The Child with Respiratory Dysfunction
UPPER RESPIRATORY TRACT INFECTIONS
INFECTIONS OF THE LOWER AIRWAYS
OTHER INFECTIONS OF THE RESPIRATORY TRACT
PULMONARY DYSFUNCTION CAUSED BY NONINFECTIOUS IRRITANTS
On completion of this chapter the reader will be able to:
 Identify the factors leading to respiratory tract infection in the infant or young child.
Identify the factors leading to respiratory tract infection in the infant or young child.
 Contrast the effects of various respiratory infections observed in infants and children.
Contrast the effects of various respiratory infections observed in infants and children.
 Describe the postoperative nursing care of the child with a tonsillectomy.
Describe the postoperative nursing care of the child with a tonsillectomy.
 Outline a nursing care plan for a child with croup.
Outline a nursing care plan for a child with croup.
 Describe priorities of nursing care for the child with acute otitis media.
Describe priorities of nursing care for the child with acute otitis media.
 Identify priorities of nursing care for the infant with respiratory syncytial virus bronchiolitis.
Identify priorities of nursing care for the infant with respiratory syncytial virus bronchiolitis.
 Describe the various therapeutic measures to relieve the symptoms of asthma.
Describe the various therapeutic measures to relieve the symptoms of asthma.
 Outline a plan for teaching home care management of the child with asthma.
Outline a plan for teaching home care management of the child with asthma.
 Describe the physiologic effects of cystic fibrosis on the gastrointestinal and pulmonary systems.
Describe the physiologic effects of cystic fibrosis on the gastrointestinal and pulmonary systems.
 Outline a care plan for the child with cystic fibrosis.
Outline a care plan for the child with cystic fibrosis.
 List the major signs of respiratory distress in infants and children.
List the major signs of respiratory distress in infants and children.
 Describe emergent procedures for the relief of foreign body obstruction in an infant or child.
Describe emergent procedures for the relief of foreign body obstruction in an infant or child.
RESPIRATORY INFECTION
Infections of the respiratory tract are described according to the anatomic area of involvement. The upper respiratory tract, or upper airway, consists of the oronasopharynx, the pharynx, the larynx, and the upper part of the trachea. The lower respiratory tract consists of the lower trachea, mainstem bronchi, segmental bronchi, subsegmental bronchioles, terminal bronchioles, and alveoli. In this discussion, the trachea is considered with lower tract disorders, and infections of the epiglottis and larynx are categorized as croup syndromes. However, respiratory infections seldom fall into discrete anatomic areas. Infections often spread from one structure to another because of the contiguous nature of the mucous membrane lining the entire tract. Consequently, respiratory tract infections involve several areas rather than a single structure, although the effect on one area may predominate in any given illness.
Etiology and Characteristics
Respiratory tract infections account for the majority of acute illnesses in children. The etiology and course of these infections are influenced by the age of the child, the season, living conditions, and preexisting medical problems.
Infectious Agents.: The respiratory tract is subject to a wide variety of infective organisms. Most infections are caused by viruses, particularly respiratory syncytial virus (RSV), nonpolio enteroviruses (coxsackieviruses A and B), adenoviruses, parainfluenza viruses, and human metapneumoviruses. Other agents involved in primary or secondary invasion include group A b-hemolytic streptococci (GABHS), staphylococci, Haemophilus influenzae, Chlamydia trachomatis, Mycoplasma organisms, and pneumococci.
Age.: Healthy full-term infants under age 3 months are presumed to have a lower infection rate than older infants because of the protective function of maternal antibodies; however, infants may be susceptible to specific respiratory tract infections, namely pertussis, during this period. The infection rate increases from 3 to 6 months of age, the time between the disappearance of maternal antibodies and the infant’s own antibody production. The viral infection rate remains high during the toddler and preschool years. By 5 years of age, viral respiratory tract infections are less frequent, but the incidence of Mycoplasma pneumoniae and GABHS infections increases. The amount of lymphoid tissue increases throughout middle childhood, and repeated exposure to organisms confers increasing immunity as children grow older.
Some viral agents produce a mild illness in older children but severe lower respiratory tract illness or croup in infants. For example, pertussis causes a relatively harmless tracheobronchitis in childhood but is a serious disease in infancy.
Size.: Anatomic differences influence the response to respiratory tract infections. The diameter of the airways is smaller in young children and subject to considerable narrowing from edematous mucous membranes and increased production of secretions. The distance between structures within the respiratory tract is also shorter in the young child, and organisms may move rapidly down the respiratory tract, causing more extensive involvement. The relatively short and open eustachian tube in infants and young children allows pathogens easy access to the middle ear.
Resistance.: The ability to resist pathogens depends on several factors. Deficiencies of the immune system place the child at risk for infection. Other conditions that decrease resistance are malnutrition, anemia, fatigue, and chilling of the body. Conditions that weaken defenses of the respiratory tract and predispose children to infection also include allergies (e.g., allergic rhinitis), preterm birth, bronchopulmonary dysplasia (BPD), asthma, history of RSV infection, cardiac anomalies that cause pulmonary congestion, and cystic fibrosis (CF). Daycare attendance, especially if the caregivers smoke, increases the likelihood of infection.
Seasonal Variations.: The most common respiratory pathogens appear in epidemics during the winter and spring months. Mycoplasmal infections occur more often in autumn and early winter. Infection-related asthma (e.g., bronchitis) occurs more frequently during cold weather, whereas winter and early spring are typically the “RSV season.”
Clinical Manifestations
Infants and young children, especially those between 6 months and 3 years of age, react more severely to acute respiratory tract infection than older children. Young children display a number of generalized signs and symptoms, as well as local manifestations (Box 23-1).
Nursing Care Management
Assessment of the respiratory system follows the guidelines described in Chapter 6 (for assessment of the ears, nose, mouth and throat, chest, and lungs). Special attention should also be given to the components and observations listed in Box 23-2. The nursing process in the care of the child with acute respiratory tract infection is outlined in the Nursing Process box.
Ease Respiratory Efforts.: Many acute respiratory tract infections are mild and cause few symptoms. Although children may feel uncomfortable and have a “stuffy” nose and some mucosal swelling, respiratory distress occurs infrequently. Interventions delivered at home are usually sufficient to relieve minor discomfort and ease respiratory efforts. However, in some cases the infant or child may require close observation by health professionals for adequate oxygenation and fluid and electrolyte status.
Warm or cool mist is a common therapeutic measure for symptomatic relief of respiratory discomfort. The moisture soothes inflamed membranes and is beneficial when there is hoarseness or laryngeal involvement. Mist tents are sometimes used in the hospital for humidifying the air and relieving discomfort. The use of steam vaporizers in the home is often discouraged because of the hazards related to their use and limited evidence to support their efficacy. Shallow pans with wide surface areas for evaporation increase humidity, but they should be placed where they do not pose a safety hazard.
A time-honored method (albeit not evidence based!) of producing steam is the shower. Running a shower of hot water into the empty bathtub or open shower stall with the bathroom door closed produces a quick source of steam. Keeping a child in this environment for approximately 10 to 15 minutes offers the same advantages as the mist tent without the fear and restraint often associated with the confines of a tent. A small child can be held on the lap of a parent or other adult. Older children can sit in the bathroom under the supervision of an adult.
Promote Rest.: Children who have an acute febrile illness should have limited activity or be placed on bed rest. This is usually not difficult while the temperature is elevated but may become a problem when children begin to feel better. In fact, one of the cardinal signs that the child is feeling better is the increase in activity; this may, however, be temporary if a high fever returns after a few hours of increased activity. Often children will comply with bed rest if they are allowed to lie quietly on a couch where they can watch television, play video games, or participate in a quiet activity. If children protest, allowing them to play quietly serves the purpose of rest better than allowing them to cry in bed.
Promote Comfort.: Older children are usually able to manage nasal secretions with little difficulty. Parents are instructed in the correct administration of nose drops. For very young infants, who normally breathe through their noses, an infant nasal aspirator or a bulb syringe is helpful in removing nasal secretions, especially before being put to bed to sleep and before feeding. This practice, preceded by instillation of saline nose drops, may clear nasal passages and promote feeding. Saline nose drops can be prepared at home by dissolving 1 teaspoon of salt in 1 pint of warm water.
For older infants and children who can tolerate decongestants, vasoconstrictive nose drops may be administered 15 to 20 minutes before feeding and at bedtime. Two drops are instilled, and because this shrinks only the anterior mucous membranes, two more drops are instilled 5 to 10 minutes later. Older cooperative children often prefer nasal sprays. They are taught to compress the plastic container at the moment of inspiration. Bottles of nose drops should be used for only for one child and one illness because they are easily contaminated with bacteria. To avoid rebound congestion, nose drops or sprays should not be administered for more than 3 days. To prevent cross-contamination with nose drops, draw about 0.25 ml of nose spray solution into a clean tuberculin syringe. Inject a small amount of the nose spray solution into the child’s nostrils using the blunt syringe.
Hot or cold applications sometimes provide relief for children with painful cervical adenitis. An ice bag or heating pad applied to the neck may decrease the discomfort, but safety precautions must be observed to prevent burns. The ice bag or heating device must be covered, and the heating pad should not be set at high ranges.
Prevent Spread of Infection.: Children and families are taught to use a tissue or their hand to cover their nose and mouth when they cough or sneeze and to dispose of tissues properly, as well as to wash their hands. Remembering to cover the nose or mouth is often difficult for toddlers; therefore frequent hand washing is encouraged to prevent the spread of infection. Used tissues should be immediately thrown into the wastebasket or a special plastic or paper bag, which can be discarded when full. Children with respiratory tract infections should not share drinking cups, washcloths, or hand or face towels. To avoid contamination with respiratory viruses, wash hands and do not touch (rub) your eyes or nose. Careful handwashing is key in the prevention of childhood respiratory tract infections.
Efforts should be made to separate affected children from contact with other children. Parents should keep affected children out of school and daycare settings to prevent the spread of infection. Ideally, ill children should be isolated in a separate bedroom at the first sign of illness. However, this is a problem in households with more than one child. Well children should be told to stay away from ill children.
Reduce Body Temperature.: If the child has a significantly elevated body temperature, controlling the fever is important. Parents should know how to take a child’s temperature and read the thermometer accurately. Nurses should not assume that all parents can read a thermometer. Parents who cannot perform this skill should receive instruction.
If the practitioner prescribes acetaminophen or ibuprofen, parents may need help giving the drug. Most parents can read the label and calculate the desired dosage, but some may require detailed instruction. It is important to emphasize accuracy in determining both the amount of drug to be given and the time intervals for administration.
Cool liquids are given to reduce the temperature and minimize the chances of dehydration (see Controlling Elevated Temperatures, Chapter 22).
Promote Hydration.: Dehydration is a potential complication when children have respiratory tract infections and are febrile or anorexic, especially when vomiting or diarrhea is present. Infants are especially prone to fluid and electrolyte deficits when they have a respiratory illness because a rapid respiratory rate that accompanies such illnesses precludes adequate oral fluid intake. In addition, the presence of fever increases the total body fluid turnover in infants. If the infant has nasal secretions, this further prevents adequate respiratory effort by blocking the narrow nasal passages when the infant reclines to bottle-feed or breastfeed and ceases the compensatory mouth breathing effort, thus causing the child to limit intake of fluids. Adequate fluid intake is encouraged by offering small amounts of favorite fluids (clear liquids if vomiting) at frequent intervals. Oral rehydration solutions, such as Infalyte or Pedialyte, should be considered for infants, and sports drinks, such as Gatorade, should be considered for older children. Fluids with caffeine (tea, coffee) are avoided because these may act as diuretics and promote fluid loss. Breastfeeding infants should continue to be breastfed, since human milk confers some degree of protection from infection (see Chapter 8). Fluids should not be forced, and children should not be awakened to take fluids. Forcing fluids creates the same problem as urging unwanted food. Gentle persuasion with preferred beverages or sugar-free popsicles is usually more successful.
