Chapter 48 Drugs Affecting the Skin
The skin is the largest organ of the body; together with the hair and nails it forms the integumentary system. It serves as a barrier against the environment, protects underlying tissues, helps regulate body temperature and produces vitamin D. Drugs may be administered via topical and systemic routes for treatment of skin conditions or may be applied to the skin intended for transcutaneous absorption and systemic action. This chapter reviews the various formulations and topical products available and indications for their use. Groups of drugs that commonly cause adverse reactions in the skin are listed.
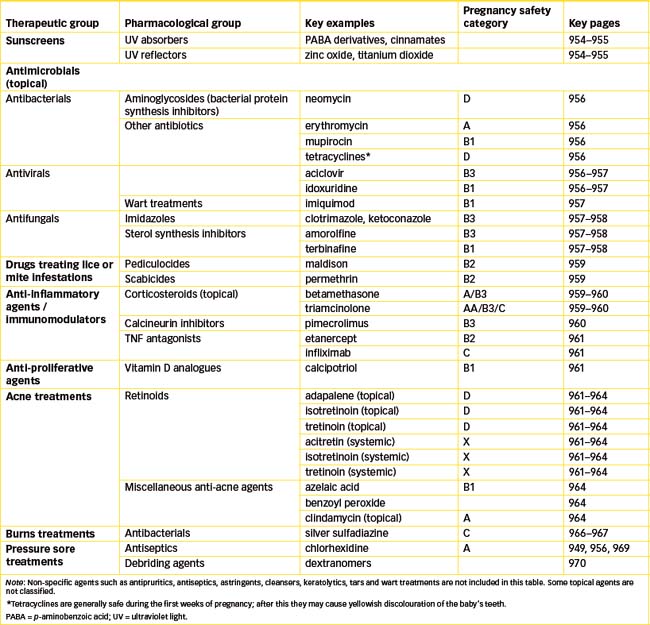
Drugs commonly applied to the skin include sunscreen preparations, antimicrobials, anti-inflammatory and immunosuppressant agents and drugs used in the treatment of acne, burns, pressure sores and leg ulcers. Their pharmacological actions, clinical uses and adverse effects are described.
Key abbreviations
Key background: structure, functions and pathologies of the skin
THE skin (or integument) has been described as the largest organ in the body. As the tissue most at risk of environmental damage, the skin often becomes infected, inflamed or impaired by antigens, mechanical injury or radiation. Medications for most diseases are administered at a site distant from the target organ, but in dermatology, medications can readily be applied directly to the target site. In addition, lipid-soluble drugs can be applied to the skin with the intention that they will be absorbed into the systemic circulation to act at distant sites, and drugs can be administered systemically to treat skin disorders.
Structure and functions of the skin
The skin is made up of two main layers, the epidermis and the dermis.
Epidermis
The epidermis, or thin outer skin layer, has no direct blood supply of its own; it is nourished only by diffusion. It consists of four layers of epithelial cells (see Figure 48-1):
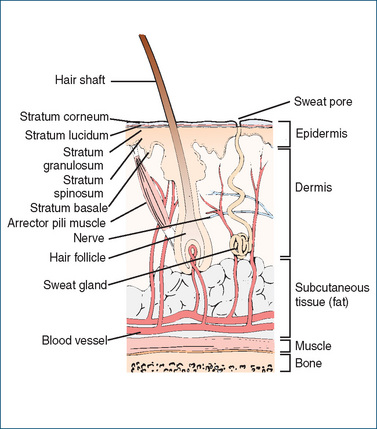
Figure 48-1 Structures of the skin.
Note: Details of nerves (autonomic and sensory) and sensory nerve endings are not shown.
Melanocytes, which are responsible for synthesising melanin, a pigment that occurs naturally in the hair and skin, are also located deep in the stratum germinativum. The more melanin that is present, the deeper brown the skin colour. Melanin is a protective agent: it blocks ultraviolet rays, thus preventing injury to the underlying dermis and tissues.
Dermis
The dermis lies between the epidermis and subcutaneous fat. It is about 40 times thicker than the epidermis and contains elastic and connective tissues that provide support for its blood vessels, nerves, lymphatic tissue, sweat glands, sebaceous glands and hair follicles.
Below the dermis is the hypodermis, or subcutaneous layer, which contributes flexibility to the skin. Subcutaneous fat tissue is an area for thermal insulation, nutrition and cushioning or padding.
The skin contains three types of exocrine glands opening on the surface of the skin through ducts in the epithelium: sebaceous (producing lubricating sebum), eccrine (producing sweat and helping cooling) and apocrine (producing odoriferous compounds). Normal skin pH is 4.5–5.5, which is weakly acidic and hence has a protective and antiseptic function. The appendages of the skin are the hair and nails.
