Antihistamines and allergic disease
Atopy, allergic disorders and anaphylaxis
Allergic responses occur in atopic individuals who are predisposed to produce antigen-specific immunoglobulin E (IgE) when exposed to common, normally harmless environmental allergens such as house dust mite, grass pollen or animal dander. Immunological memory takes about 7 days to develop, and subsequent re-exposure to the allergen results in the antigen crosslinking IgE on mast cells and basophils and triggering an allergic response as explained below. Many atopic individuals have coexisting allergic diseases such as asthma, hay fever and eczema, although these are not invariably associated with atopy.
The control of antibody production in the immune response is shown in Figure 38.2. The key to the allergic reaction is that there is a preponderance of IgE production, rather than other classes of antibodies. This is because when atopic individuals are exposed to allergens they invoke a T-helper type 2 (Th2) lymphocyte response, rather than the usually dominant Th1-cell response (Ch. 38). The release of the Th2 profile of interleukins, including IL-4, IL-10 and IL-13, stimulates B-lymphocytes to produce IgE rather than IgG, a phenomenon known as class switching. Dominance of Th1 or Th2 response is partially programmed in early life, with exposure to microbial antigens thought to promote the normal Th1 dominance.
Most allergic reactions are predominantly of the type 1 (immediate) hypersensitivity category (see Ch. 38 for definitions). Immediate hypersensitivity to an allergen in a person with atopy produces a weal and flare reaction in the skin, or sneezing and a runny nose, or wheezing, within minutes. Pre-formed and newly synthesised mediators of the allergic response are released from mast cells and basophils after allergen crosslinks IgE that is bound to cell surface receptors. The pre-formed mediators include histamine and the newly synthesised mediators include platelet-activating factor, prostaglandin D2 and the cysteinyl-leukotriene, LTC4, which is converted to LTD4 and LTE4 extracellularly (Ch. 29). These mediators act at selective G-protein-coupled receptors on smooth muscle cells, endothelial cells, epithelial cells, mucus glands and leucocytes in various tissues. Tryptase is also released and stimulates protease-activated receptors (see Ch. 1).
Some allergic reactions, such as those that produce contact dermatitis, are driven by T-cell-mediated inflammatory processes. These reactions can result from involvement of Th1 or Th2 cells, or sometimes cytotoxic T-cells.
A prolonged inflammatory reaction (delayed-type hypersensitivity) may follow the initial allergic response, reaching a peak 6–9 h later. Depending on the site of the reaction, this produces an oedematous, red, indurated swelling in the skin, or a sustained blockage in the nose, or further wheezing. This delayed reaction is associated with tissue accumulation of eosinophils and neutrophils, followed by T-cells and basophils. Some delayed reactions arise without an immediate phase and may be triggered by primary activation of T-cells rather than mast cells. Chronic allergic inflammation is maintained by continuing release of several Th2-type cytokines which promote the production of mast cells and eosinophils, stimulate the expression of adhesion molecules and enhance the synthesis of IgE. Eosinophils release toxic basic proteins, cysteinyl-leukotrienes and platelet-activating factor. T-cells, mast cells and eosinophils also produce neurotrophins that release neuropeptides such as substance P, calcitonin gene-related peptide and neurokinin A from sensory neurons. These various mediators contribute to the inflammatory response by producing vasodilation with increased vascular permeability, and in the lung promote smooth muscle contraction and mucus secretion.
Allergic reactions to antigens vary in severity. At the most severe end of the spectrum is anaphylaxis, a systemic allergic reaction that is life-threatening because of upper airway swelling and obstruction and/or hypotension. Severe anaphylactic reactions can occur within minutes of exposure to the allergen. There are several causes of anaphylaxis (Box 39.1). If the allergen exposure is via systemic injection, then hypotension and shock will predominate. Foods are more likely to cause facial and laryngeal oedema with prominent respiratory problems.
Drugs can also act directly on mast cells to release mediators without the involvement of IgE. Such reactions are called anaphylactoid, and they present in the same way as true anaphylaxis.
