Vascular System
1 Define and pronounce the key terms and anatomic terms in this chapter.
2 Identify and trace the routes of the blood vessels of the head and neck on a diagram, skull, and patient.
3 Discuss the vascular system pathology associated with the head and neck region.
4 Correctly complete the review questions and activities for this chapter.
5 Integrate an understanding of the head and neck blood supply into clinical dental practice.
(ah-nas-tah-moe-sis, ah-nas-tah-moe-sees) Communication of a blood vessel(s) with another blood vessel(s) by a connecting channel(s).
(kap-i-lare-ee) Smaller blood vessel that branches off an arteriole to supply blood directly to tissue.
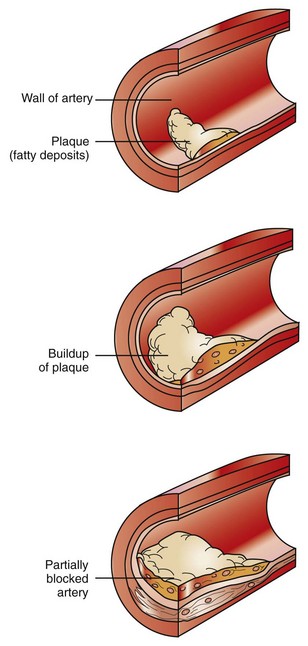
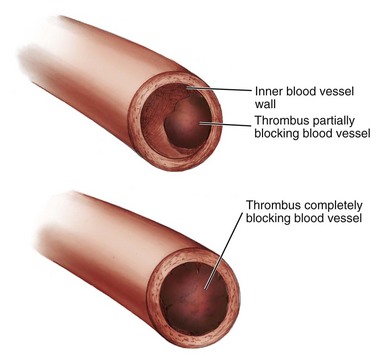
(em-bol-us, em-bol-eye) Foreign material(s) such as a thrombus (or thrombi) traveling in the blood that can block the vessel.
(hee-mah-toe-mah) Bruise that results when a blood vessel is injured and a small amount of blood escapes into the surrounding tissue and clots.
(hem-ah-rij) Large amounts of blood that escape into the surrounding tissue without clotting when a blood vessel is seriously injured.
Substance which consists of cholesterol (mainly), calcium, clotting proteins, and other substances that can be found lining arteries.
Vascular System Overview
The vascular system of the head and neck, as is the case in the rest of the body, consists of an arterial blood supply, a capillary network, and venous drainage. A large network of blood vessels is a plexus. The head and neck area contains certain important venous plexuses. Blood vessels also may communicate with each other by an anastomosis (plural, anastomoses), a connecting channel(s) among the vessels.
An artery is the component of the vascular system that arises from the heart, carrying blood away from it. Each artery starts as a large vessel and branches into smaller vessels, each one a smaller artery or an arteriole. Each arteriole branches into even smaller vessels until it becomes a network of capillaries. Each capillary is smaller than an arteriole and can supply blood to a larger tissue area only because there are so many of them.
A vein is another component of the vascular system. A vein, unlike an artery, travels to the heart and carries blood. Valves in the veins are mostly absent in the head and neck area, unlike in the rest of the body. This leads to two-way flow dictated by local pressure changes, which is the reason that facial or dental infections can lead to serious complications (see Chapter 12). After each smaller vein or venule drains the capillaries of the tissue area, the venules coalesce to become larger veins. Veins are much larger and more numerous than arteries. Veins anastomose freely and have a greater variability in location in comparison with arteries.
There are also different kinds of venous networks found in the body. Superficial veins are found immediately deep to the skin. Deeper veins usually accompany larger arteries in a more protected location within the tissue. Venous sinuses are blood-filled spaces between two layers of tissue. All these venous networks are connected by anastomoses.
Blood vessels are less numerous than lymphatic vessels. However, the pathway of venous blood vessels mainly parallels those of the lymphatic vessels (see Chapter 10). Thus these blood vessels may also spread cancer from a neoplasm to distant sites and at a faster rate than lymphatic vessels.
The dental professional must be able to locate the larger blood vessels of the head and neck because these vessels may become compromised due to a disease process or during a dental procedure such as when administering a local anesthetic injection. Blood vessels may not only spread cancer but can also spread dental or odontogenic infection (see Chapter 12).
Initially, reviewing the pathways of the arteries and veins as they exit and enter the heart is important to understanding the origins of the blood vessels of the head and neck. After the origins of blood supply to the head and neck are understood, diagrams of the blood vessels overlying the skull figure are helpful in studying this system. Correlating the tissue or organ supplied with the area’s blood vessels is an additional way of understanding the location of the various blood vessels. It is important to remember that, unlike innervation to the muscles, which is a one-to-one relationship, blood supply is more regional in coverage. Arteries supply all structures in their vicinity, and veins receive blood from all nearby structures.
Arterial Blood Supply To Head And Neck
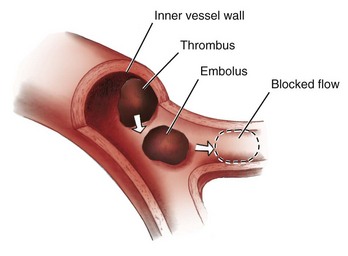
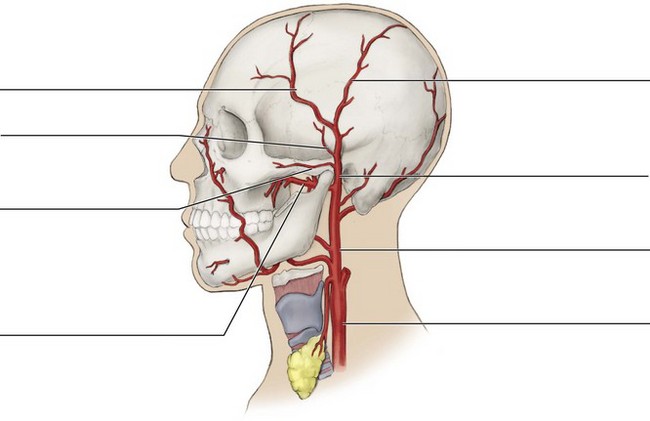
The major arteries that supply the head and neck include the common carotid and subclavian arteries. The origins from the heart to the head and neck of these two major arteries are different depending on the side of the body; in contrast, the other branching arteries of the head and neck are symmetric in their coverage.
Origins to Head and Neck
The origins from the heart of the common carotid and subclavian arteries that supply the head and neck are different for the right and left sides of the body (Figure 6-1). For the left side of the body, the common carotid and subclavian arteries arise directly from the aorta (ay-or-tah). For the right side of the body, the common carotid and subclavian arteries are both branches from the brachiocephalic artery. The brachiocephalic artery (bray-kee-o-sah-fal-ik) is a direct branch of the aorta.
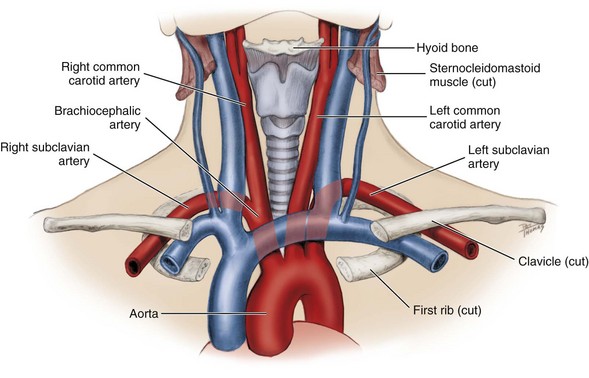
FIGURE 6-1 Origins from the heart of the arterial blood supply for the head and neck highlighting (red) the pathways of the common carotid and subclavian arteries contrasted with adjacent venous drainage (blue). Note that these pathways are different for these major arteries within either the right or left sides of the body.
