Diagnostic Evaluation
The diagnosis of MCNS in children is based on the history and clinical manifestations (edema, proteinuria, hypoalbuminemia, and hypercholesterolemia in the absence of significant hematuria and hypertension) (Ruth, Kemper, Leumann, et al, 2005). Massive proteinuria is reflected in urinary excretion of protein that often reaches levels in excess of 2 g/m2 of body surface/day, with relatively greater clearance of low-molecular-weight proteins. Hyaline casts from high protein levels and sluggish flow and oval fat bodies, as well as a few red blood cells, can be found in the urine of most affected children, although there is seldom gross hematuria. Specific gravity is high and proportionate to the amount of protein concentration. If hypovolemia is not significant and the child is well hydrated, the glomerular filtration rate is usually normal.
Total serum protein concentrations are reduced, with the albumin fractions significantly reduced (<2 g/dl) and plasma lipids elevated. Serum cholesterol may be as high as 450 to 1500 mg/dl. Hemoglobin and hematocrit are usually normal or elevated, and the platelet count is high (500,000 to 1,000,000/mm3) as a result of hemoconcentration. Serum sodium concentration is usually low, approximately 130 to 135 mEq/L.
If renal biopsy is performed, it provides information regarding the glomerular status and type of nephrotic syndrome, the likely response to drugs, and the probable course of the disease. Under the microscope the foot processes of the basement membrane appear fused. The major focuses in differential diagnosis are to establish the edema as renal in origin and to distinguish MCNS from other glomerulopathies with nephrotic syndrome as a manifestation.
Therapeutic Management
Medical management consists of both general and specific measures. The primary objective is to reduce the excretion of urinary protein and maintain protein-free urine. Additional objectives include prevention or treatment of acute infection, control of edema, establishment of good nutrition, and readjustment of any disturbed metabolic processes. Children with severe symptoms may be hospitalized for assessment and observation for evidence of infection, response to therapy, and parental education.
General Measures: General treatment is principally supportive. During the edema phase the child is often limited to quiet activities, but activity is not restricted during remission. Children can be remarkably active; there is no evidence that restriction affects the ultimate outcome. Acute and intercurrent infections are treated with appropriate antibiotics, and providers make efforts to minimize the risk of infection.
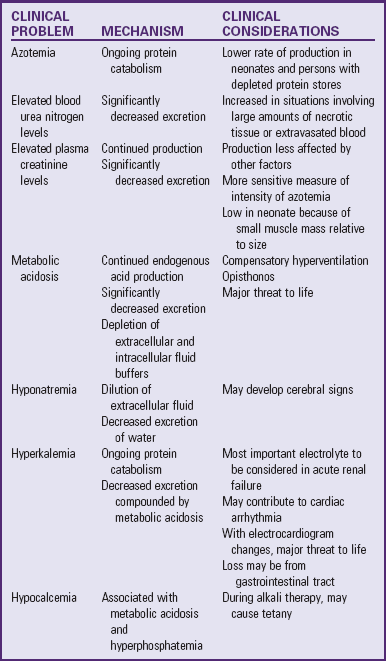
Diet: The child in remission maintains a regular diet. However, salt is restricted during periods of massive edema and while on corticosteroid therapy; no salt is added at the table, and foods with very high salt content are excluded. The child tolerates this diet for a time, but it should be adjusted to the child’s appetite and must not interfere with nutrient intake. Although a low-sodium diet will not remove edema, its rate of increase may be reduced. Water is seldom restricted. A diet generous in protein is logical, but there is no evidence that it is beneficial or alters the outcome of the disease. The presence of azotemia and renal failure is a contraindication for high-protein intake.
Corticosteroid Therapy: The response of most affected children to corticosteroids has established these drugs as prime therapeutic agents in the management of nephrotic syndrome (Kim, Bellew, Silverstein, et al, 2005). Corticosteroid therapy begins as soon as the diagnosis has been determined and is administered orally in a dosage of 60 mg/m2/day in evenly divided doses. Prednisone, the safest and least expensive drug, is the steroid of choice. The drug is continued daily for 6 weeks, then reduced to 40 mg/m2 on alternate days for 6 more weeks. Studies suggest that the duration of steroid treatment for the initial episode should be at least 3 months (Hodson, Knight, Willis, et al, 2004).
