Chapter 37The Metacarpal Region
Anatomy
This chapter discusses the examination and diagnosis of injuries to the metacarpal region of the horse. The detailed anatomy of the deep digital flexor tendon (DDFT) (see Chapter 70), the accessory ligament of the deep digital flexor tendon (ALDDFT) (see Chapter 71), the superficial digital flexor tendon (SDFT) (see Chapter 69), and the third interosseous muscle or suspensory ligament (SL) (see Chapter 72) is discussed elsewhere.
In the metacarpal region the interosseous ligaments attach the second (McII) and fourth (McIV) metacarpal bones to the third metacarpal bone (McIII). These ligaments ossify to a variable extent during skeletal maturation. Fibrous bands extend from the distal aspect of the McII and McIV to the medial and lateral proximal sesamoid bones (PSBs).
The proximal aspect of the third interosseous muscle or SL attaches to the proximal palmar aspect of the McIII and the palmar carpal ligament and lies between the McII and McIV. Large exostoses on the axial aspect of the McII or the McIV have the potential to impinge on the abaxial border of the SL. The carpal sheath (see Chapter 75) extends through the proximal third of the metacarpal region. The amount of fluid in the carpal sheath varies between horses but is usually bilaterally symmetrical.
The digital flexor tendon sheath (DFTS) envelops the SDFT and DDFT from the distal third of the metacarpal region to the middle of the middle phalanx. Palmar to the metacarpophalangeal joint, the sheath passes through the inelastic canal created by the palmar annular ligament (PAL), the palmar fibrocartilaginous surfaces of the PSBs, and the intersesamoidean ligament. Within the DFTS, proximal to the sesamoidean canal, the SDFT forms a ring (the manica flexoria) around the DDFT. In the palmar midsagittal plane, a synovial reflection, the vincula, attaches the SDFT to the DFTS wall. Proximal to the manica flexoria, the DDFT is attached medially and laterally by mesotendon to the DFTS wall. The lateral mesotendon is more substantial and extends farther distally.
The palmar and palmar metacarpal nerves innervate the palmar metacarpal region. The SL is innervated by the medial and lateral palmar metacarpal nerves, branches of the deep branch of the lateral palmar nerve. This nerve receives contributions from the ulnar and median nerves. The medial palmar metacarpal nerve has fibers only from the median nerve, whereas the lateral palmar metacarpal nerve has fibers from the ulnar and median nerves.1 The SDFT and DDFT are innervated by the palmar nerves.2
In the proximal metacarpal region, the palmar nerves lie beneath relatively thick fascia, whereas farther distally they are more superficial. In the proximal 5 cm of the metacarpal region, the palmar metacarpal nerves and the distal palmar outpouching of the carpometacarpal joint capsule are in close proximity.
Diagnosis
Clinical Examination
The metacarpal region should be examined visually from all angles to identify any changes in contour caused by swelling. If the limb is hairy, subtle swellings may easily be missed, especially in heavier breeds of horses, and if injury to the metacarpal region is suspected, then clipping the hair to facilitate examination can be useful. Palpation of the metacarpal region should be performed systematically with the limb bearing weight and with the limb semiflexed. With the limb bearing weight, the contour of the dorsal and palmar aspects of the limb should be straight. Distention of the medial palmar vein may reflect local inflammation. The size of the SL and its branches is assessed by running both thumbs down the dorsal and palmar borders from proximally to distally, medially, and laterally; they should remain equidistant. With the limb lifted, the margins of each of the SDFT, DDFT, ALDDFT, and SL should be carefully palpated to detect rounding of the margins, enlargement, or change in texture. Each structure should be squeezed, starting proximally and working distally, gently at first and then with increasing pressure to determine whether pain can be elicited. Careful comparison should be made with the contralateral limb, bearing in mind that lesions may be present bilaterally. Assess the response in light of the horse’s temperament and the recent work history. Abnormal stiffness of a structure may reflect previous injury. It is necessary to roll away the digital flexor tendons and compress the SL against the palmar aspect of the McIII to assess the most proximal part of the SL.
The axial and palmar margins of the McII and McIV should be palpated to identify any new bone formation (a splint) and to determine whether applied pressure causes pain. It is also important to assess whether the axial margin of the splint is clearly demarcated from the SL. Firm pressure should be applied to the dorsal aspects of the McIII to identify pain.
Local Analgesic Techniques
When local analgesic techniques are performed in the metacarpal region, it is important to recognize the potential for local anesthetic solution to diffuse proximally from the site of injection and thereby desensitize structures farther proximally, partially, or completely. Minimum volumes of local anesthetic solution should be used (maximum 2 mL/site and less in ponies) to minimize the risks of misinterpretation. The horse should stand still after injection before reassessment of the gait and should be reevaluated no more than 10 minutes after injection. Even then, false-positive results may be seen.
The metacarpal region seems particularly prone to development of swelling at the site of injection, which potentially may be permanent. The limb should be thoroughly scrubbed with chlorhexidine before injection to minimize the risk of adverse reaction and because of the potential for inadvertent injection into a synovial cavity (the DFTS, carpal sheath, or carpometacarpal joint capsule). The use of nonirritating local anesthetic solution (mepivacaine) is strongly recommended. It is also suggested that a stable bandage be applied to the limb for about 18 hours after injection.
Perineural analgesia of the palmar nerves at the level of the base of the PSBs desensitizes the foot and pastern regions, but in some horses it may also alleviate pain from the metacarpophalangeal joint, the proximal phalanx, PAL, SL branches, and DFTS. In horses with pain arising from the metacarpal region, lameness often appears paradoxically worse after palmar (abaxial sesamoid) nerve blocks, especially with proximal suspensory desmitis. Complete desensitization of the distal third of the metacarpal region requires perineural analgesia of the palmar nerves at the junction of the proximal two thirds and distal one third of the metacarpal region and the palmar metacarpal nerves distal to the distal aspect of the McII and McIV, the so-called low palmar or four-point block. Care should be taken to avoid inadvertent injection into the DFTS, which can occur when performing the palmar block despite no synovial fluid appearing in the needle hub. Proximal diffusion may result in partial alleviation of pain from the body of the SL in association with ultrasonographic evidence of proximal suspensory desmitis. If a unilateral lesion is suspected, the block may be performed medially or laterally alone.
Desensitization of one specific PSB can be achieved by blocking the sesamoidean nerve by introducing a needle between the insertion of the SL and the dorsal aspect of the abaxial surface of the sesamoid bone. The needle is directed toward the apex of the bone, and 0.5 mL of local anesthetic solution is injected.3
Elimination of pain from the entire metacarpal region requires blocking the palmar nerves immediately distal to the carpus and the deep branch of the ulnar nerve (and thus the palmar metacarpal nerves). However, often it is useful to be more specific and desensitize the deep structures (the palmar aspect of the McIII and the SL) or the more superficial structures (SDFT, DDFT, and ALDDFT). Perineural analgesia of the deep branch of the lateral palmar nerve or of the palmar metacarpal nerves by subcarpal injection should theoretically not abolish pain from the fetlock or more distal aspect of the limb, but this does sometimes occur. It is therefore important to perform the low 4-point block first. Blocking the palmar metacarpal nerves immediately distal to the carpus runs the risk of inadvertent injection into the distopalmar outpouchings of the carpometacarpal joint or spread of the local anesthetic solution by diffusion. Theoretically the risk of failure to desensitize the most proximal aspect of the SL exists, but diffusion of local anesthetic solution usually removes pain; false-negative results sometimes occur. The response should be compared with that following intraarticular analgesia of the middle carpal joint. Occasionally subcarpal analgesia of the palmar metacarpal nerves relieves pain associated with a primary middle carpal joint lesion better than intraarticular analgesia. Intraarticular analgesia of the middle carpal joint may relieve pain associated with proximal suspensory desmitis or a palmar cortical fatigue fracture of the McIII.
