chapter 8 Overview of balance impairments: functional implications
After completing this chapter, the reader will be able to accomplish the following:
1. Identify the systems involved in balance, and understand the assessment and evaluation of component balance skills and balance during functional activity.
2. Provide examples of treatment plans and ideas based on specific balance dysfunctions to allow the therapist to implement focused intervention.
3. Participate in the development of goals and documentation systems with emphasis on the setting for service delivery and the effect of the current health care environment.
Theory
Balance is the ability to control the center of mass over the base of support within the limits of stability; balance results in the maintenance of stability and equilibrium. A person’s ability to maintain balance in any position depends on a complex integration of multiple systems. Many theories have been proposed to explain the ability to maintain balance. In the now outdated reflex or hierarchical model, balance was considered the interaction of reflexes and reactions, which are organized hierarchically, that result in the support of the body against gravity.22,32 In this model, balance deficits result from eliminating higher central nervous system control, resulting in the release of spinal and supraspinal reflexes. This model has declined in popularity in recent years because common opinion embraces the idea that the nervous system more likely is comprised of complex interactions of multiple systems rather than organized as a distinct hierarchy. See Chapter 4.
The systems or distributed control model introduced by Bernstein describes balance as a complex interaction of musculoskeletal and neural systems.50 The ability to maintain balance is specific to and modified around the constraints of the environment and task. Within this system a disruption of balance (or instability) results from a malfunction in or disruption of any one or more of the elements of the postural control system. Likewise, balance is maintained through the interaction of sensory organization and postural control systems. The information is combined and integrated in the central nervous system.
Sensory organization
According to the systems model, information from three sensory systems is used for maintaining balance. Information from the visual, vestibular, and somatosensory systems is critically important.
The visual system (see Chapter 16) provides information regarding vertical orientation and visual flow. Visual or optical flow information, which describes movement of an image on the retina, is important input that aids detection of personal and environmental movement. Information provided by the visual system can be ambiguous and must be compared with other sensory information to determine accuracy. For example, a person sitting in a stationary car next to another stationary car at a red light then may receive optical flow information that indicates the other car is moving backward. This information alone is not adequate for determining which vehicle is moving; it only reveals relative movement. The information must be compared with the other sensory information to determine which car has moved.
Somatosensory information is comprised of cutaneous and pressure receptors on the soles of the feet and of muscle and joint receptors. This information helps determine characteristics of and the relationship of the individual to the support surface. During most tasks, somatosensory information may be the most heavily relied on input in the adult population. Like visual input, somatosensory input can be ambiguous. For example, dorsiflexion at the ankle indicates that the body is displaced anteriorly over the base of support. However, when standing on an incline, this ankle position may coincide with midline posture. The individual must consider other senses to determine which position is accurate.
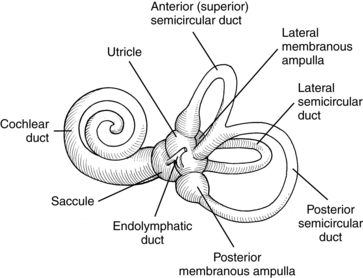
Information from the vestibular system helps determine head position and head motion in space relative to gravity. This information generally plays a minor role in balance control, unless somatosensory and visual inputs are inaccurate or unavailable. The vestibular system is the only sensory reference that is not ambiguous because it depends on gravity, which is consistent in the environment. The vestibular system (see Chapter 9) is composed of the otolith and semicircular canals. The semicircular canals sense angular acceleration, which is a change in velocity along a curved path (e.g., shaking or nodding the head). The canals are capable of detecting movement in all planes because all three are oriented in different planes (Fig. 8-1). Input from the semicircular canals influences postural responses and drives compensatory eye movements.
The otolith is composed of the utricle and saccule. Together they are responsible for determining changes in head position in the linear plane or translational movement of the head. Specifically, the utricle responds to head tilt and translations along the horizontal plane. In addition, the utricle appears to play an important role in producing small, torsional eye movements, which keep the eyes level when the head is tilted laterally. This helps with maintaining postural control and vertical orientation in space. The saccule appears to be instrumental in detecting vertical translations of the head.
In addition to these three systems, individuals’ internal representations or perceptions influence the interactions of information. Each individual possesses an internal perception related to the task, themselves, and the environment, which in turn influences sensory interactions and responses.
To use sensory information appropriately, each individual develops what is referred to as a sensory strategy. A sensory strategy is formulated when the central nervous system integrates, evaluates, and selects information received from the visual, somatosensory, and vestibular systems. The information is evaluated according to internal and external constraints, including availability of sensory information and the accuracy of environmental information. Information evaluation also may depend on the occurring movement strategy occurring. The development of a sensory strategy results in a sensory-motor interaction. The central nervous system determines the most efficient use of sensory input, which then allows for generation of appropriate motor output to complete the necessary task or reach a desired goal. This rapid process is not detectable when no deficits exist.
Postural control
An individual’s ability to maintain equilibrium depends not only on accurate evaluation and use of sensory information but also on the implementation of effective movement strategies. Movement strategies are stereotyped or synergistic patterns used to maintain the center of mass over the base of support; they are characterized as automatic, not reflexive or voluntary. Movement strategies occur too quickly to be under voluntary control but are too slow to be considered reflexive. Synergistic movement patterns are useful in that they reduce the degrees of freedom, thus decreasing the response time. Postural actions are reduced or absent when an individual uses an external support such as a cane or countertop to help maintain postural control. Automatic postural responses include ankle, hip, and stepping strategies.47
An ankle strategy is used to maintain the center of mass over the base of support when movement is centered on the ankles. Knee, hip, and trunk stability is necessary for this strategy to be effective. Ankle strategies are used to control small, slow swaying motions. They are effective when the surface area is firm and long in relation to foot length. Muscular activation while using the ankle strategy occurs in a distal to proximal sequence. Timing of muscular contractions is important to generate sufficient torque about the ankles and to maintain adequate stability at the hips, knees, and trunk. Ankle strategies frequently are used during “quiet” standing. For example, this strategy is effective in controlling the small, slow swaying motions that occur when a person stands in line (e.g., at a bank or grocery store).
Hip movement that maintains or restores equilibrium is a hip strategy. This strategy is most effective in maintaining stability when the support surface is short in relation to foot length or is compliant. Hip movement is used to control large or rapid swaying motions or when an ankle strategy is ineffective (i.e., unable to occur rapidly enough or generate adequate torque). Muscle activation while using hip strategies occurs in a proximal to distal sequence. This strategy is used more frequently than ankle strategies when the center of mass approaches the outer limits of the base of support and is more effective because of the ability to generate greater speed and range. An example of a situation in which persons would use a hip strategy would be a circumstance that requires them to stand on a narrow beam.
When ankle and hip strategies are or are perceived to be ineffective, the base of support is expanded in the direction of center of mass movement, resulting in the use of what is called a stepping strategy. In this case the person takes a step to widen the base of support. This is the strategy used effectively when taking each step while walking. The person shifts weight outside the existing base of support and takes a step to bring the base of support back under the center of mass (Fig. 8-2).
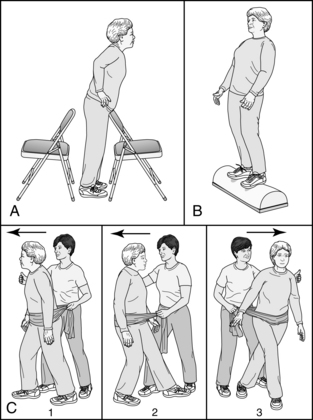
Figure 8-2 Automatic postural reactions: ankle, hip, and stepping strategies.
(From Cameron MH, Monroe LG: physical rehabilitation: evidence-based examination, evaluation, and intervention, St. Louis, 2007, Saunders.)
Each of the preceding movement strategies is a reactive response to center of mass movement. Anticipatory control is postural muscular activity that precedes and decreases center of mass movement. Previous experience weighs heavily in the determination of the appropriate sequence and degree of muscle activity required to maintain stability when anticipating a perturbation. Because anticipatory activities precede destabilization, misperceiving the needed amount of muscle activity may result in too much or too little correction. For example, when persons pull a door open, they initiate a posterior weight shift to counteract the weight of the door. If the weight of the door is lighter than anticipated, too much correction might occur and may result in a posterior perturbation of balance.
Central nervous system structures
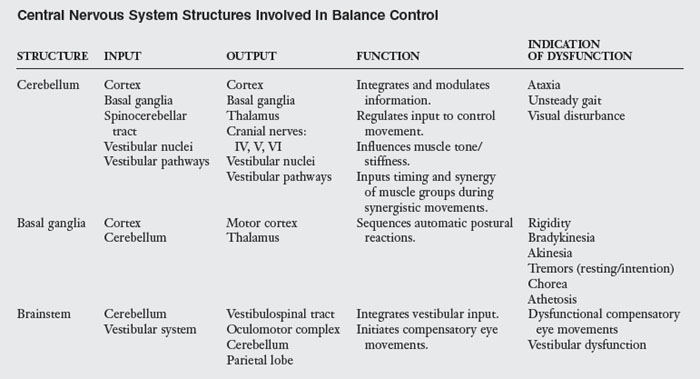
Maintaining equilibrium involves the precise integration of sensory information and the generation of appropriate and effective motor responses. Specific central nervous system structures are responsible for performing these complex tasks. The cerebellum is the primary integrating and modulating force in balance control. The cerebellum receives information from structures such as the cortex, basal ganglia, spinocerebellar tract, vestibular nuclei, and vestibular pathways. Input is modulated, interpreted, and sent out to the cortex; basal ganglia; thalamus; fourth, fifth, and sixth cranial nerves; vestibular nuclei and pathways; and indirectly to the spinal cord, providing the regulatory input needed to control movement. Damage to any one of these structures can result in difficulties with balance and postural control. Through this complex network of central nervous system interactions the cerebellum facilitates smooth coordination of movement. The cerebellum influences the timing and synergy of muscle groups during synergistic movements and muscle tone or stiffness. Symmetrical, appropriate, balanced skeletal muscle activity is necessary for maintaining postural alignment and is required for smooth, coordinated movements and stability. An example of a disorder involving the cerebellum is ataxia (poor coordination of agonist and antagonist muscles that results in jerky, poorly controlled movements). An individual with cerebellar dysfunction might have an unsteady gait or visual disturbances. See Chapter 15.