The common carotid artery (kah-rot-id) is branchless and travels superiorly along the neck, lateral to the trachea and larynx, to the superior border of the thyroid cartilage (see Figure 6-1). The common carotid artery travels in a sheath deep to the sternocleidomastoid muscle; this sheath also contains the internal jugular vein and the tenth cranial or vagus nerve. The common carotid artery ends by dividing into the internal and external carotid arteries at about the level of the larynx (Figure 6-2).
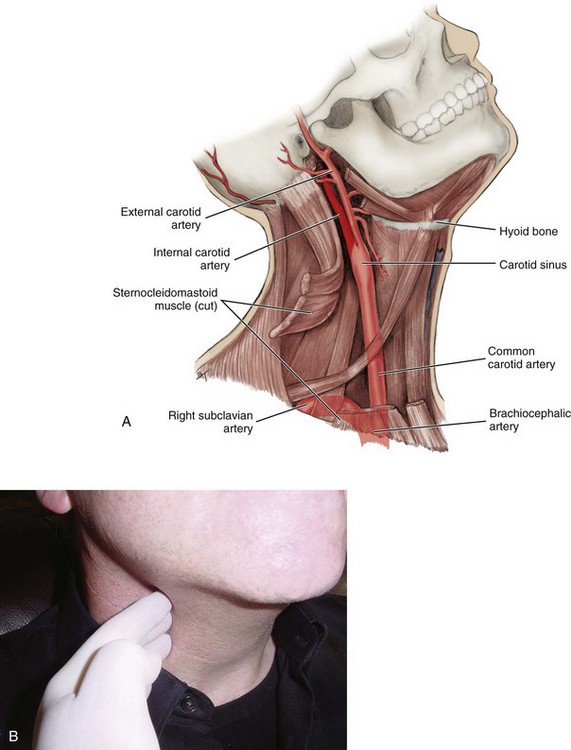
FIGURE 6-2 Pathway of the internal carotid artery after branching off from the common carotid artery (A). Location of carotid pulse that is palpated by emergency medical service personnel during an emergency. However, this compression should be avoided by dental personnel (B).
Just before the common carotid artery bifurcates into the internal and external carotid arteries, it exhibits a swelling, the carotid sinus (see Figure 6-2). When the common carotid artery is palpated against the larynx, the most reliable arterial pulse of the body can be monitored. If the anterior border of the sternocleidomastoid muscle is rolled posteriorly at the level of the thyroid cartilage of the larynx or “Adam’s apple,” the carotid pulse can be felt in the groove of tissue produced. This pulse is the most reliable on the surface of the body because the common carotid is a major artery supplying the brain. In an emergency (such as with basic life support), the common carotid remains palpable by qualified emergency medical service (EMS) personnel when peripheral arteries such as the radial artery are not. However, care must be taken to avoid compression of either the carotid sinus or one or both carotid arteries unless it is an emergency situation. Instead, dental personnel can continue to safely use the radial artery to record a patient’s baseline pulse.
The subclavian artery (sub-klay-vee-an) arises lateral to the common carotid artery (see Figure 6-1). The subclavian artery gives rise to branches that supply both intracranial and extracranial structures, but its major destination is the upper extremity (arm).
Internal Carotid Artery
The internal carotid artery is a division that travels superiorly in a slightly lateral position (in relationship to the external carotid artery) after leaving the common carotid artery (see Figure 6-2). This artery is hidden by the coverage of the large sternocleidomastoid muscle of the neck. The internal carotid artery has no branches in the neck but continues adjacent to the internal jugular vein within the carotid sheath to the skull base, where it enters the cranium. The internal carotid artery supplies intracranial structures and is the source of the ophthalmic artery (of-thal-mic), which supplies the eye, orbit, and lacrimal gland.
External Carotid Artery
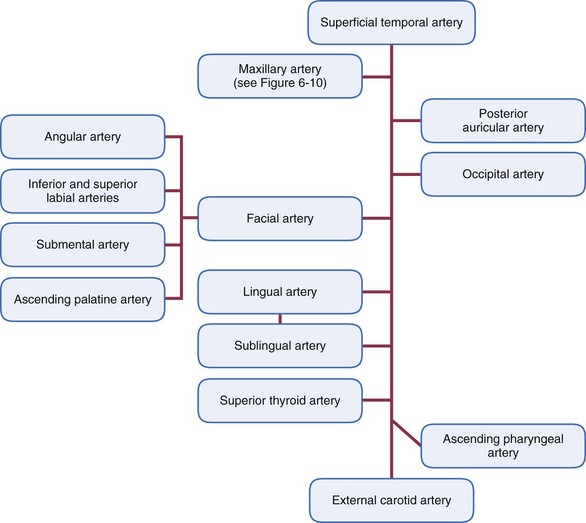
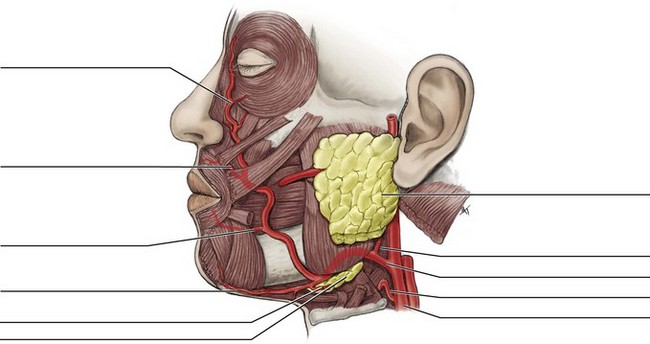
As with the internal carotid artery, the external carotid artery begins at the superior border of the thyroid cartilage, at the termination of the common carotid artery and the carotid sheath. The external carotid artery travels superiorly in a more medial position (in relationship to the internal carotid artery) after arising from the common carotid artery (Figures 6-3 and 6-4). The external carotid artery supplies the extracranial tissue of the head and neck, including the oral cavity. The external carotid artery has four sets of branches grouped according to their location to the main artery: anterior, medial, posterior, and terminal (Table 6-1).
