18 THE STRUCTURE AND FUNCTION OF THE INTEGUMENTARY SYSTEM
INTRODUCTION
The integumentary system consists of the skin and its appendages including the hair, nails, sweat glands and sebaceous glands. The word integument is derived from the Latin word meaning ‘to cover’, which is precisely the main function of the integumentary system. It is the body’s first line of defence, providing a protective barrier against microorganisms, ultraviolet (UV) radiation, dehydration and pollutants in the external environment. It is also involved in a number of major functions, including temperature regulation, sensation, vitamin D synthesis and excretion, in order to provide protection for the body and contribute to homeostasis. The functions of the skin are closely integrated to those of other systems of the body. For example, the integument functions with the skeletal and muscular systems to provide protection and support to the body.; and vitamin D produced in the skin is used for absorption of calcium from the digestive tract and renal tubules. Therefore, the integumentary system is vital to many homeostatic mechanisms of other body systems.
To understand how the disease process alters integumentary function, it is first necessary to appreciate the normal structure and function of the integumentary system and its normal structural changes across the life span. This is particularly important and contemporary for students in Australia and New Zealand, as these two countries have the highest rates of skin cancer in the world. We start our exploration of the integumentary system with the anatomy of the skin.
THE STRUCTURE OF THE SKIN
Layers of the skin
There are many amazing facts about the skin. It covers the entire body, with a surface area of approximately 1.8 m2 in the adult. And it is the largest organ of the body, accounting for approximately 7% of body weight. Yet it is only approximately 1.5–4 mm thick, meaning that generally it is thin. In fact, the skin consists of two layers: (1) the epidermis, an outer layer of epithelial tissue; and (2) the dermis, an inner layer of connective tissue. Underlying these two layers is the hypodermis — this is not part of the skin. We also refer to this layer as the subcutaneous layer, which means under the skin. The hypodermis is mainly composed of adipose cells (fat), which provide insulation, preserving heat in the body and cells involved in tissue repair, and forming connective tissue (fibroblasts) (see Figure 18-1).
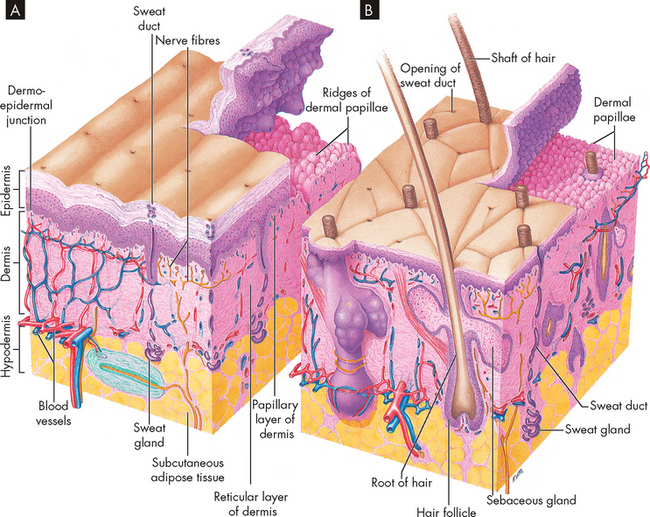
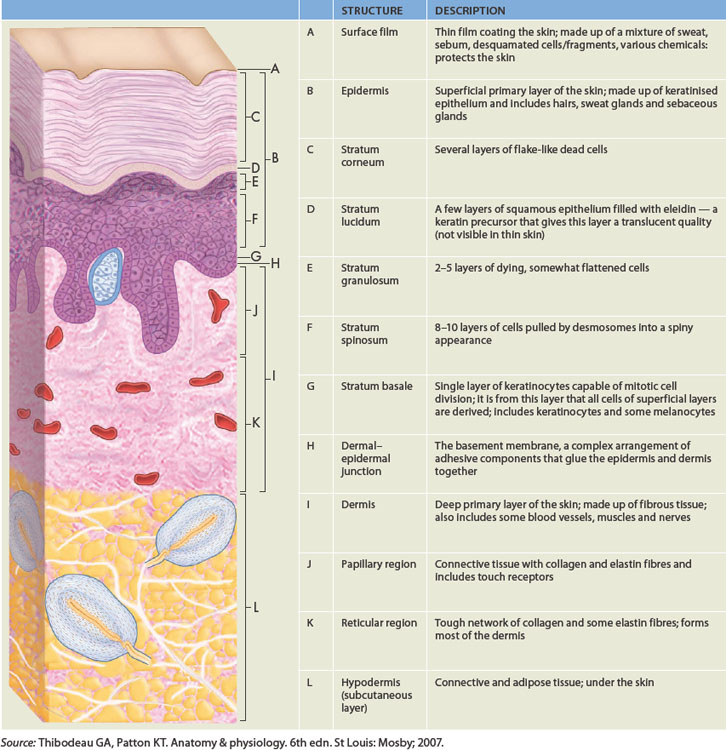
FIGURE 18-1 The structure of the skin.
