The eye
Vision depends upon the eye converting light that falls on the retina into an electrical signal to be carried to the brain through the optic nerve. The eye must focus objects sharply on the retina, a process called accommodation. To adjust the innate focus to achieve this, the ciliary muscle alters the shape of the lens, allowing the eye to accommodate to objects at different distances. The iris determines the size of the pupil and the amount of light entering the eye. The autonomic nervous system innervates the ciliary muscles and the iris.
Accommodation
The ciliary muscle is a circular (constrictor) smooth muscle that is attached to the lens by suspensory ligaments. The ciliary muscle only has a parasympathetic nerve supply (mediated by acetylcholine acting through muscarinic receptors; Ch. 4) and contracts in response to parasympathetic stimulation. This reduces tension on the suspensory ligaments and the capsule of the lens is relaxed, so that the lens becomes shorter and fatter and accommodates for viewing near objects. Drugs that are agonists at muscarinic receptors produce ciliary muscle contraction and fix the lens for viewing near objects, blurring far vision.
In the absence of parasympathetic stimulation the ciliary muscle is relaxed and tension in the suspensory ligaments increases. This pulls on the lens capsule, which flattens the lens and adjusts visual acuity for distant vision. Drugs that are antagonists at muscarinic receptors prevent ciliary muscle contraction and fix the lens for viewing far objects, with blurring of near vision. This state is called cycloplegia (Fig. 50.1).
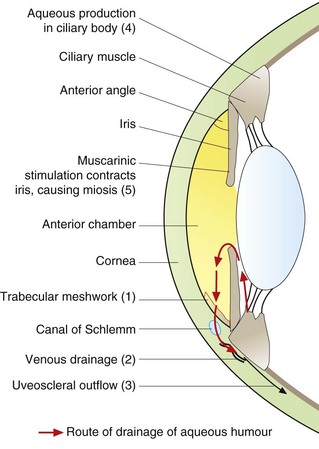
Fig. 50.1 The route of drainage of aqueous humour from the eye and the sites of action of drugs used in the treatment of glaucoma.
The mechanisms by which some drugs benefit glaucoma are still uncertain but are thought to include the following:
 in angle-closure glaucoma, muscarinic agonists, e.g. pilocarpine, facilitate aqueous humour drainage (1, 2) by constricting the iris circular constrictor pupillae (5), which widens the anterior angle,
in angle-closure glaucoma, muscarinic agonists, e.g. pilocarpine, facilitate aqueous humour drainage (1, 2) by constricting the iris circular constrictor pupillae (5), which widens the anterior angle,
 carbonic anhydrase inhibitors, e.g. acetazolamide, decrease aqueous humour production (4),
carbonic anhydrase inhibitors, e.g. acetazolamide, decrease aqueous humour production (4),
 beta-adrenoceptor antagonists, e.g. timolol, reduce aqueous humour production (4) and increase outflow (1),
beta-adrenoceptor antagonists, e.g. timolol, reduce aqueous humour production (4) and increase outflow (1),
 selective α2-adrenoceptor agonists, e.g. brimonidine, decrease aqueous humour production (4),
selective α2-adrenoceptor agonists, e.g. brimonidine, decrease aqueous humour production (4),
 prostaglandin analogues selective for stimulating the prostaglandin F2α receptor, e.g. latanoprost, enhance aqueous humour outflow (1, 2, 3) and may improve ocular blood flow.
prostaglandin analogues selective for stimulating the prostaglandin F2α receptor, e.g. latanoprost, enhance aqueous humour outflow (1, 2, 3) and may improve ocular blood flow.
Pupil size
This is determined by the relative tone in the two smooth muscle layers of the iris. The circular (constrictor) muscle is the more powerful and receives parasympathetic nervous innervation, producing muscle contraction that is mediated by acetylcholine acting on muscarinic receptors. The radial (dilator) muscle is sympathetically innervated, and contraction of the muscle is mediated by noradrenaline acting on α1-adrenoceptors.
