Moderate Nonskeletal Problems in Preadolescent Children
Preventive and Interceptive Treatment in Family Practice
Orthodontic Triage: Distinguishing Moderate from Complex Treatment Problems
For a dentist seeing a young patient with a malocclusion, the first question is whether orthodontic treatment is needed. If so, the next question is: when should it be done? Finally, who should do it? Does this patient need referral to a specialist?
In military and emergency medicine, triage is the process used to separate casualties by the severity of their injuries. Its purpose is twofold: to separate patients who can be treated at the scene of the injury from those who need transportation to specialized facilities and to develop a sequence for handling patients so that those most likely to benefit from immediate treatment will be treated first. Since orthodontic problems almost never are an emergency, the process of sorting orthodontic problems by their severity is analogous to medical triage in only one sense of the word. On the other hand, it is very important for the primary care dentist to be able to distinguish problems that generally need to be treated soon, as opposed to more routine problems that can wait for later comprehensive care. Along the same lines, sorting out moderate from complex problems is essential because this process determines which patients are appropriately treated within family practice and which are most appropriately referred to a specialist.
As with all components of dental practice, a generalist’s decision of whether to include orthodontic treatment as a component of his or her services is an individual one, best based on education, experience, and ability. The principle that the less severe problems are handled within the context of general practice and the more severe problems are referred should remain the same, however, regardless of the practitioner’s interest in orthodontics. Only the cutoff points for treating a patient in the general practice or referral should change.
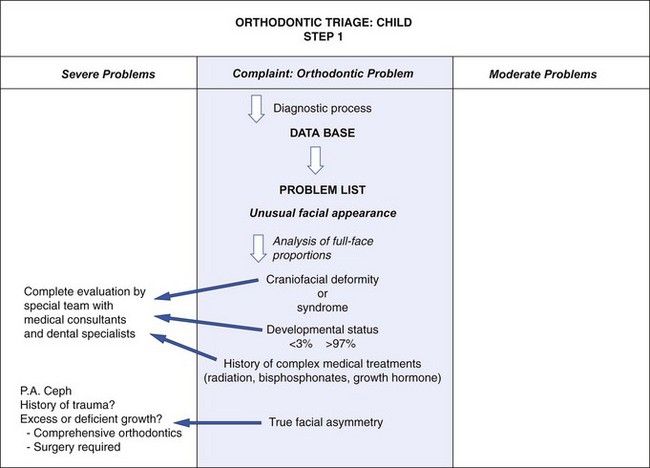
This section presents a logical scheme for orthodontic triage for children. It is based on the diagnostic approach developed in Chapter 6 and incorporates the principles of determining treatment need that have been discussed. An adequate database and a thorough problem list, of course, are necessary to carry out the triage process. A cephalometric radiograph is not required since a facial form analysis is more appropriate in the generalist’s office, but appropriate dental radiographs are needed (usually, a panoramic film; occasionally, bitewings supplemented with anterior occlusal radiographs) as are dental casts and photographs. A space analysis (see later in this chapter) is essential. A flow chart illustrating the steps in the triage sequence accompanies this section.
Step 1: Syndromes and Developmental Abnormalities
The first step in the triage process is to separate out patients with facial syndromes and similarly complex problems (Figure 11-1) so they can be treated by specialists or teams of specialists. From physical appearance, the medical and dental histories, and an evaluation of developmental status, nearly all such patients are easily recognized. Examples of these disorders are cleft lip or palate, Treacher Collins syndrome, hemifacial microsomia, and Crouzon’s syndrome (see Chapter 3). Complex medical treatments, such as radiation, bisphosphonates, and growth hormones, can affect dentofacial development and responses to treatment. Patients who appear to be developing either above the 97th or below the third percentiles on standard growth charts require special evaluation. Growth disorders may demand that any orthodontic treatment be carried out in conjunction with endocrine, nutritional, or psychologic therapy. For these patients and those with diseases that affect growth, such as juvenile rheumatoid arthritis, the proper orthodontic therapy must be combined with identification and control of the disease process.
Patients with significant skeletal asymmetry (not necessarily those whose asymmetry results from only a functional shift of the mandible due to dental interferences caused by crossbites) always fall into the severe problem category (Figure 11-2). These patients could have a developmental problem or the growth anomaly could be the result of an injury. Treatment is likely to involve growth modification and/or surgery, in addition to comprehensive orthodontics. Timing of intervention is affected by whether the cause of the asymmetry is deficient or excessive growth (see Chapter 13), but early comprehensive evaluation is always indicated.
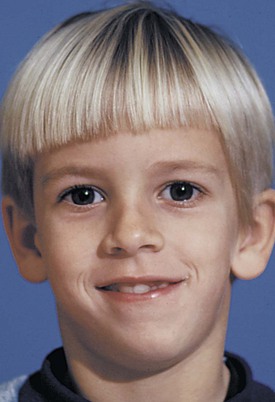
FIGURE 11-2 At age 8, this boy has a noticeable mandibular asymmetry with the chin several millimeters off to the left. A problem of this type is likely to become progressively worse and is an indication for referral for comprehensive evaluation by a facial deformities team. (From Proffit WR, White RP, Sarver DM. Contemporary Treatment of Dentofacial Deformity. St. Louis: Mosby; 2003.)
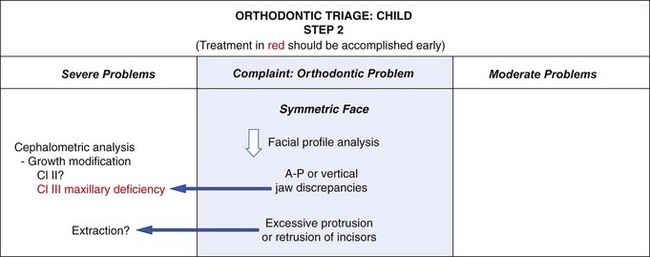
Step 2: Facial Profile Analysis (Figure 11-3)
Anteroposterior and Vertical Problems
Skeletal Class II and Class III problems and vertical deformities of the long-face and short-face types, regardless of their cause, require thorough cephalometric evaluation to plan appropriate treatment and its timing and must be considered complex problems (Figure 11-4). Issues in treatment planning for growth modification are discussed in Chapter 13. As a general rule, Class II treatment can be deferred until near adolescence and be equally effective as earlier treatment, while Class III treatment for maxillary deficiencies should be addressed earlier. Class III treatment for protrusive mandibles appears equally ineffective whenever it is attempted. Treatment of both long- and short-face problems probably can be deferred, since the former is due to growth that persists until the late teens and outstrips early focused intervention, and the latter usually can be managed well with comprehensive treatment during adolescence. As with asymmetry, early evaluation is indicated even if treatment is deferred, so early referral is appropriate.

FIGURE 11-4 Patients with a skeletal problem of even moderate severity should be identifiable clinically. A, Skeletal Class II due to mandibular deficiency. B, Skeletal Class III with a component of both maxillary deficiency and mandibular excess. Both types of problems can easily be picked up from examination of the profile. A cephalometric radiograph at this age is not needed for diagnosis, but would be indicated if early treatment is planned.
Excessive Dental Protrusion or Retrusion
Severe dental protrusion or retrusion, which also are complex treatment problems, should be recognized during the facial profile analysis. The urgency for treating these problems usually depends on the esthetic impact or in the case of protrusion, the potential for traumatic injury. Otherwise, they should be treated as noted above.
Some individuals with good skeletal proportions have protrusion of incisor teeth rather than crowding (Figure 11-5). When this occurs, the space analysis will show a small or nonexistent discrepancy because the incisor protrusion has compensated for the potential crowding. Excessive protrusion of incisors (bimaxillary protrusion, not excessive overjet) usually is an indication for premolar extraction and retraction of the protruding incisors. This is complex and prolonged treatment. Because of the profile changes produced by adolescent growth, it is better for most children to defer extraction to correct protrusion until late in the mixed dentition or early in the permanent dentition. Techniques for controlling the amount of incisor retraction are described in Chapter 15.
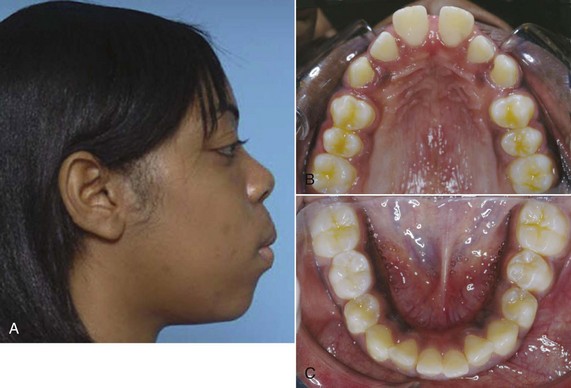
FIGURE 11-5 A, Bimaxillary dentoalveolar protrusion. Note the lip strain to bring the lips together over the teeth. The lips were separated at rest by the protruding incisors. B and C, Occlusal views show the spacing in the upper arch and very mild crowding in the lower arch. For this girl, potential crowding of the teeth is expressed almost completely as protrusion.
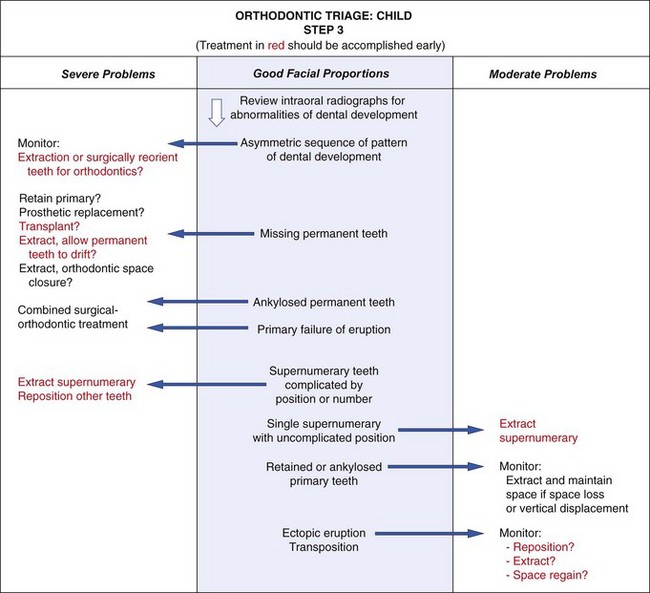
Step 3: Dental Development
Unlike the more complex skeletal problems and problems related to protruding incisors, problems involving dental development often need treatment as soon as they are discovered, typically during the early mixed dentition, and often can be handled in family practice. Considerations in making that decision are outlined in Figure 11-6, and treatment of the less severe problems of this type is presented in detail in this chapter.
Asymmetric Dental Development
Treatment for an abnormal sequence of dental development should be planned only after a careful determination of the underlying cause. Asymmetric eruption (one side ahead of the other by 6 months or more) is significant. It requires careful monitoring of the situation, and in the absence of outright pathology, often requires early treatment such as selective extraction of primary or permanent teeth. A few patients with asymmetric dental development have a history of childhood radiation therapy to the head and neck or traumatic injury. Surgical and orthodontic treatment for these patients must be planned and timed carefully and may require tooth removal or tooth reorientation. Some of these teeth have severely dilacerated roots and will not be candidates for orthodontics. These situations definitely fall into the complex category and usually require early intervention.
Missing Permanent Teeth
The permanent teeth most likely to be congenitally missing are the maxillary lateral incisors and the mandibular second premolars. Maxillary central and lateral incisors are the teeth most likely to be lost to trauma.
The treatment possibilities differ slightly for anterior and posterior teeth. For missing posterior teeth, it is possible to (1) maintain the primary tooth or teeth, (2) extract the overlying primary teeth and then allow the adjacent permanent teeth to drift, (3) extract the primary teeth followed by immediate orthodontic treatment, or (4) replace the missing teeth prosthetically or perhaps by transplantation or an implant later. For anterior teeth, maintaining the primary teeth is often less of an option due to the esthetics and the spontaneous eruption of adjacent permanent teeth into the space of the missing tooth. Also, extraction and drift of the adjacent teeth is less appealing because anterior edentulous ridges deteriorate quickly. As with other growth problems, early evaluation and planning is essential. Treatment of missing tooth problems in mixed dentition children is discussed in more detail in Chapter 12.
For all practical purposes, ankylosed permanent teeth at an early age or teeth that fail to erupt for other reasons (like primary failure of eruption) fall into the same category as missing teeth. These severe problems often require a combination of surgery (for extraction or decoronation) and orthodontics, if indeed the condition can be treated satisfactorily at all. After surgical intervention, the ultimate choices are orthodontic space closure, transplantation into the affected area, or prosthetic replacement.
Supernumerary Teeth
Ninety percent of all supernumerary teeth are found in the anterior part of the maxilla. Multiple or inverted supernumeraries and those that are malformed often displace adjacent teeth and cause problems in their eruption. The presence of multiple supernumerary teeth indicates a complex problem and perhaps a syndrome or congenital abnormality like cleidocranial dysplasia. Early removal of the supernumeraries is indicated, but this must be done carefully to minimize damage to adjacent teeth. If the permanent teeth have been displaced or severely delayed, surgical exposure, adjunctive periodontal surgery, and possibly mechanical traction are likely to be required to bring them into the arch after the supernumerary has been removed.
Single supernumeraries that are not malformed often erupt spontaneously, causing crowding problems. If these teeth can be removed before they cause distortions of arch form, extraction may be all that is needed.
Other Eruption Problems
Ectopic eruption (eruption of a tooth in the wrong place, or along the wrong eruption path) often leads to early loss of a primary tooth, but in severe cases, resorption of permanent teeth can result. Repositioning of the ectopically erupting tooth may be indicated, either surgically or by exposing the problem tooth, placing an attachment on it, and applying traction. A dramatic variation of ectopic eruption is transposition of teeth. Early intervention can reduce the extent to which teeth are malpositioned in some cases. These severe problems often require a combination of surgery and orthodontics and may be genetically linked to other anomalies. They are discussed in Chapter 12.
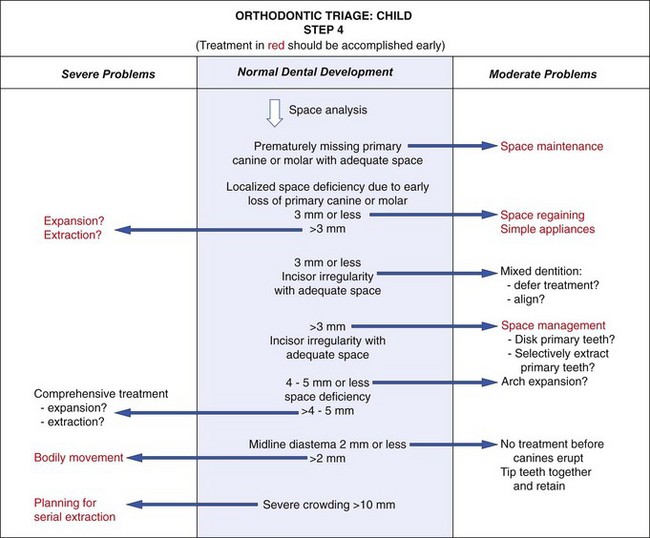
Step 4: Space Problems
Orthodontic problems in a child with good facial proportions involve crowding, irregularity, or malposition of the teeth (Figure 11-7). At this stage, regardless of whether crowding is apparent, the results of space analysis are essential for planning treatment. The presence or absence of adequate space for the teeth must be taken into account when other treatment is planned.
In interpreting the results of space analysis for patients of any age, remember that if space to align the teeth is inadequate, either of two conditions may develop. One possibility is for the incisor teeth to remain upright and well positioned over the basal bone of the maxilla or mandible and then rotate or tip labially or lingually. In this instance, the potential crowding is expressed as actual crowding and is difficult to miss (Figure 11-8). The other possibility is for the crowded teeth to align themselves completely or partially at the expense of the lips, displacing the lips forward and separating them at rest (see Figure 11-5). Even if the potential for crowding is extreme, the teeth can align themselves at the expense of the lip, interfering with lip closure. This must be detected on profile examination. If there is already a degree of protrusion in addition to the crowding, it is safe to presume that the natural limits of anterior displacement of incisors have been reached.
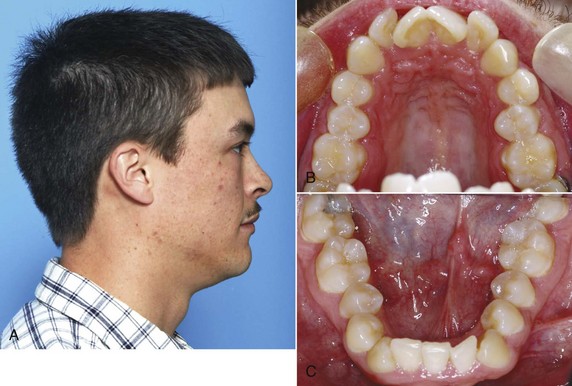
FIGURE 11-8 In some patients, as in this young adult (A), potential crowding is expressed completely as actual crowding (B and C) with no compensation in the form of dental and lip protrusion. In others (see Figure 11-5) potential crowding is expressed as protrusion. The teeth end up in a position of equilibrium between the tongue and lip forces against them (see Chapter 5).
Depending on the circumstances, the appropriate response to space deficiencies varies. For space loss of 3 mm or less, lost space can be regained. For space shortage of 4 mm or less or crowding with adequate space, repositioning incisors labially or space management during the transition are appropriate. Of these procedures, only treatment to regain space and manage transitional space is critical in terms of timing. Treatment planning for these moderate problems is outlined below in this chapter. Space discrepancies of 5 mm or more, with or without incisor protrusion, constitute complex treatment problems. In these children, if teeth are not extracted, maximum anchorage or robust mechanics must be employed, and if teeth are extracted, the anchorage considerations are critical. Severe crowding of 10 mm or more also requires careful and complex planning and often early intervention, so that permanent teeth are not impacted or deflected into eruption paths that affect other permanent teeth or bring them into the oral cavity through nonkeratinized tissue.
Generally, minor midline diastemas will close and cause little esthetic or developmental problems. Large diastemas, over 2 mm, can be esthetic concerns and inhibit adjacent teeth from erupting properly. They are cause for heightened concern and early treatment.
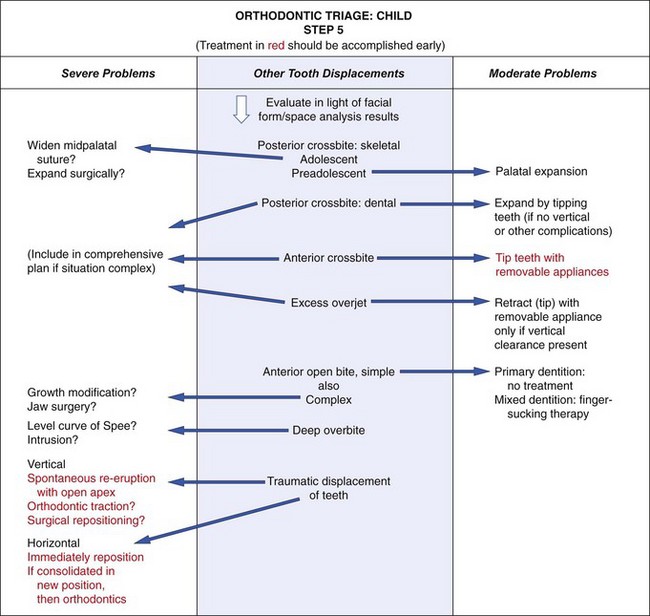
Step 5: Other Occlusal Discrepancies
Whether crossbite and overbite/open bite should be classified as moderate or severe is determined for most children from their facial form (Figure 11-9). Mixed dentition treatment for all of these problems must be discussed in the context of “should be treated” versus “can be treated.”
As a general guideline, posterior crossbite in a preadolescent child falls into the moderate category if no other complicating factors (like severe crowding) are present. It should be treated early if the child shifts laterally from the initial dental contact position. Although it can be treated early if there is no shift, often it is better to delay until the late mixed dentition so the erupting premolars and second molars can be guided into position. If a skeletal posterior crossbite is treated in adolescence, it will require heavier forces and more complex appliances.
Anterior crossbite usually reflects a jaw discrepancy but can arise from lingual tipping of the incisors or crowding as they erupt. Treatment planning for the use of removable versus fixed appliances to correct these simple crossbites early is discussed below.
Excessive overjet, with the upper incisors flared and spaced, often reflects a skeletal problem but also can develop in patients with good jaw proportions. If adequate vertical clearance is present, the teeth can be tipped lingually and brought together with a simple removable appliance when the child is almost any age, and the timing of treatment often depends on child and parent preference.
Anterior open bite in a young child with good facial proportions usually needs no treatment because there is a good chance of spontaneous correction with additional incisor eruption, especially if the open bite is related to an oral habit like finger sucking. A complex open bite (one with skeletal involvement or posterior manifestations) or any open bite in an older patient is a severe problem. A deep overbite can develop in several ways (see Chapter 6) but often is caused by or made worse by short anterior face height. This is seldom treated in the mixed dentition.
Traumatically displaced erupted incisors pose a special problem because of the resulting occlusal problems. There is a risk of ankylosis after healing occurs, especially after traumatic intrusion. If the apex is open and root development is incomplete, waiting for spontaneous re-eruption is warranted. If the injuries are more severe or in older patients, either immediate orthodontic or surgical treatment is needed, and the long-term prognosis must be guarded. Treatment planning after trauma is discussed in Chapter 13.
This triage scheme is oriented toward helping the family practitioner decide which children with orthodontic problems to treat and which to refer. Treatment for children with moderate nonskeletal problems, those selected for treatment in family practice using the triage scheme, is discussed later in this chapter. Early (preadolescent) treatment of more severe and complex nonskeletal problems is discussed in Chapter 12, and treatment for skeletal problems is discussed in Chapter 13.
Management of Occlusal Relationship Problems
Posterior crossbite in mixed dentition children is reasonably common, occurring in 7.1% of U.S. children aged 8 to 11.1 It usually results from a narrowing of the maxillary arch and often is present in children who have had prolonged sucking habits. The crossbite can be due to a narrow maxilla (i.e., to skeletal dimensions) or due only to lingual tipping of the maxillary teeth. If the child shifts on closure or if the constriction is severe enough to significantly reduce the space within the arch, early correction is indicated. If not, treatment can be deferred, especially if other problems suggest that comprehensive orthodontics will be needed later.
It is also important to determine whether any associated mandibular asymmetry is the result of a shift of the lower jaw due to dental interferences or is due to a true maxillary or mandibular asymmetry. Another critical question is whether the posterior crossbite is related to skeletal maxillary retrusion or mandibular protrusion. In these cases, the anteroposterior position of the maxilla or mandible is contributing to the crossbite, and the actual transverse dimension of the palate may be normal.
Correcting posterior crossbites in the mixed dentition increases arch circumference and provides more room for the permanent teeth. On the average, a 1 mm increase in the inter-premolar width increases arch perimeter values by 0.7 mm.2 Total relapse into crossbite is unlikely in the absence of a skeletal problem, and mixed dentition expansion reduces the incidence of posterior crossbite in the permanent dentition, so early correction also simplifies future diagnosis and treatment by eliminating at least that problem from the list.
Although it is important to determine whether the crossbite is skeletal or dental, in the early mixed dentition years the treatment is usually the same, since relatively light forces will move teeth and bones. An expansion lingual arch is the best choice at this age—heavy force from a jackscrew device is needed only when the midpalatal suture has become significantly interdigitated during adolescence (Figure 11-10; also see Chapter 13). Heavy force and rapid expansion are not indicated in the primary or early mixed dentition. There is a significant risk of distortion of the nose if this is done in younger children (see Figure 7-8).

