chapter 4 Task-oriented approach to stroke rehabilitation
After completing this chapter, the reader will be able to accomplish the following:
1. Describe the motor behavior (i.e., motor control, motor learning, and motor development) theories and model that support the occupational therapy task-oriented approach to persons after stroke.
2. Describe the evaluation framework for the occupational therapy task-oriented approach and identify specific assessments that are consistent with the approach.
3. Describe general treatment principles for the occupational therapy task-oriented approach and their application to persons after stroke.
4. Given a case study of a person after stroke, describe occupational therapy task-oriented approach evaluation and treatment strategies that you would use.
This chapter provides a theoretical foundation for the occupational therapy (OT) task-oriented approach or a function-based approach for persons after stroke. Mathiowetz and Bass-Haugen56 proposed this approach in 1994 based on the motor behavior/motor control, motor development, and motor learning-theories and research of that time. Motor behavior, OT theories, and research have evolved since then, so the OT task-oriented approach has evolved as well.5,54 This chapter represents the most recent thinking regarding this approach.
The theoretical assumptions of the neurophysiological approaches, which include Rood sensorimotor approach,71 Knott and Voss proprioceptive neuromuscular facilitation,48 Brunnstrom movement therapy,12 and Bobath neurodevelopmental treatment8,9 were based on the empirical experience and research of their time. However, as the motor behavior theories changed in the 1980s and 1990s, the assumptions of the neurophysiological approaches were challenged,34,77 and alternative approaches were proposed.14,15,40,54-56Recently the theoretical assumptions of the neurodevelopmental treatment approach were updated with current motor behavior theories.42 However, many of the neurodevelopmental treatment techniques have changed little, despite the changed theoretical assumptions. This may reflect the fact that neurodevelopmental treatment was developed empirically first, and then theoretical assumptions of the time were used to explain why it might work. In contrast, the OT task-oriented approach evaluation and interventions strategies emerged primarily from its theoretical assumptions (see Chapter 6).
Theoretical assumptions and model underlying the occupational therapy task-oriented approach
Systems model of motor control
In the past 25 to 30 years, new models of motor control have evolved from the ecological approach to perception and action29,83 and from the study of complex, dynamical systems in mathematics and the sciences.33 The new models emphasize the interaction between persons and their environments and suggest that motor behavior emerges from persons’ multiple systems interacting with unique tasks and environmental contexts.62 “Thus, the systems model of motor control is more interactive or heterarchical and emphasizes the role of the environment more than the earlier reflex-hierarchical model.”54
In the systems model, the nervous system is viewed differently from earlier reflex-hierarchical models. Instead of being the primary system controlling movement, the nervous system now is considered only one system among many systems that affect motor behavior. “The nervous system itself is organized heterarchically such that higher centers interact with the lower centers but do not control them. Closed-loop and open-loop systems work cooperatively and both feedback and feedforward control are used to achieve task goals.”54 The central nervous system interacts with multiple personal and environmental systems as a person attempts to pursue a functional goal.
Ecological approach to perception and action
The ecological approach “emphasizes the study of interaction between the person and the environment during everyday, functional tasks and the close linkage between perception and action (i.e., purposeful movement).”54 Gibson described the role of functional goals and the environment in the relationship between perception and action. He stated that direct perception involves the active search for affordances30 or the functional use of objects for a person with unique personal characteristics.87 Therefore, Gibson’s concept of affordances recognizes the close linkage between perception and action in terms of what the information available in the environment means to a specific person.30
Bernstein7 also recognized the importance of the environment and personal factors other than the central nervous system in motor behavior. He explained the role that a particular muscle has in a movement is influenced by the context or circumstances and described three potential sources of variability in muscle function. Variability is due to anatomical factors. For example, from kinesiology one knows that in a standing position, the shoulder flexor muscles contract concentrically to bring the humerus to the 90-degree position. However, in the prone position with one’s arm at one’s side, shoulder extensor muscles contract eccentrically until reaching the 90-degree position. Thus, which muscles are activated depends on the initial position of the body. Another example relates to extending the shoulder from the 90-degree position when standing. If one wants to extend it quickly or against resistance, the shoulder extensor muscles contract. In contrast, if one extends the shoulder slowly against no resistance, the shoulder flexor muscles contract eccentrically, and the shoulder extensor muscles do not need to contract at all. In both cases, the role of the muscle is determined by the context in which it is used. A second source of variability is due to mechanical factors. Many nonmuscular forces, such as gravity and inertia, determine the degree to which a muscle needs to contract. For example, a muscle must exert much less force if contracting in a gravity-eliminated plane rather than against gravity. Likewise, the contraction of the elbow extensor muscles would be different if the shoulder were extending or flexing at the same time because of the effects of inertia. Again, the effect of a muscle contraction is related to the context. A third source of variability is due to physiological factors. “When higher centers send down a command for a muscle to contract, middle and lower centers have the opportunity to modify the command. Lower and middle centers receive peripheral sensory feedback. Thus, the impact of the command on the muscle will vary depending on the context and degree of influence of the middle and lower centers. As a result, the relationship between higher center or executive commands and muscle action is not a one-to-one.”54
Mathiowetz and Wade57 also demonstrated the influence of context (informational support available in the environment) on movement. They reported that a natural informational support condition (e.g., eating applesauce with a spoon) elicited a smoother and more direct movement pattern than an impoverished informational support condition (e.g., pretending to eat applesauce with a spoon without any of the objects). Many have taken a dynamical systems view as a means to explain the complex person-environment interactions that occur in everyday life.
Dynamical systems theory
The study of dynamical systems originated in the disciplines of mathematics, physics, biology, chemistry, psychology, and kinesiology and has been applied to the professions of OT, physical therapy, nursing, adapted physical education, and some areas of medicine.13,53 Such study has influenced the development of a systems model of motor control as well. Dynamical systems theory proposes that behaviors emerge from the interaction of many systems and subsystems. Because the behavior is not specified but is emergent, it is considered to be self-organizing.46 Despite the many degrees of freedom or ways of performing a task available to persons, they tend to use relatively stable patterns of motor behavior.81 For example, when one walks or brushes the teeth, one has many choices in how to perform the task, yet one tends to use preferred patterns. These relatively stable patterns of motor behavior, which are unique to each person, provide evidence of self-organization.
Behavior can shift between periods of stability and instability throughout life. For example, behaviors can change from being stable to being less stable as a result of a stroke or aging. In fact, “it is during unstable periods, characterized by a high variability of performance, that new types of behaviors may emerge either gradually or abruptly. These transitions in behavior, called phase shifts, are changes in preferred patterns of coordinated behavior to another.”54 A gradual phase shift occurs when an infant progresses from walking while holding on to a parent’s hands to walking without a helping hand over several months. An abrupt phase shift in prehension pattern occurs when a person changes from picking up a small object such as a peanut to picking up a large object such as a large coffee mug. How can these phase shifts or changes in behavior be explained?
In the dynamical systems view, control parameters are variables that shift behavior from one form to another. They do not control the change but act as agents for reorganization of the behavior into a new form.38 Control parameters are gradable in some way. In the infant example, the degree of parental support influenced the change or phase shift from walking with support to walking without support. As parental support decreases, infants need to rely more on their own ability to maintain balance and need to increase their strength to support and control their own body weight in an upright position. In the other example, increasing the size of the object to be grasped elicited the change in prehension pattern from tip prehension to cylindrical grasp. Consequently, object size also is considered a control parameter.
Explanations of changes in motor behavior in the systems model of motor control are different from earlier reflex-hierarchical models. Thelen79 stated that an important characteristic of a system perspective is that the shift from one preferred movement pattern to another is marked by discrete, discontinuous transitions. These changes in only one or several personal or environmental systems (i.e., control parameters) can contribute to transitions in motor behavior.18 In conclusion, no inherent ordering of systems exists in terms of their influence on motor behavior, and systems themselves are subject to change over time.
Systems view of motor development
A systems view of motor development suggests that changes over time are caused by multiple factors or systems such as maturation of the nervous system, biomechanical constraints and resources, and the impact of the physical and social environment.38,54 For example, Thelen and Fisher80 reported that the disappearance of the stepping reflex at 4- to 5-months-old is due to multiple factors internal and external to the child. Internal factors included the strength of the leg muscles, weight of the legs, and arousal level of the child. External factors included the varying effects of gravity in different environments. Thus, maturation of the nervous system alone cannot explain this change in developmental behavior. A systems view also suggests that normal development does not follow a rigid sequence, as the motor milestones would suggest. In fact, children follow variable developmental sequences because of their unique personal characteristics and environmental contexts. If the traditional developmental sequences are no longer sufficient as a guide for working with children, then they are certainly not appropriate as a guide for working with adults after stroke.85
In addition, the systems view suggests that behaviors observed after central nervous system damage result from patients’ attempts to use their remaining resources to achieve functional goals. For example, the flexor pattern of spasticity often seen after stroke is due to various factors in addition to spasticity, such as weakness, inability to recruit appropriate muscles, biomechanical principles related to lever arms, and/or soft-tissue tightness. Thus, when inefficient/ineffective movement patterns are seen after stroke, therapists need to consider multiple factors as potential contributing variables (see Chapter 10).