Table 6-1
External Carotid Artery Branches
| BRANCHES OF EXTERNAL CAROTID ARTERY | POSITION OF BRANCHES | FURTHER BRANCHES |
| Superior thyroid | Anterior | Infrahyoid, sternocleidomastoid, superior laryngeal, cricothyroid |
| Lingual | Anterior | Dorsal lingual, deep lingual, sublingual, suprahyoid, tonsillar |
| Facial | Anterior | Ascending palatine, glandular, submental, inferior labial, superior labial, angular, tonsillar |
| Ascending pharyngeal | Medial | Pharyngeal, meningeal, tonsillar |
| Occipital | Posterior | Muscular, sternocleidomastoid, auricular, meningeal |
| Posterior auricular | Posterior | Auricular, stylomastoid |
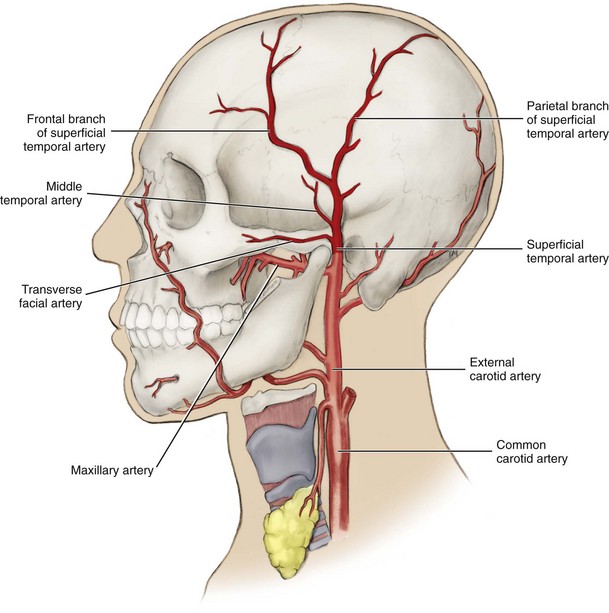
| Superficial temporal | Terminal | Transverse facial, middle temporal, frontal, parietal |
| Maxillary | Terminal | See Table 6-2 |
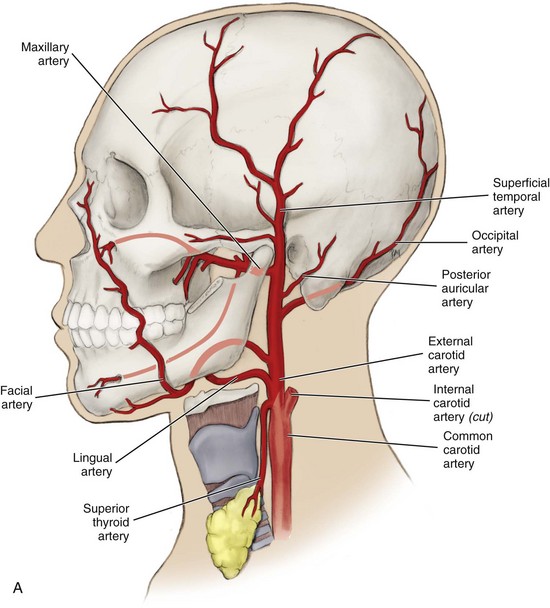
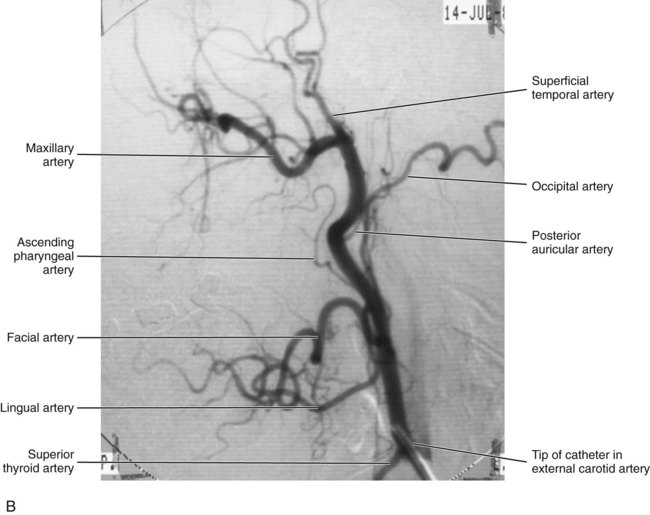
FIGURE 6-3 Pathway of the external carotid artery after branching off the common carotid artery (the medial branch of external carotid artery, ascending pharyngeal artery cannot be seen) (A). Lateral projection arteriogram of external carotid artery (B). (B from Logan BM, Reynolds PA: McMinn’s color atlas of head and neck anatomy, 4 ed, St Louis, 2010, Mosby Ltd.)
Anterior Branches Of External Carotid Artery
There are three anterior branches from the external carotid artery: the superior thyroid, the lingual, and the facial branches (see Figure 6-4). The lingual and facial arteries divide serving areas of the head and neck and are of interest to dental professionals.
Superior Thyroid Artery
The superior thyroid artery (thy-roid) is an anterior branch from the external carotid artery (see Figures 6-3 and 6-5). The superior thyroid artery has four branches: the infrahyoid artery, the sternocleidomastoid branch, the superior laryngeal artery, and the cricothyroid branch. These branches supply the tissue inferior to the hyoid bone including: the infrahyoid muscles, the sternocleidomastoid muscle, the muscles of the larynx, and the thyroid gland.
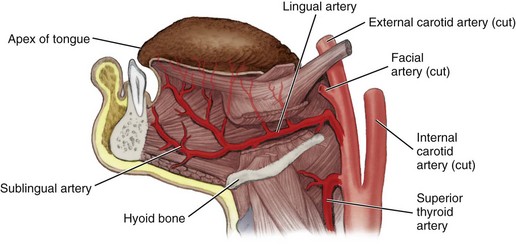
Lingual Artery.: The lingual artery is an anterior branch from the external carotid artery and arises superior to the superior thyroid artery at the level of the hyoid bone (Figure 6-5; see Figure 6-3). The lingual artery travels anteriorly to the apex of the tongue by way of its inferior surface. The lingual artery supplies the tissue superior to the hyoid bone including the suprahyoid muscles and floor of the mouth by the dorsal lingual, deep lingual, sublingual, and suprahyoid branches.
The tongue is also supplied by branches of the lingual artery including several small dorsal lingual branches to the base and body and the deep lingual artery, the terminal part of the lingual artery, to the apex. It also has tonsillar branches.
The sublingual artery (sub-ling-gwal) supplies the mylohyoid muscle, sublingual salivary gland, and mucous membranes of the floor of the mouth. The small suprahyoid branch supplies the suprahyoid muscles.
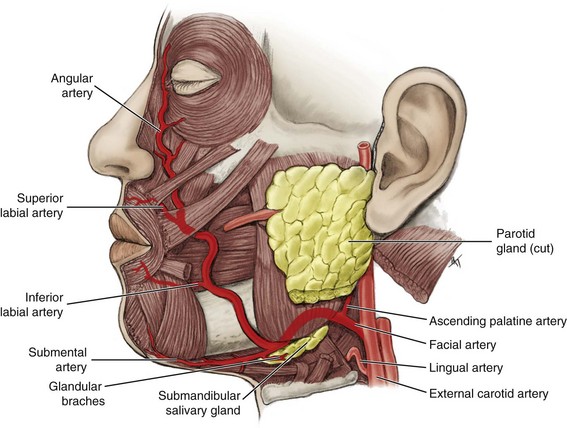
Facial Artery.: The facial artery or external maxillary artery is the final anterior branch from the external carotid artery (Figure 6-6; see Figure 6-3). The facial artery arises slightly superior to the lingual artery as it branches off anteriorly; however, in some cases the facial and lingual arteries share a common trunk. The facial artery has a complicated path as it runs medial to the mandible, over the submandibular salivary gland, and then around the mandible’s inferior border to its lateral side.
From the inferior border of the mandible, the facial artery runs anteriorly and superiorly near the angle of the mouth and along the side of the nose. The facial artery terminates at the medial canthus. Thus the facial artery supplies the face in the oral, buccal, zygomatic, nasal, infraorbital, and orbital regions.