FIGURE 11-10 In young children, lingual arch type maxillary expansion devices (W-arches and quad helixes) deliver enough force to open the midpalatal suture as demonstrated in this maxillary occlusal radiograph.
There are three basic approaches to the treatment of moderate posterior crossbites in children:
1. Equilibration to Eliminate Mandibular Shift
In a few cases, mostly observed in the primary or early mixed dentition, a shift into posterior crossbite will be due solely to occlusal interference caused by the primary canines or (less frequently) primary molars. These patients can be diagnosed by carefully positioning the mandible in centric occlusion; then it can be seen that the width of the maxilla is adequate and that there would be no crossbite without the shift (Figure 11-11). In this case, a child requires only limited equilibration of the primary teeth (often, just reduction of the primary canines) to eliminate the interference and the resulting lateral shift into crossbite.3

FIGURE 11-11 Minor canine interferences leading to a mandibular shift. A, Initial contact. B, Shift into centric occlusion. The slight lingual position of the primary canines can lead to occlusal interferences and an apparent posterior crossbite. This sole cause of posterior crossbite is infrequent and is best treated by occlusal adjustment of the primary canines.
2. Expansion of a Constricted Maxillary Arch
More commonly, a lateral shift into crossbite is caused by constriction of the maxillary arch. Even a small constriction creates dental interferences that force the mandible to shift to a new position for maximum intercuspation (Figure 11-12), and moderate expansion of the maxillary dental arch is needed for correction. The general guideline is to expand to prevent the shift when it is diagnosed, but there is an exception: if the permanent first molars are expected to erupt in less than 6 months, it is better to wait for their eruption so that correction can include these teeth, if necessary. A greater maxillary constriction may allow the maxillary teeth to fit inside the mandibular teeth—if so, there will not be a shift on closure (Figure 11-13), and there is less reason to provide early correction of the crossbite.

FIGURE 11-12 Moderate bilateral maxillary constriction. A, Initial contact. B, Shift into centric occlusion. Moderate bilateral maxillary constriction often leads to posterior interferences upon closure and a lateral shift of the mandible into an apparent unilateral posterior crossbite. This problem also is best treated by bilateral maxillary expansion.

FIGURE 11-13 Marked bilateral maxillary constriction. A, Initial contact. B, Centric occlusion (no shift). Severe constriction often produces no interferences upon closure, and the patient has a bilateral posterior crossbite in centric relation. This problem is best treated by bilateral maxillary expansion.
Although it is possible to treat posterior crossbite with a split-plate type of removable appliance, there are three problems: this relies on patient compliance for success, treatment time is longer, and it is more costly than an expansion lingual arch.4 The preferred appliance for a preadolescent child is an adjustable lingual arch that requires little patient cooperation.
Both the W-arch and the quad helix are reliable and easy to use. The W-arch is a fixed appliance constructed of 36 mil steel wire soldered to molar bands (Figure 11-14). It is activated simply by opening the apices of the W and is easily adjusted to provide more anterior than posterior expansion, or vice versa, if this is desired. The appliance delivers proper force levels when opened 4 to 6 mm wider than the passive width and should be adjusted to this dimension before being cemented. It is not uncommon for the teeth and maxilla to move more on one side than the other, so precise bilateral expansion is the exception rather than the rule, but acceptable correction and tooth position are almost always achieved.
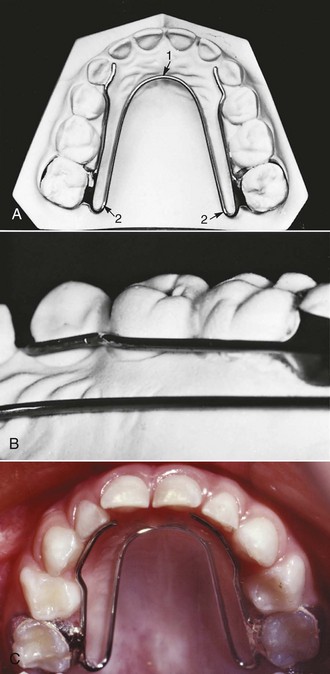
FIGURE 11-14 The W-arch appliance is ideal for bilateral maxillary expansion. A, The appliance is fabricated from 36 mil wire and soldered to the bands. The lingual wire should contact the teeth involved in the crossbite and extend not more than 1 to 2 mm distal to the banded molars to eliminate soft tissue irritation. Activation at point 1 produces posterior expansion and activation at point 2 produces anterior expansion. B, The lingual wire should remain 1 to 1.5 mm away from the marginal gingiva and the palatal tissue. C, This W-arch is being used to correct a bilateral constriction in the primary dentition.
The quad helix (Figure 11-15) is a more flexible version of the W-arch, although it is made with 38 mil steel wire. The helices in the anterior palate are bulky, which can effectively serve as a reminder to aid in stopping a finger habit. The combination of a posterior crossbite and a finger-sucking habit is the best indication for this appliance. The extra wire incorporated in it gives it a slightly greater range of action than the W-arch, but the forces are equivalent. Soft tissue irritation can become a problem with the quad helix. Both the W-arch and the quad helix leave an imprint on the tongue. Both the parents and child should be warned about this (Figure 11-16). The imprint will disappear when the appliance is removed but can take up to a year to totally do so.
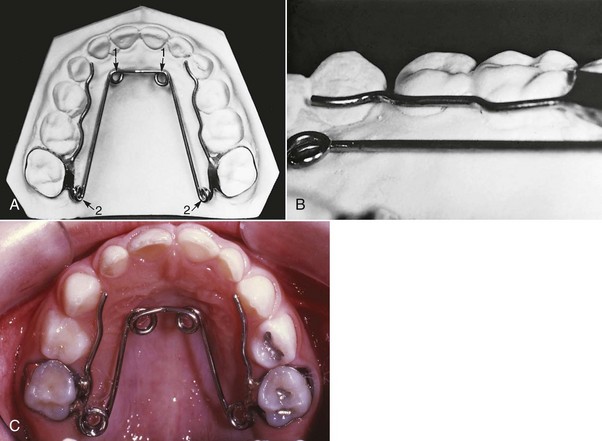
FIGURE 11-15 The quad helix used to correct bilateral maxillary constriction. A, The appliance is fabricated from 38 mil wire and soldered to the bands. The lingual wire should contact the teeth involved in the crossbite and extend no more than 1 to 2 mm distal to the banded molars to eliminate soft tissue irritation. Activation at point 1 produces posterior expansion, while activation at point 2 produces anterior expansion. B, The lingual wire should remain 1 to 1.5 mm away from the marginal gingiva and palatal tissue. C, This quad helix is being used to correct a bilateral maxillary constriction in the primary dentition.

FIGURE 11-16 W-arches, quad helixes, and habit appliances often leave indentations in the superior surface of the tongue (arrows). These often remain after appliance removal for up to 1 year. No treatment is recommended, but patients and parents should be warned of this possibility.
With both types of expansion lingual arches, some opening of the midpalatal suture can be expected in a primary or mixed dentition child, so the expansion is not solely dental. Expansion should continue at the rate of 2 mm per month (1 mm on each side) until the crossbite is slightly overcorrected. In other words, the lingual cusps of the maxillary teeth should occlude on the lingual inclines of the buccal cusps of the mandibular molars at the end of active treatment (Figure 11-17). Intraoral appliance adjustment is possible but may lead to unexpected changes. For this reason, removal and re-cementation are recommended at each active treatment visit. Most posterior crossbites require 2 to 3 months of active treatment (with the patients seen each month for adjustments) and 3 months of retention (during which the lingual arch is left passively in place). This mixed dentition correction appears to be stable in the long term.5

FIGURE 11-17 A, Posterior crossbites should be overcorrected until the maxillary posterior lingual cusps occlude with the lingual inclines of the mandibular buccal cusps, as shown here, and then retained for approximately 3 months. B, After retention, slight lingual movement of the maxillary teeth results in normal occlusion.
3. Unilateral Repositioning of Teeth
Some children do have a true unilateral crossbite due to unilateral maxillary constriction of the upper arch (Figure 11-18). In these cases, the ideal treatment is to move selected teeth on the constricted side. To a limited extent, this goal of asymmetric movement can be achieved by using different length arms on a W-arch or quad helix (Figure 11-19), but some bilateral expansion must be expected. An alternative is to use a mandibular lingual arch to stabilize the lower teeth and attach cross-elastics to the maxillary teeth that are at fault. This is more complicated and requires cooperation to be successful but is more unilateral in its effect.

FIGURE 11-18 True unilateral maxillary posterior constriction. A, Initial contact. B, Full occlusion (no shift). True unilateral constriction has a unilateral posterior crossbite in centric relation and in centric occlusion, without a lateral shift. This problem is best treated with unilateral posterior expansion.

