Chronic Illness, Disability, or End-of-Life Care for the Child and Family
PERSPECTIVES ON THE CARE OF CHILDREN WITH SPECIAL NEEDS
THE FAMILY OF THE CHILD WITH SPECIAL NEEDS
Impact of the Child’s Chronic Illness or Disability
Coping with Ongoing Stress and Periodic Crises
NURSING CARE OF THE FAMILY AND CHILD WITH SPECIAL NEEDS
Provide Support at the Time of Diagnosis
Support Family’s Coping Methods
PERSPECTIVES ON THE CARE OF CHILDREN AT THE END OF LIFE
On completion of this chapter the reader will be able to:
 Identify the scope of and changing trends in care of children with special needs.
Identify the scope of and changing trends in care of children with special needs.
 Identify the major reactions of and effects on the family of a child with a special need.
Identify the major reactions of and effects on the family of a child with a special need.
 Define the stages of adjustment to the diagnosis of a chronic condition.
Define the stages of adjustment to the diagnosis of a chronic condition.
 Recognize the impact of the illness or disability on the developmental stages of childhood.
Recognize the impact of the illness or disability on the developmental stages of childhood.
 Outline nursing interventions that promote the family’s optimal adjustment to the child’s chronic disorder.
Outline nursing interventions that promote the family’s optimal adjustment to the child’s chronic disorder.
 Outline nursing interventions that support the family at the time of death.
Outline nursing interventions that support the family at the time of death.
PERSPECTIVES ON THE CARE OF CHILDREN WITH SPECIAL NEEDS
A number of terms and defining characteristics have been used to describe chronic illness and disability in children (Box 18-1). In recent years there have been continuing efforts to develop a definition that better identifies the numbers of children living with chronic conditions, as well as the impact on health and social services (Jackson, 2000; van Dyck, Kogan, Heppel, and others, 2004). Currently children with special health care needs are defined as children who have or are at increased risk for a chronic physical, developmental, behavioral, or emotional condition and who also require health and related services of a type or amount beyond that generally required by children (Msall, Avery, Tremont, and others, 2003; Newacheck, Strickland, Shonkoff, and others, 1998).
Ongoing progress in medical and technologic disease management has contributed to the growing number of children with special health care needs (Palfrey, Tonniges, Green, and others, 2005). The number of U.S. children with acquired immunodeficiency syndrome (AIDS) diagnosed each year declined by 75% from 1992 to 2000 (Yogev and Chadwick, 2004). Technologic advances have substantially increased the survival of extremely low– and very low–birth-weight infants (Jackson, 2000). Children with disabilities are more likely to be in poor health than children without disabilities (Newacheck and Halfon, 1998). The result of such progress is that an estimated 15% to 18% of the children in the United States live with a chronic illness or disability and require specialized health care of a type or amount beyond that generally required by children (Perrin, 2004).
The most commonly occurring conditions causing disability are diseases of the respiratory tract and impairments of speech, special senses, and intelligence. Mental and nervous system disorders account for about one sixth of all childhood disability (Newacheck and Halfon, 1998).
The impact of chronic illness and disability in children is wide ranging. Chronic conditions in children present most families with additional tasks, responsibilities, and concerns (Ray, 2002). A child’s activity level and developmental opportunities can be affected. Days can be lost from school. Children with chronic illness or disability may be at increased risk for behavior or emotional problems. Parents may lose days from work, experience financial strain, and be challenged both emotionally and physically as they cope with care of the child.
Siblings are also affected by having a “different” brother or sister and may simultaneously feel guilt and anger or jealousy toward their ill sibling. Additionally, secondary losses such as the ability to participate in extracurricular activities or social events occur because of routines imposed by the affected child’s chronic condition.
TRENDS IN CARE
Focusing on the child’s developmental level rather than chronologic age or diagnosis emphasizes the child’s abilities and strengths rather than disabilities. Attention is directed to normalizing experiences, adapting the environment, and promoting coping skills. Nurses often are in vital positions to redirect attention from the pathologic model with its focus on weaknesses and problems to the developmental model to meet the unique needs of the child and family.
A developmental focus also considers family development. The life cycle of the family unit reflects changing ages and needs of family members, as well as changing external demands. A family member’s serious illness or disability can cause significant stress or crisis at any stage of the family life cycle. Just as with individual development, family development may be interrupted or even regress to an earlier level of functioning. Nurses can use the concept of family development to plan meaningful interventions and evaluate care (see Developmental Theory, Chapter 3).
Family-Centered Care
Children’s physical and emotional health, as well as cognitive and social functioning, is strongly influenced by how well their families function (Schor, 2003). The importance of family-centered care—a philosophy that considers the family as the constant in the child’s life—is especially evident in the care of children with special needs (see also Family-Centered Care, Chapter 1). As parents learn about the youngster’s health care needs, they often become experts in delivering care. Health care providers, including nurses, are adjuncts to the child’s care and need to form partnerships with parents. Effective communication and negotiation between parents and nurses are essential to forming trusting and effective partnerships and finding the best ways to meet the needs of the child and family (Corlett and Twycross, 2006). Collaborative relationships are characterized by communication, dialogue, active listening, awareness, and acceptance of differences (Schor, 2003).
Family–Health Care Provider Communication
The disclosure of a serious acute or chronic illness of a child is one of the most stressful aspects of communication between families and health care professionals. Often, parents have suspected for some time that something is wrong with their child and believe that their concerns were minimized or ignored by health care professionals (Whitehead and Gosling, 2003; Thomlinson, 2002; Cohen, 1995). After a diagnosis is made, numerous studies have shown that parents are not always satisfied with the way in which information is given. Factors that influence parent dissatisfaction with communication include unsympathetic and brief diagnostic interviews, lack of privacy during diagnostic discussions, and lack of opportunity to ask questions. Conversely, parents report satisfaction when they perceive the health care providers giving information in an open and honest manner with respect for the parents’ need for privacy and time to express emotions and ask questions (Davies, Davis, and Seibert, 2003). Similar factors are important in communication of changes in the child’s condition throughout the course of the illness.
Providing information to families with a chronically ill child should be a process of repeated discussions to allow the family to process the information and their reactions to that information, and allow them to ask for clarification and further information. Nurses play an important role in ensuring that families’ needs are met during discussions related to the child’s diagnosis, condition, and treatment. This requires assessment regarding how much information the family is comfortable with, what they understand of the information already given to them, and how they are coping with the information both cognitively and emotionally. Nurses should ensure that the appropriate health care professionals address any concerns or further questions that families may have.
Establishing Therapeutic Relationships
Another important aspect of family-centered care of chronically ill children is establishing a therapeutic relationship with the child and family, which has been shown to predict improved health-related outcomes (Denboba, McPherson, Kenney, and others, 2006). Families, most often the mother, take on enormous responsibility in providing technical care and symptom management of their child’s condition outside the health care institution (O’Brien and Wegner, 2002; Raina, O’Donnell, Rosenbaum, and others, 2005; Swallow and Jacoby, 2001). To build successful therapeutic relationships with families, it is necessary for nurses to recognize parents’ expertise with regard to their child’s condition and needs. Care conferences, especially multidisciplinary meetings that include the family and key health professionals, provide an opportunity for sharing ideas and expressing feelings or concerns.
Individual discussions, especially with the case manager, primary nurse, clinical nurse specialist, or nurse practitioner, help establish a consistent and flexible care plan that can prevent conflicts or deal with these conflicts before they disrupt care. In family-centered care, the goal is to maintain the integrity of the leadership role and support the family during times of crisis or stress.
The Role of Culture in Family-Centered Care
Issues of culture, ethnicity, and race affect access to services, utilization, and follow-through with referrals and recommendations (van Dyck, Kogan, McPherson, and others, 2004; Wise, Wampler, Chavkin, and others, 2002; Wood, Smith, Romero, and others, 2002; Zuvekas and Taliaferro, 2003). For some ethnic and minority populations, cultural understandings of illness and disability, the structure of family life, social roles for individuals who are disabled, and other factors related to the perception of children may differ from those of mainstream American culture. These factors may affect family needs and family choices regarding the care of their child with special needs.
Although culture cannot completely explain how an individual will think and act, understanding cultural perspectives can help the nurse anticipate and understand why families may make certain decisions. Cultural attributes such as values and beliefs regarding illness or disability and its causation, social roles for the ill or disabled, family structure, the role of children, childrearing practices, self vs group orientation, spirituality, and time orientation also affect a family’s response to illness or disability in a child (Carnevale, Alexander, Davis, and others, 2006; Carter, 2002; Marshall, Olsen, Mandleco, and others, 2003; Rehm, 1999; Sterling and Peterson, 2003).
When parents are informed of their child’s chronic illness, interpreters familiar with both culture and language should be used. Children, family members, and friends of the family should not be used as translators because their presence may prevent parents from openly discussing the issues. When working with people of cultural backgrounds different from their own, nurses must listen carefully with an initial goal of understanding and articulating the family’s perspective. The ability to interpret the mainstream medical culture to the family is also important. Furthermore, every effort is made to incorporate traditional cultural beliefs of a family into treatment plans. Developing a care plan in conjunction with the family, considering their preferences and priorities, is an important first step in formulating a plan that best meets the family’s needs, no matter what their cultural background (Ahmann, 1994; Ochieng, 2003).
Shared Decision Making
Shared decision making among the child, family, and health care team can result from open, honest, culturally sensitive communication and the establishment of a therapeutic relationship between the family and health care providers. In a shared decision-making model the health care professionals provide honest, clear information regarding diagnosis, prognosis, treatment options, and risk/benefit assessment. The patient and/or family then shares information with the health care team regarding important family values, acceptable levels of discomfort or inconvenience, and the ability to comply with treatments being recommended (Charles, Gafni, and Whelan, 1997). This process allows them to discuss all options in terms of the risks and benefits to the child and family, the prognosis or expected course of the illness, and the impact on the family’s resources (Box 18-2).
Normalization
Normalization refers to behaviors and intentions of the disabled to integrate into society by living life as persons without a disability would (Morse, Wilson, and Penrod, 2000). For the chronically ill or disabled child, such behaviors could include attending school, pursuing hobbies and recreational interests, and achieving employment and a level of independence. For their families, it may entail adapting the family routine to accommodate the ill or disabled child’s health and physical needs (McDougal, 2002).
Children with chronic illness and disability and their families face numerous challenges in achieving normalization. Families move between the “normal” of living with the experience of chronic childhood illness and the “normal” of the healthy outside world; they often redefine “normal” based on their particular experiences, needs, and circumstances (Nelson, 2002; Deatrick, Knafl, and Murphy-Moore, 1999).
Nurses can assist families in normalizing their lives by assessing the family’s everyday life, social support systems, coping strategies, family cohesiveness, and family and community resources. Interventions could include encouraging families to reduce stress through delegation of care and family tasks, identifying ways to incorporate care into current routines, structuring the home environment to encourage the child’s engagement in age-appropriate activities, and ensuring families have access to appropriate community support services (Jokinen, 2004; Shepard and Mahon, 2000). Being supportive of the child’s illness and treatment and actively including the family in all aspects of care will improve their self-esteem and promote further development (Shepard and Mahon, 2000).
Home care represents the return to a system and set of priorities in which family values are as important in the care of a child with a chronic health problem as they are in the care of other children. Home care seeks to achieve goals that are consistent with the developmental model (Stein, 1985):
With appropriate training and support, families provide complex procedures and treatments in the home. Parents are challenged to retain a homelike setting among monitors, ventilators, and other sophisticated equipment. Throughout the text, home care is discussed as appropriate for specific conditions. The process of transition from hospital to home is elaborated on in Chapters 20 and 21.
Paralleling normalization and home care is the process of mainstreaming, or integrating children with special needs into regular classrooms. Just as the home is the natural environment for children, so school must also be included as an essential component of the children’s overall physical, intellectual, and social development. Children who attend school have the advantages of learning and socializing with a wide group of peers. There is an increased focus on individualization as plans are made to meet the academic needs of these children along with those of the rest of the students.
A variety of supplemental programs have been designed in the school system to accommodate special needs, both at school age and younger, through early intervention, which consists of any sustained and systematic effort to assist children from birth to age 3 years who are disabled and developmentally vulnerable. This change and increasing opportunities for normalization for children with special needs in large part have resulted from the passage of (1) the Education for All Handicapped Children Act of 1975 (Public Law 94-142) and its 1990 amendments (Public Law 101-476), which changed the name of the act to the Individuals with Disabilities Education Act (IDEA); (2) the Education of the Handicapped Act Amendments of 1986 (Public Law 99-457), which directs states to develop and implement statewide comprehensive, coordinated, multidisciplinary interagency programs of early intervention services for infants and toddlers with disabilities, as well as support services for their families; and (4) the Americans with Disabilities Act of 1990. Nurses can provide parents with information about these laws and in some cases may participate in the development of individualized educational programs (IEPs) or individualized family service plans (IFSPs) for children with special needs.
Managed Care
Managed care programs have become the major form of health care provision in the United States (Jackson, 2000). The transition to this model of care presents both opportunities and challenges with respect to the care of children with special health care needs. Managed care may promote continuity and coordination of care. Children rely on adults for access to health care and follow-up with treatment regimens, making it necessary to manage the child’s care in the context of the family (McPherson, Weissman, Strickland, and others, 2004; van Dyck, Kogan, McPherson, and others, 2004).
THE FAMILY OF THE CHILD WITH SPECIAL NEEDS
A major goal in working with the family of a child with special needs is to support the family’s coping and promote their optimal functioning throughout the child’s life. Long-term, comprehensive, family-centered approaches extend beyond supporting the child and family during the critical periods of diagnosis and hospitalization. Rather, comprehensive care involves forming parent-professional partnerships that can support a family’s adaptation to the many changes that may be necessary in day-to-day life, determine expectations of and for the child, and provide a long-term perspective (Box 18-3).
The impact of a child’s medical or developmental condition is often experienced over time, initially as a crisis at the time of diagnosis, which may occur at birth, after a long period of physical or psychologic testing, or immediately after a tragic injury. The impact may also be felt before the diagnosis is made, when parents are aware that something is wrong with their child but before medical confirmation (Whitehead and Gosling, 2003; Thomlinson, 2002; Cohen, 1995).