Perineural analgesia of the lateral palmar nerve from the lateral4 or medial5 approach entails less risk of affecting the middle carpal joint, but it does not eliminate it totally. The potential to remove pain from the lateral aspect of the more distal part of the limb also exists. From the lateral approach there is also a substantial risk of desensitization of the carpal sheath. This block can be particularly useful in a difficult horse, which is easier to inject with the limb bearing weight rather than semiflexed.
Theoretically, blocking the ulnar nerve should not completely remove pain associated with the proximal aspect of the SL or the proximal palmar aspect of the McIII because of the contribution of fibers from the median nerve to the medial and lateral palmar metacarpal nerves. However, in practice it generally does. The ulnar nerve block can be particularly useful to differentiate proximal metacarpal region pain from carpal pain in horses with an equivocal response to subcarpal analgesia; however, occasionally carpal pain is reduced.
Perineural analgesia of the palmar nerves (2 mL/site) should not desensitize the deeper structures (the McIII, SL) but should alleviate pain from the more superficial structures (SDFT, DDFT, and ALDDFT). Local infiltration around a painful exostosis of the McII or the McIV seems to be the most effective way of determining whether pain from the exostosis is contributing to the lameness observed. However, occasionally perineural analgesia proximal to the painful splint exostosis is necessary to abolish pain.
Intrathecal analgesia of the DFTS usually results in improvement in lameness associated with pain from within the sheath, but a better response is frequently seen after perineural analgesia of the palmar and palmar metacarpal nerves. Injection into the DFTS is most easily performed on the palmar midline of the pastern region, distal to the proximal digital annular ligament. The likelihood of inducing iatrogenic hemorrhage at this site is small, and retrieval of synovial fluid usually is easier than from the DFTS proximal to the PAL. If distention of the DFTS is only mild, compression of the proximal part of the sheath by an assistant to increase distention in the palmar pouch in the pastern can be helpful. Injection into the carpal sheath is usually only indicated if the sheath is distended (see Chapter 75).
Imaging
Radiography and Radiology
Radiographic examination of the metacarpal region is usually tailored to each particular horse concerning the images required and the exposure factors used. With localized periosteal new bone, often finely coned-down images and use of soft exposures (low kilovolts [peak]) are required to demonstrate the lesion best. Several similar images varying slightly in obliquity may be required rather than a full series of dorsopalmar, lateromedial, dorsolateral-palmaromedial oblique, and palmarolateral-dorsomedial oblique images. Therefore a flexible approach must be used, depending on the initial clinical signs. Little soft tissue covers the metacarpal region; therefore a grid is not required. A high-definition screen with slow-speed film provides the best detail, although this may not be necessary with digital or computed radiography. Diffuse swelling in the metacarpal region makes images appear flatter, lacking contrast. Exposure factors may need to be increased slightly.
Superimposition of the McII and McIV over the McIII can create confusing radiolucent Mach lines (see page 174). The nutrient canal in the McII and McIV varies in prominence6 and should not be confused as a fracture. Ossification varies between the McII and McIV and the McIII in normal horses.
Ultrasonography
Ultrasonographic examination of the metacarpal region is discussed in detail elsewhere (see Chapters 16 and 69 to 72). In large, cob-type horses, the skin and underlying subcutaneous tissues in the metacarpal region may be thick, making it difficult to obtain high-resolution images. Dense stubble may persist after fine clipping of the hair coat, making it difficult to maintain good contact. Deep skin folds may further complicate the issue. For these horses it may be necessary to amplify the power and gain controls of the ultrasound machine and increase the focal depth of the transducer. Image quality may be enhanced by application of copious amounts of the ultrasound coupling gel to the skin for at least 15 minutes before imaging.
Nuclear Scintigraphy
Blood pool (soft tissue phase) and bone phase (delayed) images of the metacarpal region are particularly useful in horses in which pain has been localized to the metacarpal region but in which no clinically significant radiological or ultrasonographic abnormalities have been identified. Many exostoses involving the McII and the McIV, although clinically inactive, are associated with moderately increased radiopharmaceutical uptake (IRU). Clinically silent enostosis-like lesions also may have IRU.
Differential Diagnosis
Bucked or Sore Shins and Saucer (Dorsal Cortical) Fractures of the Third Metacarpal Bone
See Chapter 102 for a discussion of bucked shins and dorsal cortical (saucer) fractures of the McIII.
Medial and Lateral Condylar Fractures of the Third Metacarpal Bone
See Chapter 36 for a discussion of medial and lateral condylar fractures of the McIII (see page 408).
Incomplete, Longitudinal Palmar Cortical Fatigue Fractures of the Third Metacarpal Bone and Stress Reactions
Incomplete palmar cortical fatigue fractures of the McIII are relatively common and almost invariably involve the medial aspect of the bone,11-14 may involve the metaphyseal and proximal diaphyseal region, and sometimes extend proximally to involve the carpometacarpal joint. They are believed to be fatigue or stress fractures because increased radiopacity may be present radiologically when lameness is first recognized, indicating previous bony reaction.
These fractures occur most commonly in young horses, but they also occur in skeletally mature horses. In some horses, a recent increase in work intensity can be identified, which may be a predisposing factor. These fractures have been identified in a variety of racehorses sports horses, including horses used for flat and harness racing, National Hunt racing, and point-to-point racing, dressage, eventing, and endurance riding.
Clinical Signs
Lameness usually is sudden in onset and may be unilateral or bilateral. In some horses with bilateral injury, lameness is insidious in onset, and the horse has loss of forelimb action. Lameness varies from moderate to severe and tends to be worst on hard ground, and often the horse appears to become lamer the farther it trots. After the horse turns at the walk, the lameness then improves and again deteriorates as the horse trots. If the lameness is bilateral and similar in degree in each limb, the horse moves with a short striding, stilted gait.
Usually no localizing clinical signs suggest the source of pain. Often the horse does not react to palpation of the proximopalmar aspect of the McIII, unless the injury is acute.
Diagnosis
Lameness is substantially improved or alleviated by palmar metacarpal (subcarpal) nerve blocks or perineural analgesia of the deep branch of the lateral palmar nerve. Lameness may be improved in some horses by intraarticular analgesia of the middle carpal joint.
Dorsopalmar radiographic images of the proximal metacarpal region may reveal increased radiopacity of the proximal medial aspect of the McIII, with or without a longitudinal radiolucent line extending a variable distance proximodistally (Figure 37-1). If present, the radiolucent line is invariably located medial to the axis of the McIII. Several slightly oblique dorsopalmar images may facilitate identification of a fracture. Generally no radiological abnormality is detectable in other images, although very occasionally periosteal callus is seen on the palmar aspect of the McIII in a lateromedial image. In some horses, no detectable radiological abnormality exists at any stage.
