Health Problems of School-Age Children and Adolescents
On completion of this chapter the reader will be able to:
 Outline a care plan for the child or adolescent with a health problem.
Outline a care plan for the child or adolescent with a health problem.
 Demonstrate an understanding of the types, causes, and prevention of sports injuries in middle childhood and adolescence.
Demonstrate an understanding of the types, causes, and prevention of sports injuries in middle childhood and adolescence.
 Describe the most common causes of physical growth or maturation failure in later childhood.
Describe the most common causes of physical growth or maturation failure in later childhood.
 Demonstrate an understanding of common disorders of the male and female reproductive systems.
Demonstrate an understanding of common disorders of the male and female reproductive systems.
 Demonstrate an understanding of health problems related to adolescent sexuality.
Demonstrate an understanding of health problems related to adolescent sexuality.
 Outline a plan for discussing sexuality issues with adolescents.
Outline a plan for discussing sexuality issues with adolescents.
 Outline a care plan for the child or adolescent with an eating disorder.
Outline a care plan for the child or adolescent with an eating disorder.
 Discuss the manifestations and nursing management of selected emotional or behavioral problems.
Discuss the manifestations and nursing management of selected emotional or behavioral problems.
PROBLEMS RELATED TO ELIMINATION
Enuresis (bed-wetting), or nocturnal enuresis, is a common and troublesome disorder that is defined as intentional or involuntary passage of urine into bed (usually at night) in children who are beyond the age when voluntary bladder control should normally have been acquired. The inappropriate voiding of urine must occur at least twice a week for at least 3 months, and the chronologic or developmental age of the child must be at least 5 years. The predominant symptom is urgency that is immediate and accompanied by acute discomfort, restlessness, and urinary frequency. Enuresis is more common in boys; nocturnal bed-wetting usually ceases between 6 and 8 years of age. Enuresis can also be defined as primary (bed-wetting in children who have never been dry for extended periods) or secondary (the onset of wetting after a period of established urinary continence). The passage of urine may occur only during nighttime sleep with the child remaining dry during the day (monosymptomatic); or it may be polysymptomatic, wherein the child has daytime urinary urgency, an occasional daytime accident, in conjunction with other conditions such as sleep apnea, urinary tract infection, neurologic impairment, constipation, or emotional stressors (Berry, 2006). The nocturnal, monosymptomatic type is most common. The condition may be particularly distressing to adolescents, who may refuse therapy. Although enuresis may occur during the daytime, the following discussion primarily focuses on nocturnal enuresis.
Before psychogenic factors are considered, organic causes that may be related to enuresis should be ruled out. These include structural disorders of the urinary tract; urinary tract infection; neurologic deficits; disorders that increase the normal output of urine, such as diabetes; and disorders that impair the concentrating ability of the kidneys, such as chronic renal failure or sickle cell disease. A bladder volume of 300 to 350 ml (10 to 12 ounces) is sufficient to hold a night’s urine. Normal bladder capacity (in ounces) is the child’s age plus 2. In other cases the enuresis is influenced by emotional factors, although it is doubtful that they are causative factors. Parents report that these children sleep more soundly than other children; however, the depth of sleep has not been identified as the cause of nocturnal enuresis (Berry, 2006). Nocturnal enuresis has a strong familial tendency.
Therapeutic techniques used to manage nocturnal enuresis include medications, bladder training, restriction or elimination of fluids after the evening meal, interruption of sleep to void, and various devices designed to establish a conditioned reflex response to waken the child at the initiation of voiding (alarms).
Three types of drugs are used to treat enuresis: tricyclic antidepressants, antidiuretics, and anticholinergics. A drug used frequently to inhibit urination is the tricyclic antidepressant imipramine. Another anticholinergic drug, oxybutynin, reduces uninhibited bladder contractions and may be helpful for children with daytime urinary frequency. Desmopressin (DDAVP) nasal spray, an analog of vasopressin, reduces nighttime urinary output to a volume less than functional bladder capacity. Drugs are usually considered second-line management, and parents should be cautioned not to think that these agents will cure the condition; parents are also advised of the drug’s side effects (Sethi, Bhargava, and Shipra, 2005).
Nursing Care Management
Regardless of the techniques used, the nurse can help both children and parents understand the problem of enuresis, the treatment plan, and the difficulties they may encounter in the process. The nurse can also provide consistent support and encouragement to help sustain both the child and the parents through the inconsistent and unpredictable treatment process. Parents need to understand that punishment is contraindicated because of its negative emotional impact and limited success in reducing the behavior. Positive reinforcement of the desired behavior may be beneficial (Sethi, Bhargava, and Shipra, 2005). Children need to believe that they are helping themselves, and they need to sustain feelings of confidence and hope.
Parents should also be taught to observe for side effects of any medications used. All children with primary enuresis should be encouraged to void before bedtime. Diapering should be avoided. Positive reinforcement in the form of keeping diaries to record dry nights has been effective in motivating children.
ENCOPRESIS
Encopresis is the repeated voluntary or involuntary passage of feces of normal or near-normal consistency in places not appropriate for that purpose according to the individual’s own sociocultural setting. The event must occur at least once per month for at least 3 months, and the chronologic or developmental age of the child must be at least 4 years. The fecal incontinence must not be caused by any physiologic effect, such as a laxative, or a general medical condition.
Primary encopresis is identified by age 4 when the child has not achieved fecal continence. Secondary encopresis is fecal incontinence occurring in a child older than 4 years of age after a period of established fecal continence. The disorder is more common in boys than in girls.
One of the most common causes of encopresis is constipation, which may be precipitated by environmental change. Chronic, severe constipation has a tendency to impair the usual movement and contractions of the colon, which can lead to fecal obstruction. Abnormalities in the digestive tract (e.g., Hirschsprung disease, anorectal lesions, malformations, and rectal prolapse) and medical conditions such as hypothyroidism, hypokalemia, hypercalcemia, lead intoxication, myelomeningocele, cerebral palsy, muscular dystrophy, and irritable bowel syndrome are also associated with constipation, which can lead to encopresis (Coughlin, 2003). Children with encopresis often feel ashamed and may wish to avoid situations that might lead to embarrassment. School performance and attendance are affected as the child’s offensive odor becomes a target for scorn and ridicule from classmates.
Therapeutic management consists of determining the cause of the soiling and using appropriate interventions to correct the problem. Diet, lubricants, and a toilet ritual that encourages the child to establish normal defecation are used. Fecal impaction is relieved by lubricants such as mineral oil; osmotic laxatives such as lactulose, sorbitol, or polyethylene glycol (PEG or MiraLAX); and magnesium hydroxide. Customary dosages are usually insufficient. Mineral oil should be avoided in children who have dysphagia or vomiting to prevent risk of aspiration. Dietary changes may be helpful, including elimination of milk and dairy products; consumption of increased amounts of high-fiber foods, such as fruits, vegetables, and cereals; and increased fluids. Behavioral therapy may be indicated to eliminate any fear that has developed as a result of painful defecation. Frequently, psychotherapeutic intervention with the child and the family becomes necessary.
Nursing Care Management
The nursing care of the child with encopresis involves education and support of the family and treatment of existing constipation. Education regarding the physiology of normal defecation, toilet training as a developmental process, and the treatment outlined for the particular family is essential to a successful outcome. Family counseling is directed toward reassurance that most problems resolve successfully, although relapses during periods of stress are possible (see Family Focus box).
HEALTH PROBLEMS RELATED TO SPORTS PARTICIPATION
Every sport has the potential for injury to the participant—whether the adolescent engages in serious competition or participates for enjoyment. Serious injury occurs most often during rough contact sports or to persons who are not physically prepared for the activity. Injuries also occur when the children’s or adolescents’ bodies are not suited to the sport, when their muscles and body systems (respiratory and cardiovascular) are not conditioned to endure physical stress, or when they lack the insight and judgment to recognize that an activity exceeds their physical abilities. Rapidly growing bones, muscles, joints, and tendons are especially vulnerable to unusual strain. More injuries occur during recreational sports participation than during organized athletic competition.
The environment and the sports or recreational equipment can also present risks (Fig. 17-1). Children who participate in physical activity or sports do so in many different environments: indoors and outdoors, on floors, on the ground and snow, on or beneath water surfaces, and sometimes in free air space. Most of these activities also involve equipment, which children and adolescents may not be physically mature enough to manage safely. A common example of this would include skateboarding when the child or adolescent does not take safety precautions and perceives increased risk-taking as a part of the sport.
Acute overload injuries are those that occur suddenly during an activity and produce immediate symptoms. A blow or overstretching, twisting, or sudden stress to tissues can cause these injuries. For descriptions and management of traumatic injuries see Chapter 31.
OVERUSE SYNDROMES
To excel in sports, the young athlete is forced to train longer, harder, and earlier in life than previously. The rewards are an increased level of fitness, better performance, faster times, and the satisfaction of attaining a personal goal. With the increase in the number of children participating in sports year-round, more overuse injuries are being seen in the pediatric age-group (Lord and Winell, 2004).
The risk of overuse injury is always present and can be related to several factors: training errors, muscle-tendon imbalance, anatomic malalignment (e.g., femoral anteversion, excessive lumbar lordosis, tibial torsion), incorrect footwear or playing surface, an associated disease state, and growth (growth cartilage is less resistant to microtrauma). Athletes who run extensively frequently experience shin splints. The ligaments tear away from the tibial shaft, and this creates the pain. Ice, rest, and nonsteroidal antiinflammatory drugs (NSAIDs), such as ibuprofen or naproxen, are the usual treatment. Shin splints are rarely serious.
Chronic pain in athletes is often associated with overuse injury, which can occur at any level of athletic participation. The common feature in overuse injuries is the repetitive microtrauma that occurs to a particular anatomic structure (Lord and Winell, 2004). Performing the same movements time and time again can cause several types of injury:
 Frictional, or rubbing of one structure against another
Frictional, or rubbing of one structure against another
 Tractional, or repeated pull on a ligament or tendon
Tractional, or repeated pull on a ligament or tendon
 Cyclic, or repetitive loading of impact forces (stress fractures)
Cyclic, or repetitive loading of impact forces (stress fractures)
The end result is inflammation of the involved structure with complaints of pain, tenderness, swelling, and disability.
Bursae, tendons, muscles, ligaments, joints, and bones are all subject to overuse. Plantar fasciitis is common in athletes, and Osgood-Schlatter disease is seen in children who do a lot of jumping. The occurrence of overuse-type injuries, such as sore shoulders and strained elbows, may indicate that too much is being requested of the child in too short a period.
Stress Fractures
Given the intensity and duration of sports training, many young athletes suffer stress fractures, especially after a recent increase in training regimens. These fractures occur as a result of repeated muscle contraction and are seen most often in sports involving repetitive weight bearing such as running, gymnastics, and basketball. They occur less often in swimming (in the upper extremities). Tibial fractures are most common.
The most common symptom of stress fracture is a sharp, persistent, progressive pain or a deep, persistent dull ache located over the bone. Sometimes there is pain on impact (heel strike), but the most important clinical sign is pain over the involved bony surface. Diagnosis is based on clinical observation. Plain radiographs are rarely diagnostic of stress fractures during the initial few weeks, since callus formation is not yet evident. Occasionally a bone scan may be needed and will indicate a “hot spot.”
Therapeutic Management
Development of inflammation is common to all overuse syndromes; therefore management involves rest or alteration of activities, physical therapy, and medication. Rest is the primary therapy, usually interpreted as reduced activity and the use of alternative exercise—not bed rest or immobilization with casting. The main purpose is to alleviate the repetitive stress that initiated the symptoms. It is important to keep the child or adolescent mobile, and training can be continued. Alternative exercise is selected that maintains conditioning without aggravating the injury. For example, pool running (treading water in the deep end of a pool) can use the same movements as running but without the weight bearing; bicycling, swimming, and rowing are viable alternatives.
Other modalities include cryotherapy and cold whirlpool baths. Sometimes taping, bracing, splinting, and other orthoses are employed, depending on the injury. NSAIDs are often prescribed to reduce inflammation and pain. Topical medications are of questionable value.
NURSE’S ROLE IN SPORTS FOR CHILDREN AND ADOLESCENTS
Nurses are often involved in sports activities in the areas of preparation and evaluation for activities, prevention of injury, treatment of injuries, and rehabilitation after injury. Selecting an appropriate sport for both recreation and competition is a joint effort of the adolescent, parents, and health professionals. The best approach to counseling children, adolescents, and parents regarding sports participation is to encourage activities that are most likely to provide pleasure and physical benefits throughout childhood and into adulthood. Exposure to a variety of activities is better for young children than limiting them to one sport. Parents should be cautioned against overcommitting children to sports activities so they have time for other activities.
When children sustain athletic injuries, nurses are often responsible for instructions regarding care. Instructions (e.g., schedule for appointments, application of ice, any restrictions in activity) should be clear and accompanied by written directions. The importance of taking medications as prescribed is emphasized, especially if medications are needed for an extended period and if adherence is an issue. Medications given an hour before practice or competition may help children continue their activities.
Prevention of sports injuries is the most important aspect of athletic programs. Children should be suited to the activity; the environment and the equipment must be safe. Children should be prepared for the sport, especially if it requires strenuous or continuous physical exertion. Nurses, coaches, and athletic trainers must collaborate to ensure that safety measures are implemented. Stretching exercises, warm-up and cool-down activities, and appropriate training are requirements for safe participation. Protective measures such as pads, taping, and wrapping are also important to prevent injury. Finally, nurses must be aware of environmental safety risks.
ALTERED GROWTH AND MATURATION
The absence of physical or sexual maturation at a time when other children are experiencing positive evidence of sexual development and its associated spurt in growth and physical strength is an important concern to both the parents and their affected child. In most instances the delay in development is a simple physiologic or constitutional delay that represents one end of the normal genetically influenced variation of pubertal growth. These adolescents will go through a delayed but normal puberty and finally catch up, in their late teens, with their more rapidly developing age-mates. Growth delay may be proportionate or disproportionate; either require careful evaluation by a multidisciplinary team. Less benign causes of delayed development may be endocrine disorders such as growth hormone deficiency, a disease process such as human immunodeficiency virus (HIV) or chronic malabsorption, or a chromosomal abnormality such as Turner syndrome. Additional causes of delayed development include asthma, cystic fibrosis, malabsorption syndromes, cardiac anomalies, and chronic renal conditions. Skeletal disorders that affect growth in stature are those described as dwarfism. Most disorders are caused by congenital defects, such as achondroplasia, and by inborn errors of metabolism such as Hurler syndrome or Hunter syndrome.
The rate of maturation is important during the school years, but at puberty it assumes significant proportions to both teens and their parents. Girls or boys who lag behind their peers in physical maturation are painfully aware of their difference in growth. Adolescent girls with delayed maturation may feel out of place among companions whose hips and breasts are developing, feel cheated if they have not yet menstruated, and feel left out when their friends giggle and talk about boys. Adolescent boys with delayed maturation may feel inferior and small compared with their more muscular companions with whom they can no longer compete physically. Serial measurements of height and weight, as well as other anthropometric data, are obtained and plotted on standard growth charts to determine the pattern of growth and to compare the individual child with the norms for his or her age-group (Appendix B). When children are in the extremes of height ranges, it is important to compare their height with that of their parents and siblings.
Psychosocial, or deprivation, dwarfism is a stress-induced growth failure. It is defined as growth restriction in children older than 2 years of age that is caused by environmental (emotional) stress and is associated with a marked delay in physical growth, delayed developmental skills, and immature behavior. When these children are removed from the deprived environment, their growth proceeds at a normal or increased rate.
Management of growth delay in childhood and adolescence includes continued medical observation, attention to general health and nutrition, and psychologic support. Growth hormone is often recommended to treat growth hormone deficiency (see Hypopituitarism, Chapter 29).
Nursing Care Management
Deviation from the normal course of puberty is a significant concern for affected adolescents. For some adolescents, this concern assumes monumental proportions. Many cases of delayed development are caused by simple constitutional delay of puberty, and the child can be assured that normal development will eventually take place.
One difficulty related to a size that is incongruent with chronologic and mental age is the manner in which others relate to the child. People often respond to children with short stature as though they were younger than their age. Consequently, these children may react with babyish or juvenile behavior, thus establishing a circular pattern of behavior and response. Conversely, children who are tall or physically advanced for their age are frequently treated as though they were more advanced than their years. They are often considered clumsy, cognitively delayed, or immature when they perform according to the normal behavioral expectations for their age.
Listening to distressed adolescents and conveying interest and concern are important interventions. Slowly maturing adolescents need support and reassurance that they are unique individuals who have an important contribution to society that is equally as important as that of their peers. Counseling and therapy are individualized for each youth. Encouraging these children to focus on the positive aspects of their bodies and personalities and to adopt sound health practices and practice good grooming fosters a more positive self-image.
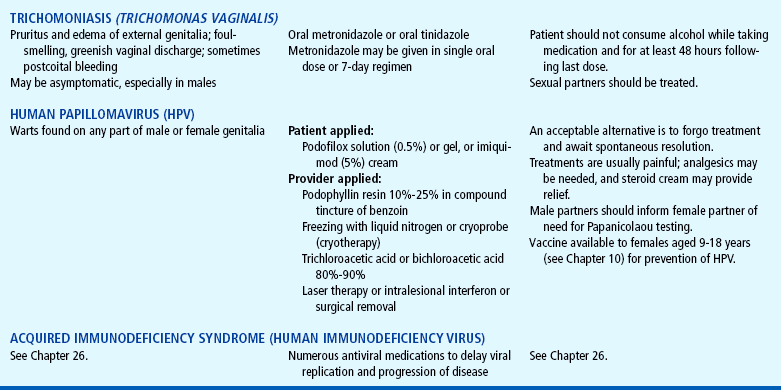
SEX CHROMOSOME DISORDERS
Most sex chromosome abnormalities are caused by an alteration in sex chromosome number (Table 17-1). The majority of these conditions are due to nondisjunction. An alteration in the number of sex chromosomes usually does not produce the profound defects that are associated with the autosomal disorders (trisomies). Intelligence may be normal or low normal, or the child may have some learning disabilities. Moderate or severe mental retardation is less common.
Turner Syndrome
Turner syndrome is caused by absence of one of the X chromosomes. Most girls who have this disorder have one X chromosome missing from all cells (45,XO). This disorder is often recognized at birth if the newborn has a webbed neck, low posterior hairline, widely spaced nipples, and edema of the hands and feet. This condition is often diagnosed in the preschool child because growth is restricted or delayed around 3 to 4 years of age. In some cases it may be diagnosed at puberty because of three features: short stature, delayed sexual development, and amenorrhea; individuals with Turner syndrome are generally infertile. They may also have difficulty with peer relationships and understanding social cues. They frequently exhibit behavioral problems, especially immature, socially isolated behavior. Diagnosis is confirmed on the basis of a negative sex chromatin test.