The facial artery is mainly parallel to the facial vein in the head area, although both blood vessels do not run adjacent to each other (see Figure 6-12). In the neck, the artery is separated from the vein by the posterior belly of the digastric muscle, stylohyoid muscle, and submandibular salivary gland. The facial artery’s major branches include: the ascending palatine, the glandular branches, the submental, the inferior labial, the superior labial, angular, and tonsillar.
The ascending palatine artery (ah-send-ing pal-ah-tine) is the first branch from the facial artery (see Figure 6-6). The ascending palatine artery supplies the soft palate, palatine muscles, and palatine tonsils and can be the source of serious blood loss or hemorrhage if it is injured during tonsillectomy (blood vessel pathology is discussed later).
The glandular branches and submental artery (sub-men-tal) are branches from the facial artery that supply the submandibular lymph nodes, submandibular salivary gland, and mylohyoid and digastric muscles.
The inferior labial artery is another branch from the facial artery that supplies the lower lip area including the muscles of facial expression such as the depressor anguli oris muscle. The superior labial artery is also a branch from the facial artery that supplies the upper lip tissue.
The angular artery (ang-u-lar) is the terminal branch of the facial artery and supplies the side of the nose (see Figure 6-6).
Medial Branch Of External Carotid Artery
Only one medial branch is from the external carotid artery, the small ascending pharyngeal artery (fah-rin-je-al) that arises close to the origin of the external carotid artery and cannot be seen in most lateral views of the head and neck (see Figure 6-3, B). The ascending pharyngeal artery has many small branches that include: the pharyngeal branch and meningeal branch (me-nin-je-al). These branches supply the pharyngeal walls (where they anastomose with the ascending palatine artery), soft palate, and meninges. It also has tonsillar branches, which can be a source of serious blood loss or hemorrhage during a tonsillectomy.
Posterior Branches Of External Carotid Artery
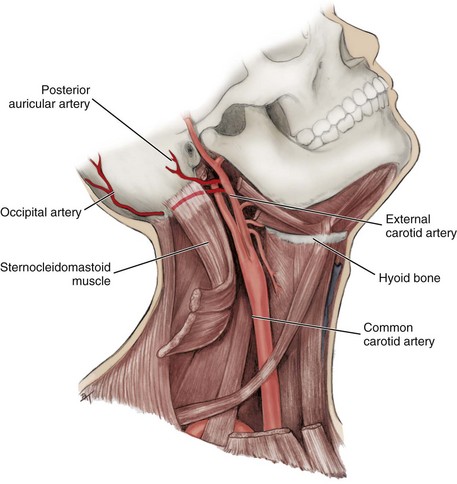
There are two posterior branches of the external carotid artery: the occipital and posterior auricular (Figure 6-7).
Occipital Artery.: The occipital artery (ok-sip-it-al), a posterior branch of the external carotid artery, arises from the external carotid artery as it passes superiorly just deep to the ascending ramus of the mandible and then travels to the posterior part of the scalp (see Figure 6-7). The occipital artery supplies the suprahyoid and sternocleidomastoid muscles, as well as the scalp and meninges in the occipital region. The artery supplies these regions through the muscular branches, sternocleidomastoid branches (stir-no-klii-do-mass-toid), auricular branches (aw-rik-yule-lar), and meningeal branches. At its origin, the occipital artery is adjacent to the twelfth cranial or hypoglossal nerve.
Posterior Auricular Artery.: The small posterior auricular artery is also a posterior branch of the external carotid artery (see Figure 6-7). The posterior auricular artery arises superior to the occipital artery and stylohyoid muscle at about the level of the tip of the styloid process. The posterior auricular artery supplies the internal ear by its auricular branch and the mastoid air cells by the stylomastoid artery (sty-lo-mass-toid).
Terminal Branches Of External Carotid Artery
The two terminal branches of the external carotid artery include the superficial temporal and maxillary (Figures 6-8, 6-9, and 6-10). The external carotid artery splits into these terminal branches within the parotid salivary gland. In addition, both terminal branches give rise to many important arteries in the head and neck area.
Superficial Temporal Artery.: The superficial temporal artery (tem-poh-ral) is the smaller terminal branch of the external carotid artery (see Figure 6-8). The artery arises within the parotid salivary gland. This artery can be visible under the skin of the temporal region in the patient. The superficial temporal artery has several branches including: the transverse facial artery, the middle temporal artery, the frontal branch, and the parietal branch.
The small transverse facial artery supplies the parotid salivary gland duct and nearby facial tissue. The equally small middle temporal artery supplies the temporalis muscle. The frontal branch (frunt-il) and parietal branch (pah-ry-it-il) both supply parts of the scalp in the frontal and parietal regions.
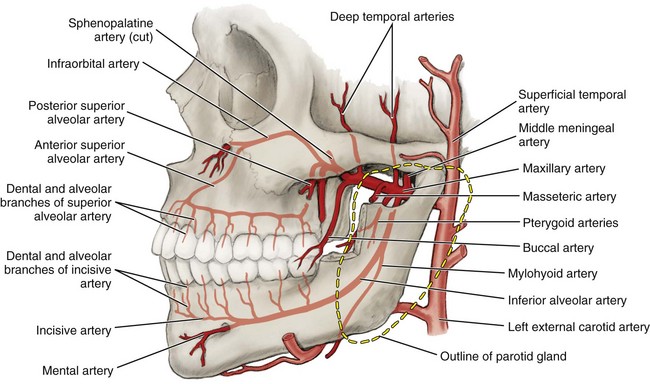
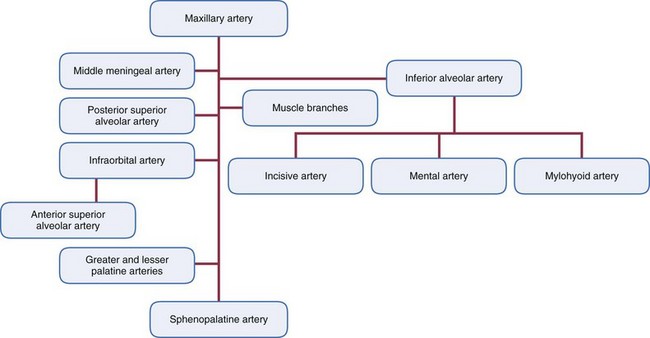
Maxillary Artery.: The maxillary artery (mak-sil-lare-ee) or internal maxillary artery is the larger terminal branch of the external carotid artery with three parts defined by location (see Figures 6-9, 6-10 and 6-11). The first part (or mandibular part) of maxillary artery begins at the neck of the mandibular condyle within the parotid salivary gland. The second part of the maxillary artery runs between the mandible and the sphenomandibular ligament anteriorly and superiorly through the infratemporal fossa (see Figure 3-61). The artery may run either superficial or deep to the lateral pterygoid muscle.