A Thick skin, found on the surface of the palms and soles of the feet. B Thin skin found on most parts of the body. The skin consists of two layers: the outer epidermis and the dermis. Underlying these layers is the hypodermis composed of fatty tissue. Note the ridges of the dermis where the epidermis has been raised.
Source: Based on Patton KT, Thibodeau GA. Anatomy & physiology. 7th edn. St Louis: Mosby; 2010.
The epidermis
The epidermis is composed of stratified squamous epithelium. This means that the cells are layered, squamous in shape and make up epithelial tissue, which is a protective lining tissue (see Chapter 3). Four types of cell are found in the epidermis:
There are four or five layers in the epidermis, depending on the location in the body. The thick skin found on the fingertips, palms of the hands and soles of the feet consists of five layers (see Figure 18-2). Thick skin is free of hair and the underlying dermal papillae are raised, producing epidermal ridges on the surface of the skin. These ridges increase friction and on the fingertips form fingerprints. The thin skin covering most of the body has four layers and a smooth surface. The layers are referred to as stratum, meaning parallel layers. The layers are shown and detailed in Figure 18-3 and Table 18-1.
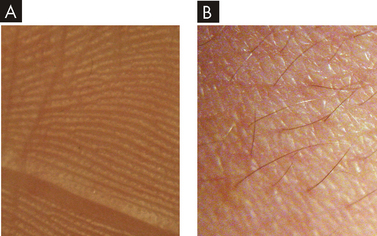
FIGURE 18-2 Thick and thin skin.
A The surface of the thick skin is hairless and has deep sulci (grooves) and friction ridges. B Thin skin has irregular sulci and contains hair.
Source: Patton KT, Thibodeau GA. Anatomy & physiology. 7th edn. St Louis: Mosby; 2010.
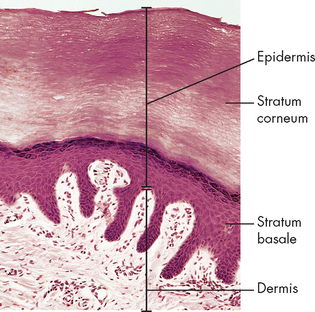
FIGURE 18-3 Photomicrograph of the skin.
The stratum basale and corneum are shown in the epidermis with the dermal layer underneath.
Source: Thibodeau GA, Patton KT. Structure and function of the body. 13th edn. St Louis: Mosby; 2008.
Let’s start with the deepest layer and work out towards the surface of the skin:
 Stratum basale. The stratum basale, sometimes referred to as the stratum germinativum, is the deepest layer of the epidermis and consists of a single row of new keratinocytes. The word basale refers to base. Stem cells undergo mitosis and continually produce new keratinocytes in this layer. The layer is also populated with melanocytes and Merkel cells.
Stratum basale. The stratum basale, sometimes referred to as the stratum germinativum, is the deepest layer of the epidermis and consists of a single row of new keratinocytes. The word basale refers to base. Stem cells undergo mitosis and continually produce new keratinocytes in this layer. The layer is also populated with melanocytes and Merkel cells. Stratum spinosum. The stratum spinosum (meaning prickly layer) consists of 8–10 rows of irregular-shaped keratinocytes that are held tightly together giving strength to the skin. Langerhans’ cells are also found in this layer.
Stratum spinosum. The stratum spinosum (meaning prickly layer) consists of 8–10 rows of irregular-shaped keratinocytes that are held tightly together giving strength to the skin. Langerhans’ cells are also found in this layer. Stratum granulosum. The stratum granulosum consists of 3–5 rows of keratinocytes that are different in shape from the basale and spinosum layers. In this layer the nuclei and cell organelles begin to degenerate and the cells flatten. The cells contain keratinohyaline, a substance that assists in the formation of keratin in the layers above. In addition, there are granules that secrete a glycolipid (carbohydrate and lipid) substance that fills the spaces between the cells preventing loss and entry of water. This essentially waterproofs the epidermis and slows water loss from the skin.
Stratum granulosum. The stratum granulosum consists of 3–5 rows of keratinocytes that are different in shape from the basale and spinosum layers. In this layer the nuclei and cell organelles begin to degenerate and the cells flatten. The cells contain keratinohyaline, a substance that assists in the formation of keratin in the layers above. In addition, there are granules that secrete a glycolipid (carbohydrate and lipid) substance that fills the spaces between the cells preventing loss and entry of water. This essentially waterproofs the epidermis and slows water loss from the skin. Stratum lucidum. The stratum lucidum, the clear layer, is found only in thick skin. It consists of 2–3 rows of clear, flat keratinocytes.
Stratum lucidum. The stratum lucidum, the clear layer, is found only in thick skin. It consists of 2–3 rows of clear, flat keratinocytes. Stratum corneum. The stratum corneum (horny layer), the outermost layer of the epidermis, consists of 20–30 rows of flattened, dead keratinocytes. Consisting mainly of keratin, this layer helps protect the body from water loss, injury and entry of foreign substances. Cells are continuously shed from the stratum corneum and replaced at the same rate by cells from the deeper layers.