Histamine as an autacoid
Histamine is a heterocyclic amine that functions as a local hormone (autacoid). It is found in mast cells which are prominent in tissues that come into contact with the outside world, for example skin, lungs and gut, where they form part of the tissue defence mechanisms. Histamine is also present in circulating basophils, where it may also participate in tissue defence. Histamine has other roles in enterochromaffin-like cells in the stomach, where it participates in acid secretion (Ch. 33), and in the brain, where it acts as a neurotransmitter (Ch. 4).
Histamine is synthesised in mast cells and basophils by decarboxylation of dietary histidine and stored in intracellular granules. It is released by degranulation after activation of the cell either by a direct physical or chemical injury, by crosslinking of attached IgE molecules or by complement proteins. After release from these cells histamine is rapidly metabolised (see Ch. 4). Its effects are mediated by four distinct types of G-protein-coupled receptor, known as H1, H2, H3 and H4 (see the table of receptors at the end of Ch. 1). In general, H1 receptors are involved in the ‘defensive’ actions of histamine and act through intracellular Ca2+ as a second messenger. Gastric acid secretion is mediated by H2 receptors that generate cAMP as a second messenger (Ch. 33). These receptors are also involved in cardiac function (stimulation of rate and force of contraction) and are inhibitory postsynaptic receptors in the brain. There also H3 and H4 receptors in various locations (see Chs 1 and 4).
Allergic reactions involve the action of histamine at H1 receptors. Histamine H1 receptors are coupled to inositol phospholipid intracellular signalling pathways and activate the ubiquitous gene transcription factor nuclear factor κB (NF-κB; Ch. 30). NF-κB stimulates production of pro-inflammatory cytokines (particularly tumour necrosis factor α, IL-6 and IL-8) and expression of epithelial and endothelial adhesion molecules that attract inflammatory cells. The following are the major consequences of H1 receptor stimulation.
 Capillary and venous dilation can produce marked hypotension. In the skin, histamine contributes to the weal and flare response; an axon reflex via H1 receptors is responsible for the spread of vasodilation or flare from the oedematous weal.
Capillary and venous dilation can produce marked hypotension. In the skin, histamine contributes to the weal and flare response; an axon reflex via H1 receptors is responsible for the spread of vasodilation or flare from the oedematous weal.
 Increased capillary permeability can produce oedema. This can lead to urticaria, angioedema and laryngeal oedema. The consequent loss of fluid from the circulating blood volume contributes to hypotension.
Increased capillary permeability can produce oedema. This can lead to urticaria, angioedema and laryngeal oedema. The consequent loss of fluid from the circulating blood volume contributes to hypotension.
 Smooth muscle contraction can occur, especially in bronchioles and the intestine.
Smooth muscle contraction can occur, especially in bronchioles and the intestine.
 Skin itching can occur (produced by histamine in combination with kinins and prostaglandins).
Skin itching can occur (produced by histamine in combination with kinins and prostaglandins).
 Pain may occur due to stimulation of nociceptors (Ch. 19).
Pain may occur due to stimulation of nociceptors (Ch. 19).
Histamine H1 receptor antagonists (antihistamines)
Mechanisms of action and effects
The antihistamines are selective antagonists at histamine H1 receptors; antagonists at other histamine receptors are traditionally not called antihistamines. Antihistamines are competitive inverse agonists (see Ch. 1) that reduce the basal level of spontaneous activity at histamine H1 receptors as well as blocking the agonist effects of histamine. Useful actions of antihistamines include:
 suppression of many of the vascular effects of histamine,
suppression of many of the vascular effects of histamine,
 inhibition of inflammatory cell accumulation in tissues by second-generation antihistamines; this may result from downregulation of the activation of NF-κB in tissues at the site of an allergic response.
inhibition of inflammatory cell accumulation in tissues by second-generation antihistamines; this may result from downregulation of the activation of NF-κB in tissues at the site of an allergic response.