The light reflex is the primary determinant of pupil size with increased light causing the pupil to constrict and reduce the amount of light that reaches the retina. Pupillary constriction is known as miosis and also accompanies accommodation for near vision, a response mediated by the parasympathetic nervous system. Miosis can be produced by drugs that stimulate muscarinic receptors and contract the circular muscle of the iris. Dilation of the pupil is called mydriasis and is caused by contraction of the radial muscle. Mydriasis can be produced by drugs that are antagonists at muscarinic receptors in the circular muscle (leaving unopposed action of the radial muscle) or by drugs that stimulate α1-adrenoceptors in the radial muscle.
Dilation of the pupil also has the effect of moving the iris towards the cornea and narrowing the anterior angle between the iris and the cornea. This can reduce aqueous humour outflow through the canal of Schlemm.
Drainage of aqueous humour
The space between the cornea, at the front of the eye (Fig. 50.1), and the iris is the anterior chamber and is filled with a clear liquid known as aqueous humour. Aqueous humour is constantly secreted by the ciliary body. Most aqueous humour flows through the pupil to the anterior chamber, and leaves the eye via the trabecular meshwork that drains to the episcleral veins through the canal of Schlemm (Fig. 50.1). Some aqueous humour drains through the sclera (uveoscleral outflow). Production of aqueous humour is influenced by innervation from the autonomic nervous system. Alpha2-adrenoceptor stimulation of the ciliary body reduces the production of aqueous humour, while β1-adrenoceptor stimulation increases its production. Outflow of aqueous humour is also influenced by innervation from the autonomic nervous system, and by prostaglandins. Contraction of the ciliary muscle aids drainage of aqueous humour through the trabecular meshwork into the episcleral veins. Pressure in the eye is maintained by a balance between the production of aqueous humour and its drainage. The intraocular pressure rises if drainage of the aqueous humour is impaired. High intraocular pressure can damage retinal ganglion cells, and is one of the factors that leads to progressive loss of vision in the disease known as glaucoma. If the anterior chamber of the eye is abnormally shallow, there will be a narrow anterior-chamber angle between the iris and cornea (iridocorneal angle) (Fig. 50.1).
Dilation of the pupil can narrow the angle further to an extent where it impedes drainage of aqueous humour through the trabecular meshwork. This can produce an acute rise in pressure in the eye (Fig. 50.1). Conversely, constriction of the circular muscle of the iris makes the pupil smaller and moves the iris away from the trabecular meshwork, widening the anterior angle and facilitating aqueous humour drainage through the canal of Schlemm.
Topical application of drugs to the eye
Drugs applied in solution to the anterior surface of the eye can penetrate to the anterior chamber and the ciliary muscle, principally via the cornea. The high water content of the cornea makes lipid solubility less important for adequate penetration of a drug than is the case for transdermal drug delivery, but formulation of the carrier is important to avoid irritation of the conjunctiva. There is little diffusion to the more posterior structures of the eye.
Systemic absorption of drug following topical application to the surface of the eye can occur either via conjunctival vessels or from the nasal mucosa after drainage of excess drug through the tear ducts. Topical administration of drugs to the eye can therefore produce systemic effects. Drainage can be reduced by shutting the eyes for at least 1 min after putting in the drops and by compressing the nasolacrimal duct at the medial corner of the eye with a finger. Both eye drops and ointments are usually administered into the pocket that can be formed by gently pulling the lower eyelid downwards (the lower fornix).
Microbial contamination is a potential problem once eye preparations have been opened. Multiple-application containers have preservative added to reduce the risk, but it is not advisable to use any eye preparation more than a month after it has been opened.
Glaucoma
Glaucoma is a group of disorders characterised by loss of retinal ganglion cells and is a form of optic neuropathy. In some cases the intraocular pressure is raised, and ischaemia of the optic nerve head may be the cause. In many cases, however, the pressure in the anterior chamber of the eye is normal and a genetic susceptibility to retinal ganglion cell apoptosis is responsible. The diagnosis requires both structural and functional changes in the eye. There is evidence of optic disc damage with deepening and widening of the depression or cup of the optic disc. Progressive visual defects occur, initially as scotomas (blind spots) in the peripheral visual field. These scotomas enlarge, resulting in tunnel vision and finally total blindness. Glaucoma is the second most common cause of blindness in the UK.