Stratum corneum. The stratum corneum (horny layer), the outermost layer of the epidermis, consists of 20–30 rows of flattened, dead keratinocytes. Consisting mainly of keratin, this layer helps protect the body from water loss, injury and entry of foreign substances. Cells are continuously shed from the stratum corneum and replaced at the same rate by cells from the deeper layers.There is a thin layer of sebum, sweat and cell fragments covering the epidermis. This surface film varies in thickness and chemical composition over different areas of the body.
The dermis
Immediately under the epidermis is the dermis. The dermis is strong and flexible and is a thicker layer than the epidermis. It consists of connective tissue and cells such as fibroblasts and macrophages. Within this tissue are fibres embedded in a semi-fluid matrix. There are collagen fibres (fibrous protein found in connective tissue), which give the skin its resilience as well as binding water to maintain skin hydration, and elastin fibres, similar to collagen but with elastic properties that cause the skin to recoil after stretching. Structures found in the dermis include blood vessels, lymphatic vessels, smooth muscles, nerve endings and hair follicles. The dermis is divided into a thinner superior layer, the papillary layer, and a deep thick layer, the reticular layer:
 The papillary layer is composed of connective tissue with a rich supply of blood vessels. Its surface forms folds called papillae that extend into the epidermis (see Figure 18-3). Diffusion of nutrients from the capillary loops located in the papillae provides nourishment to the epidermis, which has no blood supply. Also located in the papillary layer are free nerve endings (pain receptors) and touch receptors.
The papillary layer is composed of connective tissue with a rich supply of blood vessels. Its surface forms folds called papillae that extend into the epidermis (see Figure 18-3). Diffusion of nutrients from the capillary loops located in the papillae provides nourishment to the epidermis, which has no blood supply. Also located in the papillary layer are free nerve endings (pain receptors) and touch receptors. The reticular (net-like) layer forms about 80% of the dermis and is composed of dense irregular connective tissue. The dense bundles of collagen fibres provide resilience as well as binding water. Adequate water content helps maintain skin turgor (elasticity or tension produced by the water and the cell contents). The collagen and elastin fibres in each location of the body are arranged in parallel bundles that form cleavage lines. This is important when considering where to locate surgical incisions. Incisions parallel to the cleavage lines will result in less stress to the wound and therefore faster healing with less scar tissue. In contrast, overstretching of the dermis, such as during pregnancy and obesity, may damage the dermis, causing stretch marks called striae.
The reticular (net-like) layer forms about 80% of the dermis and is composed of dense irregular connective tissue. The dense bundles of collagen fibres provide resilience as well as binding water. Adequate water content helps maintain skin turgor (elasticity or tension produced by the water and the cell contents). The collagen and elastin fibres in each location of the body are arranged in parallel bundles that form cleavage lines. This is important when considering where to locate surgical incisions. Incisions parallel to the cleavage lines will result in less stress to the wound and therefore faster healing with less scar tissue. In contrast, overstretching of the dermis, such as during pregnancy and obesity, may damage the dermis, causing stretch marks called striae.Extending through the reticular layer are the hair follicles with arrector pili muscles attached, sebaceous glands, sweat glands, blood and lymphatic vessels and nerves. Cutaneous receptors located throughout the reticular layer enable the skin to receive stimuli for the sensations of touch, pressure and temperature.
The dermal–epidermal junction
The area between the dermis and epidermis, the dermal–epidermal junction, is composed of a basement membrane. The two layers are adhered together by specialised fibres and a polysaccharide gel. Downward finger-like projections of the epidermis called rete ridges fit into the upward projections of the papillary layer of the dermis. This anchors the two layers together, thereby providing resistance against shearing forces.
Skin colour
Polygenetic inheritance determines skin colour (see Chapter 5). Each individual’s skin colour results from the combination of pigments (melanin, carotene and haemoglobin) and dermal circulation. The number of melanocytes is relatively similar in all humans, so differences in skin colour are related to the amount of melanin produced and stored within each melanocyte. The melanin, once produced, is packaged into vesicles called melanosomes that are transferred to the keratinocytes. Skin colour depends on the size, number and distribution of the melanosomes rather than the density of the melanocytes.1
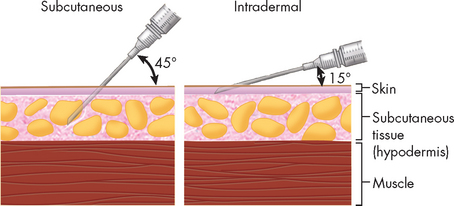
Box 18-1 INTEGUMENTARY SYSTEM INJECTIONS
In clinical practice, some drugs, such as vaccines, are administered by injection into the skin or subcutaneous tissue (see Figure 18-4). For example, insulin is administered into the subcutaneous tissue by subcutaneous injection and some vaccines are administered into the skin by intradermal injection.
