was performed on this small group of nine cats, the median survival for cats in “aggressive” and “nonaggressive” categories was 5 days and 387 days, respectively.
Table 32-17
Classification of Multiple Myeloma in Cats Based on Clinical and Diagnostic Criteria Suspected of Predicting Prognosis
| Behavior Category | Criteria |
| Aggressive | Hypocalcemia, presence of bony lesions with pathological fracture, low packed cell volume (PCV), presence of light-chain Bence Jones protein in urine, azotemia, hypercreatinemia, persistence of high serum protein level after 8 weeks of treatment, little or no clinical improvement. |
| Less aggressive | Normal serum calcium, normal creatinine, blood urea nitrogen (BUN), PCV levels, presence of bony lesions without pathologic fractures, absence of light-chain Bence Jones protein, normalization of serum protein level after 8 weeks of treatment. |
Data from Hanna F: Multiple myelomas in cats, J Feline Med Surg 7:275–287, 2005.
Experience in dogs with IgM macroglobulinemia is limited.6,40-42 Response to chlorambucil is to be expected, and in nine treated dogs, 77% achieved remission with a median survival of 11 months.6
Solitary and Extramedullary Plasmacytic Tumors
Solitary collections of monoclonal plasmacytic tumors can originate in soft tissues or bone and are referred to as extramedullary plasmacytoma (EMP) and solitary osseous plasmacytoma (SOP), respectively. The systemic, multicentric, biologically aggressive EMP syndrome encountered in cats11,24 has been discussed in the MM section and will not be included in this discussion. A number of large case compilations of cutaneous plasmacytoma have been reported in the dog.17,80-86 The most common locations for EMP in the dog are cutaneous (86%; Figure 32-28), the mucous membranes of the oral cavity and lips (9%; Figure 32-29), and the rectum and colon (4%). The skin of the limbs and head (including the ears) are most frequently reported cutaneous sites. Other sites accounted for only 1% of the remaining cases and can include stomach, spleen, genitalia, eye, uterus, liver, larynx, trachea, third eyelid, sinonasal cavity, and intracranial sites.87-94 The American cocker spaniel, English cocker spaniel, and West Highland white terrier (and perhaps Yorkshire terriers, Boxers, German shepherds, and Airedale terriers) are at increased risk for developing plasmacytomas and the median age of affected dogs is 9 to 10 years of age.86
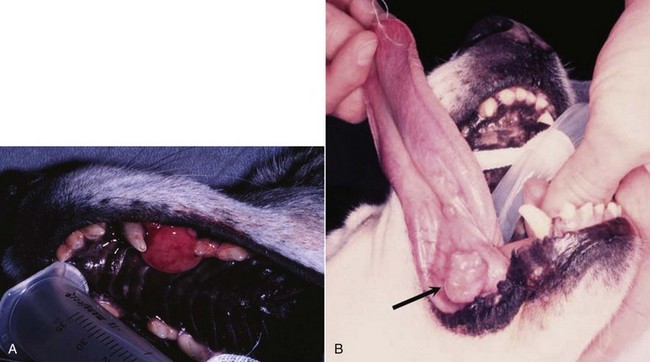
Figure 32-29 Examples of oral solitary plasmacytoma in dogs; one involving the maxilla (A), the other involving the underside of the tongue (B). Both dogs were cured following surgical excision.
Cutaneous and oral EMP in dogs are typically benign tumors that are highly amenable to local therapy. There exists, however, a rare form of multiple cutaneous plasmacytomas in dogs that is part of a more generalized biologically aggressive MM process.95,96 The natural behavior of noncutaneous/nonoral EMP appears to be somewhat more aggressive in the dog. GI EMP have been reported on a number of occasions in the veterinary literature, including the esophagus,91 stomach,97,98 and small99 and large intestine.98-101 Metastasis to associated lymph nodes is more common in these cases; however, bone marrow involvement and monoclonal gammopathies are less commonly encountered. Colorectal EMPs tend to be of low biologic aggressiveness, and most do not recur following surgical excision.100 Conversely, the majority of SOPs eventually progress to systemic MM; however, the time course from local tumor development to systemic MM may be many months to years.33,102 SOPs have been reported in the dog involving the appendicular skeleton, as well as the zygomatic arch, and ribs.33
SOPs are less common in cats, and fewer reports exist in the literature.11,22,103-107 They occur in older cats (mean ages 9 to 14 years), with no significant sex predilection. The skin is the most common site; however, other sites include the oral cavity, eye, GI tract, liver, subcutaneous tissues, and brain. Reports exist of cutaneous EMP in cats that progressed to systemic MRD.11,22,105
Clinical Signs
Clinical signs associated with SOPs relate to the location of involvement, or in those rare cases with high levels of M component, HVS may occur. Most cutaneous plasmacytomas are solitary, smooth, raised pink nodules from 1 to 2 cm in diameter (see Figure 32-28), although tumors as large as 10 cm have been reported. Combining large series, greater than 95% occur as solitary masses and less than 1% occur as part of a systemic MM process.17,80-86,95,96 Cutaneous and oral EMPs usually have a benign course with no related clinical signs. GI EMP, however, typically presents with relatively nonspecific signs, which may suggest alimentary involvement. Colorectal plasmacytomas usually present with rectal bleeding, hematochezia, tenesmus, and rectal prolapse.100 One case of ataxia and seizure activity in a dog with EMP secondary to tumor-associated hypoglycemia has been reported.64 SOP is usually associated with pain and lameness if the appendicular skeleton is affected or neurologic signs if vertebral bodies are involved.
