Alster, TS, Railan, D. Laser treatment of vascular birthmarks. J Craniofac Surg. 2006;17(4):720–723.
Altimier, L, Lutes, L. Cobedding multiples. Newborn Infant Nurs Rev. 2001;1(4):205–206.
American Academy of Pediatrics, Committee on Infectious Diseases, Pickering L, eds. Red book: 2006 report of the Committee on Infectious Diseases, ed 27, Elk Grove, Ill: The Academy, 2006.
American Academy of Pediatrics. Update on newborn screening and treatment for congenital hypothyroidism. Pediatrics. 2006;117(6):2290–2303.
American Academy of Pediatrics. Breastfeeding and the use of human milk. Pediatrics. 2005;115(2):496–506.
American Academy of Pediatrics, Task Force on Sudden Infant Death Syndrome. The changing concept of sudden infant death syndrome: diagnostic coding shifts, controversies regarding the sleeping environment, and new variables to consider in reducing risk. Pediatrics. 2005;116(5):1245–1255.
American Academy of Pediatrics, Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation (clinical practice guideline). Pediatrics. 2004;114(1):297–316.
American Academy of Pediatrics, Committee on Injury and Poison Prevention. Selecting and using the most appropriate car safety seats for growing children: guidelines for counseling parents. Pediatrics. 2002;109(3):550–553.
American Academy of Pediatrics, Committee on Bioethics. Ethical issues with genetic testing in pediatrics. Pediatrics. 2001;107(6):1451–1455.
American Academy of Pediatrics. Safe transportation of newborns at hospital discharge. Pediatrics. 1999;104(4):986–987.
American Academy of Pediatrics, American College of Obstetricians and Gynecologists. Guidelines for perinatal care, ed 6. Elk Grove Village, Ill: The Academy, 2007.
American Heart Association. Guidelines for cardiopulmonary and emergency cardiovascular care, part 13, Neonatal resuscitation guidelines. Circulation. 2005;112(24 Suppl):IV118–IV195.
American Heart Association, American Academy of Pediatrics. 2005 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care of pediatric and neonatal patients: neonatal resuscitation guidelines. Pediatrics. 2006;117(5):e1029–e1038.
Anderson, GC. Kangaroo care of the premature infant. In: Goldson E, ed. Nurturing the premature infant: developmental interventions in the neonatal intensive care nursery. New York: Oxford University Press, 1999.
Arendt, R, Angelopoulos, J, Salvator, A, et al. Motor development of cocaine-exposed children at age two years. Pediatrics. 1999;103(1):86–92.
Askin, DF, Diehl-Jones, B. Liver, part III, Pathophysiology of liver dysfunction. Neonatal Netw. 2003;22(3):5–15.
Askin, DF, Diehl-Jones, B. Cocaine: effects of in utero exposure on the fetus and newborn. J Perinat Neonatal Nurs. 2001;14(4):83–102.
Aziz, N, Baron, EJ, D’Souza, H, et al. Comparison of rapid intrapartum screening methods for group B streptococcal vaginal colonization. J Matern Fetal Neonatal Med. 2005;18(4):225–229.
Bandstra, ES, Accornero, VH. Infants of substance abusing mothers. In Martin RJ, Fanaroff AA, Walsh MC, eds.: Fanaroff and Martin’s neonatal-perinatal medicine: diseases of the fetus and infant, ed 8, St Louis: Mosby, 2006.
Barrington, KJ, Finer, NN. Inhaled nitric oxide for preterm infants: a systematic review. Pediatrics. 2007;120(5):1088–1099.
Bateman, DA, Chiriboga, CA. Dose-response effect of cocaine on newborn head circumference. Pediatrics. 2000;106(3):e33.
Beachy, JM. Investigating jaundice in the newborn. Neonatal Netw. 2007;26(5):327–333.
Beauman, SS, Swanson, A. Neonatal infusion therapy: preventing complications and improving outcomes. Newborn Infant Nurs Rev. 2006;16(4):193–201.
Bhutani, VK, Gourley, GR, Adler, S, et al. Noninvasive measurement of total serum bilirubin in a multiracial predischarge newborn population to assess the risk of severe hyperbilirubinemia. Pediatrics. 2000;106(2):e17.
Bhutani, VK, Johnson, LH, Keren, R. Diagnosis and management of hyperbilirubinemia in the term neonate: for a safer first week. Pediatr Clin North Am. 2004;51(4):843–861.
