Impact of Cognitive or Sensory Impairment on the Child and Family
On completion of this chapter the reader will be able to:
 Define the classifications of intellectual disability.
Define the classifications of intellectual disability.
 Outline nursing interventions for the child with cognitive impairment that promote optimal development, including during hospitalization.
Outline nursing interventions for the child with cognitive impairment that promote optimal development, including during hospitalization.
 Identify the major biologic and cognitive characteristics of the child with Down syndrome.
Identify the major biologic and cognitive characteristics of the child with Down syndrome.
 Outline nursing interventions for the child with Down syndrome.
Outline nursing interventions for the child with Down syndrome.
 Identify the major characteristics associated with fragile X syndrome.
Identify the major characteristics associated with fragile X syndrome.
 List the general classifications of hearing impairment and the effect on speech.
List the general classifications of hearing impairment and the effect on speech.
 Outline nursing interventions for the child with hearing impairment, including during hospitalization.
Outline nursing interventions for the child with hearing impairment, including during hospitalization.
 List the common types of visual disorders in children.
List the common types of visual disorders in children.
 Outline nursing interventions for the child with visual impairment, including during hospitalization.
Outline nursing interventions for the child with visual impairment, including during hospitalization.
 Outline nursing interventions for the child with retinoblastoma.
Outline nursing interventions for the child with retinoblastoma.
 Outline nursing interventions for the child with an autism spectrum disorder.
Outline nursing interventions for the child with an autism spectrum disorder.
COGNITIVE IMPAIRMENT
Cognitive impairment (CI) is a general term that encompasses any type of mental difficulty or deficiency. In this chapter the term is used synonymously with intellectual disability (mental retardation). Although the needs and concerns of the family are a primary focus throughout the chapter, the reader is encouraged to review Chapter 18, which details the family’s adjustment to disabilities in general.
The definition of intellectual disability in children consists of three components: intellectual functioning, functional strengths and weaknesses, and age younger than 18 years at time of diagnosis. Intellectual functioning is measured by the intelligence quotient (IQ) of 70 to 75 or below. The child with an intellectual disability must demonstrate functional impairment in at least two of 10 different adaptive skill areas: communication, self-care, home living, social skills, leisure, health and safety, self-direction, functional academics, community use, and work (American Psychiatric Association, 2000). The classification system by the American Association on Intellectual and Developmental Disabilities allows for identification of the individual’s specific needs in four established dimensions of care (Box 19-1). Careful evaluation to identify the needs of individuals with CI is focused on promoting habilitation for each person. It is anticipated that the functional capabilities of children with CI will improve over time when support is provided.
Diagnosis and Classification
The diagnosis of CI is usually made after a period of suspicion, by professionals or the family, that the child’s developmental progress is delayed. In some cases it is confirmed at birth because of recognition of distinct syndromes, such as Down syndrome and fetal alcohol syndrome. At the other extreme, the diagnosis is made when problems such as speech delays arouse concern. In all cases a high index of suspicion for developmental delay and behavioral signs (Box 19-2) is necessary for early diagnosis; routine developmental screening can assist in early identification (see Chapter 5). Delays are typically seen in gross and fine motor and speech development, although the latter is most predictive. Developmental delay can be described as any significant lag in a child’s physical, cognitive, behavioral, emotional, or social development, when compared against developmental norms. CI is a permanent impairment encompassing cognitive ability and adaptive behavior that are functioning significantly below average (see Box 19-2). In the absence of clear-cut evidence of CI, it is more appropriate to use a diagnosis of developmental delay (Biasini, Grupe, Huffman, and others, 1999).
Results of standardized tests are used in making the diagnosis of intellectual disability (mental retardation) based on cognitive deficits. Tests for assessing adaptive behaviors include the Vineland Social Maturity Scale and the AAMR Adaptive Behavior Scale. Informal appraisal of adaptive behavior may be made by those fully acquainted with the child (e.g., teachers, parents, other care providers). Frequently these observations lead parents to seek evaluation of the child’s development.
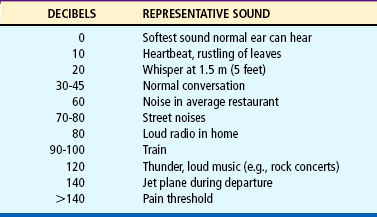
A more useful approach for clinical application is classification based on educational potential or symptom severity. For educational purposes the term educable mentally retarded (EMR) corresponds to the mildly impaired group, which constitutes about 85% of all people with CI. Trainable mentally retarded (TMR) generally applies to children with moderate levels of CI and accounts for about 10% of the intellectually disabled population (American Psychiatric Association, 2000; Walker and Johnson, 2006) (Table 19-1). Although nurses may be familiar with the approximate range of IQ for classifying severity, they should refrain from using numbers as the criterion for assessing or evaluating the child’s abilities, since numbers are of little value in counseling parents or training these children.
TABLE 19-1
Classification of Cognitive Impairment
*Data from American Psychiatric Association: Diagnostic and statistical manual of mental disorders, ed 4 (text rev) (DSM-IV TR), Washington, DC, 2000, The Association; and Rittey CD: Learning difficulties: what the neurologist needs to know, J Neurol Neurosurg Psychiatry 74(Suppl 1):30-36, 2005.
Etiology
The causes of severe CI are primarily genetic, biochemical, and infectious. Although the etiology is unknown in the majority of cases, familial, social, environmental, and organic causes may predominate. Among individuals with CI, a sizable proportion of the cases are linked to Down syndrome, fragile X syndrome, or fetal alcohol syndrome. General categories of events that may lead to CI include (Walker and Johnson, 2006; Kabra and Gulati, 2003):
 Infection and intoxication, such as congenital rubella, syphilis, maternal drug consumption (e.g., fetal alcohol syndrome), chronic lead ingestion, or kernicterus
Infection and intoxication, such as congenital rubella, syphilis, maternal drug consumption (e.g., fetal alcohol syndrome), chronic lead ingestion, or kernicterus
 Trauma or physical agent (i.e., injury to the brain suffered during the prenatal, perinatal, or postnatal period)
Trauma or physical agent (i.e., injury to the brain suffered during the prenatal, perinatal, or postnatal period)
 Inadequate nutrition and metabolic disorders, such as phenylketonuria or congenital hypothyroidism
Inadequate nutrition and metabolic disorders, such as phenylketonuria or congenital hypothyroidism
 Gross postnatal brain disease, such as neurofibromatosis and tuberous sclerosis
Gross postnatal brain disease, such as neurofibromatosis and tuberous sclerosis
 Unknown prenatal influence, including cerebral and cranial malformations, such as microcephaly and hydrocephalus
Unknown prenatal influence, including cerebral and cranial malformations, such as microcephaly and hydrocephalus
 Chromosomal abnormalities resulting from radiation; viruses; chemicals; parental age; and genetic mutations, such as Down syndrome and fragile X syndrome
Chromosomal abnormalities resulting from radiation; viruses; chemicals; parental age; and genetic mutations, such as Down syndrome and fragile X syndrome
 Gestational disorders, including prematurity, low birth weight, and postmaturity
Gestational disorders, including prematurity, low birth weight, and postmaturity
 Psychiatric disorders that have their onset during the child’s developmental period up to age 18 years, such as autism spectrum disorders
Psychiatric disorders that have their onset during the child’s developmental period up to age 18 years, such as autism spectrum disorders
 Environmental influences, including evidence of a deprived environment associated with a history of intellectual disability among parents and siblings
Environmental influences, including evidence of a deprived environment associated with a history of intellectual disability among parents and siblings
NURSING CARE OF CHILDREN WITH IMPAIRED COGNITIVE FUNCTION
Nurses play a major role in identifying children with CI. In the newborn and early infancy periods, few signs are present, with the exception of Down syndrome (p. 619). After this age, however, delayed developmental milestones are the major clues to CI. In addition, nurses must have a high index of suspicion for early behavior patterns that may suggest CI (see Box 19-2). Parental concerns, such as delayed development compared with siblings, need to be taken seriously. All children should receive regular developmental assessment, and the nurse is often the person responsible for performing such assessments (see Chapter 5). When delays are found, the nurse must use sensitivity and discretion in revealing this finding to parents (see Nursing Care Plan).
Educate Child and Family.: To teach children with CI, it is necessary to investigate their learning abilities and deficits. This is important for the nurse who may be involved in a home care program or who may be caring for the child in a health care setting. The nurse who understands how these children learn can effectively teach them basic skills or prepare them for various health-related procedures.
Children with CI have a marked deficit in their ability to discriminate between two or more stimuli because of difficulty in recognizing the relevance of specific cues. However, these children can learn to discriminate if the cues are presented in an exaggerated, concrete form and if all extraneous stimuli are eliminated. For example, the use of colors to emphasize visual cues or the use of singing or rhymes to stress auditory cues can help them learn. Their deficit in discrimination also implies that concrete ideas are learned much more effectively than abstract ideas. Therefore demonstration is preferable to verbal explanation, and learning should be directed toward mastering a skill rather than understanding the scientific principles underlying a procedure.
Another cognitive deficit is in short-term memory. Whereas children of average intelligence can remember several words, numbers, or directions at one time, children with CI are less able to do so. Therefore they need simple, one-step directions. Learning through a step-by-step process requires a task analysis, in which each task is separated into its necessary components and each step is taught completely before proceeding to the next activity.
One critical area of learning that has had a tremendous impact on education for cognitively impaired individuals is motivation. Programs based on the motivational principles of behavior modification, employing positive reinforcement for specific tasks or behaviors, have demonstrated marked improvement in children’s ability to learn. Advances in technology have greatly aided in providing reinforcement, especially in children who are severely disabled and who may have physical disabilities that limit their range of capabilities. For example, with the use of specially designed switches, children are given control of some event in the environment, such as turning on the television (Fig. 19-1). The television picture becomes reinforcement for activating the switch. Repetitive use of these switches provides an early, simplistic association with a technical device that may progress to increasingly complex aids.
Early intervention program is a systematic program of therapy, exercises, and activities designed to address developmental delays in disabled children to help achieve their full potentials (American Academy of Pediatrics, 2001; National Down Syndrome Society, 2006). There is considerable evidence that these programs are valuable for cognitively impaired children. Nurses working with these families need to be aware of the types of programs in their community. Under the Individuals with Disabilities Education Act (IDEA) of 1990 (Public Law 101–476), states are encouraged to provide full early intervention services and are required to provide educational opportunities for all children with disabilities from birth to 21 years of age. Services may be provided under statePrograms for Children with Special Health Needs or Head Start, or by private organizations such as National Down Syndrome Society,* Easter Seals,† or the Arc of the United States.‡ Parents should inquire about these programs by contacting the appropriate agencies. The child’s education should begin as soon as possible. As children grow older, their education should be directed toward vocational training that prepares them for as independent a lifestyle as possible within their scope of abilities.
Teach Child Self-Care Skills.: When a child with CI is born, parents need assistance in promoting normal developmental skills that are almost automatically learned by other children. These include self-care skills such as feeding, toileting, dressing, and grooming. Teaching these skills requires a basic knowledge of the developmental sequence in learning the skills demonstrated by children of average intelligence. For example, children with subaverage intelligence would not be expected to dress themselves as early as unaffected youngsters.
Teaching self-care skills also necessitates a working knowledge of the individual steps needed to master a skill. For example, before beginning a self-feeding program, the nurse performs a task analysis. After a task analysis, the child is observed in a particular situation, such as eating, to determine what skills are possessed and the child’s developmental readiness to learn the task. Family members are included in this process because their “readiness” is as important as the child’s. Numerous self-help aids are available to facilitate independence and can help eliminate some of the difficulties of learning, such as using a plate with suction cups to prevent accidental spills.§
Promote Child’s Optimal Development.: Optimal development involves more than achieving independence. It requires appropriate guidance for establishing acceptable social behavior and personal feelings of self-esteem, worth, and security. These attributes are not simply learned through a stimulation program. Rather, they must arise from the genuine love and caring that exist among family members. However, families need guidance in providing an environment that fosters optimal development. Often it is the nurse who can provide assistance in these areas of childrearing.
Another important area for promoting optimal development and self-esteem is ensuring the child’s physical well-being. Any congenital defects, such as cardiac, gastrointestinal, or orthopedic anomalies, should be repaired. Plastic surgery may be considered when the child’s appearance can be substantially improved. Dental health is significant, and orthodontic and restorative procedures can improve facial appearance immensely.
Encourage Play and Exercise.: Children who are cognitively impaired have the same needs for recreation and exercise as other children. However, because of the children’s slower development, parents may be less aware of the need to provide such activities. Therefore the nurse guides parents toward selection of suitable play and exercise activities. Because play has been discussed for children in each age-group in earlier chapters, only the exceptions are presented here (Fig. 19-2).
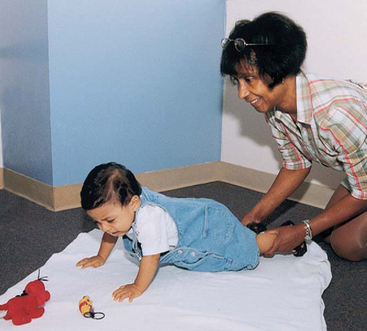
FIG. 19-2 Placing an attractive object outside the child’s reach encourages crawling movements. (Courtesy James DeLeon, Texas Children’s Hospital, Houston.)