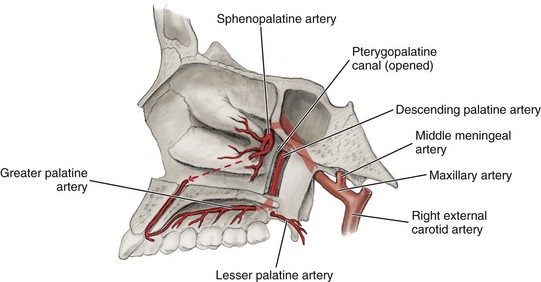
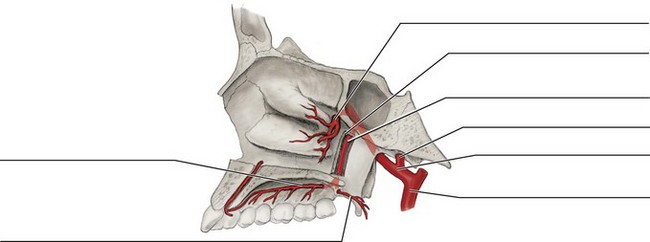
FIGURE 6-11 Pathways of the greater palatine artery, lesser palatine artery, and sphenopalatine artery.
Within the infratemporal fossa, the maxillary artery gives rise to many branches. These branches of the second part (or pterygoid part) of the maxillary artery within the infratemporal fossa include the middle meningeal and inferior alveolar arteries and several arteries to muscles (Table 6-2). The middle meningeal artery supplies the meninges of the brain by way of the foramen spinosum, located on the inferior surface of the skull, as well as the skull bones (see Figure 6-9).
TABLE 6-2
| MAJOR BRANCHES OF MAXILLARY ARTERY | FURTHER BRANCHES | TISSUE SUPPLIED |
| Middle meningeal | Meninges (or dural mater) and bones of vault | |
| Inferior alveolar | Mylohyoid, mental, and incisive | Mandibular teeth, mouth floor, and mental region |
| Deep temporal(s) | Temporalis muscle | |
| Pterygoid(s) | Lateral and medial pterygoid muscles | |
| Masseteric | Masseter muscle | |
| Buccal | Buccinator muscle and buccal region | |
| Posterior superior alveolar | Maxillary posterior teeth and maxillary sinus | |
| Infraorbital | Orbital and anterior superior alveolar | Orbital region, face, and maxillary anterior teeth |
| Greater palatine | Lesser palatine(s) | Hard and soft palates |
| Sphenopalatine | Lateral nasal, septal, and nasopalatine | Nasal cavity and anterior hard palate |
The inferior alveolar artery (al-vee-o-lar) also arises from the maxillary artery in the infratemporal fossa (see Figures 6-9 and 9-38). The artery turns inferiorly to enter the mandibular foramen and then the mandibular canal, along with the inferior alveolar nerve. The mylohyoid artery branches from the inferior alveolar artery before it enters the canal.
The mylohyoid artery (my-lo-hi-oid) arises from the inferior alveolar artery before the main artery enters the mandibular canal by way of the mandibular foramen (see Figure 6-9). The mylohyoid artery travels in the mylohyoid groove on the inner surface of the mandible and supplies the floor of the mouth and the mylohyoid muscle.
Within the mandibular canal, the inferior alveolar artery gives rise to dental and alveolar branches (see Figure 6-9). The dental branches of the inferior alveolar artery supply the pulp of the mandibular posterior teeth by way of each tooth’s apical foramen. The alveolar branches of the inferior alveolar artery supply the periodontium of the mandibular posterior teeth, including the gingiva. The inferior alveolar artery then branches into two arteries within the mandibular canal: the mental and incisive.
The mental artery (ment-il) arises from the inferior alveolar artery and exits the mandibular canal by way of the mental foramen (see Figure 6-9). The mental foramen is located on the outer surface of the mandible, usually deep to the apices of the mandibular first and second premolar teeth. After the mental artery exits the canal, the artery supplies the tissue of the chin and anastomoses with the inferior labial artery.
The incisive artery (in-sy-ziv) branches off the inferior alveolar artery, remaining within the mandibular canal to divide into dental and alveolar branches (see Figure 6-9). The dental branches of the incisive artery supply the pulp of the mandibular anterior teeth by way of each tooth’s apical foramen. The alveolar branches of the incisive artery supply the periodontium of the mandibular anterior teeth, including the gingiva, and anastomose with the alveolar branches of the incisive artery on the other side.
The second part of the maxillary artery also has branches that are located near the muscle they supply (see Figure 6-9). These arteries all accompany branches of the mandibular nerve (or division) of the fifth cranial or trigeminal nerve. The deep temporal arteries (tem-poh-ral) supply the anterior and posterior parts of the temporalis muscle. The pterygoid arteries (teh-ri-goid) supply the lateral and medial pterygoid muscles. The masseteric artery (mass-et-tehr-ik) supplies the masseter muscle. The buccal artery supplies the buccinator muscle and other soft tissue of the cheek.
After traversing the infratemporal fossa, the maxillary artery enters the pterygopalatine fossa, which is deep and inferior to the eye (see Figure 3-61). Just as the maxillary artery leaves the infratemporal fossa and enters the pterygopalatine fossa as the third part (or pterygopalatine part), it gives rise to the posterior superior alveolar artery (see Figures 6-9 and 9-7). This artery then enters the posterior superior alveolar foramina on the maxillary tuberosity, giving rise to dental branches and alveolar branches. The posterior alveolar superior alveolar artery also anastomoses with the anterior superior alveolar artery.
The dental branches of the posterior superior alveolar artery supply the pulp of the maxillary posterior teeth by way of each tooth’s apical foramen. The alveolar branches of the posterior superior alveolar artery supply the periodontium of the maxillary posterior teeth, including the gingiva. Some branches also supply the maxillary sinus.
The infraorbital artery (in-frah-or-bit-al) also branches from the third part of the maxillary artery in the pterygopalatine fossa and may share a common trunk with the posterior superior alveolar artery (see Figure 6-9). The infraorbital artery then enters the orbit through the inferior orbital fissure. While in the orbit, the artery travels in the infraorbital canal. Within the canal, the infraorbital artery provides orbital branches to the orbit and gives rise to the anterior superior alveolar artery.
The anterior superior alveolar artery arises from the infraorbital artery and gives rise to dental and alveolar branches (see Figure 6-9). The anterior superior alveolar artery also anastomoses with the posterior superior alveolar artery.
The dental branches of the anterior superior alveolar artery supply the pulp of the maxillary anterior teeth by way of each tooth’s apical foramen. The alveolar branches of the anterior superior alveolar artery supply the periodontium of the maxillary anterior teeth, including the gingiva.
After giving off these branches in the infraorbital canal, the infraorbital artery emerges onto the face from the infraorbital foramen (see Figure 6-9). The artery’s terminal branches supply parts of the infraorbital region of the face and anastomose with the facial artery.
Also in the pterygopalatine fossa, the third part of the maxillary artery gives rise to the descending palatine artery (pal-ah-tine), which travels to the palate through the pterygopalatine canal which then terminates in both the greater palatine artery and lesser palatine artery by way of the greater and lesser palatine foramina to supply the hard and soft palates, respectively (Figure 6-11).
The maxillary artery ends by becoming the sphenopalatine artery (sfe-no-pal-ah-tine), its main terminal branch, which supplies the nasal cavity by way of the sphenopalatine foramen. The sphenopalatine artery gives rise to the posterior lateral nasal branches and septal branches, including a nasopalatine branch (nay-zo-pal-ah-tine) that accompanies the nasopalatine nerve through the incisive foramen on the maxillae (see Figure 6-11).
Venous Drainage Of Head And Neck
The veins of the head and neck start out as small venules and become larger as they near the base of the neck on their way to the heart. The veins of the head and upper neck are usually symmetric in their coverage on each side of the body but have a greater variability in location than do the arteries, anastomosing freely. Veins are also generally larger and more numerous than arteries in the same tissue area.