Contemporary view of motor learning
Schmidt75 defined motor learning as “a set of processes associated with practice or experience leading to relatively permanent changes in the capabilities of responding.” Thus, recent motor learning theories acknowledge that behavior changes observed during practice may be only temporary. As a result, contemporary motor learning research not only evaluates learning after the acquisition phase (i.e., immediate effects) but also after a retention phase (i.e., short-term or long-term effects) or a transfer test (i.e., ability to generalize to new task), and thus new ways of thinking about motor learning have emerged. Motor learning research supports the idea that random practice (i.e., repetitive practice of several tasks in a varied sequence within a practice session) is better than blocked practice (i.e., repetitive practice of the same task within a practice session).76 Similarly, practicing variations of the same tasks in varied contexts is better than practicing the same task in the same context. In addition, practicing the whole task rather than parts of a task usually is better, especially if the parts are interdependent or relatively fast.73
McNevin, Wulf, and Carlson58 summarized some additional principles. When persons are learning a new task such as golfing, they should focus on the movement effects (external focus on the golf club head) rather than on their own arm movements (internal focus). Self-controlled practice (i.e., a person being trained decides when and how feedback is given and whether assistive devices are used) is better than instructor-controlled practice. Finally, dyad training, in which a person is able to alternate observing and practicing a task, is beneficial to learning a new task.
Research on the role of feedback in learning demonstrates that physical and verbal guidance enhanced immediate performance but interfered with long-term learning.73 Winstein and Schmidt88 reported that 50% feedback (i.e., feedback after half of the trials) was better than 100% feedback. Faded or decreasing feedback was better than increasing feedback. Finally, summary feedback after multiple trials is better than immediate feedback after every trial.74 In all cases, less feedback was better than more feedback.
Most research on motor learning has been performed on persons without disabilities using a brief, contrived task in laboratory environments. Therefore, therapists need to be cautious about applying these principles to persons with disabilities performing functional tasks in everyday, natural environments.
However, several studies have explored whether motor learning principles can be applied to persons after stroke. Hanlon37 provided some evidence that random practice was better than blocked practice. Merians and colleagues59 reported that practice in a condition with reduced augmented feedback was beneficial for performance consistency but not for accuracy for persons with and without stroke. Dean and Shepherd19 reported that task-related training using variable practice and varied contexts improved balance ability during seated reaching activities. Finally, Fasoli and colleagues22 reported that externally focused (task-related) instructions resulted in faster and more forceful movements than internally focused (movement-related) instructions for persons with and without stroke. Chapter 5 provides additional discussion of the application of motor learning principles to stroke rehabilitation.
Systems model of motor behavior
The model in Fig. 4-1 has been updated to include terminology from the Occupational Therapy Practice Framework.1 The figure depicts the theoretical basis of the OT task-oriented approach. The model illustrates the interaction between the person (client factors, performance skills, and performance patterns) and their environment (context and activity demands). Occupational performance tasks (i.e., activities of daily living [ADL], instrumental activities of daily living [IADL], work, education, play/leisure, rest, and sleep) and role performance (social participation) emerge from the interaction between the systems of the person (cognitive, psychosocial, and sensorimotor) and the systems of the environment (physical, socioeconomical, and cultural). Changes in any one of these systems or subsystems can affect occupational performance tasks and/or role performance. “In some cases, only one primary factor might determine occupational performance. In most cases, occupational performance tasks emerge from the interaction of many systems. The on-going interactions between all components of the model reflect its heterarchical nature.”54
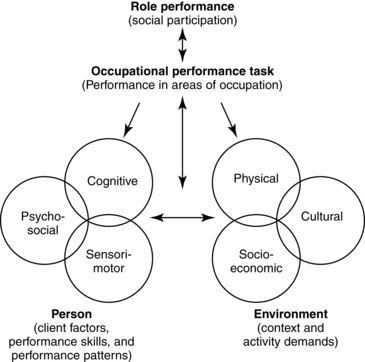
Figure 4-1 The systems model of motor behavior, which supports the occupational therapy task-oriented approach, emphasizes that occupational performance tasks and role performance emerge from an interaction of the person and their environment. In addition, any occupational performance task affects the person and environment. A continuous interaction occurs between role performance and occupational performance tasks. These interactions are ongoing across time.
(Adapted from Mathiowetz V, Bass-Haugen J: Assessing abilities and capacities: motor behavior. In Radomski MV, Latham CAT, editors: Occupational therapy for physical dysfunction, ed 6, Baltimore, 2008, Lippincott Williams & Wilkins.)
In addition, any occupational performance task affects the environment in which it occurs and the person acting. For example, if a patient with hemiplegia becomes independent in driving by using assistive technology and adaptive strategies, the patient’s ability to drive would free family members from needing to provide transportation for appointments and social events. The patient would be able to resume the role of driver and the task of driving, which were likely meaningful to the patient’s life. Thus the occupational performance task of driving affects persons and objects in the environment (i.e., assistive technology added to the car). The task also affects the person and the associated components. The ability to be less dependent on the family may affect the patient’s self-esteem positively (i.e., psychosocial subsystem). The process of driving “provides the patient the opportunity to solve problems and to discover optimal strategies for performing tasks. This influences a client’s cognitive and sensorimotor subsystems and the ability to perform other functional tasks.”54
The specific components (subsystems) of the systems, which influence occupational performance tasks, may be framed in OT terminology.1,2 Components of the cognitive (mental) system include orientation, attention, memory, problem-solving, sequencing, learning, and generalization ability. Components of the psychosocial system include a person’s interests, coping skills, self-concept, interpersonal skills, self-expression, time management, emotional regulation, and self-control skills that could affect occupational performance tasks. Strength, endurance, range of motion, sensory functions and pain, perceptual function, and postural control are components associated with the sensorimotor system. The environment includes physical, socioeconomical, and cultural characteristics of the task itself and the broader environment. Components of the physical environment system include objects, tools, devices, furniture, plants, animals, and the natural and built environments, which could limit or enhance task performance. The social supports provided by the family, friends, caregivers, social groups, community, and financial resources are components of the socioeconomical system, which could influence choice in activities. Finally, components of the cultural system include customs, beliefs, activity patterns, behavioral standards, and societal expectations, which also could affect occupational performance tasks.
The inclusion of role performance in this systems model reflects an OT, not a motor behavior perspective. “Occupational therapists believe the roles that persons want and need to fulfill determine the occupational performance tasks and activities they need to do. Conversely, the tasks and activities persons are able to do determine what roles they are able to fulfill.”54 Box 4-1 summarizes the assumptions of the OT task-oriented approach.
Box 4-1 Assumptions of the Occupational Therapy Task-Oriented Approach Based on a Systems Model of Motor Behavior
 Personal and environmental systems, including the central nervous system, are heterarchically organized.
Personal and environmental systems, including the central nervous system, are heterarchically organized.
 Functional tasks help organize behavior.
Functional tasks help organize behavior.
 Occupational performance emerges from the interaction of persons and their environment.
Occupational performance emerges from the interaction of persons and their environment.
 Experimentation with various strategies leads to optimal solutions to motor problems.
Experimentation with various strategies leads to optimal solutions to motor problems.
 Recovery is variable because patient factors and environmental contexts are unique.
Recovery is variable because patient factors and environmental contexts are unique.
 Behavioral changes reflect attempts to compensate and to achieve task performance.
Behavioral changes reflect attempts to compensate and to achieve task performance.
Data from Mathiowetz V, Bass-Haugen J: Assessing abilities and capacities: motor behavior. In Radomski MV, Latham CAT, editors: Occupational therapy for physical dysfunction, ed 6, Baltimore, 2008, Lippincott Williams & Wilkins.
Evaluation framework using the occupational therapy task-oriented approach
The therapist conducts the evaluation using a top-down approach as suggested by Latham.49 Box 4-2 gives a framework for evaluation. Evaluation efforts focus initially on role performance and occupational performance tasks because they are the goals of motor behavior. A thorough understanding of the roles that a patient wants, needs, or is expected to perform and of the tasks needed to fulfill those roles enables therapists to plan meaningful and motivating treatment programs. After a patient has identified the most important role and occupational performance limitations, therapists use task analysis to identify which subsystem of the person or environment is limiting functional performance. This process may indicate the need for evaluation of selected subsystems of the person or environment.25 The emphasis on role and occupational performance in the OT task-oriented approach is consistent with the idea that OT evaluation should be primarily at the participation and activities level rather than the impairment level, using World Health Organization90 terminology. The therapist needs to use qualitative and quantitative measures during the evaluation process.86 “Therefore, therapists use interviews, skilled observations, and standardized assessments to evaluate their clients. Although the client is the primary source of information, other sources including the client’s records, caregivers, family members, and the client’s environment contribute as well.”54 The evaluation framework is described in more detail subsequently.
