Respiratory disorders
cough, respiratory stimulants, cystic fibrosis and neonatal respiratory distress syndrome
Cough
Cough is a protective mechanism that removes excessive mucus, abnormal substances such as fluid or pus, or inhaled foreign material from the upper airways. A cough is initiated by a rapid inspiration followed by brief closure of the glottis. Forced expiration against the closed glottis raises intrathoracic pressure, and sudden opening of the glottis expels air together with secretions and debris. Flow rates can approach the speed of sound, producing vibration of upper airway structures and the typical sound of cough. Cough is under both voluntary and involuntary control.
The cough reflex is initiated by irritant receptors located at the epithelial surface of the airway mucosa, which can be activated by either chemical or mechanical stimuli. These receptors have been identified at and below the oropharynx in the large airways, and are probably present in the external auditory canals and tympanic membrane in the ear, as well as in other sites such as the oesophagus and stomach. Rapidly adapting receptors that respond mainly to mechanical stimuli may be of primary importance in eliciting the cough reflex. Neuropeptides produced by the mechanosensitive neurons following viral infection or allergen challenge probably sensitise the cough reflex.
Afferent fibres from the receptors in the airways travel in the vagus and superior laryngeal nerves to the medullary ‘cough network’ in the region of the nucleus tractus solitarius. Neuronal pathways connect this network to the respiratory pattern generator, from where efferent fibres travel in somatic nerves to respiratory muscles. Projections from the cerebral cortex to the medulla can also initiate cough or modulate the cough reflex.
Several mediators are involved in the cough reflex pathways in the medulla. One proposed model is that the afferent input to the cough centre is via glutamatergic neurons that stimulate N-methyl-D-aspartate (NMDA) receptors. These neurons can be inhibited by presynaptic serotonergic nerve synapses via serotonin type 1 (5-hydroxytryptamine1, 5-HT1) receptors. Opioids facilitate the inhibitory action of the serotonergic neurons through further interneuronal connections. The complexity of these pathways is illustrated by the number of mediators and antagonists that can experimentally initiate or inhibit cough. Selective opioids such as κ- and δ-opioid receptor agonists, tachykinin receptor antagonists, bradykinin receptor antagonists and transient receptor potential vanilloid 1 (TRPV1) receptor antagonists all have potential as future antitussives.
Cough has several diverse causes (Box 13.1). A cough is considered useful if it aids clearing excess secretions or inhaled foreign matter from the airway. By contrast, an unproductive cough has no useful function. An effective cough that can clear the airway depends on the ability to generate high airflow. An ineffective cough may result from respiratory muscle weakness, or when the mucus on the airway wall is thick and adhesive.
There are three clinical categories of cough: acute cough, lasting less than 3 weeks, subacute cough lasting 3–8 weeks and chronic cough. Acute cough is most often caused by acute viral upper respiratory tract infection (the common cold), and most subacute cough also results from an initial viral infection. Chronic productive cough is usually related to smoking or bronchiectasis. The most common causes of a chronic non-productive cough in non-smokers are upper airway cough syndrome (also called post-nasal drip syndrome), asthma and gastro-oesophageal reflux disease. There is also an entity called unexplained cough, predominantly affecting middle-aged women and associated with cough reflex hypersensitivity, for which investigations fail to identify a cause.
Drugs for treatment of cough
Antitussives (cough suppressants)
Cough suppressants fall into three classes.