Therapy is individualized for these girls and consists primarily of female hormone treatment and psychologic counseling for both the child and parents. Linear growth can be increased by the administration of growth hormone if therapy is begun early. Estrogen therapy is initiated during the usual time for puberty to promote the development of secondary sex characteristics. Responses to estrogen therapy vary from girl to girl, but gradual feminization is accomplished to some degree in most individuals.
Klinefelter Syndrome
Klinefelter syndrome, the most common of all sex chromosome disorders, is caused by the presence of one or more additional X chromosomes and only one Y chromosome. Most males with this syndrome have a chromosome complement of 47,XXY. The disorder is infrequently diagnosed before puberty, at which time varying degrees of failure of adolescent virilization occur. Some males are not diagnosed until they appear for evaluation for infertility. All have absence of sperm in the semen (azoospermia), small testes, and defective development of secondary sex characteristics (gynecomastia, hypogonadism). In 80% of these boys there is a chromatin-positive buccal smear, and the extra chromosome is apparent on chromosome analysis.
Cognitive impairment is a frequent clinical finding and appears to be related to the number of X chromosomes. Boys may also have gross motor skill difficulties, a developmental language delay, poor verbal skills, reduced auditory memory, shyness, passivity, behavioral problems, and school difficulties. Therapy is directed toward enhancing the masculine characteristics through administration of testosterone.
Nursing Care Management
The nursing care of children with Turner or Klinefelter syndrome is primarily supportive. Nurses assist in the diagnosis, explain tests and therapies, and provide support and encouragement to the child and family. Because both disorders render the individual unable to reproduce, psychologic counseling is an important aspect of care. In young adults marriage and sexual relationships are possible, but alternative reproductive options, such as artificial insemination and adoption, should be discussed.
DISORDERS RELATED TO THE REPRODUCTIVE SYSTEM
Menarche, or the first menstrual period, occurs relatively late in female pubertal development. Although girls vary in the onset and rate of progression of pubertal development, the sequence and tempo should be the same. When an adolescent is seen with a complaint of absence of menses, a careful history of the timing of her pubertal development will help to determine if there is a need for further evaluation or if reassurance is all that is necessary.
Primary amenorrhea is an absence of secondary sex characteristics and no uterine bleeding by 14 to 15 years of age, or absence of uterine bleeding with secondary sex characteristics by 16 years of age (Master-Hunter and Heiman, 2006). No uterine bleeding after attaining a sexual maturity rating of 5 on the Tanner scale (see Figures 16-1 and 16-2) for 1 year, or after breast development for 4 years, is also considered primary amenorrhea (American Academy of Pediatrics and American College of Obstetricians and Gynecologists, 2006). The cause of primary amenorrhea may be anatomic, hormonal, genetic, or idiopathic. A thorough patient and family history and physical examination will provide clues to the etiology.
Secondary amenorrhea is defined as the absence of menses for 6 months or at least three cycles after menstruation was previously established. Irregular menstrual cycles are common within the first year or two after menarche. These early cycles may be anovulatory, resulting in regular, irregular, or absent bleeding; however, cycle lengths outside the range of 21 to 45 days should be investigated (American Academy of Pediatrics and American College of Obstetricians and Gynecologists, 2006). Girls with a later onset of menarche will take longer to establish regular ovulatory cycles.
Pregnancy is the most common cause of secondary amenorrhea and should be ruled out in both types of amenorrhea, even if the adolescent denies sexual activity. Other factors that disturb the hypothalamic-pituitary-gonadal axis and cause secondary amenorrhea include physical or emotional stress; sudden environmental change; hyperthyroidism or hypothyroidism; polycystic ovary disease; chronic illness; extreme weight loss or gain; intensive exercise; anorexia nervosa or bulimia; ovarian disturbance; and extrinsic pharmacologic agents, especially phenothiazines, contraceptive steroids, and heroin.
DYSMENORRHEA
A certain amount of discomfort during the first day or two of the menstrual flow is extremely common. Most girls experience cramping, abdominal pain, backache, and leg ache, but in a few cases the pain is intolerable and incapacitating. Primary dysmenorrhea is painful menses not related to any pelvic disease. Secondary dysmenorrhea is defined as painful menses with a pathologic condition such as endometriosis, salpingitis, or congenital anomalies of the müllerian system.
Primary dysmenorrhea usually begins at the time of menarche or within 6 to 12 months. The pain begins with menstrual flow or hours before the onset of bleeding each month, usually continuing for 48 to 72 hours. The exact etiology is unknown, but the pain is clearly related to ovulatory cycles. The overproduction of uterine prostaglandins has been implicated; women with dysmenorrhea have higher levels of prostaglandins. Overproduction of vasopressin (a hormone that stimulates the contraction of muscular tissue) may also contribute to dysmenorrhea.
A careful history should include the onset of symptoms; the duration, type of pain, and relationship to menstrual flow; age at menarche; family history of dysmenorrhea; and sexual history. The nurse should also ask about previous treatments, including dosages of medications. Associated symptoms such as nausea, vomiting, diarrhea, and leg and back pain are helpful for diagnosis and treatment. Depending on the results of the history, the physical examination may include a gynecologic examination.
Therapeutic Management
First-line treatment for adolescents with dysmenorrhea is the administration of NSAIDs, which block the formation of prostaglandins for 2 to 3 days of the menstrual cycle. The girl should be instructed to begin the medication at the first sign of cramping or bleeding. Girls with regular menstrual cycles benefit from beginning the medication 1 or 2 days before the onset of their menses. The medications should be taken with food.
Cyclic estrogen therapy and oral contraceptives are also effective. Simple exercises such as pelvic rocking, assuming the knee-chest position, and breathing exercises may be beneficial. Adequate personal hygiene, participation in regular activities, and methods to decrease stress should be discussed with the adolescent. Dietary changes, supplements, and herbal medications are often used to treat dysmenorrhea. Randomized controlled clinical trials have demonstrated that vitamins B1 and E are effective in the treatment of dysmenorrhea (Dennehy, 2006).
Nursing Care Management
All adolescent girls need reassurance that menstruation is a normal function. When nurses are asked for advice regarding menstrual problems, they have a valuable opportunity to engage in health teaching concerning menstrual physiology; hygiene; and the importance of a well-balanced diet, exercise, and general health maintenance. Health teaching can dispel myths about menstruation and femininity. When assessment indicates a potential problem and the need for evaluation, referral to an appropriate practitioner, health service, or clinic may be necessary.
One of the most difficult experiences facing the adolescent girl is the gynecologic examination. Whether it is her first experience or not, she is often filled with apprehension. Almost all adolescents are extremely self-conscious about their bodies and the changes taking place. They need continuing support in the form of anticipatory guidance regarding what to expect and suggestions of what to do to relax during the procedure. Most girls favor a semisitting position, which has the additional advantage of allowing eye contact during the procedure. Sometimes a pillow helps the patient feel more comfortable and less vulnerable. The provision of a mirror for the girl to see what is taking place if she so desires helps the examiner explain various aspects of anatomy. When possible, it is important to respect the adolescent’s request for a female provider.
VAGINITIS
Vaginitis can be caused by physical, chemical, or infectious agents. Physical causes may include a forgotten tampon; chemical irritants include bubble bath, douching, deodorant pads, and tampons. Removing the offending material or discontinuing use of the irritating substance is usually all that is necessary to treat physical or chemical vaginitis. Infectious vaginitis can be caused by Candida fungi (yeast), Trichomonas protozoa parasites, or bacteria. Diagnosis is confirmed with microscopic evaluation of vaginal secretions or vaginal culture. Treatment varies depending on the infectious agent.
Health teaching is important in the prevention and management of vaginitis. Adolescent girls need reassurance that increased vaginal mucus can occur at the time of ovulation, before menstruation, or with sexual excitement. Many teenage girls mistake these variations as signs of infection. Girls should be taught to wipe from front to back after toileting and to realize that vaginitis can result from irritation, foreign objects, and sexual activity. Nurses should stress the importance of an evaluation to determine the exact cause.
DISORDERS OF THE MALE REPRODUCTIVE SYSTEM
Most obvious anomalies, such as hypospadias, hydrocele, phimosis, and cryptorchidism, are identified with corrective measures instituted during early childhood. The most frequent problems related to the reproductive organs in later childhood are:
 Infections, such as urethritis (see Urinary Tract Infection, Chapter 27)
Infections, such as urethritis (see Urinary Tract Infection, Chapter 27)
 Penile problems, such as nonretractable foreskin in uncircumcised males, carcinoma, and trauma
Penile problems, such as nonretractable foreskin in uncircumcised males, carcinoma, and trauma
 Scrotal conditions, such as varicocele (elongation, dilation, and tortuosity of the veins superior to the testicle)
Scrotal conditions, such as varicocele (elongation, dilation, and tortuosity of the veins superior to the testicle)
 Testicular torsion (a condition in which the testicle hangs free from its vascular structures, which can result in partial or complete venous occlusion with rotation)
Testicular torsion (a condition in which the testicle hangs free from its vascular structures, which can result in partial or complete venous occlusion with rotation)
Tumors of the testes are not common, but when manifested in adolescence, they are generally malignant and demand immediate evaluation. Testicular cancer is the most common solid tumor in males 15 to 34 years of age. The usual presenting symptom for testicular cancer is a heavy, hard, painless mass (either smooth or nodular) that is palpated on the testis. Treatment involves surgical removal of the affected testicle (orchiectomy) and possibly chemotherapy and radiation if metastasis has occurred.
Nursing Care Management
The adolescent boy is also self-conscious about his changing body and needs preparation for a genital examination. The most successful approach is to assume a matter-of-fact attitude toward the examination, explain precisely what will take place, and maintain a continuous commentary about what is being done and the findings at each phase of the examination.
The routine health assessment of every adolescent boy should include teaching about testicular cancer and how to perform a testicular self-examination (TSE) every month. This rare malignancy is curable if detected early. Nurses are in an ideal position to teach TSE in a manner that is respectful of the adolescent boy’s anxieties and that promotes early treatment (see Critical Thinking Exercise).
The normal testicle is a firm organ with a smooth, egg-shaped contour; the epididymis is palpated as a raised swelling on the superior aspect of the testicle and should not be taken for an abnormality.
GYNECOMASTIA
The male breast, although not strictly part of the male reproductive system, responds to hormonal changes. Some degree of bilateral or unilateral breast enlargement occurs frequently in boys during puberty. It is estimated that approximately half of adolescent boys have transient gynecomastia, usually lasting less than 1 year, which subsides spontaneously with achievement of male development. A careful assessment of the pubertal stage at the onset of gynecomastia; medication history, including anabolic steroids; and the exclusion of renal, liver, thyroid, and endocrine disorders or dysfunction allow the examiner to reassure the adolescent that the changes are pubertal gynecomastia and that no further assessment is indicated.
If the condition persists or is extensive enough to cause embarrassment or to produce doubts about gender identity in the young boy, plastic surgery may be indicated for cosmetic and psychologic considerations. Administration of testosterone has no effect on breast development or regression and may aggravate the condition.
Nursing Care Management
Treatment usually consists of assurance to the adolescent and his parents that this is a benign and temporary situation. A physical examination with palpation is necessary to differentiate gynecomastia from increased adiposity caused by being overweight. Adolescents who are distressed about physical integrity and masculinity may benefit from the knowledge that this condition occurs in more than 50% of all adolescent boys.
HEALTH PROBLEMS RELATED TO SEXUALITY
It is estimated that by the time adolescents finish high school, more than half of them will have had at least one sexual experience with a member of the same or opposite gender (Mosher, Chandra, and Jones, 2005). Many serious health consequences are associated with adolescent sexual activity, including unplanned pregnancy and sexually transmitted diseases (STDs); additional health problems may arise from an increased number of sexual partners over time and incomplete education regarding sexual practices in adolescents. Health professionals must understand the issues related to adolescent sexual activity and the psychosocial dynamics that influence them.
ADOLESCENT PREGNANCY
In recent years the teenage pregnancy rate has shown a continual downward trend. Between 1990 and 2003, birth rates for teenagers 15 to 17 and 18 to 19 years of age declined nationally for all races. In 2005 the teenage birth rate decreased 2% (from 2004) to 40.4 births per 1000 women ages 15 to 19 (Hamilton, Martin, and Ventura, 2006). The decline over the past decade has been attributed to a drop in the number of repeat pregnancies and an increase in the use of condoms and long-term hormonal contraceptive methods among adolescents. However, adolescent birth rates still remain high in the United States compared with those in other developed countries (American Academy of Pediatrics, 2005a). The number of teens initiating sexual intercourse before the age of 15 has significantly decreased in the past 10 years (Anderson, Santelli, and Morrow, 2006). Teens who postpone the initiation of sexual intercourse decrease their risk for STDs, including HIV.
The reduction in teen pregnancy is an important national goal because of the risk for negative outcomes for both mother and child. A wide range of factors put an adolescent at risk for pregnancy, including having sex with an older partner, the type of contraception used; living in poverty; having a mother who was a teen parent; school failure; lack of access to confidential health care; and living in a poor community where access to education, health care, and work may not be optimal.
With better facilities available for care, the mortality associated with teenage pregnancies is decreasing, but morbidity remains high. Teenage girls and their unborn infants are at greater risk for complications of both pregnancy and delivery. The most frequent complications are premature labor and low-birth-weight infants, high neonatal mortality, iron deficiency anemia, fetopelvic disproportion, and prolonged labor. The pregnancies of adolescents less than 15 years old are more frequently complicated by obstetric problems and neonatal morbidity and mortality than those of adolescents ages 15 to 19. The increased risk has traditionally been thought to be related to incomplete growth and physiologic immaturity. However, pregnancy can take place only after the girl has achieved an advanced state of growth and sexual maturity. Therefore concerns are dietary habits, substance use (especially cigarettes), STDs, the effects of poverty, and a late onset of prenatal care.
Nursing Care Management
A pregnant teenager needs careful assessment by the nurse to determine the level of social support available to her and her partner. The adolescent needs to make many important decisions and may not have the life experience to know how to cope with this stress. Whenever possible, guidance from the adults in her life will be invaluable. Information about options to continue the pregnancy and parent the child, continue the pregnancy with adoption, or terminate the pregnancy with abortion should be given in a nonjudgmental manner. If the adolescent chooses to continue the pregnancy, prenatal care should be initiated as soon as possible. No matter what the teenager decides, nutrition information will be necessary.
CONTRACEPTION
Family planning services have developed and expanded during recent years, but the need for contraceptive services as part of the health care of adolescents remains great. The birth control pill and condom remain the most popular methods for adolescents; 3-month injectable contraception is more popular among lower-income adolescents. Adolescents commonly delay seeking contraceptive information. The typical interval from onset of sexual intercourse until the first visit for contraception is 1 year. A pregnancy scare is usually the precipitating event for the contraception appointment. Counseling about contraceptive options should be conducted in a manner that is consistent with the cognitive level of the adolescent. The adolescent should be given accurate information about the risks and benefits of each method before making a choice.
Many teenagers feel ambivalent regarding their sexual activity and avoid many contraceptives because their use seems too premeditated and implies that sex is planned rather than a spontaneous activity. Most of these girls believe that sex is all right if it is not planned. This may often play a role in adolescents delaying contraception, waiting for a relationship that is “close enough.” A close relationship would allow the adolescents to accept and acknowledge their sexual activity.
The choice of a safe and effective contraceptive method must be suited to the individual (Table 17-2). The choice is based on preference after the adolescent is informed of the benefits and disadvantages. Motivation is necessary for most methods. For example, the pill is effective if used correctly, but the adolescent must remember to take the pill at approximately the same time every day. For many young women, a medroxyprogesterone injection (Depo-Provera) is an ideal choice because it is extremely effective and is administered every 12 weeks, but side effects such as weight gain and decreased bone mineralization may make it undesirable. Sexually active adolescents need to know that contraceptive devices other than condoms do not prevent STDs. Condom use is still important and must be discussed with all sexually and non–sexually active adolescents.
Confidentiality is a critical issue when discussing contraception with adolescents. Privacy is important to adolescents as they struggle to forge a personal identity and establish social relationships. Adolescents are particularly concerned about the judgments of others. The predominant belief among many health professionals is that parental notification is important but that the “parents’ rights” view is not necessarily sensitive to the health needs and basic rights of youth. No evidence substantiates the belief that providing contraceptive guidance contributes to sexual irresponsibility and promiscuity.
Nursing Care Management
Nurses are often involved in providing education about contraception. Such education is ideally combined with ongoing sex education. Although sexual abstinence is a highly desirable form of contraception for teenagers, nurses working with adolescents must recognize that teens feel multiple pressures to engage in sexual intercourse. Postponing sexual involvement requires effective communication and decision-making skills. Adolescents benefit from role-playing refusal skills and opportunities to practice making decisions in a safe environment. Information about safe sex must be provided, and role-playing how to discuss condom use with a partner is helpful to teenagers.
Education concerning contraception should be provided in both oral and written form. All available methods, including their benefits, disadvantages, and side effects, should be discussed. Concrete, concise language must be used, demonstrations of how to use the contraceptive should be provided, and adolescents should repeat all instructions in their own words. If teenagers are using oral contraceptive pills, they should be encouraged to use a daily activity as a reminder or cue to take the pill. A knowledgeable phone triage person should be available for questions and concerns. Parents or other important adults may be included in all discussions, with the adolescent’s permission.
SEXUALLY TRANSMITTED DISEASES
Sexually active adolescents are at increased risk (compared with adults) for the acquisition of STDs. Physiologically, the adolescent girl’s cervix has a large ectropion, which is composed of columnar epithelial cells that are much more susceptible to STDs, especially human papillomavirus (HPV) and Chlamydia infection. The adolescent’s immune system also contributes to the increased risk because the adolescent has not had an opportunity to develop resistance to these organisms (Shrier, 2004). Behavioral factors contributing to increased risk include initiating sexual intercourse at an early age, high disease prevalence among sexual partners, and inconsistent use of barrier or other types of contraceptives. In addition, adolescents may participate in unprotected oral or anal sex in the belief that STDs cannot be transmitted through those activities (Shrier, 2004). A listing of common STDs is included in Table 17-3.