Diagnosis for Solitary Plasmacytic Tumors
The diagnosis of SOP and EMP usually requires tissue biopsy or FNA for diagnosis. Cells making up solitary plasmacytic tumors in both cats and dogs have been histologically classified into mature, hyaline, cleaved, asynchronous, monomorphous blastic and polymorphous blastic cell types; however, no prognostic significance has been observed following classification, although it has been suggested that the polymorphous-blastic type may act more aggressively in the dog.17,86,103 A different classification was proposed for EMP in cats based on percentage of plasmablasts (see previous section), and some prognostic importance has been documented.24 In the case of poorly differentiated plasmacytic tumors, immunohistochemical studies, directed at detecting immunoglobulin, light- and heavy-chains, MM-1/interferon regulatory factor-4 (MUM1/IRF4), and thioflavin T, may be helpful in differentiation from other round cell tumors.33,85,86,106-110 Immunoreactivity has been demonstrated for canine IgG F(ab)2 and vimentin.82 A variant characterized by an IgG-reactive amyloid interspersed with the neoplastic cells has also been described.83 A panel of MAbs (recognizing tryptase, chymase, serotonin, CD1a, CD3, CD79a, CD18, MHC class II) in association with a histochemical stain (naphthol AS-D chloroacetate) has been advocated for use on formalin-fixed, paraffin-embedded sections of cutaneous round cell tumors to help classify poorly differentiated round cell tumors (mast cell tumors, histiocytomas, lymphomas, and plasmacytomas).109 Additionally, clonality of the immunoglobulin heavy chain variable region gene can be performed in plasmacytomas and myelomas using PCR technology, and this may have some diagnostic utility in difficult cases.
It is important to thoroughly stage dogs and cats with plasmacytomas that are at higher risk for systemic spread if contemplating local or locoregional therapy without systemic therapy. This should include bone marrow aspiration, serum electrophoresis, abdominal ultrasound, and skeletal survey radiographs to ensure the disease is confined to a local site prior to initiation of therapy. This is most important in cases of SOP and GI EMP due to their relatively high metastatic rate and less important for cutaneous, oral, and colorectal plasmacytomas because of their more typical benign behavior. For GI EMP (including colorectal EMP), endoscopic evaluation of the entire GI tract is recommended. A single case report of the use of PET/CT imaging for extramedullary splenic plasmacytoma in a dog exists; however, its utility remains unknown.111
Therapy for Solitary Plasmacytic Tumors
Cutaneous and oral plasma cell tumors in the dog are almost always benign and carry an excellent prognosis following conservative surgical excision.17,81-86,100,112 EMPs of the trachea, liver, and uterus have also been reported in dogs, and all had a benign course following local resection.92-94 Successful therapy with melphalan and prednisone has been rarely applied for a local recurrence or incomplete margins in dogs and cats. RT has been used infrequently for cases that are nonsurgical, including the application of strontium-90 plesiotherapy for lingual plasmacytoma in a dog.113 Surgery is recommended in combination with radiotherapy for those cases of SOP in which the lesion results in an unstable, long bone fracture (see Figure 32-22), or the patient is nonambulatory from neurologic compromise resulting from a vertebral body SOP. In the latter case, spinal cord decompression, mass excision, and possibly spinal stabilization may be necessary.63 Radiotherapy can be used alone (i.e., without surgery) in those cases where fractures are stable, as a palliative measure for bone pain, or in the case of vertebral SOP if the patient is ambulatory and stable. Good local control is usually achieved; however, most go on to develop systemic multiple myeloma.33,63,102 SOP of the axial skeleton can be managed by excision or radiotherapy alone. There is controversy as to whether systemic chemotherapy should be initiated at the time of local therapy for SOP when systemic involvement is not documented. Systemic spread may not occur for many months to even years beyond primary SOP diagnosis in humans and dogs, and studies in humans reveal no benefit derived from initiation of systemic chemotherapy prior to documentation of subsequent systemic spread.44,63 Two cases of SOP in cats were recently reported; one was treated with external-beam RT and one managed with melphalan chemotherapy and both enjoyed durable remissions of greater than 4 years.114 Similarly, EMP of the GI tract in humans are treated most commonly by surgical excision and thorough staging of disease. Systemic therapy is not initiated unless systemic involvement is documented. Systemic chemotherapy has been used following gastric EMP in a cat; however, the utility of adjuvant therapy in the species is unknown.115
Long-term follow-up of patients with SOP is indicated in order to recognize both recurrence of disease and systemic spread. Careful attention is given to serum globulin levels, bone pain, and radiographic appearance of bone healing in cases of SOP. Restaging of disease, including bone marrow evaluation, is indicated if systemic spread is suspected.