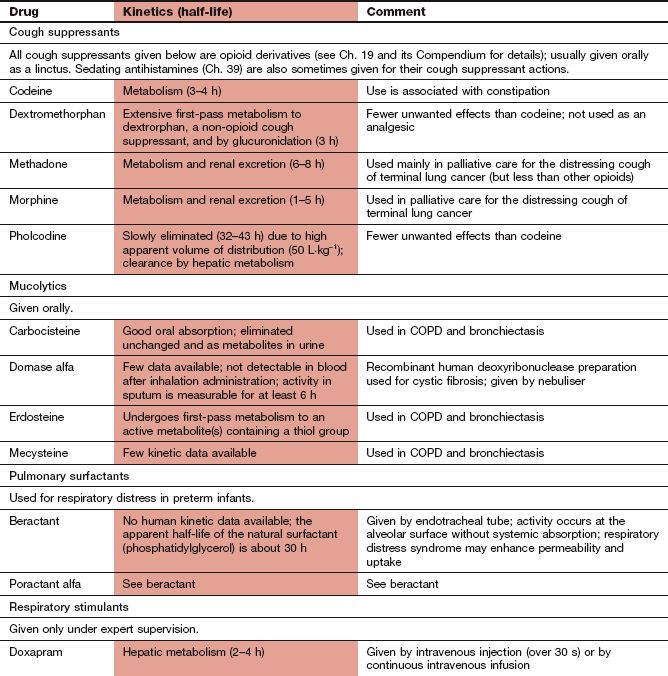
Centrally acting drugs (opioids): Opioids increase the threshold for stimulation of neurons in the medullary cough centre, and probably modulate a gating mechanism in the brain analogous to that identified for pain reception. They are most effective for cough arising from the lower airways. Weak opioid analgesics (Ch. 19) are most commonly used, especially codeine and pholcodine. These are less addictive than morphine, which should be reserved for terminal conditions. Dextromethorphan is structurally related to opioids, but is a glutamate NMDA receptor antagonist with antitussive properties and no analgesic or sedative action.
Peripherally acting drugs: Local anaesthetics such as lidocaine (Ch. 18) are used as an oropharyngeal spray to reduce cough during bronchoscopy. Antihistamines (Ch. 39) reduce post-nasal drip from allergic rhinitis, which can stimulate cough, but probably have little direct antitussive activity. Nevertheless, sedative antihistamines, such as diphenhydramine, are commonly used in compound cough preparations on sale direct to the public.
Expectorants and mucolytics
Expectorants such as guaifenesin and squill are often included in compound cough preparations, with the intention of improving clearance of mucus from the airways. There is no evidence that they have any clinical value.
Mucolytics such as mecysteine hydrochloride, erdosteine and carbocisteine can be given orally to reduce the viscosity of bronchial secretions by breaking disulphide crosslinking between molecules. Mucolytics can be useful in chronic obstructive pulmonary disease (Ch. 12) and bronchiectasis.
Management of cough
An acute cough should be treated only if it is unproductive or excessive. A self-limiting non-productive acute cough, such as that caused by a viral illness, can be suppressed by simple linctus or a weak opioid. Any cough of unknown origin that is still present after 14 days should be investigated further to identify an underlying cause.
For chronic cough, non-specific therapy has a limited role, since it should be possible to identify and treat the cause. Specific treatment for left ventricular failure, asthma, upper airway cough syndrome (with an antihistamine and a decongestant) or gastro-oesophageal reflux disease (Ch. 33) often eliminates the cough associated with those conditions.
Cough is a common unwanted effect of angiotensin-converting enzyme (ACE) inhibitors (Ch. 6) and occurs in up to 15% of people who take them. It sometimes appears hours after starting treatment, but can first arise after several months of treatment. The cough may improve with a reduction in ACE inhibitor dosage, but changing to another class of drug, such as an angiotensin II receptor antagonist, is usually necessary to eliminate the cough.
When symptomatic therapy is required for chronic cough, there are few options. Chronic non-productive cough in terminal lung cancer can be treated with a powerful opioid such as morphine. The value of mucolytics in chronic bronchitis is uncertain, but they may be useful in chronic obstructive pulmonary disease (Ch. 12). Mucolytics may make clearance of mucus easier, but are probably no more effective than hydration from inhaling steam or nebulised hypertonic saline. Mucolytics do not improve lung function in cystic fibrosis.