Bhutani, VK, Johnson, L, Sivieri, EM. Predictive ability of a predischarge hour-specific serum bilirubin for subsequent significant hyperbilirubinemia in healthy term and near-term newborns. Pediatrics. 1999;103(1):6–14.
Bin-Nun, A, Bromiker, R, Wilschanski, M, et al. Oral probiotics prevent necrotizing enterocolitis in very low birth weight neonates. J Pediatr. 2005;147(2):143–146.
Blackburn, ST. Maternal, fetal, and neonatal physiology: a clinical perspective, ed 3. Philadelphia: Saunders, 2007.
Blake, WW, Murray, JA. Heat balance. In Merenstein GB, Gardner SL, eds.: Handbook of neonatal intensive care, ed 6, St Louis: Mosby, 2006.
Boney, CM, Verma, A, Tucker, R, et al. Metabolic syndrome in childhood: association with birth weight, maternal obesity, and gestational diabetes mellitus. Pediatrics. 2005;115(3):e290–e296.
Boo, NY, Foong, KW, Mahdy, ZA, et al. Risk factors associated with subaponeurotic haemorrhage in full-term infants exposed to vacuum extraction. Br J Obstet Gynaecol. 2005;112:1516–1521.
Brown, ZA, Wald, A, Morrow, RA, et al. Effect of serologic status and cesarean delivery on transmission rates of herpes simplex virus from mother to infant. JAMA. 2003;289:203–209.
Byers, JF, Waugh, WR, Lowman, LB. Sound level exposure of high-risk infants in different environmental conditions. Neonatal Netw. 2006;25(1):25–32.
Cambell, S. Prenatal cocaine exposure and neonatal/infant outcomes. Neonatal Netw. 2003;22(1):19–21.
Carver, JD, Wu, PY, Hall, RT, et al. Growth of preterm infants fed nutrient-enriched or term formula after hospital discharge. Pediatrics. 2001;107(4):683–689.
Cashore, WJ. Bilirubin and jaundice in the micropremie. Clin Perinatol. 2000;27(1):171–179.
Centers for Disease Control and Prevention. Enterobacter sakazakii infections associated with the use of powdered infant formula—Tennessee, 2001. MMWR. 2002;51(14):98–300.
Centers for Disease Control and Prevention. Prevention of perinatal group B streptococcal disease: revised guidelines. MMWR. 2002;51(RR11):1–22.
Chiriboga, CA, Brust, JC, Bateman, D, et al. Drug-response effect on fetal cocaine exposure on newborn neurologic function. Pediatrics. 1999;103(1):79–85.
Chiriboga, CA, Kuhn, L, Wasserman, GA. Prenatal cocaine exposures and dose-related cocaine effects on infant tone and behavior. Neurotoxicol Teratol. 2007;29(3):323–330.
Chomchai, C, Na Manorom, N, Watanarungasan, P, et al. Methamphetamine abuse during pregnancy and its impact on neonates born at Siriraj Hospital, Bangkok, Thailand. Southeast Asian J Trop Med Public Health. 2004;35(1):228–231.
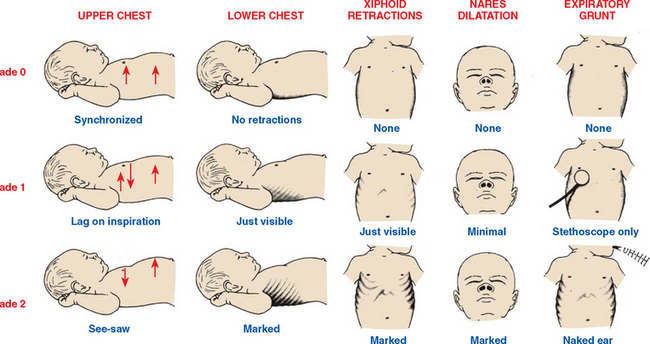
Cifuentes, J, Segars, AH, Carlo, W. Respiratory system management and complications. In Kenner C, Lott J, eds.: Comprehensive neonatal nursing: a physiologic perspective, ed 3, Philadelphia: Saunders, 2003.
Conde-Agudelo, A, Diaz-Rossello, JL, Belizan, JM. Kangaroo mother care to reduce morbidity and mortality in low birthweight infants, Cochrane Neonatal Review. http://www.nichd.nih.gov/cochraneneonatal/Vickers/Vickers.htm, 2000. [retrieved June 20, 2007, from].
Conlon, JD, Drolet, BA. Skin lesions in the neonate. Pediatr Clin North Am. 2004;51(4):863–888. [vii-viii,].