The basal ganglia are also involved in integrating information used for postural control and in a series of complex pathways, much of the exact nature of which is uncertain. The basal ganglia receive information from the cortex and cerebellum and then output information to the motor cortex via the thalamus. The basal ganglia work closely with the cerebellum and are believed to influence the sequencing of automatic postural reactions including the ankle, hip, and stepping strategies previously discussed. The continuous postural adjustments that play a role in smooth, coordinated movement are also controlled by the basal ganglia. Examples of disorders involving the basal ganglia include but are not limited to rigidity, bradykinesia (slowness of movement), akinesia, resting or intention tremors, chorea, and athetosis.
The brainstem also is involved in balance control because it houses the vestibular nuclei, which receive input from the cerebellum and the vestibular system. Information is output to the vestibulospinal tract, oculomotor complex, cerebellum, and parietal lobe. The brainstem is instrumental in the integration of the vestibular input and influences compensatory eye movements (Table 8-1).
Comprehensive evaluation
A comprehensive evaluation is crucial in helping the therapist understand specific balance problems patients may be experiencing. A comprehensive evaluation always should include a subjective client interview, an assessment of balance skills within the context of meaningful functional tasks, and an assessment of balance component skills. Evaluations may vary depending on the acuteness of the neurological insult, severity of the stroke, and setting in which care is provided (e.g., acute care, inpatient rehabilitation, skilled nursing facility/subacute unit, outpatient rehabilitation, or home health care).
Subjective interview
When conducting a subjective interview, the clinician must keep in mind that patients who have had an acute stroke may not be able to provide accurate information during the interview process due to cognitive and/or language impairments. Clinicians may need to use other sources of information, including family members, significant others, and information from the medical chart to supplement, clarify, or verify information a patient provides. Patients may improve in their ability to provide information as cognitive and language deficits improve. Patients often also demonstrate a greater awareness of their situation and surroundings as they improve and become more fully integrated into the home and community environments.
Subjective patient interviews allow patients to describe in their own words and from their own perception just how the stroke has affected their level of functioning. The interview should allow the therapist to obtain the following information about the patient:
The patient’s premorbid health history can have a significant impact on prognosis and thus appropriate goals. Having a thorough understanding of any premorbid conditions that could affect a patient’s balance functioning is important for the therapist. Examples include diabetic neuropathies, vision disturbances, vertigo, prior stroke or head injuries, prior lower extremity range of motion or strength problems, or other orthopedic issues such as lower back dysfunction.
As more details are added to this portion of the interview, the therapist will be better equipped to create an individualized treatment plan to meet the individual patient needs. The interview should include information such as the following:
 What time does the patient generally wake each morning?
What time does the patient generally wake each morning?
 Did the patient bathe at sponge level, shower level, or bathtub level? A sponge bath may indicate a prior history of balance issues that resulted in a fear of falling in the shower.
Did the patient bathe at sponge level, shower level, or bathtub level? A sponge bath may indicate a prior history of balance issues that resulted in a fear of falling in the shower.
 Did the patient need to take rest breaks or spread his or her basic activities of daily living out of a period of time? Again, this may indicate a premorbid issue with endurance related to balance.
Did the patient need to take rest breaks or spread his or her basic activities of daily living out of a period of time? Again, this may indicate a premorbid issue with endurance related to balance.
Outlining a schedule of a typical day at home may be helpful to the therapist in designing goals and a customized treatment plan. The therapist’s attendance to the specifics of performing tasks and to the order in which tasks occur is important for treatment planning and goal setting purposes.
The therapist must have a thorough understanding of the patient’s functional level before the stroke. This portion of the interview should include information such as the following:
 Whether the patient ambulated independently and what device if any was necessary for ambulation
Whether the patient ambulated independently and what device if any was necessary for ambulation
 Whether the patient required any assistance with performing daily tasks and, if so, what specific help did was required
Whether the patient required any assistance with performing daily tasks and, if so, what specific help did was required
 Whether the patient was able to function independently in the community (including specifics about activities) and whether any change in activity was experienced in the past six months. Attention should be focused on life roles the patient was engaged in (e.g., spouse, caregiver, parent, grandparent, etc.).
Whether the patient was able to function independently in the community (including specifics about activities) and whether any change in activity was experienced in the past six months. Attention should be focused on life roles the patient was engaged in (e.g., spouse, caregiver, parent, grandparent, etc.).
This area may be difficult for patients who have just had a stroke, but understanding what patients consider as problems resulting from balance deficits and what goal areas are relevant for the patient is important for the therapist to grasp. Early in the rehabilitation process, patients may cite self-care and mobility as problem areas. Later, when patients are receiving home health or outpatient services, they may no longer experience difficulty in these basic areas but may cite problems with household or community activities. This portion of the interview is important for determining patients’ awareness level about the way their balance deficit limits their participation in normal activities and for determining appropriate and meaningful goals.
Clinically, occupational therapists use a different approach to evaluation than other allied health professionals. After a complete review of the medical chart and a subjective interview, occupational therapists would next assess functional activities that are meaningful and relative to a specific patient based on the patient’s perception, the life roles a patient engages in and the specific functional goals important to the patient. Following assessment of functional activity, the occupational therapist would then complete a full assessment of component skills necessary to complete these activities. This process is more fully discussed later in this chapter. However, for the purposes of this chapter, the reader will first be introduced to the various component areas that should be assessed and that are specifically related to balance. A therapist must have a comprehensive understanding of the component skills that contribute to typical balance in order to effectively engage in skilled clinical observation during assessment of functional activity.
Component assessment
Component assessment focuses on numerous isolated skills and processes that contribute to balance. Thorough range of motion testing of active and passive range of motion, particularly of the trunk and lower extremities, must be completed and helps determine whether a patient has any biomechanical constraints that might have an effect on postural control. The therapist must evaluate the patient’s strength and appropriate patterns of skeletal muscle activity, particularly of the lower extremities and trunk, to determine neuromotor influences on postural control. The therapist also must examine the sensory systems that play a role in maintaining equilibrium. One such system is the visual system (see Chapter 16) and includes visual acuity and oculomotor function assessments. Oculomotor function includes eye movements such as voluntary movements, smooth pursuits, saccadic eye movements, and gaze stabilization. Assessment of sensation, particularly of the lower extremities, is also critical and should include light touch, deep pressure, proprioception, and kinesthesia assessments. Assessment should focus on both the ability for the patient to interpret the sensory stimulation and the ability for the brain to organize and use the sensory information available. The vestibular system is a third system that should be fully assessed. The function of the vestibular system is to provide information about head position and head motion in space relative to gravity. The vestibular system is difficult to evaluate in isolation but is discussed more fully within the context of sensory organization. The reader is also referred to Chapter 9 for a more in-depth review of vestibular assessment and rehabilitation.
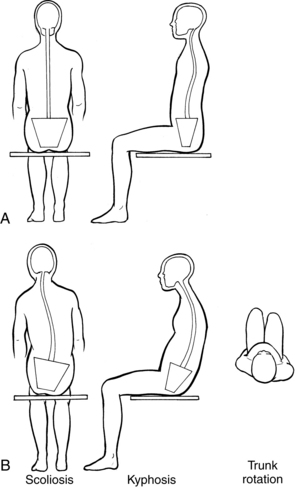
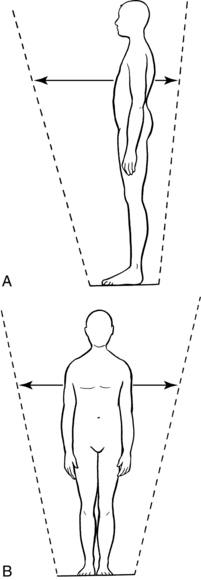
As an occupational therapist, the clinician must examine more complex tasks that integrate the specific balance components. The therapist should evaluate patients’ postural alignment while they are seated and standing. Skilled observation while a patient is engaged in functional activity is critical in performing these and subsequent assessments. Symmetrical alignment and appropriate positioning of body parts over the base of support are the goals. The therapist should note any asymmetry in alignment or bias over the base of support. In general, the posture for static standing or the “starting or ready position” should be symmetrical; the head should be in midline, centered over the shoulders; the shoulders should be centered and aligned over the pelvis; under “normal” conditions, the feet should be approximately hip distance apart; and the pelvis should be centered over the base of support created by the feet (Figs. 8-3 and 8-4). Postural alignment and symmetry is directly related to what specific activity a patient is engaged in as well. This means as a patient begins to move and engage in functional activity, the alignment and symmetry will change to allow the patient to complete the activity. For example, the postural alignment and symmetry needed to unload a dishwasher and put dishes away in an overhead cabinet is different than if the patient is vacuuming the living room rug. Skilled observation requires the therapist to have a solid understanding of both activity analysis and postural alignment and symmetry relative to that activity.
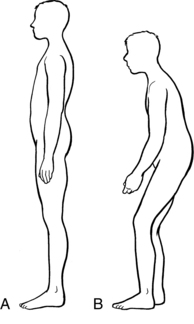
Figure 8-4 A, Correct alignment during standing. B, Flexed posture.
(Note hip/knee flexion, kyphosis, forward head posture, and change in center of gravity.)
