Orthodontic Treatment Planning
From Problem List to Specific Plan
TREATMENT PLANNING CONCEPTS AND GOALS
MAJOR ISSUES IN PLANNING TREATMENT
PLANNING TREATMENT FOR MAXIMAL ESTHETIC IMPROVEMENT
Macro-Esthetic Considerations: Correcting Facial Disproportions
Mini-Esthetic Considerations: Improving the Smile Framework
Micro-Esthetic Considerations: Enhancing the Appearance of the Teeth
Treatment Planning Concepts and Goals
Orthodontic diagnosis is complete when a comprehensive list of the patient’s problems has been developed and pathologic and developmental problems have been separated. At that point, the objective in treatment planning is to design the strategy that a wise and prudent clinician, using his or her best judgment, would employ to address the problems while maximizing benefit to the patient and minimizing cost and risk.
It is important to view the goal of treatment in that way. Otherwise, an inappropriate emphasis on some aspect of the case is likely, whether the proposed treatment is medical, dental, or just orthodontics. For example, consider a patient who seeks orthodontics because she is concerned about mildly crowded lower incisors. For that individual, controlling periodontal disease might be more beneficial than aligning teeth that would require permanent retention, and this should be emphasized when a treatment plan is discussed with the patient, even though she initially sought only orthodontic treatment. Any treatment plan should be developed, in collaboration with the patient, to do what on balance would be best for that individual.
When a group of dentists and dental specialists meet to plan treatment for a patient with complex problems, questions for the orthodontist often are along the lines of “Could you retract the incisors enough to correct the overjet?” or “Could you develop incisal guidance for this patient?” To a question phrased as, “Could you …?” the answer often is yes, given an unlimited commitment to treatment. The more appropriate question is not “Could you …?” but “Should you …?” or “Would it be best for the patient to …?” Cost-benefit and risk-benefit analyses (Figure 7-1) are introduced appropriately when the question is rephrased that way.
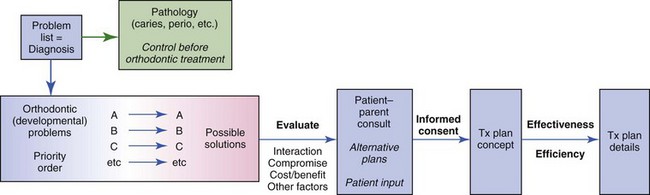
FIGURE 7-1 The treatment planning sequence. In treatment planning, the goal is wisdom, not scientific truth—judgment is required. Interaction with the patient and parent, so that they are involved in the decisions that lead to the final plan, is the key to informed consent.
A treatment plan in orthodontics, as in any other field, may be less than optimal if it does not take full advantage of the possibilities or if it is too ambitious. There is always a temptation to jump to conclusions and proceed with a superficially obvious plan without considering all the pertinent factors. The treatment planning approach advocated here is specifically designed to avoid both missed opportunities (the false negative or undertreatment side of treatment planning) and excessive treatment (the false positive or overtreatment side), while appropriately involving the patient in the planning.
At this point, before we talk in detail about the steps in going from the problem list to the final treatment plan that are outlined in Figure 7-1, let us examine some important concepts that underlie orthodontic treatment planning more generally.
Major Issues in Planning Treatment
Modern treatment planning must be an interactive process. No longer can the doctor decide, in a paternalistic way, what is best for a patient. Both ethically and practically, patients and parents must be involved in the decision-making process. Ethically, patients have the right to control what happens to them in treatment—treatment is something done for them not to them. Practically, the patient’s compliance is likely to be a critical issue in success or failure, and there is little reason to select a mode of treatment that the patient would not support. Informed consent, in its modern form, requires involving the patient in the treatment planning process. This is emphasized in the procedure for presenting treatment recommendations that is presented below.
Predictability and Complexity of Treatment
If alternative methods of treatment are available, as usually is the case, which one should be chosen? Data gradually are accumulating to allow choices to be based on evidence of outcomes rather than anecdotal reports and the claims of advocates of particular approaches. The quality of evidence for clinical decisions and how to evaluate the data as reports of treatment outcomes become available are emphasized in Chapter 1.
The complexity of the proposed treatment affects treatment planning, especially in the context of who should do the treatment. The focus of this chapter is on planning comprehensive orthodontic treatment. In orthodontics as in all areas of dentistry, it makes sense that the less complex cases would be selected for treatment in general or family practice, while the more complex cases would be referred to a specialist. In family practice, an important issue is how you rationally select patients for treatment or referral. A formal scheme is presented in Chapter 11 for separating child patients most appropriate for orthodontic treatment in family practice from those more likely to require complex treatment, and a similar scheme for adults appears in Chapter 18.
Treatment Possibilities
As further background for planning comprehensive treatment, it is important to consider two controversial aspects of current orthodontic treatment planning: the extent to which arch expansion versus extraction is indicated as a solution for crowding in the dental arches and the extent to which growth modification versus extraction for camouflage or orthognathic surgery should be considered as solutions for skeletal problems.
Dental Crowding: To Expand or Extract?
From the beginning of the specialty, orthodontists have debated the limits of expansion of the dental arches and whether the advantages of extraction of some teeth to provide space for the others outweigh the disadvantages. With extraction, the loss of a tooth or teeth is a disadvantage, greater stability of the result is likely and is an advantage, and there may be positive or negative effects on facial esthetics. But in fact for any individual patient the decision is a value judgment. It is not only appropriate but necessary to discuss the pros and cons with the patient and parent before making the expansion-extraction decision.
In a rational contemporary view, the majority of orthodontic patients can and should be treated without removal of teeth, but some will require extraction to compensate for crowding, incisor protrusion that affects facial esthetics, or jaw discrepancy. Their number varies, depending on the population being treated. Extraction for camouflage is considered separately later in this chapter, in the context of treatment for skeletal problems. The next section is a discussion of the limits of expansion, and therefore the indications for extraction, for patients with the normal jaw relationships that underlie Class I crowding/protrusion. Facial and dental esthetics, posttreatment stability, and dental occlusion are the key considerations.
Esthetic Considerations
If the major factors in extraction decisions are stability and esthetics, it is worthwhile to review existing data that relate these factors to expansion and extraction. Consider esthetics first. The conceptual relationship between expansion/extraction and esthetics is illustrated in Figure 7-2. All other things being equal, expansion of the arches moves the patient in the direction of more prominent teeth, while extraction tends to reduce the prominence of the teeth. Facial esthetics can become unacceptable on either the too-protrusive or too-retrusive side.

FIGURE 7-2 Expansion of the dental arches tends to make the teeth more prominent and extraction makes them less prominent. The choice between extraction and nonextraction (expansion) treatment is a critical esthetic decision for some patients who are toward the extremes of incisor protrusion or retrusion initially, but because there is an acceptable range of protrusion, many if not most can be treated with satisfactory esthetics either way. This is especially true if expansion is managed so as not to produce too much incisor protrusion or space closure after extraction is controlled so as not to produce too much incisor retraction. Similarly, expansion tends to make arches less stable and extraction favors stability, but the extraction/nonextraction decision probably is a critical factor in stability largely for patients who are toward the extremes of the protrusion-retrusion distribution. There are no data to show the percentage of patients who could be treated satisfactorily with either extraction or arch expansion versus the number for whom the extraction/nonextraction decision is critical in determining a satisfactory outcome.
At what point have the incisors been moved too far forward so that facial appearance is compromised? The answer is found in soft tissue not hard tissue relationships: When the prominence of the incisors creates excessive lip separation at rest so that the patient must strain to bring the lips together, the teeth are too protrusive and retracting the incisors improves the facial appearance (Figure 7-3). Note that this has remarkably little to do with the prominence of the teeth relative to the supporting bone as seen in a profile view. An individual with thick, full lips looks good with incisor prominence that would not be acceptable in someone with thin, tight lips. You simply cannot determine the esthetic limit of expansion from tooth–bone relationships on a cephalometric radiograph.

FIGURE 7-3 In patients with excessive incisor protrusion, retracting the incisors improves facial esthetics. This young woman sought treatment because of dissatisfaction with the appearance of her teeth. After orthodontic treatment with premolar extraction and incisor retraction, dental and facial appearance were significantly improved. A and B, Appearance on smile before and after treatment. C and D, Profile before and after treatment.
At what point are the incisors retracted to the point of adversely affecting facial esthetics? This too depends largely on the soft tissues. The size of the nose and chin has a profound effect on relative lip prominence. For a patient with a large nose and/or a large chin, if the choices are to treat without extraction and move the incisors forward or to extract and retract the incisors at least somewhat, moving the incisors forward is better, provided it does not separate the lips too much. The upper incisors are too far lingually if the upper lip inclines backward—it should be slightly forward from its base at soft tissue point A (Figure 7-4, A). For best esthetics, the lower lip should be at least as prominent as the chin (Figure 7-4, B). Variations in chin morphology may put the proper incisor–chin relationship beyond the control of orthodontics alone, in which case chin surgery perhaps should be considered (see the sections in this chapter on Class II camouflage and maximizing esthetic changes in treatment and Chapter 19).