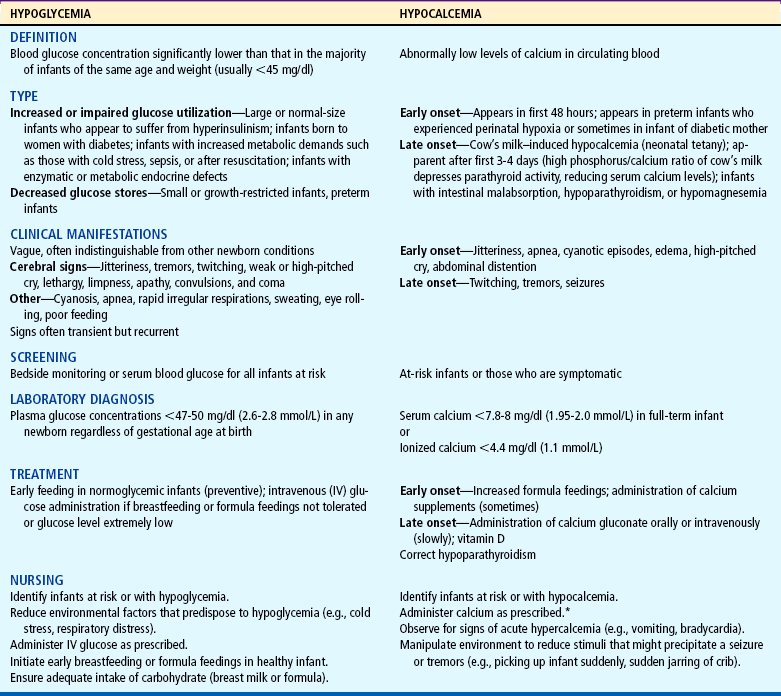
Cornblath, M, Hawdon, JM, Williams, A, et al. Controversies regarding definition of neonatal hypoglycemia: suggested operational thresholds. Pediatrics. 2000;105(5):1141.
Cowett, RM, Loughead, JL. Neonatal glucose metabolism: differential diagnoses, evaluation, and treatment of hypoglycemia. Neonatal Netw. 2002;21(4):9–19.
Crocker, E. Meth’s burning issues. Nurse Week, Heartland Ed. 2005;6(8):22–23.
Davis, PG, Henderson-Smart, DJ, Nasal continuous positive airways pressure immediately after extubation for preventing morbidity in preterm infants. Cochrane Database Syst Rev 2003;2:CD000143.
Delaney-Black, V, Cobington, C, Templin, T, et al. Prenatal cocaine exposure and child behavior. Pediatrics. 1998;102(4):945–950.
DellaPorta, K, Aforismo, D, Butler-O’Hara, M. Co-bedding of twins in the neonatal intensive care. Pediatr Nurs. 1998;24(6):529–531.
Deshpande, S, Ward Platt, M. The investigation and management of neonatal hypoglycaemia. Semin Fetal Neonatal Med. 2005;10(4):351–361.
Dodd, VL. Implications of kangaroo care for growth and development in preterm infants. J Obstet Gynecol Neonatal Nurs. 2005;34(2):218–232.
Dohil, MA, Baugh, WP, Eichenfield, LF. Vascular and pigmented birthmarks. Pediatr Clin North Am. 2000;47(4):783–812.
Doumouchtsis, SK, Arulkumaran, S. Head injuries after instrumental vaginal deliveries. Curr Opin Obstet Gynecol. 2006;18(2):129–134.
Drummond, GS, Kappas, A. Chemoprevention of severe neonatal hyperbilirubinemia. Semin Perinatol. 2004;28(5):365–368.
Ebrahim, SH, Gfoerer, J. Pregnancy-related substance use in the United States during 1996-1998. Obstet Gynecol. 2003;101(2):374–379.
Edwards, WH, Conner, JM, Soll, RF, et al. The effect of prophylactic ointment therapy on nosocomial sepsis rates and skin integrity in infants with birth weights of 501 to 1000 g. Pediatrics. 2004;113(5):1195–1203.
Engle, WA. A recommendation for the definition of “late preterm” (near-term) and the birth weight–gestational age classification system. Semin Perinatol. 2006;30(1):2–7.
Engle, WA, Tomashek, KM, Wallman, C, et al. Late-preterm infants: a population at risk. Pediatrics. 2007;120(6):1390–1401.
Eyler, FD, Behnke, M. Early development of infants exposed to drugs prenatally. Clin Perinatol. 1999;26(1):107–150.