The type of play is based on the child’s developmental age, although the need for sensorimotor play may be prolonged for several years. Parents should use every opportunity to expose the child to as many different sounds, sights, and sensations as possible. Appropriate play includes musical mobiles, stuffed toys, water play, floating toys, a rocking chair or horse, a swing, bells, and rattles. The child should be taken on outings, such as trips to the grocery store or shopping center; other people should be encouraged to visit in the home; and the child should be related to directly, such as by cuddling, holding, rocking, talking to the child in the en face (face-to-face) position, and giving “rides” on the parents’ shoulders.
Toys are selected for their recreational and educational value. For example, a large inflatable beach ball is a good water toy; it encourages interactive play and can be used to learn motor skills, such as balance, rocking, kicking, and throwing. A doll with removable clothes and different types of closures can help the child learn dressing skills. Musical toys that mimic animal sounds or respond with social phrases are excellent ways of encouraging speech. Toys should be simple in design so that the child can learn to manipulate them without help. For children with severe cognitive and physical impairment, electronic switches can be used to allow them to operate toys (Fig. 19-3).

FIG. 19-3 A manual switch allows a child with cognitive impairment to play with a battery-operated toy.
Suitable activities for physical activity are based on the child’s size, coordination, physical fitness and maturity, motivation, and health (Fig. 19-4). Some children may have physical problems that prevent participation in certain sports, suchas atlantoaxial instability in children with Down syndrome (p. 619). These children often have greater success in individual and dual sports than in team sports and enjoy themselves most with children of the same developmental level. The Special Olympics* provides these children with a unique competitive opportunity.
Safety is a major consideration in selecting recreational and exercise activities. For example, toys that may be appropriate developmentally may present dangers to a child who is strong enough to break them or use them incorrectly.
Provide Means of Communication.: Verbal skills are typically delayed more than other physical skills. Speech requires hearing and interpretation (receptive skills) and facial muscle coordination (expressive skills). Because both types of skills may be impaired, these children need frequent audiometric testing and should be fitted with hearing aids if indicated. In addition, they may need help in learning to control their facial muscles. For example, some children may need tongue exercises to correct the tongue thrust or gentle reminders to keep the lips closed.
Nonverbal communication may be appropriate for some of these children, and various devices are available. For the child without associated physical disabilities, a talking picture board is helpful. For children with physical limitations, several adaptations or types of communication devices are available to facilitate selection of the appropriate picture or word (Fig. 19-5). Some children may be taught sign language or Blissymbols—a highly stylized system of graphic symbols that represent words, ideas, and concepts. Although the symbols require education to learn their meaning, no reading skill is needed. The symbols are usually arranged on a board, and the person points or uses some type of selector to convey a message.
Establish Discipline.: Discipline must begin early. Limit-setting measures need to be simple, consistently applied, and appropriate for the child’s mental age. Control measures are based primarily on teaching a specific behavior rather than on understanding the reasons behind it. Stressing moral lessons is of little value to a child who lacks the cognitive skills to learn from self-criticism or from a lesson based on previous wrong-doing. Behavior modification, especially reinforcement of desired actions, and time-out are appropriate forms of behavior control.
Encourage Socialization.: Acquiring social skills is a complex task, as is learning self-care procedures. Active rehearsal with role-playing and practice sessions and positive reinforcement for desired behavior have been the most successful approaches. Parents should be encouraged early to teach their child socially acceptable behavior: waving goodbye, saying “hello” and “thank you,” responding to his or her name, greeting visitors, and sitting modestly. The teaching of socially acceptable sexual behavior is especially important to minimize sexual exploitation. Parents also need to expose the child to strangers so that he or she can practice manners, since there is no automatic transfer of learning from one situation to another.
Dressing and grooming are also important aspects of socialization. A child who is dressed in age-appropriate clothing and is well groomed is much more likely to be accepted and to develop good self-esteem. Clothes should be clean, up-to-date, and well fitted. Many attractive outfits can be adapted with self-adhering fasteners and elastic openings to facilitate self-dressing.
As soon as possible, parents should enroll the child in appropriate preschool programs. Not only do these programs provide education and training, but they also offer an opportunity for social experiences among the children. As children grow older, they should have peer experiences similar to those of other children, including group outings, sports, and organized activities such as scouts and Special Olympics. Nurses can assess the child’s abilities and encourage others (e.g., parents, teachers) to promote developmentally appropriate peer interaction (Johnson and Walker, 2006; Rehm and Bradley, 2006).
Provide Information on Sexuality.: Adolescence may be a particularly difficult time for the family, especially in terms of the child’s sexual behavior, possibility of pregnancy, future plans to marry, and ability to be independent. Frequently, little anticipatory guidance has been offered parents to prepare the child for physical and sexual maturation. The nurse can help in this area by providing parents with information about sexuality education that is geared to the child’s developmental level. For example, the adolescent girl needs a simple explanation of menstruation and instructions on personal hygiene during the menstrual cycle.
These adolescents also need practical sexual information regarding anatomy, physical development, and conception.* Because of their easy persuasion and lack of judgment, they need a well-defined, concrete code of conduct. The subtleties of social sexual behavior are less beneficial than specific instructions for handling certain situations. For example, an adolescent should be firmly told never to go alone anywhere with any person she does not know well. To protect him or her from abusive sexual activities, parents must closely observe their teenager’s activities and associates. The question of contraceptive protection for these adolescents is often a parental concern.
Parents of these adolescents are often concerned about the advisability of marriage between two individuals with an intellectual disability. There is no conclusive answer; each situation must be judged individually. In some instances marriage is possible, but parenthood may not be desirable because of the complexity of childrearing and the potential problem of perpetuating mental deficiency. The nurse should discuss this topic with parents and with the prospective couple, stressing suitable living accommodations and contraceptive methods to prevent pregnancy. If children are conceived, these parents require specialized assistance in learning to meet the needs of their offspring (Johnson and Walker, 2006).
Help Family Adjust to Future Care.: Not all families are able to cope with home care of their affected child, especially one who is severely or profoundly impaired or has multiple disabilities. Older parents may not be able to assume care responsibilities after they reach retirement or older age. For these parents, the decision regarding residential placement is a difficult one, and the availability of such facilities varies widely. The nurse working with a family should help them investigate and evaluate various programs, in addition to assisting them in adjusting to the decision for placement.
Care for Child During Hospitalization.: Caring for the child during hospitalization can be a special challenge. Frequently, nurses are unfamiliar with children who are cognitively impaired, and they may cope with their feelings of insecurity and fear by ignoring or isolating the child. Not only is this approach nonsupportive, but it may also be destructive for the child’s sense of self-esteem and optimal development, and it may hamper the parents’ ability to cope with the stress of the experience. One method that successfully avoids this nontherapeutic approach is the use of the mutual participation model in planning the child’s care. Parents are encouraged to stay with their child but should not be made to feel as if the responsibility is totally theirs.
When the child is admitted, a detailed history is taken (see Chapter 21), especially in terms of all self-care activity. During the interview the child’s developmental age is assessed. It is best to avoid asking directly about IQ levels, since this may make the parents uncomfortable and often tells little about the child’s actual abilities. Questions are approached positively. For example, rather than asking, “Is your child toilet trained yet?” the nurse may state, “Tell me about your child’s toileting habits.” The assessment should also focus on any special devices the child uses, effective measures of limit setting, unusual or favorite routines, and any behaviors that may require intervention. If the parent states that the child engages in self-injurious activities (such as head banging or self-biting), the nurse should inquire about events that precipitate them and techniques that the parents use to manage them (Bosch and Ringdahl, 2001;Walker and Johnson, 2006).
The nurse also assesses the child’s functional level of eating and playing; ability to express needs verbally; progress in toilet training; and relationship with objects, toys, and other children. The child is encouraged to be as independent as possible in the hospital.
Realizing that the child may be lonely in the hospital, the nurse makes certain that toys and other activities are provided. The child is placed in a room with other children of approximately the same developmental age, preferably a room with only two beds to avoid overstimulation. The nurse discusses with the other parents the child’s abilities and introduces the parents and children to each other. By the nurse’s example of treating the child with dignity and respect, others who may be fearful of what they do not understand are encouraged to accept the child.
Procedures are explained to the child through methods of communication that are at the appropriate cognitive level. Generally, explanations should be simple, short, and concrete, emphasizing what the child will experience physically. Demonstration either through actual practice or with visual aids is always preferable to verbal explanation. The nurse repeats instructions often and evaluates the child’s understanding by asking questions such as “What will it feel like?” “Show me how you must lie,” or “Where will the dressing be?” Parents are included in preprocedural teaching for their own learning and to help the nurse learn effective methods of communicating with the child.
During hospitalization the nurse should also focus on growth-promoting experiences for the child. For example, hospitalization may be an excellent opportunity to emphasize to parents abilities that the child does have but has not had the opportunity to practice, such as self-dressing. It may also be an opportunity for social experiences with peers, group play, or new educational and recreational activities. For example, one child who had the habit of screaming and kicking demonstrated a definite decrease in those behaviors after he learned to pound pegs and use a punching bag. Through social services the parents may become aware of specialized programs for the child. Hospitalization may also offer parents a respite from everyday care responsibilities and an opportunity to discuss their feelings with a concerned professional.
Assist in Measures to Prevent Cognitive Impairment: Besides having a responsibility to families with a child with CI, nurses also need to be involved in programs aimed at preventing CI. Many of the familial, social, and environmental factors known to cause mild impairment are preventable. Counseling and education can reduce or eliminate such factors (e.g., poor nutrition, cigarette smoking, chemical abuse), which increase the risk of prematurity and intrauterine growth restriction. Interventions are directed toward improving maternal health by educating women regarding the dangers of chemicals, including prenatal alcohol exposure, which affects organogenesis, craniofacial development, and cognitive ability (Wilton and Plane, 2006). Other preventive strategies that play an important role include adequate prenatal care; optimal medical care of high-risk newborns; rubella immunization; genetic counseling and prenatal screening, especially in terms of Down or fragile X syndrome; use of folic acid supplements to prevent neural tube defects during pregnancy and during the childbearing years; newborn screening for treatable inborn errors of metabolism, such as congenital hypothyroidism, phenylketonuria, and galactosemia; and early appropriate therapies and rehabilitation services for children with developmental disabilities.
DOWN SYNDROME
Down syndrome is the most common chromosomal abnormality of a generalized syndrome, occurring in one in every 800 to 1000 live births (National Down Syndrome Society, 2006; Skotko, 2005). It occurs slightly more often in Caucasians than in African-Americans, although the incidence is unchanged in various socioeconomic classes.
Etiology
The cause of Down syndrome is not known, but evidence from cytogenetic and epidemiologic studies supports the concept of multiple causality. Approximately 95% of all cases of Down syndrome are attributable to an extra chromosome 21 (group G), thus the name nonfamilial trisomy 21 (National Down Syndrome Society, 2006; Walker and Johnson, 2006). Although children with trisomy 21 are born to parents of all ages, there is a statistically greater risk in older women, particularly those older than 35 years of age. For example, in women 35 years of age the chance of conceiving a child with Down syndrome is about one in 400 live births, but in women age 40 it is about one in 110. However, the majority (about 80%) of infants with Down syndrome are born to women younger than age 35. About 3% to 4% of the cases may be caused by translocation of chromosomes 15 and 21 or 22. This type of genetic aberration is usually hereditary and is not associated with advanced parental age. From 1% to 2% of affected persons demonstrate mosaicism, which refers to mixture of normal and abnormal cell types. The degree of cognitive and physical impairment is related to the percentage of cells with the abnormal chromosome makeup.
Diagnostic Evaluation
Down syndrome can usually be diagnosed by the clinical manifestations alone (Box 19-3 and Fig. 19-6), but a chromosome analysis should be done to confirm the genetic abnormality.

FIG. 19-6 Down syndrome in an infant. Note small, square head with upward slant to eyes, flat nasal bridge, protruding tongue, mottled skin, and hypotonia.
Several physical problems are associated with Down syndrome. Many of these children have congenital heart malformations, the most common being septal defects. Respiratory tract infections are prevalent and, when combined with cardiac anomalies, are the chief causes of death, particularly during the first year of life. Hypotonicity of chest and abdominal muscles and dysfunction of the immune system probably predispose the child to the development of respiratory tract infection. Other physical problems include thyroid dysfunction, especially congenital hypothyroidism, and an increased incidence of leukemia.
Therapeutic Management
Although no cure exists for Down syndrome, a number of therapies are advocated, such as surgery to correct serious congenital anomalies (e.g., heart defects, strabismus). These children also benefit from an evaluative echocardiogram soon after birth and regular medical care. Evaluation of sight and hearing is essential, and treatment of otitis media is required to prevent auditory loss, which can influence cognitive function. Periodic testing of thyroid function is recommended, especially if growth is severely delayed. Children participating in sports that may involve stress on the head and neck, such as gymnastics, diving, butterfly stroke in swimming, high jump, and soccer, should be evaluated radiologically for atlantoaxial instability. Symptoms of the disorder include neck pain, weakness, and torticollis. Affected children are at risk for spinal cord compression.