Prognosis for solitary plasma cell tumors is generally good. Cutaneous and mucocutaneous plasmacytomas are usually cured following surgical excision.17,86,112 In large compilations of cases in dogs, the local recurrence rate was approximately 5%, and nodal or distant metastasis occurred in only 7 of 349 cases (2%).17,80-82,86 New cutaneous plasmacytomas at sites distant from the primary developed in less than 2% of cases. Neither tumor cell proliferation rate (as measured by Ki67 immunohistochemistry) in the dog nor histopathologic grading in dogs and cats were prognostic in large compilations of cases, although it has been suggested that the polymorphous-blastic and plasmablastic type may act more aggressively in the dog and cat.17,24,86 The presence of amyloid and overexpression of cyclin D1 (prognostic in human plasmacytomas) were not shown to be of prognostic value in dogs.17 Dogs with EMP of the alimentary tract and other abdominal organs (e.g., liver, uterus) treated by surgical excision alone or in combination with systemic chemotherapy (if metastasis is present) can enjoy long-term survival in the majority of cases.* In a compilation of nine dogs with colorectal plasmacytoma, two dogs had local recurrence at 5 and 8 months following surgery, and the overall median survival was 15 months following surgery alone.100 DNA ploidy and c-myc oncoprotein expression in biopsy samples were determined to be prognostic for EMPs in dogs; however, those that were malignant were all from noncutaneous sites (i.e., lymph node, colon, spleen). Therefore location appears to be as predictive.116 As previously discussed, the majority of cases of SOP will eventually develop systemic disease; however, long disease-free periods usually precede the event.
The prognosis in cats is less well-defined because of the paucity of reported cases. If disease is confined to a local site and/or regional nodes, surgical excision and chemotherapy can result in long-term control; however, early, widespread metastasis and progression to MM is also reported in cats.†
References
1. Matus, RE, Leifer, CE, MacEwen, EG, et al. Prognostic factors for multiple myeloma in the dog. J Am Vet Med Assoc. 1986;188:1288–1291.
2. Liu, S-K, Dorfman, HD, Hurvitz, AI, et al. Primary and secondary bone tumors in the dog. J Small Anim Pract. 1977;18:313–326.
3. Weiss, DJ. A retrospective study of the incidence and the classification of bone marrow disorders in the dog at a veterinary teaching hospital (1996-2004). J Vet Intern Med. 2006;20:955–961.
4. Tappin, SW, Taylor, SS, Tasker, S, et al. Serum protein electrophoresis in 147 dogs. Vet Rec. 2011;168:456.
5. Osborne, CA, Perman, V, Sautter, JH, et al. Multiple myeloma in the dog. J Am Vet Med Assoc. 1968;153:1300–1319.
6. MacEwen, EG, Hurvitz, AI. Diagnosis and management of monoclonal gammopathies. Vet Clin North Am Small Anim Pract. 1977;7:119–132.
7. Engle, GC, Brodey, RS. A retrospective study of 395 feline neoplasms. J Am Anim Hosp Assoc. 1969;5:21–31.
8. Carpenter, JL, Andrews, LK, Holzworth, J. Tumors and tumor like lesions. In: Holzworth J, ed. Diseases of the cat: medicine and surgery. Philadelphia: WB Saunders, 1987.