Eyler, FD, Behnke, M, Conlon, M. Birth outcome from a prospective, matched study of prenatal crack/cocaine use, part II, Interactive and dose effects on neurobehavioral assessment. Pediatrics. 1998;101(2):237–241.
Eyler, FD, Behnke, M, Wobie, K, et al. Relative ability of biologic specimens and interviews to detect prenatal cocaine use. Neurotoxicol Teratol. 2005;27(4):677–687.
Finer, NN. Surfactant use for neonatal lung injury: beyond respiratory distress syndrome. Paediatr Respir Rev. 2004;5(Suppl A):S289–S297.
Finnegan, LP. Neonatal abstinence. In: Nelson N, ed. Current therapy in neonatal perinatal medicine 1985-1986. Toronto: Decker, 1985.
Forsythe, SJ. Enterobacter sakazakii and other bacteria in powdered infant milk formula. Maternal Child Nutrition. 2005;1(1):44–50.
Frank, DA, Jacobs, RR, Beeghly, M, et al. Level of prenatal cocaine exposure and scores on the Bayley Scales of Infant Development: modifying effects of caregiver, early intervention, and birth weight. Pediatrics. 2002;110(6):1143–1152.
Gardner, SL, Hauser, P, Merenstein, GB. Grief and perinatal loss. In Merenstein GB, Gardner SL, eds.: Handbook of neonatal intensive care, ed 6, St Louis: Mosby, 2006.
Gardner, SL, Snell, BJ, Lawrence, RA. Breastfeeding the neonate with special needs. In Merenstein GB, Gardner SL, eds.: Handbook of neonatal intensive care, ed 6, St Louis: Mosby, 2006.
Gray, L, Watt, L, Blass, EM, Skin-to-skin contact is analgesic in healthy newborns. Pediatrics 2000;105(1):110–111. retrieved July 1, 2007, from http://www.pediatrics.org/cgi/content/full/105/1/e14
Greene, CM, Goodman, MH. Neonatal abstinence syndrome: strategies for care of the drug-exposed infant. Neonatal Netw. 2003;22(4):15–25.
Gupta, A, Della-Latta, P, Todd, B, et al. Outbreak of extended-spectrum beta-lactamase-producing Klebsiella pneumoniae in a neonatal intensive care unit linked to artificial nails. Infect Control Hosp Epidemiol. 2004;25(3):210–215.
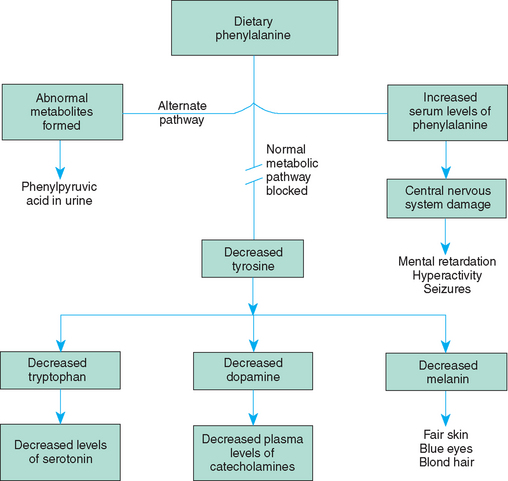
Hellekson, KL. Practice guidelines: NIH consensus statement on phenylketonuria. Am Fam Physician. 2001;63(7):1430–1432.
Holditch-Davis, D, Blackburn, ST, VandenBerg, K. Newborn and infant neurobehavioral development. In: Kenner C, Lott J, eds. Comprehensive neonatal nursing: a physiologic perspective. Philadelphia: Saunders, 2003.
Howard-Salsman, KD. Car seat safety for high-risk infants. Neonatal Netw. 2006;25(2):117–129.
Hudic, I, Fatusic, Z, Sinanovic, O, et al. Etiological risk factors for brachial plexus palsy. J Matern Fetal Neonatal Med. 2006;19(10):655–661.
Huestis, MA, Choo, RE. Drug abuse’s smallest victims: in utero drug exposure. Forensic Sci Int. 2002;128(1-2):20–30.
Hung-Chih, L, Bai-Horng, S, An-Chyi, C, et al. Oral probiotics reduce the incidence and severity of necrotizing enterocolitis in very low birth weight infants. Pediatrics. 2005;115(1):1–4.
Hurd, YL, Wang, X, Anderson, V, et al. Marijuana impairs growth in mid-gestation fetuses. Neurotoxicol Teratol. 2005;27(2):221–229.
