CHAPTER 6
Clinical Examination of the Hand
JODI L. SEFTCHICK, MOT, OTR/L, CHT, LAUREN M. DETULLIO, MS, OTR/L, CHT, JANE M. FEDORCZYK, PT, PhD, CHT, ATC, AND PAT L. AULICINO, MD
CRITICAL POINTS
▪ Observation, visual inspection, and palpation provide information regarding the patient’s general health status and present condition.
▪ Therapists and surgeons need to obtain a thorough patient history so that they can understand the patient’s problem and how it affects the patient physically, psychologically, and economically.
▪ Perform a systematic examination, documenting and organizing the results well.
▪ Include medical screening and systems review with all patients.
Clinical examination of the hand is a basic skill that both the surgeon and the therapist should master. To do so, it is necessary to understand the functional anatomy of the hand. A thorough history, a systematic examination, and knowledge of disease processes that affect the hand minimize the examiner’s diagnostic dilemmas. Radiographs, CT scans, MRI scans, electrodiagnostics, and specialized laboratory tests are ancillary tools that only confirm a diagnosis that has been made on a clinical basis (see Chapters 13 and 15).
An organized approach and clear and concise records are of paramount importance. Either line drawings of the deformities or clinical photographs should be prepared for each new patient examined. Digital photographs may be a more efficient means for storage with electronic medical records. Range of motion (ROM) of the affected parts should be recorded and dated, ideally in a table format. Any discrepancy between active and passive motion, if present, also should be noted. A good hand examination is useless if the results are not recorded accurately.
This chapter outlines one approach to examination of the hand. The most important points already have been made: perform a systematic, organized clinical examination and record the results accurately and clearly.
History
Before a patient’s hand is examined, an accurate history must be taken. The patient’s age, hand dominance, occupation, and avocations are elicited. Another option for determining hand dominance is to administer the Waterloo Handedness Questionnaire (see Fig. 12-3).1 If the patient has had an injury, the exact mechanism as well as the time and date of the injury and prior treatments are recorded. Prior surgical procedures, infections, medications, and therapy also are noted. After this background information is obtained, the patient is questioned specifically regarding the involved hand and extremity, including a pain interview. (See Box 114-1 and Chapter 114 for additional information on pain assessment.) Open-ended questions about the present signs and symptoms are included to determine what the patient is not able to do now that he or she could do before the injury or what brought the patient to the surgeon or therapist. Questions related to the history of present illness allow the clinician to develop a hypothesis about the level of irritability. Low irritability is defined as minimal to no pain at rest, transient pain with movement, and symptoms that are not easily provoked. Highly irritable conditions present with resting pain, higher pain levels with activity, and decreased mobility. The level of irritability determines how vigorously the surgeon or therapist may perform the tests and measures during the physical examination and direct treatment goals.
What are the patient goals? This question is extremely important. The patient’s reply assists the clinician in determining whether the patient has a realistic understanding of the true nature of the injury. Unrealistic expectations can never be fulfilled and result in both disappointment and frustration for both the patient and the therapist and surgeon. During this interview, it is also important to assess the effect that the injury or disease process has on the patient’s family and economic and social life. Patients who have litigation pending or possible significant secondary gain may be poorly motivated and are not optimal candidates for elective hand surgery. Successful hand surgery requires precise surgical techniques followed by expert hand therapy in conjunction with a well-motivated, compliant patient.
The patient’s pertinent medical history is obtained to determine general health status, especially regarding comorbidities that may affect the patient’s recovery or increase surgical risks? Additional questions should be asked about current medications (prescription and nonprescription), allergies, and lifestyle choices (smoking, alcohol use, or substance abuse). Current practice trends require hand surgeons and therapists to do medical screening and review of systems.2 This is a key component in medical education and training; however, it is a recent addition to the entry-level education for therapists, especially physical therapists. More information is provided later in this chapter.
The patient’s social history should be obtained. What is his support system? How well do the patient and his family understand the injury and required care? What are his avocational interests? The patient’s economic status may also influence ability to comply with therapy and follow-up care. What is his insurance coverage or co-pay amount? Does he have a limited number of authorized visits? Does his injury present a financial hardship or limit his ability to care for children or elderly parents?
If the patient is working, information should be gathered about his job description, physical demands, or essential functions, and the last date worked even if the injury is not work-related. This information may indicate the presence of risk factors associated with the injury. Therapists and surgeons can use these data to outline a plan of care that incorporates appropriate modified duty work, if available, and the use of work-oriented tasks in the clinic to keep the patient on track to return to full duty. Although it may be too early in the examination process to discern a return to work date, an experienced clinician can usually tell how motivated the patient is to return to his job based on the patient’s answers regarding employment. Patient’s who are receiving compensation for an injury or illness may be more difficult to treat, more likely to have a prolonged course of rehabilitation, and more likely to become disabled than patients with similar conditions who are not receiving compensation.3
Self-report health-related outcome measures such as Disabilities of the Arm, Shoulder, and Hand (DASH),4 Carpal Tunnel Instrument,5 or Michigan Hand Outcomes Questionnaire (MHQ)6 can serve as valuable tools for gathering information on pain, function, activity participation, disability, and patient satisfaction.7,8 These measures have all proven to be reliable and valid.4-6 The Carpal Tunnel Instrument is a condition-specific measure, whereas the DASH and MHQ are region-specific. Global measures such as the SF-36 and patient-specific scales that contain no standardized questions may also be used.7,8 These questionnaires can be invaluable in gathering information about problems with activities of daily living (ADL), such as toileting or sexual activity. Patients are not usually comfortable addressing these issues upfront. It is important for the examiner to become familiar with self-report health-related outcome measures to determine which would be most useful and clinically relevant for the patient. Chapter 16 discusses the measurement issues and use of outcome measurement in the upper extremity.
The history is completed only after the surgeon or therapist has a complete understanding of the patient’s problem and how it affects the patient physically, psychologically, and economically.
Physical Examination
Observation, Inspection, and Palpation
Hands are used to interact with the surrounding environment and for communication. People “actively” use their hands for a variety of functional activities. “Passively” the hands communicate to clinicians about the health status of their patients. When examining a patient’s upper extremity, one must be able to observe the shoulder, arm, forearm, and hand. Therefore, the patient’s entire upper extremity should be exposed. The gross appearance of the entire extremity is inspected. Table 6-1 outlines the physical characteristics of the skin and musculoskeletal tissues that should be observed, inspected, and palpated during the physical examination to determine the presence of diseases such as arthritis, impairments such as edema and loss of motion, as well as level of irritability.
Table 6-1 Physical Characteristics of the Skin and Musculoskeletal Tissues That Should Be Observed, Inspected, and Palpated During the Physical Examination
General Observations |
Clinical Significance |
Hand relationship to the body
How does the patient carry the arm?
Is there spontaneity or ease of movement? |
Cradling the arm or guarded posture is a sign of patient apprehension to movement typically due to high levels of pain associated with a high level of irritability. |
What is the quality of the movement?
Is the patient using substitution patterns with movement? |
Signs of muscle weakness or loss of motion that may be related to nerve injury, disuse, or joint contracture |
Is the patient able to place his or her hand in a functional position? |
If not, the elbow and shoulder motion may be limited and should be examined. If the hand cannot be placed in a functional position, a brilliantly reconstructed hand is useless. |
Visual Inspection |
Clinical Significance |
Muscle atrophy |
Muscle weakness due to disuse or nerve injury |
Blisters and small cuts |
Sign of decreased cutaneous sensibility due to nerve injury |
Needle marks |
Indication of current or previous substance abuse or the use of injectable prescription medication for disease such as insulin-dependent diabetes |
Wounds and scars |
Scars indicate previous injuries or surgeries. Wounds may indicate decreased cutaneous sensibility. |
Skin color, tone, moisture, and trophic changes |
Sympathetic signs of nerve injury. Dry skin indication of peripheral nerve laceration. Increased sweating (hyperhidrosis) sign of increased sympathetic activity that may be related to complex regional pain syndrome (CRPS).* |
|
Color changes due to metabolic conditions or disease |
|
Skin that has been denervated has lost its autonomic input. The finger pulp becomes atrophic, smooth, and dry, with relative loss of dermal ridges. |
|
Denervated skin does not wrinkle when placed in warm water (the “wrinkle test”).31 |
Normal skin creases or ridges |
Diminished due to presence of edema or trophic changes of the skin associated with nerve injury |
Are the nails ridged, pitted, or deformed?
Is there correct rotational alignment of the nail plates? |
Nail changes linked to chronic diseases of the kidney, liver, respiratory system. Spoon nails found in patients with iron deficiency. Changes may be related to peripheral nerve injury. |
Edema, hematoma, ecchymosis |
Indicates acute tissue injury and healing |
Loss of resting attitude of the hand |
Indicates a tendon laceration, a contracture, or peripheral nerve injury |
Contractures |
Loss of motion |
Gross deformities |
Congenital, acquired, traumatic |
Preservation of hand arches |
Flattening of the aches associated with intrinsic muscle atrophy due to nerve injury or disuse |
Palpation |
Clinical Significance |
Temperature |
Warm temperature is a sign of acute inflammation. |
|
Cool temperature is a sign of decreased blood flow; may be vasomotor instability. |
Nodules, tumors |
Likely benign lesions that may be associated with wrist instability, arthritis, Dupuytren’s or other soft tissue conditions |
Edema |
Pitting edema leaves depressions with palpation. |
|
Brawny edema is immobile and hard to palpate. |
Capillary refill |
Skin should blanch when palpated and resume normal color when pressure removed. |
Skin mobility |
Lack of mobility due to fibrosis, scar, and edema |
Scar |
Painful to touch (tactile allodynia) indicates hypersensitivity. |
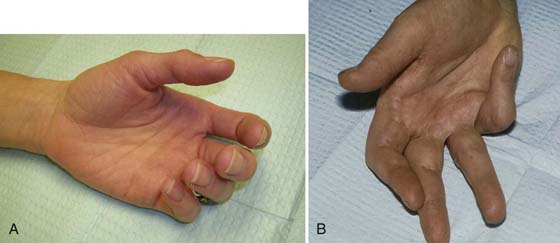
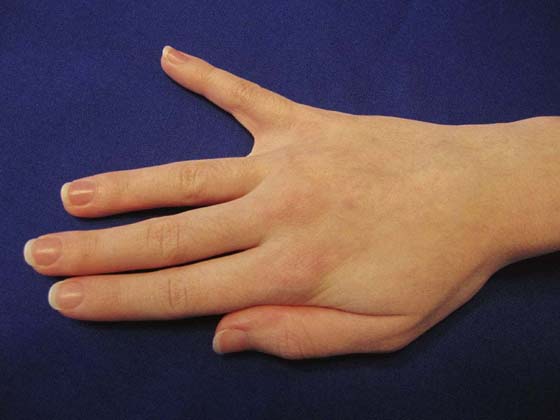
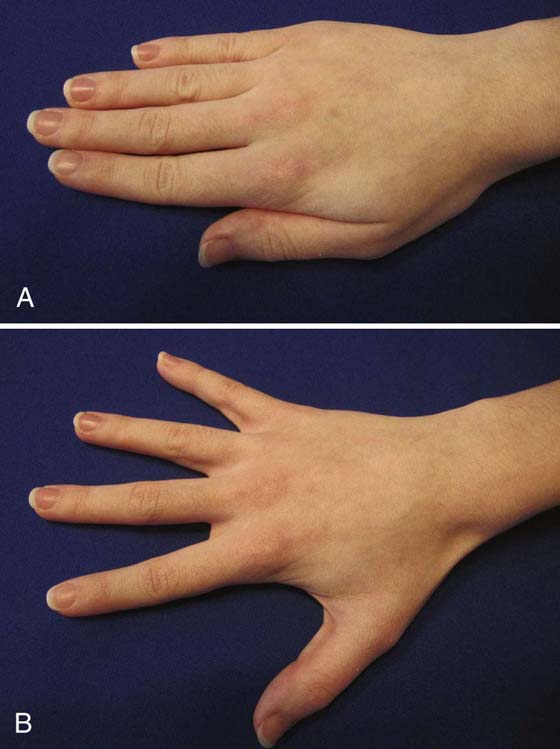
Skin and nail changes may be associated with chronic diseases of the kidney or liver as well as the respiratory system.2 A review of systems and past medical history should determine the associated condition. These changes are chronic, and the patient should already be aware of the condition. Normally, with the hand resting and the wrist in neutral, the fingers are progressively more flexed from the radial to the ulnar side of the hand. A loss of the normal resting attitude of the hand can indicate a tendon laceration, a contracture, or, possibly, a peripheral nerve injury (Fig. 6-1).