FIGURE 7-4 A, An upper lip that inclines backward relative to the true vertical line, which can result from retraction of upper incisors to correct excessive overjet, tends to compromise facial esthetics, as does a poorly-defined labiomental sulcus when lip strain is required to bring the lips together. B, Retroclined mandibular incisors, as in this patient with a prominent chin and dental compensation for a skeletal Class III jaw relationship, are another cause of a poorly-defined labiomental sulcus.
Stability Considerations
For stable results, how much can arches be expanded? The lower arch is more constrained than the upper, and so its limitations for stable expansion may be somewhat tighter than the upper arch. Current guidelines for the limits of expansion of the lower arch, admittedly based on limited data, are presented in Figure 7-5. The 2 mm limitation for forward movement of the lower incisors obviously is subject to considerable individual variation but makes sense in light of the observation that lip pressure increases sharply 2 mm out into space usually occupied by the lip (see Chapter 5). If lip pressure is the limiting factor in forward movement, as it probably is, the initial position of the incisors relative to the lip would be a consideration in how much movement could be tolerated. This suggests and clinical observation seems to confirm (again, limited data!) that incisors tipped lingually away from the lip can be moved farther forward than upright incisors. Incisors tipped labially and crowded probably represent the equivalent of a titrated end point in a chemical reaction, in that they have already become as protrusive as the musculature will allow. Moving them any further forward carries great risk of instability (see Figure 7-2).
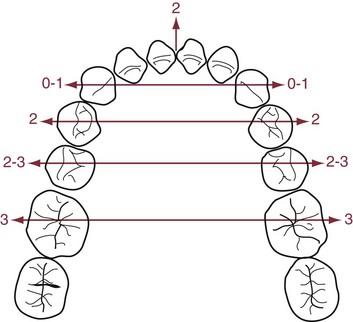
FIGURE 7-5 Because the lower arch is more constrained, the limits of expansion for stability seem to be tighter for it than the maxillary arch. The available data suggest that moving lower incisors forward more than 2 mm is problematic for stability, probably because lip pressure seems to increase sharply at about that point. A considerable body of data shows that expansion across the canines is not stable, even if the canines are retracted when they are expanded. Expansion across the premolars and molars, in contrast, can be stable if it is not overdone.
There also is a soft tissue limitation in how far the incisors, especially the lower incisors, can be moved facially. Fenestration of the alveolar bone and stripping of the gingiva become increasingly likely as the incisors are advanced. The amount of attached gingiva is a critical variable. It is important to carefully monitor patients who have a marginal amount of attached gingiva so that they can be treated promptly if a problem arises (Figure 7-6). Pretreatment consultation with a periodontist often is advisable, and depending on the amount and direction of planned tooth movement, placing a gingival graft before orthodontic treatment begins may be the best option for these patients.
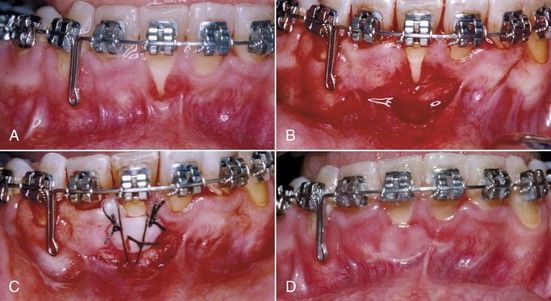
FIGURE 7-6 A, Gingival recession beginning to appear in a patient whose crowded lower incisors were aligned with some advancement despite premolar extraction to provide space. B, Preparation of a bed for a free gingival graft. C, The graft (tissue taken from the palate) sutured in position. D, 2 weeks later. (Courtesy Dr. J. Moriarty.)
Figure 7-5 suggests that there is more opportunity to expand transversely than anteroposteriorly—but only posterior to the canines. Numerous reports show that transverse expansion across the canines is almost never maintained, especially in the lower arch. In fact, intercanine dimensions typically decrease as patients mature, whether or not they had orthodontic treatment, probably because of lip pressures at the corners of the mouth. Expansion across the premolars and molars is much more likely to be maintained, presumably because of the relatively low cheek pressures.
One approach to arch expansion is to expand the upper arch by opening the midpalatal suture. If the maxillary base is narrow, this is appropriate treatment (see the discussion of transverse maxillary deficiency below). Some clinicians theorize (with no supporting evidence) that generously expanding the upper arch by opening the suture, temporarily creating a buccal crossbite, allows the lower arch then to be expanded more than otherwise would have been possible. If the limiting factor is cheek pressure, it seems unlikely that the method of expansion would make any difference. Excessive expansion carries the risk of fenestration of premolar and molar roots through the alveolar bone. There is an increasing risk of fenestration beyond 3 mm of transverse tooth movement.1
Contemporary Extraction Guidelines
Contemporary guidelines for orthodontic extraction in Class I crowding cases can be summarized as follows:
• Less than 4 mm arch length discrepancy: Extraction rarely indicated (only if there is severe incisor protrusion or in a few instances, a severe vertical discrepancy). In some cases, this amount of crowding can be managed without arch expansion by slightly reducing the width of selected teeth, being careful to coordinate the amount of reduction in the upper and lower arch.
• Arch length discrepancy 5 to 9 mm: Nonextraction or extraction treatment possible. The decision depends on both the hard- and soft-tissue characteristics of the patient and on how the final position of the incisors will be controlled; any of several different teeth could be chosen for extraction. Nonextraction treatment usually requires transverse expansion across the molars and premolars, and additional treatment time if the posterior teeth are to be moved distally, to increase arch length.
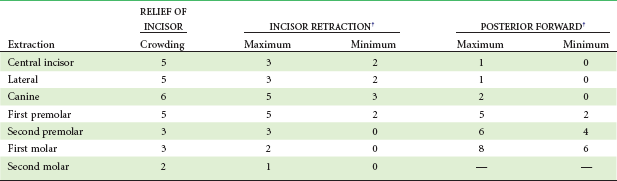
• Arch length discrepancy 10 mm or more: Extraction almost always required. For these patients, the amount of crowding virtually equals the amount of tooth mass being removed, and there would be little or no effect on lip support and facial appearance. The extraction choice is four first premolars or perhaps upper first premolars and mandibular lateral incisors. Second premolar or molar extraction rarely is satisfactory because it does not provide enough space near crowded anterior teeth or options to correct midline discrepancies (Table 7-1).
The presence of protrusion in addition to crowding, of course, complicates the extraction decision. Retracting the incisors to reduce lip prominence requires space within the dental arch. The effect is to increase the amount of arch length discrepancy. With that adjustment, the guidelines above can be applied. As a general rule, the lips will move two-thirds of the distance that the incisors are retracted (i.e., 3 mm of incisor retraction will reduce lip protrusion by 2 mm), but there is a great deal of individual variation, especially in the change that occurs when lip competence is reached. Two to three mm of lip retraction is a usual outcome.
It is interesting but not surprising that retrospective studies of changes in dental arch dimensions and facial appearance in extraction versus nonextraction cases show highly variable changes in both groups. The idea that extraction leads to incisor retraction and narrower arches and that nonextraction leads to incisor protrusion and wider arches is not well supported.2,3 The amount of change in both groups, of course, would be related to the amount of crowding and protrusion that was present initially and to the clinician’s decision as to how to manage arch expansion or closure of extraction spaces. Perhaps a final set of guidelines could be as follows:
• The more you can expand without moving the incisors forward, the more patients you can treat satisfactorily (from the perspective of both esthetics and stability) without extraction.
• The more you can close extraction spaces without overretracting the incisors, the more patients you can treat satisfactorily (again, from the perspective of both esthetics and stability) with extraction.
• For oral health, excessive expansion increases the risk of mucogingival problems.
• For masticatory function, expansion or extraction makes no difference.
Guidelines for extraction to camouflage jaw discrepancies are presented immediately below, in the discussion of that approach to skeletal problems.
Skeletal Problems: Growth Modification versus Camouflage
If it were possible, the best way to correct a jaw discrepancy would be to get the patient to grow out of it. Because the pattern of facial growth is established early in life and rarely changes significantly (see Chapter 2), this is unlikely without treatment. The important questions in planning treatment are the extent to which growth can be modified, and how advantageous it is to start treatment prior to adolescence. Now that data from randomized clinical trials are available for Class II treatment outcomes, there is less reason for controversy about the best way to treat those patients (discussed in detail below), but skeletal problems in other planes of space remain controversial. Additional information on methods for early treatment of skeletal problems is presented in Chapter 12.
Transverse Maxillary Deficiency
It is appropriate to discuss maxillary deficiency at the beginning of this discussion of skeletal problems because of its relationship to the extraction–nonextraction decision that was just reviewed. In a child with crowded teeth, a diagnosis of deficient maxillary width can become a convenient rationale for enough transverse expansion to align the teeth. If the maxilla is narrow relative to the rest of the face, a diagnosis of transverse maxillary deficiency is justified and skeletal expansion probably is appropriate. Both the width of the maxillary premolar teeth (via Pont’s index, an old and now-discredited approach)4 and the width of the palate compared to population norms have been advocated as methods to diagnose maxillary deficiency. As we have emphasized in Chapter 6, the appropriate comparison of maxillary width should be to other transverse proportions in the same patient (for example, bizygomatic width), not to population averages.
Like all craniofacial sutures, the midpalatal suture becomes more tortuous and interdigitated with increasing age (see Figure 8-30). Almost any expansion device (a lingual arch, for example) will tend to separate the midpalatal suture in addition to moving the molar teeth in a child up to age 9 or 10. By adolescence, relatively heavy force from a rigid jackscrew device (Figure 7-7) is needed to separate the partially interlocked suture, which must be microfractured. The maxilla opens as if on a hinge superiorly at the base of the nose and also opens more anteriorly than posteriorly.
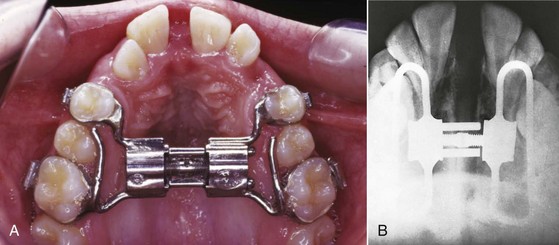
FIGURE 7-7 Transverse force across the maxilla in children and adolescents can open the midpalatal suture. A, The expansion force is usually delivered with a jackscrew mechanism fixed to maxillary teeth, as in this Hyrax expander with metal framework and jackscrew, seen at the end of rapid expansion (0.5 mm/day). The maxilla opens as if on a hinge, with its apex at the bridge of the nose. B, The suture also opens on a hinge anteroposteriorly, separating more anteriorly than posteriorly, as shown in this radiograph of a patient after rapid expansion.
It is important to realize that heavy force and rapid expansion should not be used in preschool children because of the risk of producing undesirable changes in the nose at that age (Figure 7-8). After adolescence, there is an increasing chance with advancing age that bone spicules will have interlocked the suture to such an extent that it cannot be forced open, and at that point surgery to reduce the resistance to expansion is the only way to widen the palate (see Chapter 18).
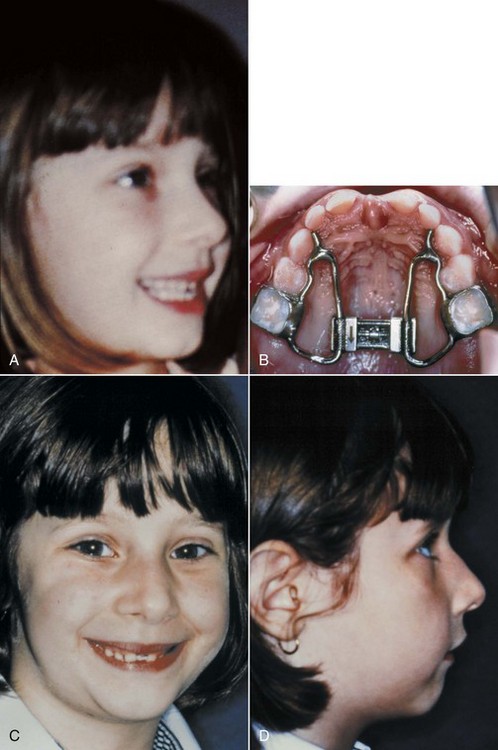
FIGURE 7-8 Rapid palatal expansion in young children can lead to undesirable changes in the nose, as in this 5-year-old who had expansion at the rate of  mm/day (2 turns/day of the jackscrew). A, Nasal contours before treatment. B, Jackscrew appliance after activation over a 10-day period. C and D, Nasal hump and paranasal swelling, which developed after the child complained of discomfort related to the expansion. (Courtesy Dr. D. Patti.)
mm/day (2 turns/day of the jackscrew). A, Nasal contours before treatment. B, Jackscrew appliance after activation over a 10-day period. C and D, Nasal hump and paranasal swelling, which developed after the child complained of discomfort related to the expansion. (Courtesy Dr. D. Patti.)
In adolescents, expansion across the suture can be done in three ways: (1) rapid expansion with a jackscrew device attached to the maxillary posterior teeth, the original (1960s) method, typically at the rate of 0.5 to 1 mm/day; (2) slow expansion with the same device at the rate of approximately 1mm per week, the method advocated more recently; or (3) expansion with a device attached to bone screws or implants, so that the force is directly applied to the bone and there is no pressure against the teeth.
Rapid Palatal Expansion: A major goal of growth modification always is to maximize the skeletal changes and minimize the dental changes produced by treatment. The object of maxillary expansion is to widen the maxilla, not just expand the dental arch by moving the teeth relative to the bone. Originally, rapid expansion of the midpalatal suture (rapid palatal expansion [RPE]) was recommended to help meet this goal. The theory was that with rapid force application to the posterior teeth, there would not be enough time for tooth movement, the force would be transferred to the suture, and the suture would open up while the teeth moved only minimally relative to their supporting bone.
With RPE at a rate of 0.5 to 1 mm/day, a centimeter or more of expansion is obtained in 2 to 3 weeks, with most of the movement being separation of the two halves of the maxilla. A space appears between the central incisors. The space created at the midpalatal suture is filled initially by tissue fluids and hemorrhage, and at this point the expansion is highly unstable. The expansion device must be stabilized so that it cannot screw itself back shut and is left in place for 3 to 4 months. By then, new bone has filled in the space at the suture, and the skeletal expansion is stable. The midline diastema decreases and may disappear during this time.
The aspect of rapid expansion that was not appreciated initially was that orthodontic tooth movement continues after the expansion is completed, until bone stability is achieved. In most orthodontic treatment, the teeth move relative to a stable bony base. It is possible, of course, for tooth movement to allow bony segments to reposition themselves while the teeth are held in the same relationship to each other, and this is what occurs during the approximately 3 months required for bony fill-in at the suture after rapid expansion. During this time, the dental expansion is maintained, but the two halves of the maxilla move back toward each other, which is possible because at the same time the teeth move laterally on their supporting bone.
If the changes were represented graphically, the plot for rapid expansion would look like Figure 7-9, A. Note that when the expansion was completed, 10 mm of total expansion would have been produced by 8 mm of skeletal expansion and only 2 mm of tooth movement. At 4 months, the same 10 mm of dental expansion would still be present, but at that point there would be only 5 mm of skeletal expansion, and tooth movement would account for the other 5 mm of the total expansion. Rapid activation of the jackscrew, therefore, is not an effective way to minimize tooth movement.
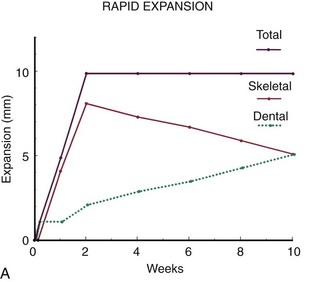
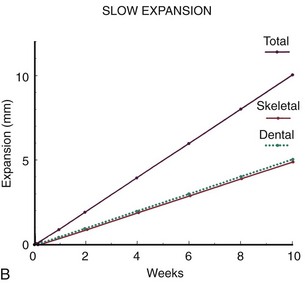
FIGURE 7-9 Diagrammatic representation of the typical skeletal and dental response to rapid (A) versus slow (B) palatal expansion. Rapid expansion was recommended when the technique was reintroduced in the 1960s because it was thought that this produced more skeletal than dental change. As the graph indicates, this is true initially: the teeth cannot respond, and the suture is opened. With 10 mm of expansion in 2 weeks, there might be 8 mm of skeletal change and only 2 mm of tooth movement at the time the expansion is completed. It was not appreciated at first that during the next 8 weeks, while bone is filling in, orthodontic tooth movement continues and allows skeletal relapse, so that although the total expansion is maintained, the percentage due to tooth movement increases and the skeletal expansion decreases. With slow expansion at the rate of 1 mm per week, the total expansion is about half skeletal/half dental from the beginning. The outcome of rapid versus slow expansion looks very different at 2 weeks but quite similar at 10 weeks.
Slow Palatal Expansion: Approximately 0.5 mm per week is the maximum rate at which the tissues of the midpalatal suture can adapt. If a jackscrew device attached to the teeth is activated at the rate of one-quarter turn of the screw (0.25 mm) every other day, the ratio of dental to skeletal expansion is about 1 to 1, tissue damage and hemorrhage at the suture are minimized, and a large midline diastema never appears. Ten mm of expansion over a 10-week period, at the rate of 1 mm per week, would consist of 5 mm of dental and 5 mm of skeletal expansion (Figure 7-9, B). The situation at the completion of active expansion is approximately analogous to RPE 2 to 3 months after expansion is completed, when bone fill-in has occurred. Thus the overall result of rapid versus slow expansion is similar,5 but with slower expansion a more physiologic response is obtained.
Implant-Supported Expansion: Now that bone screws can be placed in the maxilla to serve as temporary skeletal attachments, force can be applied directly to the maxilla instead of using the teeth to transfer force to the bone. This provides a way to expand the maxilla even if no teeth are present (Figure 7-10) and would avoid tooth movement and should produce almost total skeletal change in patients with lingual crossbite. With a jackscrew attached to skeletal anchors, minimum disruption of the suture would be desired, so slow rather than rapid expansion would be indicated.
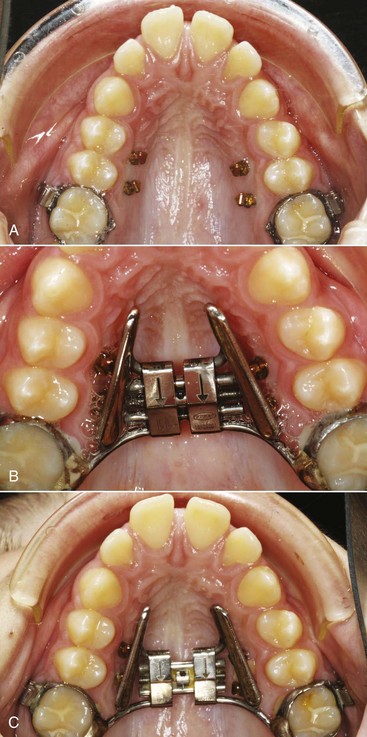
FIGURE 7-10 A, Narrow maxillary arch with palatal screws for delivery of expansion force directly to the bone. The expansion device has a wire framework that clips over the exposed head of the bone screws. B, Expansion device in place with initial activation of the jackscrew. Note that although the molars are attached to the expansion device, the attachment is to a bar along which the attachment can slide, so the expansion force will be only against the screws. C, Progress, as expansion continues and the molar attachment slides along the bar.
Following expansion by any means, a retainer is needed even after bone fill-in seems complete. The expansion appliance should remain in place for 3 to 4 months and then can be replaced with a removable retainer or other retention device.
Maxillary expansion is discussed further in Chapters 13 and 14.
Class II Problems
Changing Views of Class II Treatment: In the early years of the twentieth century, it was all but taken for granted that pressure against the growing face could change the way it grew. Extraoral force to the maxilla (headgear) was utilized by the pioneer American orthodontists of the late 1800s (Figure 7-11), who found it reasonably effective. This method of treatment was later abandoned, not because it did not work, but because Angle and his contemporaries thought that Class II elastics (from the lower molars to the upper incisors) would cause the mandible to grow forward and that this would produce an easier and better correction. At a later stage in the United States, guide planes consisting of a wire framework extending down from an upper lingual arch were used to force patients to advance the mandible upon closure, also with the idea of stimulating mandibular growth.

FIGURE 7-11 Extraoral force to the maxilla was used for Class II correction in the late 1800s and then abandoned, not because it was ineffective, but because the pioneer orthodontists thought that intraoral elastics produced the same effect. (From Angle EH. Treatment of Malocclusion of the Teeth. 7th ed. Philadelphia: SS White Manufacturing Co; 1907.)
With the advent of cephalometric analysis, it became clear that both elastics and guide planes corrected Class II malocclusion much more by displacing the mandibular teeth mesially than by stimulating mandibular growth. Even if the lack of desired change in jaw relationships is overlooked, correcting a skeletal Class II problem in this way is undesirable because the protruding lower incisors tend to upright after treatment and then lower incisor crowding and overjet return. Because of this, these methods and with them the idea of mandibular growth stimulation fell into disrepute in the United States, but growth modification with “functional appliances” that hold the mandible forward remained the mainstay of European orthodontics.
Although headgear was reintroduced into American orthodontics in the 1940s and came to be widely used in Class II treatment, it was seen primarily as a tooth-moving device until cephalometric studies in the late 1950s clearly demonstrated not only retraction of upper teeth but also effects on maxillary growth (Figure 7-12). By the 1980s, clinical success with functional appliances, including impressive amounts of mandibular growth in some cases, had been clearly demonstrated on both sides of the Atlantic, but questions remained as to whether these appliances could really stimulate mandibular growth.
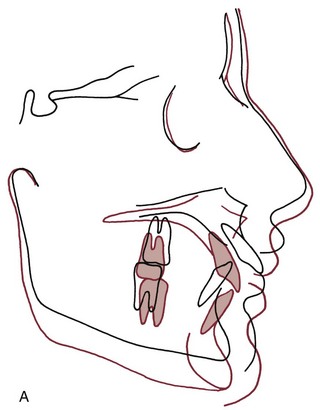