To assess their child’s level of hydration (see Chapters 9 and 24), parents are advised to observe the frequency of voiding and to notify the nurse or practitioner if there is insufficient voiding. Counting the number of wet diapers in a 24-hour period is a satisfactory method to assess output in infants and toddlers.
Provide Nutrition.: Loss of appetite is characteristic of children with acute infections. In most cases, children can be permitted to determine their own need for food. Many children show no decrease in appetite, and others respond well to foods such as gelatin, popsicles, and soup (see Feeding the Sick Child, Chapter 22). Urging solid foods on children who are sick may precipitate nausea and vomiting and cause an aversion to feeding that may extend into the convalescent period and beyond.
Family Support and Home Care.: Young children with respiratory tract infections are irritable and difficult to comfort; therefore the family needs support, encouragement, and practical suggestions concerning comfort measures and administration of medication. In addition to antipyretics and nose drops, the child may require antibiotic therapy. Parents of children receiving oral antibiotics must understand the importance of regular administration and of continuing the drug for the prescribed length of time, regardless of whether the child appears ill. Parents are cautioned against giving their child any medications that are not approved by the health practitioner and are cautioned to avoid giving antibiotics left over from a previous illness or prescribed for another child. Administering unprescribed antibiotics can produce serious side effects and adverse reactions (see Chapter 22 for administration of medications and teaching parents). See also Nursing Care Plan.
UPPER RESPIRATORY TRACT INFECTIONS
Acute nasopharyngitis, or the equivalent of the “common cold,” is caused by the rhinovirus, RSV, adenovirus, influenza virus, and parainfluenza virus. Symptoms are more severe in infants and children than in adults. Fever is common in young children, and older children have low-grade fevers, which appear early in the course of the illness. Other clinical manifestations are listed in Box 23-3.
Therapeutic Management
Children with nasopharyngitis are managed at home. There is no specific treatment, and effective vaccines are not available. Antipyretics are prescribed for mild fever and discomfort (see Chapter 22 for management of fever). Rest is recommended until the child is free of fever for at least 1 day. The provision of a humidified environment and increasing oral fluids may be beneficial to some children with a cold. Decongestants may be prescribed for children and infants older than 6 months of age to shrink swollen nasal passages. The decongestants that exert their effect by vasoconstriction are usually less effective when taken orally than when applied topically as nose drops.
Cough suppressants containing dextromethorphan may be prescribed for a dry, hacking cough in older children. However, cough preparations can cause adverse effects such as confusion, hyperexcitability, and sedation; therefore parents should monitor the child carefully for potential adverse effects.
Antihistamines are largely ineffective in treatment of nasopharyngitis. These drugs have a weak atropine-like effect that dries secretions, but they can cause drowsiness or, paradoxically, have a stimulatory effect on children. There is no support for the usefulness of expectorants, and antibiotics are usually not indicated because most infections are viral.
Prevention.: Nasopharyngitis is so widespread in the general population that it is impossible to prevent. Children are more susceptible because they have not yet developed resistance to many viruses. Young infants and those with decreased resistance and pulmonary illness are subject to serious complications such as pneumonia, and attempts should be made to protect them from exposure.
Nursing Care Management
A cold is often the parents’ first introduction to an illness in their infant. Most discomfort of nasopharyngitis is related to the nasal obstruction, especially in small infants. Elevating the head of the bed or crib mattress assists with drainage of secretions. Suctioning and vaporization may also provide relief. Saline nose drops and gentle suction with a bulb syringe before feeding and sleep time is useful.
Maintaining adequate fluid intake is essential. Although a child’s appetite for solid foods is usually diminished for several days, it is important to offer favorite fluids to prevent dehydration. Fluids can be cool or warm, depending on individual preference.
Because nasopharyngitis is spread from secretions, the best means for prevention is avoiding contact with affected persons. This goal is difficult to accomplish in family settings, classrooms, and daycare centers. Family members with a cold should try to “keep it to themselves” by carefully disposing of tissues; not sharing towels, glasses, or eating utensils; covering the mouth and nose with tissues when coughing or sneezing; and washing the hands thoroughly after nose blowing or sneezing. The most frequent carriers of infection are the human hands, which deposit viruses on doorknobs, faucets, and other everyday objects. Children should be taught to wash their hands thoroughly and avoid touching their eyes, nose, or mouth.
Family Support.: Support and reassurance are important elements of care for families of young children with recurrent upper respiratory infections (URIs). Because URIs are frequent in children less than 3 years of age, families may feel they are on an endless roller coaster of illness. They need reassurance that frequent colds are a normal part of childhood and that by 5 years of age, their children will have developed immunity to many viruses. Parents who work outside the home should expect to take time off to care for ill children during the fall and winter months. When children spend time in daycare centers, their infection rate is higher than if they are cared for in the home. Parents should know the signs of respiratory complications and should notify a health professional if complications occur or the child does not improve within 2 or 3 days (Box 23-4).
PHARYNGITIS
Children who experience GABHS infection of the upper airway (strep throat) are at risk for rheumatic fever (RF), an inflammatory disease of the heart, joints, and central nervous system (see Chapter 25), and acute glomerulonephritis (AGN), an acute kidney infection (see Chapter 27). Permanent damage can result from these sequelae, especially RF.
Clinical Manifestations
GABHS infection is generally a relatively brief illness that varies in severity from subclinical (no symptoms) to severe toxicity. The onset is often abrupt and characterized by pharyngitis, headache, fever, and abdominal pain. The tonsils and pharynx may be inflamed and covered with exudate (Fig. 23-1), which usually appears by the second day of illness. However, streptococcal infections should be suspected in children older than 2 years of age who have pharyngitis without exudate. The tongue may appear edematous and red (strawberry tongue), and the child may have a characteristic erythematous fine sandpaper rash on the trunk, axillae, elbows, and groin; the uvula is edematous and red. Anterior cervical lymphadenopathy (in about 30% to 50% of cases) usually occurs early, and the nodes are often tender. Pain can be relatively mild to severe enough to make swallowing difficult. Clinical manifestations usually subside in 3 to 5 days unless complicated by sinusitis or parapharyngeal, peritonsillar, or retropharyngeal abscess. Nonsuppurative complications may appear after the onset of GABHS—AGN in about 10 days and RF in an average of 18 days.
Diagnostic Evaluation
Although 80% to 90% of all cases of acute pharyngitis are viral, a throat culture should be performed to rule out GABHS. Most streptococcal infections are short-term illnesses, and antibody responses appear later than symptoms and are useful only for retrospective diagnosis.
Rapid identification of GABHS with diagnostic test kits (rapid antigen detection test) is possible in the office or clinic setting. Because of the high specificity of these rapid tests, a positive test result generally does not require throat culture confirmation. However, the sensitivities of these kits vary considerably, and a confirmatory throat culture is recommended in patients who have a negative test result (American Academy of Pediatrics, 2006b).
Therapeutic Management
If streptococcal sore throat infection is present, oral penicillin is prescribed in a dose sufficient to control the acute local manifestations and to maintain an adequate level for at least 10 days to eliminate any organisms that might remain to initiate RF symptoms. Penicillin does not prevent the development of AGN in susceptible children; however, it may prevent the spread of a nephrogenic strain of GABHS to others in the family. Penicillin usually produces a prompt response within 24 hours. Patients who have a history of RF or who remain symptomatic after a full course of antibiotics may require a follow-up throat swab.
Intramuscular (IM) benzathine penicillin G is an appropriate therapy, but it is painful and is not the first choice for children. Oral erythromycin is indicated for children allergic to penicillin. Other antibiotics used to treat GABHS are azithromycin, clarithromycin, oral cephalosporins, amoxicillin, and amoxicillin with clavulanic acid (American Academy of Pediatrics, 2006b; Gerber, 2005).
Nursing Care Management
The nurse often obtains a throat swab for culture and instructs the parents about administering penicillin and analgesics as prescribed. Cold or warm compresses to the neck may provide relief. In children who can cooperate, warm saline gargles may offer relief of throat discomfort. Acetaminophen and ibuprofen may be effective in decreasing the throat pain; liquid preparations or chewable forms may be preferable because of the pain associated with swallowing. Pain may interfere with oral intake, and children should not be forced to eat, but fluid intake is essential. Cool liquids or ice chips are usually more acceptable than solids.
Special emphasis is placed on correct administration of oral medication and completion of the course of antibiotic therapy (see Administration of Medication, and Compliance, Chapter 22). If an injection is required, it must be administered deep into a large muscle mass (e.g., vastus lateralis or ventrogluteal muscle). To prevent pain, application of a topical anesthetic cream such as EMLA (an eutectic mix of lidocaine and prilocaine) or LMX 4 (4% lidocaine) over the injection site before the injection is helpful (see Administration of Medication: Intramuscular Administration, Chapter 22). Parents also need to be aware of residual tenderness at the injection site, which may cause the child to limp for a day or two. Local applications of heat are helpful in relieving this discomfort.
Children are considered infectious to others at the onset of symptoms and up to 24 hours after initiation of antibiotic therapy, but they should not return to school or daycare until they have been taking antibiotics for a full 24-hour period. Nurses should remind the children to discard their toothbrush and replace it with a new one after they have been taking antibiotics for 24 hours. Parents are cautioned to prevent other household members, especially if immunocompromised, from having close contact with the sick child and avoid sharing drinking or eating items.
If the child continues to have a high fever that does not respond to antipyretics, has an extremely sore throat, refuses liquids, and appears toxic 24 to 48 hours after starting antibiotics, further evaluation by the practitioner is recommended.
TONSILLITIS
The tonsils are masses of lymphoid tissue located in the pharyngeal cavity. They filter and protect the respiratory and alimentary tracts from invasion by pathogenic organisms and play a role in antibody formation. Although their size varies, children generally have much larger tonsils than adolescents or adults. This difference is thought to be a protective mechanism because young children are especially susceptible to URIs.
Pathophysiology
Several pairs of tonsils are part of a mass of lymphoid tissue encircling the nasal and oral pharynx, known as the Waldeyer tonsillar ring (Fig. 23-2). The palatine, or faucial, tonsils are located on either side of the oropharynx, behind and below the pillars of the fauces (opening from the mouth). A surface of the palatine tonsils is usually visible during oral examination. The palatine tonsils are those removed during tonsillectomy. The pharyngeal tonsils, also known as the adenoids, are located above the palatine tonsils on the posterior wall of the nasopharynx. Their proximity to the nares and eustachian tubes causes difficulties in instances of inflammation. The lingual tonsils are located at the base of the tongue. The tubal tonsils, found near the posterior nasopharyngeal opening of the eustachian tubes, are not part of the Waldeyer tonsillar ring.
Etiology
Tonsillitis often occurs with pharyngitis. The causative agent may be viral or bacterial. Because of the abundant lymphoid tissue and the frequency of URIs, tonsillitis is a common cause of illness in young children.
Clinical Manifestations
The manifestations of tonsillitis are caused by inflammation. As the palatine tonsils enlarge from edema, they may meet in the midline (kissing tonsils), obstructing the passage of air or food. The child has difficulty swallowing and breathing. When enlargement of the adenoids occurs, the space behind the posterior nares becomes blocked, making it difficult or impossible for air to pass from the nose to the throat. As a result, the child breathes through the mouth.