However, the melanocytes of darkly pigmented skin are more active and produce up to ten times more melanin than do the melanocytes of white skin. Also, in light skin, the melanosomes are transferred to keratinocytes in the lower two layers of the epidermis and the pigment is degraded by enzymes. Therefore, there is no melanin in the upper layers of the epidermis. On the other hand, the melanosomes in dark skin are transferred to keratinocytes in more layers of the epidermis and melanin persists in the stratum corneum, leaving the skin by natural desquamation.1
Dysfunction of the melanocytes may lead to pigmentation abnormalities. For example, a recessive genetic trait causing failure to produce tyrosine (an amino acid) results in the absence of melanin, a condition called albinism. Another condition in which there is an acquired loss of melanocytes in areas of the epidermis is vitiligo. This results in patchy white areas of skin (see Figure 18-5). Damage to the melanocyte’s DNA may cause melanoma, which is discussed in Chapter 19.

Areas of patchy white skin resulting from the acquired loss of melanocytes.
Source: Thibodeau GA, Patton KT. The human body in health and disease. 4th edn. St Louis; Mosby; 2005.
In addition to melanin, carotene (an orange pigment found in some vegetables such as carrots) accumulates in epidermal cells, thereby contributing to skin colour. Finally, dermal blood flow and oxygenation also contribute to skin colour. Oxygen bound to haemoglobin gives blood a bright-red colour, causing the pink colour of light skin. Deoxygenated blood is a dark-red colour and gives the skin a bluish colour, called cyanosis. Constriction of cutaneous blood vessels reduces blood flow to the skin causing skin pallor, while vasodilation causes redness (erythema).
Often an abnormal skin colour is the sign of disease. Abnormal skin colours are summarised in Table 18-2.
Table 18-2 ALTERATIONS OF SKIN COLOUR
| ABNORMAL SKIN COLOUR | EXAMPLE |
|---|---|
| Cyanosis A bluish colour to the skin resulting from a severe decrease in blood oxygen content. |
 |
| Jaundice Yellow discolouration of the skin caused by increased blood levels of bilirubin, a substance formed when haemoglobin is broken down. Jaundice may be a sign of liver dysfunction. |
 |
| Pallor Pale skin resulting from reduced haemoglobin or temporarily reduced blood flow to the skin. Pallor may be a sign of anaemia or shock. |
 |
| Bruise A blue or purple discolouration of the skin resulting from blood seeping into the tissue from damaged blood vessels. A bruise may be caused by blunt tissue injury or it may be a sign of a coagulation disorder. |
 |
| Erythema Redness resulting from increased blood flow to the skin. Erythema may be a sign of hypertension or inflammation. |
 |
Source: A from Thibodeau GA, Patton KT. Anatomy & physiology. 6th edn. St Louis: Mosby; 2007; B from Forbes CD, Jackson WF. Color atlas and text of clinical medicine. 3rd edn. London: Mosby; 2003; C from McCance KL. Pathophysiology: the biologic basis for disease in adults and children. 5th edn. St Louis: Mosby; 2005; D from Little JW. Dental management of the medically compromised patient. 7th edn. St Louis: Mosby; 2007; E from Kliegman RM. Nelson textbook of pediatrics. 18th edn. Philadelphia: Saunders; 2007.
APPENDAGES OF THE SKIN
Arising from the epidermis are accessory structures that include the hair, nails, sweat glands and sebaceous glands (see Figure 18-6).
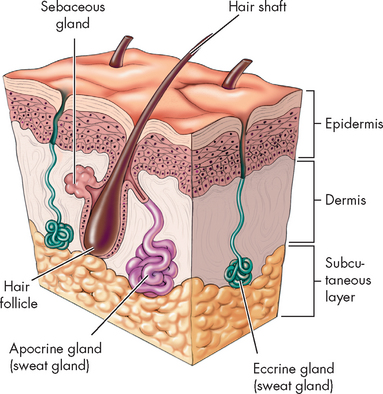
FIGURE 18-6 Appendages of the skin.
Hair and skin glands: sebaceous glands and sweat glands.
Source: Based on Herlithy B. The human body in health and illness. 3rd edn. St Louis: Saunders; 2007.
Hair
Hair is found over most of the body with the exception of the palms of the hands, the soles of the feet, the lips, nipples and parts of the external genitalia. Hairs are produced in hair follicles, cavities in the skin. The walls of the follicle consist of an internal and external root sheath, derived from the epidermis, and a dermal root sheath derived from the dermis. Attached to each hair follicle is a sebaceous gland that produces sebum to lubricate the hair and an arrector pili muscle. Contraction of this smooth muscle causes the hair to become more erect, resulting in ‘goose bumps’ when cold or frightened.