Respiratory stimulants (analeptic drugs)
Doxapram has a limited place in the short-term treatment of ventilatory failure, such as in hypercapnoeic respiratory failure due to chronic obstructive pulmonary disease which is causing drowsiness. It increases respiratory drive and arousal, and improves both rate and depth of ventilation. When combined with physiotherapy, doxapram may encourage coughing and clearance of excessive secretions. However, its use has largely been superseded by non-invasive ventilatory support, such as with nasal intermittent positive pressure ventilation. There is also a minor role for doxapram to reverse postoperative respiratory depression. Doxapram stimulates the medullary respiratory centre both by a direct action and by peripheral stimulation of the carotid body. Given by intravenous injection, its action is very brief, owing to rapid metabolism by the liver, and a continuous infusion is often used. Restlessness, muscle twitching and vomiting are common unwanted effects, and seizures can occur due to generalised stimulation of the central nervous system.
Acetazolamide (Ch. 14) is an inhibitor of carbonic anhydrase that stimulates the respiratory centre by creating a mild metabolic acidosis. This action may contribute to its ability to reduce the headache, nausea, vomiting and lethargy of acute altitude sickness by decreasing periodic nocturnal apnoea and maintaining arterial oxygen saturation. Use of acetazolamide is not a substitute for gradual acclimatisation to altitude.
Cystic fibrosis
Cystic fibrosis is an autosomal recessive disorder caused by a single gene mutation on the long arm of chromosome 7. This gene encodes the cystic fibrosis transmembrane conductance regulator (CFTR), a Cl− and HCO3− channel in the apical membranes of many epithelial cells. The transport of negative ions is accompanied by paracellular diffusion of Na+ and water, creating a fluid secretion from the cell. If the CFTR gene is faulty, then the function of the transporter is impaired or absent and Cl− transport is defective in epithelial cells in many organs, including the respiratory, hepatobiliary, gastrointestinal and reproductive tracts and the pancreas. As a result of the defective electrolyte flows, secretions become thicker. This causes obstruction in (and destruction of) exocrine glandular ducts, and in the lungs clogs respiratory cilia with mucus. Over 1700 CFTR gene mutations have already been identified (although about 15 of these account for more than 75% of clinical cases), but even a single type of mutation produces different severities of disease, suggesting that there is involvement of other genes or environmental factors.
In cystic fibrosis there is a defective periciliary liquid layer of the airway suface mucus. The more viscous mucus renders the cilia ineffective and the resulting stasis creates the environment for infection. The lung becomes colonised with bacteria that are impossible to eradicate and a chronic inflammatory response is established in the airway. The consequences of infection and inflammation are bronchiectasis and chronic airflow obstruction.
The most common and disabling clinical consequences of cystic fibrosis are lung disease and pancreatic exocrine insufficiency leading to malabsorption. These problems affect about 90% of those with the gene defect. About 20% develop pancreatic endocrine insufficiency with type 1 diabetes mellitus and a smaller number develop meconium ileus in infancy or obstructive biliary tract disease. Death in 90% of people with cystic fibrosis is due to progressive lung disease, but median life expectancy is now about 37 years due to improved treatment.
Drug treatment of cystic fibrosis
Much of the treatment for cystic fibrosis is supportive, including physiotherapy and regular inhaled antibacterial drugs to reduce exacerbations of lung disease, and intensive antibacterial therapy to treat exacerbations of lung disease. Nebulised hypertonic saline improves mucociliary clearance, and reduces the frequency of infective exacerbations. It can sometimes produce bronchospasm, which can be prevented by prior use of an inhaled β2-adrenoceptor agonist such as salbutamol (Ch. 12). Nutritional supplements are important because of the frequency of fat malabsorption.
Prevention of infection (and cross-infection), particularly during hospital admission, is important, and improved treatment of infection is the main reason for the prolongation of life expectancy in recent years. Staphylococcus aureus and Haemophilus influenzae are common pathogens in the very young person with cystic fibrosis, while Burkholderia cepacia and Burkholderia dolosa are particularly virulent pathogens. In the early years of life, anti-staphylococcal therapy is usually appropriate for exacerbations of lung disease (Ch. 51). By adolescence, Pseudomonas aeruginosa becomes the predominant pathogen, and is treated with intravenous or nebulised antibacterials. Inhalation of nebulised tobramycin or nebulised colistimethate sodium, perhaps combined with oral ciprofloxacin, is increasingly used to treat exacerbations during and after adolescence (Ch. 51). It is almost impossible to eradicate P. aeruginosa from sputum, but rapid and intensive treatment of clinical infection slows the decline in lung function.