Therapeutic Management
Because tonsillitis is self-limiting, treatment of viral pharyngitis is symptomatic. Throat cultures positive for GABHS infection warrant antibiotic treatment. It is important to differentiate between viral and streptococcal infection in febrile exudative tonsillitis. Because most infections are of viral origin, early rapid tests can eliminate unnecessary antibiotic administration.
Tonsillectomy is the surgical removal of the palatine tonsils. Absolute indications for a tonsillectomy are malignancy, recurrent peritonsillar abscess, and airway obstruction. Adenoidectomy (the surgical removal of the adenoids) is recommended for children who have hypertrophied adenoids that obstruct nasal breathing; additional indications for adenoidectomy include recurrent adenoiditis and sinusitis, otitis media (OM) with effusion, airway obstruction and subsequent sleep-disordered breathing, and recurrent rhinorrhea (Benninger and Walner, 2007a). The American Academy of Otolaryngology—Head and Neck Surgery (2000) lists “3 or more infections of the tonsils or adenoids per year despite adequate medical therapy” as an indication for tonsillectomy or adenotonsillectomy. However, for some children the effectiveness of tonsillectomy or adenoidectomy is modest and may not justify the risk of surgery (van Staaij, van den Akker, Rover, and others, 2004). In practice, many physicians rely on individualized decision making and do not subscribe to an absolute set of eligibility criteria for these surgical procedures (Paradise, Bluestone, Colborn, and others, 2002). Contraindications to either tonsillectomy or adenoidectomy are (1) cleft palate because tonsils help minimize escape of air during speech, (2) acute infections at the time of surgery because locally inflamed tissues increase the risk of bleeding, and (3) uncontrolled systemic diseases or blood dyscrasias.
Nursing Care Management
Nursing care involves providing comfort and minimizing activities or interventions that precipitate bleeding. A soft to liquid diet is preferred. A cool-mist vaporizer keeps the mucous membranes moist during periods of mouth breathing. Warm salt-water gargles, throat lozenges, and analgesic-antipyretic drugs such as acetaminophen are used to promote comfort. Often opioids are needed to reduce pain for the child to drink. Combination nonopioid and opioid elixirs or tablets such as acetaminophen with codeine or with hydrocodone (Lortab) relieve pain and should be given routinely every 4 hours.
If surgery is required, the child requires the same psychologic preparation and physical care as for any other surgical procedure (see Chapters 21 and 22). Most tonsillectomy and adenoidectomy (T&A) surgeries now take place in outpatient settings; however, the priorities of preoperative and postoperative care remain the same. The following discussion focuses on postoperative nursing care for T&A, although both procedures may not be performed.
Until they are fully awake, children are placed on their abdomen or side to facilitate drainage of secretions. Routine suctioning is avoided, and, when performed, it is done carefully to avoid trauma to the oropharynx. When alert, children may prefer sitting up. They are discouraged from coughing frequently, clearing their throat, blowing their nose, or any other activity that may aggravate the operative site.
Some secretions are common, particularly dried blood from surgery. All secretions and vomitus are inspected for evidence of fresh bleeding (some blood-tinged mucus is expected). Dark brown (old) blood is usually present in the emesis, in the nose, and between the teeth. If parents do not expect this, they often become frightened at a time when they need to be calm and reassuring.
The throat is sore after surgery. An ice collar provides relief, but many children find it bothersome and refuse to use it. Most children experience moderate pain after a T&A and need pain medication for at least the first 24 hours. Analgesics may be given rectally or intravenously to avoid the oral route. Because pain is continuous, analgesics should be administered at regular intervals. An antiemetic such as ondansetron (Zofran) may be administered postoperatively (see Pain Management, Chapter 7).
Food and fluids are restricted until children are fully alert and there are no signs of hemorrhage. Cool water, crushed ice, flavored ice pops, or diluted fruit juice may be given, but fluids with a red or brown color are avoided to distinguish fresh or old blood in emesis from the ingested liquid. Citrus juice may cause discomfort and is usually poorly tolerated. Soft foods, particularly gelatin, cooked fruits, sherbet, soup, and mashed potatoes, are started on the first or second postoperative day or as the child tolerates feeding. The pain from surgery often inhibits fluid intake, reinforcing the need for adequate pain control. Milk, ice cream, and pudding are usually not offered, since milk products coat the mouth and throat and may cause the child to clear the throat, which can initiate bleeding.
Postoperative hemorrhage is uncommon but can occur. The nurse observes the throat directly for evidence of bleeding, using a good source of light and, if necessary, carefully inserting a tongue depressor. Other signs of hemorrhage are tachycardia, pallor, frequent clearing of the throat or swallowing by a younger child, and vomiting of bright red blood. Restlessness, an indication of hemorrhage, may be difficult to differentiate from general discomfort after surgery. Decreasing blood pressure is a late sign of shock.
Surgery may be required to ligate a bleeding vessel. Airway obstruction may also occur as a result of edema or accumulated secretions and is indicated by signs of respiratory distress, such as stridor, drooling, restlessness, agitation, increasing respiratory rate, and progressive cyanosis. Suction equipment and oxygen should be available after tonsillectomy.
Family Support and Home Care.: Discharge instructions include (1) avoiding irritating or highly seasoned foods, (2) avoiding gargles or vigorous toothbrushing, (3) avoiding coughing or clearing of the throat or putting objects in the mouth, (4) using analgesics or an ice collar for pain, and (5) limiting activity to decrease the potential for bleeding. Objectionable mouth odor and slight ear pain with a low-grade fever are common for a few days postoperatively. However, persistent severe earache, fever, or cough requires medical evaluation. Most children are ready to resume normal activity within 1 to 2 weeks after the operation.
Hemorrhage may occur up to 10 days after surgery as a result of tissue sloughing from the healing process. Any sign of bleeding warrants immediate medical attention.
INFLUENZA
Influenza, or “flu,” is caused by three orthomyxoviruses, which are antigenically distinct: types A and B, which cause epidemic disease, and type C, which is unimportant from an epidemiologic standpoint. Influenza is spread from one individual to another by direct contact (large-droplet infection) or by articles recently contaminated by nasopharyngeal secretions. There is no predilection for a specific age-group, but attack rates are highest in young children who have had no previous contact with a strain. Influenza is frequently most severe in infants. During epidemics, infection among school-age children is believed to be a major source of transmission in a community. The disease is more common during the winter months and has a 1- to 3-day incubation period. Affected persons are most infectious for 24 hours before and after the onset of symptoms. The virus has a peculiar affinity for epithelial cells of the respiratory tract mucosa, where it destroys ciliated epithelium with metaplastic hyperplasia of the tracheal and bronchial epithelium with associated edema. The alveoli may also become distended with a hyaline-like material. The viruses can be isolated from nasopharyngeal secretions early after the onset of infection, and serologic tests identify the type by complement fixation or the subgroups by hemagglutination inhibition.
Clinical Manifestations
The manifestations of influenza may be subclinical, mild, moderate, or severe. Most patients have a dry throat and nasal mucosa, a dry cough, and a tendency toward hoarseness. A flushed face, photophobia, myalgia, hyperesthesia, and sometimes exhaustion and lack of energy accompany a sudden onset of fever and chills. Subglottal croup is common, especially in infants. The symptoms of influenza last for 4 or 5 days. Complications include severe viral pneumonia (often hemorrhagic); encephalitis; and secondary bacterial infections such as OM, sinusitis, or pneumonia.
Therapeutic Management
Uncomplicated influenza in children usually requires only symptomatic treatment: acetaminophen or ibuprofen for fever and sufficient fluids to maintain hydration. Amantadine hydrochloride (Symmetrel) has been effective in reducing symptoms associated with type A disease if administered within 24 to 48 hours after their onset; the symptoms associated with influenza are reportedly shortened by 24 hours, but the drug does not “cure” the disease. It is ineffective against type B or C influenza or other viral diseases. It should not be given to children under 1 year of age but is recommended for unvaccinated high-risk children.
Zanamivir and rimantadine have been approved for the treatment of flu symptoms in children under 18 years of age. Both medications must also be started within 48 hours of symptom onset. Zanamivir is an inhaled medication effective for type A and B influenza. The drug is taken twice daily for 5 days and is administered by a specially designed oral inhaler (Diskhaler). Zanamivir cannot be used for children less than 5 years of age. A fourth drug, oseltamivir (Tamiflu), is a neuroaminidase inhibitor that may be administered orally for 5 days to children over 1 year (and adults) to decrease the flu symptoms; as with other antiviral drugs, this must be taken within 2 days of the onset of symptoms. It is reported to be effective for types A and B influenza (American Academy of Pediatrics, 2006b). Bronchospasm and a decline in lung function can occur when zanamivir is used in patients with underlying airway disease such as asthma or chronic obstructive pulmonary disease. Rimantadine is effective only for type A virus; this drug is taken orally in tablet or syrup twice daily for 7 days. Rimantadine cannot be used for children less than 1 year of age. Children with influenza (or other similar viruses) should not receive aspirin because of its possible link with Reye syndrome.
Prevention.: Two vaccines may be administered to prevent influenza. Inactivated trivalent influenza viral (TIV) vaccines are safe and effective provided the antigens in the vaccine correlate with the circulating influenza viruses (see Immunizations, Chapter 10). The live-attenuated influenza vaccine (LAIV) is a nasal spray flu vaccine approved by the U.S. Food and Drug Administration (FDA) that is licensed for administration in children 2 years of age and older. However, this preparation contains a live virus and should not be used in individuals who are immunocompromised, have anaphylactic reactions to egg protein, have reactive airway disease, are receiving immunosuppressive therapy, have a chronic respiratory condition, or have a history of Guillain-Barré syndrome.
Nursing Care Management
Nursing care is the same as for any child with a URI, including implementing measures to relieve symptoms. The greatest danger to affected children is development of a secondary infection. Prolonged fever or appearance of fever during early convalescence is a sign of secondary bacterial infection and should be reported to the practitioner for antibiotic therapy.
OTITIS MEDIA
OM is one of the most prevalent diseases of early childhood. Its incidence is highest in the winter months. Many cases of bacterial OM are preceded by a viral respiratory infection. The two viruses most likely to precipitate OM are RSV and influenza. Most episodes of acute otitis media (AOM) occur in the first 24 months of life, but the incidence decreases with age, except for a small increase at age 5 or 6 years when children enter school. OM occurs infrequently in children older than 7 years of age. Preschool-age boys are affected more frequently than preschool-age girls. Children who have siblings or parents with a history of chronic OM have a higher incidence of OM. Children living in households with many members (especially smokers) are more likely to have OM than those living with fewer persons. Passive smoking increases the risk of persistent middle ear effusion by enhancing attachment of the pathogens that cause otitis to the respiratory epithelium in the middle ear space, by prolonging the inflammatory response, and by impeding drainage through the eustachian tube (American Academy of Pediatrics, 2004a). Family socioeconomic status and extent of exposure to other children are the two most important identifiable risk factors for the occurrence of OM (American Academy of Pediatrics 2004a; Kershner, 2007).
OM has been defined in a variety of ways. The standard terminology used to define OM is outlined in Box 23-5, and AOM treatment guidelines have been published (American Academy of Pediatrics, 2004a, 2004b).