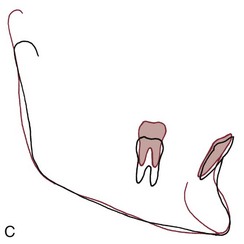
FIGURE 7-12 Cephalometric superimposition showing growth modification produced by extraoral force to the maxilla (straight-pull initially, then high-pull). In the cranial base superimposition (A), note that the maxilla has moved downward and backward, not in the downward and forward direction that would have been expected during growth (and that was shown by the mandible). From the maxillary superimposition (B), it can be seen that the protruding and spaced upper incisors were retracted, but there was very little posterior movement of the upper molars. In the mandibular superimposition (C), note that the lower molars erupted more than the upper molars (i.e., good vertical control of the upper molars was maintained).
This depends on how you look at it. Growth stimulation can be defined in two ways: (1) as the attainment of a final size larger than would have occurred without treatment or (2) as the occurrence of more growth during a given period than would have been expected without treatment. Figure 7-13 is a hypothetical plot of the response to functional appliance treatment, illustrating the difference between (1) absolute stimulation (larger as an adult) and (2) temporal stimulation (acceleration of growth). As the figure suggests, an acceleration of growth often occurs when a functional appliance is used to treat mandibular deficiency, but the final size of the mandible is little if any larger than it would have been without the treatment.6 Cephalometric superimposition often shows more mandibular growth in the first months of functional appliance treatment than would have been expected (Figure 7-14). This is likely to be followed by a decrease in growth later, so that although the mandible grew faster than normal for a while, later growth was slower than would have been expected and the ultimate size of the mandible in treated and untreated patients is similar.
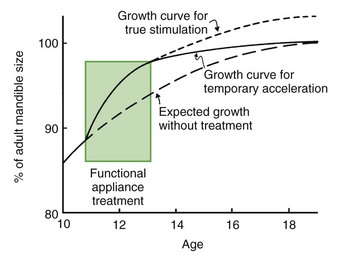
FIGURE 7-13 The difference between growth acceleration in response to a functional appliance and true growth stimulation can be represented using a growth chart. If growth occurs at a faster-than-expected rate while a functional appliance is being worn and then continues at the expected rate thereafter so that the ultimate size of the jaw is larger, true stimulation has occurred. If faster growth occurs while the appliance is being worn, but slower growth thereafter ultimately brings the patient back to the line of expected growth, there has been an acceleration not a true stimulation. Although there is a great deal of individual variation, the response to a functional appliance most often is similar to the solid line in this graph.
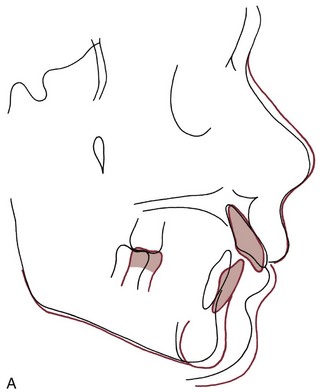
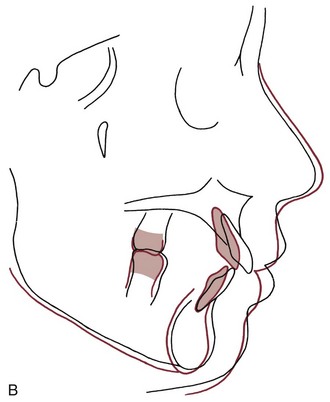
FIGURE 7-14 A, Cephalometric superimposition during treatment with a functional appliance (activator), showing excellent downward and forward mandibular growth between ages 11 and 13. B, Cephalometric superimpositions for same patient between ages 13 and 15, during fixed appliance therapy for final positioning of teeth. For this patient, the growth response to the activator was much more an acceleration than a true stimulation, as revealed by more growth than expected at first, and less growth later; yet the activator phase of treatment was quite successful in improving the jaw relationship.
If that view of their effect on mandibular growth is correct, functional appliances must do something else besides accelerate mandibular growth. Otherwise, the Class II malocclusion would never be corrected or would not stay corrected. In fact, these appliances also can affect the maxilla and the teeth in both arches. When the mandible is held forward, the elastic stretch of soft tissues produces a reactive effect on the structures that hold it forward. If the appliance contacts the teeth, this reactive force produces an effect like Class II elastics, moving the lower teeth forward and the upper teeth back, and rotating the occlusal plane. In addition, even if contact with the teeth is minimized, soft tissue elasticity can create a restraining force on forward growth of the maxilla, so that a “headgear effect” is observed (see Figure 7-14). Any combination of these effects can be observed after functional appliance treatment.
Randomized Clinical Trials of Early versus Later Class II Treatment: In the 1990s, two major projects using randomized clinical trial methodology and supported by the National Institute of Dental and Craniofacial Research were carried out at the University of North Carolina and University of Florida.7,8 More recently, an important trial at the University of Manchester that was supported by the Medical Research Council of the United Kingdom has been reported.9 The results provide by far the best data that ever have been available for the response to Class II growth modification treatment.
The data from all the trials show three important things: (1) on average, children treated prior to adolescence with either headgear or a functional appliance had a small but statistically significant improvement in their jaw relationship, while the untreated control children did not; (2) changes in skeletal relationships created during early treatment were at least partially reversed by later compensatory growth, in both the headgear and functional appliance groups; and (3) at the end of comprehensive treatment during adolescence, there were no significant differences between the early treatment patients and the previously untreated controls. In short, it seems to make remarkably little difference whether growth modification is done with headgear or a functional appliance, and it is equally effective and more efficient to do it during the adolescent growth spurt rather than prior to adolescence. Further data from the trials and data from well-designed and controlled retrospective studies are discussed in more detail in Chapter 13.
Camouflage by Tooth Movement: Tooth movement alone cannot correct a skeletal malocclusion, but if the malocclusion is corrected and the facial appearance is acceptable, the overall treatment outcome can be quite satisfactory. This is called orthodontic camouflage for the simplest of reasons: camouflage means that the jaw discrepancy is no longer apparent. Of course, treatment with tooth movement is successful only if both the facial appearance and dental occlusion are satisfactory.
The following three patterns of tooth movement can be used to correct a Class II malocclusion:
• A combination of retraction of the upper teeth and forward movement of the lower teeth, without tooth extractions
• Retraction of maxillary incisors into a premolar extraction space
• Distal movement of maxillary molars and eventually the entire upper dental arch.
Nonextraction treatment with Class II elastics: If forward movement of the lower arch can be accepted, a Class II malocclusion can be corrected just with the use of Class II elastics (or their equivalent in the form of fixed connectors). The correction is achieved, however, much more by forward movement of the lower arch than by moving the upper teeth back. Rarely, excess overjet and Class II buccal segments are due to a lower arch that is distally positioned on the mandible, and then moving the lower teeth forward is exactly what is needed. Almost always, however, Class II patients have the lower teeth normally positioned on the mandible or proclined to some extent. For these patients, the result of Class II elastics or their equivalent in the form of a fixed functional appliance is likely to be a convex profile with protrusive lower incisors and a prominent lower lip. This is best described as relapse waiting to occur (Figure 7-15). After treatment, lip pressure that moves the lower incisors lingually leads to incisor crowding, return of overjet, and return of overbite as the incisors tend to erupt back into occlusal contact from their lingual position.
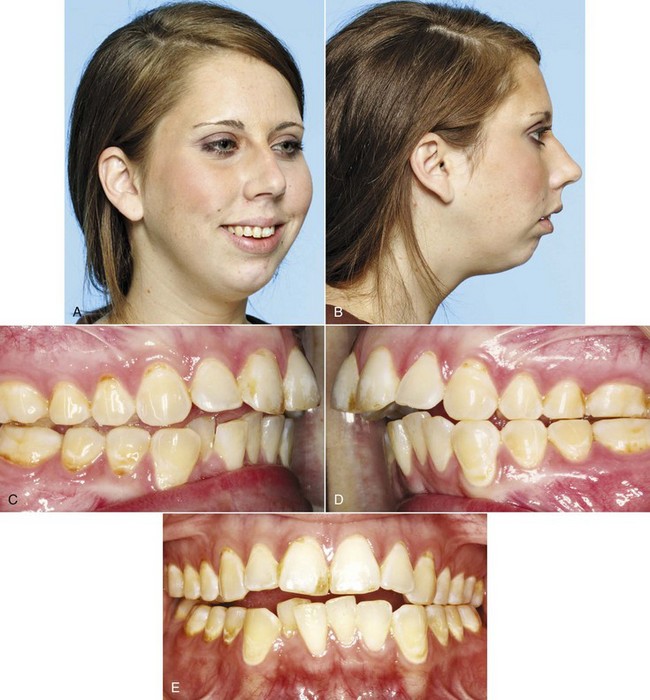
FIGURE 7-15 It is possible with Class II elastics to correct a Class II malocclusion largely by moving the mandibular teeth forward relative to the mandible, but in a patient with a skeletal Class II due to mandibular deficiency, the result is both unesthetic and unstable. This girl, treated in this way, sought retreatment 5 years after treatment of that type. A and B, Frontal and profile facial photos, showing the prominence of the lower lip relative to the chin. C to E, Intraoral photos. Note that although the molar relationship is still almost Class I on the right side and ½ cusp Class II on the left, there has been a major return of overjet because the lower incisors have tipped lingually and become crowded. Vertically, relapse toward open or deep bite, whichever was present initially, is likely, so this patient almost surely had an open bite tendency before her initial treatment.
Retraction of the upper incisors into a premolar extraction space: A straightforward way to correct excessive overjet is to retract the protruding incisors into space created by extracting the maxillary first premolars. Without lower extractions, the patient would have a Class II molar relationship but normal overjet and canine relationships at the end of treatment. Temporary skeletal anchorage is very useful when maximum incisor retraction is desired or if the maxillary molars have little anchorage value because of bone loss. If mandibular first or second premolars also are extracted, Class II elastics can be used to bring the lower molars forward and retract the upper incisors, correcting both the molar relationship and the overjet.
Although premolar extraction for Class II correction can produce excellent occlusion and an acceptable dentofacial appearance,10 there are potential problems with this approach. If the patient’s Class II malocclusion is primarily due to mandibular deficiency, retracting the maxillary incisors would create a maxillary deformity to go with the mandibular one, which is difficult to justify as correct treatment (see the discussion of Class II camouflage in adults in Chapter 18). Extractions in the lower arch allow the molars to come forward into a Class I relationship, but it would be important to close the lower space without retracting the lower incisors. If Class II elastics are used, the upper incisors are elongated as well as retracted, which can produce an undesirable “gummy smile.”
Maxillary premolar extraction for Class II correction has been criticized as a risk factor for future TM dysfunction (TMD). No relationships between symptoms of TMD and the type of orthodontic treatment were noted in any of a considerable series of reports in the early 1990s. The best data come from a study in which a careful compilation of retrospective data was used to create two groups of patients whose “borderline” Class II malocclusions could have been treated equally plausibly with or without premolar extraction. One group had extractions, the other did not. Both groups had low scores for signs or symptoms of dysfunction, and there was no difference between them in any aspect of TM joint function.11 There is simply no evidence to support the allegation that maxillary premolar extraction causes TMD.
Distal movement of the upper teeth: If the upper molars could be moved posteriorly, this would correct a Class II molar relationship and provide space into which the other maxillary teeth could be retracted. If the maxillary first molars are rotated mesiolingually, as they often are when a Class II molar relationship exists, correcting the rotation moves the buccal cusps posteriorly and provides at least a small space mesial to the molar (Figure 7-16). Tipping the crowns distally to gain space is more difficult, and bodily distal movement is more difficult still. There are two problems: (1) it is difficult to maintain the first molar in a distal position while the premolars and anterior teeth are moved back, so it must be moved back a considerable distance, especially if it is tipped distally; and (2) the farther it must be moved, the more the second and third molars are in the way.
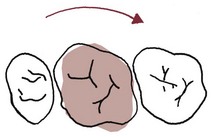
FIGURE 7-16 In a patient with Class II malocclusion, the upper first molar usually is rotated mesiolingually. Correcting this rotation, which is necessary to obtain proper occlusion with the lower first molar, usually moves the buccal cusps distally (but also tends to move the lingual cusps mesially). This improves the buccal occlusal relationship and, if the patient wears headgear as this is done, creates at least a modest amount of space for retraction of other maxillary teeth.
From this perspective, it is easy to understand that the most successful way to move a maxillary first molar distally is to extract the second molar, which creates space for the tooth movement. Until quite recently, the anchorage created by a transpalatal lingual arch was accepted as the best way to undertake distalization of the maxillary dentition. Although it is at least theoretically possible to do this with headgear, this type of treatment is time-consuming and requires excellent patient cooperation. Palatal anchorage for the molar movement can be created by splinting the maxillary premolars and including an acrylic pad in the splint so that it contacts the palatal mucosa. In theory, the palatal mucosa resists displacement; in clinical use, tissue irritation is likely. Even with the more elaborate appliances of this type (Figure 7-17), only about two-thirds of the space that opens between the molars and premolars is from distal movement of the molars, even when the molars are tipped distally. They tend to come forward again when the other maxillary teeth are retracted (see Chapter 15 for more details), so more than a half-cusp molar correction cannot be expected. The ideal patient for treatment with this approach, therefore, is one with minimal growth potential, a reasonably good jaw relationship (not severely mandibular deficient) and a half-cusp Class II molar relationship.

FIGURE 7-17 Molar distalization can be carried out with a variety of appliances that depend on the anterior teeth and the palate for anchorage. A, Combination distalization-expansion appliance (Pendex) at initial application. B, Appearance at appliance removal. Note the successful opening of space, but the tissue irritation caused by contact with the palatal mucosa. C, Nance holding arch with palatal button later in the same patient to maintain the molar position while alignment of the other teeth is completed. Appliances of this type now are rapidly being replaced by bone anchors (temporary anchorage devices [TADs]).
Using temporary skeletal anchorage greatly improves the amount of true distal movement of the maxillary dentition that can be achieved, and makes it possible to distalize both the second and first molars. It still is necessary to create some space in the tuberosity region, so removal of third molars is likely to be required later if it is not done immediately. In typical treatment, bone anchors are placed bilaterally in the vicinity of the base of the zygomatic arch (Edward Angle’s “key ridge”) or in the palate, and a nickel-titanium spring generates the force needed for distalization (Figure 7-18). For this purpose, bone screws between the teeth prevent the necessary distal movement of roots mesial to the screw. Although good data for typical treatment outcomes still do not exist, in some patients it has been possible to produce up to 6 mm of distal movement of first and second molars.12 In addition, the premolars migrate distally as the molars are moved back (which is due to the supercrestal fiber network). This makes the premolar retraction less complicated, and there also is no reaction force against the incisors to move them facially.
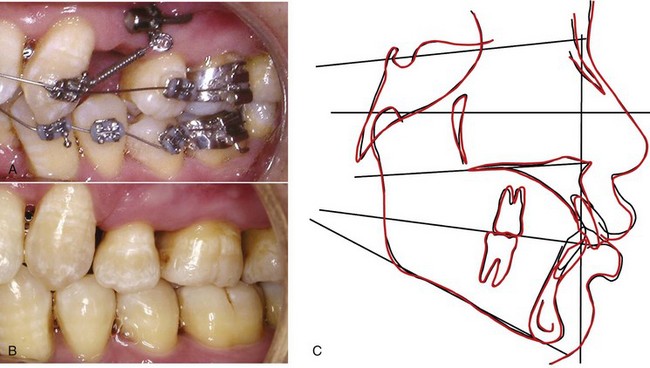
FIGURE 7-18 A, Bone anchor (miniplate attached to the base of the zygomatic arch with three screws, with only the tube for attachment of springs or screws extending into the mouth) for retraction of severely protrusive maxillary incisors in a young adult with bone loss from periodontal disease (so that the maxillary posterior teeth had little anchorage value). B, Retraction completed. Note that the Class II molar relationship has been maintained. Without skeletal anchorage the maxillary molars would have moved farther anteriorly into a super-Class II relationship. C, Cephalometric superimpositions on cranial base and maxilla, showing the extent of maxillary incisor retraction without any forward movement of the posterior teeth. For this amount of tooth movement in an adult, a single screw in the alveolar process on each side might not be stable.
The caveat, of course, is that moving the upper arch back that far may not be compatible with an acceptable facial appearance. If a Class II malocclusion is due to maxillary dental protrusion, moving the upper teeth back is a logical treatment approach. But if there is a significant component of mandibular deficiency, retraction of the maxillary incisors after distal movement of the molars and premolars has the same potential problem that can arise with first premolar extraction to allow retraction of the incisors: correcting the malocclusion in that way may detract from rather than enhance facial appearance.
Summary: In the absence of favorable growth, treating a Class II relationship in adolescents is difficult. Compromises may have to be accepted in order to correct the occlusion. Fortunately, even though growth modification cannot be expected to totally correct an adolescent Class II problem, some forward movement of the mandible relative to the maxilla does contribute to successful treatment of the average patient. The rest of the correction must occur from some combination of retraction of the upper incisors and forward movement of the lower arch. When little or no growth can be expected, orthognathic surgery to advance the mandible may be necessary to achieve a satisfactory result (see Chapter 19).
Class III Problems
Growth modification for Class III patients is just the reverse of Class II: what is needed is differential growth of the maxilla relative to the mandible. Edward Angle’s concept was that Class III malocclusion was due exclusively to excessive mandibular growth. In fact, almost any combination of deficient maxillary growth and excessive mandibular growth can be found in Class III patients, and maxillary deficiency and mandibular excess are about equally likely. The realization that maxillary deficiency is so frequently a component of skeletal Class III and the development of new possibilities for correcting it have led recently to a great increase in treatment aimed at promoting maxillary growth. Unfortunately, data from randomized clinical trials are not available, and treatment recommendations must be based on reports from small and often poorly controlled studies.
Horizontal-Vertical Maxillary Deficiency: If headgear force compressing the maxillary sutures can inhibit forward growth of the maxilla, reverse (forward-pull) headgear separating the sutures should stimulate growth. Until Delaire and coworkers in France showed that forward positioning of the maxilla could be achieved with reverse headgear, if treatment was begun at an early age, reverse pull headgear (Figure 7-19) was remarkably unsuccessful in producing anything but movement of the upper teeth. The French results suggested that successful forward repositioning of the maxilla can be accomplished before age 8, but after that, orthodontic tooth movement began to overwhelm skeletal change, and more recent studies comparing untreated Class III children to those treated with maxillary protrusion have confirmed greater skeletal change at earlier ages.13 Long-term follow-up suggests that for a good chance of success, treatment should begin by age 10 at the latest.14 The chance of successful forward movement is essentially zero by the time sexual maturity is achieved.
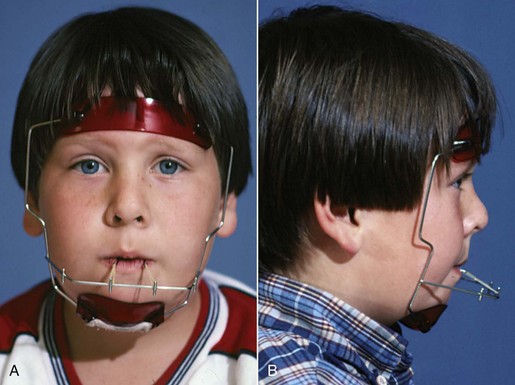
FIGURE 7-19 A and B, Delaire-type facemask (sometimes called reverse headgear) used to place forward traction against the maxilla. Because the maxilla often is deficient vertically and anteroposteriorly, a downward and forward direction of force usually is needed.
Even in young patients, two side effects of treatment are almost inevitable when reverse headgear that attaches to the teeth is used (Figure 7-20): forward movement of maxillary teeth relative to the maxilla and downward and backward rotation of the mandible. For this reason, in addition to being quite young, the ideal patients for treatment with this method would have both:
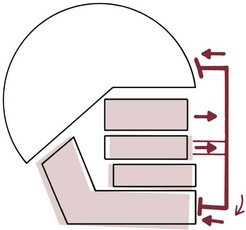
FIGURE 7-20 Forward traction against the maxilla typically has three effects: (1) some forward movement of the maxilla, the amount depending to a large extent on the patient’s age; (2) forward movement of the maxillary teeth relative to the maxilla; and (3) downward and backward rotation of the mandible because of the reciprocal force placed against the chin.
• Normally positioned or retrusive, but not protrusive, maxillary teeth
• Normal or short, but not long, anterior facial vertical dimensions
An obvious way to decrease the amount of tooth movement in face mask treatment would be to place the traction force to skeletal anchors in the maxilla (see Figure 7-10). As with all applications of skeletal anchorage, only preliminary reports with this technique are available as yet, but already it is clear that skeletal anchorage can be used to help bring the maxilla forward.15 Treatment using reverse-pull headgear is discussed in detail in Chapter 13.
Mandibular Excess: Although extraoral force applied via a chin cup is an old idea (Figure 7-21), this is not analogous to the use of extraoral force against the maxilla because there are no mandibular sutures to influence. If the cartilage of the mandibular condyle were a growth center with the capacity to grow independently, one would not expect chin cup therapy to be particularly successful. From the opposite and more contemporary view that condylar growth is largely a response to translation as surrounding tissues grow, a more optimistic view of the possibilities for growth restraint would be warranted. Research in recent years (see Chapter 2) indicates that the second view of mandibular growth is more correct. Nevertheless, results from chin cup therapy are usually discouraging. Downward-backward rotation of the mandible, not a real diminution in mandibular growth, is the usual observation.
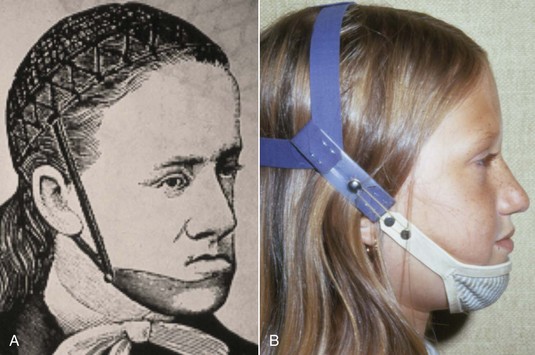
FIGURE 7-21 A, Illustration from an orthodontic text of the 1890s, showing a chin cup device to try to restrain mandibular growth. B, Chin cup appliance from the 1970s, with a soft rather than hard cup. The soft cup is more comfortable but increases the chance that the lower incisors will be tipped lingually, which is undesirable in skeletal Class III patients. Neither version is really effective in restraining growth. The comment over a century ago was “Unfortunately this doesn’t work very well.” The same comment applies now. (From Proffit WR, White RP, Sarver DM. Contemporary Treatment of Dentofacial Deformity. St. Louis: Mosby; 2003.)
DeClerck and coworkers have recently reported that when relatively light but full-time force from Class III elastics is used from skeletal anchors in the maxilla to skeletal anchors in the mandible, effects on both maxillary and mandibular growth are observed.16,17 This intriguing new approach is discussed in some detail in Chapter 13.
Class III Camouflage: It is quite possible to correct moderately severe Class III malocclusions by proclining the maxillary incisors and retracting the mandibular incisors into an extraction space, and applications of skeletal anchorage now make it possible to move the entire mandibular dentition distally. Unfortunately, this often becomes an illustration of camouflage failure rather than successful treatment (Figure 7-22). Failure is especially likely when the patient has a large and prominent mandible. The problem is that retracting the mandibular teeth tends to make the chin more prominent. Improving the dental occlusion while making the jaw discrepancy more obvious is not successful treatment.18