International Human Genome Sequencing Consortium. Finishing the euchromatic sequence of the human genome. Nature. 2004;431:931–945.
Jansen, JL. A bereavement model for the intensive care nursery. Neonatal Netw. 2003;22(3):17–23.
Johnson, CB. Head, eyes, ears, nose, mouth and neck assessment. In Tappero EP, Honeyfield ME, eds.: Physical assessment of the newborn: a comprehensive approach to the art of physical assessment, ed 3, Santa Rosa, Calif: NICU Ink, 2003.
Johnson, K, Gerada, C, Greenough, A. Treatment of neonatal abstinence syndrome. Arch Dis Child Fetal Neonatal Educ. 2003;88(1):F2–F5.
Jones, KL. Smith’s recognizable patterns of human malformation, ed 4. Philadelphia: Saunders, 2006.
Joyner, B, Soto, MA, Adam, HM. Brachial plexus injury. Pediatr Rev. 2006;27(6):238–239.
Kandall, SR. Treatment strategies for drug-exposed neonates. Clin Perinatol. 1999;26(1):231–243.
Kato, T, Mittal, N, Nishida, S, et al. The role of intestinal transplantation in the management of babies with extensive gut resections. J Pediatr Surg. 2003;38(2):145–149.
Kaye, CI, Committee on Genetics, Accurso, F, et al. Newborn screening fact sheets. Pediatrics. 2006;118(3):e934–e963.
Kenner, C. Resuscitation and stabilization of the newborn. In Kenner C, Lott JW, eds.: Comprehensive neonatal nursing, ed 3, Philadelphia: Saunders, 2003.
Kimberlin, DW. Herpes simplex virus infections of the newborn. Semin Perinatol. 2007;31(1):19–25.
Kimberlin, DW. Herpes simplex virus infections in neonates and early childhood. Semin Pediatr Infect Dis. 2005;16:271–281.
Kirkpatrick, JM, Alexander, J, Cain, RM. Recovering urine from diapers: are test results accurate? MCN. 1997;22(2):96–102.
Kliegman, RM. The relationship of neonatal feeding practices and the pathogenesis and prevention of necrotizing enterocolitis. Pediatrics. 2003;111(3):671–672.
Koren, G, Nulman, I, Rovet, J, et al. Long-term neurodevelopmental risks in children exposed in utero to cocaine: the Toronto adoption study. Ann NY Acad Sci. 1998;846:306–312.
Laborada, G, Rego, M, Jain, A, et al. Diagnostic value of cytokines and C-reactive protein in the first 24 hours of neonatal sepsis. Am J Perinatol. 2003;20(8):491–501.
LaMar, K, Dowling, DA. Incidence of infection for preterm twins cared for in cobedding in the neonatal intensive-care unit. J Obstet Gynecol Neonatal Nurs. 2006;35(2):193–198.
Lashley, FR. Newborn screening: new opportunities and new challenges. Newborn Infant Nurs Rev. 2002;2(4):228–242.
Lawrence, RA, Lawrence, RM. Breastfeeding: a guide for the medical profession, ed 6. St Louis: Mosby, 2005.
Lester, BM, Tronick, EZ, Brazelton, TB. The Neonatal Intensive Care Unit Network Neurobehavioral Scale procedures. Pediatrics. 2004;113(3 Suppl):641–667.
L’Herault, J, Petroff, L, Jeffrey, J. The effectiveness of a thermal mattress in stabilizing and maintaining body temperature during the transport of very low–birth weight newborns. Appl Nurs Res. 2001;14(4):210–219.
Lucas, A, Fewtrell, MS, Morley, R, et al. Randomized trial of nutrient-enriched formula versus standard formula for postdischarge preterm infants. Pediatrics. 2001;108(3):703–711.
Ludington-Hoe, SM, Hosseini, R, Torowicz, DL. Skin-to-skin contact (kangaroo care) analgesia for preterm infant heel stick. AACN Clin Issues. 2005;16(3):373–387.
Lund, CH, Kuller, JM. Assessment and management of the integumentary system. In Kenner C, Lott JW, eds.: Comprehensive neonatal nursing, ed 3, Philadelphia: Saunders, 2003.
Maisels, MJ. Jaundice. In: MacDonald MG, Seshia MMK, Mullett MD, eds. Avery’s neonatology. Philadelphia: Lippincott, 2005.
Maisels, MJ, Watchko, JF. Treatment of jaundice in low birthweight infants. Arch Dis Child Fetal Neonatal Educ. 2003;88(6):F459–F463.