Prognosis.: Life expectancy for those with Down syndrome has improved in recent years but remains lower than for the general population. More than 80% survive to age 55 years and beyond. As the prognosis continues to improve for these individuals, it will be important to provide for their long-term health care, social, and leisure needs (National Down Syndrome Society, 2006; Van Riper, 2003). (See Ethical Case Study.)
Nursing Care Management
Support Family at Time of Diagnosis.: Because of the unique physical characteristics, the infant with Down syndrome is usually diagnosed at birth, and parents should be informed of the diagnosis at this time. Parents usually prefer that both of them be present during the informing interview so that they can support one another emotionally. They appreciate receiving reading material about the syndrome* and being referred to others for help or advice, such as parent groups or professional counseling.
After parents are aware of the diagnosis, they are confronted with the crisis of losing their perfect or dream child and grieving for and accepting their reality child. Consequently, the parents’ responses to the child may greatly influence decisions regarding future care. Whereas some families willingly take the child home, others consider immediate residential placement. The nurse must carefully answer questions regarding developmental potential. Institutionalization is no longer an option. For families unable or unready to choose taking the newborn home, specialized foster care or adoption are other options (see Critical Thinking Exercise).
Assist Family in Preventing Physical Problems.: Many of the physical characteristics of Down syndrome present nursing problems. The hypotonicity of muscles and hyperextensibility of joints complicate positioning. The limp, flaccid extremities resemble the posture of a rag doll; as a result, holding the infant is difficult and cumbersome. Sometimes parents perceive this lack of molding to their bodies as evidence of inadequate parenting. The extended body position promotes heat loss because more surface area is exposed to the environment. Parents are encouraged to swaddle or wrap the infant tightly in a blanket before picking up the child to provide security and warmth. The nurse also discusses with parents their feelings concerning attachment to the child, emphasizing that the child’s lack of clinging or molding is a physical characteristic, not a sign of detachment or rejection.
Decreased muscle tone compromises respiratory expansion. In addition, the underdeveloped nasal bone causes a chronic problem of inadequate drainage of mucus. The constant stuffy nose forces the child to breathe by mouth, which dries the oropharyngeal membranes, increasing the susceptibility to upper respiratory tract infections. Measures to lessen these problems include clearing the nose with a bulb-type syringe, rinsing the mouth with water after feedings, increasing fluid intake, and using a cool-mist vaporizer to keep the mucous membranes moist and the secretions liquefied. Other helpful measures include changing the child’s position frequently, performing postural drainage with percussion if necessary, practicing good hand washing, and properly disposing of soiled articles such as tissues. If antibiotics are ordered, the nurse stresses the importance of completing the full course of therapy for successful eradication of the infection and prevention of growth of resistant organisms.
Inadequate drainage resulting in pooling of mucus in the nose also interferes with feeding. Because the child breathes by mouth, sucking for any length of time is difficult. When eating solids, the child may gag on the food because of mucus in the oropharynx. Parents are advised to clear the nose before each feeding; give small, frequent feedings; and allow opportunities for rest during mealtime.
The protruding tongue also interferes with feeding, especially of solid foods. Parents need to know that the tongue thrust is not an indication of refusal to feed, but a physiologic response. Parents are advised to use a small but long, straight-handled spoon to push the food toward the back and side of the mouth. If food is thrust out, it should be refed.
Dietary intake needs supervision. Decreased muscle tone affects gastric motility, predisposing the child to constipation. Dietary measures such as increased fiber and fluid promote evacuation. The child’s eating habits may need careful scrutiny to prevent obesity. Height and weight measurements should be obtained on a serial basis, especially during infancy. Because these children grow more slowly than the general pediatric population’s trends, special growth charts developed for these children should be used (American Academy of Pediatrics, 2001).
During infancy the child’s skin is pliable and soft. However, it gradually becomes rough and dry and is prone to cracking and infection. Skin care involves the use of minimum soap and application of lubricants. Lip balm is applied to the lips, especially when the child is outdoors, to prevent excessive chapping.
Assist in Prenatal Diagnosis and Genetic Counseling.: Prenatal diagnosis of Down syndrome is possible through chorionic villus sampling and amniocentesis, since chromosome analysis of fetal cells can detect the presence of trisomy or translocation. However, analysis will not identify sporadic cases in young women when there is no indication for prenatal testing. Testing for low maternal serum α-fetoprotein, high chorionic gonadotropin, low unconjugated estriol levels, and maternal serum fetal cell markers may identify an affected fetus in women, who can then undergo amniocentesis (National Down Syndrome Society, 2006; Peterson, 2006; Hall, 2004).
Prenatal testing and genetic counseling should be offered to women of advanced maternal age or those who have a family history of the disorder. If prenatal testing indicates the fetus is affected, the nurse must allow the parents to express their feelings concerning elective abortion and support their decision to terminate or proceed with the pregnancy.
FRAGILE X SYNDROME
Fragile X syndrome is the most common inherited cause of CI and the second most common genetic cause of CI after Down syndrome. It has been described in all ethnic groups and races; the incidence of affected males is one in 3600; the incidence of affected females is one in 4000 to 6000; and the incidence of carrier females is one in 100 to 260 and the incidence of carrier males is one in 250 to 800 worldwide (National Fragile X Foundation, 2006; Phalen, 2005; Crawford, 2001).
The syndrome is caused by an abnormal gene on the lower end of the long arm of the X chromosome. Chromosome analysis may demonstrate a fragile site (a region that fails to condense during mitosis and is characterized by a nonstaining gap or narrowing) in the cells of affected males and females and in carrier females. This fragile site has been determined to be caused by a gene mutation that results in excessive repeats of nucleotide in a specific deoxyribonucleic acid (DNA) segment of the X chromosome. The number of repeats in a normal individual is between six and 50. An individual with 50 to 200 base-pair repeats is said to have a permutation and is therefore a carrier. When passed from a parent to a child, these base-pair repeats can expand from 200 or more, which is termed a full mutation. This expansion occurs only when a carrier mother passes the mutation to her offspring; it does not occur when a carrier father passes the mutation to his daughters.
The inheritance pattern has been termed X-linked dominant with reduced penetrance. This is in distinct contrast to the classic X-linked recessive pattern in which all carrier females are normal, all affected males have symptoms of the disorder, and no males are carriers. Consequently, genetic counseling of affected families is more complex than that for families with a classic X-linked disorder, such as hemophilia. Prenatal diagnosis of the fragile X gene mutation is now possible with direct DNA testing in a family with an established history, using amniocentesis or chorionic villus sampling (Centers for Disease Control and Prevention, 2002; Crawford, 2001). Both affected sexes are fertile and therefore capable of transmitting the fragile X disorder.
Clinical Manifestations
The classic trend of physical findings in adult men with fragile X syndrome consists of a long face with a prominent jaw (prognathism); large, protruding ears; and large testes (macroorchidism). In prepubertal children, however, these features may be less obvious, and behavioral manifestations may initially suggest the diagnosis (Box 19-4). In carrier females the clinical manifestations are extremely varied.
Therapeutic Management
No cure exists for fragile X syndrome. Medical treatment may include the use of serotonin agents such as carbamazepine (Tegretol) or fluoxetine (Prozac) to control violent temper outbursts and the use of central nervous system stimulants or clonidine (Catapres) to improve attention span and decrease hyperactivity. Protein replacement and gene therapy are treatment options that are being investigated (Phalen, 2005).
All affected children require referral to early intervention program (speech and language therapy, occupational therapy, and special education assistance) and multidisciplinary assessment, including cardiology (i.e., mitral valve prolapse), neurology (i.e., seizures), and orthopedic anomalies (Alanay, Unal, Turanh, and others, 2007).
Nursing Care Management
Because CI is a fairly consistent finding in individuals with fragile X syndrome, the care given to these families is the same as for any child with CI. Because the disorder is hereditary, genetic counseling is necessary to inform parents and siblings of the risks of transmission. In addition, any male or female with unexplained or nonspecific mental impairment should be referred for genetic testing and, if needed, counseling. Families with a member affected by the disorder should be referred to the National Fragile X Foundation.*
SENSORY IMPAIRMENT
Hearing impairment is one of the most common disabilities in the United States. An estimated three in 1000 well infants have hearing loss of varying degrees (Gregg, Wiorek, and Arvedson, 2004). For infants admitted to the neonatal intensive care unit, the incidence rises sharply to approximately two to four per 100 neonates (Cunningham, Cox, and Committee on Practice and Ambulatory Medicine and the Section on Otolaryngology and Bronchoesophagology, 2003; American Academy of Pediatrics, 1999). In the United States there are about 1 million children with hearing impairment ranging in age from birth to 21 years, and almost a third of these children have other disabilities, such as visual or cognitive deficits.
Definition and Classification
Hearing impairment is a general term indicating disability that may range in severity from mild to profound and includes the subsets of deaf and hard-of-hearing. Deaf refers to a person whose hearing disability precludes successful processing of linguistic information through audition, with or without a hearing aid. Hard-of-hearing refers to a person who, generally with the use of a hearing aid, has residual hearing sufficient to enable successful processing of linguistic information through audition. Other terms, such as deaf and dumb, mute, or deaf-mute, are unacceptable. Hearing-impaired persons are not dumb and, if mute, have no physical speech defect other than that caused by the inability to hear.
Hearing defects may be classified according to etiology, pathology, or symptom severity. Each is important in terms of treatment, possible prevention, and rehabilitation.
Etiology.: Hearing loss may be caused by a number of prenatal and postnatal conditions. These include a family history of childhood hearing impairment, anatomic malformations of the head or neck, low birth weight, severe perinatal asphyxia, perinatal infection (cytomegalovirus, rubella, herpes, syphilis, toxoplasmosis, bacterial meningitis), chronic ear infection, cerebral palsy, Down syndrome, or administration of ototoxic drugs (Smith, Bale, and White, 2005; Gregg, Wiorek, and Arvedson, 2004).
In addition, high-risk neonates who survive formerly fatal prenatal or perinatal conditions may be susceptible to hearing loss from the disorder or its treatment. For example, sensorineural hearing loss may be a result of continuous humming noises or high noise levels associated with incubators, oxygen hoods, or intensive care units, especially when combined with the use of potentially ototoxic antibiotics.
Environmental noise is a special concern. Sounds loud enough to damage sensitive hair cells of the inner ear can produce irreversible hearing loss. Very loud, brief noise, such as gunfire, can cause immediate, severe, and permanent loss of hearing. Longer exposure to less intense but still hazardous sounds, such as loud persistent music via headphones, sound systems, concerts, or industrial noises, can also produce hearing loss (Daniel, 2007; Kenna, 2004; Segal, Eviatar, Lapinsky, and others, 2003). Loud noises combined with the toxic substances of smoking produces a synergistic effect on hearing that causes hearing loss (Mizoue, Miyamoto, and Shimizu, 2003).
Pathology.: Disorders of hearing are divided according to the location of the defect. Conductive or middle-ear hearing loss results from interference of transmission of sound to the middle ear. It is the most common of all types of hearing loss and most frequently a result of recurrent serous otitis media. Conductive hearing impairment involves mainly interference with loudness of sound.
Sensorineural hearing loss, also called perceptive or nerve deafness, involves damage to the inner ear structures or the auditory nerve. The most common causes are congenital defects of inner ear structures or consequences of acquired conditions, such as kernicterus, infection, administration of ototoxic drugs, or exposure to excessive noise. Sensorineural hearing loss results in distortion of sound and problems in discrimination. Although the child hears some of everything going on around him or her, the sounds are distorted, severely affecting discrimination and comprehension.
Mixed conductive-sensorineural hearing loss results from interference with transmission of sound in the middle ear and along neural pathways. It frequently results from recurrent otitis media and its complications.
Central auditory imperception includes all hearing losses that are not linked to defects in the conductive or sensorineural structures. They are usually divided into organic or functional losses. In the organic type of central auditory imperception, the defect involves the reception of auditory stimuli along the central pathways and the expression of the message into meaningful communication. Examples are aphasia, the inability to express ideas in any form, either written or verbal; agnosia, the inability to interpret sound correctly; and dysacusis, difficulty in processing details or discriminating among sounds. In the functional type of hearing loss, no organic lesion exists to explain a central auditory loss. Examples of functional hearing loss are conversion hysteria (an unconscious withdrawal from hearing to block remembrance of a traumatic event), infantile autism, and childhood schizophrenia.