Functions of the skin
The skin serves many functions in the body; some of the major functions are listed here.
Protection
The skin forms a protective covering for the entire body. As the old song puts it, ‘Skin’s what keeps your insides in’ and, more importantly, keeps the outsides out. Thus it is a barrier against microorganism invasion, chemicals, loss of water and heat and physical abrasion.
Sensation
Nerve endings permit the transfer of sensations, such as heat, cold, touch, pressure and pain.
Body temperature regulation
Skin helps maintain body temperature homeostasis by regulating heat loss or heat conservation. Blood vessels in the dermis area can dilate, and perspiration increases when the body temperature is elevated, encouraging evaporative cooling. If the body temperature is below normal, the skin blood vessels constrict and perspiration is decreased.
Body image
Skin (and hair) contributes to the concept of body image and a feeling of wellbeing. A disfiguring or chronic skin condition such as psoriasis, acne or alopecia can lead to emotional problems and depression.
Absorption, metabolism and excretion
Skin excretes fluid and electrolytes (via sweat glands), stores fat and synthesises vitamin D: when skin is exposed to sunlight or ultraviolet rays, the steroid 7-dehydrocholesterol, which is normally present in the skin, is converted to vitamin D3 (see Figure 33-3G, and Clinical Interest Box 37-2). Skin can also be a site for absorption of drugs, fat-soluble vitamins (A, D, E and K), oestrogens, corticosteroid hormones and lipid-soluble agents (see Clinical Interest Box 48-1).
Clinical Interest Box 48-1 Poisoned through the skin!
Some of the most toxic agents liable to be absorbed through the skin are the organophosphorus anticholinesterases, such as dyflos and malathion (now known as maldison). These were intended to be highly lipid-soluble, as they were developed to be absorbed through the lungs and skin of humans (as war gases) or through the cuticle of insects (as insecticides). Cases of toxicity occurring after transdermal absorption of these agents are quite common, e.g. in chemical workers, pest controllers and gardeners.
A case was reported in Melbourne in 1997 of an ambulance transporting an elderly man who had accidentally ingested insecticide solution (metasystox), mistaking it for a cough mixture. One of the ambulance officers also became dizzy, disoriented and nauseous from the fumes in the ambulance; he had been poisoned indirectly both by handling the clothing and by inhaling fumes escaping through the skin of the patient. Both patient and ‘ambo’ were successfully treated.
Source: The Age, Melbourne, 11 April 1997.
Skin disorders
Causes of skin disorders
Disorders of the skin may be due to allergy, infection, sensitivity to drugs or other chemicals, emotional stress, genetic predisposition (e.g. atopic eczema or psoriasis), hormonal imbalances or degenerative disease. Sometimes the cause of the skin disorder is unknown and the treatment is empirical, in the hope that the right remedy will be found; corticosteroids are often used in skin disorders for their anti-inflammatory and immunosuppressant actions.
Chemicals causing skin disorders
Table 48-1 is a summary of the vast range of dermatological reactions caused by chemicals (including drugs); some of these can be life-threatening, with high fever, pharyngitis, neck stiffness and epidermal necrolysis. It is important to be aware of the patient’s drug history and current therapy in order to relate such reactions to the appropriate cause, as simply discontinuing a particular drug may resolve a complicated dermatological problem of unknown origin.
Table 48-1 Drugs and other chemicals commonly causing dermatological conditions
| Skin condition | Description of pathology | Drugs & other chemicals potentially involved |
| Exfoliative dermatitis | Skin is inflamed, red and scaly & will eventually slough off; hair & nails may also be affected; hyperkeratosis, pruritis & physiological dysfunctions may occur. Eruption may take weeks or months to resolve after causative agent is stopped; can be fatal | Amiodarone, barbiturates, carbamazepine, frusemide, gold salts, griseofulvin, nifedipine, penicillin, phenothiazines, phenytoin, sulfonamides, tetracyclines |
| Stevens–Johnson syndrome (erythema multiforme) | Severe form involves widespread mucocutaneous lesions usually on face, neck, arms, legs, hands & feet. May also involve fever, haemorrhagic crusts, ocular lesions leading to blindness & multi-system involvement; can be life-threatening | Many drugs, especially carbamazepine, penicillins & cefalosporins, phenytoin, sulfonamides, tetracyclines |
