Family-Centered Care of the Child During Illness and Hospitalization
What Is Family Centered Care?,
Stressors of Hospitalization and Children’s Reactions
Stressors and Reactions of the Family of the Child Who Is Hospitalized
Nursing Care of the Child Who Is Hospitalized
Preventing or Minimizing Separation
Minimizing Loss of Control and Autonomy
Preventing or Minimizing Fear of Bodily Injury
Providing Developmentally Appropriate Activities
Using Play and Expressive Activities to Minimize Stress
http://evolve.elsevier.com/wong/ncic
Administration of Medication, Ch. 27
Communication and Physical and Developmental Assessment of the Child, Ch. 6
Compliance, Ch. 27
Family-Centered Care of the Child with Chronic Illness or Disability, Ch. 22
Family-Centered End-of-Life Care, Ch. 23
Family-Centered Home Care, Ch. 25
Neonatal Pain, Ch. 7
Nursing Care of the Surgical Neonate, Ch. 11
Preparation for Diagnostic and Therapeutic Procedures, Ch. 27
Social, Cultural, and Religious Influences on Child Health Promotion, Ch. 2
Surgical Procedures, Ch. 27
What is Family-Centered Care?
The theory of family-centered care began to materialize in health care in the late 1960s, as physicians realized the necessity of meeting patient’s psychosocial and developmental needs, as well as including families in care. Now the American Academy of Pediatrics (2003) defines family-centered care as “an approach to health care that shapes health care policies, programs, facility design, and day-to-day interactions among patients, families, physicians, and other health care professionals.” Proponents of family-centered care believe that collaboration must exist between patients, family members, physicians, nurses, and all members of the health care team in order to reach desired outcomes for the patient. In addition, the Institute for Family-Centered Care acknowledges that families are “essential to patients’ health and well-being and are allies for quality and safety within the health care system” (Conway, Johnson, Edgman-Levitan, et al, 2006). The family-centered care movement gained further momentum due to a report from the Institute of Medicine (2001) titled “Crossing the Quality Chasm: A New Health System for the 21st Century,” which calls for changes in the health care environment to improve patient safety and quality of care. In this report, the Institute of Medicine called for increased involvement of patients in their own health care decisions, better communication to patients regarding treatment options, and care that is respectful of patient preferences and values.
Nursing professionals should engage patients and families in the care planning and decision-making process. Inherent in nursing philosophy is the idea that nurses nurture patients and form a partnership with parents or families. This collaboration leads to nurses and parents working together to treat the child holistically, thus meeting all of his or her needs. As a partner in care, nurses are challenged to incorporate family and child preferences to decrease stress, minimize the negative effects of hospitalization, maximize the benefits of hospitalization, ensure adequate discharge planning and preparation, and provide overall comfort and support.
Stressors of Hospitalization and Children’s Reactions
Often illness and hospitalization are the first crises children must face. Especially during the early years, children are particularly vulnerable to the crises of illness and hospitalization because (1) stress represents a change from the usual state of health and environmental routine and (2) children have a limited number of coping mechanisms to resolve stressors. Major stressors of hospitalization include separation from parents and loved ones; fear of the unknown; loss of control and autonomy; bodily injury resulting in discomfort, pain, and mutilation; and the fear of death. Children’s developmental age; previous experience with illness, separation, or hospitalization; their innate and acquired coping skills; the seriousness of the diagnosis; and the support system available influence their reaction to these crises.
Separation Anxiety
The major stress from middle infancy throughout the preschool years, especially for children ages 16 to 30 months, is separation anxiety, also called anaclitic depression. Box 26-1 summarizes the principal behavioral responses of these children to the three phases of separation anxiety.
During the phase of protest, children react aggressively to separation from the parent. They cry and scream for their parents, refuse the attention of anyone else, and are inconsolable in their grief (Fig. 26-1). They may continue this behavior for a few hours to several days. Some children may protest continuously, ceasing only from physical exhaustion. If a stranger approaches them, children initially protest even louder. During the phase of despair, the crying stops and depression is evident. The child is much less active, is uninterested in play or food, and withdraws from others. The child looks sad, lonely, isolated, and apathetic (Fig. 26-2).

Fig. 26-1 In the protest phase of separation anxiety, children cry loudly and are inconsolable in their grief for the parent. (Courtesy James DeLeon, Texas Children’s Hospital, Houston.)
Fig. 26-2 During the despair phase of separation anxiety, children are sad, lonely, and uninterested in play or food.
During the third phase, detachment, or denial, the child appears to have finally adjusted to the loss. The child becomes more interested in the surroundings, plays with others, and seems to form new relationships. In this phase, care givers and health care professionals often think the child has adjusted to hospitalization. However, this behavior is a result of resignation and is not a sign of contentment. The child detaches from the parent in an effort to escape the emotional pain of desiring the parent’s presence. The child copes by forming shallow relationships with others, becoming increasingly self-centered, and attaching primary importance to material objects. This is the most serious phase because reversal of the potential adverse effects is less likely to occur once detachment is established. However, if separations imposed by hospitalization are temporary, they do not cause prolonged parental absences that lead to detachment. In addition, considerable evidence suggests that, even with stresses such as separation, permanent ill effects are rare.
Although progression to detachment is uncommon, the initial phases of separation anxiety are frequently observed even with brief separations from either parent. Without understanding the meaning of each stage of behavior, health team members may erroneously label the behaviors as positive or negative. In the phase of protest, they may view the loud crying as “bad” behavior. Because the protesting increases if a stranger approaches, staff may interpret the reaction as evidence of their need to stay away. During the quiet, withdrawn phase of despair, they regard the child as finally “settling in” to the new surroundings and see the detachment behaviors as proof of a “good adjustment.” The faster a child reaches this stage, the more likely it is that health care providers will regard the child as the ideal patient.
If parents cannot remain with their child throughout the hospitalization, children may exhibit a variety of responses to parental presence or visitation. During the protest phase, children do not outwardly appear happy to see their parents and may even cry louder than they did before the visit began. Depressed children may protest when parents visit or completely reject their parents’ company. Other children may cling to their parents to force their continued presence. In the phase of detachment, children respond no differently to their parents than to any other person. Due to these negative responses and reactions, uninformed observers may think that parental visitation is disturbing the child’s adjustment and feel justified in restricting visitation.
Seeing these reactions to hospitalization is distressing to parents, who may be unaware of their meaning. Because of their child’s behaviors, parents may see their absence as beneficial to the child’s adjustment and recovery. They may respond to the child’s behavior by staying for short periods, decreasing the frequency of visits, or deceiving the child when it is time to leave. The result is a destructive cycle of misunderstanding and unmet needs.
Early Childhood
Separation anxiety is the greatest stress imposed by hospitalization during early childhood. If separation is avoided or decreased, young children have a tremendous capacity to withstand any other stress. In this age-group, the typical reactions just described are seen. However, children in the toddler stage demonstrate more goal-directed behaviors. For example, they may verbally plead for their parents to stay and physically attempt to secure or find them. They may demonstrate displeasure on the parents’ return or departure by having temper tantrums; refusing to comply with the usual routines of mealtime, bedtime, or toileting; or regressing to more primitive levels of development. Temper tantrums, bed-wetting, or other behaviors may also be explained as expressions of anger or can be a physiologic response to stress.
Because preschoolers are much more secure interpersonally than toddlers, they can tolerate brief periods of separation from their parents and are more inclined to develop substitute trust in other significant adults. The stress of illness, however, usually renders them less able to cope with separation. As a result, they manifest many of the behaviors of separation anxiety, although the protest behaviors are more subtle and passive than those seen in younger children. Preschoolers may demonstrate separation anxiety by refusing to eat, having difficulty sleeping, crying quietly for their parents, continually asking when they will visit, or withdrawing from others. They may express anger indirectly by breaking their toys, hitting other children, or refusing to cooperate during usual self-care activities. Nurses need to be sensitive to these less obvious signs of separation anxiety in order to intervene appropriately.
Later Childhood
Previous research, usually based on adult recollections, indicated that the family does not play as important a role for school-age children as it does during the toddler and preschool years. However, in a qualitative study of children ages 5 to 9 years, children described hospitalization in stories that focused on being alone and feeling scared, mad, or sad. These children also described the need for protection and companionship while hospitalized (Wilson, Megel, Enenbach, et al, 2010).
Although school-age children are better able to cope with separation in general, the stress and often accompanying regression imposed by illness or hospitalization may increase their need for parental security and guidance. This is particularly true for young school-age children who have only recently left the safety of the home and are struggling with the crisis of school adjustment. Middle and late school-age children may react more to the separation from their usual activities and peers than to absence of their parents. These children have a high level of physical and mental activity that frequently finds no suitable outlets in the hospital environment. Even when they dislike school, they admit to missing its routine and associated activities and worry that they will not be able to compete or “fit in” with their classmates on returning to school. Feelings of loneliness, boredom, isolation, and depression are common. Such reactions may occur more as a result of separation than from concern over the illness, treatment, or hospital setting.
School-age children may need and desire parental guidance or support from other adult figures, but be unable or unwilling to ask for it. Because the goal of attaining independence is so important in this age-group, they are reluctant to seek help directly for fear that they will appear weak, childish, or dependent. Cultural expectations to “act like a man” or to “be brave and strong” bear heavily on these children, especially boys, who tend to react to stress with stoicism, withdrawal, or passive acceptance. Often the need to express hostility, anger, or other negative feelings finds alternate outlets, such as irritability and aggression toward parents, withdrawal from hospital personnel, inability to relate to peers, rejection of siblings, or subsequent problems in school.
For adolescents, separation from home and parents may be difficult. However, loss of peer-group contact may be a severe emotional threat because of loss of group status, inability to exert group control or leadership, and loss of group acceptance. Deviations within peer groups are poorly tolerated, and although members may express concern for the adolescent’s illness or need for hospitalization, they continue their group activities, quickly filling the gap of the absent member. During the temporary separation from their usual group, ill adolescents may benefit from group associations with other hospitalized teenagers.
Loss of Control
The amount of perceived control that children have in the hospital environment directly influences the amount of stress imposed by hospitalization. Lack of control increases the perception of threat and can affect children’s coping skills. Many hospital situations decrease the amount of control a child feels. Although the usual sensory stimulations are lacking, the additional hospital stimuli of sight, sound, and smell may be overwhelming. Without an insight into the type of environment conducive to children’s optimum growth, the hospital experience can at best temporarily slow development and at worst permanently retard it. Because the needs of children vary greatly depending on their age, the major areas of loss of control in terms of physical restriction, altered routine or rituals, and dependency are discussed for each age-group.
Infants
Infants are developing the most important attribute of a healthy personality, trust. Trust is established through consistent, loving care by a nurturing person. Infants attempt to control their environment through emotional expressions, such as crying or smiling. In the hospital setting, cues may be missed or misinterpreted, and routines may be established to meet the hospital staff’s needs instead of the infant’s needs. Inconsistent care and deviations from the infant’s daily routine may lead to mistrust and a decreased sense of control.
Toddlers
Toddlers are striving for autonomy, and this goal is evident in most of their behaviors: motor skills, play, interpersonal relationships, activities of daily living, and communication. When their egocentric pleasures meet with obstacles, toddlers react with negativism, especially temper tantrums. Any restriction or limitation of movement, such as the simple act of laying toddlers on their backs, can cause forceful resistance and noncompliance.
Loss of control also results from altered routines and rituals. Toddlers rely on the consistency and familiarity of daily rituals to provide a measure of stability and control in their life. The experience of hospitalization or illness severely limits their sense of expectation and predictability, since practically every detail of the hospital environment differs from that of home.
Toddlers’ main areas for rituals include eating, sleeping, bathing, toileting, and play. When the routines are disrupted, difficulties can occur in any or all of these areas. The principal reaction to such change is regression. For example, when mealtime and food choices differ from those at home, toddlers often refuse to eat, demand a bottle, or request that others feed them. Although regression to earlier forms of behavior may seem to increase toddlers’ security and comfort, in reality it is threatening for them to relinquish their most recently acquired achievements.
Enforced dependency is a chief characteristic of the sick role and accounts for the numerous instances of toddler negativism. For example, rigid schedules, altered caregiving activities, unfamiliar surroundings, separation from parents, and medical procedures take over toddlers’ control over their world. Although most toddlers initially react negatively and aggressively to such dependency, prolonged loss of autonomy may result in passive withdrawal from interpersonal relationships and regression in all areas of development. Therefore the effects of the sick role are most severe in instances of chronic, long-term illnesses or in families that foster the sick role despite the child’s improved state of health.
Preschoolers
Preschoolers also suffer from loss of control caused by physical restriction, altered routines, and enforced dependency. However, their specific cognitive abilities, which make them feel all powerful, also make them feel out of control. This loss of control in the context of their sense of self-power is a critical factor influencing their perception of and reaction to separation, pain, illness, and hospitalization.
Preschoolers’ egocentric and magical thinking limits their ability to understand events because they view all experiences from their own self-referenced perspective. Without adequate preparation for unfamiliar settings or experiences, preschoolers’ fantasy explanations are usually more exaggerated, bizarre, and frightening than the facts. One typical fantasy to explain the reason for illness or hospitalization is that it represents punishment for real or imagined misdeeds. In response to such thinking the child usually feels shame, guilt, and fear.
Preschoolers’ preoperational thinking means that they understand explanations only in terms of real events. Verbal instructions are often inadequate because of their inability to abstract and synthesize beyond what their senses tell them. When combined with their egocentric and magical thinking, this characteristic may lead them to interpret messages according to their particular past experiences. Even with the best preparation for a procedure, they may misconstrue the details.
Transductive reasoning implies that preschoolers deduce from the particular to the particular, rather than from the specific to the general, or vice versa. For example, if preschoolers’ concept of nurses is that they inflict pain, preschoolers will think that every nurse or caregiver will also inflict pain.
School-Age Children
Because of their striving for independence and productivity, school-age children are particularly vulnerable to events that may lessen their feeling of control and power. In particular, their loss of control may stem from altered family roles; physical disability; and fears of death, abandonment, or permanent injury. Loss of peer acceptance, lack of productivity, and inability to cope with stress according to perceived cultural expectations can also reduce their feelings of control.
Because of the nature of the patient role, many routine hospital activities take priority over individual power and identity. For these children, dependent activities such as enforced bed rest, use of a bedpan, inability to choose meals, lack of privacy, help with a bath, or transport by a wheelchair or stretcher can be a direct threat to their security. Although all these procedures seem routine and inconsequential, they allow no freedom of choice to children who want to “act grown-up.” However, when children are allowed to exert a measure of control, regardless of how limited it may be, they generally respond well to any procedure. For example, some of the most cooperative, satisfied, and contented patients are school-age children who help make their beds, choose their schedule of activities, and assist in procedures. An increased sense of control usually results from a feeling of usefulness and productivity.
