Physical Assessment as a Screening Tool
In the medical model, clients are often assessed from head to toe. The doctor, physician assistant, nurse, or nurse practitioner starts with inspection, followed by percussion and palpation, and finally by auscultation.
In a screening assessment, the therapist may not need to perform a complete head-to-toe physical assessment. If the initial observations, client history, screening questions, and screening tests are negative, move on to the next step. A thorough examination may not be necessary.
In most situations, it is advised to assess one system above and below the area of complaint based on evidence supporting a regional-interdependence model of musculoskeletal impairments (i.e., symptoms present may be caused by musculoskeletal impairments proximal or distal to the site of presenting symptoms distinct from the phenomenon of referred pain).1
When screening for systemic origins of clinical signs and symptoms, the therapist first scans the area(s) that directly relate to the client’s history and clinical presentation. For example, a shoulder problem can be caused by a problem in the stomach, heart, liver/biliary, lungs, spleen, kidneys, and ovaries (ectopic pregnancy). Only the physical assessment tests related to these areas would be assessed. These often can be narrowed down by the client’s history, gender, age, presence of risk factors, and associated signs and symptoms linked to a specific system.
More specifically, consider the postmenopausal woman with a primary family history of heart disease who presents with shoulder pain that occurs 3 to 4 minutes after starting an activity and is accompanied by unexplained perspiration. This individual should be assessed for cardiac involvement. Or think about the 45-year-old mother of five children who presents with scapular pain that is worse after she eats. A cardiac assessment may not be as important as a scan for signs and symptoms associated with the gallbladder or biliary system.
Documentation of physical findings is important. From a legal standpoint, if you did not document it, you did not assess it. Look for changes from the expected norm, as well as changes for the client’s baseline measurements. Use simple and clear documentation that can be understood and used by others. As much as possible, record both normal and abnormal findings for each client.2 Keep in mind that the client’s cultural and educational background, beliefs, values, and previous experiences can influence his or her response to questions.
Finally, screening and ongoing physical assessment is often a part of an exercise evaluation, especially for the client with one or more serious health concerns. Listening to the heart and lung sounds before initiating an exercise program may bring to light any contraindications to exercise. A compromised cardiopulmonary system may make it impossible and even dangerous for the client to sustain prescribed exercise levels.
The use of quick and easy screening tools such as the Physical Therapist Community Screening Form for Aging Adults can help therapists identify limitations to optimal heath, wellness, and fitness in any of seven areas (e.g., posture, flexibility, strength, balance, cardiovascular fitness) for adults aged 65 and older. With the 2007 House of Delegates position statement recommending that all individuals visit a physical therapist at least once a year to promote optimal health and wellness, evidence-based tests of this type will become increasingly available.3
General Survey
Physical assessment begins the moment you meet the client as you observe body size and type, facial expressions, evaluate self-care, and note anything unusual in appearance or presentation. Keep in mind (as discussed in Chapter 2) that cultural factors may dictate how the client presents himself (e.g., avoiding eye contact when answering questions, hiding or exaggerating signs of pain).
A few pieces of equipment in a small kit within easy reach can make the screening exam faster and easier (Box 4-1). Using the same pattern in screening each time will help the therapist avoid missing important screening clues.
As the therapist makes a general survey of each client, it is also possible to evaluate posture, movement patterns and gait, balance, and coordination. For more involved clients the first impression may be based on level of consciousness, respiratory and vascular function, or nutritional status.
In an acute care or trauma setting the therapist may be using vital signs and the ABCDE (airway, breathing, circulation, disability, exposure) method of quick assessment. A common strategy for history taking in the trauma unit is the mnemonic AMPLE: Allergies, Medications, Past medical history, Last meal, and Events of injury.
In any setting, knowing the client’s personal health history will also help guide and direct which components of the physical examination to include. We are not just screening for medical disease masquerading as neuromusculoskeletal (NMS) problems. Many physical illnesses, diseases, and medical conditions directly impact the NMS system and must be taken into account. For example inspection of the integument, limb inspection, and screening of the peripheral vascular system is important for someone at risk for lymphedema.
Neurologic function, balance, reflexes, and peripheral circulation become important when screening a client with diabetes mellitus. Peripheral neuropathy is common in this population group, often making walking more difficult and increasing risk of other problems developing.
Therapists in all settings, especially primary care therapists, can use a screening physical assessment to provide education toward primary prevention, as well as intervention and management of current dysfunctions and disabilities.
Mental Status
Level of consciousness, orientation, and ability to communicate are all part of the assessment of a client’s mental status. Orientation refers to the client’s ability to answer correctly questions about time, place, and person. A healthy individual with normal mental status will be alert, speak coherently, and be aware of the date, day, and time of day.
The therapist must be aware of any factor that can affect a client’s current mental status. Shock, head injury, stroke, hospitalization, surgery (use of anesthesia), medications, age, and the use of substances and/or alcohol (see discussion, Chapter 2) can cause impaired consciousness.
Other factors affecting mental status may include malnutrition, exposure to chemicals, and hypothermia or hyperthermia. Depression and anxiety (see discussion, Chapter 3) also can affect a client’s functioning, mood, memory, ability to concentrate, judgment, and thought processes. Educational and socioeconomic background along with communication skills (e.g., English as a second language, aphasia) can affect mental status and function.
In a hospital, transition unit, or extended care facility, mental status is often evaluated and documented by the social worker or nursing service. It is always a good idea to review the client’s chart or electronic record regarding this information before beginning a physical therapy evaluation.
Risk Factors for Delirium
It is not uncommon for older adults to experience a change in mental status or go through a stage of confusion about 24 hours after hospitalization for a serious illness or trauma, including surgery under a general anesthetic. Physicians may refer to this as iatrogenic delirium, anesthesia-induced dementia, or postoperative delirium. It is usually temporary but can last several hours to several weeks.
The cause of deterioration in mental ability is unknown. In some cases, delirium/dementia appears to be triggered by the shock to the body from anesthesia and surgery.4 It may be a passing phase with complete recovery by the client, although this can take weeks to months. The likelihood of delirium associated with hospitalization is much higher with hip fractures and hip and knee joint replacements,5,6 possibly attributed to older age, slower metabolism, and polypharmacy (more than four prescribed drugs at admission).7
The therapist should pay attention to risk factors (Box 4-2) and watch out for any of the signs or symptoms of delirium. Physical exam should include vital signs with oxygen concentration measured, neurologic screening exam, and surveillance for signs of infection. A medical diagnosis is needed to make the distinction between postoperative delirium, baseline dementia, depression, and withdrawal from drugs and alcohol.5
Several scales are used to assess level of consciousness, performance, and disability. The Confusion Assessment Method (CAM) is a bedside rating scale physical therapists can use to assess hospitalized or institutionalized individuals for delirium. This tool has been adapted for use with patients who are ventilated and in an intensive care unit (CAM-ICU).8
There are two parts to the assessment instrument: part one screens for overall cognitive impairment. Part two includes four features that have the greatest ability to distinguish delirium or reversible confusion from other types of cognitive impairment. The tool identifies the presence of delirium but does not assess the severity of the condition.9
As a screening tool, the CAM has been validated for use by physicians and nurses in palliative care and intensive care settings (sensitivity of 94% to 100% and specificity of 90% to 95%). Values for positive predictive accuracy were 91% to 94%, and values for negative predictive accuracy were 100% and 90% for the two populations assessed (general medicine, outpatient geriatric center).9
The Glasgow Outcome Scale10,11 describes patients/clients on a 5-point scale from good recovery (1) to death (5). Vegetative state, severe disability, and moderate disability are included in the continuum. This and other scales and clinical assessment tools are not part of the screening assessment but are available online for use by health care professionals.12
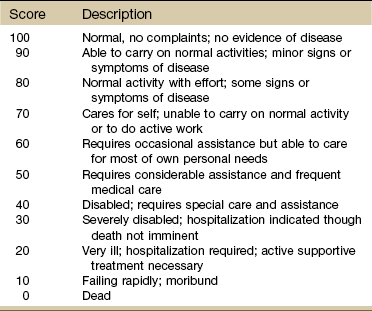
The Karnofsky Performance Scale (KPS) in Table 4-1 is used widely to quantify functional status in a wide variety of individuals, but especially among those with cancer. It can be used to compare effectiveness of intervention and to assess individual prognosis. The lower the Karnofsky score, the worse the prognosis for survival.
The most practical performance scale for use in any rehabilitation setting for most clients is the Eastern Cooperative Oncology Group (ECOG) Performance Status Scale (Table 4-2). Researchers and health care professionals use these scales and criteria to assess how an individual’s disease is progressing, to assess how the disease affects the daily living abilities of the client, and to determine appropriate treatment and prognosis.
TABLE 4-2
| Grade | Level of Activity |
| 0 | Fully active, able to carry on all pre-disease performance without restriction (Karnofsky 90%-100%) |
| 1 | Restricted in physically strenuous activity but ambulatory and able to carry out work of a light or sedentary nature (e.g., light house work, office work) (Karnofsky 70%-80%) |
| 2 | Ambulatory and capable of all self-care but unable to carry out any work activities. Up and about more than 50% of waking hours (Karnofsky 50%-60%) |
| 3 | Capable of only limited self-care, confined to bed or chair more than 50% of waking hours (Karnofsky 30%-40%) |
| 4 | Completely disabled. Cannot carry on any self-care. Totally confined to bed or chair (Karnofsky 10%-20%) |
| 5 | Dead (Karnofsky 0%) |
The Karnofsky Performance Scale allows individuals to be classified according to functional impairment. The lower the score, the worse the prognosis for survival for most serious illnesses.
ECOG, Eastern Cooperative Oncology Group.
From Oken MM, Creech RH, Tormey DC, et al: Toxicity and response criteria of the Eastern Cooperative Oncology Group, Am J Clin Oncol 5:649-655, 1982. Available at www.ecog.org/general/perf_stat.html.
Any observed change in level of consciousness, orientation, judgment, communication or speech pattern, or memory should be documented regardless of which scale is used. The therapist may be the first to notice increased lethargy, slowed motor responses, or disorientation or confusion.
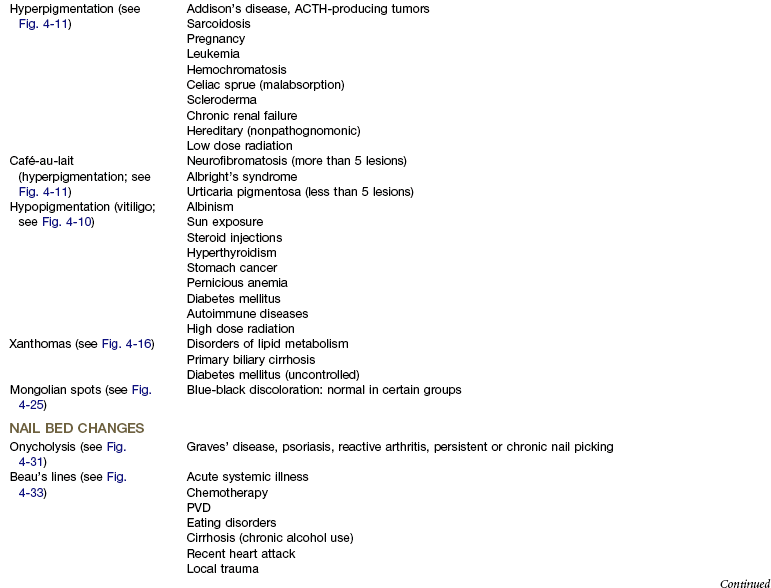
Confusion is not a normal change with aging and must be reported and documented. Confusion is often associated with various systemic conditions (Table 4-3). Increased confusion in a client with any form of dementia can be a symptom of infection (e.g., pneumonia, urinary tract infection), electrolyte imbalance, or delirium. Likewise, a sudden change in muscle tone (usually increased tone) in the client with a neurologic disorder (adult or child) can signal an infectious process.
TABLE 4-3
Systemic Conditions Associated with Confusional States
AIDS, Acquired immunodeficiency syndrome; CHF, congestive heart failure; TIA, transient ischemic attack; CVA, cerebrovascular accident; COPD, chronic obstructive pulmonary disease; SLE, systemic lupus erythematosus.
Modified from Dains JE, Baumann LC, Scheibel P: Advanced health assessment & clinical diagnosis in primary care, ed 2, St. Louis, 2003, Mosby; p 425.
Nutritional Status
Nutrition is an important part of growth and development and recovery from infection, illness, wounds, and surgery. Clients can exhibit signs of malnutrition or overnutrition (obesity).
Be aware in the health history of any risk factors for nutritional deficiencies (Box 4-3). Remember that some medications can cause appetite changes and that psychosocial factors such as depression, eating disorders, drug or alcohol addictions, and economic variables can affect nutritional status.
It may be necessary to determine the client’s ideal body weight by calculating the body mass index (BMI).13,14 Several websites are available to help anyone make this calculation. There is a separate website for children and teens sponsored by the National Center for Chronic Disease Prevention and Health Promotion.15
Whenever nutritional deficiencies are suspected, notify the physician and/or request a referral to a registered dietitian.
Body and Breath Odors
Odors may provide some significant clues to overall health status. For example, a fruity (sweet) breath odor (detectable by some but not all health care professionals) may be a symptom of diabetic ketoacidosis. Bad breath (halitosis) can be a symptom of dental decay, lung abscess, throat or sinus infection, or gastrointestinal (GI) disturbances from food intolerances, Helicobacter pylori bacteria, or bowel obstruction. Keep in mind that ethnic foods and alcohol can affect breath and body odor.
Clients who are incontinent (bowel or bladder) may smell of urine, ammonia, or feces. It is important to ask the client about any unusual odors. It may be best to offer an introductory explanation with some follow-up questions:
Vital Signs
The need for therapists to assess vital signs, especially pulse and blood pressure is increasing.16 Without the benefit of laboratory values, physical assessment becomes much more important. Vital signs, observations, and reported associated signs and symptoms are among the best screening tools available to the therapist.
Vital sign assessment is an important tool because high blood pressure is a serious concern in the United States. Many people are unaware they have high blood pressure. Often primary orthopedic clients have secondary cardiovascular disease.17
Physical therapists practicing in a primary care setting will especially need to know when and how to assess vital signs. The Guide to Physical Therapist Practice18 recommends that heart rate (pulse) and blood pressure measurements be included in the examination of new clients. Exercise professionals are strongly encouraged to measure blood pressure during each visit.19
Taking a client’s vital signs remains the single easiest, most economic, and fastest way to screen for many systemic illnesses. All the vital signs are important (Box 4-4); temperature and blood pressure have the greatest utility as early screening tools for systemic illness or disease, while pulse, blood pressure, and oxygen (O2) saturation level offer valuable information about the cardiovascular/pulmonary systems.
As an aside comment: using vital signs is an easy, yet effective way to document outcomes. In today’s evidence-based practice, the therapist can use something as simple as pulse or blood pressure to document changes that occur with intervention.
For example, if ambulating with a client morning and afternoon results in no change in ease of ambulation, speed, or distance, consider taking blood pressure, pulse, and O2 saturation levels before and after each session. Improvement in O2 saturation levels or faster return to normal of heart rate after exercise are just two examples of how vital signs can become an important part of outcomes documentation.
Assessment of baseline vital signs should be a part of the initial data collected so that correlations and comparisons with future values are available when necessary. The therapist compares measurements taken against normal values and also compares future measurements to the baseline units to identify significant changes (normalizing values or moving toward abnormal findings) for each client.
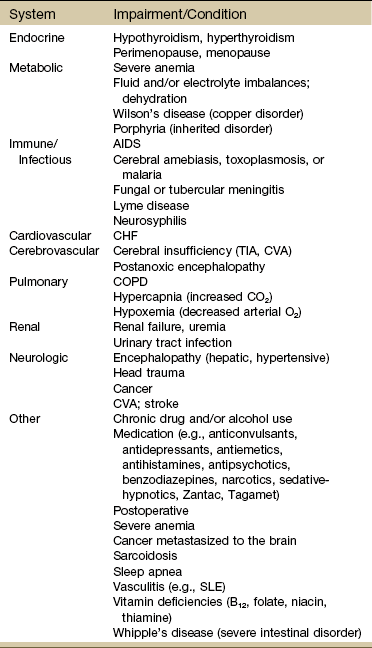
Normal ranges of values for the vital signs are provided for the therapist’s convenience. However, these ranges can be exceeded by a client and still represent normal for that person. Keep in mind that many factors can affect vital signs, especially pulse and blood pressure (Table 4-4). Substances such as alcohol, caffeine, nicotine, and cocaine/cocaine derivatives as well as pain and stress/anxiety can cause fluctuations in blood pressure. Adults who monitor their own blood pressure may report wide fluctuations without making the association between these and other factors listed. It is the unusual vital sign in combination with other signs and symptoms, medications, and medical status that gives clinical meaning to the pulse rate, blood pressure, and temperature.
TABLE 4-4
Factors Affecting Pulse and Blood Pressure
SBP, Systolic blood pressure; ACE, angiotensin-converting enzyme.
*Conditions, such as chronic kidney disease, renovascular disorders, primary aldosteronism, and coarctation of the aorta, are identifiable causes of elevated blood pressure. Chronic overtraining in athletes, use of steroids and/or nonsteroidal antiinflammatory drugs (NSAIDs), and large increases in muscle mass can also contribute to hypertension.38 Treatment for hypertension, dehydration, heart failure, heart attack, arrhythmias, anaphylaxis, shock (from severe infection, stroke, anaphylaxis, major trauma), and advanced diabetes can cause low blood pressure.
From Goodman CC, Fuller K: Pathology: implications for the physical therapist, ed 3, Philadelphia, 2009, WB Saunders.
Pulse Rate
The pulse reveals important information about the client’s heart rate and heart rhythm. A resting pulse rate (normal range: 60 to 100 beats per minute [bpm]) taken at the carotid artery or radial artery (preferred sites) pulse point should be available for comparison with the pulse rate taken during treatment or after exercise. A pulse rate above 100 bpm indicates tachycardia; below 60 bpm indicates bradycardia.
Do not rely on pulse oximeter devices for pulse rate because these units often take a sample pulse rate that reflects a mean average and may not reveal dysrhythmias (e.g., a regular irregular pulse rate associated with atrial fibrillation). It is recommended that the pulse always be checked in two places in older adults and in anyone with diabetes (Fig. 4-1). Pulse strength (amplitude) can be graded as
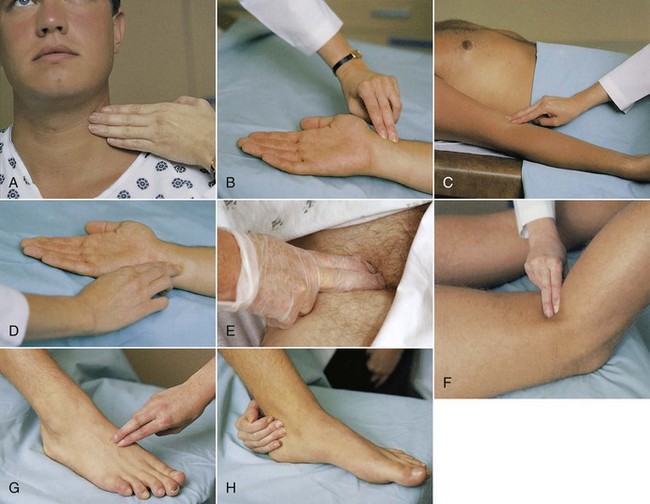
Fig. 4-1 Pulse points. The easiest and most commonly palpated pulses are the (A) carotid pulse and (B) radial pulse. Other pulse points include brachial pulse (C), ulnar pulse (D), femoral pulse (E), popliteal pulse (knee slightly flexed) (F), dorsalis pedis (G), and posterior tibial (H). The anterior tibial pulse becomes the dorsalis pedis and is palpable where the artery lies close to the skin on the dorsum of the foot. Peripheral pulses are more difficult to palpate in older adults and anyone with peripheral vascular disease. (From Potter PA: Fundamentals of nursing, ed 7, St. Louis, 2009, Mosby.)
| 0 | Absent, not palpable |
| 1+ | Pulse diminished, barely palpable |
| 2+ | Easily palpable, normal |
| 3+ | Full pulse, increased strength |
| 4+ | Bounding, too strong to obliterate |
Keep in mind that taking the pulse measures the peripheral arterial wave propagation generated by the heart’s contraction—it is not the same as measuring the true heart rate (and should not be recorded as heart rate when measured by palpation). A true measure of heart rate requires auscultation or electrocardiographic recording of the electrical impulses of the heart. The distinction between pulse rate and heart rate becomes a matter of concern in documentation liability and even greater importance for individuals with dysrhythmias. In such cases, the output of blood by some beats may be insufficient to produce a detectable pulse wave that would be discernible with an electrocardiogram.20
Pulse amplitude (weak or bounding quality of the pulse) gives an indication of the circulating blood volume and the strength of left ventricle ejection. Normally, the pulse increases slightly with inspiration and decreases with expiration. This slight change is not considered significant.
Pulse amplitude that fades with inspiration instead of strengthening and strengthens with expiration instead of fading is paradoxic and should be reported to the physician. Paradoxic pulse occurs most commonly in clients with chronic obstructive pulmonary disease (COPD) but is also observed in clients with constrictive pericarditis.21
Constriction or compression around the heart from pericardial effusion, tension pneumothorax, pericarditis with fluid, or pericardial tamponade may be associated with paradoxical pulse. When the person breathes in, the increased mechanical pressure of inspiration added to the physiologic compression from the underlying disease prevents the heart from contracting fully and results in a reduced pulse. When the person breathes out, the pressure from chest expansion is reduced and the pulse increases.
A pulse increase with activity of more than 20 bpm lasting for more than 3 minutes after rest or changing position should also be reported. Other pulse abnormalities are listed in Box 4-5.
The resting pulse may be higher than normal with fever, anemia, infections, some medications, hyperthyroidism, anxiety, or pain. A low pulse rate (below 60 bpm) is not uncommon among trained athletes. Medications, such as beta-blockers and calcium channel blockers, can also prevent the normal rise in pulse rate that usually occurs during exercise. In such cases the therapist must monitor rates of perceived exertion (RPE) instead of pulse rate.
When taking the resting pulse or pulse during exercise, some clinicians measure the pulse for 15 seconds and multiply by 4 to get the rate per minute. For a quick assessment, measure for 6 seconds and add a zero. A 6-second pulse count can result in an error of 10 bpm if a 1-beat error is made in counting. For screening purposes, it is always best to palpate the pulse for a full minute. Longer pulse counts give greater accuracy and provide more time for detection of some dysrhythmias (Box 4-6).19
Pulse assessment following vascular injuries (especially dislocation of the knee) should not be relied upon as the only diagnostic testing procedure as occult arterial injuries can be present even when pulses are normal. A meta-analysis of 284 dislocated knees concluded that abnormal pulse examinations have a sensitivity of .79 and specificity of .91 for detection of arterial injuries.22,23 On the other hand, there are reports of normal pulse examinations at the time of the initial knee injury in people who later developed ischemia leading to amputation.24,25
Respirations
Try to assess the client’s breathing without drawing attention to what is being done. This measure can be taken right after counting the pulse while still holding the client’s wrist.
Count respirations for 1 minute unless respirations are unlabored and regular, in which case the count can be taken for 30 seconds and multiplied by 2. The rise and fall of the chest equals 1 cycle.
The normal rate is between 12 and 20 breaths per minute. Observe rate, excursion, effort, and pattern. Note any use of accessory muscles and whether breathing is silent or noisy. Watch for puffed cheeks, pursed lips, nasal flaring, or asymmetric chest expansion. Changes in the rate, depth, effort, or pattern of a client’s respirations can be early signs of neurologic, pulmonary, or cardiovascular impairment.
Pulse Oximetry
O2 saturation on hemoglobin (SaO2) and pulse rate can be measured simultaneously using pulse oximetry. This is a noninvasive, photoelectric device with a sensor that can be attached to a well-perfused finger, the bridge of the nose, toe, forehead, or ear lobe. Digital readings are less accurate with clients who are anemic, undergoing chemotherapy, or who use fingernail polish or nail acrylics. In such cases, attach the sensor to one of the other accessible body parts.
The sensor probe emits red and infrared light, which is transmitted to the capillaries. When in contact with the skin, the probe measures transmitted light passing through the vascular bed and detects the relative amount of color absorbed by the arterial blood. The SaO2 level is calculated from this information.
The normal SaO2 range at rest and during exercise is 95% to 100%. Referral for medical evaluation is advised when resting saturation levels fall below 90%. The exception to the normal range listed here is for clients with a history of tobacco use and/or COPD. Some individuals with COPD tend to retain carbon dioxide and can become apneic if the oxygen levels are too high. For this reason, SaO2 levels are normally kept lower for this population.
The drive to breathe in a healthy person results from an increase in the arterial carbon dioxide level (PaCO2). In the normal adult, increased CO2 levels stimulate chemoreceptors in the brainstem to increase the respiratory rate. With some chronic lung disorders these central chemoreceptors may become desensitized to PaCO2 changes resulting in a dependence on the peripheral chemoreceptors to detect a fall in arterial oxygen levels (PaO2) to stimulate the respiratory drive.
Too much oxygen delivered as a treatment can depress the respiratory drive in those individuals with COPD who have a dampening of the CO2 drive. Monitoring respiratory rate, level of oxygen administered by nasal canula, and SaO2 levels is very important in this client population.
Some pulmonologists agree that supplemental oxygen levels can be increased during activity without compromising the individual because they will “blow it (carbon dioxide) off” anyway. To our knowledge, there is no evidence yet to support this clinical practice.
Any condition that restricts blood flow (including cold hands) can result in inaccurate SaO2 readings. Relaxation and physiologic quieting techniques can be used to help restore more normal temperatures in the distal extremities. A handheld device such as the PhysioQ26 can be used by the client to improve peripheral circulation. Do not apply a pulse oximetry sensor to an extremity with an automatic blood pressure cuff.27
SaO2 levels can be affected also by positioning because positioning can impact a person’s ability to breathe. Upright sitting in individuals with low muscle tone or kyphosis can cause forward flexion of the thoracic spine compromising oxygen intake. Tilting the person back slightly can open the trunk, ease ventilation, and improve SaO2 levels.28 Using SaO2 levels may be a good way to document outcomes of positioning programs for clients with impaired ventilation.
Other factors affecting pulse oximeter readings can include nail polish and nail coverings, irregular heart rhythms, hyperemia (increased blood flow to the area), motion artifact, pressure on the sensor, electrical interference, and venous congestion.20
In addition to SaO2 levels, assess other vital signs, skin and nail bed color and tissue perfusion, mental status, breath sounds, and respiratory pattern for all clients using pulse oximetry. If the client cannot talk easily whether at rest or while exercising, SaO2 levels are likely to be inadequate.
Blood Pressure
Blood pressure (BP) is the measurement of pressure in an artery at the peak of systole (contraction of the left ventricle) and during diastole (when the heart is at rest after closure of the aortic valve, which prevents blood from flowing back to the heart chambers). The measurement (in mm Hg) is listed as:
BP depends on many factors; the normal range differs slightly with age and varies greatly among individuals (see Table 4-4). Normal systolic BP (SBP) ranges from 100 to 120 mm Hg, and diastolic BP (DBP) ranges from 60 to 80 mm Hg. Highly trained athletes may have much lower values. Target ranges for BP are listed in Table 4-5 and Box 4-7.
TABLE 4-5
Classification of Blood Pressure
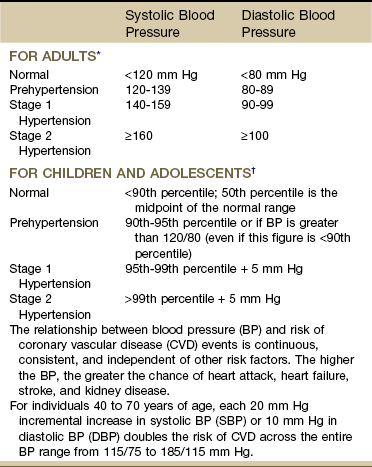
*From The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, NIH Publication No. 03-5233, May 2003. National Heart, Lung, and Blood Institute (NHLBI) www.nhlbi.nih.gov/.
†From National Heart, Lung, and Blood Institute (NHLBI): Fourth Report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents, Pediatrics 114(2):555-576, August 2004.
Assessing Blood Pressure: BP should be taken in the same arm and in the same position (supine or sitting) each time it is measured. The baseline BP values can be recorded on the Family/Personal History form (see Fig. 2-2).
Cuff size is important and requires the bladder width-to-length be at least 1 : 2. The cuff bladder should encircle at least 80% of the arm. BP measurements are overestimated with a cuff that is too small; if a cuff is too small, go to the next size up. Keep in mind that if the cuff is too large, falsely lower BPs may be recorded.29
Do not apply the blood pressure cuff above an intravenous (IV) line where fluids are infusing or an arteriovenous (AV) shunt, on the same side where breast or axillary surgery has been performed, or when the arm or hand have been traumatized or diseased. Until research data supports a change, it is recommended that clients who have undergone axillary node dissection (ALND) avoid having BP measurements taken on the affected side.
Although it is often recommended that anyone who has had bilateral axillary node dissection should have BP measurements taken in the leg, this is not standard clinical practice across the United States.30 Leg pressures can be difficult to assess and inaccurate.
Some oncology staff advise taking BP in the arm with the least amount of nodal dissection. Technique in measuring BP is a key factor in all clients, especially those with ALND (Box 4-8).
A common mistake is to pump the BP cuff up until the systolic measurement is 200 mm Hg and then take too long to lower the pressure or to repeat the measurement a second time without waiting. Repeating the BP without a 1-minute wait time may damage the blood vessel and set up an inflammatory response.31 This poor technique is to be avoided, especially in clients at risk for lymphedema or who already have lymphedema.
Take the BP twice at least a minute apart in both arms. If both measurements are within 5 mm Hg of each other, record this as the resting (baseline) measurement. If not, wait 1 minute and take the BP a third time. Monitor the BP in the arm with the highest measurements.21 Record measurements exactly; do not round numbers up or down as this can result in inaccuracies.32
For clients who have had a mastectomy without ALND (i.e., prophylactic mastectomy), BP can be measured in either arm. These recommendations are to be followed for life.33
Until automated BP devices are improved enough to ensure valid and reliable measurements, the BP response to exercise in all clients should be taken manually with a BP cuff (sphygmomanometer) and a stethoscope.33
It is advised to invest in the purchase of a well-made, reliable stethoscope. Older models with tubing long enough to put the earpieces in your ears and still place the bell in a lab coat pocket should be replaced. Tubing should be no more than 50 to 60 cm (12 to 15 inches) and 4 mm in diameter. Longer and wider tubing can distort transmitted sounds.34
For the student or clinician learning to take vital signs, it may be easier to hear the BP (tapping, Korotkoff) sounds in adults using the left arm because of the closer proximity to the left ventricle. Arm position does make a difference in BP readings. BP measurements are up to 10% higher when the elbow is at a right angle to the body with the elbow flexed at heart level. The preferred position is seated with the arms parallel and extended in a forward direction (if supine, then parallel to the body).35
It is more accurate to evaluate consecutive BP readings over time rather than using an isolated measurement for reporting BP abnormalities. BP also should be correlated with any related diet or medication.
Before reporting abnormal BP readings, measure both sides for comparison, re-measure both sides, and have another health professional check the readings. Correlate BP measurements with other vital signs, and screen for associated signs and symptoms such as pallor, fatigue, perspiration, and/or palpitations. A persistent rise or fall in BP requires medical attention and possible intervention.
Pulse Pressure: The difference between the systolic and diastolic pressure readings (SBP − DBP) is called pulse pressure normally around 40 mm Hg. Pulse pressure is an index of vascular aging (i.e., loss of arterial compliance and indication of how stiff the arteries are). A widened resting pulse pressure often results from stiffening of the aorta secondary to atherosclerosis. Resting pulse pressure consistently greater than 60 to 80 mm Hg is a yellow (caution) flag and is a risk factor for new onset of atrial fibrillation.36
Widening of the pulse pressure is linked to a significantly higher risk of stroke and heart failure after the sixth decade. Some BP medications increase resting pulse pressure width by lowering diastolic pressure more than systolic while others (e.g., angiotensin-converting enzyme [ACE] inhibitors) can lower pulse pressure.37
Narrowing of the resting pulse pressure (usually by a drop in SBP as the DBP rises) can suggest congestive heart failure (CHF) or a significant blood loss such as occurs in hypovolemic shock. A high pulse pressure accompanied by bradycardia is a sign of increased intracranial pressure and requires immediate medical evaluation.
In a normal, healthy adult, the pulse pressure generally increases in direct proportion to the intensity of exercise as the SBP increases and DBP stays about the same.38 A difference of more than 80 to 100 mm Hg taken during or right after exercise should be evaluated carefully. In a healthy adult, pulse pressure will return to normal within 3 to 10 minutes following moderate exercise.
The key is to watch for pulse pressures that are not accommodating during exercise. Expect to see the systolic rise slightly while diastolic stays the same. If diastolic drops while systolic rises or if the pulse width exceeds 100 mm Hg, further assessment and evaluation is needed. Depending on all other parameters (e.g., general health of the client, past medical history, medications, concomitant associated signs and symptoms), the therapist may monitor pulse pressures over a few sessions and look for a pattern (or lack of pattern) to report if/when generating a medical consult.39
Variations in Blood Pressure: There can be some normal variation in SBP from side to side (right extremity compared to left extremity). This is usually no more than 5 to 10 mm Hg DBP or SBP (arms) and 10 to 40 mm Hg SBP (legs). A difference of 10 mm Hg or more in either systolic or diastolic measurements from one extremity to the other may be an indication of vascular problems (look for associated symptoms; in the upper extremity test for thoracic outlet syndrome).
Normally the SBP in the legs is 10% to 20% higher than the brachial artery pressure in the arms. BP readings that are lower in the legs as compared with the arms are considered abnormal and should prompt a medical referral for assessment of peripheral vascular disease.33
With a change in position (supine to sitting), the normal fluctuation of BP and heart rate increases slightly (about 5 mm Hg for systolic and diastolic pressures and 5 to 10 bpm in heart rate).
Systolic pressure increases with age and with exertion in a linear progression. If systolic pressure does not rise as workload increases, or if this pressure falls, it may be an indication that the functional reserve capacity of the heart has been exceeded.
The deconditioned, menopausal woman with coronary heart disease (CHD) requires careful monitoring, especially in the presence of a personal or family history of heart disease and myocardial infarct (personal or family) or sudden death in a family member.
On the other hand, women of reproductive age taking birth control pills may be at increased risk for hypertension, heart attack, or stroke. The risk of a cardiovascular event is very low with today’s low-dose oral contraceptives. However, smoking, hypertension, obesity, undiagnosed cardiac anomalies, and diabetes are factors that increase a woman’s risk for cardiovascular events. Any woman using oral contraceptives who presents with consistently elevated BP values must be advised to see her physician for close monitoring and follow-up.40,41
The left ventricle becomes less elastic and more noncompliant as we age. The same amount of blood still fills the ventricle, but the pumping mechanism is less effective. The body compensates to maintain homeostasis by increasing the blood pressure. BP values greater than 120 mm Hg (systolic) and more than 80 mm Hg (diastolic) are treated with lifestyle modifications first then medication.
Blood Pressure Changes with Exercise: As mentioned, the SBP increases with increasing levels of activity and exercise in a linear fashion. In a healthy adult under conditions of minimal to moderate exercise, look for normal change (increase) in SBP of 20 mm Hg or more.
The American College of Sports Medicine (ACSM) suggests the normal SBP response to incremental exercise is a progressive rise, typically 10 mm + 2 mm Hg for each metabolic equivalent (MET) where 1 MET = 3.5 mL O2/kg/min. Expect to see a 40 to 50 mm change in SBP with intense exercise (again, this is in the healthy adult). These values are less likely with individuals taking BP medications, anyone with a significant history of heart disease, and well-conditioned athletes.
Diastolic should be the same side to side with less than 10 mm Hg difference observed. DBP generally remains the same or decreases slightly during progressive exercise.38
In an exercise-testing situation, the ACSM recommends stopping the test if the SBP exceeds 260 mm Hg.38 In a clinical setting without the benefit of cardiac monitoring, exercise or activity should be reduced or stopped if the systolic pressure exceeds 200 mm Hg.
This is a general guideline that can be changed according to the client’s age, general health, use of cardiac medications, and other risk factors. DBP increases during upper extremity exercise or isometric exercise involving any muscle group. Activity or exercise should be monitored closely, decreased, or halted if the diastolic pressure exceeds 100 mm Hg.
This is a general (conservative) guideline when exercising a client without the benefit of cardiac testing (e.g., electrocardiogram [ECG]). This stop-point is based on the ACSM guideline to stop exercise testing at 115 mm Hg DBP. Other sources suggest activity should be decreased or stopped if the DBP exceeds 130 mm Hg.42
Other warning signs to moderate or stop exercising include the onset of angina, dyspnea, and heart palpitations. Monitor the client for other signs and symptoms such as fever, dizziness, nausea/vomiting, pallor, extreme diaphoresis, muscular cramping or weakness, and incoordination. Always honor the client’s desire to slow down or stop.
Hypertension (See Further Discussion on Hypertension in Chapter 6): In recent years, an unexpected increase in illness and death caused by hypertension has prompted the National Institutes of Health (NIH) to issue new guidelines for more effective BP control. More than one in four Americans has high blood pressure, increasing their risk for heart and kidney disease and stroke.43
In adults hypertension is a systolic pressure above 140 mm Hg or a diastolic pressure above 90 mm Hg. Consistent BP measurements between 120 and 139 (systolic) and between 80 and 89 diastolic is classified as pre-hypertensive. The overall goal of treating clients with hypertension is to prevent morbidity and mortality associated with high blood pressure. The specific objective is to achieve and maintain arterial blood pressure below 120/80 mm Hg, if possible (Box 4-9).34
The older adult taking nonsteroidal antiinflammatory drugs (NSAIDs) is at risk for increased BP because these drugs are potent renal vasoconstrictors. Monitor BP carefully in these clients and look for sacral and lower extremity edema. Document and report these findings to the physician. Use the risk factor analysis for NSAIDs presented in Chapter 2 (see Box 2-13 and Table 2-6).
Always beware of masked hypertension (normal in the clinic but periodically high at home) and white-coat hypertension, a clinical condition in which the client has elevated BP levels when measured in a clinic setting by a health care professional. In such cases, BP measurements are consistently normal outside of a clinical setting.
Masked hypertension may affect up to 10% of adults; white-coat hypertension occurs in 15 to 20% of adults with stage I hypertension.44 These types of hypertension are more common in older adults. Antihypertensive treatment for white coat hypertension may reduce office BP but may not affect ambulatory BP. The number of adults who develop sustained high BPs is much higher among those who have masked or white-coat hypertension.44
At-home BP measurements can help identify adults with masked hypertension, white-coat hypertension, ambulatory hypertension, and individuals who do not experience the usual nocturnal drop in BP (decrease of 15 mm Hg), which is a risk factor for cardiovascular events.45 Excessive morning BP surge is a predictor of stroke in older adults with known hypertension and is also a red-flag sign.46 Medical referral is indicated in any of these situations.
Hypertension in African Americans: Nearly 40% of African Americans suffer from heart disease and 13% have diabetes. Hypertension contributes to these conditions or makes them worse. African Americans are significantly more likely to die of high BP than the general public because current treatment strategies have been unsuccessful.47,48
Guidelines for treating high blood pressure in African Americans have been issued by the International Society on Hypertension in Blacks (ISHIB).49 The ISHIB recommends a blood pressure target of less than 130/80 mm Hg for African Americans with BP screening for all African-American adults and early prevention for anyone in the pre-hypertensive range. Aggressive treatment for hypertension is advised using drug combinations.48
The therapist can incorporate blood pressure screening into any evaluation for clients with ethnic risk factors. Any client of any ethnic background with risk factors for hypertension should also be screened (see Table 6-6).
Hypertension in Hispanics: The Hispanic population in the United States is expected to be reported by the 2010 census as the largest minority group in the nation. Research on hypertension among Hispanics has shown that their incidence of high BP is greater than that of whites and Asians and less than that of blacks. More Hispanics than whites have undiagnosed hypertension and are generally less knowledgeable in heart disease prevention. Factors that contribute to elevated BP in Hispanics include high rates of obesity and diabetes, as well as a genetic predisposition and low socioeconomic status.50 With equal access to medical care and medication, Hispanic men and women have as good or greater chance as non-Hispanics of controlling their high BP.51
Hypertension in Children and Adolescents52: Up to 3% of children under age 18 also have hypertension. New guidelines for children have been published by the National Heart, Lung, and Blood Institute (NHLBI) (see Table 4-5). Tables with BP levels for boys and girls by age and height percentile are available.52
The updated BP tables for children and adolescents are based on recently revised child height percentiles. Any child with readings above the 95th percentile for gender, age, and height on three separate occasions is considered to have hypertension. The 50th percentile has been added to the tables to provide the clinician with the BP level at the midpoint of the normal range.
Under the new guidelines, children whose readings fall between the 90th and 95th percentile are now considered to have pre-hypertension. Earlier guidelines called this category “high normal.”
The long-term health risks for hypertensive children and adolescents can be substantial; therefore it is important that elevated BP is recognized early and measures taken to reduce risks and optimize health outcomes.52
Children ages 3 to 18 seen in any medical setting should have the BP measured at least once during each health care episode. The preferred method is auscultation with a BP cuff and stethoscope. Correct measurement requires a cuff that is appropriate to the size of the child’s upper arm.
The right arm is preferred with children for comparison with standard tables and in the possible event there is a coarctation of the aorta (see Fig. 6-6), which can lead to a false low reading in the left arm.53
Preparation of the child can affect the BP level as much as technique. The child should be seated with feet and back supported. The right arm should be supported parallel to the floor with the cubital fossa at heart level.54,55 Children can be affected by white-coat hypertension as much as adults. Follow the same guidelines for adults as presented in Box 4-8.
Hypotension: Hypotension is a systolic pressure below 90 mm Hg or a diastolic pressure below 60 mm Hg. A BP level that is borderline low for one person may be normal for another. When the BP is too low, there is inadequate blood flow to the heart, brain, and other vital organs.
The most important factor in hypotension is how the BP changes from the normal condition. Most normal BPs are in the range of 90/60 mm Hg to 120/80 mm Hg, but a significant change, even as little as 20 mm Hg, can cause problems for some people.
Lower standing SBP (less than 140 mm Hg) even within the normotensive range is an independent predictor of loss of balance and falls in adults over age 65.56 DBP does not appear to be related to falls. Older adult women with lower standing SBP and a history of falls are at greatest risk. The therapist has an important role in educating clients with these risk factors in preventing falls and related accidents. See discussion in Chapter 2 related to taking a history of falls.
In older adults a decrease in BP may be an early warning sign of Alzheimer’s disease. DBP below 70 or declines in systolic pressure equal to or greater than 15 mm Hg over a period of 3 years raises the risk of dementia in adults 75 or older. For each 10-point drop in pressure, the risk of dementia increases by 20%.57,58
It is unclear if the steady drop in BP during the 3 years before a dementia diagnosis is a cause or effect of dementia as reduced blood flow to the brain accelerates the development of dementia. Perhaps brain cell degeneration characteristic of dementia damages parts of the brain that regulate BP.57
Postural Orthostatic Hypotension: A common cause of low BP is orthostatic hypotension (OH), defined as a sudden drop in BP when changing positions, usually moving from supine to an upright position.
Physiologic responses of the sympathetic nervous system decline with aging putting them at greater risk for OH. Older adults are prone to falls from a combination of OH and antihypertensive medications. Volume depletion and autonomic dysfunction are the most common causes of OH (see Table 2-5).
Postural OH is more accurately defined as a decrease in SBP of at least 20 mm Hg or decrease in diastolic pressure of at least 10 mm Hg and a 10% to 20% increase in pulse rate. Changes must be noted in both the BP and the pulse rate with change in position (supine to sitting, sitting to standing) (Box 4-10 and Case Example 4-1).45
The client should lie supine 2 to 3 minutes prior to BP and pulse check. At least a 1-minute wait is recommended after each subsequent position change before taking the BP and pulse. Standing postural orthostatic hypotension is measured after 3 to 5 minutes of quiet standing. Food ingestion, time of day, age, and hydration can impact this form of hypotension, as can a history of Parkinsonism, diabetes, or multiple myeloma.43
Throughout the procedure assess the client for signs and symptoms of hypotension, including dizziness, lightheadedness, pallor, diaphoresis, or syncope (or arrhythmias if using a cardiac monitor). Assist the client to a seated or supine position if any of these symptoms develop and report the results. Do not test the client in the standing position if signs and symptoms of hypotension occur while sitting.
Gravitational effects on the circulatory system can cause a 10 mm Hg drop in SBP when a person changes position from supine to sitting to standing. This drop usually occurs without symptoms as the body quickly compensates to ensure there is no reduction in cardiac output.
In clients on prolonged bed rest or on antihypertensive drug therapy, there may be either no reflexive increase in heart rate or a sluggish vasomotor response. These clients may experience larger drops in BP and often experience lightheadedness.
Other clients at risk for postural OH include those who have just donated blood, anyone with autonomic nervous system disease or dysfunction, and postoperative patients. Other risk factors for OH in aging adults include hypovolemia associated with dehydration and the overuse of diuretics, anticholinergic medications, antiemetics, and various over-the-counter (OTC) cough/cold preparations.
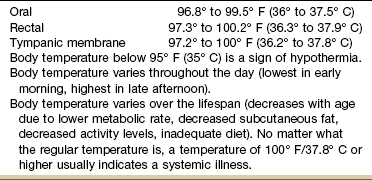
Core Body Temperature
Normal body temperature is not a specific number but a range of values that depends on factors such as the time of day, age, medical status, medication use, activity level, or presence of infection. Oral body temperature ranges from 36° to 37.5° C (96.8° to 99.5° F), with an average of 37° C (98.6° F) (Table 4-6). Hypothermic core temperature is defined as less than 35° C (95° F). Hyperthermia is defined as a temperature greater than 38° C (100.4° F).
Older adults (over age 65) are less likely to have a fever even in the presence of severe infection, so the predictive value of taking the body temperature is less. Due to age-related changes in the thermoregulatory system, they are also more likely to develop hypothermia than young adults. There is a tendency among the aging population to develop an increase in temperature on hospital admission or in response to any change in homeostasis. However, some persons with infectious disease remain afebrile, especially the immunocompromised and those with chronic renal disease, alcoholics, and older adults. A low-grade fever can be an early sign of life-threatening infections (most commonly pneumonia, urinary tract infection). Unexplained fever in adolescents may be a manifestation of drug abuse or endocarditis.
Postoperative fever is common and may be from an infectious or noninfectious cause. Medical evaluation is needed to make this determination. In the home health setting, wound infection, abscess formation, or peritonitis may appear as a hectic fever pattern 3 to 4 days postoperatively with increases and declines of body temperature but no return to baseline (normal). Such a situation would warrant telephone consultation with the physician’s office nurse.
Any client who has back, shoulder, hip, sacroiliac, or groin pain of unknown cause must have a temperature reading taken. Temperature should also be assessed for any client who has constitutional symptoms (see Box 1-3), especially “sweats” (gradual increase followed by a sudden drop in body temperature), pain, or symptoms of unknown etiologic basis and for clients who have not been medically screened by a physician. Ask about the presence of other signs and symptoms of infection.
When measuring body temperature, the therapist should ask if the person’s normal temperature differs from 37° C (98.6° F). A persistent elevation of temperature over time is a red-flag sign; a single measurement may not be sufficient to cause concern. Any measurement outside of normal for that individual should be rechecked.
It is also important to ask whether the client has taken aspirin (or other NSAIDs) or acetaminophen (Tylenol) to reduce the fever, which might mask an underlying problem. Clients taking dopamine blockers, such as Thorazine, Mellaril, or the less commonly used Navane for schizophrenia, have a lowered “normal” temperature (around 96° F/35.6° C). Anyone who is chronically immunosuppressed (such as an organ transplant recipient, a person being treated with chemotherapy, and any older adult) may have an infection without elevation of temperature.
When using a tympanic membrane (ear) thermometer, perform a gentle ear tug to straighten the ear canal. In a child, pull the ear straight back; in an adult, pull it slightly upward and backward. While holding the ear in this position, use a small rotation movement to insert the probe gently and slowly.59
The probe must penetrate at least one-third of the external ear canal to prevent air temperature from affecting the reading. Aim the probe toward the tympanic membrane where it will indirectly measure core body temperature by taking infrared temperature readings of the tympanic membrane (eardrum).59
Temperatures can vary from side to side, so record which ear was used and try to use the same ear each time the temperature is recorded. For the client with hearing aid(s), take the temperature in the ear without an aid. Or, if hearing aids are present in both ears, remove one hearing aid and wait 20 minutes before measuring that side. The presence of excessive earwax will prevent an accurate reading.
There are some additional concerns reported in the literature about the accuracy of tympanic thermometers with evidence of significant variability possibly related to the condition of the censor, presence of ear wax, placement in the ear canal, operator error, and maintenance of the equipment.60-62 Such concerns may be more important in critical care ICUs compared with outpatient screening, but no studies comparing these two populations have been published.
Newer handheld digital forehead thermometers are noninvasive and are quick and easy to use. The forehead plastic temperature strip (forehead thermometer, fever strip) and the pacifier thermometer for children are not the most reliable methods to take a temperature.
The therapist should use discretionary caution with any client who has a fever. Exercise with a fever stresses the cardiopulmonary system, which may be further complicated by dehydration. Severe dehydration can occur from vomiting, diarrhea, medications (e.g., diuretics), or heat exhaustion.
Clients at greatest risk of dehydration include postoperative patients, aging adults, and athletes. Severe fluid volume deficit can cause vascular collapse and shock. Clients at risk of shock include burn or trauma patients, clients in anaphylactic shock or diabetic ketoacidosis, and individuals experiencing severe blood loss.
Walking Speed: The Sixth Vital Sign
Walking speed is used by some as a general indicator of function63 and as such, a reflection of many variables such as health status, motor control, muscle strength, and endurance to name only a few. It is a reliable, valid, and sensitive measure of functional ability with additional predictive value in assessing future health status, functional decline, potential for hospitalization, and even mortality.64
The test is conducted using a timed 10-meter walk test on a 20-meter long straight path. Complete descriptions of the test and expected results are available.63-66 As a screening tool, walking speed may not indicate the presence of systemic pathology, but as specialists in human movement and function, the therapist can use it as a practical and predictive “vital sign” of general health that can be used to monitor change (improvement or decline) in health and function.
Techniques of Physical Examination
There are four simple techniques used in the medical physical examination: inspection, palpation, percussion, and auscultation. Percussion and some auscultation techniques require advanced clinical skill and are beyond the scope of a screening examination.
Throughout any screening examination the therapist also assesses function of the integument, musculoskeletal, neuromuscular, and cardiopulmonary systems. Assessment techniques are relatively simple; it is using the finding that is more difficult. The saying, “What one knows, one sees” underscores the idea that knowledge of physical assessment techniques and experience in performing these are extremely important and come from practice.
Inspection
Good lighting and good exposure are essential. Always compare one side to the other. Assess for abnormalities in all of the following:
| Texture | Tenderness |
| Size | Shape, contour, symmetry |
| Position, alignment | Mobility or movement |
| Color | Location |
The therapist should try to follow the same pattern every time to decrease the chances of missing an assessment parameter and to increase accuracy and thoroughness.
Palpation
Palpation is used to discriminate between textures, dimensions, consistencies, and temperature. It is used to define things that are inspected and to reveal things that cannot be inspected. Textures are best detected using the fingertips, whereas dimension or contours are detected using several fingers, the entire hand, or both hands, depending on the area being examined.
Inspection and palpation are often performed at the same time; be sure and look at the client and not at your hands. Muscle tension interferes with palpation so the client must be positioned and draped appropriately in a room with adequate lighting and temperature.
Assess skin temperature with both hands at the same time. The back of the therapist’s hands sense temperature best because of the thin layer of skin. Use the palm or heel of the hand to assess for vibration. The finger pads are best to assess texture, size, shape, position, pulsation, consistency, and turgor. Heavy or continued pressure dulls the examiner’s palpatory skill and sensation.
Light palpation is used first, looking for areas of tenderness followed by deep palpation to examine organs or look for masses and elicit deep pain. Light palpation (skin is depressed up to  to
to  inch) is also used to assess texture, temperature, moisture, pulsations, vibrations, and superficial lesions. Deep palpation is used for assessing abdominal structures. During deep palpation, enough pressure is used to depress the skin up to 1 inch; applying too much pressure decreases sensation.
inch) is also used to assess texture, temperature, moisture, pulsations, vibrations, and superficial lesions. Deep palpation is used for assessing abdominal structures. During deep palpation, enough pressure is used to depress the skin up to 1 inch; applying too much pressure decreases sensation.
Tender or painful areas are assessed last while carefully observing the client’s face for signs of discomfort.
Percussion
Percussion (tapping) is used to determine the size, shape, and density of tissue using sound created by vibration. Percussion can also detect the presence of fluid or air in a body cavity such as the abdominal cavity. Most percussive techniques are beyond the scope of a screening examination and are not discussed in detail.
Percussion can be done directly over the client’s skin using the fingertip of the examiner’s index finger. Indirect percussion is performed by placing the middle finger of the examiner’s nondominant hand firmly against the client’s skin then striking above or below the interphalangeal joint with the pad of the middle finger of the dominant hand. The palm and fingers stay off the skin during indirect percussion. Blunt percussion using the ulnar surface of the hand or fist to strike the body surface (directly or indirectly) detects pain from infection or inflammation (see Fig. 4-54).
The examiner must be careful not to dampen the sound by dull percussing (sharp percussion is needed), holding a finger too loosely on the body surface, or resting the hand on the body surface. Percussive sounds lie on a continuum from tympany to flat based on density of tissue.
Auscultation
Some sounds of the body can be heard with the unaided ear; others must be heard by auscultation using a stethoscope. The bell side of the stethoscope is used to listen to low-pitched sounds such as heart murmurs and BP (although the diaphragm can also be used for BP).
Pressing too hard on the skin can obliterate sounds. The diaphragm side of the stethoscope is used to listen to high-pitched sounds such as normal heart sounds, bowel sounds, and friction rubs. Avoid holding either side of the stethoscope with the thumb to avoid hearing your own pulse.
Auscultation usually follows inspection, palpation, and percussion (when percussion is performed). The one exception is during examination of the abdomen, which should be assessed in this order: inspection, auscultation, percussion, then palpation as percussion and palpation can affect findings on auscultation.
Besides measuring BP, auscultation can be used to listen for breath sounds, heart sounds, bowel sounds, and abnormal sounds in the blood vessels called bruits. Bruits are abnormal blowing or swishing sounds heard on auscultation as blood travels through narrowed or obstructed arteries such as the aorta or renal, iliac, or femoral arteries. Bruits with both systolic and diastolic components suggest the turbulent blood flow of partial arterial occlusion possible with aneurysm or vessel constriction. All large arteries in the neck, abdomen, and limbs can be examined for bruits.
A medical assessment (e.g., physician, nurse, physician assistant) may routinely include auscultation of the temporal and carotid arteries and jugular vein in the head and neck, as well as vascular sounds in the abdomen (e.g., aorta, iliac, femoral, and renal arteries). The therapist is more likely to assess for bruits when the client’s history (e.g., age over 65, history of coronary artery disease), clinical presentation (e.g., neck, back, abdominal, or flank pain), and associated signs and symptoms (e.g., syncopal episodes, signs and symptoms of peripheral vascular disease) warrant additional physical assessment.
The results from inspection, percussion (when appropriate), and palpation should always be correlated with the client’s history, risk factors, clinical presentation, and any associated signs and symptoms before making the decision regarding medical referral.
Integumentary Screening Examination
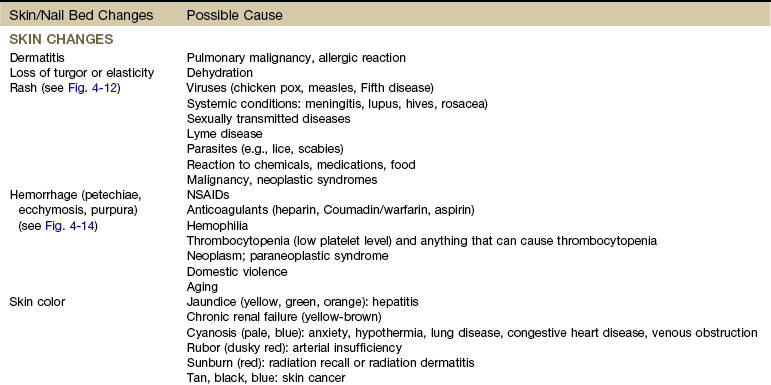
When screening for systemic disease, the therapist must increase attention to what is observable on the outside, primarily the skin and nail beds. Changes in the skin and nail beds may be the first sign of inflammatory, infectious, and immunologic disorders and can occur with involvement of a variety of organs.
For example, dermatitis can occur 6 to 8 weeks before primary signs and symptoms of pulmonary malignancy develop. Clubbing of the fingers can occur quickly in various acute illnesses and conditions. Skin, hair, and nail bed changes are common with endocrine disorders. Renal disease, rheumatic disorders, and autoimmune diseases are all accompanied by skin and nail bed changes in many physical therapy clients.
When assessing skin conditions of any kind, even benign lesions such as psoriasis (Fig. 4-2) or eczema, the therapist always should use standard precautions because any disruption of the skin increases the risk of infection. Chronic skin conditions of this type may have new, more effective treatment available. In such cases, the therapist may be able to guide the uninformed client to obtain updated medical treatment.