FIGURE 11-19 An unequal and asymmetric W-arch used to correct a true unilateral maxillary constriction. The side of the arch to be expanded has fewer teeth against the lingual wire than the anchorage unit. Even with this arrangement, both sides can be expected to show some expansion movement and the extent cannot be predicted.
All of the appliances described above are aimed at correction of teeth in the maxillary arch, which is usually where the problem is located. If teeth in both arches contribute to the problem, cross-elastics between banded or bonded attachments in both arches (Figure 11-20) can reposition both upper and lower teeth. The best choice is a latex elastic with a  -inch (5 mm) lumen generating 6 ounces (170 gm) of force. The force from the elastics is directed vertically as well as faciolingually, which will extrude the posterior teeth and reduce the overbite. Therefore cross-elastics should be used with caution in children with increased lower face height or limited overbite. Crossbites treated with elastics should be overcorrected, and the bands or bonds left in place immediately after active treatment. If there is too much relapse, the elastics can be reinstated without rebanding or rebonding. When the occlusion is stable after several weeks without elastic force, the attachments can be removed. The most common problem with this form of crossbite correction is lack of cooperation from the child.
-inch (5 mm) lumen generating 6 ounces (170 gm) of force. The force from the elastics is directed vertically as well as faciolingually, which will extrude the posterior teeth and reduce the overbite. Therefore cross-elastics should be used with caution in children with increased lower face height or limited overbite. Crossbites treated with elastics should be overcorrected, and the bands or bonds left in place immediately after active treatment. If there is too much relapse, the elastics can be reinstated without rebanding or rebonding. When the occlusion is stable after several weeks without elastic force, the attachments can be removed. The most common problem with this form of crossbite correction is lack of cooperation from the child.
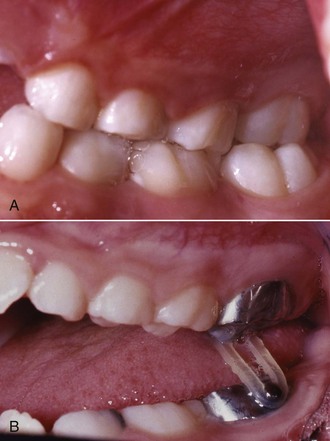
FIGURE 11-20 A, This patient has the permanent maxillary left first molar displaced lingually and the permanent mandibular left first molar displaced facially, which resulted in a posterior crossbite between these teeth. B, A short and relatively heavy cross-elastic is placed between the buttons welded on the bands. The elastic can be challenging for some children to place but should be worn full-time and changed frequently.
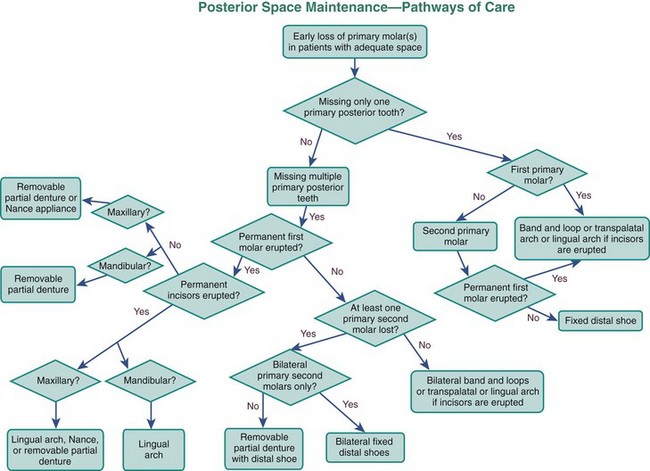
A flowchart is provided to help guide decision making for posterior crossbites (Figure 11-21).
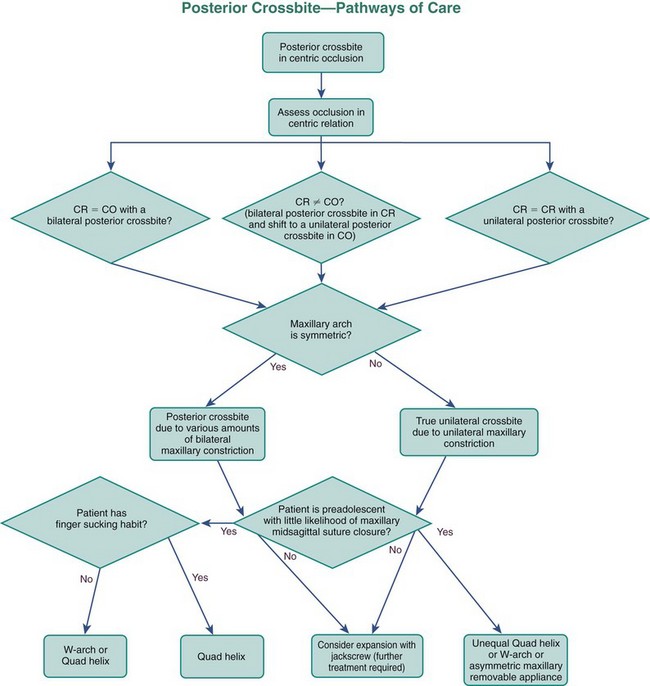
FIGURE 11-21 This flowchart can be used to aid decision making regarding possible options for posterior crossbite correction in the primary and mixed dentitions. Answers to the questions posed in the chart should lead to successful treatment pathways. The approaches to skeletal correction of posterior crossbites are described in Chapter 13.
Anterior Crossbite
Anterior crossbite, particularly crossbite of all of the incisors, is rarely found in children who do not have a skeletal Class III jaw relationship. A crossbite relationship of one or two anterior teeth, however, may develop in a child who has good facial proportions. When racial/ethnic groups in the U.S. population are combined, about 3% of children have an anterior crossbite in the mixed dentition (see Figure 1-7).
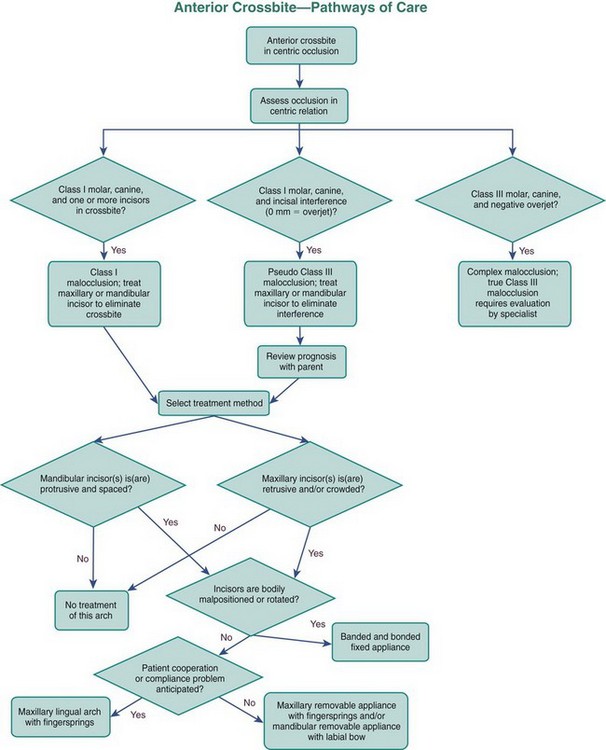
In planning treatment for anterior crossbites, it is critically important to differentiate skeletal problems of deficient maxillary or excessive mandibular growth from crossbites due only to displacement of teeth.6 If the problem is truly skeletal, simply changing the incisor position is inadequate treatment, especially in more severe cases (see Chapter 13).
Anterior crossbite affecting only one or two teeth almost always is due to lingually displaced maxillary central or lateral incisors. These teeth tend to erupt to the lingual because of the lingual position of the developing tooth buds and may be trapped in that location, especially if there is not enough space (Figure 11-22). Sometimes, central incisors are involved because they were deflected toward a lingual eruption path by supernumerary anterior teeth or overretained primary incisors. More rarely, trauma to maxillary primary teeth reorients a permanent tooth bud or buds lingually.

FIGURE 11-22 Although there was adequate space, this permanent maxillary right central incisor erupted into crossbite. Most likely this was caused by the lingual position of the tooth bud.
The most common etiologic factor for nonskeletal anterior crossbites is lack of space for the permanent incisors, and it is important to focus the treatment plan on management of the total space situation, not just the crossbite. If the developing crossbite is discovered before eruption is complete and overbite has not been established, the adjacent primary teeth can be extracted to provide the necessary space (Figure 11-23).

FIGURE 11-23 An anterior crossbite that is developing as erupting permanent incisors are deflected lingually can be treated by extracting adjacent primary teeth if space is not available for the erupting permanent teeth. A, The permanent maxillary right lateral incisor is beginning to erupt lingual to the other anterior teeth. B, Extraction of both primary maxillary canines has allowed spontaneous correction of the crossbite although all the irregularity has not been resolved.
Treatment of Nonskeletal Anterior Crossbite
Lingually positioned incisors limit lateral jaw movements, and they or their mandibular counterparts sometimes suffer significant incisal abrasion. In addition, when oral hygiene is less than ideal and gingival inflammation occurs, anterior teeth that are in crossbite, especially the lower incisors, are likely to have gingival recession. So, for these reasons, early correction of this type of anterior crossbite is indicated.
Only occasionally is it indicated to correct anterior crossbite in the primary dentition by moving the primary teeth because crowding severe enough to cause it is rare and the teeth often exfoliate before they can be successfully moved. Dental anterior crossbites typically develop as the permanent incisors erupt. Those diagnosed after overbite is established require appliance therapy for correction. The first concern is adequate space for tooth movement, which usually requires reducing the width of some teeth, extraction of the adjacent primary teeth, or opening space orthodontically. The diagnostic evaluation should determine whether tipping will provide appropriate correction. Often it will because the problem arose as eruption paths were deflected. If teeth are tipped when bodily movement is required, stability of the result is questionable.
In a young child, one way to tip the maxillary and mandibular anterior teeth out of crossbite is with a removable appliance, using fingersprings for facial movement of maxillary incisors (Figure 11-24) or, less frequently, an active labial bow for lingual movement of mandibular incisors. Two maxillary anterior teeth can be moved facially with one 22-mil double-helical cantilever spring. The appliance should have multiple clasps for retention, but a labial bow is usually contraindicated because it can interfere with facial movement of the incisors and would add little or no retention.
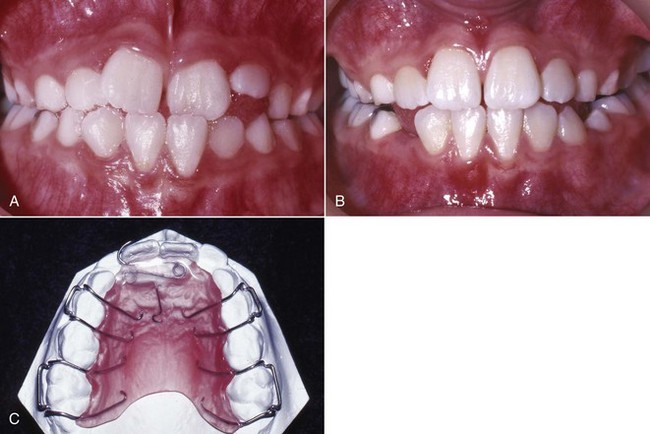
FIGURE 11-24 Anterior crossbite correction with a removable appliance to tip teeth. A, The permanent maxillary left central incisor has erupted into crossbite and (B) has been corrected with a removable appliance. C, This appliance is used to tip both central incisors facially with a 22 mil double helical fingerspring activated 1.5 to 2 mm per month to produce 1 mm per month of tooth movement. Note that plastic baseplate material extends over the spring to maintain its vertical position. The appliance is retained with multiple Adams’ clasps.
An anterior or posterior biteplate, or bonded adhesive on the occlusal surfaces of posterior teeth to reduce the overbite while the crossbite is being corrected, usually is not necessary in children. Unless the overbite is exceptionally deep, a biteplate would be needed only in a child with a clenching or grinding habit. A reasonable approach is to place the removable appliance without a biteplate and attempt tooth movement. If, after 2 months, the teeth in the opposing arch are moving in the same direction as the teeth to which the force is being applied, the bite can be opened by adding orthodontic banding cement to the occlusal surfaces of the lower posterior molars. When the crossbite is corrected, the cement can be removed relatively easily, and it does not require alteration of the appliance. Using a biteplate or opening the bite risks the chance that teeth not in contact with the appliance or the opposing arch will erupt excessively.
A removable appliance of this type requires nearly full-time wear to be effective and efficient. If the lingual fingersprings are activated 1.5 to 2 mm, they will produce approximately 1 mm of tooth movement in a month. The offending teeth should be slightly overcorrected and retained until overbite is adequate to retain the corrected tooth positions. One or 2 months of retention with a passive appliance is usually sufficient. The most common problems associated with these simple removable appliances are lack of patient cooperation, poor design leading to lack of retention, and improper activation.
One of the simplest fixed appliances for correction of maxillary incisors with a moderate anterior crossbite is a maxillary lingual arch with fingersprings (sometimes referred to as whip springs). This appliance (Figure 11-25) is indicated for a child with whom compliance problems are anticipated. The springs usually are soldered on the opposite side of the arch from the tooth to be corrected, in order to increase their length. They are most effective if they are approximately 15 mm long. When these springs are activated properly at each monthly visit (advancing the spring about 3 mm), they produce tooth movement at the optimum rate of 1 mm per month. The greatest problems are distortion and breakage from poor patient cooperation and poor oral hygiene, which can lead to decalcification and decay.

FIGURE 11-25 A, An anterior crossbite caused by lingual position of the maxillary incisors can be corrected using (B) a 36 mil lingual arch with soldered 22 mil fingersprings. A guidewire can be placed between the incisors as shown here to keep the springs from moving incisally. C, After correction, the appliance can be modified to serve as a retainer by soldering the free ends of the springs to the lingual arch.
It also is possible to tip the maxillary incisors forward with a 2 × 4 fixed appliance (2 molar bands, 4 bonded incisor brackets). In the rare instance when there is no skeletal component to the anterior crossbite, this is the best choice for a mixed dentition patient with crowding, rotations, the need for bodily movement, and more permanent teeth in crossbite (Figure 11-26). When the anterior teeth are bonded and moved prior to permanent canine eruption, it is best to place the lateral incisor brackets with some increased mesial root tip so that the roots of the lateral incisors are not repositioned into the canine path of eruption, with resultant resorption of the lateral incisor roots. If torque or bodily repositioning is needed for these teeth, finishing with a rectangular wire is required even in early mixed dentition treatment. Otherwise, the teeth will tip back into crossbite again.
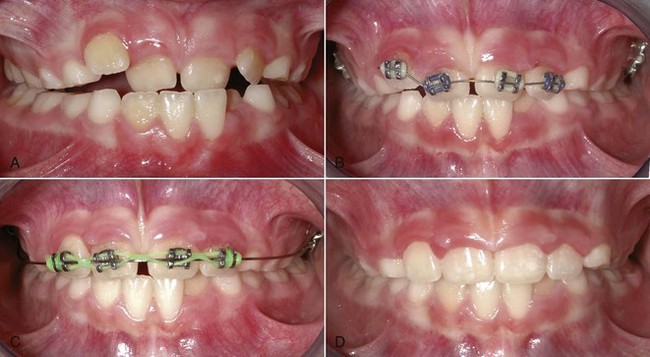
FIGURE 11-26 A, This patient has an anterior crossbite and irregular maxillary anterior teeth. B, A 14 mil segmental NiTi archwire was used from maxillary lateral to lateral incisors to take advantage of the archwire’s extreme flexibility for alignment. C, This was followed by a heavier stainless steel archwire that extended to the molars for more control and stability for diastema space closure with an elastomeric chain. D, Final alignment.
See Figure 11-27 for a flowchart to help guide decision making for anterior crossbites.
Anterior Open Bite
An open bite in a preadolescent child with normal vertical facial proportions has several possible causes: the normal transition when primary teeth are replaced by the permanent teeth, a habit like finger sucking or tooth displacement by resting soft tissue, or a skeletal problem (excessive vertical growth and rotation of the jaws that would create a disproportionately large lower anterior face height. All told, these problems affect less than 4% of the mixed dentition population (see Figure 1-8). Many of the transitional and habit problems resolve with either time or cessation of the sucking habit. Open bites that persist until adolescence, with the exception of those related to habits, or those that involve more than just the incisors almost always have a significant skeletal component, and careful diagnosis of the contributing factors is required.7 These are termed complex open bites and require advanced treatment methods (see Chapter 13).
Effects of Sucking Habits: During the primary dentition and early mixed dentition years, many children engage in digit and pacifier sucking, with girls predominating. Although it is possible to deform the alveolus and dentition during the primary dentition years with a prolonged and intense habit, much of the effect is on eruption of the permanent anterior teeth. The effect of such a habit on the hard and soft tissues depends on its frequency (hours per day) and duration (months/years) (see Chapter 5). With frequent and prolonged sucking, maxillary incisors are tipped facially, mandibular incisors are tipped lingually, and eruption of some incisors is impeded. As one would expect, overjet increases and overbite decreases. In many children, maxillary intercanine and intermolar width is narrowed, resulting in a posterior crossbite.
When the effect of digit sucking is compared to pacifier use, there is some evidence for increased prevalence of posterior crossbites with pacifiers, and especially with pacifier use for more than 18 months. Pacifier shapes that are designed to produce a more physiologic sucking pattern have not been proven to be beneficial when compared with other pacifiers or to finger sucking.8 It is also apparent that longer breastfeeding leads to fewer non-nutritive sucking habits.9 Most children have a non-nutritive sucking habit at 24 months, but only 40% have one at 36 months.10 These habits decrease with age and pacifier habits are observed less often with older children than digit habits. The social pressures of school are a strong deterrent.
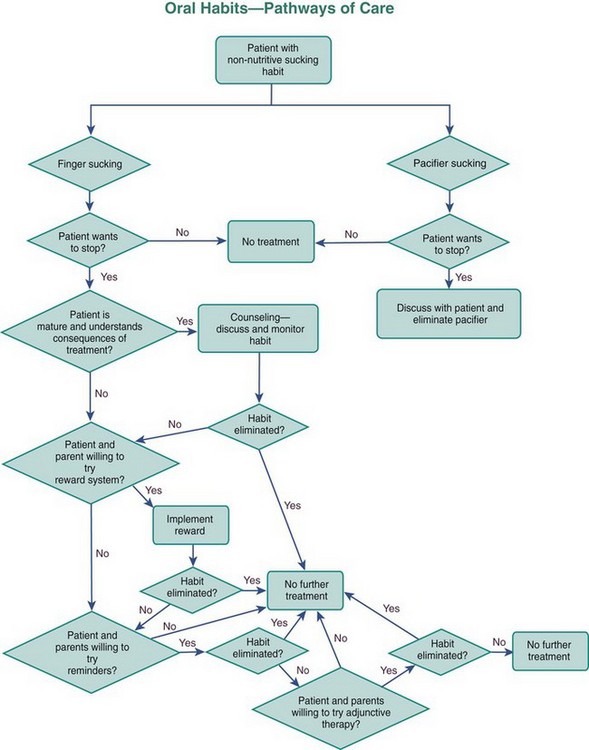
As long as the habit stops before the eruption of the permanent incisors, most of the changes resolve spontaneously with the exception of posterior crossbite (Figure 11-28).11 By that time, the majority of children have stopped their sucking habit. Another group still suck but want to stop, and yet another small group do not want to stop and appear to be immune to social pressure. If a child does not want to quit sucking, habit therapy (especially appliance therapy) is not indicated.