In addition to the hospital environment, illness may also cause a feeling of loss of control. One of the most significant problems of children in this age-group is boredom. When physical or enforced limitations curtail their usual abilities to care for themselves or to engage in favorite activities, school-age children generally respond with depression, hostility, or frustration. Keeping a normally active child confined to a small hospital room or on bed rest is difficult. However, emphasizing areas of control and capitalizing on quiet activities, particularly hobbies such as building models or playing appropriate video and computer games, promote their adjustment to physical restriction.
Adolescents
Adolescents’ struggle for independence, self-assertion, and liberation centers on the quest for personal identity. Anything that interferes with this poses a threat to their sense of identity and results in a loss of control. Illness, which limits one’s physical abilities, and hospitalization, which separates one from usual support systems, constitutes major situational crises (see Family-Centered Care box).
The patient role fosters dependency and depersonalization. Adolescents may react to dependency with rejection, uncooperativeness, or withdrawal. They may respond to depersonalization with self-assertion, anger, or frustration. Regardless of which response they manifest, hospital personnel often regard them as difficult, unmanageable patients. Parents may not be a source of help, since these behaviors further isolate them from understanding the adolescent. Although peers may visit, they may not be able to offer the type of support and guidance needed. Sick adolescents often voluntarily isolate themselves from age-mates until they think they can compete on an equal basis and meet group expectations. As a result, ill adolescents may be left with virtually no support system.
Loss of control also occurs for many of the reasons discussed for school-age children. However, adolescents are more sensitive than younger children to potential instances of loss of control and dependency. For example, both groups seek information about their physical status and rely heavily on anticipatory preparation to decrease fear and anxiety. Adolescents, however, react not only to information supplied them, but also to the means by which it is conveyed. They may feel threatened by others who relate facts in a condescending manner. Adolescents want to know that others can relate to them on their own level. This necessitates a careful assessment of their intellectual abilities, previous knowledge, and present needs. It may also require the nurse to learn the adolescent’s language.
Bodily Injury and Pain
Fears of bodily injury and pain are prevalent among children. The consequences of these fears can be far-reaching. Adults who experience more medical fear and pain in childhood are more fearful of medical pain as adults and tend to avoid medical care (Justus, Wyles, Wilson, et al, 2006; Brewer, Gleditsch, Syblik, et al, 2006).
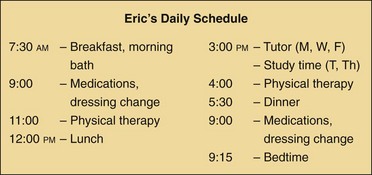
In caring for children, nurses must appreciate their concerns about bodily harm and the reactions to pain at different developmental periods. Table 26-1 summarizes developmental considerations related to children’s understanding of illness and pain.
TABLE 26-1
CHILDREN’S DEVELOPMENTAL CONCEPTS OF ILLNESS AND PAIN
*From Bibace R, Walsh ME: Development of children’s concepts of illness, Pediatrics 66(6):912-917, 1980.
†From Hurley A, Whelan EG: Cognitive development and children’s perception of pain, Pediatr Nurs 14(1):21-24, 1988.
Infants
Newborns and infants undergo a significant number of painful events related to hospitalization. These can include blood draws, lumbar punctures, urinary catheterization, and intravenous (IV) line insertions. The infant’s response to pain varies markedly in measures of distress, especially initial cry and heart rate, which may decrease in some infants. The most consistent indicator of distress is a facial expression of discomfort (Fig. 26-3). Infants may express pain physically by actions such as squirming or flailing (Franck, Greenberg, and Stevens, 2000). Some infants may cry loudly after the procedure, whereas a gentle hug may calm others easily. It is important to recognize and respect such early signs of individuality and to realize that children who react less intensely may still be experiencing significant discomfort.

Fig. 26-3 Facial expressions reflect distress and are consistent behavioral indicators of pain in infants. (Courtesy E. Jacob, Texas Children’s Hospital, Houston.)
Infants younger than 6 months of age seem to have no obvious memory of previous painful experiences and may react to a potentially stressful situation with less apprehension and fear than older children. Research has found that infants have stored memories of acute pain experiences (such as repeated heelsticks) and react in subsequent painful events with heightened responses to pain (Taddio, Shah, Gilbert-MacLeod, et al, 2002; Taddio and Katz, 2005). There is also evidence that repeated painful procedures can alter brain structure and behavioral and hormonal response to pain (American Academy of Pediatrics, 2000; Anand and Scalzo, 2000).
After 6 months of age, children’s response to pain is influenced by their memory of prior painful experiences and the emotional reaction of parents during the procedure. Older infants react intensely with physical resistance and uncooperativeness. They may refuse to lie still, attempt to push the person away, or try to escape with whatever motor activity they have achieved. Distraction does little to lessen their immediate reaction to pain, and anticipatory preparation, such as showing them the equipment, tends to increase their fear and resistance.
Toddlers
Toddlers’ concept of body image, particularly the definition of body boundaries, is poorly developed. Intrusive experiences, such as examining the ears or mouth or taking a rectal temperature, produce anxiety. Toddlers may react to such painless procedures as intensely as they do to painful ones.
Toddlers’ reactions to pain are similar to those seen during infancy, except that the variables influencing the individual response are highly complex and varied. Memory, physical restraint, separation from the parent or guardian, emotional reactions of others, and lack of preparation partially determine the intensity of the behavioral response. In general, children in this age-group continue to react with intense emotional upset and physical resistance to any actual or perceived painful experience. Behaviors indicating pain include grimacing; clenching the teeth or lips; opening the eyes wide; rocking; rubbing; and aggressiveness, such as biting, kicking, hitting, or running away. Unlike adults, who usually decrease their activity when in pain, young children typically become restless and overactive; frequently this response is not recognized as a consequence of pain.
By the end of this age period, toddlers usually are able to communicate about their pain. Although they have not developed the ability to describe the type or intensity of the pain, they usually are able to localize it by pointing to a specific area.
Preschoolers
Concepts of illness begin during the preschool period and are influenced by the cognitive abilities of the preoperational stage. Preschoolers differentiate poorly between themselves and the external world. Their thinking is focused on externally perceived events, and causality is based on the proximity of two events. Consequently, children define illness according to what they are told or are given external evidence of, such as “You are sick because you have a fever.” The cause of illness is a concrete action the child does or fails to do, such as “catching a stomach virus because you don’t wash your hands.” Consequently, illness implies a degree of responsibility and self-blame. Another explanation may be based on contagion, that is, the proximity of two objects or persons causes the illness (e.g., “A person gets a cold when someone else with a cold gets near him”).
The psychosexual conflicts of children in this age-group make them vulnerable to threats of bodily injury. Intrusive procedures, whether painful or painless, are threatening to preschoolers, whose concept of body integrity is still poorly developed. Preschoolers may react to an injection with as much concern for withdrawal of the needle as for the actual pain. They fear that the intrusion or puncture will not close and that their “insides” will leak out.
Concerns of mutilation are paramount during this age period. Loss of any body part is threatening, but preschool boys’ fears of castration complicate their understanding of surgical or medical procedures associated with the genital area, such as circumcision, repair of hypospadias or epispadias, cystoscopy, or catheterization. Their limited comprehension of body functioning also increases their difficulty in understanding how or why body parts are “fixed.” For example, telling preschoolers that their tonsils are to be removed may be interpreted as “taking out their voice.” Preschoolers understand words such as dye, cut off, take out, or draw (as in “draw some blood”), and using these words can lead to confusion and fear. (See Communicating with Children, Chapter 6.)
Reactions to pain tend to be similar to those seen during toddlerhood, although some differences become apparent. For example, preschoolers respond more favorably to preparatory interventions, such as explanation and distraction, than younger children. Physical and verbal aggression is more specific and goal directed. Instead of showing total body resistance, preschoolers may push the offending person away, try to secure the equipment, or attempt to lock themselves in a safe place. Much more thought is evident in their plan of attack or escape.
Verbal expression in particular demonstrates their advanced development in response to stress. They may verbally abuse the attacker by stating, “Go away” or “I hate you.” They may also use the more cunning approach of trying to persuade the person to delay the intended activity. A common plea is “I have to go to the bathroom.” Some statements are not only attempts to avoid the event but also evidence of children’s perceptions about the experience.
School-Age Children
Fears of the physical nature of the illness surface at this time. School-age children may be less concerned with pain than with disability, uncertain recovery, or possible death. Because of their developing cognitive abilities, school-age children are aware of the significance of different illnesses, the indispensability of certain body parts, potential hazards in treatment, lifelong consequences of permanent injury or loss of function, and the meaning of death. A major concern of hospitalized school-age children is their fear of being told that something is wrong with them. They generally take an active interest in their health or illness. Even those children who rarely ask questions usually accumulate detailed information on their condition by attentively listening to all that is said around them. They request factual information and quickly perceive lies or half-truths. Seeking information tends to be one way they maintain a sense of control despite the stress and uncertainty of illness.
School-age children define illness by a set of multiple concrete symptoms, such as signs of a cold, and view the cause as primarily germs or bacteria. The germs have a powerful, almost magical quality, so that in the child’s mind, illness can be prevented by avoiding people with the germs. They also believe in the idea of contamination, which is similar to that seen in the younger age-group. For example, the illness occurs because of physical contact or because the child engaged in a harmful action and became contaminated. Consequently, feelings of self-blame and guilt may be associated with the reason for becoming ill.
School-age children begin to show concern for the potential beneficial and hazardous effects of procedures. Besides wanting to know if a procedure will hurt, they want to know what it is for, how it will make them well, and what injury or harm could result. For example, these children fear the actual procedure of anesthesia. Unlike preschoolers, who fear the mask and the strange surroundings, school-age children fear what might happen while they are asleep, whether they will wake up, and whether they might die. Preadolescents also worry about the procedure itself, particularly one that will result in visible changes in body appearance.
Intrusive procedures, such as routine physical examination of the ears, nose, mouth, and throat, are generally well tolerated. However, concerns for privacy become increasingly significant. Although school-age children may cooperate during examination of, or procedures performed on, the genital area, it is usually stressful for them, especially for preadolescents who are beginning pubertal changes. Nurses who respect children’s need for privacy can provide them with assurance and support.
By the age of 9 or 10, most school-age children show less fright or overt resistance to pain than younger children. They generally have learned passive methods of dealing with discomfort, such as holding rigidly still, clenching their fists or teeth, or trying to act brave. If they display signs of overt resistance, such as biting, kicking, pulling away, trying to escape, crying, or plea bargaining, they may deny such reactions later, especially to their peers, for fear of embarrassment.
School-age children verbally communicate about their pain in respect to its location, intensity, and description. Unlike younger children, who may have difficulty choosing words to describe pain, children 8 years and older (like adults) use a wide variety of words and phrases, such as hurting, sore, burning, stinging, and aching (Franck, Greenberg, and Stevens, 2000).
School-age children also use words as a means of controlling their reactions to pain. For example, these children may ask the nurse to talk to them during a procedure. Some prefer to participate in a procedure, whereas others choose to distance themselves by not looking at what is happening. Most appreciate an explanation of the procedure and seem less fearful when they know what to expect. Others try to gain control by attempting to postpone the event. A typical request is, “Start the IV when I am finished with this.” Although the ability to make decisions does increase their sense of control, unlimited procrastination and bargaining result in heightened anxiety. When choices are allowed, such as which arm for the IV line, it is best to structure the number of options and to limit the number of procrastination or bargaining techniques. Nurses must also exercise caution when asking the child to make choices to ensure that the choice can be honored.
Similar to their more passive acceptance of pain is their nondirective request for support or help. School-age children rarely initiate a conversation about their feelings or ask someone to stay with them during a lonely or stressful period. Their visible composure, calmness, and acceptance often mask their inner longing for support. It is especially important to be aware of nonverbal clues, such as a serious facial expression, a halfhearted reply of “I am fine,” silence, lack of activity, or social isolation, as signs of the need for help. Usually when someone identifies the unspoken messages and offers support, they readily accept it.
Adolescents
Although the development of body image begins early in life, its relevance is paramount during adolescence. Injury, pain, disability, and death are viewed primarily in terms of how each affects adolescents’ views of themselves in the present. Any change that differentiates the adolescent from peers is regarded as a major tragedy. For example, chronic diseases such as diabetes mellitus often present a more difficult adjustment period for children in this age-group than for younger children because of the necessary changes in lifestyle. Conversely, serious, even life-threatening illnesses that entail no visible bodily changes or physical restrictions may have less immediate significance for the adolescent. Therefore the nature of bodily injury may be more important in terms of adolescents’ perception of the illness than its actual degree of severity.
Adolescents’ rapidly changing body image during pubertal development often makes them feel insecure about their bodies. Illness, medical or surgical intervention, and hospitalization increase their existing concerns for normalcy. They may respond to such events by asking numerous questions, withdrawing, rejecting others, or questioning the adequacy of care. Frequently their fear for loss of control and body image change is demonstrated as overconfidence.
Because of the development of secondary sexual characteristics, adolescents are concerned about privacy. Lack of respect for this need can cause greater stress than physical pain. In addition, adolescents look for signs that indicate they are developing normally and according to acceptable standards. When illness occurs, they fear that growth may be retarded, leaving them behind their peers. Although they may not voice this concern, they may demonstrate it by carefully observing others’ reactions to them.
Adolescents typically react to pain with much self-control. Physical resistance and aggression are unusual at this age, unless the adolescents are unprepared for a procedure. As with older school-age children, they are concerned with remaining composed and feel embarrassed and ashamed of losing control. They are able to describe their pain experience and to use the pain assessment tools developed for adults. However, they may be reluctant to disclose their pain, requiring the nurse to listen closely and observe physical indications, such as limited movement, excessive quiet, or irritability. Adolescents may also believe that the nurse knows how they feel; thus they may see no need to ask for analgesia.
Effects of Hospitalization on the Child
Children may react to the stresses of hospitalization before admission, during hospitalization, and after discharge (Box 26-2). A child’s conception of illness is even more important than age and intellectual maturity in predicting the level of adjustment before hospitalization. This may or may not be affected by the duration of the condition or prior hospitalizations. Therefore nurses should avoid making incorrect assumptions regarding the illness concepts of children with prior medical experience.
Individual Risk Factors
A number of risk factors make some children more vulnerable than others to the stresses of hospitalization (Box 26-3). Because separation is such an important issue surrounding hospitalization for young children, children who are active and have a strong will tend to fare better when hospitalized than youngsters who are passive. Nurses should be alert to children who passively accept all changes and requests, since these children may need more support than the “oppositional” child.
The stressors of hospitalization may cause young children to experience short- and long-term negative outcomes. Adverse outcomes may be related to the length and number of admissions, multiple invasive procedures, and parents’ anxiety. Common responses include regression, separation anxiety, apathy, fears, and sleep disturbances, especially for children younger than 7 years of age (Melnyk, 2000). Supportive practices, such as family-centered care, frequent family visits, and mothers who know exactly how they can be involved in their child’s care, may lessen the detrimental effects of hospitalization. Research also indicates that the child’s pain experience determines how the child will experience the overall hospitalization. Consequently, nurses should attempt to identify children who are at risk for poor coping outcomes (Small, 2002).