The diagnosis and initial discharge home are critical times for parents (Coffey, 2006). Several factors can make it particularly difficult, including a long duration of uncertainty in the diagnostic process, negative perceptions of chronic illness or disability, insufficient information, and lack of mutual trust between parents and their child’s health care team (Cohen, 1995; Garwick, Patterson, Bennett, and others, 1995; Nuutila and Salanterä, 2006). Parental feelings of shock, helplessness, isolation, fear, and depression are common (Coffey, 2006; Nuutila and Salanterä, 2006). Throughout the first year, parents struggle to accept the child’s diagnosis, care, and uncertainty of the future (Coffey, 2006). Providing explicit and uncomplicated information to parents in an empathic way (Nuutila and Salanterä, 2006); assessing the family’s daily routine, living conditions, background knowledge, skills and abilities, and coping behaviors; and evaluating the family’s understanding of the information can encourage optimal support at the time of diagnosis and initial discharge home. It is also necessary to reassess parental needs for information and support on a routine basis (Nuutila and Salanterä, 2006).
Other critical times include the exacerbation of the child’s physical symptoms, which increases parental care; significant milestones for the child and his or her peers, particularly toddlerhood, entering kindergarten, and turning 18 years old, which increases parental stress; and advocating for the child during these times. Supporting parents, respecting their stress and emotions, and acknowledging their role as team members in the care of their child are important aspects of nursing care (Coffey, 2006; Nuutila and Salanterä, 2006).
IMPACT OF THE CHILD’s CHRONIC ILLNESS OR DISABILITY
Each member of a family who has a child with special needs is affected by the experience (Sullivan-Bolyai, Sadler, Knafl, and others, 2003). The effects on the parents and their responses are so critical that they directly influence the other members’ reactions and the child’s own coping.
Parents
In addition to the stress of grieving for the loss of a perfect child, parents are affected by whether or not they receive positive feedback from transactions with their child. Many parents feel satisfaction and fulfillment from the parenting role. For others, parenting may be a series of unrewarding experiences that contribute to feelings of inadequacy and failure (Box 18-4). These responses may be most evident in parents who are responsible for the child’s care. For example, parents may become preoccupied with their ability to carry out certain procedures, overlooking the child’s personal comfort and satisfaction or failing to offer praise for anything less than perfect cooperation or performance. They may pursue a frustrating activity until they achieve “success”–long after the child has become irritable and uncooperative. As a result, parents can become caught in a pattern of interaction that is mutually unrewarding and minimally productive. For these parents, several strategies may be helpful: education regarding what can reasonably be expected of their child, assistance in identifying the child’s strengths, praise for a parental job well done, and respite care so that parents can renew their energies.
Parental Roles.: Parenting a child with a chronic illness or disability requires much more than raising a typical child. In addition to attending to the routine aspects of parenting, parents of chronically ill children take on the added responsibility of performing complex technical care and symptom management, advocating for their child, and seeking and coordinating health and social services for their ill or disabled child. These added responsibilities must then be balanced with the needs of other family members, extended family and friends, and personal health and obligations to minimize consequences to the overall functioning of the family (Coffey, 2006; Ray, 2002).
Enormous demands may be placed on parental time, energy, and financial resources.
Often one partner remains at home to manage existing family responsibilities while the other remains with the ill child. The partner who is not included in the caregiving activities may feel neglected because all of the attention is directed toward the child and resentful that he or she is not sufficiently informed to be competent in the care. Without active participation in the child’s care, the parent has little appreciation of the time and energy involved in performing those activities. When this partner does attempt to participate, the other parent may criticize the less skillful efforts. As a result, communication and support for each other may be adversely affected.
The nurse can assist parents in avoiding role conflicts by providing anticipatory guidance early on. Teaching should address stressors often identified as having an impact on the marriage: (1) the burden of care at home assumed by primarily one parent, (2) the financial burden, (3) the fear of the child dying, (4) pressure from relatives, (5) the hereditary nature of the disease (if applicable), and (6) fear of pregnancy. Other causes of tension may center on the inconveniences associated with care, such as long waits for an appointment, lack of parking near care facilities, or lack of overnight accommodations. Certainly, these last stressors are within health professionals’ domain to minimize, if not eliminate.
Mother-Father Differences.: Mothers and fathers in the same family often adjust and cope differently as parents of a child with special needs. Some mothers experience a peaks-and-valleys periodic crisis pattern, whereas most fathers tend to experience a steady, gradual recovery. Some research suggests that mothers of children with certain conditions may be more susceptible to psychologic distress and fatigue than fathers (Tong, Kandala, Haig, and others, 2002). Mothers are most often the primary caregiver and are more likely than fathers to give up their job to care for their child, often resulting in social isolation (Coffey, 2006). Mothers often have greater needs for social support and positive appraisal of the situation, whereas fathers are more likely to use self-controlling behaviors to cope (Goldbeck, 2001; Mastroyannopoulou, Stallard, Lewis, and others, 1997).
The father of a child with special needs struggles with issues that may be distinct from those of the mother. He may think that his role of protector is challenged because he does not know how to help and cannot protect the family from the seemingly overwhelming recurring problems. With today’s increased emphasis on fathers’ involvement in the lives of their children, this loss is felt more profoundly than in the past. The extensive stresses in the family can leave the father feeling depressed, weak, guilty, powerless, isolated, embarrassed, and angry. Fearful that he will lose control or be viewed as weak or ineffectual, however, the father often hides his feelings and displays an outward confidence that may lead others to believe that everything is fine. Fathers worry about what the future holds for their children, their ability to manage the increasing financial burden, and the daily disruptions of the entire family (Davies, Gudmundsdottir, Worden, and others, 2004). Some fathers escape in their work as a means of dulling the pain. Common coping strategies are problem oriented and include praying, getting information, looking at options, and weighing choices, in addition to withdrawal (Mastroyannopoulou, Stallard, Lewis, and others, 1997).
Single-Parent Families.: Single-parent families are of special concern. The absence of a parent may result from divorce or death, or the parents may never have married. As the only parent of a child who may require extensive, sophisticated, and lifelong care, the single parent may feel an enormous burden. Available financial and emotional resources may already be stretched to the limit. A special effort should be made to assist the single parent in finding financial and support services that can ease the burden of care. Nurses can also assist the single parent in identifying helping roles that may be acceptable to relatives and friends.
Siblings
Results of studies on how siblings, almost exclusively European Americans, are affected by having a brother or sister with special needs are unclear (Barlow and Ellard, 2006). Generally, there is evidence that there is a negative effect on siblings of children with a chronic illness when compared with siblings of healthy children. This effect appears, however, to be decreasing in significance in recent years—most likely because of changes in public attitudes toward the ill and disabled (Sharpe and Rossiter, 2002). Siblings of children with chronic illness or disability report depression and anxiety more often than their peers (Rossiter and Sharpe, 2001). However, most investigators do agree that brothers and sisters of children with special needs are no more at risk for severe psychiatric problems than are siblings of children without chronic or disabling conditions. A number of factors increase the risk of negative effects for siblings of ill children. Responsibility for caregiving, differential treatment by parents, and limitations in family resources and recreational time are often the experience of siblings of ill or disabled children (Lobato and Kao, 2002) (Box 18-5).
An important factor in sibling adjustment and coping is information and knowledge regarding their brother’s or sister’s illness or disability. What siblings piece together or overhear is often much worse than the truth. Often they imagine gruesome things regarding the experiences related to the illness, treatment, and hospitalization (Shepard and Mahon, 2000). Latino siblings have reported less accurate information about their sibling’s condition than non-Latino siblings (Lobato, Kao, and Plante, 2005). Parents are usually in the best position to impart information, although they are often overwhelmed with the medical crisis at hand (Fleitas, 2000). Nurses can encourage parents to talk with the siblings about how they perceive their sick brother or sister and to be accepting of the siblings’ feelings. Nurses can be ideal educators and counselors of siblings during the course of their brother’s or sister’s illness (Shepard and Mahon, 2000).
COPING WITH ONGOING STRESS AND PERIODIC CRISES
Professionals can help families cope with stress by providing anticipatory guidance, providing emotional support, assisting the family in assessing and identifying specific stressors, aiding the family in developing coping mechanisms and problem-solving strategies, and working collaboratively with parents so that they become empowered in the process.
Concurrent Stresses Within the Family
The ability to deal with the overwhelming stress of a lifelong disability or illness is challenged further when additional stresses are present. Stressors may be situational or developmental. They may be related to marital difficulties, sibling needs, homelessness, or social isolation. Some families may simultaneously be struggling with a family member’s alcohol or other drug problem. Even relatively minor stressors, such as arranging care for siblings, managing the home, and traveling to distant treatment centers, can challenge a family’s ability to cope successfully.
Most families, regardless of their income or insurance coverage, have financial concerns. The costs of caring for a child with special needs can be overwhelming. Nurses and social workers can help a family review various options for financial assistance, including insurance, managed care, or health maintenance organization policies; Medicaid; Supplemental Security Income; Women, Infants, and Children program (WIC); the state Program for Children with Special Health Needs; disease-related associations; and local philanthropic organizations.
Coping Mechanisms
Coping mechanisms are behaviors aimed at reducing the tension caused by a crisis. Approach behaviors are coping mechanisms that result in movement toward adjustment and resolution of the crisis. Avoidance behaviors result in movement away from adjustment and represent maladaptation to the crisis. Several approach and avoidance behaviors used in coping with a chronic illness or disability are listed in the Nursing Care Guidelines box. None of the indexes can be used singly to assess the possible success or failure in resolving the crisis. Each behavior must be viewed in the context of all of the variables affecting the family. For example, the observation of several avoidance behaviors in an emotionally healthy family may denote significantly less risk to the successful resolution of the crisis than an equal number of avoidance behaviors in an individual who has few available supports.
Parental Empowerment
Empowerment can be seen as a process of recognizing, promoting, and enhancing competence. For parents of children with chronic conditions, empowerment may occur gradually as strength and capabilities are drawn on to master the child’s care, manage family life, and plan for the future. Advocating for the child and developing parent-professional partnerships are part of taking charge (Ray, 2002).
ASSISTING FAMILY MEMBERS IN MANAGING THEIR FEELINGS
Although some previous research has postulated stages of adaptation to a chronic illness or disability, there is a great deal of individual variation in responses to the diagnosis, adjustments made, and time frames for coming to terms with a diagnosis. It is important that professionals recognize and respect a wide range of reactions and coping mechanisms. In fact, members of the family of a child with a chronic illness or disability may experience a number of difficult emotions, including fear, guilt, anger, resentment, and anxiety. Learning to manage these emotions promotes adaptive coping (see Nursing Care Guidelines box). Support from professionals, other family members, and friends can assist family members in managing their feelings. The following discussion examines some common phases of adjustment and emotional reactions.
Shock and Denial
The initial diagnosis of a chronic illness or disability is often met with intense emotion and is characterized by shock, disbelief, and sometimes denial, especially if the disorder is not obvious, as in chronic illness. Denial as a defense mechanism is a necessary cushion to prevent disintegration and is a normal response to grieving for any type of loss. Probably all family members experience various degrees of adaptive denial as they learn of the impact that the diagnosis has on their lives.
Shock and denial can last from days to months, sometimes even longer. Examples of denial that may be exhibited at the time of diagnosis include:
 Attributing the symptoms of the actual illness to a minor condition
Attributing the symptoms of the actual illness to a minor condition
 Refusing to believe the diagnostic tests
Refusing to believe the diagnostic tests
 Delaying consent for treatment
Delaying consent for treatment
 Acting happy and optimistic despite the revealed diagnosis
Acting happy and optimistic despite the revealed diagnosis
 Refusing to tell or talk to anyone about the condition
Refusing to tell or talk to anyone about the condition
 Insisting that no one is telling the truth, regardless of others’ attempts to do so
Insisting that no one is telling the truth, regardless of others’ attempts to do so
 Denying the reason for admission
Denying the reason for admission
 Asking no questions about the diagnosis, treatment, or prognosis
Asking no questions about the diagnosis, treatment, or prognosis
Generally, these mechanisms should be respected as short-term responses that allow individuals to distance themselves from the tremendous emotional impact and to collect and mobilize their energies toward goal-directed, problem-solving behaviors.
In children, the importance of denial has repeatedly been demonstrated as a factor in their positive coping with the diagnosis. Denial allows the child to maintain hope in the face of overwhelming odds and to function adaptively and productively. Like hope, denial may be an adaptive mechanism for dealing with loss that persists until a family or patient is ready or needs other responses.
Denial is probably the least understood and most poorly dealt-with reaction. Health professionals typically label denial as maladaptive and act inappropriately by attempting to strip it away by repeated and sometimes blunt explanations of the prognosis. However, denial becomes maladaptive only when it prevents recognition of treatment or rehabilitative goals necessary for the child’s optimal survival or development.
Adjustment
For most families, adjustment gradually follows shock and is usually characterized by an open admission that the condition exists. This stage may be accompanied by several responses, which are normal parts of the adaptation process. Probably the most universal of these feelings are guilt and self-accusation. Guilt is often greatest when the cause of the disorder is directly traceable to the parent, as in genetic diseases or accidental injury. However, it can occur even without any scientific or realistic basis for parental responsibility. Frequently the guilt stems from a false assumption that the disability is a result of personal failure or wrongdoing, such as not doing something correctly during pregnancy or the birth. Guilt may also be associated with cultural or religious beliefs. Some parents are convinced that they are being punished for some previous misdeed. Others may see the disorder as a trial sent by God to test their religious strength and faith. With correct information, support, and time, most parents master guilt and self-accusation. The ability to master resentful and self-accusatory feelings of having “caused” the child’s disorder is a crucial factor in determining the parents’ acceptance of their child.
Children, too, may interpret their serious illness as retribution for past misbehavior. The nurse should be particularly sensitive to the child who passively accepts all painful procedures. This child may believe that such acts are inflicted as deserved punishment. It is vital that parents and health care professionals reassure children that their illness is not their fault.