| Lupus erythematosus | Autoimmune connective tissue disorder; erythematous rash may be flat or elevated on cheeks and across nose (butterfly); joint swelling & pain, rash, oral ulcers, serositis; renal, haematological, pulmonary & other systems may be affected. Reversible when drug is stopped | Hydantoins, hydralazine, isoniazid, procainamide, quinidine |
| Acneiform reaction | Reddened skin lesions resembling acne, an inflammatory disease of the pilosebaceous unit (hair follicle & sebaceous gland) | ACTH, androgenic hormones, corticosteroids, cyanocobalamin, hydantoins, iodides, oral contraceptives |
| Purpura | Multiple small haemorrhages in the skin and mucous membranes | ACTH, allopurinol, amitriptyline, anticoagulants, corticosteroids, digoxin, fluoxymesterone, gold salts, griseofulvin, iodides, nifedipine, paracetamol, penicillins, phenothiazines, quinidine, sulfonamides, thiazides |
| Urticaria | Skin oedema and wheals due to vasodilation & increased capillary permeability; may be immune-mediated | Aciclovir, amitriptyline, cefalosporins, chloramphenicol, chlorhexidine, enzymes, erythromycin, gold salts, griseofulvin, hydantoins, insulins, iodides, nitrofurantoin, opioids, penicillins, phenothiazines, salicylates, streptomycin, sulfonamides, tetracyclines, vaccines |
| Alopecia | Lack or loss of hair from area of skin where hair is normally present; baldness | Alkylating agents, anticoagulants, antimetabolites, antitumour antibiotics, heparin, lithium, norethisterone, spironolactone |
| Lichenoid reactions | Skin lesion resembling lichen, i.e. small, firm papules set close together | Chloroquine, gold salts, nifedipine, quinidine, thiazides |
| Fixed drug eruptions | Circumscribed inflammatory bullous or vesicular skin lesion that recurs at same site in response to administration of a drug, often with itching or burning, with rapid resolution after stopping the drug, possibly leaving residual pigmentation | Antihistamines, atropine, atorvastatin, barbiturates, bismuth salts, chloral hydrate, chlorpromazine, digoxin, disulfiram with alcohol, ergot alkaloids, eucalyptus oil, gold compounds, griseofulvin, iodine, opioids, penicillins, phenytoin, quinidine, quinines, salicylates, saccharin, streptomycin, sulfonamides, tetracyclines, vaccines |
| Contact dermatitis or eczema | Inflammation of the skin due to contact with a substance; may have allergic or irritant mechanism; allergic eczema = atopic dermatitis | Antihistamines, antiseptics, aspirin, bleomycin, captopril, cefalosporins, chloramphenicol, chlorpromazine, cosmetics, formaldehyde, glyceryl trinitrate, gold salts, iodine, lanolin, local anaesthetics, miconazole, neomycin, paraben preservatives, penicillins, peru balsam, phenol, quinines, streptomycin, sulfonamides, tetracyclines, transdermal patches |
| Photosensitivity | Abnormal response of the skin to sunlight or artificial light at wavelengths 280–400 nm; it may be photoallergy or phototoxicity | Amiodarone, anaesthetics (procaine group), antihistamines, antimalarials, barbiturates, benzene, bergamot (perfume), carbamazepine, carrots (wild), celery, chlorhexidine, chlorophyll, citrus fruits, clover, coal tar, corticosteroids (topical), desipramine, dill, disopyramide, dyes (fluorescein, methylene blue, toluidine blue), fennel, 5-fluorouracil, gold salts, grass (meadow), griseofulvin, haloperidol, mercaptopurine, methoxsalen, methoxypsoralen, mustards, naphthalene, oils (cedar, lavender, lime, sandalwood, vanillin), oral contraceptives, p-aminobenzoic acid, parsley, parsnips, phenolic compounds, phenothiazines, phenytoin, porphyrins, quinines, salicylates, silver salts, sulfasalazine, sulfonamides, sulfonylureas, sunscreens, tetracyclines, thiazide diuretics, toluene, tricyclic antidepressants, xylene |
Signs and symptoms
Common dermatological disorders include acne vulgaris (cystic acne and acne scars), atopic dermatitis, eczema, folliculitis, fungal infections, herpes simplex, lichen simplex, psoriasis, seborrhoeic dermatitis, skin cancers, verrucae (warts) and vitiligo. Reactions or disorders of the skin are manifested by symptoms such as itching, pain or tingling and by signs such as swelling, redness, papules, pustules, blisters and hives.
Dermatological diagnosis may require physical assessment; personal and family medical history; drug history including over-the-counter (OTC) medications; and laboratory tests, cytodiagnosis and biopsy. When the nature of the lesion has been established, its characteristics should be defined according to size, shape, surface and colour (Figure 48-2) and distribution on the body.