9. Patel, RT, Caceres, A, French, AF, et al. Multiple myeloma in 16 cats: a retrospective study. Vet Clin Pathol. 2005;34:341–352.
10. Taylor, SS, Tappin, SW, Dodkin, SJ, et al. Serum protein electrophoresis in 155 cats. J Feline Med Surg. 2010;12:643–653.
11. Mellor, PJ, Haugland, S, Murphy, S, et al. Myeloma-related disorders in cats commonly present as extramedullary neoplasms in contrast to myeloma in human patients: 24 cases with clinical follow-up. J Vet Intern Med. 2006;20:1376–1383.
12. Hanna, F. Multiple myelomas in cats. J Feline Med Surg. 2005;7:275–287.
13. Potter, M. A resume of the current status of the development of plasma cell tumors in mice. Cancer Res. 1968;28:1891–1896.
14. Potter, M, Morrison, S, Weiner, F, et al. Induction of plasmacytomas with silicone gel in genetically susceptible strains of mice. J Natl Cancer Inst. 1994;86:1058–1065.
15. Imahori, S, Moore, GE. Multiple myeloma and prolonged stimulation of RES. N Y State J Med. 1972;72:1625–1628.
16. Porter, DD. The development of myeloma-like condition in mink with Aleutian disease. Blood. 1967;25:736–741.
17. Cangul, IT, Wunen, M, van Garderen, E, et al. Clinico-pathological aspects of canine cutaneous and mucocutaneous plasmacytomas. J Vet Med A Physiol Pathol Clin Med. 2002;49:307–312.
18. London, CA, Hannah, AL, Zadovoskaya, R, et al. Phase I dose-escalating study of SU11654, a small molecule receptor tyrosine kinase inhibitor, in dogs with spontaneous malignancies. Clin Cancer Res. 2003;9:2755–2768.
19. Bourget, CC, Grufferman, S, Delzell, E, et al. Multiple myeloma and family history of cancer. Cancer. 1985;56:2133–2139.
20. Cuzick, J, DeStavola, B. Multiple myeloma: A case control study. Br J Cancer. 1988;57:516–520.
21. Linet, MS, Sioban, DH, McLaughlin, JK. A case-control study of multiple myeloma in whites: chronic antigenic stimulation, occupation and drug use. Cancer Res. 1987;47:2978–2981.
22. Radhakrishnan, A, Risbon, RE, Patel, RT, et al. Progression of a solitary, malignant cutaneous plasma-cell tumour to multiple myeloma in a cat. Vet Comp Oncol. 2004;2:36–42.
23. Burnett, RC, Blake, MK, Thompson, LJ, et al. Evolution of a B-cell lymphoma to multiple myeloma after chemotherapy. J Vet Intern Med. 2004;18:768–771.
24. Mellor, PJ, Haugland, S, Smith, KC, et al. Histopathologic, immunohistochemical, and cytologic analysis of feline myeloma-related disorders: further evidence for primary extramedullary development in the cat. Vet Pathol. 2008;45:159–173.
25. Valli, VE, Jacobs, RM, Parodi, AL, et al. Histological classification of hematopoietic tumors of domestic animals. Washington, DC: Armed Forces Institute of Pathology and The World Health Organization; 2002.
26. Drazner, FH. Multiple myeloma in the cat. Comp Cont Ed Pract Vet. 1982;4:206–216.
27. Jacobs, RM, Couto, CG, Wellman, ML. Biclonal gammopathy in a dog with myeloma and cutaneous lymphoma. Vet Pathol. 1986;23:211–213.
28. Peterson, EN, Neininger, AC. Immunoglobulin A and immunoglobulin G biclonal gammopathy in a dog with multiple myeloma. J Am Anim Hosp Assoc. 1997;33:45–47.
29. Ramaiah, SK, Sequin, MA, Carwile, HF, et al. Biclonal gammopathy associated with immunoglobulin A in a dog with multiple myeloma. Vet Clin Pathol. 2002;31:83–89.
30. Giraudel, JM, Pages, JP, Guelfi, JF. Monoclonal gammopathies in the dog: A retrospective study of 18 cases (1986-1999) and literature review. J Am Anim Hosp Assoc. 2002;38:135–147.
31. Bienzle, D, Silverstein, DC, Chaffin, K. Multiple myeloma in cats: Variable presentation with different immunoglobulin isotypes in two cats. Vet Pathol. 2000;37:364–369.