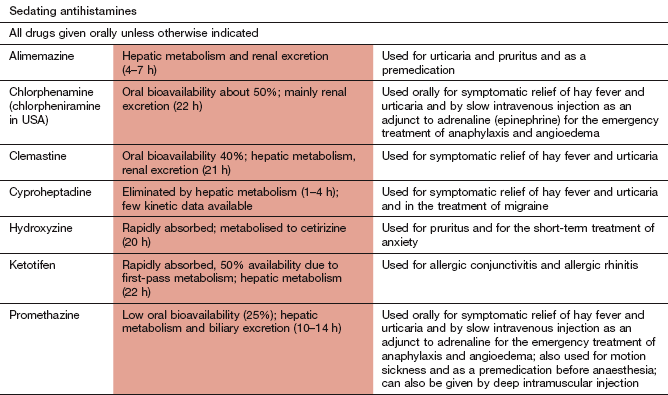
First-generation antihistamines have other actions that can be used therapeutically. They are lipophilic and cross the blood–brain barrier, producing sedation. They also have central antimuscarinic effects that may be clinically useful in suppressing nausea in motion sickness (e.g. cyclizine [no longer used as an antihistamine], promethazine; Ch. 32).
Second-generation (non-sedating) antihistamines such as cetirizine, fexofenadine, loratadine and mizolastine are either more hydrophilic or more ionised at physiological pH; they do not penetrate the blood–brain barrier well, and have little sedative effect. They also have little antimuscarinic action.
So-called ‘third-generation’ antihistamines, such as desloratadine, are active metabolites or optical isomers of second-generation drugs. They have similar efficacy to second-generation drugs but may have a different profile of unwanted effects.
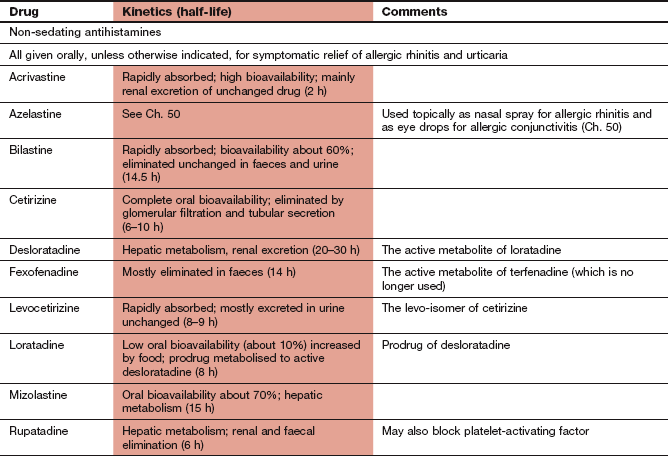
Pharmacokinetics
Chlorphenamine is more slowly absorbed from the gut than promethazine; both undergo considerable first-pass hepatic metabolism to inactive compounds and have half-lives of 10–20 h. Formulations of chlorphenamine and promethazine are available for administration by intravenous or intramuscular injection in medical emergencies.
Most second-generation antihistamines are rapidly absorbed from the gut and metabolised in the liver to active compounds with half-lives ranging from 2 to 20 h. Cetirizine and fexofenadine undergo little metabolism and are mainly eliminated unchanged by the kidneys.
There are several topical formulations of antihistamines, including nasal sprays for allergic rhinitis, eye drops for allergic conjunctivitis and topical skin preparations for insect stings (although the latter are relatively ineffective).
Unwanted effects
 Drowsiness or psychomotor impairment, especially with first-generation compounds, although paradoxical stimulation can occur in children and the elderly.
Drowsiness or psychomotor impairment, especially with first-generation compounds, although paradoxical stimulation can occur in children and the elderly.
 Dry mouth, blurred vision, urinary retention and gastrointestinal upset from the antimuscarinic effects of first-generation compounds.
Dry mouth, blurred vision, urinary retention and gastrointestinal upset from the antimuscarinic effects of first-generation compounds.