FIGURE 11-28 A to D, Photos at 1-year intervals of a child who stopped sucking his thumb at the time of the first photo. Gradual closure of the open bite, without a need for further intervention, usually occurs in patients with normal facial proportions after habits stop. E, If a sucking habit persists, a crib of this type can be used to help extinguish the habit. A crib is most effective in a child who wants to stop the thumb- or finger-sucking and accepts the crib as a reminder not to do so.
Nondental Intervention: As the time of eruption of the permanent incisors approaches, the simplest approach to habit therapy is a straightforward discussion between the child and the dentist that expresses concern and includes an explanation by the dentist of the problems caused by a prolonged finger habit. This “adult” approach (and restraint from intervention by the parents) may be enough to terminate the habit during this first part of the transition to the permanent dentition but is most effective with older children.
Another level of intervention is reminder therapy. This is for the child who wants to quit but needs help. Any one of several reminders that are introduced with an explanation to the child can be useful. One of the simplest approaches is to secure an adhesive bandage with waterproof tape on the finger that is sucked (Figure 11-29). The anterior portion of the quad helix appliance also can be quite useful as a reminder when it is placed in the appropriate position in the palate (see Figure 11-15).

FIGURE 11-29 An adhesive bandage can be applied over the end of the finger to remind the child not to suck and to reduce the enjoyment. The bandage should be anchored at its base for retention with waterproof tape, so that it will stay in place if sucking is still attempted. (Courtesy Dr. B. Joo.)
If the reminder approach fails, a reward system can be implemented that provides a small tangible daily reward for not engaging in the habit. In some cases, a large reward must be negotiated for complete cessation of the habit.
If all of these fail and the child really wants to quit, an elastic bandage loosely wrapped around the elbow prevents the arm from flexing and the fingers from being sucked. If this is used, wearing it only at night and 6 to 8 weeks of intervention should be sufficient. The child should understand that this is not punishment.
Appliance Therapy: If the previous methods have not succeeded in eliminating the habit, a removable reminder appliance is contraindicated because lack of compliance is part of the problem. The child who wants to stop can be fitted with a cemented reminder appliance that impedes sucking (Figure 11-30). These appliances can be deformed and removed by children who are not compliant and do not truly wish to stop the habit, so cooperation still is important. If this is understood by the child as a “helping hand” rather than punishment, the treatment will be successful and psychologic problems will not result.12 The preferred method is a maxillary lingual arch with an anterior crib device, making it extremely difficult for the child to place the thumb or other object in the mouth.

FIGURE 11-30 A cemented habit crib made of 38 to 40 mil wire can be used as a reminder to interrupt a finger-sucking habit. The appliance can be cemented to either primary or permanent molars and should be extended anteriorly to interfere with the finger position during sucking. The amount of overbite will also help determine the appliance position.
In about half of the children for whom such a crib is made, thumb-sucking stops immediately and the anterior open bite usually begins to close relatively rapidly thereafter. In the remaining children, thumb-sucking persists for a few weeks, but the crib device is eventually effective in extinguishing thumb-sucking in 85% to 90% of patients.13 It is a good idea to leave the crib in place for 6 months after the habit has apparently been eliminated. Commonly, these cemented reminders, like lingual arch expanders, leave an imprint on the tongue (see Figure 11-16) that will resolve some time after the appliance is removed. The appliances also trap food and can lead to mouth odor, so excellent oral hygiene is important.
The open bites associated with sucking in children with normal jaw relationships often resolve after sucking stops and the remaining permanent teeth erupt (see Figure 11-28). An appliance to laterally expand a constricted maxillary arch will be required, and flared and spaced incisors may need retraction, but the open bite should require no other treatment in children with good skeletal proportions.
A flowchart is provided to help guide decision making for open bite problems related to oral habits (Figure 11-31).
Deep Bite: Before treating an overbite problem, it is necessary to establish its cause. Significant deep bites affect approximately 20% of mixed dentition patients (see Figure 1-8). The problem may result from reduced lower face height, lack of eruption of posterior teeth, or overeruption of the anterior teeth. The possible treatments are quite different and mutually exclusive.
True reduced lower face height is a skeletal problem and requires more complex treatment (see Chapter 13). Undereruption of posterior teeth or overeruption of anterior teeth also usually are complex problems that are addressed during comprehensive treatment. They are rarely treated during the mixed dentition years.
Management of Eruption Problems
A permanent tooth should replace its primary predecessor when approximately three-fourths of the root of the permanent tooth has formed, whether resorption of the primary roots is or is not to the point of spontaneous exfoliation. Given enough time, the primary tooth will exfoliate, but a primary tooth that is retained beyond this point should be removed because it often leads to gingival inflammation and hyperplasia that cause pain and bleeding and sets the stage for deflected eruption paths of the permanent teeth that can result in irregularity, crowding, and crossbite. If a portion of the permanent tooth crown is visible and the primary tooth is mobile to the extent that the crown will move 1 mm in the facial and lingual direction, it is probably advisable to encourage the child to “wiggle” the tooth out. If that cannot be accomplished in a few days, extraction is indicated. Most overretained primary maxillary molars have either the buccal roots or the large lingual root intact; most overretained primary mandibular molars have either the mesial or distal root still intact and hindering exfoliation.
Once the primary tooth is out, if space is adequate, moderately abnormal facial or lingual positioning will usually be corrected by the equilibrium forces of the lip, cheeks, and tongue. Generally, incisors will erupt lingually and then move facially when overretained primary incisors exfoliate or are removed (Figure 11-32). If spontaneous correction has not occurred when overbite is achieved, however, further alignment is unlikely in either the anterior or posterior quadrants, and active tooth movement will be required to correct the crossbite.

FIGURE 11-32 Permanent teeth often erupt in abnormal positions as a result of retained primary teeth. A, These lower central incisors erupted lingually because the permanent incisors have not been lost and their tooth buds are positioned lingual to the primary incisors. This is a common occurrence in this area and is the main reason lingual arches should not be placed until after lower incisors erupt. B, This maxillary premolar has been deflected facially because of the retained primary molar. In both the circumstances shown here, removal of the retained primary tooth or teeth will allow some spontaneous alignment.
Ectopic Eruption
Eruption is ectopic when a permanent tooth causes either resorption of a primary tooth other than the one it is supposed to replace or resorption of an adjacent permanent or primary tooth. When the permanent lateral incisor erupts, resorption of the primary canine is common. Loss of one or both primary canines from ectopic eruption usually indicates lack of enough space for all the permanent incisors but occasionally may result solely from an aberrant eruption path of the lateral incisor. Space analysis, including an assessment of the anteroposterior incisor position and the facial profile, is needed to determine whether space maintenance, space management, space regaining, or more complex treatment is indicated. In some patients, this type of ectopic eruption is just a symptom of the temporary incisor crowding that is normal in the early mixed dentition (see Chapter 4) and not an indication of long-term crowding. These problems can become complex when the midline shifts and causes localized space problems combined with arch asymmetry. For this reason, management of all but the most basic problems associated with lateral incisor ectopic eruption are better managed in specialty practice, and addressed in Chapter 12.
When one primary canine is lost, treatment is needed to prevent a shift of the midline. Depending on the overall space assessment, the dentist can take several approaches. If the space is adequate and no midline shift has occurred, the position of the lateral incisor on the side of the canine loss can be stabilized using a lingual arch with a spur (Figure 11-33). If both mandibular primary canines are lost, the permanent incisors can tip lingually, which reduces the arch circumference and increases the apparent crowding. A passive lingual arch to prevent lingual tipping and maintain adequate space is indicated. If the midline has moved, even with adequate space, or the midline has moved and space has been lost, the problems rapidly become complex. These types of problems need to be resolved prior to canine eruption and are addressed in Chapter 12.
Maxillary First Molars
Ectopic eruption of a permanent first molar presents an interesting problem that is usually diagnosed from routine bitewing radiographs rather than clinically because it is painless. When only small amounts of resorption (<1 to 1.5 mm) are observed (Figure 11-34), a period of watchful waiting is indicated because self-correction is possible and occurs in about two-thirds of the cases. If the blockage of eruption persists for 6 months or if resorption continues to increase, treatment is indicated. Lack of timely intervention may cause loss of the primary molar and space loss as the permanent molar erupts mesially and rotates mesiolingually.
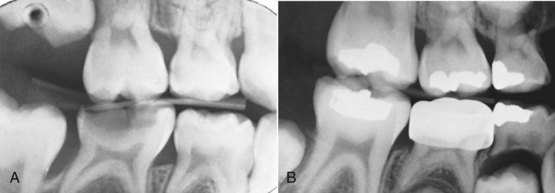
FIGURE 11-34 Ectopic eruption of the permanent first molar is usually diagnosed from routine bitewing radiographs. If the resorption is limited, immediate treatment is not required. A, The distal root of the primary maxillary second molar shows minor resorption from ectopic eruption. B, This radiograph taken approximately 18 months later illustrates that the permanent molar was able to erupt without treatment.
Several methods can be helpful when intervention is necessary.14 The basic approach is to move the ectopically erupting tooth away from the primary molar it is resorbing. If a limited amount of movement is needed but little or none of the permanent first molar is visible clinically, a 20 or 22 mil brass wire looped and tightened around the contact between the primary second molar and the permanent molar is suggested (Figure 11-35). It may be necessary to anesthetize the soft tissue to place the brass wire, and depending on the tooth position and depth of the contact between the permanent and primary molars, it can be difficult to successfully direct the brass wire subgingivally. The brass wire should be tightened at each adjustment visit, approximately every 2 weeks, so that it will not move in relation to the teeth. If the wire is not tightened to the point that the patient feels some discomfort, it has not been appropriately adjusted. Treatment is slow but reliable.
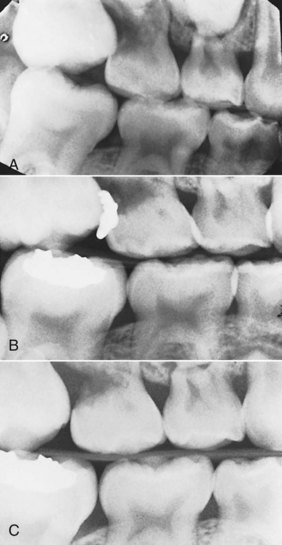
FIGURE 11-35 Moderately advanced resorption from ectopic eruption of the permanent maxillary first molar requires active intervention. A, This distal root of the primary maxillary second molar shows enough resorption that self-correction is highly unlikely. B, A 20 or 22 mil dead soft brass wire is guided under the contact (starting from either the facial or lingual and proceeding with the most advantageous approach) and then looped around the contact between the teeth and tightened at approximately 2-week intervals. C, The permanent tooth is dislodged distally and erupts past the primary tooth that is retained.
A steel spring clip separator, available commercially, may work if only a small amount of resorption of the primary molar roots exists. These clips are difficult to place if the point of contact between the permanent and primary molars is much below the cement-enamel junction of the primary molar, although some are available that have greater vertical distances for just these situations (Figure 11-36). They can be activated on a biweekly basis.