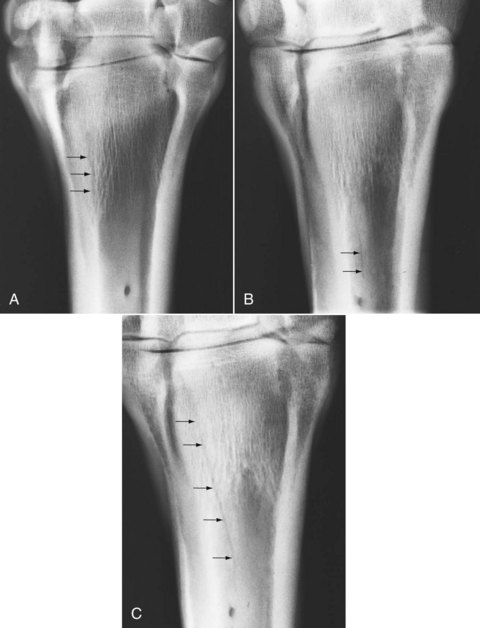
Fig. 37-1 A, Dorsopalmar radiographic image of the right third metacarpal bone of a 6-year-old Thoroughbred hurdler with moderate right forelimb lameness recognized 7 days previously and alleviated by subcarpal analgesia of the palmar metacarpal nerves. Medial is to the left. The medial aspect of the metaphyseal and proximal diaphyseal regions of the third metacarpal bone has increased radiopacity. A poorly defined longitudinal radiolucent line (arrows) represents an incomplete longitudinal palmar cortical fatigue fracture. B, Dorsopalmar radiographic image of the right proximal metacarpal region of a 6-year-old Arabian endurance horse with a moderate right forelimb lameness of 3 weeks’ duration. Lameness was alleviated by perineural analgesia of the deep branch of the lateral palmar nerve. Well-defined increased radiopacity immediately proximal to the nutrient foramen surrounds a longitudinal radiolucent line in the third metacarpal bone (arrows). C, The same horse as in B after 4 weeks of box rest. The radiolucent line extends further proximally (arrows).
Diagnostic ultrasonography usually reveals no detectable abnormality. Rarely a defect in the palmar cortex of the McIII can be identified. Nuclear scintigraphic images usually demonstrate moderate to intense IRU in the proximal palmar aspect of the McIII in dorsal and lateral bone phase images (Figure 37-2). Early radiopharmaceutical uptake in the proximal palmar aspect of the McIII may also be evident in pool phase images. This pattern of uptake is indistinguishable from that associated with an avulsion fracture of the McIII at the attachment of the SL. It is not known whether horses without radiological change, but with scintigraphic evidence of an increased bone modeling in the proximal aspect of the McIII, would develop a radiologically evident incomplete palmar cortical fracture of the McIII if the horses were kept in work, or whether this is a different manifestation of the response of bone to exercise.
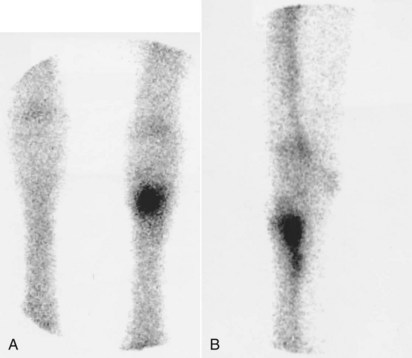
Fig. 37-2 Dorsal (A) and lateral (B) scintigraphic images of the carpal and proximal metacarpal regions of the forelimbs of an 8-year-old advanced event horse with acute-onset moderate left forelimb lameness of 3 weeks’ duration. The left forelimb is on the right in the dorsal image (A). Lameness was alleviated by subcarpal analgesia of the palmar metacarpal nerves. The character of the lameness was typical of a palmar cortical fatigue fracture, but no radiological or ultrasonographic abnormality was detected. Intense focal increased radiopharmaceutical uptake in the proximal, medial, palmar aspect of the third metacarpal bone is compatible with a stress or fatigue fracture.
MRI in a small number of Thoroughbred (TB) racehorses with no detectable radiological abnormality revealed diffuse areas of reduced signal intensity in the proximal palmar aspect of the McIII in T1 gradient echo (GRE) images and increased signal intensity in fat-suppressed and T2-weighted GRE images (surrounded by a hypointense rim in T2-weighted images, the result of a fluid-fat cancellation artefact), consistent with bone trauma.15 In some horses a cortical defect consistent with a fracture was identified, usually medially. The clinical characteristics of the lameness in these horses were not described and scintigraphy was not performed. It is not clear whether these injuries are stress-related bone injuries that reflect a continuum with palmar cortical fatigue fractures. Similar abnormalities have also been seen in endurance and other sports horses, in association with IRU, and similar lameness characteristics of those described for palmar cortical fatigue fractures.10 Generally the entire palmar aspect of the McIII is involved, sometimes accompanied by signal alterations in the McII or the McIV, unlike the palmar cortical stress fractures described above in which radiological abnormalities are usually restricted to the medial aspect of the McIII. However, the MR signal alterations were usually most extensive medially.
Treatment
Most horses respond well to rest, with box rest for 1 month and then box rest and controlled walking exercise for another 2 months. Horses are then able to slowly and progressively resume normal work. The incidence of recurrent injury is small. Every attempt should be made to identify any problem with the previous training program that may have predisposed the horse to injury.
Midshaft Fractures of the Third Metacarpal Bone
See page 502 for a discussion of midshaft fractures of the McIII.
Transverse Stress Fractures of the Distal Metaphyseal Region of the Third Metacarpal Region
Transverse stress fractures of the distal metaphyseal region of the McIII are relatively uncommon.16 I have seen this fracture in horses of 4 to 7 years of age in the first season of racing over fences, in young polo ponies, and in pleasure horses that have galloped on the beach. These fractures are believed to be stress fractures because endosteal and periosteal callus has usually been identified radiologically at the first recognition of the lameness. Acute fractures have also been identified in young TB flat racehorses, sometimes only in light work.
Clinical Signs
In young immature TB racehorses there is usually acute-onset severe lameness unassociated with work. There is rapid development of swelling in the distal third of the metacarpal region on the palmar, palmaromedial, or palmarolateral aspects, which is exquisitely painful on palpation and may mimic cellulitis. Radiographs are usually negative initially, but within 7 to 10 days a tranverse radiopaque line becomes apparent across the distal metaphyseal region and ill-defined periosteal new bone proximally and distally, resulting in distortion of the distal aspect of the McII or the McIV. In some horses, a radiolucent fracture line may eventually be identified. Lameness takes several months to resolve, and there is slow remodeling of the periosteal callus.
In older horses, lameness is usually acute in onset after fast work, is moderate to severe, and may be unilateral or bilateral. Lameness may improve rapidly with the horse appearing sound within a few days. In horses with long-standing lameness, a change in contour of the distal dorsal aspect of the McIII is visible and is associated with periosteal callus formation. In these horses, pain may be elicited by firm pressure applied to the distal dorsal or palmar aspects of the McIII. Twisting the McIII may also induce pain. However, horses with acute lameness may have no localizing signs.
Diagnosis
If lameness persists, local analgesic techniques can be used to isolate the pain, but in some horses this is not possible because of the rapid resolution of lameness, unless the horse is maintained in full work. Lameness is eliminated by palmar (midcannon) and palmar metacarpal (distal to the button of the McII and the McIV) nerve blocks, but it is not influenced by intraarticular analgesia of the metacarpophalangeal joint.
Dorsopalmar, dorsolateral-palmaromedial oblique, dorsomedial-palmarolateral oblique, and lateromedial radiographic images of the fetlock region should be obtained. Flexed lateromedial images are preferable because this technique lifts the PSBs away from the palmar cortex of the McIII, allowing better evaluation. Radiological abnormalities may include a horizontal fracture line and endosteal and periosteal callus (Figure 37-3). Some horses, in particular those with acute lameness, may have no detectable abnormality.