Open-angle glaucoma is caused by obstruction to outflow through the trabecular meshwork, caused by injury or death of cells. It can be associated with raised intraocular pressure, but in other cases the pressure in the eye is normal and retinal cell loss is related to the ability of the optic nerve head to withstand stress imposed by the pressure in the eye.
Angle-closure glaucoma is less common, and results from the iris blocking the drainage angle and preventing drainage through the trabecular meshwork. This usually arises when there is a shallow anterior chamber, such as occurs in long-sighted individuals. The condition is usually chronic and asymptomatic, with a risk of acute attacks of high intraocular pressure with pain and sudden visual loss.
Drugs for glaucoma
Beta-adrenoceptor antagonists reduce the formation of aqueous humour by the ciliary body. They have no effect on accommodation or pupil size. Systemic absorption can produce the typical unwanted effects associated with these compounds, particularly bronchospasm, bradycardia and worsening of uncontrolled heart failure (Ch. 5). The contraindications for topical use in the eye are the same as those for oral use. Timolol is a non-selective β-adrenoceptor antagonist whereas betaxolol is ‘cardioselective’, but they have similar efficacy in the eye.
Sympathomimetics
Brimonidine is a selective α2-adrenoceptor agonist that reduces aqueous humour production. It can cause dry mouth, gastrointestinal disturbances, taste disturbances and headache.
Carbonic anhydrase inhibitors
The intracellular mechanism of action of carbonic anhydrase inhibitors is discussed in Ch. 14. Carbonic anhydrase in the eye plays a key role in controlling aqueous humour production. It is responsible for secreting about 70% of the Na+ that enters the anterior chamber, which is accompanied by water to maintain isotonicity. Therefore, inhibition of the enzyme reduces aqueous humour production.
Acetazolamide is taken orally. Dorzolamide and brinzolamide are topical preparations for the eye, with fewer systemic unwanted effects; their duration of action in the eye is 6–12 h, but they have extremely long plasma half-lives (≥2 weeks) due to retention within erythrocytes.
Prostaglandin analogues
These drugs are analogues of prostaglandin F2α. Their precise mechanism of action in glaucoma remains uncertain, but they increase uveoscleral outflow of aqueous humour. This may result in part from an increase in extracellular matrix metalloproteinases in ciliary smooth muscle cells, and from remodelling of the uveal meshwork. Prostaglandin analogues also increase blood flow to the optic nerve, and this may contribute to neuroprotection in the retina. The reduction in intraocular pressure is greater than that achieved by β-adrenoceptor antagonists. The major disadvantage of prostaglandin analogues is an increase in brown pigmentation of the iris and growth of eyelashes. A rare complication in people who have no lens in the eye (aphakia) is the development of cystoid macular oedema, which responds to treatment with non-steroidal anti-inflammatory drugs. The prostaglandin analogues have a long duration of action of 1–2 days that is not a reflection of their half-lives.
Miotic drugs (muscarinic agonists)
Pilocarpine is usually given for angle-closure glaucoma to contract the circular sphincter muscle of the iris to produce miosis and open up the drainage channels in the anterior chamber of the eye (see also Ch. 4). The miotic effect lasts for about 4 h, but more prolonged miosis can be achieved by the use of a gel delivery system. It is not widely used since ciliary muscle spasm is an undesirable consequence and produces blurred vision and an ache over the eye (especially in younger people).
Treatment of glaucoma
In open-angle glaucoma, reducing intraocular pressure can slow the rate of disease progression sufficiently to prevent significant visual impairment. A target pressure reduction of at least 30% below the presenting pressure is usually set. Treatment of ocular hypertension without evidence of visual loss may prevent the onset of glaucoma.
In primary open-angle glaucoma, a topical β-adrenoceptor antagonist or a prostaglandin analogue is the treatment of choice, because of their relative lack of ocular unwanted effects. If either treatment alone is insufficient, then a combination can give an additive effect. If these agents cannot be used then the choice of a second-line drug lies between a topical carbonic anhydrase inhibitor or a sympathomimetic. Surgery may also be considered at this point. Laser burns applied to the trabecular meshwork can produce a temporary increase in aqueous humour outflow, but drug treatment may still be required. Drainage surgery is the alternative and can often bring about long-term pressure control. The therapeutic challenge is to develop neuroprotective drugs to retard neuronal apoptosis in the retina.