Since inflammation is a major component of the airway disease, several anti-inflammatory therapies have been studied. Oral corticosteroids (Ch. 44) reduce the rate of decline in lung function and reduce the frequency of infections, but unwanted effects preclude their long-term use. Inhaled corticosteroid does not improve lung function unless there is associated airway hyperreactivity.
There are several pharmacological interventions under investigation for improving the conductance of the defective Cl− channel in cystic fibrosis. The first of these, ivacaftor, is now available for treatment of the 5% of people with cystic fibrosis with a specific type of CFTR gene defect.
In addition to antibacterial treatment of respiratory infection, current therapies for respiratory and gastrointestinal symptoms of cystic fibrosis include the following.
Dornase alfa
Dornase alfa (recombinant human deoxyribonuclease I, or rhDNase I) is an enzyme that digests extracellular DNA. DNA released from dying neutrophils in the airways contributes to the increased sputum viscosity in cystic fibrosis. Dornase alfa is given by inhalation using a jet nebuliser (see Ch. 12) and is probably most effective when given on alternate days. It reduces sputum viscoelasticity, improves lung function in the short- to medium-term (although long-term benefits are much less certain) and results in fewer exacerbations of lung disease. Improved lung function should be measurable after 2 weeks in responders. Unwanted effects are rare, and include transient pharyngitis and hoarseness.
Pancreatic enzyme supplements (pancreatin)
Pancreatin consists of protease, lipase and amylase, enzymes which are inactivated by gastric acid and by heat. Supplements, therefore, must be taken with food (but not mixed with very hot food), and either with gastric acid suppression therapy (e.g. given 1 h after cimetidine; Ch. 33) or as enteric-coated formulations to protect them from gastric acid. Pancreatin preparations in clinical use are all of porcine origin. Dosage is adjusted according to the size, number and consistency of stools. Unwanted effects include irritation of the mouth and perianal skin, nausea, vomiting and abdominal discomfort. Some higher-strength formulations should be avoided in children under 15 years of age with cystic fibrosis, since they have been associated with the formation of large bowel strictures. Pancreatin is also used for pancreatic exocrine insufficiency following pancreatectomy, gastrectomy or chronic pancreatitis.
Neonatal respiratory distress syndrome
Pulmonary surfactant is responsible for reducing surface tension at the air–liquid interface in the alveoli, preventing lung collapse at resting lung pressures. Surfactant is a macromolecular complex largely composed of phospholipids, mainly phosphatidylcholine (of which dipalmitoylphosphatidylcholine is the major surface-active component), neutral lipids and surfactant-specific proteins A–D. The phospholipid monolayer stabilises the lungs and prevents end-expiratory alveolar collapse by reducing the deflating force in the alveolus. Surfactant proteins B and C are hydrophobic and critical for adsorption and spreading of the surfactant layer at the air–liquid interface. The hydrophilic surfactant proteins A and D are involved in surfactant metabolism and host defence.
Surfactant is synthesised by epithelial cells lining the alveoli and is normally present in substantial amounts at full term delivery. However, preterm infants may produce too little surfactant, leading to neonatal respiratory distress syndrome.
Mortality is high in neonatal respiratory distress syndrome, but it can be reduced by administration of surfactant via an endotracheal tube into the lung. There are two natural therapeutic surfactants: beractant (bovine lung extract) and poractant alfa (porcine lung phospholipid fraction), which do not retain the surfactant proteins A and D. New synthetic compounds with peptides that mimic the natural surfactant proteins are under clinical development. The potential advantages of a synthetic compound include easier production and elimination of the infection risk associated with animal products.