Etiology
Streptococcus pneumoniae, H. influenzae, and Moraxella catarrhalis are the three most common bacteria causing AOM. The etiology of noninfectious OM is unknown, although OM may occur because of blocked eustachian tubes from the edema of URIs, allergic rhinitis, or hypertrophic adenoids. Chronic OM is frequently an extension of an acute episode.
A relationship has been observed between the incidence of OM and infant feeding methods. Infants fed breast milk have a lower incidence of OM compared with formula-fed infants. Breastfeeding may protect infants against respiratory viruses and allergy because it contains secretory immunoglobulin A, which limits the exposure of the eustachian tube and middle ear mucosa to microbial pathogens and foreign proteins. Reflux of milk up the eustachian tubes is less likely in breast-fed infants because of the semivertical positioning during breastfeeding compared with bottle-feeding.
Pathophysiology
OM is primarily a result of malfunctioning eustachian tubes. The eustachian tube is part of a contiguous system composed of the nares, nasopharynx, eustachian tube, middle ear, and mastoid antrum and air cells. Eustachian tubes have three functions relative to the middle ear: (1) protection of the middle ear from nasopharyngeal secretions, (2) drainage of secretions produced in the middle ear into the nasopharynx, and (3) ventilation of the middle ear to equalize air pressure within the middle ear and atmospheric pressure in the external ear canal and to replenish oxygen that has been absorbed.
Mechanical or functional obstruction of the eustachian tube causes accumulation of secretions in the middle ear. Intrinsic obstruction can be caused by infection or allergy; extrinsic obstruction is usually a result of enlarged adenoids or nasopharyngeal tumors. Persistent collapse of the tube during swallowing can cause functional obstruction associated with decreased stiffness or an inefficient opening mechanism. Eustachian tube obstruction results in negative middle ear pressure and, if persistent, produces a transudative middle ear effusion. Drainage is inhibited by sustained negative pressure and impaired ciliary transport within the tube. When the passage is not totally obstructed, contamination of the middle ear can take place by reflux, aspiration, or insufflation during crying, sneezing, nose blowing, and swallowing when the nose is obstructed.
Diagnostic Evaluation
Careful assessment of tympanic membrane mobility with a pneumatic otoscope is essential to differentiate AOM from OM with effusion (OME) (American Academy of Pediatrics, 2004b). A diagnosis of AOM is made if visual inspection of the tympanic membrane reveals a purulent discolored effusion and a bulging or full, opacified, or reddened immobile membrane. Some practitioners also consider the presence of acute onset of less than 48 hours of ear pain with the above criteria to be a diagnostic factor in AOM (Powers, 2007). An immobile tympanic membrane or an orange discolored membrane indicates OME. Clinical symptoms of otitis are also helpful in making the diagnosis (Box 23-6). In AOM, symptoms such as acute onset of ear pain, fever, and a bulging yellow or red tympanic membrane are usually present. In OME, these symptoms may be absent, and other nonspecific symptoms such as rhinitis, cough, or diarrhea are often present (American Academy of Pediatrics, 2004a, 2004b).
Therapeutic Management
Treatment for AOM is one of the most common reasons for antibiotic use in the ambulatory setting. Recently, however, concerns about drug-resistant S. pneumoniae and other drug resistances have led infectious disease authorities to recommend careful and judicious use of antibiotics for treatment of this illness. Current literature indicates that waiting up to 72 hours for spontaneous resolution is safe and appropriate management of AOM in healthy infants over 6 months and children (American Academy of Pediatrics, 2004a; Bhetwal and McConaghy, 2007). Furthermore some reviews of the treatment of AOM reveal no clear evidence that antibiotics improve outcomes in children younger than 2 years of age with uncomplicated AOM. However, the watchful waiting approach is not recommended for children younger than 2 years who have persistent acute symptoms of fever and severe ear pain (Carlson and Scudder, 2004). In addition, all cases of AOM in infants younger than 6 months of age should be treated with antibiotics because of the infant’s immature immune system and the potential for infection with bacteria other than the three most common organisms found in older infants and children with AOM.
When antibiotics are warranted, oral amoxicillin in high doses (80 to 90 mg/kg/day, divided twice daily) is the treatment of choice for initial episodes of AOM in children who have not received antibiotics within the past month (American Academy of Pediatrics, 2004a; Bhetwal and McConaghy, 2007; Pichichero and Casey, 2005). The recommendation for the duration of antibiotic therapy is 10 to 14 days; in children 6 years and older with uncomplicated AOM, shorter courses may be sufficient (American Academy of Pediatrics, 2006b).
Second-line antibiotics used to treat OM include amoxicillin–clavulanate; azithromycin; and cephalosporins such as cefdinir, cefuroxime, and cefpodoxime. IM ceftriaxone is used if the causative organism is a highly resistant pneumococcus or if the parents are noncompliant with the therapy. An important consideration with the use of single-dose IM injections is the pain involved in this therapy. One strategy to minimize pain at the injection site is to reconstitute the cephalosporin with 1% lidocaine. The use of steroids, decongestants, and antihistamines to treat AOM is not recommended.
Supportive care or symptomatic treatment of AOM includes treating the fever and pain. For fever or discomfort associated with OM, analgesic-antipyretic drugs such as acetaminophen or ibuprofen may be given. Topical pain relief is recommended by external application of heat or cold, or the practitioner may prescribe topical pain relief drops such as benzocaine drops. Antihistamines and decongestants are not recommended. Antibiotic ear drops have no value in treating AOM.
Myringotomy, a surgical incision of the eardrum, may be necessary to alleviate the severe pain of AOM. A myringotomy is also performed to provide drainage of infected middle ear fluid in the presence of complications (mastoiditis, labyrinthitis, or facial paralysis) or to allow purulent middle ear fluid to drain into the ear canal for culture. A minimally invasive laser-assisted myringotomy procedure may be performed in outpatient settings.
Tympanostomy tube placement and adenoidectomy are surgical procedures that may be done to treat recurrent OM. Tympanostomy tubes are pressure-equalizer (PE) tubes or grommets that facilitate continued drainage of fluid and allow ventilation of the middle ear. Adenoidectomy is not recommended for treatment of AOM and is performed only in children with recurrent AOM or chronic OME with postnasal obstruction, adenoiditis, or chronic sinusitis.
In some children, residual middle ear effusions remain after episodes of AOM. Some children have fluid that persists in the middle ear for weeks or months. Antibiotics are not required for initial treatment of OME, but may be indicated for children with persistent effusion for more than 3 months (American Academy of Pediatrics, 2004a). Placement of tympanostomy tubes is recommended after a total of 4 to 6 months of bilateral effusion with a bilateral hearing deficit (American Academy of Pediatrics, 2004b). This therapy allows for mechanical drainage of the fluid, which promotes healing of the membrane and prevents scar formation and loss of elasticity. Myringotomy with or without insertion of PE tubes should not be performed for initial management of OME but may be recommended for children who have recurrent episodes of OME with a long cumulative duration (American Academy of Pediatrics, 2004b). Tonsillectomy either alone or with adenoidectomy is not considered an effective treatment of OME (American Academy of Pediatrics, 2004b).
OME is frequently associated with mild to moderate impairment of hearing; therefore a hearing test should also be performed 3 months after the acute episode of AOM, if OME persists for 3 months or more, or if there is evidence of language or learning delays. Follow-up examinations of children with chronic OME should be maintained on a 3- to 6-month basis until the OME is resolved, a significant hearing loss is identified, or structural defect of the tympanic membrane or middle ear is identified (American Academy of Pediatrics, 2004a). Children with hearing loss should be referred to an otolaryngologist and should receive a speech and language evaluation as necessary.
Prevention.: The pneumococcal conjugate vaccine PCV has decreased the incidence of invasive pneumococcal infections by 80% in children under 2 years of age since the year 2000 (American Academy of Pediatrics, 2006b).
Parents are encouraged to reduce risk factors for AOM by breastfeeding infants for at least the first 6 months of life, avoiding propping the bottle, decreasing or discontinuing pacifier use after 6 months, and preventing exposure to tobacco smoke (American Academy of Pediatrics, 2004a).
Nursing Care Management
Nursing objectives for the child with AOM include (1) relieving pain, (2) facilitating drainage when possible, (3) preventing complications or recurrence, (4) educating the family in care of the child, and (5) providing emotional support to the child and family.
Analgesic drugs such as acetaminophen and ibuprofen are used to treat mild pain. For more severe pain, the American Academy of Pediatrics (2004a) guidelines recommend a stronger analgesic such as codeine.
If the ear is draining, the external canal may be cleaned with sterile cotton swabs or pledgets coupled with topical antibiotic treatment. If ear wicks or lightly rolled sterile gauze packs are placed in the ear after surgical treatment, they should be loose enough to allow accumulated drainage to flow out of the ear; otherwise, infection may be transferred to the mastoid process. The wicks need to stay dry during shampoos or baths. Occasionally, drainage is so profuse that the auricle and the skin surrounding the ear become excoriated from the exudate. This is usually prevented by frequent cleansing and application of various moisture barriers (e.g., Proshield Plus) or petrolatum jelly (e.g., Vaseline).
Tympanostomy tubes may allow water to enter the middle ear, but recommendations for earplugs are inconsistent. Research indicates that swimming without earplugs poses a slight increased risk of infection (Goldstein, Mandel, Kurs-Lasky, and others, 2005). However, lake and river water is potentially contaminated, and wearing earplugs while swimming in a lake prevents total flooding of the external canal. Bathwater and shampoo water should be kept out of the ear, if possible, because soap reduces the surface tension of water and facilitates entry through the tube. Parents should be aware of the appearance of a grommet (usually a tiny, white, plastic spool-shaped tube) so that they can recognize it if it falls out. They are reassured that this is normal and requires no immediate intervention, although they should notify the practitioner.
Prevention of recurrence requires adequate education regarding antibiotic therapy. The symptoms of pain and fever usually subside within 24 to 48 hours, but nurses must emphasize that all of the prescribed medication should be taken. Parents should be aware that potential complications of OM, such as hearing loss, can be prevented with adequate treatment and follow-up care.
Parents also need anticipatory guidance regarding methods to reduce the risks of OM, especially in children under 2 years of age. Reducing the chances of OM is possible with simple measures, such as sitting or holding an infant upright for feedings, maintaining routine childhood immunizations, and exclusively breastfeeding until at least 6 months of age. Propping bottles is discouraged to avoid pooling of milk while the child is in the supine position and to encourage human contact during feeding. Eliminating tobacco smoke and known allergens is also recommended. Early detection of middle ear effusion is essential to prevent complications. Infants and preschool children should be screened for effusion, and all schoolchildren, especially those with learning disabilities, should be tested for middle ear effusion. Frequent audiologic evaluations, medical consultation, and education of parents and children are advised when middle ear effusion is detected.
INFECTIOUS MONONUCLEOSIS
Infectious mononucleosis is an acute, self-limiting infectious disease that is common among adolescents. The illness is characterized by an increase in the mononuclear elements of the blood and by general symptoms of an infectious process. The course is usually mild but occasionally can be severe or, rarely, accompanied by serious complications.
Etiology and Pathophysiology
The herpes-like Epstein-Barr virus (EBV) is the principal cause of infectious mononucleosis. It appears in both sporadic and epidemic forms, but the sporadic cases are more common. The mechanism of spread has not been proved, but it is believed to be transmitted in saliva by direct intimate contact. It is mildly contagious, but the period of communicability is unknown. There is evidence that the virus is spread through sexual contact, especially when multiple partners are involved (Rimsza and Kirk, 2005). The incubation period following exposure is approximately 30 to 50 days (American Academy of Pediatrics, 2006).
