Complex Nonskeletal Problems in Preadolescent Children
Preventive and Interceptive Treatment
The problems discussed in this chapter are more challenging than those addressed in Chapter 11. Even though they are categorically similar, most require more skill to diagnose and treat—especially to carry out the mechanics to achieve proper tooth and root position while managing the reciprocal effects (anchorage) of forces aimed at more complicated tooth movement. General practitioners will need to be selective and match the treatment problems with their skills.
Eruption Problems
Transposition is a rare positional interchange of two adjacent teeth. It occurs with a prevalence of approximately 0.3% and equally affects males and females.1 There appears to be a genetic component to this problem.2
In the early mixed dentition years, transposition can develop when distally directed eruption of the permanent mandibular lateral incisor leads to loss of the primary mandibular canine and primary first molar (Figure 12-1). If left untreated, this can result in a true transposition of the permanent lateral incisor and canine.3 Interceptive treatment requires repositioning the lateral incisor mesially (Figure 12-1, C), which eliminates the possibility of the complete transposition with the canine. This means either bonding the tooth or gaining surgical access to the tooth and applying traction to tip the tooth back to its natural position. In addition to a labial fixed appliance, a lingual arch usually is required for supplemental anchorage. The benefit of this type of early intervention is that simple tipping movement usually can reposition the tooth. Left until later, bodily movement of the erupted teeth is required. One adverse consequence of this early repositioning is potential resorption of the lateral incisor root because it may be brought into contact with the unerupted canine. This is unlikely but should be discussed with the patient and parents prior to treatment. Beginning treatment before the canine is actively erupting is important.

FIGURE 12-1 A, This radiograph shows that the mandibular lateral incisor is erupting ectopically and has resorbed the roots of the primary canine and first molar. B, Failure to reposition the lateral incisor will lead to true transposition of the permanent lateral and canine. C, The lateral incisors have been repositioned with fixed appliances and are now retained.
Later in the mixed dentition, the more prevalent transposition is of the maxillary canine and first premolar or maxillary canine and lateral incisor.4 Treatment of transpositions involving the maxillary canine if not addressed early is quite challenging. Moving the teeth to their natural positions can be difficult because this requires bodily repositioning, translating the canine facially or lingually past the other tooth. Careful consideration of alveolar width and the integrity of the attached supporting tissue is required. Often, the best approach is to move a partially transposed tooth to a total transposed position or to leave fully transposed teeth in that position. This requires careful finishing with reshaping the transposed teeth to improve both their appearance and fit within the dental arch. Although this can be difficult, the time and difficulty in correcting the transposition is even more challenging.
Primary Failure of Eruption
Primary failure of eruption is characterized by failure of eruption of permanent posterior teeth when there is no overlying mechanical interference, and now is known to have a genetic etiology5 (see Chapter 5). This usually is noted in the late mixed dentition when some or all the permanent first molars still have not erupted and eruption of other posterior teeth in affected quadrants of the dental arch appears abnormal (Figure 12-2). The affected teeth are not ankylosed but do not erupt and do not respond normally to orthodontic force. If tooth movement is attempted, usually the teeth will ankylose after 1 to 1.5 mm of movement in any direction, so obtaining a genetic analysis and confirmation of the diagnosis can help guide treatment and circumvent unwanted reciprocal forces. In the long term, prosthetic replacement of the teeth that failed to erupt, acceptance of premolar occlusion in affected quadrants, or possibly segmental osteotomies (possibly even distraction osteogenesis) after growth is complete are almost the only treatment possibilities.

FIGURE 12-2 Primary failure of eruption is characterized by failure of some or all posterior permanent teeth to erupt even though their eruption path has been cleared. The cause is a failure of the eruption mechanism, apparently due to an abnormal periodontal ligament (PDL), and because of the PDL abnormality, the unerupted permanent teeth do not respond to orthodontic force and cannot be moved into the dental arch even though they are not ankylosed.
Impact of Radiation Therapy and Bisphosphonates
Due to the increased prevalence of successful stem cell transplantation (SCT) and total body irradiation (TBI) for treatment of childhood cancers, more patients with missing teeth and altered tooth morphology are being observed. The early age of SCT (less than 5 years old) is more of a risk factor than TBI.6 Shortened roots are the result of high-dose chemotherapy and TBI, especially when treatment is in the 3 to 5 years age group.7 Because these patients have high survival rates, they now seek orthodontic treatment. Some of the irradiated teeth fail to develop, others fail to erupt, and some may erupt even though they have extremely limited root development. Although the roots are short, light forces can be used to reposition these teeth and achieve better occlusion without fear of tooth loss (Figure 12-3).

FIGURE 12-3 This patient’s panoramic radiograph shows shortening of the roots of multiple permanent teeth following radiation therapy. These teeth can be moved orthodontically, if necessary, with limited objectives and light forces. (Courtesy Dr. D. Grosshandler.)
Children are increasingly receiving bisphosphonates in conjunction with other aggressive and lifesaving therapies. This drug class has known implications for dentistry and orthodontic tooth movement in particular (see Chapter 8).8 Currently, as these patients reach the age when orthodontic tooth movement will be a possibility, it will be important to assess the impact of this therapy. Orthodontic treatment should not be attempted while bisphosphonates are being used.
Traumatic Displacement of Teeth
Immediately following a traumatic injury, teeth that have not been irreparably damaged usually are repositioned with finger pressure to a near normal position and out of occlusal interference. They are then stabilized (with a light wire or nylon filament) for 7 to 10 days. At this point, the teeth usually exhibit physiologic mobility. If the alveolus has been fractured, then the teeth should be stabilized with a heavy wire for approximately 6 weeks. Following either of these initial treatments, if the teeth are not in ideal positions or have consolidated in a facial or lingual position that causes an esthetic problem or occlusal interference, orthodontic treatment to reposition them is indicated, and it can begin at that time, using light force. But even tipping forces can lead to loss of vitality and root resorption for previously traumatized teeth.9 This increased risk also applies to patients who have trauma (more extensive than crown fracture and especially luxation, intrusion, and extrusion injuries) during active orthodontic treatment.10 Prior to moving traumatized teeth, multiple radiographs at numerous vertical and horizontal angulations (or cone-beam CT [CBCT]) with a small field of view should be obtained to rule out vertical and horizontal root fractures that may make it impossible to save the tooth or teeth (Figure 12-4). During orthodontic treatment, it is reasonable to follow the teeth clinically by observing clinical mobility, sensitivity to percussion and cold, and electric pulp testing. The patients should report tooth discoloration, pain, swelling, and any discharge from the surrounding tissues. Radiographically, observation is sensible to determine periapical pathology at 2 to 3 weeks, 6 to 8 weeks, and 1 year. If the apex is complete at the time of the injury, it is more likely that the tooth will become nonvital from luxation injuries. If that happens, pulpal extirpation and treatment is recommended. External root resorption can jeopardize the tooth quite rapidly. Again, pulpal extirpation and treatment is recommended.

FIGURE 12-4 Multiple vertically positioned radiographs are required for an adequate diagnosis of previously traumatized teeth. A, This radiograph displays no periapical pathology 2 weeks after the trauma to the central incisors, but this radiograph (B) exposed at the same time from a different vertical position shows a periapical radiolucency at the apex of the maxillary right central incisor.
Vertical displacement of teeth presents an orthodontic treatment dilemma. If the patient is under 12 years old and if the apex is open, the best option in terms of pulpal necrosis, root resorption, and marginal bone healing is to allow the tooth to re-erupt.11,12 Re-eruption may take several months. In the meantime, the teeth should be monitored as described above. Any signs of nonvitality should be addressed with endodontic treatment. Even with severe intrusion, in the 12 to 17 years age group and with a closed apex, teeth that are allowed to re-erupt have better marginal bone healing, but nearly all of this group will have pulpal necrosis that requires endodontics.11 Based on this background, when the apex is open, it is best to allow re-eruption, regardless of the extent of the injury in a child. If the apex is closed and the intrusion is less than 6 mm, then re-eruption or orthodontic treatment (Figure 12-5) is probably indicated. Intrusions beyond this amount are best addressed by surgery due to the time involved. The goal is to preserve pulpal vitality, but with intruded teeth and the poor pulpal prognosis, repositioning is critical to improve access for endodontics and complete the diagnosis; crown and root fractures can remain undiagnosed even following extensive radiographs. Within 2 weeks of the injury, the intruded tooth should have been moved enough to allow endodontic access to reduce the possibility and extent of resorption. At that point, the tooth should be at or near its pretrauma position; if not, gingivectomy should be used to facilitate access.