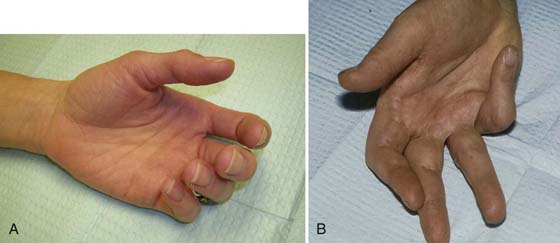
Figure 6-1 A, Normal attitude of the hand in a resting position. Notice that the fingers are progressively more flexed from the radial aspect to the ulnar aspect of the hand. B, This normal attitude is lost because of contractures of the digits as a result of Dupuytren’s disease.
Edema
Another important component of the clinical examination of the hand is to assess edema if noted on visual inspection. Edema may be assessed using circumferential or volumetric measurements. Volumetry is primarily used if the entire hand is edematous, but not for an isolated finger. Chapters 63 through 65 present detailed information on the examination and management of edema and lymphedema in the hand and upper extremity.
Range of Motion
The motion of the entire upper extremity and cervical region should be screened with hand injuries and compared with that of the opposite side for possible loss of motion and pain. Joints that demonstrate loss of active or passive motion (or both) should be measured with an appropriately sized goniometer.9 Measurements have been shown to be relatively reliable within and between examiners; intrarater and inter-rater variability is in the range of 5 to 10 degrees.10 If possible, the same examiner should take measurements.
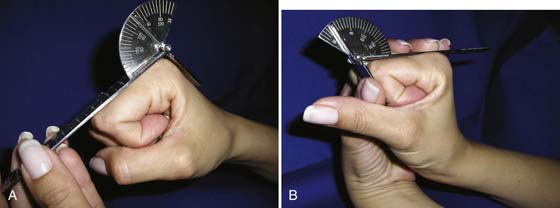
Digital motion is typically assessed with the metal finger goniometer placed on the dorsal aspect of the phalanges (Fig. 6-2). If it is not possible to place the goniometer on the dorsal aspect of the digit, then a lateral goniometer placement may be used and this exception should be documented. When possible, active measurements of the finger joints are taken in a composite manner by asking the patient to make a fist for flexion and then straighten the hand for extension. Isolated motions may be performed for an individual joint, typically with stabilization of the proximal joint; however, this should be recorded (Fig. 6-3).
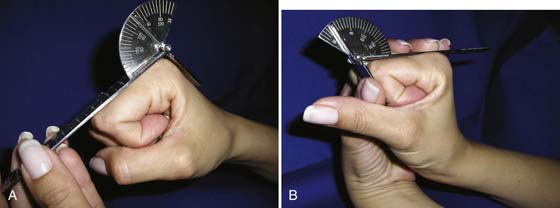
Figure 6-2 Digital motion is typically assessed with the metal finger goniometer placed on the dorsal aspect of the phalanges A, Measuring metacarpophalangeal flexion with the hand in composite flexion. B, Measuring proximal interphalangeal joint flexion with the hand in composite flexion.
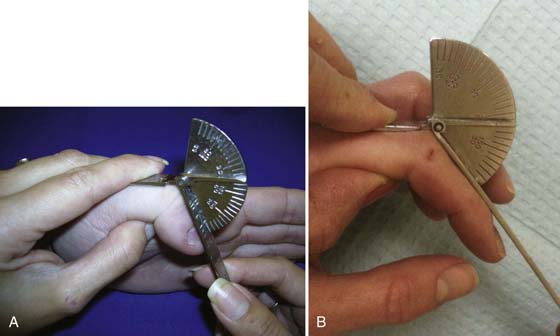
Figure 6-3 A, A finger goniometer is used to measure the range of motion (ROM) of the interphalangeal (IP) joint of the thumb. B, A finger goniometer is used to measure the ROM of the proximal IP joint of the index finger. Note proximal joint stabilization.
Total active motion (TAM) and total passive motion (TPM) measurements can be assessed for the individual digits. TAM is calculated by adding the composite flexion measurement of the metacarpophalangeal (MCP), proximal interphalangeal (PIP), and distal interphalangeal (DIP) joints and subtracting the sum of any extension deficits at these joints.11 TPM is computed the same way, except passive measurements are used. Both TAM and TPM provide relevant data on composite motion of the finger and allow ease of comparison over time. This type of documentation is frequently used in research.
Goniometry manuals should be reviewed for detailed information on measuring joint motion of the hand and upper extremity.12,13 When measuring carpometacarpal (CMC) motion of the thumb, some manuals describe the procedures differently. The starting angle for CMC extension or abduction is never 0 degrees; it is typically 25 to 30 degrees. Some manuals direct the clinician to measure the starting angle and subtract it from the measurements at the end of the available ROM. Some manuals just recommend that the examiner measure the end range motion. In terms of clinical relevance, only the end range motion is significant as it correlates with the patient’s ability to open the first webspace. Therapists and surgeons working together should agree on a standard procedure for their patients to allow comparison of measurements.
If motion is lacking, the distance from the tip of the finger to the distal palmar crease (DPC) is measured. If the finger touches the palm but does not reach the crease, as occurs with profundus tendon disruption, this should be noted, and the distance from the tip of the finger to the DPC should be recorded; however, it should be stated that the finger did touch the palm but did not reach the DPC (Fig. 6-4).

Figure 6-4 A ruler is used to measure the distance of the pulp of the finger from the distal palmar crease. Active and passive motions should be noted and recorded.
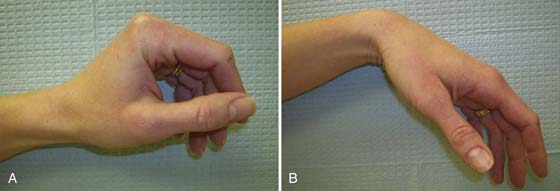
After all active and passive motions have been examined; the wrist is flexed and extended to see if the normal tenodesis effect is present. In an uninjured hand, when the wrist is flexed, the fingers and the thumb extend, and as the wrist is extended, the fingers assume an attitude of flexion and the thumb opposes the fifth digit (Fig. 6-5). This is an automatic motion of the hand and requires only that the patient be relaxed. The alignment of the digits is then inspected. The nail plates all should be parallel to one another, and their alignment should be similar to that of the other hand. Each finger should point individually to the scaphoid tuberosity, and the longitudinal axis of all fingers when flexed should point in the direction of the scaphoid (Fig. 6-6).
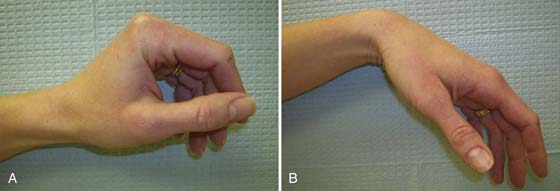
Figure 6-5 Tenodesis of the hand. In an uninjured hand (A), on wrist extension the fingers and thumb flex, and (B), on flexion of the wrist the thumb and fingers extend. In the presence of a tendon laceration, contractures of the joints, or adhesions of the flexor or extensor systems, the normal tenodesis effect is lost. This test can be performed actively by the patient or passively by the examiner.
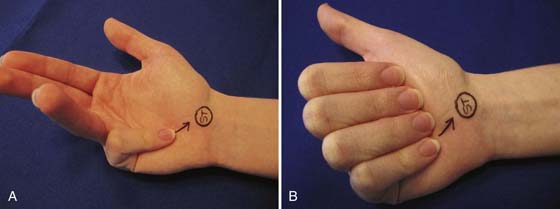
Figure 6-6 A, On flexion the tip of the fifth finger points directly to the scaphoid tuberosity, as do all the fingers when individually flexed. B, When all the digits are flexed simultaneously, the finger tips come together distal to the tuberosity, but the longitudinal axes of all fingers converge at an area proximal to the scaphoid tuberosity because of crowding of the adjacent digits. If there is a malunited fracture, the rotational alignment will be off and often there will be crossover of the digits.
Muscle Testing
The hand is powered by intrinsic and extrinsic muscles. The extrinsic muscles have their origin in the forearm and the tendinous insertions in the hand. The extrinsic flexors are on the volar side of the forearm and flex the digits and the wrist. The extrinsic extensors originate on the dorsal aspect of the forearm and extend the fingers, thumb, and wrist. The intrinsic muscles originate and insert in the hand. These include the thenar and hypothenar muscles as well as the lumbricals and the interossei. The thenar and hypothenar muscles help position the thumb and the fifth finger and also aid in opposition of the thumb and with pinch. The interossei assist in abduction and adduction of the digits. The interossei flex the MCP joints and extend the interphalangeal (IP) joints along with the lumbricals.