Other common and normal reactions to a diagnosis are bitterness and anger. Anger directed inward may be evident as self-reproaching or punitive behavior, such as neglecting one’s health and verbally degrading oneself. Anger directed outward may be manifested in either open arguments or withdrawal from communication and may be evident in the person’s relationship with any number of individuals, such as the spouse, the child, and siblings. Passive anger toward the ill child may be evident in decreased visiting, refusal to believe how sick the child is, or inability to provide comfort. Among the most common targets for parental anger are members of the staff. Parents may complain about the nursing care, the insufficient time physicians spend with them, or the lack of skill of those who draw blood or start intravenous infusions.
Children are apt to respond with anger as well, and this includes the affected child and the well siblings. Children are aware of the loss engendered by their illness or disability and may react angrily to the restrictions imposed or the feelings of being different. Siblings may also feel anger and resentment toward the ill child and parents for the loss of routine and parental attention. It is difficult for older children and almost impossible for younger children to comprehend the plight of the affected child. Their perception is of a brother or sister who has the undivided attention of their parents, is showered with cards and gifts, and is the focus of everyone’s concern.
During the period of adjustment, four types of parental reactions to the child influence the child’s eventual response to the disorder:
Overprotection, in which the parents fear letting the child achieve any new skill, avoid all discipline, and cater to every desire to prevent frustration (Box 18-6)
Rejection, in which the parents detach themselves emotionally from the child but usually provide adequate physical care or constantly nag and scold the child
Denial, in which parents act is if the disorder does not exist or attempt to have the child overcompensate for it
Gradual acceptance, in which parents place necessary and realistic restrictions on the child, encourage self-care activities, and promote reasonable physical and social abilities
Reintegration and Acknowledgment
For many families the adjustment process culminates in the development of realistic expectations for the child and reintegration of family life with the illness or disability in a manageable perspective. Because a large portion of this phase is one of grief for a loss, total resolution is not possible until the child dies or leaves home as an independent adult. Therefore one can regard adjustment as “increased comfort” with everyday living rather than a complete resolution.
This adjustment phase also involves social reintegration in which the family broadens its activities to include relationships outside of the home, with the child as an acceptable and participating member of the group. This last criterion often differentiates the reaction of gradual acceptance during the adjustment period from total acceptance, or perhaps is more descriptive of the acknowledgment process.
Many parents of children with chronic illnesses experience chronic sorrow, feelings of sorrow and loss that recur in waves over time. As the child’s condition progresses, parents experience repeated losses that represent further declines and new caregiving demands. Consequently, families must be assessed on an ongoing basis and offered appropriate support and resources as their needs change over time (Gravelle, 1997).
ESTABLISHING A SUPPORT SYSTEM
The diagnosis of a child with a serious health problem or disability is a major situational crisis that affects the entire family system. However, families can experience positive outcomes as they successfully deal with the many challenges that accompany a child with chronic illness or disability.
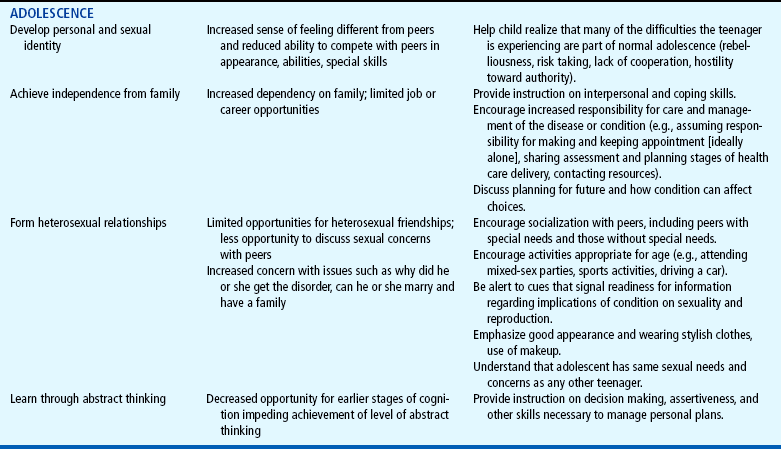
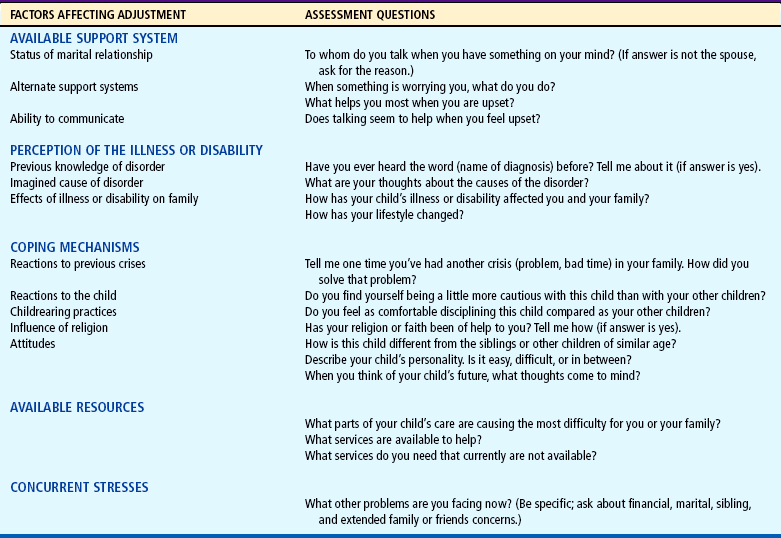
One nursing goal is to assess which families are at greater or lesser risk for succumbing to the effects of the crisis. Several variables—available support system, perception of the event, coping mechanisms, reactions to the child, available resources, and concurrent stresses within the family—influence the resolution of a crisis. Although most families cope well, the needs of families at risk are great. If they receive emotional support and guidance early, there is an increased likelihood that they will also cope successfully.
Although it is easy to assume that families of children with the most severe illnesses or disabilities would have the poorest adjustment, the severity of the condition reflects only one part of the overall picture. The level of adjustment is significantly influenced by the functional burden on the individual family (Stein, 1985). This concept considers the issues related to caring for and living with the child in relation to the family’s resources and ability to cope (Box 18-7). The family of a child with multiple disabilities demanding complex care, yet having many resources and coping skills, may adjust more successfully to the child’s situation than the family of a child with a less serious condition and few resources to counterbalance.
Intrafamilial resources, social support from friends and relatives, parent-to-parent support, parent-professional partnerships, and community resources interweave to provide a flexible web of support for the family of a child with a chronic condition.
THE CHILD WITH SPECIAL NEEDS
The child’s reaction to chronic illness or disability depends to a great extent on his or her developmental level, temperament, and available coping mechanisms; on the reactions of family members or significant others; and, to a lesser extent, on the condition itself. A child’s conceptual understanding of his or her own illness is based not only on age and developmental level, but also on the duration and type of experience accumulated with the disease. Knowledge of these variables is essential in providing the kind of information and support needed by these children to cope with a sometimes overwhelming situation.
DEVELOPMENTAL ASPECTS
The impact of a chronic illness or disability is influenced by the age at onset. Chronic illness affects children of all ages, but the developmental aspects of each age-group dictate particular stresses and risks for the child. The nurse must also recognize that children need to redefine their condition and its implications as they develop and grow. For example, appearance, skills, and abilities are highly valued by peers (Fig. 18-1); a teenager who is limited in any of these qualities is subject to rejection. This is especially marked when a physical disability interferes with sexual attractiveness.

FIG. 18-1 Children with any type of impairment should have the opportunity to develop their skills. (Courtesy Poyo/Hinton Photography.)
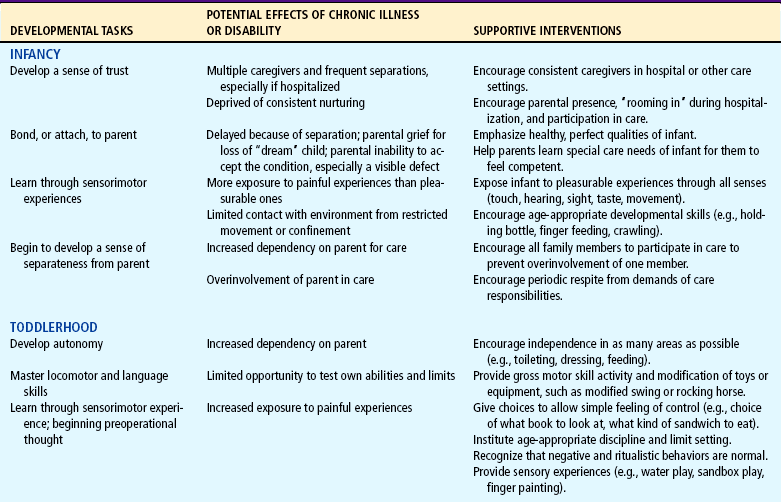
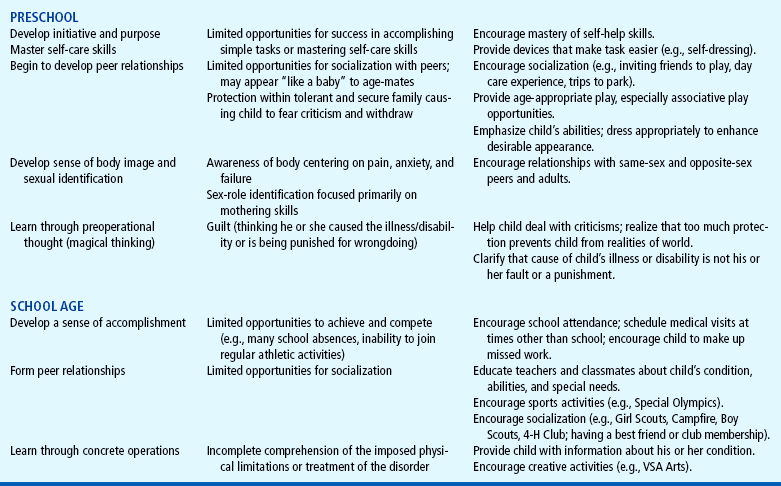
Children’s developmental concepts of illness are discussed in Chapter 21. An understanding of these developmental factors facilitates planning care to support the child and minimize the risks. Developmental aspects of chronic illness or disability on children are described in Table 18-2.
COPING MECHANISMS
Children with chronic conditions tend to use five distinct patterns of coping (Box 18-8). Children with more positive and accepting attitudes about their chronic illness use a more adaptive coping style characterized by optimism, competence, and compliance. They show fewer behavior problems at home and at school. The two maladaptive coping patterns— “Feels different and withdraws” and “Is irritable, is moody, and acts out”—are associated with poorer adaptation; children using these strategies have poorer self-concepts, more negative attitudes about their conditions, and more behavior problems at home and at school.
Well-adapted children gradually learn to accept their physical limitations and find achievement in a variety of compensatory motor and intellectual pursuits. They function well at home, at school, and with peers. They have an understanding of their disorder that allows them to accept their limitations, assume responsibility for care, and assist in treatment and rehabilitation regimens. They express appropriate emotions, such as sadness, anxiety, and anger, at times of exacerbations but confidence and guarded optimism during periods of clinical stability (Fig. 18-2). They are able to identify with other similarly affected individuals, promoting positive self-images and displaying pride and self-confidence in their ability to master a productive, successful life despite the disability.

FIG. 18-2 Periods of sadness and anger are appropriate in the child’s adjustment to a chronic illness or disability, especially during exacerbations of the disorder.
Hopefulness
Children, particularly adolescents, are sensitive to the presence or absence of hope. Hopefulness is an internal quality that mobilizes humans into goal-directed action that may be satisfying and life sustaining. A sense of hopefulness can produce increased participation in health-seeking behaviors and an improved sense of well-being (Ritchie, 2001).
Health Education and Self-Care
Health education is an intervention that promotes coping. Children need information about their condition, the therapeutic plan, and how the disease or the therapy might affect their particular situation. Children nearing puberty also need to understand the maturation process and how their disability may alter this event. For example, a youngster with Crohn disease should understand that this disorder is associated with growth failure and delayed puberty; a child with diabetes needs to know that hormonal changes and increased growth needs will alter food and insulin requirements at this time; and a sexually active girl with sickle cell anemia or systemic lupus erythematosus needs to be aware of the risks of pregnancy. The information should not be given all at once but should be timed appropriately to meet the changing needs of the youngsters, and it should be described and repeated as often as the situation demands.
RESPONSES TO PARENTAL BEHAVIOR
Parental behavior towards the child is one of the most important factors influencing the child’s adjustment. Children’s perceptions of their mothers’ support and maternal perceptions of psychosocial impact of the child’s chronic illness on the family were shown to be two of the greatest predictors of children’s psychologic adjustment (Immelt, 2006). In addition, family organization and illness-related support and involvement of parents influence children’s adjustment to chronic illness (Schor, 2003). They often display pride and confidence in their ability to cope successfully with the challenges imposed by their disorder. Anticipatory guidance by the nurse and encouragement of normalizing practices may assist parents in facilitating positive adjustment in their children.
TYPE OF ILLNESS OR DISABILITY
The type of illness or disability also influences the child’s emotional response. Interestingly, children with more severe disorders often cope better than those with milder conditions. However, the presence of multiple conditions may place a child at risk for more behavioral problems (Newacheck and Halfon, 1998). Considering children’s cognitive ability and their delay in achieving abstract thinking until adolescence, it is likely that an obvious condition is easier to accept because its limitations are concrete. For example, children who are blind or physically disabled are constantly reminded of their inability to run. However, children with cardiac defects not only live by rules they do not understand, but also only vaguely and occasionally sense their illness, such as when they try to run and experience dyspnea and fatigue. Therefore some chronic illnesses pose special threats to children.
The onset of a disabling condition may generate a state of confusion for children, who may have trouble differentiating between actual bodily functions and their image of their bodies. They may also experience problems in identifying themselves and those extensions of self (e.g., wheelchairs, braces, crutches, other mechanical or prosthetic devices) and may have difficulty in accepting functional aids.
NURSING CARE OF THE FAMILY AND CHILD WITH SPECIAL NEEDS
Because the nurse may meet a family during any phase of the adjustment process, several assessment areas are important (see Nursing Process box). The family’s ability to cope with previous stresses influences the current situation, and answers to questions about their usual coping skills are enlightening. Knowledge of concurrent stresses, such as financial, marital or nonmarital, and career or unemployment, helps identify families who may have fewer resources to cope with the child’s needs.