TABLE 17-3
Selected Sexually Transmitted Diseases*
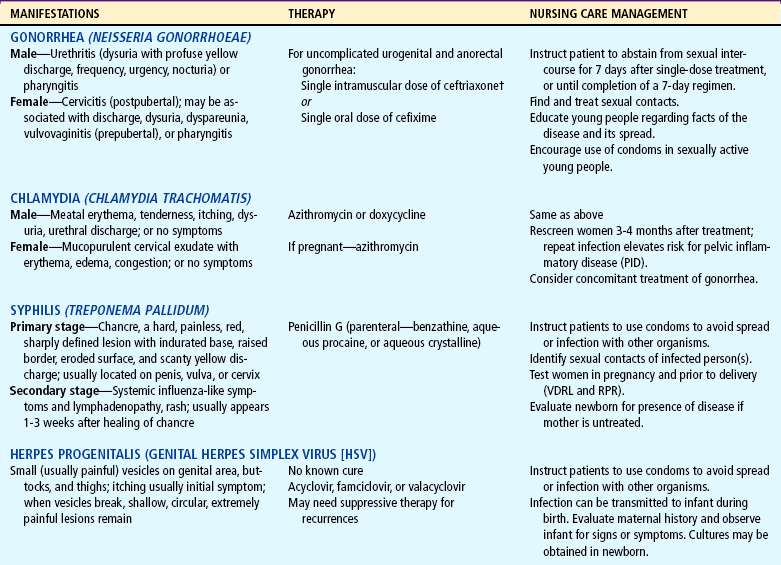
*Updated information on specific treatment of STDs may be accessed at http://www.cdc.gov/std/treatment.
†Centers for Disease Control and Prevention: Update to CDC’s Sexually transmitted disease treatment guidelines, 2006: fluoroquinolones no longer recommended for treatment of gonococcal infections, MMWR 56(14):332-336, 2007.
The rates of chlamydia and gonorrhea are reported to be highest among adolescent girls ages 15 to 19 years, and high rates of HPV exist in the adolescent population (Centers for Disease Control and Prevention, 2006a). Whereas much emphasis has been placed on prevention of HIV in the past decade, other STDs have received little attention in regards to prevention. Lack of awareness regarding one’s susceptibility to STDs when engaged in unprotected sexual activity, be it oral, anal, or vaginal intercourse, is perhaps one of the greatest dangers adolescents face.
Therapeutic Management
Effective treatment of both males and females with an STD involves administration of the appropriate therapeutic agent. Treatment of sexual partners is also an essential part of therapy. Adolescents need help to develop strategies to inform their partner and to abstain from sex until both have completed treatment.
A totally effective prophylaxis against infection is not yet available; therefore preventive efforts must be directed toward finding and treating affected persons, locating and examining contacts of affected persons, educating young people regarding the facts of the disease and its spread, and encouraging the use of condoms in sexually active young people.
Nursing Care Management
Nursing responsibilities encompass all aspects of STD education, confidentiality, prevention, and treatment. Part of the sex education of young people should include providing information about these diseases, including their symptoms and treatment, and dispelling the myths associated with their mode of transmission. Many vulnerable adolescents are uninformed or misinformed about STDs.
Primary prevention efforts for STDs include encouraging abstinence and postponing sexual involvement; encouraging condom use; and ensuring vaccination for hepatitis A and B and HPV. Nurses play a role in secondary prevention by helping to identify early cases and referring adolescents for treatment. Nurses can also be involved in tertiary prevention by decreasing the medical and psychologic effects of STDs; conducting support groups for adolescents with HIV, herpes simplex virus, and HPV infections; and assisting pregnant adolescents in obtaining adequate prenatal screening and treatment of STDs.
PELVIC INFLAMMATORY DISEASE
Pelvic inflammatory disease (PID) is an infection of the upper genital tract (endometrium, fallopian tubes, and ovaries), most commonly caused by sexually transmitted bacteria, such as Neisseria gonorrhoeae, Chlamydia trachomatis, and a variety of other anaerobic bacteria.
The long-term effects of PID include infertility because of tubal scarring, ectopic pregnancy, and chronic abdominal pain. It is estimated that each year 1 million females of reproductive age experience an episode of PID, with approximately 20% of cases occurring in teenagers. Women under the age of 25 years have a one in eight chance of experiencing PID compared with those over age 25 years, whose risk is one in 80.
Presenting symptoms in the adolescent may be generalized, including fever; abdominal pain; urinary tract symptoms; and vague influenza-like manifestations, such as malaise, nausea, diarrhea, or constipation. A pelvic examination is indicated for every sexually active female who complains of lower abdominal pain to evaluate for the possibility of PID.
PID is of major concern to nurses because of its devastating effects on the reproductive tract. Approximately 25% of females experiencing PID may have short-term complications, such as acute abscess formation in the fallopian tubes (tubo-ovarian abscess), or long-term complications, such as chronic pelvic pain, dyspareunia (painful coitus), or adhesion formation. Most significant, however, is the increased risk for ectopic pregnancy or infertility, which results from tubal scarring.
Prevention is the primary concern of health care professionals. Barrier contraceptive methods, such as condoms, seem to offer the best protection for preventing STDs and PID. Sexually active female teenagers should be screened every 6 months to detect asymptomatic STDs, and treatment should be initiated to prevent PID and all associated complications. Reinfection with Chlamydia organisms is associated with a higher incidence of PID. Females who have had a Chlamydia infection should be rescreened for Chlamydia 3 months after treatment.
SEXUAL ASSAULT (RAPE)
The adolescent girl is particularly vulnerable to sexual assault, and 75% of adolescents who are raped know their assailant (Clements, Speck, Crane, and others, 2004). Females are more likely to report these experiences than males (Neinstein, 2002). In each instance the victim is potentially subjected to serious physical or emotional harm. There is no typical victim. Sexual assault victims are of all ages, ethnic groups, and economic groups and are of either gender, although adolescents and children with a physical or developmental disability are more vulnerable to sexual abuse than their peers. Acquaintance rape is far more common than stranger rape; however, stranger rape is reported more often.
An understanding of the legal definitions of sexual assault, rape, acquaintance rape, and statutory rape is essential for the nurse to identify, treat, and manage adolescent victims (Box 17-1).
Statutory rape laws have been revised in many states across the country. The motivation for tougher laws and greater enforcement is to decrease teen pregnancy, increase male responsibility, and decrease welfare dependency. Traditionally, statutory rape laws have been concerned with the protection of girls. In the past 20 years, many laws have been rewritten to be gender neutral. Statutory rape laws require reporting to child protective services or local law enforcement. One risk of strict statutory rape enforcement is that girls may not seek health care for reproductive care, prenatal care, or domestic violence. Young people may fear not only for themselves, but also for their partner. However, sexual coercion of teens by adults remains a problem and results in STDs and adolescent pregnancy.
In the United States, it is illegal for anyone to have sexual intercourse with a child under the age of 12 years. These laws protect the health and safety of children incapable of protecting themselves. When consensuality is considered in statutory rape laws and cases, it implies that adolescents are morally and socially responsible for sexual contact that occurs with adults. This does not afford adolescents the same protections provided to children under the age of 12 (Kandakai and Smith, 2007).
Nurses can obtain information about their state statutory rape reporting responsibilities from state or local child protective services agencies, legal counsel, rape crisis organizations, state or local law enforcement agencies, or the state nurses’ association. The limits of confidentiality should be clearly reviewed with each adolescent patient before beginning the interview about sexual activity.
There has been a reported increase in the use of drug-facilitated sexual assaults. Older adolescents and young adults at parties, bars, and raves are at risk for having a drug slipped into their beverage when they are not looking. Substances most often referred to as “date rape” drugs are flunitrazepam (Rohypnol), a sedative-hypnotic benzodiazepine; γ-hydroxybutyric acid (GHB), a sleep aid; and ketamine, an anesthetic agent (Schwartz, Milteer, and LeBeau, 2000). However, alcohol is the most widely used drug in such assaults. These fast-acting drugs cause disinhibition, passivity, relaxation of muscles, and lasting amnesia. The victim wakes up in strange surroundings and realizes she has been sexually assaulted. She may not report the crime for days or weeks or may never report it. Acquaintance rape is frequently underreported because the victim may believe she contributed to the act in some way. The victim may not identify the experience as rape because it does not fit the standard concept.
Diagnostic Evaluation
The rape victim may exhibit a variety of reactions (Box 17-2), and the circumstances of the initial medical evaluation may be frightening and stressful. The initial contact with the rape victim must be supportive because the interrogation and associated activities have the potential to add to the trauma of the sexual assault. First of all, the victim needs to know that she (or he) is (1) all right and (2) not being blamed for the situation.
It is important to obtain a clear account of the circumstances of an alleged rape without forcing the victim to relive a painful experience. Information includes date, time, location, and an accurate description of any type of sexual contact. The physical examination is carried out as soon as possible, since physical evidence deteriorates rapidly. The victim should not bathe or shower before the examination.
The young person is always told in advance in understandable terms exactly what to expect in the way of tests and procedures, and the explanation is accompanied by strong emotional support. The victim is examined thoroughly, including nongenital areas, for evidence of injury that might substantiate the use of force.
The forensic examination of a sexual assault victim must follow strict legal requirements. The medical record may provide key evidence for the legal case. Practitioners specially trained for rape examination should be used when possible. Nurses are often members of this group and are known as sexual assault nurse examiners (SANEs). Evaluation for STDs is an important part of the evaluation. All potential infection sites are tested to detect gonorrhea, chlamydia, and trichomoniasis. Blood samples for syphilis, hepatitis B virus, and HIV are obtained as a baseline (American Academy of Pediatrics, 2001a). The adolescent is reexamined at appropriate intervals (4 to 6 weeks for syphilis; 2 to 3 days for gonorrhea) to determine if a disease was acquired from the assailant.
Prophylactic treatment for chlamydia and gonorrhea is recommended. Female victims should be provided with emergency contraception. The recommendation for HIV prophylaxis varies depending on the geographic area, the circumstances of the assault, and the known HIV status of the perpetrator. The Centers for Disease Control and Prevention (2006a) maintains updates and recommendations for treatment of STDs incurred as a result of sexual assault.*
Therapeutic Management
Adolescents who have been raped arrive at the emergency department or practitioner’s office under a variety of circumstances. They are usually brought by parents, friends, or police officers, but some may seek medical help on their own. It is advisable to obtain parental consent for examination, but the examination may be performed without parental consent if the adolescent is mature and the parents are unavailable. A female observer should be present during the history and examination of female victims who are examined by a male practitioner. Whether a parent should be present during the examination is determined on an individual basis. The parent’s presence is usually encouraged if the parent is supportive and the young person agrees.
Rape Trauma Syndrome
The term rape trauma syndrome refers to the victim’s reaction to a sexual assault. The syndrome involves two phases: (1) the acute phase of disorganization of lifestyle and (2) a long-term process of reorganization. These phases encompass behavioral, somatic, and psychologic reactions to the stressful event. Counseling should begin immediately upon the adolescent’s entrance into the emergency department with follow-up within the first 24 hours. Early intervention has been shown to be effective in decreasing the extent of rape trauma syndrome (Patel and Minshall, 2001).
Nursing Care Management
Many of the approaches that have been described for the sexually abused child (see Chapter 14) apply to the adolescent. Sexual assault is a devastating experience with long-lasting effects. The primary goal of nursing care is to avoid inflicting further stress on the adolescent, who is often angry, confused, frightened, embarrassed, and filled with self-blame. The nurse must do everything possible to reduce the stress of the interrogation and examination. Although most health professionals and law enforcement officers are sensitive to the needs of the adolescent and attempt to make the process as nonstressful as possible, the nurse should be alert to cues that indicate the victim is being overstressed.
Follow-up care of the rape victim is essential and extends over a long period. Aside from the universal need for emotional support, the needs of rape victims vary widely and depend on the nature of the incident, the victim’s age when the rape occurred, the physical and emotional injuries sustained by the victim, the legal actions being considered as a result, the resources available for informal support, and the anticipated reactions of persons in the informal support network (see Family Focus box).*
EATING DISORDERS
Few problems in childhood and adolescence are so obvious to others, are so difficult to treat, and have such long-term effects on health as obesity. Several different definitions have been proposed for obesity and overweight. Obesity has been defined as an increase in body weight resulting from an excessive accumulation of body fat relative to lean body mass. Overweight refers to the state of weighing more than average for height and body build. Currently, the body mass index (BMI) measurement is recommended as the most accurate method for screening children and adolescents for obesity. The BMI measurement is strongly associated with subcutaneous and total body fat and also with skinfold thickness measurements. It is also highly specific for children with the greatest amount of body fat. Pediatric growth charts that include BMI for age and gender are available from Centers for Disease Control and Prevention.* Children with a BMI between the 85th and 95th percentiles are considered overweight, and obesity is defined by a BMI greater than the 95th percentile (Moran, 2003).
Regardless of the definition used, the number of overweight children in the United States is increasing and may be approaching epidemic status (Shulman, 2004). In children ages 6 to 11 years, the prevalence of childhood overweight remained fairly constant in the years 1963 and 1974 at approximately 4% and 5.5%, respectively. However, in the National Health and Nutrition Examination Survey, those numbers have steadily climbed to reach 16% in both 6- to 11-year-olds and 12- to 19-year-olds in 2001 to 2002; almost 32% of children ages 6 to 19 were at risk for overweight (Hedley, Ogden, Johnson, and others, 2004). African-American and Hispanic children and youth are disproportionately represented by a higher prevalence of overweight (21.5% and 21.8%, respectively) when compared with non-Hispanic Caucasian children (12.3%) (National Institute for Health Care Management Foundation, 2003). These numbers double if they include children defined as being at risk for overweight (<85th percentile on growth chart). A study of 9464 American Indian schoolchildren ages 5 to 18 years found that 39% were overweight, and a further review of tribes across the United States found that 30% to 46% of American Indians were at risk for overweight (<85th percentile) (Hardy, Harrell, and Bell, 2004).
Because adult obesity is associated with increased mortality and morbidity from a variety of complications, both physical and psychologic, adolescent obesity is a serious condition. Research indicates that overweight children and adolescents are at risk of continuing to be obese as adults, thereby experiencing the health and social consequences of obesity much earlier than children and adolescents of normal weight. Parental obesity increases the risk of overweight by twofold to threefold (Baker, Barlow, Cochran, and others, 2005). The probability that overweight school-age children will become obese adults is estimated at 50%, whereas the likelihood that overweight adolescents will become obese adults is estimated at 70% to 80% (National Institute for Health Care Management Foundation, 2003).
Obesity in childhood and adolescence has been related to elevated blood cholesterol, high blood pressure, respiratory disorders, orthopedic conditions (Taylor, Theim, Mirch, and others, 2006), cholelithiasis, some types of adult-onset cancer (MacKenzie, 2000), nonalcoholic fatty liver disease (NAFLD) (Baker, Barlow, Cochran, and others, 2005; Angulo, 2002), and type 2 diabetes mellitus (Ehtisham, Barrett, and Shaw, 2000). The incidence of metabolic syndrome was 50% in a study group of overweight and obese adolescents (Weiss, Dziura, Burgert, and others, 2004). Common emotional consequences of obesity include poor body image, low self-esteem, social isolation, and feelings of depression and rejection (Sjöberg, Nilsson, and Leppert, 2005).
Etiology and Pathophysiology
Obesity results from a caloric intake that consistently exceeds caloric requirements and expenditure and may involve a variety of interrelated influences, including metabolic, hypothalamic, hereditary, social, cultural, and psychologic factors (Fig. 17-2). Because the etiology of obesity is multifactorial, the treatment requires multilevel interventions.
Birth weight is not a contributing factor in detection and prediction of childhood obesity; obese children do not have higher birth weights than nonobese children. There is, however, a high correlation between childhood adiposity and parental adiposity.
A balance between energy intake and energy expenditure is a critical factor in regulating body weight. Factors that raise energy intake or decrease energy expenditure by even small amounts can have a long-term impact on the development of overweight and obesity. For example, a positive balance of one serving of a sweetened juice or soft drink (about 120 kcal) per day would produce a 50 kg (110 pound) increase in body mass over a 10-year period (Hill, Wyatt, Reed, and others, 2003).
Familial influence is an epidemiologic consideration in regard to a child’s weight. Twin studies suggest that approximately 50% to 70% of the tendency toward obesity is inherited (Kiess, Galler, Reich, and others, 2001). Twin studies have also suggested that this tendency is a combination of genetic and environmental factors. If both parents are lean, the likelihood of the child becoming overweight is just 9%. When both parents are obese, there is a 60% to 80% increase in the likelihood of the child becoming obese (Koeppen-Schomerus, Wardle, and Plomin, 2001). The specific influences of genes and environment within the developing child is not well defined. The increasing rates of obesity within genetically stable populations suggest that environmental and some perinatal factors (e.g., bottle feeding) are contributors to the current increases in childhood obesity (National Institute for Health Care Management Foundation, 2003).
Fewer than 5% of the cases of childhood obesity can be attributed to an underlying disease. Such diseases include hypothyroidism; adrenal hypercorticoidism; hyperinsulinism; and dysfunction or damage to the central nervous system as a result of tumor, injury, infection, or vascular accident. Obesity is a frequent complication of muscular dystrophy, paraplegia, Down syndrome, spina bifida, and other chronic illnesses that limit mobility.
A major focus of obesity research has been on appetite regulation. The expression of appetite is chemically coded in the hypothalamus by distinctive circuitry. Orexigenic substances produce signals that promote eating behaviors, and anorexigenic substances promote the cessation of eating behaviors. Feedback loops between signals have been identified where one signal peptide is able to alter the secretion of another signal peptide. No one signal has been identified as the gatekeeper of appetite. It is apparent that an entire network of signals, including their frequency and amplitude, is responsible for triggering eating behaviors.
There is little evidence to support a relationship between obesity and “low metabolism.” Small differences may exist in regulation of dietary intake or metabolic rate between obese and nonobese children that could lead to an energy imbalance and inappropriate weight gain, but these small differences are difficult to accurately quantify. No differences in basal metabolic rate, sleeping metabolic rate, respiratory quotient, heart rate, or total energy expenditure have been found in normal weight children with or without a familial predisposition to overweight (Baker, Barlow, Cochran, and others, 2005). In childhood, overeating is the dominant feature in obesity, whereas in adult life, reduced physical activity with normal intake is more likely.
The tendency toward obesity is manifested whenever environmental conditions are favorable to excessive caloric intake, such as an abundance of food, limited access to low-fat foods, reduced or minimum physical activity, and snacking combined with excessive television viewing. Family and cultural eating patterns, as well as psychologic factors, play an important role; many families and cultures consider fat to be an indication of good health. It is not uncommon for obese children to have families that emphasize large meals or admonish children for leaving food on their plates. Parents may have an exaggerated concept of the amount of food children require and expect them to eat more than they need. The prevalence of obesity shows a marked difference between upper- and lower-class children, with differences often becoming apparent before 6 years of age. Lower socioeconomic groups have a greater prevalence of obesity, especially in girls. Physical activity may also be influenced by sociocultural factors.