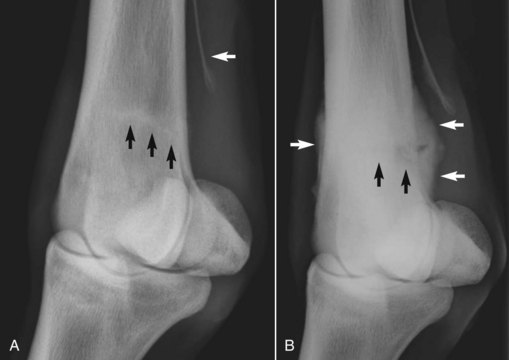
Fig. 37-3 Dorsolateral-palmaromedial oblique radiographic images of fetlock region of a 3-year-old Thoroughbred flat racehorse obtained 4 days (A) and 33 days (B) after onset of severe lameness, associated with soft tissue swelling in the distal metacarpal region. There is a transverse stress fracture of the distal metaphyseal region of the third metacarpal bone (black arrows) with periosteal callus (white arrows). Note the distortion of the distal aspect of the fourth metacarpal bone.
Nuclear scintigraphy is invaluable for determining the likely presence of a stress fracture in those horses that lack radiological abnormalities or in which lameness rapidly resolves. There is IRU in the distal metaphyseal region of the McIII.
Treatment
Most horses respond well to 3 months’ rest, with 1 month of box rest and then box rest combined with walking exercise. Work intensity can then be progressively increased. The previous training program should be reviewed to try to identify any features that may have predisposed the horse to fracture. Extensive periosteal callus gradually remodels.
Dorsomedial Articular Fractures of the Third Metacarpal Bone
Dorsomedial articular fractures of the McIII have only been recorded in the Standardbred (STB) racehorse,17 although similar fractures have been identified in the McIII of TBs. The condition usually affects horses 2 to 4 years of age and occurs most commonly in pacers.
Clinical Signs
Lameness is acute in onset, after racing or training, and severe. Lameness persists despite rest. A bony swelling may be palpable on the proximal, dorsomedial aspect of the McIII. Direct pressure may elicit pain.
Diagnosis
Lameness is generally improved by intraarticular analgesia of the middle carpal joint. Diagnosis is based on radiological identification of the fracture, best viewed in a dorsolateral-palmaromedial oblique image. The fracture is articular, nondisplaced, and usually incomplete (Figure 37-4). Active periosteal new bone invariably exists at the distal aspect of the fracture, close to the insertion of the extensor carpi radialis tendon, even in an acute injury.

Fig. 37-4 Dorsolateral-palmaromedial oblique xeroradiographic view of the proximal metacarpal region of a 3-year-old Standardbred male with a dorsomedial articular fracture of the third metacarpal bone. The wide oblique incomplete fracture line (arrows) and presence of proliferative new bone along the dorsomedial aspect of the third metacarpal bone indicate that bone activity in this region preceded the development of acute lameness.
(Courtesy Mike Ross, Kennett Square, Pennsylvania, United States.)
Treatment
Treatment consists of rest for a minimum of 3 months. The fractures usually heal with modeling of the periosteal reaction and progressive loss of distinction of the fracture line. Lameness resolves, and horses are able to withstand training before the fracture line completely disappears radiographically.
Stress Reactions in the Condyles of the Third Metacarpal Bone
See Chapter 36 for a discussion of stress reactions (see page 398).
Subchondral Bone Trauma
Osseous trauma of the condyles of the distal aspect of the McIII is a diagnosis made using MRI.18,19 There is usually acute-onset lameness with no localizing clinical signs. Pain is localized to the fetlock region using perineural analgesia. The response to perineural analgesia is often better than to intraarticular analgesia. Radiographic and ultrasonographic examinations usually reveal no detectable abnormality. Scintigraphy usually reveals IRU. There is increased signal intensity in fat-suppressed magnetic resonance images, with reduced signal intensity in T1- and T2-weighted images, in a variable distribution in the distal aspect of the the McIII. In young TB racehorses, subchondral bone trauma is thought to represent stress–adaptation mismatch and is a manifestation of stress-related bone injury (see page 398), often occurring bilaterally. However, in mature sports horses, it more often occurs unilaterally and may reflect single episode trauma. Lameness usually resolves with rest in sports horses, but young TB racehorses may be difficult to keep sound when returned to training.
Avulsion Fracture of the Third Metacarpal Bone at the Origin of the Suspensory Ligament
Avulsion fracture of the McIII at the origin of the SL occurs most commonly in young racehorses (STBs more than TBs).20-24 Some fractures described as avulsions appear to occur immediately distal to the site of attachment of the SL.
Clinical Signs
Onset of lameness usually is acute, and lameness is generally moderate to severe and unilateral. In the acute stage, the horse generally resents pressure applied over the palmar proximal aspect of the McIII. Eliciting pain may be more difficult in horses with chronic lameness. Lameness generally improves but may not resolve by box rest.
Diagnosis
In horses with acute lameness, diagnosis usually can be based on the clinical signs and ultrasonographic or radiological demonstration of a fracture. In horses with more chronic lameness, local analgesic techniques may be required. Perineural analgesia of the palmar metacarpal (subcarpal) nerves or of the deep branch of the lateral palmar nerve usually improves lameness substantially. Intraarticular analgesia of the middle carpal joint, performed by palmar or dorsal approaches, may also improve the lameness.
An avulsion fracture is best detected radiologically in dorsopalmar or slightly oblique dorsopalmar images and lateromedial, or flexed lateromedial, images. The fracture may appear as an almost straight or saucer-shaped lucent line (with the base proximal or distal) (Figure 37-5) or as a punched-out lesion.

Fig. 37-5 A, Dorsopalmar radiographic image of the proximal aspect of the left metacarpal region of a 4-year-old Thoroughbred with acute-onset moderate left forelimb lameness. Lameness was alleviated by perineural analgesia of the lateral palmar nerve just distal to the accessory carpal bone. The curved radiolucent line (arrows) in the proximal aspect of the third metacarpal bone represents an avulsion fracture at the origin of the suspensory ligament. B, Dorsopalmar radiographic image of the proximal metacarpal region of a 3-year-old Thoroughbred with lameness of 2 weeks’ duration. A punched-out radiopacity distal to a crescent-shaped lucent area (arrows) in the third metacarpal bone represents an avulsion fracture at the origin of the suspensory ligament.
An avulsed fragment is usually easiest to detect by ultrasonography in longitudinal images and, if displaced, appears as a discontinuity of the palmar cortex of the McIII. An incomplete fracture may be more difficult to detect. Examining the limb while the horse is bearing weight and not bearing weight can be helpful. Slight periosteal callus may be seen in horses with a more chronic fracture. A small focal tear in the dorsal aspect of the SL at the site of the fracture may be visible in transverse and longitudinal images. Nuclear scintigraphy has been used diagnostically.25
Treatment
The horse should be restricted to box rest for 6 weeks, followed by box rest and controlled exercise for at least another 6 weeks. The horse should be monitored clinically, radiologically, and ultrasonographically. Lameness caused by avulsion fracture generally takes longer to resolve than in horses with primary proximal suspensory desmitis, sometimes up to 2 months. A fracture may remain detectable radiologically for between 2 and 4 months. Periosteal callus is best seen by ultrasonography and usually is undetectable until 4 to 6 weeks after injury. The total convalescent period is usually between 4 and 6 months. Most TBs ultimately make a complete recovery and return to full athletic function without recurrent injury. Occasionally the fracture fragment may sequestrate or suspensory desmitis may progress, which results in a more guarded prognosis. However, some STBs have long-term lameness that is refractory to treatment. Superior results may be achieved using osteostixis.26
Osteoarthritis of the Carpometacarpal Joint
Osteoarthritis (OA) of the carpometacarpal joint is an unusual cause of forelimb lameness. It usually occurs in mature horses used for any discipline. Clusters of Arabians with severe OA have been described27,28 but the condition can occur in horses of any breed.28
Clinical Signs
Lameness may be acute or insidious in onset and ranges from mild to severe. In my clinical experience usually no localizing clinical signs are present, although sometimes there is localized swelling associated with extensive periarticular proliferative new bone, which may be a more typical clinical presentation in Arabians and Quarter Horses.28 Carpal flexion is often not restricted or resented in association with mild radiological abnormalities, but when extensive new bone formation is present carpal flexion is restricted.