32. Facchini, RV, Bertazzolo, W, Zuliani, D, et al. Detection of biclonal gammopathy by capillary zone electrophoresis in a cat and a dog with plasma cell neoplasia. Vet Clin Pathol. 2010;39:440–446.
33. MacEwen, EG, Patnaik, AK, Hurvitz, AI, et al. Nonsecretory multiple myeloma in two dogs. J Am Vet Med Assoc. 1984;184:1283–1286.
34. Seelig, DM, Perry, JA, Avery, AC, et al. Monoclonal gammopathy without hyperglobulinemia in 2 dogs with IgA secretory neoplasm. Vet Clin Pathol. 2010;39:447–453.
35. Braund, KG, Everett, RM, Bartels, JE, et al. Neurologic complications of IgA multiple myeloma associated with cryoglobulinemia in a dog. J Am Vet Med Assoc. 1979;174:1321–1325.
36. Hurvitz, AI, MacEwen, EG, Middaugh, CR, et al. Monoclonal cryoglobulinemia with macroglobulinemia in a dog. J Am Vet Med Assoc. 1977;170:511–516.
37. Hickford, FH, Stokol, T, vanGessel, YA, et al. Monoclonal immunoglobulin G cryoglobulinemia and multiple myeloma in a domestic shorthair cat. J Am Vet Med Assoc. 2000;217:1029–1033.
38. Cowgill, ES, Meel, JA, Ruslander, D. Light-chain myeloma in a dog. J Vet Intern Med. 2004;18:119–121.
39. Yamada, O, Tamura, K, Yagihara, H, et al. Light-chain multiple myeloma in a cat. J Vet Diagn Invest. 2007;19:443–447.
40. Gentilini, F, Calzolari, C, Buonacucina, A, et al. Different biological behaviour of Waldenstrom macroglobulinemia in two dogs. Vet Comp Oncol. 2005;3:87–97.
41. Hill, RR, Clatworthy, RH. Macroglobulinemia in the dog, the canine analogue of gamma M monoclonal gammopathy. J S Afr Vet Med Assoc. 1971;42:309–313.
42. Hurvitz, AI, Haskins, SC, Fischer, CA. Macroglobulinemia with hyperviscosity syndrome in a dog. J Am Vet Med Assoc. 1970;157:455–460.
43. Anderson, K. Plasma cell tumors. In Holland JF, Frei E, Bast RC, et al, eds.: Cancer medicine, ed 3, Philadelphia: Lea & Febiger, 1993.
44. Salmon, SE, Cassady, JR. Plasma cell neoplasms. In DeVita VT, Hellman S, Rosenberg SA, eds.: Cancer: principles and practice of oncology, ed 5, Philadelphia: JB Lippincott, 1997.
45. Shull, RM, Osborne, CA, Barrett, RE, et al. Serum hyperviscosity syndrome associated with IgA multiple myeloma in two dogs. J Am Anim Hosp Assoc. 1978;14:58–70.
46. Center, SA, Smith, JF. Ocular lesions in a dog with hyperviscosity secondary to an IgA myeloma. J Am Vet Med Assoc. 1982;181:811–813.
47. Kirschner, SE, Niyo, Y, Hill, BL, et al. Blindness in a dog with IgA-forming myeloma. J Am Vet Med Assoc. 1988;193:349–350.
48. Hendrix, DV, Gelatt, KN, Smith, PJ, et al. Ophthalmic disease as the presenting complaint in five dogs with multiple myeloma. J Am Anim Hosp Assoc. 1998;34:121–128.
49. Hawkins, EC, Feldman, BF, Blanchard, PC. Immunoglobulin A myeloma in a cat with pleural effusion and serum hyperviscosity. J Am Vet Med Assoc. 1986;188:876–878.
50. Williams, DA, Goldschmidt, MH. Hyperviscosity syndrome with IgM monoclonal gammopathy and hepatic plasmacytoid lymphosarcoma in a cat. J Small Anim Pract. 1982;23:311–323.
51. Forrester, SD, Greco, DS, Relford, RL. Serum hyperviscosity syndrome associated with multiple myeloma in two cats. J Am Vet Med Assoc. 1992;200:79–82.
52. Hribernik, TN, Barta, O, Gaunt, SD, et al. Serum hyperviscosity syndrome associated with IgG myeloma in a cat. J Am Vet Med Assoc. 1982;181:169–170.