The course of the disease is fairly predictable. There is little change during the first few days of therapy. In most patients diuresis occurs as the urinary protein excretion diminishes within 7 to 21 days after the initiation of steroid therapy. Other clinical manifestations stabilize or return to normal shortly thereafter. Almost 95% of patients between 1 and 10 years of age who have satisfactory laboratory measurements of C3 complement and a renal clearance of immunoglobulin G, as well as no hypertension, hematuria, or renal insufficiency, will have complete resolution of proteinuria with therapy. If the child has not responded to therapy within 28 days of daily steroid administration, the likelihood of subsequent response diminishes rapidly.
Children with MCNS are often described according to their response to corticosteroid therapy (Box 30-4). Children with MCNS typically relapse one to three times per year. Steroid-dependent children tend to have frequent relapses over many years and receive large amounts of steroids, which results in cushingoid features and may cause growth retardation. They also require supportive treatment (diuretics, diet). Steroid-resistant children are thought to have a high risk of developing chronic renal failure (CRF) (Kim, Bellew, Silverstein, et al, 2005).
Immunosuppressant Therapy: It is possible to reduce the relapse rate and induce long-term remission in children with frequent relapsing or steroid-resistant nephrotic syndrome with administration of an oral alkylating agent, usually cyclophosphamide (Cytoxan) or chlorambucil. Prolonged courses of cyclosporin and levamisole reduce the risk of relapse in children compared with corticosteroids alone (Durkan, Hodson, Willis, et al, 2005). The drugs share many characteristics, and the response to oral alkylating agents appears to depend on dose, duration of therapy, age, and duration of the disease.
The nurse must consider significant side effects of cyclophosphamide and discuss them with parents of children for whom this drug is contemplated. Anticipate leukopenia, and remember that cyclophosphamide may cause azoospermia with potential sterility in males treated for more than 2 to 3 months and may cause variable effects on gonadal function in females.
Diuretics: One characteristic of the edema of nephrotic syndrome is its usual lack of responsiveness to diuretic agents. However, loop diuretics, usually furosemide in combination with metolazone, are sometimes useful in cases in which edema interferes with respiration or there is hypotension, hyponatremia, or skin breakdown. In addition, plasma expanders such as salt-poor human albumin may be administered to severely edematous children requiring prompt control; however, they must be administered frequently because the glomeruli are readily permeable to albumin in the acute stage.
Prognosis: The prognosis for ultimate recovery in most cases is good. MCNS is a self-limiting disease, and in children who respond to steroid therapy the tendency to relapse decreases with time. With early detection and prompt implementation of therapy to eradicate proteinuria, progressive basement membrane damage is minimized so that renal function is usually normal or near normal when the tendency for relapses is past. It is estimated that approximately 80% of affected children have this favorable prognosis, although half the children have relapses even after 5 years, and 20% after 10 years (Bagga and Mantan, 2005).
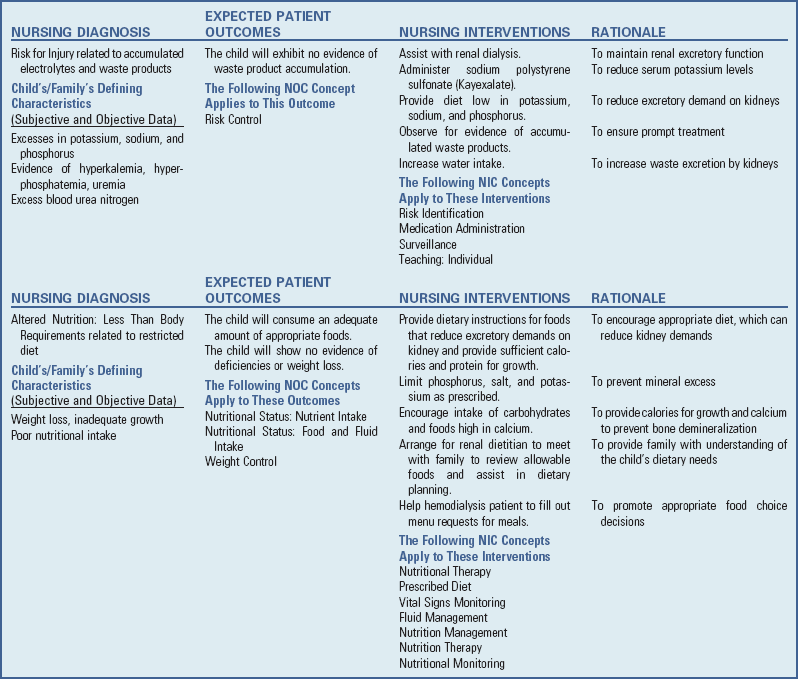
Nursing Care Management
Daily monitoring of intake and output is an important nursing function. Strict and accurate measurement is essential but may be difficult in very young children. In these cases the nurse can measure for output by methods such as weighing diapers. Other methods of monitoring progress include examination of the urine for albumin, daily weight, and measurement of abdominal girth. Assessment of edema such as increased or decreased swelling around the eyes and dependent areas, the degree of pitting (if noted), and the color and texture of the skin are part of nursing care. The nurse monitors vital signs to detect any early signs of complications such as shock or an infectious process.