Some community factors that influence activity patterns include unsafe neighborhoods that keep children from playing outside. Many communities lack affordable and accessible areas for low-income youth to be active, thus limiting opportunities for young people to participate in physical activities. Social policies also contribute to obesity. The increased availability of high-fat foods, pricing strategies that promote unhealthy food choices, and overzealous food advertising that targets children and adolescents with high-fat and high-sugar foods are some examples.
Institutional factors also influence patterns of obesity and decreased physical activity. Many school policies allow students to leave school for lunch. Vending machines in school often are filled with high-fat and high-calorie foods and soft drinks. Although well-balanced, nutritious school lunches may be available to students, they will often opt for less nutritious choices such as high-fat snacks.
Physical inactivity has also been identified as an important contributing factor in the development and maintenance of childhood overweight. There is little doubt that physical activity has decreased in elementary and secondary schools in the United States. Consequently, most of a child’s physical activity must occur within the family or outside of school. Decreased physical activity within the family is a powerful influence on children, since children imitate their parents and other adults. Parental obesity and low levels of physical activity are correlated with decreased physical activity in children.
The growing attraction and availability of many sedentary activities, including television, video games, computers, and the Internet, have greatly influenced the amount of time that children spend participating in sedentary behaviors. A study conducted by the Kaiser Family Foundation demonstrated that children watch an average of 2½ hours of television per day, and that one in five kids watches TV for 5 hours or more every day (Rideout, Foehr, Roberts, and others, 1999). When combining television viewing with video games, it is estimated that children may spend as much as 6½ hours per day on various media, which takes time away from meaningful activities such as exercise and reading (American Academy of Pediatrics, 2001b).
Psychologic factors also affect eating patterns. In infancy, children experience relief from discomfort through feeding and learn to associate eating with a sense of well-being, security, and the comforting presence of a nurturing person. Eating is soon associated with the feeling of being loved. In addition, the pleasurable oral sensation of sucking provides a connection between emotions and early eating behavior. Many parents use food as a positive reinforcer for desired behaviors. This practice may become a habit, and the child may continue to use food as a reward, a comfort, and a means of dealing with depression or hostility. Many individuals eat when they are not hungry or in response to boredom, loneliness, sadness, depression, or tiredness. Difficulty in determining feelings of satiety can lead to weight problems and may compound the factor of eating in response to emotional rather than physical hunger cues.
Eating behaviors are closely related to memory. Memory and appetite are chemically encoded, with each individual having his or her own circuitry relating to eating behaviors. Like memory, the circuitry can be modified over time (Feldman, Friedman, and Sleisenger, 2002).
Diagnostic Evaluation
A careful history is obtained regarding the development of obesity, and a physical examination is performed to differentiate simple obesity from increased fat that results from organic causes. A family history of obesity, diabetes, coronary heart disease, and dyslipidemia should be obtained for all children who are overweight or at risk for overweight. Specific information from the patient and family about the effects of obesity on daily functioning—for example, problems with nighttime breathing and sleep, daytime sleepiness, pain in the joints, ability to keep up with family activities and peers at school—will be helpful. The physical examination should focus on identifying comorbid conditions and identifiable causes of obesity. For some, psychologic assessment, by interviews and standardized personality tests, may provide insight into the personality and emotional problems that contribute to obesity and that might interfere with therapy.
It is useful to estimate the degree of obesity to determine the component of body weight that can be modified. All the following methods have been used to assess obesity: BMI, body weight, weight-height ratios, weight-age ratios, hydrostatic (underwater) weight, skinfold measurements, bioelectrical analysis, computed tomography (CT), magnetic resonance imaging (MRI), and neutron activation. Each of these methods has advantages and disadvantages. Hydrostatic, or underwater, weighing provides the most accurate measurement of lean body weight.
BMI is currently considered the best method to assess weight in children and adolescents. The calculation is based on the individual’s height and weight. In adults, BMI definitions are fixed measures without regard for sex and age. The BMI in children and adolescents varies to accommodate age- and gender-specific changes in growth. The formula for BMI calculation is:
BMI measures in children and adolescents are plotted on growth charts that enable heath care professionals to determine BMI-for-age for the patient (see Appendix B).
The initial assessment of obese children and adolescents should include screening to evaluate for comorbidities. The history is an important guide to determine the workup. A complete physical examination is important. Some areas to focus on include (1) skin for stretch markings and discolorations (e.g., acanthosis nigricans), (2) joints for swelling and evidence of pain, and (3) airway for evidence of obstruction and enlarged tonsils. Basic laboratory studies include a fasting lipid panel; fasting insulin level; fasting glucose hepatic enzymes, including γ-glutamyltransferase (GGT); and, in some institutions, hemoglobin A1c. Other studies, such as a sleep study, metabolic studies, and radiographic evaluations, may be added based on the history and physical examination. These assessments may determine whether the patient needs a referral to specialty services for more focused evaluation and treatment, such as endocrinology (insulin resistance, diabetes), hepatology (elevated liver enzymes, NAFLD), orthopedics (Blount disease), or pulmonary medicine (sleep-disordered breathing, continuous positive airway pressure).
Therapeutic Management
The best approach to the management of obesity is a preventive one. Early recognition and control measures are essential before the child or adolescent reaches an obese state. Health care providers must educate families about the medical complications of obesity, and families are encouraged to be involved in the treatment plan.
The treatment of obesity is difficult. Many approaches do not achieve long-term success. The average individual only loses about 5% to 10% of his or her weight with available therapies. Losing weight can have a significant positive effect on many comorbidities, but unfortunately the lost weight is frequently regained in a year or two (Yanovski and Yanovski, 2002).
Diet modification is an essential part of weight-reduction programs. Dietary counseling is directed toward improving the nutritional quality of the diet rather than on dietary restriction. Children should avoid fad diets. Most dietitians and nutrition experts recommend a diet with low-saturated fat, moderate total fat (≤30%), and five servings of fruits and vegetables, consistent with the MyPyramid* food guide for children. Also, promoting high-fiber foods and avoiding highly refined starches and sugars will decrease caloric intake. The Dietary Guidelines for Americans† may be used as a guide for caloric intake for adolescents concerned about weight control; these guidelines also emphasize daily exercise in weight management for children and adolescents. Many programs recommend using a food diary as a helpful tool to increase awareness of food choices and eating behaviors. The goal is to encourage the individual to make healthier choices in food selection and discourage eating food by habit or to appease boredom.
In patients with severe obesity, strict diets have been used, such as the protein-sparing modified fast, a hypocaloric, ketogenic diet that is designed to provide enough protein to minimize loss of lean body mass during weight loss. Such diets need to be closely monitored and should be used only with multidisciplinary teams that include a physician, nutritionist, and behavioral therapist. Generally, the diet consists of 1.5 to 2.5 g of protein per kilogram. The intake of carbohydrates is low enough to induce ketosis. The benefits of the diet are relatively rapid weight loss and anorexia induced by ketosis. Potential complications include protein losses, hypokalemia, hypoglycemia, inadequate calcium intake, and orthostatic hypotension. Potassium and calcium supplements and adequate calorie-free beverages can minimize these complications (Baker, Barlow, Cochran, and others, 2005). It is difficult to sustain such diets over the long term, and the long-term outcomes of using these diets have not been established.
Some drugs have been used to promote weight loss in children with certain conditions such as metformin in obese adolescents with insulin resistance and hyperinsulinism, octreotide for hypothalamic obesity caused by intracranial tumors, growth hormone in children with Prader-Willi syndrome, and leptin for congenital leptin deficiency. The drug sibutramine, in addition to behavioral therapy, significantly reduced BMI and body weight more than placebo; however, the drug was associated with side effects (tachycardia and hypertension) (Berkowitz, Fujioka, Daniels, and others, 2006).
Bariatric surgery may be the only practical alternative for increasing numbers of severely overweight adolescents who have failed organized attempts to lose or maintain weight loss through conventional nonoperative approaches and who have serious life-threatening conditions. Some preliminary studies suggest that adolescents with severe obesity have successful weight loss up to 14 years after bariatric surgery; most adolescents were reported to have a significant change in lifestyle as a result of the weight loss after surgery (Sugerman, Sugerman, DeMaria, and others, 2003). Others suggest that bariatric surgery in adolescents is safe and they have fewer postoperative complications than adults, but the procedure is relatively uncommon in comparison to the number of adults having surgery for obesity (Tsai, Inge, and Burd, 2007). In general, bariatric surgery should be reserved for severely obese adolescents with comorbidities after careful consideration. Candidates for surgery should be referred to centers that offer a multidisciplinary team experienced in the management of childhood and adolescent obesity, and the surgery should be performed by surgeons who have participated in subspecialty training in bariatric medical and surgical care as detailed by the American College of Surgeons and the American Society for Metabolic and Bariatric Surgery.
Nursing Care Management
Nurses play a key role in the adherence and maintenance phases of many weight-reduction programs. Nurses assess, manage, and evaluate the progress of many overweight adolescents. They also play an important role in recognizing potential weight problems and assisting parents and adolescents in preventing obesity. The nursing process in the care of the adolescent with obesity or overweight is outlined in the Nursing Process box.
The presence of obesity may not be obvious from appearance alone. Regular assessment of height and weight and computation of the BMI facilitate early recognition. Children with a BMI greater than or equal to the 95th percentile for age and sex should receive in-depth medical assessment. Children with a BMI in the 85th to 95th percentile range should be evaluated for secondary complications, such as hypertension and hyperlipidemia, and family history (Greaser and Whyte, 2004). Evaluation includes a height and weight history of the adolescent and family members, eating habits, appetite and hunger patterns, and physical activities. A psychosocial history is also helpful in understanding the impact of obesity on the child’s life.
Before initiating a treatment plan, it is important to be certain that the family is ready for change. Lack of readiness may result in failure, frustration, and reluctance to address the problem in the future. The nurse should explore with adolescents the reasons behind the desire to lose weight, since motivation to lose weight is the key to success. Adolescents need to take a personal responsibility for dietary habits and physical activity. Teens who are forced by their parents to seek help are seldom motivated, become rebellious, and are unwilling to control their dietary intake.
Nutritional Counseling.: Preventing an increase in body fat during growth is a realistic approach. This is often accomplished by adjusting three aspects of eating:
1. Reducing the quantity eaten by purchasing, preparing, and serving smaller portions
2. Altering the quality consumed by substituting low-calorie, low-fat foods for high-calorie foods (especially for snacks)
3. Altering situations by severing associations between eating and other stimuli, such as eating while watching television
The most successful diets are those that use ordinary foods in controlled portions rather than diets that require the avoidance of specific foods. Recently, low-carbohydrate diets such as the Atkins diet have been promoted for weight loss in adults and adolescents (Sondike, Copperman, and Jacobson, 2003). However, low-carbohydrate diets can result in ketosis, insulin resistance, and glucose intolerance. More research is needed to evaluate the long-term safety and efficacy of these diets for children and adolescents.
The nurse teaches adolescents and parents how to incorporate favorite foods into their diet and to select satisfying substitutes. The dieting teen should eat what the rest of the family eats, but less of it. When parents buy and prepare smaller amounts, they eliminate tempting second helpings and leftovers. To maintain a healthy diet, it is necessary to encourage the consumption of high-nutrient foods such as fruits, vegetables, whole grains, and low-fat dairy protein products. Calories and fat should be kept to a healthy level without being significantly restricted. To be successful, a dietary program should be nutritionally sound with sufficient satiety value, produce the desired weight loss, and be accompanied by nutrition education and continued support. Children and adolescents should not initiate a reduction diet without health assessment and counseling (Schwimmer, 2004).
Behavioral Therapy.: Altering eating behavior and eliminating inappropriate eating habits are essential to weight reduction, especially in maintaining long-term weight control. Most behavioral modification programs include the following concepts:
 A description of the behavior to be controlled, such as eating habits
A description of the behavior to be controlled, such as eating habits
 Attempts to modify and control the stimuli that govern eating
Attempts to modify and control the stimuli that govern eating
 Development of eating techniques designed to control speed of eating
Development of eating techniques designed to control speed of eating
 Positive reinforcement for these modifications through a suitable reward system
Positive reinforcement for these modifications through a suitable reward system
Specific strategies to modify eating habits are included in Box 17-3.
Group Involvement.: Commercial groups (e.g., Weight Watchers) or diet workshops composed primarily of adults may be helpful to some teenagers; however, a group of other adolescents is often more effective. Teenage groups include summer camps designed for obese young people and conducted by health professionals, school groups organized and led by a school nurse, and groups associated with special clinics.
These groups are concerned not only with weight loss but also with the development of a positive self-image and the encouragement of physical activity. Nutrition education, diet planning, and the improvement of social skills are essential components of these groups. Improvement is determined by positive changes in all aspects of behavior.
Family Involvement.: There is a definite connection between family environment, interaction, and obesity. The nurse needs to educate parents in the purposes of the therapeutic measures and their role in management. The family needs nutrition education and counseling regarding the reinforcement plan, alterations in the food environment, and ways to maintain proper attitudes. They can support their child in efforts to change eating behaviors, food intake, and physical activity.
Physical Activity.: Regular physical activity is incorporated into all weight-reduction programs. Any form of increased physical activity is beneficial, provided that the activities are age appropriate and enjoyable. Recommendations for physical activity need to consider the current health status and developmental level of the child or adolescent. The best choice for exercise is any form that is enjoyable and likely to be sustainable. Aerobic and endurance exercises help oxidize body fats. Light exercises like walking may provide an opportunity for the family to increase time together and increase caloric expenditure. Walking for 30 minutes each day and decreasing caloric intake by 500 calories per day may significantly reduce the risk of chronic disease. Weight training can increase basal metabolic rate and replace fat mass with muscle mass. However, weight training is not generally recommended for prepubertal children until they have reached physical and skeletal maturity. In prepubertal children increasing outdoor playtime is likely to be beneficial. Many children find exercise videos and treadmills boring and may not continue these activities. There are a great variety of physical activities to choose from that are likely to appeal to different people. Team sports and individual sports such as dance, bike riding, swimming, and karate are some. Limiting sedentary activities such as television viewing (while eating snacks!) is the most effective way to encourage physical activity (Robinson, 2001).
Prevention.: Weight loss programs do not enjoy the success of therapeutic interventions for other disorders. Gradual accumulation of adipose tissue during childhood establishes a pattern of eating that is difficult to reverse in adolescence. Prevention of obesity should begin in early childhood with the development of healthy eating habits, regular exercise patterns, and a positive relationship between parents and children. Prevention of adolescent obesity is best accomplished by early identification of obesity in the preschool, school-age, and preadolescent periods. Health care professionals should encourage frequent health care visits for children who are overweight or obese and incorporate a dietary history and counseling into each well-infant, well-child, and well-adolescent visit.
ANOREXIA NERVOSA AND BULIMIA NERVOSA
Anorexia nervosa (AN) is an eating disorder characterized by a refusal to maintain a minimally normal body weight and by severe weight loss in the absence of obvious physical causes. Approximately 5% of adolescent females in the United States have AN, and 5% to 10% of all cases occur in males (American Academy of Pediatrics, 2003). The average age of onset is 13 years, but the disorder can occur as early as 10 years of age and as late as 25 years of age. Individuals with AN are described as perfectionists, academically high achievers, conforming, and conscientious. Typically, they have high energy levels, even with marked emaciation. Patients with AN may eventually develop bulimia (Mehler, 2001).
Bulimia (from the Greek meaning “ox hunger”) refers to an eating disorder similar to AN. Bulimia nervosa (BN) is observed more commonly in older adolescent girls and young women; males with bulimia are less common. BN patients may be of average or slightly above average weight. BN is characterized by repeated episodes of binge eating followed by inappropriate compensatory behaviors, such as self-induced vomiting; misuse of laxatives, diuretics, or other medications; fasting; or excessive exercise (American Psychiatric Association, 2000). The binge behavior consists of secretive, frenzied consumption of large amounts of high-calorie (or “forbidden”) foods during a brief time (usually less than 2 hours). The binge is counteracted by a variety of weight control methods (purging). These binge-purge cycles are followed by self-deprecating thoughts, a depressed mood, and an awareness that the eating pattern is abnormal.
Although persons with BN have many issues in common with those who have other eating disorders, impulse control and satiety regulation are important problems in BN. Many individuals with BN begin with only occasional binges and purges “just for fun,” enjoying the control over their weight while eating amounts of food that would normally produce obesity. As the condition progresses, the frequency of binges increases, the amount of food consumed increases, and they gradually lose control over the binge-purge cycle. The frequency of binging can be anywhere from once per week to seven or eight times per day. Because persons with BN usually binge on high-calorie foods, especially sweets, ice cream, and pastries, insulin production is stimulated to cope with the added carbohydrates. When the food is vomited, the unused insulin stimulates hunger and the desire to eat.
A third eating disorder, identified as EDNOS (eating disorder not otherwise specified), has components of both AN and BN with varying degrees of symptomatology that are not always characteristic of the established diagnostic criteria for AN and BN (American Dietetic Association, 2006). Binge eating disorder (BED) is a type of EDNOS. Persons with BED may diet in an attempt to control their weight but without the extreme weight-control compensatory practices of vomiting, laxative use, diuretics, and excessive exercise (American Dietetic Association, 2006; Forman, 2007).
Etiology and Pathophysiology
The etiology of these disorders remains unclear. There is a distinct psychologic component, and the diagnosis is based primarily on psychologic and behavioral criteria. Dieting appears to be common to the initiation of both AN and BN. The disorders appear to be caused by a combination of genetic, neurochemical, psychodevelopmental, and sociocultural factors. The dominant aspects of AN are a relentless pursuit of thinness and a fear of fatness, usually preceded by a period of mood disturbances and behavior changes.
Weight loss may be triggered by a typical adolescent crisis such as the onset of menstruation or a traumatic interpersonal incident that precipitates serious, out-of-control dieting. Situations of severe family stress (such as parental separation or divorce) or circumstances in which the adolescent perceives a lack of personal control (such as teasing at school, changing schools, or going to college) may precipitate a desire for control and the decision not to eat. Frequently, there is an exaggerated misinterpretation of the normal fat deposition characteristic of early adolescence or anxiety because of comments that the adolescent is putting on weight.
Many experts have associated the development of an eating disorder with family characteristics such as an adolescent perception of high parental expectations for achievement and appearance, difficulty managing conflict and poor communication styles, enmeshment and occasionally estrangement between family members, devaluation of the mother or the maternal role, and marital tension. Families struggling with an eating disorder have been characterized as often having difficulties responding positively to the changing physical and emotional needs of the adolescent. Family stress of any kind may become a significant factor in the development of an eating disorder (Forman, 2007).
Society’s emphasis and the media’s focus on tall, thin individuals may also play a role. Studies evaluating the possible association of eating disorders and sexual abuse have been conflicting. Childhood sexual abuse may be a factor in some cases of AN.