Box 4-2 Evaluation Framework for the Occupational Therapy Task-Oriented Approach Based on a Systems Model of Motor Behavior
| Role performance (social participation) | Roles: Worker, student, volunteer, home maintainer, hobbyist/amateur, participant in organizations, friend, family member, caregiver, religious participant, other? Identify past roles and whether they can be maintained or need to be changed. Determine how future roles will be balanced. |
| Occupational performance tasks (areas of occupation) | ADL: bathing, feeding, bowel and bladder management, dressing, functional mobility, and personal hygiene and grooming IADL: home management, meal preparation and cleanup, care of others and pets, community mobility, shopping, financial management, and safety procedures Work and/or education: employment seeking, job performance, volunteer exploration and participation, retirement activities, and formal and informal educational participation. Play/leisure: exploration and participation Rest and sleep: preparation and participation |
| Task selection and analysis | What client factors, performance skills and patterns, and/or contexts and activity demands limit or enhance occupational performance? |
| Person (client factors; performance skills and patterns) | Cognitive: orientation, attention span, memory, problem solving, sequencing, calculations, learning, and generalization Psychosocial: interests, coping skills, self-concept, interpersonal skills, self-expression, time management, and emotional regulation and self-control Sensorimotor: strength, endurance, range of motion, sensory functions and pain, perceptual function, and postural control |
| Environment (context and activity demands) | Physical: objects, tools, devices, furniture, plants, animals, and built and natural environment Socioeconomic: social supports: family, friends, caregivers, social groups, and community and financial resources Cultural: customs, beliefs, activity patterns, behavior standards, and societal expectations |
Adapted from Mathiowetz V, Bass-Haugen J: Assessing abilities and capacities: motor behavior. In Radomski MV, Latham CAT, editors: Occupational therapy for physical dysfunction, ed 6, Baltimore, 2008, Lippincott Williams & Wilkins.
The first step in the evaluation process is to assess role performance. “Therapists must determine which roles clients had prior to the onset of disability, and which roles they can and cannot do at this time.”54 A discussion of roles that patients want or must do in the future helps determine which roles are most important to them. In addition, therapists need to explore ways that role changes have affected or will affect patients and their families, especially the primary caregivers. Jongbloed, Stanton, and Fousek45 recommended that therapists ask questions such as “How have roles changed since the disability?” “How have family members reacted to these changes?” “Is there role flexibility when needed?” and “How competently do members perform roles?” The therapist may need to adjust these questions to the patient’s level of understanding. The patient and significant others must participate in the evaluation of role performance whenever possible.
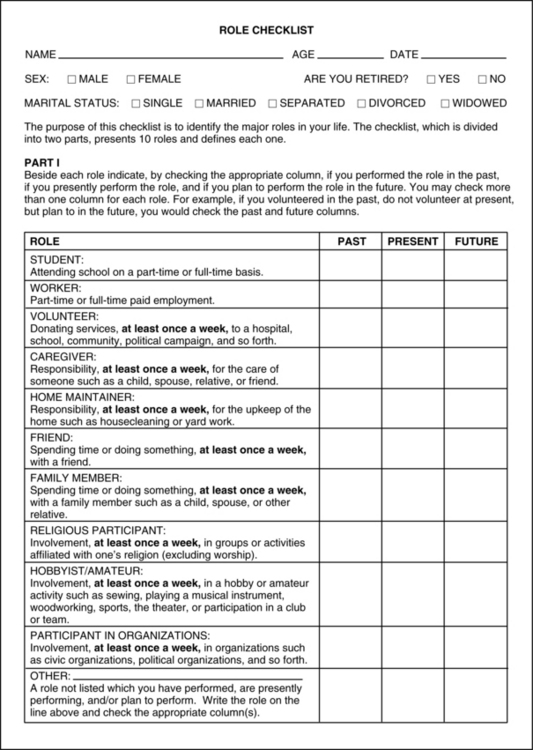
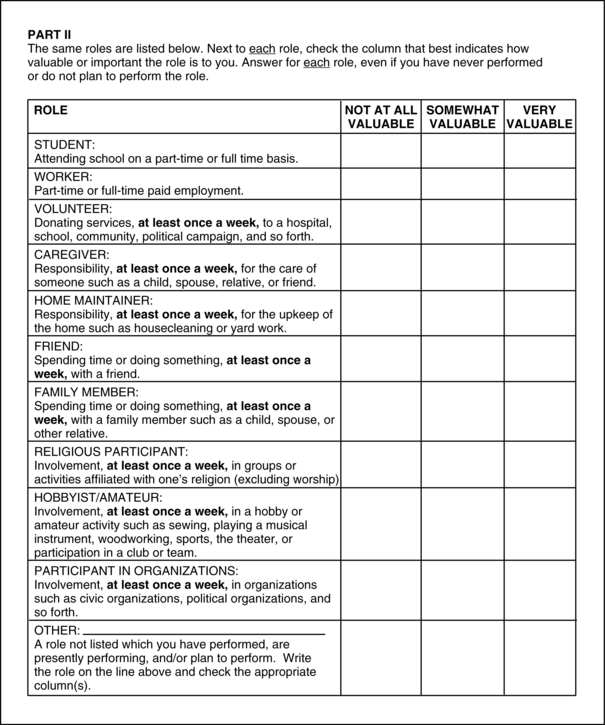
The therapist may assess role performance using a nonstandardized, semistructured interview. However, a standardized assessment tool such as the Role Checklist4,63 is suggested. The Role Checklist is a self-report, written inventory designed for adolescent, adult, or geriatric populations. In Part One, patients check the 10 roles (Fig. 4-2) that they have performed in the past, are performing in the present, and plan to perform in the future. In Part Two, patients rate the value of each role to them on a scale from “not at all valuable,” “somewhat valuable,” to “very valuable.” The Role Checklist takes 10 to 15 minutes to complete and has evidence of reliability and validity (see Fig. 4-2).
The therapist may use other assessment tools to gather information on role performance. For example, the Occupational Performance History Interview-II (OPHI-II)47 is a broad, semistructured assessment of occupational life history including work, leisure, and daily life activities. One part of it explores life roles, whereas other parts explore interests, values, organization of daily routines, goals, perceptions of ability, and environmental influences. The complete OPHI-II takes about 50 minutes and has evidence of reliability and validity. The OPHI-II includes information not only on role performance but also on occupational performance tasks, which are the next step of the evaluation process. In conclusion, after patients have identified the roles that they want or need to perform, they more easily can identify the tasks and activities needed to fulfill each role.
The second step in the evaluation process is the assessment of occupational performance tasks: ADL, IADL, work, education, and play/leisure (see Box 4-2). “Because roles, tasks, activities, and their contexts are unique to each person, a client-centered assessment tool such as the Canadian Occupational Performance Measure (COPM)50 is recommended.”54 The COPM uses a semistructured interview to measure a patient’s self-perception of occupational performance over time. First, patients identify problem areas in self-care, productivity, and leisure. Second, they rate the importance of each problem area, which assists therapists in setting treatment priorities. Third, patients rate their own performance and their satisfaction with their performance on the five most important problem areas. Therapists may use these performance and satisfaction ratings again as outcome measures, measuring change across time. If therapists are concerned that a patient cannot rate performance accurately because of a cognitive impairment or age, therapists may use direct observation of selected activities or a caregiver interview to verify the information. The information elicited by the COPM is unique to each patient and the individual’s environment, which is an essential part of the OT task-oriented approach (Fig. 4-3).
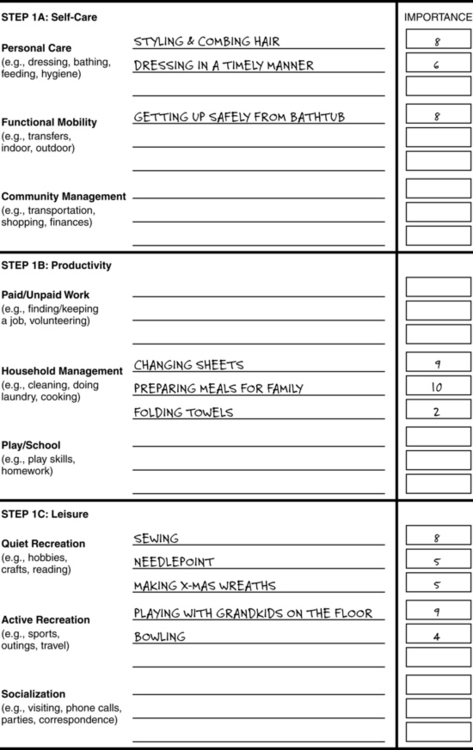
Figure 4-3 Identifying problems and rating importance via the Canadian Occupational Performance Measure.
(Modified from Law M, Baptiste S, Carswell A, et al: Canadian Occupational Performance Measure, Toronto, 1994, CAOT Publications ACE.)
Another recommended measure of occupational performance specific to ADL and IADL is the Assessment of Motor and Process Skills (AMPS).24 The assessment is client-centered because the person chooses two or three ADL or IADL tasks to be performed, which ensures that the task or activity is familiar and relevant to the person being evaluated. The purpose of the AMPS is “to determine whether or not a person has the necessary motor and process skills to effortlessly, efficiently, safely and independently perform the ADL tasks needed for community living.”24 The AMPS is appropriate for persons from diverse backgrounds and with diverse needs and interests because it has been standardized internationally and cross-culturally. “A unique feature of the AMPS is that it can adjust, through Rasch analysis, for the difficulty of tasks performed and the severity of the rater who scores the client’s performance. In addition, it allows a therapist to compare the performance of clients who performed one set of tasks on initial evaluation with the results of a re-evaluation on a different set of tasks.”54 The primary limitation of the AMPS is that it requires a five-day training workshop to learn how to administer the assessment in a reliable and valid way. Computer software to score the AMPS is provided as part of the workshop. Finally, the AMPS assists in the next step in the evaluation process, because it requires observation of patients performing occupational performance tasks (see Chapter 21).