FIGURE 7-22 It also is possible to correct a Class III malocclusion with Class III elastics, which brings the maxillary incisors forward and retracts the mandibular incisors. This patient sought retreatment 2 years after her orthodontic treatment was completed because she thought her facial appearance was unacceptable. A and B, Frontal and profile views. Note the prominence of the chin and the accentuated nasomaxillary folds, both due to the jaw discrepancy. C to E, Intraoral views. The dental occlusion is almost perfect. Before the jaw discrepancy can be corrected surgically, it will be necessary to recreate reverse overjet, advancing the mandibular incisors as much as possible.
A patient who might be a candidate for Class III camouflage would have:
• Reverse overjet largely due to protrusive mandibular incisors and retrusive maxillary incisors, with more maxillary deficiency than mandibular prognathism.
• Short anterior face height, so that downward-backward rotation of the mandible would improve both anteroposterior and vertical facial proportions.
This combination of features is rare in patients of European descent but occurs more frequently in Asians, so Class III camouflage is likely to be more useful in patients of Asian descent.
Vertical Problems
Skeletal vertical problems, both the short-face and long-face patterns, do not lend themselves to camouflage via tooth movement. For short-face patients, growth modification involves rotating the mandible down and back without creating anteroposterior mandibular deficiency, which is why a short-face Class III problem is more treatable than a long-face Class III. Functional appliances can be quite successful with short-face Class II children. This approach to treatment is discussed in detail in Chapter 13.
The long-face pattern of growth is remarkably difficult to modify,19 and elongating the anterior teeth to close an accompanying open bite is the antithesis of camouflage. It predictably makes facial appearance worse. Until recently, the only successful treatment approach required orthognathic surgery to vertically reposition the maxilla, and this still is the best treatment for severe skeletal open bite (see Chapter 19). With bone screws or bone anchors, it now is possible to intrude posterior teeth. This has opened a new avenue of treatment for patients with moderately severe long face problems, which is discussed in Chapter 18.
Reducing Uncertainty in Planning Treatment
Even when excellent data from clinical trials are available, it is difficult to predict how any one individual will respond to a particular plan of treatment. Variability must be expected. In orthodontics, two interrelated factors contribute most of the variability: the patient’s growth pattern and the effect of treatment on the expression of growth. At present, in the absence of growth, treatment responses are reasonably predictable. Unfortunately, growth can be remarkably unpredictable.
Growth Prediction
Because predicting facial growth would be of great benefit in planning orthodontic treatment, repeated efforts have been made to develop methods to do this from cephalometric radiographs. Successful prediction requires specifying both the amount and the direction of growth, in the context of a baseline or reference point. The serial cephalometric radiographs obtained during the Bolton, Burlington, and Michigan growth studies (see Chapter 4) have been treated statistically to allow their use in growth prediction, by grouping the data to provide a picture of average, normal growth changes. A convenient way to show average growth changes is with templates that show the expected direction and increment of growth at specified points or ages, or as a series of complete templates from which change at given points can be deduced (the same templates that also can be used diagnostically—see Figures 6-53 to 6-55).
The more the individual whose growth one is attempting to predict is representative of the sample from which the average changes were derived, the more accurate the prediction should be, and vice versa. Ideally, separate growth standards would be established for the two sexes, the major racial groups, and important subgroups within each of the major categories (such as patients with long- or short-face growth patterns and skeletal Class II or Class III malocclusions). Templates from the Burlington growth study (Figure 7-23) show different tracks for short, normal, and long-face growth, but it can be very difficult to determine which to use to predict an individual patient. An Italian data set of serial cephalometric radiographs of untreated Class III children has been very helpful as a control for treated Class III patients, leading to the recommendations made above. No such data exist for untreated Class II individuals, and because it is no longer ethically acceptable to take repeated x-rays of children who will not be treated, it is unlikely that the necessary quantity of data ever will be available.
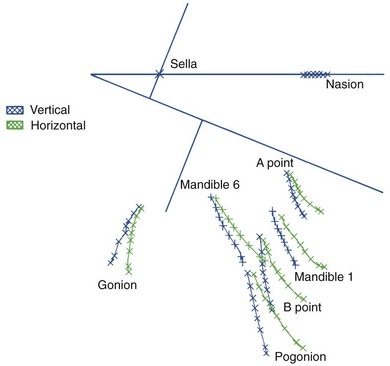
FIGURE 7-23 The varying growth direction of selected maxillary and mandibular landmarks is shown in this drawing derived from the templates of the Burlington (Ontario) growth study. The mean tracks for patients with a vertical versus a horizontal growth pattern show clearly that both the direction and magnitude of growth at various locations are quite different, and the track for individuals with the usual horizontal-vertical pattern is intermediate between these two. For accuracy in growth prediction, it would be important to place the patient in the correct group, which, unfortunately, can be quite difficult.
The major difficulty with growth prediction based on average changes is that any individual patient may have neither the average amount nor direction of growth, and thus there is the possibility of significant error. In clinical application, growth prediction is really needed for a child who has a skeletal malocclusion. His or her problem developed because of growth that deviated from the norm, and this deviant growth is likely to continue, which means that average increments and directions are unlikely to be correct. Our ability to predict facial growth, therefore, is poorest for the very patients in whom it would be most useful. At present and for the foreseeable future, accurate growth predictions simply are not possible for the children who need it most.
Predicting Treatment Outcomes: Computer Image Predictions
Placing cephalometric information into computer memory is conveniently accomplished now by digitizing points on the cephalometric tracing. Then projected changes in jaw and tooth positions can be made on the tracing as a prediction of the outcome of treatment. All current cephalometric programs allow superimposition of the profile image (preferably, a direct digital image) onto the tracing so that the doctor and patient can more readily visualize treatment effects (Figure 7-24).
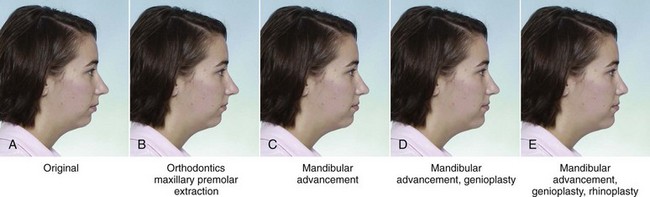
FIGURE 7-24 A to E, Presenting a computer-generated simulation of the posttreatment profile can greatly help patients understand the differences between alternative treatment approaches, in this case, the probable profile outcome of orthodontic camouflage of a skeletal Class II problem versus orthognathic surgery to correct the jaw relationship. Although showing patients these simulations heightens their esthetic awareness, it does not seem to create unrealistic expectations.
Does this mean that computerization will solve the problems of growth prediction? No, because the data on which the growth-prediction algorithms would have to be based simply do not exist. Remember, changes due to treatment in the absence of growth are predictable, and changes due to treatment during growth are not. Computer images for growing children are just as inaccurate as predictions from the old templates, and although they can be used to help parents understand the goal of treatment (see Figure 7-36), it is important for them to understand this is what is hoped for, not necessarily what is going to happen. There is no reason to believe that the same kind of prediction that can be done with adults will be possible for children any time soon. Predictions for adolescents are a middle ground—the less they will grow in the future, the more accurate the prediction, and vice versa.
Treatment Response as an Aid in Treatment Planning
A practical problem in treatment planning for children and adolescents, then, is how to reduce the uncertainty related to growth. For instance, what do you plan for a rather mature 12-year-old boy with a moderately severe skeletal Class II problem? Should you use the estimates underlying a computer prediction to make the decision, ignoring the possibility of serious error? Proceed with growth modification, regardless of the questionable prognosis? Go ahead with extractions for camouflage on the theory that this would ensure success whatever the patient’s growth? Each of these approaches has been advocated by respected orthodontic clinicians and would be the best approach to some patients—and a serious error for others.
One way to reduce the amount of uncertainty in planning treatment for children is to use the initial treatment response as an aid in treatment planning, deferring the adoption of a definitive treatment plan until some experience with the patient. This approach, sometimes called therapeutic diagnosis, allows a better evaluation of both growth response and cooperation with treatment than can be obtained by prediction alone. It is especially applicable to children with skeletal Class II and Class III problems, but also can be quite useful in Class I patients who are borderline extraction cases.
In practice, therapeutic diagnosis involves implementing a conservative (i.e., nonextraction or nonsurgical) treatment plan initially and reevaluating the patient after a few months to observe the response to this treatment. For example, an adolescent with a skeletal Class II malocclusion might be placed on a functional appliance or extraoral force to the maxilla, with minimal use of fixed appliances for tooth movement initially, to see if favorable growth reduces the jaw discrepancy. If a good response is observed after 6 to 9 months, this treatment approach is continued, with the odds of long-term success greatly improved. On the other hand, if a poor response is observed, whether because of poor cooperation or poor growth, the growth modification therapy might be dropped in favor of surgery to advance the mandible or extractions and a fixed appliance, camouflage-oriented approach.
The disadvantage of the evaluation period in the latter instance is that treatment may take longer than it would have if the surgery or extraction decision had been made initially. The advantage is a decrease in the number of incorrect decisions. Whatever the treatment plan, it is important at all stages of all types of treatment to carefully monitor the patient’s response and make appropriate adjustments in the original plan to deal with variations in response.
Planning Treatment for Maximal Esthetic Improvement
Careful clinical examination of the patient, so that important data related to facial and dental esthetics are incorporated into the database, is the key to planning treatment to obtain maximal improvement in appearance. In Chapter 6, a systematic approach to evaluation of facial proportions (macro-esthetics), the smile framework (mini-esthetics), and tooth-gingival characteristics (micro-esthetics) was described. The discussion here is of ways to deal with these esthetic issues.
Macro-Esthetic Considerations: Correcting Facial Disproportions
We already have emphasized the importance of correcting the appearance of facial disproportions. If you can make the facial disproportion disappear without actually changing the jaw proportions that underlie it (which, of course, is camouflage) or at least reduce it to the point that it is no longer a problem for the patient, you have solved the patient’s problem satisfactorily. In this sense, the success of treatment is in the eye of the beholder. Is facial appearance satisfactory enough with camouflage or is the greater change from surgery needed to overcome the patient’s perception of deformity? Only the patient can answer these questions.
In this context, computer image predictions of the outcome without and with surgery are an important tool to help the patient and parents understand (see Figure 7-24). Since surgery is contrasted to camouflage only after growth is essentially complete, the uncertainty of growth prediction is removed. Data from a randomized clinical trial show that surgery patients appreciate the improved communication that the computer predictions make possible, and compared to those who did not see their predictions prior to surgery, are more likely to be satisfied with the outcome of treatment.20 In this application, the predictions are accurate enough for clinical use. Letting the patients see their prediction images now is a routine part of surgical planning (see Chapter 19).
Esthetic Effects of Orthognathic Surgery
For everyone, advancing age is indicated by increased facial wrinkles, looser skin in the cheeks and throat because of loss of tissue in the deeper layers of the skin, and decreased fullness of the lips. Until recently, face lift surgery approached these problems primarily by pulling the skin tighter. The emphasis now is on “filling up the bag,” adding volume rather than decreasing it.
One of the advantages of mandibular advancement surgery, and to a lesser extent of maxillary advancement as well, is that it does add volume and makes adults look younger by doing so (Figure 7-25). Orthognathic procedures that decrease volume (mandibular setback and superior repositioning of the maxilla are the best examples) improve facial proportions but can make the patient look older because of the effects on the skin. For that reason, almost all surgical Class III treatment now includes maxillary advancement, which often is combined with mandibular setback in prognathic patients. The goal is to correct the jaw discrepancy without making the patient look prematurely older.

FIGURE 7-25 Surgical mandibular advancement tightens the skin around the mandible, decreasing wrinkles around and beneath the chin, which tends to make the patient look younger. A to C, age 48, prior to treatment that involved proclining the maxillary central incisors to produce overjet, then advancing the mandible. D to F, age 51, one year after completion of treatment.
Cosmetic Facial Surgery
For some patients, maximizing the improvement of esthetics requires facial plastic surgery in addition to orthodontics or orthognathic surgery (Figure 7-26). Genioplasty, the most frequently used adjunct to orthodontics, improves the stability of the lower incisors, as well as enhancing facial appearance, and so is not just a cosmetic procedure. Rhinoplasty is particularly effective when the nose is deviated to one side, has a prominent dorsal hump, or has a bulbous or distorted tip. Deficient facial areas, like the paranasal deficiency that often is seen in patients with maxillary deficiency, can be improved by placing grafts or alloplastic implants sub-periosteally.

FIGURE 7-26 It is quite possible to combine rhinoplasty with orthognathic surgery, and correcting a nasal deformity can be a significant adjunct to the improved appearance from contemporary maxillofacial surgery. A and B, Oblique and profile photos before treatment. Note that this man’s skeletal Class III problem was largely maxillary deficiency and that there was abnormal anatomy of the nasal bridge, a widened nasal base, and an enlarged and bulbous nasal tip. C and D, Oblique and profile photos after maxillary advancement and rhinoplasty. The improvement in the nose nicely complements the better projection of the maxilla.
The interactions of orthodontist and surgeon in orthognathic and facial plastic surgery are discussed in Chapter 19.
Mini-Esthetic Considerations: Improving the Smile Framework
The primary goal of mini-esthetic treatment is to enhance the smile by correcting the relationship of the teeth to the surrounding soft tissues on smile. In the development of the problem list, the examination focused on three aspects of the smile: the vertical relationship of the lips to the teeth, the transverse dimensions of the smile, and the smile arc.
Vertical Tooth–Lip Relationships
It is important to display most of the crowns of the maxillary anterior teeth on a social smile. The guideline is that at least 75% of the crown should be seen when the patient smiles, and exposure of all the crown and some gingiva is both esthetic and youthful-appearing and within the esthetic limits (see Figure 6-21 and Box 6-4). Obviously, the goal in treatment should be to position the teeth relative to the upper lip so that they are displayed on smile within these guidelines. In applying the guidelines, it should be kept in mind that tooth display is greater in females.
If the tooth display is inadequate, elongating the upper teeth improves the smile, makes the patient look younger, and is the obvious plan. There are several possible treatment approaches to accomplish this, which would be selected on the basis of other aspects of the patient’s problems. In orthodontic treatment alone, extrusive mechanics with archwires, judicious use of Class II elastics to take advantage of their tendency to rotate the occlusal plane down anteriorly, and anterior vertical elastics could be considered. Rotating the maxilla down in front as it is advanced surgically can improve smile esthetics, especially in patients with maxillary deficiency (Figure 7-27).
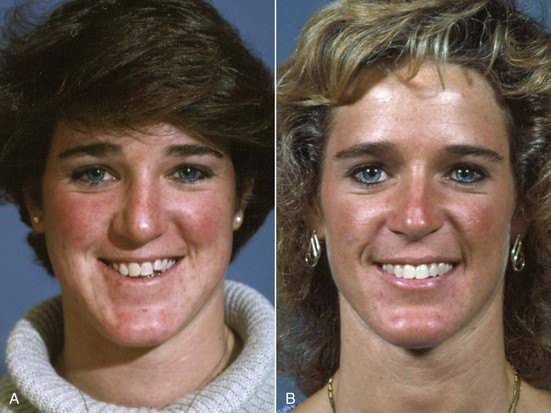
FIGURE 7-27 Inadequate exposure of the maxillary teeth impairs the appearance of the smile, and increasing incisor display for such a patient improves it. A, Prior to treatment, the patient’s chief complaint was her facial appearance. Although her problem would traditionally be described as a mild skeletal Class III due to maxillary deficiency, the frontal rather than profile appearance was (appropriately) her major concern. B, After treatment to bring the maxilla forward and rotate it down anteriorly, to increase incisor display.
Excessive display of maxillary gingiva on smile must be evaluated carefully because of the natural tendency for the upper lip to lengthen with increasing age. What looks like too much gingival exposure in early adolescence can look almost perfect a few years later (see Figure 4-26). There are now three possible treatment approaches to excessive gingival display due to incorrect dental and skeletal relationships: intrusion of the maxillary incisors using segmented arch mechanics, intrusion using temporary skeletal anchorage, and orthognathic surgery to move the maxilla up. With all these methods, it is possible to overdo intrusion of the anterior teeth, which, of course, makes the smile less attractive and the patient look older. In some patients, overgrowth of the gingiva may contribute to the initial excessive display, and if so, recontouring the gingiva to gain normal crown heights is an important part of correcting the problem. Laser surgery (see below) makes this much easier and more convenient than previously.
Transverse Dimensions of the Smile
“She has a broad, welcoming smile” often is used as a compliment. Exactly what does that mean? In patients whose arch forms are narrow or collapsed, the smile may also appear narrow, which is less appealing esthetically. In the diagnostic examination of the smile framework (see Chapter 6), the width of the buccal corridors was noted. Transverse expansion of the maxillary arch, which decreases buccal corridor width, improves the appearance of the smile if the buccal corridor width was excessive before treatment (Figure 7-28). Prosthodontists have learned that too wide a denture set-up, so that the buccal corridor is obliterated, is unesthetic. Too much expansion of the natural dentition can produce the same unnatural appearance of the teeth, so transverse expansion is not for everyone, but lay observers now usually judge a smile with minimal corridor width to be more esthetic.21
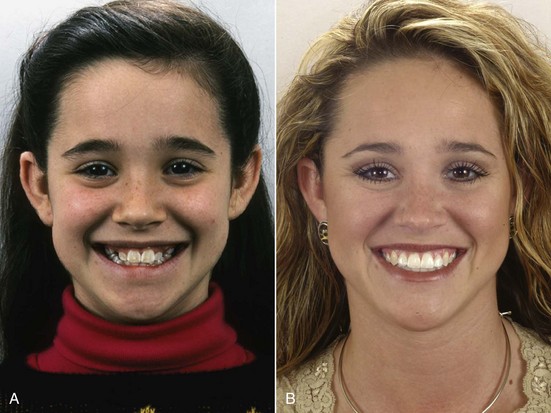
FIGURE 7-28 For patients with wide buccal corridors, transverse expansion of the maxilla can improve smile esthetics. A, Age 12, prior to treatment. B, Age 15, after orthodontic treatment with widening of the maxillary arch.
Should this be done only with dental expansion or by opening the midpalatal suture? That depends on the amount of expansion that is needed to meet the other goals of proper occlusion and long-term stability. An important consideration in widening a narrow arch form, particularly in an adult, is the axial inclination of the buccal segments. Patients in whom the posterior teeth are already flared laterally are not good candidates for dental expansion.
The Smile Arc
Obtaining and maintaining a proper smile arc requires taking this into account when brackets are placed on the teeth. The traditional guideline for placing brackets has been based on measurements from the incisal edge so that the central incisor bracket is placed about the middle of the clinical crown, the lateral incisor bracket about 0.5 mm closer to the incisal edge than the central, and the canine about 0.5 mm more apically. The effect is to position the teeth very nicely to each other, as they would be in a denture set-up, without taking into consideration the vertical tooth–lip relationship that the prosthodontist would emphasize. The result may not be compatible at all with the best appearance of the teeth on smile because the smile arc was not considered. Recent research suggests that the smile arc is more important than buccal corridor space in determining the attractiveness of the smile.22
What would you do differently in placing brackets to obtain the best smile arc? The usual problem is that the smile arc is too flat (see Figure 6-24). If that is the case, putting the maxillary central incisor brackets more gingivally would increase the arc of the dentition, bring them closer to the lower lip, and make the smile arc more consonant (Figure 7-29). If the smile arc were distorted in some other way, placing the brackets to compensate for this by altering tooth positions would be the solution. Of course, if the small arc had been flattened during treatment, step bends in the archwire would be the other way to correct it. This type of compensation may be needed in orthognathic surgery patients, as well as in patients who are to receive orthodontic treatment only.