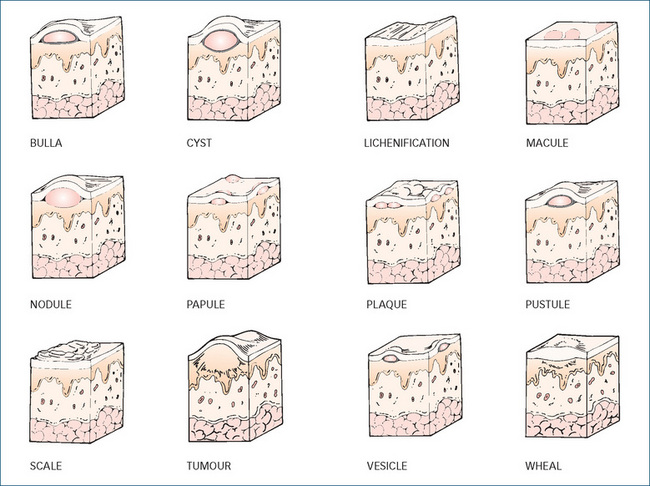
Figure 48-2 Different types of skin lesions and some conditions associated with them. Bulla: large vesicle containing serous fluid (examples: blister; pemphigus vulgaris). Cyst: elevated encapsulated cavity lined by epithelium; filled with liquid or semisolid material (example: sebaceous cyst). Lichenification: rough, thickened epidermis; accentuated skin markings due to rubbing or irritation (example: chronic dermatitis). Macule: flat; non-palpable; discoloured lesion, brown, red, purple or white (examples: freckle; flat mole; rubella; rubeola). Nodule: small collection of tissue, elevated; circumscribed; palpable; 1–2 cm in diameter (examples: erythema nodosum; lipoma). Papule: elevated; palpable; circumscribed; less than 1 cm in diameter (examples: wart; drug-related eruption; pigmented naevus; eczema). Plaque: elevated; flat-topped; solid; rough; superficial papule greater than 1 cm in diameter (examples: psoriasis; eczema). Pustule: visible collection of pus within or beneath epidermis; vesicle filled with purulent fluid (examples: impetigo; acne). Scale: irregular, thin, compacted flaky keratinised cells; dry or oily; varied size; silver, white, or tan (examples: psoriasis; exfoliative dermatitis). Tumour: elevated swelling; may or may not be clearly demarcated or differ in skin colour; growth is uncontrolled (examples: basal cell carcinoma; malignant melanoma). Vesicle: small, elevated, circumscribed, superficial sac filled with serous fluid; (examples: blister; varicella). Wheal, hives: smooth, slightly elevated, irregular-shaped area of oedema; solid, transient, often itchy (examples: urticaria; insect bite).
Source: Beare & Myers 1998; Dorland 2003.
Skin conditions vary over time. Acute conditions tend to show red, burning, blistered or weeping skin (such as from burns); thick ointments cannot be applied to these lesions, which are best treated with lotions that cool by evaporation. Subacute conditions may be oedematous, hot and chapped; creams and gels can be applied. Chronic skin conditions tend to be scaling, lichenified, crusting and dry; moisturising creams and ointments may soften such skin.
Application of drugs to the skin
The general objectives of treatment of skin disorders are to:
Topical administration of drugs
Drugs may be administered to the skin for a topical or local effect, or with the intention that the drug be absorbed and have systemic actions elsewhere in the body. Even drugs that are applied for local actions may be absorbed, and systemic effects and toxicity can occur.
How much to prescribe?
How much of a topical preparation is needed for one dose? This is less easy to estimate than the quantity of tablets or other solid dose forms. Current guidelines suggest that for a cream or ointment to cover an adult’s face and neck would require about 1.25 g for one application, so twice-daily application for 10 days would require a 25–30 g tube of cream. Another way to calculate is to follow the guidelines of the Australian Medicines Handbook, where it is suggested, for example, that for a 3–5-year-old child, twice-a-day application of a topical ointment for 1 week would require 10 g for the face and neck, 15 g for arm and hand, 20 g for leg and foot etc. Some creams are provided in a tube with dose advised by mm or cm of cream squeezed out; other prescribers might recommend ‘enough to cover a 10 cent coin’ or similar suggestion.
Hydration of skin
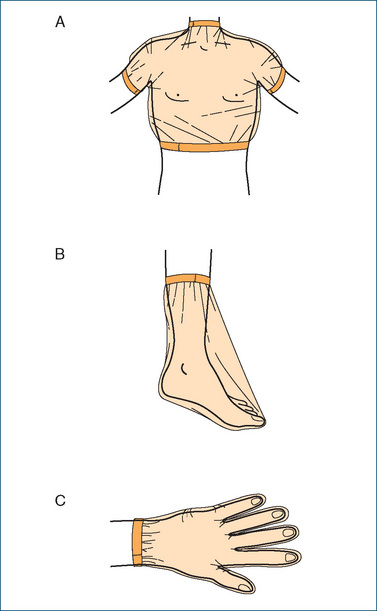
Keratin in the outer skin layer provides a waterproof barrier; to enhance drug absorption the epidermis needs to be hydrated. Some medications are therefore applied then covered with an occlusive dressing (such as plastic wrap, rubber gloves or shower cap; see Figure 48-3 later) or administered in an occlusive type of ointment (e.g. zinc cream or petroleum jelly) because both will trap and prevent water loss (sweat) from the skin, thus increasing epidermis hydration.