FIGURE 12-5 A, For teeth without open apices, traction following intrusion of permanent teeth can ensure adequate endodontic access if necessary. To begin, elastomeric chain can be used. B, A more efficient method is to use a heavy base archwire complemented by a NiTi overlay wire for rapid tooth movement. Note that the base archwire has been stepped facially to allow the bracketed tooth to pass on its lingual side.
When tooth movement during the course of routine orthodontic treatment is indicated for teeth that have had previous intrusion injuries, they are at increased risk for pulp nonvitality.13 Teeth that were extruded at the time of injury and not immediately reduced pose a difficult problem. These teeth have reduced bony support and a poor crown–root ratio. Attempts to intrude them result in bony defects between the teeth, and loss of pulp vitality is a real risk (especially for lateral incisors), so orthodontic intrusion is not a good plan.14 When the discrepancy is minor to moderate, reshaping the elongated tooth by crown reduction may be the best plan (Figure 12-6). This risk also applies to previously traumatized teeth with some obliteration of the pulp. The greater the obliteration, the greater the risk of loss of pulpal vitality during orthodontic treatment.15 An endodontically treated tooth that will need orthodontics can be successfully moved without much fear of resorption either before or after the final fill.16

FIGURE 12-6 A, This patient had extrusive displacement injuries to the permanent incisors. B, Because it is difficult to intrude these teeth and there is a risk of a subsequent bony defect, the crowns of these teeth were reduced to provide a better crown–root ratio and improve the appearance.
Another consideration for patients with traumatically injured anterior teeth that cannot be restored is to retain the root of the compromised tooth until vertical growth is largely completed and an implant can be placed into the area.17 This adjunctive procedure reduces the chance of ridge resorption and the need for later bone grafting. If the tooth is compromised and can still be moved orthodontically, it can be repositioned and the root buried. Root burial entails decorination (removal of the clinical crown and root structure to below the soft tissue level) and closure of the soft tissue. The root can subsequently be removed or the implant placed through it (Figure 12-7).
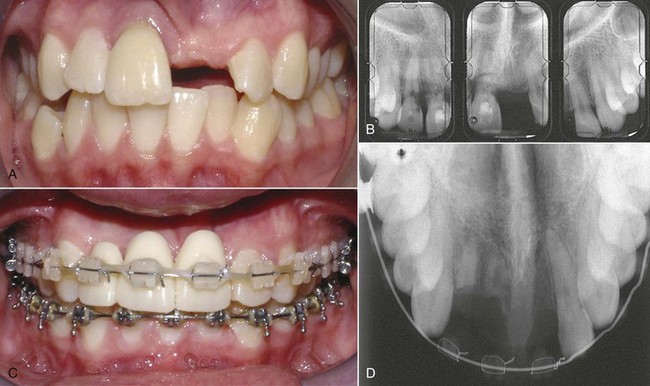
FIGURE 12-7 This patient had root burial to retain the maxillary anterior alveolar bone. A, The maxillary left central incisor was avulsed. B, The maxillary radiograph shows severe resorption of the roots of the maxillary right central and lateral incisors. Instead of extracting these two teeth, they were decorinated (crowns removed and roots covered with soft tissue) to maintain the ridge. C, The pontics are in place during orthodontic treatment for space control and esthetics, while the roots maintain the ridge as seen on the radiograph (D).
Space-Related Problems
Irregular and malaligned teeth in the early mixed dentition arise from two major causes: (1) lack of adequate space for alignment, which causes an erupting tooth to be deflected from its normal position in the arch, and (2) interferences with eruption (drifted and tipped teeth causing space loss, overretained primary teeth, ankylosed primary teeth, supernumerary teeth, transposed teeth, and ectopically erupting teeth), which prevent a permanent tooth from erupting on a normal schedule and in the proper position.
A major goal of early treatment is to prevent molars or incisors from drifting after premature loss of primary teeth, reducing the space available for unerupted teeth. Early treatment to align crowded incisors when space ultimately would be adequate or to create some additional space when a space deficiency exists may or may not be indicated. The decision as to whether this should be done in the mixed dentition and how it will be accomplished depends on the impact on esthetics as judged by the child and parents, as well as the location and magnitude of the problem. The goal should be to keep as many sensible options open as possible but to refrain from treatment when either the problem is too minor or later treatment obviously will be needed. Intervention for crossbites, habits, eruption problems, and simpler space problems has been described in Chapter 11. The section below focuses on more complex space problems that require more expertise in diagnosis, treatment planning, and biomechanics in order to achieve a useful and timely treatment. These treatments must be truly beneficial to the patient in the long run to be justified.
Excess Space
Generalized Spacing of Permanent Teeth
In the absence of incisor protrusion, excess space is not a frequent finding in the mixed dentition. It can result from either small teeth in normal-sized arches or normal-sized teeth in large arches. Unless the space presents an esthetic problem, it is reasonable to allow eruption of the remaining permanent teeth before closing the space with fixed appliances as part of comprehensive treatment (see Chapter 15). There is little or no advantage to early treatment unless it is for compelling esthetic reasons.18
A midline diastema often is a localized excess space problem (if not complicated by pathology, supernumerary teeth, or missing adjacent teeth). Tipping anterior teeth to close a small diastema was addressed in Chapter 11, but closing a large unesthetic diastema that may also be inhibiting eruption of adjacent teeth requires bodily repositioning of the central incisors to maintain proper inclinations of the teeth. Mesial crown and root movement provides more space for the eruption of the lateral incisors and canines. When the situation demands bodily mesiodistal movement and no retraction of the teeth, an anterior segmental archwire from central to central incisor or a segmental archwire including more anterior teeth is needed. Initial alignment of the incisors with a flexible wire is required. Then a stiffer archwire can be employed as the teeth slide together (with 22-slot brackets, 18 mil round or 16 × 22 mil rectangular steel are good choices; Figure 12-8). The force to move the incisors together can be provided by an elastomeric chain. Diastema closure is more predictable if only mesiodistal movement is required. If protruding incisors are part of the problem and need to be retracted to close the space, then careful attention to the posterior anchorage, overbite, and type of needed incisor tooth movement (tipping versus bodily retraction) is required (see below).
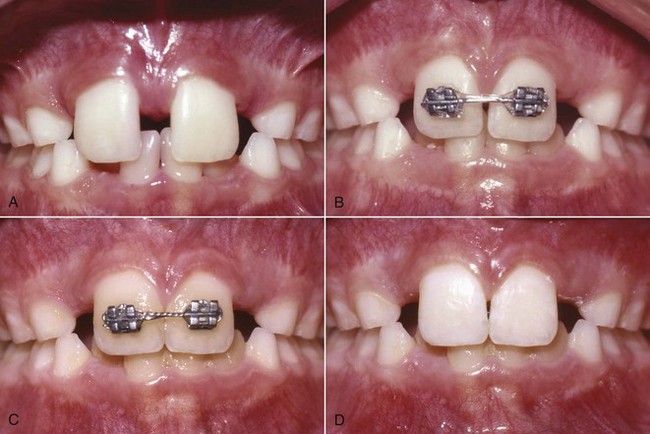
FIGURE 12-8 Closure of a diastema with a fixed appliance. A, This diastema requires closure by moving the crowns and roots of the central incisors. B, The bonded attachments and rectangular wire control the teeth in three planes of space while the elastomeric chain provides the force to slide the teeth along the wire. C, Immediately after space closure, the teeth are retained, preferably with (D) a fixed lingual retainer (see Figures 12-9 and 17-12), at least until the permanent canines erupt.
The experienced clinician’s desire to close diastemas at an early age is tempered by knowledge of how difficult it can be to keep the space closed as the other permanent teeth erupt. If the lateral incisors and canines have not erupted when the diastema is closed, a removable retainer will require constant modification. If the overbite is not prohibitively deep, a better alternative approach for retention is to bond a 17.5 mil multistrand archwire to the linguocervical portion of the incisors (Figure 12-9). This provides excellent retention with less maintenance.

FIGURE 12-9 A fixed retainer to maintain diastema closure. A bonded 17.5 mil multistrand wire with loops bent into the ends is bonded to the lingual surfaces of anterior teeth to serve as a permanent retainer. This flexible wire allows physiologic mobility of the teeth and reduces bond failure but can be used only when the overbite is not excessive.
The retention problem is due primarily to failure of the gingival elastic fibers to cross the midline when a large diastema is present but may be aggravated by the presence of a large or inferiorly attached labial frenum. A frenectomy after space closure and retention may be necessary in some cases, but it is difficult to determine the potential contribution of the frenum to retention problems from its pretreatment morphology. Therefore a frenectomy before treatment is contraindicated, and a posttreatment frenectomy should be done only if unresolved bunching of tissue between the teeth shows that it is necessary.