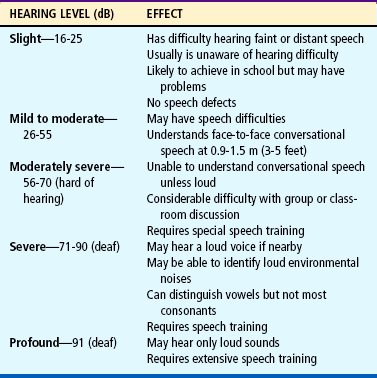
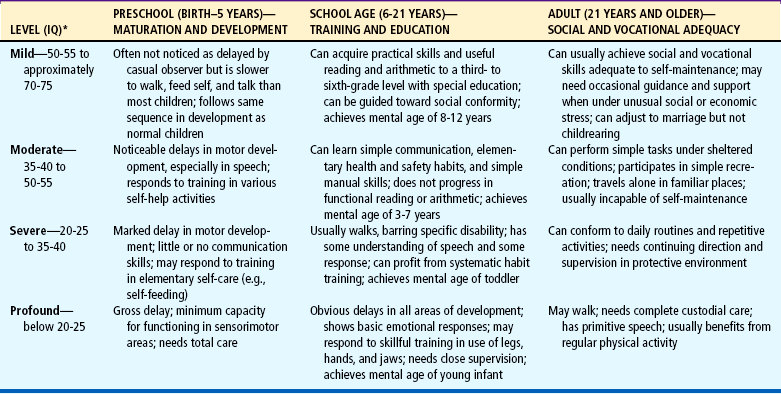
Symptom Severity.: Hearing impairment is expressed in terms of a decibel (dB), a unit of loudness (Table 19-2); hearing is measured at various frequencies, such as 500, 1000, and 2000 cycles/sec, the critical listening speech range. Hearing impairment can be classified according to hearing threshold level (the measurement of an individual’s hearing threshold by means of an audiometer) and the degree of symptom severity as it affects speech (Table 19-3). These classifications offer only general guidelines regarding the effect of the impairment on any individual child, since children differ greatly in their ability to use residual hearing.
Therapeutic Management
Conductive Hearing Loss.: Treatment of hearing loss depends on the cause and type of hearing impairment. Many conductive hearing defects respond to medical or surgical treatment, such as antibiotic therapy for acute otitis media or insertion of tympanostomy tubes for chronic otitis media. When the conductive loss is permanent, hearing can be improved with the use of a hearing aid to amplify sound.
The nurse should be familiar with the types, basic care, and handling of hearing aids, especially when the child is hospitalized.* Types of aids include those worn in or behind the ear, models incorporated into an eyeglass frame, or types worn on the body with a wire connection to the ear (Fig. 19-7). One of the most common problems with a hearing aid is acoustic feedback, an annoying whistling sound usually caused by improper fit of the ear mold. Sometimes the whistling may be at a frequency that the child cannot hear but that is annoying to others. In this case, if children are old enough, they are told of the noise and asked to readjust the aid.

FIG. 19-7 On-the-body hearing aids are convenient for young children, such as this child with severe bilateral hearing loss. Note eye patching for strabismus.
As children grow older, they may be self-conscious about the device. Every effort is made to make the aid inconspicuous, such as an appropriate hairstyle to cover behind-the-ear or in-the-ear models; attractive frames for glasses; and placement of the on-the-body type where it is not seen, such as under a blouse or sweater. Children are given responsibility for the care of the device as soon as they are able, since fostering independence is a primary goal of rehabilitation.
Sensorineural Hearing Loss.: Treatment for sensorineural hearing loss is much less satisfactory. Because the defect is not one of intensity of sound, hearing aids are of less value in this type of defect. The use of cochlear implants* (a surgically implanted prosthetic device) provides a sensation of hearing for individuals who have severe or profound hearing loss (Zeng and Liu, 2006; Downs and Buchman, 2005). Children with sensorineural hearing loss have lost or damaged some or all of their hair cells or auditory nerve fibers. Often these children cannot benefit from conventional hearing aids because they only amplify sound that cannot be processed by a damaged inner ear. A cochlear implant bypasses the hair cells to directly stimulate surviving auditory nerve fibers so that they can send signals to the brain. These signals can be interpreted by the brain to produce sound and sensations (Zeng and Liu, 2006; Gregg, Wiorek, and Arvedson, 2004).
Multichanneled implants are now available. This more sophisticated device stimulates the auditory nerve at a number of locations with differently processed signals. This type of stimulation allows a person to use the pitch information present in speech signals, leading to better understanding ofspeech. The trend is toward early use of cochlear implants, usually by 18 months of age, to give the child maximum opportunity to develop listening, language, and speaking skills.
Nursing Care Management
Assessment of children for hearing impairment is a critical nursing responsibility. Early detection of hearing loss, preferably within the first 3 to 6 months of life, is essential to improve the language and educational outcomes of those with hearing impairments (Gregg, Wiorek, and Arvedson, 2004; Kenna, 2004). To accomplish this goal, the current recommendation is universal newborn hearing screening before discharge from the newborn nursery (Gregg, Wiorek, and Arvedson, 2004; Cunningham, Cox, and Committee on Practice and Ambulatory Medicine and the Section on Otolaryngology and Bronchoesophagology, 2003; American Academy of Pediatrics, 1999). This discussion focuses on developmental and behavioral indexes associated with hearing impairment. Auditory testing is presented in Chapter 6.
Infancy.: At birth the nurse can observe the neonate’s response to auditory stimuli, as evidenced by the startle reflex, head turning, eye blinking, and cessation of body movement. The infant may vary in the intensity of the response, depending on the state of alertness. However, a consistent absence of a reaction should lead to suspicion of hearing loss. Box 19-5 summarizes other clinical manifestations of hearing impairment in the infant.
Childhood.: The child who is profoundly deaf is much more likely to be diagnosed during infancy than the less severely affected one. If the defect is not detected during early childhood, it likely will become evident during entry into school, when the child has difficulty learning. Unfortunately, some of these children are mistakenly placed in special classes for students with learning disabilities or CI. Therefore it is essential that the nurse suspect a hearing impairment in any child who demonstrates the behaviors listed in Box 19-5.
Of primary importance is the effect of hearing impairment on speech development.* A child with a mild conductive hearing loss may speak fairly clearly but in a loud, monotone voice. A child with a sensorineural defect usually has difficulty in articulation. For example, inability to hear higher frequencies may result in the word spoon being pronounced “poon.” Children with articulation problems need to have their hearing tested.
Lipreading.: Even though the child may become an expert at lipreading, only about 40% of the spoken word is understood, and less if the speaker has an accent, mustache, or beard. Exaggerating pronunciation or speaking in an altered rhythm further reduces comprehension. Parents can help the child understand the spoken word by using the suggestions in the Nursing Care Guidelines box. The child learns to supplement the spoken word with sensitivity to visual cues, primarily body language and facial expression (e.g., tightening the lips, muscle tension, eye contact).
Cued Speech.: This method of communication is an adjunct to straight lipreading. It uses hand signals to help the child with a hearing impairment distinguish between words that look alike when formed by the lips (e.g., mat, bat). It is most often used by children with hearing impairments who are using speech rather than those who are nonverbal.
Sign Language.: Sign language, such as American Sign Language (ASL) or British Sign Language (BSL), is a visual gestural language that uses hand signals that roughly correspond to specific words and concepts in the English language. Family members are encouraged to learn signing because using or watching hands requires much less concentration than lipreading or talking. Also, a symbol method enables some children to learn more and to learn faster.
Speech Language Therapy.: The most formidable task in the education of a child who is profoundly hearing impaired is learning to speak. Speech is learned through a multisensory approach, using visual, tactile, kinesthetic, and auditory stimulation. Parents are encouraged to participate fully in the learning process.
Additional Aids.: Everyday activities present problems for older children with hearing impairment. For example, they may not be able to hear the telephone, doorbell, or alarm clock. Several commercial devices are available to help them adjust to these dilemmas. Flashing lights can be attached to a telephone or doorbell to signal its ringing. Trained hearing ear dogs can provide great assistance because they alert the person to sounds, such as someone approaching, a moving car, a signal to wake up, or a child’s cry. Special teletypewriters or telecommunications devices for the deaf (TDD or TTY) help people with impaired hearing communicate with each other over the telephone; the typed message is conveyed via the telephone lines and displayed on a small screen.*
Any audiovisual medium presents dilemmas for these children, who can see the picture but cannot hear the message. However, with closed captioning a special decoding device is attached to the television, and the audio portion of a program is translated into subtitles that appear on the screen.†
Socialization.: As children learn to compensate for their lack of hearing, they become extremely perceptive to visual and vibratory changes. Children often know when another person wants to talk to them because the person will walk close by but not pass. They learn to be alert to other people approaching them by seeing their shadows or feeling the vibrations of their footsteps. They are acutely aware of facial expressions and may comprehend unspoken messages more quickly than the spoken word.
Because socialization is extremely important to the child’s development, the nurse discusses with the family methods of fostering social contact. If children attend a special school for the deaf, they are able to socialize with peers in that setting. Classmates become a potential source of close friendships because they communicate more easily among themselves. Parents are encouraged to promote these relationships whenever possible.
Children with a hearing impairment may need special help with school or social activities. For children wearing hearing aids, background noise should be kept to a minimum. Because many of these children are able to attend regular classes, the teacher may need assistance in adapting methods of teaching for the child’s benefit. The school nurse is often in an optimal position to emphasize methods of facilitated communication, such as lipreading (see Nursing Care Guidelines box, p. 626). Because group projects and audiovisual teaching aids may hinder the child’s learning, these educational methods should be carefully evaluated.
In a group setting it is helpful for the other members to sit in a semicircle in front of the child. Because one of the difficulties in following a group discussion is that the child is unaware of who will speak next, someone should point out each speaker. Speakers can also be given numbers, or their names can be written down as each person talks. If one person writes down the main topic of the discussion, the child is able to follow lipreading more closely. Such suggestions can increase the child’s ability to participate in sports, organizations such as Boy Scouts or Girl Scouts, and group projects.
Support Child and Family.: After the diagnosis of hearing impairment is made, parents need extensive support to adjust to the shock of learning about their child’s disability and an opportunity to realize the extent of the hearing loss. If the hearing loss occurs during childhood, the child also requires sensitive, supportive care during the long and often difficult adjustment to this sensory loss. Early rehabilitation is one of the best strategies for fostering adjustment. However, progress in learning communication may not always coincide with emotional adjustment. Depression or anger is common, and such feelings are a normal part of the grieving process. (See also Chapter 18 for an extensive discussion of the emotional support of the child and family.)
Care for Child During Hospitalization.: The needs of the hospitalized child with impaired hearing are the same as those of any other child, but the disability presents special challenges to the nurse (see Critical Thinking Exercise). For example, verbal explanations must be supplemented by tactile and visual aids, such as books or actual demonstration and practice. Children’s understanding of the explanation needs to be constantly reassessed. If their verbal skills are poorly developed, they can answer questions through drawing, writing, or gesturing. For example, if the nurse is attempting to clarify where a spinal tap is done, the child is asked to point to where the procedure will be done on the body. Because these children often need more time to grasp the full meaning of an explanation, the nurse needs to be patient, allowing ample time for understanding.
When communicating with the child, the nurse should use the same principles as those outlined for facilitating lipreading. Ideally, nurses without foreign accents should be assigned to the child. The child’s hearing aid is checked to ensure that it is working properly. If it is necessary to awaken the child at night, the nurse gently shakes the child or turns on the hearing aid before arousing the child. The nurse always makes certain that the child can see him or her before any procedures, even routine ones such as changing a diaper or regulating an infusion. It is important to remember that the child may not be aware of one’s presence until alerted through visual or tactile cues.
Ideally, parents are encouraged to room with the child. However, it must be conveyed to them that this is not to serve as a convenience to the nurse but as a benefit to the child. Although the parents’ aid can be enlisted in familiarizing the child with the hospital and explaining procedures, the nurse also talks directly to the youngster, encouraging expression of feelings about the experience. If the child’s speech is difficult to understand, the nurse makes an effort to become familiar with his or her pronunciation of words. Parents often can be helpful by explaining the child’s usual speech habits. Nonverbal communication devices that employ pictures or words that the child can point to are also available. Such boards can also be made by drawing pictures or writing the words of common needs on cardboard, such as parent, food, water, or toilet.
The nurse has a special role as child advocate and is in a strategic position to alert other health team members and other patients to the child’s special needs regarding communication. For example, the nurse should accompany other practitioners on visits to the child’s room to ensure that they speak to the child and that the child understands what is said. Caregivers sometimes forget that the child has the abilities to perceive and learn despite a hearing loss, and consequently they communicate only with the parents. As a result, the child’s needs and feelings remain unrecognized and unmet.
Because children with impaired hearing may have difficulty forming social relationships with other children, the child is introduced to roommates and encouraged to engage in play activities. The hospital setting can provide growth-promoting opportunities for social relationships. With the assistance of a child life specialist, the child can learn new recreational activities, experiment with group games, and engage in therapeutic play. The use of puppets, dollhouses, role-playing with dress-up clothes, building with a hammer and nails, finger painting, and water play can help the child express feelings that previously were suppressed.
Assist in Measures to Prevent Hearing Impairment.: A primary nursing role is prevention of hearing loss. Because the most common cause of impaired hearing is chronic otitis media, it is essential that appropriate measures be instituted to treat existing infections and prevent recurrences (see Chapter 23). Children with a history of ear or respiratory infections or any other condition known to increase the risk of hearing impairment should receive periodic auditory testing.