Transcutaneous absorption of drugs
Skin layers to be crossed
For transcutaneous absorption (aka percutaneous absorption) of drugs into the bloodstream, the layers of skin cells and membranes through which drugs must pass are:
Nicotine, hyoscine, oestrogens, fentanyl and glyceryl trinitrate are formulated in ointments or patches for transdermal absorption. Chemicals can also be absorbed unintentionally across the skin, with unexpected consequences (see case history in Clinical Interest Box 48-1).
Factors affecting transcutaneous absorption
Absorption through the skin is slow, incomplete and variable (except for lipid-soluble agents). The extent of absorption depends on:
Larger molecules and more water-soluble drugs can have their permeation through the skin enhanced by physical methods such as iontophoresis, ultrasound and skin abrasion.
Formulations and medications for topical application
There are many more types of formulations for topical administration than for any other route (see below). This is the field of pharmaceutics, and detailed methods of formulation are beyond the scope of this text.
Vehicles and emulsions
The drug is dissolved or mixed into a vehicle, i.e. the liquid or solid which carries the drug to the site of application on the skin. Many formulations are emulsions (liquid or semi-solid mixtures of an aqueous phase and an oily phase, with one phase distributed as tiny droplets in the other).1 A lipid-soluble drug such as oestradiol, nicotine or glyceryl trinitrate will distribute into the oily phase of an emulsion, whereas a water-soluble drug (diphen hydramine, lignocaine) will distribute into the aqueous phase. Microemulsions, with nanoparticle-sized droplets, are being formulated to increase markedly the surface area for delivery of the drug to the skin.
Wet or dry preparations
Some topical formulations or vehicles may provide a useful effect without an active ingredient—simply rubbing in or dabbing on may have a warming or drying effect. The old saying in dermatology was ‘If it’s wet, dry it; if it’s dry, wet it’. For dry, scaly skin as found in psoriasis or dry eczema, an ointment with an occlusive emollient (softening) effect is helpful, such as lanolin or zinc cream. An area of acute inflammation that is oozing often needs a soothing evaporative lotion such as aluminium acetate solution or calamine lotion or a powder. If the skin lesion is painful, wet and located on an area rubbed by clothing, then a dusting powder such as talcum or starch may be appropriate to reduce friction and help dry the area. However, it has been shown that lesions heal better with less scarring when kept moist, so the current emphasis is on moist wound healing, e.g. under a medicated dressing (described later under ‘Treatment of pressure sores’).
Multiple ingredients
Pharmaceutical formulations for topical administration may include a wide range of ingredients, such as ointment or cream bases, water, suspending agents, emulsifying agents, preservatives, antioxidants, thickening agents, long-chain fatty acid esters and alcohols, colouring agents and perfumes, as well as the active drug. For example, one commercial ‘lip revitaliser’ contains 38 listed ingredients plus flavours! (It has been said that calamine lotion may make a lot of mess without doing a lot of good. This could be said of many old-fashioned topical preparations, which may remain in the pharmacopoeia without ever having been subjected to controlled clinical trials of safety and efficacy.)
Formulations and agents
Antipruritic agents
Antipruritics (preparations that relieve itching) include dilute solutions containing phenol, menthol, pine tar, potassium permanganate, aluminium subacetate, boric acid or physiological saline solution. Lotions such as calamine or calamine with phenol, cornstarch or oatmeal baths, and hydrocortisone lotion or ointment may also be used. Local anaesthetics such as benzocaine can decrease pruritus, but they readily induce allergic reactions. Antihistamines are poorly absorbed topically, so are less useful than might be expected in relieving allergic and itchy conditions unless administered systemically.
Antiseptics
Antiseptics (or skin disinfectants) are products that reduce the microbial flora on the skin; they are generally broadspectrum but not active against spores. Examples are chlorhexidine, cetrimide, benzoyl peroxide, povidoneiodine and triclosan (see also Appendix 2).
Astringents
Astringents are solutions which, when applied topically, cause precipitation of proteins, vasoconstriction and reduced cell permeability; examples are aluminium acetate or calcium hydroxide solutions, calamine lotion, hama melis (witch hazel), potassium permanganate and the alcohol vehicle in aftershave lotions.
Baths and soaks
Baths and soaks are used to cleanse or medicate the skin or to reduce temperature, usually with soap and water or with oils that have a moistening and soothing effect. Water generally has an antipruritic (anti-itch) effect, as well as cooling and drying by evaporation. Soaps have a detergent and drying action and can be very alkaline.