Maxillary Dental Protrusion and Spacing
Treatment for maxillary dental protrusion during the early mixed dentition is indicated only when the maxillary incisors protrude with spaces between them and are esthetically objectionable or in danger of traumatic injury. When this occurs in a child who has no skeletal discrepancies, it is often a sequel to a prolonged finger-sucking habit. Eliminating the finger habit prior to tooth movement is necessary (see Chapter 11). The more common cause for maxillary incisor protrusion is a Class II malocclusion that often has a skeletal component, and, in that case, treatment must address the larger problem (see Chapter 13).
If there is adequate vertical clearance (not a deep bite) and space within the arch, maxillary incisors that are proclined or have been tipped facially by a sucking habit can be tipped lingually with a removable appliance as described in Chapter 11. When the teeth require bodily movement or correction of rotations, a fixed appliance is required (Figure 12-10). In these cases, an archwire should be used with bands on posterior teeth and bonded brackets on anterior teeth. This appliance must provide a retracting and space-closing force, which can be obtained from closing loops incorporated into the archwire or from a section of elastomeric chain. To ensure bodily movement, a rectangular archwire must be used so that the crown and root movement are controlled (as described in Chapter 9), and undue tipping does not occur and leave the patient with upright or “rabbited” teeth. Bodily incisor retraction places a large strain on the posterior teeth, which tends to pull them forward. Depending on the amount of incisor retraction and space closure, a headgear, chosen with consideration for vertical facial and dental characteristics, may be necessary for supplemental anchorage support.

FIGURE 12-10 This closing loop archwire was used to retract protrusive maxillary incisors and close space. Each loop was activated approximately 1 mm per month, and the posterior anchorage was reinforced with headgear.
If the overbite is deep, it will bring the upper and lower incisors into vertical contact before the upper incisors can be retracted enough to close spaces between them and eliminate the excess overjet. In some properly selected patients this can be addressed with a biteplate that allows eruption of posterior teeth and reduces the overbite, but it is rare that Class II malocclusion is not part of the total picture when excessive overjet and overbite both are present. This presents a much more complex treatment problem that requires skeletal change and most likely comprehensive orthodontic treatment.
Missing Permanent Teeth
When permanent teeth are congenitally missing, the patient must have a thorough evaluation to determine the correct treatment because any of the diagnostic variables of profile, incisor position, tooth color and shape, skeletal and dental development or position, and space availability or deficiency can be crucial in treatment planning. The most commonly missing permanent teeth are second premolars (especially mandibular) and maxillary lateral incisors. These two conditions pose different problems.
Missing Second Premolars: Second premolars have a tendency to form late and may be thought to be missing, only to be discovered to be forming at a subsequent visit. Good premolars seldom form after the child is 8 years of age, so careful observation and caution are required. Contralateral teeth also can serve as a useful guide when evaluating tooth development.
If the patient has an acceptable occlusion, maintaining the primary second molars is a reasonable plan, since many can be retained at least until the patient reaches the early twenties or beyond (Figure 12-11). Many reports exist of primary molars surviving until the patient is 40 to 60 years of age. Some reduction of their mesiodistal width often is necessary to improve the interdigitation of the posterior teeth. Most clinicians believe that when the size of a primary molar is reduced, the mesiodistal diverging roots of the primary molar will resorb when they contact the adjacent permanent tooth roots. Even if eventual replacement of the primary molar with an implant or bridge is required, keeping the primary molar as long as possible is an excellent way to maintain alveolar bone in that area.
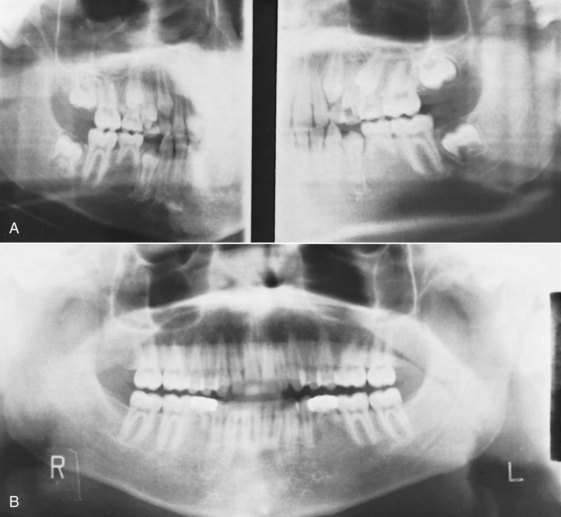
FIGURE 12-11 Primary mandibular second molars can be retained when the second premolars are missing. A, This patient was identified before orthodontic treatment as having missing mandibular second premolars. B, The decision was to retain the primary mandibular second molars because of the lack of crowding in the mandibular arch and their excellent root structure. These teeth were reduced mesiodistally and restored with stainless steel crowns during the finishing stages of orthodontic treatment to provide good occlusion.
If the space, profile, and jaw relationships are good or somewhat protrusive, it is possible to extract primary second molars that have no successor at age 7 to 9 and allow the first molars to drift mesially (Figure 12-12). This can produce partial or even complete space closure. Unfortunately, the amount and direction of mesial drift varies (Figure 12-13). Unless the second premolars are missing in all quadrants, it may be necessary to extract teeth in the opposing arch to reach a near ideal Class I occlusion. Otherwise, missing upper second premolars alone or missing lower second premolars alone with space closure will result in a Class II or Class III molar relationship, respectively, which is a problem more because unopposed second molars may overerupt than because of the molar relationship itself.
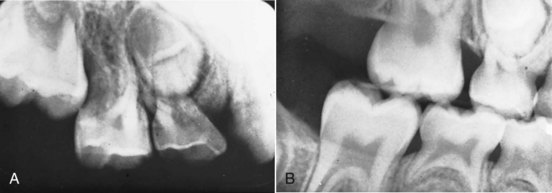
FIGURE 12-12 Missing second premolars can be treated by extraction of primary second molars to allow drifting of the permanent teeth and spontaneous space closure. A, This patient has ectopic eruption of the permanent maxillary first molar and a missing permanent maxillary second premolar. Since there was no other evidence of a malocclusion, the primary molar was extracted and (B) the permanent molar drifted anteriorly and closed the space during eruption. This eliminates the need for a prosthesis at a later date.
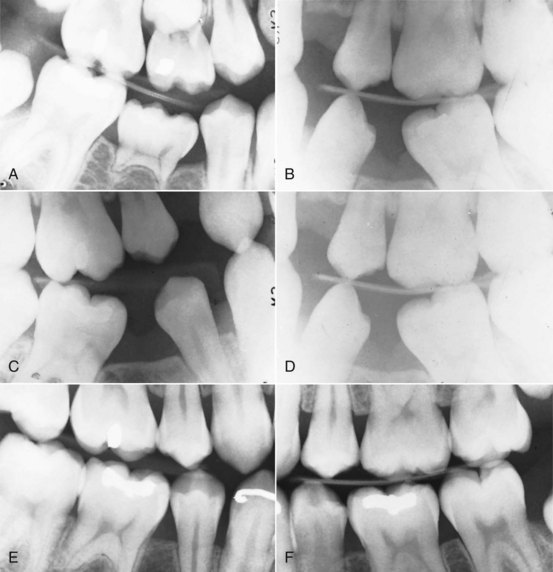
FIGURE 12-13 A and B, In this patient with bilaterally missing permanent mandibular second premolars, the decision was made to extract the retained primary molars to allow as much spontaneous drift and space closure as possible before full appliance therapy. C and D, Although posterior teeth did drift anteriorly and the anterior teeth distally, the space did not completely close. The pattern of drift to close the space of congenitally missing mandibular second premolars is highly variable and unpredictable. E and F, The residual space was closed and the roots paralleled with full appliances.
Early extraction can reduce the treatment time when the space of missing second premolars is to be closed, but later comprehensive orthodontic treatment usually is needed. If only one primary molar is missing, unless there has been true unilateral space loss or there is considerable crowding on the contralateral side, restorative rather than conventional orthodontic resolution of the problem is usually indicated. It is nearly impossible to close space unilaterally in the mixed dentition without affecting the midlines and other anterior interarch relationships. Remember that temporary anchorage devices (TADs) to facilitate unilateral space closure are not indicated prior to about 12 years of age due to bone density, so this is a treatment method that would have to be reserved for a later time period. Another solution to missing second premolars is to gradually reduce the size of the second premolar during comprehensive orthodontic treatment and combine hemisectioning of the primary tooth and pulp therapy so that the first permanent molar is protracted into the primary molar space without loss of alveolar bone from a more long-standing extraction. This type of treatment is described in Chapter 15.