To prevent the causes of hearing loss that begin prenatally and perinatally, pregnant women need counseling regarding the necessity of early prenatal care, including genetic counseling for known familial disorders; avoidance of all ototoxic drugs, especially during the first trimester; tests to rule out syphilis, rubella, or blood incompatibility; medical management of maternal diabetes; strict control of alcohol intake; adequate dietary intake; and avoidance of smoke exposure. The necessity of routine immunization during childhood to eliminate the possibility of acquired sensorineural hearing loss from rubella, mumps, or measles (encephalitis) is stressed.
Excessive noise pollution with or without smoke exposure causes sensorineural hearing loss (Daniel, 2007). The nurse should routinely assess the possibility of environmental pollution (e.g., loud noise and smoking) and advise children and parents of the potential danger of hearing loss. When individuals engage in activities associated with high-intensity noise, such as flying model airplanes, target shooting, or snowmobiling, they should wear ear protection such as earmuffs or earplugs. Even common household equipment, such as lawn mowers, vacuum cleaners, and cordless telephones, may cause noise-induced hearing loss.
VISUAL IMPAIRMENT
Visual impairment is a common problem during childhood. In the United States the prevalence of blindness and serious visual impairment in the pediatric population is estimated at 30 to 64 children per 100,000 population. Vision problems occur in 5% to 10% of all preschoolers and include refractive error, strabismus, and amblyopia (Tingley, 2007). The nurse’s role is clearly one of early assessment and detection, prevention, referral, and, in some instances, rehabilitation.
Definition and Classification
Visual impairment is a general term that refers to visual loss that cannot be corrected with regular prescription lenses. However, more useful definitions for classifying visual impairments exist. School vision (also known as partially sighted) refers to visual acuity between 20/70 and 20/200. The child should be able to obtain an education in the usual public school system with the use of normal-sized print. Near vision is almost always better than distance vision. Legal blindness, visual acuity of 20/200 or less and/or a visual field of 20 degrees or less in the better eye, is useful only as a legal definition, not as a medical diagnosis. It allows special considerations with regard to taxes, entrance into special schools, eligibility for aid, and other benefits.
Etiology
Visual impairment can be caused by a number of genetic and prenatal or postnatal conditions. These include perinatal infections (herpes, chlamydia, gonococci, rubella, syphilis, toxoplasmosis); retinopathy of prematurity; trauma; postnatal infections (meningitis); and disorders such as sickle cell disease, juvenile rheumatoid arthritis, Tay-Sachs disease, albinism, and retinoblastoma. In many instances, such as with refractive errors, the cause of the defect is unknown.
Refractive errors are the most common types of visual disorders in children. The term refraction means bending and refers to the bending of light rays as they pass through the lens of the eye. Normally, light rays enter the lens and fall directly on the retina. However, in refractive disorders the light rays either fall in front of the retina (myopia) or beyond it (hyperopia). Other eye problems, such as strabismus, may or may not include refractive errors, but they are important because, if untreated, they result in blindness from amblyopia. These, along with other less frequent visual disorders, are summarized in Box 19-6. In addition to these disorders, other visual problems can be a result of infection or trauma.
Trauma.: Trauma is a common cause of blindness in children. Injuries to the eyeball and adnexa (supporting or accessory structures, such as eyelids, conjunctiva, or lacrimal glands) can be classified as penetrating or nonpenetrating. Penetrating wounds are most often a result of sharp instruments, such as sticks, knives, or scissors; propulsive objects, such as firecrackers, guns, arrows, or slingshots; or a powerful contusion by a blunt object, which may occur during a fight or from a serious car accident. Nonpenetrating injuries may be a result of foreign objects in the eyes, lacerations, a blow from a blunt object such as a ball (baseball, softball, basketball, racquet sports) or fist, or thermal or chemical burns.
Treatment is aimed at preventing further ocular damage and is primarily the responsibility of the ophthalmologist. It involves adequate examination of the injured eye (with the child sedated or anesthetized in severe injuries); appropriate immediate intervention, such as removal of the foreign body or suturing of the laceration; and prevention of complications, such as administration of antibiotics or steroids and complete bed rest to allow the eye to heal and blood to reabsorb (see Emergency Treatment box). The prognosis varies according to the type of injury. It is usually guarded in all cases of penetrating wounds because of the high risk of serious complications.
Infections.: Infections of the adnexa and structures of the eyeball or globe may occur in children. The most common eye infection is conjunctivitis (see Chapter 14). Treatment is usually with ophthalmic antibiotics. Severe infections may require systemic antibiotic therapy. Steroids are used cautiously because they exacerbate viral infections such as herpes simplex, increasing the risk of damage to the involved structures.
Nursing Care Management
Assessment of children for visual impairment is a critical nursing responsibility. Discovery of a visual impairment as early as possible is essential to prevent social, physical, and psychologic damage to the child. Assessment involves (1) identifying those children who by virtue of their history are at risk, (2) observing for behaviors that indicate a vision loss, and (3) screening all children for visual acuity and signs of other ocular disorders such as strabismus. This discussion focuses on clinical manifestations of various types of visual problems (see Box 19-6). Vision testing is discussed in Chapter 6.
Infancy.: At birth the nurse should observe the neonate’s response to visual stimuli, such as following a light or object and cessation of body movement. The infant may vary in the intensity of the response, depending on the state of alertness.
Of special importance in detecting visual impairment during infancy are the parents’ concerns regarding visual responsiveness in their child. Their concerns, such as lack of eye contact from the infant, must be taken seriously. During infancy the child should be tested for strabismus. Lack of binocularity after 4 months of age is considered abnormal and must be treated to prevent amblyopia.
Childhood.: Because the most common visual impairment during childhood is refractive errors, testing for visual acuity is essential. The school nurse usually assumes major responsibility for vision testing in schoolchildren. Besides refractive errors, the nurse should be aware of signs and symptoms that indicate other ocular problems. If a referral is made to the family requesting further eye testing, the nurse is responsible for follow-up concerning the recommendation.
The shock of learning that their child is blind or partially sighted is an immense crisis for families. The family is encouraged to investigate appropriate stimulation and educational programs for their child as soon as possible. Sources of information include state commissions for the blind, local schools for the blind, American Foundation for the Blind,* National Federation of the Blind,† National Association for Parents of Children with Visual Impairments,‡ National Association for Visually Handicapped,§ American Council of the Blind, and CNIB.¶
and CNIB.¶
Promote Parent-Child Attachment.: A crucial time in the life of blind infants is when they and their parents are getting acquainted with each other. Pleasurable patterns of interaction between the infant and parents may be lacking if there is not enough reciprocity. For example, if the parent gazes fondly at the infant’s face and seeks eye contact but the infant fails to respond because he or she cannot see the parent, a troubled cycle of responses may occur. The nurse can help parents learn to look for other cues that indicate the infant is responding to them, such as whether the eyelids blink; whether the activity level accelerates or slows; whether respiratory patterns change, such as faster or slower breathing, when the parents come near; and whether the infant makes throaty sounds when they speak to the infant. In time parents learn that the infant has unique ways of relating to them. They are encouraged to show affection using nonvisual methods, such as talking or reading, cuddling, and walking the child.
Promote Child’s Optimal Development.: Promoting the child’s optimum development requires rehabilitation in a number of important areas. These include learning self-help skills and appropriate communication techniques to become independent. Although nurses may not be directly involved in such programs, they can provide direction and guidance to families regarding the availability of programs and the need to promote these activities in their child.
Development and Independence.: Motor development depends on sight almost as much as verbal communication depends on hearing. From earliest infancy, parents are encouraged to expose the infant to as many visual-motor experiences as possible, such as sitting supported in an infant seat or swing and being given opportunities for holding up the head, sitting unsupported, reaching for objects, and crawling.
Despite visual impairment, the child can become independent in all aspects of self-care. The same principles used for promoting independence in sighted children apply, with additional emphasis on nonvisual cues. For example, the child may need help in dressing, such as special arrangement of clothing for style coordination and braille tags to distinguish colors and prints.
The blind child also must learn to become independent in navigational skills. The two main techniques are the tapping method (use of a cane to survey the environment for direction and to avoid obstacles) and guides, such as a sighted human guide or a dog guide, such as a Seeing Eye dog. Children who are partially sighted may benefit from ocular aids, such as a monocular telescope.
Play and Socialization.: Blind children do not learn to play automatically. Because they cannot imitate others or actively explore the environment as sighted children do, they depend much more on others to stimulate and teach them how to play. Parents need help in selecting appropriate play material, especially those that encourage fine and gross motor development and stimulate the senses of hearing, touch, and smell. Toys with educational value are especially useful, such as dolls with various clothing closures.
Blind children have the same needs for socialization as sighted children. Because they have little difficulty in learning verbal skills, they are able to communicate with age-mates and participate in suitable activities. The nurse discusses with parents opportunities for socialization outside the home, especially regular preschools. The trend is to include these children with sighted children to help them adjust to the outside world for eventual independence.
To compensate for inadequate stimulation, these children may develop blindisms (self-stimulatory activities, such as body rocking, finger flicking, or arm twirling). Such habits restrict the child’s social acceptance and are discouraged. Behavior modification is often successful in reducing or eliminating blindisms.
Education.: The main obstacle to learning is the child’s total dependence on nonvisual cues. Although the child can learn via verbal lecturing, he or she is unable to read the written word or to write without special education. Therefore the child must rely on braille, a system that uses raised dots to represent letters and numbers. The child can then read the braille with the fingers and can write a message using a braille writer. However, unless others read braille, this system is not useful for communicating with others. A more portable system for written communication is the use of a braille slate and stylus or a microcassette tape recorder. A recorder is especially helpful for leaving messages for others and taking notes during classroom lectures. For mathematic calculations, portable calculators with voice synthesizers are available.*
Records and tapes are significant sources of reading material other than braille books, which are large and cumbersome. The Library of Congress† has talking books, braille books, and a special records program, which are available at many local and state libraries and directly from the Library of Congress. The talking book machine and tape player are provided at no cost to families, and there is no postage fee for returning the materials. Recording for the Blind and Dyslexic‡ also provides texts and tapes of books, which are helpful for secondary and college students who are blind.
Learning to use a regular typewriter is another form of writing but has the disadvantage of the blind person’s being unable to check what he or she has written. Computers eliminate this drawback; a home computer with a voice synthesizer can be adapted to speak each letter or word that has been typed.
The child with partial sight benefits from specialized visual aids that produce a magnified retinal image. The basic devices are accommodation (e.g., bringing the object closer), special plus lenses, handheld and stand magnifiers, telescopes, video projection systems, and large print. Special equipment is available to enlarge print. Information about services for the partially sighted is available from the National Association for Visually Handicapped and American Foundation for the Blind. Children with diminished vision often prefer to do close work without their glasses and compensate by bringing the object very near to their eyes. This should be allowed. The exception is the child with vision in only one eye, who should always wear glasses for protection.
Care for the Child During Hospitalization.: Because nurses are more likely to care for children who are hospitalized for procedures that involve temporary loss of vision than for children who are blind, the following discussion concentrates primarily on the needs of such children. The nursing care objectives in either situation are to (1) reassure the child and family throughout every phase of treatment, (2) orient the child to the surroundings, (3) provide a safe environment, and (4) encourage independence. Whenever possible, the same nurse should care for the child to ensure consistency in the approach.
When sighted children temporarily lose their vision, almost every aspect of the environment becomes bewildering and frightening. They are forced to rely on nonvisual senses for help in adjusting to the blindness without the benefit of any special training. Nurses have a major role in minimizing the effects of temporary loss of vision. They need to talk to the child about everything that is occurring, emphasizing aspects of procedures that are felt or heard. They should approach the child by always identifying themselves as soon as they enter the room. Because unfamiliar sounds are especially frightening, these are explained. Parents are encouraged to room with their child and participate in the care. Familiar objects, such as a teddy bear or doll, should be brought from home to help lessen the strangeness of the hospital. As soon as the child is able to be out of bed, he or she is oriented to the immediate surroundings. If the child is able to see on admission, this opportunity is taken to point out significant aspects of the room. The child is encouraged to practice ambulating with the eyes closed to become accustomed to this experience.
The room is arranged with safety in mind. For example, a stool or chair is placed next to the bed to help the child climb in and out of bed. The furniture is always placed in the same position to prevent collisions. Cleaning personnel are reminded of the need to keep the room in order. If the child has difficulty navigating by feeling the walls, a rope can be attached from the bed to the point of destination, such as the bathroom. Attention to details such as well-fitting slippers or robes that do not drag on the floor is important in preventing tripping. Unlike the child who is blind, these children are not familiar with navigating with a cane.
The child is encouraged to be independent in self-care activities, especially if the visual loss may be prolonged or potentially permanent. For example, during bathing the nurse sets up all the equipment and encourages the child to participate. At mealtime the nurse explains where each food item is on the tray, opens any special containers, prepares cereal or toast, and encourages the child in self-feeding. Favorite finger foods, such as sandwiches, hamburgers, hot dogs, or pizza, may be good selections. The child is praised for efforts at being cooperative and independent. Any improvements made in self-care, no matter how small, are stressed.