While evaluating occupational performance tasks, “therapists must observe both the outcome and the process (i.e., the preferred movement patterns, their stability or instability, the flexibility to use other patterns, efficiency of the patterns, and ability to learn new strategies) to understand the motor behaviors used to compensate and to achieve functional goals.”54 Determining the stability of the motor behavior is important to determine the feasibility of achieving behavioral change in treatment. “Behaviors that are very stable will require a great amount of time and effort to change. Behaviors that are unstable are in transition, the optimal time for eliciting behavioral change.”54 Thus, when behaviors are more stable, a compensatory approach may be most appropriate; when behaviors are unstable, a remediation approach may be more successful. Quantitative and qualitative measures are needed to evaluate the process of task performance.
The third step in the evaluation process involves task selection and analysis. The tasks selected for observation should be ones that patients have identified as important but difficult to do. Task analysis requires therapists to observe their patients performing one or more occupational performance tasks. In most cases, observation of performance happens as part of the second step described previously. Therapists use task/activity analysis to evaluate activity demands, context, patient factors, performance skills, and performance patterns to determine whether a match exists that enables persons to perform occupational tasks within a relevant environment. If the person is unable to perform the task, therapists attempt to determine which person or environment subsystems are interfering with occupational performance. “In dynamical systems theory, these are considered the critical control parameters or the variables that have the potential to shift behavior to a new level of task performance.”54 Each person has unique strengths, limitations, and environmental context after a stroke. Therefore, the critical control parameters that support or limit occupational performance tasks are also unique. An effective intervention strategy for one person after stroke may not be effective for the next person. Another concept of dynamical systems theory is that critical control parameters also change as persons and their environments change over time. Therefore, an intervention that worked well early in a patient’s rehabilitation might not work well late in the rehabilitation process or vice versa.
The identification of critical control parameters is the most challenging part of the evaluation process. However, evidence in the research literature indicates that some variables or subsystems of the person and/or environment are potential critical control parameters for persons after stroke. Gresham and colleagues36 reported that psychosocial and environmental factors were significant determinants of functional deficits in persons for the long term after stroke. In a review, Gresham and colleagues35 reported that 11% to 68% of persons experience depression after stroke, with 10% to 27% meeting the criteria for major depression. In the cognitive area, Galski and colleagues28 reported that for persons after stroke, “deficits in cognition, particularly higher-order cognitive abilities (e.g., abstract thinking, judgment, short-term verbal memory, comprehension, orientation) play an important role in determining length of stay and in predicting functional status at the end of hospital stay.” In the sensorimotor area, weakness,65 fatigue,44 impaired motor function,6 and visuospatial deficits82 are associated with poorer functional outcomes. For example, Bernspang and colleagues6 reported that motor function measured with the Fugl-Meyer Assessment27 was correlated moderately (r = 0.64) with self-care ability.
Practitioners must use the aforementioned literature on potential control parameters with caution. Most of these were correlation studies, which indicate relationships between these variables and functional performance, but they do not prove a causal link. In addition, most correlations were moderate or low, which suggests that any one variable explains a relatively small percentage of the variance associated with functional performance. However, Reding and Potes70 provided evidence that as the number of impairments increased, functional outcomes decreased. “Thus, multiple variables contribute to functional performance for most persons with central nervous system dysfunction. The challenge is to identify those variables that are most critical to your clients.”54
Bobath9 suggested that spasticity is the primary cause of motor deficits in persons after stroke and that weakness and decreased range of motion are due to spastic antagonists. However, evidence is increasing that indicates that spasticity is not a critical control parameter.11 For example, Sahrmann and Norton72 reported electromyography findings that indicated movements were not limited by antagonist stretch reflexes (spasticity) but were limited by delayed initiation and cessation of agonist contraction. Similarly, Fellows, Kaus, and Thilmann23 found no relationship between movement impairments and passive muscle hypertonia in the antagonist muscles. O’Dwyer, Ada, and Neilson64 found no relationship between spasticity and either weakness or loss of dexterity. “Thus, research evidence challenges the assumption that spasticity causes the weakness and decreased range of motion often seen in persons with central nervous system dysfunction.”54 Recently, the Neuro-Developmental Treatment Association acknowledged this change in thinking: “There is not a direct relationship between spasticity and constraints on motor impairments or functional performance, as the Bobaths first proposed”42 (see Chapter 10).
After identifying the critical control parameters that support or constrain occupational performance, the therapist must assess the interactions of these systems. Consider two patients who have complete loss of voluntary control of their dominant hand. The role and occupational performance tasks of the patient as a worker may or may not be affected. If the worker were an automobile mechanic, the interaction of this personal limitation with the activity demands of the work environment would likely make the task of repairing a car engine difficult or impossible to perform. However, if the worker were a self-employed writer, the person could learn to use a one-handed keyboard with the nondominant hand and could continue writing because the interaction of performance skills and activity demands would not interfere with role and task performance. This part of the evaluation requires the therapist to use qualitative and quantitative assessments and clinical reasoning to determine how subsystem of the person and the environment might affect occupational performance.
The fourth step in the evaluation process is to perform specific assessments of client factors, performance skills, and performance patterns, which are thought to be critical control parameters. The critical control variables are the only ones that need to be evaluated. “The evaluation of selected variables according to the OT task-oriented approach contrasts with bottom-up approaches that evaluate all component variables. This selective approach eliminates the need to evaluate variables that have little functional implication and saves therapists’ time, which is critical for cost containment.”54
Occupational therapists use a variety of assessments to evaluate patient factors, performance skills, and performance patterns that support or constrain occupational performance. Some assessments were designed to examine one or more impairments within the context of occupational performance. The Arnadottir OT-ADL Neurobehavioral Evaluation (A-ONE)3 facilitates evaluation of perceptual and cognitive systems within the context of ADL (see Chapter 18 for details). From a task-oriented perspective, this is a preferred assessment tool because it links impairments more closely to occupational performance. In contrast, most assessments of impairments are conducted independent of occupational performance.
The fifth step of the evaluation process is evaluation of the environment: context and activity demands. The inclusion of physical, social, and cultural environments in American Occupational Therapy Association2 uniform terminology acknowledges their important impact on occupational performance. A number of OT theories16,21,51,78 emphasize the importance of assessing environmental context as part of the overall evaluation process. See Radomski68 and Cooper and colleagues17 for specific assessments of environmental contexts. See Chapter 27.
Treatment principles using the occupational therapy task-oriented approach
Help patients adjust to role and task performance limitations
Many patients are not able to continue some of the roles and tasks that they performed before their strokes. This is a frustrating and sometimes depressing situation for many persons after stroke. Therapists can help by exploring alternative ways of fulfilling roles and of performing the associated tasks. Therapists also can explore potential new roles and new tasks. For example, in the case study presented at the end of this chapter, an important role for G.W. was continuing to help his son on the farm. The therapist helped the patient identify the tasks with which he had helped in the past and which ones would be impossible or difficult to perform in the future. For G.W., heavy or bilateral tasks (e.g., moving bales of hay and repairing heavy equipment) would fit this category. Brainstorming about alternative tasks that he could do unilaterally or relatively light tasks (e.g., record keeping) that he could still perform would enable him to continue his role as an assistant to his son. Inclusion of the son in this discussion was important, because he had suggestions that G.W. had not considered.
Create an environment that uses the common challenges of everyday life
Therapists need to be creative in creating environments within their clinical settings that provide typical challenges. Some facilities have purchased more real-life environments such as Easy Street, whereas other facilities have remodeled their clinics to simulate environments in which patients typically have to interact. Some have created small apartments to create a more realistic environment, in contrast to a typical hospital room, in which patients can interact before being discharged. Home care settings are ideal situations for following this treatment principle because the patient’s own environment and objects can be used for therapy.
A stroke unit provides a more effective environment for improving functional outcomes.43 The physical environment is set up to enable patients to function more independently. Patients are encouraged to wear their own clothing instead of hospital gowns. Thus, they are confronted with the common clothing of everyday life. In addition, staff members are trained to encourage independent behaviors. In G.W.’s case, nursing staff on the previous unit had assisted him in dressing and bathing. On the rehabilitation unit, nursing staff would encourage him to perform as many self-care tasks as possible. In addition, most rehabilitation units have patients eat together in a dining area instead of in their own rooms. This is a more typical way of eating, plus it facilitates social interaction and support from others struggling with many of the same problems. In addition, dining with others facilitates learning from and problem-solving with each other.
Practice functional tasks or close simulations to find effective and efficient strategies for performance
In all cases, the therapist must use the functional tasks and activities that have been identified as important and meaningful to their patients. This demonstrates to patients that the therapist has listened to them and respects their choices and priorities. As a result, patients more easily understand the relevance of therapy to their lives.
Use of functional, natural tasks rather than rote exercise in treatment is important. A number of studies have demonstrated that the kinematics of movement are different when one performs a real task instead of rote exercise.57,91 A metaanalytical review52 provided evidence that “engagement in purposeful activity produces better quality of movement than concentration on movement per se.” Nelson and colleagues61 demonstrated that after stroke, persons who performed an occupationally embedded exercise had significantly greater supination active range of motion than persons who did rote exercises. These studies support the idea that the use of functional tasks has beneficial therapeutic effects.