Changes in the Pediatric Population
Children are hospitalized for different reasons today than two decades ago. Despite the growing trend toward shortened hospital stays and outpatient surgery, a greater percentage of the children hospitalized today have more serious and complex problems than those hospitalized in the past. Many of these children are medically fragile newborns and children with severe injuries or disabilities who survived because of incredible technologic advances, yet were left with chronic or disabling conditions that require frequent and lengthy hospital stays. The nature of their conditions increases the likelihood that this group of children will experience more invasive and traumatic procedures while they are hospitalized. These factors make them more vulnerable to the emotional consequences of hospitalization and result in their needs being significantly different from those of short-term patients. (See Chapter 22 for further discussion on children with special needs.) The majority of these children are infants and toddlers, the age-group most vulnerable to the effects of hospitalization.
Concern in recent years has focused on the increasing length of hospitalization because of complex medical and nursing care, elusive diagnoses, and complicated psychosocial issues. Without special attention devoted to meeting the child’s psychosocial and developmental needs in the hospital environment, the damaging consequences of prolonged hospitalization may be severe.
Beneficial Effects of Hospitalization
Although hospitalization can be and usually is stressful for children, it can also be beneficial. The most obvious benefit is the recovery from illness, but hospitalization also can present an opportunity for children to master stress and feel competent in their coping abilities. The hospital environment can provide children with new socialization experiences that can broaden their interpersonal relationships. The psychologic benefits need to be considered and maximized during hospitalization. Appropriate nursing strategies to achieve this goal are presented later in this chapter.
Stressors and Reactions of the Family of the Child Who is Hospitalized
The crisis of childhood illness and hospitalization is a major source of stress and anxiety for every member of the nuclear family. Parents’ reactions to their child’s illness depend on a variety of factors. Although one cannot predict which factors are most likely to influence their response, a number of variables have been identified (Box 26-4).
Fear, anxiety, and frustration are common feelings expressed by parents. Fear and anxiety may be related to the seriousness of the illness and the type of medical procedures involved. Anxiety is frequently related to the trauma and pain inflicted on the child from the various procedures. Parents may question why they and their child have to go through this experience, as well as the purpose of pain and suffering (Feudtner, Haney, and Dimmers, 2003). Frustration is often related to lack of information about procedures and treatments, unfamiliarity with hospital rules and regulations, unfriendly staff, or fear of asking questions. Nurses can alleviate much frustration in the pediatric unit by making parents aware of what to expect and what is expected of them, encouraging them to participate in their child’s care, and treating them as the most significant contributors to the child’s total health.
Parents eventually may react with some degree of depression. Mothers often comment on their feeling of physical and mental exhaustion after all the other family members have adapted to the crisis. Parents may also worry about and miss their other children, who may be left in the care of family, friends, or neighbors. Other reasons for anxiety and depression are related to concerns for the child’s future well-being, including negative effects produced by the hospitalization and any subsequent financial burden incurred.
In a retrospective database survey of more than 50,000 parents of a hospitalized child, parents identified seven priorities from their perspective to improve the care of the hospitalized child (Miceli and Clark, 2005). The parents’ highest priority was to improve staff’s sensitivity to the disruption and inconvenience of the child being hospitalized. Additional leading suggestions included improving the degree to which hospital staff address the family’s emotional and spiritual needs during the child’s hospitalization, improving staff’s response when parents express concerns or voice complaints during the child’s stay, including parents in decisions regarding treatments, improving visitor (family) accommodations and comfort, providing information about nearby services and lodging facilities for family members, and improving staff concerns to make the child’s stay as restful and comfortable as possible. In each of the seven categories the researchers provide additional issues parents raised in relation to the primary theme.
Studies highlight the need for family-centered nursing care that considers the effects of hospitalization on the child and the parents (Miceli and Clark, 2005; Stratton, 2004; Feudtner, Haney, and Dimmers, 2003). Hospital staff members must continually assess the parents’ need for information and reassurance. Although the child’s care may take precedence over parents’ needs, nurses must make every effort to improve parent coping to optimize patient outcomes. By maintaining sensitivity to the family’s needs, the nurse can become equal partners with parents in the child’s care.
Sibling Reactions
Siblings’ reactions to a sister’s or brother’s illness or hospitalization are discussed in Chapters 22 and 23 and differ little when a child has an acute illness. Siblings may experience loneliness, fears, and worry. Siblings frequently fear acquiring the illness of their ill sibling. Behavioral reactions include anger, resentment, jealousy, and guilt. Various factors have been identified that influence the siblings’ reactions to the child’s hospitalization. Although these factors are similar to those seen when a child has a chronic illness, Craft (1993) reported that the following factors are related specifically to the hospital experience and have been found to increase the effects on the sibling:
• Being younger and experiencing many changes
• Being cared for outside the home by care providers who are not relatives
• Receiving little information about their ill brother or sister
• Perceiving their parents as treating them differently compared with before their sibling’s hospitalization
Parents are often unaware of the effect on siblings of a sick child’s hospitalization and of the benefit of simple interventions to minimize such effects, such as explicit explanations about the illness and provisions for the siblings to remain at home. Sibling visitation is advocated and is usually advantageous. However, unless siblings are prepared for what they may see, their visits may confuse them, leaving room for greater anxiety and worry when they are home, away from their hospitalized brother or sister. Siblings need to be given developmentally appropriate information about their sibling’s illness or injury and be given an opportunity to ask questions.
Altered Family Roles
In addition to the effects of separation on family roles, loss of the parent and sibling roles may affect each family member differently. One of the most common reactions of parents is intensified attention toward the sick child. The other siblings may regard this as unfair and interpret the parents’ attitude toward them as rejection and abandonment. Although such responses are usually unconscious and unintended, they place unique burdens on ill children. For example, the ill child may feel obligated to play the sick role to meet parents’ expectations, especially in the case of children who have had limited physical ability and regain normal health status, such as following corrective heart surgery. Parents also may have difficulty perceiving the child’s recovery and therefore continue the pattern of overprotection and indulgent attention.
Ill children may also feel jealousy and resentment from siblings. Because of their singular position in the family, they may be denied the companionship of their brothers and sisters. Rivalry tends to be greatest with the sibling who is nearest the ill child’s age. Without an understanding of the interpersonal dynamics between siblings, parents are likely to blame the well children for antisocial behavior. Illness may also result in a child’s loss of status within either the family or peer group. For example, illness in the oldest child may temporarily terminate special privileges as “big” brother or sister.
Nursing Care of the Child Who is Hospitalized
Children and their families require competent and sensitive care to minimize the potential negative effects of hospitalization and also to promote positive benefits from the experience. Interventions should focus on (1) eliminating or minimizing the stressors of separation, loss of control, and bodily injury and pain for children; and (2) providing specific supportive strategies for family members, such as fostering family relationships and providing information.
Initiate a family assessment using the guidelines in Box 26-7. Assess the parents and other immediate family members for coping and for special assistance needs (e.g., temporary child care for siblings, lodging, meals, and transportation to and from hospital).
Preventing or Minimizing Separation
A primary nursing goal is to prevent separation, particularly in children under 5 years of age. Hospitals no longer consider parents “visitors” and welcome their presence at all times throughout the child’s hospitalization. Many hospitals have adopted a philosophy of family-centered care, which recognizes the integral role of the family in a child’s life and acknowledges the family as an essential part of the child’s care and illness experience. In the broadest sense, the family is considered to be partners in the care of the child (Smith and Conant Rees, 2000). Emphasis is placed on providing services that demonstrate the value of collaboration between the health care provider, the child, and the family. Many hospitals provide a chair or bed for at least one person per child, unit kitchen privileges, and other amenities that create a welcoming atmosphere for parents. Still, the parents’ own schedules may prevent them from being present. In such instances, strategies to minimize the effects of separation must be implemented.
Parent Participation
Although some health facilities provide special accommodations for parents, the concept of family-centered care can be instituted anywhere. The first requirement is the staff’s positive attitude toward parents. A negative attitude toward parent participation can create barriers to collaborative working relationships (Smith and Conant Rees, 2000). Unfortunately, although nurses often express explicit support for the concept of family-centered care, some of their practices and beliefs suggest otherwise (Newton, 2000).
Hospital staff who genuinely appreciate the importance of continued parent-child attachment foster an environment that encourages parents to be active caregivers. When nurses include parents in the care planning and ensure them that they are contributing to the child’s recovery, parents are more inclined to remain with their child and have more emotional reserves to support themselves and the child through the crisis. An empowerment model of helping allows the nurse to focus on parents’ strengths and to seek ways to promote growth and family functioning (Fig. 26-4). Strategies such as bedside reporting that allow parents to be involved in the discussion of the child’s current status are moving health care settings closer to family-centered care (Anderson and Mangino, 2006). Liaison nursing roles in tertiary care settings are also focused on improving communication between parents and health care providers (Caffin, Linton, and Pellegrini, 2007).

Fig. 26-4 Family presence during hospitalization, including during procedures, provides emotional support. (Courtesy Paul Vincent Kuntz, Texas Children’s Hospital, Houston.)
Parents may display different and varied needs regarding involvement in their child’s care. Not all parents feel comfortable assuming responsibility, and they may be under such great emotional stress that they need a temporary reprieve from caregiving activities. Others may feel insecure in participating in specialized care. On the other hand, some parents may feel a need to control their child’s care and wish to be involved in every way possible. Individual assessment of each parent’s preferred involvement is necessary to prevent the effects of separation while supporting parents’ needs. Because the mother tends to be the usual family caregiver, she may spend more time in the hospital than the father (Fig. 26-5). Fathers need to be included in the care plan and respected for their parental role. For some fathers, the child’s hospitalization may represent an opportunity to alter their usual caregiving role and increase their involvement. In single-parent families the caregiver may not be a parent but an extended family member, such as a grandparent or aunt. Parents and other family members should be prepared and supported for the roles they choose.

Fig. 26-5 Despite changing lifestyles and gender roles, mothers tend to be the usual family caregiver and spend more time at the hospital than fathers.
One of the potential problems with continuous parent visitation is that the parent often neglects the need for sleep, nutrition, and relaxation. The sleeping accommodations may be limited to a chair, and sleep is disrupted by nursing procedures. After a few days, parents may become exhausted but feel obligated to stay at their child’s bedside. Encouraging them to leave for brief periods, arranging for sleeping quarters on the unit but outside the child’s room, and planning a schedule of alternating visitation with the other parent or with a family member can minimize the stresses for the parent.
All too often, nurses respond to parental participation by abandoning their patient responsibilities. Nurses need to restructure their roles to complement and augment the parents’ caregiving functions and to promote family health (Hopia, Tomlinson, Paavilainen, et al, 2005). Even in units structured to promote care by parents, parents frequently feel anxiety in their caregiving responsibilities. Those more involved in direct care may feel greater anxiety than those less involved. A moderate amount of visitation and participation may be optimum for many. Nursing assistance should always be available to these families.
Strategies to Minimize the Effects of Separation
When separation cannot be prevented, the nurse can employ numerous strategies to minimize the effects of temporary separation on children. Ideally, a primary nurse is assigned to meet the child’s needs. The nurse should obtain a thorough, detailed history that specifically identifies the child’s daily routine (see Box 26-7, p. 988). Usual daily activities such as meal preparation and method of feeding help establish a complementary schedule of caregiving practices. It also helps the parents feel as though they are participating in the child’s care but through another person. A consistent staff member can also keep the family informed of the child’s condition and support the family’s concerns and priorities.
The nurse caring for the child must be aware of the child’s separation behaviors. As discussed earlier, phases of protest and despair are normal. The child is allowed to cry. Even if the child rejects strangers, the nurse provides support through physical presence. This includes spending time being physically close to the child, using a quiet tone of voice, appropriate words, eye contact, and touch in ways that establish rapport and communicate empathy. If detachment behaviors are evident, the nurse maintains the child’s contact with the parents by frequently talking with them; encouraging the child to remember them; and stressing the significance of their visits, telephone calls, or letters.
Separation may be equally difficult for parents, especially when they do not understand the behaviors of separation anxiety. To avoid the immediate protest, parents may sneak out or lie to the child about leaving. As a result, the child does not learn to associate absence with a guaranteed return because there is an element of uncertainty. Helping parents recognize that separation behaviors are normal and expected can decrease anxiety and may ease their fears about leaving the child. Explaining to parents how the child reacts after they leave may also be helpful. Many parents think the child cries for hours after they leave, whereas in reality the child may cry for a few minutes but then settle down when comforted by someone else.
Toddlers and preschoolers have a limited concept of time. Time is measured in associations, such as “eating dinner when daddy comes home.” Therefore, when helping parents with their fears of separation, nurses need to suggest ways of explaining leaving and returning. For example, if parents must leave to go to work or to make meals for the other family members, they should tell the hospitalized child the reason for leaving. They also need to convey the expected time of return in terms of anticipated events. For example, if the parents return in the morning, they can tell the child that they will see him or her “when it’s time for breakfast” or “when [a favorite program] is on television.”
The young child’s ability to tolerate parental absence is limited. Therefore parental visits should be frequent. For example, it is better for parents to visit three times a day for short periods than once a day for an extended time. This may necessitate that each parent visit at different times to lessen the length of separation. When parents cannot visit, the presence of other significant people may comfort the child (Fig. 26-6).

Fig. 26-6 When parents cannot visit, other significant persons can provide comfort to the hospitalized child.
If parents leave after the child is asleep, they still need to communicate their absence. The parents of a 5-year-old boy solved this problem by devising a sign; on one side they drew a picture of a telephone and on the other a hamburger. Before they left, they turned the sign to the appropriate side to tell the child when he awoke that they were out using the telephone or eating.
For older children who know how to tell time, it is helpful to give them a clock or watch. However, these children have the same needs for honesty from their parents regarding visiting schedules. Because peer groups are also important, adolescents often appreciate planning visiting hours to provide them with some private time for friends. Many hospitals today also offer Internet connectivity, which allows older children and adolescents to remain in contact with family members and peers via e-mail or social networking sites.
Familiar surroundings also increase the child’s adjustment to separation. If parents cannot stay with the child, they should leave favorite articles from home, such as a blanket, toy, bottle, feeding utensil, or article of clothing. Because young children associate such objects with significant people, they gain comfort and reassurance from these possessions. They make the association that, if the parent left this, the parent will surely return. Other mementos of home include photographs and recordings of family members reading a story, singing a song, or relating events at home. Some units allow pets to visit, which can be a special event for a child and can have therapeutic benefits.
Older children also appreciate familiar articles from home, particularly photographs, a favorite toy or game, and their own pajamas. The importance of treasured objects for school-age children may be overlooked or criticized. However, approximately half of school-age children have a special object to which they formed an attachment in early childhood. This is a normal and healthy phenomenon. Therefore such treasured or transitional objects can help even older children feel more comfortable in a strange environment.
The sights and sounds in the hospital that are commonplace for the nurse can be strange, frightening, and confusing for children. It is important for the nurse to try to evaluate stimuli in the environment from the child’s point of view (considering also what the child may see or hear happening to other patients) and to make every effort to protect the child from frightening and unfamiliar sights, sounds, and equipment. The nurse should offer explanations or prepare the child for those experiences that are unavoidable. Combining familiar or comforting sights with the unfamiliar can relieve much of the harshness of medical care.