Missing Maxillary Lateral Incisors: Long-term retention of primary laterals, in contrast to primary molars, is almost never an acceptable plan. When the lateral incisors are missing, one of two sequelae usually is observed. In some patients, the erupting permanent canine resorbs the primary lateral incisor and spontaneously substitutes for the missing lateral incisor, which means that the primary canine has no successor and is sometimes retained (Figure 12-14). Some of these patients are seen as adults with primary canines in place, but most primary canines are lost by the end of adolescence even if their successors have erupted mesially. Less often, the primary lateral is retained when the permanent canine erupts in its normal position. This usually means that the lateral incisor space is reduced to the size of the primary lateral incisor and the remaining primary incisor is unesthetic. Having the permanent canine erupt in the position of a congenitally missing lateral incisor is advantageous, whether or not the ultimate treatment is substitution of the canine for the lateral or opening space for a prosthetic lateral replacement because it generates alveolar bone in that area. Additionally, the canine shape and color can be determined, which may have some influence on whether they are retracted and implants placed or substituted for the lateral incisors and the space closed. Both solutions have their place.
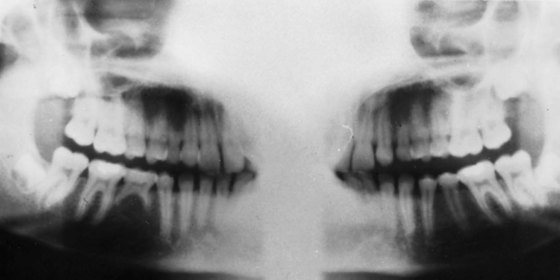
FIGURE 12-14 Missing permanent maxillary lateral incisors are often replaced spontaneously by permanent canines. This phenomenon occurs without intervention, but the resorption noted on the retained primary canines probably will continue to progress. If implants to eventually replace the missing laterals are planned, it is desirable for the canines to erupt mesially so that alveolar bone forms in the area of the future implant. The canines can be moved into their final position just prior to the implant surgery (see Chapter 18).
If space closure is the goal and the primary lateral incisors are replaced by the permanent canines as they erupt, little immediate attention is necessary. Sometimes the absence of lateral incisors causes a large diastema to develop between the permanent central incisors. To maximize mesial drift of the erupting permanent canines, this diastema can be closed and retained (Figure 12-15). Later in the transition to the permanent dentition, the primary canines should be extracted if they are not resorbing, so the premolars can migrate into the canine positions and other posterior teeth can move mesially and close space (Figure 12-16). This space closure option is best when the incisors are slightly protrusive and the molars are tending toward Class II in the posterior so that reciprocal space closure can be employed between the anterior and posterior teeth and moving the maxillary posterior teeth forward is easier. Space closure is usually avoided when the patients are full Class I or have a Class III tendency and the possibility exists of creating an anterior crossbite with incisor retraction during space closure. Once again, TADs can help in these less than ideal situations. These are intricacies of comprehensive treatment.
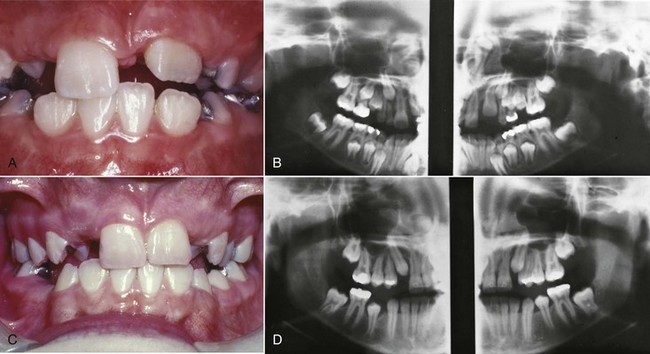
FIGURE 12-15 When permanent lateral incisors are congenitally missing, often a large diastema develops between the permanent central incisors. A, This patient has that type of diastema, and the unerupted permanent canines will be substituted for the missing lateral incisors. B, This radiograph shows the unerupted canines in an excellent position for substitution for the lateral incisors. C, The diastema has been closed to obtain maximum mesial drift of the canines. D, This technique enables the canines to erupt closer to their final position and eliminates unnecessary tooth movement during full appliance therapy.
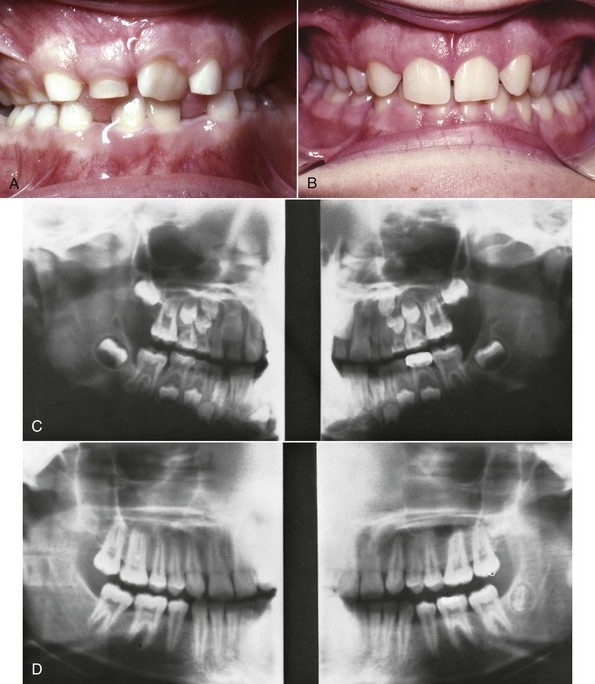
FIGURE 12-16 Selective removal of primary teeth when permanent maxillary lateral incisors are missing can lead to a shortened second phase of fully banded treatment. A and B, This patient had primary canines and primary first molars extracted to maximize the mesial drift of the permanent posterior teeth. C and D, This intervention resulted in good tooth position that will require little fixed appliance therapy to complete.
Generally, unilateral orthodontic space closure in the anterior region of the mouth is not recommended. There is probably a better chance of matching the existing teeth with restorative solutions or substituting for both lateral incisors than with reshaping the existing teeth on only one side. A unilateral missing lateral incisor might require the extraction of the other lateral incisor prior to eruption of the canines to maximize the drift pattern for ultimate space closure and substitution, especially when the remaining primary incisor is pegged (Figure 12-17), but generally the option to move the canines back into their proper position exists prior to premolar eruption. These same considerations generally apply for the lower anterior area, too, where one or two lateral incisors sometimes are missing. The details for completing comprehensive treatment and finishing for missing laterals are covered in Chapters 14 and 18.
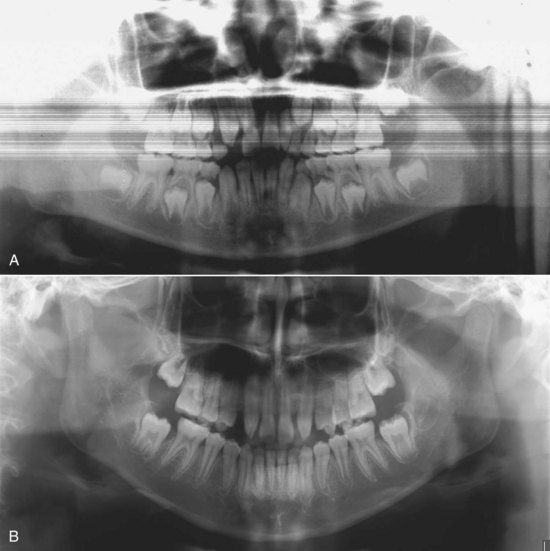
FIGURE 12-17 A, This patient’s panoramic radiograph shows that one permanent maxillary lateral incisor is missing and the other peg-shaped. B, Instead of opening or closing space unilaterally the peg lateral was extracted and the teeth allowed to drift and erupt. The patient will now be treated with bilateral space closure or implants to improve symmetry and esthetics.
Autotransplantation: In patients with a congenitally missing tooth or teeth in one area but crowding in another, autotransplantation is a possible solution. Teeth can be transplanted from one position to another in the same mouth with a good prognosis for long-term success, if this is done when the transplanted tooth has approximately two-thirds to three-fourths of its root formed.19 This means that the decision for autotransplantation must be made during the mixed dentition (Figure 12-18).