Each individual also possesses an area about which the center of mass may be moved over any given base of support without disrupting equilibrium. This is referred to as the limits of stability. Assessment of patients’ ability to move within their limits of stability and noting the symmetry and extent of those limits is necessary. Because of the biomechanical constraints of the foot and ankle, the limits are greatest in the anterior/posterior direction and smaller in the lateral direction. The greatest degree of movement usually occurs anteriorly. The area created by the limits of stability is in the form of an ellipse (Fig. 8-5). Therapists need to assess both actual and perceived limits of stability. Actual limits of stability are the true ellipse that a patient can achieve relative to foot length and available motor control. Perceived limits of stability are the ellipse a patient perceives he or she can move; patients may underestimate or overestimate this area. If patients underestimate the limit, usually due to fear of falling, it results in an inability to weight shift normally to complete the activity. If the patient overestimates this area, usually due to sensory or perceptual deficits, it results in a fall.
The limits of stability may be measured in a number of ways. An experienced evaluator with a strong understanding of typical limits of stability might ask patients to shift their weight as far as they can in all directions and then observe and note the patients’ ability to move over their base of support. The therapist also may ask patients to perform a task that requires the center of mass to move over the base of support while observing their performance. Several computerized pressure plate systems on the market are able to compute an individual’s “normal” limits of stability based on height by force plate analysis. The therapist then can compare normal and actual figures. These pieces of equipment are costly and are not available in all clinics. It is crucial that therapists determine if the patient is actually shifting the center of mass over the base of support or substituting abnormal movement patterns, such as bending at the hips or shifting at the shoulders, in an attempt to accomplish the task.
Postural control system
Information regarding biomechanical and neuromuscular parameters available to the patient has been established through the comprehensive component evaluation. Integration and the effectiveness of these capabilities in the central nervous system are tested by assessing automatic postural responses; patients must be exposed to conditions that normally would elicit particular responses.
Ankle strategies are most effective when used with a firm support surface that is long in relation to foot length. They are used to control small, slow swaying motions. For an initial assessment, the patient should be standing on a firm surface with the feet approximately hip distance apart. The therapist should note oscillations about the ankles. If the patient is able to perform this task effectively, increasing the demands of the task by narrowing the base of support may be necessary. The therapist may ask patients to place their feet together to decrease the size of the base of support, narrow the limits of stability, and increase the need to control center of mass oscillations. The therapist should note increased use of ankle strategies, and if swaying increases in speed or magnitude, the patient may initiate a hip strategy.47 Individuals should be able to maintain their balance in this position with an ankle strategy and perhaps with minimal use of a hip strategy. Not using ankle strategies or using stepping strategies in this position indicates a disturbance in the ability to generate automatic postural responses.
Several methods exist for assessing hip strategies. Hip strategies are most effective when used with a support surface that is short in relation to foot length, the support surface is compliant, or ankle strategies are (or are perceived to be) ineffective. Simulation of each of these conditions should result in the use of a hip strategy. For higher level patients, the therapist may ask the patient to stand on a 4-inch balance beam so that only the middle of the foot receives support. Ankle strategies are ineffective under these circumstances because adequate torque cannot be produced around the ankle when the support surface is this short. The therapist should note use of primarily anterior/posterior hip strategies. Attempts to use ankle strategies only or any use of stepping strategies indicates a dysfunction in the ability to generate an appropriate hip strategy. Compliant support surfaces also result in use of hip strategies in “normal” subjects. The therapist can simulate this condition by having the patient stand on a 4-inch-thick piece of medium-density foam. Adequate torque around the ankles is not possible under this condition, and the patient uses hip strategies in all planes/directions. As stated previously, excessive attempts to use ankle strategies or exclusive use of stepping strategies indicates dysfunction.
The therapist may assess lateral hip strategies by having the patient assume a tandem stance (a heel-toe position in which one foot is directly in front of the other). This position significantly narrows the lateral limits of the base of support; because ankle strategies have a limited lateral range of effectiveness, the patient uses hip strategies. This position on a firm support surface would not be challenging enough to elicit hip strategy use in some patients. These patients could perform the same task on a 4-inch balance beam to further narrow the base of support.
When one assesses use of hip strategies in any of these conditions, observation of strategy sequence is important. The therapist also should note the effectiveness of the target strategy. Use of ineffective strategies (i.e., loss of balance) indicates that a particular strategy has failed.
The therapist may elicit use of the stepping strategy47 by further challenging the postural control system (e.g., by combining all of the previous test conditions). For example, the therapist may ask patients to stand with feet together or in tandem on a compliant surface. A delay in or lack of a stepping strategy that results in a loss of balance indicates dysfunction. (See Fig. 8-2.)
Sensory organization
In addition to automatic postural response assessments, assessments of sensory organizational abilities are also important. In other words, therapists must assess patients’ abilities to organize and evaluate the orientationally correct sense used to generate appropriate responses. Six test conditions are considered acceptable for thoroughly assessing sensory organization. Computerized tests of sensory organization are available commercially and often are combined with force plates that can measure motor responses to test conditions (to a degree). The sensory organization portion of the apparatus usually consists of a safety harness, movable foot plate, and a movable visual screen that surrounds the subject. Test conditions also have been simulated in the clinic by using 4-inch medium-density foam as a compliant surface, and a visual “dome” that encompasses the patient’s visual field and is worn on the head.48
The first condition for testing sensory organization allows subjects to receive accurate input from all sensory systems. Patients stand on a firm support surface with their eyes open, and the therapist records responses.
During the second condition, the therapist asks patients to close their eyes, which deprives them of visual input. Therefore, only somatosensory and vestibular inputs are available to help patients maintain equilibrium. Under this test condition, patients may have a postural response if conflicting information is received from the available sources or the individual is accustomed to relying heavily on visual input.
In the third test condition, patients wear the visual screen or dome and thus receive conflicting visual information. The screen or dome is “sway referenced,” which means that it moves along with the individual’s naturally occurring sway and provides the visual system with the illusion that no sway is occurring: optical flow input indicates that the environment and the individual are stationary. In this test condition, the support surface is firm and fixed, so somatosensory and vestibular information is accurate; although visual information is available, it is inaccurate. The patient must check and evaluate incoming sensory information and use only the accurate information. Too heavy a reliance on visual input might result in increased sway caused by delayed identification of the need to adjust to spontaneous sway.
The fourth condition uses a sway-referenced support surface; the support surface is sway referenced to naturally occurring sway. The therapist also may use the 4-inch foam to provide inaccurate somatosensory information. Under these circumstances, visual and vestibular information are accurate, and somatosensory information is available but inaccurate. Once again, an inappropriate postural response indicates an inability to use accurate information or identify and censor inaccurate somatosensory information.
The fifth and sixth test conditions are the most complex and require patients to use vestibular information. During the fifth test condition, patients must close their eyes, which deprive them of visual information. The support surface is sway referenced or foam is used, thus the only accurate information that helps maintain postural control is vestibular. Difficulty maintaining balance may result from a disturbance in the vestibular system or ability to integrate the information.
The sixth test condition uses sway-referenced visual and somatosensory information; vestibular information is the only accurate input. Disruption of the postural control may result because of the inability to evaluate the information (a more difficult process because two systems are providing inaccurate information) or a disruption of the central or peripheral vestibular system48 (Fig. 8-6).
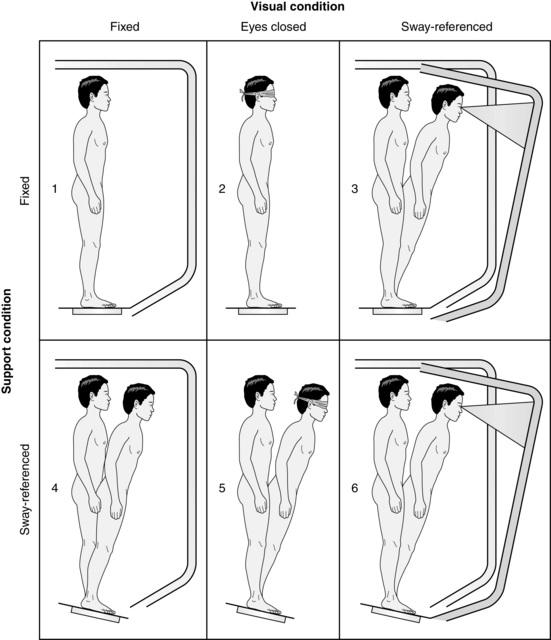
Figure 8-6 Test of sensory organization.
(From Cameron MH, Monroe LG: Physical rehabilitation: evidence-based examination, evaluation, and intervention, St. Louis, 2007, Saunders.)
This hierarchy of test conditions (Table 8-2) allows therapists to assess the ability of the central nervous system to integrate information appropriately. The hierarchy is also a method for determining whether a person is relying too heavily on a particular source of information. These tests also can provide preliminary information about vestibular system function and may indicate a need for further testing.
Table 8-2 Test of Sensory Organization
| TEST CONDITION | ACCURATE SENSORY INFORMATION | INACCURATE OR ABSENT SENSORY INFORMATION |
|---|---|---|
| 1 | Visual, vestibular, somatosensory | |
| 2 | Somatosensory, vestibular | Absent vision |
| 3 | Somatosensory, vestibular | Inaccurate vision |
| 4 | Visual, vestibular | Inaccurate somatosensory |
| 5 | Vestibular | Absent vision, inaccurate somatosensory |
| 6 | Vestibular | Inaccurate vision, inaccurate somatosensory |
Balance assessments
In addition to those mentioned, numerous other functional balance assessments have been developed.21,24,34,47 A large body of evidenced based research is available for many of these assessments. Discussed next is a brief overview of the more commonly used standardized or formal assessments used with either the stroke population or the neuro population in general. It is at times difficult to balance the restricted amount of time clinicians have with their patients with the need to use more standardized and formal assessments tools to assist with such things as predicting length of stay, establishing appropriate treatment plans and long term goals, justification of skilled intervention, recommendations for adaptive equipment, risk of falls, and discharge planning. Each venue of care and each provider of service must weigh and decide for themselves what tools are most useful and most efficient for their specific patient population. There is no one single assessment tool that clinicians can use to fully assess balance, and therefore clinicians should consider using a variety of tools.