 Topical antihistamines for use on the skin can cause hypersensitivity reactions.
Topical antihistamines for use on the skin can cause hypersensitivity reactions.
Management of allergic disorders
Most allergic reactions involve a complex series of chemical processes. However, the mainstay of treatment for many conditions is the use of antihistamines. Their efficacy indicates the importance of histamine as a mediator of allergic responses.
Anaphylaxis
Anaphylaxis is a medical emergency and requires rapidly acting treatments. It most commonly arises as an allergic response to stings, nuts, penicillins, cephalosporins and muscle-relaxant drugs. The person should be laid flat with their feet raised if there is hypotension, and the airway secured. Adrenaline (epinephrine; Ch. 4) should be given intramuscularly and doses repeated every 10 min until the clinical state is stable. Adrenaline produces vasoconstriction by its action at α1-adrenoceptors, reducing oedema, and bronchodilates via β2-adrenoceptors. It also attenuates the release of mediators from mast cells by binding to cell surface β2-adrenoceptors. People known to have allergies that cause anaphylaxis can carry a preloaded adrenaline syringe for emergencies, accompanied by detailed instructions on its appropriate use. Intravenous adrenaline should only be given if there is profound shock, and then in a very dilute solution with close cardiac monitoring. Intravenous use carries a risk of arrhythmias and intense vasoconstriction with myocardial ischaemic damage.
Once adrenaline has been given, late relapse can be prevented by intramuscular injection or slow intravenous injection of chlorphenamine and hydrocortisone (Ch. 44). Oxygen should be given in high concentration, and an inhaled β2-adrenoceptor agonist such as salbutamol (Ch. 12) administered if there is marked bronchospasm. This can be particularly useful if a β-adrenoceptor antagonist has previously been taken, when adrenaline may be less effective on the airways. If there is persistent hypotension, intravenous fluid should be given rapidly, preferably a crystalloid such as isotonic saline.
Seasonal and perennial rhinitis
Allergic inflammation of the lining of the nose produces symptoms of rhinitis including nasal obstruction, sneezing and itching. These result from increased glandular secretions producing nasal obstruction and mucous rhinorrhoea, as well as afferent nerve stimulation, which is responsible for itching and sneezing. Allergies can cause both perennial rhinitis (usually house dust mite) and seasonal rhinitis (pollens and moulds). The allergic response makes individuals more susceptible to the nasal irritant effects of other, non-allergenic stimuli, such as tobacco smoke and changes in temperature. Rhinitis also has several non-allergic causes, including acute infection and chronic sinus infection for which antibacterial treatment is indicated. Aspirin and other non-steroidal anti-inflammatory drugs can produce rhinitis (as well as asthma, see Ch. 12) in sensitive subjects, probably by enhancing cysteinyl-leukotriene generation. Less frequent causes include β-adrenoceptor antagonists (Ch. 5) and angiotensin-converting enzyme (ACE) inhibitors (Ch. 6).
Oral antihistamines are useful for reducing itching, sneezing and rhinorrhoea, but they are less effective for nasal obstruction. They can also suppress associated allergic conjunctivitis. Azelastine is an antihistamine used as a topical nasal spray. For more severe allergic rhinitis, a topical intranasal corticosteroid spray (Ch. 44) is the treatment of choice, providing relief from most symptoms. Topical sodium cromoglicate or nedocromil (Ch. 12) can be useful in atopic individuals, but they are less effective than antihistamines or topical corticosteroids and are no longer preferred treatments. An oral leukotriene receptor antagonist (montelukast) may be beneficial in allergic rhinitis with concomitant asthma. The antimuscarinic drug ipratropium bromide (Ch. 12) can be used topically for relief of non-allergic rhinorrhoea.
Topical nasal decongestants have a short-term role in treatment. These contain α1-adrenoceptor agonists such as ephedrine or xylometazoline and produce local vasoconstriction. Prolonged use impairs ciliary activity in the nasal mucosa and can be associated with rebound nasal congestion during long-term use. Oral corticosteroids are reserved for the most severe symptoms.