Fig. 4-2 Psoriasis. A common chronic skin disorder characterized by red patches covered by thick, dry silvery scales that are the result of excessive buildup of epithelial cells. Lesions often come and go and can be anywhere on the body but are most common on extensor surfaces, bony prominences, scalp, ears, and genitals. Arthritis of the small joints of the hands often accompanies the skin disease (psoriatic arthritis). (From Lookingbill DP, Marks JG: Principles of dermatology, ed 3, Philadelphia, 2000, WB Saunders.)
Consider all findings in relation to the client’s age, ethnicity, occupation, and general health. The presence of skin lesions may point to a problem with the integumentary system or may be an integumentary response to a systemic problem.
For example, pruritus is the most common manifestation of dermatologic disease but is also a symptom of underlying systemic disease in up to 50% of individuals with generalized itching.67 In both situations, skin rash is a common accompanying sign. The most common visceral system causing pruritus is the hepatic system. Look for other associated signs and symptoms of liver or gallbladder impairment such as liver flap (asterixis), carpal tunnel syndrome, liver palms (palmar erythema), and spider angiomas (see Fig. 9-3).
At the same time, be aware that pruritus, or itch, is very common among aging adults. The natural attrition of glands that moisturize the skin combined with the effects of sun exposure, medications, excessive bathing, and harsh soaps can result in dry, irritable skin.68
Some clients may describe formication, also referred to as a tactile hallucination, the sensation of ants crawling on the skin, sometimes described as an itching, prickling, or crawling feeling. The most common cause is menopause, but chronic drug or alcohol use can also cause formication. Some schizophrenics also experience formication. As one of the many side effects of crystal methamphetamine addiction, formication is also referred to as speed bumps, meth sores, and crank bugs.
The therapist may see scratch marks or even broken skin where the sufferer has scratched violently. Open, red (often bleeding) sores appear most commonly on the face and arms but can be anywhere on the body. These lesions can become inflamed, swollen, and pus-filled in the presence of a Staphylococcus infection. Left untreated, pathogens can enter the bloodstream, causing dangerous sepsis or deeper abscess. There is no cure, but medical evaluation is needed; topical treatment and cryotherapy can help, and antibiotic treatment is needed when there is infection.
New onset of skin lesions, especially in children, should be medically evaluated (Fig. 4-3). Many conditions in adults and children can be treated effectively; some, but not all, can be cured.