Each hair consists of a bulb from where the hair originates, a root that is the portion of hair in the follicle and a shaft, the portion of hair extending from the surface of the skin (see Figure 18-7).
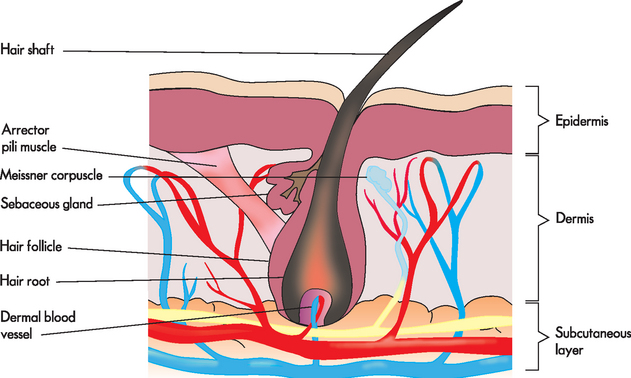
FIGURE 18-7 The structure of the hair and skin.
Source: Based on Herlithy B. The human body in health and illness. 3rd edn. St Louis: Saunders; 2007.
The hair bulb contains a mass of undifferentiated cells, the matrix, which produces the hair. Extending into the bulb is the dermal papilla containing blood capillaries, which provide nourishment to the cells of the matrix. Once formed by the matrix, the cells become keratinised and push upwards as new cells are added.
Nails
The distal ends of the fingers and toes are protected by plates of hard keratinised epithelial cells, the fingernails and toenails. The nails consist of a distal visible section, the nail body, and a proximal section concealed under the skin, the nail root. The nail body is bounded by nail grooves and nail folds. The proximal nail fold forms the eponychium, or cuticle. A layer of epithelium called the nail bed lies under the nail (see Figure 18-8).
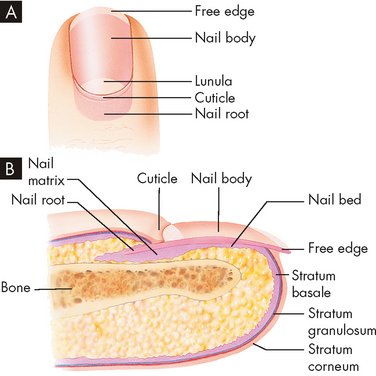
FIGURE 18-8 The structure of the fingernail.
A Viewed from above. B Sagittal section.
Source: Patton KT, Thibodeau GA. Anatomy & physiology. 7th edn. St Louis: Mosby; 2010.
As a result of the rich blood supply in the underlying dermis the nail appears pink. In clinical practice, when patients have a sudden fall in oxygen levels to the tissues, the first location that cyanosis is often observed is the nail bed. Nail growth occurs from the matrix at the base of the nail root. New cells are produced by mitosis in the stratum basale of the matrix. These cells become keratinised and move distally.
Sweat glands
Sweat glands are the most numerous glands in the skin. There are two types of sweat glands, eccrine and apocrine, which vary with location and type of secretion.
Eccrine sweat glands
Eccrine sweat glands are more numerous and widespread than apocrine sweat glands, with a particular abundance on the palms of the hands, the soles of the feet and forehead. Eccrine sweat glands are coiled tubular glands with the secretory portion of the gland located in the dermis. The duct opens at a pore on the skin surface.
Eccrine sweat glands secrete sweat that is produced in the secretory part of the gland. Sympathetic stimulation of the sweat glands causes the sweat to be secreted onto the surface of the skin, which is a powerful mechanism for heat loss and therefore plays an important role in the regulation of body temperature.
Sweat is a hypotonic solution (lesser concentration of solute) derived from the blood. It is acidic with a pH of 4–6.8. It consists primarily of water with small quantities of electrolytes (such as sodium and chloride) and some metabolic wastes (such as urea and ammonium) and dermacidin, an antimicrobial peptide.
Apocrine sweat glands
Apocrine sweat glands are located in the axilla, areolar of the breast and pubic regions. They are simple branched glands whose ducts empty into hair follicles. Apocrine sweat glands are larger than eccrine sweat glands and do not develop until puberty. Apocrine sweat is more viscous and milky than eccrine sweat. As well as water and electrolytes, it also contains fatty acids and protein. Although odourless when secreted, degradation by bacteria is the cause of body odour.
Sebaceous glands
Sebaceous glands are simple branched glands whose ducts mainly open into hair follicles. The ducts of some structures such as the glans penis open onto the skin surface. The sebaceous glands secrete an oily substance, sebum, which contains triglycerides, fatty acids, cholesterol, proteins and electrolytes. Sebum functions to lubricate the hair and skin. It also has an antimicrobial action.
THE FUNCTION OF THE INTEGUMENTARY SYSTEM
The function of the integumentary system is to protect the underlying tissues from physical, chemical and microbial damage and to maintain homeostasis.