FIGURE 7-29 The smile arc is the most important single thing in smile esthetics. A and B, Full face and close-up views of the smile prior to treatment. Note the flat smile arc and inadequate display of maxillary incisors. C and D, One year later, after orthodontic (not orthognathic surgery) treatment. The improvement in facial appearance is largely due to better lip support by the upper teeth that decreased the paranasal folds and attainment of a correct smile arc.
Smile Symmetry
An asymmetric smile sometimes is a patient’s major concern. It is possible that this is due to more eruption of the teeth or different crown heights on one side, and if so, repositioning the teeth or changing the gingival contours should be included in the treatment plan. Often, however, greater elevation of the lip on one side on smile, which is an innate characteristic that cannot be changed, gives the appearance of a cant to the maxillary dentition when it really is symmetric. For a patient who complains about smile asymmetry, this becomes an important informed consent issue—the patient must understand that the asymmetric lip movements will not be changed by treatment.
Micro-Esthetic Considerations: Enhancing the Appearance of the Teeth
Treatment plans for problems relating directly to the appearance of the teeth fall into three major categories: (1) reshaping teeth to change tooth proportions and/or correct “black triangles” between the teeth; (2) orthodontic preparation for restorations to replace lost tooth structure and correct problems of tooth shade and color; and (3) reshaping of the gingiva.
Reshaping Teeth
Often, it is desirable to do minor reshaping of the incisal edges of anterior teeth to remove mamelons or smooth out irregular edges from minor trauma. When minor reshaping is planned, it must be taken into account when brackets are placed, and it may be easier to do this before beginning fixed appliance treatment.
Changing Tooth Proportions: Extensive changes in tooth proportions are needed primarily when one tooth is to substitute for another, and the most frequent substitution is substituting maxillary canines for congenitally missing maxillary lateral incisors. When a lateral incisor is missing, the treatment alternatives always are closing the space and substituting the canine, or prosthetic replacement of the missing tooth with a single-tooth implant or fixed bridge. Closing the space and reshaping the canine to look like a lateral incisor can provide an excellent esthetic result, perhaps superior to an implant in the long run.
The technique for reshaping a canine is illustrated in Figure 7-30. It requires significant removal of facial, occlusal, interproximal, and lingual enamel. In some patients, composite buildups of ceramic laminates are needed to obtain good tooth color.

FIGURE 7-30 To reshape a maxillary canine that is to substitute for a missing maxillary lateral incisor (A and B), the steps in treatment consist of interproximal reduction (C), flattening the tip (D), flattening the facial surface (E), reducing cingulum thickness (F), and rounding the corners of the flattened crown (G). At that point, a lateral bracket can be placed on the canine during orthodontic treatment. If the gingival margin of the canine is visible, it can be brought down by elongating the tooth and increasing the amount of gingival reduction. Recontouring of the gingiva over the first premolar that becomes a substitution for the canine also enhances appearance. In H, note that the gingival margin of the first premolar has been reshaped (with a diode laser) to make it look more like a canine. I, Smile at completion of treatment.
Canine substitution works best, however, when the dental arch was crowded anyway and may not be compatible with excellent occlusion and smile esthetics if closing the lateral incisor space would result in significant retraction of the central incisors. In that circumstance, encouraging the permanent canine to erupt into the lateral incisor position so that alveolar bone is formed in the area of the missing tooth, and then moving the canine distally to open space is the best way to prepare for an eventual implant.23 The implant should not be placed until vertical growth is essentially complete, in the late teens or early twenties (see Chapter 18 for a further discussion of this important point).
Correcting Black Triangles: Decreasing or eliminating spaces between teeth above the contact points, which are unsightly if they are not filled with an interdental papilla, can be accomplished most readily by removing enamel at the contact point so the teeth can be moved closer together (see Figure 6-29). Moving the contact area apically eliminates much if not all the space. When this is done, however, care is required not to distort the proportional relationships of the teeth to each other, and if possible the progression of connector heights (see below) should be maintained. Clinically, this means that if the central incisors are narrowed, it may be necessary also to slightly narrow the lateral incisors and move their contact area more apically to maintain a good dental appearance.
Interaction Between Orthodontist and Restorative Dentist
When the teeth are small or if tooth color or appearance is to be improved by restorative dentistry, during orthodontic treatment it is necessary to position them so that the restorations will bring them to normal size and position. In modern practice, the restorations are either composite buildups or ceramic laminates, laminates being used particularly when it is desirable to change tooth color and shade in addition to the size of the crown (Figure 7-31).

