Screening for Hepatic and Biliary Disease
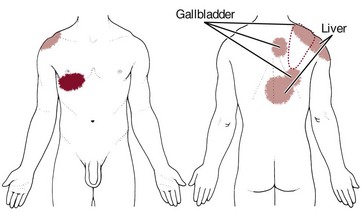
As with many of the organ systems in the human body, the hepatic and biliary organs (liver, gallbladder, and common bile duct) can develop diseases that mimic primary musculoskeletal lesions (Fig. 9-1). The musculoskeletal symptoms associated with hepatic and biliary pathologic conditions are generally confined to the mid-back, scapular, and right shoulder regions. These musculoskeletal symptoms can occur alone (as the only presenting symptom) or in combination with other systemic signs and symptoms discussed in this chapter.
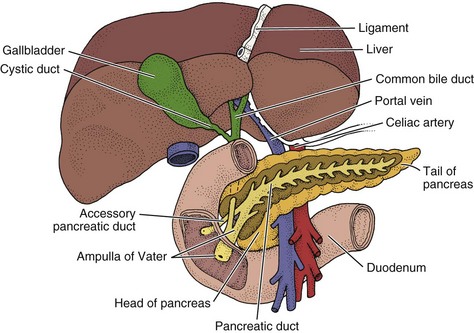
Fig. 9-1 Anatomy of the liver, gallbladder, common bile duct, and pancreas. The pear-shaped gallbladder is tucked up under the right side of the liver. The pancreas is located behind the stomach anterior to the L1 to L3 vertebral bodies. It is about 6 inches long, wide at one end (the head), then tapered through the body to the narrow end called the tail.
Hepatic and Biliary Signs and Symptoms
The major causes of acute hepatocellular injury include hepatitis, drug-induced hepatitis, and ingestion of hepatotoxins. The physical therapist is most likely to encounter liver or gallbladder diseases manifested by a variety of signs and symptoms outlined in this section.
Taking a careful history and making close observations of the client’s physical condition and appearance can detect telltale signs of hepatic disease. Most of the liver is contained underneath the rib cage and is largely inaccessible (Fig. 9-2). An enlarged liver that is palpable is always a red flag (see Fig. 4-51). Medical diagnosis of liver or gallbladder disease is made by x-ray examination or ultrasonic scanning of the gallbladder and computed tomography (CT) scanning of the abdomen, including the liver.
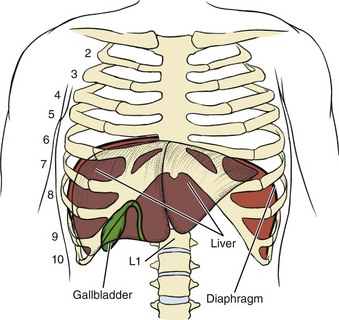
Fig. 9-2 Location of the liver and gallbladder. The liver is located just below the respiratory diaphragm, predominately on the right side, but with a portion crossing the midline to the left side. It is a large organ and spans many vertebral levels. The most superior part is the dome of the right lobe. The “peak” of the dome lies at about T8 or T9 during expiration. The inferior border of the left lobe is located just below the level of the left nipple and inclines downwards to the right at the tip of the 8th costal margin. The right lobe angles downward to the 9th and 10th costal margins. Posteriorly, the liver is located from approximately T9 to L1 at the midline. This varies from person to person and with inhalation (moves up a level or two) and exhalation (moves down). The fundus (base) of the gallbladder usually appears below the edge of the liver in contact with the anterior abdominal wall at the tip of the 9th right costal cartilage.
Other tests, such as a cholescintigraphy, may be used to track the flow of radioactivity into and out of the gallbladder to confirm gallstones. Blood tests may be used to look for signs of infection, obstruction, or jaundice. Laboratory tests useful in the diagnosis and treatment of liver and biliary tract disease are listed inside the back cover.
Skin and Nail Bed Changes
Skin changes associated with impairment of the hepatic system include jaundice, pallor, and orange or green skin in a Caucasian individual. Change in skin tones may be visible in Black or Asian people, but these may only be observable to the affected individual or to those who know him or her well. In some situations jaundice may be the first and only manifestation of disease. It is first noticeable in people of all skin colors in the sclera of the eye as a yellow hue when bilirubin reaches levels of 2 to 3 mg/dL. When the bilirubin level reaches 5 to 6 mg/dL, changes in skin color occur.
Other skin changes may include pruritus (itching), bruising, spider angiomas (Fig. 9-3), and palmar erythema (see Fig. 9-5). Spider angiomas (arterial spider, spider telangiectasis, vascular spider), branched dilations of the superficial capillaries resembling a spider in appearance (Fig. 9-4), may be vascular manifestations of increased estrogen levels (hyperestrogenism). Spider angiomas and palmar erythema both occur in the presence of liver impairment as a result of increased estrogen levels normally detoxified by the liver.

Fig. 9-3 Spider Angioma. Permanently enlarged and dilated capillaries visible on the surface of the skin caused by vascular dilation are called spider angiomas. These capillary radiations can be flat or raised in the center. They present on the upper half of the body, primarily on the face, neck, chest, or abdomen and occur as a normal development or in association with pregnancy, chronic liver disease, or estrogen therapy. They do not go away when the underlying condition is treated; laser therapy is available to remove them for cosmetic reasons. (From Swartz, MH: Textbook of physical diagnosis: history and examination, ed 6, Philadelphia, 2009, Saunders.)
Fig. 9-4 Arterial spider. Schematic diagram of an arterial spider formed by a coiled arteriole that spirals up to a central point and then branches out into thin-walled vessels that merge with normal capillaries resembling a spider in appearance. Exposure to heat (e.g., hot tubs, warm shower) will cause temporary vasodilation. The skin lesion will appear larger until vasoconstriction occurs.
Palmar erythema (warm redness of the skin over the palms, also called liver palms), caused by an extensive collection of arteriovenous anastomoses, is especially evident on the hypothenar and thenar eminences and pulps of the finger (Fig. 9-5). The person may complain of throbbing, tingling palms. The soles of the feet may be similarly affected. Throbbing and tingling may be associated with these anastomoses.

Fig. 9-5 Palmar erythema caused by liver impairment presents as a warm redness of the skin over the palms and soles of the feet in the Caucasian population. Darker skin tones may change from a tan color to a gray appearance. Look for other signs of liver disease such as nail bed changes, spider angiomas, liver flap, and bilateral carpal or tarsal tunnel syndrome. Palmar erythema can occur in healthy individuals and in association with nonhepatic diseases. (From Barrison I, ed: Gastroenterology in practice, St. Louis, 1992, Mosby.)
Various forms of nail disease have been described in cases of liver impairment such as the white nails of Terry (Fig. 9-6). Other nail bed changes, such as white bands across the nail plate (leukonychia), clubbed nails (see Fig. 4-36), or koilonychia (see Fig. 4-32), can occur, but these are not specific to liver impairment and can develop in the presence of other diseases as well.

Fig. 9-6 Nails of Terry. Opaque white nails of Terry in a patient with cirrhosis. Various forms of nail disease have been described in patients with cirrhosis. This is an example of the classic white nails of Terry characterized by an opaque nail plate with a narrow line of pink at the distal end instead of the more normal pink nail plate in the Caucasian. Nails of Terry can also present as a result of malnutrition, diabetes mellitus, hyperthyroidism, trauma, and sometimes for unknown reasons (idiopathic). (From Callen JP, Jorizzo JL, editors: Dermatological signs of internal disease, ed 4, Philadelphia, 2009, WB Saunders.)