Extrinsic Muscle Testing—The Extrinsic Flexors
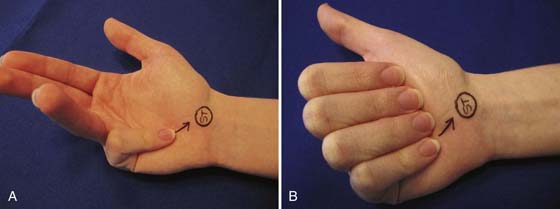
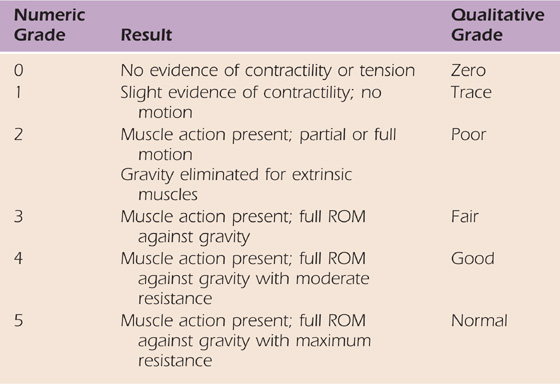
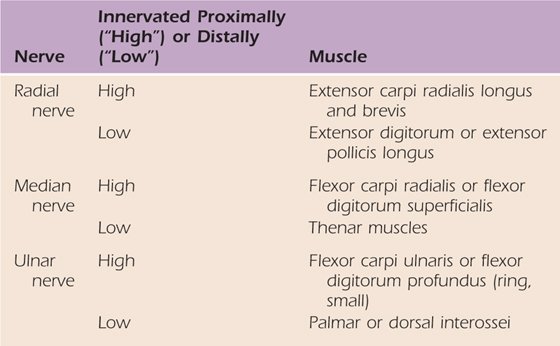
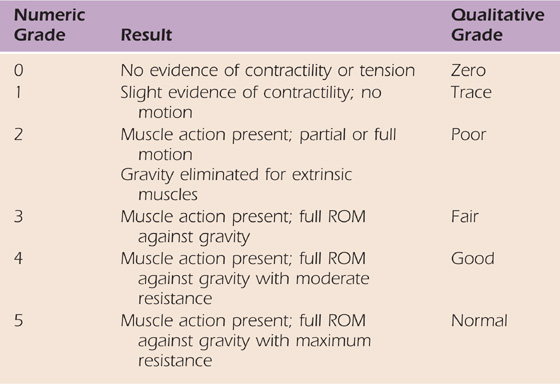
As each specific extrinsic muscle–tendon unit is tested, its strength should be graded and recorded (Table 6-2). The extrinsic muscles should be tested with respect to gravity, but this is not essential for the intrinsic muscles. Note tendon excursion during muscle contraction, which is reflected in ROM of the joints that the tendon acts on.
Table 6-2 Manual Muscle Testing Grades for Hand Muscles
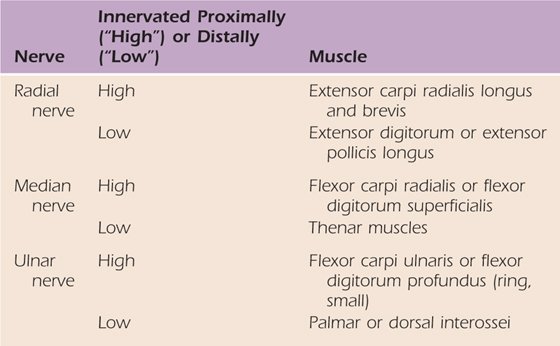
It is not necessary to test each hand muscle during examination. Key muscles for each nerve, radial, ulnar, and median, can be selected for screening. For each nerve, select one muscle that is innervated proximally (“high”) and one muscle that is innervated distally (“low”). Table 6-3 provides examples. If nerve injury is present, all muscles innervated by the injured nerve should be assessed to determine the level of injury and to document return.
Table 6-3 Key Muscles to Screen for Peripheral Nerve Function
The flexor pollicis longus (FPL) long flexor of the thumb flexes the IP joint of the thumb. This muscle is tested by asking the patient to actively flex the last joint of his thumb (Fig. 6-7).

Figure 6-7 Testing the flexor pollicis longus. A, With the thumb in a position of full extension at the interphalangeal joint. B, The patient is asked to actively flex this joint. C, It is also important to note whether the motion is obtained with or without blocking of the proximal joint by the examiner. This applies not only to testing the flexor pollicis longus but also to testing all other flexor systems because more power and motion can be obtained when blocking is used.
The flexor digitorum profundus of the fingers are then tested, in sequence, by having the patient flex the DIP joint of the finger being tested while the examiner holds the digit in full extension and blocks motion at the PIP joint and the MCP joint. During the testing of each profundus tendon, the other fingers may unintentionally flex due to the common muscle belly of the long, ring, and small finger profundus tendons, and this is permitted (Fig. 6-8).


Figure 6-8 Profundus test. A, The flexor digitorum profundus tendon flexes the distal interphalangeal joint. B, With the metacarpophalangeal joint and the proximal interphalangeal joint held in extension by the examiner, the patient is asked to flex the distal interphalangeal joint. (Redrawn from Hoppenfeld S: Physical Examination of the Spine and Extremities. New York: Appleton-Century-Crofts, 1976.)
The flexor digitorum superficialis of each finger is then tested. The examiner must hold the adjacent fingers in full extension. The PIP joint of the finger being tested is not blocked (Fig. 6-9). If the flexor system is functioning properly, the PIP will flex and the DIP joint will remain in extension. The fifth finger often has a deficient superficialis.14 That is, it is not strong enough to flex the IP joint: on testing, the MCP joint flexes and the DIP joint and the PIP joint remain in extension. In the presence of a deficient superficialis tendon of the fifth digit, simultaneous testing of the fourth and fifth digits often reveals normal superficialis function of the fourth digit.
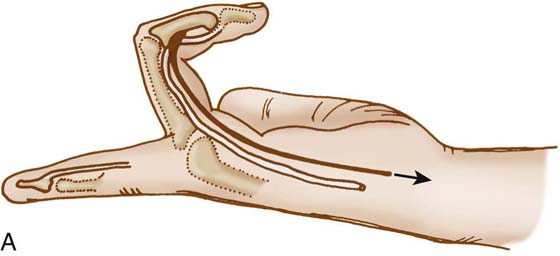

Figure 6-9 Superficialis test. A, The flexor digitorum superficialis tendon flexes the proximal interphalangeal (PIP) joint. B, The examiner must hold the adjacent fingers in full extension while asking the patient to flex the finger being tested. If the flexor system is functioning normally, the PIP joint will flex, while the distal interphalangeal joint remains in extension. (Redrawn by permission from Hoppenfeld S: Physical Examination of the Spine and Extremities. New York: Appleton-Century-Crofts, 1976.)
The flexors of the wrist can be tested by having the patient flex the wrist against resistance in a radial and then in an ulnar direction while the examiner palpates each tendon. The flexor carpi radialis (FCR) is palpated on the radial side of the wrist, and the flexor carpi ulnaris (FCU) is palpated on the ulnar side of the wrist. The palmaris longus tendon can be palpated just ulnar to the FCR tendon.
Extrinsic Muscle Testing—The Extensors
As previously stated, the extensors of the digits and the wrist originate on the dorsal aspect of the forearm and pass through six discrete retinacular compartments at the dorsum of the wrist before their insertions in the hand.
The first dorsal compartment contains the abductor pollicis longus (APL) and the extensor pollicis brevis (EPB) tendons. The APL usually has multiple tendon slips and inserts on the base of the first metacarpal. It often has insertions on the trapezium. The EPB often runs in a separate compartment within the first dorsal compartment. The EPB and APL function in unison and are responsible for abduction of the first metacarpal and extension into the plane of the metacarpals. The EPB is also an extensor of the MCP joint of the thumb. These musculotendinous units are tested by asking the patient to bring the thumb “out to the side and then back.” Pain in the area of the first dorsal compartment and radial styloid is common and often a result of stenosing tenovaginitis of these tendons. This was first described by de Quervain in 1895 and now is a well-established clinical entity that bears his name. In 1930, Finkelstein stated that acute flexion of the thumb and deviation of the wrist in an ulnar direction produces excruciating pain at the first dorsal compartment, near the radial styloid, in patients who had stenosing tenovaginitis. This examination is now universally known as Finkelstein’s test15 (see Fig. 7-9). The extensor carpi radialis longus and brevis run in the second dorsal compartment. The longus inserts on the base of the second metacarpal and the brevis on the third. These are tested by asking the patient to make a tight fist and to strongly extend or dorsiflex the wrist. The two tendons are then palpated by the examiner.
The extensor pollicis longus (EPL) runs in the third dorsal compartment. This tendon both extends the IP joint of the thumb and adducts the first ray. The tendon passes sharply around Lister’s tubercle and may rupture spontaneously after a distal radius fracture or in rheumatoid arthritis.16 Its function is tested by placing the patient’s hand flat on the examining table and having him or her lift only the thumb off the table. The EPL can be visualized and palpated (Fig. 6-10A).

Figure 6-10 A, The extensor pollicis longus (EPL) tendon is tested by placing the patient’s hand flat on the examining table and asking the patient to lift the thumb off the table. The EPL can then be visualized and palpated. B, Note that the EPL serves as the ulnar border to the anatomic snuff box and the extensor pollicis brevis and abductor pollicis longus create the radial border.
The area of the wrist just distal to the radial styloid and bounded by the EPL ulnarly and the APL and EPB radially is known as the anatomic snuffbox (Fig. 6-10B). In this area runs the dorsal branch of the radial artery. A sensory branch of the radial nerve also passes over this area. The scaphoid can be palpated in the base of the snuffbox. Tenderness in this area is suggestive of an acute scaphoid fracture or a painful scaphoid nonunion. However, strong pressure over this area results in pain in the normal individual caused by pressure on the sensory radial nerve and dorsal branch of the radial artery.
The fourth dorsal compartment contains the extensor indicis proprius (EIP) and the extensor digitorum communis (EDC). These tendons are responsible for extension of the MCP joints of the fingers. The EIP allows independent extension of the index MCP joint. The EIP is tested by having the patient extend the index finger while the other fingers are flexed into a fist. The mass action of the EDC tendons is tested by having the patient extend the MCP joints. This test is performed with the IP joints flexed because the PIP joints are extended by the intrinsic muscles and not the long extensors of the hand. This may be a source of confusion to an inexperienced examiner. Patients with a high radial nerve palsy are still be able to extend the IP joints through the intrinsics.
The fifth dorsal compartment contains the extensor digiti minimi (EDM), which is responsible for independent extension of the MCP joint of the little finger. It is tested by having the patient extend the fifth finger while the others are flexed. Because the EDM and the EIP work independently of the communis tendons, most examiners test them simultaneously by having the patient extend the index and fifth fingers while the middle and ring fingers are flexed.
The sixth dorsal compartment contains the extensor carpi ulnaris (ECU), which inserts into the base of the fifth metacarpal and helps extend the wrist in an ulnar direction. This is tested by having the patient pull the hand dorsally and in an ulnar direction while the examiner palpates the tendon.