In children hospitalized with MCNS, elevating edematous parts may be helpful to shift fluid to more comfortable distributions, but diuresis with medications and salt and water restriction to remove edema fluid are the best therapy. Areas that are particularly edematous, such as the scrotum, abdomen, and legs, may require support. Clean skin surfaces and separate them with clothing, cotton, or antiseptic powder to prevent intertrigo.
Because these children are particularly vulnerable to upper respiratory tract infection, protect them from contact with infected roommates, family, or visitors. Spontaneous peritonitis can occur secondary to migration of intestinal bacteria across the bowel wall and into the peritoneum. Monitor vital signs to detect any early signs of an infectious process.
Loss of appetite that accompanies active nephrosis creates a perplexing problem for nurses. During this time the combined efforts of the nurse, dietitian, parents, and child are necessary to formulate a nutritionally adequate and attractive diet. Salt and fluids are restricted during the edema phase. Make every effort to serve attractive meals with a minimum of fuss, but it usually requires a little creativity to get the child to eat. Games, rewards, and special treats often help, but each child is unique; trial and error may be necessary to arrive at a successful strategy. Also, the same strategy may not work consistently. (See Feeding the Sick Child, Chapter 27.)
As the edema subsides, children are allowed increased fluids. Suitable recreational and diversional activities are also an important part of their care. Once the edema fluid has been lost, children resume their usual activities without problems. Irritability and mood swings accompanying the disease process and steroid therapy are not unusual manifestations in these children and create an additional challenge to the nurse and the family.
Family Support and Home Care: Most children are treated at home during relapses. Teach parents to detect signs of relapse and to notify the health care provider if they occur. Home care is preferred unless the edema and proteinuria are severe. Instruct parents in urine testing for albumin, administration of medications, and general care. Urine is usually tested daily while the child is receiving medicine for nephrotic syndrome or if the child has an illness, and twice a week during remission. Salt is restricted to no additional salt during relapse and steroid therapy, but a regular diet is suitable for the child in remission. Instruct parents regarding avoiding contact with infected playmates, but the child is permitted to attend school. It is important for parents of children on corticosteroid therapy to be aware of the common side effects of steroid therapy (e.g., rounding of the face, increased appetite, behavior changes, abdominal distention, and hirsutism) and to distinguish some of these from the edema formation of the disease. Reassure parents that the symptoms will disappear gradually after discontinuation of the drug. The child should receive close medical or nursing observation to detect unusual but more serious side effects (see Critical Thinking Exercise).
The prolonged course of the relapsing form of nephrotic syndrome is taxing to both the child and the family. In the worst cases of frequent remissions and exacerbations with periodic disruption of family life by hospitalization, a severe strain is placed on the child and the family, both psychologically and financially. Parents of children with frequent relapses poorly responsive to medications need reassurance regarding this characteristic of the disease so they do not become discouraged. At the same time, impress on them the importance of long-term care to gain their cooperation. A satisfactory response is more likely when relapses are detected and therapy is instituted early, and remissions are prolonged when instructions are carried out faithfully. For example, one child had an exacerbation when his mother reduced the dosage of his drug because it was so expensive.
Social isolation is a problem for these children. Isolation is related to frequent hospitalization or confinement during relapse, the risk of infection that may precipitate an exacerbation, lack of energy, and the child’s reluctance to face friends at home or school because of the changes in appearance resulting from the disease or the medication. Both parents and child need someone to listen to their complaints, to assist them in coping with both short- and long-term problems associated with the disease, and to find solutions to their problems. Continuous support of the child and family is one of the major nursing considerations.