Higgins39 suggested that persons need to practice functional, everyday activities to find the most effective and efficient way of doing the activity. Because persons are unique, their performance patterns and levels of skill vary. Therefore, therapists should not expect that one way of performing a task would be the most effective and efficient way of performing a task for all patients. Thus, therapists should encourage patients to experiment to find the most effective and efficient way of performing functional tasks. In one evidence-based review, the authors concluded, “There is strong evidence that patients benefit from exercise programmes in which functional tasks are directly and intensively trained.”84
Provide opportunities for practice outside of therapy time
Therapists need to recognize that the amount of time they have to work with a patient is short relative to the total time in a day. Therefore, enticing patients to continue therapy on their own time is important. Therapists can provide homework assignments for patients to work on their own. If homework is given, follow-up is important, and therapists should ask their patients how their homework went. What worked for the patients, and what did not work for them? Effective communication with other rehabilitation staff and family members is crucial, so that their attempts to be helpful do not reduce the opportunities for patients to practice outside of therapy time. Most important is for therapists to help patients find new ways to use their involved extremity, even if it is only to stabilize objects. A good homework assignment is to challenge the patient to find a new way to use the involved arm each day.26 Ultimately, the goal is to get patients to use their involved arm without thinking about it.
Use contemporary motor learning principles in training or retraining skills
Therapists should consider the following three motor learning principles:
 Use random and variable practice within natural contexts in treatment.
Use random and variable practice within natural contexts in treatment.
 Provide decreasing amounts of physical guidance and verbal feedback.
Provide decreasing amounts of physical guidance and verbal feedback.
 Develop task analysis and problem-solving skills of patients so that they can find their own solutions to occupational performance problems in home and community environments.
Develop task analysis and problem-solving skills of patients so that they can find their own solutions to occupational performance problems in home and community environments.
Although blocked or repetitive practice of the same task normally is not recommended, such practice may be helpful or necessary when a patient is first learning the requirements of a new task.74 However, therapists should shift to random and variable practice schedules as soon as possible to enhance motor learning. Random practice involves practicing more than one task within a session (i.e., avoiding repetitive practice of the same task). Variable practice involves experimenting with different tools for completing a task, with different location of the tools relative to the person, or with varied environments for performing a task. In addition, patients should practice tasks in their natural context whenever possible. Therefore, ADL tasks normally done in a patient’s room should be practiced there rather than in the OT clinic. Even better would be patients practicing ADL tasks in their own homes.
When therapists are beginning to teach patients new tasks or new ways to perform previously learned tasks, they may need to provide some physical guidance and verbal feedback.73 However, guidance and feedback should be tapered off quickly so that the person does not become dependent on them. For a therapist not to provide guidance and feedback when a patient is struggling to perform a task is difficult. However, providing physical guidance prevents patients from learning how to use their remaining resources to get the job done, and providing immediate and frequent feedback prevents patients from learning how to use their own feedback mechanisms to monitor and evaluate their own performance. If patients are unaware of a deficit (e.g., neglect to use involved extremity in a task), the use of a videotape of their performance can supplement their usual feedback mechanisms.69 By the time a patient is approaching discharge, therapists should be providing minimal guidance or feedback. The therapist should remember that the goal of rehabilitation is to train the patient to be independent without the therapist’s presence.
In a related issue, patients need to learn how to analyze tasks and to problem-solve on their own. If the therapist always analyzes tasks for patients and solves all their problems, the patients will not learn how to do those things themselves. In the limited therapy time available, preparing patients for all possible tasks, activities, and environments that they will confront after they are discharged is impossible. The therapist’s role is to train patients how to do task analysis and problem-solving during the rehabilitation process, so that by the time they are discharged, they are capable of doing those things on their own. From early in rehabilitation, the therapist should involve patients in task analysis and guide them through the process. As occupational problems are addressed, the therapist should keep patients involved in trying to find solutions to problems. Therapists should encourage experimentation to find the optimal solution for that specific person. The therapist should remember that the same solution does not work for all patients (see Chapter 5).
Minimize ineffective and inefficient movement patterns
As described previously, during observation of a patient performing an occupational performance task, therapists attempt to identify what may be critical personal or environmental factors that are interfering with effective and efficient movement patterns. The following strategies are ways that therapists can intervene to reduce ineffective and inefficient movement.
Remediate a client factor (impairment) if it is the critical control parameter.
When therapists identify person factors in the cognitive, psychosocial, or sensorimotor systems as possible critical control parameters, then they should attempt to remediate those factors, assuming that is possible. For example, Flinn26 identified decreased strength as one critical control parameter that interfered with occupational performance tasks for a person after stroke. Thus, she attempted to remediate this sensorimotor variable through the use of exercise and increased use of the involved extremity for functional tasks. For this person, the use of exercise was meaningful because she saw a clear connection between her exercise program and her ability to use her involved arm and hand for everyday tasks. The therapist also encouraged her to use her involved extremity whenever possible in therapy and for various homework assignments.
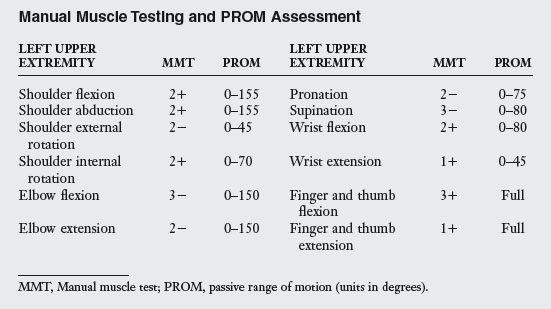
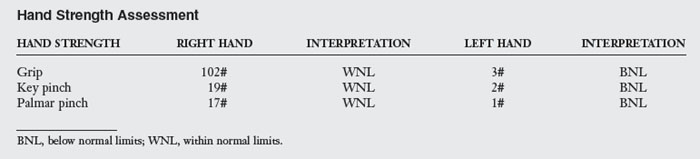
In the case of G.W., decreased strength, impaired sensation, and neglect of the left upper extremity were identified as possible control parameters. Therefore, attempts to remediate these factors were warranted in this case. However, sometimes remediation of a potential control parameter is impossible because of the severity of the disease process or limited time available for therapy. In such cases, a more compensatory approach to treatment is indicated.
Adapt the environment, modify the task, use assistive technology, and/or reduce the effects of gravity.
For many patients, the quickest and most effective approach to improving occupational performance is to adapt the task and/or the environment. For example, Gillen31 described a patient with severe limitations in self-care activities following multiple sclerosis and ataxia. Tremor, impaired postural control, paraparesis, and decreased endurance limited his occupational performance. The patient’s priority was to gain access to the community and community resources. He did not have adequate motor control to operate a manual chair or to control a standard power chair. Therefore, a specialized power chair was prescribed that provided optimal head and trunk stability, allowed independent tilting, included a joystick with tremor-dampening electronics, and a forearm trough to provide maximal stability to the arm controlling the joystick. A volar wrist splint provided additional stability to the wrist. With training in varied environments, the patient improved from total assistance in mobility to minimal supervision. Thus, the use of assistive technology, task modification, and training in varied environments was the most efficient and effective means of improving the mobility independence of this patient.
For G.W., a standard bath chair enabled independent and safe tub transfers. For shoe tying, G.W. preferred the use of Kno-Bows, an adapted device, for fastening his shoes rather than learning one-handed shoe tying. For cutting meat, an enlarged-handled fork was tried to encourage use of the left hand. However, this was not feasible at the time, so a rocker knife was prescribed. Thus a variety of adapted devices increased the ADL independence of G.W.
For patients unable to raise their arms up against gravity (i.e., grade 2 shoulder flexion and shoulder abduction muscles), the use of technology that minimizes the effects of gravity on their arms may help strengthen those weak muscles and enable increased functional performance. The use of body weight support during treadmill training has resulted in increased lower extremity strength and increased ambulation ability of person’s poststroke.84 Unfortunately, there has been limited application of this concept to the upper extremity. Devices such as mobile arm supports with elevation assist (e.g., Jaeco Multilink Elevation Assist) or deltoid aide counterbalanced slings (e.g., Swedish Help Arm or Mobility Arm) minimize the effects of gravity on a patient’s arm and can be graded to provide less assistance as the person increases in strength. When these patients have some hand function, these devices can be used effectively for task-specific training. When these patients have limited hand function, the Armeo or T-WREX (www. hocoma.com) may be effective devices. They enable patients with upper extremity weakness and limited grasp and release to exercise their arm while using virtual reality simulated functional activities such as grocery shopping and cleaning a stove top. These task-specific activities can be adjusted to each patient’s ability, and they motivate patients to use the available function in their arms and hands.41 These devices that minimize the effects of gravity on a patient’s arm have the potential to increase upper extremity strength and to improve functional performance. However, more research is needed to evaluate their effectiveness. See Chapters 11 and 28.
For persons with poor control of movement, constrain the degrees of freedom.