Musculoskeletal Pain
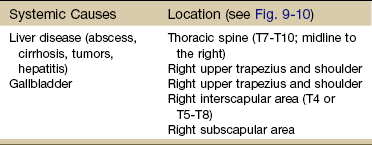
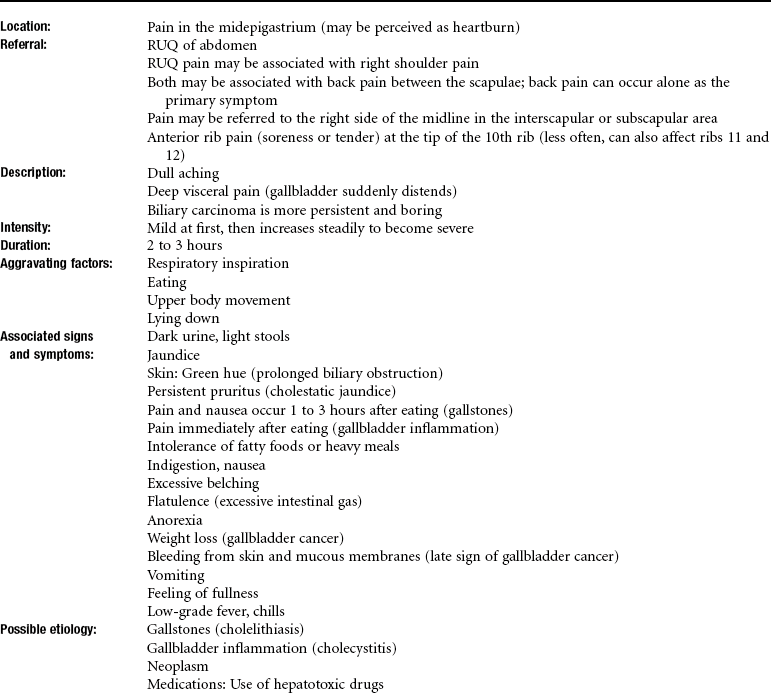
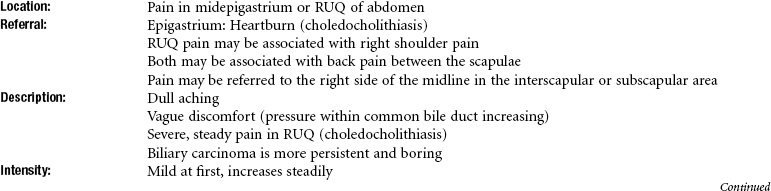
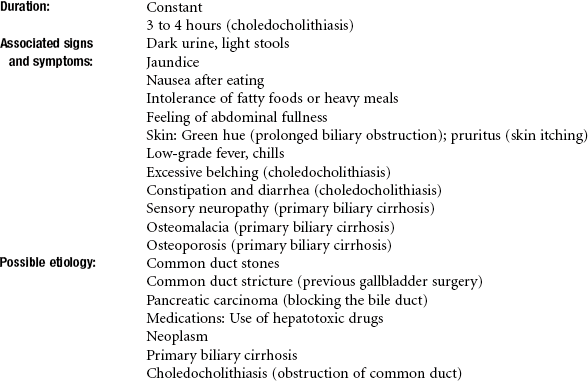
Musculoskeletal pain associated with the hepatic and biliary systems includes thoracic pain between the scapulae, right shoulder, right upper trapezius, right interscapular, or right subscapular areas (see Fig. 9-10 and Table 9-1).
Referred shoulder pain may be the only presenting symptom of hepatic or biliary disease. Afferent pain signals from the superior ligaments of the liver and the superior portion of the liver capsule are transmitted by the phrenic nerves. Sympathetic fibers from the biliary system are connected through the celiac (abdominal) and splanchnic (visceral) plexuses to the hepatic fibers in the region of the dorsal spine (see Fig. 3-3).
The celiac and splanchnic connections account for the intercostal and radiating interscapular pain that accompanies gallbladder disease. Although the innervation is bilateral, most of the biliary fibers reach the cord through the right splanchnic nerves, synapsing with adjacent phrenic nerve fibers innervating the diaphragm and producing pain in the right shoulder (see Fig. 3-4).
Hepatic osteodystrophy, abnormal development of bone, can occur in all forms of cholestasis (bile flow suppression) and hepatocellular disease, especially in the alcoholic person. Either osteomalacia or more often, osteoporosis frequently accompanies bone pain from this condition. Vertebral wedging, vertebral crush fractures, and kyphosis can be severe; decalcification of the ribcage and pseudofractures1 occur frequently.
Pseudofractures, or Looser’s zones, are narrow lines of radiolucency (areas of darkness on x-ray film), usually oriented perpendicular to the bone surface. This may represent a stress fracture that is repaired by laying down inadequately mineralized osteoid, or these sites may occur as a result of mechanical erosion caused by arterial pulsations, since arteries frequently overlie sites of pseudofractures.
Osteoporosis associated with primary biliary cirrhosis and primary sclerosing cholangitis parallels the severity of liver disease rather than its duration. Painful osteoarthropathy may develop in the wrists and ankles as a nonspecific complication of chronic liver disease. Rhabdomyolysis is a potentially fatal condition is which myoglobin and other muscle tissue contents are released into the bloodstream as a result of muscle tissue disintegration. This could occur with acute trauma (e.g., crush injuries, significant blunt trauma, high-voltage electrical burns, surgery2), severe burns, overexertion,3 or in the case of liver impairment, from alcohol abuse or alcohol poisoning or the use of cholesterol-lowering drugs called statins (e.g., Zocor, Lipitor, Crestor, Mevacor, Pravachol).4
Rhabdomyolysis is characterized by muscle aches, cramps, soreness, and weakness. It may be accompanied by other symptoms of respiratory muscle myopathy (impaired diaphragmatic function)5 or liver or renal involvement. Laboratory testing will show a creatine kinase (CK) level more than 10 times the upper limit of normal.
Although the literature reports the incidence of this severe myopathy with statin use as about 0.1% to 2.0% in clinical trials,6 therapists (and others) report seeing cases more often than the low percentage would suggest. Any anatomic region can be affected, but the back and extremity musculoskeletal pain are the two areas of involvement reported most often.7,8
Statin-associated myopathy appears to occur more often in people with complex medical problems and/or those taking illegal drugs (e.g., cocaine, heroin, LSD) or abusing prescription drugs (e.g., barbiturates and amphetamines).9 Other risk factors that increase the chances of this condition include excessive alcohol use, advancing age (over 80 years), recent history of surgery, and small physical stature.4 For additional discussion, see Screening for Side Effects of Statins in Chapter 6.
Neurologic Symptoms
Neurologic symptoms, such as confusion, sleep disturbances, muscle tremors, hyperreactive reflexes, and asterixis, may occur. When liver dysfunction results in increased serum ammonia and urea levels, peripheral nerve function can be impaired.
Ammonia from the intestine (produced by protein breakdown) is normally transformed by the liver to urea, glutamine, and asparagine, which are then excreted by the renal system. When the liver does not detoxify ammonia, ammonia is transported to the brain, where it reacts with glutamate (excitatory neurotransmitter), producing glutamine.
The reduction of brain glutamate impairs neurotransmission, leading to altered central nervous system (CNS) metabolism and function. Symptoms of poor concentration, fatigue, and other symptoms of encephalopathy can result.
Another outward sign of liver disease producing CNS dysfunction is asterixis. Impaired inflow of joint and other afferent information to the brainstem reticular formation produces this movement dysfunction. Also called flapping tremors or liver flap, asterixis is described as the inability to maintain wrist extension with forward flexion of the upper extremities. It is tested by asking the client to actively hyperextend the wrist and hand with the rest of the arm supported on a firm surface or with the arms held out in front of the body (Fig. 9-7).10 The test is positive if quick, irregular extensions and flexions of the wrist and fingers occur. Asterixis may also be observed when releasing the pressure in the arm cuff during blood pressure readings.