Diagnostic Tests
The onset of symptoms may be acute or insidious and may appear anywhere from 10 days to 6 weeks after exposure. The presenting symptoms vary greatly in type, severity, and duration (Box 23-7). The clinical manifestations of infectious mononucleosis are usually less severe (often subclinical or unapparent) and the convalescent phase is shorter in younger children than in older children and young adults. The leukocyte count may be normal or low. Usually lymphocytic leukocytosis develops, and there is an increase in atypical leukocytes in the peripheral blood smear. The heterophil antibody test determines the extent to which the patient’s serum will agglutinate sheep red blood cells; the response in this test is primarily to immunoglobulin M, which is present in the first 2 weeks of the illness in adolescents.
The spot test (Monospot) is a slide test of venous blood that has high specificity. It is rapid, sensitive, inexpensive, and easy to perform, and has the advantage over the heterophil antibody test that it can detect significant agglutinins at lower levels, thus allowing earlier diagnosis. Blood is usually obtained for the test by finger puncture or venous sampling and is placed on special paper. If the blood agglutinates, forming fragments or clumps, the test is positive for the infection.
Therapeutic Management
No specific treatment exists for infectious mononucleosis. Simple remedies ordinarily relieve the symptoms. A mild analgesic is often sufficient to relieve the headache, fever, and malaise. Rest is encouraged for fatigue but is not imposed for any specific period. Affected persons are instructed to regulate activities according to their own tolerance unless complicating factors are present. Contact sports are discouraged in the presence of splenomegaly.
Antibiotics are contraindicated unless β-hemolytic streptococci are present. If sore throat is severe, effective therapies include gargles; hot drinks; anesthetic troches; or analgesics, including opioids. Corticosteroids have been used to treat respiratory distress from significant tonsillar inflammation, hemolytic anemia, thrombocytopenia, and neurologic complications; however, routine use of steroids is not recommended (American Academy of Pediatrics, 2006).
Prognosis.: The course of this disease is usually self-limiting and uncomplicated. Acute symptoms often disappear within 7 to 10 days, and persistent fatigue subsides within 2 to 4 weeks. Some adolescents may need to restrict activities for 2 to 3 months, but the disease rarely extends for longer periods. Complications are uncommon, but can be serious and require appropriate management.
Nursing Care Management
Nursing responsibilities are directed toward providing comfort measures to relieve symptoms and helping affected adolescents and their families to determine appropriate activities for the stage of the disease. The child is advised to limit exposure to persons outside the family, especially during the acute phase of illness. Children and adolescents may need diet counseling to select foods that contain sufficient calories to meet growth and energy needs but are easy to swallow. It may be more comfortable to limit intake to liquids during the acute phase; milk shakes are a good alternative to solid foods on a temporary basis. Throat pain may be severe enough to require a mild analgesic such as codeine. Careful nursing assessment of swallowing ability is essential because the edema may cause serious airway compromise in some children.
CROUP SYNDROMES
Croup is a general term applied to a symptom complex characterized by hoarseness, a resonant cough described as “barking” or “brassy” (croupy), varying degrees of inspiratory stridor, and varying degrees of respiratory distress resulting from swelling or obstruction in the region of the larynx. Acute infections of the larynx are important in infants and small children because of their increased incidence in these age-groups and because the small diameter of the airway in infants and children places them at risk for significant narrowing with inflammation.
Croup syndromes can affect the larynx, trachea, and bronchi. However, laryngeal involvement often dominates the clinical picture because of the severe effects on the voice and breathing. Croup syndromes are described according to the primary anatomic area affected (i.e., epiglottitis [or supraglottitis], laryngitis, laryngotracheobronchitis [LTB], and tracheitis). In general, LTB occurs in very young children, and epiglottitis is more common in older children. A comparison of croup syndromes is provided in Table 23-1.
With widespread immunization programs aimed at preventing H. influenzae type b, the cause of most cases of croup in the United States is attributed to viruses, namely parainfluenza virus, human metapneumovirus, influenza types A and B, adenovirus, and measles.
ACUTE EPIGLOTTITIS
Acute epiglottitis, or acute supraglottitis, is a serious obstructive inflammatory process that occurs predominantly in children 2 to 8 years of age (Rotta and Wiryawan, 2003), but can occur from infancy to adulthood. The disorder requires immediate attention. The obstruction is supraglottic as opposed to the subglottic obstruction of laryngitis. The responsible organism is usually H. influenzae. LTB and epiglottitis do not occur together.
Clinical Manifestations
The onset of epiglottitis is abrupt, and it can rapidly progress to severe respiratory distress. The child usually goes to bed asymptomatic to awaken later, complaining of sore throat and pain on swallowing. The child has a fever; appears sicker than clinical findings suggest; and insists on sitting upright and leaning forward, with the chin thrust out, mouth open, and tongue protruding (tripod position). Drooling of saliva is common because of the difficulty or pain on swallowing and excessive secretions.
The child is irritable and extremely restless and has an anxious, apprehensive, and frightened expression. The voice is thick and muffled, with a froglike croaking sound on inspiration, but the child is not hoarse. Suprasternal and substernal retractions may be evident. The child seldom struggles to breathe, and slow, quiet breathing provides better air exchange. The sallow color of mild hypoxia may progress to frank cyanosis. The throat is red and inflamed, and a distinctive large, cherry red, edematous epiglottis is visible on careful throat inspection.
Therapeutic Management
The course of epiglottitis may be fulminant, with respiratory obstruction appearing suddenly. Progressive obstruction leads to hypoxia, hypercapnia, and acidosis followed by decreased muscular tone; reduced level of consciousness; and, when obstruction becomes more or less complete, a rather sudden death. A presumptive diagnosis of epiglottitis constitutes an emergency.
The child who is suspected of having epiglottitis should be examined in a setting where emergency airway equipment is readily available. Examination of the throat with a tongue depressor is contraindicated until experienced personnel and equipment are available to proceed with immediate intubation or tracheostomy in the event that the examination precipitates further or complete obstruction.
If a lateral neck film is indicated, experienced personnel should accompany the child to the radiology department. For a young child who is likely to become more agitated by the procedure, it is preferable that the child not be transported but remain on the parent’s lap in the examination area during portable radiology. Other procedures, such as insertion of an intravenous (IV) line, that are likely to further agitate the child are delayed until adequate airway is maintained.
Nasotracheal intubation or tracheostomy is usually considered for the child with epiglottitis with severe respiratory distress. It is recommended that the intubation or tracheostomy and any invasive procedure, such as starting an IV infusion, be performed in an area where emergency airway maintenance can be easily and quickly accomplished. Humidified oxygen is administered as necessary either via mask in older children or flowby in younger children to avoid further agitation. Whether or not there is an artificial airway, the child requires intensive observation by experienced personnel. The epiglottal swelling usually decreases after 24 hours of antibiotic therapy, and the epiglottis is near normal by the third day. Intubated children are generally extubated at this time. Additional treatment for children with moderate or severe disease includes administration of nebulized epinephrine (racemic epinephrine) or a mixture of helium and oxygen (heliox) to decrease edema. The use of corticosteroids for reducing edema has become a mainstay in the treatment of epiglottitis. Oral corticosteroid is preferred, but other routes of administration include IM, IV, and nebulized (Wright, Rowe, Arent, and others, 2005).
Children with suspected bacterial epiglottitis are given antibiotics intravenously, followed by oral administration to complete a 7- to 10-day course.
Nursing Care Management
Epiglottitis is a serious and frightening disease for the child and family. It is important to act quickly but calmly and to provide support without increasing anxiety. The child is allowed to remain in the position that provides the most comfort and security, and parents are reassured that everything possible is being done to obtain relief for their child.
Acute care of the child is the same as that described later for the child with LTB. Continuous monitoring of respiratory status, including pulse oximetry (and blood gases if the patient is intubated), is an important part of nursing observations, and the IV infusion is maintained as described in Chapter 22.
ACUTE LARYNGITIS
Acute infectious laryngitis is a common illness in older children and adolescents. Infants and smaller children experience more generalized involvement (see the following section on LTB). Viruses are the usual causative agents, and the principal complaint is hoarseness, which may be accompanied by other upper respiratory symptoms (e.g., rhinitis, sore throat, nasal congestion) and systemic manifestations (e.g., fever, headache, myalgia, malaise). Associated complaints vary with the infecting virus. Adenoviruses, human metapneumoviruses, and influenza viruses are responsible for more systemic involvement; parainfluenza viruses, rhinoviruses, and RSV cause milder illness.
Therapeutic Management and Nursing Care Management
The disease is usually self-limited without long-term sequelae. Treatment is symptomatic with fluids and humidified air (see Nursing Care Plan, pp. 759–761).
ACUTE LARYNGOTRACHEOBRONCHITIS
LTB is the most common croup syndrome. It primarily affects children younger than 5 years of age, and the causative organisms are the parainfluenza virus types 2 and 3, human metapneumovirus, RSV, influenza A and B, and M. pneumoniae. The disease is usually preceded by a URI, which gradually descends to adjacent structures. It is characterized by gradual onset of low-grade fever, and the parents often report that the child went to bed and later awoke with a barky, brassy cough. Inflammation of the mucosa lining the larynx and trachea causes a narrowing of the airway. When the airway is significantly narrowed, the child struggles to inhale air past the obstruction and into the lungs, producing the characteristic inspiratory stridor and suprasternal retractions; other classic manifestations include cough and hoarseness. Respiratory distress in infants and toddlers may be manifested by nasal flaring, intercostal retractions, tachypnea, and continuous stridor. The typical child with LTB is a toddler who develops the classic barking or seal-like cough and acute stridor after several days of rhinitis. When the child is unable to inhale a sufficient volume of air, symptoms of hypoxia become evident. Obstruction that is severe enough to prevent adequate ventilation and exhalation of carbon dioxide can cause respiratory acidosis and eventually respiratory failure. The progression of symptoms is outlined in Box 23-8.
Therapeutic Management
The major objective in medical management is maintaining the airway and providing adequate respiratory exchange. Children with mild croup (no stridor at rest) can be managed at home. Parents are taught the signs of respiratory distress and instructed to summon professional help early if needed. Children who progress to stage II respiratory symptoms should receive medical attention (see Box 23-8).
High humidity with cool mist provides relief for most children. A cool-air vaporizer can be used at home. In the hospital, a nebulized mist for older infants and toddlers may be used to provide increased humidity and supplemental oxygen. However, controversy surrounds the use of mist therapy to treat croup. Studies have failed to demonstrate any improvement in subglottic edema with mist therapy (Moore and Little, 2006).
Nebulized epinephrine (racemic epinephrine) is often used in children with severe disease, stridor at rest, retractions, or difficulty breathing. The α-adrenergic effects cause mucosal vasoconstriction and subsequently decrease subglottic edema. The onset of action is rapid, and the peak effect is observed in 2 hours. Children may be discharged home following racemic epinephrine after a 2- to 3-hour period of observation for return of acute symptoms
Oral steroids have proven effective in the treatment of croup; IM dexamethasone may be given to children who are unable to tolerate oral dosing. Nebulized budesonide may be administered in conjunction with IM dexamethasone. A single dose of oral corticosteroid has been shown to decrease hospitalizations and the need for multiple racemic epinephrine treatments in children with mild croup.
In severe cases of LTB the administration of heliox may serve to reduce the work of breathing and relieve airway obstruction. Because helium has a lower density than room air, it forms a respirable gas (with oxygen) that reduces airway turbulence.