Angle-closure glaucoma is treated by laser peripheral iridotomy or surgical peripheral iridectomy to provide a channel for aqueous humour to flow through the iris. If drug therapy is required after surgery then topical treatment with a prostaglandin analogue or a β-adrenoceptor antagonist can be used.
Mydriatic and cycloplegic drugs
Antimuscarinic drugs (see also Ch. 4) are both mydriatic (dilating the pupil) and cycloplegic (paralysing the ciliary muscle). Tropicamide is weak and short-acting (about 3 h), which makes it useful for dilating the pupil for fundal examination. Cyclopentolate is longer-acting (up to 24 h) and has a rapid onset of action. Homatropine and atropine have actions up to 3 and 7 days, respectively. The longer-acting compounds are used to prevent adhesions (posterior synechiae) in anterior uveitis (often in combination with phenylephrine). Dark irises are more resistant to pupillary dilation with these drugs, as the pigments adsorb the applied drug.
The degree of cycloplegia will depend on the dose of drug; small doses produce pupil dilation and diffusion is insufficient to reach the ciliary muscle and has little effect on accommodation. UK law does not specifically prohibit driving after pupil dilation, but many people find that their vision is impaired for several hours. Care must be taken when using these drugs in individuals predisposed to acute angle-closure glaucoma. Local irritation in the eye is the most common unwanted effect, but systemic effects occasionally occur in children or the elderly (see Ch. 4).
Sympathomimetics
Phenylephrine is a relatively selective α1-adrenoceptor agonist that stimulates the radial muscle of the iris and produces mydriasis. It does not affect the ciliary muscle, and therefore does not affect accommodation. It is a vasoconstrictor, and can decrease vascular congestion of the conjunctiva and oedema of the eyelid in allergic conjunctivitis. In this role it is often combined with an antihistamine in over-the-counter preparations. Local irritation is the most common unwanted effect, although systemic vasoconstriction with hypertension or coronary artery spasm can occur occasionally. It is often given together with muscarinic receptor-blocking drugs to produce pupil dilation for procedures such as cataract operations.
Other topical applications for the eye
Several other drugs are used topically in the eye.
Antibacterial agents
These are given for local infections such as blepharitis, conjunctivitis or trachoma (caused by chlamydial infection) (see also Ch. 51). Aqueous solutions are diluted rapidly or flushed away by lacrimation and should initially be used every 1–2 h; ointments are often given for longer action, for example at night. Examples of broad-spectrum antibacterial agents are gentamicin, chloramphenicol, ciprofloxacin, fusidic acid, neomycin and (for trachoma) chlortetracycline.
Antiviral agents
These are mainly used for herpes simplex infection, which causes dendritic corneal ulcers (see also Ch. 51). Aciclovir is most frequently used.
Corticosteroids
Local inflammatory conditions of the anterior part of the eye, such as uveitis and scleritis, are treated with corticosteroids, for example dexamethasone or prednisolone (Ch. 44). Care must be taken to exclude a viral dendritic ulcer and glaucoma before using them, since these conditions can be exacerbated by corticosteroids. Prolonged use of corticosteroids can lead to thinning of the sclera or cornea, or formation of a ‘steroid cataract’.
Antiallergic agents
Topical antihistamines such as antazoline (usually given in combination with the sympathomimetic xylometazoline) or levocabastine (Ch. 39) can be given for allergic conjunctivitis. Topical sodium cromoglicate or nedocromil (Ch. 12) are generally less effective than antihistamines.
Local anaesthetics
Oxybuprocaine or lidocaine eye drops provide surface anaesthesia (Ch. 18) for tonometry (measurements of pressure in the anterior chamber). For minor surgical procedures, such as removal of cataracts, tetracaine gives more profound anaesthesia and may be combined with injection of a small amount of lidocaine into the anterior chamber.
Non-steroidal anti-inflammatory drugs
Diclofenac, flurbiprofen and ketorolac (Ch. 29) can be applied topically for pain following surgery or laser treatment in the eye.
Artificial tears
Hypromellose (hydroxypropyl-methylcellulose) is most commonly used to treat dry eyes, such as occurs in Sjögren's syndrome. It may need to be reapplied every hour. The surface mucin in the eye is often abnormal when there is tear deficiency, and the mucolytic agent acetylcysteine is often added to hypromellose. Carbomers, synthetic high-molecular-weight polymers of acrylic acid, cling better to the surface of the eye than hypromellose and need less frequent application.