Intrinsic Muscle Testing
The intrinsic musculature of the hand consists of the thenar and hypothenar muscles and the lumbricals and the interossei. All of these muscles originate and insert within the hand. There is a delicate balance between the intrinsic and extrinsic muscles, which is necessary for normal functioning of the hand.
The thenar muscles consist of the abductor pollicis brevis (AbPB), the flexor pollicis brevis (FPB), the opponens pollicis (OP), and the adductor pollicis (AdP). These muscles position the thumb and help perform the complex motions of opposition and adduction of the thumb.17 Opposition, according to Bunnell, takes place in the intercarpal, CMC, and MCP joints.18 All three of these joints contribute to the angulatory and rotatory motions that produce true opposition. If one observes the thumb during opposition, it first abducts from the hand and then follows a semicircular path. The thumb pronates, and the proximal phalanx angulates radially on the first metacarpal. If the nail plate is observed, one can see that before beginning opposition, the thumbnail is perpendicular to the plane of the metacarpals. At the end of the opposition, the thumbnail is parallel to the plane of the metacarpals. During adduction, the thumb sweeps across the palm without following the semicircular path. The nail plate remains perpendicular to the plane of the metacarpals at all times. Because opposition is median nerve innervated and adduction is usually ulnar nerve innervated, one can easily see the difference between these two motions by comparing the hands of a patient with a longstanding low median nerve palsy on one side (Fig. 6-11).

Figure 6-11 Hands of a patient with a low median nerve palsy on the right side, resulting from a longstanding carpal tunnel syndrome. Notice that in attempted opposition, the nail plate is perpendicular to the plane of the metacarpals on the affected side (right), while the nail plate is parallel to the plane of the metacarpals on the normal side (left). Tip-to-tip pinch is impossible on the side with the loss of opposition.
Opposition is tested by having the patient touch the tip of the thumb to the tip of the little finger. At the end of opposition, the thumbnail should be perpendicular to the nail of the little finger and parallel to the plane of the metacarpals.
The AbPB, which is the most radial and superficial of the thenar muscles, is usually the first to atrophy with severe median-nerve dysfunction, such as that resulting from a longstanding carpal tunnel syndrome. This muscle can be tested by having the patient abduct the thumb while the examiner palpates the muscle.
Thumb adduction is performed by the adductor pollicis (AdP), which is an ulnar-nerve-innervated muscle. This muscle, in combination with the first dorsal interosseus, is necessary for strong pinch. The adductor stabilizes the thumb during pinch and also helps extend the IP joint of the thumb through its attachment into the dorsal apparatus. Thumb adduction can be tested by having the patient forcibly hold a piece of paper between the thumb and the radial side of the proximal phalanx of the index finger. When adduction is weak or nonfunctional, the IP joint of the thumb flexes during this maneuver; this is known as Froment’s sign19 (Fig. 6-12). Froment’s sign is an indication of weak or absent adductor function. Jeanne’s sign is hyperextension of the MCP joint of the thumb during pinch.19
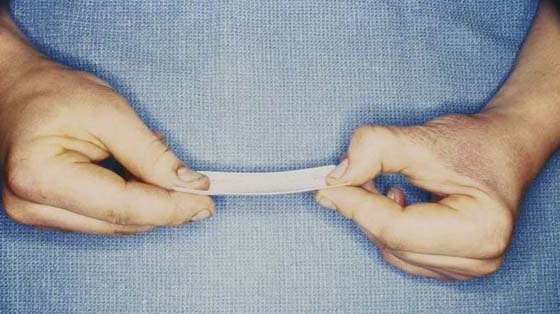
Figure 6-12 Patient with low ulnar nerve palsy on the right. Weakness of pinch is demonstrated by Froment’s and Jeanne’s signs on the affected side (right). (Photo courtesy of Mark Walsh, PT, DPT, MS, CHT, ATC.)
The hypothenar muscles consist of the abductor digiti minimi, the flexor digiti minimi, and the opponens digiti minimi. The abductor and flexor aid in abduction of the fifth digit and in MCP joint flexion of that digit. The deeper opponens digiti minimi aids in adduction and rotation of the fifth metacarpal during opposition of the thumb to the fifth finger. This helps cup the hand during grip and opposition. The hypothenar muscles are tested as one unit by having the patient abduct the little finger while the examiner palpates the muscle mass (Fig. 6-13).
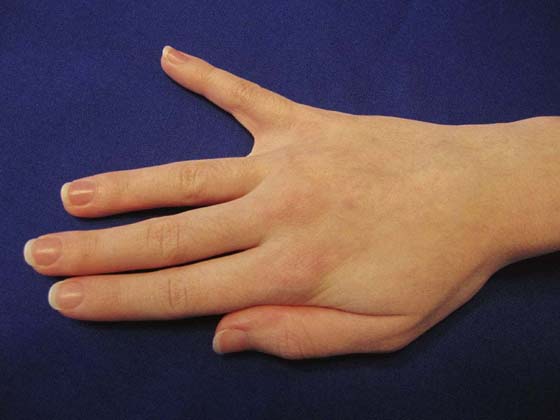
Figure 6-13 Testing function of the hypothenar muscles by having patient abduct the fifth digit.
The anatomy of the interossei is very complex, with much variation in their origins and insertions. There are seven interossei: four dorsal and three palmar. These muscles arise from the metacarpal shafts but have variable insertions. The palmar interossei almost always insert into the dorsal apparatus of the finger. The first dorsal interosseus almost always inserts into bone. The remaining dorsal interossei have varying insertions. Refer to the work of Eyler and Markee for a more detailed description of the anatomy.20 The interossei are usually ulnar nerve innervated, with a few exceptions.
There are four lumbricals, which originate on the radial side of the profundus tendons and usually insert on the dorsal apparatus. Occasionally, a few fibers insert into the base of the proximal phalanges. Because these muscles are a link between the extrinsic flexor and extrinsic extensor mechanisms, they act as a modulator between flexion and extension of the IP joints.21
The interossei are much stronger than the lumbricals; however, both muscle groups work in conjunction. All of these muscle groups are of fundamental importance in extension of the IP joints and flexion of the MCP joints. The interossei also abduct and adduct the fingers. The dorsal interossei are the primary abductors, and the volar interossei are the primary adductors of the fingers.
The preceding statements are an oversimplification of the anatomy and functional significance of the interossei and the lumbricals. The clinical examination of these two groups of muscles is, however, rather easy.
To test interossei function, one should ask the patient to spread his or her fingers apart. This is best done with the hand flat on the examining table to eliminate the action of the long extensors, which can simulate the function of the dorsal interossei (Fig. 6-14). To supplement this test, one can have the patient radially and ulnarly deviate the middle finger while it is flexed at the MCP joint. This cannot be performed if the interossei are paralyzed; this test is known as Egawa’s sign.19
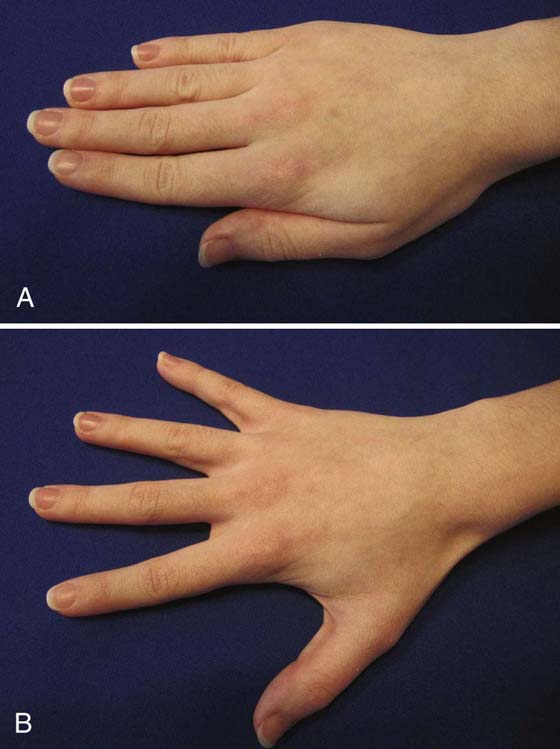
Figure 6-14 Testing function of the interossei. Abduction and adduction are assessed from the relationship of the digits to the axis of the third metacarpal. A, All fingers adducted toward the third metacarpal. B, All fingers abducted away from third metacarpal.
The first dorsal interosseus is a very strong radial abductor of the index finger and plays an important role in stabilizing that digit during pinch. It can be tested separately by having the patient strongly abduct the index finger in a radial direction while the examiner palpates the muscle belly (Fig. 6-15). The IP extension function of the lumbricals and interossei is tested by having the patient extend the IP joints of the digits while the examiner holds the MCP joints in flexion (Fig. 6-16).
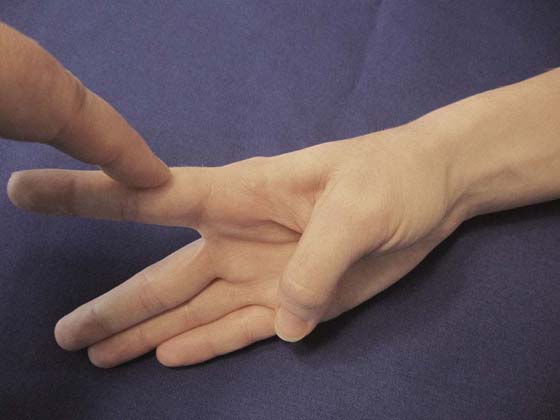
Figure 6-15 On abduction of the patient’s index finger, the examiner can palpate the first dorsal interosseus. This is the last muscle to receive innervation from the ulnar nerve.
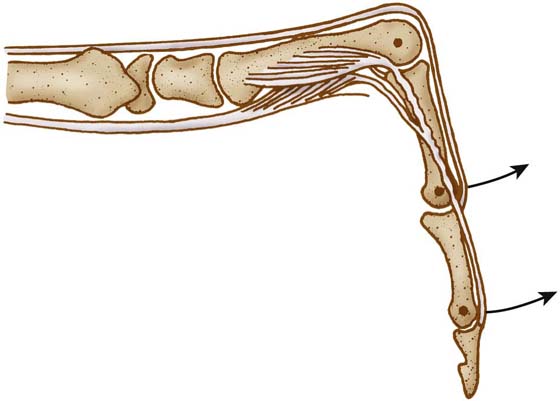
Figure 6-16 The intrinsic muscles, by means of their attachment into the lateral bands and proximal phalanges, produce flexion of the metacarpophalangeal (MCP) joints and extension of the proximal interphalangeal (PIP) joints. The function of the lumbricals and interossei is tested by having the patient extend the PIP joints of the digits while the examiner holds the MCP joints in flexion. (Redrawn from Tubiana R: The Hand. Philadelphia: WB Saunders, 1973.)