Nursing Care Management
The most important nursing function in the care of children with LTB is continuous, vigilant observation and accurate assessment of respiratory status. Pulse oximetry is commonly used for monitoring oxygenation status. Changes in therapy are frequently based on the nurses’ observations and assessments, the child’s response to therapy, and tolerance of procedures. The trend away from early intubation of children with LTB emphasizes the importance of nursing observations and the ability to recognize impending respiratory failure so that intubation can be implemented without delay. Intubation equipment must be readily accessible and taken with the child during transport to other areas (e.g., radiology, operating room).
Infants or small children find that being enclosed in a tent, coughing, having laryngeal spasms, and needing IV therapy are additional sources of distress. In many acute care facilities the mist tent has been abandoned and the infant is allowed to be held by the parent; if cool mist is used in the treatment, it can be administered through a tube held in front of the patient while the child is held on the parent’s lap.
Children with mild croup are allowed to drink beverages they like as long as respiratory status is stable, and parents are encouraged to try whatever comforting measures work best (e.g., holding their child, rocking, singing). If the child is unable to take oral fluids, IV fluids may be required in addition to IV medications (dexamethasone).
The rapid progression of croup, the alarming sound of the cough and stridor, and the child’s apprehensive behavior and ill appearance combine to create a frightening experience for the parents. Parents need reassurance regarding their child’s progress and an explanation of treatments. The family should be allowed to remain with their child as much as possible.
The nurse should provide the parents with an opportunity to express their feelings and referrals as necessary. Parents need frequent reassurance provided in a calm, quiet manner and education regarding what they can do to make their child more comfortable. Home care includes continued humidity, adequate hydration, and nourishment.
ACUTE SPASMODIC LARYNGITIS
Acute spasmodic laryngitis (spasmodic croup, “midnight croup,” or “twilight croup”) is distinct from laryngitis and LTB and is characterized by paroxysmal attacks of laryngeal obstruction that occur chiefly at night. Signs of inflammation are absent or mild, and there is often a history of previous attacks lasting 2 to 5 days, followed by uneventful recovery. This condition usually affects children ages 1 to 3 years. Some children appear to be predisposed to the condition; allergies may be implicated in some cases.
The child goes to bed feeling well or with mild respiratory symptoms but awakens suddenly with characteristic barking, metallic cough; hoarseness; noisy inspirations; and restlessness. The child appears anxious and frightened. Dyspnea is aggravated by excitement, but there is no fever, the attack subsides in a few hours, and the child appears well the next day.
Therapeutic Management and Nursing Care Management
Spasmodic croup is usually self-limiting, and most children are managed at home. A cool mist humidifier may be recommended for home treatment. Sometimes the spasm is relieved by sudden exposure to cold air (as when the child is taken out into the night air to see the practitioner). Parents are usually advised to have the child sleep in humidified air until the cough has subsided to prevent subsequent episodes. Children with moderately severe symptoms may be hospitalized for observation and therapy with cool mist and racemic epinephrine, as for LTB. Some patients respond to corticosteroid therapy.
BACTERIAL TRACHEITIS
Bacterial tracheitis, an infection of the mucosa of the upper trachea, is a distinct entity with features of both croup and epiglottitis. The disease occurs in children under 3 years of age and may be a serious cause of airway obstruction that is severe enough to cause respiratory arrest. It is believed to be a complication of LTB, and although Staphylococcus aureus is the most frequent organism responsible, M. catarrhalis, S. pneumonia, and H. influenzae have also been implicated.
Many of the manifestations of bacterial tracheitis are similar to those of LTB but are unresponsive to LTB therapy. There is a history of previous URI with croupy cough, stridor unaffected by position, toxicity, absence of drooling, and high fever. A prominent manifestation is the production of thick, purulent tracheal secretions. Respiratory difficulties are secondary to these copious secretions. Children with this condition may develop a life-threatening upper airway obstruction, respiratory failure, acute respiratory distress syndrome (ARDS), and multiple organ dysfunction (Hopkins, Lahiri, Salerno, and others, 2006).
Therapeutic Management and Nursing Care Management
Bacterial tracheitis requires vigorous management with antipyretics and antibiotics. Many children require endotracheal intubation and mechanical ventilation; patients are closely monitored for impending respiratory failure if not intubated. Early recognition to prevent life-threatening airway obstruction is essential.
INFECTIONS OF THE LOWER AIRWAYS
The reactive portion of the lower respiratory tract includes the bronchi and bronchioles in children. Cartilaginous support of the large airways is not fully developed until adolescence. Consequently, the smooth muscle in these structures represents a major factor in the constriction of the airway, particularly in the bronchioles, that portion that extends from the bronchi to the alveoli. Table 23-2 compares some of the major features of bronchial and bronchiolar infections.
TABLE 23-2
Comparison of Conditions Affecting the Bronchi
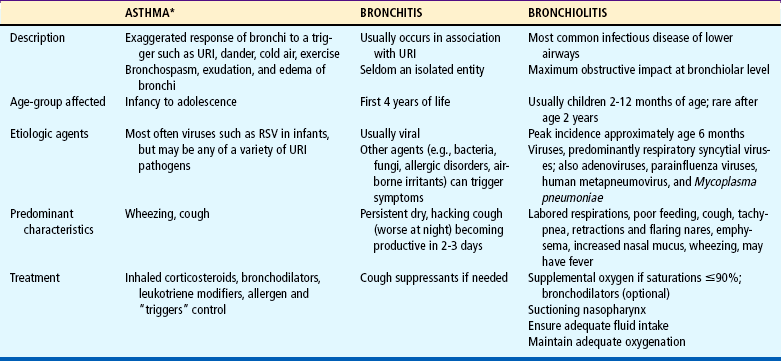
URI, Upper respiratory infection.
*See Asthma, p. 783.
BRONCHITIS
Bronchitis (sometimes referred to as tracheobronchitis) is inflammation of the large airways (trachea and bronchi), which is frequently associated with a URI. Viral agents are the primary cause of the disease, although M. pneumoniae is a common cause in children older than 6 years of age. A dry, hacking, nonproductive cough that worsens at night and becomes productive in 2 or 3 days characterizes this condition.
Bronchitis is a mild, self-limiting disease that requires only symptomatic treatment, including analgesics, antipyretics, and humidity. Cough suppressants may be useful to allow rest but can interfere with clearance of secretions. Most patients recover uneventfully in 5 to 10 days.
RESPIRATORY SYNCYTIAL VIRUS AND BRONCHIOLITIS
Bronchiolitis is an acute viral infection with maximum effect at the bronchiolar level. The infection occurs primarily in winter and early spring. By age 3 years most children have been infected at least once. RSV infection is the most frequent cause of hospitalization in children less than 1 year old. In addition, severe RSV infections in the first year of life represent a significant risk factor for the development of asthma up to age 13 (Chávez-Bueno, Mejías, Jafri, and others, 2005). RSV infection may also occur in children older than 1 year who have a chronic or serious disabling illness. Although most cases of bronchiolitis are caused by RSV, adenoviruses and parainfluenza viruses are also implicated; recently, human metapneumovirus has also been associated with bronchiolitis in children.
Pathophysiology
RSV affects the epithelial cells of the respiratory tract. The ciliated cells swell, protrude into the lumen, and lose their cilia. RSV produces a fusion of the infected cell membrane with cell membranes of adjacent epithelial cells, thus forming a giant cell with multiple nuclei. At the cellular level this fusion results in multinucleated masses of protoplasm, or syncytia.
The bronchiolar mucosa swells, and lumina are subsequently filled with mucus and exudate. The walls of the bronchi and bronchioles are infiltrated with inflammatory cells, and peribronchiolar interstitial pneumonitis is usually present. Because luminal epithelial cells are shed into the bronchioles when they die, the lumina are frequently obstructed, particularly on expiration. The varying degrees of obstruction produced in small air passages lead to hyperinflation, obstructive emphysema resulting from partial obstruction, and patchy areas of atelectasis. Dilation of bronchial passages on inspiration allows sufficient space for intake of air, but narrowing of the passages on expiration prevents air from leaving the lungs. Thus air is trapped distal to the obstruction and causes progressive overinflation (emphysema).
Clinical Manifestations
The illness usually begins with a URI after an incubation of about 5 to 8 days. Symptoms such as rhinorrhea and low-grade fever often appear first. OM and conjunctivitis may also be present. In time a cough may develop. If the disease progresses, it becomes a lower respiratory tract infection and manifests typical symptoms (Box 23-9). Infants may have several days of URI symptoms or no symptoms except slight lethargy, poor feeding, or irritability.
Once the lower airway is involved, classic manifestations include signs of altered air exchange, such as wheezing, retractions, crackles, dyspnea, tachypnea, and diminished breath sounds. Apnea may be the first recognized indicator of RSV infection in very young infants.
Diagnostic Evaluation
Identification has been simplified by the development of tests done on nasal or nasopharyngeal secretions, using either a rapid immunofluorescent antibody—direct fluorescent antibody staining (DFA) or an enzyme-linked immunosorbent assay (ELISA) for RSV antigen detection (see Respiratory Secretion and Throat Specimens, Chapter 22).
Therapeutic Management
Bronchiolitis is treated symptomatically with cool humidified oxygen, adequate fluid intake, airway maintenance, and medications. Most children with bronchiolitis can be managed at home. Hospitalization is usually recommended for children with respiratory distress or those who cannot maintain adequate hydration. Other reasons for hospitalization include complicating conditions, such as underlying lung or heart disease or associated debilitated states, or a home environment where adequate management is questionable. The infant who is tachypneic or apneic, has marked retractions, seems listless, or has a history of poor fluid intake should be admitted.
Humidified oxygen is administered in concentrations sufficient to maintain adequate oxygenation (Spo2) at or above 90% as measured by pulse oximetry. The administration of humidified mist is controversial. Routine chest physical therapy (CPT) is not recommended; infants with abundant nasal secretions benefit from periodic suctioning. Fluids by mouth may be contraindicated because of tachypnea, weakness, and fatigue; therefore IV fluids are preferred until the acute stage of the disease has passed.
Clinical assessments, noninvasive oxygen monitoring, and blood gas values guide therapy. Medical therapy for bronchiolitis is primarily supportive and aimed at decreasing airway hyperresonance and inflammation and promoting adequate fluid intake. Bronchodilators may provide short-term benefits, yet overall significant improvement in the child’s condition is not always appreciable. Racemic epinephrine has been shown to produce modest improvement in ventilation status. Corticosteroids and antihistamines have not been shown to be effective in controlled studies and are not recommended for routine use. Antibiotics are not part of the treatment of RSV unless there is a coexisting bacterial infection such as OM (American Academy of Pediatrics, 2006a). Additional treatment recommendations in the American Academy of Pediatrics (2006a) practice guideline are to encourage breastfeeding; avoid passive tobacco smoke exposure; and promote preventive measures, including hand washing and the administration of palivizumab (Synagis) to high-risk infants.
Ribavirin, an antiviral agent (synthetic nucleoside analog), is the only specific therapy approved for hospitalized children; however, use of this drug is controversial because of concerns about the high cost, aerosol route of administration, potential toxic effects among exposed health care personnel, and conflicting results of efficacy trials (American Academy of Pediatrics, 2006a; Chávez-Bueno, Mejías, Jafri, and others, 2005; Ventre and Randolph, 2007). This drug is aerosolized and delivered via a small-particle aerosol generator. It may be administered by hood, tent, or mask or through ventilator tubing for 12 to 20 hours daily; average duration of therapy is 3 days.