FIGURE 7-31 Laminate veneers can be used to correct both the color and contour of teeth in canine substitution treatment. A and B, Appearance of teeth on full-face smile and close-up. Note the buildups on canines used to fill in the space of congenitally missing maxillary lateral incisors. C and D, Appearance after space closure and laminate veneers for the maxillary anterior teeth. Among the things that can be corrected with laminate veneers is the length of the teeth so that there is proper display on smile.
There are two ways to manage the orthodontic-restorative interaction. The first is to carefully plan where the teeth are to be placed, place a vacuum-formed retainer immediately after the orthodontic appliance is removed that the patient wears full time, and send the patient to the restorative dentist for completion of the treatment. A new retainer is needed as soon as the restorations have been completed. This has two advantages: the restorative work can be scheduled at everyone’s convenience after the orthodontic treatment is completed, and any gingival swelling related to the orthodontic treatment has time to resolve. It also has disadvantages: excellent patient cooperation is required to maintain the precise spacing needed for the best restorations, so the restorative work may be compromised by tooth movement, and the teeth are unesthetic until this is accomplished.
An alternative, which is most applicable when composite buildups rather than laminates are planned, is for the orthodontist to deliberately provide slightly more space than the restorative dentist requires to bring the teeth to just the right size, remove the brackets from the teeth to be restored, send the patient immediately to the restorative dentist, replace the brackets the same day after the restorations are completed, and close any residual space before removing the orthodontic appliance (Figure 7-32). This has the advantage of eliminating compromises in the restorative work, but the disadvantage that careful coordination of the appointments is required.
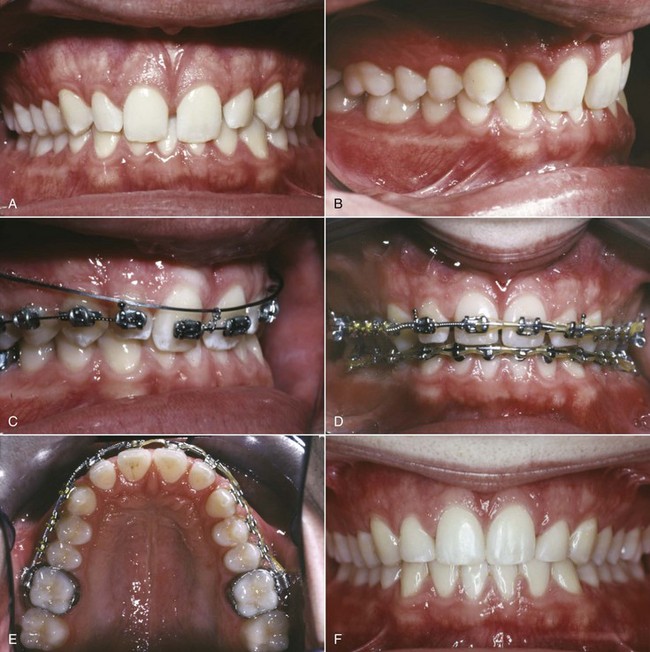
FIGURE 7-32 A and B, This patient’s complaint was the appearance of his upper incisors. The central incisors were elongated and quite upright; the lateral incisors were small, and the excess space was seen as a maxillary midline diastema. C, Intrusion archwire to central incisors. D and E, After intrusion and spacing of the incisors to allow buildups of the lateral incisors. F, Completion of orthodontic and restorative treatment.
Reshaping Gingival Contours: Applications of a Soft Tissue Laser
Appropriate display of the teeth requires removal of excessive gingiva covering the clinical crown, and is enhanced by correcting the gingival contours. Treatment of this type now can be carried out effectively with the use of a diode laser (see Figure 7-40). A laser of this type, in comparison to the carbon dioxide (CO2) or erbium-doped yttrium aluminium garnet (Er-YAG) lasers also used now in dentistry, has two primary advantages: (1) it does not cut hard tissue, so there is no risk of damage to the teeth or alveolar bone if it is used for gingival contouring, and (2) it creates a “biologic dressing” because it coagulates, sterilizes, and seals the soft tissue as it is used. There is no bleeding, no other dressing is required, and there is no waiting period for healing.
Use of a soft tissue laser as part of finishing procedures is discussed further in Chapter 16.
Planning Comprehensive Orthodontic Treatment
Steps in Planning Comprehensive Treatment
The focus of the rest of this chapter is on comprehensive treatment, in adolescence or later, when the permanent teeth are present at least for the latter part of the treatment period. Planning for mixed dentition treatment to prevent later problems or prevent them from getting worse is covered in Chapter 11, and planning more complex dental and skeletal treatment for a child who is likely to need later comprehensive treatment is discussed in Chapters 12 and 13.
At any stage of treatment, orthodontic diagnosis results in a comprehensive list of the patient’s problems. Although any number of pathologic problems might be noted, if the five characteristics of malocclusion are used to structure the problem list, there can be a maximum of five major developmental problems. Most patients will not have that many. As the problem list is developed, the findings related to malocclusion can and should be grouped as the classification scheme suggests to make the treatment planning process work efficiently. Having too many overlapping problems on the problem list only creates confusion.
The goal of treatment is to deal with the problems in a way that creates maximum benefit to the patient—not just to straighten the teeth. Using a logical sequence of steps on the way from the problem list to the final plan, keeping this goal in mind, is strongly recommended. The sequence of steps is illustrated in Figure 7-1. Let us now consider this sequence and the logic behind it as we develop the treatment plan for the patient whose diagnostic workup was illustrated in Chapter 6 (see Figures 6-75 to 6-78). Her problem list (diagnosis) is repeated in Box 7-1.
Pathologic versus Developmental Problems
An important principle is that a patient does not have to be in perfect health to have orthodontic treatment, but any problems related to disease and pathology must be under control (i.e., the progression of any acute or chronic conditions must be stopped). For this reason, pathologic problems must be addressed before treatment of orthodontic (developmental) problems can begin. Thus in a treatment sequence, orthodontic treatment must appear after control of systemic disease, periodontal disease, and caries.
The first step in treatment planning is to separate pathologic from developmental (orthodontic) problems (Figure 7-33). Even when pathologic problems are mild, as one would expect them to be in the healthy adolescents who are the majority of orthodontic patients, they must not be overlooked in the treatment plan. For a typical patient of that type, the plan for the pathologic problems would include oral hygiene instruction and monitoring gingival health during orthodontic treatment. Other items might be included for specific problems, as in our example patient (Box 7-2). For patients with more complex disease-related problems, the plan often is appropriate referral to another medical or dental clinician before orthodontic treatment begins.
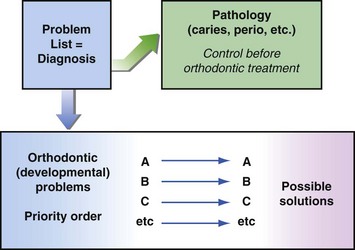
FIGURE 7-33 The last step in diagnostic evaluation of potential orthodontic patients is to separate pathologic from developmental problems; the first step in treatment planning is to consider the management of the pathologic problems. They must be brought under control before orthodontic treatment begins, not because they are necessarily more important, but because orthodontic treatment in the presence of active disease can accentuate the pathology. After that, the first and most important step toward an orthodontic treatment plan is to put the orthodontic (developmental) problems in priority order, so that possible solutions to each problem can be considered from the perspective of what is most important for this patient.
Periodontal health is an important issue, especially for older patients, and interaction with a periodontist often is needed to plan and carry out appropriate orthodontic treatment. Two important points must be kept in mind: (1) orthodontic treatment in the presence of active periodontal disease is likely to accelerate the disease process, so periodontal control is essential before orthodontics begins; but (2) in the absence of active disease, even if significant bone loss has occurred previously, careful orthodontic treatment will not lead to further bone loss and can facilitate other types of dental treatment such as restorative dentistry, prosthodontics, and periodontal surgery.
Setting Priorities for the Orthodontic Problem List
Putting the patient’s orthodontic (developmental) problems in priority order (Figure 7-34) is the most important single step in the entire treatment planning process. In order to maximize benefit to the patient, the most important problems must be identified, and the treatment plan must focus on what is most important for that particular patient. The patient’s perception of his or her condition is important in setting these priorities.
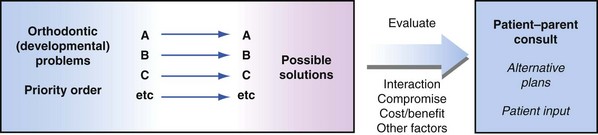
FIGURE 7-34 The possible solutions to the patient’s prioritized problems must be evaluated from several important perspectives: interaction among the solutions, compromise in the sense of modifying treatment goals to best fit this patient, cost/benefit considerations, and other pertinent factors.
It is always difficult for the clinician to avoid imposing his or her own feelings at this stage, and it is not totally inappropriate to do so; but ignoring the patient’s chief complaint can lead to serious errors in planning treatment. For instance, consider the patient who complains of a protruding chin and who has a Class III malocclusion. If the clinician formulates the problem as Class III malocclusion and concentrates on bringing the teeth into correct occlusion while ignoring the chin, it is not likely that the patient will be happy with the treatment result. The plan did not deal with the patient’s problem.
The doctor does not have to agree with the patient’s initial thoughts as to what is most important. Indeed, often it is necessary to educate the patient about the nature of the problems. But the importance of various problems must be discussed, and informed consent to treatment has not been obtained unless the patient agrees that the focus of the plan is what he or she wants. The prioritization for our example patient is shown in Box 7-3.
Factors in Evaluating Treatment Possibilities
The next step in the planning process is to list the possibilities for treatment of each of the problems, beginning with the highest priority problem. At this stage, each problem is considered individually, and for the moment the possible solutions are examined as if this problem were the only one the patient had. Broad possibilities, not details of treatment procedures, are what is sought at this stage (Box 7-4). The more complex the total situation, the more important it is to be sure no possibilities are overlooked.
As we continue to develop the treatment plan for our illustrative patient, references to aspects of treatment that have not yet been presented in the text are inevitable. The first-time reader is urged to follow the logic rather than concentrate on details that will be discussed more fully in the following chapters.
First, let’s consider the possible solutions to this patient’s most important problem: the unattractive smile and appearance of the maxillary incisors. Correcting this will require alignment of the teeth, but proper anterior tooth relationships cannot be achieved until overjet is reduced and the deep bite is corrected. Therefore the best solution to the first problem can be determined only after the impact of possible solutions to overjet and overbite have been considered.
As we have noted, there are three ways that the Class II jaw relationship and overjet can be treated (Figure 7-35): (1) differential forward growth of the mandible, which is ideal if it can be achieved; (2) orthodontic camouflage, retracting the maxillary incisors and proclining the mandibular incisors to make the teeth fit even though the jaws do not; or (3) orthognathic surgery to correct the jaw position. Since our patient has not yet reached the adolescent growth spurt, growth modification would be the primary possibility, with camouflage and surgery as possibilities if growth modification did not succeed.
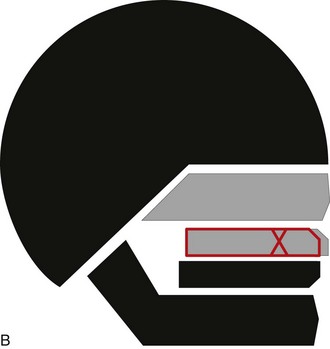
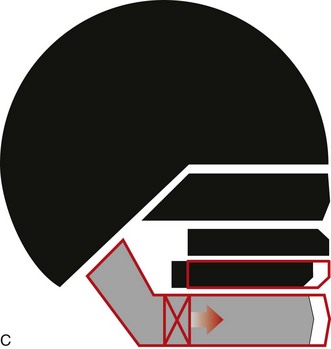
FIGURE 7-35 The possibilities for correction of a skeletal Class II problem include the following: A, Differential forward growth of the mandible, which is the ideal method if the patient has not yet gone through the adolescent growth spurt; B, camouflage by retraction of the maxillary incisors, which can be quite successful if the other facial features allow it; and C, orthognathic surgery to move the mandible forward to a normal relationship. In the absence of growth, camouflage and surgery are the only possibilities.
Class II growth modification can be done in several ways, which are discussed in detail in Chapter 13. For this patient, differential forward growth of the mandible while maintaining vertical control of the maxillary posterior teeth and bringing the maxillary incisors downward and facially would increase the display of the maxillary incisors and the prominence of the chin (Figure 7-36). The two most effective ways to do that would be high-pull headgear or a fixed functional appliance like the Herbst appliance. The functional appliance would be more likely to move the lower incisors forward, which is undesirable for this patient, so headgear would be preferred if she would agree to wear it.
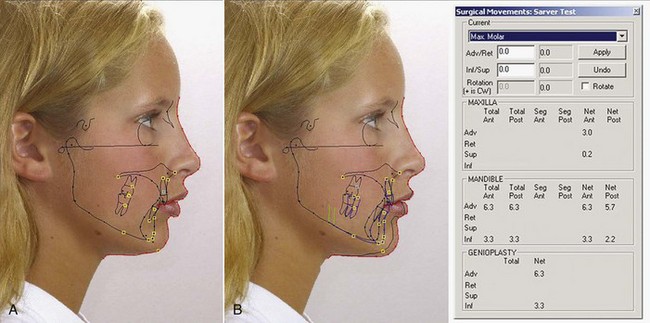
FIGURE 7-36 Computer predictions of growing patients often are inaccurate because of the difficulty of predicting growth but nevertheless can be used to help the patient and parents understand what is expected to occur. A, Patient F.P., cephalometric tracing merged with facial profile image, using the Orthotrac imaging system. B, Prediction of treatment with forward growth of the mandible while the maxilla is held in place and the upper incisors tipped facially and elongated. An adolescent is more likely to cooperate with treatment if he or she understands exactly what is desired and what the benefit would be, and images of changes in your own face are easier to understand than word descriptions, pictures of a different patient, or other generalized educational materials.
There also are three ways to correct the anterior overbite (Figure 7-37): (1) absolute intrusion of the upper and lower incisors, moving their root apices closer to the nose and lower border of the mandible respectively; (2) relative intrusion of the incisors, keeping them where they are while the mandible grows and the posterior teeth erupt; and (3) extrusion of the posterior teeth, which would rotate the mandible downward and backward. Relative intrusion of incisors and extrusion of posterior teeth are identical in terms of the tooth movement. The difference is whether vertical growth of the ramus compensates for the increase in molar height (i.e., whether the mandibular plane angle is maintained [relative intrusion] or increases as the mandible rotates downward and backward [extrusion]).
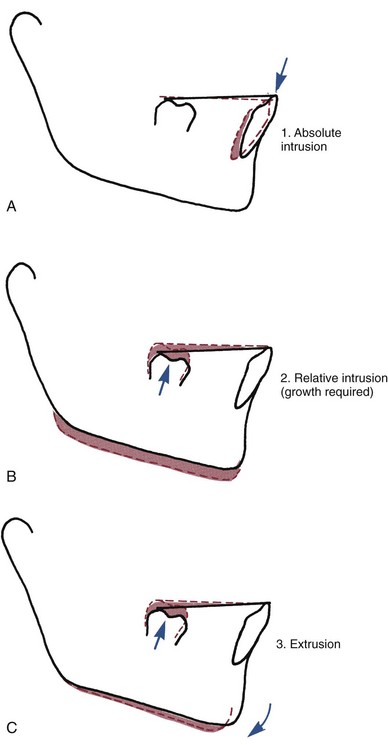
FIGURE 7-37 There are three possible ways to level out a lower arch with an excessive curve of Spee: (1) absolute intrusion; (2) relative intrusion, achieved by preventing eruption of the incisors while growth provides vertical space into which the posterior teeth erupt; and (3) elongation of posterior teeth, which causes the mandible to rotate downward in the absence of growth. Note that the difference between (2) and (3) is whether the mandible rotates downward and backward, which is determined by whether the mandibular ramus grows longer while the tooth movement is occurring.
In an immature 12-year-old like our patient, vertical growth can be expected, so relative intrusion would be the preferred approach. It is significant that in the absence of growth, leveling the arches by extrusion of posterior teeth would cause the mandible to rotate downward and backward, accentuating a Class II tendency (Figure 7-38), which would be highly undesirable for this patient. Controlling the vertical position of the maxillary posterior teeth so that the vertical space between the jaws created by growth could be used largely for elongation of the lower molars would facilitate leveling by relative intrusion. Thus the high-pull headgear that appears to be the best approach to the skeletal Class II problem also would facilitate correction of the deep bite, if used along with a fixed appliance to level the lower arch.
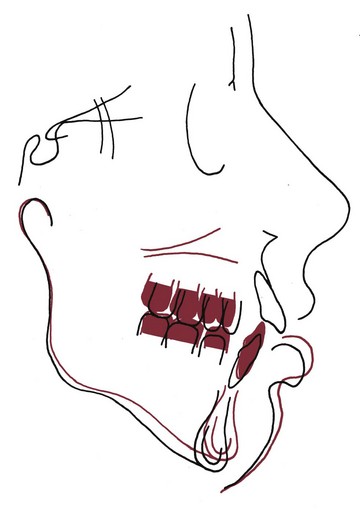
FIGURE 7-38 There is a strong interaction between the vertical position of the maxilla and both the anteroposterior and vertical positions of the mandible, because the mandible rotates backward as it moves downward and forward as it moves upward. This superimposition (red = initial, black = progress) shows excessive vertical growth of the maxilla and excessive eruption of the maxillary posterior teeth. This was not matched by vertical growth of the ramus, leading to downward-backward rotation of the mandible in the classic long-face pattern that made the Class II jaw relationship worse. Superior repositioning of the maxilla and/or intrusion of maxillary posterior teeth (see Chapters 18 and 19) would be the key to both reducing face height and correcting the Class II relationship.
Often, the same problem list prioritized differently results in a different treatment plan. For this patient, if the Class II malocclusion was considered the most important problem and the relationship of the upper incisors to the lip and gingiva was not considered important, Class II camouflage might be chosen as the most efficient approach to treatment. Class II elastics, with or without premolar extraction, would correct the malocclusion but might harm rather than enhance the dental and facial appearance.
The objective at this stage of treatment planning is to be sure that no reasonable possibilities are overlooked. It is easy to develop the mindset that “For this problem, we always …” Sometimes an alternate approach would be better but is overlooked unless a conscious effort is made to keep an open mind. In this patient’s case, if obtaining proper soft tissue relationships to the upper incisors is not a priority in treatment, an optimal result is unlikely.
Four additional factors that are pertinent in evaluating treatment possibilities now must be considered (Figure 7-39).
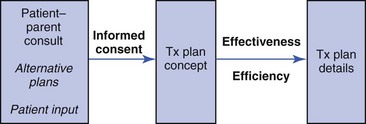
FIGURE 7-39 At the conference with the patient (and parents if the patient is a minor) at which alternative possible plans were discussed and patient input was sought, the outcome should be informed consent to a treatment plan concept. The doctor’s role at that point is to determine the treatment plan details, considering effectiveness and efficiency of the various methods to achieve the desired outcome.
Interaction Among Possible Solutions
The interaction among possible solutions to a patient’s various problems is much easier to see when the possibilities are listed as previously described. As in the case of the girl in the previous section, it will be clear for nearly every patient that some possible solutions to a high-priority problem would also solve other problems, while others would not and might even make other things worse.
Consider the opposite situation to our example patient, a patient with an anterior open bite. Often, this problem is due not to decreased eruption of incisors but to excessive eruption of posterior teeth and downward-backward rotation of the mandible (see Figure 6-12, A). If so, using vertical elastics to elongate the anterior teeth is not a solution. Treatment should be aimed at depressing the elongated posterior teeth, or preventing them from erupting further while everything else grows (relative intrusion). This would allow the mandible to rotate upward, bringing the incisor teeth together. But if the mandible rotates upward, it also will come forward—which would be good if the patient had a skeletal Class II malocclusion to begin with but bad if the malocclusion was Class I or Class III.
Another important interaction, which also came into play in our illustrative case (Box 7-5), is the relationship between incisor prominence and facial appearance, especially on smile. If the teeth are crowded, is expansion of the arches indicated to gain the space needed to align them? The answer depends on the relationship of the teeth to their soft tissue environment. In developing the treatment plan, it is necessary to plan the final position of the incisors and then determine what is needed in order to put them in the desired position. Quantifying the extent of the crowding does not tell you what to do about it. You have to look at the effect of the possible treatments on the patient’s appearance.
Compromise
In patients with many problems, it may not be possible to solve them all. This type of compromise has nothing to do with the clinician’s skill. In some cases, no plan of treatment will solve all of the patient’s problems. Then, careful setting of priorities from the problem list is particularly important.
In a broad sense, the major goals of orthodontic treatment are ideal occlusion, ideal facial esthetics, and ideal stability of result. Often, it is impossible to maximize all three. In fact, attempts to achieve an absolutely ideal dental occlusion, especially if this is taken to prohibit extractions, can diminish both facial esthetics and stability after treatment. In the same way, efforts to achieve the most stable result after orthodontic treatment may result in less than optimal occlusion and facial esthetics, and positioning the teeth to produce ideal facial esthetics may detract from occlusion and stability.
One way to avoid having to face compromises of this type, of course, is to emphasize one of the goals at the expense of the others. In the early twentieth century, Edward Angle, the father of modern orthodontics, solved this problem by focusing solely on the occlusion and declaring that facial esthetics and stability would take care of themselves. Unfortunately, they did not. Echoes of Angle’s position are encountered occasionally even now, particularly among dentists strongly committed to avoiding extraction at all costs.
As important as dental occlusion is, it is not the most important consideration for all patients. Sometimes, ideal occlusion must be altered by extraction or otherwise to gain acceptable esthetics and stability. Adjustments in the other goals also may be needed. It is quite possible that placing the teeth for optimal facial esthetics may require permanent retention because they are not stable in that position, or alternatively, that placing the teeth in a position of maximum stability is likely to make the facial appearance worse not better.
If various elements of a treatment plan are incompatible, benefit to the patient is greatest if any necessary compromises are made so that the patient’s most important problems are solved, while less important problems are deferred or left untreated. If all of the three major goals of orthodontic treatment cannot be reached, those of greatest importance to that patient should be favored. Doing this successfully requires both judgment and thought on the part of the clinician and input from the patient and parent. For our example patient, would better stability of the result if the incisors were retracted to correct the excess overjet be worth the negative impact on her facial appearance? Given her chief complaint, almost certainly not.
Analysis of Benefit versus Cost and Risk
Practical considerations related to the difficulty of various treatment procedures compared with the benefit to be gained from them also must be considered in evaluating treatment possibilities. The difficulty should be considered in both risk and cost to the patient, not only in money but also in cooperation, discomfort, aggravation, time, and other factors that can be collectively labeled as the “burden of treatment” (see Figure 7-34). These must be contrasted to the probable benefit from that procedure.
For instance, for a patient with anterior open bite, jaw surgery to decrease face height has greater cost and risk than elastics to elongate the incisors or occlusal reduction of the posterior teeth, which are two other possibilities for correcting the bite relationship. But if the simpler and less risky procedures would provide little real benefit to the patient, while jaw surgery would provide considerable benefit, the cost-risk/benefit analysis might still favor the more difficult procedure. “Is it worth it?” is a question that must be answered not only from the point of view of what is involved but also in terms of the benefit to the patient.
Other Considerations
At this stage, it is important to take into account any pertinent special considerations about the individual patient. Should the treatment time be minimized because of possible exacerbation of periodontal disease? Should treatment options be left open as long as possible because of uncertainty of the pattern of growth? Should visible orthodontic appliances be avoided because of the patient’s vanity, even if it makes treatment more difficult? Such questions must be addressed from the perspective of the individual patient. Rational answers can be obtained only when the treatment possibilities and other important factors influencing the treatment plan have been considered.
For our example patient, interactions, thoughts about necessary compromises, and other considerations (which in her case are quite minor) are shown in Box 7-5. The information now has been assembled. Only at this point are treatment possibilities ready to be discussed with the patient and parents in order to finalize the treatment plan (Box 7-6).
Patient–Parent Consultation: Obtaining Informed Consent
Not so long ago, it was taken for granted that the doctor should analyze the patient’s situation and should prescribe what he or she had determined to be the best treatment—with little or no regard for whether that treatment was what the patient desired. This is best described as a paternalistic approach to patient care: the doctor, as a father figure, knows best and makes the decisions.
At present, this approach is not defensible, ethically or legally.24,25 From an ethical perspective, patients have the right to determine what is done to them in treatment, and increasingly they demand that right. It is unethical not to inform patients of the alternatives, including the likely outcome of no treatment, that are possible in their case. The modern doctrine of informed consent has made the ethical imperative a legal one as well. Legally, the doctor now is liable for problems arising from failure to fully inform the patient about the treatment that is to be performed. Informed consent is not obtained just from a discussion of the risks of treatment. Patients must be told what their problems are, what the treatment alternatives are, and what the possible outcomes of treatment or no treatment are likely to be in a way they can understand. Simply providing a brochure, video, or written consent form that uses complex language often does not lead the patient to really comprehend the treatment and its consequences. Unfortunately, consent forms endorsed by orthodontic societies often have this problem.
This really is a matter of health literacy, being able to read, understand, and act on health information in written form. Those who did not speak English before entering school, those who had less education, and those who get their health information primarily from radio and television are most likely to not understand informed consent discussions.26 For them, understanding the risks and limitations of treatment quite possibly is better with a formal audiovisual presentation than even an extensive discussion.27 Recent studies have demonstrated that patient recall of information presented to them is enhanced by putting the information in a layman’s terminology and by using visual presentation (images on a computer screen) instead of just words.28
The problem-oriented method of diagnosis and treatment planning lends itself very well to the patient involvement that modern treatment planning requires. A discussion with the patient and parents should begin with an outline of the patient’s problems, and patient involvement begins with the prioritization of the problem list. Perhaps the doctor’s single most important question in obtaining informed consent is, “Your most important problem, as I see it, is …. Do you agree?” When problems related to informed consent for orthodontic treatment arise, almost always they result from treatment that failed to address what was most important to the patient, or from treatment that focused on what was not an important problem to the patient.
The problem-oriented method requires examining the possible solutions to the patient’s problems, starting with the most important one. This is exactly the way in which a discussion with the patient and parents is structured most effectively (see Box 7-6). Interactions, unavoidable compromises, and practical considerations must not only be considered by the doctor, they must be shared with the patient as the treatment plan is developed. Under most circumstances, there are advantages and disadvantages to the possible treatment approaches. The doctor’s role is to clarify this to the best of his or her ability, involving the patient in the final decision as to the treatment approach that will be employed.
From a practical perspective, involving the patient and parents in decisions about treatment has important advantages. It places the responsibility where it belongs: on a patient who has been led to understand the uncertainties involved. The problems, after all, belong to the patient, not the doctor. For both adults and children, a patient who “owns” the problems and recognizes that this is the case is more likely to be cooperative and oriented toward helping with treatment than one who takes the attitude that it is all up to the doctor.29
Specific Points for Discussion
Several specific situations in orthodontics particularly require interaction between the doctor and the patient and parent in choosing the final treatment plan. Perhaps the most frequent situation revolves around the issue of arch expansion versus extraction in solving crowding problems. A second frequent problem requiring input from the patient is whether to begin treatment for a skeletal problem prior to adolescence or wait until the adolescent growth spurt. In this situation, two aspects must be discussed: the efficacy of beginning treatment early versus waiting for adolescence, and if early treatment is chosen, the mode of treatment.
The patient’s desire for treatment and potential cooperation also must be taken into account when treatment timing is considered. There is little reason to proceed with headgear or functional appliance treatment for a child who has no intention of wearing the device. Treatment results with the two methods are not precisely the same but can be considered more similar than different, and if the patient would wear one but not the other, it would be wise to select the one he or she would prefer. For our example patient, her level of sexual maturation indicates that she is approaching the ideal time for treatment, and headgear is the preferred approach, but the patient and parent need to understand why these are the recommendations and what alternatives exist.
When a severe skeletal problem exists, a third frequent issue for discussion with the patient and parents is whether orthodontic treatment alone would produce an acceptable result, or whether orthognathic surgery should be selected. Sometimes this difficult decision revolves around jaw function. In most instances, however, it is primarily an esthetic decision. The facial appearance is likely to be better if the jaw relationship is corrected. Is that improvement worth the additional risk, cost, and morbidity of surgery? In the final analysis, only the patient and parents can—or should—make that decision. In decisions like surgery versus orthodontic camouflage and whether to expand the dental arches or extract, a picture is worth a thousand words (see Figure 7-36).
Patient Interaction in Treatment Planning Decisions
Sometimes, involving patients in treatment planning discussions is interpreted as allowing the patient and parent to make all the decisions. Clearly, this is not the case. It is the doctor’s responsibility to explain the options to the patient and parents and to negotiate with them the final treatment plan. It is not the doctor’s responsibility to do anything the patient wants. Just as any patient has the right to refuse to accept treatment, the doctor has the right to refuse to carry out treatment that he or she considers not in the patient’s best interest. At one time, the doctor decided what was to be done and that was that. Now, establishing the concept of the final treatment plan is and must be an interactive process between the doctor and the patient.
In our example case, the patient and her parents understood the importance of correcting the Class II malocclusion and deep bite if a better facial appearance was to be achieved, accepted the suggestion that headgear during the adolescent growth spurt would be the best approach, and acknowledged that a change in the treatment plan to include extraction or even orthognathic surgery might be needed if the patient did not respond well to the more conservative initial treatment plan. They also reviewed the anticipated risks of treatment in her case, the primary concerns being root resorption (especially of the maxillary incisors) and the possibility of damage to the teeth from inadequate hygiene. The result was both informed consent in the broad (and correct) sense and approval of the treatment plan concept (Box 7-7).
The Detailed Plan: Specifying the Treatment Procedures
Note that for this patient, the conceptual plan leads directly to the therapy plan, which usually is the case. For any patient, the selected treatment procedures must meet two criteria: effectiveness in producing the desired result and efficiency in doing so without wasting either doctor or patient time. Progress and completion of this case are shown in Figures 7-40 to 7-44.
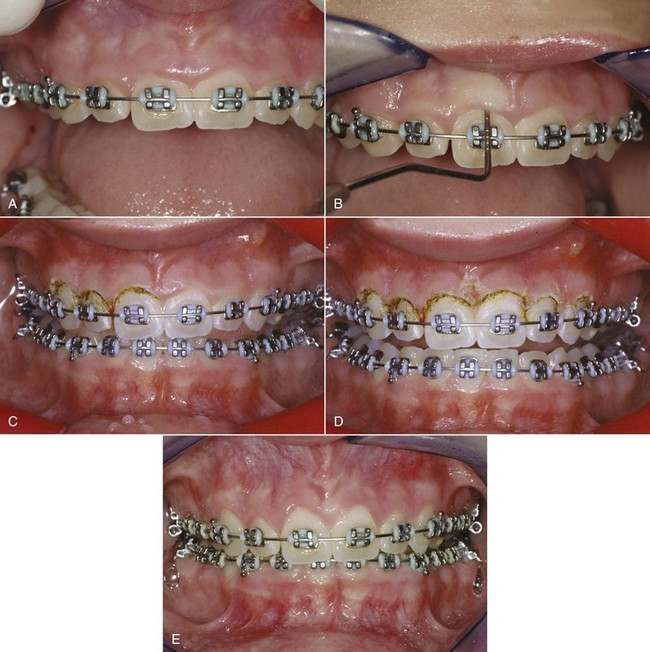
FIGURE 7-40 For patient F.P., whose diagnostic workup is illustrated in Figures 6-75 to 6-78 (see Figure 7-36 for computer image predictions), treatment was deferred until she was entering her adolescent growth spurt. A fixed appliance was placed at age 12-5, and high-pull headgear was started at age 12-10. Dentally and skeletally, she responded well to treatment, but the gingival overgrowth of the maxillary incisors worsened rather than improved (A). A diode laser now offers a painless and efficient way to manage problems of this type, and she was scheduled for gingival recontouring at age 13-11. A periodontal probe was used to establish the depth of the gingival sulcus (B), and the laser was used to recontour the tissue (C, one side done; D, gingival recontouring completed). Because the tissue is ablated (vaporized) and the heat of the laser seals the ablation site, no bleeding occurs and no periodontal dressing is needed. Healing occurs within a few days. E, The greatly improved tissue contours 4 weeks later.
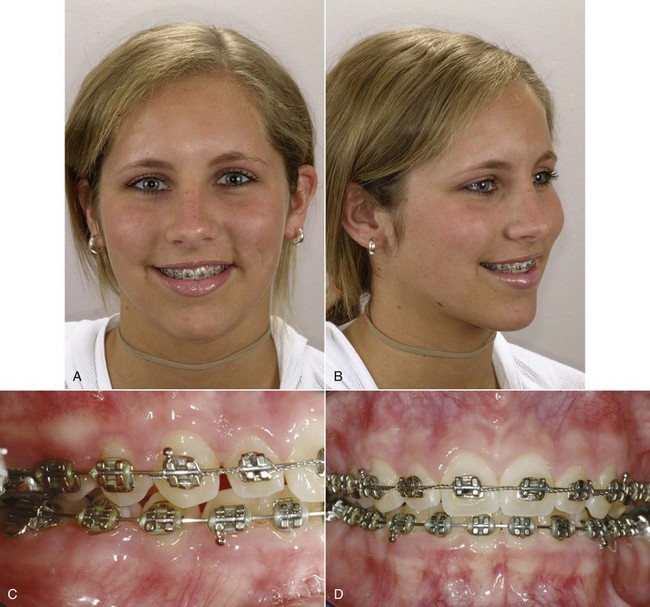
FIGURE 7-41 For patient F.P., fixed appliance treatment and high-pull headgear were continued following the gingival surgery, with an effort to elongate the maxillary incisors for better display on smile while maintaining the overbite correction. A and B, Progress records at age 14-5 showed good incisor display; and, C and D, a nearly corrected malocclusion.