FIGURE 11-36 An Arkansas spring, a scissors-like spring that extends below the contact point, can be effective in tipping a permanent first molar distally so that it can erupt. The posterior bow is crimped to bring the subgingival legs together and apply pressure to separate the teeth.
Elastomeric separators wedged mesial to the first molar also can be used to push it distally so it can erupt but are not recommended. The current elastomeric separators are large. They are well retained for normally positioned teeth, but they require substantial force to place them below the contact of an impacted molar. They have the potential to become dislodged in an apical direction and cause periodontal irritation. If this occurs, the separators are hard to locate and retrieve, especially if the material is not radiopaque.
If resorption is severe and more distal movement is required than can be provided by these simple appliances, the situation becomes more complex. If access can be gained to the occlusal surface of the molar, a simple fixed appliance can be fabricated to move the molar distally. The appliance consists of a band on the primary molar (which can be further stabilized with a transpalatal arch) with a soldered spring that is bonded to the permanent molar (Figure 11-37). In lieu of using a soldered appliance that must be fabricated in the laboratory, a similar but alternative appliance can be fabricated intraorally, either a band and looped spring (Figure 11-38, A) or two bonded brackets (a first molar bracket on the primary molar and a second molar bracket on the first molar) and a looped spring (Figure 11-38, B). Using either appliance, if the movement is not sufficient in 2 weeks, the loop can be reactivated.
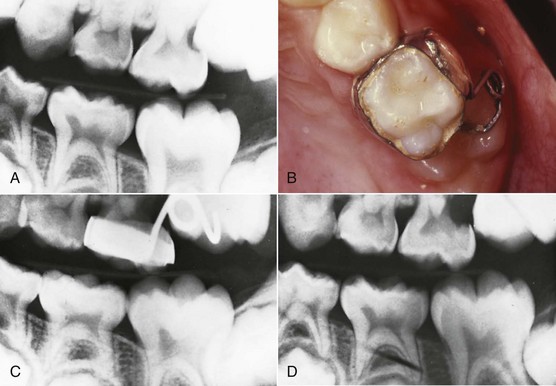
FIGURE 11-37 Ectopic eruption with severe resorption may require appliance therapy. A, This primary maxillary second molar shows severe resorption. B, If the occlusal surface of the permanent molar is accessible, the primary molar can be banded and a 20 mil spring soldered to the band. C, The permanent molar is tipped distally out of the resorption defect and (D) once disengaged, is free to erupt.
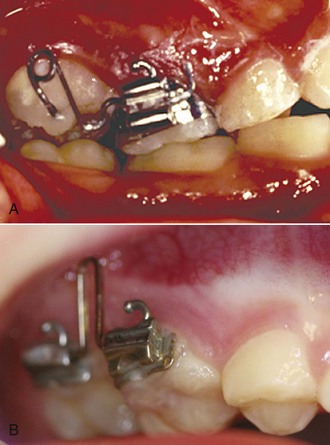
FIGURE 11-38 A fixed appliance to reposition an ectopically erupting maxillary first molar can be fabricated intraoral with a savings of time and laboratory expense. A, To make a band and spring appliance, a band with an attachment having a buccal tube is cemented on the primary second molar. Next, a large omega-shaped loop and a helical loop are bent distal to the primary molar. The spring is activated, and the wire is inserted into the primary molar tube from the distal and secured with a bend anterior to the molar tube. The helical loop is compressed during bonding to the occlusal surface of the permanent first molar. The appliance is reactivated intraorally by opening the omega loop with a loop-forming pliers with the round beak positioned superior to the wire. B, Another option for repositioning an ectopically erupting first molar is to bond archwire tubes on both the primary second molar and the permanent first molar. Then, bend an opening loop from either rectangular beta-Ti or stainless steel wire and compress it to seat from the distal into the primary molar tube and from the mesial into the permanent molar tube. The force from the activated loop will retain the rectangular wire, which can be carefully positioned adjacent to the soft tissue.
If the permanent molar has caused extensive resorption of the primary molar, there may be no choice but to extract the primary tooth, which allows the permanent molar to continue to move mesially and shorten the arch length. Unless the second premolar is missing and the arch length is purposefully to be reduced or unless considerable mesial molar movement is tolerable and later premolar extraction is planned, a distal shoe that guides the erupting molar should be placed after the extraction (see below). Even if this technique is used, some space has already been lost and the permanent molar will have to be repositioned distally after it fully erupts using another type of space-regaining appliance as described later in this chapter and in Chapter 12.
A flowchart summarizes the decision making for ectopic eruption of permanent first molars (Figure 11-39).
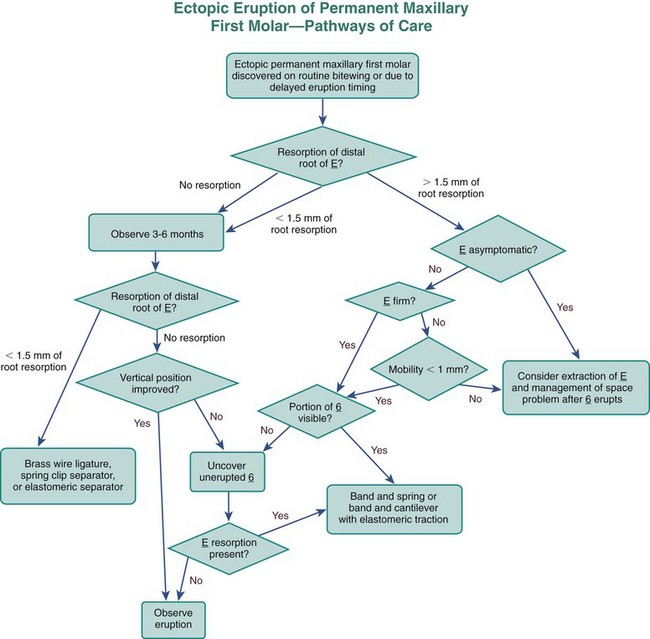
FIGURE 11-39 This flowchart can be used to aid decision making regarding possible options when a permanent molar is ectopically erupting during the mixed dentition. Answers to the questions posed in the chart should lead to successful treatment pathways. (Modified from Kennedy D, Turley P. Am J Orthod Dentofac Orthop 92:336-345, 1987.)
Maxillary Canines
At approximately age 10, if the primary canine is not mobile and there is no observable or palpable facial canine bulge, ectopic eruption of maxillary canines should be considered because it is a relatively frequent occurrence (the incidence of ectopic eruption and impaction of canines is in the 1% to 2% range).15 This can lead to either or both of two problems: (1) impaction of the canine and/or (2) resorption of permanent lateral and/or central incisor roots.16 There appears to be a genetic basis for this eruption phenomenon, and in some cases, it is related to small or missing maxillary lateral incisors and missing second premolars.17 Root resorption of the permanent incisors is significantly more likely to occur when no space is available for the canine.18
Although multiple studies now have shown that cone-beam computed tomography (CBCT) images are superior to two-dimensional (2-D) images for both localization of impacted canines and evaluation of resorption of roots of other teeth,19 it is probably better to get a full view of the status of the patient first with a digital panoramic radiograph because dental anomalies are genetically related, and other anomalies may well be present (peg or missing lateral incisors, missing premolars, and transposed teeth).20 Then, depending on the findings, it is more sensible to obtain detailed information on root resorption and position of the canine eruption from a small field-of-view (FOV) CBCT (Figure 11-40). These views can be supplemented with a traditional cephalometric digital image if required for limited or comprehensive orthodontic care. This is less radiation than to initially obtain a full field CBCT (see Table 6-6).
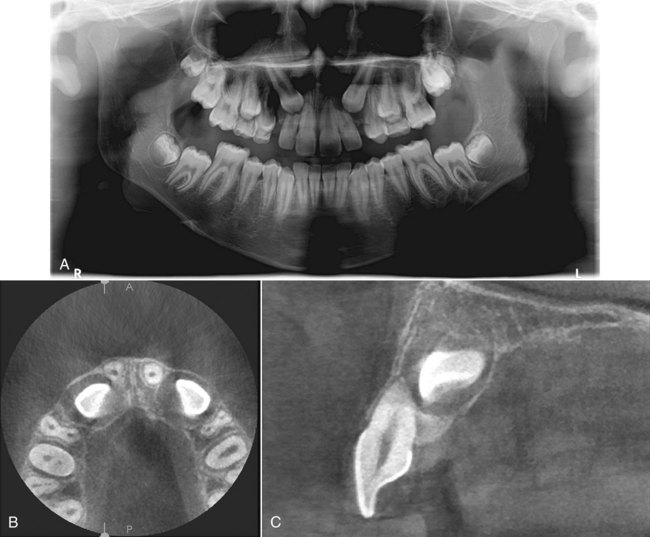
FIGURE 11-40 A, Panoramic radiograph showing damage to the maxillary lateral incisor roots from ectopically erupting canines. B and C, 3-D images from small field-of-view CBCT, which clarify the position of the unerupted canines, show that the right central incisor root also has been damaged, and establish the initial direction of movement of the canines that will be needed to prevent further damage to the incisors. The radiation exposure for a CBCT of this type is about the same as with a digital panoramic radiograph, and in a situation like this, CBCT is needed because of its potential to change the treatment plan.
Given the potential complications of continued ectopic canine eruption, early diagnosis and intervention are warranted to either prevent or limit root resorption. When a mesial position of the erupting permanent canine is detected and incisor root resorption is threatened but has not yet occurred, extraction of the primary canine is indicated (Figure 11-41). Ericson and Kurol found that if the permanent canine crown was overlapping less than half of the root of the lateral incisor, there was an excellent chance (91%) of normalization of the path of eruption. When more than half of the lateral incisor root was overlapped, early extraction of the primary tooth resulted in a 64% chance of normal eruption and likely improvement in the position of the canine even if it was not totally corrected.21
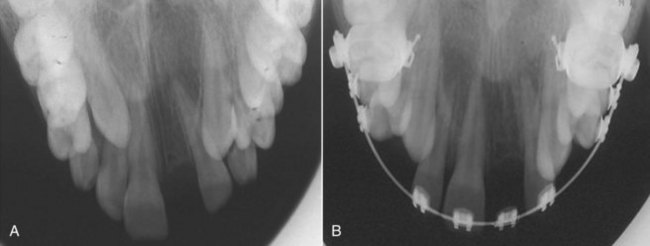
FIGURE 11-41 A, This patient has a maxillary right canine positioned over the root of the maxillary right lateral incisor with more than 50% overlap. The left permanent canine overlapped less than 50% of the permanent lateral incisor root. This type positioning is associated with an increased risk of resorption of the incisor roots. The adjacent primary canines were extracted and, B, improvement was observed as the right canine nearly totally corrected while the left one made only minor changes in lateral position. This probably would not have occurred without the intervention.
If resorption of the permanent lateral or central incisor roots is occurring, usually it is necessary to surgically expose the permanent canine and use orthodontic force to bring it to its correct position (Figure 11-42). This will stop the resorption caused by the ectopic tooth, but some continued resorption and blunting of the roots may continue. This comprehensive treatment will extend into the early permanent dentition period (see Chapter 14).
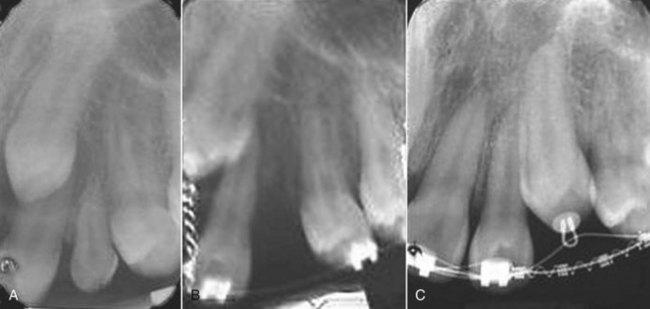
FIGURE 11-42 A, The maxillary left canine is positioned over the root of the adjacent lateral incisor and causing some initial root resorption. B, Because of the resorption, the primary canine was extracted, the crown of the permanent canine was exposed surgically, and an attachment and metal chain were bonded to its crown and ligated to the archwire. Attachments sometimes are difficult to bond because of contamination of the tooth surface by saliva and hemorrhage, but the alternative approach of looping a wire around the cervical part of the crown is no longer recommended. That requires more extensive bone removal and increases the risk of ankylosis and potential reduced gingival attachment. Using an acid etch as opposed to a combination etch/sealant usually will stop hemorrhage for a short time to enable the bonding. C, Subsequently, the canine was repositioned distally away from the lateral incisor and into its correct position. This limited the continued resorption of the lateral incisor.
Supernumerary Teeth
Supernumerary teeth can disrupt the normal eruption of other teeth and cause crowding or spacing. Treatment is aimed at extracting the supernumeraries before problems arise or at minimizing the effect if other teeth have already been displaced.
The most common location for supernumerary teeth is the anterior maxilla. These teeth are often discovered on a panoramic or occlusal radiograph when a child is about 6 to 7 years of age, either during a routine examination or when permanent incisors fail to erupt. The simple cases are those in which a single supernumerary tooth is present and superficially located. If the tooth is not inverted, it will often erupt before or along with the normal tooth and can be extracted before it interferes with the adjacent teeth.
The choice of which tooth to retain and which one is the supernumerary can be difficult, but in reality it makes no difference. The tooth that should be retained is the one with the best size, color, morphology, and position related to the other teeth. All other things being equal, the tooth that is nearest to the ultimate final position should be retained. These decisions are difficult to make from conventional radiographs when the teeth are unerupted, and CBCT can be helpful.
In a few instances, multiple supernumerary teeth are located superficially, and uncomplicated extractions can be performed without interfering appreciably with the normal teeth. As a general rule, the more supernumeraries there are, the more abnormal their shape and the higher their position, the harder it will be to manage the situation. Several abnormal supernumeraries are likely to have disturbed the position and eruption timing of the normal teeth before their discovery, and tubercle teeth are unlikely to erupt. Extractions should be completed as soon as the supernumerary teeth can be removed without harming the developing normal teeth (Figure 11-43). The surgeon may wish to delay extraction until continued growth has improved both access and the child’s ability to tolerate surgery and until further root development has improved the prognosis for the teeth that will remain. This is reasonable, but the earlier the supernumeraries can be removed, the more likely that the normal teeth will erupt without further intervention. Conversely, the later the extractions, the more likely it is that the remaining unerupted normal teeth will need surgical exposure, orthodontic traction, or both to bring them into the arch.
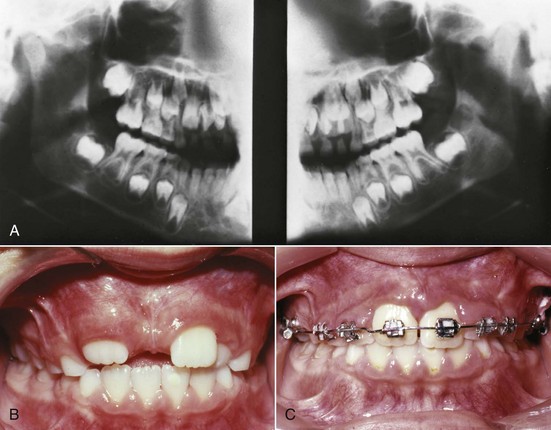
FIGURE 11-43 Multiple supernumerary teeth in the anterior maxilla, although rare, can cause spacing and delayed eruption of anterior teeth. A, This patient has an exceptionally wide diastema and delayed eruption of the maxillary lateral incisors. B, The panoramic radiograph reveals three supernumeraries of various shapes and orientations. Conical and noninverted supernumeraries usually erupt, whereas tubercle-shaped and inverted ones do not. C, The supernumeraries were removed, the diastema closed, and the incisors were aligned with fixed appliances after they erupted.
Delayed Incisor Eruption
When an incisor has failed to erupt more than a year past the normal eruption time and adjacent teeth have erupted, there is no excuse for delaying treatment. The esthetic and social consequences along with the impact on ultimate eruption and development of the dentition are bound to be significant. These situations require timely intervention. A retained primary tooth, supernumerary tooth, or some type of pathology is most commonly associated with delayed incisor eruption.
The first consideration in evaluating this situation is the morphology (usability) of the unerupted tooth and its position. Then the likelihood that the tooth will erupt or can be brought into the arch must be considered. Next is the need for space in the arch. If there is enough space available and the tooth is likely to erupt without orthodontic traction, surgically uncovering it is warranted. If the delayed incisor is located superficially, it can be exposed with a simple soft tissue excision and usually will erupt rapidly.
When the tooth is more deeply positioned, the overlying and adjacent tissue should be repositioned apically to expose the crown (Figure 11-44). This usually leads to normal eruption, but if there is any doubt regarding the potential for eruption or adequate exposure, the tooth should have an attachment placed on it. A metal chain (not a wire ligature around the cervical portion of the tooth) is attached to the bracket or button and extended out of the tissue so traction can be applied using a fixed appliance, if necessary (Figure 11-45). If space is not adequate, preoperative space opening should have been accomplished so the sequence of treatment is seamless. Generally, the force against the unerupted tooth is applied using a heavy base wire with bonded brackets on several teeth for anchorage and either elastomeric chain or a nickel–titanium (NiTi) overlay wire to supply the force. The chain is good for initial movement because it is not as irritating to the soft tissue. As the tooth erupts, often the bracket requires repositioning since the initial bonding during the surgical procedure was less than ideal. Final root positioning can be left until a second stage of treatment during the permanent dentition if one is anticipated.

FIGURE 11-44 A, This patient had a superficially positioned permanent maxillary right central incisor that was unerupted and substantially delayed. B, The radiograph shows the tooth at the crestal bone level. C, The flap has been released on both sides, repositioned apically and sutured in place while leaving adequate exposed tooth structure. If there is doubt that the tissue is controlled, an attachment and metal chain should be bonded to the exposed tooth. The chain can be ligated to the orthodontic appliances. If no appliances are in place, it can be ligated to the cervical of an adjacent tooth. If the tooth erupts, the attachment can easily be discarded, but it is good insurance in the event of abnormal healing. D, One-week postsurgery, the tissue is healing well. E, Appliances in place for the final positioning. Note the uneven gingival borders of the two central incisors, which will become more similar with age as the left central incisor’s attachment migrates apically.