Cleansers
These are usually free of soap or are modified soap products that are recommended for people with sensitive, dry or irritated skin, or for those who have had a previous reaction to a soap product. Soap-free cleansers are less irritating, may contain an emollient substance and may also have been adjusted to a less alkaline or neutral pH.
‘Cosmeceuticals’
This (dreadful) term, combining ‘cosmetic’ and ‘pharmaceutical’, has been coined to refer to preparations developed with the hope of pharmacological efficacy in reversing the effects of ageing on the skin and restoring a youthful appearance. Preparations containing epidermal growth factors with antioxidants, skin conditioners and ‘matrixbuilding agents’ are sold at great expense, with little evidence of efficacy.
Creams and ointments
Creams and ointments are thick semisolid preparations to be smoothed onto the skin; they may consist of one phase (usually oily, as in ointments) or may be emulsions, i.e. two-phase preparations (creams). Water-in-oil (W/O) creams, such as lanolin, zinc cream and cold cream, feel greasy, are occlusive and help retard water loss through the skin; they effectively deliver lipid-soluble drugs to the skin. Oil-in-water (O/W) preparations, such as aqueous cream and vanishing creams, have cooling and moisturising effects, are good vehicles for water-soluble drugs, but are more easily washed off. Creams and ointments have emollient and protective properties and may be used as the vehicle for active drugs, e.g. eye ointments containing antibiotics or anti-inflammatory agents, and aqueous cream as a base for drug application to the skin.
Emollients
Emollients are fatty or oily substances that are used to soften or soothe irritated skin or as a vehicle for other drugs. Examples of emollients include lanolin, petroleum jelly (Vaseline), soft paraffins, silicones (e.g. dimethicone), oils, vitamin A and D ointments and aqueous cream.
Gels
Gels are viscous, non-oily, water-miscible, semi-solid preparations that contain gelling agents; they have a cooling effect as the solvent evaporates and leave a film on the skin.
Keratolytics
Keratolytics (keratin dissolvers) are drugs that soften skin squames (scales) and loosen the outer horny layer of the skin. Salicylic acid (5%–20%), resorcinol, alpha-hydroxy acids and urea have been the drugs of choice; newer agents used to remove solar keratoses are diclofenac 3% gel, fluorouracil 5% cream or imiquimod 5% cream. Their action makes the penetration of other medicinal substances easier. Keratolytics may be used in treatment of psoriasis, eczema, ichthyosis, warts, corns, acne and dandruff. Salicylic acid is used at concentrations up to 20% in ointments, plasters or collodion; higher concentrations are used to remove warts and corns. In treatment of dandruff, a type of seborrhoeic dermatitis of the scalp, shampoos may contain active ingredients such as coal tar, pyrithione zinc, selenium sulfide, an imidazole antifungal agent and Aloe vera (see Clinical Interest Box 48-2).
Clinical Interest Box 48-2 Sydney university’s aloe vera: ancient plants with modern uses
The University of Sydney’s huge Aloe vera plants, growing along the Parramatta Road boundary, fascinated generations of students and locals. Aloe vera, the Cape aloe, and Aloe barbadensis, the Barbados or Curacao aloe, are members of the lily family. Aloe vera was originally called Aloe ferox (ferocious); it looks like enormous cactuses with thick spiky leaves and can grow to 10–20 m in height, with stems as thick as 3 m in circumference. Aloes currently have become trendy in topical formulations, as natural products.
Aloes (i.e. the reddish-brown, brittle, glassy solid deposit that remains after evaporation of the exudate from cut leaves) have been a valuable commodity since the Greek and Roman empires, when they were traded from Africa along with tortoiseshell, myrrh and other spices. There are records dating back to the 9th century AD of trade from China and Sumatra (Indonesia) via Arabia and Persia to Europe, with aloes, camphor, cloves, cardamom and sandalwood being highly prized. Aloes are also mentioned in the visions of the 12th century mystic, healer and composer Hildegard of Bingen (Germany). In traditional Chinese medicine, the juice is squeezed from the thick, succulent leaves, then boiled and stored; it is used ‘to purge faeces, to clear heat in the liver and to kill worms’.
Aloin, the alcoholic extract of the leaf exudate, contains glycosides called anthraquinones, mono- and polysaccharides, lignans, sterols, salicylic acid and many vitamins and minerals. The extract has an enormously wide range of claimed medicinal properties, including laxative, antimicrobial, anti-inflammatory, immunostimulating and wound healing effects. It has again become very popular and is widely used particularly for treatment of skin conditions such as burns, ulcers, frostbite, psoriasis and dermatitis. Its more traditional uses are for constipation, dyspepsia, GIT ulcers and irritable bowel syndrome. Aloe vera is present in a wide range of commercial topical medicinal and cosmetic preparations such as creams, lotions, skin washes, shampoos and cleansers.