The Berg Balance Scale4 is by far the most commonly used balance assessment. This assessment tool can assist with predicting fall risk, determining lengths of stays, and determining adaptive equipment and discharge planning recommendation.1,7,23,30,35,51,56,61 The test does not help the therapist in determining why patients might lose their balance and therefore is limited in its ability to assist with treatment planning. The test examines a number of factors, such as unsupported sitting and standing, transfers, reaching forward, picking objects up from the floor, turning 360 degrees, and standing on one foot, and each is graded on a 5-point scale. The assessment outlines the specific scoring criteria. This test examines many aspects of balance and has been shown to have high interrater reliability and validity in older adults.5,7,14,35,51 This test has been developed primarily for and used with the older population and stroke patients.3,14,51 The Berg can be time consuming, however. A new, shorter version of the Berg, referred to as the Berg Balance Scale 3P (7 item) Test, has been developed. Tasks in the shortened version include reaching forward with outstretched arm, standing with eyes closed, standing with one foot in front, turning to look behind, retrieving object from floor, standing on one foot, and sitting to standing. Available research suggests that this shortened version demonstrates similar psychometric properties as the original Berg Assessment.14,60
The Timed Up and GO (i.e., TUG) test is another common, highly used evaluation. The TUG has three subtests. The TUG Alone requires the patient to stand up from a chair with armrests, walk a short distance, turn around, return to the chair, and sit again.34 The TUG Cognitive requires the same activity while the patient counts backward from 20. The Tug Manual again requires the same basic activity while the patient carries a full glass of water. These three subtests have established cut-offs to assist the therapist in predicting likelihood of falls under different conditions and therefore can be useful in recommnendations.1,46 Performance is rated on a somewhat nonspecific 5-point scale. This test is used with the older adult population and, because of its varying rating criteria, the criteria should be evidence-based and consistent in use within a facility if used as an assessment tool.42
The Clinical Test of Sensory Organization and Balance,49 which was described previously, uses six test conditions to assess an individual’s ability to access, use, and organize sensory information. Within this formalized procedure, the therapist times the tests, measures the amount of sway, and records complete loss of balance falls. This test is also appropriate for use in children, patients with hemiplegia,19 and patients with vestibular disorders.15
This formalized assessment provides specific information to the therapist about why patients may lose their balance and is therefore is very useful in developing individualized treatment plans. This test can be time consuming, however (see Fig. 8-6).
The functional reach test21 requires the patient to stand next to a wall with a yardstick placed parallel to the floor. The patient is asked to reach as far forward as possible, and the reach length is measured. This test is quick and easy to perform and does not require expensive equipment. Test/retest and interrater reliability are high.21,51,62 The test has been used with a variety of populations spanning children through the elderly.20,21,62 The disadvantage of this examination is that it only measures one functional task and only assesses skills in the anterior direction.63
The Postural Assessment Scale for Stroke Patients (PASS)9,30,35 tests the ability for patients to maintain a given posture as well as to maintain equilibrium while changing positions. Specifically, this test is a 12-item test that looks at various postures and transitions of postures including lying, sitting, and standing, and uses a 0-3 rating scale. Research indicates that this test has high construct validity, high correlation with functional measures such as the Functional Independence Measure, high interrater reliability, and test-retest qualities. This test is most predictive in the first 30 days poststroke and takes approximately 10 minutes to administer. A short form of the PASS has been developed and tested, and it contains only five items and uses the 0-3 scale for scoring; initial research indicates that the short form may also demonstrate high interrater reliability and validity.13,60
The Activities Specific Balance Confidence Scale (ABCS)9,41,44,45 is a patient perception test that attempts to capture the patient’s view of his or her disability related to functional activities and perceived fall risk. It is a 16-item test that asks patients to score their perception of their risk of falling when engaging in a particular task. This test is best used in an outpatient or home health setting. Research suggests that perception of fall risk may be positively related to functional mobility and greater community reintegration.41,45 The Falls Efficiency Scale (FES) is also a confidence assessment scale used in much the same manner.40
The Brunnel Balance Assessment Scale (BBAS) is a scale that measures balance at three levels: sitting, standing, and stepping. The entire assessment scale can be administered at the same time, or it may be administered in sections. The advantage of this assessment is that it can be used repetitively as the patient progresses in mobility; because of this, the assessment easily lends itself to one that can be used across an entire continuum of care and across a wide range of patients with varying levels of mobility. Research suggests that this assessment tool demonstrates high reliability and validity and is a potentially useful predictive validity.55,57
The Motor Assessment Scale (MAS) is a relatively lengthy assessment (15 to 60 minutes depending on the patient’s participation) that focuses on supine to sidelying, supine to sitting edge of bed, sitting balance, sit to stand, walking, and effect of upper arm function, hand movements, and advanced hand movements on balance. It uses a 1- to 6-point scale. This assessment is reliable, valid, and sensitive to change over time.23,25,56 Disadvantages include the amount of time needed to administer the test, especially with more mobile patients and a more in-depth training needed for consistent therapist use. Advantages are similar to the Brunnel Balance Assessment Scale.
The assessment and treatment of balance disorders for recovering stroke patients are complex. Therapists need to understand the balance system and have a comprehensive way to assess balance function and dysfunction. They then determine realistic short- and long-term goals that are appropriate for each patient based on diagnostic and evaluation information. The therapist should devise a comprehensive treatment plan to improve specific balance deficits and ultimately assist the patient with transitioning to a more independent lifestyle.
Assessment of balance in relation to function
Occupational therapists should complete the initial assessment of function in relation to balance in the same way they assess all functional activities. A thorough understanding of typical movement and excellent observation skills are essential when assessing balance through functional activity. As with any skill therapists acquire, these abilities develop and improve as the therapists gain experience. Patients should attempt the activity, and therapists should determine whether patients can do the task, the quality of the performance, and whether patients are unsuccessful and why. Therapists may not have determined the specific balance deficits yet, but they can look for a pattern of dysfunction. Observations during functional activities should focus on when patients lose and do not lose their balance. Therapists should then determine what might be causing the loss of balance.
Specifically, therapists should observe what happens during functional activities when patients have to move their center of mass over their base of support, move their head, stand on uneven surfaces, function in lower lighting, move from one type of surface to another, or function on a narrower base of support. Therapists also should observe patients’ postural alignment, whether a bias in posture exists and in which direction that bias occurs, patients’ limits of stability, the width between their feet during functional tasks, and what patients do after losing their balance (e.g., use ankle, hip, or step strategy or no strategy at all). The initial contact with patients engaged in functional tasks should involve only observations (and guarding for safety). Therapists must allow patients to “fail” or lose their balance in a safe way, so that they can determine what patients do during functional tasks.
The specific functional tasks to be used during evaluation depends on what the patient’s goals are at the time of intervention and the setting in which treatment is being received. Stroke survivors may receive rehabilitation services in a number of settings. Inpatient settings would include acute care, acute inpatient rehabilitations settings, a skilled nursing facility or a subacute unit within a hospital or skilled nursing facility. Follow-up services may be received by home health therapists or in an outpatient rehabilitation setting. Often, patients will initially receive home health services and then transition to an outpatient center based on individual need and patient progress. Determination of where a patient receives services depends on many factors, including medical necessity, ability to tolerate at least three hours of therapy a day, discharge plan and availability for a 24-hour caregiver, availability of transportation, and health insurance policies.
As lengths of stays in all inpatient settings have dramatically shortened, as have the number of approved visits for outpatient and home health services, it is imperative for therapists to be aware of what the focus should be, based on the venue of care in which they work, the patients’ goals, and the discharge plan and situation. Acute and inpatient therapists usually focus on bathing and dressing; basic transfers including bed, toilet, and shower (if applicable); and basic home management tasks if the patient will be required to complete these tasks at discharge. Given that the average length of stay in acute care is three to five days and the average length of stay in an inpatient rehab setting is 14 days, patients rarely return home independent in these basic areas. This means that many outpatient or home health therapists may still need to focus on basic self-care and mobility tasks. As the patient progresses, outpatient and home health therapists may also have the opportunity to address home management tasks such as meal preparation, cleaning, and doing laundry, and community tasks such as grocery shopping, banking, going to church, using public transportation, and participating in leisure activities. See Chapters 3 and 21. Patients receiving services in a skilled nursing facility may be eligible to receive up to a 100 days of therapy services; given this, the focus of treatment for therapists and patients in this setting would begin with basic self-care and mobility and, as the patient progresses, graduate to addressing home management tasks and community reentry activities as appropriate.
After therapists have had an opportunity to observe patients during functional activities, they should begin to develop hypotheses about the reasons patients are losing their balance during various activities. The component evaluation and the diagnostic information can assist therapists in determining whether their hypotheses are substantiated. For example, patients may lose their balance when attempting to put on their pants while standing. Therapists may hypothesize that the loss of balance results from a poor ability to shift weight accurately, poor postural alignment when attempting to shift weight, and a lack of lateral hip strategy used when standing on one leg. These hypotheses can be supported by testing patients’ limits of stability, evaluation of their postural alignment, and assessment of whether they are using an available hip strategy. These steps allow therapists to develop individualized treatment plans and set realistic short- and long-term goals for each patient.