Appropriate recreational activities are provided, and if a child life specialist is available, such planning is done jointly. Because children with temporary blindness have a wide variety of play experiences to draw on, they are encouraged to select activities. For example, if they like to read, they may enjoy being read to. If they prefer manual activity, they may appreciate playing with clay or building blocks or feeling different textures and naming them. If they need an outlet for aggression, activities such as pounding or banging on a drum can be helpful. Simple board and card games can be played with a “seeing partner” or an opponent who helps with the game. They should have familiar toys from home to play with, since familiar items are more easily manipulated than new ones. If parents want to bring presents, they should be objects that stimulate hearing and touch, such as a radio, music box, or stuffed animal.
Occasionally, children who are blind come to the hospital for procedures to restore their vision. Although this is an extremely happy time, it also requires intervention to help them adjust to sight. They need an opportunity to take in all that they see. They should not be bombarded with visual stimuli. They may need to concentrate on people’s faces or their own to become accustomed to this experience. They often need to talk about what they see and to compare the visual images with their mental ones. The children may also go through a period of depression, which must be respected and supported. The nurse or parents should refrain from statements such as “How can you be so sad when you can see again?” Instead the children should be encouraged to discuss how it feels to see, especially in terms of seeing themselves.
Newly sighted children also need time to adjust to the ability to engage in activities that were impossible before. For example, they may prefer to use braille to read, rather than learning a new “visual approach,” because of familiarity with the touch system. Eventually, as they learn to recognize letters and numbers, they will integrate these new skills into reading and writing. However, parents and teachers must be careful not to push them before they are ready. This applies to social relationships and physical activities as well as learning situations.
Assist in Measures to Prevent Visual Impairment.: An essential nursing goal is to prevent visual impairment. This involves many of the same interventions discussed under hearing impairments:
 Prenatal screening for pregnant women at risk, such as those with rubella or syphilis infection and family histories of genetic disorders associated with visual loss
Prenatal screening for pregnant women at risk, such as those with rubella or syphilis infection and family histories of genetic disorders associated with visual loss
 Adequate prenatal and perinatal care to prevent prematurity
Adequate prenatal and perinatal care to prevent prematurity
 Periodic screening of all children, especially newborns through preschoolers, for congenital blindness and visual impairments caused by refractive errors, strabismus, and other disorders
Periodic screening of all children, especially newborns through preschoolers, for congenital blindness and visual impairments caused by refractive errors, strabismus, and other disorders
 Rubella immunization of all children
Rubella immunization of all children
 Safety counseling regarding the common causes of ocular trauma and safe practices when working with, playing with, or carrying objects such as scissors, knives, and balls
Safety counseling regarding the common causes of ocular trauma and safe practices when working with, playing with, or carrying objects such as scissors, knives, and balls
After detection of eye problems, the nurse has a responsibility to prevent further ocular damage by ensuring that corrective treatment is used. For the child with strabismus, this often necessitates occlusion patching of the stronger eye. Compliance with the procedure is greatest during the early preschool years. It is more difficult to encourage school-age children to wear the occlusive patch because the poor visual acuity of the uncovered weaker eye interferes with school work and the patch sets them apart from their peers. In school they benefit from being positioned favorably (closer to the chalkboard or other visual media) and allowed extra time to read or complete an assignment. If treatment of the eye disorder requires instillation of ophthalmic medication, the family is taught the correct procedure (see Chapter 22).
For the child with refractive errors, the nurse helps the child adjust to wearing glasses. Young children who often pull glasses off benefit from temporal pieces that wrap around the ears or an elastic strap attached to the frames and around the back of the head to hold the glasses on securely. After children appreciate the value of clear vision, they are more likely to wear the corrective lenses.
Glasses should not interfere with any activity. Special protective guards are available during contact sports to prevent accidental injury, and all corrective lenses should be made from safety glass, which is shatterproof. Often, corrective lenses improve visual acuity so dramatically that children are able to compete more effectively in sports. This in itself is a tremendous inducement to continue wearing glasses.
Contact lenses are a popular alternative, especially for adolescents. Several types are available, such as hard lenses, including gas-permeable ones, and soft lenses, which may be designed for daily or extended wear. Contact lenses offer several advantages over glasses, such as greater visual acuity, total corrected field of vision, convenience (especially with the extended-wear type), and optimal cosmetic benefit. Unfortunately, they are usually more expensive and require much more care than glasses, including considerable practice to learn techniques for insertion and removal. If they are prescribed, the nurse can be helpful in teaching parents or older children how to care for the lenses.
Because trauma is the leading cause of blindness, the nurse has the major responsibility of preventing further eye injury until specific treatment is instituted. The major principles to follow when caring for an eye injury are outlined in the Emergency Treatment box on p. 630. Because patients with a serious eye injury fear blindness, the nurse should stay with the child and family to provide support and reassurance.
DEAF-BLIND CHILDREN
The most traumatic sensory impairment is loss of sight and hearing. Obviously, auditory and visual disabilities have profound effects on the child’s development. They interfere with the normal sequence of physical, intellectual, and psychosocial growth. Although such children often achieve the usual motor milestones, their rate of development is slower. These children learn communication only with specialized training. Finger spelling is one desirable method often taught to these children. Some deaf-blind children, especially those with residual hearing or sight, can learn to speak. Whenever possible, speech is encouraged because it allows communication with other individuals.
The future prospects for deaf-blind children are, at best, unpredictable. Congenital blindness or deafness may be accompanied by other physical or neurologic problems, which further diminish the child’s learning potential. The most favorable prognosis is for children who have acquired deafness and blindness and have few, if any, associated disabilities. Their learning capacity is greatly potentiated by their developmental progress before the sensory impairments. Although total independence, including gainful vocational training, is the goal, some deaf-blind children are unable to develop to this level. They may require lifelong parental or residential care. The nurse working with such families helps them deal with future goals for the child, including possible alternatives to home care during the parents’ advancing years.
RETINOBLASTOMA
Retinoblastoma, which arises from the retina, is the most common congenital malignant intraocular tumor of childhood. Approximately 11 cases per million occur annually, primarily in children younger than 5 years of age. Retinoblastoma is caused by a mutation in a gene and may occur sporadically or be inherited (Hurwitz, Shields, Shields, and others, 2006). Retinoblastoma develops when the mutated gene is unable to produce the natural signals to stop the growth of retinal cells. Of all cases, the majority are nonhereditary and unilateral, with the remainder divided between hereditary and unilateral, and hereditary and bilateral. Hereditary retinoblastomas are transmitted as an autosomal dominant trait with a 90% penetrance (Hurwitz, Shields, Shields, and others, 2006).
Diagnostic Evaluation
Retinoblastoma has few grossly obvious signs (Box 19-7). Typically the most common sign is observed by the parent as a whitish “glow” in the pupil, known as the white reflex or leukokoria. Leukokoria represents visualization of the tumor as the light momentarily falls on the mass (Fig. 19-8). The second most common sign of retinoblastoma is acquired strabismus (Hurwitz, Shields, Shields, and others, 2006).
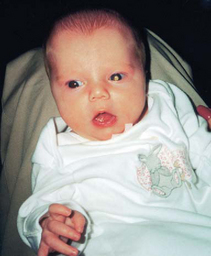
FIG. 19-8 White reflex. Whitish appearance of lens is produced as light falls on tumor mass in left eye.
The first step in diagnosis is carefully listening to and recognizing the significance of reports from family members regarding suspected abnormalities within the eye. Eye abnormalities, including white reflex, strabismus, decreased vision, and persistent painful erythematous eyes, are referred to an ophthalmologist. Definitive diagnosis is usually based on ophthalmoscopic examination with the patient under general anesthesia. Imaging studies, including ultrasonography and computed tomography of the orbit, are done to determine the extent of the disease.
Therapeutic Management
The aim of therapy is to preserve useful vision and eradicate the tumor. Treatment of retinoblastoma depends chiefly on the stage of the tumor at the time of diagnosis. Some of the common focal therapies are (1) plaque brachytherapy (surgical radioactive implant on the sclera until maximum dose has been delivered to the tumor), (2) laser photocoagulation (laser beam to coagulate blood supply to the tumor), (3) cryotherapy (freezing the tumor by destroying the microcirculation to the tumor through microcrystal formation, and (4) thermotherapy (using microwaves or infrared radiation to deliver heat to the tumor) (Melamud, Palekar, and Singh, 2006; De Potter, 2002; Schouten–van Meeteren, Moll, Imhof, and others, 2002).
Chemotherapy is being used in the early RE groups in an attempt to reduce tumor size to facilitate focal intraocular treatment (chemoreduction). Chemotherapy has been used for several years to prevent metastatic disease in the RE groups IV and V and relapsed patients (chemoprevention or chemoprophylaxis). Chemoreduction and chemoprevention minimize the use of external beam radiation treatment and therefore reduce the risk of radiation-induced malignancies and facial disfigurement.
With advanced tumor growth into the optic nerve, choroid, orbit, and anterior chamber or no hope for useful vision, enucleation (removal) of the affected eye is the treatment of choice. After enucleation, an orbital implant is placed to provide a more natural cosmetic appearance, minimize sinking of the prosthesis, and enable motility of the prosthesis. With bilateral disease, every attempt is made to preserve useful vision in both eyes. Chemotherapy, external beam, radiotherapy, and other treatments (i.e., cryotherapy, laser, plaque brachytherapy, thermotherapy) to both eyes may prevent the need for enucleation.
Prognosis.: The overall prognosis for retinoblastoma is favorable, with a survival rate of nearly 90% for both unilateral and bilateral tumors. Retinoblastoma is one of the tumors that may spontaneously regress. Of major concern in long-term survivors is the development of decreased visual acuity, facial disfiguration, and secondary tumors—especially osteogenic sarcoma, other sarcomas, and melanoma. Children with bilateral disease (hereditary form) are more likely to develop secondary cancers than are children with unilateral disease. It is thought that these individuals are predisposed to developing cancer and that radiation increases their risk.
Nursing Care Management
One of the most important nursing goals is to have a high index of suspicion for this rare malignancy. If parents report noticing a strange light in the eye or expression, these concerns must be taken seriously. Families with a history of retinoblastoma require follow-up, and the nurse can be instrumental in reminding parents of appointments.
Because the tumor is usually diagnosed in infants or very young children, most of the preparation for diagnostic tests and treatment involves parents. After indirect ophthalmoscopy, the child may not see clearly, or the eyes may be sensitive to light because of pupillary dilation. Parents are made aware of these normal reactions before the procedure. Screening tests, such as bone surveys and bone marrow aspiration, are rarely performed unless metastatic disease is suspected.
The treatment plan may include focal intraocular therapy with or without chemotherapy, external beam radiation, and, if necessary, enucleation. Enucleation is the treatment of choice if there is extensive disease threatening metastasis or no chance for useful vision. The enucleation procedure and the positive benefits of a prosthesis are explained to the parents. Showing them pictures of another child with an artificial eye may help them adjust to the thought of disfigurement (Fig. 19-9).
After surgery the parents are prepared for the child’s facial appearance. An eye patch is in place, and the child’s face may be edematous or ecchymotic. Parents often fear seeing the surgical site because they imagine a cavity in the skull. A surgically implanted sphere maintains the shape of the eyeball, and the implant is covered with conjunctiva. When the lids are open, the exposed area resembles the mucosal lining of the mouth. After the child is fitted for a prosthesis, usually within 3 weeks, the facial appearance returns to normal. Initial instructions for care of the prosthesis are given by the ocularist who fits and manufactures the device.
Care of the socket is minimal and easily accomplished. The wound itself is clean and has little or no drainage. If an antibiotic ointment is prescribed, it is applied in a thin line on the surface of the tissues of the socket. To cleanse the site, an irrigating solution may be ordered and is instilled daily or more frequently, before application of the antibiotic ointment. The dressing, consisting of an eye pad taped over the surgical site, is changed daily. After the socket has healed completely, a dressing is no longer necessary, although it is a preventive measure against infection.
AUTISM SPECTRUM DISORDERS
Autism spectrum disorders (ASDs) are complex neurodevelopmental disorders of brain function accompanied by intellectual and social behavioral deficits. ASDs include autistic disorder, Asperger syndrome, and pervasive developmental disorder not otherwise specified, which are impairments ranging from mild to severe (Croen, Najjar, Ray, and others, 2006). ASD is typically noticed during early childhood, primarily from 24 to 48 months of age. It occurs in one in 166 children; is about four times more common in males than in females (although females are more severely affected); and is not related to socioeconomic level, race, or parenting style (Courtney-Manning, 2007; Schaefer and Lutz, 2006; Fombonne, 2003).