If all of the interossei and lumbricals are functioning properly, the patient will be able to put his or her hand into the “intrinsic-plus position”; that is, the MCP joints are flexed and the PIP joints are in full extension. James has recommended this as the position of immobilization for the injured hand to maintain the length of the collateral ligaments of the MCP joint and prevent joint contractures at the IP joints.22
Injuries to the median or ulnar nerves, or both, or a crushing injury to the hand can result in paralysis or contractures of the intrinsic muscles. A hand without intrinsic function is known as the intrinsic-minus hand.23,24 This hand has lost its normal cupping. The arches of the hand disappear, and there is wasting of all intrinsic musculature. Clawing of the fingers is evident, as described by Duchenne in 1867.19 The claw deformity is defined as hyperextension of the MCP joints and flexion of the PIP and DIP joints (Fig. 6-17). This is the result of an imbalance between the intrinsic and extrinsic muscles of the hand.25 The extrinsic extensors hyperextend the MCP joints, and the extrinsic flexors flex the PIP and DIP joints. The flexion vector, induced by the intrinsics, across the MCP joint is lost.26 In time, the volar capsular–ligamentous structures stretch out, and the claw deformity increases in severity.27

Figure 6-17 Intrinsic-minus hand resulting from a longstanding low ulnar palsy. Notice loss of normal arches of the hand and wasting of all intrinsic musculature between metacarpals. Notice hyperextension of the metacarpophalangeal joints and flexion of the proximal and distal interphalangeal joints because of an imbalance of the extrinsic flexor and extensor systems as a result of paralysis of the ulnar innervated intrinsic muscles. (Photo courtesy of Mark Walsh, PT, DPT, MS, CHT, ATC.)
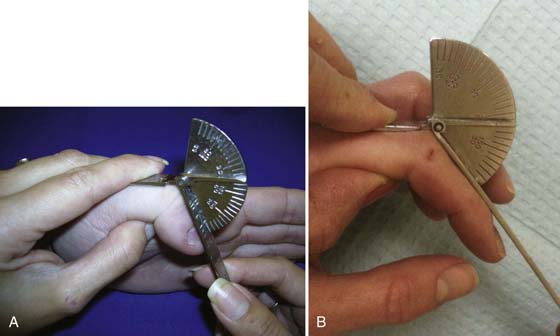
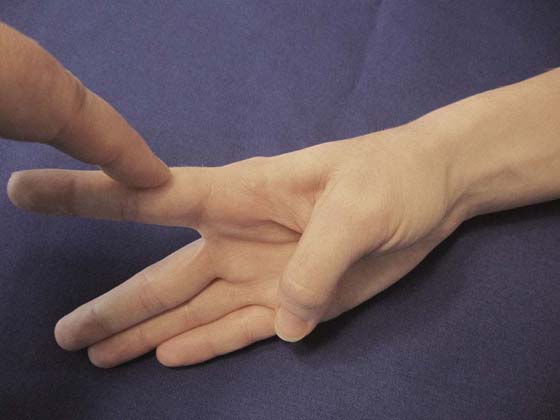
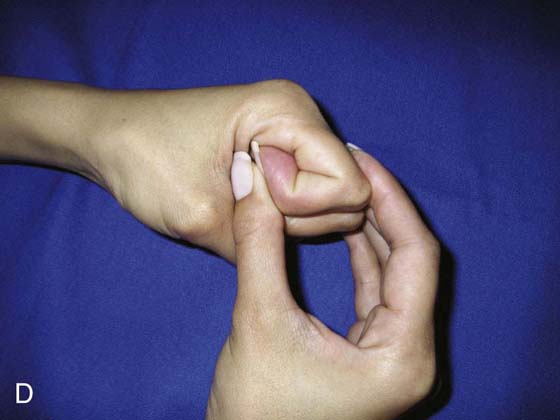
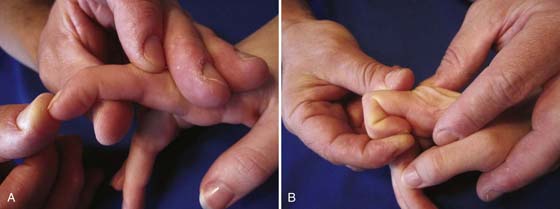
Injury to the intrinsics, which can be caused by ischemia, crushing injuries, or other pathologic states (e.g., rheumatoid arthritis), can result in tightening of the intrinsic muscles. A test for intrinsic tightness was first described by Finochetto in 1920.28 Later, Bunnell and then Littler redescribed this test.29 The intrinsic tightness test is performed by having the examiner hold the patient’s MCP joint in maximum extension (stretching the intrinsics) and then passively flexing the PIP joint. The MCP joint is then held in flexion (relaxing the intrinsics), and the examiner passively flexes the PIP joint again. If the PIP joint can be passively flexed more when the MCP joint is in flexion than when it is in extension, there is tightness of the intrinsic muscles28-30 (Fig. 6-18). In patients with rheumatoid arthritis, intrinsic tightness is common and may result in a swan-neck deformity.31 The swan neck is a result of the strong pull of the contracted intrinsics, through the lateral bands, which subsequently sublux dorsal to the axis of rotation of the PIP joint. The resultant deformity is one of hyperextension at the PIP joint and flexion at the DIP joint.



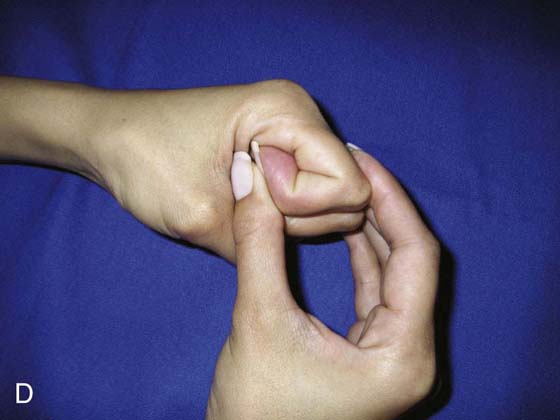
Figure 6-18 Intrinsic tightness test. A, B, The intrinsics are put on stretch by the examiner, who then passively flexes the proximal interphalangeal (PIP) joint. C, D, The intrinsics are then relaxed by flexing the metacarpophalangeal (MCP) joint. If the PIP joint can be passively flexed more with the MCP joint in flexion than when it is in extension, the intrinsic muscles are tight. (Redrawn from Hoppenfeld S: Physical Examination of the Spine and Extremities, New York: Appleton-Century-Crofts, 1976.)
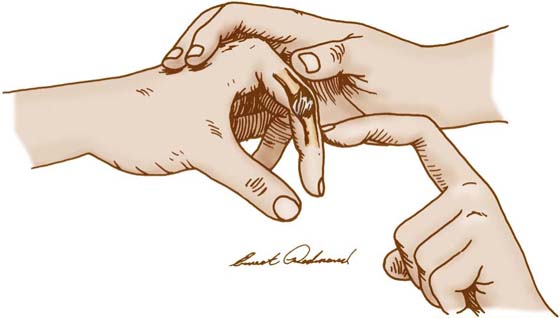
Occasionally, there is confusion as to the cause of limited PIP joint flexion. Is the condition a result of intrinsic tightness, of extrinsic extensor tightness (e.g., scarring of the long extensors proximal to the PIP joint), or of the joint itself (i.e., capsular and collateral ligament tightness)? Three simple tests clarify the situation. The intrinsic tightness test helps the examiner either rule out or identify intrinsic muscle problems. The extrinsic tightness test is just the opposite of the intrinsic test. Again, the examiner holds the MCP joint in maximum extension, passively flexes the PIP joint, and notes the amount of flexion. He or she then flexes the MCP joint and passively flexes the PIP joint again. If extrinsic extensor tightness (because the long extensors are scarred) is present, passive flexion of the PIP joint will be greater when the MCP joint is held in extension than when it is held in flexion. If the motion of the PIP joint is unchanged regardless of the position of the MCP joint, then the limitation is attributed to PIP joint capsular and collateral ligament tightness (Fig. 6-19).
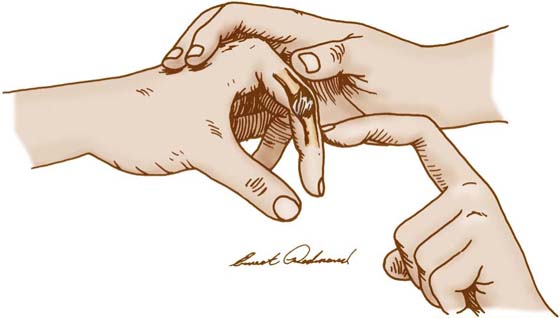
Figure 6-19 Proximal interphalangeal joint (PIP) contracture. Collateral ligament tightness limits PIP motion, regardless of the position of the metacarpophalangeal joint.
Oblique Retinacular Ligament Test
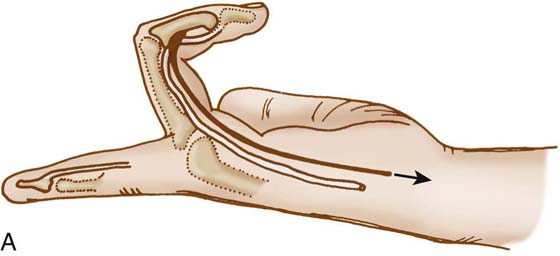
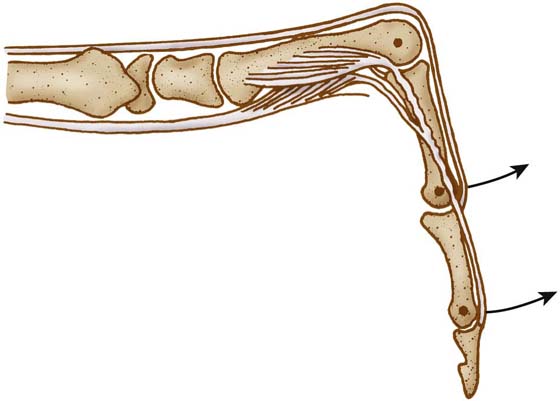
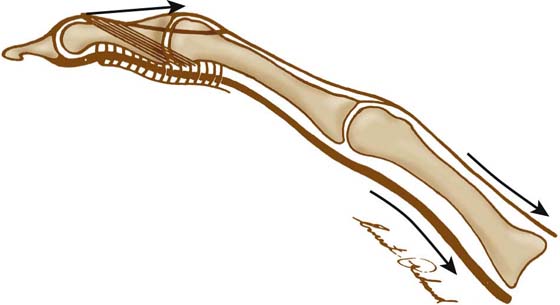
Occasionally, a patient exhibits a lack of active flexion at the DIP joint. This may be caused by a joint contracture or a contracture of the oblique retinacular ligament.32 The oblique retinacular ligament arises from the volar lateral ridge of the proximal phalanx and has a common origin with the distal A2 and C1 pulleys. It then traverses distally and dorsally to attach to the dorsal apparatus near the DIP joint (Fig. 6-20). As pointed out by Shrewsbury and Johnson, the tendon varies in its development and occurrence.33 However, it is consistently made taut by flexion of the DIP joint, particularly with the PIP joint in extension. If this ligament is contracted, DIP motion will be limited. The oblique retinacular ligament tightness test is performed by passively flexing the DIP joint with the PIP joint in extension and then repeating this with the PIP joint in flexion. If there is greater motion when the PIP joint is flexed than when it is extended, there is tightness of the ligament (Fig. 6-21). Equal loss of flexion indicates a joint contracture.