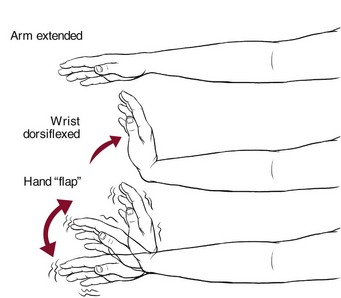
Fig. 9-7 To test for asterixis or liver flap, have the client extend the arms, spread the fingers, extend the wrist, and observe for the abnormal “flapping” tremor at the wrist. If a tremor is not readily apparent, ask the client to keep the arms straight while gently hyperextending the client’s wrist. There is an alternate method of testing for this phenomenon: have the client relax the legs in the supine position with the knees bent. The feet are flat on the table. As the legs fall to the sides, watch for a flapping or tremoring of the legs at the hip. The knees appear to come back toward the midline repeatedly.10
Asterixis and numbness/tingling (the latter are misinterpreted as carpal tunnel syndrome) can occur as a result of this ammonia abnormality, causing an intrinsic nerve pathologic condition (Case Example 9-1). There are many potential causes of carpal tunnel syndrome, both musculoskeletal and systemic (see Table 11-2). Careful evaluation is required (Box 9-1).
A careful history and close observation of the client are important in determining whether a person may need a medical referral for possible liver disease. Jaundice in the postoperative client is not uncommon, but it can be a potentially serious complication of liver damage that occurs following surgery and anesthesia. Clues to screening for hepatic disease (see Clues to Screening for Hepatic Disease at the end of this chapter) should be taken into consideration when evaluating the clinical history and observations.
Gastrointestinal System
Normally, bilirubin, excreted in bile and carried to the small intestines, is reduced to a form that causes the stool to assume a brown color. Light-colored (almost white) stools and urine the color of tea or cola indicate an inability of the liver or biliary system to excrete bilirubin properly. Gallbladder disease, hepatotoxic medications, or pancreatic cancer blocking the bile duct may cause light stools.
Hepatic and Biliary Pathophysiology
Hepatitis
Hepatitis is an acute or chronic inflammation of the liver. It can be caused by a virus, a chemical, a drug reaction, or alcohol abuse. In addition, hepatitis can be secondary to disease conditions, such as an infection with other viruses (e.g., Epstein-Barr virus or cytomegalovirus).
Viral Hepatitis: Viral hepatitis is an acute infectious inflammation of the liver caused by one of the following identified viruses: A, B, C, D, E, and G (Table 9-2).
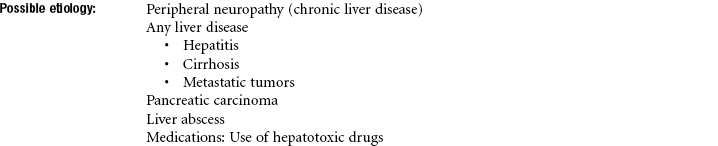
TABLE 9-2
Comparison of Major Types of Viral Hepatitis
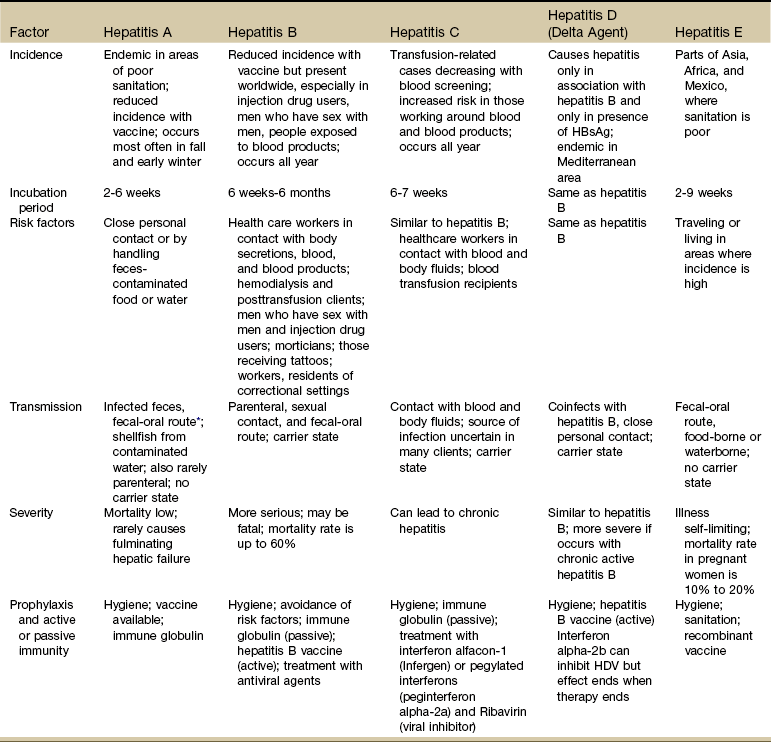
HBsAg, Hepatitis B surface antigen; HDV, hepatitis D virus.
*The oral-fecal route of transmission is primarily from poor or improper handwashing and personal hygiene, particularly after using the bathroom and then handling food for public consumption. This route of transmission may also occur through shared use of razors and oral utensils such as straws, silverware, and toothbrushes.
From Centers for Disease Control and Prevention (CDC): Division of Viral Hepatitis. Viral Hepatitis for Health Professionals. Available online at www.cdc.gov/hepatitis. Accessed Oct. 18, 2010.
Hepatitis is a major uncontrolled public health problem for several reasons: not all the causative agents have been identified, there are limited specific drugs for its treatment, its incidence has increased in relation to illicit drug use, and it can be communicated before the appearance of observable clinical symptoms.
Viral hepatitis is spread easily to others and usually results in an extended period of convalescence with loss of time from school or work. It is estimated that 60% to 90% of viral hepatitis cases are unreported because many cases are subclinical or involve mild symptoms.11,12
Hepatitis A and E are transmitted primarily by the fecal-oral route. Common source outbreaks result from contaminated food or water. Hepatitis A virus (HAV) must also be considered a potential problem in situations where fecal-oral communication along with food handling and/or unsanitary conditions occur. Some examples of potential sources of contact with HAV might include restaurants, day care centers, correctional institutions, sewage plants, and countries where these viruses are endemic.13,14
Hepatitis viruses B, C, D, and G are primarily bloodborne pathogens that can be transmitted from percutaneous or mucosal exposures to blood or other body fluids from an infected person.
Hepatitis B virus (HBV) is usually transmitted by inoculation of infected blood or blood products or by sexual contact and is also found in body fluids (e.g., spinal, peritoneal, pleural), saliva, semen, and vaginal secretions. Hepatitis D virus (HDV) must have HBV present to coinfect. Groups at risk include homosexuals and intravenous (IV) drug users; health care workers in any area in which contact with blood, blood products, or body fluids is likely; and residents and workers in correctional settings.14,15
Hepatitis C virus (HCV) is transmitted similarly to HBV and HDV. Risk factors are also very similar with the addition of people who have received blood transfusions or organ transplants, including anterior cruciate ligament (ACL) reconstruction allograft.16,17 There has been growing concern worldwide about the risk of occupational transmission of HCV.