Fig. 4-3 Tinea corporis or ringworm of the body presents anywhere on the body in adult or children but more commonly on the chest, abdomen, back of arms, face, and dorsum of the feet. The circular lesions with clear centers can form singly or in clusters and represent a fungal infection that is both contagious and treatable. Tinea pedis (not shown), also known as ringworm of the feet or “athlete’s foot” occurs most often between the toes, but also along the sides of the feet and the soles (easily spread and treatable). (From Hurwitz S: Clinical pediatric dermatology: a textbook of skin disorders of childhood and adolescence, ed 2, Philadelphia, 1993, WB Saunders.)
Skin Assessment
With the possible exception of a dermatologist, the therapist sees more skin than anyone else in the health care system. Clients are more likely to point out skin lesions or ask the therapist about lumps and bumps. It is important to have a working knowledge of benign versus pathologic skin lesions and know when to refer appropriately.
The hands, arms, feet, and legs can be assessed throughout the physical therapy examination for changes in texture, color, temperature, clubbing, circulation including capillary filling, and edema (Box 4-11). Abnormal texture changes include shiny, stiff, coarse, dry, or scaly skin.
Skin mobility and turgor are affected by the fluid status of the client. Dehydration and aging reduce skin turgor (Fig. 4-4), and edema decreases skin mobility. The therapist should be aware of medications that cause skin to become sensitive to sunlight. The most commonly prescribed medications linked with photosensitivity are listed in Box 4-12.