FIGURE 11-45 A, For initial traction to an unerupted incisor it is acceptable to use a heavy base archwire and elastomeric chain to the teeth. Although this places relatively heavy forces on the teeth and has limited range, the limited invasiveness and bulk make it a sensible starting method. B, A simple and more efficient option is to use the flexibility of a superelastic auxiliary archwire (A-NiTi) while stabilizing with another stiffer wire to control the reciprocal forces. This is accomplished by tying the superelastic wire over the base archwire, except in the area of the unerupted tooth, and deflecting it gingivally to provide the traction. Remember, the longer the overlay wire, the more resistance it will create as it slides through the brackets and ligatures and the less effective it will be. The overlay wire should be tied with steel ligatures to further reduce friction and released at adjustment appointments so the wire regains its superelastic properties. As the tooth erupts, it can be incorporated in a continuous flexible wire or the base wire will have to be offset to allow for the bracket to pass it.
Ankylosed Primary Teeth
Ankylosed primary teeth with permanent successors, especially ankylosed primary molars, constitute a potential alignment problem for the permanent teeth. Although these teeth usually resorb without creating long-term problems, occasionally they fail to resorb or are retained by a bony attachment in the cervical region. This delays the erupting permanent tooth and can deflect it from the normal eruption path. Appropriate management of an ankylosed primary molar consists of maintaining it until an interference with eruption or drift of other teeth begins to occur (Figure 11-46), then extracting it and placing a lingual arch or other appropriate fixed appliance if needed. If adjacent teeth have tipped over the ankylosed tooth, they will need to be repositioned to regain space. Vertical bony discrepancies will be eradicated when the permanent tooth brings bone with it during eruption.
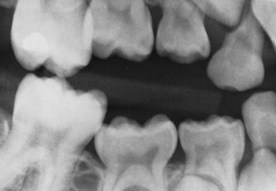
FIGURE 11-46 This radiograph demonstrates both anterior and posterior teeth tipping over adjacent ankylosed primary molars. The ankylosed teeth should be removed if significant tipping and space loss are occurring.
The situation is completely different when an ankylosed primary tooth has no permanent successor. Then, to avoid long-term periodontal problems, the ankylosed tooth should be extracted before a large vertical occlusal discrepancy develops (Figure 11-47).22 Because erupting teeth bring alveolar bone with them, in planning and executing treatment it is best to move teeth at least partially into the edentulous space so that new bone is created there, even if the long-range plan is prosthetic replacement of the missing tooth. Space maintenance therefore is contraindicated. The longer the ankylosed primary tooth is left in place, the greater the chance of a long-term defect because alveolar bone is not formed in that area. Although extraction of the primary tooth without a successor will result in some loss of alveolar bone, this is preferable to a long-term periodontal problem.
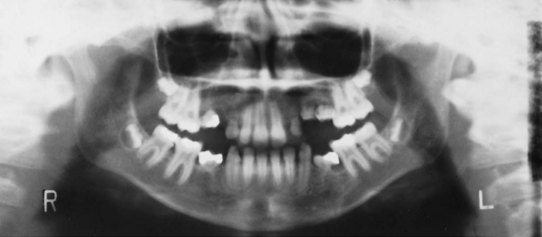
FIGURE 11-47 If they have no successors, ankylosed primary teeth should be carefully removed when vertical discrepancies begin to develop. It is better to allow permanent teeth to drift into the edentulous space and bring bone with them, and then reposition the teeth prior to implant or prosthetic replacement, so that large periodontal defects, such as those adjacent to the primary molars in this patient, do not develop.
It is advisable to have an experienced clinician remove these teeth. Unless the extraction is managed carefully, an even worse periodontal defect may occur.
Management of Space Problems
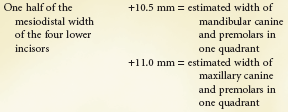
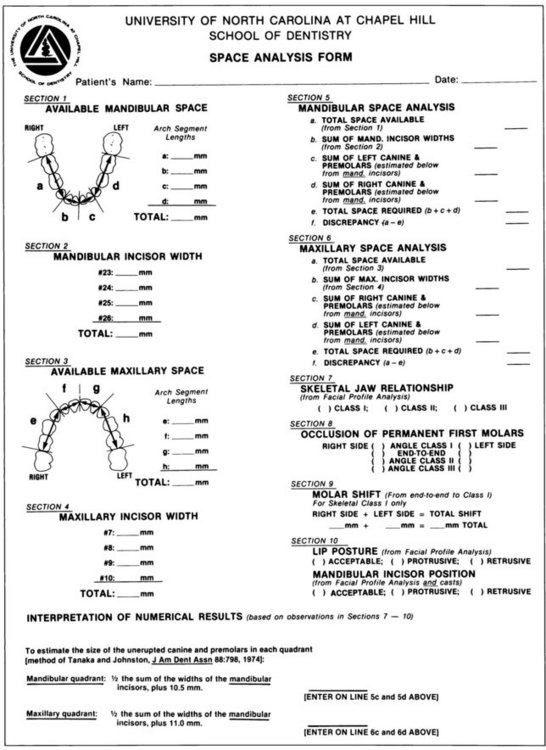
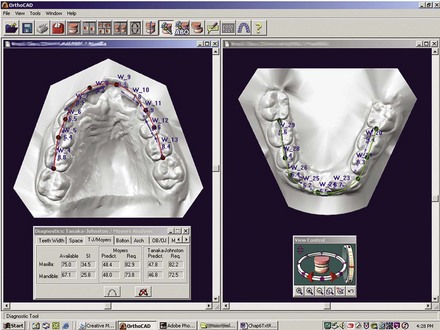
Space Analysis: Quantification of Space Problems
Space problems must be considered from the viewpoint of the space available, which is quantified by the space analysis. The space analysis results must be considered in the context of the profile because reducing protrusion reduces the amount of available space. Conversely, when teeth are retroclined and then moved facially to the correct position, more space is available. The vertical dimension also has an impact on space. It is generally contraindicated to expand when there is limited overbite because tipping teeth facially usually moves them vertically as well and an anterior open bite may develop. In a child with a deep overbite and an accentuated curve of Spee, leveling the arch will make teeth more protrusive.
It is important to quantify the amount of crowding within the arches because treatment varies, depending on the severity of the crowding. Space analysis, using the dental casts, is required for this purpose. Such an analysis is particularly valuable in evaluating the likely degree of crowding for a child in the mixed dentition when the permanent teeth are erupting and real or transitional crowding is evident, and in that case it must include prediction of the size of unerupted permanent teeth.
Principles of Space Analysis
Space analysis requires a comparison between the amount of space available for the alignment of the teeth and the amount of space required to align them properly in the dental arches (Figure 11-48). The analysis can be done either directly on the dental casts or by a computer algorithm after appropriate digitization of the arch and tooth dimensions (by scanning the casts, either in the dental office or at a commercial company).
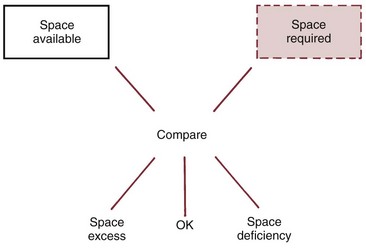
FIGURE 11-48 A comparison of space available to space required establishes whether a deficiency of space within the arch will ultimately lead to crowding, whether the correct amount of room is available to accommodate the teeth, or whether excess space will result in gaps between the teeth.
Whether the space analysis is done manually or in the computer, the first step is calculation of space available. This is accomplished by measuring arch perimeter from the mesial of one first molar to the other, over the contact points of posterior teeth and incisal edge of anteriors. There are two basic ways to accomplish this manually: (1) by dividing the dental arch into segments that can be measured as straight line approximations of the arch (Figure 11-49) or (2) by contouring a piece of wire (or a curved line on the computer screen) to the line of occlusion and then straightening it out for measurement. The first method is preferred for manual calculation because of its greater reliability. Either method can be used with an appropriate computer program.
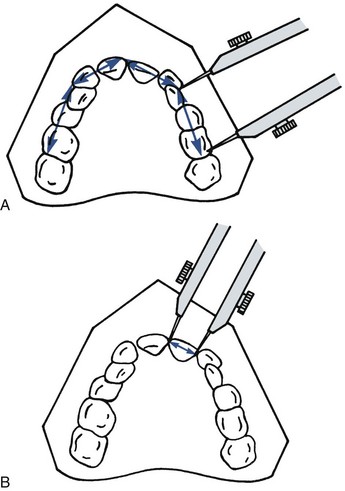
FIGURE 11-49 A, Space available can be measured most easily by dividing the dental arch into four straight segments as shown. Each segment is measured individually with a divider or sharpened Boley gauge. B, Space required is the sum of the mesiodistal widths of all individual erupted permanent teeth plus the estimated sizes of the unerupted permanent teeth.
The second step is to calculate the amount of space required for alignment of the teeth. This is done by measuring the mesiodistal width of each erupted tooth from contact point to contact point, estimating the size of unerupted permanent teeth, and then summing the widths of the individual teeth (see Figure 11-49, B). If the sum of the widths of the permanent teeth is greater than the amount of space available, there is a space deficiency and crowding would occur. If available space is larger than the space required (excess space), gaps between some teeth would be expected.
Space analysis carried out in this way is based on three important assumptions: (1) the anteroposterior position of the incisors is correct (i.e., the incisors are neither excessively protrusive nor retrusive), (2) the space available will not change because of growth and dental compensatory tipping, and (3) all the teeth are present and reasonably normal in size. None of these assumptions can be taken for granted. All of them must be kept in mind when space analysis is done.
With regard to the first assumption, it must be remembered that incisor protrusion is relatively common and that retrusion, though uncommon, does occur. There is an interaction between crowding of the teeth and protrusion or retrusion: if the incisors are positioned lingually (retruded), this accentuates any crowding; but if the incisors protrude, the potential crowding will not be fully expressed. Crowding and protrusion are really different aspects of the same phenomenon. If there is not enough room to properly align the teeth, the result can be crowding, protrusion, or (most likely) some combination of the two. For this reason, information about how much the incisors protrude must be available from clinical examination to evaluate the results of space analysis. This information comes from facial form analysis (or from cephalometric analysis if available).
The second assumption, that space available will not change during growth, is valid for most but not all children. In a child with a well-proportioned face, there is little or no tendency for the dentition to be displaced relative to the jaw during growth, but the teeth often shift anteriorly or posteriorly in a child with a jaw discrepancy. For this reason, space analysis is less accurate and less useful for children with skeletal problems (Class II, Class III, long face, short face) than in those with good facial proportions.
Even in children with well-proportioned faces, the position of the permanent molars changes when primary molars are replaced by the premolars (see Chapter 3 for a detailed review). If space analysis is done in the mixed dentition, it is necessary to adjust the space available measurement to reflect the shift in molar position that can be anticipated.
The third assumption can (and must) be checked by clinical and radiographic examination, looking at the teeth as a set rather than as individual units. Anomalies in tooth size have significant implications for space in the dental arches (see Figure 5-23).
Estimating the Size of Unerupted Permanent Teeth
There are two basic approaches to doing this:
1. Measurement of the Teeth on Radiographs: This requires an undistorted radiographic image, which is achieved with individual periapical radiographs. Even with individual radiographs, it is often difficult to obtain an undistorted view of the canines, and this inevitably reduces the accuracy. With any type of radiograph, it is necessary to compensate for enlargement of the radiographic image. This can be done by measuring an object that can be seen both in the radiograph and on the casts, usually a primary molar tooth. A simple proportional relationship can then be set up. Accuracy is fair to good, depending on the quality of the radiographs and their position in the arch. The technique can be used in maxillary and mandibular arches for all ethnic groups, but the radiation burden is justified only in unusual cases.
2. Estimation from Proportionality Tables: There is a reasonably good correlation between the size of the erupted permanent incisors and the unerupted canines and premolars. These data have been tabulated for white American children by Moyers.23 To use the Moyers prediction tables, the mesiodistal width of the lower incisors is measured, and this number is used to predict the size of both the lower and upper unerupted canines and premolars. The size of the lower incisors correlates better with the size of the upper canines and premolars than does the size of the upper incisors because upper lateral incisors are extremely variable teeth. Despite a tendency to overestimate the size of unerupted teeth, accuracy with this method is fairly good for the northern European white children on whose data it is based. No radiographs are required, and it can be used for the upper or lower arch.
Tanaka and Johnston developed another way to use the width of the lower incisors to predict the size of unerupted canines and premolars (Box 11-1).24 For children from a European population group, the method has good accuracy despite a small bias toward overestimating the unerupted tooth sizes. It requires neither radiographs nor reference tables (once the simple equation is memorized), which makes it very convenient, but specifically it tends to overestimate the required space for Caucasian females in both arches and underestimate the space required in the lower arch for African-American males.
Most computer algorithms for space analysis are based on correlations of tooth sizes, and should be used with caution if the radiographs show anything unusual (unless the computer program allows for introduction of radiographic information).
Summary: Which of these methods is best for an individual patient depends on the circumstances. The prediction tables work surprisingly well when applied to the population group from which they were developed, white school children of northern European descent. On balance, the Tanaka-Johnston method probably is most practical for manual calculation because no radiographs are required and the simple ratio can be printed right on the space analysis form or memorized, so that no reference tables must be consulted.
On the other hand, if the patient does not fit the population group from which the correlations were derived, as an African or Asian child would not, direct measurement from the radiographs is the best approach, and computer analysis should be avoided unless a modified equation from Tanaka-Johnston is available for that particular group. In addition, if obvious anomalies in tooth size or form are seen in the radiographs, the correlation methods (which assume normal tooth size relationships) should not be used.
A contemporary form for mixed dentition space analysis is shown in Figure 11-50. Note that (1) a correction for mesial movement of the lower molars following the exchange of the dentition is included, (2) the Tanaka-Johnston method for predicting the size of unerupted canines and premolars is used, and (3) the result from facial form analysis is requested to check for appropriateness of the analysis and for interpretation of the results. A screen capture from a commercial computer analysis is shown in Figure 11-51. Computer analysis is faster and easier, but it is important to remember that its accuracy will depend on the accuracy of the digitized input and how well the patient meets the assumptions that underlie a correlation approach.
Treatment of Space Problems
In the section of the chapter that follows, you will recognize that the problems become increasingly more complex but are still within reach of many general practitioners. Other space problems, more complex still, usually would be addressed in a specialty practice and are discussed in Chapter 12.
Premature Tooth Loss with Adequate Space: Space Maintenance
Early loss of a primary tooth presents a potential alignment problem because drift of permanent or other primary teeth is likely unless it is prevented. Space maintenance is appropriate only when adequate space is available, and when all unerupted teeth are present and at the normal stage of development. If a permanent successor will erupt within 6 months (i.e., if more than one-half to two-thirds of its root has formed), a space maintainer is unnecessary. If there is not enough space for the permanent tooth or if it is missing, space maintenance alone is inadequate or inappropriate, and the other treatment approaches discussed below will be needed.
Several treatment techniques can be used successfully for space maintenance, depending on the specific situation. Because these appliances are at risk for breakage and loss, they must be monitored carefully to be successful.
Band-and-Loop Space Maintainers
The band and loop is a unilateral fixed appliance indicated for space maintenance in the posterior segments. The simple cantilever design makes it ideal for isolated unilateral space maintenance (Figure 11-52). Because the loop has limited strength, this appliance must be restricted to holding the space of one tooth and is not expected to accept functional forces of chewing. Although bonding a rigid or flexible wire across the edentulous space has been advocated as an alternative, this has not proved satisfactory clinically. It also is no longer considered advisable to solder the loop portion to a stainless steel crown because this precludes simple appliance removal and replacement. Teeth with stainless steel crowns should be banded like natural teeth.
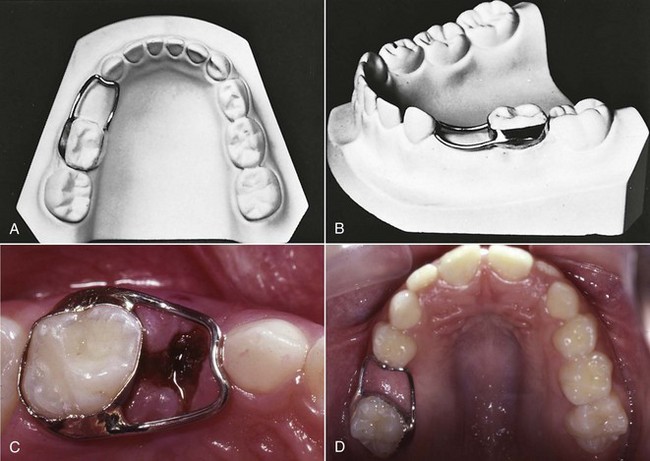
FIGURE 11-52 A band-and-loop space maintainer is generally used in the mixed dentition to save the space of a single prematurely lost primary molar. It consists of a band on either a primary or permanent molar and a wire loop to maintain space. A, The loop portion made from 36 mil wire is carefully contoured to the abutment tooth without restricting lateral movement of the primary canine and (B) the loop is also contoured to within 1.5 mm of the alveolar ridge. The solder joints should fill the angle between the band and wire to avoid food and debris accumulation. C, A completed band-and-loop maintainer in place after extraction of a primary first molar. D, An occlusal rest, shown here on the primary first molar, can be added to the loop portion to prevent the banded teeth from tipping mesially.
If a primary second molar has been lost, the band can be placed on either the primary first molar or the erupted permanent first molar. Some clinicians prefer to band the primary tooth in this situation because of the risk of decalcification around any band, but primary first molars are challenging to band because of their morphology, which converges occlusally and makes band retention difficult. A more important consideration is the eruption sequence of the succedaneous teeth. The primary first molar should not be banded if the first premolar is developing more rapidly than the second premolar because loss of the banded abutment tooth would require replacement of the appliance because the abutment tooth was lost.
Before eruption of the permanent incisors, if a single primary molar has been lost bilaterally, a pair of band-and-loop space maintainers is recommended instead of the lingual arch that would be used if the patient were older. This is advisable because the permanent incisor tooth buds are lingual to the primary incisors and often erupt lingually. The bilateral band and loops enable the permanent incisors to erupt without interference from a lingual wire. At a later time, the two band-and-loop appliances can be replaced with a single lingual arch if necessary.
The survival of band and loops is not impressive. It has been judged to be approximately 18 months with cement failure cited as the most frequent problem.25 This speaks to the need to evaluate these space maintainers at routine recall visits.
Partial Denture Space Maintainers
A partial denture is most useful for bilateral posterior space maintenance when more than one tooth has been lost per segment and the permanent incisors have not yet erupted. In these cases, because of the length of the edentulous space, band-and-loop space maintainers are contraindicated, and the likely lingual position of the permanent incisors at initial eruption makes the lingual arch a poor choice. The partial denture also has the advantage of replacing some occlusal function.
Another indication for this appliance is posterior space maintenance in conjunction with replacement of missing primary or delayed permanent incisors (Figure 11-53). Anterior space maintenance is unnecessary because arch circumference generally is not lost even if the teeth drift and redistribute the space. Anterior teeth are not required for nutrition or speech development and children adapt readily to missing teeth in most cases, so replacement of missing anterior teeth is done solely to improve appearance. This may have social advantages, however, even for young children.