Protection
The skin’s primary function is to protect the body from invasion of harmful substances, damage by environmental factors such as ultraviolet radiation, and loss of fluids and electrolytes. The integument’s physical, chemical and biological barriers provide this protection.
Physical barrier
An intact skin provides a formidable barrier preventing the entry of microorganisms and is the body’s first line of defence. Constant renewal of the epidermis and desquamation with the elimination of adhering microorganisms ensures maintenance of an intact physical barrier. The barrier is created by the continuity of keratinocytes filled with the tough, insoluble protein, keratin. Keratin is the predominant component of the epithelial cells and constitutes 85% of the cellular protein in keratinised cells of the stratum corneum.2 Deeper in the epidermis between the stratum granulosum and stratum spinosum, a water barrier is formed by lipids secreted by the keratinocytes and the tight junctions between the cells. This barrier functions to retain water in the body. Although the epidermis prevents entry by most substances, a small amount of lipid-soluble substances, organic solvents and heavy metal salts are able to penetrate the skin.
In clinical practice, transdermal drug delivery systems have been developed to enable drugs to be administered through the skin to obtain systemic effects. This delivery system has advantages, such as a controlled release into the patient, reduced systemic effects and improved drug compliance. However, for the drug to be able to diffuse through the epidermis it must be soluble in the lipophilic layer as well as the more aqueous structures and have a small molecular size.3,4 A number of drugs are now administered via this route including fentanyl (Durogesic® patch), glyceryl trinitrate (Transiderm-nitro® patch) and nicotine.
Chemical barrier
The skin and its appendages secrete a number of chemicals that provide protection against microorganisms and other harmful substances. The pH of the skin is acidic, resulting mainly from the secretion of sweat from the eccrine glands. This ‘acid mantle’ creates an environment on the skin surface that is not conducive to microorganism growth. Secretion of antimicrobial substances also contributes to the chemical barrier — for instance, lysozyme (an enzyme) from apocrine sweat glands breaks down bacterial cell walls.5–7 4 6 In addition, melanin protects cells from ultraviolet radiation. It forms a protective cap over the nuclei of viable skin cells, absorbing the ultraviolet light and shielding DNA from damage.8
Biological barrier
A number of cells in the skin provide a biological barrier to prevent invasion by foreign substances such as bacteria. Langerhans’ cells located in the epidermis process and present antigens to helper T cells to stimulate antibody production (see Chapter 12). In addition, virus particles are presented to cytotoxic T cells which trigger immune responses.9 Memory T cells in the skin also provide local immunity against pathogens. If foreign substances penetrate the epidermis, they may come into contact with this line of defence cells, the dermal macrophages. Furthermore, eccrine sweat glands contain secretory IgA that is believed to have a role in cutaneous immunity.10
Regulation of body temperature
The integumentary system plays an important role in thermoregulation. Structures of the integumentary system that function in the regulation of body temperature are the peripheral thermoreceptors, sweat glands and cutaneous blood vessels. The thermoreceptors in the skin are stimulated by hot or cold conditions. After these afferent nerve signals have been interpreted and processed by the hypothalamus, efferent nerve signals are sent to the blood vessels and sweat glands in the skin. When body temperatures are elevated, sweat glands are activated and sweat is evaporated from the surface of the skin, thus cooling the body. The cutaneous blood vessels dilate, thereby allowing more warm blood to be brought to the surface for heat dissipation. In cold conditions, the cutaneous blood vessels constrict, causing warm blood to be retained in the body core. In addition, shivering in skeletal muscles increases heat production, thereby raising body temperature. Thermoregulation is discussed fully in Chapter 13.
Cutaneous sensation
The skin contains a number of sensory receptors that enable the body to detect and respond to changes in the environment. For instance, thermoreceptors and nociceptors (stimulated by pain) are located in the dermis. Merkel cells, located in the basal layer of the epidermis, are involved in the sensation of light touch. Other receptors involved in touch include Meissner’s corpuscles located in the dermal papillae (which assist with two-point discrimination), Ruffini’s end organs (which detect continuous touch or pressure) and pacinian corpuscles (which detect deep pressure and vibration). Hair follicle receptors respond to bending of hairs and detect light touch.
Synthesis of vitamin D
The major source of vitamin D in the body is exposure to sunlight. When exposed to ultraviolet radiation, a cholesterol-related steroid located in the skin is converted into a form of vitamin D (vitamin D3), which, when passing through the liver and kidneys, is converted to the active form of vitamin D (calcitriol). Vitamin D is required by the small intestine for absorption of calcium and phosphorus.
Excretion
The skin has only a small role in excretion. Small amounts of ammonia, urea and uric acid are excreted in the sweat.