Diagnosis
Lameness may be improved by palmar metacarpal (subcarpal) nerve blocks, probably because of proximal diffusion of the local anesthetic solution. Intraarticular analgesia of the middle carpal joint also improves lameness. Radiological examination usually reveals that changes are restricted to the medial or lateral side of the joint, with narrowing of the joint space between the carpus and the McII or the McIV, with subchondral increased radiopacity (see Figure 3-2; Figure 37-6) and often periosteal new bone extending along the proximal metaphyseal region of the McII or the McIV. Lucent zones may appear in the base (head) of the McII or the McIV. In Arabians and Quarter Horses the majority of radiological abnormalities were medial.28
Treatment
Response to intraarticular medication of the carpometacarpal joint has been poor.27,28 Palliative treatment with a nonsteroidal antiinflammatory drug (NSAID) may allow horses with mild lameness to be maintained in work. Partial carpal arthrodesis may alleviate pain (see Chapter 38).29,30 Athrodesis resulted in 10 of 12 horses (83%) being described as sound approximately 2 years postoperatively, but only six horses (50%) returned to ridden activity.30
Osseous Cystlike Lesions in the Proximal Aspect of the Second Metacarpal Bone
Osseous cystlike lesions sometimes are identified in the proximal aspect of the McII (Figure 37-7) in association with lameness that is localized to the proximal metacarpal or distal carpal regions. These osseous cystlike lesions occur most commonly in the presence of a first carpal bone,11 which also may have radiolucent zones. These lesions often occur bilaterally, although lameness may be unilateral. These lesions are generally considered incidental abnormalities unassociated with pain, and the clinician should search for another potential cause of lameness.

Fig. 37-7 A, Dorsomedial-palmarolateral oblique radiographic image of the proximal metacarpal region of a 7-year-old Thoroughbred. There is an osseous cystlike lesion in the second carpal bone in association with the presence of a first carpal bone. Both forelimbs were identical. B, Dorsomedial-palmarolateral oblique image of the proximal metacarpal region of a 6-year-old riding horse. The radiolucent areas in the palmar aspect of the second carpal bone and proximal palmar aspect of the second metacarpal bone are associated with the presence of a first carpal bone. These were incidental radiological findings not related to lameness.
Syndesmopathy between the Second and Third or Fourth and Third Metacarpal Bones
Interosseous ligaments between the McII and the McIII and between the McIV and the McIII ossify to a variable extent. Occasionally complete osseous union develops throughout the length of the bones with internal increased radiopacity of both bones. The biomechanical implications of this are currently not understood. Inflammation of the interosseous ligament with entheseous or endosteal new bone at the ligaments’ attachments was identified using MRI as the only detectable abnormality in horses with pain localized to the metacarpal region or in association with SL pathology.10,31
Exostoses of the Second and Fourth Metacarpal Bones (Splints)
Exostoses on the McII or the McIV (splints) may develop because of direct trauma, resulting in subperiosteal hemorrhage and lifting of the periosteum, or instability between the McII (or the McIV) and the McIII. However, many splints do not involve the interosseous space between the McII (or the IV) and the McIII and develop without evidence of trauma. Some splints develop without associated pain and lameness, with little evidence of active inflammation, whereas others result in a localized soft tissue inflammatory reaction, pain, and lameness. The reasons for these differences are not known. Splints may occur at any level but most commonly involve the proximal half of the bone. Lesions involving the McII occur most commonly.
Lesions may develop in young, immature horses or, less commonly, in older horses. Horses with bench (offset) carpal conformation seem particularly prone to develop splints involving the McII, but often these develop without associated lameness.
Clinical Signs
Lameness may be sudden or insidious in onset and tends to deteriorate with work and be worst on hard ground. There is usually an obvious palpable swelling comprising a bony exostosis, surrounded by an edematous soft tissue reaction, with localized heat and pain on firm palpation. The swelling should be palpated carefully with the limb not bearing weight because sometimes only focal areas of the swelling appear to be painful.
It is important to assess the axial aspect of the exostosis to determine whether there may be impingement on the adjacent SL. Such horses may have had a preexisting splint that was previously inactive. The horse often has a history of more extensive soft tissue swelling developing with hard work. Lameness may be provoked by hard work but rapidly improves with rest or light work. With the limb not bearing weight it may be difficult to palpate the border of the SL adjacent to the exostosis, and pain may be elicited by firm pressure applied to this localized area of the SL.
Diagnosis
Diagnosis of a straightforward splint often can be based on clinical signs, and further diagnostic procedures may not be necessary. Radiology may be useful to document the size and activity of the exostosis (Figure 37-8). Several oblique images using soft exposures are required. Care should be taken not to confuse as fracture radiolucent lines that are caused by layers of new bone being superimposed, by incorporation of fibrous tissue, or an edge effect created by the parent bone. Radiography cannot properly document the axial extent of any exostosis.
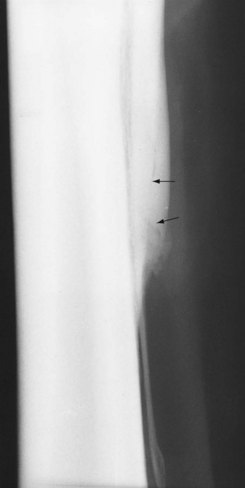
Fig. 37-8 Dorsomedial-palmarolateral oblique image of the metacarpal region. There is smoothly outlined enlargement of the middle of the diaphysis of the second metacarpal bone, with ill-defined, irregularly outlined periosteal new bone at the distal end of the middle third of the bone. The ill-defined radiolucent lines (arrows) within the bone result from new bone formation and should not be confused with fractures.
Nerve blocks or local infiltration may be necessary to prove or disprove that an exostosis is the primary cause of pain resulting in lameness and to identify any concurrent problem(s). Diagnostic ultrasonography is essential if an impingement on the SL is suspected. Identification of echogenic tissue axial to the exostosis and contiguous with the SL may be possible (Figure 37-9). The ipsilateral border of the SL may be irregular and reduced in echogenicity. In a small proportion of horses, adhesions between the SL and the McII or the McIV can only be identified using MRI.8,10
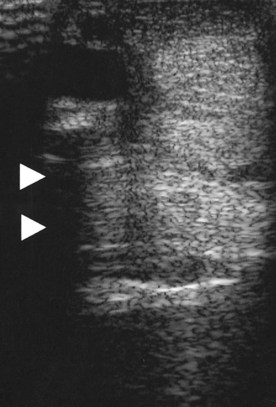
Fig. 37-9 Transverse ultrasonographic image of the palmar metacarpal soft tissues at 14 cm distal to the accessory carpal bone. Medial is to the left. The irregular medial border of the suspensory ligament and the echogenic material (arrowheads) medial to it are apparent. A moderate size exostosis (splint) on the second metacarpal bone extended axially to impinge on the suspensory ligament. Granulomatous-like tissue was interposed between the splint and the suspensory ligament.