FIGURE 11-53 In a young child, a removable partial denture is used to replace anterior teeth for esthetics. At the same time, it can maintain the space of one or more prematurely lost primary molars. For this patient, the four incisors are replaced by the partial denture. Multiple clasps, preferably Adams’ clasps, are necessary for good retention. Both the clasps and the acrylic need frequent adjustment to prevent interference with physiologic adjustment of primary teeth during eruption of permanent teeth. The C-clasps on the primary canines provide limited retention and are good examples of clasps that need continued careful attention.
Distal Shoe Space Maintainers
The distal shoe has a unique application and is the appliance of choice when a primary second molar is lost before eruption of the permanent first molar. This appliance consists of a metal or plastic guide plane along which the permanent molar erupts. The guide plane is attached to a fixed or removable retaining device (Figure 11-54). When fixed, the distal shoe is usually retained with a band instead of a stainless steel crown so that it can be replaced by another type of space maintainer after the permanent first molar erupts. Unfortunately, this design limits the strength of the appliance and provides no functional replacement for the missing tooth. If primary first and second molars are missing, the appliance must be removable and the guide plane is incorporated into a partial denture because of the length of the edentulous span. This type of appliance can provide some occlusal function.
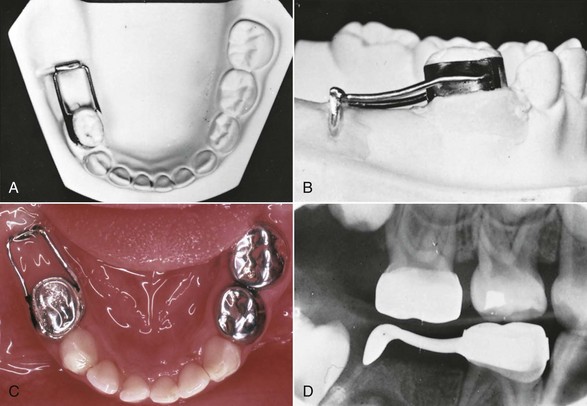
FIGURE 11-54 The distal-shoe space maintainer is indicated when a primary second molar is lost before eruption of the permanent first molar and is usually placed at or very soon after the extraction of the primary molar. A, The loop portion, made of 36 mil stainless steel wire, and the intraalveolar blade are soldered to a band so the whole appliance can be removed and replaced with another space maintainer after the permanent molar erupts. B, The loop portion must be contoured closely to the ridge since the appliance cannot resist excessive occlusal forces from the opposing teeth. C, This distal-shoe space maintainer was placed at the time of extraction of the primary second molar. D, The blade portion must be positioned so that it extends approximately 1 mm below the mesial marginal ridge of the erupting permanent tooth to guide its eruption. This position can be measured from pretreatment radiographs and verified by a radiograph taken at try-in or postcementation. An additional occlusal radiograph can be obtained if the faciolingual position is in doubt.
To be effective, the guide plane must extend into the alveolar process so that it is located approximately 1 mm below the mesial marginal ridge of the permanent first molar, at or before its emergence from the bone. An appliance of this type is tolerated well by most children but is contraindicated in patients who are at risk for subacute bacterial endocarditis or are immunocompromised because complete epithelialization around the intraalveolar portion has not been demonstrated.26 Careful measurement and positioning are necessary to ensure that the blade will ultimately guide the permanent molar. Faulty positioning and loss of the appliance are the most common problem with this appliance.
Lingual Arch Space Maintainers
A lingual arch is indicated for space maintenance when multiple primary posterior teeth are missing and the permanent incisors have erupted (Figure 11-55, A and B). A conventional lingual arch, attached to bands on the primary second or permanent first molars and contacting the maxillary or mandibular incisors, prevents anterior movement of the posterior teeth and posterior movement of the anterior teeth.
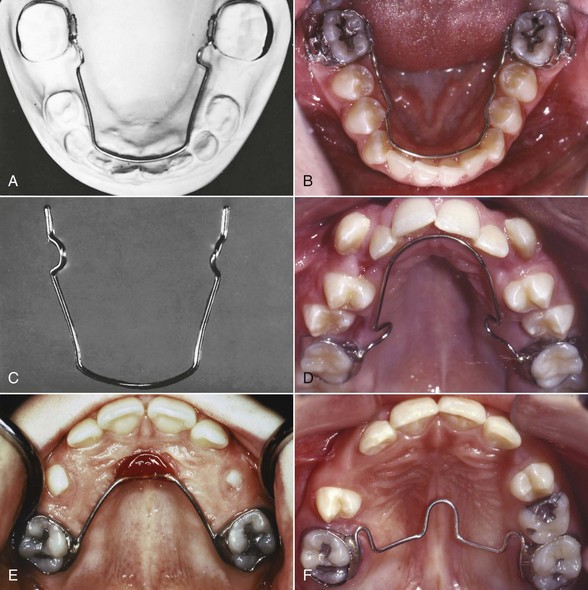
FIGURE 11-55 A lingual holding arch usually is the best choice to maintain space for premolars after premature loss of the primary molars when the permanent incisors have erupted. A, The lingual arch is made of 36 mil wire with adjustment loops mesial to the permanent first molars. B, This soldered lingual arch successfully maintained the space for the premolars. C, The lingual arch is stepped away from the premolars to allow their eruption without interference, which results in a keyhole design. The wire is also 1.5 mm away from the soft tissue at all points. D, A maxillary lingual arch is used when the overbite is not excessive, or (E) a Nance arch with an acrylic button in the palatal vault is indicated if the overbite is excessive. The palatal button must be monitored because it may cause soft tissue irritation. F, The transpalatal arch prevents a molar from rotating mesially into a primary molar extraction space, and this largely prevents its mesial migration. Several teeth should be present on at least one side of the arch when a transpalatal design is employed as a sole space maintainer.
A lingual arch space maintainer is usually soldered to the molar bands but can be fabricated to be removable by the doctor. Removable lingual arches (e.g., those that fit into attachments welded onto the bands) are more prone to breakage and loss. Regardless of whether it is removable, the lingual arch should be positioned to rest on the cingula of the incisors, approximately 1 to 1.5 mm off the soft tissue, and should be stepped to the lingual in the canine region to remain away from the primary molars and unerupted premolars so there is no interference with their eruption (Figure 11-55, C). Lingual arches should have ideal arch form so the teeth can align if they have space. Making the arch conform to dental irregularities is not appropriate. Approximately 25% to 30% of lingual arch type appliances fail, usually due to cement loss and solder joint breakage. Their survival time is estimated at less than 24 months.27 Careful instructions to parents and patients can reduce these problems, but regular recall is advisable.
Maxillary lingual arches as space maintainers are not familiar to many clinicians, but are contraindicated only in patients whose bite depth causes the lower incisors to contact the archwire on the lingual of the maxillary incisors (Figure 11-55, D). When bite depth does not allow use of a conventional design, either the Nance lingual arch (Figure 11-55, E) or a transpalatal arch (Figure 11-55, F) can be used. The Nance arch is an effective space maintainer, but soft tissue irritation can be a problem. The best indication for a transpalatal arch is when one side of the arch is intact and more than one primary tooth is missing on the other side. In this situation, the rigid attachment to the intact side usually provides adequate stability for space maintenance. When primary molars have been lost bilaterally, however, both permanent molars may tip mesially despite the transpalatal arch, and a conventional lingual arch or Nance arch is preferred.
A flowchart is provided to help guide decision making for space maintenance (Figure 11-56).
Localized Space Loss (3 mm or Less): Space Regaining
Potential space problems can be created by drift of permanent incisors or molars after early extraction of primary canines or molars, which usually begins during the first 6 months after extraction. Then, repositioning the teeth to regain space and reduce the space discrepancy to zero, followed by a space maintainer, is necessary to prevent further drift and space loss until the succedaneous teeth have erupted. A space maintainer alone is not adequate treatment for a space deficiency.
Up to 3 mm of space can be reestablished in a localized area with relatively simple appliances and a good prognosis. Space loss greater than that constitutes a severe problem and usually requires comprehensive treatment to achieve acceptable results. The methods to regain major space loss are considered in Chapter 12. The treatment necessary to regain the space during the mixed dentition, especially if a second stage of treatment will be required in any event, may be more than is reasonable when one analyzes the cost/benefit ratio. Extraction with space closure often is a better choice. In that circumstance, often the crowding can be accepted during the mixed dentition so that the ultimate space closure occurs under control when the complete fixed appliances are present.
Maxillary Space Regaining
Generally, space is easier to regain in the maxillary than in the mandibular arch because of the increased anchorage for removable appliances afforded by the palatal vault and the possibility for use of extraoral force (headgear). Permanent maxillary first molars can be tipped distally to regain space with either a fixed or removable appliance, but bodily movement requires a fixed appliance. Because the molars tend to tip forward and rotate mesiolingually, distal tipping and de-rotation to regain 2 to 3 mm often is satisfactory.
A removable appliance retained with Adams’ clasps and incorporating a helical fingerspring adjacent to the tooth to be moved is very effective. This appliance is the ideal design for distally tipping one molar (Figure 11-57). One posterior tooth can be moved up to 3 mm distally during 3 to 4 months of full-time appliance wear. The spring is activated approximately 2 mm to produce 1 mm of movement per month. The molar generally will de-rotate spontaneously as it is tipped distally.
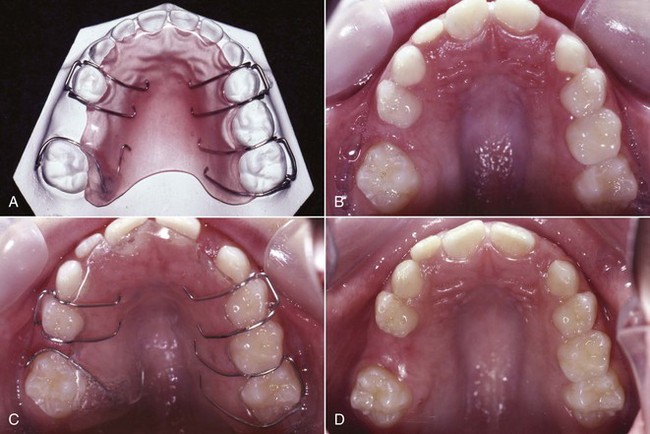
FIGURE 11-57 A removable appliance with a fingerspring can be used to regain space by tipping a permanent first molar distally. A, The appliance incorporates multiple Adams’ clasps and a 28 mil helical spring that is activated 1 to 2 mm per month. B, Premature loss of the primary second molar has led to mesial drift and rotation of the permanent first molar. C, This removable appliance can be used to regain up to 3 mm of space. D, After space regaining, the space should be maintained with a band and loop or lingual arch if the permanent incisors have erupted.
For unilateral space regaining with bodily movement of the permanent first molar, a fixed appliance is preferred. The anchorage provided by the remaining teeth can support the forces generated by a coil spring on a segmental archwire, with good success (Figure 11-58), but to be effective, the support of a modified Nance arch usually is needed.
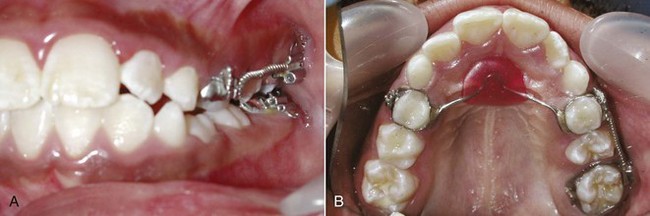
FIGURE 11-58 A, A fixed appliance also can be used to regain space in the maxillary posterior regions, with a coil spring generating the distalizing force. B, Palatal anchorage was gained using a Nance arch and the erupted teeth.
Regardless of the method used to regain space, a space maintainer is required when adequate space has been restored. A fixed space maintainer is recommended, rather than trying to maintain the space with the removable appliance that was used for space regaining because it may become distorted and allow inadvertent space loss.
Regaining bilateral localized space loss of any amount is more complex and is discussed in Chapter 12.
Mandibular Space Regaining
For moderate amounts of space regaining, removable appliances can be used in the mandibular arch just as they are in the maxillary arch, but as a rule they are less satisfactory because they are more fragile and prone to breakage. They do not fit as well and lack the palatal anchorage support. Problems with tissue irritation frequently are encountered, and patient acceptance tends to be poorer than with maxillary removable appliances.
For unilateral mandibular space regaining, the best choice is a fixed appliance. A lingual arch can be used to support the tooth movement and provide anchorage when used in conjunction with a segmental archwire and coil spring (Figure 11-59).
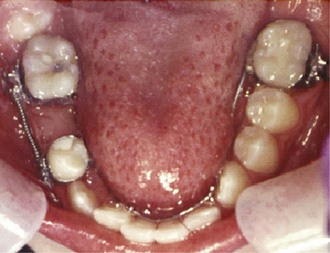
FIGURE 11-59 Moving molars distally in the mandibular arch, especially unilaterally, is quite challenging and requires support from a number of teeth. Using a lingual arch to incorporate anchorage from the permanent and primary molars, as well as the incisors, and force from a coil spring on a segmental archwire can be effective.
If space has been lost bilaterally due to lingual incisor tipping, there are two choices short of bands and brackets: a lip bumper or an adjustable lingual arch. With the lip bumper, which is a labial appliance fitted to tubes on the molar teeth (Figure 11-60), the idea is that the appliance presses against the lip, which creates a distal force to tip the molars posteriorly without affecting the incisors. Although some posterior movement of the molars can be observed when a lip bumper is used, the appliance also alters the equilibrium of forces against the incisors, removing any restraint from the lip on these teeth. The result is forward movement of the incisors.28 Depending on the type of lip bumper used and its clinical manipulation, transverse widening also may occur.

FIGURE 11-60 A, A lip bumper constructed of a 36 mil wire bow with an acrylic pad, which fits into tubes on the permanent first molars, is sometimes used to increase arch length. This occurs when the appliance stretches the lower lip and transmits force to move the molars back. The appliance also disrupts the equilibrium between the lip and tongue and allows the anterior teeth to move facially. The result is nearly equal molar and incisor change. This appliance can be used for either minor space regaining or for moderate arch expansion. B, The lip bumper is ligated in place so that it remains in the proper position during treatment and to increase compliance. Periodically, it needs to be advanced a couple of millimeters facial to the incisors so they can migrate facially.
When an active lingual arch pits posterior movement of both molars against the anchorage offered by the incisors, significant forward displacement of the incisors must be expected (Figure 11-61). The expansion can be accomplished by slightly opening the loops located mesial to the banded molars. Small amounts of activation are necessary since the wire is large and capable of delivering heavy forces. The appliance can then serve as a passive retainer or be replaced with a soldered lingual arch.
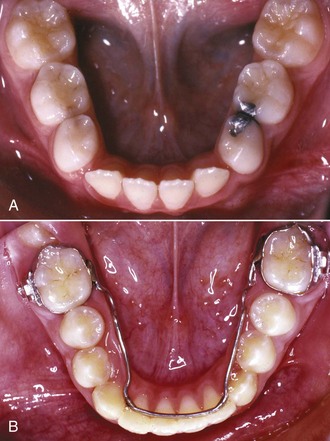
FIGURE 11-61 A, Limited space regaining or moderate lower arch expansion can be accomplished using a lingual arch when the incisors have good alignment and little spacing, as in this patient who requires additional arch length to accommodate the unerupted premolars and canines. B, When the lingual arch is placed and is active, it will rest high on the lingual surface of the incisors and should exert a downward tipping force. Two or three 1 to 1.5 mm activations at 4 to 6 week intervals will achieve the desired movement.
On balance, the effects of an active lingual arch and a lip bumper are similar. A lingual arch can be left in place as a space maintainer after space has been regained. A lip bumper is not a good space maintainer and should be replaced with a lingual arch when long-term maintenance of the regained space is needed.
Bilateral molar distalization to regain space or moving the mandibular midline to resolve an asymmetric loss are both considered complex problems and are addressed in Chapter 12.
Mild-to-Moderate Crowding of Incisors with Adequate Space
Irregular Incisors, Minimal Space Discrepancy
In some children, space analysis shows that enough space for all the permanent teeth ultimately will be available, but relatively large permanent incisors and the clinical reality of the “incisor liability” (see Chapter 4) cause transient crowding of the permanent incisors. This crowding is usually expressed as mild faciolingual displacement or rotation of individual anterior teeth.
Studies of children with normal occlusion indicate that when they go through the transition from the primary to the mixed dentition, up to 2 mm of incisor crowding may resolve spontaneously without treatment. From this perspective, as a general rule there is no need for treatment when mild incisor crowding is observed during the mixed dentition. Not only is correction of this small amount of crowding probably not warranted, but also there is no evidence that long-term stability will be greater if the child receives early treatment to improve alignment. The only reason for treatment is temporary esthetic improvement.
If exaggerated parental concern makes mild or moderate crowding a problem, one could consider disking the interproximal enamel surfaces of the remaining primary canines and first primary molars (Figure 11-62) as the anterior teeth erupt. This can help with faciolingual discrepancies but not rotations. It is possible to gain as much as 3 to 4 mm of anterior space through this procedure, but the teeth may align in a more lingual position and actually make the space problem worse. Remember, at this point in the transitional dentition no disking or interproximal stripping should be attempted on permanent teeth. This could create a tooth-size discrepancy that later will be difficult to resolve. Permanent tooth stripping should not be undertaken until all the permanent teeth have erupted and their interarch size relationships can be evaluated.
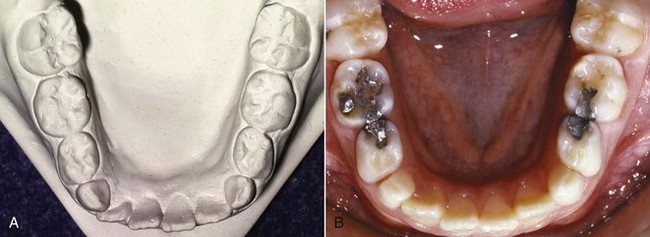
FIGURE 11-62 Disking can be used on multiple surfaces of primary teeth, especially the primary canines, when limited transitional crowding is apparent. A, This pretreatment cast shows minor anterior crowding. B, Disking of the mesial and distal surfaces of the primary canines allowed spontaneous alignment to occur without appliance therapy.
Correction of incisor rotations caused by this transitional crowding requires space and controlled movement to align and de-rotate them, using an archwire and bonded attachments on the incisors. It is rare that a child who needs this type of treatment in the mixed dentition does not require further treatment after all permanent teeth have erupted, so extensive early treatment is usually not indicated.
Space Deficiency Largely Due to Allowance for Molar Shift—Space Management
In some children, more severe transitional crowding occurs when the incisors erupt. Space analysis often shows that the space available is adequate or nearly so. A major component of the projected space deficiency is the allowance for mesial movement of the permanent first molars to a Class I relationship when the second primary molars are lost. For these patients, if the loss of leeway space could be prevented, there would be little or no space deficiency. Gianelly reported that in patients seeking treatment at Boston University, 75% would have approximately enough space to align the teeth if molar drift were prevented.29 One can look at these children from either of two perspectives: (1) there is minimal benefit from early treatment unless there are major esthetic concerns, and therefore little or no reason to intervene, or alternatively (2) this group does not need much treatment, it should be relatively easy to provide, and there is always the possibility that if early treatment is done, later treatment might not be necessary.
Rather than beginning treatment in the early mixed dentition, the current recommendation for children with moderate crowding but little or no space discrepancy is to begin intervention with a lingual arch in the late mixed dentition, just before the second primary molars exfoliate. The transitional incisor crowding would simply be tolerated up to that time, on the theory that it could be corrected along with other crowding in the arch when the space occupied by the large second primary molars became available. In these patients, beginning comprehensive treatment earlier is judged not to be cost-effective—it takes longer for both patient and doctor, without producing a better long-term result.
A primary indication does exist, however, for starting treatment earlier in some of these patients who have overall adequate space but various amounts of transitional crowding. This is early loss of one primary canine as the lateral incisors erupt. Loss of both primary canines usually indicates more severe crowding and an overall arch length deficiency that may indicate a different treatment approach, as outlined below. When one primary canine is lost, placement of a lingual arch will maintain arch symmetry and midline relationships, and will prevent distal movement of the incisors that shortens arch length (Figure 11-63).30 The lingual arch should be left in position until the second premolars erupt, so the start of comprehensive treatment can be delayed. With this approach to space management, there also is some evidence for better postretention and long term stability.31
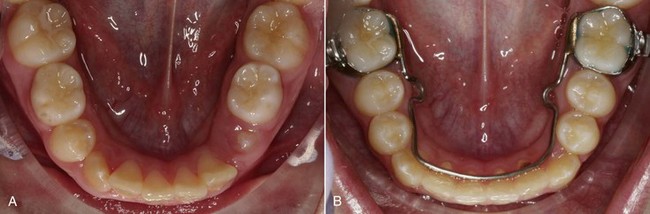
FIGURE 11-63 A lingual arch in conjunction with primary tooth extraction or exfoliation can be an effective way to take advantage of the leeway space and reduce crowding. A, The primary second molars are in place, and there is some anterior crowding that is within the range of the leeway space. B, With the lingual arch in place to take advantage of the leeway space, the second premolars erupted and incisor and canine alignment improved spontaneously.
In the absence of early loss of primary teeth, the major reason for early intervention in a child who has transitional crowding is esthetic concern because of the obvious crowding. If the parents insist on doing something sooner rather than later, a combination of early extraction of primary canines and disking to reduce the width of primary molars can provide space to allow the permanent incisors and canines to erupt and align. This can be carried further posteriorly in the arch by disking the second primary molar to allow the first premolars to erupt (Figure 11-64). The minimum orthodontic appliance therapy is a lingual arch that will support the incisor teeth and control the molar position and arch perimeter by preventing any mesial shift. If necessary, the lingual arch can be activated slightly to tip molars distally and incisors facially to obtain a modest increase in arch length (see Figure 11-61). A lip bumper also can be used in the lower arch to maintain the position of the molars or perhaps tip them slightly distally, while removing lip pressure and allowing the incisors to move facially.