Persons learning a new task initially restrict the degrees of freedom at their joints by self-imposing some form of freezing of body segments.39 As a result, their performance appears stiff and uncoordinated. With practice, the performance becomes smoother and more coordinated as the restrictions on the degrees of freedom decrease. Unfortunately, some persons with central nervous system damage are not able to constrain the degrees of freedom at their joints. For example, Gillen identified poor postural stability and tremor as interfering with the functional performance of a person with multiple sclerosis and ataxia. He speculated “that performance would be improved by increasing postural stability and decreasing the number of joints (decreasing the degrees of freedom) required to participate in chosen tasks.”32 Therefore, he used orthotic devices, assistive technology, and adaptive positioning of the trunk and upper extremity to help his patient constrain the degrees of freedom and to increase stability, which enabled improved ADL performance. Thus, the occupational performance of a patient with tremor was enhanced by strategies to decrease the degrees of freedom at those joints.
For persons who do not use returned function in their involved extremities, use constraint-induced therapy.
A growing body of literature supports the beneficial effects of constraint-induced movement therapy (CIMT) for persons after stroke with active wrist extension and active finger extension.10,60,89 The original CIMT involves intensive therapy (i.e., about six hours per day for 10 days in a two-week period) while the less involved arm is constrained by a sling or glove. As a result, participants are forced to use their involved extremity to complete functional tasks, and thus CIMT counteracts the learned nonuse seen in many persons after stroke. CIMT is consistent with two assumptions of the OT task-oriented approach: “functional tasks help organize behavior and experimentation with various strategies leads to optimal solutions to motor problems”54 (see Chapters 6 and 10).
In most clinical settings, CIMT as originally proposed would not fit into the current structure of inpatient rehabilitation programs and current reimbursement practices. However, there is growing evidence that a less intense (i.e., less times per day) and more distributed (i.e., spread out longer than two weeks) form of CIMT is also effective.20,66,92 Thus, modified CIMT can be used within current rehabilitation programs. However, after stroke many persons do not meet the minimal eligibility requirements during their initial rehabilitation, so most CIMT programs are conducted on an outpatient basis for persons who are six months or more poststroke and who have sufficient return of function to benefit from CIMT. No evidence indicates that CIMT is effective for persons without some active wrist and finger extension. In the case of G.W., with the neglect of his involved extremity, he would not be a good candidate for CIMT now because he does not have sufficient active wrist and finger extension to benefit. At a later time, when that function does return, a trial of CIMT would be indicated. Chapters 6 and 10 contain more detailed discussions of CIMT. For a more detailed discussion of the OT task-oriented approach treatment, see Bass-Haugen, Mathiowetz, and Flinn.5
Summary
This chapter describes an OT task-oriented approach for persons after stroke and describes the theoretical basis for and assumptions of the approach, based on contemporary motor control, motor learning, and motor development literature. The chapter also provides a top-down evaluation framework that emphasizes the importance of evaluating role and occupational performance tasks first and then the selective assessment of personal and environmental factors. In addition, the chapter describes the application of treatment principles to various patient problems and, finally, includes a case study describing the application of the OT task-oriented approach to a specific person after stroke.
CASE STUDY Occupational Therapy Task-Oriented Approach for a Stroke Survivor
G.W. is a 69-year-old retired farmer who suffered a right cerebral vascular accident with resultant left hemiparesis five days ago. He was admitted to the acute care hospital and was then transferred to the rehabilitation unit today.
From the chart, it was learned that he is now medically stable. He is taking angiotensin-converting enzyme inhibitors for high blood pressure and Coumadin for prevention of a second stroke. He has been living in a small town with his wife since moving from their farm three years ago. His son, daughter-in-law, and their three children are farming in the local community.
Initial evaluation
The Role Checklist was administered to evaluate G.W.’s role performance. Although retired, he continued to help out his son part-time as needed on the farm. He did most of the home maintenance, including the yard and a small garden. He attended church regularly, was a member of the men’s club, and volunteered for the annual church dinner. In addition to his son who farms, he has another son and daughter, who are married and live within a two-hour drive. He has eight grandchildren. He and his wife enjoyed traveling with another retired couple from their church.
The COPM was administered to evaluate occupational performance tasks. The following five tasks were rated as most important to him: dressing, bathing, driving, gardening, and helping his son on the farm. His performance and satisfaction for these tasks were rated low. However, he had not had the opportunity to try the latter three tasks since his stroke, and nursing staff assisted him with dressing and bathing. He reported that he was independent in sink hygiene tasks, feeding (except for cutting meat), and toileting (except for pulling up and fastening trousers). He could ambulate 10 feet with a large, quad-based cane with moderate assistance. His wife did all the grocery shopping and cooking. G.W. had helped his wife with the laundry. He was unsure whether he would be able to play cards in the men’s club now.
Dressing and bathing were chosen as tasks to be observed on the following day. G.W. was not able to dress himself independently primarily because of inability to use and/or neglect in using his left upper extremity. When cued to use his left arm, he demonstrated some voluntary control of his left shoulder and elbow and limited movement in the wrist and fingers. He complained of numbness in his left hand. During the bathing assessment, he needed assistance getting into and out of a tub. However, he could transfer in and out of the tub using a standard transfer bench. Once in the tub, he could control the water and bathe himself with one hand. He demonstrated good sitting balance during these activities, and he could stand independently when he could hold onto something with his right arm. He complained about the amount of time and energy it took him to perform self-care tasks. He demonstrated no evidence of cognitive or perceptual deficits except for some neglect of his left arm and left visual space. Based on these observations, it appeared that sensorimotor factors (decreased strength, endurance, range of motion, sensation, and neglect) were potential causes of limitations in occupational performance tasks, so these factors were selected for further evaluation. In contrast, cognitive and psychosocial factors appeared to be potential supports for increased independence. In addition, it appeared that modification of the environment (e.g., use of adaptive equipment such as a bath chair, Kno-Bows for shoe fasteners, and rocker knife) could be used to enable occupational performance tasks. However, more information was needed regarding his home and community environment to prepare for his discharge to home.
Tables 4-1 and 4-2 show the results of manual muscle testing, passive range of motion, and hand strength assessments for the left upper extremity only.
Sensory testing indicated a loss of protective sensation and diminished light touch in the left hand (Semmes-Weinstein monofilaments) and impaired proprioception in the left forearm, wrist, and hand. A line bisection test showed moderate visual neglect of the left side.
Home environment
G.W. and his wife live in a small two-story home. Their bedroom, bathroom, kitchen, living room, and dining room are on the main floor. The upstairs has two bedrooms, a bathroom, and storage space. The washer and dryer are located in the basement. The front and back of the home have five steps with a handrail on one side only. They have a one-car detached garage that is close to the house. They have a 10-year-old car with a stick shift. They have a 10 × 20 foot vegetable and flower garden in their backyard.
Their home is paid for, and they receive modest checks from Social Security and some farm rental income from their son. If they stay healthy, their income is adequate for what they want to do. However, they are worried that if one or both of them were to become disabled and require nursing home care, then their income would not be sufficient to cover expenses.
Community environment
Their house is located one block from their church and four blocks from the downtown area, which includes a grocery store, drug store, barber shop, post office, liquor store, and a small cafe. Their small town has no clothing or hardware store. They must drive 20 miles to a larger town for these supplies and medical care. Their son’s farm is located five miles from their house. The church has a split-level entrance with 10 steps to church level and 10 steps to the basement where the men’s club meets. Fortunately, the church installed a chair glide to assist persons with mobility problems to get into church. However, no chair glide is available for the basement level. At this time, he knows that he cannot get up and down 10 steps, and this is a concern.
After a discussion of the evaluation results, the patient and therapist agreed on the following goals.
Week 1 treatment plan
1. Increase active use of the left upper extremity during ADL and leisure tasks (i.e., avoid neglect and learned nonuse of the left arm and hand).
2. Increase independence in ADL and leisure tasks.
3. Begin planning for discharge to home and for possible roles for him on his son’s farm.
The patient became aware through the evaluation process that he tended to neglect his left arm and hand and was motivated to improve its function. Thus, he was open to experimenting with using his left upper extremity to assist during functional tasks. He was taught one-handed dressing techniques with reminders to use his left arm and hand as much as possible. For example, G.W. was encouraged to raise his left arm as he slid his shirt on and to use his left hand to stabilize his shirt and pants while buttoning. Various options for tying his shoes were explored. He chose to use Kno-Bows because of the ease of using them compared with alternatives. A rocker knife was chosen to enable independent cutting of meat. The therapist communicated with his wife and nursing staff on what he was able to do relative to ADL tasks and what adapted equipment (e.g., bath chair) he needed to be independent. G.W. was independent in bathing himself when the bath chair was available to him. He expressed some concern about slipping and falling when he would get home. Plans were made to order the grab bars, bath chair, and nonskid bath mat.
In addition, various leisure activities including card playing were explored. He was able to pull cards toward himself with his left hand but was unable to pick them up or hold them. A cardholder was prescribed so that he could play cards immediately. Although he only had a mild interest in playing checkers, he found out that he could slide enlarged checkers with his left hand and was willing to work at this activity to improve his left arm and hand function.
During one session, his son and wife came to discuss his roles at home and on his son’s farm. Both of them suggested that they could get help for the things that he could not do. Although G.W. agreed that there were some tasks he could no longer do or did not care to do, he still wanted to do some gardening and to help with some things on the farm. He did not want just to sit around and watch television. After brainstorming what roles and tasks might still be possible, the discussion shifted to adapted strategies and equipment that might be needed to make these tasks possible.