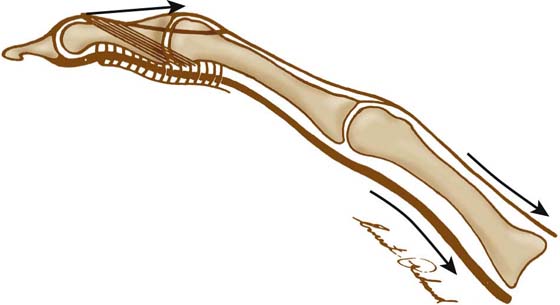
Figure 6-20 Oblique retinacular ligament. (Redrawn from Tubiana R: The Hand, Philadelphia: WB Saunders, 1981.)
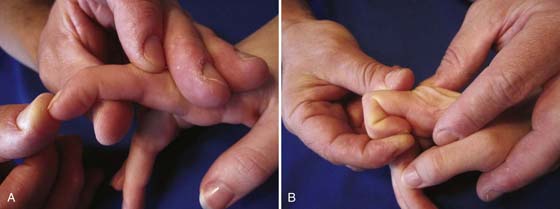
Figure 6-21 The oblique retinacular ligament tightness test. A, The distal interphalangeal (DIP) joint is passively flexed with the proximal interphalangeal (PIP) joint held in extension. B, The DIP joint is then passively flexed with the PIP joint flexed. If there is greater motion when the PIP joint is flexed than when it is extended, there is tightness of the ligament. Equal loss of DIP joint motion regardless of PIP joint position indicates a joint contracture.
Grip and Pinch Strength
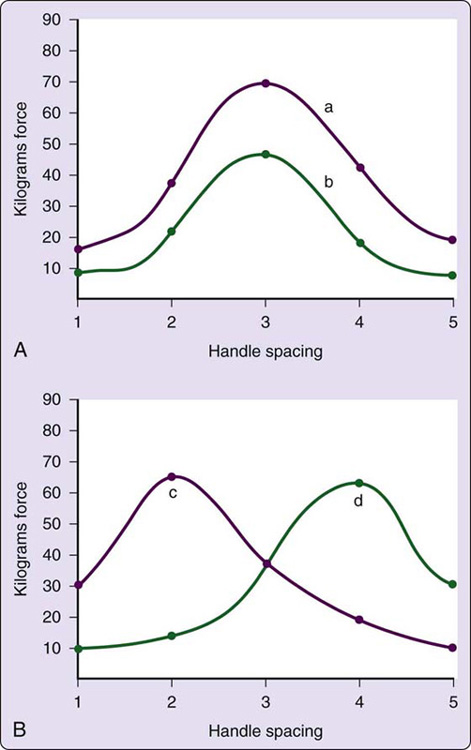
The next step after examination of intrinsic and extrinsic musculature of the hand is determination of gross grip and pinch strength of the injured versus the noninjured hand. Several devices for objective measurement of grip strength are commercially available. The grip dynamometer (see Fig. 12-4) with adjustable handle spacings provides an accurate evaluation of the force of grip.34 This dynamometer has five adjustable spacings at 1.0, 1.5, 2.0, 2.5, and 3.0 inches. The patient is shown how to grasp the dynamometer and is instructed to grasp it with his maximum force. The grip test position should be standardized. The forearm should be in neutral rotation and the elbow flexed 90 degrees. The shoulder should be adducted. The patient self-selects a wrist position with the gripping motion. O’Driscoll states that optimal grip strengths are achieved at 35 degrees of wrist extension.35 Grip strength is measured at each of the five handle positions. The right and left hands are tested alternately, and the force of each grip effort is recorded. The test is paced at a rate to eliminate fatigue. If only one level is measured, an average of three trials is recommended for each hand.11 According to Bechtol, there is usually a 5% to 10% difference between the dominant hand and the nondominant hand in normal subjects.34 A graph of the grip measurements at the five handle positions forms a bell curve if the patient provides maximal effort and has not sustained a median or ulnar nerve injury; grip strength is typically greatest at the middle handle position and weakest at each end resulting from the differential action of extrinsic and intrinsic muscles involved with grip at each handle position. At the widest handle position, extrinsic finger flexor muscle action is predominantly involved; at the most narrow handle position, intrinsic muscle action predominates. At the middle spacings there is a combination of both intrinsic and extrinsic muscle action, resulting in greater strength output and thus, the bell curve configuration of grip readings at all five handle positions. With generalized weakness of the hand, the bell curve pattern is usually still present (Fig. 6-22). However, patients with an intrinsic-minus hand are an exception to this rule. Their curve is flattened as their grip increases from level I to V because the extrinsic flexors are at a better mechanical advantage with the wider handle positions.36 Other patients that may present with a “flattened” curve may be using submaximal effort;34 however, it may be proportional to the amount of forced produced.37,38
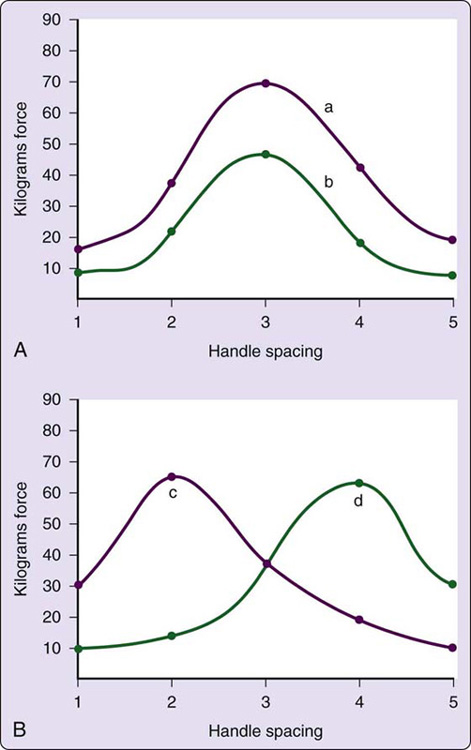
Figure 6-22 A, The grip strengths of a patient’s uninjured hand (a) and injured hand (b) are plotted. Despite the patient’s decrease in grip strength because of injury, curve b maintains a bell-shaped pattern and parallels that of the normal hand. These curves are reproducible in repeated examinations, with minimal change in values. B, If the patient has an exceptionally large hand, the curve will shift to the right (d); with a very small hand, the curve shifts to the left (c). Notice, however, that the bell-shaped pattern is maintained despite the curve’s shift in direction.
For years, the rapid exchange grip (REG) test has been used to detect submaximal effort. The REG test is administered with a dynamometer at the setting that achieves maximum grip during static testing. During testing, the clinician holds the dynamometer in place. The patient is then instructed to maximally grip the dynamometer, alternating hands as rapidly as possible. Each hand grips the dynamometer 5 to 10 times. A positive REG test shows a significant increase in grip strength on the affected side compared with static scores. A positive REG test in the presence of a flat curve on static testing suggests inconsistent effort by the patient.39,40 A more recent study has concluded that the REG is not a reliable or valid way to detect submaximal effort due to a lack of standardization in the procedures.40
There are three basic types of pinch: (1) chuck, or three-fingered pinch; (2) lateral, or key pinch; and (3) tip pinch (Fig. 6-23). These can be tested with a pinch meter (see Fig. 12-6). Many disease processes can affect pinch power: basilar arthritis of the thumb, ulnar nerve palsy, and anterior interosseus nerve palsy, to mention a few.

Figure 6-23 A, Chuck, or three point, pinch. B, Lateral, or key, pinch. C, Tip pinch.
Additional information on grip and pinch functional strength measures is presented in Chapter 12 on functional tests.
Nerve Supply of the Hand—Motor and Sensory
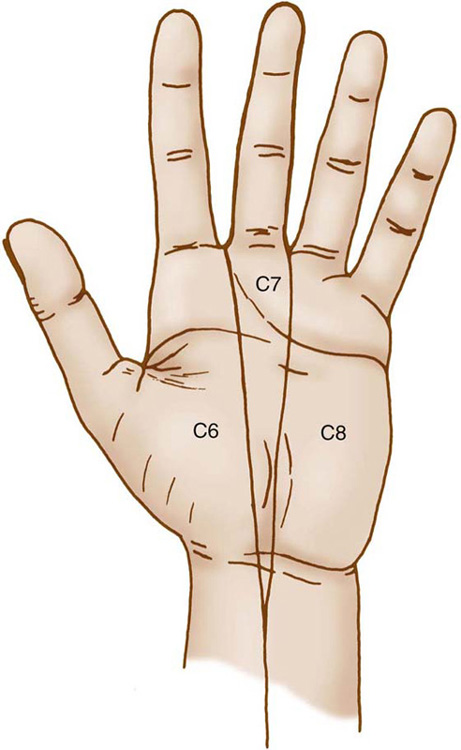
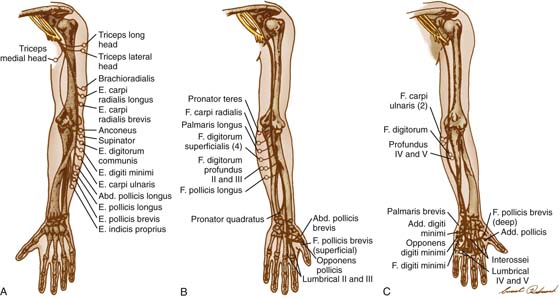
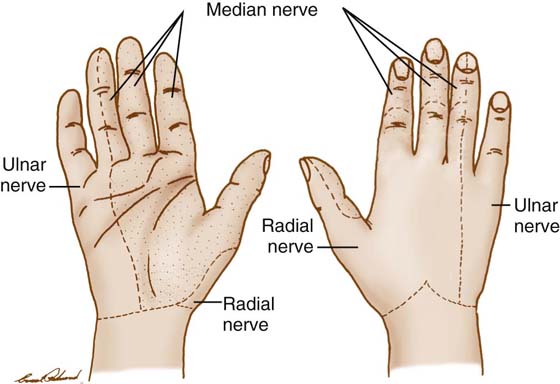
Three nerves provide motor and sensory function to the hand: the median, radial, and ulnar nerves. The motor and sensory innervation of the hand also is subject to much variation, as pointed out by Rowntree.41 The median, radial, and ulnar nerves are peripheral branches of the brachial plexus. The radial nerve is formed from the C6 and C7 nerve roots. The median and ulnar nerves are formed by branches of the C7, C8, and T1 nerve roots. The neurologic levels represented by the sensory dermatomes are illustrated in Figure 6-24. The terminal branches of the median, radial, and ulnar nerves are shown in Figure 6-25. It is necessary to have a fundamental knowledge of the branches and their sequence of innervation to appropriately pinpoint the level of an injury or to follow the path of a regenerating nerve.