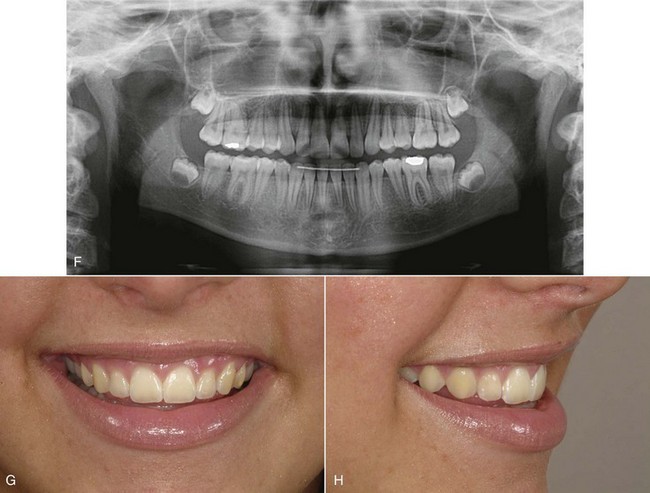
FIGURE 7-42 Patient F.P.: the orthodontic appliance was removed at age 14-9, 23 months after treatment began. The intraoral views and panoramic radiograph (A to F) show excellent alignment and occlusion, with normal gingival contours. Note (D) the bonded maxillary retainer to maintain the rotation correction and space closure for the maxillary central incisors and (E) the bonded canine-to-canine retainer for the lower arch. In the close-up smile images (G and H), note the consonant smile arc and improved maxillary incisor display.
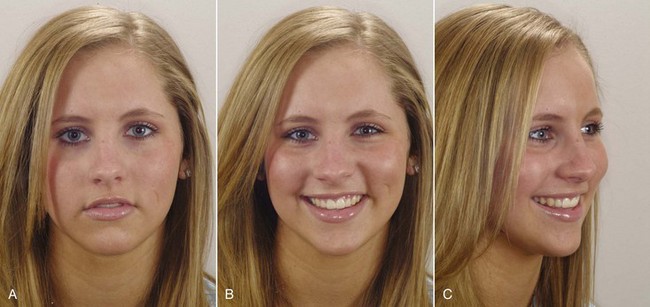

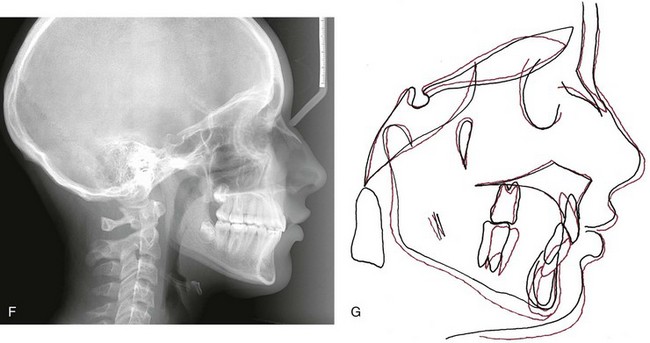
FIGURE 7-43 Patient F.P.: A to C, The posttreatment facial appearance. D and E, Posttreatment facial appearance. F, The posttreatment cephalometric radiograph and (G) a cephalometric superimposition showing the changes during treatment. In the superimposition tracing, note the improvement in upper incisor angulation through palatal root torque, without intrusion or facial tipping of the incisors that would have elevated their incisal edges. One potential solution to a “gummy smile” is intrusion of the maxillary incisors but in this case that would have flattened the smile arc and decreased incisor display, both of which were undesirable. Downward and forward growth of the mandible relative to the maxilla, while the vertical position of the maxillary molars was maintained, was the desired result from use of high-pull headgear.

FIGURE 7-44 Patient F.P., age 21, 6-year follow-up. A to C, Facial photos. D, Smile arc. E and F, Dental occlusion. She had almost no growth after completion of treatment, cooperated with wearing retainers at night to age 18, and had a stable result.
For a relatively simple treatment plan, the associated treatment procedures are also reasonably simple or at least straightforward. Nevertheless, choices must be made and clearly specified in the treatment plan. For example, if the plan is to expand a narrow maxillary arch, it would be possible to do this with an expansion lingual arch, an expansion labial arch, or a banded or bonded maxillary palatal expander. The treatment plan must specify which, and the effectiveness and efficiency of the various possibilities must be considered. There is a time and a place for everything, and this last step is the place for the practical considerations of which treatment method and what orthodontic therapy to use.
The most serious errors in orthodontic treatment planning are those that result from first thinking of which appliance to use, not what the appliance is supposed to accomplish. The treatment mechanics should not be allowed to determine the treatment result. It is an error to establish the treatment mechanics before establishing the broader goal of treatment. The treatment procedures should be manipulated to produce the desired result, not the other way around.
Treatment Planning in Special Circumstances
At one time there was concern that endodontically treated teeth could not be moved. It is now clear that as long as the periodontal ligament is normal, endodontically treated teeth respond to orthodontic force in the same way as teeth with vital pulps. Although some investigators have suggested that root-filled teeth are more subject to root resorption, the current consensus is that this is not a major concern.30 Occasionally, hemisection of a posterior tooth, with removal of one root and endodontic treatment of the remaining root, is desirable. It is perfectly feasible to orthodontically reposition the remaining root of a posterior tooth, should this be necessary, after the endodontics is completed. In general, prior endodontic treatment does not contraindicate orthodontic tooth movement, but teeth with a history of severe trauma may be at greater risk of root resorption, whether they have received endodontic treatment or not.
Essentially all periodontal treatment procedures may be used in bringing a pre-orthodontic patient to the point of satisfactory maintenance, with the exception of osseous surgery. Scaling, curettage, flap procedures, and gingival grafts should be employed as appropriate before orthodontic treatment so that progression of periodontal problems during orthodontic treatment can be avoided. Children or adults with a lack of adequate attached gingiva in the mandibular anterior region should have free gingival grafts to create attached gingiva before the beginning of orthodontics. This is especially true if tooth movement would place the teeth in a more facial position.
Further details in the sequencing of treatment for adults with multiple problems are provided in Chapter 18.
Systemic Disease Problems
Patients who are suffering from systemic disease are at greater risk for complications during orthodontic treatment but can have successful orthodontic treatment as long as the systemic problems are under control.
In adults or children, the most common systemic problem that may complicate orthodontic treatment is diabetes or a prediabetic state. If the diabetes is under good control, periodontal responses to orthodontic force are essentially normal and successful orthodontic treatment, particularly the adjunctive procedures most often desired for adult diabetics, can be carried out successfully. The rapid progression of alveolar bone loss in patients with diabetes is well recognized, however, and if diabetes is not under good control, there is a real risk of accelerated periodontal breakdown (Figure 7-45). For this reason, careful monitoring of a diabetic patient’s compliance with medical therapy is essential during any phase of orthodontic treatment. Prolonged comprehensive orthodontic treatment should be avoided in these patients if at all possible.
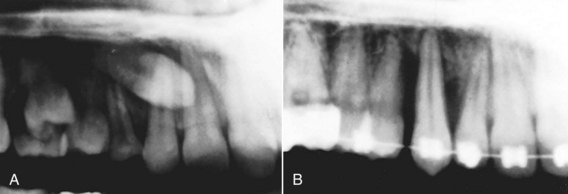
FIGURE 7-45 Patients with uncontrolled diabetes may experience rapid bone loss during orthodontic tooth movement. A, Impacted canine in a 13-year-old girl. B, 1 year later. Note the extent of bone loss around the tooth as it was being moved. During the year of active treatment, the patient had great difficulty in controlling her diabetes and was hospitalized for related problems on two occasions. (Courtesy Dr. G. Jacobs.)
Arthritic degeneration may also be a factor in orthodontic planning. Juvenile rheumatoid arthritis (JRA) frequently produces severe skeletal mandibular deficiency, and adult-onset rheumatoid arthritis can destroy the condylar process and create a deformity (Figure 7-46). Reduced mandibular growth has been reported after steroid injections into the TM joint in JRA treatment,31 and long-term administration of steroids as part of the medical treatment may increase the possibility of periodontal problems during orthodontics. Keep in mind that children on steroids may also be taking bisphosphonates, which make orthodontic tooth movement almost impossible. Prolonged orthodontic treatment should be avoided in patients with either type of rheumatoid arthritis because the potential for harm is at least as great as the potential benefit.
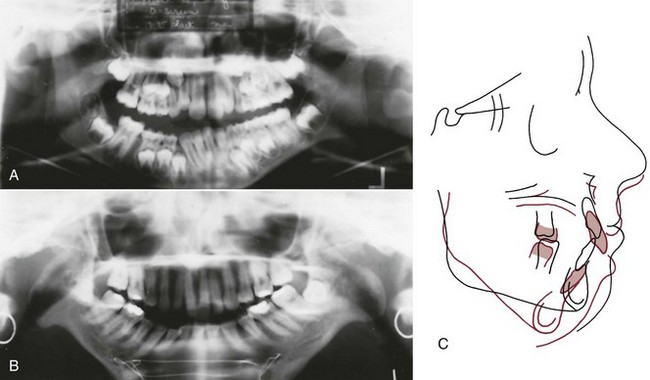
FIGURE 7-46 Rheumatoid arthritis can affect the condylar process and in the worst case can lead to loss of the entire condylar process. A, Panoramic radiograph of a child with rheumatoid arthritis. Note the early degenerative changes in the condyle on the left side (compare the left with the as yet unaffected right side). B, Panoramic radiograph of a young adult with complete destruction of the condylar processes. C, Cephalometric superimpositions for a patient with severe degeneration of the condylar process of the mandible because of rheumatoid arthritis. Age 18, after uneventful orthodontic treatment (black); age 29 (red), by which time the condylar processes had been destroyed. Note the downward-backward rotation of the mandible. (B, Courtesy Dr. M. Goonewardene; C, courtesy Dr. J. R. Greer.)
Comprehensive orthodontic treatment for children with other systemic diseases also is possible if the disease is controlled but requires careful judgment about whether the benefit to the patient warrants the orthodontic treatment. It is not uncommon for the parents of a child with a severe systemic problem (e.g., cystic fibrosis) to seek orthodontic consultation in their bid to do everything possible for their child. With the increasing long-term survival after childhood malignancies and other major problems, children with complex medical backgrounds (such as radiation therapy, long-term steroids, and drugs to prevent loss of bone mass) also are now being seen as potential orthodontic patients. Although treatment for patients with a poor long-term prognosis is technically feasible, it is usually good judgment to limit the scope of treatment plans, accepting some compromise in occlusion to limit treatment time and intensity.
Finally, although orthodontic treatment can be carried out during pregnancy, there are risks involved. Gingival hyperplasia is likely to be a problem, and the hormonal variations in pregnancy sometimes can lead to surprising results from otherwise predictable treatment procedures. Because of bone turnover issues during pregnancy and lactation, an orthodontist theoretically should be vigilant about loss of alveolar bone and root resorption at this time, but radiographs to check on the status of bone and tooth roots are not permissible during pregnancy. Treatment for a potential patient who is already pregnant should be deferred until the pregnancy is completed. If a patient becomes pregnant during treatment, the possible problems should be discussed, and it is wise to place her in a holding pattern during the last trimester, limiting the amount of active tooth movement.
Anomalies and Jaw Injuries
Fortunately, because their consequences are difficult to manage, injuries to the maxilla in children are rare. If the maxilla is displaced by trauma, it should be repositioned immediately if this is possible. When immediate attention to a displaced maxilla is impossible because of other injuries, protraction force from a face mask before fractures have completely healed can successfully reposition it.
Asymmetric Mandibular Deficiency
The causes of asymmetric deficiency are discussed in Chapter 3, and the information on hemifacial microsomia versus condylar injury should be reviewed at this point. In planning treatment, it is important to evaluate whether the affected condyle can translate normally. If it can, as one would expect in a mild-to-moderate form of hemifacial microsomia or posttraumatic injury, a functional appliance could be helpful and should be tried first. If translation of the condyle is severely restricted by posttraumatic scarring, a functional appliance will be ineffective and should not be attempted until the restriction on growth has been removed.
Asymmetry with deficient growth on one side but some translation on that side is a particular indication for custom-designed “hybrid” functional appliances (see Chapter 13) because requirements for the deficient side will be different from those for the normal or more normal side. Often, it is desirable to incorporate a bite block between the teeth on the normal side while providing space for eruption on the deficient side so that the vertical component of the asymmetry can be addressed. In the construction bite, the mandible would be advanced more on the deficient side than on the normal side. The severe restriction of growth that accompanies little or no translation of the condyle can lead to a progressively more severe deformity as growth of other parts of the face continues. Progressive deformity of this type is an indication for early surgical intervention. There is nothing to be gained by waiting for such a deformity to become worse. The goal of surgery is to create an environment in which growth is possible, and orthodontic treatment with a hybrid functional usually is needed after surgery to release ankylosis to guide the subsequent growth.
Hemimandibular Hypertrophy
Mandibular and facial asymmetry can also be caused by excessive growth at a mandibular condyle. Growth problems of this type are almost never symmetric. They appear to be caused by an escape of the growing tissues on one side from normal regulatory control.32 The mechanism by which that could happen is not understood. The condition typically appears in the late teens, most frequently in girls, but may begin at an earlier age. Because the body of the mandible is distorted by the excessive growth (usually by bowing downward on the affected side), the condition is appropriately described as hemimandibular hypertrophy; however, since excessive growth at the condyle is the cause, the old name for this condition, condylar hyperplasia, was not totally wrong.
There are two possible modes of treatment, both surgical: (1) a ramus osteotomy to correct the asymmetry resulting from unilateral overgrowth, after the excessive growth has ceased; and (2) condylectomy to remove the excessively growing condyle and reconstruct the joint. The reconstruction usually is done with a section of rib incorporating the costochondral junction area but occasionally can be accomplished just by recontouring the condylar head (“condylar shave”). Since surgical involvement of the temporomandibular joint should be avoided if possible, the asymmetric ramus osteotomy is preferable. This implies, however, that the abnormal growth has stopped or, in a younger patient, will stop within reasonable limits. As a practical matter, removal of the condyle is likely to be necessary in the more severe and more rapidly growing cases, while a ramus osteotomy is preferred for the less severe problems.
The bone-seeking isotope 99mTc can be used to distinguish an active rapidly growing condyle from an enlarged condyle that has ceased growing. This short-lived gamma-emitting isotope is concentrated in areas of active bone deposition. 99mTc imaging of the oral structures typically shows high activity in areas around the alveolar ridge, particularly in areas where teeth are erupting. The condyles are not normally areas of intense imaging, and a “hot” condyle is evidence of active growth at that site (Figure 7-47).
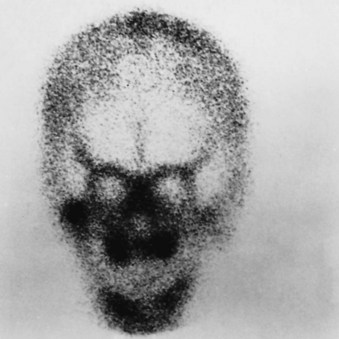
FIGURE 7-47 Bone scan with 99mTc (Towne’s view with the mouth open) in a 10-year-old boy with suspected hyperplasia of the right mandibular condyle. Note the “hot spot” in the area of the right condyle and the difference in uptake of the isotope between the right and left sides. Eruption of teeth and apposition of bone at the alveolar processes normally create heavy imaging along the dental arches.
Unfortunately, though false positive images are rare, false negatives are not, so a negative bone scan of the condyles cannot be taken as evidence that hyperplastic growth of one condyle is not occurring. A positive unilateral condylar response on a bone scan indicates that condylectomy will probably be required, whereas a negative response means that further observation for continuing growth is indicated before the surgical procedure is selected.
Cleft Lip and Palate
Patients with cleft lip and palate routinely require extensive and prolonged orthodontic treatment. Orthodontic treatment may be required at any or all of four separate stages: (1) in infancy before the initial surgical repair of the lip, (2) during the late primary and early mixed dentition, (3) during the late mixed and early permanent dentition, and (4) in the late teens after the completion of facial growth, in conjunction with orthognathic surgery. The typical sequence of treatment is outlined in Box 7-8, and the treatment procedures are discussed in more detail in the next section.
Infant Orthopedics
An infant with a cleft lip and palate will have a distorted maxillary arch at birth in nearly every instance. In patients with a bilateral cleft, the premaxillary segment is often displaced anteriorly while the posterior maxillary segments are lingually collapsed behind it (Figure 7-48). Less severe distortions occur in infants with unilateral palatal clefts (Figure 7-49, A and B). If the distortion of arch form is extremely severe, surgical closure of the lip, which is normally carried out in the early weeks of life, can be extremely difficult. Orthodontic intervention to reposition the segments and to bring the protruding premaxillary segment back into the arch may be needed to obtain a good surgical repair of the lip. This “infant orthopedics” is one of the few instances in which orthodontic treatment for a newborn infant, before eruption of any teeth, may be indicated.