Finally, awareness of the family members’ reactions to the child and the illness or disability is important. Sample questions that the nurse and family can use to evaluate the support system, perception of the illness, coping mechanisms, resources, and concurrent stresses are listed in Table 18-1. Because factors affecting the family’s response may change at any point during the illness, assessment must be a continuous process.
Special challenges exist in assessing the child’s feelings about having a disability. Chapter 6 presents several approaches to encourage a child to discuss feelings about the condition. The nurse should use a variety of communication techniques, such as drawing and play, as assessment tools rather than relying solely on parental reports. Often, children are neglected partners in their care, and their unique needs are not identified (Young, Dixon-Woods, Windridge, and others, 2003; Dixon-Woods, Young, and Henry, 1999).
The needs of working parents and siblings also should be assessed, a goal that requires flexibility in scheduling appointments to include these important family members. When working parents know that their input is valuable, they will often change their work schedule to meet with a health professional. Because siblings can be of any age, the use of appropriate communication strategies for assessment must be considered. Nonverbal techniques such as those discussed in Chapter 6 should be considered for these children.
The main objective in working with the family is to help them cope effectively with those stresses imposed by the child’s special needs. To achieve this goal, the entire family should be considered in every aspect of the implementation process (see Family Focus box).
PROVIDE SUPPORT AT THE TIME OF DIAGNOSIS
The diagnosis is a critical time for parents and can influence how they perceive their health care providers throughout care. Although they may not hear or remember all that is said to them, they frequently sense a certain attitude of acceptance, rejection, hope, or despair that may influence their ability to absorb the shock and begin adapting to the family’s altered future.
Parents may be encouraged to be together when they are informed of their child’s condition, thus avoiding the problem of one parent having to interpret complex findings and deal with the initial emotional reaction of the other. The informing session should take place in a private, comfortable setting free of distractions and interruptions, in an atmosphere in which the parents feel free to express their emotions (Fig. 18-3). Their emotional needs are acknowledged by showing acceptance of such expressions as crying, sadness, anger, and disappointment. Emotional support is offered by having tissues available if a family member cries and demonstrating through facial and body language that indeed this is a difficult and painful period. Although touching is a powerful expression of empathy, it must be used wisely. For example, it can prematurely terminate free expression of feelings, especially when combined with statements such as “Everything will be all right.” Nurses should also be aware of cultural issues regarding touching (see Chapter 4).

FIG. 18-3 Informing session should take place in a private, comfortable setting free of distractions and interruptions.
Parents should receive the kind of information they desire. This can be assessed by asking questions such as, “Do you prefer to hear detailed information?” Parents or other family members may have different preferences regarding the amount of information they wish to hear. Most parents want a clear, simple explanation of the diagnosis; a prediction of possible futures for the child; advice on what to do next; an opportunity to ask questions; a warm, sympathetic listener; and, most important, time. Understanding of explanations is elicited with such questions as “Do you see what I mean?” or “Is this clear to you?” Technical terms are used with simple definitions. If the parents are unaware of the term, they are given written literature or at least a written summary of the diagnosis.
Finally, the informing conference does not end with the presentation of devastating news. Instead, the child’s strengths, appealing behaviors, and potential for development are stressed, as are available rehabilitation efforts or treatment. Parents can be encouraged to view their experiences as a series of challenges that they are capable of handling, particularly with available professional feedback. The parents are assured that the nurse will be available to answer questions and to provide further assistance as needed.
The preceding discussion relates primarily to the initial informing interview. However, because of the need for long-term follow-up, it is only one in a series of continuing discussions. In all interactions the family’s input is solicited and incorporated into the care plan. Some situations require consideration of special problems (see Nursing Care Guidelines box).
SUPPORT FAMILY’S COPING METHODS
For the family to meet the stresses of optimally adjusting to the child’s condition, each member must be individually supported so that the family system is strong. Although the family can indefinitely support a member who is in need of assistance, its greatest strength lies in every member supporting each other. The nurse should bear in mind that the family member in greatest need is not necessarily the affected child but may be a parent or sibling who is dealing with stresses that require intervention.
Parents
The nurse can provide support by being attentive to families’ responses to their children. Mothers and fathers need to experience success, joy, and pride in their children to give the support they need. Children, too, require support for their interactions, adjustments, and efforts. They must be reinforced for attempts to get to know their care providers and to communicate their needs to them.
It is important for nurses to examine their attitudes to determine their ability to engage in parent-professional partnerships. An essential characteristic is the belief that parents are equal to professionals and are experts regarding their child (see Nursing Care Guidelines box).
Communication among all family members is encouraged. Parent group sessions can help parents verbalize thoughts and feelings to each other but often do not take into account siblings’ or the child’s viewpoint. Therefore the nurse may need to set up a family session, such as during a home or clinic visit. Although the ideal situation is to have all the members present at one time, often this is not possible. Inviting members to participate at various visits is an appropriate alternative.
Parents can be encouraged to discuss their feelings toward the child, the impact of this event on their marriage, and associated stresses such as financial burdens. For most families, regardless of their income or insurance coverage, financial concerns exist. The costs of caring for a child with special needs can be overwhelming. In addition, the family wage earner may have to sacrifice job opportunities to remain close to a medical facility or to avoid losing insurance benefits.*
The nurse regards fathers as able, effective parents, competent and capable of coping with the challenges they face. Every effort is made to include the father in visits, such as to the nursery, clinic, special school, and stimulation programs. The father is included in the assessment process, with specific emphasis on having him describe the child’s strengths and difficulties. It is not unusual to find two parents who have differing views of the child’s abilities, especially in the area of developmental disabilities.
Numerous volunteer and community resources are available that provide assistance, rehabilitation, equipment, and funding for a variety of health problems.* National and local disease-oriented organizations may provide needed assistance and support to families that qualify. Many of these are discussed elsewhere in the text under the specific diagnosis. State and federal departments of health, mental health, social service, and labor may be able to help locate appropriate regional resources. For example, state programs for Children with Special Health Needs (formerly Crippled Children’s Services) provide financial assistance for children with many disabling conditions. Local and national sources of respite care and medical day care may be useful to families. Nurses should become acquainted with those in their communities and with vocational programs for special groups.
Parent-to-Parent Support
Just being with another parent who has shared similar experiences is helpful. It may not need to be a parent of a child with the same diagnosis, since parents in the process of adjusting to a child with special needs—or finding respite services, educational or rehabilitative services, special equipment vendors, and financial counseling—tread a common path. If the agency does not have a parent staff position, the nurse can contact parent groups that will often send a representative. Another strategy is to ask another parent to talk to the parents. The nurse should seek out a parent who is a good listener, has a nonjudgmental approach to differences in families, and possesses good advocacy and problem-solving skills.
The parent self-help group is another way to promote parent-to-parent support.* Group members feel less alone and have the opportunity to observe both coping and mastery role modeling from other members. Parents’ groups are rich resources for information. Even if parents are unable to attend meetings, they can still benefit from group newsletters and other literature that often accompany membership. The nurse can foster parent participation in self-help groups by serving as a referral agent, a group advisory board member, a resource person, a group member, or an assistant in founding a group. Sometimes all that is required in starting a group is identifying one or two parents as leaders; sharing with them the names, telephone numbers, and addresses of other families who have expressed both an interest and a willingness to release their phone number and address; and guiding them in how to initiate a first meeting.
Advocate for Empowerment
Nurses can advocate for methods that foster opportunities for parent empowerment. For example, nurses can suggest reimbursement for travel and child care, plus stipends to enable parents’ voices to be heard at meetings and conferences. They can encourage parent membership on staff, committees, and boards. They can keep parents informed of pending legislation on child health issues or take action when parents inform them.
The Child
Through ongoing contacts with the child, the nurse (1) observes the child’s responses to the disorder, ability to function, and adaptive behaviors within the environment and with significant others; (2) explores the child’s own understanding of his or her illness or condition; and (3) provides support while the child learns to cope with his or her feelings. Children are encouraged to express their concerns rather than allowing others to express them for them, since open discussions may reduce anxiety.
One of the most important interventions is alleviating the child’s feeling of being different and normalizing his or her life as much as possible (see Nursing Care Guidelines box). Whenever possible, the nurse assists the family in assessing the child’s daily routine for indications of a need for normalizing practices. For example, the child who remains in a bedroom all day requires a restructured daily routine to provide activities in different parts of the house, such as eating in the kitchen or dining room with the family. Such children may also be deprived of social, recreational, and academic activities that can be better accommodated by applying normalization practices. For example, home and out-of-home health-related treatments should be planned at times that least interfere with normal daily activities.
Children who are concerned that their condition detracts from their physical attractiveness need attention focused on the normal aspects of appearance and capabilities. Health professionals help strengthen and consolidate the self-image by emphasizing the normal, while allowing children to express anger, isolation, fear of rejection, feelings of sadness, and loneliness. The children need positive reinforcement for compliance and any evidence of improvement. Anything that might improve attractiveness and contribute to a positive self-image is employed, such as makeup for a teenager with a scar, clothing that disguises a prosthesis, or a hairstyle or wig to cover a deformity or lost hair.
Siblings
The presence of a child with special needs in a family may result in parents paying less attention to the other children. Siblings may respond by developing negative attitudes toward the child or by expressing anger in different forms. The nurse can help by using anticipatory guidance, questioning the parents about what they believe is the best way to have siblings respond to the child and guiding them through ways to meet their other children’s needs for attention. This questioning should take place before serious negative effects occur.
Siblings may also experience embarrassment associated with having a brother or sister with an illness or disability. Parents are then faced with the difficulty of responding to this embarrassment in an understanding and appropriate manner without punishing the siblings for how they feel. Parents are encouraged to talk with the siblings about how they view their affected sibling. For example, siblings of a child who is retarded may express fears about their ability to bear normal children. Adolescents in particular may not be able to discuss these vital issues with their parents and may prefer to consult with the nurse. Many siblings benefit from sharing their concerns with other young people who are experiencing a similar situation. Support groups for siblings can help decrease isolation, promote expression of feelings, and provide examples of effective coping skills.
Many parents express concern about when and how to inform the other children in the family about a sibling’s disability. The answer depends on each child’s level of sophistication and understanding. However, it is usually best to inform the siblings before a neighbor or other nonfamily member does so. Uninformed siblings may fantasize or develop apprehensions that are out of proportion to the child’s actual condition. Furthermore, if parents choose to be silent or deceptive about the issue, they are setting a negative precedent for the siblings to follow, rather than encouraging the siblings to cope with the experience in a healthy and nurturing way.
The nurse is sensitive to the reactions of siblings and whenever possible intervenes to promote more positive adjustment. For example, siblings often mention that they are expected to take on additional responsibilities to help the parents care for the child. It is not unusual for them to express a positive reaction to assuming the extra duties but a negative response to feeling unappreciated for doing so. Such feelings can often be minimized by encouraging siblings to discuss this with the parents and by suggesting to parents ways of showing gratitude, such as an increase in allowance, special privileges, and, most significantly, verbal praise.
EDUCATE ABOUT THE DISORDER AND GENERAL HEALTH CARE
Educating the family about the disorder is actually an extension of revealing the diagnosis. Education involves not only supplying technical information, but also discussing how the condition will affect the child. Parents may be able to digest only so much information at a time. It may be helpful to provide essential information and then follow by asking, “What else would you like to know about your child’s condition?” Responding to parents’ questions and concerns ensures that their information needs are met.
Activities of Daily Living
Parents also need guidance in how the condition may interfere with or alter activities of daily living, such as eating, dressing, sleeping, and toileting. One area frequently affected is nutrition. Common problems are undernutrition resulting from food being inappropriately restricted or loss of appetite, vomiting, or motor deficits that interfere with feeding; overnutrition may also occur, usually because of a caloric intake in excess of energy expenditure or boredom and lack of stimulation in other areas. Although the child requires the same basic nutrients as other children, the daily requirements may differ. Special nutritional considerations are discussed as appropriate throughout the text.
Safe Transportation
Modifications may also be needed regarding car safety. Children with conditions such as low birth weight (see Discharge Planning and Home Care, Chapter 9) or orthopedic, neuromuscular, or respiratory problems often cannot safely use conventional car restraints. For example, children with hip spica casts cannot sit properly in child safety seats (see Developmental Dysplasia of the Hip, Chapter 31). Modifications can be made to some commercial models, and for older children a special vest is available that secures the child to the back seat in a lying-down position.*
If a child requires a wheelchair, the family should consult the wheelchair manufacturer for specific instructions regarding safe car transportation. Considerations for wheelchairs used with vehicle transportation must address securing both the wheelchair and the occupant in the wheelchair. Wheelchairs should be secured facing forward with tie downs at four points. The tie-down system should be dynamically crash tested, as should the occupant securement system that secures the child in the wheelchair. For example, use of trays would not be recommended for transportation. With children who must travel with additional medical equipment, this equipment (e.g., oxygen, monitors, or ventilators) should be anchored to the floor or underneath the vehicle seat or wheelchair. Soft padding should be added around the equipment to reduce movement. A second adult should be present to monitor the condition of a medically fragile child while traveling.
Primary Health Care
Children with special needs require all the usual health care recommended for any child. Attention to injury prevention, immunizations, dental health, and regular physical examinations is essential. Nurses can play an important role in reminding parents of these aspects of care that are so often neglected when the concern is focused on the child’s illness or disability. Specific discussions of nutrition, sleep and activity, dental health, and injury prevention are presented in the chapters on health promotion for specific age-groups. Immunizations are discussed in Chapter 10.
Parents also need to be aware of the importance of communicating the child’s condition in the event of a medical emergency. Young children are unable to give information about their disorder, and although older children may be reliable sources, after an accident they may be physically unable to speak. Therefore all children with any type of chronic condition that may affect medical care should wear some type of identification, such as a MedicAlert bracelet,† or carry a card in their wallet that lists the medical condition and a phone number for emergency medical records and other personal information.
PROMOTE NORMAL DEVELOPMENT
Aside from knowledge of the condition and its effect on the child’s abilities, the family must be guided toward fostering appropriate development in their child. Although each stage may take longer to achieve, parents are guided toward helping the child fully realize his or her potential in preparation for the next developmental stage. Table 18-2 outlines developmental aspects of chronic illness or disability and supportive interventions. With appropriate planning and knowledge of strategies to improve the child’s functional abilities, most children can live fulfilling and productive lives.