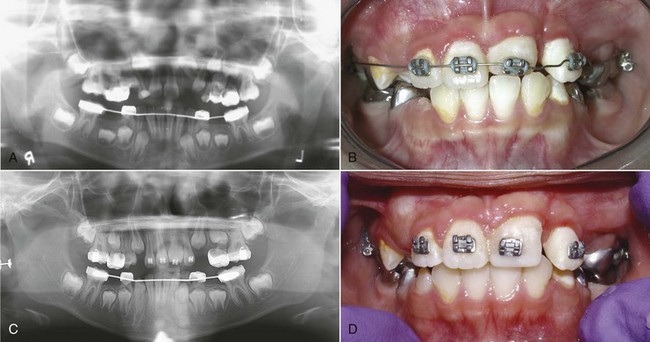
FIGURE 12-18 A, This patient has an unerupted permanent maxillary left central incisor with a dilacerated root, possibly due to previous trauma. It was determined that it could not be repositioned surgically or moved orthodontically. B, To relieve crowding, premolar extraction was indicated, and the maxillary left first premolar was transplanted to the maxillary left central incisor position and moved after a short healing period. C, Root development and healing have continued and indicate a vital tooth. D, The tooth will continue to be recontoured and restored with resin prior to definitive restorative treatment.
Transplantation is most commonly used to move premolars into the location of missing maxillary incisors due to developmental problems or trauma.20 It can also be used to replace missing first molars with third molars, a decision that can be made a little later (Figure 12-19).21 A combination of careful surgical intervention and positioning of the transplant, 3 months of healing, followed by light orthodontic forces to achieve final tooth position, and restorative treatment to recontour the crown of the transplanted tooth can result in long-term functional and esthetic success. The success rate with this type of treatment is high and predictable.
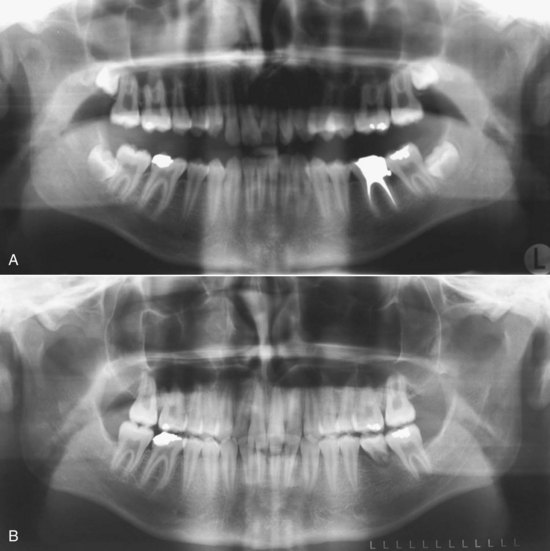
FIGURE 12-19 A, The mandibular permanent first molar was restoratively compromised. With the developing third molar in the maxillary left quadrant available (B), it was decided to transplant it into the first molar position when the root development was appropriate, rather than plan a restoration for the first molar. The transplanted third molar was subsequently repositioned during orthodontic treatment and served well as a replacement.
Localized Moderate-To-Severe Crowding
In some children, there is moderate-to-severe localized crowding (>3 mm). This is most likely the result of severe space loss or ectopic eruption and typically prevents eruption of a succedaneous tooth.
In the posterior quadrants, it is sensible to extract the impacted tooth and close the space. This generally takes less time than regaining space and encouraging eruption of the impacted tooth or teeth. If space regaining is the goal after carefully weighing the options, the biomechanical issues are sizable and include unilateral space opening without disruption of the rest of the arch or occlusion. Sometimes the space loss may be bilateral. Distal molar movement is often part of the equations for correction of the problem. Reciprocal forces, which are the easiest and most predicable for our use, cannot be employed. These types of treatment are covered later in this chapter under distal molar movement.
In the anterior portion of the arch, the most common problem of this type is a shift of the mandibular dental midline. Tooth movement is more often used to solve this problem than simple single tooth extraction. If the midline has moved and no permanent teeth will be extracted, midline correction is needed before the remaining permanent teeth erupt in asymmetric positions and localized crowding becomes worse. If the midline has moved and the space is inadequate, both the space and midline problems need to be addressed before the canines erupt. This is most successfully accomplished using a supportive lingual arch to maintain molar symmetry and control, bonding of the incisors, and correction of the midline with a coil spring (Figure 12-20). In some cases, disking or extraction of a primary canine or molar will be required to provide the necessary room to reestablish the midlines and space. A lingual arch can then be used as a retainer to maintain the correction.

FIGURE 12-20 Some midline shifts require bodily tooth movement. A, The midline of the mandibular arch has bodily shifted to the patient’s right because of premature loss of a primary canine. B, The teeth were moved back to their proper position using a fixed appliance and are supported until eruption of the canines with a lingual holding arch. C, This type of movement is best achieved with an archwire and coil springs to generate the tooth moving forces. Active coil springs can be replaced with passive coils to gain stability prior to retention.
If both mandibular primary canines are lost and the permanent incisors tip lingually, which reduces the arch circumference and increases the apparent crowding, an active lingual arch for expansion may be indicated. In some children, space analysis will reveal that the crowding associated with ectopic eruption of lateral incisors is more severe and fixed appliances are needed to expand the arch.
Generalized Moderate and Severe Crowding
Expansion versus Extraction in Mixed Dentition Treatment
For children with a moderate space deficiency, usually there is generalized but not severe crowding of the incisors, but sometimes the primary canines are lost to ectopic eruption of the lateral incisors and more severe crowding goes largely unrecognized. Children with the largest arch length discrepancies often have reasonably well-aligned incisors in the early mixed dentition because both primary canines were lost when the lateral incisors erupted.
Potentially severe crowding usually is obvious in the primary dentition, even before a space analysis can be completed. These children have little developmental spacing between primary incisors and occasionally some crowding in the primary dentition. The two major symptoms of severe crowding in the early mixed dentition are severe irregularity of the erupting permanent incisors and early loss of primary canines caused by eruption of the permanent lateral incisors. After a definitive analysis of the profile and incisor position, these patients face the same decision as those with moderate crowding: whether to expand the arches or extract permanent teeth and when this should be done (see Chapter 7 for a review of factors influencing this decision). In the presence of severe crowding, limited mixed dentition treatment will not be sufficient and extraction has to be considered.
Expansion for Treatment of Crowding in the Early Mixed Dentition
For most children with crowding and inadequate space in the early mixed dentition, some facial movement of the incisors and expansion can be accommodated, especially if:
• The lower incisor position is normal or somewhat retrusive.
• Lips are normal or retrusive.
• There is good keratinized tissue facial to the lower incisors.
If facial movement is anticipated and the amount and quality of gingival tissue is questionable, a periodontal consultation about a gingival graft is appropriate. Surgical or nonsurgical management of the soft tissue may be required prior to or following tooth movement.
A key question is whether early expansion of the arches (before all permanent teeth erupt) gives more stable results than later expansion (in the early permanent dentition). Partly in response to the realization that recurrent crowding occurs in many patients who were treated with premolar extractions (see Chapter 7), a number of approaches to early arch expansion recently have gained some popularity in spite of a lack of data to document their effectiveness. This early expansion can involve any combination of several possibilities:
• Maxillary dental or skeletal expansion, moving the teeth facially or opening the midpalatal suture
• Mandibular buccal segment expansion by facial movement of the teeth
• Advancement of the incisors and distal movement of the molars in either arch
The most aggressive approach to early expansion, in terms of timing, uses maxillary and mandibular lingual arches in the complete primary dentition. This produces an increase in both arch perimeter and width, which must be maintained for variable periods during the mixed dentition years. The ability of expansion in the primary dentition to meet the challenge of anterior crowding is highly questionable and unsubstantiated.22
A conservative approach to moderate crowding in the early mixed dentition is to place a lingual arch after the extraction of the primary canines and allow the incisors to align themselves. Ultimately, a lingual arch or another appliance can be used to increase the arch length, or extractions can be done with more certainty that this really was required. Clinical experience indicates that a considerable degree of faciolingual irregularity will resolve if space is available, but rotational irregularity will not. If the incisors are rotated, severely irregular, or spaced and early correction is felt to be important, a fixed appliance will be needed for treatment, either in the mixed or early permanent dentition (Figure 12-21).
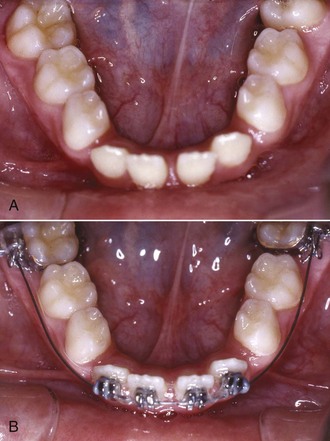
FIGURE 12-21 A, In this patient who had lower anterior teeth that were lingually tipped and spaced, lower arch expansion with a fixed appliance was required because the spacing could not be adequately controlled with a lingual arch or lip bumper. B, The fixed appliance in place during alignment and prior to space closure in the incisor area. After space closure, the incisors can be further proclined if necessary.