Fig. 4-4 To check skin turgor (elasticity or resiliency), gently pinch the skin between your thumb and forefinger, lifting it up slightly, then release. Skin turgor can be tested on the forehead or sternum, beneath the clavicle (A), and over the extensor surface of the arm (B) or hand. Expect to see the skin lift up easily and return to place quickly. The test is positive for decreased turgor (often caused by dehydration) when the pinched skin remains lifted 5 or more seconds after release and returns to normal very slowly. (A from Seidel HM: Mosby’s guide to physical examination, ed 7, St. Louis, 2011, Mosby. B from Potter P, Perry A: Basic nursing: essentials for practice, ed 6, St. Louis, 2007, Mosby.)
Chronically ill or hospitalized patients should be examined frequently for signs of skin breakdown. Check all pressure points, including the ears, sacrum, scapulae, shoulders, area over the greater trochanters, heels, malleoli, and the back of the head. Document staging of any pressure ulcers (Table 4-7).
TABLE 4-7
Staging of Pressure Ulcers*
| Pressure ulcers have been defined by the National Pressure Ulcer Advisory Panel (NPUAP) in conjunction with the European Pressure Ulcer Advisory Panel (EPUAP) as localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure or pressure in combination with shear. |
| Stage | Description |
| Stage I | Skin changes observable (increased or decreased temperature, tissue consistency), sensation (pain, itching). |
| Stage II | Epidermis and dermis layers are damaged (partial-thickness); ulcer is superficial and presents as an abrasion, blister, or shallow crater. |
| Stage III | Damage through to subcutaneous tissue (full-thickness skin loss); does not extend through fascia; appears as a deep crater; this is a “never event” (i.e., should never happen). |
| Stage IV | Involvement of muscle, bone, tendon, joint capsule or other supporting structures (full-thickness tissue loss); this is also a “never event” (i.e., should never happen). |
*Staging does not indicate the process of wound healing. The NPUAP also provides the Pressure Ulcer Scale for Healing (PUSH Tool) as a quick, reliable tool to monitor the change in pressure ulcer status over time. Updated staging system available on-line at: http://www.npuap.org/push3-0.html.
From U.S. Department of Health and Human Services: Pressure ulcers in adults: prediction and prevention. Clinical practice guideline no. 3. AHCPR publication no. 92-0047, Rockville, Maryland, 1992, DHHS; European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory Panel. Prevention and Treatment of Pressure Ulcers: Clinical Practice Guidelines. Washington, DC, 2009, NPUAP.
The staging system developed by National Pressure Ulcer Advisory Panel (NPUAP) is an anatomic description of tissue destruction or wound depth designed for use only with pressure ulcers or wounds created by pressure. While it is essential to have this information, it is also very important to document other wound characteristics, such as size, drainage, and granulation tissue, to make the wound assessment complete.
Coordinate with nursing staff to remove prostheses, restraints, and dressings to look beneath them. Anyone with an IV line, catheter, or other insertion sites must be examined for signs of infiltration (e.g., pus, erythema), phlebitis, and tape burns.
Observe for signs of edema. Edema is an accumulation of fluid in the interstitial spaces. Pitting edema in which pressing a finger into the skin leaves an indentation often indicates a chronic condition (e.g., chronic kidney failure, liver failure, CHF) but can occur acutely as well (e.g., face) (Fig. 4-5). The location of edema helps identify the potential cause. Bilateral edema of the legs may be seen in clients with heart failure or with chronic venous insufficiency.