Helping children maintain their usual contacts also minimizes the effects of separation imposed by hospitalization. This includes continuing school lessons during the illness and confinement, visiting with friends either directly or through e-mail, and participating in stimulating projects whenever possible (Fig. 26-7). For extended hospitalizations, youngsters enjoy personalizing the hospital room to make it “home” by decorating the walls with posters and cards and rearranging the furniture (when possible).
Minimizing Loss of Control and Autonomy
Feelings of loss of control result from separation, physical restriction, changed routines, enforced dependency, magical thinking, and altered roles within the family or peer group. Although some of these cannot be prevented, most can be minimized through individualized nursing care.
Promoting Freedom of Movement
Younger children react most strenuously to any type of physical restriction or immobilization. Although some restraint may be necessary, such as temporarily immobilizing an extremity for maintenance of an IV line, most physical restriction can be avoided if the nurse gains the child’s cooperation.
For young children, particularly infants and toddlers, preserving parent-child contact is the best means of decreasing the need for or stress of restraint. For example, the nurse can perform almost the entire physical examination with the child in a parent’s lap, with the parent hugging the child for procedures such as otoscopy. For painful procedures the nurse assesses the parents’ preferences for assisting, observing, or waiting outside the room.
Environmental factors may restrict movement. Keeping children in cribs or playpens may not represent immobilization in the strictest sense, but it certainly limits sensory stimulation. Increasing mobility by transporting children in carriages, wheelchairs, carts, or wagons provides them with a sense of freedom.
In some cases physical restraint or isolation is necessary. Whenever possible, remove restraints to allow the child some period of supervised freedom, such as during baths or visits from parents. When restraints or isolation cannot be discontinued, such as with severe burns, the environment can be altered to increase sensory freedom. Moving the bed toward the door or window; opening window shades; providing musical, visual, or tactile toys; and increasing interpersonal contact can substitute mental mobility for the limitations of physical movement.
Maintaining the Child’s Routine
Altered daily schedules and loss of rituals are particularly stressful for toddlers and early preschoolers and may increase separation anxiety. As stated previously, the nursing admission history provides a baseline for planning care around the child’s usual home activities.
Children’s response to loss of routine and ritualism is often demonstrated in problems with activities such as eating, sleeping, dressing, bathing, toileting, and social interaction. Although some regression is expected, sensitivity to the child’s special needs can minimize the negative effects. For example, loss of appetite and marked food preferences are common in children who are ill or hospitalized. In addition, the food selections on hospital menus may differ greatly from preferred cultural or ethnic food preparation. Encouraging the child to eat is often a challenge, yet it is an essential nursing responsibility. Chapter 27 discusses suggestions for feeding sick children.
A frequently neglected aspect of altered routines is the change in the child’s daily activities. A nonhospitalized child’s day, especially during the school years, is structured with specific times for eating, dressing, going to school, playing, and sleeping. However, this time structure vanishes when the child is hospitalized. Although the nurses have a set schedule, the child is frequently unaware of it. Many children obtain significantly less sleep in the hospital than at home, primarily because sleep is delayed and then ends early due to hospital routines. Not only are hours of sleep disrupted, but waking hours are spent in passive activities. For example, few institutions impose any restrictions on the amount of time children spend watching television, which tends to be considerably more time than they spend watching at home.
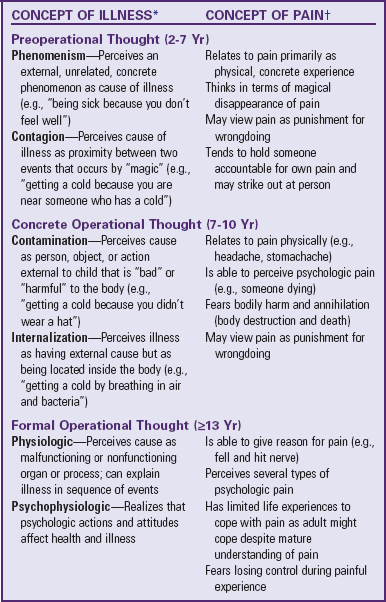
One technique that can minimize the disruption in the child’s routine is establishing a daily schedule. This approach is most suitable for the noncritically ill school-age and adolescent child who has mastered the concept of time. It involves scheduling the child’s day to include all necessary activities that are important to patient care procedures, activities of daily living, mealtimes, and medications. Together, the nurse, parent, and child plan a daily schedule with times and activities written down, with blocks of free time available for playroom activities, hobbies, and television viewing (Fig. 26-8). The child is given a copy of the schedule and a clock. For lengthy hospitalizations, a calendar may be constructed identifying special events such as favorite television programs, visits by friends or relatives, events in the playroom, holidays or birthdays, and any expected changes in treatment (e.g., “beginning physical therapy in 2 days”).
Encouraging Independence
The dependent role of being hospitalized imposes feelings of loss on older children. Principal interventions should focus on respect for individuality and the opportunity for decision making. Although these sound simple, their efficacy depends on nurses who are flexible and tolerant. It is also important to empower the patient and not be threatened by a sense of lessened control.
Fostering children’s control involves helping them maintain independence and promoting self-care. Self-care refers to the practice of activities that individuals initiate and perform on their own behalf to maintain life, health, and well-being (Orem, 2001). Although self-care is limited by the child’s age and physical condition, most children beyond infancy can perform some activities with little or no help. Whenever possible, encourage these activities in the hospital. Other approaches include structuring time and allowing the child to jointly plan care, wear street clothes, make choices in food selections and bedtime, continue school activities, and room with an appropriate age-mate. For example, adolescents generally prefer a roommate their own age and, ideally, quarters separate from the pediatric unit.
Promoting Understanding
Loss of control can occur both from feelings of having too little influence on one’s destiny and from sensing overwhelming control or power over fate. Although preschoolers’ cognitive abilities predispose them most to creative thinking and delusions of power, all children are vulnerable to misinterpreting causes for stresses such as illness and hospitalization.
Most children feel more in control when they know what to expect, since this reduces the element of fear. Providing anticipatory preparation and information helps greatly to lessen stress and prevent misunderstanding. (See Preparation for Diagnostic and Therapeutic Procedures, Chapter 27.)
Informing children of their rights while hospitalized fosters greater understanding and may relieve some of the feelings of powerlessness they experience. Standards used to accredit hospitals recommend that hospitals providing services to children have a hospital-wide policy on the rights and responsibilities of these patients and of their parents or guardians (Joint Commission on Accreditation of Healthcare Organizations, 2004). Present information regarding patient rights to children and their families during the admission process.
Preventing or Minimizing Fear of Bodily Injury
Beyond early infancy all children fear bodily injury either from mutilation, intrusion, body image change, disability, or death. In general, preparation of children for painful procedures decreases their fears. Manipulating procedural techniques for children in each age-group also minimizes fear of bodily injury. For example, since toddlers and young preschoolers are traumatized by insertion of a rectal thermometer, axillary or tympanic electronic temperature probes can be effectively substituted. Whenever procedures are performed on young children, the most supportive intervention is to do them as quickly as possible and maintain parent-child contact.
Because of the toddler’s and preschooler’s poorly defined body boundaries, the use of bandages may be particularly helpful. For example, telling children that the bleeding will stop after the needle is removed does little to relieve their fears, whereas applying a Band-Aid usually reassures them. The size of bandages is also significant to children in this age-group. The larger the bandage, the more importance is attached to the wound. Successively smaller surgical dressings are one way they measure healing and improvement. Removing a dressing may cause them concern for their well-being.
In children who fear mutilation of body parts, repeatedly stressing the reason for a procedure and evaluating their understanding are essential to minimize fear. For example, explaining cast removal to preschoolers may seem simple enough, but the child’s comprehension of the details may vary considerably. Asking them to draw a picture of what they think will happen provides substantial evidence of how they perceive events.
Children may fear bodily injury from a great variety of sources. Diagnostic imaging machines, strange equipment for examinations, unfamiliar rooms, or awkward positions can be perceived as potentially hazardous. In addition, thoughts and actions can be imagined sources of bodily damage. Therefore it is important to investigate imagined reasons for illness. Children may fear revealing such thoughts, and techniques such as drawing or doll play may help reveal their misconceptions.
Older children fear bodily injury of both internal and external origins. For example, school-age children are aware of the heart’s significance and may fear an actual procedure involving the heart as much as the pain, the stitches, and the possible scar. Adolescents may express concern for the surgery but be much more anxious over the resulting scar. An appreciation of each child’s special concerns helps nurses focus on critical areas when preparing patients for procedures or explaining the disease processes.
Children can grasp information only if it is presented on or close to their level of cognitive development. This necessitates an awareness of the words used to describe events or processes. For example, young children told that they are going to have a CAT scan may wonder, “Will there be cats? Or something that scratches?” It is clearer to describe the procedure in simple terms and explain what the letters of the common name stand for.
When children are upset about their illness, the nurse can change their perception by (1) providing a somewhat different and less negative account of the disease or (2) offering an explanation that is characteristic of the next stage of cognitive development. An example of the first strategy is reassuring a preschool child who, after a tonsillectomy, fears that another sore throat means a second operation. Explaining that once tonsils are “fixed,” they do not need fixing again can help relieve the fear. An example of the second strategy is to explain that germs made the tonsils sick and even though germs can cause another sore throat, they cannot cause the tonsils to ever be sick again. This higher-level explanation is based on the school-age child’s concept of germs as a cause of disease.
Providing Developmentally Appropriate Activities
A primary goal of nursing care for the child who is hospitalized is to minimize threats to the child’s development. Many strategies (e.g., minimizing separation) have been discussed and may be all that the short-term patient requires. However, children who experience prolonged or repeated hospitalization are at greater risk for developmental delay or regression. The nurse who provides opportunities for the child to participate in developmentally appropriate activities further normalizes the child’s environment and helps reduce interference with the child’s ongoing development. (See Normalization, Chapter 22.)
Child life specialists are health care professionals with extensive knowledge of child growth and development and the special psychosocial needs of children who are hospitalized and their families (Box 26-5). They help prepare children for hospitalization, surgery, and procedures. Although all members of the health care team share these responsibilities, this is the primary role of the child life specialist. A collaborative effort between the nurse, child life specialist, and other members of the child’s health care team will help ensure the best possible hospital experience for the child and family (American Academy of Pediatrics, 2000).
Using Play and Expressive Activities to Minimize Stress
![]() Play is one of the most important aspects of a child’s life and one of the most effective tools for managing stress. Because illness and hospitalization constitute crises in the child’s life and often involve overwhelming stresses, acting out fears and anxieties gives the child a means to cope with these stresses. Children who play are coping positively; children who cannot play are waiting, testing, holding back, or making some inner decisions about the setting.
Play is one of the most important aspects of a child’s life and one of the most effective tools for managing stress. Because illness and hospitalization constitute crises in the child’s life and often involve overwhelming stresses, acting out fears and anxieties gives the child a means to cope with these stresses. Children who play are coping positively; children who cannot play are waiting, testing, holding back, or making some inner decisions about the setting.
Play is essential to children’s mental, emotional, and social well-being. As with their developmental needs, the need for play does not stop when children are ill or when they enter the hospital. On the contrary, play in the hospital serves many functions (Box 26-6). Of all hospital facilities, no room probably does more to alleviate the stressors of hospitalization than the playroom. In this room children temporarily distance themselves from the fears of separation, loss of control, and bodily injury. They can work through their feelings in a nonthreatening, comfortable atmosphere and in the manner most natural for them. They also know that the boundaries of this room are safe from intrusive or painful procedures, strange faces, and probing questions. The playroom becomes a sanctuary of peace and safety in an otherwise frightening environment (see Critical Thinking Exercise).
Engaging in play activities puts children in charge, removing them for a time from the usual passive role of recipients of a constant stream of procedures and hospital routines. In the hospital environment most decisions are made for the child, but play and other expressive activities offer the child much-needed opportunities to make choices. Even if a child chooses not to participate in a particular activity, the nurse has offered the child a choice, perhaps one of but a few real choices the child has had that day.
Children who are ill and hospitalized typically have lower energy levels than healthy children. Therefore children may not appear enthusiastic about an activity even when they are enjoying the experience. Rather than assuming otherwise, the nurse can observe for subtle signs—such as a fleeting smile or intense concentration—or simply ask children if they are enjoying themselves.
Children in various age-groups require different types of play facilities. Infants and toddlers need maximum safety, whereas school-age children and adolescents benefit most from group activities. Providing space for special needs of children in each age-group can be difficult in institutions where space is limited, but innovative solutions can ensure practical answers. Structure playroom schedules to allow one age-group at a time; for example, adolescents can use the facility in the evening when younger children are asleep. Older children can also congregate in one patient’s room and listen to music, play games, or just talk. If the location of the session rotates each evening, older children can look forward to arranging or setting up for the activities.
Diversional Activities
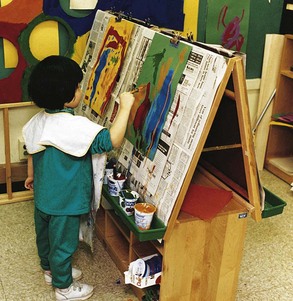
Almost any form of play can be used for diversion and recreation, but the activity should be selected on the basis of the child’s age, interests, and limitations (Fig. 26-9). Children do not necessarily need special direction for using play materials. All they require are the materials with which to work and adult approval and supervision to help keep their natural enthusiasm or expression of feelings from getting out of control. Young children enjoy a variety of small, colorful toys they can play with in bed or in their room or more elaborate play equipment, such as playhouses, sandboxes, rhythm instruments, and large boxes and blocks, that may be a part of the hospital playroom.

Fig. 26-9 Play materials for children in the hospital need to be appropriate for their age, interests, and limitations.
Games that can be played alone or with another child or an adult are popular with older children, as are puzzles; reading material; quiet individual activities such as sewing, stringing beads, and weaving; and Tinker-Toys, Lego blocks, and other building materials. Assembling models is an excellent pastime, and developmentally appropriate books are of infinite value to the child. Having someone read aloud provides hours of pleasure and is of special value to the child who has limited energy to expend in play.
Computers with access to the Internet are popular features in hospital playrooms and offer a window to the world for hospitalized children. A child can talk electronically with others and share experiences or even join a virtual support group. Today’s technology also provides the opportunity for children to explore every imaginable interest. As with television and other types of electronic entertainment, parents and nurses should monitor both the content and the time that a child spends engaging in these activities to avoid their becoming a substitute for social interaction or therapeutic play.
When supervising play for children who are ill or convalescing, it is best to select activities that are simpler than would normally be chosen according to the child’s developmental level. Children may not have the energy to cope with more challenging activities. Other limitations also influence the type of activities. Special consideration must be given to the child who has limited movement, has a restricted extremity, or is isolated. Toys for children on isolation must be disposable or be disinfected after use. For this reason stuffed animals are not recommended for use as community toys on a hospital unit.