Etiology
ASD is now recognized as a genetic disorder of prenatal and postnatal brain development (Bloom-DiCicco, Lord, Zwaigenbaum, and others, 2006). Immune and environmental factors (e.g., viral infections) may interact with the genetic susceptibility to increase the incidence of ASD (Bloom-DiCicco, Lord, Zwaigenbaum, and others, 2006). Individuals with ASD may have abnormal electroencephalograms, epileptic seizures, delayed development of hand dominance, persistence of primitive reflexes, metabolic abnormalities (elevated blood serotonin), cerebellar vermal hypoplasia (part of the brain involved in regulating motion and some aspects of memory), and infantile abnormal head enlargement (Dawson, 2007; Bloom-DiCicco, Lord, Zwaigenbaum, and others, 2006).
The strong evidence for a genetic basis in twins is consistent with an autosomal recessive pattern of inheritance. Twin studies demonstrate a high concordance (60% to 96%) for monozygotic (identical) twins and less than 5% concordance for dizygotic (nonidentical) twins. In addition, between 5% and 16% of males with ASD are positive for the fragile X chromosome.
There is a relatively high risk of recurrence of ASD in families with one affected child (Schaefer and Lutz, 2006; Muhle, Trentacoste, and Rapin, 2004). Although several genes have been suggested as possible causative factors in ASD, no specific gene for the disorder has been identified (Dawson, 2007; Kolevzon, Gross, and Reichenberg, 2007; Schanen, 2006).
Contrary to previous reports, autism does not appear to be caused by the measles-mumps-rubella (MMR) and thimerosal-containing vaccines (D—Souza, Fombonne, and Ward, 2006; DeStefano, Bhasin, Thompson, and others, 2004; Muhle, Trentacoste, and Rapin, 2004) (see Evidence-Based Practice box). ASD has been reported in association with a number of conditions such as fragile X syndrome, tuberous sclerosis, metabolic disorders, fetal rubella syndrome, Haemophilus influenzae meningitis, and structural brain anomalies (Dawson, 2007; Muhle, Trentacoste, and Rapin, 2004). Recent reports have retrospectively tied ASD to prenatal and perinatal events such as maternal and paternal ages over 40 years (for fathers, one in 116 births; for mothers, one in 123 births), uterine bleeding during pregnancy, low Apgar score, fetal distress, and neonatal hyperbilirubinemia (Croen, Najjar, Fireman, and others, 2007; Kolevzon, Gross, and Reichenberg, 2007; Muhle, Trentacoste, and Rapin, 2004). These same researchers, however, urge caution in interpreting these findings.
Clinical Manifestations and Diagnostic Evaluation
Children with ASD demonstrate several peculiar and often seemingly bizarre characteristics, primarily in social interactions, communication, and behavior. One hallmark characteristic is the inability to maintain eye contact with another person. Parents of autistic children have noted their infants had difficulties with eye contact, avoidance of body contact, and language delay at a very early age (Belschner, 2007; Dawson, 2007). Children with ASD also display limited functional play and may interact with toys in an unusual or odd manner (Belschner, 2007). ASD children may have significant gastrointestinal symptoms. Constipation is a common symptom and can be associated with acquired megarectum in children with ASD (Afzal, Murch, Thirrupathy, and others, 2003). Other clinical manifestations typically seen in children with autism are described in Box 19-8.
Children with autism do not always have the same manifestations, from mild forms requiring minimal supervision, to severe forms in which self-abusive behavior is common. The majority (50% to 70%) of children with autism have some degree of cognitive impairment, with scores typically in the moderate to severe range. More females than males tend to have very low intelligence scores. Despite their relatively moderate to severe disability, some children with autism (known as savants) excel in particular areas, such as art, music, memory, mathematics, or perceptual skills such as puzzle building.
Speech and language delays are also common in ASD children. Any child who does not display such language skills as babbling or gesturing by 12 months, single words by 16 months, and two-word phrases by 24 months is recommended for immediate hearing and language evaluation (Grizzle and Simms, 2005). A sudden deterioration in extant expressive speech is also a red-flag event for further evaluation.
Early recognition, referral, diagnosis, and intensive early intervention tend to improve outcomes for children with ASD (Belschner, 2007; Courtney-Manning, 2007). Unfortunately, diagnosis is often not made until 2 to 3 years after symptoms are first recognized. The American Academy of Neurology report has a comprehensive set of suggested diagnostic criteria to be used to either rule out or establish the diagnosis of childhood ASD (Belschner, 2007; Filipek, Accardo, Ashwal, and others, 2000) (see Box 19-8).
Prognosis
ASD is usually a severely disabling condition. However, some children improve with acquisition of language skills and communication with others (Bloom-DiCicco, Lord, Zwaigenbaum, and others, 2006). Some ultimately achieve independence, but most require lifelong adult supervision. Aggravation of psychiatric symptoms occurs in about half of the children during adolescence, with girls having a tendency for continued deterioration.
Early recognition of behaviors associated with ASD is critical to implement appropriate interventions and family involvement. The prognosis is most favorable for children with communicative speech development by age 6 years and an IQ above 50 at the time of diagnosis.
Nursing Care Management
Therapeutic intervention for the child with ASD is a specialized area involving professionals with advanced training. Although there is no cure for ASD, numerous therapies have been used. The most promising results have been through highly structured and intensive behavior modification programs. In general, the objective in treatment is to promote positive reinforcement, increase social awareness of others, teach verbal communication skills, and decrease unacceptable behavior. Providing a structured routine for the child to follow is a key in the management of ASD.
When these children are hospitalized, the parents are essential to planning care and ideally should stay with the child as much as possible. Nurses should recognize that not all children with ASD are the same and will require individual assessment and treatment. Decreasing stimulation by using a private room, avoiding extraneous auditory and visual distractions, and encouraging the parents to bring in possessions the child is attached to may lessen the disruptiveness of hospitalization. Because physical contact often upsets these children, minimum holding and eye contact may be necessary to avoid behavioral outbursts. Care must be taken when performing procedures on, administering medicine to, or feeding these children, since they may be either fussy eaters who willfully starve themselves or gag to prevent eating or indiscriminate hoarders, swallowing any available edible or inedible items, such as a thermometer. Eating habits of ASD children may be particularly problematic for families and may involve food refusal, mouthing objects, eating nonedibles, and smelling and throwing food (Belschner, 2007; Caronna, Augustyn, and Zuckerman, 2007).
Children with ASD need to be introduced slowly to new situations, with visits with staff caregivers kept short whenever possible. Because these children have difficulty organizing their behavior and redirecting their energy, they need to be told directly what to do. Communication should be at the child’s developmental level, brief, and concrete.
Family Support.: ASD, as with so may other chronic conditions, involves the entire family and often becomes “a family disease.” Nurses can help alleviate the guilt and shame often associated with this disorder by stressing what is known from a biologic standpoint and provide family support. It is imperative to help parents understand that they are not the cause of the child’s condition.
Parents need expert counseling early in the course of the disorder and should be referred to the Autism Society of America.* The society provides information about education, treatment programs and techniques, and facilities such as camps and group homes. Other helpful resources for parents of children with ASD are the local and state departments of mental health and developmental disabilities; these organizations provide important programs for ASD children and in-school programs throughout the United States.
As much as possible, the family is encouraged to care for the child in the home. With the help of family support programs in many states, families are often able to provide home care and assist with the educational services the child needs. As the child approaches adulthood and parents become older, the family may require assistance in locating a long-term placement facility.
REFERENCES
Afzal, N, Murch, S, Thirrupathy, K, et al. Constipation with acquired megarectum in children with autism. Pediatrics. 2003;112(4):939–942.
Alanay, Y, Unal, F, Turanh, G, et al. Multidisciplinary approach to the management of individuals with fragile X syndrome. J Intellect Disabil Res. 2007;51:151–161.
Al-Hay, AA, MacNeil, SJ, Yacoub, M, et al. Complete atrioventricular septal defect, Down syndrome, and surgical outcome: risk factors. Ann Thorac Surg. 2003;75(2):412–421.
American Academy of Pediatrics, Committee on Genetics. Health supervision for children with Down syndrome. Pediatrics. 2001;107(2):442–449.
American Academy of Pediatrics, Task Force on Newborn and Infant Hearing. Newborn and infant hearing loss: detection and intervention. Pediatrics. 1999;103(2):527–530.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders, ed 4 (text rev) (DSM-IV TR). Washington, DC: The Association, 2000.
Belschner, RA. Stop, assess and motivate: the SAM approach to autism spectrum disorder. Am J Nurse Pract. 2007;11(4):43–50.
Biasini, FJ, Grupe, L, Huffman, L, et al, Mental retardation: a symptom and a syndrome. Netherton, SD, Holmes, D, Walker, E, eds. Child and adolescent psychological disorders: a comprehensive textbook, vol 4. New York: Oxford University Press, 1999.
Bittles, AH, Glasson, EJ. Clinical, social, and ethical implications of changing life expectancy in Down syndrome. Dev Med Child Neurol. 2004;46(4):282–286.
Bloom-DiCicco, E, Lord, C, Zwaigenbaum, L, et al. The development neurobiology of autism spectrum disorder. J Neurosci. 2006;26(26):6897–6906.
Bosch, JJ, Ringdahl, J. Functional analysis of problem behavior in children with mental retardation: what is it, and why should pediatric nurses care? MCN. 2001;26(6):307–311.
Caronna, EB, Augustyn, M, Zuckerman, B. Revisiting parental concerns in the age of autism spectrum disorders. Arch Pediatr Adolesc Med. 2007;161:406–407.
Centers for Disease Control and Prevention. Delayed diagnosis of fragile X syndrome—United States, 1990-1999. MMWR. 2002;51(33):740–742.
Coats, AJ. Making choices in cardiology: difficulties of rationing and equality of access. Int J Cardiol. 2001;78(3):209–212.
Courtney-Manning, P. Addressing the crisis in access to autism treatment using health care improvement science. Arch Pediatr Adolesc Med. 2007;161:414–415.
Crawford, DC. FMR1 and the fragile X syndrome, CDC Fact Sheet. http://www.cdc.gov/genomics/hugenet/factsheets/FS_FragileX.htm, 2001. [retrieved Feb 28, 2008, from].
Croen, LA, Najjar, DV, Fireman, B, et al. Maternal and paternal age and the risk of autism spectrum disorders. Arch Pediatr Adolesc Med. 2007;161:334–340.
Croen, LA, Najjar, DV, Ray, T, et al. A comparison of health care utilization and costs of children with and without autism spectrum disorders in a large group-model health plan. Pediatrics. 2006;118(4):1203–1211.
Cunningham, M, Cox, EO, Committee on Practice and Ambulatory Medicine and the Section on Otolaryngology and Bronchoesophagology. Hearing assessment in infants and children: recommendations beyond neonatal screening. Pediatrics. 2003;111(2):436–440.
Dalton, R, Forman, MA, Boris, NW. Pervasive development disorders and childhood psychosis. In Behrman RE, Kliegman RM, Jenson HB, eds.: Nelson textbook of pediatrics, ed 17, Philadelphia: Saunders, 2004.
Daniel, E. Noise and hearing loss: a review. J School Health. 2007;77(5):225–231.
Dawson, G. Despite major challenges, autism research continues to offer hope. Arch Pediatr Adolesc Med. 2007;161:411–412.
Day, SM, Strauss, DJ, Shavelle, RM, et al. Mortality and causes of death in persons with Down syndrome in California. Dev Med Child Neurol. 2005;47(3):171–176.
De Potter, P. Current treatment of retinoblastoma. Curr Opin Ophthalmol. 2002;13(5):331–336.
DeStefano, F, Bhasin, TK, Thompson, WW, et al. Age at first measles-mumps-rubella vaccination in children with autism and school-matched control subjects: a population-based study in metropolitan Atlanta. Pediatrics. 2004;113(2):259–266.
Downs, BW, Buchman, CA. External auditory canal translocation for cochlear implantation. Laryngoscope. 2005;115:555–556.
D’Souza, Y, Fombonne, E, Ward, BJ. No evidence of persisting measles virus in blood mononuclear cells from children with autism spectrum disorder. Pediatrics. 2006;118:1664–1675.
Filipek, P, Accardo, PJ, Ashwal, S, et al. Practice parameter: screening and diagnosis of autism: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Child Neurology Society. Neurology. 2000;55(2 of 2):468–479.
Fombonne, E. The prevalence of autism. JAMA. 2003;289:87–89.
Formigari, R, Di Donato, RM, Garguilo, G, et al. Better surgical prognosis for patients with complete atrioventricular septal defect and Down’s syndrome. Ann Thorac Surg. 2004;78(2):666–672.
Glasson, EJ, Sullivan, SG, Hussain, R, et al. The changing survival profile of people with Down’s syndrome: implications for genetic counseling. Clin Genet. 2002;62(5):390–393.
Gregg, RB, Wiorek, MA, Arvedson, JC. Pediatric audiology: a review. Pediatr Rev. 2004;25(7):224–234.
Grizzle, KL, Simms, MD. Early language development and language learning disabilities. Pediatr Rev. 2005;26(8):274–283.
Hall, JG. Chromosomal clinical abnormalities. In Behrman RE, Kliegman RM, Jenson HB, eds.: Nelson textbook of pediatrics, ed 17, Philadelphia: Saunders, 2004.