Malanga, CJ, Kosofsy, BE. Mechanism of action of drugs of abuse on the developing fetal brain. Clin Perinatol. 1999;26(1):17–37.
Mangurten, HH. Birth injuries. In Martin RJ, Fanaroff AA, Walsh MC, eds.: Fanaroff and Martin’s neonatal-perinatal medicine: diseases of the fetus and infant, ed 8, St Louis: Mosby, 2006.
Marcellus, L. Care of substance-exposed infants: the current state of practice in Canadian hospitals. J Perinat Neonatal Nurs. 2002;16(3):51–68.
Mari, G. Noninvasive diagnosis by Doppler ultrasonography of fetal anemia due to maternal red-cell isoimmunization. N Engl J Med. 2000;342(1):9–14.
Matalon, R, Michaels-Matalon, K, Koch, R, et al. Response of patients with phenylketonuria in the US to tetrahydrobiopterin. Mol Genet Metab. 2005;86(Suppl 1):S17–S21.
Mazela, J, Merritt, TA, Finer, NN. Aerosolized surfactants. Curr Opin Pediatr. 2007;19(2):155–162.
McCain, GC. An evidence-based guideline for introducing oral feeding to healthy preterm infants. Neonatal Netw. 2003;22(5):45–50.
McCain, GC, Ludington-Hoe, SM, Swinth, JY, et al. Heart rate variability responses of a preterm infant to kangaroo care. J Obstet Gynecol Neonatal Nurs. 2005;34(6):689–694.
McCall, EM, Alderdice, FA, Halliday, HL, et al, Interventions to prevent hypothermia at birth in preterm and/or low birthweight babies. Cochrane Database Syst Rev 2005;1:CD004210.
McCance, K, Huether, S. Pathophysiology: the biological basis for disease in infants and children, ed 5. St Louis: Mosby, 2006.
McPhee, SJ, Ganong, WF. Pathophysiology of disease: an introduction to clinical medicine, ed 5. New York: Lang Medical Books, 2006.
Merenstein, GB, Gardner, SL. Handbook of neonatal intensive care, ed 6. St Louis: Mosby, 2006.
Merrill, J, Ballard, R. Pulmonary surfactant for neonatal respiratory disorders. Curr Opin Pediatr. 2003;15(2):149–154.
Messinger, DS, Bauer, CR, Das, A, et al. The maternal lifestyle study: cognitive, motor, and behavioral outcomes of cocaine-exposed and opiate-exposed infants through three years of age. Pediatrics. 2004;113(6):1677–1685.
Mills, JF, Tudehope, D, Fibreoptic phototherapy for neonatal jaundice. Cochrane Database Syst Rev 2005;1:CD002060.
Moise, KJ. Management of rhesus alloimmunization in pregnancy. Obstet Gynecol. 2002;100(3):600–611.
Moolenaar, RL, Crutcher, JM, San Joaquin, VH, et al. A prolonged outbreak of Pseudomonas aeruginosa in a neonatal intensive care unit: did staff fingernails play a role in disease transmission? Infect Control Hosp Epidemiol. 2000;21(2):80–85.
Moore, KA, Coker, K, DuBuisson, AB, et al. Implementing potentially better practices for improving family-centered care in neonatal intensive care units: successes and challenges. Pediatrics. 2003;111(4):e450–e460.
Morrow, CE, Culbertson, JL, Accornero, VH, et al. Learning disabilities and intellectual functioning in school-aged children with prenatal cocaine exposure. Dev Neuropsychol. 2006;30(3):905–931.
Mundy, CA. Intravenous immunoglobulin in the management of hemolytic disease of the newborn. Neonatal Netw. 2005;24(6):17–24.
Neal, JL. RhD isoimmunization and current management modalities. J Obstet Gynecol Neonatal Nurs. 2001;30(6):589–607.
Nussbaum, RL, McInnes, RR, Willard, HF. Thompson and Thompson genetics in medicine, ed 6 (rev reprint). Philadelphia: Saunders, 2004.
Paige, PL, Moe, PC. Neurologic disorders. In Merenstein GB, Gardner SL, eds.: Handbook of neonatal intensive care, ed 6, St Louis: Mosby, 2006.
Parker, LA, Montrowl, SJ. Neonatal herpes infection: a review. Newborn Infant Nurs Rev. 2004;4(1):62–69.
Pinelli, J, Symington, A, Non-nutritive sucking for promoting physiologic stability and nutrition in preterm infants. Cochrane Database Syst Rev 2005;4:CD001071.