Occupational exposure to HCV accounts for approximately 4% of new infections. On average, the chance of acquiring HCV after a needle-stick injury involving an infected patient is 1.8% (range, 0% to 7%). Reports of HCV transmission from health care workers to patients are extremely uncommon.14
Hepatitis G virus (HGV) designation has been applied to a virus that is percutaneously transmitted and associated with bloodborne viral presence lasting approximately 10 years. HGV has been detected primarily in IV drug users, clients on hemodialysis, clients with hemophilia, and in a small percentage of blood donors. It does not appear to cause important liver disease or affect the response rate of those with chronic HBV or HCV to antiviral therapy.18
Hepatitis affects people in three stages: the initial or preicteric stage, the icteric or jaundiced stage, and the recovery period (Table 9-3). During the initial or preicteric stage, which lasts for 1 to 3 weeks, the person experiences vague gastrointestinal (GI) and general body symptoms. Fatigue, malaise, lassitude, weight loss, and anorexia are common.
TABLE 9-3
Four Phases or Stages of Hepatitis
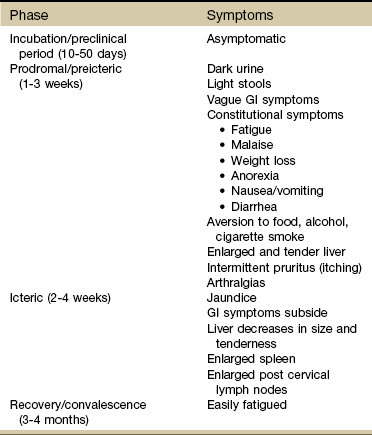
Source: World Health Organization. Global alert and response to hepatitis. Available online at www.who.int. Accessed February 1, 2011.
Modified from Goodman CC, Fuller KS: Pathology: implications for the physical therapist, ed 3, Philadelphia, 2009, WB Saunders.
Many people develop an aversion to food, alcohol, and cigarette smoke. Nausea, vomiting, diarrhea, arthralgias, and influenza-like symptoms may occur. There is a strong association between hepatitis-induced arthralgia and age with increasing incidence of joint involvement with increased age; arthralgia in children is much less common.19,20 The liver becomes enlarged and tender (see Fig. 4-51), and intermittent itching (pruritus) may develop. From 1 to 14 days before the icteric stage, the urine darkens and the stool lightens as less bilirubin is conjugated and excreted.
The icteric (acute) stage is characterized by the appearance of jaundice, which peaks in 1 to 2 weeks and can persist for 6 to 8 weeks. During this stage, the acuteness of the inflammation subsides. The GI symptoms begin to disappear, and after 1 to 2 weeks of jaundice the liver decreases in size and becomes less tender. During the icteric stage the post-cervical lymph nodes and spleen are enlarged (see Fig. 4-53). Persons who have been treated with human immune serum globulin (ISG) may not develop jaundice.
The recovery stage lasts for 3 to 4 months, during which time the person generally feels well but fatigues easily.
People with mild-to-moderate acute hepatitis rarely require hospitalization. The emphasis is on preventing the spread of infectious agents and avoiding further liver damage when the underlying cause is drug-induced or toxic hepatitis. People with fulminant (sudden and severe or prolonged) hepatitis require special management because of the rapid progression of their disease and the potential need for urgent liver transplantation.
An entire spectrum of rheumatic diseases can occur concomitantly with HBV and HBC, including transient arthralgias, vasculitis, polyarteritis nodosa, rheumatoid arthritis (RA), fibromyalgia, lymphoma, Sjögren’s syndrome, and persistent synovitis. Some conditions, such as RA and fibromyalgia, occur only in association with HCV, whereas others, such as polyarteritis nodosa, are observed in association with both forms of hepatitis.20-22
Rheumatic manifestations of hepatitis are varied early in the course of disease and can be indistinguishable from mild RA. The therapist should be suspicious of anyone with risk factors for hepatitis, including injection drug use; previous blood transfusion, especially before 1991; hemodialysis; or other exposure to blood products/body fluids, such as a health care worker (Box 9-2), or a past history of hepatitis that currently appears with arthralgias (Case Example 9-2).
Other red flag symptoms include joint or muscle pain that is disproportionate to the physical findings and the presence of palmar tendinitis in someone with RA and positive risk factors for hepatitis.
Chronic Hepatitis: Chronic hepatitis is the term used to describe an illness associated with prolonged inflammation of the liver after unresolved viral hepatitis or associated with chronic active hepatitis (CAH) of unknown cause. Chronic is defined as inflammation of the liver for 6 months or more. The symptoms and biochemical abnormalities may continue for months or years. It is divided into CAH and chronic persistent hepatitis (CPH) by findings on liver biopsy.
Chronic Active Hepatitis: This type of hepatitis refers to seriously destructive liver disease that can result in cirrhosis. CAH is often a result of viral infection (HBV, HCV, and HDV), but it can also be secondary to drug sensitivity (e.g., methyldopa [Aldomet], an antihypertensive medication, and isoniazid [INH], an antitubercular drug).
Steroid therapy is sometimes recommended for clients with evidence of aggressive liver inflammation and necrosis (identified by liver biopsy) as a result of these drugs. If CAH is left untreated, its course is unpredictable and may range from progressive deterioration of liver function to spontaneous remissions and exacerbations.
Steroids may be used to treat CAH. They are usually prescribed for a period of 3 to 5 years. In addition, recombinant interferon-alpha-2b injections in low doses over a 6-month period have been shown to improve hepatic function in persons with CAH. Treatment of HCV is relatively new and consists of the use of interferons (IFNs), a protein naturally occurring in the healthy body in response to infection such as the hepatitis virus.
Conventional IFN has been used for many years in the treatment of chronic HCV in clients who persistently maintain HCV/RNA blood levels. Combining IFNs with the drug ribavirin has resulted in better control of chronic HCV in some individuals, but the treatment is not well tolerated because of side effects from the ribavirin.23,24
Pegylated IFNs, such as Pegasys (peginterferon alpha-2a), are improved forms of IFNs that allow a decrease in dosage and offer improved efficacy. Peginterferons (PEGs) in combination with ribavirin are now considered the standard treatment for chronic HCV infection. These new PEG interferons do not eliminate the known side effects associated with classical interferon treatment (e.g., fatigue, headache, myalgia, fever, anxiety, irritability, GI upset).19,25
Metabolic Disease: The most common metabolic diseases that can cause chronic hepatitis and are of interest to a physical therapist are Wilson’s disease and hematochromatosis, also termed hemochromatosis. Both of these diseases are dealt with in greater detail as metabolic disorders in Chapter 11.
Wilson’s disease is an autosomal recessive disorder in which biliary excretion of copper is impaired, and as a consequence, total body copper is progressively increased. There may be mild-to-severe neurologic dysfunction, depending on the rate of hepatocyte injury.
Hemochromatosis is the most common genetic disorder (autosomal recessive defect in iron absorption) causing liver failure. Excessive iron is stored in various parenchymal organs with subsequent development of fibrosis. Arthralgias and arthropathy may develop and are often confused with RA or osteoarthritis. The second and third metacarpophalangeal joints are usually involved first. Knees, hips, shoulders, and lower back may be affected. Acute synovitis with pseudogout of the knees has been observed.
Nonviral Hepatitis: Nonviral hepatitis is considered to be a toxic or drug-induced form of liver inflammation. This type of hepatitis occurs secondary to exposure to alcohol, certain chemicals, or drugs such as antiinflammatories, anticonvulsants, antibiotics, cytotoxic drugs for the treatment of cancer, antituberculars, radiographic contrast agents for diagnostic testing, antipsychotics, and antidepressants (Box 9-3).
Acetaminophen, the popular over-the-counter (OTC) pain reliever, has been found to be the leading cause of sudden liver failure in adults in the United States.26 The drug is safe when taken properly, but even a small overdose in some people can trigger sudden liver failure. The use of this drug becomes even more dangerous with taken by individuals with an already impaired liver.27
The mechanism by which these agents induce overt injury may be dose-related and predictable or idiosyncratic and unpredictable, with the latter caused by an unusual susceptibility of the individual. Some drugs (e.g., oral contraceptives) may impair liver function and produce jaundice without causing necrosis, fatty infiltration of liver cells, or a hypersensitivity reaction.