Age-related macular degeneration
Age-related macular degeneration (ARMD) is the main cause of irreversible visual loss in the Western world. Damage to the macula, the central part of the retina, leads to partial or complete loss of central vision. There are two clinical types:
 dry (non-exudative) ARMD that involves hypertrophic changes in the retinal pigment epithelium under the macula, with formation of yellow deposits called drusen,
dry (non-exudative) ARMD that involves hypertrophic changes in the retinal pigment epithelium under the macula, with formation of yellow deposits called drusen,
 wet (exudative) ARMD with development of new blood vessels (choroidal neovascularisation) under the macula, with leakage of blood and fluid.
wet (exudative) ARMD with development of new blood vessels (choroidal neovascularisation) under the macula, with leakage of blood and fluid.
Dry maculopathy is common (85–90% of all macular pathology) and is associated with minor visual disturbance. By contrast, wet ARMD produces severe visual loss in 70% of eyes within 2 years. The dry form of ARMD can progress to the wet form.
Treatment of age-related macular degeneration
Treatment is only available for wet ARMD. Options include:
 laser photocoagulation of neovascular tissue,
laser photocoagulation of neovascular tissue,
 photodynamic therapy using the photosensitising agent verteporfin. Verteporfin is infused intravenously and activated in the eye by non-thermal red light, producing cytotoxic derivatives,
photodynamic therapy using the photosensitising agent verteporfin. Verteporfin is infused intravenously and activated in the eye by non-thermal red light, producing cytotoxic derivatives,
 intravitreal injection of a vascular endothelial growth factor (VEGF) inhibitor such as the monoclonal antibodies ranibizumab or bevacizumab (Ch. 52). VEGF is a protein that induces angiogenesis and increases vascular permeability
intravitreal injection of a vascular endothelial growth factor (VEGF) inhibitor such as the monoclonal antibodies ranibizumab or bevacizumab (Ch. 52). VEGF is a protein that induces angiogenesis and increases vascular permeability
Treatment of exudative ARMD slows the loss of visual acuity in 20–30% of eyes compared to no treatment.
True/false questions
1. The production of aqueous humour is not altered in glaucoma.
2. Brimonidine reduces aqueous humour secretion and causes mydriasis.
3. Stimulation of β-adrenoceptors in the ciliary body reduces aqueous humour production.
4. Tropicamide should be avoided in people with glaucoma.
5. Accommodation of the lens is controlled by the sympathetic autonomic nervous system.
6. Cocaine causes mydriasis when administered topically to the eye.
7. Cyclopentolate is a short-acting mydriatic drug used for fundal examination.
8. Pilocarpine causes accommodation for near vision.
9. Dry (non-exudative) age-related macular degeneration (AMRD) produces severe visual loss.
10. Bevacizumab may be given by intravitreal injection in wet AMRD.
Extended-matching-item questions
Match each statement 1–4 below with the appropriate drug from options A–F.
1. An antagonist of receptors in the ciliary body that will reduce aqueous production in glaucoma but with no effect on pupil size.
2. A drug that dilates the pupil without affecting accommodation or production of aqueous humour.
3. A relatively short-acting drug that will dilate the pupil and is weakly cycloplegic.
4. A long-acting and strongly cycloplegic drug that can be used to prevent adhesions (posterior synechiae) in anterior uveitis.
1. True. Glaucoma is due to reduced outflow of aqueous humour, resulting from obstruction of the trabecular meshwork or closure of the anterior angle.
2. False. The selective action of brimonidine on α2-adrenoceptors reduces aqueous humour production in the ciliary body but does not cause mydriasis or reduce the anterior angle.
3. False. Aqueous humour production in the ciliary body is reduced by antagonists of β-adrenoceptors, such as timolol.
4. True. Tropicamide blocks muscarinic receptors in the circular muscle of the iris, causing mydriasis, which narrows the anterior angle and may reduce aqueous drainage in angle-closure glaucoma.