Plessinger, M. Prenatal exposure to amphetamines. Obstet Gynecol Clin North Am. 1998;25(1):119–138.
Polak, JD, Ringler, N, Daugherty, B. Unit based procedures: impact on the incidence of nosocomial infections in the newborn intensive care unit. Newborn Infant Nurs Reviews. 2004;4(1):38–45.
Porter, ML, Dennis, BL. Hyperbilirubinemia in the term newborn. Am Fam Physician. 2002;65(4):599–606. [613-614,].
Premji, SS, Paes, B, Jacobson, K, et al. Evidence-based feeding guideline for very low birthweight infants. Adv Neonatal Care. 2002;2(1):5–18.
Price, AE, Ditaranto, P, Yaylali, I, et al. Botulinum toxin type A as an adjunct to the surgical treatment of the medial rotation deformity of the shoulder in birth injuries of the brachial plexus. J Bone Joint Surg Br. 2007;89(3):327–329.
Putta, LV, Spencer, JP. Assisted vaginal delivery using the vacuum extractor. Am Fam Physician. 2000;62(6):1316–1320.
Ramsey, PS, Goldenberg, PL. Obstetric management of prematurity. In Martin RJ, Fanaroff AA, Walsh MC, eds.: Fanaroff and Martin’s neonatal-perinatal medicine: diseases of the fetus and infant, ed 8, St Louis: Mosby, 2006.
Read, CY. The demands of biochemical genetic disorders: a survey of mothers of children with mitochondrial disease or phenylketonuria. J Pediatr Nurs. 2003;18(3):181–186.
Reynolds, RM, Thureen, PJ. Special circumstances: trophic feeds, necrotizing enterocolitis and bronchopulmonary dysplasia. Semin Fetal Neonatal Med. 2007;12(1):64–70.
Richardson, GA, Hamel, SC, Goldschmidt, L, et al. The effects of prenatal cocaine use on neonatal neurobehavioral status. Neurotoxicol Teratol. 1996;18(5):519–528.
Sarici, SU, Yurdakok, M, Serdar, MA, et al. An early (sixth-hour) serum bilirubin measurement is useful in predicting the development of significant hyperbilirubinemia and severe ABO hemolytic disease in a selective high-risk population of newborns with ABO incompatibility. Pediatrics. 2002;109(4):e53.
Saugstad, OD. Optimal oxygenation at birth and in the neonatal period. Neonatology. 2007;91(4):319–322.
Saugstad, OD, Ramji, S, Irani, SF, et al. Resuscitation of newborn infants with 21% or 100% oxygen: follow-up at 18 and 24 months. Pediatrics. 2003;112(2):296–300.
Schanler, RJ, Shulman, RJ, Lau, C, et al. Feeding strategies for premature infants: randomized trial of gastrointestinal priming and tube-feeding method. Pediatrics. 1999;103(2):434–439.
Schultze, A, Lindner, M, Kohlmüller, D, et al. Expanded newborn screening for inborn errors of metabolism by electrospray ionization–tandem mass spectrometer: results, outcomes, and implications. Pediatrics. 2003;111(6):1399–1406.
Selva, KA, Harper, A, Downs, A, et al. Neurodevelopmental outcomes in congenital hypothyroidism: comparison of dose and time to reach target T4 and TSH. J Pediatr. 2005;147:775–780.
Sgro, M, Shah, V, Campbell, D. Canadian Paediatric Surveillance Program: Challenge of early discharge: newborn assessment for jaundice. http://www.cps.ca/English/Surveillance/CPSP/Resources/NHS.htm, 2005. [retrieved June 28, 2007, from].
Shaw, N. Assessment and management of the hematologic system. In Kenner C, Lott J, eds.: Comprehensive neonatal nursing: a physiologic perspective, ed 3, Philadelphia: Saunders, 2003.
Singer, LT, Arendt, R, Minnes, S, et al. Cognitive and motor outcomes of cocaine-exposed infants. JAMA. 2002;287(15):1952–1960.
Singer, LT, Minnes, S, Short, E, et al. Cognitive outcomes of preschool children with prenatal cocaine exposure. JAMA. 2004;291(20):2448–2456.
Smith, L, Yonekura, ML, Wallace, T, et al. Effects of prenatal methamphetamine exposure on fetal growth and drug withdrawal symptoms in infants born at term. J Devel Behav Pediatr. 2003;24(1):17–23.
Steffensrud, S. Hyperbilirubinemia in term and near-term infants: kernicterus on the rise? Newborn Infant Nurs Rev. 2004;4(4):191–202.