Fig. 4-5 Pitting edema in a patient with cardiac failure. A depression (“pit”) remains in the edema for some minutes after firm fingertip pressure is applied. (From Forbes CD, Jackson WD. Color atlas and text of clinical medicine, ed 3, London, 2003, Mosby.)
Abdominal and leg edema can be seen in clients with heart disease, cirrhosis of the liver (or other liver impairment), and protein malnutrition. Edema may also be noted in dependent areas, such as the sacrum, when a person is confined to bed. Localized edema in one extremity may be the result of venous obstruction (thrombosis) or lymphatic blockage of the extremity (lymphedema).
Change in Skin Temperature
Skin temperature can be an indication of vascular supply. A handheld, noninvasive, infrared thermometer can be used to measure skin surface temperature. The most common use of this device is for temperature observation and comparison of both feet in individuals with diabetes for the purpose of identifying increased skin temperatures, intended as an early warning of inflammation, impending infection, and possible foot ulceration. Temperature differences of four or more degrees between the right and left foot is a predictive risk factor for foot ulcers; self-monitoring has been shown to reduce the risk of ulceration in high-risk individuals.69-72
Other signs and symptoms of vascular changes of an affected extremity may include paresthesia, muscle fatigue and discomfort, or cyanosis with numbness, pain, and loss of hair from a reduced blood supply (Box 4-13).
Change in Skin Color
Capillary filling of the fingers and toes is an indicator of peripheral circulation. Perform a capillary refill test by pressing down on the nail bed and releasing. Observe first for blanching (whitening) followed by return of color within 3 seconds after release of pressure (normal response).
Skin color changes can occur with a variety of illnesses and systemic conditions. Clients may notice a change in their skin color before anyone else does, so be sure and ask about it. Look for pallor; increased or decreased pigmentation; yellow, green, or red skin color; and cyanosis.
Color changes are often observed first in the fingernails, lips, mucous membranes, conjunctiva of the eye, and palms and soles of dark-skinned people.
Skin changes associated with impairment of the hepatic system include jaundice, pallor, and orange or green skin.
In some situations, jaundice may be the first and only manifestation of disease. It is first noticeable in the sclera of the eye as a yellow hue when bilirubin level reaches 2 to 3 mg/dL. Dark-skinned persons may have a normal yellow color to the outer sclera. Jaundice involves the whole sclera up to the iris.
When the bilirubin level reaches 5 to 6 mg/dL, the skin becomes yellow. Other skin and nail bed changes associated with liver disease include palmar erythema (see Fig. 9-5), spider angiomas (see Figs. 9-3 and 9-4), and nails of Terry (see Fig. 9-6; see further discussion in Chapter 9).
A bluish cast to skin color can occur with cyanosis when oxygen levels are reduced in the arterial blood (central cyanosis) or when blood is oxygenated normally but blood flow is decreased and slow (peripheral cyanosis). Cyanosis is first observed in the hands and feet, lips, and nose as a pale blue change in color. The client may report numbness or tingling in these areas.
Central cyanosis is caused by advanced lung disease, congestive heart disease, and abnormal hemoglobin. Peripheral cyanosis occurs with CHF (decreased blood flow), venous obstruction, anxiety, and cold environment.
Rubor (dusky redness) is a common finding in peripheral vascular disease as a result of arterial insufficiency. When the legs are raised above the level of the heart, pallor of the feet and lower legs develops quickly (usually within 1 minute). When the same client sits up and dangles the feet down, the skin returns to a pink color quickly (usually in about 10 to 15 seconds). A minute later the pallor is replaced by rubor, usually accompanied by pain and diminished pulses. Skin is cool to the touch and trophic changes may be seen (e.g., hair loss over the foot and toes, thick nails, thin skin).
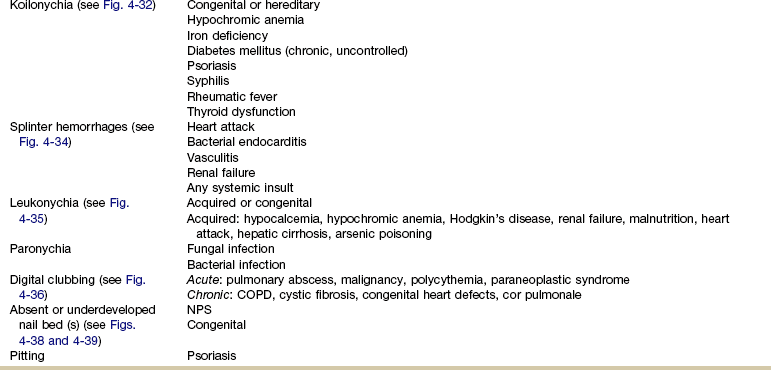
Diffuse hyperpigmentation can occur with Addison’s disease, sarcoidosis, pregnancy, leukemia, hemochromatosis, celiac sprue (malabsorption syndrome), scleroderma, and chronic renal failure.
This presents as patchy tan to brown spots most often but may occur as yellow-brown or yellow to tan with scleroderma and renal failure. Any area of the body can be affected, although pigmentation changes in pregnancy tend to affect just the face (melasma or the mask of pregnancy).
Assessing Dark Skin
Clients with dark skin may require a slightly different approach to skin assessment than the Caucasian population. Observe for any obvious changes in the palms of the hands and soles of the feet; tongue, lips, and gums in the mouth; and in the sclera and conjunctiva of the eyes.
Pallor may present as a yellow or ashen-gray due to an absence of the normally present underlying red tones in the skin. The palms and the soles show changes more clearly than the skin. Skin rashes may present as a change in skin texture so palpating for changes is important. Edema can be palpated as “tightness” and darker skin may appear lighter. Inflammation may be perceived as a change in skin temperature instead of redness or erythema of the skin.
Jaundice may appear first in the sclera but can be confused for the normal yellow pigmentation of dark-skinned clients. Be aware that the normal oral mucosa (gums, borders of the tongue, and lining of the cheeks) of dark-skinned individuals may appear freckled.
Petechiae are easier to see when present over areas of skin with lighter pigmentation such as the abdomen, gluteal area, and volar aspect of the forearm. Petechiae and ecchymosis (bruising) can be differentiated from erythema by applying pressure over the involved area. Pressure will cause erythema to blanch, whereas the skin will not change in the presence of petechiae or ecchymosis.
Examining a Mass or Skin Lesion
When examining a skin lesion or mass of any kind, follow the guidelines provided earlier in Box 4-11. In addition, the American Cancer Society (ACS) and the Skin Cancer Foundation advocate using the following ABCDEs to assess skin lesions for cancer detection (Fig. 4-6):
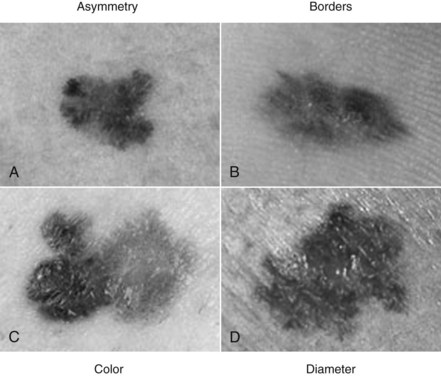
Fig. 4-6 Common characteristics associated with early melanomas are described and shown in this photo. A, Asymmetry: a line drawn through the middle does not produce matching halves. B, Borders are uneven, fuzzy, or have notched or scalloped edges. C, Color changes occur with shades of brown, black, tan, or other colors present at the same time. D, Diameter is greater than the width of a pencil eraser. Not shown: Evolving (change), in size, shape, color, elevation, or another trait, or any new symptom, such as bleeding, itching, or crusting, requires evaluation. (From Dermik Laboratories [www.dermnet.com], 2005. Used with permission.)
The ABCD (now including E) criteria have been verified in multiple studies, documenting the effectiveness and diagnostic accuracy of this screening technique. Their efficacy has been confirmed with digital image analysis; sensitivity ranges from 57% to 90% and specificity from 59% to 90%.73
Round, symmetric skin lesions such as common moles, freckles, and birthmarks are considered “normal.” If an existing mole or other skin lesion starts to change and a line drawn down the middle shows two different halves, medical evaluation is needed.
Common moles and other “normal” skin changes usually have smooth, even borders or edges. Malignant melanomas, the most deadly form of skin cancer, have uneven, notched borders.
Benign moles, freckles, “liver spots,” and other benign skin changes are usually a single color (most often a single shade of brown or tan) (Fig. 4-7). A single lesion with more than one shade of black, brown, or blue may be a sign of malignant melanoma.
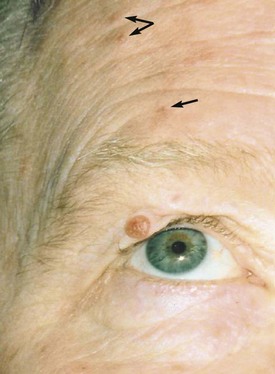
Fig. 4-7 Seborrheic keratosis, a benign well-circumscribed, raised, tan-to-black lesion often presents on the face, neck, chest, or upper back. This lesion represents a buildup of keratin, which is the primary component of the epidermis. There is a family tendency to develop these lesions. The more serious lesions are the red patches located on this client’s forehead (arrows), precancerous lesions called actinic keratosis, the result of chronic sun exposure. These lesions have a “sandpaper” feel when palpated. Medical treatment is needed for this premalignant lesion. (Courtesy Catherine C. Goodman, 2005. Used with permission.)
Even though some of us have moles we think are embarrassingly large, the average mole is really less than  of an inch (about the size of a pencil eraser). Anything larger than this should be inspected carefully.
of an inch (about the size of a pencil eraser). Anything larger than this should be inspected carefully.
The Skin Cancer Foundation (www.skincancer.org) has many public education materials available to help the therapist identify suspicious skin lesions. In addition to their website, they have posters, brochures, videos, and other materials available for use in the clinic. It is highly recommended that these types of education materials be available in waiting rooms as part of a nationwide primary prevention program.
Other websites (www.skincheck.com [Melanoma Education Foundation]; http://www.melanomafoundation.com.au/ [The Melanoma Foundation of the University of Sydney Australia]) provide additional photos of suspicious lesions with more screening guidelines. The therapist must become as familiar as possible with what suspicious skin aberrations may look like in order to refer as early as possible.
Remember to evaluate risk factors when screening for skin cancer. The average lifetime risk of developing melanoma (Caucasians) is 1 in 58.73 This has increased from 1 in 90 just in the last two decades. Your risk is much higher if you have any of the risk factors listed in Box 13-2.
For all lesions, masses, or aberrant tissue, observe or palpate for heat, induration, scarring, or discharge. Use the mnemonic in Box 4-11. Make note of how long the client has had the lesion, if it has changed in the last 6 weeks to 6 months, and whether it has been medically evaluated. Always ask appropriate follow-up questions with this assessment:
How you ask is just as important as what you say. Do not frighten people by first telling them you always screen for skin cancer. It may be better to introduce the subject by saying that as health care professionals, therapists are trained to observe many body parts, including the skin, joints, posture, and so on. You notice the client has an unusual mole (or rash … or whatever you have observed) and you wonder if this is something that has been there for years. Has it changed in the last 6 weeks to 6 months? Has the client ever shown it to the doctor?
Assess Surgical Scars
It is always a good idea to look at surgical scars (Fig. 4-8), especially sites of local cancer removal. Any suspicious scab or tissue granulation, redness, or discoloration must be noted (photographed if possible).
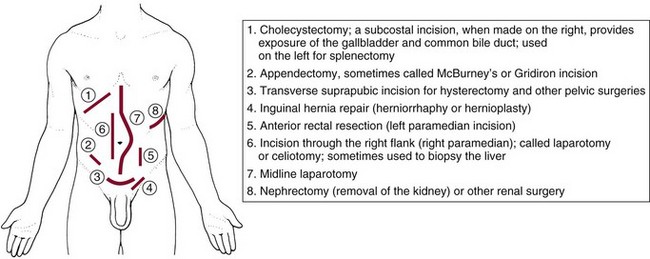
Fig. 4-8 Abdominal surgical scars. Not shown: puncture sites for laparoscopy, usually close to the umbilicus and one or two other sites.
Start by asking the client if he or she has noticed any changes in the scar. Continue by asking:
If the client declines or refuses, be sure to follow-up with counsel to perform self-inspection and report any changes to the physician.
In Fig. 4-9, the small scab and granular tissue forming above the scar represent red flags of suspicious local recurrence. Even if the client suggests this is from “picking” at the scar, a medical evaluation is well advised.

Fig. 4-9 Squamous cell carcinoma in scar. Always ask to see and examine scars from previous surgeries, especially when there has been a history of any kind of cancer, including skin cancer. Even in this black and white photo, you can see many skin changes to suggest the need for medical evaluation. Look to the far right of the raised scar tissue. You will see a normal, smooth scar. This is what the entire scar should look like. In this photo there is a horizontal line of granulation along the upper edge of the scar, as well as a scabbed over area in the middle of the raised scar. There is also a change in skin color on either side of the scar. (From Swartz MH: Textbook of physical diagnosis, ed 4, Philadelphia, 2001, WB Saunders.)
The therapist has a responsibility to report these findings to the appropriate health care professional and make every effort to ensure client/patient compliance with follow-up.
Common Skin Lesions
A lack of pigmentation from melanocyte destruction (vitiligo) (Fig. 4-10) can be hereditary and have no significance or it can be caused by conditions such as hyperthyroidism, stomach cancer, pernicious anemia, diabetes mellitus, or autoimmune diseases.
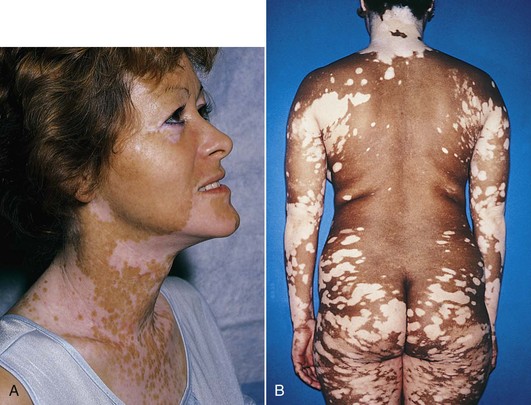
Fig. 4-10 Vitiligo is a term derived from the Greek word for “calf” used to describe patches of light skin caused by loss of epidermal melanocytes. Note the patchy loss of pigment on the face, trunk, and axilla. This condition can affect any part of the face, hands, or body and can be very disfiguring, especially in dark-skinned individuals. This skin change may be a sign of hyperthyroidism. (From Swartz MH: Textbook of physical diagnosis, ed 5, Philadelphia, 2006, WB Saunders.)
Lesions can occur anywhere on the body but tend to develop in sun-exposed areas, body folds, and around body openings. Intraarticular steroid injections can cause temporary loss of pigmentation at the injection site. Anyone with any kind of skin type and skin color can be affected by vitiligo.
Café-au-lait
Café-au-lait (coffee with milk) spots describe the light-brown macules (flat lesion, different in color) on the skin as shown in Fig. 4-11. This benign skin condition may be associated with Albright’s syndrome or a hereditary disorder called neurofibromatosis. The diagnosis is considered when a child presents with five or more of these skin lesions or if any single patch is greater than 1.5 cm in diameter.