Patients with eating disorders commonly have psychiatric problems, including affective disorder, anxiety disorder, obsessive-compulsive disorder, and personality disorder. Adult women with eating disorders were found to have higher rates of obsessive-compulsive behavior traits in their childhood. Patients with eating disorders have also been found to have higher reported rates of substance abuse, with alcohol problems being more common in those with BN than AN (Forman, 2007). It is important to note that many of the clinical findings are directly related to the state of starvation and improve with weight gain.
Many sports and artistic endeavors that emphasize leanness (e.g., ballet and running) and sports in which the scoring is partly subjective (e.g., skating and gymnastics) have been associated with a higher incidence of eating disorders such as AN. The term female athlete triad, characterized by disordered eating behavior, amenorrhea, and osteoporosis, has been applied to young women with restrictive eating disorders and amenorrhea (Rome, Ammerman, Rosen, and others, 2003).
A genetic role has been postulated for eating disorders; a significant number of young females with a first-degree relative having an eating disorder were at a significantly higher rate of having an eating disorder (Forman, 2007).
Diagnostic Evaluation
Diagnosis of AN is made on the basis of clinical manifestations (Box 17-4) and conformity to the criteria established by the American Psychiatric Association (2000) (Box 17-5). Diagnosis of BN is confirmed, according to the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (2000) (Box 17-6), by at least two binge-eating episodes per week for the preceding 3 months.
A complete history and physical examination are important to rule out other causes for weight loss. The medical assessment of an eating disorder focuses on the complications of altered nutritional status and purging. A careful history assesses weight changes, dietary patterns, and the frequency and severity of purging and excessive exercise. The patient’s weight and height should be measured and evaluated for appropriateness according to standard weight for height, age, and sex determined according to the percentile of his or her expected body weight or BMI.
Additional diagnostic measures may include a complete blood count to evaluate for anemia and other hematologic abnormalities; erythrocyte sedimentation rate or C-reactive protein to detect evidence of inflammation; electrolytes as well as calcium, magnesium, phosphorus, blood urea nitrogen, and creatinine; urinalysis, including specific gravity; and bone density studies for osteopenia, which is commonly observed in patients with AN. In patients with prolonged amenorrhea, human chorionic gonadotropin (hCG) is assessed to determine the presence of pregnancy. Other tests for patients with amenorrhea include thyroid function tests and measurement of serum prolactin and follicle-stimulating hormone to help rule out prolactinoma (hormone-secreting pituitary tumor), hyperthyroidism, hypothyroidism, or ovarian failure. In addition, a comprehensive cardiac evaluation is often recommended in those with AN. Further diagnostic tests may be required based on the history and findings from above diagnostic tests.
Therapeutic Management
The treatment of AN involves four major goals:
1. Restoration of a healthy weight
2. Establishment of healthy eating patterns
3. Resolution of disturbed patterns of family interaction
4. Individual psychotherapy to correct deficits and distortions in psychologic functioning
Most adolescents are treated on an outpatient basis, but those with problems requiring immediate medical attention, such as severe malnutrition or electrolyte or psychiatric disturbances (severe depression or suicidal ideation), require hospitalization. A multidisciplinary team of dietitians, physicians, nurses, and counselors provide the interventions.
Persons with BN may benefit from cognitive behavioral therapy, other psychotherapy, antidepressant medications, or a combination of antidepressant medication and psychotherapy (Forman, 2007).
Nutrition Therapy.: The most important goal is to treat any life-threatening malnutrition and to restore dietary stability and weight gain. This may require the administration of tube feedings or intravenous fluids if the malnutrition is severe. In most cases, it is best to reintroduce food and snacks slowly in a stepwise manner. A reasonable goal is to reach an eventual intake of 2000 to 3000 kcal per day and a weight gain of 0.22 to 0.45 kg (0.5 to 1 pound) per week (American Dietetic Association, 2006). When restoring nutrition, health professionals must avoid the refeeding syndrome, which consists of cardiovascular, neurologic, and hematologic complications that occur when nutritional replacement is given too rapidly. This syndrome can be avoided with slow refeeding and the addition of phosphorus when total body phosphorus is depleted. Treatment goal weights are individualized and based on age, height, stage of puberty, premorbid weight, and previous growth charts. In girls who have reached menarche, resumption of menses is an objective measure of return to biologic health.
Dietary interventions are combined with psychotherapy to improve the underlying psychologic misconceptions about weight loss. Another aspect of treatment is to relieve the anxiety related to eating and the depression that accompanies the disorder. The administration of antianxiety or antidepressant medications is beneficial. However, when these drugs are used, patients should be carefully monitored for cardiovascular side effects.
Psychotherapy.: Behavioral interventions are often necessary to encourage patients to accomplish the desired caloric intake and weight gain. Weight restoration as an outpatient is accomplished with behavioral contracts negotiated between the therapists and patient. The goal is to increase the patient’s feelings of control and responsibility toward achieving recovery. The contract can stipulate at what weight tube feedings will be implemented. Individual psychotherapy is aimed at helping the young person resolve the adolescent identity crisis, particularly as it relates to a distorted body image. If the disorder is related to a dysfunctional family situation, therapy is most successful when it is started soon after the onset of illness and directed toward disengagement and redirection of malfunctioning processes in the family.
Pharmacologic Therapy.: Pharmacotherapy in the treatment of AN has been disappointing so far. The few studies that have been done have primarily evaluated medications’ efficacy in the treatment of comorbid disorders such as obsessive-compulsive disorders and depression. Anxiolytic medications may be helpful before meals to relieve some patients’ anxiety.
Tricyclic antidepressants and fluoxetine belong to a group of medications known as selective serotonin reuptake inhibitors (SSRIs), which have been more successful when used with BN. There is also some evidence that tricyclic antidepressants such as desipramine, imipramine, and amitriptyline; monoamine oxidase inhibitors; and buspirone are more effective compared with a placebo in decreasing binging and vomiting in patients with BN. Topiramate, an antiepileptic agent, and the selective serotonin antagonist ondansetron may have some benefit in treating BN.
Nursing Care Management
Nurses need to adopt and maintain a kind and supportive yet firm manner in managing the care of the adolescent with eating disorders without creating a passive-dependent attitude. The individual requires sustained support and reassurance to cope with ambivalent feelings related to body concept and the desire to be seen as cooperative, reliable, and worthy of receiving kindness. Encouraging the adolescent with education and activities that strengthen self-esteem facilitates the resocialization process and promotes social acceptance among peers.
It is important for nurses to be aware of the physical side effects of AN. Patients frequently limit their fluid intake. Urinary tract problems are common, and ketones and protein may be detected in the urine as a result of breakdown of fat and protein. Vital sign instability can be severe and can include orthostatic hypotension; the pulse becomes irregular, and the rate decreases markedly. Bradycardia and hypothermia can result in cardiac arrest (see Critical Thinking Exercise).
The team responsible for the management of young people with AN arranges a carefully structured environment. First, there must be consistency. The team decides on an approach and adheres to it. The plan is structured with reality testing regarding caloric intake and body-image perception as an essential component. The team members provide a unified front to avoid any possibility of manipulation or inconsistency. Second, all team members are involved; responsibility for the program cannot be left to one person. The role and boundaries of each member are clearly spelled out. Third, continuity of team members is important; it is helpful to have the same team members all the time.
Fourth, communication among team members is essential. Communication with the patient regarding what is expected is also important. Sometimes the limit setting may seem unreasonable; if the adolescent does not understand the rationale for the limits, he or she may sabotage the entire program. It is also important to communicate with the family. Fifth, the plan must provide for support of the adolescent, the family, and team members. The adolescent’s efforts should be supported, and positive feedback should be provided for accomplishments made in normalizing eating habits. Meetings are held to discuss the feelings and concerns of the patient, immediate caregivers, and team members.
A behavioral contract, an agreement that the adolescent makes with others to change a maladaptive behavior, has proved to be effective in some cases. The written contract is constructed by the therapeutic team and approved and signed by the adolescent. Unless the adolescent agrees to its terms, the contract can become the source of a power struggle. However, it can be an effective tool that places the responsibility for weight gain or other behavioral change on the adolescent.
Nursing care of the adolescent with BN is similar to care of the patient with AN. Acute care involves careful monitoring of fluid and electrolyte alterations and observation for signs of cardiac complications. Nutritional consultation and follow-up care are essential. The nurse should encourage the adolescent and family members to structure the environment to reduce the binging behavior. Getting rid of binge foods; restricting eating to one room of the house; not engaging in other activities while eating; and substituting exercise, crafts, visualization, and relaxation techniques for binging are helpful interventions.
Health professionals, patients, and families can find assistance and information from several organizations. The National Association of Anorexia Nervosa and Associated Disorders, Inc.,* and the National Eating Disorders Association† provide counseling, referrals, and self-help programs.
DISORDERS WITH BEHAVIORAL COMPONENTS
ATTENTION DEFICIT HYPERACTIVITY DISORDER AND LEARNING DISABILITY
Attention deficit hyperactivity disorder (ADHD) refers to developmentally inappropriate degrees of inattention, impulsiveness, and hyperactivity. To be diagnosed as ADHD, the symptoms must have been present before age 7 years and must be present in at least two settings. In addition, the persistence of developmentally inappropriate and marked inattention must not be a symptom of another disorder (American Psychiatric Association, 2000). A learning disability (LD) refers to a heterogeneous group of disorders manifested by significant difficulties in the acquisition and use of listening, speaking, reading, writing, reasoning, or mathematic skills.
ADHD and LDs affect every aspect of the child’s life but are most obvious in the classroom. Early identification of affected children is important because the characteristics of these disorders significantly interfere with the normal course of emotional and psychologic development. Many children develop maladaptive behavior patterns that impede psychosocial adjustment while they try to cope with cognitive dysfunction. Their behavior evokes negative responses from others, and repeated exposure to negative feedback adversely affects their self-concept. The characteristics of ADHD affect the child’s written and adaptive skills, social status, and self-esteem (Myers, Eisenhauer, and Ryan, 2003).
Diagnostic Evaluation
The behaviors exhibited by the child with ADHD are not unusual. The difference lies in the quality of motor activity and developmentally inappropriate inattention, impulsivity, and hyperactivity that the child displays. The manifestations may be numerous or few, mild or severe, and vary with the child’s developmental level. Any given child will not have every symptom of the condition. The basic characteristics of ADHD are outlined in Box 17-7.
A comprehensive battery of tests is needed to confirm an LD. These include intelligence tests (many children have normal or above-average intelligence quotients [IQs]); hand-eye coordination tests; and measurements of auditory and visual perception, spatial organization, comprehension, and memory. Often there is a wide gap between verbal and performance scores on IQ tests.
Behavioral checklists and adaptive scales are also helpful in measuring school adaptive functioning in children with ADHD. Psychiatric disorders, medical problems, and traumatic experiences are ruled out, including lead poisoning, seizures, partial hearing loss, psychosis, and witnessing of sexual activity or violence.
Therapeutic Management
Management of the child with ADHD usually involves multiple approaches that include family education and counseling, medication, proper classroom placement, environmental manipulation, and behavioral therapy or psychotherapy for the child. Interventions for children with LD are primarily educational.
Pharmacologic Therapy.: Stimulant medications or behavioral therapy are appropriate for the school-age child with ADHD (American Academy of Pediatrics, 2001c). The most frequently prescribed medications are the psychostimulants methylphenidate hydrochloride (Ritalin) and dextroamphetamine sulfate (Dexedrine). These medications increase dopamine and norepinephrine levels that lead to simulation of the inhibitory system of the central nervous system. The tricyclic antidepressants imipramine, desipramine, and nortriptyline are also used; these antidepressants block norepinephrine and serotonin at the nerve endings and increase the action of these substances in nerve cells. Clonidine, used occasionally in the treatment of ADHD, has been recommended primarily for children with ADHD and coexisting conditions such as sleep disturbances (American Academy of Pediatrics, 2001c). Atomoxetine (Strattera), a presynaptic norepinephrine transport inhibitor (nonstimulant), is now available for use in children and adolescents and has proved effective in the treatment of adolescents with ADHD (Michelson, Faries, Wernicke, and others, 2001; Spencer, Wilens, Biederman, and others, 2006).
Regularly scheduled evaluations of the child are essential with all these medications. Children taking stimulant medication may have side effects that include nervousness, tics, insomnia, increased blood pressure, and decreased appetite with subsequent weight loss (see Critical Thinking Exercise). Long-term use of dextroamphetamine may result in suppression of growth.
Behavioral Therapy.: Behavioral therapy focuses on the prevention of undesired behavior. Families are helped to identify new appropriate contingencies and reward systems to meet the child’s developing needs. They may also receive instruction in effective parenting skills, such as delivering positive reinforcement, rewarding small increments of desired behaviors, and providing age-appropriate consequences (e.g., time-out, response cost). Use of organizational charts for completing self-care activities and use of a word processor instead of manually writing out assignments are emphasized. Through collaborative teamwork, parents learn techniques to help the child become more successful at home and in school.
Environmental Manipulation.: Families are encouraged to learn how to modify the environment to allow the child to be more successful. Consistency is especially important for children with ADHD. Consistency between families and teachers in terms of reinforcing the same goals is essential. Fostering improved organizational skills requires a more highly structured environment than most children need. The child should be encouraged to make more appropriate choices and to take responsibility for his or her actions.
Other helpful interventions include teaching parents how to make organizational charts (e.g., listing all activities that must be performed before leaving for school) and decrease distractions in the environment while the child is completing homework (e.g., turning the television off, having a consistent study area equipped with needed supplies) and helping parents to understand ways to model positive behaviors and problem solving. The focus is on strategies to help the child succeed and cope with deficits while emphasizing strengths.
Appropriate Classroom Placement.: Children with ADHD need an orderly, predictable, and consistent classroom environment with clear and consistent rules. Homework and classroom assignments may need to be reduced, and more time may need to be allotted for tests to allow the child to complete the task. Verbal instructions should be accompanied by visual references such as written instructions on the blackboard. Schedules may need to be arranged so that academic subjects are taught in the morning when the child is experiencing the effects of the morning dose of medication. Low-interest and high-interest classroom activities should be intermingled to maintain the child’s attention and interest. Regular and frequent breaks in activity are helpful because sitting in one place for an extended time may be difficult. Computers are helpful for children who have difficulty with writing (dysgraphia) and fine motor skills; in such children handwriting will not improve. They need to find alternatives to physical competition that requires coordination of movement (Selekman and Snyder, 2000).
If the child has an LD, special training activities may be accomplished in self-contained classes limited to six to eight children, in special resource rooms with equipment and teaching teams, by mobile consultants who move from room to room to provide assistance to teachers and children, and in special first-grade programs in which high-risk children receive special attention to prevent or reduce the need for services as they progress. The purpose of programs for children with LDs is to assist them toward more successful achievement, personal adjustment, and retention in the regular classroom.
Prognosis.: With appropriate intervention ADHD is relatively stable through early adolescence for most children. Some children experience decreased symptoms during late adolescence and adulthood, but a significant number of these children carry their symptoms into adulthood. The goal for children with LDs is to help them identify their areas of weakness and learn to compensate for them.
Nursing Care Management
Nurses are active participants in all aspects of management of the child with ADHD or LD. Nurses in the community work with families and school personnel on a long-term basis to help plan and implement therapeutic regimens and to evaluate the effectiveness of therapy. They coordinate services and serve as a liaison between health and education professionals directly involved in the child’s therapy program. School nurses understand the child’s special needs and work with teachers (see Family Focus box). Nurses in any setting (community, school, hospital, practitioner’s office) provide support and guidance to children and families during the difficult period of the child’s growing up with a disabling condition.
Management begins with an explanation to the parents and the child about the diagnosis, including the nature of the problem and the practitioner’s concept of the underlying central nervous system basis for the disorder. Most parents are confused and feel some measure of guilt. To some parents, a diagnosis of ADHD is confirmation of the fear that their child has some irreversible, serious disease; to others it is a relief. All need the opportunity to vent their feelings and suspicions.
Parents need information about the prognosis and an understanding of the treatment plan. The greater their understanding of the disorder and its effects, the more likely they will be to carry out the recommended program of therapy. It is important that they understand that the therapy is not necessarily a panacea and that it will extend over a long period. This has particular significance for changes they need to make in environmental management. Reading material to help the child and family can be obtained from a variety of sources.
POSTTRAUMATIC STRESS DISORDER
Posttraumatic stress disorder (PTSD) refers to the development of characteristic symptoms after exposure to an extremely traumatic experience or catastrophic event. The traumatic experience is typically life-threatening to self or a significant other and may involve grotesque mutilation or death, serious injury, or physical coercion (e.g., an assault, a natural disaster, sexual abuse, witnessing violence). It is important to note that PTSD is not limited to children who have lived in “war-torn” countries. Events such as automobile, school, or recreational accidents and bullying have been identified as causes of PTSD (Sundelin-Wahlsten, Ahmad, and von Knorring, 2001). The characteristic symptoms are persistent reexperiencing of the traumatic event, avoidance of stimuli associated with the event or trauma, numbing of general responsiveness, and increased arousal.
The response to the event takes place in three stages. The initial response involves intense arousal, which usually lasts for a few minutes to 1 or 2 hours. The stress hormones are at the maximum as the individual prepares for “fight or flight.” A prolonged arousal phase may indicate psychosis.
The second phase, which lasts approximately 2 weeks, is one in which defense mechanisms are mobilized. It is a period of quiescence in which the event appears to have produced no impression. The child feels numb, and stress hormone secretion is absent. Defense mechanisms are less adaptive to specific situations and may not be what the situation demands. Denial that anything is wrong is a frequently observed defense mechanism.
The third phase is one of coping and consciously directed inquiry, which normally extends over 2 to 3 months. The victims want to know what happened and appear to be getting worse, when actually they are getting better. Numerous psychologic symptoms, such as depression, phobia, anxiety, and conversion reactions, may be present. Children frequently display repetitive actions. They play out the situation over and over again in an attempt to come to terms with their fear. Flashbacks are common. This phase can be self-perpetuating, and a prolonged reaction can develop into an obsession with the traumatic event. Some traumatic effects remain indefinitely.
Nursing Care Management
Children need to deal with any traumatic event. Their reactions depend heavily on their social environment and the way in which their caretaking adults react to the event. In the second phase of PTSD, the appropriateness of the defense mechanism must be assessed, and children must be assisted in application of their defense. If children do not engage in some catharsis or if their defense phase is prolonged, they need referral for special psychologic help.