FIGURE 11-64 Disking primary posterior teeth in conjunction with space maintenance is an effective method to use the leeway space and all available arch length. Note that the disking must be completed perpendicular to the occlusal plane so that the height of contour of the tooth is reduced. Occlusally convergent slices that do not reduce the mesiodistal width of the tooth are not helpful.
When space is created in this way, the incisors often align spontaneously if the irregularity is from faciolingual tipping, but rotations are less likely to resolve. An exception is the child whose incisor segment is straight, without anterior arch curvature. In these children, extraction of primary canines usually leads to spacing of the incisors or maintenance of essentially the same arch form. Alignment does not improve even when the space is available and a lingual arch is in place to serve as a template for tooth position (Figure 11-65). Correction of incisor rotations or residual irregularity in incisor position requires a fixed appliance, using an archwire and bonded attachments on the incisors. Accepting some incisor crowding and deferring treatment until as late as possible—when the premolars are erupting—usually is the best judgment.
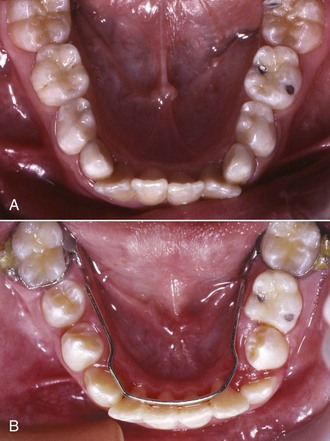
FIGURE 11-65 Anterior crowding combined with a straight anterior incisor segment. A and B, Straight incisor segments with lateral incisors that overlap the mesial of the primary canine usually do not align into ideal arch form when the primary canines are extracted, even if a lingual arch is used.
Because the molars have not been allowed to shift forward into the leeway space when space management is employed, they often are maintained in the end-to-end relationship that is normal before the premolars erupt, instead of moving into a Class I relationship. For that reason, correction of the molar relationship also must become a goal of treatment. Doing this during the second phase of treatment, when a complete fixed appliance is available, is the most efficient approach. The techniques used for molar correction are discussed in detail in Chapter 15.
Generalized Moderate Crowding
A child with a generalized arch length discrepancy of 2 to 4 mm and no prematurely missing primary teeth can be expected to have moderately crowded incisors. This occurs in about 25% of each ethnic group in the United States (see Figure 1-13). Unless the incisors are severely protrusive, the long-term plan would be generalized expansion of the arch to align the teeth. The major advantage of doing this in the mixed dentition is esthetic, and the benefit is largely for the parents, not the child.
If the parents strongly desire early treatment for moderate crowding, in the mandibular arch an adjustable lingual arch is the appliance of choice for simple expansion by tipping tooth movement. In the maxilla, either a removable or fixed appliance can be employed (Figure 11-66). Keep in mind that rotated incisors usually will not correct spontaneously even if space is provided, so early correction would require bonded attachments for these teeth.
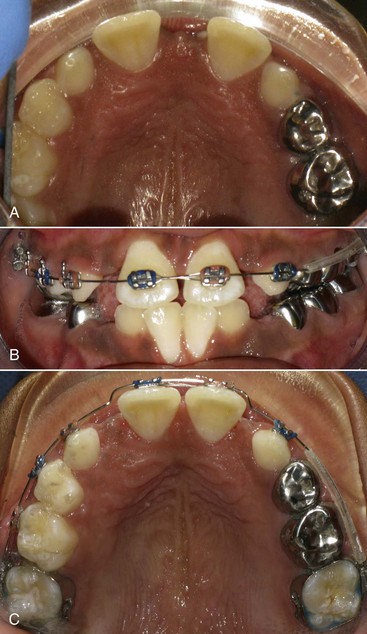
FIGURE 11-66 Limited maxillary appliances can be used in the mixed dentition to align teeth and distribute space. A, This patient had unerupted maxillary lateral incisors as a result of the large midline diastema. B and C, The teeth were aligned and the diastema closed. Note the tubing that protects the patient’s lip from the expanse of continuous wire on the patient’s left side.
Other Tooth Displacements
Spaced and Flared Maxillary Incisors
In children with spaced and flared maxillary incisors who have Class I molar relationships and good facial proportions, space analysis should show that the space available is excessive rather than deficient. This condition often is found in the mixed dentition after prolonged thumb-sucking and frequently occurs in connection with some narrowing of the maxillary arch. A thumb or finger habit should be eliminated before attempting to retract the incisors. Physiologic adaptation to the space between the anterior teeth requires placing the tongue in this area to seal off the gap for successful swallowing and speech. This “tongue thrust” is not the cause of the protrusion or open bite and should not be the focus of therapy. If the teeth are retracted, the tongue thrust will disappear as the tongue adapts to the new morphology.
If the upper incisors are flared forward and there is no contact with the lower incisors, the protruding upper incisors can be retracted quite satisfactorily with a removable appliance. A Hawley-type appliance utilizing multiple clasps and a labial bow can be effective for this purpose (Figure 11-67). Of course, the patient must be cooperative in wearing the appliance, and it must be constructed with adequate retention and a flexible labial bow (28 mil wire). Incorporating loops in the bow can aid the flexibility. During the course of treatment the appliance is adjusted approximately 2 mm per month to achieve 1 mm of lingual tipping of the incisors and space closure. The palate-covering plastic lingual to the incisors must be removed to provide space for posterior movement of the teeth and gingiva. After space closure, the teeth need to be retained with either a lingual bonded retainer or the existing removable appliance.
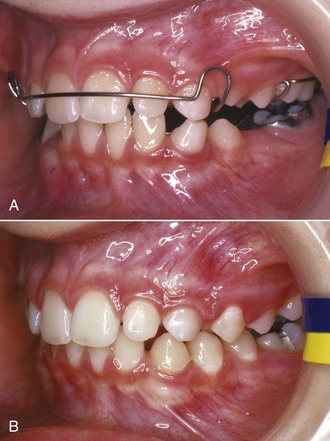
FIGURE 11-67 A removable appliance can be used in the mixed dentition to retract spaced and protruding anterior teeth. A, The labial bow is activated 1.5 to 2 mm and will achieve approximately 1 mm of retraction per month as the maxillary anterior teeth tip lingually. At each appointment, the labial bow should be adjusted and lingual acrylic removed to provide space for the tooth movement. B, A near normal occlusion in the late mixed dentition.
On the other hand, if there is a deep overbite, protruding upper incisor teeth cannot be retracted until it is corrected. The lower incisors biting against the lingual of the upper incisors prevent the upper teeth from being moved lingually. Even if anteroposterior jaw relationships are Class I, a skeletal vertical problem may be present, and complex treatment is likely to be required.
Teeth that are flared and rotated or that require bodily movement during retraction are more difficult to move and control. This is a complex problem and discussed in Chapter 12.
Maxillary Midline Diastema
A small maxillary midline diastema, which is present in many children, is not necessarily an indication for orthodontic treatment. The unerupted permanent canines often lie superior and distal to the lateral incisor roots, which forces the lateral and central incisor roots toward the midline while their crowns diverge distally (Figure 11-68). In its extreme form, this condition of flared and spaced incisors is called the “ugly duckling” stage of development (see Chapter 4). These spaces tend to close spontaneously or at least reduce in size when the canines erupt and the incisor root and crown positions change—the prevalence of a midline diastema drops from about 25% in the early mixed dentition to approximately 7% at ages 12 to 17).1 Until the permanent canines erupt, it is difficult to be certain whether the diastema will close completely or only partially.

FIGURE 11-68 The “ugly duckling” phase of dental development. A, Spacing and mesial root position of the maxillary incisors results from the position of the unerupted permanent canines. B, This panoramic radiograph shows that the canines are erupting and in close proximity to the roots of the lateral incisors. The spaces between the incisors, including the midline diastema, decrease and often completely disappear when the canines erupt.
A small but unesthetic diastema (2 mm or less) can be closed in the early mixed dentition by tipping the central incisors together. A maxillary removable appliance with clasps, fingersprings, and possibly an anterior bow can successfully complete this type of treatment (Figure 11-69). Under no circumstances should an unsupported elastic be looped around the central incisors—there is a high probability that the elastic will slip apically and destroy the periodontal attachment. The elastic can become an effective way to extract the teeth.
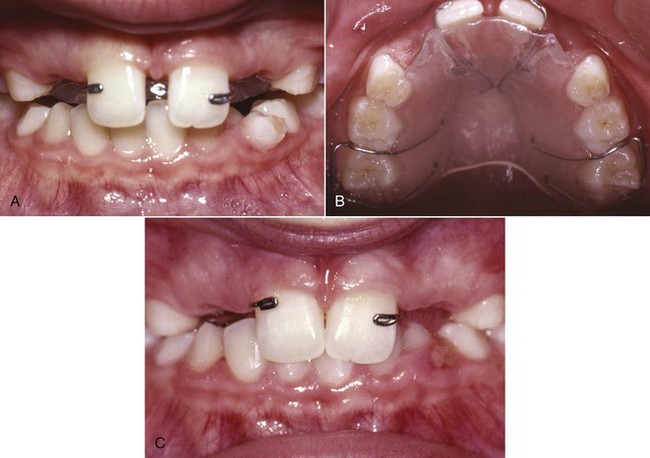
FIGURE 11-69 A, Closure of a midline diastema can be accomplished with a removable appliance and fingersprings to tip the teeth mesially. B, The 28 mil helical fingersprings are activated to move the incisors together. C, The final position can be maintained with the same appliance.
When a larger diastema (>2 mm) is present, a midline supernumerary tooth or intrabony lesion must always be suspected (Figure 11-70), and complete spontaneous closure is unlikely. A diastema this large is disproportionately prevalent in the African-American population. Depending on what radiographs are already available, one of several images may be appropriate—a panoramic radiograph, a maxillary occlusal radiograph, or a maxillary anterior CBCT with a small field of view. Missing permanent lateral incisors also can lead to a large space between the central incisors because the permanent central incisors frequently move distally into the available space. Some digit-sucking habits can lead to diastemas and spacing.


FIGURE 11-70 In the mixed dentition, sizable diastemas should be investigated to determine if they are the result of a supernumerary tooth, pathology, or missing permanent lateral incisors. In this case, at least one lateral incisor is present along with the diastema (A), but the accompanying radiograph (B) shows that a midline supernumerary is present. Clearly, the cause dictates different treatment responses.
Whatever its cause, a diastema greater than 2 mm is unlikely to close spontaneously.32
This type of treatment will usually require bodily tooth movement and is addressed in Chapter 12.
Sometimes the soft tissue of the midline frenum attachment is blamed for the space between the central incisors, but it is hard to be sure whether this is the case. Usually it is advisable to proceed with the tooth movement and determine if there are further problems with retention. If there are, then a frenectomy can be considered if there is excessive tissue bunched up in the midline. Early frenectomy should be avoided.
References
1. Brunelle, JA, Bhat, M, Lipton, JA. Prevalence and distribution of selected occlusal characteristics in the US population, 1988-91. J Dent Res. 1996;75:706–713.
2. Adkins, MD, Nanda, RS, Currier, GF. Arch perimeter changes on rapid palatal expansion. Am J Orthod. 1990;97:10–19.
3. Harrison JE, Ashby D. Orthodontic treatment for posterior crossbites. Cochrane Database of System Rev 1:Art. No.: CD000979. DOI: 10.1002/14651858.CD000979, 2001.
4. Godoy, F, Godoy-Bezerra, J, Rosenblatt, A. Treatment of posterior crossbite comparing 2 appliances: a community-based trial. Am J Orthod Dentofac Orthop. 2011;139:e45–e52.
5. Petrén, S, Bjerklin, K, Bondemark, L. Stability of unilateral posterior crossbite correction in the mixed dentition: a randomized clinical trial with a 3-year follow-up. Am J Orthod Dentofac Orthop. 2011;139:e73–e81.
6. Ngan, P, Hu, AM, Fields, HW. Treatment of Class III problems begins with differential diagnosis of anterior crossbites. Pediatr Dent. 1997;19:386–395.
7. Ngan, P, Fields, H. Open bite: a review of etiology and management. Pediatr Dent. 1997;19:91–98.
8. Melink, S, Vagner, MV, Hocevar-Boltezar, I, et al. Posterior crossbite in the deciduous dentition period: its relation with sucking habits, irregular orofacial functions, and otolaryngological findings. Am J Orthod Dentofac Orthop. 2010;138:32–40.
9. Scavone Jr, H, Guimarães Jr, CH, Ferreira, RI, et al. Association between breastfeeding duration and non-nutritive sucking habits. Am J Orthod Dentofac Orthop. 2010;137:54–58.
10. Duncan, K, McNamara, C, Ireland, AJ, et al. Sucking habits in childhood and the effects on the primary dentition: findings of the Avon Longitudinal Study of Pregnancy and Childhood. Int J Paediatr Dent. 2006;18:178–188.
11. Warren, JJ, Slayton, RL, Bishara, SE, et al. Effects of nonnutritive sucking habits on occlusal characteristics in the mixed dentition. Pediatr Dent. 2005;27:445–450.
12. Haryett, R, Hansen, R, Davidson, P, et al. Chronic thumbsucking: the psychological effects and the relative effectiveness of the various methods of treatment. Am J Orthod. 1967;53:559–585.
13. Villa, NL, Cisneros, GJ. Changes in the dentition secondary to palatal crib therapy in digit-suckers. Pediatric Dent. 1997;19:323–326.
14. Kennedy, DB, Turley, PK. The clinical management of ectopically erupting first permanent molars. Am J Orthod Dentofac Orthop. 1987;92:336–345.
15. Aydin, U, Yilmaz, HH, Yildirim, D. Incidence of canine impaction and transmigration in a patient population. Dentomaxillofacial Radiol. 2004;33:164–169.
16. Naoumova, J, Kurol, J, Kjellbert, H. A systematic review of the interceptive treatment of palatally displaced maxillary canines. Eur J Orthod. 2011;33:143–149.
17. Garib, DG, Alencar, BM, Lauris, JR, et al. Agenesis of maxillary lateral incisors and associated dental anomalies. Am J Orthod Dentofac Orthop. 2010;137:e1–e6. [732].
18. Cernochova, P, Krupa, P, Izakovicova-Holla, LA. Root resorption associated with ectopically erupting maxillary permanent canines: a computed tomography study. Eur J Orthod. 2011;33:483–491.
19. Botticelli, S, Verna, C, Cattaneo, PM, et al. Two- versus three-dimensional imaging in subjects with unerupted maxillary canines. Eur J Orthod. 2011;33:344–349.
20. Alqerban, A, Jacobs, R, Fieuws, S, et al. Comparison of two cone-beam computed tomographic systems versus panoramic imaging for localization of impacted maxillary canines and detection of root resorption. Eur J Orthod. 2011;33:93–102.
21. Ericson, S, Kurol, J. Early treatment of palatally erupting maxillary canines by extraction of the primary canines. Eur J Orthod. 1988;10:283–295.
22. Kurol, J, Thilander, B. Infraocclusion of primary molars with aplasia of the permanent successor: A longitudinal study. Angle Orthod. 1984;54:283–294.
23. Moyers, RE. Handbook of Orthodontics, 3rd ed. Chicago: Mosby; 1973.
24. Tanaka, MM, Johnston, LE. The prediction of the size of unerupted canines and premolars in a contemporary orthodontic population. J Am Dent Assn. 1974;88:798–801.
25. Sasa, IS, Hasan, AA, Qudeimat, MA. Longevity of band and loop space maintainers using glass ionomer cement: a prospective study. Eur Arch Paediatr Dent. 2009;10:6–10.
26. Mayhew, M, Dilley, G, Dilley, D, et al. Tissue response to intragingival appliances in monkeys. Pediatr Dent. 1984;6:148–152.
27. Moore, TR, Kennedy, DB. Bilateral space maintainers: a 7-year retrospective study from private practice. Pediatr Dent. 2006;28:499–505.
28. Hashish, DI, Mostafa, YA. Effect of lip bumpers on mandibular arch dimensions. Am J Orthod Dentofac Orthop. 2009;135:106–109.
29. Gianelly, AA. Crowding: timing of treatment. Angle Orthod. 1994;64:415–418.
30. Brennan, M, Gianelly, AA. The use of the lingual arch in the mixed dentition to resolve crowding. Am J Orthod Dentofac Orthop. 2000;117:81–85.
31. Little, RM. Stability and relapse: early treatment of arch length deficiency. Am J Orthod Dentofac Orthop. 2002;121(6):578–581.
32. Huang, WJ, Creath, CJ. The midline diastema: a review of its etiology and treatment. Pediatr Dent. 1995;17:171–179.