One important aspect of promoting normal development is to encourage the child’s self-care abilities in both activities of daily living and the medical regimen. An assessment of the child’s age and physical, emotional, and mental capacities, as well as the support and structure provided by the family, should be considered in determining the appropriate level of self-care in the medical regimen. Even toddlers can be involved in their own care by holding supplies for the parent during a procedure. Over time, children should be encouraged toward greater autonomy in the self-care arena.
Early Childhood
During infancy the child is achieving basic trust through a satisfying, intimate, consistent relationship with his or her parents. However, the affected child’s early existence may be stressful, chaotic, and unsatisfying. Consequently, he or she may need more parental support and expressions of affection to achieve trust. Likewise, the parents require assistance in finding ways to meet the infant’s needs, such as how to hold a rigid or flaccid infant, how to feed a child with tongue thrust or episodes of dyspnea, and how to stimulate a child who seems incapable of achieving any skills. If hospitalizations are frequent or prolonged, every effort is made to preserve the parent-child relationship (see also Chapter 21). Hospital policies should promote visitation by and involvement of families.
During early childhood the goal is to achieve separation from parents, autonomy, and initiative. However, the natural parental response to having a sick child is overprotection. Parents need help in realizing the importance of brief separations of the child from them and from others involved in the child’s care and of providing social experiences outside the home whenever possible. Respite care, which provides temporary relief for family members, can be essential in allowing caregivers time away from the daily burdens.
Young children also need the opportunity to develop independence. Frequently the child is able to learn self-help skills, such as holding the bottle, finger feeding, and removing simple articles of clothing, but the parent continues to perform the act. The nurse can guide parents to the usual milestones expected from the child. When a child is unable to perform a skill independently, functional aids should be used. With innovation, many adaptations can be implemented in children’s environments to increase their mobility and independence and allow them to play like other children their age. For example, with slight modifications, a child with physical limitations may be able to ride a tricycle (Fig. 18-4).

FIG. 18-4 A modified tricycle with block pedals, self-adhesive straps for support, and modified seat and handle bars can help a child with disabilities gain mobility.
Another critical component for normal child development is discipline. Discipline and guidance serve several purposes, such as providing children with boundaries on which to test out their behavior and teaching them socially acceptable behavior. Resentment and hostility can arise among siblings if different standards are applied to each child. The nurse’s responsibility is to help parents learn successful methods of managing a child’s behaviors before they become problems (see Limit Setting and Discipline, Chapter 3).
School Age
For school-age children the major tasks are entry into school and achieving a sense of industry. Although the importance of school in the life of all children is well known, school absences are significantly higher among children with chronic illness than among their healthy peers. The more school absences the child experiences, the more difficult it is to resume attendance, and school phobia may result. The child should return to school as soon as possible after diagnosis or treatments.
Preparation for entry into or resumption of school is best accomplished through a team approach with the parents, child, teacher, school nurse, and primary nurse in the hospital. Ideally, this planning should begin before hospital discharge, provided that the child is well enough to resume usual activities. A structured plan should be developed, with attention to those aspects of care that must be continued during school hours, such as administration of medication or other treatments.
Children also need preparation before entering or resuming school. Having a tutor in the hospital or home as soon as children are physically able helps them realize that school will continue and gives them time to consider this prospect (Fig. 18-5). They need to investigate possible answers to the many questions others will ask. One method of anticipatory preparation is to role-play, with the child as the “returned pupil” and the nurse or parent as “other schoolmates.” If the child returns to school with some obvious physical change, such as hair loss, amputation, or visible scar, the nurse might also ask questions about these alterations to prompt preparatory responses from the child.

FIG. 18-5 Children with special needs should continue their schooling as soon as their condition permits.
Classroom peers also need preparation, and a joint plan of the teacher, nurse, and child is best. At a minimum, classmates should be given a description of the child’s condition, prepared for any visible changes in the child, and allowed an opportunity to ask questions. The child should have the option of attending this session. As the child’s condition changes, particularly if the illness is potentially fatal, school personnel, including the students, need periodic apprisal of the child’s status and preparation for what to expect.
Children with special needs are encouraged to maintain or reestablish relationships with peers and to participate according to their capabilities in any age-appropriate activities. Alternative activities may be substituted for those that are impossible or that place a strain on the child’s condition. Programs such as the Special Olympics*. Several pamphlets on sports and recreation for children with disabilities are available from Easter Seals (see footnote, p. 589) and American Alliance for Health, Physical Education, Recreation and Dance, 1900 Association Drive, Reston, VA 20191; (703) 476-3400 or (800) 213-7193; http://www.aahperd.org. offer children an opportunity to compete witheir peers and to achieve athletic skill. Summer camps†. allow children to associate with peers and develop a wide variety of skills. Children with special needs can derive enormous benefits from expressive activities, such as art, music, poetry, dance, and drama. With adaptive equipment and imagination, children can participate in a variety of activities. Organizations such as VSA Arts allow children to celebrate and share their accomplishments.*. Children need the opportunity to interact with healthy peers and to engage in activities with groups or clubs composed of similarly affected age-mates. Such organizations as ostomy clubs, diabetes clubs, and cerebral palsy groups share information and provide support related to the special problems the members face.
Adolescence
Adolescence can be a particularly difficult period for the teenager and family. All of the needs discussed previously apply to this age-group as well. Developing independence or autonomy, however, is a major task for the adolescent as planning for the future becomes a prominent concern. Although the emphasis in the past has been on achieving independence from physical assistance, recent developments in the fields of special education, adolescent development, and family systems suggest redefining autonomy in terms of individuals’ capacities to take responsibility for their own behavior, to make decisions regarding their own lives, and to maintain supportive social relationships. Given this understanding, even individuals with severe impairment can be viewed as autonomous if they perceive their own needs and take responsibility for meeting them, either directly or by engaging the assistance of others. As adolescents become more autonomous, the nurse can help them articulate needs, participate in developing their own care plan, and discover and express how others can be of greatest assistance.
Physical symptoms are high on the teenager’s list of health-related concerns. Because adolescence is a time of enormous physical and emotional changes, it is important for the nurse to distinguish between body changes that are related to disability and those that are a result of normal body development. It can be a great comfort for teenagers with disabling conditions to know that many of the changes they experience are normal developmental outcomes.
A sense of feeling different from peers can lead to loneliness, isolation, and depression. Participation in groups of teenagers with chronic conditions or disabilities can alleviate feelings of isolation and smooth the transition to a meaningful relationship with one person in adulthood.
ESTABLISH REALISTIC FUTURE GOALS
One of the most difficult adjustments is setting realistic future goals for the child and for those involved in his or her continued care. Sometimes the impact of this decision does not surface until the child finishes school or the parents approach retirement, when a crisis can arise because of disruption of all of the family roles and relationships that maintained stability.
Planning for the future should be a gradual process. All along, the parents should cultivate realistic vocations for the child. For example, if children have physical disabilities, they are directed to intellectual, artistic, or musical pursuits. Children with developmental disabilities are taught manual skills. In this way, the child’s development proceeds in the direction of self-support through gainful employment.
With prolonged survival, young people with chronic illnesses must deal with new decisions and problems, such as marriage, employment, and insurance coverage. With appropriate guidance, individuals with disabilities can attain gainful employment, marriage, and a family. For those whose conditions are genetic, counseling is needed regarding future offspring. Prospective spouses often benefit from an opportunity to discuss their feelings regarding marriage to an individual with continued health needs and possibly a limited life span. Health insurance coverage is a critical issue because some private carriers may no longer insure a young person who leaves home or may be unwilling to reinsure the person who is independent. Life insurance is another dilemma, especially when children have serious defects, such as congenital heart anomalies.
PERSPECTIVES ON THE CARE OF CHILDREN AT THE END OF LIFE
Although most childhood illnesses and many injuries and other trauma respond favorably to treatment, some do not. When a child and family face a prolonged and possibly terminal illness, health professionals must confront the challenge of providing the best possible care to meet the physical, psychologic, spiritual, and emotional needs of the child and family during the uncertain course of the illness and at the time of death. When death is sudden and unexpected, nurses are challenged to respond to grief and shock in families and provide comfort and support in the absence of a prior relationship.
Many factors affect the causes of death that nurses are likely to encounter in children: developmental factors, medical advances and technology, and changing social patterns. In infants the leading causes of death are congenital anomalies, respiratory distress syndrome, disorders related to short gestation and low birth weight, and sudden infant death syndrome (Arias, MacDorman, Strobino, and others, 2003) (see Chapter 1). The leading causes of death in children 5 to 9 years of age include injuries (accidents), malignant neoplasms, congenital anomalies, assault (homicide), and heart disease. In children 10 to 14 years of age, suicide is the third leading cause of death, after injuries (accidents) and malignant neoplasms. In youths 15 to 19 years of age, assault (homicide), suicide, malignant neoplasms, and heart disease follow accidents as the most prevalent causes of death (Anderson and Smith, 2005).
A child who is diagnosed with a life-threatening illness or who is suffering serious, life-threatening trauma needs medical diagnosis and intervention, as well as nursing assessment and care—sometimes for a short time and sometimes over a lengthy period. When cure is no longer possible and life-prolonging measures result in pain and distress to the child, parents need information about care options that are available to assist them in deciding how they want the remaining time with their child to be managed by the health care team. It is important that families are reassured that although their child cannot be cured, active care will continue to be provided to maintain the child’s comfort. Support is provided to assist the child and family during the dying process. As a result, nurses may care for children and families who are making the difficult transition from curative or restorative treatments to palliative care.
PRINCIPLES OF PALLIATIVE CARE
Palliative care involves a multidisciplinary approach to the management of a terminal illness or the dying process that focuses on symptom control and support rather than on cure or life prolongation in the absence of the possibility of a cure (Field and Behrman, 2004). The World Health Organization (1996) defines palliative care as the “active total care of patients whose disease is not responsive to curative treatment. Control of pain, of other symptoms, and of psychological, social and spiritual problems is paramount. The goal of palliative care is the achievement of the best possible quality of life for patients and their families.”
Palliative care interventions do not serve to hasten death; rather, they provide pain and symptom management, attention to issues faced by the child and family with regard to death and dying, and promotion of optimal functioning and quality of life during the time the child has remaining. The implementation of neonatal and pediatric palliative care consulting services within hospitals has led to enhanced quality of life and end-of-life care for children and their families and support for their care providers (Jennings, 2005; Pierucci, Kirby, and Leuthner, 2001). Several principles are hallmarks of palliative care.
The child and family are considered the unit of care. The death of a child is an extremely stressful event for a family because it is out of the natural order of things. Children represent health and hope, and their death calls into question the understanding of life. A multidisciplinary team of health care professionals consisting of social workers, chaplains, nurses, personal care aides, and physicians skilled in caring for dying patients assist the family by focusing care on the complex interactions between physical, emotional, social, and spiritual issues.
Palliative care seeks to create a therapeutic environment, as homelike as possible, if not in the child’s own home. Through education and support of family members, an atmosphere of open communication is provided regarding the child’s dying process and its impact on all members of the family (see Evidence-Based Practice box).
DECISION MAKING AT THE END OF LIFE
Discussions concerning the possibility that a child’s illness or condition is not curable and that death is an inevitable outcome cause everyone involved a great deal of stress. Physicians, other members of the health care team, and families must consider all information regarding the child’s situation and make decisions that all parties agree to and that will have a profound impact on the child and family.
Ethical Considerations in End-of-LifeDecision Making
A number of ethical concerns arise when parents and health care professionals are deciding on the best course of care for the dying child. Many parents and health care providers are concerned that not offering treatment that would cause potential pain and suffering, but might extend life, would be considered euthanasia or assisted suicide. To eliminate such concerns, it is necessary to understand the various terms. Euthanasia involves an action carried out by a person other than the patient to end the life of the patient suffering from a terminal condition. The intent of this action is based on the belief that the act is “putting the person out of his or her misery”; this action has also been called mercy killing. Assisted suicide occurs when someone provides the patient with the means to end his or her life and the patient uses that means to do so. The important distinction between these two actions involves who is actually acting to end the person’s life.
The American Nurses Association Code of Ethics for Nurses (2001) does not support the active intent on the part of a nurse to end a person’s life. However, it does permit the nurse to provide interventions to relieve symptoms in the dying patient even when the interventions involve substantial risks of hastening death. When the prognosis for a patient is poor and death is the expected outcome, it is ethically acceptable to withhold or withdraw treatments that may cause pain and suffering and provide interventions that promote comfort and quality of life. Therefore providing palliative care for patients is the ethically correct choice in such a circumstance.
Physician–Health Care Team Decision Making
Decisions by physicians regarding care are often made on the basis of the progression of the disease or amount of trauma, the availability of treatment options that would provide cure from disease or restoration of health, the impact of such treatments on the child, and the child’s overall prognosis (Davis and Eng, 1998). Often the main determinants prompting physicians to discuss end-of-life issues and options for children with critical illnesses include the child’s age, premorbid cognitive condition and functional status, pain or discomfort, probability of survival, and quality of life (Masri, Farrell, Lacroix, and others, 2000). When the physician discusses this information openly with families, a shared decision-making process can occur regarding do-not-resuscitate (DNR) orders and care that is focused on the comfort of the child and family during the dying process.
Unfortunately, many families are not given the option of terminating treatment and pursuing care that is focused on comfort and quality of life when cure is unlikely, and staff may be reluctant to raise the question of DNR orders. This occurs for a number of reasons, including the belief that not being able to “save” a child is a “failure.” Also, the physician and other members of the health care team may lack knowledge of and experience with the principles of palliative care (Field and Behrman, 2004; Sumner, 2003; Sahler, Frager, Levetown, and others, 2000).
Parental Decision Making
Rarely are families prepared to cope with the numerous decisions that must be made when a child is dying. When the death is unexpected, as in the case of an accident or trauma, the confusion of emergency services and possibly an intensive care setting presents challenges to parents as they are asked to make difficult choices. If the child has either experienced a life-threatening illness such as cancer or lived with a chronic illness that has now reached its terminal phase, parents are often unprepared for the reality of their child’s impending death (see Family Focus box). Numerous studies have found that families facing the impending death of a child depend on information provided to them by the health care team, particularly an honest appraisal of the child’s prognosis, to make difficult decisions regarding care options for their child (Wolfe, Friebert, and Hilden, 2002; Hinds, Oakes, Furman, and others, 2001; James and Johnson, 1997).