Prevention of RSV Infection
The only product available in the United States for prevention of RSV is palivizumab, a monoclonal antibody, which is given monthly in an IM injection. According to the American Academy of Pediatrics (2006a) practice guideline, candidates for palivizumab include infants born before 32 weeks’ gestation who required medical therapy such as supplemental oxygen or mechanical ventilation. Infants and children younger than 2 years of age with BPD who have received medical therapy (supplemental oxygen, bronchodilator, diuretic, or corticosteroid therapy) for BPD within 6 months before the anticipated RSV season may benefit from palivizumab prophylaxis. Children with more severe BPD may benefit from palivizumab prophylaxis for two RSV seasons. Children with severe immunodeficiencies (e.g., severe combined immunodeficiency or acquired immunodeficiency syndrome [AIDS]) may also benefit from prophylaxis. Infants and children younger than 2 years of age with hemodynamically significant congenital heart disease will benefit from 5 monthly IM injections of palivizumab. Prophylaxis for RSV should be initiated at the onset of the RSV season and terminated at the end of the season (November to March). Additional age and condition recommendations are outlined in the American Academy of Pediatrics practice guideline (2006a).
A second-generation monoclonal antibody, motavizumab, is currently undergoing phase III clinical trials; this drug is reported to be more effective in the prevention of RSV than palivizumab (De Vincenzo, 2008).
Nursing Care Management
Children admitted to the hospital with suspected RSV infection may be assigned separate rooms or grouped with other RSV-infected children. Contact and standard precautions are employed, including hand washing, not touching the nasal mucosa or conjunctiva, and using gloves and gowns when entering the patient’s room. Other isolation procedures of potential benefit are those aimed at diminishing the number of hospital personnel, visitors, and uninfected children in contact with the child. Another measure is to make patient assignments so that nurses assigned to children with RSV are not caring for other patients who are considered high risk.
Infants with RSV often have copious nasal secretions, making breathing and nursing or bottle-feeding difficult. This engenders concerns that the child will lose weight or stop breastfeeding altogether. Encourage breastfeeding mothers to continue feeding the infant or, if feedings are contraindicated due to the acuity of the illness, mothers should pump their milk and store appropriately for later use (see Chapter 8). Parents are taught how to instill normal saline drops into the nares and suction the mucus with a bulb syringe before feedings and before bedtime so the child may eat and rest better; unfortunately no medications appropriate for infants can help with these symptoms. To address the issue of decreased fluid intake, parents may offer small amounts of clear fluids, 5 to 10 ml at a time, with a medication syringe every 10 minutes or so to maintain adequate hydration. Infants may cough or vomit as the secretions settle in the stomach and make them prone to emesis of such secretions.
Additional nursing care is aimed at monitoring oxygenation with pulse oximetry, ensuring bronchodilator therapy is optimized by using a small mask for delivery, and providing information for the parent regarding the infant’s status. The unpredictability of the infant’s individual response to the disease compounds parental anxiety when they hear about children who had serious morbidity or died from RSV. However, for the most part infants recover quickly from the disease and resume normal daily activities, including fluid intake. Such infants are at risk for further episodes of wheezing that may or may not involve an RSV infection; parents, however, may be concerned that the infant has another serious case of RSV.
PNEUMONIAS
Pneumonia, inflammation of the pulmonary parenchyma, is common in childhood but occurs more frequently in infancy and early childhood. Clinically, pneumonia may occur either as a primary disease or as a complication of another illness. The various types of pneumonia include:
Lobar pneumonia—All or a large segment of one or more pulmonary lobes is involved.
Bronchopneumonia—This begins in the terminal bronchioles, which become clogged with mucopurulent exudate to form consolidated patches in nearby lobules; also called lobular pneumonia.
Interstitial pneumonia—The inflammatory process is more or less confined within the alveolar walls (interstitium) and the peribronchial and interlobular tissues.
Although the morphologic classification is typically used, the most useful classification of pneumonia is based on the etiologic agent (e.g., viral, bacterial, mycoplasmal, or aspiration of foreign substances) (see Aspiration Pneumonia, p. 781). Histomycosis, coccidioidomycosis, and other fungi also cause pneumonia. Other terms that describe pneumonias are hemorrhagic, fibrinous, and necrotizing. Pneumonitis is a localized acute inflammation of the lung without the toxemia associated with lobar pneumonia.
The clinical manifestations of pneumonia vary depending on the etiologic agent, the child’s age, the child’s systemic reaction to the infection, the extent of the lesions, and the degree of bronchial and bronchiolar obstruction. The causative agent is identified from the clinical history, the child’s age, the general health history, the physical examination, radiography, and the laboratory examination.
Viral Pneumonia
Viral pneumonias, which occur more frequently than bacterial pneumonias, are seen in children of all ages and are often associated with viral URIs. Viruses that cause pneumonia include RSV in infants and parainfluenza, influenza, human metapneumovirus, and adenovirus in older children. There are few clinical symptoms that are unique to a specific virus, and differentiation among viruses is usually made by clinical features such as child’s age, past medical history, season of the year, and radiographic and laboratory examination (Box 23-10).
The prognosis is generally good, although viral infections of the respiratory tract render the affected child more susceptible to secondary bacterial invasion, especially when there is denuded bronchial mucosa. Treatment is symptomatic and includes measures to promote oxygenation and comfort, such as oxygen administration with cool mist, CPT and postural drainage, antipyretics for fever management, fluid intake, and family support. Some authorities recommend antimicrobial therapy in the hopes of reducing or preventing secondary bacterial infection, but this therapy should be reserved for children in whom a bacterial infection is demonstrated by appropriate cultures.
Primary Atypical Pneumonia
Atypical pneumonia refers to pneumonia that is caused by pathogens other than the traditionally most common and readily cultured bacteria (e.g., S. pneumoniae). In the category of atypical pneumonias, M. pneumoniae and Chlamydia pneumoniae are the most common cause of community-acquired pneumonia in children 5 years or older (Rafei and Lichenstein, 2006). It occurs in the fall and winter months and is more prevalent in crowded living conditions. Most affected persons recover from acute illness in 7 to 10 days with symptomatic treatment, followed by a week of convalescence. Hospitalization is rarely necessary.
Severe Acute Respiratory Syndrome
A severe form of atypical pneumonia identified as severe acute respiratory syndrome (SARS) was first reported in Asia in 2003. SARS is caused by a previously unrecognized coronavirus called SARS-associated coronavirus (SARS Co-V). Additional human coronavirus types have since been identified in Canada, Hong Kong, and the Netherlands. Clinical manifestations of this disorder include a fever greater than 38° C (100.4° F); headache; cough; shortness of breath; difficulty breathing; and, after 2 to 7 days, a dry, nonproductive cough and dyspnea. In some patients the symptoms are severe enough to require intubation and mechanical ventilation. The disease is spread by close contact with a person with SARS. Most cases have involved people who have cared for or lived with someone with SARS or people who have traveled to areas with reported cases of SARS.
In children, two distinct forms of the illness have been observed. Adolescents have malaise, myalgia, chills, and rigor, whereas young children have mainly cough and runny nose. In younger children the clinical course seems to be milder and the disease resolves more quickly than in adolescents or adults (Denison, 2005; Stockman, Massoudi, Helfand, and others, 2007).
Laboratory findings include lymphopenia; leukopenia; thrombocytopenia; and elevated lactate dehydrogenase, aspartate aminotransferase, and creatinine kinase levels. The most reliable laboratory diagnostic test is positive antibodies for the SARS Co-V. Chest radiographs in a substantial number of patients reveal focal interstitial infiltrates that progress to more generalized, patchy interstitial infiltrates.
Treatment of SARS involves predominantly supportive care measures. Other therapies such as antibiotics, antiviral drugs such as ribavirin, and steroids have been used with mixed results (O’Connor, 2003).
Nursing Care Management.: The Centers for Disease Control and Prevention recommends that patients with SARS receive the same treatment as any patient with serious community-acquired atypical pneumonia. This includes the use of strict hand washing, contact precautions, and airborne precautions (e.g., an isolation room with negative pressure relative to the surrounding area and the use of an N95 filtering disposable respirator for persons entering the room). Recommendations for stopping the spread of SARS have also been developed. When triaging patients, nurses should place a surgical mask on any patient who has had close contact with someone who has SARS or who has a history of international travel to an area with cases of SARS. Health care workers who have had high-risk, unprotected exposure to SARS should be excluded from duty and remain home from work to monitor their health for 10 days.
Avian Influenza Virus
Several types of influenza were identified in Asian countries that caused mild to severe disease in adults and children. The avian influenza that has resulted in several deaths in Hong Kong, Vietnam, and Thailand has been identified as subtypes H5 and H7 and has as its host chickens and wild ducks, in which the mortality rates range from 90% to 100% (Lee and Krilov, 2005). The virus has also been reported to spread among other animals such as pigs and tigers. In humans the viral manifestations of avian influenza often consist of fever and respiratory symptoms—sore throat, rhinorrhea, and cough—occurring within 3 to 5 days of illness (Chokephaibulkit, 2004). Laboratory findings include leukopenia and thrombocytopenia, and moderately elevated liver transaminases are often identified. Patients may rapidly progress to ARDS with acute lung injury. In some children the virus is manifest only as an eye infection (conjunctivitis).
Treatment is aimed at prompt diagnosis and intervention to reduce the onset of ARDS. The virus may respond to influenza drugs such as amantadine, rimantadine, oseltamivir, and zanamivir, but cases of avian flu in Southeast Asia were resistant to amantadine and rimantadine (Lee and Krilov, 2005). Rimantadine is not indicated for children. At present laboratory testing in the United States is indicated only in the case of a hospitalized patient with a severe respiratory illness without a diagnosis who has traveled to a country with documented avian influenza (Lee and Krilov, 2005). To obtain updated information on the emergence and progress in treatment of these and other respiratory viruses, the reader is encouraged to visit the Centers for Disease Control and Prevention website.*
Bacterial Pneumonia
S. pneumoniae is the most common bacterial pathogen responsible for community-acquired pneumonia in both children and adults (Rafei and Lichenstein, 2006). Other bacteria that cause pneumonia in children are group A streptococcus, S. aureus, M. catarrhalis, M. pneumoniae, and C. pneumoniae.
Beyond the neonatal period, bacterial pneumonias display distinct clinical patterns that facilitate their differentiation from other forms of pneumonia. The onset of illness is abrupt and generally follows a viral infection that disturbs the natural defense mechanisms of the upper respiratory tract.
The child with bacterial pneumonia usually appears ill. Symptoms include fever, malaise, rapid and shallow respirations, cough, and chest pain. The pain of pneumonia may be referred to the abdomen and confused with appendicitis. Chills and meningeal symptoms (meningism) are common.
Most older children with pneumonia can be treated at home if the condition is recognized and treatment is initiated early. Antibiotic therapy, bed rest, liberal oral intake of fluid, and administration of an antipyretic for fever are the principal therapeutic measures. Follow-up examination is recommended for small infants and toddlers. Hospitalization is indicated when pleural effusion or empyema accompanies the disease, in situations where compliance with therapy is estimated to be poor, in infants less than 1 month old, and when there are chronic illnesses such as congenital heart disease or BPD (Rafei and Lichenstein, 2006). IV fluids may be necessary to ensure adequate hydration, and oxygen is required if the child is in respiratory distress; some children may require initial therapy with parenteral antibiotics due to the severity of illness.
Complications.: At present the classic features and clinical course of pneumonia are seen infrequently because of early and vigorous antibiotic and supportive therapy. However, some children, especially infants, with staphylococcal pneumonia develop empyema, pyopneumothorax, or tension pneumothorax. AOM and pleural effusion are common in children with pneumococcal pneumonia.