53. Boyle, TE, Holowaychuk, MK, Adams, AK, et al. Treatment of three cats with hyperviscosity syndrome and congestive heart failure using plasmapheresis. J Am Anim Hosp Assoc. 2011;47:50–55.
54. Mundy, GR, Bertolini, DR. Bone destruction and hypercalcemia in plasma cell myeloma. Semin Oncol. 1986;13:291–297.
55. Rosol, TJ, Nagode, LA, Couto, CG, et al. Parathyroid hormone (PTH)-related protein, PTH, and 1,25-dihydroxyvitamin D in dogs with cancer associated hypercalcemia. Endocrinology. 1992;131:1157–1164.
56. Sheafor, SE, Gamblin, RM, Couto, CG. Hypercalcemia in two cats with multiple myeloma. J Am Animal Hosp Assoc. 1996;32:503–508.
57. Twomey, JJ. Infections complicating multiple myeloma and chronic lymphocytic leukemia. Arch Intern Med. 1973;132:562–565.
58. Webb, J, Chary, P, Northrup, N, et al. Erythrophagocytic multiple myeloma in a cat. Vet Clin Pathol. 2008;37:302–307.
59. Yearly, JH, Stanton, C, Olivry, T, et al. Phagocytic plasmacytoma in a dog. Vet Clin Pathol. 2007;36:293–296.
60. Hoenig, M, O’Brien, JA. A benign hypergammaglobulinemia mimicking plasma cell myeloma. J Am Anim Hosp Assoc. 1988;24:688–690.
61. Dewhirst, MW, Stamp, GL, Hurvitz, AI. Idiopathic monoclonal (IgA) gammopathy in a dog. J Am Vet Med Assoc. 1977;170:1313–1316.
62. Van Bree, H, Pollet, L, Cousemont, W, et al. Cervical cord compression as a neurologic complication in an IgG multiple myeloma in a dog. J Am Anim Hosp Assoc. 1983;19:317–323.
63. Rusbridge, C, Wheeler, SJ, Lamb, CR, et al. Vertebral plasma cell tumors in 8 dogs. J Vet Intern Med. 1999;13:126–133.
64. DiBartola, SP. Hypoglycemia and polyclonal gammopathy in a dog with plasma cell dyscrasia. J Am Vet Med Assoc. 1982;180:1345–1348.
65. Villiers, E, Dobson, J. Multiple myeloma with associated polyneuropathy in a German shepherd dog. J Small Anim Pract. 1998;39:249–251.
66. Mitcham, SA, McGillivray, SR, Haines, DM. Plasma cell sarcoma in a cat. Can Vet J. 1985;26:98–100.
67. O’Keefe, DA, Couto, CG. Fine-needle aspiration of the spleen as an aid in the diagnosis of splenomegaly. J Vet Intern Med. 1987;1:102–109.
68. Werner, JA, Woo, JC, Vernau, W, et al. Characterization of feline immunoglobulin heavy chain variable region genes for the molecular diagnosis of B-cell neoplasia. Vet Pathol. 2005;42:596–607.
69. Munshi, NC, Anderson, KC. Plasma cell neoplasms. In DeVita VT, Hellman S, Rosneberg SA, eds.: Cancer principles & practice of oncology, ed 7, Philadelphia: Lippincott Williams & Wilkins, 2005.
70. Matus, RE, Leifer, CE, Jurvitz, AI. Use of plasmapheresis and chemotherapy for treatment of monoclonal gammopathy associated with Ehrlichia canis infection in a dog. J Am Vet Med Assoc. 1987;190:1302–1304.
71. Breitschwerdt, EB, Woody, BJ, Zerbe, CA, et al. Monoclonal gammopathy associated with naturally occurring canine ehrlichiosis. J Vet Intern Med. 1987;1:2–9.
72. MacEwen, EG, Hurvitz, AI, Hayes, A. Hyperviscosity syndrome associated with lymphocytic leukemia in three dogs. J Am Vet Med Assoc. 1977;170:1309–1312.
73. Font, A, Closa, JM, Mascort, J. Monoclonal gammopathy in a dog with visceral leishmaniasis. J Vet Intern Med. 1994;8:233–235.
74. Fan, TM, Kitchell, BE, Dhaliwal, RS, et al. Hematological toxicity and therapeutic efficacy of lomustine in 20 tumor-bearing cats: critical assessment of a practical dosing regimen. J Am Anim Hosp Assoc. 2002;38:357–363.