Toys: Parents of hospitalized children often ask nurses about the types of toys that would be best to bring for their child. Most want to bring new ones to cheer and comfort the child and assuage their guilt regarding the child’s need for hospitalization. The nurse should tell the parents that, although wanting to provide these things for their child is natural, it is often better to wait to bring new things, especially for younger children. Small children need the comfort and reassurance of familiar things, such as the stuffed animal the child hugs for comfort and takes to bed at night. These are a link with home and the world outside the hospital. The nurse is responsible for assessing the safety of the toys brought to the child.
Large numbers of toys often confuse and frustrate a small child. A few small, well-chosen toys are usually preferred to one large, expensive one. Children who are hospitalized for an extended time benefit from changes. Rather than a confusing accumulation of toys, replace older toys periodically as interest wanes.
A highly successful diversion for a child who is hospitalized for a long time is a box with small, inexpensive, and brightly wrapped items with a different day of the week printed on the outside. The child will eagerly anticipate the time for opening each one. When the parents know when their next visit will be, they can provide the number of packages that corresponds to the days between visits. In this way the child knows that the diminishing packages also represent the anticipated visit from the parent.
Expressive Activities
Play provides one of the best opportunities for encouraging emotional expression, including the safe release of anger and hostility. Nondirective play that allows children freedom for expression can be therapeutic. Therapeutic play, however, should not be confused with the psychologic technique of play therapy. Play therapy is reserved for use by trained and qualified therapists who use the technique as an interpretative method with emotionally disturbed children. Therapeutic play, on the other hand, is an effective nondirective modality for helping children deal with their concerns and fears; at the same time, it often helps the nurse gain insights into their needs and feelings.
Tension release can be facilitated through almost any activity. With younger ambulatory children, large-muscle activity, such as the use of tricycles and wagons, is especially beneficial. Much aggression can be safely directed into games and activities that involve pounding and throwing. Beanbags are often thrown at a target or open receptacle with surprising vigor and hostility. A pounding board is employed with enthusiasm by young children; clay and play dough are beneficial at any age.
Creative Expression: Although all children derive physical, social, emotional, and cognitive benefits from engaging in art or other creative activities, children’s need for such activities increases when they are hospitalized. Drawing and painting are excellent media for expression (Fig. 26-10). Children are more at ease expressing their thoughts and feelings through art than through words. The child needs only the raw materials, such as crayons and paper. Children usually require little direction for self-expression; however, older children may be given some direction in what to paint or draw. Groups of children can enjoy this creative activity either working individually or collaborating on a group project such as a mural painted on a long piece of paper.
Although interpretation of children’s drawing requires special training, observing changes in a series of the child’s drawings over time can be helpful in assessing psychosocial adjustment and coping. The nurse can use children’s drawings, stories, poetry, and other products of creative expression as a springboard for discussion of thoughts, fears, and understanding of concepts or events. A child’s drawing before surgery or chemotherapy, for example, will often reveal unvoiced concerns about mutilation, body changes, and loss of self-control.
Holidays provide stimulus and direction for unlimited creative projects. Making pictures and decorations for their rooms gives the children a sense of pride and accomplishment. This is especially beneficial for immobilized and isolated children. Making gifts or decorations for someone at home helps maintain interpersonal ties.
Dramatic Play: Dramatic play is a well-recognized technique for emotional release, allowing children to reenact frightening or puzzling hospital experiences. Through use of puppets and replicas or actual hospital equipment, children can act out the situations that are a part of their hospital experience (Fig. 26-11). Dramatic play enables children to learn about procedures and events that are of concern to them and to assume the roles of the adults in the hospital environment.

Fig. 26-11 Playing with miniature hospital equipment allows children to explore feelings and concerns and achieve mastery over hospital situations. (Courtesy St. Louis Children’s Hospital.)
Puppets are particularly effective for communicating with children. Most young children view them as peers and readily communicate with them. Children will tell the puppet feelings that they would hesitate to express to adults. Puppets dressed to represent figures in the child’s environment (e.g., a physician, nurse, child patient, therapist, and members of the child’s own family) are especially useful. Small, appropriately attired dolls are also effective in encouraging the child to play out situations, although puppets are usually best for direct conversation.
Playing must accommodate medical needs, but at times a procedure can be postponed for a short time to allow the child to complete a special activity. Playing also must consider any limitations imposed by the child’s condition. For example, small children may eat paste and other creative media; therefore a child who is allergic to wheat should not be given finger paint made from wallpaper paste or play dough made with flour. A child with restricted salt intake should not play with modeling dough, since salt is one of its major components.*
Maximizing Potential Benefits of Hospitalization
Fostering Parent-Child Relationships
The crisis of illness or hospitalization can mobilize parents into more acute awareness of their child’s needs. For example, hospitalization provides opportunities for parents to learn more about their child’s growth and development. When parents understand children’s usual reactions to stress, such as regression or aggression, they not only are better able to support the child through the hospital experience, but also may extend their insight into childrearing practices after discharge.
Difficulties in parent-child relationships that may result in feeding problems, negative behavior, and enuresis may decrease during hospitalization. The temporary cessation of such problems sometimes alerts parents to the role they may be playing in propagating the negative behavior. With assistance from health professionals, parents can restructure ways of relating to their children to foster more positive behavior.
On occasion, hospitalization may represent a temporary reprieve or refuge from a disturbed home. Typically, abused or neglected children’s dramatic physical and social improvement during hospitalization is proof of the growth potential of this experience. Hospitalized children temporarily are able to seek support, reassurance, and security from new relationships, particularly with nurses and hospitalized peers.
Providing Educational Opportunities
School is an integral part of the school-age child’s and adolescent’s development. Accreditation standards for hospitals consider access to appropriate educational services when a child’s treatment requires a significant absence from school (Joint Commission on Accreditation of Healthcare Organizations, 2004). The nurse can encourage children to resume schoolwork as quickly as their condition permits, help them schedule and protect a selected time for studies, and help the family coordinate hospital educational services with their children’s schools. Children should have the opportunity to continue to progress through art and music classes, as well as their academic subjects.
Hospitalization also presents an excellent opportunity for children and other family members to learn more about their bodies, each other, and the health professions. For example, during a child’s admission for a diabetic crisis, the child may learn about the disease. The parents may also learn about the child’s needs for independence, normalcy, and appropriate limits. Each of them may find a new support system in the hospital staff.
Promoting Self-Mastery
The experience of facing a crisis such as illness or hospitalization, coping successfully with it, and maturing as a result of it constitutes an opportunity for self-mastery. Younger children have the chance to test out fantasy versus reality. They realize that they were not abandoned, mutilated, or punished. In fact, they were loved, cared for, and treated with respect for their individual concerns. It is not unusual for children who have undergone hospitalization or surgery to tell others that “it was nothing” or to proudly display their scars or bandages. For older children, hospitalization may represent an opportunity for decision making, independence, and self-reliance. They are proud of having survived the experience and may feel a genuine self-respect for their achievements. Nurses can facilitate such feelings of self-mastery by emphasizing aspects of personal competence in the child and not acknowledging uncooperative or negative behavior.
Providing Socialization
Hospitalization may offer children a special opportunity for social acceptance. Lonely, asocial, and even delinquent children find a sympathetic environment in the hospital. Children who have physical disabilities or are different in some other way from their peers may find an accepting social peer group. Although this does not always spontaneously occur, nurses can structure the environment to foster a supportive child group. For example, judicious selection of a roommate can help children gain a new friend and learn more about themselves. Forming relationships with significant members of the health care team, such as the physician, nurse, child life specialist, or social worker, can greatly enhance the child’s adjustment in many areas of life.
Parents may also encounter a new social group in other parents who have similar problems. They meet while in the hospital or clinic and discuss their children’s illnesses and treatment. Nurses can capitalize on this informal gathering by encouraging parents to discuss collectively their concerns and feelings. They can also refer parents to organized parent groups or can solicit the help and support of parents of recovered hospitalized patients. It is important that nurses emphasize that each child responds differently to certain aspects of the disease or treatment and that parents should clarify with a nurse or physician any questions or concerns raised in discussions with other parents. (See discussion of parent-to-parent support in Chapter 22.)
Supporting Family Members
Family-centered care is the focus of pediatric care because nursing care of children is not optimum unless the family as a whole is the designated patient. (See Family-Centered Care, Chapter 1.) Family-centered care supports the family by establishing the priority of their values and needs, developing collaborative relationships, and empowering the family unit (Lewandowski and Tesler, 2003).
Providing emotional support for family members involves the willingness to be present and listen to parents’ verbal and nonverbal messages. Sometimes the nurse does not give support directly. For example, the nurse may offer to stay with the child to allow the parents time alone or may discuss with other family members the parents’ need for relief. Extended family and friends may want to help but do not know how. The nurse can suggest baby-sitting, preparing meals, cleaning the house, doing laundry, or transporting the siblings to school and activities as ways to lessen the parents’ responsibilities. An ongoing parent support group held on the pediatric unit has also proved effective in helping parents share emotions and concerns related to hospitalization.
The clergy may also provide support. Parents with religious beliefs may appreciate the counsel of a clergy member, but because of their stress they may not have sufficient energy to initiate the contact. Nurses can be supportive by assessing spiritual needs, arranging for clergy to visit, and respecting and upholding parents’ religious beliefs (Feudtner, Haney, and Dimmers, 2003).
Support involves acceptance of cultural, socioeconomic, and ethnic values. For example, various ethnic groups define health and illness differently. For some, disorders that have few outward manifestations of illness, such as diabetes or cardiac problems, are not viewed as a sickness. Consequently, following a prescribed treatment may seem unnecessary. Nurses who appreciate the influences of culture are more likely to intervene therapeutically. (See Chapter 2 for an extensive discussion of cultural and religious influences on health care.)
Parents may need help in accepting their own feelings toward the ill child. If given the opportunity, parents often disclose their feelings of loss of control, anger, and guilt. They often resist admitting to such feelings because they expect others to disapprove of behavior that is less than perfect.
Providing Information
One of the most important nursing interventions is to provide information regarding (1) the disease, its treatment, and prognosis; (2) the child’s emotional and physical reaction to illness and hospitalization; and (3) the probable emotional reactions of family members to the crisis.
For many families the child’s illness is their first contact with hospitalization. Often parents are not prepared for the child’s behavioral reactions to hospitalization, such as separation anxiety, regression, aggression, and hostility. Providing the parents with information about these normal and expected behaviors can decrease the parents’ stress during the hospital admission. The family is equally unfamiliar with hospital rules, which often adds to their confusion and anxiety. Therefore the family needs clear explanations about what to expect and what is expected of them. Nurses can also help family members become more adept at seeking information about their child’s condition by asking questions that elicit meaningful information (see Nursing Care Guidelines box). In giving information, nurses need to be alert to information overload. Repetition can be helpful.
Parents also need to be aware of the effects of illness on the family and strategies that prevent negative changes. Specifically, parents should keep the family informed and communicating as much as possible. They should treat all the children as equally and as normally as before the illness. Discipline, which initially may be lessened for the ill child, should be continued to provide a measure of security and predictability. When ill children know that their parents expect certain standards of conduct from them, they feel certain they will recover. When all limits are removed, they fear that something catastrophic will happen.
Helping parents understand and accept the meaning of posthospitalization behaviors in the sick child is necessary for them to tolerate and support such behaviors. Consequently, the nurse should warn them of the common reactions following discharge. Parents who do not expect such reactions may misinterpret them as evidence of the child’s “being spoiled” and demand perfect behavior at a time when the child is still reacting to the stress of illness and hospitalization. If the behaviors, especially the demand for attention, are dealt with in a supportive manner, most children are able to relinquish them and assume precrisis levels of functioning.
Nurses should also prepare parents for some of the common reactions of siblings to the ill child—particularly anger, jealousy, and resentment. Older siblings may deny such reactions because they provoke guilt. However, everyone needs outlets for emotions, and the repressed feelings may surface as problems in school or with peers, as psychosomatic illnesses, or in delinquent behavior.
Probably one of the most neglected areas involves giving information to siblings. Age frequently becomes the primary factor that leads to an awareness of this need, since older children may begin to ask questions or request explanations. However, even in this situation the information may be seriously inadequate. Children in every age-group deserve some explanation of the child’s illness or hospitalization, preferably appropriate written information for older children. Although the exact wording may differ, the answer should focus on the following concerns: (1) Will I get sick and have to go to the hospital? (2) Did I cause the illness? (for actual or imagined reasons), and (3) Will my parents abandon me if my brother or sister does not recover? By addressing these three questions, parents or nurses can minimize the siblings’ fears of illness, guilt, and abandonment.
Nursing approaches with siblings can be direct or indirect. Direct services might include (1) incorporating siblings into hospital admission programs; (2) liberalizing visiting regulations; (3) extending parent participation programs to include sibling involvement, such as through family dining or group play sessions; and (4) developing programs designed specifically for siblings, such as group sessions to discuss their concerns or posthospital discharge visits to evaluate the siblings’ adjustment. Older siblings may not wish to attend a group; the nurse can be available for casual talks or for a tour, which may encourage the youngster to talk or ask questions (Lewandowski and Tesler, 2003).
Indirect services (which can be influenced by any existing nursing role) involve helping parents understand, cope with, and support the siblings’ reactions to the experience. Siblings do best with as little disruption in their lives as possible. Other interventions include helping well siblings maintain contact with the child who is hospitalized through telephone calls, recordings, letters, or postcards (see Family-Centered Care box).
Preparation for Hospitalization
![]() The rationale for preparing children for the hospital experience and related procedures is based on the principle that fear of the unknown exceeds fear of the known. Therefore decreasing the elements of the unknown results in less fear. When children do not have paralyzing fears to cope with, they can direct their energies toward dealing with the other unavoidable stresses of hospitalization and benefit optimally from the growth potential of the experience.
The rationale for preparing children for the hospital experience and related procedures is based on the principle that fear of the unknown exceeds fear of the known. Therefore decreasing the elements of the unknown results in less fear. When children do not have paralyzing fears to cope with, they can direct their energies toward dealing with the other unavoidable stresses of hospitalization and benefit optimally from the growth potential of the experience.
![]() Nursing Care Plan—The Child Undergoing Surgery
Nursing Care Plan—The Child Undergoing Surgery
For children past infancy and early toddlerhood, in-hospital or home preparation for hospitalization reduces their stress. Even when children are too young to benefit from direct preparation, parents benefit from prehospital counseling to lessen their fears and thus increase their ability to support the child psychologically. Prehospital counseling has two major goals:
1. To make the hospital less strange and frightening to parents and children
2. To establish a positive atmosphere and trusting relationship with hospital staff and family members
Although preparation may create stress for children initially, eventually the process results in greater trust in parents and staff, increased integration of information, and greater ability to cooperate and participate in treatment.