Lower incisor teeth usually can be tipped 1 to 2 mm facially without much difficulty, which creates up to 4 mm of additional arch length, but only if overbite is not excessive and overjet is adequate. To create substantial space and control the tooth movement, it is best to band the permanent molars, bond brackets on the incisors, and use a compressed coil spring on a labial archwire to gain the additional space (Figure 12-22). The multiple band and bond technique is usually followed with a lingual arch for retention. The advantage of the bonded and banded appliance is to provide rotational and mesiodistal space control and bodily movement if necessary. Some expansion of the buccal segments can be included in addition to solely incisor movement.

FIGURE 12-22 Moderate arch-length increases can be accomplished using a multiple bonded and banded appliance and a mechanism for expansion. A, This patient has moderate lower arch irregularity and space shortage. B, The appliance is in place with the tooth movement completed. In this case, coil springs served to generate the tooth moving force, but other methods using loops and flexible archwires are available. Note the lingual arch used to control transverse molar dimensions. C, The lingual arch is adjusted by opening the loops and advancing the arch so it can serve as a retainer following removal of the archwire and bonded brackets.
A somewhat more aggressive approach is to expand the upper arch transversely in the early mixed dentition, not to correct posterior crossbite but specifically to gain more space in the dental arch. This is accomplished using a lingual arch or jackscrew expander to produce dental and skeletal changes (Figure 12-23), but jackscrew expansion must be done carefully and slowly if it is used in the early mixed dentition. The theory is that this would assure more space at a later time.23 To date, there is no credible long-term postretention evidence that early intervention to “prepare,” “develop,” “balance,” or expand arches by any other name has any efficacy in providing a less crowded permanent dentition later. Unfortunately, even in children who had mild crowding initially, incisor irregularity can recur soon after early treatment if retention is not managed carefully. Parents and patients should know the issues and uncertainties associated with this type of treatment.

FIGURE 12-23 A and B, Some practitioners advocate early expansion by opening the midpalatal suture, usually using a jackscrew type appliance as in this patient, even in the absence of a posterior crossbite or an apparent arch length shortage, on the theory that this will improve the long-term stability of arch expansion. Little or no data exist to support this contention.
It has been suggested that this type of early expansion not only provides more space and better esthetics, but also can reduce occlusal disharmonies between the arches that are present in Class II malocclusions.24 Data supporting the long-term effectiveness of this technique are unavailable. It seems unlikely that the soft tissues, which establish the limits for arch expansion, would react quite differently to transverse expansion at different ages (see the discussion of equilibrium influences in Chapter 5) or that jaw growth in other planes of space would be greatly affected by transverse expansion.
Expansion for Crowding in the Late Mixed Dentition: Molar Distalization
Transverse expansion to gain additional space can be used in the late as well as the early mixed dentition, and the previous comments also apply to the late mixed dentition. An additional approach in the late mixed dentition is to obtain additional space by repositioning molars distally. Unless TADs are used, which is not recommended prior to age 12 due to inadequate bone density, intraoral appliances for distal molar movement will be accompanied by facial incisor movement. With this knowledge, there are some indications for this type of treatment:
• Probably less than 4 to 5 mm per side of required space by predominantly tipping.
• Erupted maxillary anterior teeth and ideally, first premolars for anchorage.
• The lip and maxillary dental protrusion should be normal or retrusive because about one-third of the movement will be experienced as facial incisor movement.
• Likewise, overjet should be limited.
• The vertical facial dimensions should be normal or with a short-face tendency because the distal movement of the molars can open the bite.
• Similarly, the overbite should be somewhat greater than normal due to the bite opening mechanics.
Until relatively recently, headgear to move maxillary molars distally was the preferred approach. It has the advantage of simplicity and the major disadvantage that good patient compliance is needed. To tip or bodily move molars distally, extraoral force via a facebow to the molars is a straightforward method. The force is directed specifically to the teeth that need to be moved, and reciprocal forces are not distributed on the other teeth that are in the correct positions. The force should be as nearly constant as possible to provide effective tooth movement and should be moderate because it is concentrated against only two teeth. The more the child wears the headgear, the better; 12 to 14 hours per day is minimal. Approximately 400 gm of force per side is appropriate but not particularly friendly to the teeth. The teeth should move at the rate of 1 mm/month, so a cooperative child would need to wear the appliance for 3 months to obtain the 3 mm of correction that would be a typical requirement in this type of treatment.
For the short-term duration of this type of treatment, either cervical or high-pull headgear can be chosen, but high-pull headgear is an excellent option (Figure 12-24). Baumrind et al reported that this approach is particularly effective in producing distal molar movement.25

FIGURE 12-24 A high-pull headgear has been demonstrated to be the most effective extraoral appliance to move molars distally. Of course, compliance is required, but no reciprocal incisor protrusion occurs.
If bodily distal movement of one or both permanent maxillary first molars is needed to adjust molar relationships and gain space, if there are adequate anterior teeth for anchorage, if some anterior incisor movement can be tolerated and the overbite is adequate, several appliances can be considered. All are built around the use of a heavy lingual arch, usually with an acrylic pad against the anterior palate to provide anchorage (Figure 12-25). Often, the anterior teeth also are bonded and stabilized with an archwire. Then, a force to move the molar distally is generated by a palate-covering appliance with helical springs (the pendulum appliance), steel or superelastic coil springs, or other device (see Figures 15-4 to 15-6).26 In the mandibular arch, unerupted second molars make distalization of the first molars more difficult, and use of a fixed appliance to bring the lower incisors forward may be more acceptable (Figure 12-26).
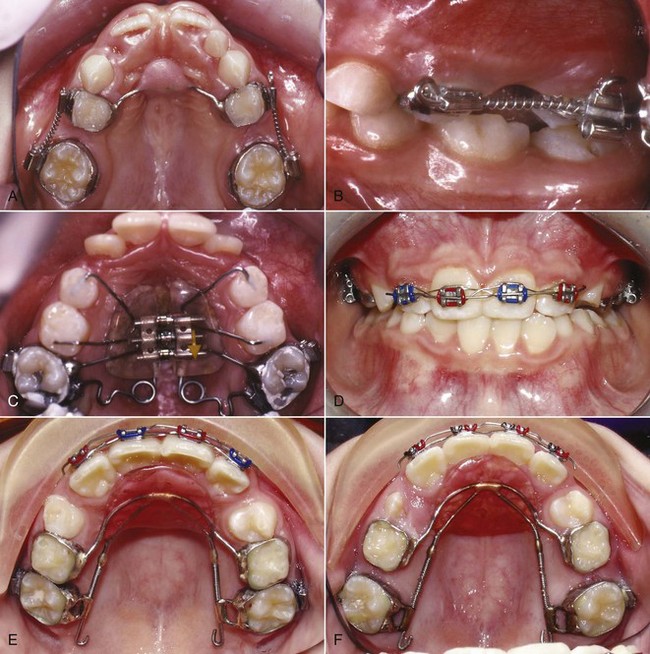
FIGURE 12-25 Several approaches can be taken to increasing arch circumference by distalizing molars, if the correct diagnosis is made and the incisor protrusion that usually results can be accepted. A and B, Bilateral coil springs provide the force that is resisted by the anchorage of the primary molars and the palate using a Nance arch. C, Alternatively, a pendulum appliance can be used that also gains anchorage from the palate but uses helical springs to supply the force. D to F, This fixed appliance also uses palatal and dental anchorage and NiTi coil springs to slide the molars along heavy lingual wires. Once placed, the appliance can be monitored until the desired tooth movement is achieved and then it can be modified to serve as a retainer. (A to C courtesy Dr. M. Mayhew.)

FIGURE 12-26 For mixed dentition treatment of significant lower crowding and irregularity, banded/bonded attachments and an archwire provide the most efficient approach. This patient has crowding and irregularity that indicates fixed appliance treatment. Note the use of a superelastic coil spring to create space for the erupting mandibular right canine.
The primary method now for distalization of molars, which can be used with children 12 years of age and older, is the use of TAD-supported molar-distalizing appliances (Figure 12-27).27 These appliances can distalize molars in both arches without creating forward movement of the incisors because of the nearly absolute anchorage. There are three major limitations to this approach: (1) the surgery to place and remove the TADs, which is quite acceptable to patients but can have complications, (2) the long duration of treatment to move and retain the teeth from the mixed dentition through the eruption of the permanent teeth, which is not shorter with TADs, and (3) the uncertain stability of the long-term result. The question is not whether the tooth movement is possible—it is. Rather, the question is the wisdom of major expansion of the arches or distal movement, especially in the mixed dentition.