Cirrhosis
Cirrhosis is a chronic hepatic disease characterized by the destruction of liver cells and by the replacement of connective tissue by fibrous bands. As the liver becomes more and more scarred (fibrosed), blood and lymph flow become impaired, causing hepatic insufficiency and increased clinical manifestations. The causes of cirrhosis can be varied, although alcohol abuse is the most common cause of liver disease in the United States.
In addition, about 25% of Americans have a problem called nonalcoholic fatty liver disease (NAFLD), defined as fatty infiltration of the liver exceeding 5% to 10% by weight. NAFLD is an illness closely associated with diabetes, obesity, and insulin resistance or metabolic syndrome.28,29 It is an independent risk factor for cardiovascular disease29 and may make liver damage caused by other agents (e.g., alcohol, industrial toxins, hepatotrophic viruses) worse.30,31
Ten percent to 20% of people with NAFLD will develop liver inflammation leading to liver scarring and cirrhosis.32 Prevention and treatment of diabetes, obesity, and insulin resistance and protection of the liver from medications that cause fatty infiltration and toxins can help to limit the course of this disease.31
The activity level of the client with damage from chronic liver impairment is determined by the symptoms. Because hepatic blood flow diminishes with moderate exercise, rest periods are advised and are adjusted according to the level of fatigue experienced by the client both during the exercise and afterward at home.
The person may return to work with medical approval but is advised to avoid straining, such as lifting heavy objects if portal hypertension and esophageal varices are a problem. Because stress decreases hepatic blood flow, any reduction of stress at home, at work, or during treatment is therapeutic.
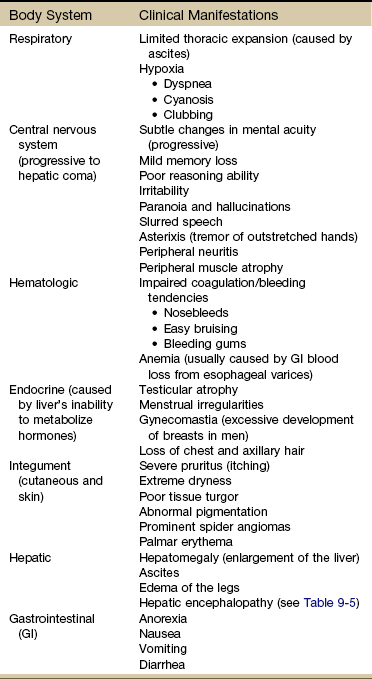
Progression of Cirrhosis: As the cirrhosis progresses and hepatic insufficiency develops, a series of conditions emerges, including portal hypertension, ascites, and esophageal varices. Late symptoms affecting the entire body develop (Table 9-4).
Portal hypertension is elevated pressure in the portal vein (through which blood passes from the GI tract and spleen to the liver), occurring as portal blood meets increased resistance to flow in the fibrotic liver. The blood then backs up into esophageal, stomach, and splenic structures and bypasses the liver through collateral vessels.
Ascites is an abnormal accumulation of fluid containing large amounts of protein and electrolytes in the peritoneal cavity as a result of portal backup and loss of proteins that presents as a distended abdomen, bulging flanks, and a protruding, displaced umbilicus (see Fig. 9-8). It is the result of free fluid in the peritoneal cavity. For the physical therapist, abdominal hernias and lumbar lordosis observed in clients with ascites may present symptoms that mimic musculoskeletal involvement, such as groin or low-back pain (Case Example 9-3).
Esophageal varices are dilated veins of the lower esophagus that occur as a result of portal vein blood backup. These varices are thin-walled and can rupture, causing severe hemorrhage and sometimes death.
Hepatic Encephalopathy (Hepatic Coma)
Hepatic coma is a neurologic disorder resulting from the inability of the liver to detoxify ammonia (produced from protein breakdown) in the intestine. Increased serum levels of ammonia are directly toxic to central and peripheral nervous system function, causing an array of neurologic symptoms. Flapping tremors (asterixis) and numbness/tingling (misinterpreted as carpal/tarsal tunnel syndrome) are common symptoms of this ammonia abnormality.
Clinical Signs and Symptoms: Clinical manifestations of hepatic encephalopathy vary, depending on the severity of neurologic involvement, and develop in four stages as the ammonia level increases in the serum. The accompanying clinical features are presented in Table 9-5.
TABLE 9-5
Stages of Hepatic Encephalopathy
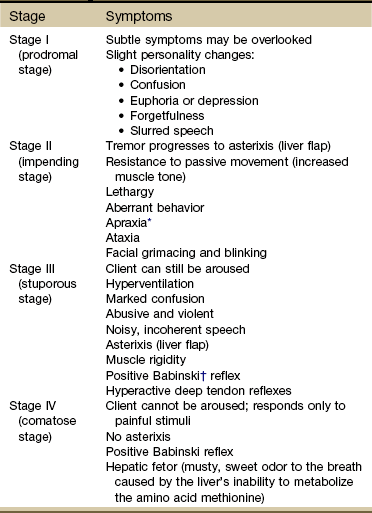
*This type of motor apraxia can be best observed by keeping a record of the client’s handwriting and drawings of simple shapes such as a circle, square, triangle, rectangle. Check for progressive deterioration.
†A reflex action of the toes that is normal during infancy but abnormal after 12 to 18 months. It is elicited by a firm stimulus (usually scraping with the handle of a reflex hammer) on the sole of the foot from the heel along the lateral border of the sole to the little toe, across the ball of the foot to the big toe. Normally, such a stimulus causes all the toes to flex downward. A positive Babinski reflex occurs when the great toe flexes upward and the smaller toes fan outward.
For the physical therapist, the inpatient with impending hepatic coma has difficulty in ambulating and is unsteady. Protection from falling and seizure precautions must be taken. Skin breakdown in a client who is malnourished because of liver disease, immobile, jaundiced, and edematous can occur in less than 24 hours. Careful attention to skin care, passive exercise, and frequent changes in position are required.
Newborn Jaundice
Jaundice affects approximately 60% of newborn infants because liver function is somewhat slow to develop in the first few days of life.33 In a small percentage of infants, extreme jaundice can occur and if left untreated for too long can result in brain damage from toxic levels of bilirubin in the blood. It is critically important for all newborns to be screened for the development of this condition. Development of any color change in newborns needs immediate referral and testing for abnormal bilirubin levels.34,35
Liver Abscess
Liver abscess is relatively rare but occurs when bacteria (e.g., Escherichia coli), fungi (e.g., Candida), or protozoa (ameba) destroy hepatic tissue and produce a cavity that fills with infectious organisms, liquefied liver cells, and leukocytes. Necrotic tissue then isolates the cavity from the rest of the liver. Biliary tract disease (obstruction of bile flow allows for bacterial invasion) is the most frequent cause of liver abscess. Less common causes include appendicitis, immune disorders, and infections in other organs.36
The development of new radiologic techniques, the improvement in microbiologic identification, and the advancement of medical treatment, as well as improved supportive care, have decreased mortality rates from 30% to 50% down to 5% to 30%; yet the prevalence of liver abscess has remained relatively unchanged. Untreated, this infection remains uniformly fatal.36,37
Liver Cancer
Metastatic tumors to the liver occur 20 times more often than primary liver tumors. The liver filters blood coming from the GI tract, making it a primary metastatic site for tumors of the stomach, colorectum, and pancreas. It is also a common site for metastases from other primary cancers such as esophagus, lung, and breast.