Fig. 4-11 Café-au-lait patches of varying sizes in a client with neurofibromatosis. Occasional (less than 5) tan macules are not significant and can occur normally. Patches 1.5 cm in diameter or larger raise the suspicion of underlying pathology even if there is only one present. (From Epstein O, Perkin GD, deBono DP, et al: Clinical examination, London, 1992, Gower Medical Publishing. Used with permission, Elsevier Science.)
Skin Rash
There are many possible causes of skin rash, including viruses (e.g., chicken pox, measles, Fifth disease, shingles), systemic conditions (e.g., meningitis, lupus, hives), parasites (e.g., lice, scabies), and reactions to chemicals.
A common cause of skin rash seen in a physical therapy practice is medications, especially antibiotics (Fig. 4-12). The reaction may occur immediately or there may be a delayed reaction of hours up to 6 to 8 weeks after the drug is stopped.

Fig. 4-12 Skin rash (reactive erythema) caused by a drug reaction to phenobarbital. Hypersensitivity reactions to drugs are most common with antibiotics (especially penicillin), sulfonamides (“sulfa drugs,” antiinfectives), and phenobarbital as shown here. (From Callen JP, Paller AS, Greer KE, et al: Color atlas of dermatology, ed 2, Philadelphia, 2000, WB Saunders.)
Skin rash can also occur before visceral malignancy of many kinds. Watch for skin rash or hives in someone who has never had hives before, especially if there has been no contact with medications, new foods, new detergents, or new perfumes or travel.
Hemorrhagic Rash
Hemorrhagic rash requires medical evaluation. A hemorrhagic rash occurs when small capillaries under the skin start to bleed forming tiny blood spots under the skin (petechiae). The petechiae increase over time as bleeding continues.
This type of rash does not fade under pressure with continued bleeding. Press a clear see-through drinking glass against the skin. Rashes from allergies or viral infections are more likely to fade and the skin will become white or pale. During later stages of hemorrhagic bleeding the rash does not fade or become pale with the pressure test; this test is not as reliable during early onset of hemorrhage. Left untreated, hemorrhagic spots may become bruises and then large red-purple areas of blood. Pressure on a bruise will not cause it to blanch.
Dermatitis
Dermatitis (sometimes referred to as eczema) is characterized by skin that is red, brown, or gray; sore; itchy; and sometimes swollen. The skin can develop blisters and weeping sores. Skin changes, especially in the presence of open lesions, puts the client at increased risk of infection. In chronic dermatitis, the skin can become thick and leathery.
There are different types of dermatitis diagnosed on the basis of medical history, etiology (if known), and presenting signs and symptoms. Contributing factors include stress, allergies, genetics, infection, and environmental irritants. For example, contact dermatitis occurs when the skin reacts to something it has come into contact with such as soap, perfume, metals in jewelry, and plants (e.g., poison ivy or oak).
Dyshidrotic dermatitis can affect skin that gets wet frequently. It presents as small, itchy bumps on the sides of the fingers or toes and progresses to a rash. Atopic dermatitis often accompanies asthma or hay fever. It appears to affect genetically predisposed clients who are hypersensitive to environmental allergens. This type of dermatitis can affect any part of the body, but often involves the skin inside the elbow and on the back of the knees.
Rosacea
Rosacea is a chronic facial skin disorder seen most often in adults between the ages of 30 and 60 years. It can cause a facial rash easily mistaken for the butterfly rash associated with lupus. Features include erythema, flushing, telangiectasia, papules, and pustules affecting the cheeks and nose of the face. An enlarged nose is often present, and the condition progressively gets worse (Fig. 4-13).
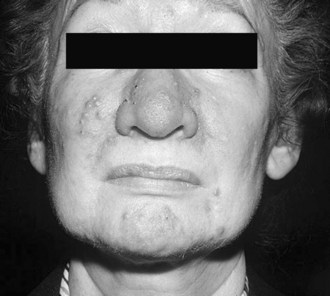
Fig. 4-13 Rosacea, a form of adult acne, may be associated with Helicobacter pylori; medical evaluation and treatment is needed to rule out this possibility. (Courtesy University of Iowa Virtual Hospital. Copyright protected material used with permission of the authors and the University of Iowa’s Virtual Hospital; www.vh.org/adult/provider/dermatology/PietteDermatology/BlackTray/33Rosacea.html.)
Rosacea can be controlled with dermatologic or other medical treatment in some cases. Recent studies suggest rosacea may be linked to GI disease caused by the H. pylori bacteria.74-76 Such cases may respond favorably to antibiotics. Medical referral is needed for an accurate diagnosis.
Thrombocytopenia
Decrease in platelet levels can result in thrombocytopenia, a bleeding disorder characterized by petechiae (tiny purple or red spots), multiple bruises, and hemorrhage into the tissues (Fig. 4-14). Joint bleeds, nose and gum bleeds, excessive menstruation, and melena (dark, tarry, sticky stools from oxidized blood in the GI tract) can occur with thrombocytopenia.

Fig. 4-14 Purpura. Petechiae and ecchymoses are seen in this flat macular hemorrhage from thrombocytopenia (platelet level less than 100,000/mm3). This condition also occurs in older adults as blood leaks from capillaries in response to minor trauma. It can occur in fair-skinned people with skin damage from a lifetime of exposure to ultraviolet (UV) radiation. Exposure to UVB and UVA rays can cause permanent damage to the structural collagen that supports the walls of the skin’s blood vessels. Combined with thinning of the skin that occurs with aging, radiation-impaired blood vessels are more likely to rupture with minor trauma. (From Hurwitz S: Clinical pediatric dermatology: a textbook of skin disorders of childhood and adolescence, ed 2, Philadelphia, 1993, WB Saunders.)
There are many causes of thrombocytopenia. In a physical therapy practice, the most common causes seen are bone marrow failure from radiation treatment, leukemia, or metastatic cancer; cytotoxic agents used in chemotherapy; and drug-induced platelet reduction, especially among adults with rheumatoid arthritis treated with gold or inflammatory conditions treated with aspirin or other NSAIDs.
Postoperative thrombocytopenia can be heparin-induced for patients receiving IV heparin. Watch for limb ischemia, cyanosis of fingers or toes, signs and symptoms of a stroke, heart attack, or pulmonary embolus. (See further discussion on Thrombocytopenia in Chapter 5.)
Xanthomas
Xanthomas are benign fatty fibrous yellow plaques, nodules, or tumors that develop in the subcutaneous layer of skin (Fig. 4-15), often around tendons. The lesion is characterized by the intracellular accumulation of cholesterol and cholesterol esters.

Fig. 4-15 Xanthelasma. Soft, raised yellow plaques, also known as xanthomas, commonly occur with aging and may be a sign of high cholesterol levels. Shown here on the eyelid, these benign lesions also occur on the extensor surfaces of tendons, especially in the hands, elbows, and knees. They may have no pathologic significance, but they often appear in association with disorders of lipid metabolism. (From Albert DM, Jakobeic FA: Principles and practice of ophthalmology, vol 3, Philadelphia, 1994, WB Saunders.)
These are seen most often associated with disorders of lipid metabolism, primary biliary cirrhosis, and uncontrolled diabetes (Fig. 4-16). They may have no pathologic significance but can occur in association with malignancy such as leukemia, lymphoma, or myeloma. Xanthomas require a medical referral if they have not been evaluated by a physician. When associated with diabetes, these nodules will resolve with adequate glucose control.

Fig. 4-16 A slightly different presentation of xanthomas, this time associated with poorly controlled diabetes mellitus. Although the lesion is considered “benign,” the presence of these skin lesions in anyone with diabetes signals the need for immediate medical attention. The therapist also plays a key role in client education and the development of an appropriate exercise program to bring blood glucose levels under adequate control. (From Callen JP, Jorizzo J, Greer KE, et al: Dermatological signs of internal disease, Philadelphia, 1988, WB Saunders.)
The therapist has an important role in education and prescriptive exercise for the client with xanthomas from poorly controlled diabetes. Gaining control of glucose levels using the three keys of intervention (diet, exercise, and insulin or oral hypoglycemic medication) is essential and requires a team management approach.
Rheumatologic Diseases
Skin lesions are often the first sign of an underlying rheumatic disease (Box 4-14). In fact, the skin has been called a “map” to rheumatic diseases. The butterfly rash over the nose and cheeks associated with lupus erythematosus can be seen in the acute (systemic) phase, whereas discoid lesions are more common with chronic integumentary form of lupus (Fig. 4-17).77

Fig. 4-17 Skin lesions associated with discoid lupus erythematosus. These disk-shaped lesions look like warts or squamous cell carcinoma. A medical examination is needed to make the definitive differential diagnosis. (From Callen JP, Jorizzo J, Greer KE, et al: Dermatological signs of internal disease, Philadelphia, 1988, WB Saunders.)
Individuals with dermatomyositis often have a heliotrope rash and/or Gottron papules. Scleroderma is accompanied by many skin changes; pitting of the nails is common with psoriatic arthritis. Skin and nail bed changes are common with some sexually transmitted diseases that also have a rheumatologic component (see Figs. 3-10 and 4-22).78
Steroid Skin and Steroid Rosacea
Steroid skin is the name given when bruising or ecchymosis occurs as a result of chronic use of topical or systemic corticosteroids (Fig. 4-18). In the case of topical steroid creams, this is a red flag that pain is not under control and medical attention for an underlying (probably inflammatory) condition is needed.

Fig. 4-18 Ecchymosis as a result of steroid application. Also note the cutaneous atrophy produced by topical steroids. This skin condition is referred to as “steroid skin” when associated with chronic oral or topical steroid use. Medical referral may be needed for better pain control. (From Callen JP, Jorizzo J, Greer KE, et al: Dermatological signs of internal disease, Philadelphia, 1988, WB Saunders.)
The use of topical corticosteroids for more than 2 weeks to treat chronic skin conditions affecting the face can cause a condition characterized by rosacea-like eruptions known as steroid rosacea. Attempts to stop using the medication may result in severe redness and burning called steroid addiction syndrome (Fig. 4-19).

Fig. 4-19 Steroid addiction appearing to be acne. This condition was caused by long-term application of a moderate-potency steroid and Mycostatin combined. (From Weston WL: Weston color textbook of pediatric dermatology, ed 4, St. Louis, 2007, Mosby.)
Whenever signs and symptoms of chronic corticosteroids are seen, a medical evaluation may be needed to review medical management of the problem. In the case of steroid skin from chronic systemic corticosteroid use, ask if the physician has seen (or knows about) the signs and symptoms and how long it has been since medications have been reviewed. The multiple side effects of chronic corticosteroid use are discussed in association with Cushing’s syndrome (see Chapter 11).
Erythema Chronicum Migrans
One or more erythema migrans rash may occur with Lyme disease. There is no one prominent rash. The rash varies in size and shape and may have purple, red, or bruised-looking rings. The rash may appear as a solid red expanding rash or blotch or as a central red spot surrounded by clear skin that is ringed by an expanding red rash. It may be smooth or bumpy to the touch, and it may itch or ooze. The Lyme Disease Foundation provides a photo gallery of possible rashes associated with Lyme disease.78
This rash, which develops in most people with Lyme disease, appears most often 1 to 2 weeks after the disease is transmitted (via tick bite) and may persist for 3 to 5 weeks. It usually is not painful or itchy but may be warm to the touch. The bull’s-eye rash may be more difficult to see on darker-skinned people. A dark, bruise-like appearance is more common in those cases. Other symptoms are listed in Chapter 12.
Effects of Radiation
Radiation for the treatment of some cancers has some specific effects on the skin. Pigment producing cells can be affected by either low dose radiation causing hyperpigmentation or by high dose radiation resulting in depigmentation (vitiligo). Pigmentation changes can be localized or generalized.79
Radiation recall reaction can occur months later as a postirradiation effect. The physiologic response is much like overexposure to the sun with erythema of the skin in the same pattern as the radiation exposure without evidence of disease progression at that site. It is usually precipitated by some external stimuli or event such as exposure to the sun, infection, or stress.
Radiation recall is also more likely to occur when an individual receives certain chemotherapies (e.g., cyclophosphamide, paclitaxel, doxorubicin, gemcitabine) after radiation.80,81 The chemotherapy causes the previously radiated area to become inflamed and irritated.
Radiation dermatitis and x-ray keratosis, separate from radiation recall, are terms used to describe acute (expected) skin irritation caused by radiation at the time of radiation.
Skin changes can also occur as a long-term effect of radiation exposure. Radiation levels administered to oncology patients even 10 years ago were much higher than today’s current treatment regimes. Always look at previous radiation sites for evidence of long-term effects.
Sexually Transmitted Diseases/Infections
Sexually transmitted diseases (STDs) are a variety of clinical syndromes caused by pathogens that can be acquired and transmitted through sexual activity.82 STDs, also known as sexually transmitted infections (STIs), are often accompanied by skin and/or nail bed lesions and joint pain. Being able to recognize STIs is helpful in the clinic. Someone presenting with joint pain of “unknown cause” and also demonstrating signs of a STI (see Fig. 3-10) may help bring the correct diagnosis to light sooner than later.
Around the world, STIs pose a major health problem. In 1970, there were two major STIs; today, there are 25. The prevalence of STIs is rapidly increasing to epidemic proportions in the United States. Two-thirds of all STIs occur in people 25 years of age or younger.83,84
STIs have been positively identified as a risk factor for cancer. Not all STIs are linked with cancer, but studies have confirmed that human papillomavirus (HPV) is the primary cause of cervical cancer (Fig. 4-20).85 HPV is the leading viral STI in the United States. More than 70 types of HPV have been identified: 23 infect the cervix and 13 types are associated with cancer in men and women. Infection with one of these viruses does not predict cancer, but the risk of cancer is increased.82

Fig. 4-20 Common warts of the hands caused by human papillomavirus (HPV) via nonsexual transmission. The virus can be transmitted through sexual contact and is a precursor to cancer of the cervix. Genital warts do not typically occur by autoinoculation from the hands. In other words, warts on the fingers caused by HPV are probably NOT transmitted from finger to genitals. They occur with contact of someone else’s genital warts. Warts on the fingers caused by sexually transmitted HPV do not transmit the sexually transmitted infection (STI) to the therapist if the therapist shakes hands with the client or touches the warts. However, standard precautions are always recommended whenever skin lesions of any kind are present. For a summary of Standard Precautions, see Goodman et al., 2003.85 (From Parkin JM, Peters BS: Differential diagnosis in AIDS, London, 1991, Mosby-Wolfe.)
Syphilis is on the rise again with the number of cases doubled in the last few years among gay and bisexual men, suggesting an erosion of safe sex practices.86,87 It is highly contagious, spread from person to person by direct contact with a syphilis sore on the body of an infected person. Sores occur at the site of infection, mainly on the external genitals, vagina, anus, or rectum. Sores can also occur on the lips and in the mouth.
Transmission occurs during vaginal, anal, or oral sex. An infected pregnant woman can also pass the disease to her unborn child. Syphilis cannot be spread by contact with toilet seats, doorknobs, swimming pools, hot tubs, bathtubs, shared clothing, or eating utensils.
In the first stage of syphilis, a syphilis chancre may appear (Fig. 4-21) at the site of inoculation (usually the genitals, anus, or mouth). The chancre occurs 4 weeks after initial infection and is often not noticed in women when present in the genitalia. The chancre is often accompanied by lymphadenopathy.