FIGURE 12-27 A, This patient had TAD-supported molar distalization in the late mixed dentition to accommodate the initial crowding and a nonextraction treatment plan. This is not recommended for patients much younger than 12 years due to inadequate bone density and resulting TAD instability. B, The wire framework supports the TADs in the anterior palate with the distal force provided by the coil springs. No anchorage is provided by the anterior teeth. C, Good tooth movement with intact TADs at the end of active distalization, even with the second molars erupted. D, The final arch in retention.
No matter how molars were moved distally, if the time before eruption of the premolars will be longer than a few months, it will be necessary to hold them back after they are repositioned. Maxillary and mandibular lingual arch space maintainers (see Figure 11-55) are the best insurance to guard against space loss. Remember, too, that this new posterior molar position has to be guarded no matter how it was achieved if incisors are to be retracted. This is a difficult task without TADs.
Early (Serial) Extraction
In many children with severe crowding, a decision can be made during the early mixed dentition that expansion is not advisable and that some permanent teeth will have to be extracted to make room for the others. A planned sequence of tooth removal can reduce crowding and irregularity during the transition from the primary to the permanent dentition.28 It will also allow the teeth to erupt over the alveolus and through keratinized tissue, rather than being displaced buccally or lingually. This sequence, often termed serial extraction, simply involves the timed extraction of primary and, ultimately, permanent teeth to relieve severe crowding. It was advocated originally as a method to treat severe crowding without or with only minimal use of appliance therapy but is now viewed as an adjunct to later comprehensive treatment instead of a substitute for it.
Although serial extraction makes later comprehensive treatment easier and often quicker, by itself it almost never results in ideal tooth position or closure of excess space. Serial extraction is directed toward severe dental crowding. For this reason, it is best used when no skeletal problem exists and the space discrepancy is large—greater than 10 mm per arch. If the crowding is severe, little space will remain after the teeth are aligned, which means there will be little tipping and uncontrolled movement of the adjacent teeth into the extraction sites. If the initial discrepancy is smaller, more residual space must be anticipated. It is unwise for a nonspecialist to start serial extraction in a child who has a skeletal problem because the closure of extraction spaces would be affected by how the skeletal problem was being addressed.
Serial extraction treatment begins in the early mixed dentition with extraction of primary incisors if necessary, followed by extraction of the primary canines to allow eruption and alignment of the permanent incisors (Figure 12-28). As the permanent teeth align without any appliances in place, there is usually some lingual tipping of the lower incisors, and overbite often increases during this stage. Labiolingual displacements resolve better than rotational irregularity. After extraction of the primary canines, crowding problems are usually under control for 1 to 2 years, but foresight is necessary. The goal is to influence the permanent first premolars to erupt ahead of the canines so that they can be extracted and the canines can move distally into this space. The maxillary premolars usually erupt before the canines, so the eruption sequence is rarely a problem in the upper arch. In the lower arch, however, the canines often erupt before the first premolars, which causes the canines to be displaced facially. To avoid this result, the lower primary first molar should be extracted when there is one-half to two-thirds root formation of the first premolar. This usually will speed up the premolar eruption and cause it to enter the arch before the canine (Figure 12-28, C). The result is easy access for extraction of the first premolar before the canine erupts (Figure 12-28, D).
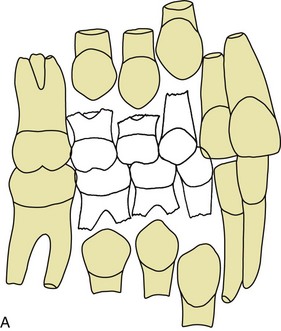
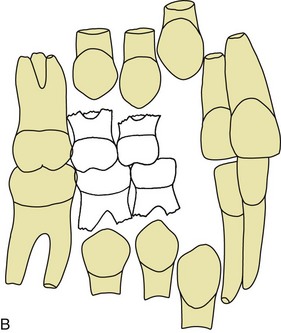
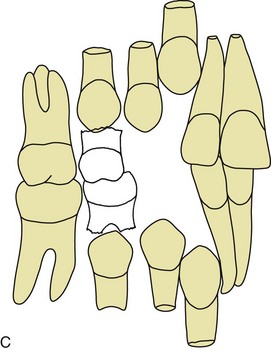
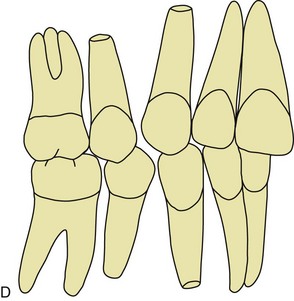
FIGURE 12-28 Serial extraction is used to relieve severe arch length discrepancies. A, The initial diagnosis is made when a severe space deficiency is documented and there is marked incisor crowding. B, The primary canines are extracted to provide space for alignment of the incisors. C, The primary first molars are extracted when one-half to two-thirds of the first premolar root is formed, to speed eruption of the first premolars. D, When the first premolars have erupted they are extracted and the canines erupt into the remaining extraction space. The residual space is closed by drifting and tipping of the posterior teeth unless full appliance therapy is implemented.
A complication can occur if the primary first molar is extracted early and the first premolar still does not erupt before the canine. This can lead to impaction of the premolar that requires later surgical removal (Figure 12-29). At the time the primary first molar is removed, it may be obvious that the canine will erupt before the premolar. In this case the underlying premolar can also be extracted at the same time—a procedure termed enucleation. If possible, however, enucleation should be avoided because the erupting premolar brings alveolar bone with it. Early enucleation can leave a bone defect that persists.
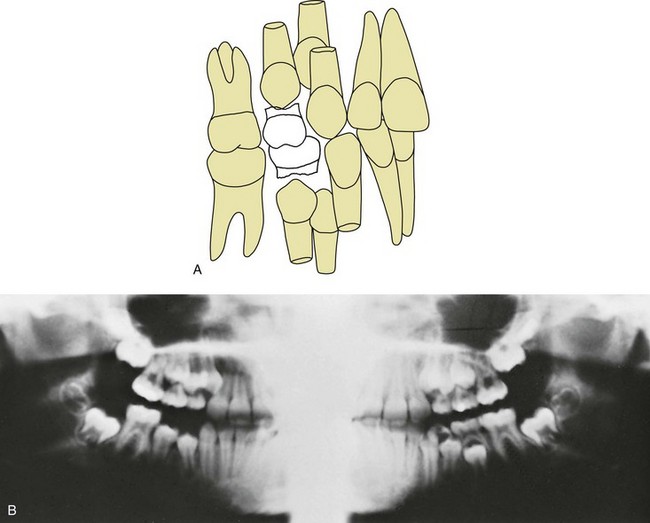
FIGURE 12-29 A complication of serial extraction is premature eruption of the permanent canines. A, When this occurs, the first premolars are impacted between the canines and the second premolars. B, In this situation (note the lower right quadrant for this patient), the first premolars usually have to be surgically removed (a procedure often called enucleation).
The increase in overbite mentioned previously can become a problem during later treatment. A variation in the extraction sequence can be used to help in controlling this problem. The mandibular primary canines are retained, and some space for anterior alignment is made available when the permanent laterals erupt by extracting the primary first molars instead. With this approach, eruption of the permanent first premolars is encouraged, and the incisors are less prone to tip lingually (Figure 12-30). The major goal of serial extraction is prevention of incisor crowding, however, and some crowding often persists if the primary canines are retained. In many patients with severe crowding, the primary canines are lost to ectopic eruption of the laterals and cannot be maintained.
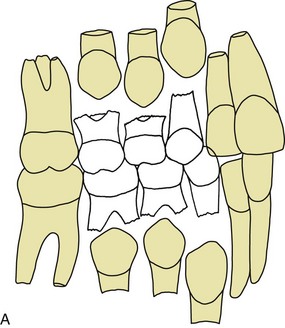
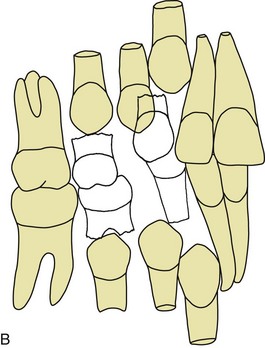
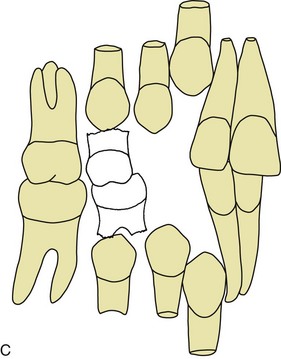
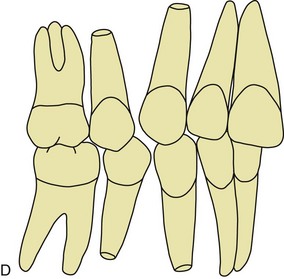
FIGURE 12-30 A, An alternative approach to serial extraction is implemented slightly later but under the same conditions and (B) begins with extraction of the primary first molars so that there is less lingual tipping of the incisors and less tendency to develop a deep bite. Extraction of the primary first molars also encourages early eruption of the first premolars. C, When the first premolars have erupted, they are extracted and the canines erupt into the remaining extraction space. D, The residual space is closed by drifting and tipping of the posterior teeth unless full appliance therapy is implemented.