The internal jugular vein drains the brain as well as most of the other tissue of the head and neck (Table 6-3), whereas the external jugular vein drains only a small part of the extracranial tissue. However, the two veins have many anastomoses. The beginnings of both veins are discussed initially and, later, their route to the heart is discussed.
TABLE 6-3
| REGION OR TRIBUTARIES DRAINED | DRAINAGE VEINS | MAJOR VEINS |
| Meninges of brain (only dura mater layer and vault bones) | Middle meningeal | Pterygoid plexus |
| Lateral scalp area | Superficial temporal and posterior auricular | Retromandibular and external jugular |
| Frontal region | Supratrochlear and supraorbital | Facial and ophthalmic |
| Orbital region | Ophthalmic(s) | Cavernous sinus and pterygoid plexus |
| Superficial temporal and maxillary veins | Retromandibular | External jugular |
| Upper lip area | Superior labial | Facial |
| Maxillary teeth | Posterior superior alveolar | Pterygoid plexus |
| Lower lip area | Inferior labial | Facial |
| Mandibular teeth and submental region | Inferior alveolar | Pterygoid plexus |
| Submental region | Submental | Facial |
| Lingual and sublingual regions | Lingual | Facial or internal jugular |
| Deep facial areas and posterior superior alveolar and inferior alveolar veins | Pterygoid plexus | Maxillary |
| Pterygoid plexus of veins | Maxillary | Retromandibular |
Facial Vein
The facial vein drains into the internal jugular vein, which is discussed later (Figure 6-12). The facial vein begins at the medial corner of the eye with the junction of two veins from the frontal region, the supratrochlear vein (soo-prah-trok-lere) and supraorbital vein (soo-prah-or-bit-al). The supraorbital vein also anastomoses with the ophthalmic veins. The ophthalmic veins (of-thal-mic) drain the tissue of the orbit. This anastomosis provides a communication with the cavernous sinus, which may become fatally infected through the spread of dental infection (discussed later, see also Figure 12-9). This is especially significant because the facial vein, like other veins of the head, has no valves to control the direction of blood flow; this may allow the backflow of infectious materials.
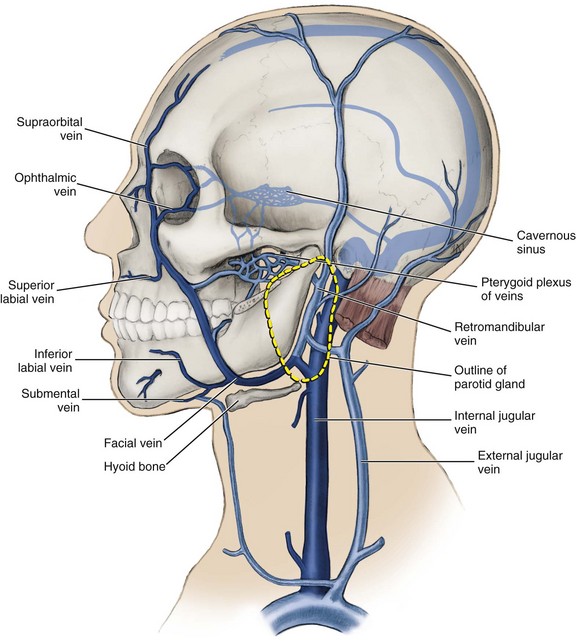
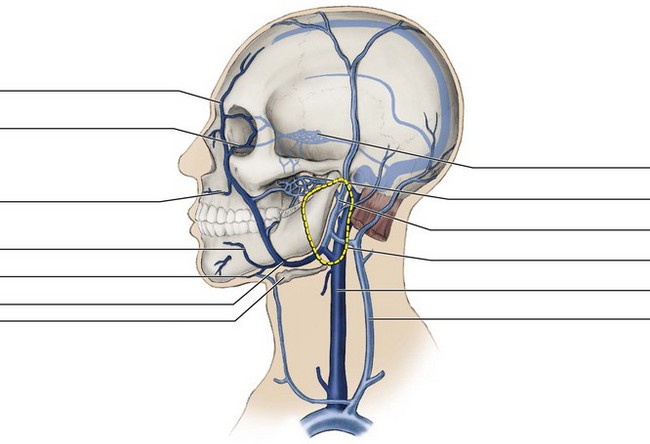
FIGURE 6-12 Pathways of the internal jugular vein and facial vein, as well as the location of the cavernous sinus.
The facial vein receives branches from the same areas of the face that are supplied by the facial artery. This vein anastomoses with the deep veins such as the pterygoid plexus in the infratemporal fossa and with the large retromandibular vein before joining the internal jugular vein at the level of the hyoid bone (discussed later).
The facial vein has some important tributaries in the oral region (see Figure 6-12). The superior labial vein drains the upper lip; the inferior labial vein drains the lower lip. The submental vein (sub-men-tal) drains the tissue of the chin as well as the submandibular region.
One excellent example of the venous variability concerns the lingual veins. These include the dorsal lingual veins that drain the dorsal surface of the tongue, the highly visible deeper lingual veins that drain the ventral surface of the tongue, and the sublingual veins that drain the floor of the mouth (see Figure 2-18). These lingual veins may join to form a single vessel or may empty into larger vessels separately; they also may drain indirectly into the facial vein or directly into the internal jugular vein.
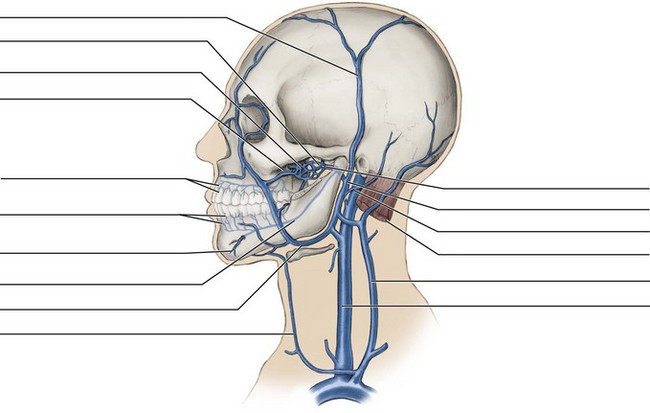
Retromandibular Vein
The retromandibular vein (reh-tro-man-dib-you-lar) will form the external jugular vein from a part of its route. The retromandibular vein is formed from the merger of the superficial temporal vein and maxillary vein (Figure 6-13). The retromandibular vein emerges from the parotid salivary gland and courses inferiorly. This vein and its beginning venules drain areas similar to those supplied by the superficial temporal and maxillary arteries.