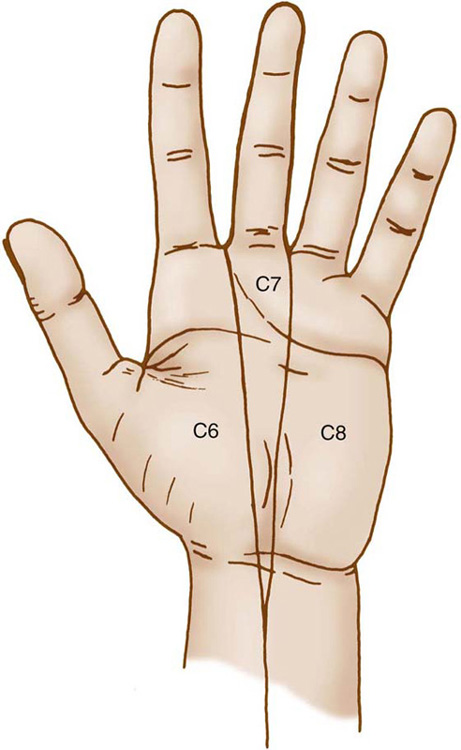
Figure 6-24 Sensory dermatomes of the hand, by neurologic levels. (Redrawn from Hoppenfeld S: Physical Examination of the Spine and Extremities. New York: Appleton-Century-Crofts, 1976.)
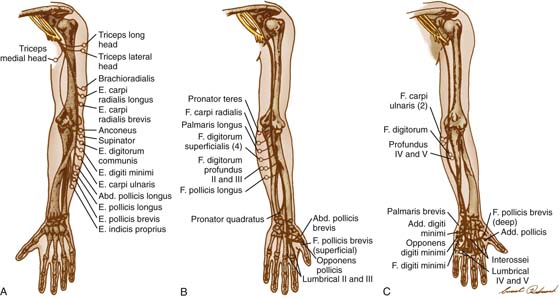
Figure 6-25 Terminal branches of the radial (A), median (B), and ulnar (C) nerves. (Redrawn from American Society for Surgery of the Hand: The Hand, Examination and Diagnosis, Aurora, Colo.: The Society, 1978.)
The median, radial, and ulnar nerves enter the forearm through various muscle and fascial planes and have multiple potential sources of entrapment. These nerve conditions may be associated with traumatic injuries such as fractures of the elbow, forearm, or wrist. Entrapment of these nerves results in classic clinical presentations, with loss of motor function (in longstanding compression) and paresthesias in the distribution of each nerve.42-46 Careful and systematic examination of cutaneous sensibility and motor function is required to determine the extent of the compression. The examination and management of these compression syndromes are discussed elsewhere in this book.
Cutaneous Sensibility
Normal sensibility is a prerequisite to normal hand function. A patient with a median nerve injury has essentially a “blind hand” and is greatly disabled, even if all motor function is present. The assessment of sensibility is therefore an integral and important part of the examination of the hand. The distribution of sensory nerves is subject to as much variation as the distribution of the motor branches.41 The classic distribution of the median, ulnar, and radial nerves is shown in Figure 6-26.
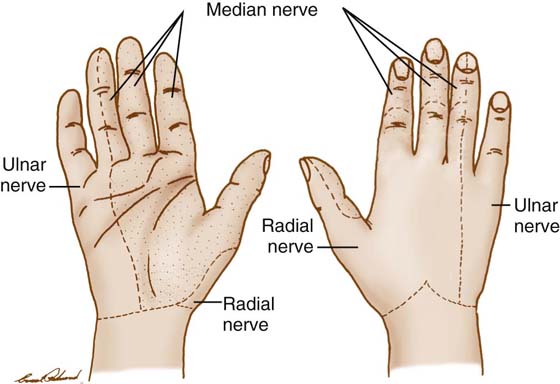
Figure 6-26 Sensory distribution of the median, radial, and ulnar nerves in the hand. (Redrawn from Weeks PM, Wray RC: Management of Acute Hand Injuries: A Biological Approach, St Louis: Mosby, 1973.)
There are many ways to assess sensibility, including monofilaments, Moberg’s Picking-up Test, Seddon’s coin test, the moving two-point discrimination test described by Dellon, and Weber’s two-point discrimination test.49-51 Chapter 11 in this edition of the book and Chapter 14 from the fifth edition (located in the archived chapters section on the companion Web site) discuss sensibility testing in detail.
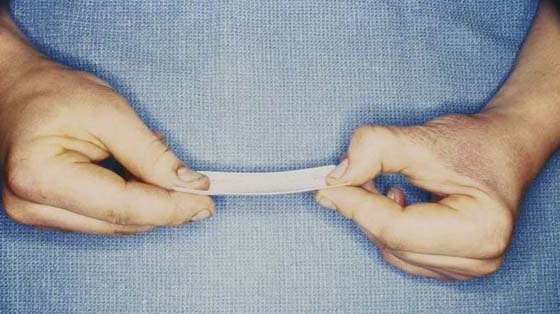
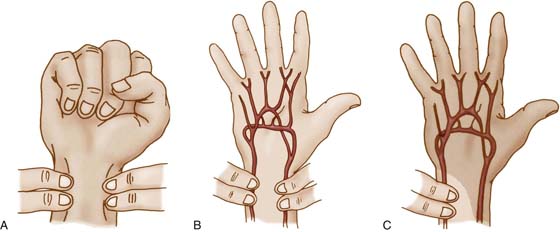
Vascularity of the Hand
The vascular supply of the hand is usually extensive; however, it should be examined carefully before any surgery on the hand. The primary blood supply to the hand is through the radial and ulnar arteries. In some individuals, the dominant blood supply to the hand can be from one artery. The ulnar artery gives rise to the superficial palmar arch, and the radial artery gives rise to the deep arch. These arches usually have extensive anastomoses.52,53 The superficial palmar arch gives rise to four common digital arteries, which then branch to form the proper digital arteries. The superficial arch may supply blood to the thumb, or the thumb may be completely vascularized by a branch of the radial artery known as the princeps pollicis artery. To assess blood supply to the hand, one should check the color of the hand (red, pale, or cyanotic), digital capillary refill, the radial artery and ulnar artery pulses at the wrist, and perform Allen’s test. In 1929, Allen described a simple clinical test to determine the patency of the radial and ulnar arteries in thromboangiitis obliterans.54 This test is performed by having the patient open and close his or her hand to exsanguinate it while the examiner occludes the radial and ulnar arteries at the wrist with digital pressure. The patient then opens the hand, which is white and blanched. The examiner then releases either the ulnar or the radial artery and watches for revascularization of the hand. If the hand does not flush, the artery is occluded. This test is then repeated with the opposite artery (Fig. 6-27).
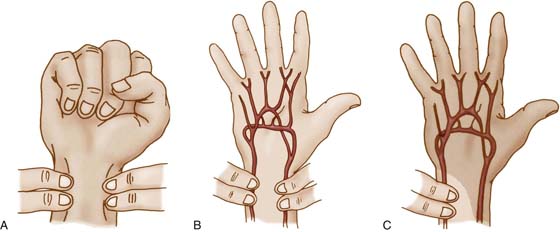
Figure 6-27 Allen’s test for arterial patency. A, The examiner places her fingers over the ulnar and radial arteries at the wrist. B, The patient then forcibly opens and closes his hand to exsanguinate it while the examiner occludes the radial and ulnar arteries. C, Next the patient opens his hand, and the examiner releases one artery and observes the flushing of the hand. The steps are then repeated, and the other artery is tested for patency. (Redrawn from American Society for Surgery of the Hand: The Hand, Examination and Diagnosis, Aurora, Colo.: The Society, 1978.)
A modification of Allen’s test can be performed on a single digit.55 The steps are the same as just outlined, except that the examiner occludes and releases the radial and ulnar digital arteries.
Medical Screening and Review of Systems
Direct access is the right of the public to obtain physical therapy services without a legal need for referral. It is now available in 45 states within the United States.56 This legislation occurring in the past decade prompted the need to teach medical screening to professional physical therapy students. It became apparent that medical screening was needed by both physical and occupational therapists even without direct access because any patient may present with risk factors, precautions, or “red flags” to therapeutic interventions.
Current practice trends suggest that patients are discharged more quickly from the hospital and more likely to have outpatient same-day surgery. This means that patients are not monitored as closely as they used to be. If the patient is referred to therapy postoperatively, he or she may present with more medical issues or complications. The public is generally sicker, with almost 80% of patients over 70 years of age having at least one chronic disease.2 Therapists need to identify these comorbidities. Patients are being referred to hand therapy clinics with a signed prescription, without an adequate medical screening, because they never saw the physician or ancillary medical personnel, and sometimes when they do see the doctor, they are not examined. Finally, knowledge related to screening for risk factors has increased significantly over the past decade for several medical conditions and diseases. For example, screening criteria have been developed for female patients with low bone mass (osteoporosis) that present in the clinic with an upper extremity fracture due to a fall. Screening tests for risk factors and balance following a wrist fracture have been developed so that therapists can serve as “gatekeepers” to address falls risk, balance impairments, or low bone mass.
Goodman created a five-step model for medical screening2 that includes: (1) personal and family history; (2) risk factor assessment, (3) clinical presentation, (4) associated signs and symptoms of systemic diseases, and (5) review of systems. Box 6-1 presents selected examples for review of systems pertaining to upper extremity patients.