At the end of the first week, he was able to perform all ADL task with minimal supervision (i.e., reminders to use his left hand and to search his left visual space). He could now walk 30 feet with his cane and was practicing going up and down steps in physical therapy.
Week 2 treatment plan
1. Explore the possibility of driving and continued gardening.
2. Finalize plans for discharge to home, including ordering and installing adapted devices.
The patient was evaluated on some aspects of driving using a modified car. He was able to transfer in and out of the car with moderate supervision. He was discouraged that he was not able to push in the clutch with his left foot. He preferred driving a stick shift but could see that a car with an automatic transmission would be easier for him. He agreed to discuss getting a different car with his wife and son. Other adaptations that might make driving easier and safer were explored. The issue of neglect of his left visual field was discussed and evaluated using a driving simulator. He did have problems (i.e., simulated crashes) because of neglect. It was decided that additional practice with the simulator and other activities to improve his visual scanning were necessary before he could drive again.
G.W. continued to use various leisure and ADL activities to increase active use of his left arm and hand. Set-up of the activities was structured to require increased visual scanning as he did these activities.
Although G.W. continued to improve in his walking and stair-climbing ability, it was decided that a second handrail should be installed at both entrances to the home and in the basement and upstairs stairways. His son agreed to arrange for someone to do this. In addition, he agreed to install grab bars in the bathroom and in the hallway between the bathroom and bedroom. Sometimes, G.W. needed to use the bathroom at night.
Although he was improving in his performance on the driving simulator, he was told that he was not yet safe to drive. G.W. was referred to a regional driving center, which evaluates and trains persons with disabilities in safe driving. His wife or son would drive him until he could drive again.
A home program was developed with a variety of tasks and activities that required the use of his left arm and hand. He was now approaching the level of function that made him an appropriate candidate for CIMT. Unfortunately, access to this type of program was not feasible for G.W. because of distance and money. The therapist explained the concept of CIMT and developed a modified program that G.W. could do on his own. The modified program was adapted from a small study by Page and colleagues67 and provided some evidence that an outpatient program of CIMT could be beneficial. Three outpatient follow-ups were scheduled to monitor and upgrade his home program.
Review questions
1. What are at least four assumptions of the occupational therapy task-oriented approach?
2. What is the primary focus of an evaluation of persons after stroke using the occupational therapy task-oriented approach?
3. From an occupational therapy task-oriented approach perspective, when is it appropriate to evaluate a performance component?
4. Describe at least four intervention principles of the occupational therapy task-oriented approach and how they could be applied to persons after stroke.
5. Describe at least two ways that contemporary motor learning principles could be applied to persons after stroke.
1. American Occupational Therapy Association. Occupational therapy practice framework. domain and process, ed. 2. Am J Occup Ther. 2008:62;6:625-683.
2. American Occupational Therapy Association. Uniform terminology for occupational therapy, ed 3. Am J Occup Ther. 1994;48(11):1047-1054.
3. Arnadattoir G. In The brain and behavior: assessing cortical dysfunction through activities of daily living. St Louis: Mosby; 1990.
4. Barris R, Oakley F, Kielhofner G. The role checklist. In: Hemphill BJ, editor. Mental health assessment in occupational therapy. Thorofare, NJ: Slack, 1988.
5. Bass-Haugen J, Mathiowetz V, Flinn N. Optimizing motor behavior using the occupational therapy task-oriented approach. In Radomski MV, Latham CAT, editors: Occupational therapy for physical dysfunction, ed 6, Baltimore: Lippincott Williams & Wilkins, 2008.
6. Bernspang B, Asplund K, Eriksson S, et al. Motor and perceptual impairments in acute stroke patients. effects on self-care ability. Stroke. 1987:18;6:1081-1086.
7. Bernstein N. The coordination and regulation of movements. Elmsford, NY: Pergamon Press; 1967.
8. Bobath B. Adult hemiplegia: evaluation and treatment, ed 3. Oxford: Butterworth-Heinemann; 1990.
9. Bobath B. Adult hemiplegia: evaluation and treatment, ed 2. London: William Heinemann Medical Books; 1978.
10. Bonaiuti D, Rebasti L, Sioli P. The constraint induced movement therapy. a systematic review of randomized controlled trials on the adult stroke patients. Eura Medicophys. 2007:43;2:139-146.
11. Bourbonnais D, Vanden Noven S. Weakness in patients with hemiparesis. Am J Occup Ther. 1989;43(5):313-319.
12. Brunnstrom S. Movement therapy in hemiplegia,. New York: Harper & Row; 1970.
13. Burton AW, Davis WE. Optimizing the involvement and performance of children with physical impairments in movement activities. Pediatr Exerc Sci. 1992;4:236-248.
14. Carr JH, Shepherd RB. Neurological rehabilitation: optimizing motor performance. Oxford: Butterworth-Heinemann; 1998.
15. Carr JH, Shepherd RB. A motor relearning programme for stroke, ed. 2. Rockville, MD: Aspen; 1987.
16. Christiansen C, Baum C. Person-environment occupational performance. a conceptual model for practice. Christiansen C, Baum C, editors. Occupational therapy: enabling function and well-being,. Thorofare, NJ: Slack, 1997.
17. Cooper B, Letts L, Rigby P, et al. Measuring environmental factors. In: Law M, Baum C, Dunn W, editors. Measuring occupational performance: supporting best practice in occupational therapy. Thorofare, NJ: Slack, 2001.
18. Davis WE, Burton AW. Ecological task analysis. translating movement behavior theory into practice. Adapted Phys Activity Q. 1991:8;2:154-177.
19. Dean CM, Shepherd RB. Task-related training improves performance of seated reaching tasks after stroke. Stroke. 1997;28(4):722-728.
20. Dettmers C, Teske U, Hamzei F, et al. Distributed form of constraint-induced movement therapy improves functional outcome and quality of life after stroke. Arch Phys Med Rehabil. 2005;86(2):204-209.
21. Dunn W. Measurement of function. actions for the future. Am J Occup Ther. 1993:47;4:357-359.
22. Fasoli S, Trombly CA, Tickle-Degnen L, et al. Effect of instructions on functional reach in persons with and without cerebrovascular accident. Am J Occup Ther. 2002;56(4):380-390.
23. Fellows SJ, Kaus C, Thilmann A. Voluntary movement at the elbow in spastic hemiparesis. Ann Neurol. 1994;36(3):397-407.
24. Fisher A. Assessment of motor and process skills, ed 3. Fort Collins, CO: Three Star Press; 1999.
25. Fisher AG, Short-DeGraff M. Improving functional assessment in occupational therapy. recommendations and philosophy for change. Am J Occup Ther. 1993:47;3:199-201.
26. Flinn N. A task-oriented approach to the treatment of a client with hemiplegia. Am J Occup Ther. 1995;49(6):560-569.
27. Fugl-Meyer AR, Jääskö L, Leyman I, et al. The post-stroke hemiplegic patient. a method for evaluation of physical performance. Scand J Rehabil Med. 1975:7;1:13-31.
28. Galski T, Bruno RL, Zorowitz R, et al. Predicting length of stay, functional outcome, and aftercare in the rehabilitation of stroke patients. the dominant role of higher-order cognition. Stroke. 1993:24;12:1794-1800.
29. Gibson JJ. In The ecological approach to visual perception. Boston: Houghton Mifflin; 1979.
30. Gibson JJ. The theory of affordances. In: Shaw R, Bransford J, editors. Perceiving, acting, and knowing,. Hillsdale, NJ: Erlbaum, 1977.
31. Gillen G. Improving mobility and community access in an adult with ataxia. Am J Occup Ther. 2002;56(4):462-466.
32. Gillen G. Improving activities of daily living performance in an adult with ataxia. Am J Occup Ther. 2000;54(1):89-96.
33. Gleick J. Chaos: making a new science. New York: Penguin Books; 1987.
34. Gordon J, et al. Assumptions underlying physical therapy interventions. theoretical and historical perspectives. Carr JH, Shepherd RB, Gordon J, editors. Movement science: foundations for physical therapy in rehabilitation. Rockville, MD: Aspen, 1987.
35. Gresham GE, Duncan PW, Stason WB, et al. Post-stroke rehabilitation: clinical practice guidelines. No 16, AHCPR Pub No 95–0662, Rockville, MD: US Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research; 1995.
36. Gresham GE, Phillips T, Wolf P, et al. Epidemiologic profile of long-term stroke disability. the Framingham study. Arch Phys Med Rehabil. 1979:60;11:487-491.
37. Hanlon RE. Motor learning following unilateral stroke. Arch Phys Med Rehabil. 1996;77(8):811-815.
38. Heriza C. Motor development. traditional and contemporary theories. Lister MJ, editor. Contemporary management of motor control problems: proceedings of the II STEP conference,. Alexandria, VA: Foundation for Physical Therapy, 1991.
39. Higgins S. Motor skill acquisition. Phys Ther. 1991;71(2):123-139.
40. Horak FB. Assumptions underlying motor control for neurologic rehabilitation. In: Lister MJ, editor. Contemporary management of motor control problems: proceedings of the II STEP conference. Alexandria, VA: Foundation for Physical Therapy, 1991.