Coping is a learned response, and children in the third phase can be helped to deal with their fear. Children usually are willing to accept reasoning. Those who are assisted in their catharsis and allowed expression will survive without serious lasting effects. They should be encouraged to play out the stress and to discuss their feelings about the event. If they are unable to do this, they may become obsessed with the traumatic event and require professional help. Conversion reactions are common obsessive behaviors in children suffering from PTSD.
Children need professional help if any of the phases of PTSD are prolonged. Boys tend to have a prolonged defense phase more often than girls. Occasionally the event will be unrecognized, and the affected child will engage in what is considered to be unusual behavior. Children exhibiting any sudden change in behavior need to be assessed for a traumatic event. When the change in behavior is traced to a traumatic event, treatment can be implemented.
SCHOOL PHOBIA
Children, other than beginning students, who resist going to school or who demonstrate extreme reluctance to attend school for a sustained period as a result of severe anxiety or fear of school-related experiences are said to have school phobia. The terms school refusal and school avoidance are also used to describe this behavior. School avoidance behaviors occur in both boys and girls and in children from all socioeconomic levels.
Physical symptoms are prominent and may affect any part of the body (e.g., anorexia, nausea, vomiting, diarrhea, dizziness, headache, leg pains, abdominal pains, even a low-grade fever). A striking feature of school phobia is the prompt subsiding of symptoms when it is evident that the child can remain home. Another significant observation is absence of symptoms on weekends and holidays unless they are related to other places such as Sunday school or parties. Occasional mild reluctance is not uncommon among school children, but if the fear continues for longer than a few days, it must be considered a serious problem.
Nursing Care Management
Treatment for school phobia depends on the cause. The primary goal is to return the child to school. The longer a child is permitted to stay out of school, the more difficult it is for the child to reenter. Parents must be convinced gently but firmly that immediate return is essential and that it is their responsibility to insist on school attendance.
A school reentry protocol may be necessary for the child with severe symptoms. In reentry programs, the child role-plays routines involved in getting ready for school and that occur at school. Relaxation techniques are also used. The child usually goes to school initially for a half-day and then progresses to a full day. Often the school nurse is asked to provide support to the parents and the teacher during the reentry process. If the problem persists, professional help is recommended.
RECURRENT ABDOMINAL PAIN
Recurrent abdominal pain (RAP) is a complaint that is often attributed to psychogenic factors, although it can be a symptom of either psychosomatic or organic disease. RAP is defined as three or more separate episodes of abdominal pain during a 3-month period that interferes with functioning; the symptoms may be similar to the “spastic” or “irritable” colon syndrome of adulthood. The American Academy of Pediatrics (2005b) recently suggested retiring the term recurrent abdominal pain in favor of functional abdominal pain, noting that the majority of cases of chronic abdominal pain in children are functional. Functional abdominal pain is categorized as one or a combination of the following: irritable bowel syndrome, functional stomach upset (dyspepsia), or abdominal migraine. In functional abdominal pain, or RAP, there is no demonstrable evidence of a pathologic condition. Children with RAP have real pain that is usually located in the periumbilical or epigastric area. On palpation the pain is likely to be experienced in the epigastric area or in the lower right or left quadrant and is accompanied by vague tenderness without muscle guarding. The pain is irregular in time, duration, and intensity and associated with either loose or pellet-formed stools. Other symptoms that may accompany the pain are headache, pallor, dizziness, dysuria, flushing, vomiting, diarrhea, and fatigue.
Children at risk for RAP tend to be high achievers who have extensive personal goals or whose parents have unusually high expectations. They are described as sensitive and overly concerned about what others think of them. They are uncomfortable with expressions of anger or argument, especially with persons who are significant in their life. School attendance is adversely affected, and these children may exhibit poor learning performance. It is not uncommon for symptoms to be aggravated during school days.
Treatment involves providing reassurance and reducing or eliminating the symptoms. Hospitalization may be necessary, and the child frequently shows improvement in the hospital. Initial efforts are directed toward ruling out organic causes of the pain, relieving discomfort, and attempting to determine the situations that precipitate attacks. A high-fiber diet, psyllium bulk agents, lubricants such as mineral oil, and bowel training are emphasized for pain associated with bowel patterns. Treatment may also include acid-reduction therapy for pain associated with dyspepsia, antispasmodic agents, smooth muscle relaxants, or low doses of psychotropic agents. Other treatments include cognitive-behavioral therapy and biofeedback.
Nursing Care Management
Once the diagnosis has been established, the parents and the child need an explanation of the pain, which can be compared to a skeletal muscle cramp, “charley horse,” or headache for easier comprehension. Reassurance that the symptoms are not unique to their child and that the pain is rarely associated with a severe disease can be helpful in relieving parental fears and anxieties.
The simple measure of having the child rest in a peaceful, quiet environment and providing comfort will often relieve the symptoms in a short time. A heating pad may also help ease the discomfort (see Nonpharmacologic Management, Chapter 7). When pain is not relieved by these simple measures, the parents are taught how to administer antispasmodics, if prescribed. For example, if pain is precipitated by meals, having the child take the medication 20 to 30 minutes before mealtime may prevent an episode.
The most valuable assistance that the nurse can provide is support and reassurance to the family. When open communication is established and families appreciate the relationship between stress-provoking situations and the child’s symptoms, the chance for remedial action is enhanced. Follow-up care and continued support are essential because the symptoms tend to remit and exacerbate. The availability of a supportive health professional is a source of comfort to the child and family.
CONVERSION REACTION
Conversion reaction, also known as hysteria, hysterical conversion reaction, and childhood hysteria, is a psychophysiologic disorder with a sudden onset that can usually be traced to a precipitating environmental event. In childhood the disorder is observed with equal frequency in both sexes, but girls outnumber boys during adolescence.
The manifestations involve primarily the voluntary musculature and special senses. Symptoms include abdominal pain, fainting, pseudoseizures, paralysis, headaches, and visual field restriction. The most common symptom is seizure activity, which can be differentiated from symptoms of neurogenic origin by formal tests. A normal electroencephalogram indicates that the origin is not neurogenic. Many children with a conversion reaction have experienced a major family crisis (such as the loss of a parent or other significant person through death, divorce, or moving) before the onset of symptoms.
CHILDHOOD DEPRESSION
Depression in childhood is often difficult to detect because children may be unable to express their feelings and tend to act out their problems and concerns. Some states of depression are temporary, such as acute depression precipitated by a traumatic event. The event might include a period of hospitalization; loss of a parent through death or separation; or loss of a significant relationship with something (a pet), a person (a friend, significant other, or family member), or a place (move from a familiar home, neighborhood, or city). Children with depression may demonstrate a variety of behaviors (Box 17-8). Most responses in children are not sustained and can be modified with social and family support.
More serious and less common are the depressive responses to chronic stress and loss; these are frequently observed in children with chronic illness or disability when other family members have denial depression. There is no apparent precipitating event, but there is often a history of frequent disruptions in important relationships. Often, there is also a history of depressive illness in one or both parents. Manifestations in the child are similar to those observed in acute depression, but they occur more frequently and extend over a longer period.
Nursing Care Management
Depressed children are managed by a health team especially prepared in the care of children with mental disorders. Treatment is highly individualized and undertaken in the least restrictive environment. Suicidal children are admitted to the hospital for protection if the family is unable to provide constant monitoring. Pharmacotherapy may involve tricyclic antidepressants or SSRIs such as fluoxetine (Prozac), trazodone (Desyrel), sertraline (Zoloft), paroxetine (Paxil), bupropion (Wellbutrin), and venlafaxine (Effexor).
Nurses should be aware that depression is a problem that can be easily overlooked in the child and one that can interrupt normal growth and development. Recognizing depression and suicidal tendencies in depressed adolescents and making appropriate referrals are important nursing functions. Identification of the depressed child requires a careful history (health, growth and development, social and family health); interviews with the child; and observations by the nurse, parents, and teachers (see also Suicide, p. 568). Some antidepressant medications may cause increased suicidal thinking and behaviors in pediatric patients. This has prompted the U.S. Food and Drug Administration (FDA) to recommend black box drug warnings detailing potential suicide-related risks for pediatric patients (Jick, Kaye, and Jick, 2004; US Food and Drug Administration, 2004). In 2007 the FDA expanded the black box warning, noting that the risk of suicide was highest among adolescents and young adults ages 18 to 24 years, yet added that there is risk in not administering antidepressants. Some data suggest that the suicide rate among adolescents on therapeutic doses of SSRIs was lower than among those who were not being treated with antidepressant medication (Gibbons, Hur, Bhaumik, and others, 2006). However, the issue remains controversial, and further studies are needed.
CHILDHOOD SCHIZOPHRENIA
Childhood schizophrenia is a term that refers to severe deviations in ego functioning and is generally reserved for psychotic disorders that appear in children younger than 15 years of age. Childhood schizophrenia is a rare illness among children in the general population; among children with mental illness, only about two in every 1000 have childhood schizophrenia.
Childhood schizophrenia is characterized by symptoms that last for at least 6 months and that seriously interfere with the child’s functioning in school, at home, or in other social situations. The basic disturbance is a lack of contact with reality and the subsequent development of a world of the child’s own. Other areas of development that may be impaired include cognition, perception, emotion, language, and physical motor control. The most common manifestations involve language disturbances, impaired interpersonal relationships, and inappropriate affect (outward expression of emotion). Treatment involves management of the symptoms, prevention of relapse, and social and occupational rehabilitation of the young person. Antipsychotic drugs that may be used include haloperidol, clozapine, chlorpromazine, olanzapine, quetiapine fumarate, and risperidone. Family interventions and family therapy often result in improvements in psychotic symptoms, thought disorders, and social functioning among children with schizophrenia.
Nursing Care Management
Nursing of psychotic children is a highly specialized area. However, nurses should be alert to the possibility that schizophrenia can occur in children and refer children who consistently demonstrate abnormal behavior to a psychiatrist for evaluation. In addition, nurses will need to teach family members of children taking antipsychotic drugs to observe for possible side effects. Common side effects of these drugs include dizziness; drowsiness; tachycardia; hypotension; and extrapyramidal effects, such as abnormal movements and seizures.
SERIOUS HEALTH PROBLEMS OF LATER CHILDHOOD AND ADOLESCENCE
Although experimentation with drugs during childhood and adolescence is widespread, most children and teens do not become high-risk users. National and statewide surveys indicate that despite a steady increase in the incidence of adolescents using tobacco, alcohol, and marijuana between the ages of 12 and 18, experimentation is limited to one adolescent in eight for stimulants and inhalants and to less than one adolescent in 10 for “hard” drugs such as hallucinogens, sedatives, and crack cocaine. It has been reported that as many as 51% of American youth have tried an illegal drug by the time of high school graduation (American Academy of Pediatrics, 2005c). Although surveys demonstrate a modest decrease in the use of certain substances among youth (marijuana, amphetamines, barbiturates, and tranquilizers), abuse of other drugs (cocaine, steroids, heroine, flunitrazepam) has remained steady (American Academy of Pediatrics, 2005c; Centers for Disease Control and Prevention, 2006b).
Drug abuse, misuse, and addiction are culturally defined and are voluntary behaviors. Drug tolerance and physical dependence are involuntary physiologic responses to the pharmacologic characteristics of the drugs, such as opioids and alcohol. Consequently, an individual can be addicted to a narcotic with or without being physically dependent. A person can also be physically dependent on a narcotic without being addicted (e.g., patients who use opioids to control pain).
Motivation
Most drug use begins with experimentation. The drug may be used only once, may be used occasionally, or may become part of a drug-centered lifestyle. Children and adolescents initiate drug use out of curiosity. Adolescents who use drugs may fall into one of two broad categories—experimenters and compulsive users—or they may fall into a third category somewhere on the continuum between these extremes, referred to as recreational users, principally of drugs such as marijuana, cocaine, alcohol, and prescription drugs. For many the goal is peer acceptance; these users fit more closely with the experimenting, intermittent users. For others the goal is intoxication or the sustained intense effects from using a particular drug; these users resemble the compulsive users. These users may engage in periodic heavy use, or binges. The groups of greatest concern to health care workers are those whose patterns of use involve high doses or mixed drugs with the danger of overdose, and those compulsive users with the threat of dependence, withdrawal syndromes, and altered lifestyle.
Types of Drugs Abused
Any drug can be abused, and most are potentially harmful to adolescents still going through formative life experiences. Although rarely considered drugs by society, the chemically active substances frequently abused are the xanthines and theobromines contained in chocolate, tea, coffee, and colas. Ethyl alcohol and nicotine are other drugs that are legal and socially sanctioned. Any of these substances can produce mild to moderate euphoric or stimulant effects and can lead to physical and psychologic dependence.
Drugs with mind-altering abilities that are available on the “street” and are of medical and legal concern are the hallucinogenic, narcotic, hypnotic, and stimulant drugs. In addition, health professionals are concerned about the use of alcohol and volatile substances that are inhaled to achieve altered sensation (such as gasoline, antifreeze, plastic model airplane cement, typewriter correction fluid, and organic solvents). Recently, abuse of prescription and synthetic drugs such as oxycodone, alprazolam (Xanax), and amphetamine-dextroamphetamine (Adderall) has become a concern for professionals who work with children and adolescents. Many of the prescription drugs are available at a decreased cost in comparison to the more exotic drugs of abuse and are often found in the medicine cabinet at home. Internet websites also promote the “safe use” of some psychoactive drugs and supply information on new “designer” drugs that are not detectable on a standard urine drug screening test.
Tobacco.: Cigarette smoking has continued to decline since the late 1990s, in part due to increased costs, changes in community attitudes about smoking among adults, decreased advertising of cigarettes to children, and increased antismoking advertising as a result of the government lawsuits against tobacco companies (Johnston, O’Malley, Bachman, and others, 2005). From 2001 to 2002, 13.3% of children in middle school and 28.2% of high school students reported tobacco use of some type (Centers for Disease Control and Prevention, 2006c). In another survey cigar smoking ranked second for form of tobacco used among those surveyed, and smokeless tobacco reportedly was third (Centers for Disease Control and Prevention, 2006b).
Although the number of adult and adolescent smokers has declined in recent years, cigarette smoking is still considered the chief avoidable cause of death. The hazards of smoking at any age are undisputed; however, a preventive approach to teenage smoking is especially important. Because of its addictive nature, smoking begun in childhood and adolescence can result in a lifetime habit, with increased morbidity and early mortality. Smoking in adolescence has also been related to other risk behaviors: approximately three times as many adolescents who smoke report carrying weapons and drinking alcohol compared with adolescents who do not smoke; other associated risks in Caucasians include use of smokeless tobacco, marijuana use, multiple sexual partners, not using bicycle helmets, and binge drinking. Research also indicates an association between current use of tobacco and the development of depression (Goodman and Capitman, 2000) and sleep problems (Patten, Choi, Gillin, and others, 2000) in adolescence. Cigarettes are considered to be a gateway drug, and teenagers who smoke are 11.4 times more likely to use illicit drugs (Gordon, 2000).
The effects of second-hand smoke exposure are also well known and include increased incidence of low birth weight and subsequent illness, increased incidence of sudden infant death syndrome (if mother smoked during pregnancy), increased incidence of acute lower respiratory tract infections, and exacerbation of asthma symptoms (wheezing, cough, phlegm, breathlessness) in asthmatic children (US Department of Health and Human Services, 2006).
Etiology.: Teenagers begin smoking for a variety of reasons, including imitation of adult behavior; peer pressure; a desire to imitate behaviors and lifestyles portrayed in movies and advertisements; and a desire to control weight, especially among females. Teenagers who do not smoke usually have family members and friends who do not smoke or who oppose smoking. Most teens who refrain from smoking have a desire to succeed in academics or athletics (particularly high-performance sports, such as basketball, swimming, and track) and plans to go to college (see Community Focus box). Although smoking among college students has increased in recent years, rates of smoking are highest among adolescents who do not complete high school.
Smokeless Tobacco.: The term smokeless tobacco refers to tobacco products that are placed in the mouth but not ignited (e.g., snuff and chewing tobacco). This substitute for cigarettes continues to pose a hazard to adolescents, although use has declined by about 50% since the peak prevalence in 1995; in 2004 only 16.7% of teens tried smokeless tobacco by the twelfth grade (Johnston, O’Malley, Bachman, and others, 2005). Many children and adolescents believe that smokeless tobacco is a safe alternative to cigarette smoking and is not addictive, and they believe they can stop using it at any time. However, the number of adolescents who identify it as a health risk has increased since the mid-1990s, with nearly half now agreeing it has health risks (Johnston, O’Malley, Bachman, and others, 2005). These products have also been proved to be carcinogenic, and regular use can cause dental problems, foul-smelling breath, and tooth erosion or loss.
Nursing Care Management.: Prevention of regular smoking in teenagers is the most effective way to reduce the overall incidence of smoking. A variety of methods have been employed. Posters, charts, displays, statistics, and the use of examples of actual damaged lungs to communicate the hazards of smoking all have their supporters and doubters. Some schools also use films and demonstrations in science classes.
For the most part, smoking-prevention programs that focus on the negative, long-term effects of smoking on health have been ineffective. Youth-to-youth programs and those emphasizing the immediate effects are more effective but primarily in improving teenagers’ attitudes toward not smoking. Because smoking and smoking-related behaviors are social symbols, antismoking campaigns must address the norms of potential smokers. Anything that ridicules or threatens the social norms of the peer group can be unproductive or counterproductive. Investigators have found that teaching resistance to peer pressure to smoke is effective in early adolescence. Although the effects of these programs may decrease with time, the effects can be enhanced in older adolescents by presenting information in class instead of simply handing out written material to the students (Adelman, Duggan, Hauptman, and others, 2001).
Two areas of focus for antismoking programs are peer-led programs and use of media in smoking prevention (e.g., CDs, videotapes, and films). Peer-led programs emphasizing the social consequences of smoking have proved most successful. If a significant number of influential peers can “sell” their classmates on the idea that the habit is not popular, the followers will imitate their behavior. Such programs emphasize short-term rather than long-term consequences (e.g., the effects of smoking on personal appearance, such as unattractive stains on teeth and hands and unpleasant odor of breath and clothing).
The impact of school-based antismoking programs can be strengthened by expanding these programs to include parents, mass media, youth groups, and community organizations. For example, mass media efforts that involve antismoking radio campaigns have been identified as the most cost-effective mass media intervention.
Smoking bans in schools also accomplish several goals: (1) they discourage students from starting to smoke, (2) they reinforce knowledge of the health hazards of cigarette smoking and exposure to environmental tobacco smoke, and (3) they promote a smoke-free environment as the norm (see Community Focus box).