Primary liver tumors (hepatocellular carcinoma [HCC]) are often associated with cirrhosis but can be linked to other predisposing factors such as fungal infection (common in moldy foods of Africa), viral hepatitis, excessive use of anabolic steroids, trauma, nutritional deficiencies, and exposure to hepatotoxins.
Cholangiocarcinoma (CCC), a serious and often fatal form of liver cancer, is the second most common form of hepatic malignancy. CCC originates from the epithelium of the bile ducts and has many of the same risk factors as HCC, but preexisting biliary disease is the primary risk factor.38
Several types of benign and malignant hepatic neoplasms can result from the administration of chemical agents. For example, adenoma (a benign tumor) can occur in recipients of oral contraceptives. Regression of the tumor occurs after withdrawal of the drug.
In most instances, interference with liver function does not occur until approximately 80% to 90% of the liver is replaced by metastatic carcinoma or primary carcinoma. Signs of liver impairment are often late in the presentation, making early detection and successful treatment less likely. The alert physical therapist may be the first to identify liver involvement when the neuromuscular or musculoskeletal systems are affected.
Gallbladder and Duct Diseases
Gallstones are stonelike masses called calculi (singular: calculus) that form in the gallbladder, possibly as a result of changes in the normal components of bile. Although there are two types of stones, pigment and cholesterol stones, most types of gallstone disease in the United States, Europe, and Africa are associated with cholesterol stones.
Cholelithiasis, the presence or formation of gallstones, can be asymptomatic, detected incidentally during medical imaging. Problems arise if a stone leaves the gallbladder and causes obstruction somewhere else in the biliary system, presenting as biliary colic, cholecystitis, or cholangitis.
Cholelithiasis is the fifth leading cause of hospitalization among adults and accounts for 90% of all gallbladder and duct diseases. The incidence of gallstones increases with age, occurring in more than 40% of people older than 70. See Box 9-4 for risk factors to watch for in a client’s history that correlate with the incidence of gallstones.
Clients with gallstones may be asymptomatic or may have symptoms of a gallbladder attack described in the next section. The prognosis is usually good with medical treatment, depending on the severity of disease, presence of infection, and response to antibiotics.
Biliary Colic
With biliary colic, the stone gets lodged in the neck of the gallbladder (cystic duct). Pain results as the gallbladder contracts and tries to push the stone through. The classic symptom of this problem is right upper abdominal pain that comes and goes in waves. The pain builds to a peak and then fades away.
Obstructions of the gallbladder can result in biliary stasis, delayed gallbladder emptying, and subsequent mixed stone formation. Stasis and delayed gallbladder emptying can occur with any pathologic conditions of the liver, hormonal influences, and pregnancy (usually third trimester when the developing fetus compresses the mother’s gallbladder up against the liver).
Cholecystitis
Cholecystitis, the blockage or impaction of gallstones in the cystic duct (Fig. 9-9), leads to infection or inflammation of the gallbladder. This condition may be acute or chronic, causing painful distention of the gallbladder. The affected individual may feel steady, severe pain that increases rapidly, lasting several minutes to several hours. Nausea, vomiting, and fever may be present.
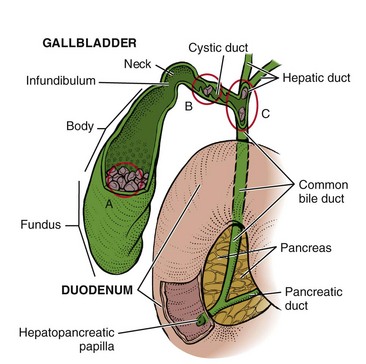
Fig. 9-9 The gallbladder and its divisions: fundus, body, infundibulum, and neck. A, Cholelithiasis, the presence or formation of gallstones, can be asymptomatic, detected incidentally during medical imaging. Problems arise if a stone leaves the gallbladder and causes obstruction somewhere else in the biliary system. B, If a gallstone enters the cystic duct and becomes lodged there, it can lead to cholecystitis (inflammation of the gallbladder). C, Obstruction of either the hepatic or common bile duct by stone or spasm blocks the exit of bile from the liver where it is formed. Jaundice is often the first symptom. If an infection develops and backs up into the liver, a condition called cholangitis can occur, a potentially life-threatening problem.
Other causes of acute cholecystitis may be typhoid fever or a malignant tumor obstructing the biliary tract. Whatever the cause of the obstruction, the normal flow of bile is interrupted and the gallbladder becomes distended and ischemic.
Gallstones may also cause chronic cholecystitis (persistent gallbladder inflammation), in which the gallbladder atrophies and becomes fibrotic, adhering to adjacent organs. It is not unusual for affected clients to have repeated episodes before seeking medical attention.
Cholangitis
Gallstones lodged further down in the system in the common bile duct can cause cholangitis. Blocking the flow of bile at this point in the biliary tree can lead to jaundice. Infection can develop here and travel up to the liver, becoming a potentially life-threatening situation.
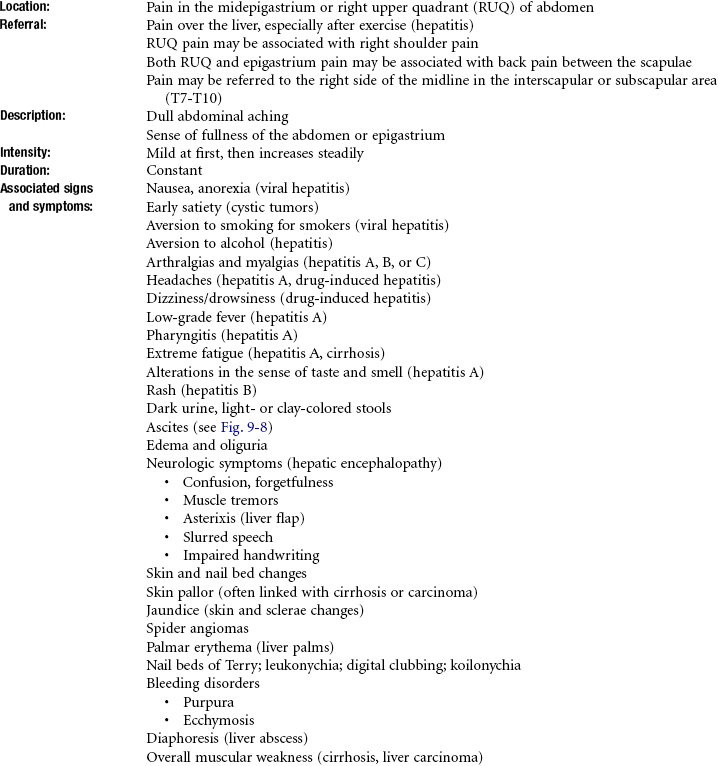
Clinical Signs and Symptoms
The typical pain of gallbladder disease has been described as colicky pain that occurs in the right upper quadrant (RUQ) of the abdomen after the person has eaten a meal that is high in fat (although food that provokes an attack of pain does not need to be “fatty”). However, the pain is not necessarily limited to the RUQ, and more likely than not, it is constant, not colicky.
Like the stomach, pylorus, and duodenum, the liver and gallbladder can cause spasm of the rectus abdominis muscles above the umbilicus. This occurs when disturbances within the hepatic and biliary systems as part of the overall GI system affect motor reflexes.
These disturbances can be reflected in muscular contractions of the spinal, abdominal, and other muscles supplied by the motor nerves from the anterior horn of the segment innervating the affected viscera.39
It looks just like a musculoskeletal problem, but the pain pattern is the result of viscero-somatic reflexes as discussed in Chapter 3 (Case Example 9-4). Ask about the timing of symptoms in relation to eating or drinking. Watch for symptoms that are worse immediately after eating (gallbladder inflammation) or pain and nausea 1 to 3 hours after eating (gallstones).