The use of a surfactant in neonatal respiratory distress syndrome reduces the risk of death by 40%, whether the treatment is given prophylactically or as a rescue treatment. There is also a reduced risk of pneumothorax and of subsequent chronic lung disease. Surfactant is given as soon as possible after delivery to infants with neonatal respiratory distress syndrome, or to those considered to be at risk of developing it.
In women at risk of preterm delivery, a corticosteroid such as dexamethasone (Ch. 44) can increase the production of surfactant in the fetal lung, which may prevent neonatal respiratory distress syndrome.
True/false questions
1. Postviral cough can last for 3–6 weeks.
2. Angiotensin II receptor antagonists frequently cause cough.
3. Many compound cough preparations sold over the counter contain sedating antihistamines.
4. Dextromethorphan is a synthetic opioid with cough suppressant, sedative and analgesic activity.
5. There is little evidence that any preparation can specifically facilitate expectoration.
6. Pulmonary surfactant increases surface tension in the alveoli.
7. Therapeutic surfactant is identical to natural human surfactant.
8. Doxapram should not be used in postoperative respiratory failure.
9. The mucolytic mecysteine acts by inhibiting the production of mucus.
1. True. Treatment of postviral cough should include increased humidity of inspired air and cough suppressants; other drugs are of little value.
2. False. Angiotensin II receptor antagonists do not cause cough. However, inhibitors of angiotensin-converting enzyme (ACE), which reduce the formation of angiotensin II, also prevent the breakdown of bradykinin and this causes cough in 15% of people.
3. True. Diphenhydramine and chlorpheniramine are common constituents of over-the-counter cough mixtures.
4. False. Dextromethorphan has the same cough suppressant potency as codeine but does not share its sedative or analgesic effects; dextromethorphan may act by blocking N-methyl-D-aspartate (NMDA) receptors.
5. True. Expectorants may nevertheless serve a useful placebo function.
6. False. Surfactant has a detergent-like action to lower surface tension, enabling the alveoli to expand and retain an expanded shape.
7. False. Therapeutic surfactants such as beractant and poractant alfa are animal products lacking the two hydrophilic surfactant proteins SP-A and SP-D.
8. False. Doxapram is sometimes used in hospitals for postoperative respiratory failure. It stimulates the respiratory centre and the carotid chemoreceptors, but its precise mode of action is unknown.
9. False. Mecysteine breaks the disulphide cross-bridges that maintain the polymeric gel-like structure of mucus.
10. True. Dornase alpha is a recombinant deoxribonuclease that digests DNA released by dying neutrophils in sputum; it is given by nebuliser to reduce viscosity of lung secretions in cystic fibrosis.
Bolser, DC. Current and future centrally acting antitussives. Resp Physiol Neurobiol. 2006;152:349–355.
Chang, AB. The physiology of cough. Paediatr Resp Rev. 2006;7:2–8.
Dicpinigaitis, PV. Current and future peripherally-acting antitussives. Respir Physiol Neurobiol. 2006;152:356–362.
Dicpinigaitis, PV. Cough: an unmet clinical need. Br J Pharmacol. 2011;163:116–124.
Irwin, RS, Madison, JM. Primary care: the diagnosis and treatment of cough. N Engl J Med. 2000;343:1715–1721.
Boyle, MP. Adult cystic fibrosis. JAMA. 2007;298:1787–1793.
Cuthbert, AW. New horizons in the treatment of cystic fibrosis. Br J Pharmacol. 2011;163:141–172.
Davies, JC, Alton, EWFW, Bush, A. Cystic fibrosis. BMJ. 2007;335:1255–1259.
Elborn, JS. Practical management of cystic fibrosis. Chron Resp Dis. 2006;3:161–165.
Neonatal respiratory distress syndrome
Curstedt, T, Johansson, J. New synthetic surfactants – basic science. Biol Neonate. 2005;87:332–337.
Pfister, RH, Soll, RF. New synthetic surfactants: the next generation? Biol Neonate. 2005;87:338–344.
Whitsett, JA, Weaver, TE. Mechanisms of disease: hydrophobic surfactant proteins in lung function and disease. N Engl J Med. 2002;347:2142–2148.