Alcohol.: Acute or chronic abuse of alcohol (ethanol) is responsible for many acts of violence, suicide, accidental injury, and death. Alcohol drinking is likely to begin in the middle school years and increases with age. By 18 years of age, 80% to 90% of adolescents have tried alcohol. Ethanol is a depressant that reduces inhibitions against aggressive and sexual acting out. Severe physical and psychologic symptoms accompany abrupt withdrawal, and long-term use leads to slow tissue destruction, especially of the brain and liver cells. The most noticeable effects of alcohol occur within the central nervous system and include changes in cognitive and autonomic functions such as judgment, memory, learning ability, and other intellectual capacities. Young alcoholics often drink alone and cannot control their use of alcohol. They often rely on the substance as a defense against depression, anxiety, fear, or anger. Not all of these characteristics are observed in the adolescent who is abusing alcohol, but if several signs are evident, the child or adolescent should be considered at risk. Referral to a health care professional and detoxification therapy may be necessary. Information about alcohol and answers to questions are available through the Alcohol Hotline.* Other groups that provide support and counseling for families are Al-Anon, Ala-Teen, Ala-Tot, and Alcoholics Anonymous (an organization that has listings in all local telephone directories).
Cocaine.: Although cocaine is not pharmacologically considered a narcotic, it is legally categorized as such. Cocaine is available in two forms: water-soluble cocaine hydrochloride, which is administered by “snorting” or intravenous injection, and nonsoluble alkaloid (freebase) cocaine, which is used primarily for smoking. Crack, or “rock,” is a purer, more menacing form of the drug. It can be produced cheaply and smoked in either water pipes or mentholated cigarettes. The use of cocaine has increased in recent years because of its availability and affordability, its association with persons in glamorous occupations, peer pressure, and its reputation as a sexually enhancing drug.
Cocaine creates a sense of euphoria, or an indefinable high. Withdrawal does not produce the dramatic symptoms observed in withdrawal from other substances. The effects are those commonly seen in depression, including lack of energy and motivation, irritability, appetite changes, psychomotor retardation, and irregular sleep patterns. More serious symptoms include cardiovascular manifestations and seizures. Physical withdrawal should not be confused with the so-called crash after a cocaine high, which consists of a long period of sleep. Answers to questions about the risks of using cocaine are available at the National Cocaine Hotline,† which also provides referrals to support groups and treatment centers.
Narcotics.: Narcotic drugs include opiates such as heroin and morphine, and opioids (opiate-like drugs), such as hydromorphone (Dilaudid), hydrocodone, fentanyl, meperidine (Demerol), and codeine. These drugs produce a state of euphoria by removing painful feelings and creating a pleasurable experience and a sense of success accompanied by clouding of the consciousness and a dreamlike state. Physical signs of narcotic abuse include constricted pupils, respiratory depression, and, often, cyanosis. Needle marks may be visible on the arms or legs in chronic users. Physical withdrawal from opiates is extremely unpleasant unless controlled with supervised tapering doses of the opioid or substitution of methadone.
As important as the physical effects are the indirect consequences related to the illegal status of narcotic use and the problems associated with securing the drug (e.g., the time-consuming searches to obtain the drug and the often illegal methods used to meet the high cost of purchasing it). Health problems also result from self-neglect of physical needs (nutrition, cleanliness, dental care); overdose; contamination; and infection, including HIV and hepatitis B and C infection.
Central Nervous System Depressants.: Central nervous system depressants include a variety of hypnotic drugs that produce physical dependence and withdrawal symptoms on abrupt discontinuation. They create a feeling of relaxation and sleepiness but impair general functioning. Drugs in this category include barbiturates, nonbarbiturates, and alcohol. Barbiturates combined with alcohol produce a profound depressant effect. Flunitrazepam (Rohypnol), known as the “date rape drug,” is a recent hypnotic drug abused by adolescents. Many women and men report being raped after unknowingly being given Rohypnol in a drink. Rohypnol is 10 times more powerful than diazepam (Valium). It produces prolonged sedation, a feeling of well-being, and short-term memory loss.
Central Nervous System Stimulants.: Amphetamines and cocaine do not produce strong physical dependence and can be withdrawn without much danger. However, psychologic dependence is strong, and acute intoxication can lead to violent aggressive behavior or psychotic episodes characterized by paranoia, uncontrollable agitation, and restlessness. When combined with barbiturates, the euphoric effects are particularly addictive.
Methamphetamine can be snorted, injected, swallowed, or smoked and produces a burst of energy in its users, along with intense, alternating attacks of boldness and paranoia. It provokes excitement far more intense than that caused by cocaine. The drug, with the street names crank, meth, and crystal, is inexpensive and has a longer period of action than cocaine. Instead of a short (few minutes) high, as achieved with cocaine, a user can remain “up” for hours on a similar dose of crank.
Health care professionals are concerned about the use of various volatile substances, or inhalants such as gasoline, model airplane cement, and organic solvents; these substances are inhaled by the user to achieve an altered sensation, and the most recent surveillance has indicated a modest increase in use, after nearly a decade of decline. Adolescents breathe or place these substances into paper or plastic bags or soda cans from which they rebreathe the fumes to produce a feeling of euphoria and altered consciousness. These substances contain chemical solvents and are extremely hazardous. Dusters contain Freon, a substance that can cause fatal cardiac arrhythmias. The use of inhalants is increasing, and inhalants are becoming a gateway drug for young children and preteens, who often progress to other harder drugs such as marijuana, heroin, and cocaine. Many young children are unaware of the dangers of “sniffing” or “huffing.” In addition to rapid loss of consciousness and respiratory arrest, these substances may cause visual scanning problems, language deficiencies, motor instability, memory deficits, and attention and concentration problems.
Mind-Altering Drugs.: Hallucinogens (psychedelics, psychotomimetics, psychotropics, or illusionogenics) are drugs that produce vivid hallucinations and euphoria. These drugs do not produce physical dependence, and they can be abruptly withdrawn without ill effect. However, the acute and long-term effects are variable, and in some individuals the dissociative behavior may be prolonged. Cannabis (marijuana, hashish) and lysergic acid diethylamide (LSD) are also included in this category of drugs.
Nursing Care Management Related to Therapeutic Management
Nurses who have contact with children and adolescents are in an excellent position to provide information about substance abuse and to serve as patient advocates. The nurse most often encounters young drug abusers when they are (1) experiencing overdose or withdrawal symptoms, (2) manifesting bizarre behavior or confusion secondary to drug ingestion, (3) worried that they are or will become addicted, or (4) worried about a friend or family member who is addicted.
In particular, nurses who care for hospitalized adolescents need to know if these youths use drugs compulsively. Drug withdrawal can seriously complicate other illnesses. Nurses should be alert for any physical or behavioral clues that indicate the onset of withdrawal or the effects of drugs. School nurses and nurses who work in the community play an essential role in identifying children, adolescents, and families with substance abuse problems. The school nurse may be the first to identify a child or adolescent who has ingested a particular drug by the child’s erratic behavior in class or on the school grounds. Early identification of those at risk for substance abuse problems is an essential aspect of prevention. Pediatric health care professionals also prevent substance abuse by creating trusting relationships so that children and adolescents feel comfortable asking questions about drugs and health professionals can alert them to websites and other aspects of society that encourage experimentation with drugs.
Acute Care.: Adolescents experiencing toxic drug effects or withdrawal symptoms are usually seen initially in the emergency department. Experienced emergency department personnel are familiar with the management of acute drug toxicity and the signs, symptoms, and behavioral characteristics associated with a variety of substances. When the drug is questionable or unknown, knowledge of these factors facilitates management and treatment. Often, observation or description of the child’s or adolescent’s behavior is more valuable than reports by patients or their friends
The treatment for drug toxicity or withdrawal varies according to the drug and the method used. Every effort is made to determine the type, the time of ingestion, the amount of drug taken, the mode of administration, and the factors related to the onset of presenting symptoms. It is helpful to know the individual’s pattern of use. For example, if two types of drugs are involved, they may require different treatments. Gastric lavage may be employed when the drug has been ingested recently and the cough reflex is intact, but it is of little value when the drug has been administered by the intravenous (“mainlined”) or intranasal (“sniffed”) route. Because the actual content of most street drugs is highly questionable, other pharmaceutical agents are administered with caution, except perhaps the narcotic antagonists in cases of suspected opiate overdoses. It is also necessary to assess for possible trauma sustained while the patient was under the influence of the drug.
Long-Term Management.: A major factor in the treatment and rehabilitation of young drug users is careful assessment in the nonacute stage to determine the function that the drug plays in the adolescent’s life. The motivation phase is directed toward exploring the factors that influence drug use. It also involves establishing a feeling of self-worth and a commitment to self-help in the teen.
Rehabilitation begins when adolescents decide that they can and are willing to change. Rehabilitation involves fostering healthy interdependent relationships with caring and supportive adults and exploring alternate mechanisms for problem solving while simultaneously reducing or eliminating drug use. Persons working with troubled youth must be prepared for recidivism, or the tendency to relapse, and maintain a plan for reentry into the treatment process.
Family Support.: Most treatment programs for substance abusers are based on adult 12-step models such as Alcoholics Anonymous. Research is needed to determine whether these adult models are effective for adolescents. Tough Love* is one program that is based on the conviction that parents have the right and responsibility to be the policymakers in the family, to set limits on the behavior of their children, and to take control of the household from out-of-control adolescents. The premise is that allowing teenagers to experience the negative consequences of their behavior will bring them closer to accepting help or changing their behavior. Another group that provides support and counseling for families experiencing substance abuse and seeking strategies to cope with their children is Parents Anonymous.† Another source of information is the Substance Abuse and Mental Health Services Administration’s National Clearinghouse for Alcohol and Drug Information.‡
Prevention.: Nurses play an important role in education efforts, as well as in individual observation, assessment, and therapy related to substance abuse. In recent years a variety of educational programs have been applied with promising results. The most effective prevention strategies are those that are part of a broader, more general effort to promote overall health and success. Health-compromising behaviors are often interconnected and have common antecedents. Prevention efforts that focus on changing only one behavior (e.g., alcohol, other drug use) are less likely to be successful. Successful programs are those that have promoted parenting skills, social skills among distractible children, academic achievement, and skills to resist peer pressure.
Peer pressure is a powerful tool and can be used effectively in substance abuse prevention. A group that has had some success in reducing injury from drunk driving is Students Against Destructive Decisions (SADD).§ Techniques used by this group include peer counseling, parental guidelines for teenage parties, and community awareness. Nurses should encourage the formation of SADD chapters in the high schools in their communities.
SUICIDE
Suicide is defined as the deliberate act of self-injury with the intent that the injury results in death. Most experts distinguish between suicidal ideation, suicide attempt (or parasuicide), and suicide.
Suicidal ideation involves a preoccupation with thoughts about committing suicide and may be a precursor to suicide. Although it is not uncommon for adolescents to experience occasional suicidal thoughts, expressions of preoccupation with suicide should be taken seriously, and an assessment should be conducted for appropriate referral. A suicide attempt is intended to cause injury or death. The term parasuicide is used to refer to behaviors ranging from gestures to serious attempts to kill oneself. Parasuicide is a preferred term because it makes no reference to intent and because a person’s motive may be too difficult or complex to determine. However, all parasuicidal activity should be taken seriously.
Recent results from the Youth Risk Behavior Surveillance, 2005, indicated that 8.4% of students nationwide had attempted suicide at least once during the 12 months preceding the survey; the range of suicide attempts by adolescents across the states varied from 6.2% to 13.1% (Centers for Disease Control and Prevention, 2006b). The overall incidence of youth suicide has decreased since 1992, yet the Centers for Disease Control and Prevention notes the incidence is still too high. Approximately 13% of the students in this survey reported that they had made a specific plan to attempt suicide in the 12 months preceding the survey. Suicide is currently the third leading cause of death during the teenage years, surpassed only by death from motor vehicle crash and homicide (see Chapter 1).
Etiology
Individual, family, and social or environmental factors have all been implicated in suicide. The single most important individual factor is the presence of an active psychiatric disorder (depression, bipolar disorder, psychosis, substance abuse, or conduct disorder). Comorbidity of an affective disorder and substance abuse also increases the risk for suicide. Alcohol use has been associated with more than 50% of suicides (American Academy of Pediatrics, 2000). Gay and lesbian adolescents are at particularly high risk for suicide completion, especially if raised in an environment in which they are denied support systems (see Community Focus box). Family factors influencing suicide include parental loss; family disruption; a family history of suicide, depression, substance abuse, or emotional disturbance; child abuse or neglect; unavailable parents; poor communication and isolation within the family; family conflict; and unrealistically high parental expectations or parental indifference with low expectations. Social or environmental factors include incarceration, isolation, acute loss of a boyfriend or girlfriend, lack of future options, and availability of firearms in the home.
Methods
Firearms are by far the most commonly used instruments in completed suicides among males and females (American Academy of Pediatrics, 2000). For adolescent males, the second and third most common means of suicide are hanging and overdose, respectively; for females the second and third most common means are overdose and strangulation, respectively.
The most common method of suicide attempt is overdose or ingestion of a potentially toxic substance, such as drugs. The second most common method of suicide attempt is self-inflicted laceration.
Motivation
Suicidal ideation is not uncommon in adolescents. It represents numerous fantasies, such as relief from suffering, a means of gaining comfort and sympathy, or a means of revenge against those who have hurt them. Adolescents have the erroneous perception that the act of suicide will evoke remorse and pity and that they will be able to return and witness the grief. Angry children who are unable to directly punish those who have injured or insulted them may take revenge on those who love them through self-destruction (“They’ll be sorry when they find me dead”; “They’ll be sorry they were mean to me”).
For adolescents who are severely depressed, suicide seems to be the only release from their despair. These adolescents rarely provide evidence of their intent and frequently conceal their suicidal thoughts. Many adolescents, however, tell their peers of their suicidal thoughts or plans but avoid telling adults. Social isolation is a significant factor in distinguishing adolescents who will kill themselves from those who will not. It is also more characteristic of those who complete suicide than of those who make attempts or threats.
The frequency of contagion, or copycat suicides (i.e., an increase in youth suicide that occurs after the suicide of one teenager is publicized) is disturbing and may indicate that teenagers perceive suicide as glamorous. In addition, young people may not realize the finality of suicide because they have become desensitized from constantly viewing violence and death on television.
Diagnostic Evaluation
Depression is common among adolescents who attempt suicide. Depression is characterized by both subjective symptoms and objective signs that reflect the adolescent’s sadness and despair. Adolescents describe feelings of sadness, despair, helplessness, hopelessness, boredom, loss of interest, and isolation. They may also feel self-reproach, self-deprecation, and guilt. Subjective symptoms of depression or specific changes in behavior place an adolescent at risk for suicide.
Therapeutic Management
Threats of suicide should always be taken seriously. There has been a tendency to dismiss a suicide attempt as an impulsive act resulting from a temporary crisis or depression. If a suicide attempt fails to draw attention to their problems or makes them worse, the child or adolescent may conclude that suicide is the only answer. Children and adolescents need to know that someone cares and must be provided with swift and efficient crisis intervention. Although ordinary practitioners can manage an acute depressive reaction without difficulty, the adolescent who has made a serious attempt or has a specific plan for suicide should receive immediate attention and competent psychiatric care.
Nursing Care Management
Nurses play a pivotal role in reducing adolescent suicide. Nurses have the opportunity to provide anticipatory guidance to parents and adolescents. They can teach parents to be supportive and to develop positive communication patterns that help teens feel connected with and loved by their families. To foster healthy development, parents can be encouraged to provide teens with creative outlets and to assist young people in accepting strong emotions—pain, anger, and frustration—as a normal part of the human experience.
Care of the suicidal adolescent includes early recognition, management, and prevention. The most important aspect of management is the recognition of warning signs that indicate an adolescent is troubled and might attempt suicide. Health professionals must be alert to the signs of depression, and anyone who exhibits such behavior should be referred for thorough psychologic assessment. Depression is manifested differently in children and adolescents than in adults. In teens it may be masked by impulsive aggressive behaviors. Defiance, disobedience, behavior problems, and psychosomatic disturbances can indicate underlying depression, suicidal ideation, and impending suicide attempts.
Peers or other confidants are valuable observers and excellent sources of information about potential suicide attempts. They may not be able to diagnose depression, but they are able to sense when a friend has undergone a marked personality change. It is important to emphasize that the peer who detects any changes in a friend is a potential rescuer and should not remain silent about the observations. Friendship does not imply collusion. A peer who believes that a friend may be suicidal should alert someone who can help (e.g., a parent, teacher, guidance counselor, school nurse).
Routine health assessments of adolescents should include questions that assess the presence of suicidal ideation or intent. The following questions can be asked (Greydanus and Pratt, 1995):
 Do you consider yourself more a happy person, an unhappy person, or somewhere in the middle?
Do you consider yourself more a happy person, an unhappy person, or somewhere in the middle?
 Have you ever been so unhappy or upset that you felt like being dead?
Have you ever been so unhappy or upset that you felt like being dead?
 Have you ever thought about hurting yourself?
Have you ever thought about hurting yourself?
 Have you ever developed a plan to hurt yourself or kill yourself?
Have you ever developed a plan to hurt yourself or kill yourself?
If children or adolescents express suicidal intent, nurses make a contract, asking them to sign an agreement that they will not attempt suicide during an agreed-on period and that they will call the 24-hour crisis line immediately if they feel that they cannot keep to their contract. The amount of time an adolescent feels comfortable contracting is usually an indication of his or her risk and stability.
Because a suicide attempt is frequently an outgrowth of family distress, it is essential to intervene with the family. It is important to assess family interactions and to recognize disturbed relationships. The most effective approach is recognition of susceptible adolescents during the early stages of family distress so that family counseling can be started. Prevention must be directed toward improving childrearing practices through support and education of parents and changing societal conditions that generate defeat, despair, and maladaptive behavior.
Although confidentiality is an essential part of adolescent counseling, in the case of self-destructive behaviors confidentiality cannot be honored. Suicidal behavior is reported to the family and other professionals, and adolescents are informed that this will be done. Such action conveys an important message to the youth: that the professionals understand and care.
Many schools have instituted suicide prevention programs. These programs include services such as drop-in counseling and a peer-counseling telephone line. Information can also be obtained from the American Association of Suicidology.*
REFERENCES
Adelman, WP, Duggan, AK, Hauptman, P, et al. Effectiveness of a high school smoking cessation program. Pediatrics. 2001;107(4):e50.
America Academy of Pediatrics, Committee on Infectious Diseases. Red book: 2006 report of the Committee on Infectious Diseases, ed 27. Elk Grove Village, Ill: The Academy, 2006.
American Academy of Pediatrics, Committee on Adolescence. Adolescent pregnancy: current trends and issues. Pediatrics. 2005;116(1):281–286.
American Academy of Pediatrics, Subcommittee on Chronic Abdominal Pain. Chronic abdominal pain in children. Pediatrics. 2005;115(3):812–815.