If drugs fail the possibility of structural abnormalities such as nasal polyposis, hypertrophied inferior turbinates or a deviated nasal septum should be considered, since surgery may be helpful.
Urticaria
Acute urticarial reactions often occur to the same allergens that cause anaphylaxis. Antihistamines are the treatment of choice, with an oral corticosteroid (Ch. 44) for more severe episodes.
Chronic urticaria can be provoked by physical factors such as cold, sun, scratching the skin or exercise, or it can be caused by urticarial vasculitis in association with connective tissue diseases such as systemic lupus erythematosus. In some cases, the cause may be autoimmune, caused by IgG autoantibodies to the IgE receptors on mast cells and basophils. Antihistamines can be useful to suppress the itch from urticaria, but often they have little effect on the weal. About 15% of the histamine receptors in the skin are H2 receptors, and a histamine H2 receptor blocker (Ch. 33) may be useful in addition to an antihistamine. Leukotriene receptor antagonists such as montelukast (Ch. 12) may be helpful for some people. Corticosteroids (Ch. 44) can be used in high dosage for severe symptoms, but long-term use should be avoided because of the unwanted effects. Immunosuppression with ciclosporin (Ch. 38) has been used successfully for some severe autoimmune urticarias.
Allergic conjunctivitis
Topical treatment with antihistamines, such as azelastine or levocabastine, or with sodium cromoglicate or nedocromil, is usually successful (see Ch. 50).
Asthma
Although asthma often has an allergic component, antihistamines have little or no role. The management of asthma is considered in Chapter 12.
True/false questions
1. Antihistamines do not reduce acid secretion from the gastric parietal cells.
2. Histamine is synthesised de novo when mast cell IgE receptors are crosslinked by allergen.
3. Loratadine is a non-sedating antihistamine.
4. Fexofenadine is associated with electrocardiographic (ECG) changes.
5. Fexofenadine reduces the release of histamine from mast cells.
6. Corticosteroids are effective for treating allergic rhinitis.
7. Histamine is the only mediator that causes symptoms in rhinitis.
8. Antihistamines have a well-defined place in the management of asthma.
One-best-answer (OBA) questions
1. Which one of the following contributes to an allergic response in an atopic individual?
A Increased production of cytokines from Th1-cells
2. Choose the correct statement below concerning antihistamines.
A Second-generation antihistamines readily cross the blood–brain barrier.
B Second-generation antihistamines have fewer antimuscarinic effects than first-generation antihistamines.
C First-generation antihistamines are the preferred first-line treatment for vomiting induced by cytotoxic drugs.
Case-based questions
A 10-year-old boy visited his doctor with his mother in the spring. His current symptoms of rhinorrhoea, nasal congestion, sneezing and itching eyes were interfering with his schoolwork. He gave a history of repeated episodes of recurrent otitis media, rhinorrhoea, nasal congestion, sneezing and itching eyes occurring over a 3-year period, but predominantly in the spring and autumn. He had had three episodes of otitis media over the previous 2 years, the last being 6 months before, which were treated with antibiotics because of prolonged residence of fluid in the middle ear. The boy had atopic dermatitis as an infant. He had no history of asthma; his mother had allergic rhinitis; they had two cats. Other than antibacterial drug treatment for his otitis media, he had taken no medication. Examination of the ears revealed healthy tympanic membranes with no current otitis media. He had no hearing loss and he was otherwise fit.
1. True. The term antihistamine is traditionally confined to H1 receptor antagonists; these drugs do not block H2 histamine receptors on the gastric parietal cells; selective histamine H2 receptor antagonists include cimetidine and ranitidine.
2. False. Histamine is synthesised and stored in mast cell granules ready for release by IgE-dependent stimuli; in contrast, lipid mediators such as leukotrienes and prostaglandins are synthesised de novo after stimulation.