Stevens, TP, Sinkin, RA. Surfactant replacement therapy. Chest. 2007;131(5):1577–1582.
Stoll, BJ, Hansen, N, Fanaroff, AA, et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics. 2002;110(2 Pt 1):285–291.
Stoll, BJ, Hansen, NI, Higgins, RD, et al. Very low birth weight preterm infants with early onset neonatal sepsis: the predominance of gram-negative infections continues in the National Institute of Child Health and Human Development Neonatal Research Network, 2002-2003. Pediatr Infect Dis J. 2005;24(7):635–639.
Stoll, BJ. Metabolic disturbances. In Behrman R, ed.: Nelson textbook of pediatrics, ed 18, Philadelphia: Saunders, 2007.
Symington, A, Pinelli, J. Developmental care for promoting development and preventing morbidity in preterm infants (Cochrane Review). In: The Cochrane Library. Oxford: Update Software; 2003. [Issue 1].
Tappero, E. Musculoskeletal system assessment. In Tappero E, Honeyfield MA, eds.: Physical assessment of the newborn, ed 3, Santa Rosa, Calif: NICU Ink, 2003.
Thayyil, S, Marriott, L. Can transcutaneous bilirubinometry reduce the need for serum bilirubin estimations in term and near term infants? Arch Dis Child. 2005;90(12):1311–1312.
Tronick, EZ, Beeghly, M. Prenatal cocaine exposure, child development, and the compromising effects of cumulative risk. Clin Perinatol. 1999;26(1):151–171.
Tyson, JE, Kennedy, KA, Trophic feedings for parenterally fed infants. Cochrane Database Syst Rev 2005;3:CD000504.
Uchil, D, Arulkumaran, S. Neonatal subgaleal hemorrhage and its relationship to delivery by vacuum extraction. Obstet Gynecol Surv. 2003;58:687–693.
Uhing, MR. Management of birth injuries. Pediatr Clin North Am. 2004;51(4):1169–1186.
Vento, M, Saugstad, O. Oxygen therapy. In Martin RJ, Fanaroff AA, Walsh MC, eds.: Fanaroff and Martin’s neonatal-perinatal medicine: diseases of the fetus and infant, ed 8, St Louis: Mosby, 2006.
Volante, E, Moretti, S, Pisani, F, et al. Early diagnosis of bacterial infection in the neonate. J Matern Fetal Med. 2004;16(Suppl 2):13–16.
Volpe, JJ. Neurology of the newborn, ed 4. Philadelphia: Saunders, 2001.
Wagner, C, Katikaneni, LD, Cox, TH, et al. The impact of prenatal drug exposure on the neonate. Obstet Gynecol Clin North Am. 1998;25(1):169–194.
Walter, JH, White, FJ. Blood phenylalanine control in adolescents with phenylketonuria. Int J Adolesc Med Health. 2004;16(1):41–45.
Westrup, B, Sizun, J, Lagercrantz, H. Family-centered developmental supportive care: a holistic and humane approach to reduce stress and pain in neonates. J Perinatol. 2007;27(Suppl 1):S12–S18.
Wheeler, BJ. Kernicterus: ancient history or ongoing threat? Mother Baby J. 2000;5(2):21–30.
Witt, C. Skin assessment. In Tappero EP, Honeyfield ME, eds.: Physical assessment of the newborn, ed 3, Petaluma, Calif: NICU Ink, 2003.
Zahorodny, W, Rom, C, Whitney, W, et al. The neonatal withdrawal inventory: a simplified score of newborn withdrawal. Devel Behav Pediatr. 1998;19(2):89–93.
Zlatunich, CO, Packman, S. Galactosaemia: early treatment with an elemental formula. J Inherit Metab Dis. 2005;28:163–168.
 FAMILY FOCUS
FAMILY FOCUS CRITICAL THINKING EXERCISE
CRITICAL THINKING EXERCISE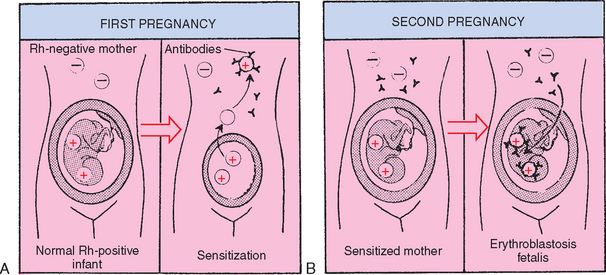

 FAMILY FOCUS
FAMILY FOCUS