As the group of health professionals who are most involved with families, nurses are in an excellent position to ensure that families are presented with the options available to them. The nurse’s first responsibility is to explore the family’s wishes. This is best done in concert with the physician, but at times may need to be initiated by the nurse. Statements such as “Tell me about your thoughts for the type of care you want your child to receive when he is dying” or “Have you considered the types of interventions you would like us to use when your child is near death?” can begin discussion of this sensitive but critical aspect of terminal care.
The Dying Child
Children need honest and accurate information about their illness, treatments, and prognosis; this information needs to be given in clear, simple language. In most situations this best occurs as a gradual process over time, characterized by increasingly open dialogue between parents, professionals, and the child (Young, Dixon-Woods, Windridge, and others, 2003). Providing an atmosphere of open communication early in the course of an illness facilitates answering difficult questions as the child’s condition worsens. Providing appropriate literature about the disease, as well as the experience of illness and possible death, is also helpful. Exactly how and when to involve children in decisions regarding care during their dying process and death is an individual matter. The child’s age or developmental level is an important consideration in the process (Table 18-3). In general, parents should be asked how they would like their child to be told of their prognosis, and they should be included in his or her care. Some parents may request that their child not be told that he or she is dying, even if the child asks. This often places health care providers in a difficult situation. Children, even at a young age, are perceptive. Even if they are not told outright that they are dying, they realize that something is seriously wrong and that it involves them. Often, helping parents understand that honesty and shared decision making between them and their child are important to the child’s and family’s emotional health will encourage parents to allow discussion of dying with their child. Parents may require professional support and guidance in this process from a nurse, social worker, or child life specialist who has a good relationship with the child and family.
If given the opportunity, children will tell others how much they want to know. Asking questions such as “If the disease came back, would you want to know?” “Do you want others to tell you everything, even if the news isn’t good?” or “If someone were not getting better [or more directly, “were dying”], do you think he would want to know?” helps children set the limits of how much truth they can accept and cope with. Children need time to process many feelings and much information so that they can assimilate and ideally accept the inevitable fact of mortality.
Care of the dying adolescent requires the nurse to become knowledgeable about any possible delays or alterations in normal growth and development. Legal and ethical issues also come to the forefront with respect to the age at which an adolescent should have autonomy in decision making with regard to care and treatment. Effective communication between the patient, family, and health care team is an important part of optimal care for the dying adolescent (Freyer, 2004).
Treatment Options for Terminally Ill Children
Based on the child’s and family’s decision regarding their wishes for terminal care, they have several options from which to choose.
Hospital.: Families may choose to remain in the hospital to receive care if the child’s illness or condition is unstable and home care is not an option or the family is uncomfortable with providing care at home. If a family chooses to remain at the hospital for terminal care, the setting should be made as homelike as possible. Families are encouraged to bring familiar items from the child’s room at home. In addition, there should be a consistent and coordinated care plan for the child’s and family’s comfort.
Home Care.: Some families prefer to take their child home and receive services from a home care agency. Generally, these services entail periodic nursing visits to administer a treatment or provide medications, equipment, or supplies. The child’s care continues to be directed by the primary physician. Home care is often the option chosen by physicians and families because of the traditional view that a child must be considered to have a life expectancy of less than 6 months to be referred to hospice care. Fortunately, a number of hospice organizations are expanding their services to children based on the presence of a life-limiting disease process for which cure is not possible, rather than on the sole criteria of a limited time-projected prognosis.
Hospice Care.: Parents should be offered the option of caring for their child at home during the final phases of an illness with the assistance of a hospice organization. Hospice is a community health care organization that specializes in the care of dying patients by combining the hospice philosophy with the principles of palliative care. Hospice philosophy regards dying as a natural process and care of dying patients as including management of the physical, psychologic, social, and spiritual needs of the patient and family. Care is provided by a multidisciplinary group of professionals in the patient’s home or an inpatient facility that employs the hospice philosophy. Hospice care for children was introduced in the 1970s, and a number of community hospice organizations now accept children into their care (Davies, Davis, and Sibert, 2003; Forrester, 2003; Winkler and Mardegian, 2001; Faulkner and Armstrong-Dailey, 1997). Collaboration between the child’s primary treatment team and the hospice care team is essential to the success of hospice care. Families may continue to see their primary care physicians as they choose.*
Hospice care is based on a number of important concepts that significantly set it apart from hospital care:
 Family members are usually the principal caregivers and are supported by a team of professional and volunteer staff.
Family members are usually the principal caregivers and are supported by a team of professional and volunteer staff.
 The priority of care is comfort. The child’s physical, psychologic, social, and spiritual needs are considered. Pain and symptom control are primary concerns, and no extraordinary efforts are used to attempt a cure or prolong life.
The priority of care is comfort. The child’s physical, psychologic, social, and spiritual needs are considered. Pain and symptom control are primary concerns, and no extraordinary efforts are used to attempt a cure or prolong life.
 The family’s needs are considered to be as important as those of the patient.
The family’s needs are considered to be as important as those of the patient.
 Hospice is concerned with the family’s postdeath adjustment, and care may continue for a year or more.
Hospice is concerned with the family’s postdeath adjustment, and care may continue for a year or more.
The goal of hospice care is for children to live life to the fullest without pain, with choices and dignity, in the familiar environment of their home, and with the support of their family. Hospice care is covered under state Medicaid programs and by most insurance plans. The service provides home visits from nurses, social workers, chaplains, and, in some cases, physicians. Medications, medical equipment, and any necessary medical supplies are all provided by the hospice organization providing care.
With children, the home has been the more common environment for implementing the hospice concept; it benefits the family in a variety of ways. Children who are dying are allowed to remain with those they love and with whom they feel secure. Many children who were thought to be in imminent danger of death have gone home and lived longer than expected. Siblings can feel more involved in the care and often have more positive perceptions of the death. Parental adaptation is often more favorable, demonstrated by their perceptions of how the experience at home affected their marriage, social reorientation, religious beliefs, and views on the meaning of life and death.
If the home is chosen for hospice care, the child may or may not die in the home. Reasons for final admission to a hospital vary but may be related to the parents’ or siblings’ wish to have the child die outside the home; exhaustion on the part of the caregivers; and physical problems such as sudden, acute pain or respiratory distress.
NURSING CARE OF THE CHILD AND FAMILY AT THE END OF LIFE
Regardless of where the child is cared for during the terminal stage of illness, both the child and the family usually experience fear of (1) pain and suffering, (2) dying alone (child) or not being present when the child dies (parent), and (3) actual death. Nurses can help families by lessening their fears through attention to the care needs of the child and family (see Nursing Care Plan).
FEAR OF PAIN AND SUFFERING
The presence of unrelieved pain in a terminally ill child can have detrimental effects on the quality of life experienced by the child and family. Parents feel that having their child in pain is unendurable and results in feelings of helplessness and a sense that they must be present and vigilant to get the necessary pain medications. Persistent pain also has an impact on the family as a whole. Nurses can alleviate the fear of pain and suffering by providing interventions aimed at treating the pain and symptoms associated with the terminal process in children.
Pain and Symptom Management
Pain control for children in the terminal stages of illness or injury must be given the highest priority. Despite ongoing efforts to educate physicians and nurses on pain management strategies in children, studies have reported that children continue to be undermedicated for their pain (Wolfe, Grier, Klar, and others, 2000). Nearly all children experience some amount of pain in the terminal phase of their illness. The current standard for treating children’s pain follows the World Health Organization’s analgesic stepladder (1996), which promotes tailoring the pain interventions to the child’s level of reported pain. Children’s pain should be assessed frequently, and medications adjusted as necessary. Pain medications should be given on a regular schedule, and extra doses for breakthrough pain should be available to maintain comfort. Opioid drugs such as morphine should be given for severe pain, and the dose should be increased as necessary to maintain optimal pain relief. Techniques such as distraction, relaxation techniques, and guided imagery (Lambert, 1999) should be combined with drug therapy to provide the child and family strategies to control pain (see Chapter 7 for further discussion of pain management strategies).
In addition to pain, children experience a variety of symptoms during their terminal course as a result of their disease process or as a side effect of medicines used to manage pain or other symptoms. These symptoms include fatigue, nausea and vomiting, constipation, anorexia, dyspnea, congestion, seizures, anxiety, depression, restlessness, agitation, and confusion (Wolfe, Friebert, and Hilden, 2002; Hellsten, Hockenberry, Lamb, and others, 2000). Each of these symptoms should be aggressively managed with appropriate medications or treatments and with interventions such as repositioning, relaxation, massage, and other measures to maintain the child’s comfort and quality of life.
Occasionally, children require very high doses of opioids to control pain. This may occur for several reasons. The child on long-term opioid pain management can become tolerant of the drug, meaning that it is necessary to give more drugs to maintain the same level of pain relief. This should not be confused with addiction, which is a psychologic dependence on the side effects of opioids. Addiction is not a factor in managing terminal pain in children. Other obvious reasons for requiring increased doses of opioids include progression of disease and other physiologic experiences of pain. It is important to understand that there is no maximum dose that can be given to control pain. However, nurses often express concern that administering doses of opioids that exceed what they are familiar with will hasten the child’s death. The principle of double effect (Box 18-9) addresses such concerns. It provides an ethical standard that supports the use of interventions intended to relieve pain and suffering even though there is a foreseeable possibility that death may be hastened (Rousseau, 2001). In cases in which the child is terminally ill and in severe pain, using large doses of opioids and sedatives to manage pain is justified when no other treatment options are available that would relieve the pain but make the risk of death less likely (Hawryluck and Harvey, 2000). See Chapter 7 for an extensive discussion of pain assessment and management.
Parents’ and Siblings’ Need for Education and Support
Parents are the primary caregivers when the child is at home, and nurses providing care to the child and family need to teach the family about the medications being given to the child, how to administer medications, and the use of non-pharmacologic techniques. Parents are kept informed of all medications and treatments given to a child in the hospital, and they are encouraged to participate in the child’s care to the extent that they desire. This empowers parents and provides a sense of control over the child’s comfort and well-being, reducing their fear that their child will be in pain or suffering as he or she is dying. Additionally, better bereavement outcomes (e.g., adaptive coping; family cohesion; less anxiety, stress, and depression) have been reported by parents who were actively involved in the care of their child (Goodenough, Drew, Higgins, and others, 2004; Lauer, Mulhern, Schell, and others, 1989). The grief work of fathers in particular seems to be facilitated when their child dies in the home setting. This finding may be related to the increased opportunity of working fathers to provide care to and spend time with their child at home vs the hospital setting.
Siblings may feel isolated and displaced during the time that their brother or sister is dying. Parents devote the majority of their time to the care and comfort of the dying child, causing siblings to feel left out of the parent–sick child relationship. Siblings may become resentful of their sick sibling and begin to feel guilty or ashamed about such feelings (Murray, 1999). Nurses can assist the family by helping the parents identify ways to involve siblings in the caring process, perhaps by bringing some supplies or favorite toy, game, or food item. Parents should also be encouraged to schedule time to spend with the other children where their focus is on them. Helping parents identify a trusted friend or family member who can sit with the ill child for a short period will allow them to attend to their own needs or those of their other children.
FEAR OF DYING ALONE OR OF NOT BEING PRESENT WHEN THE CHILD DIES
When a child is being cared for at home, the burden of care on parents and family members can be great. Often, as the child’s condition declines, family members begin the “death vigil.” Rarely is a child left alone for any length of time. This can be exhausting for family members, and nurses can assist the family by helping them arrange shifts so that friends or family members can be present with the child and allow others to rest. If the family has limited resources, community organizations such as hospice or churches often have volunteers who are willing to visit and sit with children. It is important that whoever is sitting with the child be aware of when the parent(s) would like to be notified to return to the child’s bedside (Fig. 18-6).

FIG. 18-6 For the dying child there is no greater comfort than the security and closeness of a parent.
When a child is dying in the hospital, parents should be given full access to the child at all times. If parents need to leave, they should be provided with a pager or other means of immediate communication and alerted if staff members note any change in the child that may indicate imminent death. Nurses advocate for parents’ presence in intensive care and emergency departments and attend to the parents’ needs for food, drinks, comfortable chairs, blankets, and pillows.
FEAR OF ACTUAL DEATH
The majority of children receiving hospice care die at home, often in their own room with family, pets, and other loved possessions around them. The physical process of dying can be distressing to parents because often the child slowly become less alert in the days before the actual death. The nurse can assist the family by providing them with information about what changes will occur as the child progresses through the dying process (Box 18-10). During this time, nursing visits often become more frequent and longer in duration to provide the family with additional support as the death nears. The most distressing change for parents to observe is the change in the respiratory pattern. In the final hours of life, the dying patient’s respirations may become labored, with deep breaths and long periods of apnea, referred to as Cheyne-Stokes respirations. Families are reassured that this is not distressing to the child and that it is a normal part of the dying process. However, the use of opioids can slow the respirations to make the child breathe more easily, and scopolamine, usually applied as a topical patch, can help reduce noisy respirations known as the “death rattle.” Noisy respirations are more likely to occur if the child is overhydrated.
All families have the option of admitting their child to the hospital if they feel unable to deal with the death. The child who dies at home must be pronounced dead; hospice programs typically have provisions so that this proceeds smoothly. In some circumstances the police may be notified, with an explanation of the circumstances to prevent unnecessary concern regarding abuse. Providing the police with the number of the responsible practitioner is usually all that is necessary to confirm the cause of death.
Hospital Deaths
Children dying in the hospital of terminal illnesses who are receiving supportive care interventions will experience a similar process. Again, increased nursing presence and attendance to the child’s and family’s needs provide comfort and support for many families.
Death resulting from accident or trauma or acute illness in settings such as the emergency department or intensive care unit often requires the active withdrawal of some form of life-supporting intervention, such as a ventilator or bypass machine. These situations often raise difficult ethical issues (Sine, Sumner, Gracy, and others, 2001), and parents are often less prepared for the actual moment of death. Nurses can assist these parents by providing detailed information about what will happen as supportive equipment is withdrawn, ensuring that appropriate pain medications are administered to prevent pain during the dying process, and allowing the parents time before the start of the withdrawal to be with and speak to their child. It is important that the nurse attempt to control the environment around the family at this time by providing privacy, asking if they would like to play music, softening lights and monitor noises, and arranging for any religious or cultural rituals that the family may want performed.