American Academy of Pediatrics. Tobacco, alcohol, and other drugs: the role of the pediatrician in prevention, maintenance, and identification of substance abuse. Pediatrics. 2005;115(3):816–821.
American Academy of Pediatrics, Committee on Adolescence. Identifying and treating eating disorders. Pediatrics. 2003;111(1):204–211.
American Academy of Pediatrics, Committee on Adolescence. Care of the adolescent sexual assault victim. Pediatrics. 2001;107(6):1476–1479.
American Academy of Pediatrics, Committee on Public Education. Children, adolescents, and television. Pediatrics. 2001;107(2):423–426.
American Academy of Pediatrics. Treatment of the school-aged child with attention-deficit/hyperactivity disorder. Pediatrics. 2001;108(4):1033–1044.
American Academy of Pediatrics, Committee on Adolescence. Suicide and suicide attempts in adolescents. Pediatrics. 2000;105(4):871–874.
American Academy of Pediatrics, American College of Obstetricians and Gynecologists. Menstruation in girls and adolescents: using the menstrual cycle as a vital sign. Pediatrics. 2006;118(5):2245–2250.
American Dietetic Association. Position of the American Dietetic Association: Nutrition intervention in the treatment of anorexia nervosa, bulimia nervosa, and other eating disorders. J Am Diet Assoc. 2006;106(12):2073–2082.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders, ed 4 (text rev) (DSM-IV TR). Washington, DC: The Association, 2000.
Anderson, JE, Santelli, JS, Morrow, B. Trends in adolescent contraceptive use, unprotected and poorly protected sex, 1991-2003. J Adolesc Health. 2006;38(6):734–739.
Angulo, P. Nonalcoholic fatty liver disease. N Engl J Med. 2002;346(16):1221–1231.
Baker, S, Barlow, S, Cochran, W, et al. Overweight children and adolescents: a clinical report of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2005;40:533–543.
Berkowitz, RI, Fujioka, K, Daniels, SR, et al. Effects of sibutramine treatment in obese adolescents. Ann Intern Med. 2006;145(2):81–90.
Berry, AK. Helping children with nocturnal enuresis: the wait-and-see approach may not be in everyone’s interest. Am J Nurs. 2006;106(8):56–63.
Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2006. MMWR. 2006;55(RR-11):1–94.
Centers for Disease Control and Prevention. Youth risk behavior surveillance—United States, 2005. MMWR. 2006;55(SS-5):1–64.
Centers for Disease Control and Prevention. Youth tobacco surveillance—United States, 2001-2002. MMWR. 2006;55(SS03):1–56.
Clements, PT, Speck, PM, Crane, PA, et al. Issues and dynamics of sexually assaulted adolescents and their families. Int J Mental Health Neurosurg. 2004;13:267–274.
Coughlin, EC. Assessment and management of pediatric constipation in primary care. Pediatr Nurs. 2003;29(4):296–301.
Dennehy, CE. The use of herbs and dietary supplements in gynecology: an evidence-based review. J Midwifery Womens Health. 2006;51(6):402–409.
Ehtisham, S, Barrett, TG, Shaw, NJ. Type 2 diabetes mellitus in UK children—an emerging problem. Diabetes Med. 2000;17(12):867–871.
Feldman, M, Friedman, LS, Sleisenger, MH. Obesity: a historical perspective and disease prevalence estimates. In Feldman M, Friedman LS, Sleisenger MH, eds.: Sleisenger and Fordtran’s gastrointestinal and liver disease, ed 7, Philadelphia: Saunders, 2002.
Forman, SF. Eating disorders: epidemiology, pathogenesis, and clinical features, UpToDate. http://www.uptodate.com, 2007. [retrieved July 31, 2007, from].
Gibbons, RD, Hur, K, Bhaumik, DK, et al. The relationship between antidepressant prescription rates and rate of early adolescent suicide. Am J Psychiatry. 2006;163(11):1898–1904.
Goodman, E, Capitman, J. Depressive symptoms and cigarette smoking among teens. Pediatrics. 2000;106(4):748–755.
Gordon, SM. Adolescent drug use: trends in abuse, treatment and prevention. Wernersville, Penn: Caron Foundation, 2000.
Greaser, J, Whyte, JJ. Childhood obesity: is there effective treatment? Consult Pediatr. 2004;4(10):474–478.
Greydanus, DE, Pratt, HD. Emotional and behavioral disorders of adolescence, part 2. Adolesc Health Update. 1995;8(1):1–8.
Hamilton, BE, Martin, JA, Ventura, SJ. Births: preliminary data for 2005. Natl Vital Stat Rep. 2006;55(11):1–18.
Hardy, LR, Harrell, JS, Bell, RA. Overweight in children: definitions, measurements, confounding factors, and health consequences. J Pediatr Nurs. 2004;19(6):376–383.
Hedley, AA, Ogden, CL, Johnson, CL, et al. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999-2002. JAMA. 2004;291(3):2847–2850.
Hill, JO, Wyatt, HR, Reed, GW, et al. Obesity and the environment: where do we go from here? Science. 2003;299(5608):853–855.
Jick, H, Kaye, JA, Jick, SS. Antidepressants and the risk of suicidal behaviors. JAMA. 2004;292(3):338–343.
Johnston, LD, O’Malley, PM, Bachman, JG, et al. Monitoring the future national results on adolescent drug use: overview of key findings, 2004. Bethesda, Md: National Institute on Drug Abuse, 2005. NIH Pub No 05-5726
Kandakai, TL, Smith, LC. Denormalizing a historical problem: teen pregnancy, policy and public health action. Am J Health Behav. 2007;31(2):170–180.
Kiess, W, Galler, A, Reich, A, et al. Clinical aspects of obesity in childhood and adolescence. Obesity Rev. 2001;1:29–36.
Koeppen-Schomerus, G, Wardle, J, Plomin, R. A genetic analysis of weight and overweight in 4-year-old twin pairs. Int J Obes Relat Metab Dis. 2001;25(6):838–844.
Lord, J, Winell, JJ. Overuse injuries in pediatric athletes. Curr Opin Pediatr. 2004;16(1):47–50.
MacKenzie, NR. Childhood obesity: strategies for prevention. Pediatr Nurs. 2000;26(5):527–530.
Master-Hunter, T, Heiman, DL. Amenorrhea: evaluation and treatment. Am Fam Physician. 2006;73(8):1374–1382.
Mehler, PS. Diagnosis and care of patients with anorexia nervosa in primary care settings. Ann Intern Med. 2001;134:1048–1059.
Michelson, D, Faries, D, Wernicke, J, et al. Atomoxetine in the treatment of children and adolescents with attention-deficit/hyperactivity disorder: a randomized, placebo-controlled, dose-response study. Pediatrics. 2001;108:E83.
Moran, R. Breaking the cycle of childhood obesity. Clin Advisor. 2003;6(2):62–67.
Mosher, WD, Chandra, A, Jones, J. Sexual behavior and selected health measures: men and women 15-44 years of age, United States, 2002. Adv Data, Sep. 2005;15(362):1–55.
Myers, SM, Eisenhauer, NJ, Ryan, ME. ADHD: it is real, and it can be treated. Clin Advisor. 2003;6(3):15–25.
National Institute for Health Care Management Foundation. Childhood obesity: advancing effective prevention and treatment: an overview for health professionals. Washington, DC: prepared for National Institute for Health Care Management Foundation Forum, 2003.
Neinstein, LS. Adolescent health care: a practical guide, ed 4. Philadelphia: Lippincott Williams & Wilkins, 2002.
Patel, M, Minshall, L. Management of sexual assault. Emerg Clin North Am. 2001;19(3):817–831.
Patten, CA, Choi, WS, Gillin, JC, et al. Depressive symptoms and cigarette smoking predict development and persistence of sleep problems in US adolescents. Pediatrics. 2000;106(2):E23.
Rideout, VJ, Foehr, UG, Roberts, DF, et al. Kids and media @ new millennium. New York: Kaiser Family Foundation, 1999.
Rimsza, ME, Kirk, GM. Common medical problems of the college student. Pediatr Clin North Am. 2005;52(1):9–24. [vii,].
Robinson, TN. Television viewing and childhood obesity. Pediatr Clin North Am. 2001;48:1017–1025.
Rome, ES, Ammerman, S, Rosen, DS, et al. Children and adolescents with eating disorders: the state of the art. Pediatrics. 2003;111(1):e98–e108.
Schwartz, RH, Milteer, R, LeBeau, MA. Drug facilitated sexual assault (“date rape”). South Med J. 2000;93(6):558–561.
Schwimmer, JB. Managing overweight in older children and adolescents. Pediatr Ann. 2004;33(1):39–44.
Selekman, J, Snyder, M. Learning disabilities and/or attention deficit disorder. In Jackson P, Vessey JA, eds.: Primary care of children with chronic conditions, ed 3, St Louis: Mosby, 2000.
Sethi, S, Bhargava, S, Shipra, PM. Nocturnal enuresis: a review. J Pediatr Neurol. 2005;3(1):11–18.
Shrier, LA. Sexually transmitted diseases in adolescents: biologic, cognitive, psychologic, behavioral, and social issues. Adolesc Med Clin. 2004;15(2):215–234.
Shulman, ST. The overweight epidemic. Pediatr Ann. 2004;33(1):6.
Sjöberg, RL, Nilsson, KW, Leppert, J. Obesity, shame, and depression in school-aged children: a population-based study. Pediatrics. 2005;116(3):e389–e393.
Sondike, S, Copperman, N, Jacobson, MS. Effects of a low-carbohydrate diet on weight loss and cardiovascular risk factors in overweight adolescents. J Pediatr. 2003;142(3):253–258.
Spencer, TJ, Wilens, TE, Biederman, J, et al. Efficacy and safety of mixed amphetamine salts extended release (Adderall XR) in the management of attention-deficit hyperactivity disorder in adolescent patients: a 4-week, randomized, double-blind, placebo-controlled, parallel-group study. Clin Ther. 2006;28(2):266–279.
Sugerman, HJ, Sugerman, EL, DeMaria, EJ, et al. Bariatric surgery for severely obese adolescents. J Gastrointest Surg. 2003;7(1):102–107.
Sundelin-Wahlsten, V, Ahmad, A, von Knorring, A-L. Traumatic experiences and post-traumatic stress reactions in children from Kurdistan and Sweden. Acta Paediatr. 2001;90:563–568.
Taylor, ED, Theim, KR, Mirch, MC, et al. Orthopedic complications of overweight in children and adolescents. Pediatrics. 2006;117(6):2167–2173.
Tsai, WS, Inge, TH, Burd, RS. Bariatric surgery in adolescents: recent national trends in use and in-hospital outcomes. Arch Pediatr Adolesc Med. 2007;161(3):217–221.
US Department of Health and Human Services. The health consequences of involuntary exposure to tobacco smoke: a report of the surgeon general. Washington, DC: US Department of Health and Human Services, 2006.
US Food and Drug Administration. Antidepressant use in children, adolescents, and adults. http://www.fda.gov/cder/drug/antidepressants/default.htm, 2004. [(updated July 12, 2005), retrieved Jan 22, 2008, from].
Weiss, R, Dziura, J, Burgert, TS, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004;350(23):2362–2374.
Yanovski, SZ, Yanovski, JA. Obesity. N Engl J Med. 2002;346(8):591–602.
*http://www.cdc.gov/std/treatment.
*For information about local organizations, contact National Organization for Victim Assistance, Courthouse Square, 510 King St., Suite 424, Alexandria, VA 22314; (800) 879-6682 or (703) 535-6682; e-mail: NOVA@trynova.org; http://www.trynova.org.
*http://www.cdc.gov/growthcharts.
*http://www.mypyramid.gov/kids/index.html.
†http://www.health.gov/dietaryguidelines/dga2005/document/default.htm.
*PO Box 7, Highland Park, IL 60035; (847) 831-3438; e-mail: info@anad.org; http://www.anad.org.
†603 Stewart St., Suite 803, Seattle, WA 98101; (800) 931-2237; http://www.nationaleatingdisorders.org.
†675 W. Foothill Blvd., Suite 220, Claremont, CA 91711; (909) 621-6184; http://www.parentsanonymous.org.
‡PO Box 2345, Rockville, MD 20847; (800) 729-6686; e-mail: info@health.org; http://ncadi.samhsa.gov.
§255 Main St., Marlborough, MA 01752; (877) SADD-INC; http://www.sadd.org.
*5221 Wisconsin Ave. NW, Washington, DC 20015; (202) 237-2280; http://www.suicidology.org.
 IN TEXT
IN TEXT FAMILY FOCUS
FAMILY FOCUS
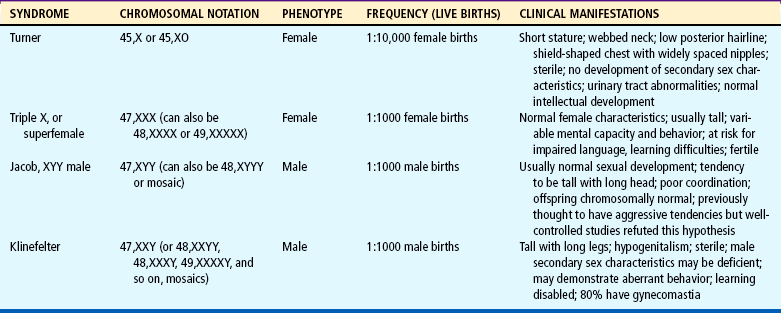
 CRITICAL THINKING EXERCISE
CRITICAL THINKING EXERCISE
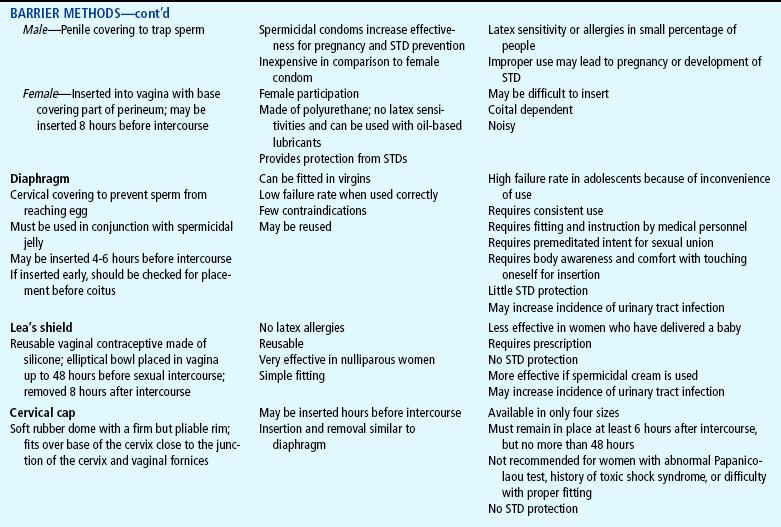
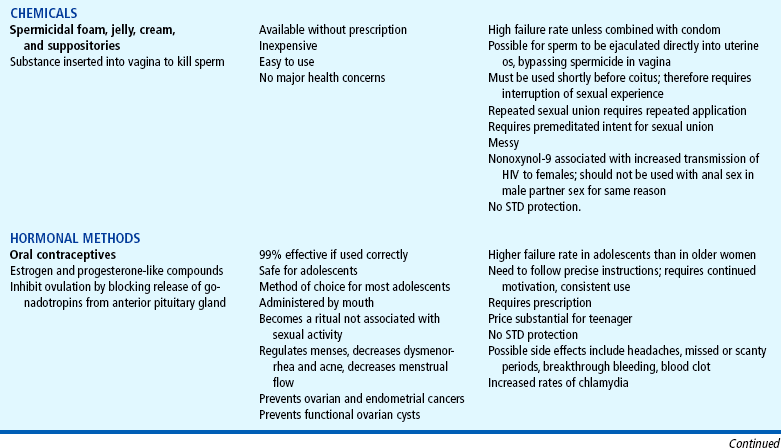
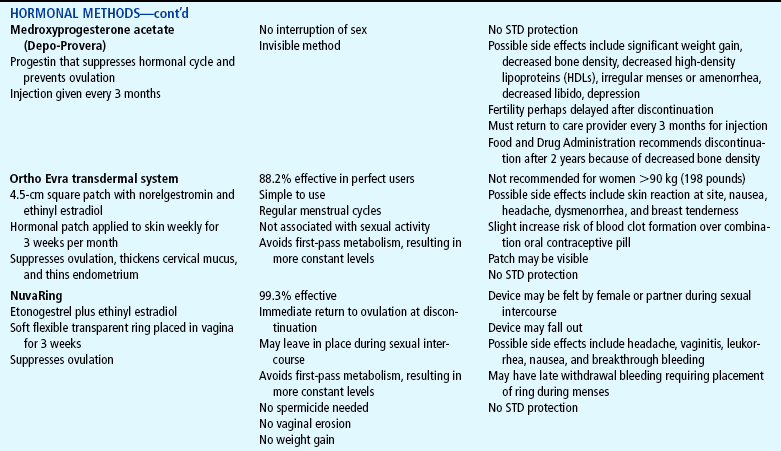
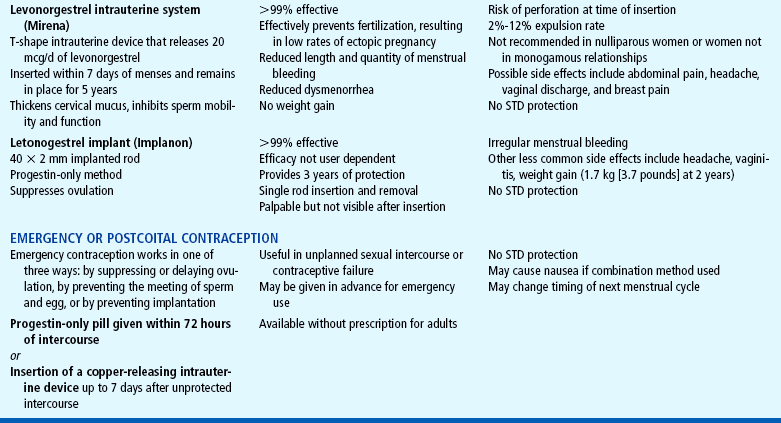
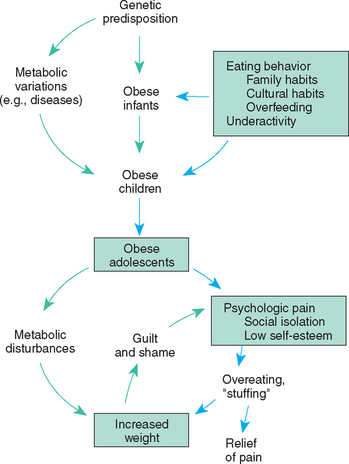
 COMMUNITY FOCUS
COMMUNITY FOCUS