75. Ferhangi, M, Osserman, EF. The treatment of multiple myeloma. Sem Hematol. 1973;10:149–161.
76. Bartges, JW. Therapeutic plasmapheresis. Sem Vet Med Surg. 1997;12:170–177.
77. Farrow, BRH, Penny, R. Multiple myeloma in a cat. J Am Vet Med Assoc. 1971;158:606–611.
78. Milner, RJ, Farese, J, Henry, CJ, et al. Bisphosphonates and cancer. J Vet Intern Med. 2004;18:597–604.
79. Kisseberth, WC, MacEwen, EG, et al. Response to liposome-encapsulated doxorubicin (TLC D-99) in a dog with myeloma. J Am Vet Med Assoc. 1995;9:425–428.
80. Clark, GN, Berg, J, Engler, SJ, et al. Extramedullary plasmacytomas in dogs: results of surgical excision in 131 cases. J Am Anim Hosp Assoc. 1992;28:105–111.
81. Rakich, PM, Latimer, KS, Weiss, R, et al. Mucocutaneous plasmacytomas in dogs: 75 cases (1980-1987). J Am Vet Med Assoc. 1989;194:803–810.
82. Baer, KE, Patnaik, AK, Gilbertson, SR, et al. Cutaneous plasmacytomas in dogs: A morphologic and immunohistochemical study. Vet Pathol. 1989;26:216–221.
83. Rowland, PH, Valentine, BA, Stebbins, KE, et al. Cutaneous plasmacytomas with amyloid in six dogs. Vet Pathol. 1991;28:125–130.
84. Lucke, VM. Primary cutaneous plasmacytomas in the dog and cat. J Small Anim Pract. 1987;28:49–55.
85. Kyriazidou, A, Brown, PJ, Lucke, VM. An immunohistochemical study of canine extramedullary plasma cell tumours. J Comp Pathol. 1989;100:259–266.
86. Platz, SJ, Breuer, W, Pfleghaar, S, et al. Prognostic value of histopathological grading in canine extramedullary plasmacytomas. Vet Pathol. 1999;36:23–27.
87. Witham, A, French, A, Hill, K. Extramedullary laryngeal plasmacytoma in a dog. N Z Vet J. 2012;60:61–64.
88. Hayes, AM, Gregory, SP, Murphy, S, et al. Solitary extramedullary plasmacytoma of the canine larynx. J Small Anim Pract. 2007;48:288–291.
89. Perlmann, E, Dagli, ML, Martins, MC, et al. Extramedullary plasmacytoma of the third eyelid gland in a dog. Vet Ophthalmol. 2009;12:102–105.
90. Schoniger, S, Bridger, N, Allenspach, K, et al. Sinonasal plasmacytoma in a cat. J Vet Diagn Invest. 2007;19:573–577.
91. Van Wettere, AJ, Linder, KE, Suter, SE, et al. Solitary intracerebral plasmacytoma in a dog: microscopic, immunohistochemical, and molecular features. Vet Pathol. 2009;46:949–951.
92. Chaffin, K, Cross, AR, Allen, SW, et al. Extramedullary plasmacytoma in the trachea of a dog. J Am Vet Med Assoc. 1998;212:1579–1581.
93. Choi, YK, Lee, JY, Park, JI, et al. Uterine extramedullary plasmacytoma in a dog. Vet Rec. 2004;154:699–700.
94. Aoki, M, Kim, T, Shimada, T, et al. A primary hepatic plasma cell tumor in a dog. J Vet Med Sci. 2004;66:445–447.
95. Fukumoto, S, Hanazono, K, Kawasaki, N, et al. Anaplastic atypical myeloma with extensive cutaneous involvement in a dog. J Vet Med Sci. 2011. [Epub ahead of print].
96. Mayer, MN, Kerr, ME, Grier, CK, et al. Immunoglobulin A multiple myeloma with cutaneous involvement in a dog. Can Vet J. 2008;49:694–702.
97. Hamilton, TA, Carpenter, JL. Esophageal plasmacytoma in a dog. J Am Vet Med Assoc. 1994;204:1210–1211.
98. MacEwen, EG, Patnaik, AK, Johnson, GF, et al. Extramedullary plasmacytoma of the gastrointestinal tract in two dogs. J Am Vet Med Assoc. 1984;184:1396–1398.
99. Jackson, MW, Helfand, SC, Smedes, SL, et al. Primary IgG secreting plasma cell tumor in the gastrointestinal tract of a dog. J Am Vet Med Assoc. 1994;204:404–406.