Therapists must keep in mind that they do not treat balance deficits separately from other deficits a stroke survivor may have. The treatment of balance dysfunction obviously is affected by any existing cognitive, visual perceptual, motor, or sensory deficits, such as memory deficits or a left neglect. For example, patients with cognitive deficits undoubtedly benefit more from a treatment program that incorporates familiar, repetitive functional tasks rather than an exercise program with activities that are meaningless to them. Therapists should incorporate multiple goals into each treatment session.
Because of current, ongoing changes in health care reimbursement, therapists’ collaboration with patients to focus treatment around goals that enable discharge home, often with family supports, is crucial. This approach allows patients to transition as quickly as possible to less restrictive environments. Failure to focus on goals may result in patients being discharged to more restrictive environments that allow less independent lifestyles (e.g., to a nursing home instead of home or an assisted living arrangement). Therapists should also focus on treating specific balance deficits to develop an individualized treatment plan that will assist patients with becoming independent as soon as possible. The balance between remediation versus compensation will be influenced by many factors, including patient prognosis for recovery, the discharge environment (physical environment and the availability of a caregiver), and the period in which a therapist is given to work with a patient.
Establishing goals and treatment plans
Setting goals for patients with balance disorders can be difficult. Therapists must have a thorough understanding of patients’ specific neuropathological condition. Although a complete neuroanatomy review is beyond the scope of this chapter, appropriate resources are listed in the references. Several factors contribute to whether patients receive a positive or poor prognosis and may include size and location of the lesion and any secondary factors that have developed, such as extensions of the original stroke, brain edema, and anoxia. The clinical presentation of the patient following a stroke will also affect the ability for patients to make realistic progress; for example, a patient with a pure motor stroke would likely have a better prognosis for recovery than a patient who also has sensory and cognitive impairments. Typically, the more skill areas influenced, the poorer the prognosis. Age and prior lifestyle of the patient may also affect prognosis. The previous medical history must also be considered for determining eventual functional outcomes. Factors to consider include any prior stroke, a history of alcohol use, any head trauma, diabetic neuropathies, age-related changes (such as the loss of inner ear hairs), orthopedic issues and balance problems (such as vertigo). Prior problems may interfere with a patient’s ability to compensate for the new neurological insult.
Ideally, a treatment team consists of an otolaryngologist or neurologist, a physical therapist, an occupational therapist, the patient, and the patient’s family (if applicable). The occupational therapist is not responsible for prognosticating, but to set realistic goals and an appropriate treatment plan, the therapist must have input from the otolaryngologist or neurologist concerning prognosis. If therapists are not fortunate enough to work directly with an otolaryngologist, they should contact the neurologist treating the patient for the stroke. Occupational therapists also must work closely with physical therapists to ensure that the treatment plans of both disciplines support and reinforce each other rather than work against or duplicate each other.
After receiving the prognosis, the therapist must decide whether to design a treatment plan that focuses on remediation, compensation, or both. The plan may be affected greatly by the setting in which the therapist provides treatment, the amount of time a therapist has to work with a patient, and, if it is inpatient setting, the discharge plan. If the prognosis indicates considerable improvement within two weeks, a therapist providing inpatient services may decide to emphasize remediation initially and then compensation just before discharge to ensure that the patient is functional in basic tasks. A therapist providing outpatient treatment for the same patient may focus solely on remediation because the patient already has established a safe way to function in the environment and is now focusing on improving balance deficits. If a patient has a poor prognosis for recovery of balance function, the inpatient therapist may emphasize compensation early in treatment to ensure functional success at discharge, especially if the support at home is an elderly spouse. A patient’s cognitive status also significantly affects when compensatory devices are introduced into treatment. A patient with memory loss requires more repetition and time to learn to use a walker while performing kitchen tasks than a patient without memory loss. Introducing devices and training the patient and his or her family or significant other in their use early in treatment is more likely to facilitate learning specific techniques.
Despite the decision therapists make regarding compensation versus remediation, therapists need to understand the implications of prescribing use of compensatory devices for patients with balance deficits. When a walker or cane is introduced into treatment before a patient is even given a chance to function without it, the therapist cannot accurately assess the patient’s ability to remediate the balance deficits. A walker or cane instantly increases the base of support and thus decreases the demand on the patient’s balance system to improve. It also greatly changes the way in which a patient moves during functional activities and alters normal movement. The patient no longer has to shift weight in a normal way. Instead, weight is shifted through the upper extremities during ambulation. Postural muscle activity has been shown to be altered even with light upper extremity support. See Chapter 15.
Therapists must make informed decisions about using equipment during treatment. They must take into consideration all of the factors discussed previously when choosing a treatment plan. Tub seats and reachers may be appropriate for patients with orthopedic limitations or who have a poor prognosis for recovery of balance function; however, introducing too many devices too early in treatment may in fact hinder recovery of balance function. For example, if patients are given tub benches or shower seats and are never given the opportunity to attempt to stand for brief periods in the shower, they may not be able to reach their full level of independence. This is not to suggest that devices should not be considered or recommended—numerous patients are able to function only because of their adaptive equipment and devices—it is only to suggest that when planning treatment, therapists should be aware of the implications of using each device. Therapists may consider training patients to use devices outside of therapy that provide greater independence but limit their use during actual therapy sessions. Patients then can maintain their independence while still working toward improving their balance. Therapists may help patients function more safely and become more active, even if they continue to use a device. Decisions regarding equipment, as with all treatment decisions, should be carefully thought-out relative to each individual patient. See Chapter 28.
Using functional activities and emphasizing functional outcomes always have been basic principles of occupational therapy, and they are now beginning to be embraced by many other disciplines. Hsieh and colleagues27 stated that using added-purpose occupation is motivating during performance. They added that numerous studies suggest that using meaningful tasks in treatment improves movement and performance.6,26,28,29,31,36-38,43,52,53,64,65 Traditional treatment of balance disorders has been focused on exercise with the hope and assumption that patients would carry over what they learned in exercise into daily function. Although occupational therapists always have centered treatment on functional activities, during the past few decades therapists may have treated daily activities as secondary in their attempt to integrate older neurophysiological treatment approaches. Currently available information supports the use of functional tasks as primary intervention tools (Boxes 8-1 and 8-2). The tasks specifically should address the balance component disturbances that have been identified during evaluation, so that occupational therapists can provide individualized and functional treatment.
Box 8-1 Sample Treatment Activities and Goals While in Standing Postures
 Static standing (no engagement in activity) graded by timed tolerance for the posture
Static standing (no engagement in activity) graded by timed tolerance for the posture
 Static standing while holding a glass of water
Static standing while holding a glass of water
 Standing while fastening shirt closures
Standing while fastening shirt closures
 Retrieving an object (graded by size and weight of object) from a shelf at chest level
Retrieving an object (graded by size and weight of object) from a shelf at chest level
 Retrieving an object from a shelf at knee level (graded by weight and size of object)
Retrieving an object from a shelf at knee level (graded by weight and size of object)
 Pulling up pants from ankles while standing
Pulling up pants from ankles while standing
 Setting table, including covering table with table cloth
Setting table, including covering table with table cloth
 Opening refrigerator and retrieving object from top shelf
Opening refrigerator and retrieving object from top shelf
 Opening refrigerator and retrieving object from bottom shelf
Opening refrigerator and retrieving object from bottom shelf
 Donning pajama pants while standing
Donning pajama pants while standing
 Picking up phone book from floor
Picking up phone book from floor
These treatment activities do not necessarily represent a progression of difficulty.
Box 8-2 Sample Treatment Activities and Goals for Ambulatory Patients
 Carrying empty shopping bag 30 feet (graded by distance and surface)
Carrying empty shopping bag 30 feet (graded by distance and surface)
 Carrying bag of groceries 30 feet (graded by weight, distance, and surface)
Carrying bag of groceries 30 feet (graded by weight, distance, and surface)
 Carrying a half-full glass of water 30 feet
Carrying a half-full glass of water 30 feet
 Carrying a full glass of water 30 feet
Carrying a full glass of water 30 feet
 Carrying a full cup on a saucer 30 feet
Carrying a full cup on a saucer 30 feet
These treatment activities do not necessarily represent a progression of difficulty.
Treating asymmetrical weight distribution
Patients who have had a stroke often have an impaired ability to control their center of mass over their base of support, both in sitting and standing. These patients often assume an asymmetrical posture during activities that require static and dynamical balance skills. Asymmetrical posture and poor upright stability have been correlated with an increased risk for falls.63 In addition, an unstable upright posture also has been correlated with diminished functional assessment on the Barthel index.33 Wu and colleagues63 indicated that one functional goal in rehabilitating persons with hemiplegia should be “to improve symmetrical characteristics of postural control.” The most common form of treatment for asymmetrical weight-bearing and poor postural control is using passive and active weight shifting. This treatment traditionally has been provided in the form of exercise or introduction of outside perturbations to encourage postural reactions. The underlying assumption is that practicing the repetition of postural adjustments will result in long-term improvements in balance during functional sitting balance, ambulation, and functional activities.18 Numerous authors have advocated the use of passive and active weight shifting as a viable treatment approach.8,10,11,59 If patients are not able actively to shift their weight, they initially may need guidance from the therapist and assistance with moving in effective patterns. Ultimately, patients also must be able to actively shift their weight. Active weight shifting requires postural adjustments that are intrinsic to the activity being performed.18 Patients must be able to initiate and execute a skilled weight shift that is an appropriate response to the perturbation actually experienced to maintain balance. Patients who experience difficulty with perceiving weight shifts and limits of stability may overestimate or underestimate the amount of weight shift required to adjust to the perturbation. Other patients may know a weight shift is needed, but may not be able to execute the coordinated motor movements and timing to make it effective.