Nuclear scintigraphy is generally unnecessary, but it should be noted that even long-standing splints, which appear to be insignificant clinically, often have mild to moderate IRU compared with the parent bone. Why active bone modeling occurs is not known.
Treatment
Lameness associated with a clinically active exostosis usually resolves with rest, and the surrounding soft tissue swelling resolves. The exostosis remodels and is usually ultimately somewhat smaller. However, sometimes irregular-appearing, palisade-like new bone may persist radiologically. The time taken for the bony reaction to settle is extremely variable, ranging from 2 to 3 weeks to 2 to 3 months. This can be difficult to predict accurately and may reflect how quickly the condition was recognized and box rest instituted. Local infiltration with corticosteroids may facilitate reduction of the soft tissue reaction, but whether this alters the course of the condition is debatable. Topical application of dimethyl sulfoxide has a similar effect.
Work should not resume until firm palpation of the exostosis fails to induce pain. Premature return to work is likely to exacerbate the problem. Some degree of fitness may be maintained by swimming exercise.
Some horses seem particularly predisposed to produce large amounts of new bone. The reason for this is unknown. Large exostoses on the McII are vulnerable to direct trauma from the contralateral limb, especially if the horse moves closely in front, or dishes. Some protection may be provided by always applying protective boots when the horse is worked or turned out. In horses with severe exostoses, surgical amputation of the exostosis and more distal aspect of the metacarpal bone should be considered. Ostectomy of the exostosis and liberal removal of the surrounding periosteum from the splint bone and the McIII without removing the distal segment of the splint bone also have been cosmetically and functionally successful in some horses. Surgical technique may influence the risk of reformation of periosteal new bone.32
In some horses chronic pain associated with a splint persists, despite appropriate conservative management. Pin-firing is suggested if pain persists longer than 6 weeks after lameness was first recognized (see Chapter 88). An additional 6 weeks of walking is required before normal work can be resumed after firing.
If there is axial impingement of the exostosis on the SL or adhesions between the splint exostosis and SL, surgical treatment is required. Amputation of the McII or the McIV proximal to the exostosis is the treatment of choice, assuming that this leaves the proximal third of the bone intact, providing stability to the carpus. Often a granulomatous-type reaction occurs between the exostosis and the ipsilateral margin of the SL; this material should also be removed. Alternatively, segmental ostectomy can be performed. One Editor (MWR) prefers to use a different approach because instability of the proximal segment of the McII or the McIV often results in recurrence of lameness and bony proliferation at the ostectomy site. A combination of metacarpal fasciotomy, ostectomy of the exostosis on the axial aspect of the McII or the McIV, adhesiolysis, and the local deposition of antiinflammatory products such as hyaluronan is used.
Fractures of the Second and Fourth Metacarpal Bones
Fractures of the McII and McIV bones may result from direct external trauma or internal forces, frequently in association with suspensory desmitis.33-37 The latter is particularly common in horses that race over fences, STBs, and, less frequently, event horses.
Fractures caused by internal forces usually occur at the junction between the proximal two thirds and distal one third of the metacarpal bone. The distal ends of the McII and the McIV are connected by fibrous bands to the abaxial surface of the medial and lateral PSBs. Hyperextension of the fetlock and stretching of these fibrous bands may predispose to fracture. Suspensory desmitis may precede fracture and result in modeling and progressive deviation of the distal part of the bone away from the McIII because of pressure or adhesions, thus predisposing to fracture. Fractures at this location unassociated with suspensory desmitis are relatively uncommon, but they do occasionally occur.
Fractures Caused by Internal Trauma
Clinical Signs
Lameness is acute in onset and moderate. Diffuse edematous soft tissue swelling rapidly develops in the distal half of the metacarpal region, more extensively medially if the McII is fractured and laterally if the McIV is involved. Occasionally both the McII and the McIV bones are fractured simultaneously. One or both forelimbs may be affected. Careful palpation reveals enlargement of the body and/or branch of the SL. Palpating instability of the distal piece of the fractured bone may be possible, but extensive soft tissue swelling may prevent this.
Diagnosis
Radiographic examination should include the metacarpal bone and the ipsilateral PSB because lesions may occur at both sites concurrently. Preexisting abnormalities of the McII or the McIV suggest long-term suspensory desmitis (Figure 37-10, A). The fracture should be evaluated to determine the degree of displacement and the presence of comminution and callus. Ultrasonographic examination is performed to assess the degree of suspensory desmitis, which is the most important prognostic factor.
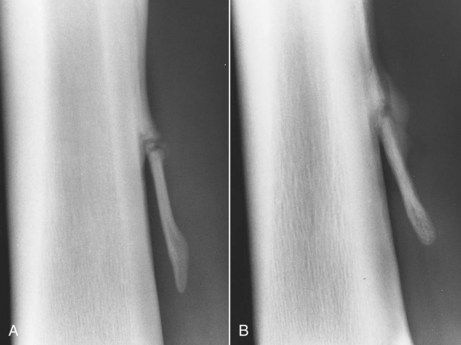
Fig. 37-10 A, Dorsomedial-palmarolateral oblique radiographic image of the second metacarpal bone of a 7-year-old Thoroughbred steeplechaser. There is a complete, displaced fracture at the junction between the middle and distal thirds of the bone. The axial deviation of the bone indicates previous distortion of the bone in association with desmitis of the medial branch of the suspensory ligament. Some endosteal and periosteal callus is present. B, Dorsomedial-palmarolateral oblique radiographic image of the second metacarpal bone of an endurance pony. There is a healing fracture of the second metacarpal bone, associated with desmitis of the medial branch of the suspensory ligament.
Treatment
Some controversy exists concerning the optimal treatment for horses with fractures of the distal third of the McII and the McIV. Some infer that most horses can be managed conservatively, whereas others advocate surgical removal of the fracture fragment. Nondisplaced or slightly displaced fractures usually heal satisfactorily within 4 to 6 weeks if the horse is confined to box rest. Only a small amount of callus develops, which subsequently remodels (see Figure 37-10, B). Small radiolucent defects may persist because of incorporation of fibrous tissue. If a fracture is moderately displaced, a larger amount of callus may develop, or a thick layer of fibrous tissue may be laid down, which envelops the entire distal aspect of the metacarpal bone. A large exostosis may impinge on the SL. Therefore surgical removal of these fragments is recommended. The convalescent program is dictated by the degree of suspensory desmitis. Prognosis is better in STBs than in TBs.
Fractures Caused by External Trauma
Fractures of the McII or the McIV caused by external trauma may be simple or comminuted, open or closed.
Clinical Signs
Lameness is acute in onset and is associated with soft tissue swelling around the fracture site, heat, and pain. An open wound may be present. Thorough debridement, cleaning, and lavage of open wounds are important to minimize the risks of infection.
Diagnosis
Radiographic examination is essential to determine the precise position and nature of the fracture (Figure 37-11). If the fracture is chronic or associated with an open wound, the radiographs should be appraised carefully for evidence of infectious osteitis.

Fig. 37-11 Dorsolateral-palmaromedial oblique radiographic image of the metacarpal region. There is a comminuted, displaced articular fracture of the proximal third of the fourth metacarpal bone. The fracture was repaired surgically using a small plate, but osteoarthritis of the carpometacarpal joint developed subsequently.