Sources: Braun & Cohen 2007; Bellamy & Pfister 1992.
Keratoplastics
These are agents that stimulate the epidermis and thus cause thickening of the cornified layer; examples are coal tar and sulfur preparations and low concentrations (1%–2%) of salicylic acid.
Liniments and rubs
These are indicated for pain relief for intact skin; pain caused by muscle aches, neuralgia, rheumatism, arthritis and sprains usually responds to these products. Simply massaging an oily substance into the skin causes dilation of skin blood vessels and has a rubefacient (reddening) effect and may assist healing. The ingredients in the preparations may include a counter-irritant (e.g. camphor or oil of cloves), an antiseptic (chloroxylenol, eugenol, thymol), a local anaesthetic (benzocaine) or analgesic (salicylate-containing substances such as methyl salicylate, aka Oil of Wintergreen).
Lotions and solutions
Liquid preparations have soothing and cooling effects due to their evaporation. They may be suspensions of an insoluble powder that is left behind on the skin, such as calamine lotion, or they may be mild acidic or alkaline solutions, such as boric acid solution, limewater or aluminium acetate, used as wet dressings and soaks. Aluminium acetate solution (Burow’s solution) is a mild astringent that coagulates bacterial and serum protein. It is diluted with 10–40 parts water before application.
Calamine lotion contains calamine (a powdered mixture of zinc carbonate and ferric oxide), zinc oxide, bentonite (a suspending agent), phenol and glycerol in a sodium citrate solution. It is a soothing, drying and mildly astringent lotion used for the dermatitis caused by plant secretions, insect bites, sunburn and prickly heat.
Pastes
These are very thick mixtures of solids in cream or oint ment bases. Magnoplasm is a commercial magnesium sulfate and glycerin paste with very high osmotic pressure, used to withdraw fluid from lesions such as boils.
Patches
A transdermal patch is rather like an adhesive dressing that has a reservoir of active drug incorporated in the dressing behind a rate-controlling polymer membrane designed to deliver the drug to the skin at a specified rate (see Figure 23-2). Patches are useful for delivery of potent lipid-soluble drugs, such as glyceryl trinitrate, oestradiol, fentanyl or nicotine. They eliminate many variables affecting oral absorption, including gastric emptying time, stomach acidity, presence of food and the first-pass effect; and obviate the need for frequent oral dosing.
Powders
Powders are mixtures of finely divided drugs in a dry form. Dusting powders based on talcum, zinc oxide or starch are intended for external application. They are useful in body fold areas, where they reduce friction and promote drying, and are used as vehicles for antimicrobial agents, especially antifungals for application to the feet.
Preservatives
These are chemicals added to aqueous formulations to retard oxidation or microbial growth. Common preservatives are hydroxybenzoates, alcohols, chlorocresol and benzalkonium chloride. Preservatives can frequently cause contact dermatitis. Preparations such as ointments and pastes with very little or no water usually do not pose a problem with respect to microbial growth (because of their high osmotic pressure) and hence do not require preservatives.
Protectants
Skin protectants are soothing, cooling preparations that form a film on the skin. They are used to coat minor skin irritations or to protect the person’s skin from chemical irritants. They can also help healing by preventing crusting and trauma.
Examples are Compound Benzoin Tincture (see below) and Collodion, a 5% solution of pyroxylin in a mixture of ether and alcohol; the solvents evaporate to leave a transparent, protective film that adheres to the skin. Non-absorbable powders (including zinc stearate, zinc oxide, certain bismuth preparations, talcum powder and aluminium silicate) are also protectants; however, they adhere to wet surfaces and may have to be scraped off.
Psoralens
Psoralens are plant constituents that have been known for centuries to induce pigmentation in skin, and are used for treatment of vitiligo, a condition in which there is patchy whitening of the skin and hair. They are photosensitising agents that absorb ultraviolet radiation (UVR), so are also used in conjunction with exposure to UVR in treatment of psoriasis. An example is methoxsalen (aka 8-methoxypsoralen), given orally or applied as a lotion or wash, 1–2 hours before exposure to UVR in phototherapy procedures.
Rubefacients
‘Rubefacient’ means ‘making red’—simply rubbing an inert lubricant such as an oil or cream into the skin can cause a mild inflammatory response with vasodilation and warmth and can act as a counter-irritant, distracting the mind from another itch or pain. Many ointments or creams, even with ingredients such as salicylates or antihistamines, have no proven pharmacological efficacy when applied topically, simply acting as rubefacients.
Soaps
Ordinary soap, the sodium salt of palmitic, oleic or stearic acids alone or in a mixture, is made by saponifying fats or oils with alkalis. The consistency of the soap depends on the acid and alkali used. All soaps are relatively alkaline and are potential sources of skin irritation, as are perfumes or antiseptics added to soaps. Soaps are irritating to mucous membranes and can be used in enemas.