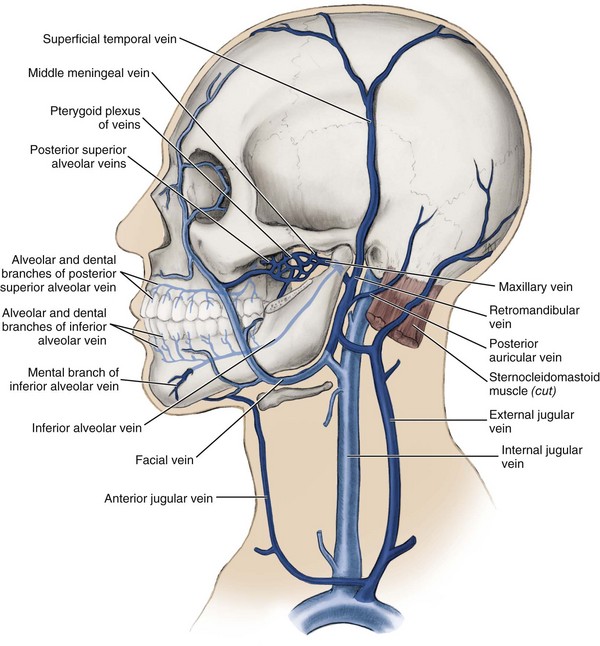
FIGURE 6-13 Pathways of the retromandibular vein and external jugular vein including the anterior jugular vein.
Inferior to the parotid, the retromandibular vein usually divides (see Figure 6-13). The anterior division joins the facial vein, and the posterior division continues its inferior course on the surface of the sternocleidomastoid muscle. After being joined by the posterior auricular vein (aw-rik-you-lar), which drains the lateral scalp posterior to the ear, this posterior division of the retromandibular veins becomes the external jugular vein (discussed later).
Superficial Temporal Vein
The superficial temporal vein (tem-poh-ral) drains the lateral scalp and is superficially located (see Figure 6-13). The superficial temporal vein goes on to drain into and form the retromandibular vein, along with the deeper maxillary vein.
Maxillary Vein
The maxillary vein (mak-sil-lare-ee) or internal maxillary vein is deeper than the superficial temporal vein and begins in the infratemporal fossa by collecting blood from the pterygoid plexus, accompanying the maxillary artery (see Figure 6-13). Through the pterygoid plexus, the maxillary vein receives the middle meningeal, posterior superior alveolar, inferior alveolar, and other veins such as those from the nasal cavity and palate (those areas served by the maxillary artery). After receiving these veins, the maxillary vein merges with the superficial temporal vein to drain into and form the retromandibular vein.
Pterygoid Plexus of Veins.: The pterygoid plexus of veins (ter-i-goid) is a collection of small anastomosing vessels located around the pterygoid muscles and surrounding the second part (or pterygoid part) of the maxillary artery on each side of the face within the infratemporal fossa (see Figure 6-13). This plexus anastomoses with both the facial and retromandibular veins. The pterygoid plexus protects the maxillary artery from being compressed during mastication; by either filling or emptying, the pterygoid plexus can accommodate changes in volume of the infratemporal fossa that occur when the mandible moves.
The pterygoid plexus drains the veins from the deep parts of the face and then drains into the maxillary vein. The middle meningeal vein also drains the blood from both the dura mater of the meninges (not the arachnoid or pia mater) and the bones of the vault into the pterygoid plexus of veins.
Some parts of the pterygoid plexus of veins are near the maxillary tuberosity, reflecting the drainage of dental tissue into the plexus. Thus there is a possibility of piercing the pterygoid plexus of veins when a posterior superior alveolar block is incorrectly administered with the needle being overinserted (see Figure 9-7). When the pterygoid plexus of veins is pierced such as in this situation, a small amount of the blood escapes and enters the tissue, causing tissue tenderness, swelling, and the discoloration of a hematoma (discussed later).
A spread of dental or odontogenic infection along the needle tract deep into the tissue can also occur when the posterior superior alveolar block is incorrectly administered. This may involve a serious spread of infection to the cavernous sinus (discussed later; and see also Chapter 12).
Posterior Superior Alveolar Vein.: The pterygoid plexus of veins also drains the posterior superior alveolar vein, which is formed by the merging of its dental and alveolar branches (see Figure 6-13). The dental branches of the posterior superior alveolar vein drain the pulp of the maxillary teeth by way of each tooth’s apical foramen. The alveolar branches of the posterior alveolar vein drain the periodontium of the maxillary teeth, including the gingiva.
Inferior Alveolar Vein.: The inferior alveolar vein forms from the merging of its dental branches, alveolar branches, and mental branches in the mandible, where they also drain into the pterygoid plexus (see Figure 6-13). The dental branches of the inferior alveolar vein drain the pulp of the mandibular teeth by way of each tooth’s apical foramen. The alveolar branches of the inferior alveolar vein drain the periodontium of the mandibular teeth, including the gingiva.
The mental branches of the inferior alveolar vein enter the mental foramen after draining the chin area on the outer surface of the mandible, where they anastomose with branches of the facial vein. The mental foramen is on the surface of the mandible, usually inferior to the apices of the mandibular first and second premolars.
Venous Sinuses
The venous sinuses in the brain are located in the meninges. Being more specific, these sinuses are within the dura mater of the brain, a dense connective tissue that lines the inside of the cranium (see Figure 8-4). These dural sinuses are channels by which blood is conveyed from the cerebral veins into the veins of the neck, particularly the internal jugular vein.
The venous sinus most important to dental care is the cavernous sinus (kav-er-nus) located on the lateral surface of the body of the sphenoid bone (see Figure 6-12). Each cavernous sinus communicates by anastomoses with the contralateral sinus and also with the pterygoid plexus of veins and superior ophthalmic vein, which anastomoses with the facial vein. The internal carotid artery and certain cranial nerves or their branches (III, IV, V1, V2 and VI) pass through this blood-filled space; it is the only anatomic location in which an artery travels completely through a venous structure. This sinus is important to dental professionals since the cavernous sinus may be involved with the spread of dental or odontogenic infection, which can lead to fatal results (see Figure 12-9).
Internal Jugular Vein
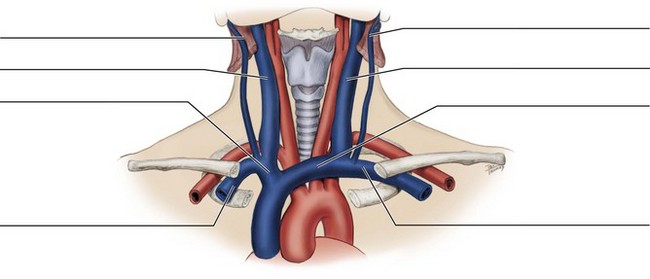
The internal jugular vein (jug-you-lar) drains most of the tissue of the head and neck (Figure 6-14; see Figure 6-12). As mentioned earlier, the internal jugular vein, unlike many veins in other parts of the body, does not have any one-way valves, nor do any head and neck veins (except for the external jugular vein discussed next). Not having any valves to prevent the backward flow of blood, this vein may become involved with the spread of infection (see Chapter 12).
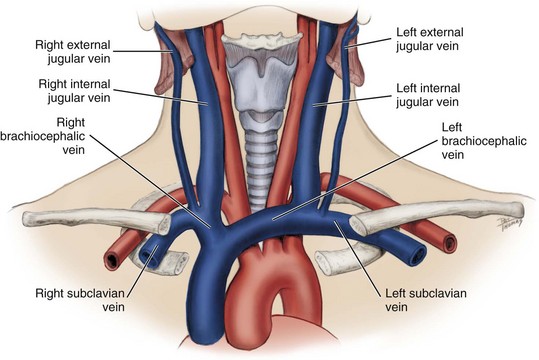
FIGURE 6-14 Pathways to the heart from the head and neck of the venous drainage (blue) including the external and internal jugular veins, subclavian vein, brachiocephalic veins, and superior vena cava contrasted with the adjacent arterial supply (red).