FIGURE 7-48 In this photograph of an infant with a bilateral cleft of the lip and palate, note the forward displacement of the premaxillary segment and medial collapse of the lateral maxillary segments. This displacement of the segments nearly always is seen in infants with a bilateral cleft. An expansion appliance, to create space for retraction of the premaxilla, can be seen in the child’s mouth.


FIGURE 7-49 Long-term observation of treatment of a girl with unilateral cleft lip and palate (through Figure 7-50). A and B, Age 8 weeks prior to lip repair. Note the displacement of the alveolar segments at the cleft site. C and D, Age 9 weeks after lip closure. A palatal plate has been pinned into position to control the alveolar segments, while lip pressure molds them into position. E and F, Age 2, prior to palate closure. G, Age 8, after eruption of maxillary incisors. H, Age 9, incisor alignment in preparation for alveolar bone graft. I, Panoramic radiograph, age 9, just prior to bone graft. J, Panoramic radiograph, age 12, at completion of orthodontic treatment, showing bone fill-in at the cleft site.
In a child with a bilateral cleft, two types of movement of the maxillary segments may be needed. First, the collapsed maxillary posterior segments must be expanded laterally; then pressure against the premaxilla can reposition it posteriorly into its approximately correct position in the arch. This can be accomplished by a light elastic strap across the anterior segment, by an orthodontic appliance pinned to the segments that applies a contraction force, or even by pressure from the repaired lip if lip repair is done after the lateral expansion. In patients with extremely severe protrusion, an appliance held to the maxillary segments by pins might be required, while an elastic strap or the pressure of the lip itself would be adequate with less severe problems.
In infants, the segments can be repositioned surprisingly quickly and easily, so that the period of active treatment is a few weeks at most. If presurgical movement of maxillary segments is indicated, this typically would be done beginning at 3 to 6 weeks of age so that the lip closure could be carried out at approximately 10 weeks. A passive plate, similar to an orthodontic retainer, is then used for a few months after lip closure (see Figure 7-49, C and D).
Soon after this treatment, the infants who have had presurgical orthopedics look much better than those who have not had it. With each passing year, however, it becomes more difficult to tell which patients had segments repositioned in infancy and which did not. The short-term benefit is more impressive than the long-term benefit.33 For some infants with extremely malpositioned segments, which occur almost exclusively in bilateral cleft lip and palate, presurgical infant orthopedics remains useful. For the majority of patients with cleft lip or palate, however, the orthodontist is no longer called to reposition segments in infants. Instead, if the segments protrude, the lip repair may be carried out in two stages, first with a lip adhesion to provide an elastic force from the lip itself, followed at a somewhat later stage by definitive lip repair.
At some centers, bone grafts were placed across the cleft alveolus soon after the infant orthopedics to stabilize the position of the segments. Although a few clinicians still advocate this procedure, the consensus is that early grafting of the alveolar process is contraindicated because it tends to interfere with later growth. Alveolar bone grafts are better deferred until the early mixed dentition.
Late Primary and Early Mixed Dentition Treatment
Many of the orthodontic problems of cleft palate children in the late and early mixed dentition result not from the cleft itself but from the effects of surgical repair. Although the techniques for repair of cleft lip and palate have improved tremendously in recent years, closure of the lip inevitably creates some constriction across the anterior part of the maxillary arch and closure of a cleft palate causes at least some degree of lateral constriction. As a result, surgically treated cleft palate patients have a tendency toward both anterior and lateral crossbite, which is not seen in patients with untreated clefts. This result is not an argument against surgical repair of the lip and palate, which is necessary for esthetic and functional (speech) reasons. It simply means that orthodontic treatment must be considered a necessary part of the habilitation of such patients.
Orthodontic intervention is often unnecessary until the permanent incisor teeth begin to erupt but is usually imperative at that point (Figure 7-49, E to J). As the permanent teeth come in, there is a strong tendency for the maxillary incisors to erupt rotated and often in crossbite. The major goal of orthodontic treatment at this time is to correct incisor position and prepare the patient for an alveolar bone graft.
The objective is to have a permanent tooth erupt through the grafted area so that the cleft is obliterated. An erupting tooth brings bone with it, creating new bone beyond the limits of the previous graft.34 If the permanent lateral incisors are present, the graft should be placed at about age 7, before they erupt. If the laterals are missing, the graft can be delayed but should be done before the permanent canines erupt. Any necessary alignment of incisors or expansion of posterior segments should be completed before the alveolar grafting. The alveolar graft now is a routine part of contemporary treatment, and doing it at the right time is critically important.
Early Permanent Dentition Treatment
As the canine and premolar teeth erupt, posterior crossbite is likely to develop, particularly on the cleft side in a unilateral cleft patient, and the teeth are likely to be malaligned (Figure 7-50). The more successful the surgery, the fewer the problems, but in essentially every instance, fixed appliance orthodontic treatment is necessary in the late mixed or early permanent dentition. New bone fills in the grafted cleft as the canine erupts, which makes it possible to close spaces due to missing teeth, and this now is a major objective of this phase of treatment (see Figure 7-49, I and J).35
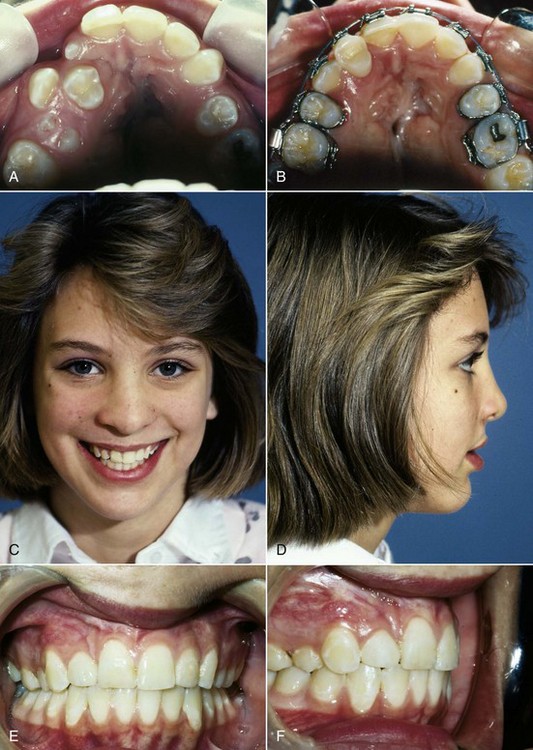

FIGURE 7-50 A, Age 11, transposed first premolar erupting in the grafted area. B, First premolar in lateral incisor position toward the end of active orthodontics, age 12. A tooth that erupts in a grafted area or that is moved orthodontically into the area stimulates formation of new bone that eliminates the cleft. Because teeth bring alveolar bone with them and this bone is lost in the absence of teeth, this is the only way to completely repair an alveolar cleft. C and D, Facial and (E and F) intraoral photos, age 12. G and H, Facial and (I and J) intraoral photos, age 21. At this point the occlusion is stable and both the facial and alveolar cleft can hardly be discerned. Though the palate repair is obvious on intraoral examination, it does not affect appearance or function.
If space closure is not possible, orthodontic tooth movement may be needed to position teeth as abutments for eventual fixed prosthodontics. In that circumstance, a resin-bonded bridge that provides a semipermanent replacement for missing teeth can be extremely helpful. Orthodontic treatment is often completed at age 14, but a permanent bridge in many instances cannot be placed until age 17 or 18. The semipermanent fixed bridge is preferable to prolonged use of a removable retainer with a replacement tooth. Dental implants are not appropriate for cleft areas.
Orthognathic Surgery for Patients with Cleft Lip and Palate
In some patients with cleft lip and palate, more often in males than females, continued mandibular growth after the completion of active orthodontic treatment leads to the return of anterior and lateral crossbites. This result is not so much from excessive mandibular growth as from deficient maxillary growth, both anteroposteriorly and vertically, and it is seen less frequently now because of the improvements in cleft lip/palate surgery in recent years. Orthognathic surgery to bring the deficient maxilla downward and forward may be a necessary last stage in treatment of a patient with cleft lip or palate, typically at about age 18 if required. Occasionally, surgical mandibular setback also may be needed. After this, the definitive restorative work to replace any missing teeth can be carried out. A pharyngeal flap to control leakage of air through the nose often is needed after maxillary advancement in cleft patients.
There has been a striking decrease in recent years in the number of teen-age cleft patients needing either prosthodontic replacement of missing teeth or orthognathic surgery to correct maxillary deficiency. The standard of care now is atraumatic palatal surgery that minimizes interferences with growth, and closure of the space where teeth are missing, made possible by alveolar grafts in the early mixed dentition.
References
1. Betts, NJ, Vanarsdall, RJ, Barber, HD, et al. Diagnosis and treatment of transverse maxillary deficiency. Int J Adult Orthod Orthogn Surg. 1995;10:75–96.
2. Bowman, SJ, Johnston, LE. The esthetic impact of extraction and non-extraction treatments on Caucasian patients. Angle Orthod. 2000;70:3–10.
3. Kim, E, Gianelly, AA. Extraction vs non-extraction: arch widths and smile esthetics. Angle Orthod. 2003;73:354–358.
4. Nimkarn, Y, Miles, PG, O’Reilly, MT, et al. The validity of maxillary expansion indices. Angle Orthod. 1995;65:321–326.
5. Huynh, T, Kennedy, DB, Joondeph, DR, et al. Treatment response and stability of slow maxillary expansion using Haas, hyrax and quad-helix appliances. Am J Orthod Dentofac Orthop. 2009;136:331–339.
6. Pancherz, H, Fackel, U. The skeletofacial growth pattern pre- and post-dentofacial orthopedics. Eur J Orthod. 1990;12:209–218.
7. Tulloch, JFC, Proffit, WR, Phillips, C. Permanent dentition outcomes in a two-phase randomized clinical trial of early Class II treatment. Am J Orthod Dentofac Orthop. 2004;125:657–667.
8. King, GJ, McGorray, SP, Wheeler, TT, et al. Comparison of peer assessment ratings (PAR) from 1-phase and 2-phase treatment protocols for Class II malocclusions. Am J Orthod Dentofac Orthop. 2003;123:489–496.
9. O’Brien, K, Wright, J, Conboy, F, et al. Early treatment for Class II division 1 malocclusion with the twin-block appliance. Am J Orthod Dentofac Orthop. 2009;135:573–579.
10. Luppapornlap, S, Johnston, LE. The effects of premolar extraction: a long-term comparison of outcomes in “clear-cut” extraction and nonextraction Class II patients. Angle Orthod. 1993;63:257–272.
11. Beattie, JR, Paquette, DE, Johnston, LE. The functional impact of extraction and non-extraction treatments: A long-term comparison in patients with “borderline,” equally susceptible Class II malocclusions. Am J Orthod Dentofac Orthop. 1994;105:444–449.
12. Polat-Ozsoy, O, Kircelli, BH, Arman-Ozcirpici, A, et al. Pendulum appliances with 2 anchorage designs: conventional anchorage vs. bone anchorage. Am J Orthod Dentofac Orthop. 133, 2008. [339, e9-e17].
13. Baccetti, T, Franchi, L, McNamara, JA. Cephalometric variables predicting long-term success or failure of combined RPE and face mask therapy. Am J Orthod Dentofac Orthop. 2004;126:16–22.
14. Wells, AW, Sarver, DM, Proffit, WR. Long-term efficacy of reverse-pull headgear therapy. Angle Orthod. 2006;76:915–922.
15. Kircelli, BH, Pektas, ZO. Midfacial protraction with skeletally anchored face mask therapy: a novel approach and preliminary results. Am J Orthod Dentofac Orthop. 2008;122:349–352.
16. DeClerck, H, Cevidanes, L, Baccetti, T. Dentofacial effects of bone-anchored maxillary protraction: a controlled study of consecutively treated Class III patients. Am J Orthod Dentofac Orthop. 2010;138:577–581.
17. Heymann, GC, Cevidanes, L, Cornelis, M, et al. Three-dimensional analysis of maxillary protraction with intermaxillary elastics to miniplates. Am J Orthod Dentofac Orthop. 2010;137:274–284.
18. Burns, NR, Musich, DR, Martin, C, et al. Class III camouflage treatment: what are the limits? Am J Orthod Dentofac Orthop. 2010;137:9e1–e13. [eds summary 137:9-11].
19. Freeman, CS, McNamara, JA, Baccetti, T, et al. Treatment effects of the bionator and high-pull facebow combination followed by fixed appliances in patients with increased vertical dimensions. Am J Orthod Dentofac Orthop. 2007;131:184–195.
20. Phillips, C, Hill, BJ, Cannac, C. The influence of video imaging on patients’ perceptions and expectations. Angle Orthod. 1995;65:263–270.
21. Parekh, J, Fields, H, Beck, M, et al. The perception of selected aspects of smile esthetics—smile arcs and buccal corridors. Am J Orthod Dentofac Orthop. 2006;129:711–717.
22. Ker, AJ, Chan, R, Fields, HW, et al. Esthetic and smile characteristics from the layperson’s perspective: a computer-based survey study. J Am Dent Assoc. 2008;139:1318–1327.
23. Kokich, VO, Kinzer, GA. Managing congenitally missing lateral incisors. Part I. Canine substitution. J Esthet Restor Dent. 2005;17:5–10. [Part II. Tooth-supported restorations, 17:76-84, 2005; Part III. Implants, 17:202-210, 2005].
24. Sfikas, PM. A duty to disclose: issues to consider in securing informed consent. J Am Dent Assoc. 2003;134:1329–1333.
25. Mortensen, MG, Kiyak, HA, Omnell, L. Patient and parent understanding of informed consent in orthodontics. Am J Orthod Dentofac Orthop. 2003;124:541–550.
26. Kutner M, Greenberg E, Jin Y, et al. The health literacy of America’s adults: results from the 2003 National Assessment of Adult Literacy. US Department of Education, National Center for Education Statistics. NCES 2006-483.
27. Carr KM, Fields HW, Beck FM, et al. Improving orthodontic informed consent: a new approach. Am J Orthod Dentofac Orthop, in press.
28. Kang, EY, Fields, HW, Kiyak, A, et al. Informed consent recall and comprehension in orthodontics: traditional versus improved readability and processability methods. Am J Orthod Dentofac Orthop. 2009;136:488. [e1-e13].
29. Bandura, A, Barbaranelli, C, Capara, GV, et al. Self-efficacy beliefs as shapers of children’s aspirations and career trajectories. Child Development. 2001;72:187–206.
30. Llamas-Carreras, JM, Amarilla, A, Solano, E, et al. Study of external root resorption during orthodontic treatment in root filled teeth compared with their contralateral teeth with vital pulps. Int Endod J. 2010;43:654–662.
31. Stostrup, P, Kristensen, KD, Kuseler, A, et al. Reduced mandibular growth in experimental arthritis in the TM joint treated with intra-articular corticosteroids. Eur J Orthod. 2008;30:111–119.
32. Eslami, B, Behnia, H, Javadi, H, et al. Histopathologic comparison of normal and hyperplastic condyles. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:711–717.
33. Bongaarts, CAM, Prahl-Andersen, B, Bronkhorst, EW, et al. Infant orthopedics and facial growth in complete unilateral cleft lip and palate until six years of age (Dutchcleft). Cleft Palate Craniofac J. 2009;46:654–663.
34. Goudy, S, Lott, D, Burton, R, et al. Secondary alveolar bone grafting: outcomes, revisions and new applications. Cleft Palate Craniofac J. 2009;46:610–612.
35. Oosterkamp, BCM, Dijkstra, PU, Remmelink, HJ, et al. Orthodontic space closure versus prosthetic replacement of missing upper lateral incisors in patients with bilateral cleft lip and palate. Cleft Palate Craniofac J. 2010;47:591–596.