Fig. 4-21 The first stage (primary syphilis) is marked by a very infectious sore called a chancre. The chancre is usually small, firm, round with well-demarcated edges, and painless. It appears at the spot where the bacteria entered the body. Chancres last 1 to 5 weeks and heal on their own. (From A close look at venereal disease, Public service slide presentation. Courtesy Pfizer Laboratories, Pfizer Inc, New York. Permission granted 2004.)
Without treatment, the spread of the bacteria through the blood causes the second stage (secondary syphilis). Therapists may see lesions associated with secondary syphilis (Fig. 4-22). Neurologic (untreated) infection may present as cranial nerve dysfunction, meningitis, stroke, acute or chronic altered mental status, loss of vibration sense, and auditory or ophthalmic abnormalities.82
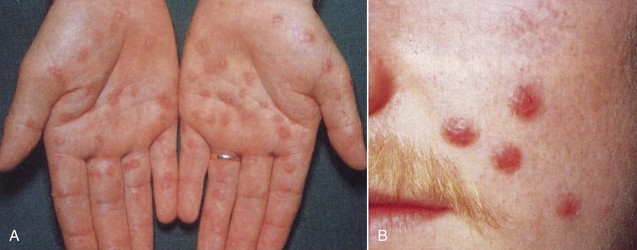
Fig. 4-22 Maculopapular rash associated with secondary syphilis appears as a pink, dusky, brownish-red or coppery, indurated, oval or round lesion with a raised border. These are referred to as “copper penny” spots. The lesions do not bleed and are usually painless. They usually appear scattered on the palms (A) or the bottom of the feet (not shown) but may also present on the face (B). The second stage begins 2 weeks to 6 months after the initial chancre disappears. The client may report joint pain with general flu-like symptoms (e.g., headache, sore throat, swollen glands, muscle aches, fatigue). Patchy hair loss may be described or observed. (From Mir MA: Atlas of clinical diagnosis, London, 1995, WB Saunders; p 198.)
The client may report or present with a characteristic rash that can appear all over the body, most often on the palms and soles. The appearance of these skin lesions occurs after the primary chancre disappears. During this time the risk of human immunodeficiency virus (HIV) transmission from unsafe sexual practices is increased twofold to fivefold.
Syphilis can be tested for with a blood test and treated successfully with antibiotics. Left untreated, tertiary (late stage) syphilis can cause paralysis, blindness, personality changes or dementia, and damage to internal organs and joints. The therapist can facilitate early detection and treatment through immediate medical referral. See further discussion on Infectious Causes of Pelvic Pain in Chapter 15, including special questions to ask concerning sexual activity and STIs. (See also Appendix B-33.)
Herpes Virus: Several herpes viruses are accompanied by characteristic skin lesions. Herpes simplex virus (HSV)-1 and -2 are the most common. Most people have been exposed at an early age and already have immunity. In fact, four out of five Americans harbor HSV-1. Due to the universal distribution of these viruses, most individuals have developed immunity by the ages of 1 to 2 years.
The HSV-1 and -2 viruses are virtually identical, sharing approximately 50% of their DNA. Both types infect the body’s mucosal surfaces, usually the mouth or genitals, and then establish latency in the nervous system.88 Both can cause skin and nail bed changes.
Cold sores caused by HSV-1 (also known as recurrent herpes labialis; “fever blister”) are found on the lip or the skin near the mouth. HSV-1 usually establishes latency in the trigeminal ganglion, a collection of nerve cells near the ear. HSV-1 generally only infects areas above the waistline and occurs when oral secretions or mucous membranes infected with HSV come in contact with a break in the skin (e.g., torn cuticle, skin abrasion).
HSV-1 can be transmitted to the genital area during oral sex. In fact, HSV-1 can be transmitted oral-to-oral, oral-to-genital, anal-to-genital, and oral-to-anal. HSV-1 actually predominates for oral transmission, while a second herpesvirus (genital herpes; HSV-2) is more often transmitted sexually.
HSV 2, also known as “genital herpes” can cause cold sores but usually does not; rather, it is more likely to infect body tissues below the waistline as it resides in the sacral ganglion at the base of the spine.
Most HSV-1 and -2 infections are not a major health threat in most people but slowing the spread of genital herpes is important. The virus is more of a social problem than a medical one. The exception is that genital lesions from herpes can make it easier for a person to become infected with other viruses, including HIV, which increases the risk of developing acquired immunodeficiency syndrome (AIDS).
Nonmedical treatment with OTC products is now available for cold sores. Outbreaks of genital herpes can be effectively treated with medications, but these do not “cure” the virus. HSV-1 is also the cause of herpes whitlow, an infection of the finger and “wrestler’s herpes,” a herpes infection on the chest or face.
Herpetic Whitlow: Herpetic whitlow, an intense painful infection of the terminal phalanx of the fingers is caused by HSV-1 (60%) and HSV-2 (40%). The thumb and index fingers are most commonly involved. There may be a history of fever or malaise several days before symptoms occur in the fingers.
Common initial symptoms of infection include tingling pain or tenderness of the affected digit, followed by throbbing pain, swelling, and redness. Fluid-filled vesicles form and eventually crust over, ending the contagious period. The client with red streaks down the arm and lymphadenopathy may have a secondary infection. Take the client’s vital signs (especially body temperature) and report all findings to the physician.89
As in other herpes infections, viral inoculation of the host occurs through exposure to infected body fluids via a break in the skin such as a paper cut or a torn cuticle. Autoinoculation can occur in anyone with other herpes infections such as genital herpes. It is an occupational risk among health care workers exposed to infected oropharyngeal secretions of clients, easily prevented by using standard precautions.90
Herpes Zoster: Varicella-zoster virus (VZV), or herpes zoster or “shingles,” is another herpes virus with skin lesions characteristic of the condition. VZV is caused by the same virus that causes chickenpox. After an attack of chickenpox, the virus lies dormant in the nerve tissue, usually the dorsal root ganglion. If the virus is reactivated, the virus can reappear in the form of shingles.
Shingles is an outbreak of a rash or blisters (vesicles with an erythematous base) on the skin that may be associated with severe pain (Fig. 4-23). The pain is associated with the involved nerve root and associated dermatome and generally presents on one side of the body or face in a pattern characteristic for the involved site (Fig. 4-24). Early signs of shingles include burning or shooting pain and tingling or itching. The rash or blisters are present anywhere from 1 to 14 days.
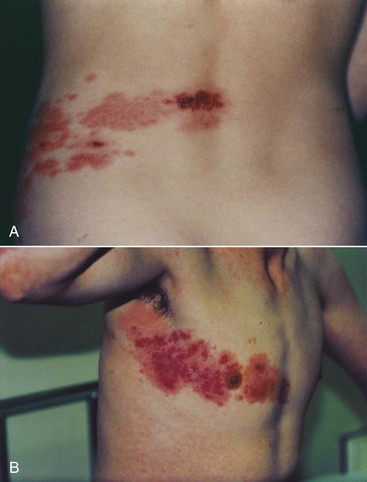
Fig. 4-23 Herpes zoster (shingles). A, Lesions appear unilaterally along the path of a spinal nerve. B, Eruptions involving the T4 dermatome. (A from Callen J, Greer K, Hood H, et al: Color atlas of dermatology, Philadelphia, 1993, WB Saunders; B from Marx J, Hockberger R, Walls R: Rosen’s emergency medicine: concepts and clinical practice, ed 6, St. Louis, 2006, Mosby.)
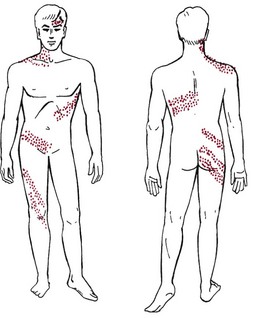
Fig. 4-24 Symptoms of shingles appear on only one side of the body, usually on the torso or face. Most often, the lesions are visible externally. In unusual cases, clients report the same symptoms internally along the dermatome but without a corresponding external skin lesion. (From Malasanos L, Barkauskas V, Stoltenberg-Allen K: Health assessment, ed 4, St. Louis, 1990, Mosby.)
Complications of shingles involving cranial nerves include hearing and vision loss. Postherpetic neuralgia (PHN), a condition in which the pain from shingles persists for months, sometimes years, after the shingles rash has healed, can also occur. PHN can be very debilitating. Early intervention within the first 72 hours of onset with anti-retroviral medications may diminish or eliminate PHN. Early identification and intervention is very important to outcomes.
Adults with shingles are infectious to anyone who has not had chickenpox. Anyone who has had chickenpox can develop shingles when immunocompromised. Other risk factors for VZV include age (young or old) and immunocompromise from HIV infection, chemotherapy or radiation treatment, transplants, aging, and stress. It is highly recommended that health care professionals with no immunity to VZV receive the varicella vaccine. Therapists who have never had chickenpox (and especially women of childbearing age who have not had the chickenpox) should be tested for immune status.
Cutaneous Manifestations of Abuse
Signs of child abuse or domestic violence in adults may be seen as skin lesions. Cigarette burns leave a punched out ulceration with dry, purple crusts (see www.dermatlas.org). Splash marks or scald lines from thermal (hot water) burns occur most often on the buttocks and distal extremities.91 Bruising from squeezing and shaking involving the mid-portion of the upper arms is a suspicious sign.
Accidental bruising in young children is common; the therapist should watch for nonaccidental bruising found in atypical areas, such as the buttocks, hands, and trunk, or in a child who is not yet biped (up on two feet) and cruising (walking along furniture or holding an object while taking steps). To make an accurate assessment, it is important to differentiate between inflicted cutaneous injuries and mimickers of physical abuse.
For example, infants with bruising may be demonstrating early signs of bleeding disorders.91 Mongolian spots can also be mistaken for bruising from child abuse (see next section). The therapist is advised to take digital or Polaroid photos of any suspicious lesions in children under the age of 18. Document the date and provide a detailed description.
The law requires that professionals report suspected child abuse and neglect to the appropriate authorities. It is not up to the health care professional to determine child abuse has occurred; this is left up to investigating officials. See other guidelines regarding child abuse and domestic violence in Chapter 2. Understanding the reporting guidelines helps direct practitioners in their decision making.91
Mongolian Spots: Discoloration of the skin in newborn infants called Mongolian spots (Fig. 4-25) can be mistaken for signs of child abuse. The Mongolian spot is a congenital, developmental condition exclusively involving the skin and is very common in children of Asian, African, Indian, Native American, Eskimo, Polynesian, or Hispanic origins.

Fig. 4-25 Mongolian spots (congenital dermal melanocytosis). Mongolian spots are common among people of Asian, East Indian, Native American, Inuit, African, and Latino or Hispanic heritage. They are also present in about one in ten fair-skinned infants. Bluish gray to deep brown to black skin markings, they often appear on the base of the spine, on the buttocks and back, and even sometimes on the shoulders, ankles, or wrists. Mongolian spots may cover a large area of the back. When the melanocytes are close to the surface, they look deep brown. The deeper they are in the skin, the more bluish they look, often mistaken for signs of child abuse. These spots “fade” with age as the child grows and usually disappear by age 5. (Courtesy Dr. Dubin Pavel, 2004.)
These benign pigmentation changes appear as flat dark blue or black areas and come in a variety of sizes, shapes, and colors. The skin changes result from entrapment of melanocytes (skin cells containing melanin, the normal pigment of the skin) during their migration from the neural crest into the epidermis.
Cancer-Related Skin Lesions
When screening for primary skin cancer, keep in mind there are other cancer-related skin lesions to watch out for as well. For example, skin rash can present as an early sign of a paraneoplastic syndrome before other manifestations of cancer or cancer recurrence (Fig. 4-26). See further discussion of paraneoplastic syndromes in Chapter 13.

Fig. 4-26 Metastatic carcinoma presenting as a cellulitic skin rash on the anterior chest wall as a result of carcinoma of the lung. This rash can be red, tan, or brown with a flat or raised appearance. When associated with a paraneoplastic syndrome, it may appear far from the site of the primary cancer. (From Callen JP, Jorizzo J, Greer KE, et al: Dermatological signs of internal disease, Philadelphia, 1988, WB Saunders.)
Pinch purpura, a purplish, brown, or red discoloration of the skin can be mistaken by the therapist for a birthmark or port wine stain (Fig. 4-27). Using the question “How long have you had this?” can help differentiate between something the person has had his or her entire life and a suspicious skin lesion or recent change in the integument.

Fig. 4-27 Pinch purpura in an individual with multiple myeloma caused by amyloidosis of the skin. The purpura shown here is a recent skin change for this client. (From Callen JP, Jorizzo J, Greer KE, et al: Dermatological signs of internal disease, ed 2, Philadelphia, 1995, WB Saunders.)
When purpura causes a raised and palpable skin lesion, it is called palpable purpura. The palpable hemorrhages are caused by red blood cells extravasated (escaped) from damaged vessels into the dermis. This type of purpura can be associated with cutaneous vasculitis, pulmonary-renal syndrome, or drug reaction. The lower extremities are affected most often.
Many older adults assume this is a “normal” sign of aging (and in fact, purpura does occur more often in aging adults; see Fig. 4-14); they do not see a physician when it first appears. Early detection and referral is always the key to a better prognosis. In asking the three important questions, the therapist plays an instrumental part in the cancer screening process.
A client with a past medical history of cancer now presenting with a suspicious skin lesion (Fig. 4-28) that has not been evaluated by the physician must be advised to have this evaluated as soon as possible. We must be aware of how to present this recommendation to the client. There is a need to avoid frightening the client while conveying the importance of early diagnosis of any unusual skin lesions.