Treatment for patients should focus on value-added occupations specific to individual patients. The therapist can use information gained during the patient interview to determine in which performance areas a patient is experiencing balance deficits (e.g., weight shifting in sitting to don socks, donning pants while standing or reaching into a lower cabinet during meal preparation) and which activities the patient values. Occupational therapists must perform task analyses to determine which weight shifts are required to complete the tasks patients want to perform. The therapist also should consider information from the component evaluation (e.g., poor ability to shift center of mass laterally and anteriorly when reaching up to a high cabinet in the kitchen) when making the treatment plan.
The Royal College of Physicians in their recommendations for stroke care have included information that skills gained within therapy should be integrated into daily life activities.58 Incorporating active weight shifting into a specific activity or using weight shifting that is inherent to successful completion of an activity allows patients to learn more normal postural responses to particular activities; therapists should not assume training has transferred from an exercise to an activity. Therapists also must be sure that the type of weight shifting they are asking patients to do is appropriate for particular tasks. Patients then are able to incorporate an anticipatory set based on the specific task, an important component of motor learning. It has been postulated that learning or relearning strategies that reduce simultaneous cognitive demands may be beneficial for stroke rehabilitation.39 Activities can be graded by the amount of weight shifting required, size of the base of support, and complexity of the task. Weight shifting can occur due to present anticipatory controls (e.g., shifting the center of gravity laterally to prepare to don pants while standing) or outside perturbations (e.g., getting on or off an escalator). Weight shifts also can occur in response to movement initiated by the upper extremities (e.g., putting a table cloth on a table). The therapist can make these activities more difficult by gradually increasing the force required by the upper extremities to perform the task (e.g., picking up an empty suitcase and then a full suitcase). Breaking down activities into a hierarchy of tasks ranging from simple to more complex is advisable, and treatment should involve selection of tasks based on patients’ abilities and their typical daily activities. For example, the task of making a bed requires numerous weight shifts but may not necessarily be an appropriate activity for a patient who did not make beds before the stroke.
Patients may be able to use a variety of feedback mechanisms to improve symmetrical postural alignment. Therapists can instruct them to use somatosensory information about pressure they receive through their feet while weight shifting (if sensation is intact). If patients have a lateral bias, the therapist needs to cue them. For example, a therapist can cue a patient with an anterior or posterior bias to locate foot pressure in relation to the balls of the feet. Caution should be used in attempting to use too much conscious cognitive control over these automatic responses; asserting cognitive effort has been shown to slow motor learning. The ultimate goal is to develop an automatic motor response absent of conscious control.
The therapist also may instruct patients to use visual information. Therapists may need to use a mirror for patients with a posterior bias so that the patients can see they are drifting away from the mirror. This method may be most appropriate when performing self-care tasks that normally involve the use of a mirror.
Treatment planning and sensory organization
As stated previously, the central nervous system uses information from the visual, vestibular, and somatosensory systems to maintain balance. Shumway-Cook and Horak49 stated that the central nervous system uses this feedback to monitor the relationship between the position of the body in space and the forces acting on it. The therapist must incorporate information obtained from all of the component balance assessments, including the test of sensory organization, into the treatment planning process. The therapist usually will be able to establish a correlation among functional observations, the component assessments, and the test for sensory organization. Occupational therapists are in a unique position and require astute critical thinking skills to compile the required information from all assessment procedures and to establish an appropriate treatment plan. Any particular patient following a stroke may present with a conglomerate of functional neuromotor deficits, cognitive impairments, and somatosensory organization difficulties. Careful consideration of the setting of treatment, length of stay, discharge plan, and family support should also be taken into account when planning treatment. Collaboration among other disciplines is critical to a successful treatment as well.
Inclusion of the manipulation of sensory information into treatment of stroke survivors has been shown to increase functional balance.2 Because of careful analysis of the results of the sensory organization test, the therapist should be able to identify functional tasks that place patients at risk for loss of balance; these activities can become part of the treatment plan (Table 8-3). Patients who lose their balance while transitioning from linoleum to carpet in their house usually perform poorly under testing conditions forcing them to maintain balance on uneven surfaces. Likewise, patients who lose their balance while walking in a mall or busy area with a great deal of peripheral movement usually perform poorly under the testing conditions forcing them to maintain their balance while receiving conflicting visual input. Therapists need to observe patients’ performances during component testing and functional tasks. Therapists also must determine possible compensations or strategies patients may use when one or more systems are impaired. Patients with somatosensory dysfunctions usually become visually-dependent, whereas patients with visual disturbances usually become dependent on surfaces. Patients with vestibular dysfunctions may become visually- or surface-dependent. These compensatory strategies can work for patients in isolated environments but prevent true independence and result in a higher risk for falls for patients who are active in the home and/or community. Patients often limit their participation in home activities or simply stop going out into the community to compensate for balance deficits, which results in social isolation or depression. The therapist can obtain this information from the initial patient interview.
Table 8-3 Correlation of Component Testing and Functional Activities
| SENSORY INFORMATION* | STRATEGIES | TASK |
| Absent hip strategy | Standing on carpet while opening a lower drawer with flexed hips and knees; walking outside on grass or beach and picking up object off ground; getting on or off escalator or moving sidewalk | |
| Excessive ankle/step strategies | Walking in mall; scanning items in kitchen cabinets; scanning items in grocery store; hanging clothes on line out of basket; rinsing shampoo out of hair while in shower with eyes closed and head tipped backward | |
| Delayed strategies | Getting up at night to go to bathroom (e.g., walking in low light down carpeted hallway and transitioning to linoleum in bathroom); walking in dark movie theater down incline while searching for seat | |
| None or delayed lateral hip strategies | Standing on one foot to don pants; standing in near tandem to reach up or down into cabinet; walking from one point to another; standing in near tandem to pick something up off of floor (e.g., cat’s dish) |
* Numbers refer to test conditions (see Table 8-2).
After determining which systems are impaired, therapists should identify activities that are both important to the patient and involve those systems. Those impaired systems can be challenged gradually by controlling the conditions in which the activities are performed. Surface-dependent patients may be more likely to lose their balance when transitioning from one surface to another in the home (e.g., from the kitchen linoleum to the living room carpet). Carrying an object from the kitchen into the living room may be a functional task that places patients at risk for loss of balance. Therapists can develop a treatment plan that initially requires patients to practice holding an item while standing on an uneven surface. The next step would be to have patients reach for an item while standing on an uneven surface. Patients would then carry an item as they transitioned from an uneven surface to an even surface and vice versa. These particular patients also would be at risk for loss of balance during other functional tasks that are required for community (beyond the household) ambulation. Sidewalks, gravel, grass, and sand are all uneven surfaces. The somatosensory information received from the feet of surface-dependent patients remains unchecked and may indicate to the central nervous system that the patients are falling. A balance reaction that is inappropriate to the task (e.g., walking on an uneven surface) but appropriate to the information the central nervous system is receiving and processing may result. Therapists first should have patients practice simple functional tasks on uneven surfaces and then increase the challenge by asking them to engage in more complex tasks while transitioning to and from uneven and even surfaces. The tasks should be meaningful to patients and related to their lifestyles.
Visually dependent patients often are at risk for loss of balance when their vision is obscured for any reason (e.g., when they are in the dark or poorly lit areas) or the central nervous system receives “false” visual information (e.g., peripheral images of persons walking past patients telling the central nervous system they are falling forward when they are not).
Patients may be at risk for losing their balance when getting up in the middle of the night to get a drink or go to the bathroom, walking in a movie theater, or taking a nighttime stroll outside if they are too reliant on their vision. Treatment plans can be developed that require patients to perform various activities in low lighting or with obscured vision. Common examples of this include closing the eyes in the shower while rinsing out shampoo, stepping from a brightly lit environment into a darker environment, and carrying a glass of liquid while walking (patients must keep their eyes on the glass rather than on the floor and the environment to make sure they do not spill the contents). Even walking while engaged in conversation can be difficult for visually-dependent patients because persons normally look at one another rather than the environment while talking.
Patients also may lose their balance during functional activities if they have difficulty with head-eye coordination and gaze stabilization. Activities such as walking in a busy mall, scanning the grocery store shelves for items, and placing groceries on various shelves can cause loss of balance. The central nervous system is unable to override the false visual information that results from these tasks, and thus the patients feel like they are losing their balance. Patients then institute postural reactions that are incongruent with the actual events that are occurring. Therapists can develop treatment plans that challenge patients’ ability to maintain gaze stability during functional activities requiring coordinated head-eye movements.
Patients with impaired vestibular function are generally visually- and surface-dependent, although they usually rely more heavily on one system. Patients with premorbid health issues may be more reliant on one system for a predetermined reason. For example, patients with diabetic neuropathies may be more visually dependent because they do not have access to somatosensory information through their lower extremities. Most traditional treatment approaches have relied on graded, repetitive head movements in the form of exercise to improve vestibular functions.12,17 Cohen and colleagues16 outline a treatment approach that incorporates this basic premise into functional activity. They stress that treatment activities must include head movements and positions that elicit the vestibular dysfunction during assessment. They also stress that activities must be interesting to patients; their use may assist patients with relating to real-life experiences. Suggested activities include retrieving towels in a basket on the floor and hanging them on an overhead clothesline, ambulating in the hallways while scanning and describing objects placed at various heights, playing badminton, and dribbling a basketball back and forth across the room. A thorough and accurate assessment of the specific impaired balance deficit is necessary to design the most efficacious treatment plan. See Chapter 9.
Throughout this process, careful consideration of safety and fall risks must also be considered, especially when treatment occurs in home care or on an outpatient basis. Thorough patient and family education outlining the reasons for particular difficulties and safety modifications to reduce the risk of falls while treatment is ongoing is essential. For example, a person living at home with unreliable somatosensory feedback and on overreliance on visual information may need to have night lights or hallway lights left on to ensure safe walking to the bathroom at night. See Chapter 14.