After the child’s death, the family should be allowed to remain with the body and hold or rock the child if they desire. After the nurse has removed all tubes and equipment from the body, parents should be given the option of assisting with the preparation of the body, such as bathing and dressing. It is important for the nurse to determine whether the family has any specific needs, since many cultures have adopted specific methods for coping with and mourning death and impeding these practices may interfere with the grieving process (Clements, Vigil, Manno, and others, 2003).
At some point the nurse discusses whether the family has made preparations for the burial service and whether the staff can help in any way. Parents often have concerns about the funeral, such as siblings’ involvement in the death rituals. Although no absolute answers exist regarding the question of siblings attending the funeral or burial services, the consensus is that the surviving children benefit from being involved in these events. However, children need preparation for postdeath services. They should be told what to expect, particularly how the deceased person will look if the coffin is open; allowed their private time to say good-bye; and permitted to stay as long as they wish. Ideally, the parents should prepare the siblings. If the parents’ grief prevents this communication, a significant family member or friend should substitute (see Family Focus box).
ORGAN OR TISSUE DONATION AND AUTOPSY
For some families organ or tissue donation may be a meaningful act—one that benefits another human being despite the loss of their child. Unfortunately, initiating a discussion about tissue donation is often stressful for staff, and there may be confusion regarding whose responsibility this is. In centers in which transplants are performed, a full-time transplant coordinator is usually available to inform the family about organ donation and to take care of details. If such services are not available, the staff needs to determine which members should discuss this topic with the family. Ideally, the person who knows the family best, knows when the death is expected, or has the opportunity to spend time with the family when the death is unexpected takes the role. Often nurses are in an optimal position to suggest tissue donation after consultation with the attending physician. When possible, the topic should be raised before death occurs. The request should be made in a private and quiet area of the hospital and should be simple and direct, with questions such as “Are you a donor family?” or “Have you ever considered organ donation?”
Many states have legislated a mandatory request for organ or tissue donation when a child dies, especially if the patient is brain dead. Written consent from the family is required before donation can proceed. When requests for organ donation are made, health care practitioners must address common misunderstandings families have about brain death and organ donation (Franz, DeJong, Wolfe, and others, 1997). Training health care professionals on sensitive approaches to requests for organ donation has been shown to increase families’ willingness to consent to organ donation (American Academy of Pediatrics, 2002; Evanisko, Beasley, Brigham, and others, 1998). The option to donate organs should always be separate from the communication of impending or actual death.
Nurses need to be aware of common questions about organ donation to help families make an informed decision. Healthy children who die unexpectedly are excellent candidates for organ donation. Children with cancer, chronic disease, or infection or those who have suffered prolonged cardiac arrest may not be suitable candidates, although this is individually determined. The nurse should ask whether organ donation was discussed with the child or whether the child ever expressed such a wish. Any number of body tissues or organs can be donated (skin, corneas, bone, kidney, heart, liver, pancreas), and their removal does not mutilate or desecrate the body or cause any suffering. The family may have an open casket, and there is no delay in the funeral. There is no cost to the donor family, but organ donation does not eliminate funeral or cremation responsibilities. Most religions permit organ donation as long as the recipient benefits from the transplant, although Orthodox Judaism forbids it.
In cases of unexplained death, violent death, or suspected suicide, autopsy is required by law. In other instances it may be optional, and parents should be informed of this choice. The procedure, as well as forms that require signing, should be explained. The family should know that the child can be in an open casket after an autopsy.
GRIEF AND MOURNING
Grief is a process, not an event, of experiencing physiologic, psychologic, behavioral, social, and spiritual reactions to the loss of a child. Grief is highly individualized, encompassing a broad range of manifestations from person to person. It is a natural and expected reaction to loss. It is neither orderly nor predictable. Grieving in any form is necessary for healing to occur. When death is the expected or a possible outcome of a disorder, the child and family members may experience anticipatory grief. Anticipatory grief may be manifested in varying behaviors and intensities and may include denial, anger, depression, and other psychologic and physical symptoms.
Anticipatory guidance may assist grieving family members. Health care professionals should emphasize that grief reactions such as hearing the dead person’s voice, feeling distant from others, or seeking reassurance that they did everything possible for the lost person are normal, necessary, and expected. They in no way signify poor coping, insanity, or an approaching mental breakdown. On the contrary, such behaviors signify that the survivor is working through the acute grief. They are a necessary part of grief work. Anticipatory guidance regarding the mourning process may help families recognize the normalcy of their experiences.
It is important to recognize that some family members may experience complicated grief. Complicated grief reactions (more than a year after the loss) include such symptoms as intense intrusive thoughts, pangs of severe emotion, distressing yearnings, feelings of excessive loneliness and emptiness, unusual sleep disturbance, and maladaptive levels of loss of interest in personal activities (Horowitz, Siegel, Holen, and others, 1997). Bereaved persons experiencing such prolonged and complicated grief should be referred to an expert in grief and bereavement counseling.
Another important aspect of grief is the individual nature of the grief experience. Each member of the family will experience the grief of the child’s death in his or her own way based on the particular relationship with that child. This can create potential conflict for families, since each family member has expectations that the other family members should feel and grieve as they do. Nurses caring for families experiencing grief should be aware of the different grieving styles and help the family learn to recognize and support the uniqueness of each other’s grief.
Parental Grief
Parental grief after the death of a child has been found to be the most intense, complex, long-lasting, and fluctuating grief experience when compared with that of other bereaved individuals. Although parents experience the primary loss of their child, many secondary losses are felt such as the loss of part of one’s self, hopes and dreams for the child’s future, the family unit, prior social and emotional community supports, and often spousal support. It is common for parents of the same child to experience different grief reactions.
Studies with bereaved parents have shown that grieving does not end with the severing of the bond with the deceased child, but rather involves a continuing bond between the parent and the deceased child (Klass, 2001). Parental resolution of grief is a process of integrating the dead child into daily life where the pain of losing a child is never completely gone, but lessens. There are occasions of brief relapse, but not to the degree experienced when the loss initially occurred. Thus parental grief work is never completed and is a timeless process of accommodating the new reality of being without a child, as it changes over time (Davies, 2004). A child’s death can also challenge the marital relationship in several ways. Maternal and paternal reactions often differ (Birenbaum, Stewart, and Phillips, 1996; Moriarty, Carroll, and Cotroneo, 1996; Vance, Najman, Thearle, and others, 1995). Different grieving styles between the couple may hinder communication and support for each other. Differing needs and expectations can place a strain on the marriage.
Sibling Grief
Each child grieves in his or her own way and on his or her own timeline. Children, even adolescents, grieve differently than adults. Adults and children differ more widely in their reactions to death than in their reactions to any other phenomenon. Children of all ages grieve the loss of a loved one, and their understanding and reactions to death depend on their age and developmental level. Children grieve for a longer duration, revisiting their grief as they grow and develop new understandings of death. However, they do not grieve 100% of the time. They grieve in spurts and can be emotional and sad in one instance and then, just as quickly, off and playing. Children express their grief though play and behavior. Children can be exquisitely attuned to their parents’ grief and will try to protect them by not asking questions or by trying not to upset them. This can set the stage for the sibling to try to become the “perfect child.” Children exhibit many of the grief reactions of adults, including physical sensations and illnesses, anger, guilt, sadness, loneliness, withdrawal, acting out, seep disturbances, isolation, and search for meaning. Again, nurses should be attentive for signs that siblings are struggling with their grief and provide guidance to parents when possible.
At times family members may need assistance in their grieving (see Nursing Care Guidelines box). Communication with the bereaved family is essential, but often nurses do not know what to say and feel helpless in offering words of comfort. The most supportive approach is to avoid judging the family’s reactions or offering advice or rationalizations and to focus on feelings. Perhaps the most valuable supportive measure the nurse can perform for families is to listen. Families understand that no words will relieve their pain; all they want is acceptance, understanding, and respect for their grief.
It is important for families to understand that mourning takes a long time. Whereas acute grief may last only weeks or months, resolving the loss is measured in years. Holidays and anniversaries can be particularly difficult, and people who previously had been supportive may now expect the family to have “adjusted.” Consequently, prolonged mourning is often silent and lonely.
Many families never receive the support and guidance that could help them resolve the loss. A plan for regular follow-up with bereaved families can be beneficial. At minimum, one follow-up phone call or meeting with the family should be arranged. Families can also be referred to self-help groups. When such groups are not available, nurses can be instrumental in bringing families together or facilitating parent and sibling groups. Formal bereavement programs or bereavement counseling can be helpful as well.
For more information on end-of-life care, visit these websites:
Americans for Better Care of the Dying—http://www.abcd-caring.org
End-of-Life/Palliative Education Resource Center—http://www.eperc.mcw.edu
Growth House—http://www.growthhouse.org
Robert Wood Johnson Foundation—http://www.rwjf.org
NURSES’ REACTIONS TO CARING FOR DYING CHILDREN
The death of a patient is one of the most stressful aspects of critical care or oncology nursing (see Family Focus box).* Nurses experience reactions to a fatal illness that are very similar to the responses of family members, including denial, anger, depression, guilt, and ambivalent feelings.
Strategies that can assist the nurse in maintaining the ability to work effectively in these settings include maintaining good general health, developing well-rounded interests, using distancing techniques such as taking time off when needed, developing and using professional and personal support systems, cultivating the capacity for empathy, focusing on the positive aspects of the caregiver role, and basing nursing interventions on sound theory and empiric observations. Attending shared-remembrance rituals assists some nurses in resolving grief (Davis and Eng, 1998). Similarly, attending the funeral services can be a supportive act for both the family and the nurse and in no way detracts from the professionalism of care.
References
Ahmann, E. “Chunky stew”: appreciating cultural diversity while providing health care for children. Pediatr Nurs. 1994;20(3):320–324.
American Academy of Pediatrics. Committee on Hospital Care and Section on Surgery: Pediatric organ donation and transplantation. Pediatrics. 2002;109(5):982–984.
American Nurses Association. Code of ethics for nurses with interpretive statements. Washington, DC: ANA Publishing, 2001.
Anderson, RN, Smith, BL. Deaths: leading causes. Natl Vital Stat Rep. 2005;53(17):1–89.
Arias, E, MacDorman, MF, Strobino, DM, et al. Annual summary of vital statistics—2002. Pediatrics. 2003;112(6):1215–1230.
Barlow, JH, Ellard, DR. The psychosocial well-being of children with chronic disease, their parents and siblings: an overview of the research evidence base. Child Care Health Dev. 2006;32(1):19–31.
Birenbaum, LK, Stewart, BJ, Phillips, DS. Health status of bereaved parents. Nurs Res. 1996;45(2):105–109.
Carnevale, FA, Alexander, E, Davis, M, et al. Daily living with distress and enrichment: the moral experience of families with ventilator-assisted children at home. Pediatrics. 2006;117(1):e48–60.
Carter, B. Chronic pain in childhood and the medical encounter: professional ventriloquism and hidden voices. Qual Health Res. 2002;12:28–41.
Charles, C, Gafni, A, Whelan, T. Shared decision making in the medical encounter: what does it mean? Soc Sci Med. 1997;44:681–692.
Clements, PT, Vigil, GJ, Manno, MS, et al. Cultural perspectives of death, grief, and bereavement. J Psychosoc Nurs Ment Health Serv. 2003;41(7):18–26.
Coffey, JS. Parenting a child with chronic illness: a metasynthesis. Pediatr Nurs. 2006;32(1):51–59.
Cohen, MH. The stages of the prediagnostic period in chronic life-threatening childhood illness: a process analysis. Res Nurs Health. 1995;18(1):39–48.
Corlett, J, Twycross, A. Negotiation of parental roles within family-centered care: a review of the research. J Clin Nurs. 2006;15(10):1308–1316.
Davies, B, Gudmundsdottir, M, Worden, B, et al. “Living in the dragon’s shadow”: fathers’ experiences of a child’s life-limiting illness. Death Studies. 2004;28(2):111–135.
Davies, R. New understandings of parental grief: literature review. J Adv Nurs. 2004;46(5):506–513.
Davies, R, Davis, B, Sibert, J. Parents’ stories of sensitive and insensitive care by paediatricians in the time leading up to and including diagnostic disclosure of a life-limiting condition in their child. Child Care Health Dev. 2003;29(1):77–82.
Davis, B, Eng, B. Special issues in bereavement and staff support. In Doyle D, Hanks GWC, MacDonald N, eds.: Oxford textbook of palliative medicine, ed 2, Oxford: Oxford University Press, 1998.
Deatrick, JA, Knafl, KA, Murphy-Moore, C. Clarifying the concept of normalization. Image J Nurs Sch. 1999;31:209–214.
Denboba, D, McPherson, MG, Kenney, MK, et al. Achieving family and provider partnerships for children with special health care needs. Pediatrics. 2006;118(4):1607–1615.
Dixon-Woods, M, Young, B, Henry, D. Partnerships with children. Br J Med. 1999;319:778–780.
Evanisko, MJ, Beasley, CL, Brigham, LE, et al. Readiness of critical care physicians and nurses to handle requests for organ donation. Am J Crit Care. 1998;7(1):4–12.
Faulkner, KW, Armstrong-Dailey, A. Care of the dying child. In: Pizzo PA, Poplack DG, eds. Principles and practice of pediatric oncology. Philadelphia: Lippincott-Raven, 1997.
Field MJ, Behrman RE, eds. When children die: improving palliative and end-of-life care for children and their families. Washington, DC: National Academies Press, 2004.
Fleitas, J. When Jack fell down … Jill came tumbling after: siblings in the web of illness and disability. MCN. 2000;25:267–273.
Forrester, L. One to one care in children’s hospice. Nurs Times. 2003;99(16):44–45.
Franz, HG, DeJong, W, Wolfe, SM, et al. Explaining brain death: a critical feature of the donation process. J Transplant Coord. 1997;7(1):14–21.
Freyer, DR. Care of the dying adolescent: special considerations. Pediatrics. 2004;113(2):381–388.