Fig. 4-28 Metastatic renal carcinoma presenting as a nodule in the scalp. Observing any skin lesions no matter what part of the body the therapist is examining must be followed by the three assessment questions listed in the text. (From Callen JP, Jorizzo J, Greer KE, et al: Dermatological signs of internal disease, Philadelphia, 1988, WB Saunders.)
Kaposi’s Sarcoma
Kaposi’s sarcoma is a form of skin cancer common in older Jewish men of Mediterranean descent that presents with a wide range of appearance. A gallery of photos can be seen by doing a Google search of “Kaposi’s sarcoma.” (Go to www.Google.com and type in the words: Kaposi’s sarcoma, then click on the word “Images” on the Google page.) It is not contagious to touch and does not usually cause death or disfigurement.
More recently, Kaposi’s sarcoma has presented as an opportunistic disease in adults with HIV/AIDS. With the more successful treatment of AIDS with antiretroviral agents, opportunistic diseases, such as Kaposi’s sarcoma, are on the decline.
Even though this skin lesion will not transmit skin cancer or HIV, the therapist is always advised to use standard precautions with anyone who has skin lesions of any type.
Lymphomas
Round patches of reddish-brown skin with hair loss over the area are lymphomas, a type of neoplasm of lymphoid tissue (Fig. 4-29). The most common forms of lymphoma are Hodgkin’s disease and non-Hodgkin’s lymphoma (NHL).
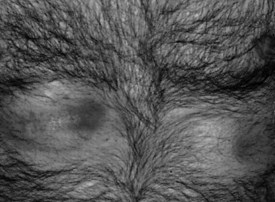
Fig. 4-29 Lymphomas seen here just below the nipples on the chest of an adult male arise in individuals who are chronically immunosuppressed for any reason. (From Conant MA: The link between HIV and skin malignancies, The Skin Cancer Foundation Journal, Vol XII, 1994.)
Typically, the appearance of a painless, enlarged lymph node or skin lesion of this type is followed by weakness, fever, and weight loss. A history of chronic immunosuppression (e.g., antirejection drugs for organ transplants, chronic use of immunosuppressant drugs for inflammatory or autoimmune diseases, cancer treatment) in the presence of this clinical presentation is a major red flag.
Nail Bed Assessment
As with assessment of the skin, nail beds (fingers and toes) should be evaluated for color, shape, thickness, texture, and the presence of lesions (Box 4-15). Systemic changes affect both fingernails and toenails, but the signs are typically more prominent in the faster-growing fingernails.92
The normal nail consists of three parts: the nail bed, the nail plate, and the cuticle (Fig. 4-30). The nail bed is highly vascularized and gives the nail its pink color. The hard nail is formed at the proximal end (the matrix). About one-fourth of the nail is covered by skin known as the proximal nail fold. The cuticle seals and protects the space between the proximal fold and the nail plate.92
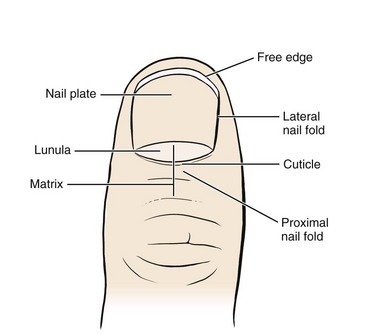
Fig. 4-30 Normal nail structure. The nail matrix forms the nail plate and begins about 5 mm to 8 mm beneath the proximal nail fold and extends distally to the edge of the lunula, where the nail bed begins. The lunula (half-moon) is the exposed part of the nail matrix, distal to the proximal nail fold; it is not always visible.
Many individual variations in color, texture, and grooming of the nails are influenced by factors unrelated to disease, such as occupation, chronic use of nail polish or acrylics, or exposure to chemical dyes and detergents. Longitudinal lines of darker color (pigment) may be seen in the normal nails of clients with darker skin.
In assessing the older adult, minor variations associated with the aging process may be observed (e.g., gradual thickening of the nail plate, appearance of longitudinal ridges, yellowish-gray discoloration).
In the normal individual, pressing or blanching the nail bed of a finger or toe produces a whitening effect; when pressure is released, a return of color should occur within 3 seconds. If the capillary refill time exceeds 3 seconds, the lack of circulation may be due to arterial insufficiency from atherosclerosis or spasm.
Nail Bed Changes
Some of the more common nail bed changes seen in a physical therapy practice are included in this chapter. With any nail or skin condition, ask if the nails have always been like this or if any changes have occurred in the last 6 weeks to 6 months. Referral may not be needed if the physician is aware of the new onset of nail bed changes. Ask about the presence of other signs and symptoms consistent with any of the conditions listed here that can cause any of these nail bed changes.
Again, as with visual inspection of the skin, this section of the text is only a cursory look at the most common nail bed changes. Many more are not included here. A well-rounded library should include at least one text with color plates and photos of various nail bed changes.93-97 This is not to help the therapist diagnose a medical problem but rather to provide background information, which can be used in the referral decision-making process.
Onycholysis
Onycholysis, a painless loosening of the nail plate occurs from the distal edge inward (Fig. 4-31). Fingers and toes may both be affected as a consequence of dermatologic conditions such as dermatitis, fungal disease, lichen planus, and psoriasis. Systemic diseases associated with onycholysis include myeloma, neoplasia, Graves’ disease, anemia, and reactive arthritis.98

Fig. 4-31 Onycholysis. Loosening of the nail plate, usually from the tip of the nail, progressing inward and from the edge of the nail moving inward. Possible causes include Graves’ disease, psoriasis, reactive arthritis, and obsessive-compulsive behaviors (nail pickers). (From Arndt KA, Wintroub BU, Robinson JK, et al: Primary care dermatology, Philadelphia, 1997, WB Saunders.)
Medications, such as tetracycline, fluoroquinolones, anticancer drugs, nonsteroidal antiinflammatories, psoralens, retinoids, zidovudine, and quinine, can cause photo-onycholysis (toes must be exposed to the sun for the condition to occur).98
Local causes from chemical, physical, cosmetic, or traumatic sources can bring on this condition. In the case of trauma, a limited number of nails are affected. For example, in clients with onycholysis as a result of nervous or obsessive-compulsive behaviors, only one or two nails are targeted. The individual picks around the edges until the nail is raised and separated from the nail bed. When there is an underlying systemic disorder, it is more common to see all the nail plates affected.
Koilonychia
Koilonychia or “spoon nails” may be a congenital or hereditary trait and as such is considered “normal” for that individual. These are thin, depressed nails with lateral edges tilted upward, forming a concave profile (Fig. 4-32).

Fig. 4-32 Koilonychia (spoon nails). In this side-by-side view, the affected nail bed is on the left and the normal nail on the right. With a spoon nail, the rounded indentation would hold a drop or several drops of water, hence the name. (From Swartz MH: Textbook of physical diagnosis, ed 5, Philadelphia, 2006, WB Saunders.)
Koilonychia can occur as a result of hypochromic anemia, iron deficiency (with or without anemia), poorly controlled diabetes of more than 15 years duration, chemical irritants, local injury, developmental abnormality, or psoriasis. It can also be an outward sign of thyroid problems, syphilis, and rheumatic fever.
Beau’s lines
Beau’s lines are transverse grooves or ridges across the nail plate as a result of a decreased or interrupted production of the nail by the matrix (Fig. 4-33). The cause is usually an acute illness or systemic insult such as chemotherapy for cancer. Other common conditions associated with Beau’s lines are poor peripheral circulation, eating disorders, cirrhosis associated with chronic alcohol use, and recent myocardial infarction (MI).

Fig. 4-33 Beau’s lines or grooves across the nail plate. A depression across the nail extends down to the nail bed. This occurs with shock, illness, malnutrition, or trauma severe enough to impair nail formation such as acute illness, prolonged fever, or chemotherapy. A dent appears first at the cuticle and moves forward as the nail grows. All nails can be involved, but with local trauma, only the involved nail will be affected. This photo shows a client postinsult after full recovery. At the time of the illness, nail loss is obvious often with change in nail bed color such as occurs with chemotherapy. (From Callen JP, Greer KE, Hood AF, et al: Color atlas of dermatology, Philadelphia, 1994, WB Saunders.)
Since the nails grow at an approximate rate of 3 mm/month, the date of the initial onset of illness or disease can be estimated by the location of the line. The dent appears first at the cuticle and moves forward as the nail grows. Measure the distance (in millimeters) from the dent to the cuticle and add 3 to account for the distance from the cuticle to the matrix. This is the number of weeks ago the person first had the problem.
Beau’s lines are temporary until the impaired nail formation is corrected (if and when the individual returns to normal health). These lines can also occur as a result of local trauma to the hand or fingers.
In the case of an injury, the dent may be permanent. Hand therapists see this condition most often. If it is not the result of a recent injury, the client may be able to remember sustaining an injury years ago.
Splinter Hemorrhages
Splinter hemorrhages may be the sign of a silent MI or the client may have a known history of MI. These red-brown linear streaks (Fig. 4-34) can also signal other systemic conditions such as bacterial endocarditis, vasculitis, or renal failure.

Fig. 4-34 Splinter hemorrhages. These red-brown streaks, embolic lesions, occur with subacute bacterial endocarditis, sepsis, rheumatoid arthritis, vitamin C deficiency, or hematologic neoplasm. They can occur from local trauma in which case only the injured nail beds will have the telltale streak. Splinter hemorrhages also may be a nonspecific sign. (From Hordinsky MK, Sawaya ME, Scher RK: Atlas of hair and nails, Philadelphia, 2000, Churchill Livingstone.)
In a hospital setting, they are not uncommon in the cardiac care unit (CCU) or other ICU. In such a case, the therapist may just take note of the nail bed changes and correlate it with the pathologic insult probably already a part of the medical record.
When present in only one or two nail beds, local trauma may be linked to the nail bed changes. Asking the client about recent trauma or injury to the hand or fingers may bring this to light.
Whenever splinter hemorrhages are observed in the nails, visually inspect both hands and the toenails as well. If the client cannot recall any recent illness, look for a possible cardiac history or cardiac risk factors. In the case of cardiac risk factors with no known cardiac history, proper medical follow-up and diagnosis is essential in the event the client has had a silent MI.
Leukonychia
Leukonychia, or white nail syndrome, is characterized by dots or lines of white that progress to the free edge of the nail as the nail grows (Fig. 4-35). White nails can be congenital, but more often, they are acquired in association with hypocalcemia, severe hypochromic anemia, Hodgkin’s disease, renal failure, malnutrition from eating disorders, MI, leprosy, hepatic cirrhosis, and arsenic poisoning.

Fig. 4-35 Leukonychia, acquired or inherited white discoloration in the nail. There is a wide range of possibilities in the clinical presentation of leukonychia. Spots, vertical lines, horizontal lines, and even full nail bed changes can occur on individual nail beds of the fingers and/or toes. One or more nails may be affected. (From Jarvis C: Physical examination and health assessment, ed 5, Philadelphia, 2008, WB Saunders.)
Acquired leukonychia is caused by a disturbance to the nail matrix. Repeated trauma, such as keyboard punching, is a more recently described acquired cause of this condition.99 When the entire nail plate is white, the condition is called leukonychia totalis (Case Example 4-2).
Paronychia
Paronychia (not shown) is an infection of the fold of skin at the margin of a nail. There is an obvious red, swollen site of inflammation that is tender or painful. This may be acute as with a bacterial infection or chronic in association with an occupationally induced fungal infection referred to as “wet work” from having the hands submerged in water for long periods of time.
The client may also give a history of finger exposure to chemical irritants, acrylic nails or nail glue, or sculpted nails. Paronychia of one or more fingers is not uncommon in people who pick, bite, or suck their nails. Health care professionals with these nervous habits working in a clinical setting (especially hospitals) are at increased risk for paronychia from infection with bacteria such as Streptococcus or Staphylococcus. Green coloration of the nail may indicate Pseudomonas infection.
Paronychia infections may spread to the pulp space of the finger, developing a painful felon (an infection with localized abscess). Untreated infection can spread to the deep spaces of the hand and beyond.
It is especially important to recognize any nail bed irregularity because it may be a clue to malignancy. Likewise, anyone with diabetes mellitus, immunocompromise, or history of steroids and retroviral use are at increased risk for paronychia formation. Early identification and medical referral are imperative to avoid more serious consequences.
Clubbing
Clubbing of the fingers (Fig. 4-36) and toes usually results from chronic oxygen deprivation in these tissue beds. It is most often observed in clients with advanced chronic obstructive pulmonary disease, congenital heart defects, and cor pulmonale but can occur within 10 days in someone with an acute systemic condition such as a pulmonary abscess, malignancy, or polycythemia. Clubbing may be the first sign of a paraneoplastic syndrome associated with cancer. Clubbing can be assessed by the Schamroth method (Fig. 4-37).

Fig. 4-36 Rapid development of digital clubbing (fingers as shown on the left or toes [not shown]) over the course of a 10-day to 2-week period requires immediate medical evaluation. Clubbing can be assessed using the Schamroth method shown in Fig. 4-37. (From Swartz MH: Textbook of physical diagnosis, ed 6, Philadelphia, 2009, WB Saunders.)
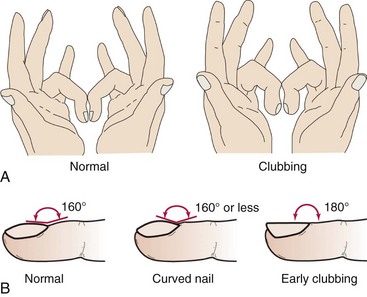
Fig. 4-37 Schamroth method. A, Assessment of clubbing by the Schamroth method. The client places the fingernails of opposite fingers together and holds them up to a light. If the examiner can see a diamond shape between the nails, there is no clubbing. Clubbing is identified by the absence of the diamond shape. It occurs first in the thumb and index finger. B, The index finger is viewed at its profile, and the angle of the nail base is noted (it should be about 160 degrees). The nail base is firm to palpation. Curved nails are a variation of normal with a convex profile. They may look like clubbed nails, but the angle between the nail base and the nail is normal (i.e., 160 degrees or less). Clubbing of nails occurs with congenital chronic cyanotic heart disease, emphysema, cystic fibrosis, and chronic bronchitis. In early clubbing the angle straightens out to 180 degrees, and the nail base feels spongy to palpation. (A from Ignatavicius DD, Bayne MV: Assessment of the cardiovascular system. In Ignatavicius DD, Bayne MV, editors: Medical-surgical nursing, Philadelphia, 1993, WB Saunders. B from Jarvis C: Physical examination and health assessment, Philadelphia, 2004, WB Saunders.)
Any positive findings in the nail beds should be viewed in light of the entire clinical presentation. For example, a positive Schamroth test without observable clinical changes in skin color, capillary refill time, or shape of the fingertips may not signify systemic disease but rather a normal anatomic variation of nail curvature.
Nail Patella Syndrome
Nail patella syndrome (NPS), also called Fong’s disease, hereditary onycho-osteodysplasia (HOOD), or Turner-Kieser syndrome, is a genetic disorder characterized by an absence or underdevelopment of nail bed changes as shown here (Fig. 4-38, A). Lack of skin creases is also a telltale sign (Fig. 4-39).
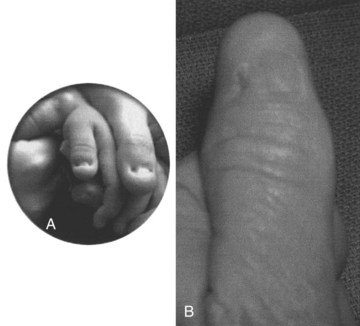
Fig. 4-38 Nail patella syndrome (NPS). Nail bed changes associated with NPS are presented here. Effects vary greatly between individuals but usually involve absence of part or all of the nail bed. For more photos of the skeletal changes associated with NPS, see http://members.aol.com/pacali/NPSpage.html (Accessed October 25, 2005). A, The thumbnails are affected the most with involvement decreasing toward the little finger. Nail changes occur more severely on the ulnar side of the affected nail. Toenails can be affected; it is often the little toenail that is involved.100 B, Note the altered nail bed (more on the ulnar side) and especially the triangular-shaped lunula, a very distinctive sign of NPS. (Courtesy Nail Patella Syndrome Worldwide, 2005.)

Fig. 4-39 Nail changes are the most constant feature of NPS and may be absent, underdeveloped (hypoplastic), or abnormal in size or shape (dysplastic). Alternately, there may be longitudinal ridges, pitting, or discoloration. Note the lack of creases in the distal interphalangeal (DIP) joints of the fingers in this photo. The condition may be present at birth and usually presents symmetrically and bilaterally. (Courtesy Gary Ross, RN, BSN, Board Member, Nail Patella Syndrome Worldwide, 2005.)
Nail abnormalities vary and range from a sliver on each corner of the nail bed to a full nail that is very thick with splits. Some people have brittle, underdeveloped, cracked, or ridged nails while others are absent entirely. They are often concave, causing them to split and flip up, catching on clothing and bedding. Often, the lunula (the light crescent “half-moons” of the nail near the cuticle) are pointed or triangular-shaped (Fig. 4-38, B).
The therapist may be the first to see this condition because skeletal and joint problems are a common feature with this condition. The elbows, hips, and knees are affected most often. Absence or hypoplasia (underdevelopment) of the patella and deformities of the knee joint itself often give them a square shape. Knee instability with patellar dislocation is not uncommon due to malformations in the bones, muscles, and ligaments; there is often much instability in the knee joint.
The client may also develop scoliosis, glaucoma, and kidney disease. Medical referral to establish a diagnosis is important, as clients with NPS need annual screening for renal disease, biannual screening for glaucoma in adulthood, and magnetic resonance imaging (MRI) for orthopedic abnormalities before physical therapy is considered.100
When a client presents with skin or nail bed changes of any kind, taking a personal medical history and reviewing recent (last 6 weeks) and current medications can provide the therapist with important clues in knowing whether to make an immediate medical referral. Table 4-8 provides a summary of the most common skin changes encountered in a physical therapy practice and possible causes for each one.