Retraining balance strategies
As discussed previously, part of the balance assessment is evaluating what patients do to regain their balance. Three strategies were outlined as normal balance strategies: ankle, hip, and step strategies. A component assessment allows therapists to determine whether a strategy is being used, the amount of delay in strategy use (and therefore its effectiveness), and whether the strategy is appropriate. Therapists must be able to complete skilled, accurate task analyses to determine which strategy should be used in particular activities. Therapists should see a correlation between functional activity observations and the results of component testing. This information can be used to determine which functional activities may place patients at risk for loss of balance. The identified activities then may become part of the treatment plan (see Table 8-3).
Because these strategies are automatic, the therapist should perform careful activity analysis in treatment planning in order for the treatment activities to elicit the appropriate response. Therapists can elicit ankle strategies by asking patients to engage in tasks requiring small weight shifts on solid support surfaces that are larger than their feet. For example, patients could reach up into a cabinet to put away groceries or put away laundry on a shelf in a closet. Therapists can extract hip strategies by asking patients to engage in tasks requiring larger weight shifts on narrow bases of support. These tasks could include playing toss and catch on a balance beam. Therapists also can acquire hip strategies by asking patients to reach into drawers or cabinets without locking their knees in extension; hip flexion is necessary to counteract the resulting anterior weight shift (Fig. 8-7). Therapists can attain step strategies by engaging patients in activities that require them to make weight shifts outside of their base of support, such as hitting a tennis ball against a wall or reaching out of their base of support to pick up work boots off the floor.
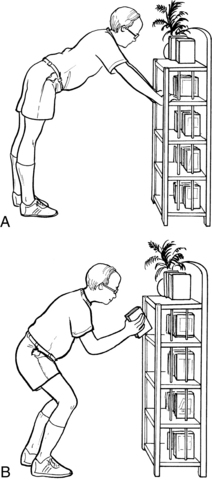
Figure 8-7 A, Knees are hyperextended and locked during functional activity, with weight shifted forward onto the upper extremities. Upper extremities are used as a base of support rather than for function. B, Hips and knees are flexed (as during hip strategy use) to allow center of mass to remain over lower extremity base of support. Upper extremities are free to be used for function.
Other factors affecting treatment planning
Therapists must consider other factors that may impair patients’ balance while functioning. A common factor often overlooked, especially early in the rehab process, is endurance. When patients are treated in an inpatient setting, they often are not asked to complete the entire task. For example, when bathing or dressing, the therapist unintentionally may “help” patients who are bathing or dressing by gathering their clothes or getting towels. Inpatient settings also often have large periods between therapy sessions when patients are not engaged in activity. Therefore, a day in an inpatient setting may ask the patient to participate in activity between one to four hours, but this may not accurately reflect patients’ daily home life related to the amount or timing of activity a patient engages in.
In an inpatient setting, patients usually have breakfast brought to them and often eat it in bed. They then may have a break before occupational therapists arrive to address self-care tasks. Patients then may have another break before physical therapists arrive to address gait activities. This type of schedule can result in an inaccurate picture of patients’ independence and clearly does consider whether patients’ endurance levels will affect their balance at home. Therapists need to devise a treatment plan that resembles the patients’ typical day at home as closely as possible.
Other factors that can influence a patient’s balance during functional activities are cognitive and visual perception impairments. Familiar, functionally based activities can help to reduce the effects of these impairments, but clearly occupational therapists must address these issues during treatment as well.
Medical factors such as fluctuating blood pressures, fluctuating blood sugar levels, infections, metabolic disturbances, and medications also can affect a patient’s balance skills. Any significant changes that therapists observe should be reported immediately to the physician. See Chapter 1.
Documentation
Accurate and thorough documentation should include a full written evaluation, including a detailed diagnosis at the impairment level, activity participation level, and life role level. It should also include a detailed clinical impression that links diagnosis, specific impairments, comorbidities, current level of function, and anticipated level of function relative to the discharge plan from a particular venue of care. The written evaluation should include a description of the treatment plan based on patient-specific impairments, short- and long-term goals, and patient outcomes, which must be functional and measurable. Because of the current climate of managed health care, documentation should be as streamlined as possible and easily understood by any person who accesses the information, including other team members, case managers, third-party payers, patients, and family members. The documentation format should span the continuum of care where possible and should be adjusted easily to meet the patient’s needs and for the setting in which intervention is being provided (e.g., acute care, inpatient rehabilitation, or outpatient clinic). Standardized and formal assessments and treatment interventions should be supported by evidenced-based research as much as possible. Uniformity and consistency of use of evaluation and documentation tools should be a priority if providing care within a continuum.
Documentation tools, if developed appropriately, can help structure thought processes and reinforce clinical reasoning skills in the areas of assessment, treatment planning, and the establishment of goals. The true “skill” of the therapist lies in the ability to assess, synthesize, and develop appropriate overall plans for a specific patient. The more specific the documentation requires the clinician to be, the more directed the treatment plan and goals will be. As length of stays become shorter, it becomes imperative for a documentation tool to function not only as a recording tool, but also as a guide to any therapist using the document, including the novice therapist or the student. Documentation should encompass and reflect information from standardized and formal assessments, functional status, specific impairment deficits, treatment, and goals. Documentation tools should be reliable, valid, sensitive, and specific. They should also reflect real-life situations.
Documentation tools should also easily and quickly convey progress to the reader. Often, the setting determines the frequency of intermittent assessment notes, but each visit or treatment session should be recorded, and evidence of progression should be demonstrated. In the event that a patient fails to progress, documentation should be able to clearly demonstrate why the patient is not progressing, and the intervening timely adjustments in treatment planning, goal setting, and discharge planning that are occurring in response to the lack of progress. Every setting is unique, so therapists should develop documentation formats that meet the needs of the patients served in each particular setting and ensure that documentation focuses on functional outcomes.
Summary
The assessment and treatment of balance disorders for recovering stroke patients are complex. Therapists need to understand the balance system and have a comprehensive way to assess balance function and dysfunction. They then determine realistic short- and long-term goals that are appropriate for each patient based on diagnostic and evaluation information. The therapist should devise a comprehensive treatment plan to improve specific balance deficits and ultimately assist the patient in transitioning to a more independent lifestyle.
CASE STUDY Improving Function Through Balance Retraining
M.J. is 58-year-old female who was diagnosed with a right middle cerebral artery stroke. She was assessed first by an inpatient rehabilitation occupational therapist who determined that the patient had difficulty controlling her balance during bathing, grooming, and dressing. The patient stated that she wanted to perform all of these activities independently. The therapist noted that M.J. had a postural bias to the right in both sitting and standing, used a wide base of support when standing during functional tasks, and was unable to control her center of gravity when shifting her leg to the left to complete a task. M.J. was able to support weight on her left lower extremity. Sensation was impaired but not absent in her left lower extremity. M.J.’s perceived limits of stability were not congruent with her actual limits of stability. She underestimated her ability to shift weight to the left and thus could not complete tasks that required her to shift weight to the left. When assisted with a left weight shift, M.J. was not able to control the shift because of poor coordination and timing of muscle activation. Because she lost control whenever she shifted weight to the left, M.J. compensated by maintaining an asymmetrical postural alignment. When asked to shift her weight actively to the left, M.J. altered her postural alignment by attempting to shift her shoulders rather than her center of mass.
Inpatient rehabilitation treatment initially centered on assisting M.J. in relearning appropriate motor responses in sitting. Activities that involved reaching and intrinsically incorporated weight shifts to the left were used. Activities of daily living were incorporated with facilitation of midline posture, and weight shifts during this functional task were used. She progressed to standing tasks and incorporating these same principles into standing tasks. The therapist selected parts of self-care tasks that did not require large weight shifts (e.g., combing her hair, washing her face, and selecting clothing from her closet) and focused on maintaining midline. The therapist helped M.J. learn to use visual and somatosensory information when possible to provide information about her position in space. M.J. was discharged home with continued needs in the areas of functional balance skills. Patient and family education focused on appropriate use of adaptive equipment, environmental modifications, and safety in the home.
Following discharge from acute rehabilitation, home care and outpatient therapy services continued. As M.J. improved her ability to achieve and maintain midline during additional static standing tasks, the therapist began to introduce tasks requiring a more significant weight shift from right to left (e.g., putting on her shirt while standing, reaching for objects on the sink, and getting objects out of the closet that were placed to elicit a left weight shift). Emphasis was placed on assisting M.J. with developing an awareness of her actual limits of stability. As M.J.’s control improved, the therapist also focused on narrowing her base of support to the more normal site dictated by particular activities. M.J. improved to the point that she could maintain midline and actively shift weight laterally during self-care activities without assistance from the therapist. Upon discharge from outpatient therapy, M.J. was provided with a comprehensive home program designed to continue to challenge and improve motor control involved in balance skills.
Review questions
1. Name the three sensory systems involved in balance control and describe their roles.
2. What purpose do automatic postural responses serve in balance control?
3. What is the role of the cerebellum in balance control?
4. What composes a component assessment of balance skills?
5. Describe three balance assessments.
6. Why should a therapist observe a patient during functional activity? What information should be gathered?
7. In what way does a therapist determine the focus of treatment (e.g., remediation or compensation)?
8. In what way does the treatment of balance deficits by occupational therapy differ from traditional physical therapy treatment?
1. Andersson AG, Kamwendo K, Siger A, et al. How to identify potential fallers in a stroke unit. a validity indexes of 4 test methods. J Rehabil Med. 2006:38;3:186-191.
2. Bayok JF, Boucher JP, Leroux A. Balance training following stroke. effects of task-oriented exercises with and without sensory input. Int J Rehabil Res. 2006:29;1:51-59.
3. Berg KO. Balance and its measure in the elderly. a review. Physiother Can. 1989:41;5:240.
4. Berg KO, Maki BE, Williams JI, et al. Clinical and laboratory measures of postural balance in the elderly population. Arch Phys Med Rehabil. 1992;73(11):1073-1080.