Continuous closed chest drainage may be instituted when purulent fluid is aspirated. If a large amount of purulent drainage is obtained, an appropriate antibiotic is instilled into the chest cavity, and chest drainage is discontinued for approximately 1 hour after the instillation. Closed drainage is continued until drainage fluid is free of pathogens, which rarely requires more than 5 to 7 days. Sometimes, repeated pleural taps are sufficient to remove fluid; however, if the purulent drainage accumulates rapidly and is highly viscous, continuous drainage is preferred. Thoracotomy with open debridement of the infected lung tissue may be required; if empyema and pneumothorax tend to recur, a partial thoracoscopic lobectomy may be performed.
Prognosis.: The prognosis for pneumonia is generally good, with rapid recovery when symptoms are recognized and treated early. Streptococcal infections vary in duration but usually resolve spontaneously. The course of staphylococcal pneumonia is generally prolonged. The prognosis varies with the length of illness before treatment is begun, although early recognition and treatment are usually effective.
Prevention.: The use of the heptavalent pneumococcal vaccine (PCV; Prevnar) is recommended for infants and children younger than 23 months of age to be administered at 2, 4, 6, 12, and 15 months of age; studies have demonstrated a decrease in pneumococcal pneumonia in children less than 24 months. The polyvalent pneumococcal vaccine (PPV) provides protection from pneumococcal serotypes in children 24 months old and older (American Academy of Pediatrics, 2006b). (See Immunizations, Chapter 10.)
Nursing Care Management
For the child being cared for at home the nurse educates the parent regarding antibiotic and antipyretic administration, assessment of respiratory status, and oral fluid intake. If the child is ill, solid foods may be rejected; fluid intake is encouraged until the child feels well enough to eat solids. Parents are reassured that the child’s appetite will return once the acute phase of the illness has passed. If the cough is disturbing, judicious use of antitussives, especially at bed time, is often helpful. Most sick children are adept at self-regulation of activity and rest; parents are encouraged to allow the child appropriate rest and discourage vigorous activities until the child has been afebrile for 24 hours or more. Return to school or daycare is usually permitted according to the type of pneumonia, severity of illness, and practitioner recommendation. It should be emphasized that the infection may be transmitted to other children with close contact.
Nursing care of the hospitalized child with pneumonia is primarily supportive and symptomatic but necessitates thorough respiratory assessment, antibiotics, and evaluation of hydration status; supplemental oxygen may be required if oxygenation status is compromised. The child’s respiratory rate and oxygenation status, as well as vital signs, pain level, and general disposition and level of activity, are frequently assessed. Isolation procedures are implemented according to hospital policy, but standard and contact precautions are recommended initially for all children with a URI until the exact cause is known. To prevent dehydration, fluids are frequently administered intravenously during the acute phase.
If needed, supplemental oxygen may be administered by nasal cannula or face mask (or face tent [bucket]); small infants may be given humidified oxygen via a plastic head hood or rarely via a mist tent. Children are usually more comfortable in a semierect position (Fig. 23-3) but should be allowed to determine the position of comfort. Lying on the affected side (if pneumonia is unilateral) splints the chest on that side and reduces the pleural rubbing that often causes discomfort. Fever is controlled by the cool environment and administration of antipyretic drugs.

FIG. 23-3 Child placed in semierect position is often more comfortable, and this position enhances diaphragmatic expansion.
Children, especially infants, with ineffectual cough or difficulty handling secretions require suctioning to maintain a patent airway. A simple bulb suction syringe is usually sufficient for clearing the nares and nasopharynx of infants, but mechanical suction should be readily available if needed. A noninvasive suction device may be used to suction the infant’s nares without the danger of causing nasal trauma; the device may be connected to mechanical suction for best results. Older children can usually handle secretions without assistance. Postural drainage, CPT, and nebulized bronchodilator treatments may be prescribed depending on the child’s condition.
The hospitalized child may be apprehensive, and the treatments and tests are frightening and stress producing. It is important to involve the entire family in the care as appropriate and to encourage questions and facilitate effective communication. Allowing the child to be involved in regular activities such as quiet play may help reduce the anxiety of hospitalization and separation from friends and family. Reducing anxiety and apprehension reduces psychologic distress in the child, and when the child is more relaxed, the respiratory efforts are lessened. Easing respiratory efforts makes the child less apprehensive, and encouraging the presence of the caregiver provides the child with a source of comfort and support.
OTHER INFECTIONS OF THE RESPIRATORY TRACT
Pertussis, or whooping cough, is an acute respiratory tract infection caused by Bordetella pertussis, which in the past primarily occurred in children younger than 4 years of age who were not immunized. It is highly contagious and is particularly threatening in young infants, who have a higher morbidity and mortality rate. Infants less than 6 months of age may not come in to the practitioner with the typical cough; in this age-group, apnea is a common presenting manifestation (American Academy of Pediatrics, 2006b). Likewise, older children are known to manifest the disease with a persistent cough and the absence of the characteristic whoop (see Table 14-1 for signs, symptoms, and management of pertussis). The incidence is highest in the spring and summer months, and a single attack confers lifetime immunity. The resurgence of pertussis in the United States, particularly among children 10 years old and older, has prompted concerns of the long-term effects of the pertussis vaccine. Consequently two acellular pertussis booster vaccines have been approved for children: Boostrix (for children ages 10 to 18 years) and Adacel (for persons ages 11 to 64 years). (See also Immunizations, Chapter 10.)
 IN TEXT
IN TEXT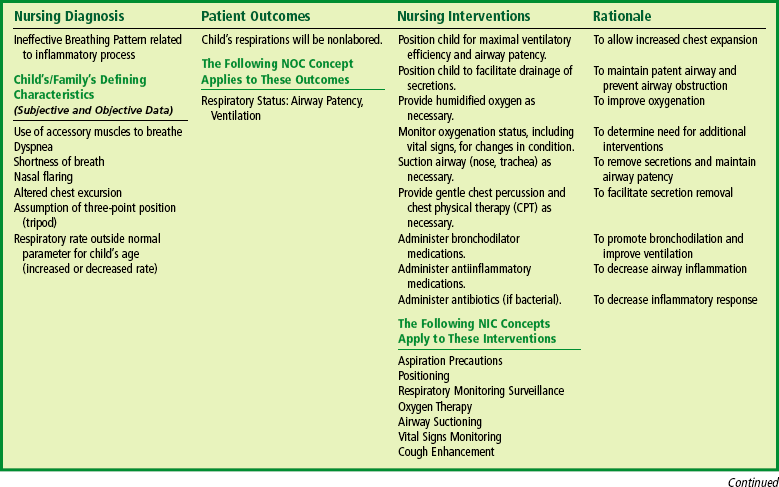
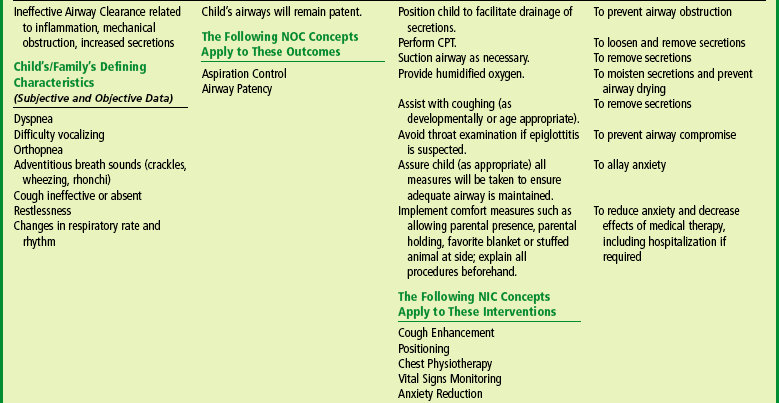
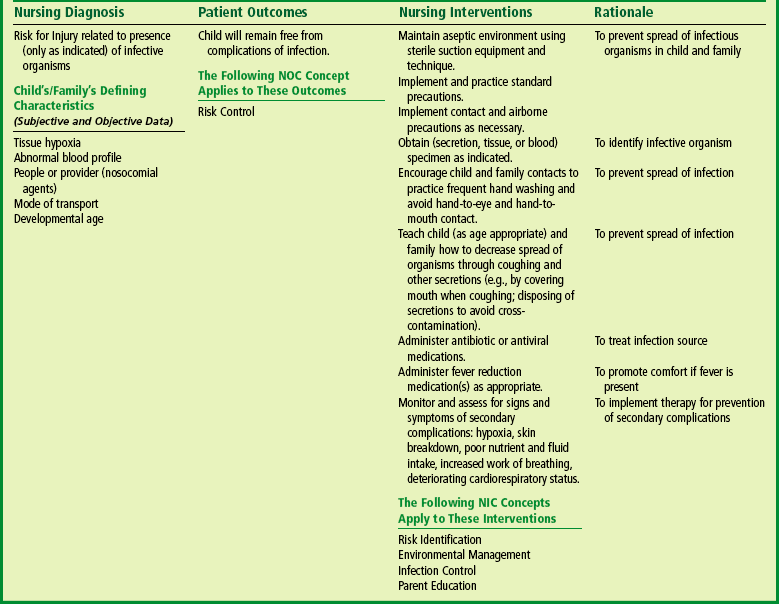
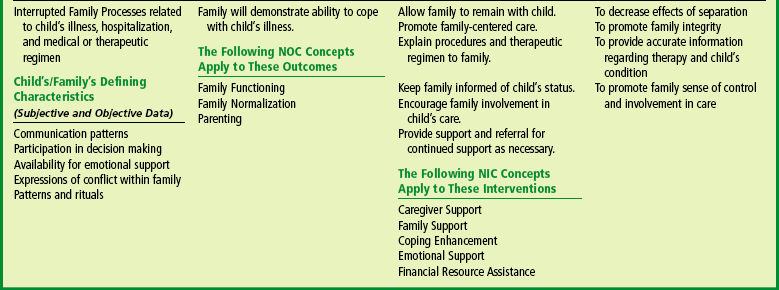

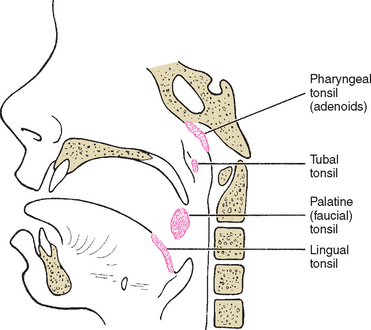
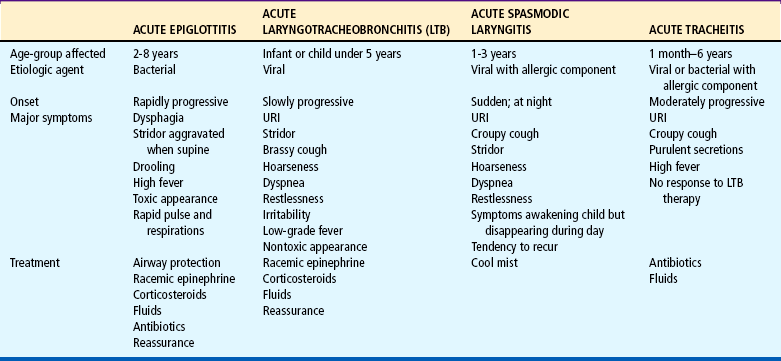
 CRITICAL THINKING EXERCISE
CRITICAL THINKING EXERCISE