5. False. The ciliary muscle of the lens is innervated only by parasympathetic autonomic nerves.
6. True. Formerly used as a local anaesthetic, cocaine causes mydriasis by preventing reuptake of released noradrenaline, which contracts the iris radial muscle.
7. False. Cyclopentolate acts for 12–24 h; tropicamide acts for about 3 h and is therefore more useful for fundal examination.
8. True. Pilocarpine is a muscarinic receptor agonist; it contracts the ciliary muscle, causing the lens to accommodate for near vision, and the iris circular muscle, causing miosis.
9. False. Dry AMRD causes only minor visual disturbance. Wet (exudative) ARMD produces severe visual loss in 70% of eyes within 2 years.
10. True. Bevacizumab is a vascular endothelial growth factor (VEGF) inhibitor that reduces angiogenesis in wet AMRD.
Extended-matching-item answers
1. Answer E. Timolol is a β-adrenoceptor antagonist and reduces aqueous production but does not affect the pupil size, which is controlled by muscarinic and α1-adrenergic receptors on the iris circular and radial muscles, respectively.
2. Answer B. Phenylephrine will dilate the pupil by α1-adrenoceptor stimulation of the iris, but not the ciliary muscle (muscarinic receptors).
3. Answer D. Tropicamide is a relatively short-acting muscarinic antagonist with only a relatively weak blocking action on muscarinic receptors on the ciliary muscle.
4. Answer F. Atropine is a long-acting mydriatic that can be used to prevent adhesions but strongly blocks accommodation for near vision (cycloplegia).
Case-based answers
A Reduced drainage of aqueous humour through the trabecular meshwork into the canal of Schlemm and the episcleral veins.
B Beta-adrenoceptor antagonists or prostaglandin analogues are the drugs of first choice for open-angle glaucoma. Alpha2-adrenoceptor agonists, carbonic anhydrase inhibitors or muscarinic agonists could also be used.