Guidelines in Preparing for Hospitalization
![]() Although preparation for hospitalization is a common practice, no universal standard or program is advocated in both general and children’s hospitals. Some hospital admission programs focus on group preparation before actual admission, whereas others prepare each child either before or the day of admission. The preparation process may include tours, puppet shows, or therapeutic play with toy or real medical equipment (Justus, Wyles, Wilson, et al, 2006). Other strategies for preparation include books, photograph albums, videos, or films; or it may be a simple description of the major aspects of a hospital stay. Ono, Oikawa, Hirabayashi, and colleagues (2008) developed a customized picture book that included a story of the operation day and the hospital stay plus a guidebook for parents. They found that the picture book played an important role in parent and child education at the time of day surgery.
Although preparation for hospitalization is a common practice, no universal standard or program is advocated in both general and children’s hospitals. Some hospital admission programs focus on group preparation before actual admission, whereas others prepare each child either before or the day of admission. The preparation process may include tours, puppet shows, or therapeutic play with toy or real medical equipment (Justus, Wyles, Wilson, et al, 2006). Other strategies for preparation include books, photograph albums, videos, or films; or it may be a simple description of the major aspects of a hospital stay. Ono, Oikawa, Hirabayashi, and colleagues (2008) developed a customized picture book that included a story of the operation day and the hospital stay plus a guidebook for parents. They found that the picture book played an important role in parent and child education at the time of day surgery.
![]() Skill—Preparing the Child for Surgery
Skill—Preparing the Child for Surgery
The primary audience of most hospital preparation programs is children and families who are experiencing an initial hospitalization. Subsequent readmissions, however, may also be stressful and anxiety provoking. Children’s fear and fantasies may not subside with repeated hospital stays but may intensify. Also, concerns change as children develop and grow. Older children need preparation as well, although the type of program needs to be individualized and may differ from the following guidelines for planning prehospital tours for groups or individual families who have not yet experienced hospital admission.
Ideally, preparatory procedures should be:
• Planned by hospital staff before the child’s admission to the hospital
• Appropriately designed for each child’s developmental age
• Sufficiently individualized to account for different children’s previous experience with hospitalization, present reason for admission, and available support system
Child life programs have become the standard in pediatric settings to address the psychosocial concerns precipitated by hospitalization and other health care experiences. Child life programs facilitate coping and the adjustment of children and families by presenting developmentally appropriate information about events and procedures, providing therapeutic play experiences, and establishing therapeutic relationships with children and parents to encourage and support family involvement in the children’s care (American Academy of Pediatrics, 2000). (In addition to the following discussion, the reader should review Preparation for Diagnostic and Therapeutic Procedures, Chapter 27.)
Group Size and Timing of Preparation
If group preparation is used, group size should be small (about 10 children) to provide individualized attention and facilitate discussion. If tours are arranged for each child, the parents and possibly the well siblings should be included.
Because standardized programs cannot adequately meet the needs of the full age range of pediatric patients, some hospitals have developed preparation programs that target a specific age-group, such as toddlers or adolescents. The length of the session should be suited to the children’s attention span: the younger the child, the shorter the program. The optimum approach is one that is individualized for each child and family.
Setting of the Tour
The hospital tour should avoid any frightening aspects of the environment and should typically include an inpatient room, the playroom (a highlight of the tour), the parents’ waiting room, the nurses’ station, and other special areas such as the group dining room. Other areas that may be visited are the radiology department and laboratory area, the preoperative area, and the recovery room. Different hospitals may tailor this tour to include special rooms, such as the “OR playroom,” where children and parents first go before anesthesia induction is administered. Children who are undergoing serious surgery requiring special postoperative care may be taken to visit the intensive care unit (ICU). Children scheduled for special tests, such as cardiac catheterization or cystoscopy, are sometimes shown these areas. Young children may respond better to shorter tours that concentrate on the areas of most concern, such as the pediatric unit, playroom, and recovery room. In any case, throughout the tour, the nurse (or other guide) must be alert to signs of concern or fear in the children. Strange noises, sights, sounds, and smells that are routine to hospital personnel can be frightening to children.
Preparatory Materials
The most suitable type of presentation for children includes a variety of preparatory materials, including films, lecture, demonstration, and play. The following discussion explores some of the typical methods used in preparing children for elective surgery.
A puppet show may reenact the basic steps of hospitalization: admission procedures, preparation for surgery, the operating and recovery rooms, and postsurgical treatment. Each scene focuses on concrete actions and models to familiarize family members with what will occur. The puppets talk about children’s common fears: pain, anesthesia, and parent separation. Although the sophistication of the materials varies, the basic characters should include a puppet family (mother, father, and child) and hospital staff (physician, nurse) that are ethnically representative of the patient and hospital population. For example, both African-American and Caucasian dolls are required in many areas. Hospital equipment includes mask, cap, gloves, gown, IV equipment, syringes, thermometer, blood pressure machine, stethoscope, scale, oxygen mask, suture removal set, bandages, bed, and sheets. If children are routinely admitted for diagnostic evaluations, miniature replicas of equipment (e.g., diagnostic imaging machines) or slides may be used as visual aids. The use of scaled-down models is especially beneficial for young children, who may be frightened by the actual proportions of some equipment. However, the intent of what is conveyed greatly surpasses the sophistication of the materials used.
Opportunity for Discussion
Any type of preparatory program needs to provide ample opportunity for discussion both before and after the tour. During the tour, encourage family members to ask questions and to familiarize themselves with the environment by sitting on a bed, using the electric bed controls, riding in a wheelchair, or handling the equipment in the special rooms. Ideally, the tour should also be an opportunity for meeting the child’s primary nurse. Although this is not always possible because of staffing schedules, the nursing staff should be introduced to the children by name. Introducing them to one specific nurse, such as the head nurse, clinical specialist, or nurse practitioner, helps them feel more comfortable in knowing who is available for questions or concerns during the hospital stay.
After the tour a question-and-answer period should be held in which the nurse is a participant. Sometimes the group is reticent about asking questions. In this case the nurse can stimulate discussion by posing a question to the audience or inviting the children to see and touch the puppets and equipment. Allowing children to play with the equipment and having them draw pictures about what they observed are excellent methods of evaluating the learning process and clarifying any misconceptions. The parents should also be encouraged to contact the appropriate provider before admission if questions or concerns arise.
Prehospital Counseling by Parents
In many situations the preparation of children for hospitalization is left up to parents. Parents may abandon this responsibility for a variety of reasons. For example, they sometimes think the child is too young to understand or is better off not knowing beforehand. Often they are unable to prepare the child because of their own lack of knowledge and understanding.
Professionals can help parents prepare their children by adequately informing them of the specific details of hospitalization and related procedures, through both direct discussion and written material. Nurses working with these parents should also assess their level of anxiety regarding the impending hospitalization. A parent who is at ease will convey that feeling to the child.
Hospital Admission Procedure
![]() The preparation that children require on the day of admission depends on their prehospital counseling. If they have been prepared in a formalized program, they usually know what to expect in terms of initial medical procedures, inpatient facilities, and nursing staff. However, prehospital counseling does not preclude the need for support during procedures such as drawing blood, x-ray tests, or physical examination. For example, undressing young children before they feel comfortable in their new surroundings can be upsetting. Causing needless anxiety and fear during admission may adversely affect the nurse’s establishment of trust with these children. Therefore nursing assistance during the admission procedure is vital, regardless of how well prepared any child is for the hospitalization. In addition, spending this time with the child gives the nurse an opportunity to evaluate understanding of subsequent procedures, such as surgery (Fig. 26-12). The usual admission procedures for children are outlined in the Nursing Care Guidelines box.
The preparation that children require on the day of admission depends on their prehospital counseling. If they have been prepared in a formalized program, they usually know what to expect in terms of initial medical procedures, inpatient facilities, and nursing staff. However, prehospital counseling does not preclude the need for support during procedures such as drawing blood, x-ray tests, or physical examination. For example, undressing young children before they feel comfortable in their new surroundings can be upsetting. Causing needless anxiety and fear during admission may adversely affect the nurse’s establishment of trust with these children. Therefore nursing assistance during the admission procedure is vital, regardless of how well prepared any child is for the hospitalization. In addition, spending this time with the child gives the nurse an opportunity to evaluate understanding of subsequent procedures, such as surgery (Fig. 26-12). The usual admission procedures for children are outlined in the Nursing Care Guidelines box.

Fig. 26-12 The initial admission procedures may be coordinated by a nurse practitioner who examines the child on admission. (Courtesy Paul Vincent Kuntz, Texas Children’s Hospital, Houston.)
![]() Skill—Admitting a Child to the Health Care System
Skill—Admitting a Child to the Health Care System
Nursing Admission History
The nursing admission history refers to a systematic collection of data about the child and family that allows the nurse to plan individualized care. The nursing admission history presented in Box 26-7 facilitates the formulation of nursing diagnoses. (See Nursing Diagnosis, Chapter 1.) One of the main purposes of the history is to assess the child’s usual health habits at home to promote a more normal environment in the hospital. Therefore questions related to activities of daily living are a major part of the assessment. The questions under the health perception–health management pattern are directed toward evaluation of the child’s preparation for hospitalization and are key factors in determining whether additional preparation is needed.
As with any history form, the questions are only guidelines; for optimum communication, nurses should ask these questions as a part of conversation, not as a direct questionnaire. Answers to questions that are broad and nonspecific, such as “What does your child know about this hospitalization?” need to be followed by more specific questions, such as “Tell me what you told him.” Children may respond to questions regarding their knowledge of hospitalization with statements such as “I don’t know why I am here.” Although this may be correct, frequently they have been given some explanation concerning the reason for hospitalization. Such an answer may mean that the explanation was inadequate, their anxiety blocked the recall, or they are testing out the explanation by prompting the nurse to supply additional information.
The nurse should also inquire about the use of any complementary or alternative medicine (CAM) practices. Results from the 2007 National Health Interview Survey found that approximately one in nine children (11.8%) used CAM in the past 12 months (Barnes, Bloom, and Nahin, 2009). The most commonly used therapies were nonvitamin, nonmineral, natural products (3.9%) and chiropractic or osteopathic manipulation (2.8%). Children whose parent used CAM were almost five times as likely (23.9%) to use CAM as children whose parent did not use CAM (5.1%). See the Complementary and Alternative Therapy box for other examples of CAM (see also Critical Thinking Exercise and Box 26-7).
Once the nurse has collected data as part of the nursing admission history, they must be applied to the nursing process and communicated to other staff. It makes little sense to assess a child’s home routine if none of this knowledge is integrated into the care plan. Most nursing units have provisions for care plans in which specific information about the child’s habits and needs are recorded.
Physical Assessment
Although physical examinations by practitioners are a required part of the admission procedure, nurses should also use the valuable information gained from physical assessments in their planning of care. (See Chapter 6.) Subjecting children to two separate examinations is unnecessary if the nurse and other practitioners cooperate during the procedure. For example, the nurse can also use the opportunity to observe the child’s body for any bruises, rashes, signs of neglect, deformities, or physical limitations. Collaboration also prevents the often frustrating and needless waste of the family’s time in repeating histories and examinations, especially when the child has a chronic condition that requires many hospitalizations.
The nurse should listen to the heart and lungs or do other target assessments pertinent to the illness or reason for hospitalization. It is impossible to evaluate improvement in respiratory function in a child admitted with pulmonary disease unless baseline data are available with which to compare subsequent findings.
Placing the Child
Room assignments are usually made before the child is admitted to the pediatric unit. The minimum considerations for room assignment are age, sex, and nature of the illness. Ideally, however, room selection should be based on a variety of developmental and psychobiologic needs. Determining compatible roommates, both for the children and for parents, greatly influences satisfaction with the hospital experience.
Although no absolute rules govern room selection, in general, placing children of the same age-group and with similar types of illness in the same room is both psychologically and medically advantageous (Fig. 26-13). However, there are many exceptions. For example, a child in traction may be therapeutic for another child confined to bed because of a serious illness. A child who is independent despite physical disabilities may help another child with limitations and the parents achieve deeper insight and acceptance of the disorder.
Adolescent Unit
To meet the unique needs of adolescents, hospitals have developed special units that provide privacy, increased socialization, and appropriate activities. Typically these units are set apart from the general pediatric facility so that the teenagers do not share space with younger children, who are often perceived as a threat to their maturity. These units also provide more flexible routines and activities, such as more group activity, provisions to leave the adolescent unit temporarily, and access to the items important to teenagers—telephones, computers, compact disc players, DVD players, video game systems, and televisions. Because adolescents’ food habits are rarely limited to three meals a day, a supply of snacks should be available. One of the most important benefits of these units is increased socialization with peers. In addition, many staff members enjoy working with this age-group and are well suited to establishing the trust that is essential for communication.
Despite the advantages of adolescent units, all young people require preparation for the experience. They need orientation to the unit, introduction to staff and other patients, and an atmosphere of warmth and welcome. Just as teenagers form cliques in normal social relationships, this also occurs in the hospital. Staff must be aware of exclusiveness of group membership, especially when new patients are admitted. Scheduled and supervised group meetings are effective in preventing feelings of “nonbelonging” and in facilitating introductions and new friendships. They also provide an excellent opportunity for discussions about typical adolescent concerns (e.g., sexuality, drugs, alcohol, parental relations) and special illness-related concerns of adolescents (e.g., peer rejection for being different).
Nursing Care During Special Hospital Situations
In addition to a general pediatric unit, children may be admitted to special facilities, such as an ambulatory/outpatient setting, an isolation room, or intensive care.
Ambulatory/Outpatient Setting
The ambulatory/outpatient setting provides needed medical services for the child without an overnight admission. Among the benefits of ambulatory/outpatient care are (1) minimization of the stressors of hospitalization, especially separation from the family; (2) reduced risk of infection; and (3) cost savings. Admission to the ambulatory/outpatient hospital setting usually is for surgical or diagnostic procedures, such as insertion of myringotomy tubes, hernia repair, adenoidectomy, tonsillectomy, cystoscopy, or bronchoscopy. In addition, improved outpatient care and treatment of chronic conditions have resulted in the need for fewer overnight hospitalizations.
In the ambulatory/outpatient setting, adequate preparation is particularly challenging. Ideally, the child and parents should receive preadmission preparation, including a tour of the facility and a review of the day’s events. Parents need information in advance to help prepare the child and themselves for surgery and enable them to care for the child at home after the procedure. Parents also appreciate suggestions for items to bring for the child’s trip home, such as blankets or stuffed animals. When preadmission preparation is not possible, allow time on the day of the procedure for children to become acquainted with their surroundings and for nurses to assess, plan, and implement appropriate teaching.
Waiting is practically inevitable in ambulatory/outpatient settings. Families often report waiting to be the most stressful part of the hospitalization experience. Providing a pager allows the family (and in many instances, the child) to leave the area and then be paged to return when needed. The need for creating a welcoming environment for children and families often may be overlooked in the ambulatory/outpatient setting, particularly in day surgery centers or settings that are not exclusively focused on pediatric patients. Toys, books, and other play materials should be available to children while they wait.
Explicit discharge instructions are important after outpatient surgery (see Family-Centered Care box). Parents need guidelines on when to call their practitioner regarding a change in the child’s condition. A telephone follow-up system allows nurses to check on the child’s progress within 48 to 72 hours after discharge. It provides an opportunity for the nurse to review discharge information and answer questions.