PAEDIATRICS AND THE INTEGUMENTARY SYSTEM
The skin undergoes a number of changes from birth through to old age. The newborn infant has soft, velvety skin covered with an oily substance, vernix caseosa — a mixture of desquamating cells and sebum. Skin surface lipids are low in cholesterol and high in wax esters in the first two weeks after birth.11 Shortly after birth the sebaceous glands begin a period of inactivity until puberty. As a result of low melanocyte function the skin of the newborn is less pigmented. The nerve network and cutaneous receptors, with the exception of Meissner’s corpuscles, are completely developed by birth. At birth the skin’s acid mantle develops12 and within the first hours of life colonisation by skin microorganisms, which are part of the skin flora, occurs.13 During childhood the skin remains smooth and flexible. There are fewer sweat glands and the sebaceous glands remain inactive throughout childhood.
With the secretion of sex hormones at puberty, the apocrine sweat glands and sebaceous glands are activated. Increased production of sebum causes the skin to be oilier. With secretion of apocrine sweat body odour develops. Also, evaporation of sweat plays a greater role in thermoregulation than in childhood. These glands remain active during adolescence and adulthood with activity decreasing after middle-age. At puberty there is a change in the skin flora with greater numbers of Propionibacterium acne present on the skin surface.
AGEING AND THE INTEGUMENTARY SYSTEM
Ageing of the skin is a complex process consisting of both an intrinsic component that is genetically determined and an extrinsic component that is related to environmental factors (these concepts are elaborated on in Chapter 37). It is now believed that ageing is not ‘coded’ in the genome but modifications in gene functions are involved.14 Researchers have shown that gene expression is significantly altered during human skin ageing.15 For example, regulation of genes involved in cell cycle control, manufacture of elastin and collagen and manufacture of the extracellular matrix have been shown to be altered in ageing.15,16
Extrinsic factors that cause ageing include exposure to sunlight, cigarette smoking and health status. Exposure to sunlight is the most significant extrinsic factor causing skin ageing. Ultraviolet radiation is absorbed by skin molecules, generating reactive oxygen species that damage cellular components (refer to Chapter 4), interfere with enzymes that are required for DNA repair and interfere with Langerhans’ cells.17,18 Ultraviolet radiation also initiates damage to genetic material resulting in mutations. Thus photoageing (the effects of chronic ultraviolet light exposure on the skin) causes ageing by both directly damaging cellular components and amplifying the effects associated with normal intrinsic ageing. Nicotine damages skin by decreasing blood flow and thus oxygen and nutrients to the skin.17
Ageing causes changes to both the epidermis and the dermis of the skin, as well as the subcutaneous layer and skin appendages. Epidermal cell production slows, causing the skin surface to become thinner and more easily damaged. The number of melanocytes and Langerhans’ cells in the epidermis decreases, resulting in less protection from microbiological invasion and ultraviolet radiation. In addition, the mechanisms required to synthesise vitamin D in epidermal cells become less efficient, leading to lower levels of vitamin D in the elderly.19 Finally, the dermal–epidermal junction flattens with destruction of the dermal papillae and rete pegs so that the epidermal layer can separate from the dermis more easily.20
In the dermis there are age-related changes to the fibres, cells and appendages. The dermis atrophies with a 20% reduction in dermal thickness.21 Decreased numbers of collagen and elastin fibres and increased linkage of the fibres cause the skin to become thin, fragile and inelastic. As a result, after stretching the skin fails to recover its shape and wrinkles develop.22 Dermal cells such as fibroblasts are decreased in number. Reduced numbers and increased fragility of the dermal capillaries cause the skin to be more easily bruised. With reduced numbers of nerve endings sensory perception is affected and there may be difficulty in discriminating between heat, pain and itching.23 Structural modifications and an overall decline in numbers of Meissner’s corpuscles and pacinian corpuscles have been associated with diminished vibration perception and two-point discrimination. It has been suggested that these changes to perception could contribute to a higher number of falls in the aged.24 In addition, a reduction in the number and function of the sebaceous and sweat glands causes the skin to become drier and thermoregulation is less efficient. The hair follicles are reduced in number and so the hair thins, and with the reduction in melanocyte function the hair also becomes grey.
The subcutaneous layer, which consists primarily of adipose tissue and provides protection and insulation to the body, also atrophies with age. The changes to the integumentary system resulting from the ageing process lead to an increased risk of injury to the skin, slower wound healing and an increased risk of skin infections. In addition to these effects, older skin may not respond as efficiently to topical medications.
The structure of the skin
 The epidermis is a stratified squamous epithelium composed of the stratum basale, stratum spinosum, stratum granulosum, stratum lucidum and stratum corneum.
The epidermis is a stratified squamous epithelium composed of the stratum basale, stratum spinosum, stratum granulosum, stratum lucidum and stratum corneum. Types of cells found in the epidermis are keratinocytes, melanocytes, Langerhans’ cells and Merkel cells.
Types of cells found in the epidermis are keratinocytes, melanocytes, Langerhans’ cells and Merkel cells. Keratinocytes are formed by mitosis of stem cells in the stratum basale. As they are pushed up towards the surface they lose their nuclei and organelles and become filled with keratin. Dead cells desquamate from the stratum corneum.