After the first premolar has been extracted, the second primary molars should exfoliate normally. The premolar extraction spaces close partially by mesial drift of the second premolars and permanent first molars but largely by distal eruption of the canines. If serial extraction is not followed by mechanotherapy, ideal alignment, root positioning, correct rather than deep overbite, and space closure usually are not achieved (Figure 12-31).
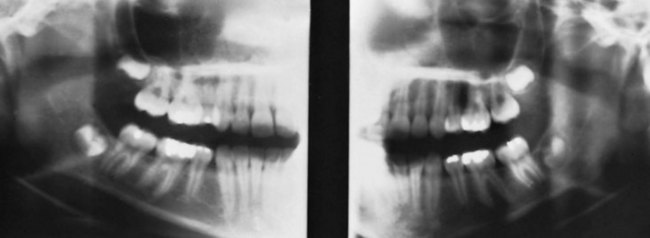
FIGURE 12-31 This patient had serial extraction that was not followed by fixed appliance treatment, with an excellent result. Properly timed serial extraction usually results in incomplete space closure. Teeth drift together by tipping, which results in nonparallel roots between the canine and second premolar. Lack of root parallelism, residual space, and other irregularities can be addressed with subsequent fixed appliance therapy.
Serial extraction was used much more frequently 20 to 30 years ago than now. It was overused then and perhaps is underused now. It can be a useful adjunct to treatment, shortening the time of comprehensive treatment if it is used correctly, but the patients must be chosen carefully and supervised carefully as they develop. It is far from a panacea for treatment of crowding.
The Borderline Crowding Case: What Do You Do?
If early extraction is only for the few patients with extremely severe crowding, and early expansion offers little advantage over expansion during later comprehensive treatment, what is the best approach to moderately crowded and irregular teeth during the mixed dentition? The wisest course of action, in most cases, is simply to keep the options open for the later comprehensive treatment that these children will need. Unless crowding is severe, maintaining leeway space during the last part of the transition to the permanent dentition increases the chance of successful nonextraction treatment if space is adequate or borderline. Early extraction of primary canines often can provide space for some spontaneous alignment of permanent incisors and also can decrease the chance of canine impaction, but a lower lingual arch to maintain space is needed to keep the nonextraction option open when this is done. Beyond that, the advantages of early appliance therapy are questionable and must be viewed in the context of an increased burden of treatment versus little or no additional benefit.
References
1. Papadopoulos, MA, Chatzoudi, M, Kaklamanos, EG. Prevalence of tooth transposition. A meta-analysis. Angle Orthod. 2010;80:275–285.
2. Garib, DG, Peck, S, Gomes, SC. Increased occurrence of dental anomalies associated with second-premolar agenesis. Angle Orthod. 2009;79:436–441.
3. Shapira, Y, Kuftinec, MM. Intrabony migration of impacted teeth. Angle Orthod. 2003;73:738–743.
4. Peck, S, Peck, L. Classification of maxillary tooth transpositions. Am J Orthod Dent Orthop. 1995;107:505–517.
5. Frazier-Bowers, SA, Simmons, D, Wright, JT, et al. Primary failure of eruption and PTH1R: the importance of a genetic diagnosis for orthodontic treatment planning. Am J Orthod Dentofac Orthop. 2010;137:160.e1–160.e7. [discussion 160-161].
6. Hölttä, P, Alaluusua, S, Saarinen-Pihkala, UM, et al. Agenesis and microdontia of permanent teeth as late adverse effects after stem cell transplantation in young children. Cancer. 2005;103:181–190.
7. Hölttä, P, Hovi, L, Saarinen-Pihkala, UM, et al. Disturbed root development of permanent teeth after pediatric stem cell transplantation. Dental root development after SCT. Cancer. 2005;103:1484–1493.
8. Iglesias-Linares, A, Yáñez-Vico, RM, Solano-Reina, E, et al. Influence of bisphosphonates in orthodontic therapy: systematic review. J Dent Res. 2010;38:603–611.
9. Brin, I, Ben-Bassat, Y, Heling, I, et al. The influence of orthodontic treatment on previously traumatized permanent incisors. Eur J Orthod. 1991;13:372–377.
10. Bauss, O, Röhling, J, Meyer, K, et al. Pulp vitality in teeth suffering trauma during orthodontic therapy. Angle Orthod. 2009;79:166–171.
11. Andreasen, JO, Bakland, LK, Andreasen, FM. Traumatic intrusion of permanent teeth. Part 3. A clinical study of the effect of treatment variables such as treatment delay, method of repositioning, type of splint, length of splinting and antibiotics on 140 teeth. Dent Traumatol. 2006;22:99–111.
12. Wigen, TI, Agnalt, R, Jacobsen, I. Intrusive luxation of permanent incisors in Norwegians aged 6-17 years: a retrospective study of treatment and outcome. Dent Traumatol. 2008;24:612–618.
13. Bauss, O, Schäfer, W, Sadat-Khonsari, R, et al. Influence of orthodontic extrusion on pulpal vitality of traumatized maxillary incisors. J Endodont. 2010;36:203–207.
14. Bauss, O, Röhling, J, Sadat-Khonsari, R, et al. Influence of orthodontic intrusion on pulpal vitality of previously traumatized maxillary permanent incisors. Am J Orthod Dentofac Orthop. 2008;134:12–17.
15. Bauss, O, Röhling, J, Rahman, A, et al. The effect of pulp obliteration on pulpal vitality of orthodontically intruded traumatized teeth. J Endodont. 2008;34:417–420.
16. Esteves, T, Ramos, AL, Pereira, CM, et al. Orthodontic root resorption of endodontically treated teeth. J Endodont. 2007;33:119–122.
17. Rodd, HD, Davidson, LE, Livesey, S, et al. Survival of intentionally retained permanent incisor roots following crown root fractures in children. Dent Traumatol. 2002;18:92–97.
18. Little, R, Riedel, R. Postretention evaluation of stability and relapse—mandibular arches with generalized spacing. Am J Orthod. 1989;95:37–41.
19. Paulsen, HU, Andreasen, JO, Schwartz, O. Tooth loss treatment in the anterior region: autotransplantation of premolars and cryopreservation. World J Orthod. 2006;7:27–34.
20. Zachrisson, BU, Stenvik, A, Haanaes, HR. Management of missing maxillary anterior teeth with emphasis on autotransplantation. Am J Orthod Dentofac Orthop. 2004;126:284–288.
21. Bauss, O, Sadat-Khonsari, R, Engelke, W, et al. Results of transplanting developing third molars as part of orthodontics space management. Part 2. Results following the orthodontic treatment of transplanted developing third molars in cases of aplasia and premature loss of teeth with atrophy of the alveolar process. J Orofac Orthop. 2003;64:40–47.
22. Lutz, HD, Poulton, D. Stability of dental arch expansion in the deciduous dentition. Angle Orthod. 1985;55:299–315.
23. O’Grady, PW, McNamara, JA, Jr., Baccetti, T, et al. A long-term evaluation of the mandibular Schwarz appliance and the acrylic splint expander in early mixed dentition patients. Am J Orthod Dentofac Orthop. 2006;130:202–213.
24. McNamara, JA, Jr., Sigler, LM, Franchi, L, et al. Changes in occlusal relationships in mixed dentition patients treated with rapid maxillary expansion. A prospective clinical study. Angle Orthod. 2010;80:230–238.
25. Baumrind, S, Korn, EL, Isaacson, RJ, et al. Quantitative analysis of orthodontic and orthopedic effects of maxillary traction. Am J Orthod. 1983;84:384–398.
26. Antonarakis, GS, Kiliaridis, S. Maxillary molar distalization with noncompliance intramaxillary appliances in Class II malocclusion. A systematic review. Angle Orthod. 2008;78:1133–1140.
27. Polat-Ozsoy, O, Kircelli, BH, Arman-Ozçirpici, A, et al. Pendulum appliances with 2 anchorage designs: conventional anchorage vs. bone anchorage. Am J Orthod Dentofac Orthop. 2008;133:339.e9–339.e17.
28. Hotz, RP. Guidance of eruption versus serial extraction. Am J Orthod. 1970;58:1–20.