Hurwitz, RL, Shields, CL, Shields, JA, et al. Retinoblastoma. In Pizzo PA, Poplack DG, eds.: Principle and practice of pediatric oncology, ed 5, Philadelphia: Lippincott, 2006.
Johnson, CP, Walker, WO. Mental retardation: management and prognosis. Pediatr Rev. 2006;27(7):249–256.
Kabra, M, Gulati, S. Mental retardation. Indian J Pediatr. 2003;70(2):153–158.
Kenna, MA. Medical management of childhood hearing loss. Pediatr Ann. 2004;33(12):822–832.
Kolevzon, A, Gross, R, Reichenberg, A. Prenatal and perinatal risk factors for autism: a review and integration of findings. Arch Pediatr Adolesc Med. 2007;161:326–333.
Melamud, A, Palekar, R, Singh, A. Retinoblastoma. Am Fam Physician. 2006;73(6):1041–1044.
Mizoue, T, Miyamoto, R, Shimizu, T. Combined effect of smoking and occupational exposure to noise on hearing loss in steel factory workers. J Occup Environ Med. 2003;60(10):56–59.
Muhle, E, Trentacoste, SV, Rapin, I. The genetics of autism. Pediatrics. 2004;113(5):e472–486.
National Down Syndrome Society. About Down syndrome. http://www.ndss.org, 2006. [retrieved March 7, 2008, from].
National Fragile X Foundation. Prevalence of fragile X syndrome. http://www.fragilex.org/html/prevalence.htm, 2006. [retrieved Jan 21, 2007, from].
Peterson, CC. A review of biochemical and ultrasound markers in detection of Down syndrome. J Perinatal Educ. 2006;15(1):19–25.
Phalen, JA. Fragile X syndrome. Pediatr Rev. 2005;26(5):181–182.
Pueschel, SM. The child with Down syndrome. In Levine MD, Carey WB, Crocker AC, eds.: Developmental-behavioral pediatrics, ed 3, Philadelphia: Saunders, 1999.
Rehm, RS, Bradley, JF. Social interactions at school of children who are medically fragile and developmentally delayed. J Pediatr Nurs. 2006;21(4):299–307.
Schaefer, GB, Lutz, RE. Diagnostic yield in the clinical genetic evaluation of autism spectrum disorders. Genet Med. 2006;8(9):549–556.
Schanen, NC. Epigenetics of autism spectrum disorders. Hum Molec Genet. 2006;15(R1-2):R138–R150.
Schouten–van Meeteren, AYN, Moll, AC, Imhof, SM, et al. Overview chemotherapy for retinoblastoma: an expanding area of clinical research. Med Pediatr Oncol. 2002;38:428–438.
Segal, S, Eviatar, E, Lapinsky, J, et al. Inner ear damage in children due to noise exposure from toy cap pistols and firecrackers: a retrospective review of 53 cases. Noise Health. 2003;5(18):13–18.
Skotko, B. Mothers of children with Down syndrome reflect on their postnatal support. Pediatrics. 2005;115(1):64–77.
Smith, RJH, Bale, JF, White, KR. Sensorineural hearing loss in children. Lancet. 2005;365:879–890.
Tingley, DH. Vision screening essentials: screening today for eye disorders in the pediatric patient. Pediatr Rev. 2007;28(2):54–61.
Van Riper, M. A change of plans: the birth of a child with Down syndrome doesn’t have to be a negative experience. Am J Nurs. 2003;103(6):71–74.
Walker, WO, Johnson, CP. Mental retardation: overview and diagnosis. Pediatr Rev. 2006;27(6):204–212.
Wilton, G, Plane, MB. The family empowerment network: a service model to address the needs of children and families affected by fetal alcohol spectrum disorders. Pediatr Nurs. 2006;32(4):299–305.
Zeng, FG, Liu, S. Speech perception in individuals with auditory neuropathy. J Speech Lang Hearing Res. 2006;49:367–380.
*Information on early intervention programs in each state is available from the National Down Syndrome Society, 666 Broadway, New York, NY 10012-2317; (800) 221-4602; fax: (212) 979-2873; http://www.ndss.org.
†230 W. Monroe St., Suite 1800, Chicago, IL 60606-4802; (800) 221-6827; TTY: (312) 726-4258; fax: (312) 726-1494; http://www.easterseals.com.
‡1010 Wayne Ave., Suite 650, Silver Spring, MD 20910; (301) 565-3842 or (800) 433-5255; fax: (301) 565-5342; http://www.thearc.org.
§A resource for a variety of self-help equipment is Sammons Preston, PO Box 5071, Bolingbrook, IL 60440-5071; (800) 323-5547; fax: (800) 547-4333; http://www.sammonspreston.com. In Canada: (800) 665-9200.
*1133 19th St. NW, Washington, DC 20036; (800) 700-8585 or (202) 628-3630; fax: (202) 824-0200; http://www.specialolympics.org. (Website includes listing of state offices.) In Canada: Special Olympics Canada, 60 St. Clair Ave. E, Suite 700, Toronto, Ontario M4T 1N5; (416) 927-9050; fax: (416) 927-8475; http://www.specialolympics.ca.
*Sources of information on sexuality and conception are the Arc of the United States (see footnote, p. 613) and Planned Parenthood Federation of America, 434 W. 33rd St., New York, NY 10001; (212) 541-7800 or (800) 230-7526; fax: (212) 245-1845; http://www.plannedparenthood.org.
*Sources of information include the Arc of the United States (see footnote, p. 613); the American Association on Intellectual and Developmental Disabilities, 444 N. Capitol Street NW, Suite 846, Washington, DC 20001-1512; (800) 424-3688; fax: (202) 387-2193; http://www.aamr.org; the National Down Syndrome Society (see footnote, p. 613); and the National Down Syndrome Congress, 1370 Center Drive, Suite 102, Atlanta, GA 30338; (800) 232-6372 or (770) 604-9500; http://www.ndsccenter.org.
*PO Box 37, Walnut Creek, CA 94597; (800) 688-8765 or (925) 938-9300; fax: (925) 938-9315; http://www.fragilex.org.
*Information about hearing aids is available from the International Hearing Society, 16880 Middlebelt Road, Suite 4, Livonia, MI 48154; (800) 521-5247 or (734) 522-7200; fax: (734) 522-0200; http://ihsinfo.org.
*Hearing Enrichment Language Program of the Hough Ear Institute, 3434 N.W. 56th St., Oklahoma City, OK 73112; (405) 945-7186; fax: (405) 947-6266; http://www.integris-health.com/INTEGRIS/en-US/Specialties/EarInstitute/HELP.
*Other sources of information on several aspects of hearing loss and on the International Parents’ Organization are the Alexander Graham Bell Association for the Deaf and Hard of Hearing, 3417 Volta Place NW, Washington, DC 20007; voice: (202) 337-5220; TTY: (202) 337-5221; fax: (202) 337-8314; http://www.agbell.org; and Canadian Hearing Society, 271 Spadina Road, Toronto, Ontario M5R 2V3; voice: (416) 928-2500; TTY: (416) 964-0023; fax: (416) 928-2506; http://www.chs.ca.
*Directory listings stating “TDD or TTY only” before a phone number indicate that regular telephone use is not possible; “TDD or TTY and voice” indicates that both TDD/TTY users and speaking, hearing people can use the telephone number.
†Additional information is available from the National Captioning Institute, 1900 Gallows Road, Suite 3000, Vienna, VA 22182; (703) 917-7600; fax: (703) 917-9878; http://www.ncicap.org.
*11 Penn Plaza, Suite 300, New York, NY 10001; (800) 232-5463 or (212) 502-7600; fax: (212) 502-7777; http://www.afb.org.
†1800 Johnson St., Baltimore, MD 21230; (410) 659-9314; fax: (410) 685-5653; http://www.nfb.org.
‡PO Box 317, Watertown, MA 02471; (800) 562-6265; fax: (617) 972-7444; http://www.napvi.org.
§22 W. 21st St., 6th Floor, New York, NY 10010; (212) 889-3141; fax: (212) 727-2931; http://www.navh.org.
 1155 15th St. NW, Suite 1004, Washington, DC 20005; (800) 424-8666; fax: (202) 467-5085; http://www.acb.org.
1155 15th St. NW, Suite 1004, Washington, DC 20005; (800) 424-8666; fax: (202) 467-5085; http://www.acb.org.
¶1929 Bayview Ave., Toronto, Ontario M4G 3E8; (800) 563-2642; fax: (416) 480-7700; http://www.cnib.ca.
*A catalog of numerous products for people with vision problems is available from American Foundation for the Blind (see previous footnote) and from Lighthouse International, 111 E. 59th St., New York, NY 10022-1202; (212) 821-9200 or (800) 829-0500; http://www.lighthouse.org.
†National Library Service for the Blind and Physically Handicapped, (888) 657-7323; TTD: (202) 707-0744; fax: (202) 707-0712; http://www.loc.gov/nls. (A state-by-state listing of libraries for blind and physically handicapped readers, as well as other reference circulars, is available from this office.)
‡20 Roszel Road, Princeton, NJ 08540; (800) 221-4792 or (866) RFBD-585; http://www.rfbd.org.
*See footnote on p. 635.
 IN TEXT
IN TEXT
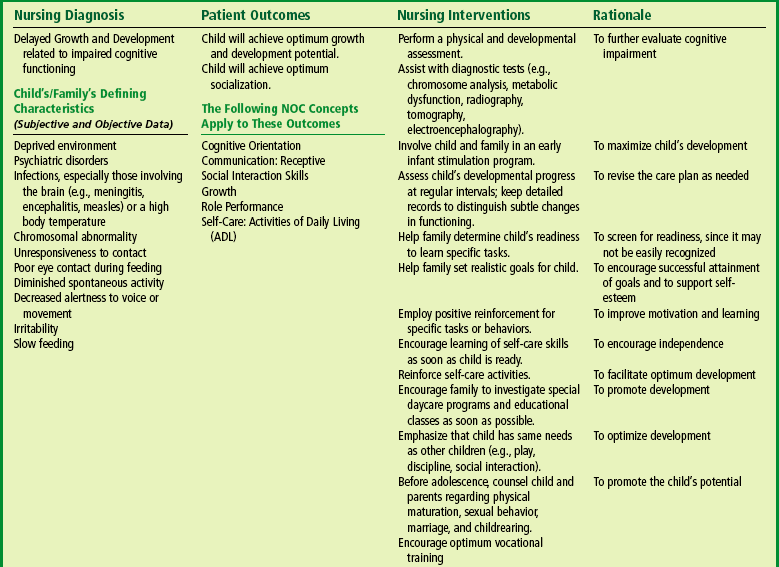
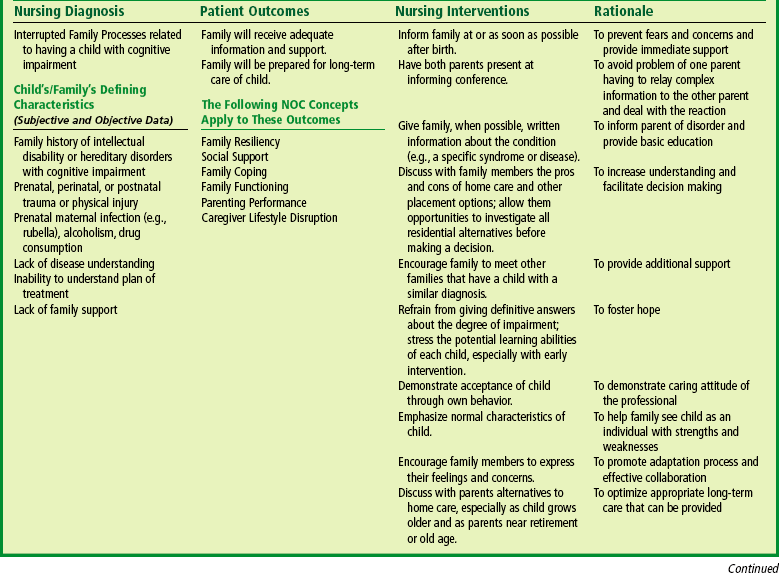
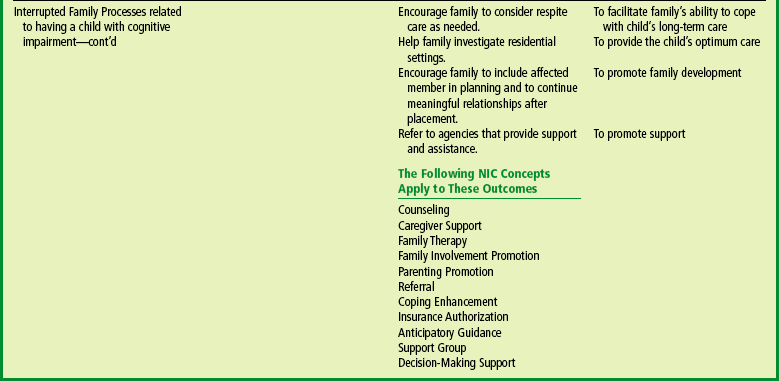



 CRITICAL THINKING EXERCISE
CRITICAL THINKING EXERCISE