Keratinocytes are formed by mitosis of stem cells in the stratum basale. As they are pushed up towards the surface they lose their nuclei and organelles and become filled with keratin. Dead cells desquamate from the stratum corneum. The dermis is composed of connective tissue and is divided into two layers, the papillary and reticular layers. Extending through the dermis are hair follicles, sweat glands, sebaceous glands, blood and lymphatic vessels, and nerves. Receptors that receive sensory stimuli are also located in the dermis.
The dermis is composed of connective tissue and is divided into two layers, the papillary and reticular layers. Extending through the dermis are hair follicles, sweat glands, sebaceous glands, blood and lymphatic vessels, and nerves. Receptors that receive sensory stimuli are also located in the dermis.Appendages of the skin
 Hair is composed of dead keratinised cells. Each hair has three parts: (1) the bulb that produces hair; (2) the root; and (3) the shaft.
Hair is composed of dead keratinised cells. Each hair has three parts: (1) the bulb that produces hair; (2) the root; and (3) the shaft. Nails contain keratinised epidermal cells. They consist of the nail body, the visible section of the nail, and the nail root, the section concealed under the skin. Nails grow by mitosis of cells in the stratum basale of the matrix. Nails protect the distal ends of the fingers and toes.
Nails contain keratinised epidermal cells. They consist of the nail body, the visible section of the nail, and the nail root, the section concealed under the skin. Nails grow by mitosis of cells in the stratum basale of the matrix. Nails protect the distal ends of the fingers and toes. There are two types of sweat glands: eccrine sweat glands and apocrine sweat glands. Eccrine sweat glands are the more numerous being distributed over most of the body. They are small, simple coiled tubular glands that open onto the skin surface. They secrete sweat, excrete wastes and help regulate body temperature. Apocrine sweat glands are distributed in the axilla, areolar of the breast and pubic area. They are large, simple branched tubular glands and empty into hair follicles. They begin to function at puberty.
There are two types of sweat glands: eccrine sweat glands and apocrine sweat glands. Eccrine sweat glands are the more numerous being distributed over most of the body. They are small, simple coiled tubular glands that open onto the skin surface. They secrete sweat, excrete wastes and help regulate body temperature. Apocrine sweat glands are distributed in the axilla, areolar of the breast and pubic area. They are large, simple branched tubular glands and empty into hair follicles. They begin to function at puberty.The function of the integumentary system
 The skin protects the body from invasion of harmful substances, damage by environmental factors, and loss of fluids and electrolytes. It protects the body by physical barriers (continuous layer of keratinised cells), chemical barriers (acid pH, antimicrobial substances, melanin) and biological barriers (Langerhans’ cells, dermal macrophages).
The skin protects the body from invasion of harmful substances, damage by environmental factors, and loss of fluids and electrolytes. It protects the body by physical barriers (continuous layer of keratinised cells), chemical barriers (acid pH, antimicrobial substances, melanin) and biological barriers (Langerhans’ cells, dermal macrophages). Peripheral thermoreceptors, sweat glands and cutaneous blood vessels play an important role in the regulation of body temperature.
Peripheral thermoreceptors, sweat glands and cutaneous blood vessels play an important role in the regulation of body temperature. Sensory receptors located in the skin enable the body to respond to temperature, touch, pressure and pain.
Sensory receptors located in the skin enable the body to respond to temperature, touch, pressure and pain.Ageing and the integumentary system
 In childhood the skin is smooth and flexible. There are fewer sweat glands and sebaceous glands are quiescent.
In childhood the skin is smooth and flexible. There are fewer sweat glands and sebaceous glands are quiescent. Ageing of the skin involves both intrinsic (genetically determined) and extrinsic (environmental) factors. Changes to the skin include thinning of the skin surface, reduced numbers of melanocytes and Langerhans’ cells, atrophy of the dermis, decreased numbers of elastin and collagen fibres, increased fragility of dermal capillaries, reduced numbers of sebaceous and sweat glands, reduced number of hair follicles and atrophy of the subcutaneous layer.
Ageing of the skin involves both intrinsic (genetically determined) and extrinsic (environmental) factors. Changes to the skin include thinning of the skin surface, reduced numbers of melanocytes and Langerhans’ cells, atrophy of the dermis, decreased numbers of elastin and collagen fibres, increased fragility of dermal capillaries, reduced numbers of sebaceous and sweat glands, reduced number of hair follicles and atrophy of the subcutaneous layer.Jean is 85 years old and is a resident in an aged-care facility. She has a history of coronary artery disease and has a Transiderm-nitro® (glyceryl trinitrate) patch applied each day and removed at night. Jean walks with the aid of a walking frame, and although she prefers to remain in her room, the nurses encourage her to sit outside for about 10 minutes each day. Recently, when undressing, Jean sustained a skin tear to her arm. The epidermis separated from the dermis and epidermal tissue was lost. The wound was cleaned with normal saline and a nonadherent dressing was secured with a bandage.