The internal jugular vein originates in the cranial cavity and leaves the skull through the jugular foramen. It receives many tributaries including the veins from the lingual, sublingual, and pharyngeal areas as well as the facial vein. The internal jugular vein runs with the common carotid artery and its branches as well as the vagus nerve in the carotid sheath (see Figure 11-3). Within the carotid sheath, the deep cervical group of lymph nodes forms a chain along the internal jugular vein. The internal jugular vein descends in the neck to merge with the subclavian vein.
External Jugular Vein
As mentioned earlier, the posterior division of the retromandibular vein becomes the external jugular vein. The external jugular vein continues the descent inferiorly along the neck, terminating in the subclavian vein (see Figures 6-13 and 6-14). Unlike the rest of the veins of the head and neck, the external jugular vein is the one that has valves, which are near its entry into the subclavian vein. Usually the external jugular vein is visible as it crosses the large sternocleidomastoid muscle; to increase its visibility, it can be distended by gentle supraclavicular digital pressure to block outflow (see Figure 4-2).
The anterior jugular vein drains into the external jugular vein (or directly into the subclavian vein) before it joins the subclavian vein (see Figure 6-13). The anterior jugular vein begins inferior to the chin, communicating with veins in the area, and descends near the midline within the superficial fascia, receiving branches from the superficial cervical structures. Only one anterior jugular vein may be present, but usually two veins are present, anastomosing with each other through a jugular venous arch.
Pathways to Heart from Head and Neck
On each side of the body, the external jugular vein joins the subclavian vein from the arm, and then the internal jugular vein merges with the subclavian vein (sub-klay-vee-an) to form the brachiocephalic vein (bray-kee-oo-sah-fal-ik) (see Figure 6-14). The brachiocephalic veins unite to form the superior vena cava (vee-na kay-va) and then travel to the heart. Because the superior vena cava is on the right side of the heart, the brachiocephalic veins are asymmetric. The right brachiocephalic vein is short and vertical, and the left brachiocephalic vein is long and horizontal.
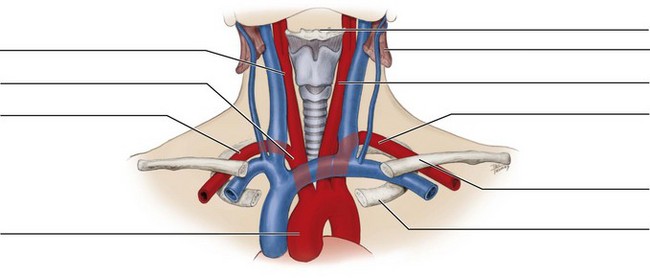
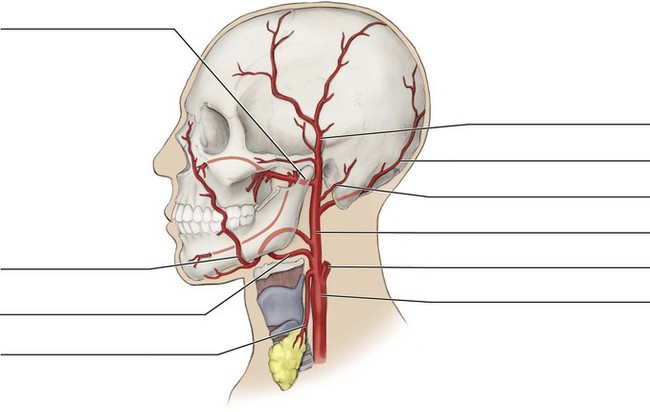
Identification Exercises
Identify the structures on the following diagrams by filling in each blank with the correct anatomic term. You can check your answers by looking back at the figure indicated in parentheses for each identification diagram.
1. (Figure 6-1)
2. (Figure 6-3, A)
3. (Figure 6-5)
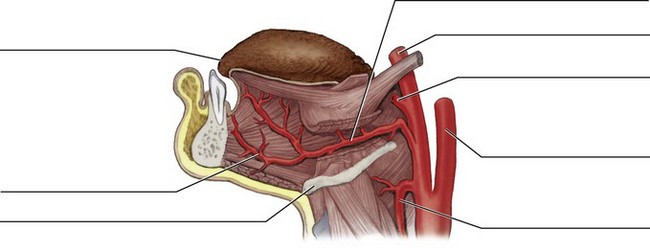
4. (Figure 6-6)
5. (Figure 6-8)
6. (Figure 6-9)
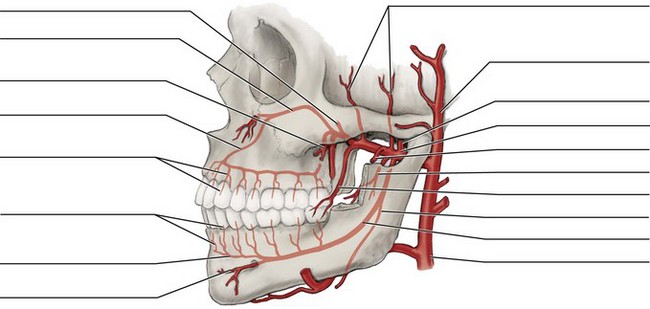
7. (Figure 6-11)
8. (Figure 6-12)
9. (Figure 6-13)
10. (Figure 6-14)
1. The posterior superior alveolar artery and its branches supply the
A maxillary posterior teeth and periodontium.
B mandibular posterior teeth and periodontium.
2. Which of the following descriptions concerning the pterygoid plexus is CORRECT?
A Located around the infrahyoid muscles
B Protects the superficial temporal artery
3. Which of the following veins results from the merger of the superficial temporal vein and maxillary vein?
4. Which of the following arteries arises from the inferior alveolar artery before the artery enters the mandibular canal?
5. Which of the following artery and transmitting foramen pairs below is a CORRECT match?
A Buccal artery–infraorbital foramen
B Middle meningeal artery–foramen spinosum
C Incisive artery–mental foramen
6. Which of the following arteries supply the mucous membranes and glands of the hard and soft palates?
A Greater and lesser palatine arteries
B Posterior superior alveolar artery
7. Which of the following vascular lesions may result when a clot on the inner blood vessel wall becomes dislodged and travels in the vessel?
8. Which of the following descriptions concerning the maxillary artery is CORRECT?
A Arises from the internal carotid artery
B Enters the pterygopalatine fossa and forms terminal branches
C Arises from the zygomaticofacial foramen to emerge on the face
D Has mandibular, maxillary, nasal, palatine, and occipital branches
9. A venous sinus within the vascular system is a
10. Which of the following arteries is a branch from the facial artery?
11. Which of the following structures are smaller vessels that branch off an arteriole to supply blood directly to tissue?
12. The carotid pulse can be palpated by emergency medical service personnel at the level of the
13. The tongue is supplied mainly by a branch from the
14. Which of the following arteries can sometimes be visible under the skin of the temporal region on a patient?
15. Which of the following arteries anastomoses with the anterior superior alveolar artery?
16. Which of the following vascular lesions results in a small amount of blood escaping into the surrounding tissue and clotting?
17. For the left side of the body, the common carotid and subclavian arteries arise directly from the
18. Which of the following is the larger terminal branch of the external carotid artery?
19. The brachiocephalic veins unite to form the
20. Which of the following structures are contained within the carotid sheath?