Treatment
Fractures involving the proximal third of the bone may require surgical stabilization of the bone to prevent carpal instability, especially if the fracture involves McII. Insertion of small plates with screws into the McII without traversing the interosseous space is the preferred method of management. Oblique fractures of the proximal aspect of the McII or the McIV can be repaired using 3.5-mm bone screws and stainless steel wire using the tension band principle in an intrabone technique (screws only engage the involved splint bone and not the McIII). Alternatively, screws placed between the McII and the McIII can be used, but fixation may be unstable, and chronic lameness could develop because of synostosis between the two bones or reaction from the implants themselves. When horses have simple displaced or comminuted fractures of the McII or the McIV, but with infection, all efforts should be made to resolve infection before surgical fixation is attempted. However, if the fracture is comminuted and the carpus appears to be stable, conservative management may be satisfactory. Simple or more complicated fractures in the distal two thirds of the bone can be treated either conservatively or by surgical removal, depending on the size of the pieces and their location.
Avulsion of the Attachment of the Palmar Annular Ligament from a Proximal Sesamoid Bone
See Chapter 72 for a discussion of avulsion of the attachment of the PAL from a proximal sesamoid bone.
Constriction of the Digital Flexor Tendon Sheath by the Palmar Annular Ligament
See Chapter 74 for a discussion of constriction of the DFTS by the PAL.
Tenosynovitis of the Digital Flexor Tendon Sheath: Primary and Secondary
See Chapter 74 for a discussion of primary and secondary tenosynovitis of the DFTS.
Desmitis of the Body of the Suspensory Ligament
See Chapter 72 for a discussion of desmitis of the body of the SL.
Desmitis of the Medial or Lateral Branch of the Suspensory Ligament
See Chapter 72 for a discussion of desmitis of the medial or lateral branch of the SL.
Desmitis of the Accessory Ligament of the Deep Digital Flexor Tendon
See Chapter 71 for a discussion of desmitis of the ALDDFT.
Superficial Digital Flexor Tendonitis
See Chapter 69 for a discussion of superficial digital flexor tendonitis.
Traumatic Lacerations of the Superficial Digital Flexor Tendon and the Deep Digital Flexor Tendon
See Chapter 81 for a discussion of traumatic lacerations of the SDFT and DDFT.
Differential Diagnosis of Diffuse Filling in the Metacarpal Region
Diffuse filling in the metacarpal region, with or without stiffness or lameness, is common. The clinician makes a diagnosis of the cause through review of the history of the horse and careful clinical examination (Box 37-1).
The clinician should assess the following points:
Hemorrhage
Hemorrhage in the proximal metacarpal region is an occasional cause of acute-onset, severe lameness during work. Extensive soft tissue swelling rapidly develops, mimicking a severe tear of the ALDDFT. The swelling makes it difficult to palpate accurately specific structures. However, ultrasonographic examination reveals no detectable structural abnormality of the digital flexor tendons and the ALDDFT. Application of a large support bandage and treatment with NSAIDs brings rapid relief. The bandage should be maintained and changed as needed for approximately 7 to 10 days. When the bandage is removed, the limb is usually of normal contour. The limb should be reexamined by ultrasonography to confirm that no structural abnormalities exist before allowing the horse to resume normal work. The cause of this condition is unknown, and the likelihood of recurrence is small.
Thrombosis
Thrombosis of the medial palmar vein is a rare cause of lameness in the horse. Partial thrombosis may result in periodic diffuse filling of the distal limb associated with lameness. Complete occlusion may result in severe lameness and distal limb swelling soon after starting any exercise. Diagnosis is based on careful palpation of the vasculature combined with ultrasonography, including Doppler. Treatment requires vascular surgery.
Infection of Tendons
Infection of the SDFT or DDFT, without any evidence of a penetrating wound, is an unusual cause of lameness, but unless infection is recognized early and treated aggressively, it can have catastrophic consequences.38
Clinical Signs
Sudden-onset, severe unilateral lameness involves a forelimb or hindlimb. Frequently this follows within 24 hours of strenuous exercise. The horse is usually reluctant to bear weight on the limb, and effective control of pain can be difficult. Considerable peritendonous edema develops rapidly, precluding accurate palpation of the digital flexor tendons. Palpation reveals localized heat and exquisite pain. The skin may become tight, and if the infection is unrecognized and untreated, pus may exude through defects in the skin within several days.
Diagnosis
Ultrasonographic evaluation reveals a central anechogenic defect within the infected tendon (Figure 37-12) that progresses rapidly and may extend the length of the metacarpal or metatarsal region within a few days. In the early stages, lameness may be disproportionately severe relative to the perceived amount of tendon damage. Bacterial culture has frequently yielded a coagulase-positive Staphylococcus.
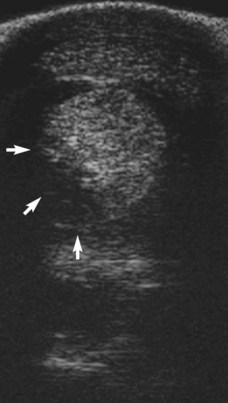
Fig. 37-12 Transverse ultrasonographic image of the plantar metatarsal region. There is subcutaneous edema. The deep digital flexor tendon is enlarged and has a large anechogenic region dorsomedially (arrows) that progressed rapidly. The horse had extensive peritendonous soft tissue swelling and severe lameness associated with the infected tendon.
Treatment
Aggressive systemic antimicrobial therapy with crystalline penicillin, gentamicin, and metronidazole has usually proved inadequate, with progression of tendon destruction despite therapy. Drainage of pus and lavage combined with antimicrobial therapy has successfully controlled infection in some, but not all, horses. However, the prognosis for return to athletic function is extremely guarded.
Cellulitis, Skin Necrosis, and Necrosis of the Superficial Digital Flexor Tendon after Topical Applications
Cellulitis, skin necrosis, and subsequent necrosis of the SDFT are poorly understood conditions. The syndrome has been recognized in National Hunt racehorses.39 After racing, many horses receive a topical application of a claylike substance to the metacarpal regions, with or without overlying bandages.
Clinical Signs
Clinical signs are apparent within 24 to 72 hours and include peritendonous edema and serum ooze progressing to skin slough and exposure of the SDFT. The tendon may also be affected, without evidence of preexisting strain-type injury. Lameness varies from moderate to severe. The condition may be unilateral or bilateral. The horse may have had the same topical application previously but not necessarily so. Frequently other horses have been treated with the same batch of the proprietary claylike substance with no adverse effects. A variety of different proprietary products have been incriminated. Curiously, to my knowledge, the condition has not been seen in event horses, although many receive similar treatments after competing.
Treatment
The condition usually progresses to a huge area of skin loss on the palmar aspect of the metacarpal region, with or without major damage to the underlying SDFT. No therapy has successfully halted this progression. Healing is by granulation tissue and fibrosis. If the horse survives, it has a massively thickened limb, and most horses have not returned to racing.
Cellulitis Associated with Superficial Digital Flexor Tendonitis
Cellulitis sometimes occurs with superficial digital flexor tendonitis. Clinical signs are usually recognized within 24 to 48 hours after competition. The horse has diffuse filling in the metacarpal region(s), and pinpoint pricks appear in the skin through which serum oozes within several days. The horse may be slightly lame or have a stiff gait. Symptomatic therapy usually resolves the majority of filling and lameness, and a primary tendon injury may go unrecognized without careful inspection. Careful ultrasonographic evaluation is mandatory because almost invariably primary tendonitis is present. Care should be taken in the presence of clinically significant subcutaneous edema because acoustic enhancement may mask a subtle tendon lesion. Such horses should be reevaluated after resolution of the edema.