Muscle guarding and tenderness of the spinal musculature in the presence of constitutional symptoms (e.g., fever, sweats, chills, nausea) is another red flag. Ask about a previous history of GI, liver, or gallbladder problems, and review the client’s risk factors for hepatic involvement.
In the case of gallbladder disease, it is also possible to get tender points in the soma corresponding to visceral innervation. A gallbladder problem can result in a sore 10th rib tip (right side anteriorly) when messages from the viscera entering the spinal cord at the same level as the innervation of the rib are misinterpreted as a somatic problem. The gallbladder has most of its innervation from the right side of the cervical ganglia to the splanchnic nerves, which explains the predominance of right-sided somatic symptoms.
When visceral and cutaneous fibers enter the spinal cord at the same level, the nervous system may respond with sudomotor changes, such as pruritus (itching of the skin) or a sore rib, instead of gallbladder symptoms. The clinical presentation appears as a biomechanical problem, such as a rib dysfunction, instead of nausea and food intolerances normally associated with gallbladder dysfunction.
Likewise, from our understanding of viscerogenic pain patterns based on embryologic development, we know that the visceral pericardium of the heart (see Fig. 6-5) is derived from the same embryologic tissue as the gallbladder. A gallbladder problem can also cause referred pain to the heart and must be ruled out by the physician as a possible cause of chest pain.
Primary Biliary Cirrhosis
Primary biliary cirrhosis (PBC) is a chronic, progressive, autoimmune disease of the liver that involves primarily the intrahepatic bile ducts and results in impairment of bile secretion. The disease, which often affects middle-aged women (in particular Native American women), begins with pruritus or biochemical evidence of cholestasis and progresses at a variable rate to jaundice, portal hypertension, and liver failure.40
The cause of PBC is unknown, although various factors are being investigated. An autoimmune pathogenesis is widely accepted, based on the presence of autoantibodies and autoreactive T cells.41 Many clients have associated autoimmune features, particularly Sjögren’s syndrome, autoimmune thyroiditis, and renal tubular acidosis.42 In more rare cases, clients may exhibit sensory peripheral neuropathies of the hands and feet.
Fatigue and pruritus are the most common symptoms of PBC, but the majority of people are asymptomatic at first presentation.43 The most significant clinical problem for clients with PBC is bone disease characterized by impaired osteoblastic activity and accelerated osteoclastic activity. Calcium and vitamin D should be carefully monitored and appropriate replacement instituted. Physical activity following an osteoporosis protocol should be encouraged.
Gallbladder Cancer
Gallbladder cancer, closely associated with gallstone disease, often has a poor outcome due to delay in diagnosis. The primary associated risk factors include cholelithiasis (especially symptomatic, untreated), obesity, reproductive abnormalities, chronic gallbladder infections, and exposure to radon and certain industrial exposures including cellulose acetate fiber manufacturing. Testing and treatment of symptomatic gallstones is the only preventive measure identified at this time for gallbladder cancer.44
Physician Referral
A careful history and close observation of the client are important in determining whether a person may need a medical referral for possible hepatic or biliary involvement. Any client with mid-back, scapular, or right shoulder pain (see Table 9-1) without a history of trauma (e.g., forceful movement of the spine, repetitive movements of the shoulder or back, or easy lifting) should be screened for possible systemic origin of symptoms.
For the physical therapist treating the inpatient population, jaundice in the postoperative individual is not uncommon but can be a potentially serious complication of surgery and anesthesia.
Clinical management of jaundice is complicated by anything capable of damaging the liver, including physical stress associated with physical therapy intervention. Hypoxemia, blood loss, infection, and administration of multiple drugs can add additional physical stress.
When making the referral, it is important to report to the physician the results of your objective findings, especially when there is a lack of physical evidence to support a musculoskeletal lesion. The Special Questions to Ask may assist in assessing the client’s overall health status.
Guidelines to Physician Referral
• Obvious signs of hepatic disease, especially with a history of previous cancer or risk factors for hepatitis (see Box 9-2)
• Development of arthralgias of unknown cause in anyone with a previous history of hepatitis or risk factors for hepatitis
• Presence of bilateral carpal tunnel syndrome accompanied by bilateral tarsal tunnel syndrome unknown to the physician, asterixis, or other associated hepatic signs and symptoms
• Presence of sensory neuropathy of unknown cause accompanied by signs and symptoms associated with hepatic system impairment
Clues to Screening for Hepatic Disease
• Right shoulder/scapular and/or upper mid-back pain of unknown cause (see also Clues to Screening Shoulder Pain in Chapter 18).
• Shoulder motion is not limited by painful symptoms; client is unable to localize or pinpoint pain or tenderness.
• Presence of GI symptoms, especially if there is any correlation between eating and painful symptoms.
• Bilateral carpal/tarsal tunnel syndrome, especially of unknown origin; check for other signs of liver impairment such as liver flap, liver palms, and skin or nail bed changes (see Box 9-1).
• Personal history of cancer, liver, or gallbladder disease.
• Personal history of hepatitis, especially with joint pain associated with rheumatoid arthritis or fibromyalgia accompanied by palmar tendinitis.
• Recent history of statin use (cholesterol-lowering drugs such as Zocor, Lipitor, Crestor) or other hepatotoxic drugs.
• Recent operative procedure (possible postoperative jaundice).
• Recent (within last 6 months) injection drug use, tattoo (receiving or removal), acupuncture, ear or body piercing, dialysis, blood or plasma transfusion, active homosexual activity, heterosexual sexual activity with homosexuals, consumption of raw shellfish (hepatitis).
• Changes in skin (yellow hue, spider angiomas, palmar erythema) or eye color (jaundice).
• Employment or lifestyle involving alcohol consumption (jaundice).
• Contact with jaundiced persons (health care worker handling blood or body fluids, dialysis clients, injection drug users, active homosexual sexual activity, heterosexual sexual activity with homosexuals).
1. Referred pain patterns associated with hepatic and biliary pathologic conditions produce musculoskeletal symptoms in the:
2. What is the mechanism for referred right shoulder pain from hepatic or biliary disease?
3. Why does someone with liver dysfunction develop numbness and tingling that is sometimes labeled carpal tunnel syndrome?
4. When a client with bilateral carpal tunnel syndrome is being evaluated, how do you screen for the possibility of a pathologic condition of the liver?
5. What is the first most common sign associated with liver disease?
6. You are treating a 53-year-old woman who has had an extensive medical history that includes bilateral kidney disease with kidney removal on one side and transplantation on the other. The client is 10 years posttransplant and has now developed multiple problems as a result of the long-term use of immunosuppressants (cyclosporine to prevent organ rejection) and corticosteroids (prednisone). For example, she is extremely osteoporotic and has been diagnosed with cytomegalovirus and corticosteroid-induced myopathy. The client has fallen and broken her vertebra, ankle, and wrist on separate occasions. You are seeing her at home to implement a strengthening program and to instruct her in a falling prevention program, including home modifications. You notice the sclerae of her eyes are yellow-tinged. How do you tactfully ask her about this?
7. Clients with significant elevations in serum bilirubin levels caused by biliary obstruction will have which of the following associated signs?
8. Preventing falls and trauma to soft tissues would be of utmost importance in the client with liver failure. Which of the following laboratory parameters would give you the most information about potential tissue injury?
9. Decreased level of consciousness, impaired function of peripheral nerves, and asterixis (flapping tremor) would probably indicate an increase in the level of:
10. An inpatient who has had a total hip replacement with a significant history of alcohol use/abuse has a positive test for asterixis. This may signify:
11. A decrease in serum albumin is common with a pathologic condition of the liver because albumin is produced in the liver. The reduction in serum albumin results in some easily identifiable signs. Which of the following signs might alert the therapist to the condition of decreased albumin?