Box 6-1 Review of Systems (Selected Examples)
GENERAL QUESTIONS
Fever, chills, sweating (constitutional symptoms)
Fatigue, malaise, weakness (constitutional symptoms)
Vital signs: blood pressure, temperature, pulse, respirations
Dizziness, falls
INTEGUMENTARY (INCLUDE SKIN, HAIR, AND NAILS)
Recent rashes, nodules, or other skin changes
Increased hair growth (hirsutism)
Nail bed changes
MUSCULOSKELETAL AND NEUROLOGIC
Frequent or severe headaches
Paresthesias (numbness, tingling, “pins and needles” sensation)
Weakness; atrophy
Problems with coordination or balance; falling
Involuntary movements; tremors
Radicular pain
RHEUMATOLOGIC
Presence and location of joint swelling
Muscle pain, weakness
Skin rashes
Raynaud’s phenomenon
CARDIOVASCULAR
Chest pain or sense of heaviness of discomfort
Limb pain during activity (claudication; cramps, limping)
Pulsating or throbbing pain anywhere, but especially in the back or abdomen
Peripheral edema; nocturia
Fatigue, dyspnea, orthopnea, syncope
High or low blood pressure, unusual pulses
PULMONARY
Shortness of breath (dyspnea, orthopnea)
Night sweats; sweats anytime
Pleural pain
PSYCHOLOGICAL
Stress levels
Fatigue, psychomotor agitation
Depression, confusion, anxiety
Irritability, mood changes
GASTROINTESTINAL
Abdominal pain
Diarrhea or constipation
Skin rash followed by joint pain (Crohn’s disease)
HEPATIC AND BILIARY
Feeling of abdominal fullness, ascites
Changes in skin color (yellow, green)
Skin changes (rash, itching, purpura, spider angiomas, palmar erythema)
HEMATOLOGIC
Skin color or nail bed changes
Bleeding: nose, gums, easy bruising, melena
Hemarthrosis, muscle hemorrhage, hematoma
GENITOURINARY
Reduced stream, decreased output
Burning or bleeding during urination; change in urine color
Urinary incontinence, dribbling
GYNECOLOGIC
Pain with menses or intercourse
Surgical procedures
Pregnancy, birth, miscarriage, and abortion histories
ENDOCRINE
Fruity breath odor
Headaches
Carpal or tarsal tunnel syndrome
Periarthritis, adhesive capsulitis
CANCER
Constant, intense pain, especially bone pain at night
Excessive fatigue
Rapid onset of digital clubbing (10–14 days)
IMMUNOLOGIC
Skin or nail bed changes
Fever or other constitutional symptoms
Lymph node changes
Summary
Clinical examination is an art that improves with practice and experience. This chapter presents a systematic approach to clinical examination of the hand. Hand surgeons and therapists need to use valid and reliable tests and measures to collect impairment data to assess treatment outcomes. Diagnostic special tests used in clinical examination must be evaluated for their diagnostic accuracy and interpretation of results.57 Research is needed to determine the sensitivity, specificity, and likelihood ratios of diagnostic tests used in hand and upper extremity clinical examinations.
REFERENCES
1. Steenhuis RE, Bryden MP, Schwartz M, et al. Reliability of hand preference items and factors. J Clin Exp Neuropsychol. 1990; 12 (6):921–930.
2. Goodman CC. Screening for medical problems in patients with upper extremity signs and symptoms. J Hand Ther. 2010; 23: 105–125.
3. Dereberry VJ, Howard LL. Management of the painful arm: cumulative trauma revisited. Physical Medicine and Rehabilitation: State of the Art Reviews. Vol. 12. No. 2, June 1998. Philadelphia, Hanley & Belfus, Inc. pp. 215-224.
4. Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder, and hand). Am J Ind Med. 1996; 29: 602–608.
5. Levine DW, Simmons BP, Koris MJ, et al. A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J Bone Joint Surg Am. 1993; 75: 1585–1592.
6. Chung KC, Pillsbury MS, Walters MR, Hayward RA. Reliability and validity testing of the Michigan hand outcomes questionnaire. J Hand Surg. 1998; 23A: 575–587.
7. Amadio PC. Outcome assessment in hand surgery and hand therapy: an update. J Hand Ther. 2001; 14: 63–67.
8. Beattie P. Measurement of health outcomes in the clinical setting: applications to physiotherapy. Physiother Theory Pract. 2001; 17: 173–185.
9. Noer HR, Pratt D. A goniometer designed for the hand. J Bone Joint Surg. 1958; 40A: 1154–1156.
10. Marx RG, Bombardier C, Wright J. What do we know about the reliability and validity of physical examination tests used to examine the upper extremity? J Hand Surg. 1999; 24A: 185–193.
11. American Society of Hand Therapists. A., American Society of Hand Therapists Clinical Assessment Recommendations. Chicago: The Society; 1992.
12. Norkin CC, White JD. Measurement of Joint Motion: A Guide to Goniometry. 4th ed Philadelphia: FA Davis; 2009.
13. Reese NB, Bandy WD. Joint Range of Motion and Muscle Length Testing. 2nd ed St. Louis: Saunders; 2010.
14. Baker D, Gaul JS, Williams VK, Graves M. The little finger superficialis: clinical investigation of its anatomical and functional shortcomings. J Hand Surg. 1981; 6: 374–378.
15. Finkelstein H. Stenosing tenovaginitis at the radial styloid process. J Bone Joint Surg. 1930; 12: 509–540.
16. McFarlane R. Observations on the functional anatomy of the intrinsic muscles of the thumb. J Bone Joint Surg. 1962; 44A: 1073–1088.
17. Bunnell S. Opposition of the thumb. J Bone Joint Surg. 1938; 20: 269–284.
18. Mannerfelt L. Studies on the hand in ulnar nerve paralysis: a clinical-experimental investigation in normal and anomalous innervation. Acta Orthop Scand. 1966; 87 (Suppl):1.
19. Eyler D, Markee J. The anatomy and function of the intrinsic musculature of the fingers. J Bone Joint Surg. 1954; 36A: 1–9.
20. Mehta H, Gardner W. A study of lumbrical muscles in the human hand. Am J Anat. 1961; 109: 227–238.
21. James JIP. The assessment and management of the injured hand. Hand. 1970; 2: 97–105.
22. Bunnell S. Surgery of the intrinsic muscles of the hand other than those producing opposition of the thumb. J Bone Joint Surg. 1942; 24: 1–31.
23. Harris C, Riordan D. Intrinsic contracture in the hand and its surgical treatment. J Bone Joint Surg. 1954; 36A: 10–20.
24. Srinivasan H. Clinical features of paralytic claw fingers. J Bone Joint Surg. 1979; 61A: 1060–1063.
25. Mick J, Reswick J, Hager DL. The mechanism of the intrinsic-minus finger: a biomechanical study. J Hand Surg. 1978; 3: 333–341.
26. Mulder J, Landsmeer J. The mechanism of the claw finger. J Bone Joint Surg. 1968; 50B: 664–668.
27. Zancolli E. Structural and Dynamic Basis of Hand Surgery. Philadelphia: JB Lippincott; 1968.
28. Bunnell S. Ischaemic contracture, local, in the hand. J Bone Joint Surg. 1953; 35A: 88–101.
29. Smith R. Non-ischemic contractures of the intrinsic muscles of the hand. J Bone Joint Surg. 1971; 53A: 1313–1331.
30. Nalebuff E, Millender L. Surgical treatment of the swan-neck deformity in rheumatoid arthritis. Orthop Clin North Am. 1975; 6: 733–752.
31. Landsmeer JMF. The anatomy of the dorsal aponeurosis of the human finger and its functional significance. Anat Rec. 1949; 104: 31–44.
32. Shrewsbury M, Johnson R. A systematic study of the oblique retinacular ligament of the human finger: its structure and function. J Hand Surg. 1977; 2: 194–199.
33. Bechtol C. Grip test: the use of a dynamometer with adjustable handle spacings. J Bone Joint Surg. 1954; 36A: 820–824.
34. O’Driscoll SW, Horii E, Ness R, et al. The relationship between wrist position, grasp size, and grip strength. J Hand Surg. 1992; 17A: 169–177.
35. Kozin SH, Porter S, Clark P, Thoder JJ. The contribution of the intrinsic muscles to grip and pinch strength. J Hand Surg. 1999; 24A: 64–72.
36. Gutierrez Z, Shechtman O. Effectiveness of the five-handle position grip strength test in detecting sincerity of effort in men and women. Am J Phys Med Rehabil. 2003; 82: 847–855.
37. Shechtman O, Gutierrez Z, Kokendofer E. Analysis of the statistical methods used to detect submaximal effort with the five-rung grip strength test. J Hand Ther. 2005; 18: 10–18.
38. Hildreth D, Breidenbach WC, Lister GD, Hodges AD. Detection of submaximal effort by use of the rapid exchange grip test. J Hand Surg. 1989; 14A: 742–745.
39. Stokes H, Landrieu KW, Domangue B, Kunen S. Identification of low-effort patients through dynamometer. J Hand Surg. 1995; 20A: 1047–1056.
40. Shechtman O, Goodall SK. The administration and interpretation of the rapid exchange grip test: a national survey. J Hand Ther. 2008; 21: 18–26.
41. Rowntree T. Anomalous innervation of the hand muscles. J Bone Joint Surg. 1949; 31B: 505–510.
42. Hartz C, Linscheid RL, Gramse RR, Daube JR. The pronator teres syndrome: compressive neuropathy of the median nerve. J Bone Joint Surg. 1981; 63A: 885–890.
43. Spinner M. The anterior interosseous nerve syndrome with special attention to its variations. J Bone Joint Surg. 1970; 52A: 84–94.
44. Shea J, McClain E. Ulnar nerve compression syndromes at and below the wrist. J Bone Joint Surg. 1969; 51A: 1095–1103.
45. Roles N, Maudsley R. Radial tunnel syndrome: resistant tennis elbow as a nerve entrapment. J Bone Joint Surg. 1972; 54B: 499–508.
46. Phalen G. The carpal tunnel syndrome: seventeen years’ experience in diagnosis and treatment of 654 hands. J Bone Joint Surg. 1966; 48A: 211–228.
47. Bowden R, Napier J. The assessment of hand function after peripheral nerve injuries. J Bone Joint Surg. 1961; 43B: 481–492.
48. Dellon A. The moving two-point discrimination test: clinical evaluation of the quickly adapting fiber-receptor system. J Hand Surg. 1978; 3: 474–481.
49. Levin S, Pearsall G, Ruderman R. Von Frey’s method of measuring pressure sensibility in the hand: an engineering analysis of the Weinstein-Semmes pressure aesthesiometer. J Hand Surg. 1978; 3: 211–216.
50. Moberg E. Objective methods for determining the functional value of sensibility in the hand. J Bone Joint Surg. 1958; 40B: 454–476.
51. Seddon HJ. “Coin test” for cutaneous sensibility. Br Med J. 1966; 1: 1599.
52. Coleman S, Anson B. Arterial patterns in the hand based upon a study of 650 specimens. Surg Gynecol Obstet. 1961; 113: 408–424.
53. Markee J, Wray J. Circulation of the hand: injection-corrosion studies. J Bone Joint Surg. 1959; 41A: 673–680.
54. Allen E. Thromboangiitis obliterans: methods of diagnosis of chronic occlusive arterial lesions distal to the wrist with illustrative cases. Am J Med Sci. 1929; 178: 237–243.
55. Ashbell T, Kutz J, Kleinert H. The digital Allen test. Plast Reconstr Surg. 1967; 39: 311–312.
56. American Physical Therapy Association. Map of Direct Access States. Available at www.apta.org. Accessed March 12, 2010
57. Fritz JM, Wainner RS. Examining diagnostic tests: an evidence-based perspective. Physical Therapy. 2001; 81: 1546–1564.