C Beta-adrenoceptor antagonists: avoid in asthma, bradycardia, heart block, heart failure. Prostaglandin analogues: avoid in pregnancy and asthma. Alpha2-adrenoceptor agonists: avoid in severe cardiovascular disease. Carbonic anhydrase inhibitors: avoid in pregnancy; they can cause hypokalaemia and electrolyte imbalance. Muscarinic agonists: avoid in conjunctival or corneal damage, cardiac disease, asthma.
Compendium: drugs used in the eye
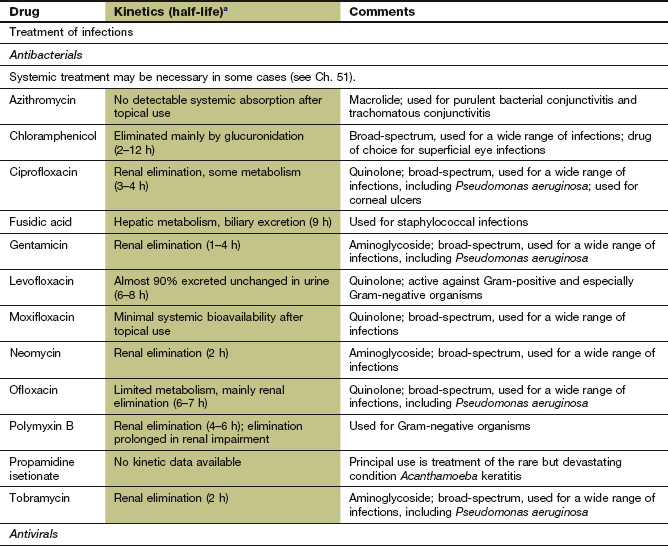
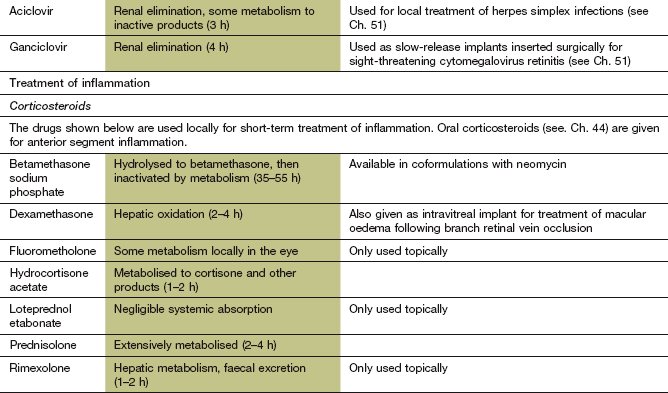
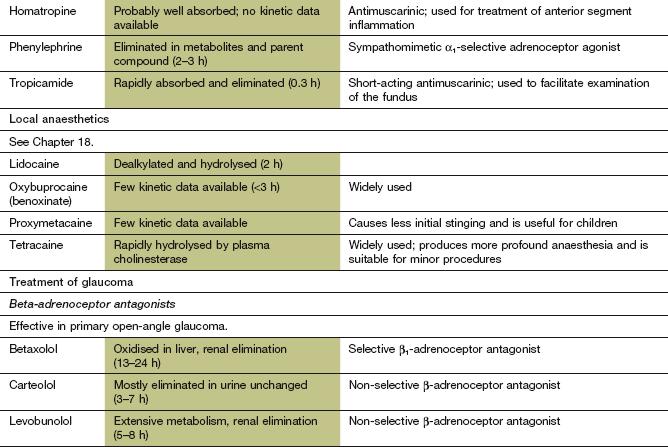
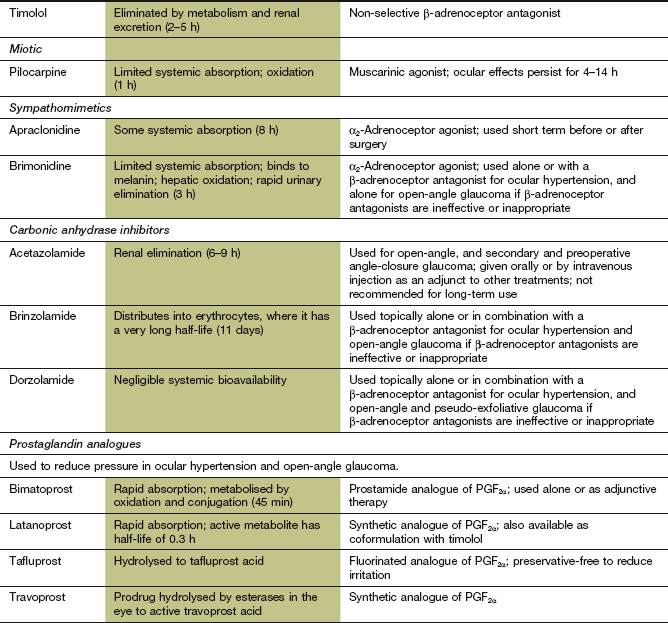
aThe half-life data are systemic data following absorption into the general circulation; the duration of local action will depend on the rate of uptake by, and removal from, the eye. Drugs are usually given topically to reduce unwanted systemic effects.
Bielory, L. Ocular allergy guidelines. Drugs. 2002;62:1611–1634.
Chakravarthy, U, Evans, J, Rosenfeld, PJ. Age related macular degeneration. BMJ. 2010;340:c981.
Ghate, D, Edelhauser, HF. Barriers to glaucoma drug delivery. J Glaucoma. 2008;17:147–156.
Hylton, C, Robin, AL. Update on prostaglandin analogs. Curr Opin Ophthalmol. 2003;14:65–69.
Ishida, N, Odani-Kawabata, N, Shimazaki, A, et al. Prostanoids in the therapy of glaucoma. Cardiovasc Drug Rev. 2006;24:1–10.
Jager, RD, Mieler, WF, Miller, JW. Age-related macular degeneration. N Engl J Med. 2008;358:2606–2617.
Quigley, HA. Glaucoma. Lancet. 2011;377:1362–1377.
Saw, S-M, Gazzard, G, Friedman, DS. Interventions for angle-closure glaucoma. An evidence-based update. Ophthalmology. 2003;110:1869–1879.
Singh, A. Medical therapy of glaucoma. Ophthalmol Clin North Am. 2005;18:397–408.
Takeda, AL, Colquitt, J, Clegg, AJ, et al. Pegaptanib and ranibizumab for neovascular age-related macular degeneration: a systematic review. Br J Ophthalmol. 2007;91:1177–1182.