Isolation
Admission to an isolation room increases all the stressors typically associated with hospitalization. There is further separation from familiar persons; additional loss of control; and added environmental changes, such as sensory deprivation and the strange appearance of visitors. Isolation also affects orientation to time and place. These stressors are compounded by children’s limited understanding of isolation. Preschool children have difficulty understanding the rationale for isolation because they cannot comprehend the cause-and-effect relationship between germs and illness. They are likely to view isolation as punishment. Older children understand the causality better but still require information to decrease fantasizing or misinterpretation.
When a child is placed in isolation, preparation is essential for the child to feel in control. With young children, the best approach is a simple explanation, such as “You need to be in this room to help you get better. This is a special place to make all the germs go away. The germs made you sick, and you could not help that.”
All children, but especially younger ones, need preparation in terms of what they will see, hear, or feel in isolation. Therefore the nurse should show them the mask, gloves, and gown and encourage them to “dress up” in them. Playing with the strange apparel lessens the fear of seeing “ghostlike” people walk into the room. Before entering the room, nurses and other health personnel should introduce themselves and let the child see their face before donning a mask. In this way the child associates them with tangible features and gains a sense of familiarity in an otherwise strange and lonely environment.
When the child’s condition improves, provide appropriate play activities to minimize boredom, stimulate the senses, provide a real or perceived sense of movement, orient the child to time and place, provide social interaction, and reduce depersonalization. For example, the environment can be manipulated to increase sensory freedom by moving the bed toward the door or window. Opening window shades; providing musical, visual, or tactile toys; and increasing interpersonal contact can substitute mental mobility for the limitations of physical movement. Rather than dwelling on the negative aspects of isolation, encourage the child to view this experience as challenging and positive. For example, the nurse can help the child look at isolation as a method of keeping others out and letting only special people in. Children often think of intriguing signs for their doors, such as “Enter at your own risk.” These signs also encourage people “on the outside” to talk with the child about the ominous greeting.
Emergency Admission
One of the most traumatic hospital experiences for the child and parents is an emergency admission. A sudden illness or injury leaves little time for preparation and explanation. Sometimes the emergency admission is compounded by admission to an ICU or the need for immediate surgery. However, even in those instances requiring only outpatient treatment, the child is exposed to a strange, frightening environment and to experiences that may elicit fear or cause pain. Thus every medical emergency requires psychologic intervention to reduce the fear and anxiety frequently associated with the experience. Child life specialists are essential to provide teaching and support in these situations.
There is often a wide discrepancy between what constitutes a medically defined emergency and a client-defined emergency. A growing concern is the use of major emergency departments for routine primary care health visits. To offset overcrowding in emergency departments, many facilities have minor emergency units or pediatric minor emergency units for after-hours health care. Telephone triage for minor illnesses for patients is also emerging as a health care delivery mode to distinguish illnesses such as common cold from true life-threatening conditions that require immediate practitioner attention and intervention. Other factors contributing to the overuse of emergency departments (as opposed to the primary practitioner’s office) include the increasing number of uninsured persons and households where both parents work full time and cannot afford to take off during the daytime to take the sick child to a practitioner.
In pediatric populations, most visits are for respiratory tract infections, skin conditions, gastrointestinal disorders, and trauma. The most common reason parents give for bringing the child to the emergency department is concern about the illness worsening. However, practitioners may not consider the progressive symptoms as necessitating immediate or emergency care. One of the nurse’s primary goals is to assess the parents’ perception of the event and their reasons for considering it serious or life threatening.
Lengthy preparatory admission procedures are often inappropriate for emergency situations. In such instances, nurses must focus their nursing interventions on the essential components of admission counseling (see Nursing Care Guidelines box, p. 987) and complete the process as soon as the child’s condition is stabilized.
Unless an emergency is life threatening, children need to participate in their care to maintain a sense of control. Because emergency departments are frequently hectic, staff has a tendency to rush through procedures to save time. However, the extra few minutes needed to allow children to participate may save many more minutes of useless resistance and uncooperativeness during subsequent procedures. Other supportive measures include ensuring privacy, accepting various emotional responses to fear or pain, preserving parent-child contact, explaining all events before or as they occur, and remaining calm.
At times, because of the child’s physical condition, little or no preparatory counseling for emergency hospitalization can be done. In such situations, counseling after the event has therapeutic value. The process involves evaluating children’s thoughts regarding admission and related procedures. It is similar to precounseling techniques; however, instead of supplying information, the nurse listens to the child’s explanations. Projective techniques such as drawing, doll play, or storytelling are especially effective. The nurse then bases additional teaching on what has already been learned.
Intensive Care Unit
Admission to an ICU can be traumatic for both the child and parents (Fig. 26-14). The nature and severity of the illness, the circumstances surrounding the admission, and the highly technologic, unfamiliar environment are major factors, especially for parents. Parents experience significantly more stress when the admission is unexpected rather than expected. Nurses can assist with coping by asking parents to identify stressors and implement appropriate interventions. Assessment should be repeated periodically to account for changes in perceptions over time. The use of daily patient goal sheets has been successful in improving communication among health care providers caring for children in the ICU (Agarwal, Frankel, Tourner, et al, 2008; Phipps and Thomas, 2007). By clearly defining daily patient care goals, health care providers believed that care was improved.

Fig. 26-14 Parents should be encouraged to be actively involved when their infant is critically ill and requires care in an intensive care unit. (Courtesy E. Jacob, Texas Children’s Hospital, Houston.)
In a qualitative study of 19 parents of 10 children in the ICU, parents reported that they wanted nurses to nurture the child in ICU as the family would (Harbaugh, Tomlinson, and Kirschbaum, 2004). Nurse behaviors that exemplified affection, caring, watching, and protecting were perceived as helpful in decreasing stress and maintaining the family unit during the crisis of hospitalization. Nurse behaviors perceived as not helpful to the family included giving care without appearing to care, separating parents from the child, excluding parents from decision making, and communicating poorly with parents.
The family’s emotional needs are paramount when a child is admitted to an ICU. Although the same interventions discussed earlier for separation anxiety, loss of control, and bodily injury and pain apply here, additional interventions may also benefit the family and child (see Nursing Care Guidelines box, p. 987, and Family-Centered Care box). Critical care must be family centered.
Critically ill children become the focus of the parents’ lives, and the parents’ need for information regarding their child is paramount. They want to know if their child will live and, if so, whether the child will be the same as before. They need to know why various interventions are being done for the child, that the child is being treated for pain or is comfortable, and that the child may be able to hear them even though the child is not awake.
When an ICU admission is planned (e.g., postoperative care after cardiac surgery), the child and parents should be prepared for the admission. Some units advocate a tour, whereas others use picture books of the unit to familiarize the family with the environment and usual equipment. Nurses can use dolls to demonstrate the equipment, types of tubes, and dressings that the child may have.
A major stressor for parents of a child in the ICU is the child’s appearance (Latour, van Goudoever, and Hazelzet, 2008). When parents first visit the child in the ICU, they need preparation about the appearance of the child. Ideally, the nurse should accompany the family to the bedside to provide emotional support and answer any questions. If siblings visit, they need the same preparation as parents. Whether they should visit soon after the child is admitted or after the child’s condition has stabilized is controversial. Early visiting minimizes the opportunity for siblings to fantasize about the experience and imagine the situation is worse than it actually is. However, early visiting may be frightening, especially when the patient is in pain or unresponsive and attached to numerous tubes and equipment. If there is a concern that the child may not survive the illness, however, an early visit may be the only option. The length of time for sibling visitation should be planned ahead and monitored during the visit to prevent the well child from becoming overwhelmed.
Children admitted to the ICU need their parents’ comfort and security, and nurses should encourage parents to stay with their child. If visiting hours are limited, the schedule should be flexible to accommodate parental needs. Family members should be given a schedule of the visiting times permitted and assured that they can call the unit at any time. With liberalization of visiting hours, many parents think they must stay with their child. Nurses need to be sensitive to parental needs, suggesting periodic respites from the stressful ICU environment.
Because altered parental roles are a major stress for parents, nurses need to implement interventions to minimize this concern, such as (1) educating and preparing parents for the expected role changes; (2) identifying ways in which parents can continue to fulfill parenting functions, such as helping with the bath or feeding, touching, and talking to the child; and (3) determining new roles, such as helping with procedures. Information sharing can increase parents’ sense of control and responsibility, but facts must be conveyed simply and repeated often, with care taken to avoid overwhelming family members. Because medical jargon is used frequently in a complex environment such as the ICU, unfamiliar terms need to be clarified and simpler terms substituted. (See Nursing Care Guidelines boxes under Psychologic Preparation, Chapter 27.)
As in emergency admissions, there is a tendency in the ICU to perform procedures quickly and without attention to the child’s preparational needs. Therefore nurses need to remember the special concerns about bodily injury of children in each age-group. Explaining each procedure, altering it whenever possible to decrease the child’s fears, and supporting the child are essential. Giving children an object that symbolizes their coping, such as a “hero badge” or an “ICU diploma,” provides a positive memento of an otherwise stressful experience. Depending on the numerous procedures performed on the child and the nature of the illness, pain management needs to receive a high priority.
Of particular importance in decreasing fear is ensuring that discussions that do not directly include the family are held where the child and family cannot overhear them. Casual conversation in the nursing station or in the halls can often be overheard and taken out of context. When discussions are held at the bedside, it is easy to forget the patient and make remarks that are misunderstood. Usually a quiet reminder of how frightened the child can become from listening to these discussions is sufficient. If bedside conferences are necessary, the nurse interprets them for family members in words they can comprehend.
Extensive monitoring makes a usual day-night cycle difficult in an ICU. However, some schedule should be established that is similar to daily events in the child’s life. These include organizing care during normal waking hours; keeping regular bedtime schedules, including quiet times when televisions and radios are lowered or turned off; closing and opening drapes as appropriate; dimming lights; placing a curtain around the bed for privacy and decreased stimulation; and having clocks or calendars in easy view for older children. In particular, staff members must realize the need for quiet and refrain from loud talking or laughing. Equipment noise should be kept to a minimum by turning alarms as low as safely possible, scheduling nursing care in blocks of time to minimize interruptions, turning off bedside equipment not in use (e.g., suction, oxygen), and avoiding loud, abrupt noises. Such measures can reduce the sensory overload and the sleep deprivation commonly associated with ICU admissions.
Provide play opportunities for every child. Although children who are critically ill may be unable to initiate spontaneous play, others (e.g., nurse, social worker, child life specialist, parent, sibling) can structure play interactions in which children watch and direct the person who plays for them.
Despite the stresses normally associated with ICU admission, a special security develops from being carefully monitored and receiving individualized care. Therefore planning for transition to the regular unit is essential and should include (1) assignment of a primary nurse on the regular unit who visits before the transfer; (2) continued visits by the ICU staff to assess the child’s and parents’ adjustment and to act as a temporary liaison with the nursing staff; (3) explanation of the differences between the two units and the rationale for the change to less intense monitoring of the child’s physical condition; and (4) selection of an appropriate room, such as one close to the nursing station, and a compatible roommate. In one study of parents whose children were being transferred from the ICU to the regular pediatric unit, parents who received a transfer preparation letter and verbal explanation of the process had significantly lower anxiety scores than parents who did not receive this information (Bouve, Roozmus, and Giordano, 1999).
Discharge Planning and Home Care
![]() Most hospitalizations necessitate some type of discharge planning. Often this involves education of the family for continued care and follow-up in the home. Depending on the diagnosis, this may be relatively simple or complex. With the current concern for cost containment and recognition of children’s emotional needs, home care for children with technologically complex care, such as ventilators, has become increasingly common. Preparing the family for home care demands a high degree of competence in planning and implementing discharge instruction. (See Chapter 25.) Adequate preparation for optimal home care includes an interdisciplinary approach, with all members of the health care team working together with the patient and family.
Most hospitalizations necessitate some type of discharge planning. Often this involves education of the family for continued care and follow-up in the home. Depending on the diagnosis, this may be relatively simple or complex. With the current concern for cost containment and recognition of children’s emotional needs, home care for children with technologically complex care, such as ventilators, has become increasingly common. Preparing the family for home care demands a high degree of competence in planning and implementing discharge instruction. (See Chapter 25.) Adequate preparation for optimal home care includes an interdisciplinary approach, with all members of the health care team working together with the patient and family.
![]() Critical Thinking Exercise—Discharge Planning
Critical Thinking Exercise—Discharge Planning
Nurses are often key individuals in initiating the discharge process and collaborating with others in planning and implementation. Although it is not possible to discuss all the details needed for effective discharge planning and home care, this section presents a brief overview of the more critical aspects. More specific details are discussed throughout the text for conditions such as home apnea monitoring, tracheostomy care, or total parenteral nutrition, and numerous sources of information exist in the literature.
Assessment
Discharge planning for home care must begin with an assessment of the family’s desires and capability in assuming care responsibilities. Ideally, at least two individuals should be committed to learning the skills needed for home care. The family should participate in a thorough assessment of their needs and the home environment to ensure that their emotional and physical resources are sufficient to manage the tasks of home care. (For a discussion of family and home assessment strategies, see Chapters 22 and 25.) In addition to adequate family resources, an investigation of community services is needed to ensure that appropriate support agencies are available, such as emergency facilities, respite care, home health agencies, and equipment vendors. To coordinate the immense task of assessment and to plan implementation, a discharge planning coordinator should be appointed early in the process.
Planning
Ideally, preparation for hospital discharge and home care begins during the admission assessment with the establishment of short- and long-term goals. These goals are concerned with the child’s physical needs and the psychologic needs of the child and family. For children who require complex care, discharge planning focuses on obtaining appropriate equipment and health care personnel for the home and on the skills that parents or children are expected to continue at home. In planning appropriate teaching, nurses need to assess (1) the actual and perceived complexity of the skill, (2) the parents’ or child’s ability to learn the skill, and (3) the parents’ or child’s previous or present experience with such procedures. (See Compliance, Chapter 27, for guidelines for effective teaching.)
The teaching plan should incorporate levels of learning, such as observing, participating with assistance, and a return demonstration of the skill. Each skill should be divided into discrete steps, and each step taught to the family member. Return demonstration of the skill should be requested before introducing new skills. A record of teaching and performance provides an efficient checklist for evaluation. Before leaving the hospital, all families should receive detailed written instructions about home care and telephone numbers should they require assistance.
Transitional Care
Once the family is competent in performing required skills, they should be given responsibility for the care. Whenever possible, the family should have a transition or trial period to assume care with minimum supervision. This may be arranged on the unit, during a home pass, or in a facility (e.g., a motel or Ronald McDonald House) near the hospital. Some programs incorporate a hospital trial into their discharge criteria, necessitating that the family successfully manage this phase before discharge to home. Such transitions provide a safe practice period for the family, with assistance readily available when needed, and are especially valuable when the family lives far from the hospital.