5. Berg KO, Wood-Dauphinee S, Williams J. The balance scale. reliability assessment with elderly residents and patients with an acute stroke. Scand J Rehabil Med. 1995:27;1:27-36.
6. Block MW, Smith DA, Nelson DL. Heart rate, activity, duration and affect in added-purpose versus single-purpose jumping activities. Am J Occup Ther. 1989;43(1):25-30.
7. Blum L, Korner-Bitensky N. Usefulness of the berg balance scale in stroke rehabilitation. a systematic review. Phys Ther. 2008:88;5:559-566.
8. Bobath B. Adult hemiplegia. evaluation and treatment, ed 2. London: William Heinemann. 1978.
9. Botner EM, Miller WC, Eng JJ. Measurement properties of the Activities-specific Balance Confidence Scale among individuals with stroke. Disabil Rehabil. 2005;27(4):156-163.
10. Brunnstrom S. Movement therapy in hemiplegia. New York: Harper & Row; 1970.
11. Carr J, Shepherd R. Physiotherapy in disorders of the brain. Rockville, MD: Aspen; 1980.
12. Cawthorne T. The physiological basis for head exercises. Charter Soc Physiother. 1944;29:106.
13. Chien C, Lin J, Wang C, et al. Developing a short form of the postural assessment scale for people with stroke. Neurorehabil Neural Repair. 2007;21(1):81-90.
14. Chou C, Chien C, Hsueh I, et al. Developing a short form of the berg balance scale for people with stroke. Phys Ther. 2006;86(2):195-204.
15. Cohen H, Blatchly CA, Gombash LL. A study of the clinical test of sensory interaction and balance. Phys Ther. 1993;73(6):346-351.
16. Cohen H, Miller LV, Kane-Wineland M, et al. Vestibular rehabilitation with graded occupations. Am J Occup Ther. 1995;49(4):362-367.
17. Cooksey F. Physical medicine. Practitioner. 1945;155:300.
18. Daleiden S. Weight shifting as a treatment for balance deficits. a literature review. Physiother Can. 1990:42;2:81.
19. DiFabio RP, Badke MB. Extraneous movement associated with hemiplegic posture sway during dynamic goal-directed weight distribution. Arch Phys Med Rehabil. 1990;71(6):365-371.
20. Duncan PW, Studenski S, Chandler J, et al. Functional reach. predictive validity in a sample of elderly male veterans. J Gerontol. 1992:47;3:93-98.
21. Duncan PW, Weiner DK, Chandler J, et al. Functional reach. a new clinical measure of balance. J Gerontol. 1990:45;6:192-197.
22. Easton T. On the normal use of reflexes. Am Sci. 1972;60(5):591-599.
23. English CK, Hillier SL, Stiller K, et al. The sensitivity of three commonly used outcome measure to detect change amongst patients receiving inpatient rehabilitation following stroke. Clin Rehabil. 2006;20(1):52-55.
24. Fregly A, Graybiel A. An ataxia battery not requiring rails. Aerosp Med. 1968;39(3):277-282.
25. Gustavsen M, Aamodt G, Mengshoel AM. Measuring balance in subacute stroke rehabilitation. Adv Physiother. 2006;8(1):15-22.
26. Heck S. The effect of purposeful activity on pain tolerance. Am J Occup Ther. 1988;42(9):577-581.
27. Hsieh C, Nelson DL, Smith DA, et al. A comparison of performance in added-purpose occupations and rote exercise for dynamic standing balance in persons with hemiplegia. Am J Occup Ther. 1996;50(1):10-16.
28. Kircher M. Motivation as a factor of perceived exertion in purposeful versus nonpurposeful activity. Am J Occup Ther. 1984;38(3):165.
29. Lang E, Nelson D, Bush M. Comparison of performance in materials-based occupation, imagery-based occupation, and rote exercise in nursing home residents. Am J Occup Ther. 1992;46(7):607.
30. Liaw L, Hsieh C, Lo S, et al. The relative and absolute reliability of two balance performance measures in chronic stroke patients. Disabil Rehabil. 2008;30(9):656-661.
31. Licht B, Nelson D. Adding meaning to a design copy task through representational stimuli. Am J Occup Ther. 1990;44(5):408.
32. Magnus R. Some results of studies in the physiology of posture. Lancet. 1926;2(5376):531.
33. Mahoney FI, Barthel DW. Functional evaluation. the Barthel index. Md State Med J. 1965;14:61.
34. Mathias S, Nayak USL, Isaacs B. Balance in the elderly patient. the “get up and go test. Arch Phys Med Rehabil. 1986:67;6:387.
35. Mao H, Hsueh I, Tang P, et al. Analysis and comparison of psychometric properties of three balance measures for stroke patients. Stroke. 2002;33(4):1022-1027.
36. Miller L, Nelson D. Dual-purpose activity vs. single-purpose activity in terms of duration on task, exertion level, and effect. Occup Ther Ment Health. 1987;7(1):55.
37. Morton GG, Barnett DW, Hale LS. A comparison of performance measures of an added-purpose task versus a single-purpose task for upper extremities. Am J Occup Ther. 1992;46(2):128-133.
38. Mullins C, Nelson D, Smith D. Exercise through dual-purpose activity in the institutionalized elderly. Phys Occup Ther Geriatr. 1987;5(3):29.
39. Orell AJ, Eves F, Masters R. Motor Learning of a dynamic balancing task after stroke implications for stroke rehabilitation. Physical Therapy. 2006;86(3):369-380.
40. Pal J, Hale LA, Skinner MA. Investigating the reliability and validity of two balance measures in adults with stroke. Int J Ther Rehabil. 2005;12(7):308-315.
41. Pang MY, Eng JJ, Miller WC. Determinants of satisfaction with community reintegration in older adults with chronic stroke. role of balance efficacy. Phys Ther. 2007:87;3:282-291.
42. Poole JL, Whitney SL. Can balance assessments predict falls in the elderly. Denver, CO: Presentation at the American Occupational Therapy Association Annual Meeting and Conference; April 9, 1995.
43. Riccia C, Nelson D, Bush M. Adding purpose to the repetitive exercise of elderly women through imagery. Am J Occup Ther. 1990;44(8):714.
44. Salbach NM, Mayo NE, Hanley JA, et al. Psychometric evaluation of the original and Canadian French version of the activities-specific balance confidence scale among people with stroke. Arch Phys Med Rehabil. 2006;87(12):1597-1604.
45. Salbach NM, Mayo NE, Robichaud-Ekstrand S, et al. Balance self-efficacy and its relevance to physical function and perceived health status after stroke. Arch Phys Med Rehabil. 2006;87(3):364-370.
46. Shumway-Cook A, Brower S, Woolacott M. Predicting the probability for falls in community-dwelling older adults using the timed up and go test. Physical Therapy. 2000:80;9:896-903.
47. Shumway-Cook A, Horak FB. Balance disorders assessment. NERA. 1992.
48. Shumway-Cook A, Horak FB. Balance rehabilitation in the neurological patient. NERA. 1992.
49. Shumway-Cook A, Horak FB. Assessing the influence of sensory interaction on balance. Phys Ther. 1986;66(10):1548-1550.
50. Shumway-Cook A, Olmscheld R. A systems analysis of postural dyscontrol in traumatically brain-injured patients. J Head Trauma Rehabil. 1990;5(4):51.
51. Smith PS, Hembree JA, Thompson ME. Berg balance scale and functional reach. determining the best clinical tool for individuals post acute stroke. Clin Rehabil. 2004:18;7:811-818.
52. Steinbeck TM. Purposeful activity and performance. Am J Occup Ther. 1986;40(8):529-534.
53. Thibodeaux CS, Ludwig FM. Intrinsic motivation in product-oriented and non-product-oriented activities. Am J Occup Ther. 1988;42(3):169-175.
54. Tinetti ME. Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc. 1986;34(2):119-126.
55. Tyson SF, DeSouza LH. Development of the Brunel Balance Assessment. a new measure of balance disability post stroke. Clin Rehabil. 2004:18;7:801-810.
56. Tyson SF, DeSouza LH. Reliability and validity of functional balance tests post stroke. Clin Rehabil. 2004;18(8):916-923.
57. Tyson SF, Hanley M, Chillala J, et al. The relationship between balance, disability, and recovery after stroke. predictive validity of the Brunel Balance Assessment. Neurorehabil Neural Repair. 2007:21;4:341-346.
58. Tyson S, Selley A. A content analysis of physiotherapy for postural control in people with stroke an observational study. Disabil Rehabil. 2006;28;13–14:865-872.
59. Voss D. Proprioceptive neuromuscular facilitation. Am J Phys Med. 1985;46:838.
60. Wang C, Hsueh I, Sheu C, et al. Psychometric properties of 2 simplified 3-level balance scales used for patients with stroke. Phys Ther. 2004;84(5):430-438.
61. Wee JY, Wong H, Palepu A. Validation of the berg balance scale as a predictor of length of stay and discharge destination after stoke rehabilitation. Arch Phys Med Rehabil. 2003;84(5):731-735.
62. Weiner DK, Duncan PW, Chandler J, et al. Functional reach. a marker of physical frailty. J Am Geriatr Soc. 1992:40;3:203-207.
63. Wu S, Huang HT, Lin CF, et al. Effects of a program on symmetrical posture in patients with hemiplegia. a single-subject design. Am J Occup Ther. 1996:50;1:17-23.
64. Yoder RM, Nelson DL, Smith DA. Added-purpose versus rote exercise in female nursing home residents. Am J Occup Ther. 1989;43(9):581-586.
65. Yuen H. The purposeful use of an object in the development of skill with a prosthesis, master’s thesis. Kalamazoo, MI: Western Michigan University; 1988.