References
1. Key, L, Bell, NH. Osteomalacia and disorders of vitamin D metabolism. In Stein JH, ed.: Internal medicine, ed 5, St Louis: Mosby, 1998.
2. Baxter, RE, Moore, JH. Diagnosis and treatment of acute exertional rhabdomyolysis. J Orthop Sports Phys Ther. 2003;33(3):104–108.
3. Kumbhare, D. Validity of serum creatine kinase as a measure of muscle injury produced by lumbar surgery. J Spinal Disord Tech. 2008;21(1):49–54.
4. Lenfant, C. ACC/AHA/NHLBI Clinical advisory on the use and safety of statins. Cardiol Rev. 2003;20(4Suppl):9–11.
5. Chatham, K. Suspected statin-induced respiratory muscle myopathy during long-term inspiratory muscle training in a patient with diaphragmatic paralysis. Phys Ther. 2009;89(3):1–10.
6. Newman, CB, Palmer, G, Silbershatz, H, et al. Safety of atorvastatin derived from analysis of 44 completed trials in 9,416 patients. Am J Cardiol. 2003;92(6):670–676.
7. Tomlinson, SS, Mangione, KK. Potential adverse effects of statins on muscle. Phys Ther. 2005;85:459–465.
8. Buettner, C. Prevalence of musculoskeletal pain and statin use. J Gen Intern Med. 2008;23:1182–1186.
9. Ballantyne, CM, Corsini, A, Davidson, MH, et al. Risk for myopathy with statin therapy in high-risk patients. Arch Intern Med. 2003;163(5):553–564.
10. Parnes, A, Asterixis. Trinity Stud Med J 2000;1:58. Available at http://www.tcd.ie/tsmj. [Accessed Oct. 18, 2010].
11. Melnick, JL. History and epidemiology of Hepatitis A virus. J Infect Dis. 1995;171(Suppl):S2–S8.
12. McPhee S, Papadakis M, eds. Current medical diagnosis and treatment, ed 50, New York: Lange, 2011.
13. Grande, P, Cronquist, A. Public health dispatch, multistate outbreak of hepatitis A among young adult concert attendees, United States, 2003. MMWR. 2003;52(35):844–845.
14. Wolf, DC. Hepatitis, Viral. eMedicine Specialties: Gastroenterology. Updated June 25, 2010. Available online at http://emedicine.medscape.com/article/185463-overview. [Accessed February 1, 2011].
15. Weinbaum, C, Lyerla, C. Prevention and control of infections with hepatitis viruses in correctional settings. MMWR. 2003. [5201 1–33, Jan 24].
16. Parini, S. Hepatitis C. Nursing2003. 2003;33(4):57.
17. Spencer, KY, Chang, MD. Anterior cruciate ligament reconstruction: allograft vs. autograft. J Arthrosc Rel Surg. 2003;19(5):453.
18. Friedman McPhee S, Papadakis M, eds. Current medical diagnosis and treatment, ed 50, New York: Lange, 2011.
19. Sanzone, AM. Hepatitis and arthritis: an update. Infect Dis Clin N Am. 2006;20:877–889.
20. Khouqeer, RA. Viral arthritis. eMedicine Specialties: Rheumatology—Infectious arthritis. Updated August 1, 2008. Available online at http://emedicine.medscape.com/article/335692-overview. [Accessed February 1, 2011].
21. Lovy, MR, Wener, MH. Rheumatic disease: when is hepatitis C the culprit? J Musculoskel Med. 1996;13(4):27–35.
22. Rull, M, Zonay, L, Schumacher, HR. Hepatitis C and rheumatic diseases. J Musculoskel Med. 1998;15(11):38–44.
23. Foster, GR. Past, present, and future hepatitis C treatments. Semin Liver Disease. 2004;2:97–104. [Suppl].
24. Pearlman, BL. Hepatitis C treatment update. Am J Med. 2004;117(5):344–352.
25. Pullen, L. Hep-Hazard. HemAware. 2004;9(2):54–56.
26. Farrell, SE. Toxicity, Acetaminophen, eMedicine Specialties: Emergency medicine—Toxicology. Updated Nov. 19, 2010. Available online at http://emedicine.medscape.com/article/820200-overview. [Accessed February 1, 2011].
27. , Liver function: two new threats. John Hopkins Med Lett: Health after 50. 2003;15;3:2–7. www.johnshopkinshealthalerts.com/health_after_50. [Accessed Oct. 18, 2010].
28. Adams, LA, Feldstein, AE. Nonalcoholic steatohepatitis: risk factors and diagnosis. Expert Rev Gastroenterol Hepatol. 2010;4(5):623–635.
29. Feldstein, AE. Novel insights into the pathophysiology of nonalcoholic fatty liver disease. Semin Liver Dis. 2010;30(4):391–401.
30. Salt, WB. Nonalcoholic fatty liver disease (NAFLD): a comprehensive review. J Insur Med. 2004;36(1):27–41.
31. Pasumarthy, L, Srour, J. Nonalcoholic steatohepatitis: a review of the literature and updates in management. South Med J. 2010;103(6):547–550.
32. Younossi, ZM, McCullough, AJ, Ong, JP, et al. Obesity and non-alcoholic fatty liver disease in chronic hepatitis C. J Clin Gastroenterol. 2004;38(8):705–709.
33. Cohen, RS. Understanding neonatal jaundice: a perspective on causation. Pediatr Neonatol. 2010;51(3):143–148.
34. Neonatal jaundice, unwelcome return for kernicterus. Nursing2003. 2003;33(11):35.
35. Lease, M, Whalen, B. Assessing jaundice in infants of 35-week gestation and greater. Curr Opin Pediatr. 2010;22(3):352–365.
36. Peralta, R. Liver abscess. eMedicine Specialties: Abdomen. Updated Sept. 15, 2009. Available online at http://emedicine.medscape.com/article/188802-overview. [Accessed February 1, 2011].
37. Chen, SC. Severity of disease as main predictor for mortality in patients with pyogenic liver abscess. Am J Surg. 2009;198(2):164–172.
38. Bisceglie, A. Prevention of hepatocellular carcinoma complicating chronic hepatitis C. J Gastroenterol Hepatol. 2009;24(4):531–536.
39. Rex, L. Evaluation and treatment of somatovisceral dysfunction of the gastrointestinal system. Edmonds, WA: URSA Foundation; 2004.
40. Hu, CJ. Primary biliary cirrhosis: what do autoantibodies tell us? World J Gastroenterol. 2010;16(29):3616–3629.
41. Selmi, C. The etiology mystery in primary biliary cirrhosis. Dig Dis. 2010;28(1):105–115.
42. Pyrsopoulos, NT. Primary biliary cirrhosis, eMedicine Specialties: Liver. Updated Dec. 23, 2009. Available online at http://emedicine.medscape.com/article/171117-overview. [Accessed February 1, 2011].
43. Abbas, G. Fatigue in primary biliary cirrhosis. Nat Rev Gastroenterol Hepatol. 2010;7(6):313–319.
44. Mehrotra, B, Gallbladder cancer: epidemiology, risk factors, clinical features, and diagnosis, Up-To-Date August 19, 2010. Available online (subscription) at http://www.uptodate.com/contents/gallbladder-cancer-epidemiology-risk-factors-clinical-features-and-diagnosis. [Accessed February 1, 2011].
45. Kimbel, DL. Hip pain in a 50-year-old woman with RA. J Musculoskel Med. 1999;16(11):651–652.

 Key Points to Remember
Key Points to Remember