41. Housman SJ, Scott KM, Reinkensmeyer DJ. A randomized controlled trial of gravity-supported, computer-enhanced arm exercise for individuals with severe hemiparesis. Neurorehabil Neural Repair. 2009;23(5):505-514.
42. Howle JM. Neuro-developmental treatment approach: theoretical foundations and principles of clinical practice. Laguna Beach, CA: Neuro-Developmental Treatment Association; 2002.
43. Indredavik B, Bakke F, Solberg R, et al. Benefit of a stroke unit. a randomized controlled trial. Stroke. 1991:22;8:1026-1031.
44. Ingles JL, Eskes GA, Phillips SJ. Fatigue after stroke. Arch Phys Med Rehabil. 1999;80(2):173-178.
45. Jongbloed L, Stanton S, Fousek B. Family adaptation to altered roles following stroke. Can J Occup Ther. 1993;60(2):70-77.
46. Kamm K, Thelen E, Jensen JL. A dynamical systems approach to motor development. Phys Ther. 1990;70(12):763-775.
47. Kielhofner G. User’s manual for the OPHI-II. Chicago: Model of Occupational Performance Clearinghouse; 1988.
48. Knott M, Voss DE. Proprioceptive neuromuscular facilitation, ed 2. New York: Harper & Row; 1968.
49. Latham CAT. Conceptual foundations for practice. In Radomski MV, Latham CAT, editors: Occupational therapy for physical dysfunction, ed 6, Baltimore: Lippincott Williams & Wilkins, 2008.
50. Law M, Baptiste S, Carswell A, et al. Canadian Occupational Performance Measure, ed. 3. Ottawa: CAOT Publications; 1998.
51. Law M, Cooper B, Strong S, et al. Theoretical contexts for the practice of occupational therapy. In Christiansen C, Baum C, editors: Occupational therapy: enabling function and well-being, ed 2, Thorofare, NJ: Slack, 1997.
52. Lin K-C, Wu C-Y, Tickle-Degnen L, et al. Enhancing occupational performance through occupationally embedded exercise. a meta-analytic review. Occup Ther J Res. 1997:17;1:25-47.
53. Lister MJ. Contemporary management of motor control problems: proceedings of the II STEP conference. Alexandria, VA: Foundation for Physical Therapy; 1991.
54. Mathiowetz V, Bass-Haugen J. Assessing abilities and capacities. motor behavior. Radomski MV, Latham CAT, editors. Occupational therapy for physical dysfunction, ed 6. Baltimore: Lippincott Williams & Wilkins. 2008.
55. Mathiowetz V, Bass-Haugen J. Evaluation of motor behavior. traditional and contemporary views. Trombly CA, editor. Occupational therapy for physical dysfunction, ed 4, Baltimore: Williams & Wilkins, 1995.
56. Mathiowetz V, Bass-Haugen J. Motor behavior research. implications for therapeutic approaches to CNS dysfunction. Am J Occup Ther. 1994:48;8:733-745.
57. Mathiowetz VG, Wade M. Task constraints and functional motor performance of individuals with and without multiple sclerosis. Ecol Psychol. 1995;7(2):99-123.
58. McNevin NH, Wulf G, Carlson C. Effects of attentional focus, self-control, and dyad training on motor learning. implications for physical rehabilitation. Phys Ther. 2000:80;4:373-385.
59. Merians A, Winstein C, Sullivan K, et al. Effects of feedback for motor skill leaning in older healthy subjects and individuals post-stroke. Neurol Rep. 1995;19(2):23-25.
60. Morris DM, Crago JE, Deluca SC, et al. Constraint-induced movement therapy for motor recovery after stroke. NeuroRehab. 1997;9(1):29-43.
61. Nelson DL, Konosky K, Fleharty K, et al. The effects of occupationally embedded exercise on bilaterally assisted supination in persons with hemiplegia. Am J Occup Ther. 1996;50(8):639-646.
62. Newell KM. Constraints on the development of coordination. In: Wade MG, Whiting HTA, editors. Motor development in children: aspects of coordination and control. Dordrecht, Netherlands: Martinus Nijhoff, 1986.
63. Oakley F, Kielhofner G, Barris R, et al. The Role Checklist. development and empirical assessment of reliability. Occup Ther J Res. 1986:6;3:157-170.
64. O’Dwyer NJ, Ada L, Neilson PD. Spasticity and muscle contracture following stroke. Brain. 1996;119(pt 5):1737-1749.
65. Olsen TS. Arm and leg paresis as outcome predictors in stroke rehabilitation. Stroke. 1990;21(2):247-251.
66. Page SJ, Levine P, Leonard A, et al. Modified constraint-induced therapy in chronic stroke. Results of a single-blinded randomized controlled trial. Phys Ther. 2008:88;3:333-340.
67. Page SJ, Sisto SA, Levine P, et al. Modified constraint induced therapy. a randomized feasibility and efficacy study. J Rehabil Res Dev. 2001:38;5:583-590.
68. Radomski MV. Assessing context. personal, social, and cultural. Radomski MV, Latham CAT, editors. Occupational therapy for physical dysfunction, ed 6, Baltimore: Lippincott Williams & Wilkins, 2008.
69. Flinn NA, Radomski MV. Learning. In Radomski MV, Latham CAT, editors: Occupational therapy for physical dysfunction, ed 6, Baltimore: Lippincott Williams & Wilkins, 2008.
70. Reding MJ, Potes E. Rehabilitation outcomes following initial unilateral hemispheric stroke. life table analysis approach. Stroke. 1988:19;11:1354-1358.
71. Rood MS. Neurophysiological reactions as a basis for physical therapy. Phys Ther Rev. 1954;34(9):444-449.
72. Sahrmann SA, Norton BJ. The relationship of voluntary movement to spasticity in the upper motor neuron syndrome. Ann Neurol. 1977;2(6):460-465.
73. Schmidt RA. Motor learning and performance: from principles to practice. Champaign, IL: Human Kinetics; 1991.
74. Schmidt RA. Motor learning principles for physical therapy. In: Lister MJ, editor. Contemporary management of motor control problems: proceedings of the II STEP conference,. Alexandria, VA: Foundation for Physical Therapy, 1991.
75. Schmidt RA. Motor control and learning: a behavioral emphasis, ed 2. Champaign, IL: Human Kinetics; 1988.
76. Shea JB, Morgan R. Contextual interference effects on the acquisition, retention, and transfer of a motor skill. J Exp Psychol Hum Learn Mem. 1979;5(2):179-187.
77. Shumway-Cook A, Woolacott M. Motor control: theory & practical application. Baltimore: Williams & Wilkins; 1995.
78. Spencer J, Krefting L, Mattingly C. Incorporation of ethnographic methods in occupational therapy assessment. Am J Occup Ther. 1993;47(4):303-309.
79. Gunnar MR, Thelen E, Thelen E. Self-organization in developmental processes. can systems approaches work. Systems and development. Hillsdale, NJ: Erlbaum. 1989.
80. Thelen E, Fisher DM. Newborn stepping. an explanation for a “disappearing reflex. Dev Psychol. 1982:18;5:760-775.
81. Thelen E, Ulrich BD. Hidden skills. Monograph of the Society for Research in Child Development. 56 (serial no 223), Chicago: University of Chicago Press. 1991.
82. Titus MN, Gall NG, Yerxa EJ, et al. Correlation of perceptual performance and activities of daily living in stroke patients. Am J Occup Ther. 1991;45(5):410-418.
83. Turvey MT. Preliminaries to a theory of action with reference to vision. In: Shaw R, Bransford J, editors. Perceiving, acting, and knowing. Hillsdale, NJ: Erlbaum, 1977.
84. Van Peppen RPS, Kwakkel G, Wood-Dauphinee S, et al. The impact of physical therapy on functional outcomes after stroke. What’s the evidence. Clin Rehabil. 2004:18;8:833-862.
85. VanSant A. Should the normal motor developmental sequence be used as a theoretical model to progress adult patients. In: Lister MJ, editor. Contemporary management of motor control problems: proceedings of the II STEP conference,. Alexandria, VA: Foundation for Physical Therapy, 1991.
86. VanSant A. Life-span development in functional tasks. Phys Ther. 1990;70(12):788-798.
87. Warren WH. Perceiving affordances. visual guidance of stair climbing. J Exp Psychol Hum Percept Perform. 1984:10;5:683-703.
88. Winstein CJ, Schmidt RA. Reduced frequency of knowledge of results enhances motor skill learning. J Exp Psychol [Learn Mem Cogn]. 1990;16(4):677-691.
89. Wolf SL, Winstein CJ, Miller JP, et al. Effect of constraint-induced movement therapy on upper extremity function 3 to 9 months after stroke. the EXCITE randomized trial. JAMA. 2006:296;17:2095-2103.
90. World Health Organization. International classification of functioning, disability, and health. Geneva: World Health Organization; 2001.
91. Wu CY, Trombly CA, Lin KC, et al. A kinematic study of contextual effects on reaching performance in persons with and without stroke. influence of object availability. Arch Phys Med Rehabil. 2000:81;1:95-101.
92. Wu C, Chen C, Tsai W, et al. A randomized controlled trial of modified constraint-induced movement therapy for elderly stroke survivors. Changes in motor impairment, daily functioning, and quality of life. Arch Phys Med Rehabil. 2007:88;3:273-278.