Evaluation and Continuing Support
Evaluation is a critical part of any discharge plan and assumes even more importance in home care of children with complex needs. Factors to consider in home care planning include need for subsequent hospitalization, child’s developmental and physical progress, effects of home care on the family, actual versus expected use of resources by the family and home care team, and financial costs and savings.
In most instances parents need only simple instructions and understanding of follow-up care. However, the often overwhelming care assumed by some families necessitates continued professional support after discharge. A follow-up home visit or telephone call gives the nurse an opportunity to individualize care and provide information in perhaps a less stressful learning environment than the hospital; this may be coordinated with home health care providers for a smooth transition to home. Appropriate referrals and resources may include visiting nurse or home health agencies, private nurse services, the school system, physical therapist, mental health counselor, social worker, and various community agencies, including special organizations. Sharing the important issues surrounding the child’s and family’s needs is essential. Referral summaries should be concise, specific, and factual. When numerous support services are involved, periodic collaboration among the professionals (interdisciplinary conferences) and the family is an excellent strategy to ensure efficient implementation and comprehensive delivery of services.
Key Points
• Children are particularly vulnerable to the stresses of illness and hospitalization because stress represents a change from the usual state of health and routine and because they possess limited coping mechanisms.
• The three phases of separation anxiety are protest, despair, and detachment.
• Feelings of loss of control are caused by unfamiliar environmental stimuli, physical restriction, altered routine, and dependency.
• Fear of pain may be manifested in the following ways: infants—facial expressions, body movements; toddlers—intense emotional upset, physical resistance; preschoolers—aggression, verbal expression, dependency; school-age children—precise verbalization of pain, passive requests for support or help, procrastination technique; adolescents—self-control, irritability, limited movement.
• Because of their separation from significant people, children who are hospitalized may lack the opportunity to form new attachments in the strange environment and may exhibit negative behaviors after discharge.
• Family reactions are influenced by the seriousness of illness, experience with illness or hospitalization, diagnostic or therapeutic procedures, available support systems, personal ego strengths, coping abilities, additional stresses, cultural and religious beliefs, and family communication patterns.
• The following factors increase the negative effects of a brother’s or sister’s illness or hospitalization on siblings: fear of contracting the illness, their age, a close relationship with the ill sibling, substitute child care, minimum explanation of the illness, and perceived changes in parenting.
• Nursing care of children who are hospitalized is aimed at preventing or minimizing separation, decreasing loss of control, minimizing bodily injury and pain, using play and other expressive activities to lessen stress, maximizing potential benefits of hospitalization, and supporting family members.
• The child life specialist plays an important role in using play and other expressive activities as effective tools in minimizing stress.
• The nurse can maximize potential benefits of hospitalization by fostering parent-child relations, providing educational opportunities, promoting self-mastery, and encouraging socialization.
• Supporting family members involves listening to parents’ verbal and nonverbal messages; providing social and spiritual support; accepting cultural, socioeconomic, and ethnic values; and giving information to families and siblings.
• The major goals of prehospital counseling are to make the hospital less strange and frightening to parents and children and to establish a positive atmosphere and trusting relationships with staff and family members.
• In preparing families for hospitalization, the nurse should consider small group size and timing of the event, setting of the tour, inclusion of preparatory materials, time for discussion, and prehospital counseling for parents.
• Emergency admission or admission to an ambulatory/outpatient setting, isolation room, or ICU requires additional intervention strategies to meet the child’s and family’s needs.
Answers to Critical Thinking Exercises
Playroom and Hospital Procedures
1. There is sufficient evidence regarding this incident to draw some conclusions.
2. a. Regardless of how minor a procedure such as a venipuncture may seem to an adult health care worker, it represents a major threat to a child. One must consider the child’s age, illness, developmental level, and previous experiences with venipuncture.
b. Play is an important function of childhood whether the child is sick or well. Through play children may act out fears, concerns, anger, and other emotions that they may not feel comfortable expressing to adults in a confrontational manner. Play is an important part of the hospitalized child’s life, and it is a vehicle for promoting optimum development.
c. It is important to have the blood drawn so Dr. Lung may plan a therapeutic regimen; however, there appears to have been no advance preparation of the child’s skin to minimize or prevent pain from the procedure. Regardless of the phlebotomist’s skill in performing the procedure, it is also important to consider that the negative repercussions of performing the procedure at this point may outweigh the benefits.
d. All staff on the pediatric floor must agree about respecting the child’s personal space in the playroom and must adhere to unit policies or rules so that respect is maintained. Failure to respect the child’s space may engender further fear in other children who perceive that the playroom is not a safe place after all when certain procedures need to be done. The fear of having other procedures performed in the playroom may prevent children from going there to participate in therapeutic and interactive play.
3. It is important to maintain a fair balance between therapeutic management of illness and childhood recreation. It would be appropriate in this situation to intervene and ask the phlebotomist to return in 30 minutes to an hour and indicate that the child will be ready for the venipuncture in the treatment room at that time. It is important to stress that the playroom is off-limits for procedures. It would be appropriate to discuss this plan with Hannah, indicating that the procedure will be performed at the designated time. It is also important to explore pain management issues with Hannah and her parent: does she usually use EMLA (lidocaine-prilocaine) or another topical remedy to prevent pain at the site? If so, it will be necessary to make such arrangements in advance, possibly now, so her pain is managed appropriately. As the nurse, it is appropriate to discuss a delay in obtaining the laboratory results with Dr. Lung and the reasons for the delay. Medical and nursing staff on the pediatric floor must communicate effectively. Should this arrangement not suit Dr. Lung’s time frame for accomplishing certain tasks, one might suggest a trade-off. The nurse could draw the blood in the treatment room once preparations are made and Hannah agrees to a time. Remember, however, that school-age children are prone to bargain for more time to delay or prevent the event, since it is painful. One must be gently firm about the agreed-on time of the procedure and not allow further delays.
Even if one accepts the conclusion that it is okay with Hannah to have blood drawn in the playroom, it is important to consider the possible negative implications for the other children in the room, who may be confused about even a simple procedure (e.g., checking blood pressure) or the sanctuary status of the playroom. Proceeding with the blood draw in the playroom would violate the child’s trust about what adult health care workers say regarding the purpose of the playroom as a sanctuary from painful procedures. Such action would likely result in less cooperation from the children who are present and may also make other parents who are present, or who hear about the incident, wonder about the staff’s sincerity. Interrupting the children’s game is not necessary, since this does not represent a life-threatening situation.
4. Yes. There is sufficient evidence to support these decisions and the plan of action.
Complementary and Alternative Medicine
1. There is limited evidence to draw certain conclusions without obtaining more data from the parents. It would be appropriate to gather more information before jumping to any major conclusions at this time.
2. a. Complementary and alternative medicine (CAM) is more common in U.S. households than previously reported. Much of the concern surrounding complementary therapies, especially in children, is the lack of sufficient data regarding their effectiveness, benefit, and potential harm that may occur as a result of such treatments. In some cases CAM therapies may counteract certain medications or the effects of prescribed therapies. It has become more common for practitioners in emergency medicine to encounter patients who are taking CAM therapy in addition to prescription medications or treatments for conditions such as eczema, asthma, colds, and upper respiratory tract problems.
b. Folk remedies are common among certain ethnic groups and subgroups in the United States. Many are based on traditional family remedies that have been proved neither effective nor harmful. However, a few remedies could be potentially harmful, especially to children, by counteracting the effects of prescribed treatments that are known to be effective; some remedies’ ingredients may be toxic to children.
c. The nurse’s role in such cases is to gather sufficient data from the family about the practice, discuss the treatment (CAM) in a nonjudgmental manner, and be cognizant of the effects of the treatment on the child’s current health status and potential effects on other medical treatment regimens.
3. Give the family their penny and open a dialogue about the traditional practice they are using. Gather additional information in a nonjudgmental manner; the discussion should center on the family’s traditional beliefs regarding the practices, the prescribed medical regimen, and whether there is conflict or potential for harm. There is no need to stop the treatment unless potential harm to the child may occur. A discussion with the primary practitioner regarding the use of CAM for Maria should ensue, followed by a discussion with the entire family if necessary.
The contents of the bottle will likely be revealed during the discussion with the family. It is important to respect the family’s wishes regarding traditional folk or CAM rituals, yet remain mindful of potential harmful effects on the child. It is not likely that telling the family to stop the ritual will have much success, since these beliefs are deeply ingrained into cultural, religious, and medical practice; the family may continue the ritual at home on discharge and further disregard other instructions for care should the nursing and medical staff adopt a confrontational approach. The important concept for the staff and family to focus on is the ultimate well-being of the child.
What you have probably observed is Santeria, the African-Caribbean religion that was brought to the New World by slaves from West Africa. It is common among immigrants from Cuba, Puerto Rico, Brazil, and Santo Domingo; a majority of Latin immigrants will probably have contact with Santeria sometime in their lives.
4. As yet, there is insufficient evidence to indicate that harm is being done by the CAM ritual. Further data need to be gathered and then a decision made about further discussion of the CAM practice.
References
Agarwal, S, Frankel, L, Tourner, S, et al. Improving communication in a pediatric intensive care unit using daily patient goal sheets. J Crit Care. 2008;23(2):227–235.
American Academy of Pediatrics, Committee on Hospital Care. Child life services. Pediatrics. 2006;118(4):1757–1763.
American Academy of Pediatrics. Family centered care and the pediatrician’s role policy statement. Pediatrics. 2003;112(3):691–696.
American Academy of Pediatrics, Committee on Hospital Care. Child life services. Pediatrics. 2000;106(5):1156–1159.
Anand, KJ, Scalzo, FM. Can adverse neonatal experiences alter brain development and subsequent behavior? Biol Neonate. 2000;77(2):69–82.
Anderson, CD, Mangino, RR. Nurse shift report: who says you can’t talk in front of the patient? Nurs Adm Q. 2006;30(2):112–122.
Barnes, PM, Bloom, B, Nahin, RL. Complementary and alternative medicine use among adults and children: United States 2007. Natl Health Stat Report. 2009;10(12):1–23.
Bouve, LR, Roozmus, CL, Giordano, P. Preparing parents for their child’s transfer from the PICU to the pediatric floor. Appl Nurs Res. 1999;12(3):114–120.
Brewer, S, Gleditsch, SL, Syblik, D, et al. Pediatric anxiety: child life intervention in day surgery. J Pediatr Nurs. 2006;21(1):13–22.
Caffin, CL, Linton, S, Pellegrini, J. Introduction of a liaison nurse role in a tertiary paediatric ICU. Intensive Crit Care Nurs. 2007;23(4):226–233.
Conway, J, Johnson, BH, Edgman-Levitan, S, et al. Partnering with patients and families to design a patient- and family-centered health care system: a roadmap for the future—a work in progress. Institute for Family-Centered Care and Institute for Healthcare Improvement, available at www.familycenteredcare.org/pdf/Roadmap.pdf, 2006. [(accessed June 26, 2009].
Craft, MJ. Siblings of hospitalized children: assessment and intervention. J Pediatr Nurs. 1993;8(5):289–297.
Feudtner, C, Haney, J, Dimmers, MA. Spiritual care needs of hospitalized children and their families: a national survey of pastoral care providers’ perceptions. Pediatrics. 2003;111(1):e67–e72.
Franck, LS, Greenberg, CS, Stevens, B. Pain assessment in infants and children. Pediatr Clin North Am. 2000;47:487–512.
Gaynard, L, Wolfer, J, Goldberger, J, et al. Psychosocial care of children in hospitals. Bethesda, Md: Association for the Care of Children’s Health; 1990.
Harbaugh, BL, Tomlinson, PS, Kirschbaum, M. Parents’ perceptions of nurses’ caregiving behaviors in the pediatric intensive care unit. Issues Compr Pediatr Nurs. 2004;27(3):163–177.
Hopia, H, Tomlinson, PS, Paavilainen, E, et al. Child in hospital: family experiences and expectations of how nurses can promote family health. J Clin Nurs. 2005;14(2):212–222.
Institute of Medicine, Committee on Quality of Healthcare in America. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academy Press; 2001.
Joint Commission on Accreditation of Healthcare Organizations. Comprehensive accreditation manual for hospitals. Oakbrook Terrace, Ill: The Commission; 2004.
Justus, R, Wyles, D, Wilson, J, et al. Preparing children and families for surgery: Mount Sinai’s multidisciplinary perspective. Pediatr Nurs. 2006;32(1):35–43.
Latour, JM, van Goudoever, JB, Hazelzet, JA. Parent satisfaction in the pediatric ICU. Pediatr Clin North Am. 2008;55(3):779–790.
Lewandowski, LA, Tesler, MD. Family-centered care: putting it into action. Washington, DC: American Nurses Association; 2003.
Melnyk, BM. Intervention studies involving parents of hospitalized young children: an analysis of the past and future recommendations. J Pediatr Nurs. 2000;15(1):4–13.
Miceli, PJ, Clark, PA. Your patient—my child: seven priorities for improving pediatric care from the parent’s perspective. J Nurs Care Qual. 2005;20(1):43–53.
National Association of Children’s Hospitals and Related Institutions. Pediatric excellence in healthcare delivery systems, 1996. available at www.childrenshospitals.net/AM/Template.cfm?Section=Search3§ion=Reports1&template=/CM/ContentDisplay.cfm&ContentFileID=7629. [(accessed July 27, 2009)].
Newton, MS. Family-centered care: current realities in parent participation. Pediatr Nurs. 2000;26(2):164–168.
Ono, S, Oikawa, I, Hirabayashi, Y, et al. Preparation of a picture book to support parents and autonomy in preschool children facing day surgery. Pediatr Nurs. 2008;34(1):82–83. [88].
Orem, D. Nursing concepts of practice, ed 6. St Louis: Elsevier; 2001.
Phipps, LM, Thomas, NJ. Hepatitis C: the use of a daily goals sheet to improve communication in the paediatric intensive care unit. Intensive Crit Care Nurs. 2007;23(5):264–271.
Small, L. Early predictors of poor coping outcomes in children following intensive care hospitalization and stressful medical encounters. Pediatr Nurs. 2002;28(4):393–401.
Smith, T, Conant Rees, HL. Making family-centered care a reality. Semin Nurs Manage. 2000;8(3):136–142.
Stratton, KM. Parents’ experiences of their child’s care during hospitalization. J Cult Divers. 2004;11(1):4–11.
Taddio, A, Katz, J. The effects of early pain experience in neonates on pain responses in infancy and childhood. Pediatr Drugs. 2005;7(4):245–257.
Taddio, A, Shah, V, Gilbert-MacLeod, C, et al. Conditioning and hyperalgesia in newborns exposed to repeated heel lances. JAMA. 2002;288(7):857–861.
Thompson, R. The handbook of child life: A guide for pediatric psychosocial care. Springfield, Ill: Charles C Thomas; 2009.
Thompson, R, Stanford, G. Child life in hospitals: Theory and practice. Springfield, Ill: Charles C Thomas; 1981.
Wilson, ME, Megel, ME, Enenbach, L, et al. The voices of children: stories about hospitalization. J Pediatr Health Care. 2010;24(2):95–102.