100. Kupanoff, PA, Popovitch, CA, Goldschmidt, MH. Colorectal plasmacytomas: A retrospective study of nine dogs. J Am Anim Hosp Assoc. 2006;42:37–43.
101. Trevor, PB, Saunders, GK, Waldron, DR, et al. Metastatic extramedullary plasmacytoma of the colon and rectum in a dog. J Am Vet Med Assoc. 1993;203:406–409.
102. Meis, JM, Butler, JJ, Osborne, BM, et al. Solitary plasmacytomas of bone and extramedullary plasmacytomas. Cancer. 1987;59:1475–1485.
103. Majzoub, M, Breuer, W, Platz, SJ, et al. Histopathologic and immunophenotypic characterization of extramedullary plasmacytomas in nine cats. Vet Pathol. 2003;40:249–253.
104. Michau, TM, Proulx, DR, Rushton, SD, et al. Intraocular extramedullary plasmacytoma in a cat. Vet Ophthalmol. 2003;6:177–181.
105. Carothers, MA, Johnson, GC, DiBartola, SP, et al. Extramedullary plasmacytoma and immunoglobulin-associated amyloidosis in a cat. J Am Vet Med Assoc. 1989;195:1593–1597.
106. Kryriazidou, A, Brown, PJ, Lucke, VM. Immunohistochemical staining of neoplastic and inflammatory plasma cell lesions in feline tissues. J Comp Pathol. 1989;100:337–341.
107. Breuer, W, Colbatzky, F, Platz, S, et al. Immunoglobulin-producing tumours in dogs and cats. J Comp Pathol. 1993;109:203–216.
108. Brunnert, SR, Altman, NH. Identification of immunoglobulin light chains in canine extramedullary plasmacytomas by thioflavine T and immunohistochemistry. J Vet Diagn Invest. 1991;3:245–251.
109. Fernandez, NJ, West, KH, Jackson, ML, et al. Immunohistochemical and histochemical stains for differentiating canine cutaneous round cell tumors. Vet Pathol. 2005;42:437–445.
110. Ramos-Vara, JA, Miller, MA, Valli, VE. Immunohistochemical detection of multiple myeloma 1/interferon regulatory factor 4 (MUM1/IRF-4) in canine plasmacytoma: comparison with CD79a and CD20. Vet Pathol. 2007;44:875–884.
111. Lee, AR, Lee, MS, Jung, IS, et al. Imaging diagnosis—FDG-PET/CT of a canine splenic plasma cell tumor. Vet Radiol Ultrasound. 2010;51:145–147.
112. Wright, ZM, Rogers, KS, Mansell, J. Survival data for canine oral extramedullary plasmacytoma: a retrospective analysis (1996-2006). J Am Anim Hosp Assoc. 2008;44:75–81.
113. Ware, K, Gieger, T. Use of strontium-90 plesiotherapy for the treatment of a lingual plasmacytoma in a dog. J Small Anim Pract. 2011;52:220–223.
114. Mellor, PJ, Polton, GA, Brearley, M, et al. Solitary plasmacytoma of bone in two successfully treated cats. J Feline Med Surg. 2007;9:72–77.
115. Zikes, C, Spielman, B, Shapiro, W, et al. Gastric extramedullary plasmacytoma in a cat. J Vet Intern Med. 1998;12:381–383.
116. Frazier, KS, Hines, ME, Hurvitz, AI, et al. Analysis of DNA aneuploidy and c-myc oncoprotein content of canine plasma cell tumors using flow cytometry. Vet Pathol. 1993;30:505–511.
*References 53, 177, 180, 182-186, 188, 190, 195-198.
*References 53, 86, 88, 91, 166, 188, 190, 209, 211-213.
*References 53, 82-84, 89, 91, 97, 107, 142, 156a, 156b, 170, 175, 181, 204, 207-209, 217-219, 225, 278-285.
†References 91, 119, 120, 209, 220, 221, 286-290.
‡References 53, 54, 86, 88, 91, 209, 279.
*References 16, 137, 150, 280, 292-294.
*Note that either CD21 or CD79 can be used for assessing B-cell lineage in this context.
*References 5-9, 23-34, 37-46.
*References 9, 12, 29, 39, 118, 119.
*References 1, 6, 40, 42, 45-48.
*References 1, 6, 9, 11, 12, 26.
†References 1, 6, 11, 45, 46-48.
*References 5, 9, 60, 61, 70-73.
*References 6, 9, 11, 12, 31, 26.
*References 6, 45, 53, 72, 76, 77.
*References 9, 11, 12, 26, 31, 56.