3. True. Loratadine is a second-generation antihistamine, which lack the sedative action of first-generation antihistamines.
4. False. The parent drug of fexofenadine, terfenadine, was associated with ventricular arrhythmias in high doses and has been withdrawn; fexofenadine retains the antihistamine activity without the unwanted effects on the heart.
5. False. Fexofenadine blocks histamine activity only by blocking H1 receptors.
6. True. Nasal corticosteroids are very effective in allergic rhinitis.
7. False. Mast cells also release prostaglandins and leukotrienes that contribute to nasal symptoms.
8. False. Antihistamines are not effective in asthma and have no place in asthma management guidelines.
OBA answers
A Incorrect. In atopy there is a predominance of a Th2 response profile which is partially genetically determined and partly related to early life environment.
B Incorrect. The Th2 response leads to increased production of IgE.
C Incorrect. Mast cells degranulate following allergen crosslinking of IgE.
D Correct. Although the main effect of histamine in allergy is on the H1 receptor, actions on H2 receptors may also contribute to the allergic symptoms.
E Incorrect. Leukotriene synthesis in mast cells is increased and contributes to allergic responses.
A Incorrect. Second-generation drugs are less able to cross the blood–brain barrier than first-generation drugs and cause less sedation.
B Correct. Second-generation antihistamines have less antagonist activity at muscarinic receptors.
C Incorrect. Antihistamines can be effective in motion sickness but not in vomiting caused by cancer chemotherapeutic agents.
D Incorrect. Topical antihistamines may cause hypersensitivity reactions.
E Incorrect. Antihistamines reduce vasodilation induced by the action of histamine at the H1 receptor.
Case-based answers
A The family history of atopy and the child's atopic dermatitis as an infant increase the likelihood that he would have had allergies. He is likely to have had seasonal allergic rhinitis but he may also have had sensitisation to cat and/or dust mite or other perennial allergens. His fitness and lack of current drug intake suggest that it is not non-allergic rhinitis, which may arise because of infections, drugs, etc.
B Yes. As many as 50% of children older than 3 years with recurrent otitis media have confirmed allergic rhinitis.
C It is important to carry out sensitivity testing, and sensitivity to cat dander and house dust mite was identified in this boy. Avoidance of exposure to allergens is advisable and should be actively pursued in the home and school environment. If pharmacological treatment is required, a non-sedating oral antihistamine should reduce rhinorrhoea, sneezing and itching but will have little effect on nasal congestion. A short course of nasal inhaled corticosteroids can be effective in controlling symptoms of allergic rhinitis, including congestion. Nasal sodium cromoglicate may also offer symptom relief but is not the preferred treatment.
Antihistamines are given orally, or topically in the eye (Ch. 50), nose and on the skin. Drugs with antihistamine actions which are not used to treat allergic conditions, such as cyclizine and meclozine, are used for the treatment of vestibular disorders and nausea and vomiting, especially motion sickness (see Ch. 32).
Al Suleimani, YM, Walker, MJA. Allergic rhinitis and its pharmacology. Pharmacol Ther. 2007;114:233–260.
Ardern-Jones, MR, Friedmann, PS. Skin manifestations of drug allergy. Br J Clin Pharmacol. 2010;71:672–683.
De Groot, H, Brand, PLP, Fokkens, WF, et al. Allergic rhinoconjunctivitis in children. BMJ. 2007;335:985–988.
Greiner, AN, Hellings, PW, Rotiroti, G, et al. Allergic rhinitis. Lancet. 2011;378:2112–2122.
Kaplan, AP. Chronic urticaria and angioedema. N Engl J Med. 2002;346:175–179.
Kemp, SF. Office approach to anaphylaxis: sooner better than later. Am J Med. 2007;120:664–668.
Plaut, M, Valentine, MD. Allergic rhinitis. N Engl J Med. 2005;353:1934–1944.
Saleh, HA, Durham, SR. Perennial rhinitis. BMJ. 2007;335:502–507.