Garwick, AW, Patterson, J, Bennett, FC, et al. Breaking the news: how families first learn about their child’s chronic condition. Arch Pediatr Adolesc Med. 1995;149(9):991–997.
Goldbeck, L. Parental coping with the diagnosis of childhood cancer: gender effects, dissimilarity within couples, and quality of life. Psychooncology. 2001;10:325–335.
Goodenough, B, Drew, D, Higgins, S, et al. Bereavement outcomes for parents who lose a child to cancer: are place of death and sex of parent associated with differences in psychological functioning? Psycho-Oncology. 2004;13(11):779–791.
Gravelle, AM. Caring for a child with a progressive illness during the complex chronic phase: parents’ experience of facing adversity. J Adv Nurs. 1997;25:738–745.
Hawryluck, LA, Harvey, WR. Analgesia, virtue, and the principle of double effect. J Palliative Care. 2000;16(Suppl):S24–S30.
Hellsten, MB, Hockenberry, M, Lamb, D, et al. End-of-life care for children. Austin, Tex: Texas Cancer Council, 2000.
Hinds, PS, Oakes, L, Furman, W, et al. End-of-life decision making by adolescents, parents, and healthcare providers in pediatric oncology: research to evidence-based practice guidelines. Cancer Nurs. 2001;24:122–134.
Horowitz, MJ, Siegel, B, Holen, A, et al. Diagnostic criteria for complicated grief disorder. Am J Psychiatry. 1997;154(7):904–910.
Immelt, S. Psychological adjustment in young children with chronic medical conditions. J Pediatr Nurs. 2006;21(5):362–377.
Jackson, PL. The primary care provider and children with chronic conditions. In Jackson PL, Vessey PA, eds.: Primary care of the child with a chronic condition, ed 3, St Louis: Mosby, 2000.
James, L, Johnson, B. The needs of parents of pediatric oncology patients during the palliative care phase. J Pediatr Oncol Nurs. 1997;14(2):83–95.
Jennings, PD. Providing pediatric palliative care through a pediatric supportive care team. Pediatr Nurs. 2005;31(3):195–200.
Jokinen, P. The family life-path theory: a tool for nurses working in partnership with families. J Child Health Care. 2004;8(2):124–133.
Klass, D. The inner representation of the dead child in the psychic and social narratives of bereaved parents. In: Neimeyer RA, ed. Meaning reconstruction and the experience of loss. Washington, DC: American Psychological Association, 2001.
Lambert, S. Distraction, imagery, and hypnosis techniques for management of children’s pain. J Child Fam Nurs. 1999;2(1):5–15.
Lauer, ME, Mulhern, RK, Schell, MJ, et al. Long-term follow-up of parental adjustment following a child’s death at home or hospital. Cancer. 1989;63(5):988–994.
Lobato, DJ, Kao, BT. Integrated sibling-parent group intervention to improve sibling knowledge and adjustment to chronic illness and disability. J Pediatr Psychol. 2002;27:711–716.
Lobato, DJ, Kao, BT, Plante, W. Latino sibling knowledge and adjustment to chronic illness. J Fam Psychol. 2005;19(4):625–632.
Marshall, ES, Olsen, SF, Mandleco, BL, et al. “This is a spiritual experience”: perspectives of Latter-Day Saint families living with a child with disabilities. Qual Health Res. 2003;13:57–76.
Masri, C, Farrell, CA, Lacroix, J, et al. Decision making and end-of-life care in critically ill children. J Palliative Care. 2000;16(Suppl):S45–S52.
Mastroyannopoulou, K, Stallard, P, Lewis, M, et al. The impact of childhood non-malignant life threatening illness on parents: gender differences and predictors of parental adjustment. J Child Psychol Psychiatry. 1997;38(7):823–829.
McDougal, J. Promoting normalization in families with preschool children with type 1 diabetes. J Specialty Pediatr Nurs. 2002;7(3):113–120.
McPherson, M, Weissman, G, Strickland, BB, et al. Implementing community-based systems of services for child and youths with special health care needs: how well are we doing? Pediatrics. 2004;113(5):1538–1544.
Moriarty, H, Carroll, R, Cotroneo, M. Differences in bereavement reactions within couples following the death of a child. Res Nurs Health. 1996;19:461–469.
Morse, JM, Wilson, S, Penrod, J. Mothers and their disabled children: refining the concept of normalization. Health Care Woman Int. 2000;21(8):659–676.
Msall, ME, Avery, RC, Tremont, MR, et al. Functional disability and school activity limitations in 41,300 school-age children: relationship to medical impairments. Pediatrics. 2003;111:548–553.
Murray, JS. Siblings of children with cancer: a review of the literature. J Pediatr Oncol Nurs. 1999;16(1):25–34.
Nelson, AM. A metasynthesis: mothering other-than-normal children. Qual Health Res. 2002;12:515–530.
Newacheck, PW, Halfon, N. Prevalence and impact of disabling chronic conditions in childhood. Am J Public Health. 1998;88(4):610–617.
Newacheck, PW, Strickland, B, Shonkoff, JP, et al. An epidemiologic profile of children with special health care needs. Pediatrics. 1998;102(1):117–123.
Nuutila, L, Salanterä, S. Children with a long-term illness: parents’ experiences of care. J Pediatr Nurs. 2006;21(2):153–160.
O’Brien, ME, Wegner, CB. Rearing the child who is technology dependent: perceptions of parents and home care nurses. J Spec Pediatr Nurs. 2002;7:7–15.
Ochieng, BM. Minority ethnic families and family-centered care. J Child Health Care. 2003;7(2):123–132.
Palfrey, JS, Tonniges, TF, Green, M, et al. Introduction: addressing the millennial morbidity—the context of community pediatrics. Pediatrics. 2005;115(4 Suppl):1121–1123.
Perrin, JM. Chronic illness in childhood. In Behrman RE, Kleigman RM, Jensen HB, eds.: Nelson textbook of pediatrics, ed 17, Philadelphia: Saunders, 2004.
Pierucci, RL, Kirby, RS, Leuthner, SR. End-of-life for neonates and infants: the experience and effects of a palliative care consultation service. Pediatrics. 2001;108(3):653–660.
Raina, P, O’Donnell, M, Rosenbaum, P, et al. The health and well-being of caregivers of children with cerebral palsy. Pediatrics. 2005;115(6):e626–e636.
Ray, LD. Parenting and childhood chronicity: making visible the invisible work. J Pediatr Nurs. 2002;17(6):424–438.
Rehm, RS. Religious faith in Mexican-American families dealing with chronic childhood illness. Image J Nurs Sch. 1999;31:33–38.
Ritchie, MA. Self-esteem and hopefulness in adolescents with cancer. J Pediatr Nurs. 2001;16:35–42.
Rossiter, L, Sharpe, D. The siblings of individuals with mental retardation: a quantitative integration of the literature. J Child Fam Studies. 2001;10(1):65–84.
Rousseau, P. Ethical and legal issues in palliative care. Prim Care. 2001;28:391–400.
Sahler, O, Frager, G, Levetown, M, et al. Medical education about end-of-life care in the pediatric setting: principles, challenges, and opportunities. Pediatrics. 2000;105:575–584.
Schor, EL. Family pediatrics: report of the Task Force on the Family. Pediatrics. 2003;111:1541–1571.
Sharpe, D, Rossiter, L. Siblings of children with a chronic illness: a meta-analysis. J Pediatr Psychol. 2002;27:699–710.
Shepard, MP, Mahon, MM. Chronic conditions and the family. In Jackson PL, Vessey JA, eds.: Primary care of the child with a chronic condition, ed 3, St Louis: Mosby, 2000.
Sine, D, Sumner, L, Gracy, D, et al. Pediatric extubation: “pulling the tube,”. J Palliative Med. 2001;4:519–524.
Stein, REK. Home care: a challenging opportunity. Child Health Care. 1985;14(2):90–95.
Sterling, YM, Peterson, JW. Characteristics of African American women caregivers of children with asthma. MCN. 2003;28:32–38.
Sullivan-Bolyai, S, Sadler, L, Knafl, KA, et al. Great expectations: a position description for parents as caregivers, part I. Pediatr Nurs. 2003;29(6):52–56.
Sumner, LH. Lighting the way: improving the way children die in America. Caring. 2003;22:14–18.
Swallow, VM, Jacoby, A. Mothers’ evolving relationships with doctors and nurses during the chronic childhood illness trajectory. J Adv Nurs. 2001;36:755–764.
Thomlinson, EH. The lived experience of families of children who are failing to thrive. J Adv Nurs. 2002;39:537–545.
Tong, H, Kandala, G, Haig, AJ, et al. Physical functioning in female caregivers of children with physical disabilities compared with female caregivers of children with a chronic medical condition. Arch Pediatr Adolesc Med. 2002;156:1138–1142.
Vance, JC, Najman, JM, Thearle, MJ, et al. Psychological changes in parents eight months after the loss of an infant from stillbirth, neonatal death, or sudden infant death syndrome—a longitudinal study. Pediatrics. 1995;96(5):933–938.
Van Dyck, P, Kogan, MD, Heppel, D, et al. The national survey of children’s health: a new data resource. Matern Child Health J. 2004;8(3):183–188.
Van Dyck, PC, Kogan, MD, McPherson, MG, et al. Prevalence and characteristics of children with special health care needs. Arch Pediatr Adolesc Med. 2004;158(9):884–890.
Whitehead, LC, Gosling, V. Parent’s perceptions of interactions with health professionals in the pathway to gaining a diagnosis of tuberous sclerosis (TS) and beyond. Res Dev Disabil. 2003;24:109–119.
Winkler, WD, Mardegian, CA. Completing the continuum of care: the growth of a pediatric hospice program. Caring. 2001;20:22–25.
Wise, PH, Wampler, NS, Chavkin, W, et al. Chronic illness among poor children enrolled in the temporary assistance for needy families program. Am J Public Health. 2002;92:1458–1461.
Wolfe, J, Friebert, S, Hilden, J. Caring for children with advanced cancer integrating palliative care. Pediatr Clin North Am. 2002;49(5):1043–1062.
Wolfe, J, Grier, HE, Klar, N, et al. Symptoms and suffering at the end of life in children with cancer. N Engl J Med. 2000;342(5):326–333.
Wood, PR, Smith, LA, Romero, D, et al. Relationships between welfare status, health insurance status, and health and medical care among children with asthma. Am J Public Health. 2002;92:1446–1452.
World Health Organization. Cancer pain relief and palliative care. Geneva: The Organization, 1996.
Yogev, R, Chadwick, EG. Acquired immunodeficiency syndrome. In Behrman RE, Kleigman RM, Jensen HB, eds.: Nelson textbook of pediatrics, ed 17, Philadelphia: Saunders, 2004.
Young, B, Dixon-Woods, M, Windridge, KC, et al. Managing communication with young people who have a potentially life threatening chronic illness: qualitative study of patients and parents. BJM. 2003;326(7384):305.
Zuvekas, SH, Taliaferro, GS. Pathways to access: health, insurance, the health care delivery system and racial/ethnic disparities, 1996-1999. Health Affairs. 2003;22(2):139–153.
*Information regarding financial issues is available from the Federation for Children with Special Needs, 1135 Tremont St., Suite 420, Boston, MA 02120; (617) 236-7210; http://www.fcsn.org.
*General sources of information are the Clearinghouse on Disability Information, 550 12th St. SW, Room 5133, Washington, DC 20202-2550; (202) 245-7307; http://www.ed.gov; National Dissemination Center for Children with Disabilities, PO Box 1492, Washington, DC 20013; (202) 884-8411 or (800) 695-0285; http://www.nichcy.org. A comprehensive list of books and pamphlets for parents and teachers is available from the Easter Seals, 230 W. Monroe St., Suite 1800, Chicago, IL 60606; (312) 726-6200; http://www.easterseals.com. In Canada: Council of Canadians with Disabilities, 926-294 Portage Ave., Winnipeg, Manitoba R3C 0B9; (204) 947-0303; http://www.ccdonline.ca.
*Information about self-help groups and books and pamphlets are available from the National Self-Help Clearinghouse, 365 Fifth Ave., Suite 3300, New York, NY 10016; (217) 817-1822; http://www.selfhelpweb.org.
*Information on car safety restraints for children with special needs is available from the Automotive Safety Program, 575 West Drive, Room 004, Indianapolis, IN 46202; (800) 543-6227 or (317) 274-2997; http://www.preventinjury.org.
†MedicAlert Foundation International, 2323 Colorado Ave., Turlock, CA 95382; (888) 633-4298; http://www.medicalert.org.
*1133 19th St. NW, Washington, DC 20036; (202) 628-3630; http://www.specialolympics.org
†A directory of private/paying camps for children with a variety of chronic illnesses or general physical disabilities is available from the American Camp Association, 5000 State Road 67 North, Martinsville, IN 46151-7902; (765) 342-8456; http://www.acacamps.org
*VSA Arts has affiliate chapters in all 50 states and in selected sites internationally; yearly festivals are held throughout the world. Information is available from VSA Arts, 818 Connecticut Avenue NW, Suite 600, Washington, DC 20006; (202) 628-2800 or (800) 933-8721; http://www.vsarts.org
*For more information, contact National Hospice and Palliative Care Organization, 1700 Diagonal Road, Suite 625, Alexandria, VA 22314; (703) 837-1500; fax: (703) 837-1233; http://www.nho.org; and Children’s Hospice International, 1101 King St., Suite 360, Alexandria, VA 22314; (703) 684-0330 or (800) 24-CHILD; http://www.chionline.org.
*Other sources of publications on life-threatening illness and death are the Compassionate Friends, PO Box 3696, Oak Brook, IL 60522-3696; (630) 990-0010 or (877) 969-0010; http://www.compassionatefriends.org; Centering Corporation, 7230 Maple St., Omaha, NE 68134; (866) 218-0101; http://www.centering.org; Children’s Hospice International, 1104 King St., Suite 360, Alexandria, VA 22314; (800) 24-CHILD or (703) 684-0330; e-mail: info@chionline.org; http://www.chionline.org; and National Cancer Institute, Cancer Information Service, Building 21, Room 10A29, Bethesda, MD 20892-2580; (800) 422-6237; http://www.cancer.gov.
 IN TEXT
IN TEXT FAMILY FOCUS
FAMILY FOCUS