Enostosis-like Lesions
Enostosis-like lesions are focal areas of new bone formation within the medullary cavity of a bone, occurring on the endosteal surface or close to a nutrient foramen. They occasionally occur in the McIII and may be single or multiple. They can occur as incidental radiological abnormalities or in association with lameness. Nuclear scintigraphy may reveal IRU at the site of these lesions, but this does not necessarily imply that associated pain exists. Clinical significance can only be ascribed by eliminating all other sources of pain.
Hypertrophic Osteopathy
Hypertrophic osteopathy, or Marie’s disease, frequently involves the metacarpal region, resulting in localized or diffuse soft tissue swelling that overlies new bone formation.40 Hypertrophic osteopathy has been associated with thoracic disease, a variety of vascular lesions, granulomatous enteritis, and some tumors in the thorax and abdomen. Identification of the primary lesion and successful treatment may result in resolution of the bony lesions and associated clinical signs.
Clinical Signs
The acute stage of hypertrophic osteopathy produces heat and edematous swelling overlying areas of new bone formation. Palpation of the affected bones produces pain. All the limbs should be inspected carefully to establish the extent of the lesions. Depending on the limbs affected, the horse may show overt lameness or generalized stiffness.
Although careful clinical appraisal of the entire horse may reveal clinical signs of an underlying disease process, often no clues are present. Clinical evaluation should include palpation of all lymph nodes, auscultation of the heart and lungs, and rectal examination.
Diagnosis
Radiographic examination, using soft exposures, reveals palisading periosteal new bone in the diaphyseal and metaphyseal regions of the McIII and other affected bones but usually excluding the joints (Figure 37-13). The palisading new bone, perpendicular to the cortices, is pathognomonic.
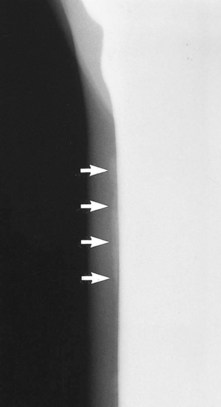
Fig. 37-13 Dorsolateral-palmaromedial oblique radiographic image of the proximal metacarpal region using soft exposure factors to show palisading new bone (arrows) on the dorsal aspect of the third metacarpal bone typical of hypertrophic osteopathy. The 7-year-old breeding stallion had avian tuberculosis and was successfully treated, with the bony lesions resolving.
Every effort should be made to try to define the primary causal lesion. Additional diagnostic tests should include thoracic radiography and echocardiography, examination of a tracheal aspirate and peritoneal fluid, and routine hematological and clinical biochemistry testing. If weight loss is evident, an oral glucose tolerance test should be performed to assess small intestinal absorption of disaccharide sugars. A labeled white blood cell nuclear scintigraphic examination of the thorax and abdomen may be helpful. Skin biopsies may reveal evidence of vasculitis.
Treatment
If the primary cause of the condition can be identified and successfully treated, then the bony lesions will resolve spontaneously. The new bone becomes progressively more radiopaque and corticalized and gradually models to restore a more normal contour. Occasionally lesions have resolved spontaneously after treatment with phenylbutazone.
Osteitis or Osteomyelitis
Infectious osteitis or osteomyelitis occurs commonly in the metacarpal region because of the relative lack of soft tissue coverage of the bones and is usually a sequel to known trauma, with or without an open wound.
Clinical Signs
There is localized soft tissue swelling and mild to moderate lameness, and usually a draining tract is apparent.
Diagnosis
Ultrasonographic evaluation reveals an anechogenic region adjacent to the bone in the acute stage, as well as the accumulation of pus, before radiological changes are evident. Radiological abnormalities may include a radiolucent region within the cortex of the bone, periosteal new bone, and a sequestrum and involucrum in horses with advanced infection (Figure 37-14).

Fig. 37-14 Dorsolateral-palmaromedial oblique image of the metacarpal region. A radiolucent zone (an involucrum) surrounds a separate radiopaque fragment within the fourth metacarpal bone (a sequestrum). Periosteal new bone appears on the diaphysis of the fourth metacarpal bone, through which is a lucent canal (a cloaca).
Use of Boots and Bandages to Prevent Injury
The use of stable bandages, protective boots and bandages for exercise, and proprietary clays and cooling agents after exercise is common among horse owners in their efforts to protect horses from injury and to help to manage preexisting injuries. Bandages that are applied too tightly have tremendous potential to cause local damage, not only to the underlying skin on the dorsal and palmar aspects of the metacarpal region but also to the underlying tendons. The midmetacarpal region appears to be particularly vulnerable. Transient (a few hours’) application of an overly tight bandage results in a “bandage bow,” localized subcutaneous edema overlying the SDFT. More prolonged application of a bandage that is too tight results in hair loss and skin necrosis. Hair that regrows is white. Excessive sustained pressure causes tendon necrosis.
Persistent bandaging at appropriate pressures does not cause damage but leaves permanent rings in the hair; if these rings are visible at a prepurchase examination, they should alert the veterinarian that the horse usually stands in bandages. Properly applied stable bandages can be used to control filled legs and in horses prone to distention of the fetlock joint capsule or the DFTS.
The use of bandages or boots during exercise is somewhat controversial. A properly applied bandage should aim to permit a normal range of motion but protect against movement in an abnormal range.41-48 Little evidence exists that a bandage applied circumferentially around the limb reduces loads on the digital flexor tendons and thereby reduces the risk of overstretch injury. Studies on cadaver models have shown that distal limb bandages may increase the amount of energy a limb can absorb during repeated loading.41,42 Strain on the proximal aspect of the SL may be decreased in a standing or walking horse.43 In exercising horses, fetlock extension was reduced.40 However, shock attenuation was unaffected.41 The effectiveness of stabilizing support bandages in people decreases rapidly with exercise, and restriction in motion may have an adverse effect on performance in healthy athletes. Athletic taping of the fetlock of horses exercised at the trot had no effect on SDFT or SL strains; fetlock extension during stance was not affected, but there was a decrease in peak vertical force measured using a force plate.46 In exercising horses the core temperature within the SDFT increases substantially, and although the role of temperature in tendon injury remains uncertain, bandaging has the potential to promote heating. The effects of a gamgee bandage, a neoprene boot, a three-layered bandage, and a Dalmar tendon support boot (Dalmar Ireland Ltd., Glanmire, Ireland) on fetlock extension were compared in an in vitro model. The Dalmar support boot reduced fetlock extension.47 Moreover, kinematic studies of fetlock extension at walk and trot comparing four different boot designs showed a small decrease (0.5-1.5 degrees) in fetlock extension at the trot with all boots compared to without boots, suggesting that this may reduce tension in the SL and SDFT. However, studies at the canter, gallop, and jumping have not been performed. Therefore little current rationale exists for use of bandages or boots to prevent tendon strain injuries.
Boots and bandages have the potential to attenuate forces from direct trauma to the limb, for example, as the result of a horse hitting a fixed fence. However, without reinforcement, none properly protects against strike injuries from the hindlimb of the same horse or from strike injuries from adjacent horses. Such strike injuries can result in severe tendon injuries. The introduction of a more resilient bulletproof type of material into part of a boot, or applied as a palmar reinforcement under a bandage, can provide some protection against these devastating injuries, but the effect of such rigid material on normal movement of the flexor tendons is not known.