Sprays
Sprays are fine mists or aerosols of drug in solution, often with a propellant gas. The vehicle evaporates and deposits the drug on the skin or mucous membrane. Sprays are used especially in the nose for topical administration of decongestants and antihistamines. Nasal sprays can also be utilised to administer drugs for systemic absorption, including hormones such as desmopressin, a posterior pituitary hormone (see Drug Monograph 33-3).
Tars
Extracts of coal tar, wood tar or bitumen are mild irritants to the skin, reduce epidermal thickness, suppress DNA synthesis and have antipruritic and antiseptic properties. Examples are coal tar solution, dithranol and ichthammol. They are used in treatment of dermatoses, including eczema, psoriasis and dandruff. Topically applied tars appear to be safe, whereas ingested or inhaled tars (such as from occupational exposure or cigarette smoking) can be carcinogenic. Tars should be kept away from sensitive areas of skin such as the face, groin, eyes and mucous membranes; some tar solutions stain the skin and clothes.
Tinctures
Tinctures are alcoholic solutions of chemicals or extracts of plant products. When the tincture is applied to the skin, the alcohol evaporates, leaving the ingredient on the skin. Alcohol has an astringent effect and can cause stinging of raw or damaged surfaces.
Compound Tincture of Benzoin (also known as Tinct Benz Co or Friar’s Balsam) is an alcoholic solution of three balsams (i.e. dried exudates from the cut stems of plants) and of aloes. It is administered as a paint or spray for its antiseptic, protective and styptic properties, and as an inhalation for upper respiratory tract infections.
Wet dressings
These liquids include some of the preparations discussed under solutions and lotions and are either a wet or an astringent type of dressing used to treat inflammatory skin conditions, e.g. due to insect bites and plant secretions. Moist dressings impregnated with antiseptics, antibiotics, collagen or honey are used to enhance wound healing.
Zinc oxide
Zinc oxide has long been used in ‘zinc cream’ as a sunscreen; however, it has many more medicinal uses in dermatology, for its astringent, soothing and protective properties in powders, ointments and lotions. Zinc is a required co-factor in healing, and zinc creams and lotions are often effective in treatment of mild inflammatory conditions such as musculoskeletal pains, skin irritations and allergic reactions, and nappy-rash in babies.
Types of drugs affecting the skin
So many dermatological products are available, both OTC and by prescription, that it would be difficult to discuss them all in this chapter. For the sake of simplicity, we discuss only a few selected groups of dermatological products: sunscreens, topical antimicrobials and antiinflammatories, retinoids and other drugs used to treat acne and agents used specifically for burns and pressure ulcers. (The detailed pharmacology of most of these drugs has been discussed in previous chapters, e.g. under hormones, anti-inflammatories and antimicrobial agents.)
Other general dermatological products include the astringents, cleansers, liniments, antiseptics and keratolytics described earlier and products such as antiperspirants, antiseptics, antidandruff shampoos, bath oils and body washes, face washes for acne, freezing sprays for warts, skin lighteners and darkeners, filling agents for wrinkles and lips, medicated toothpastes, insect repellents, hair removers and hair restorers. (Strictly speaking, topical agents acting on mucous membranes could also be included, such as eye-drops and ointments, nasal drops and sprays, mouthwashes and even suppositories and enemas.)
Natural plant extracts and oils with some proven or claimed antiseptic properties include oils of melaleuca (tea-tree), lemon, lemongrass, eucalyptus, clover leaf, thyme, pine, citronella and peppermint flowers, and extract of aloe vera (see Clinical Interest Box 48-2). Honey is also used for its antiseptic properties (and of course for sweetening, see Clinical Interest Box 32-3), and pawpaw as an analgesic and antipruritic. Most of these products are available OTC in pharmacies and supermarkets.
Sunscreen preparations
Skin damage from the sun
Phototoxicity and photoallergy reactions
Phototoxicity
Certain chemicals and drugs (e.g. dyes, suntanning preparations, tetracyclines, oestrogens, sulfonamides, thiazides and phenothiazines), plants, cosmetics and soaps can cause a phototoxic reaction—an excessive response to solar radiation occurring in the presence of a photosensitising agent. Photosensitivity, or phototoxicity, occurs when the inducing agent is present in the skin in sufficient amounts and is exposed to a particular sunlight wavelength. The substance absorbs the radiation and energy is transferred, producing a reactive molecule or free radical, which is destructive to cell membranes or lysosomes. The exposed skin rapidly becomes red, painful, prickling or burning, with peak skin reaction reached within 24–48 hours of exposure. This reaction does not involve the immune system but resembles excessive sunburn.
Photoallergy
A photoallergy reaction is different from a phototoxic reaction; it is less common and requires prior exposure to a photosensitising agent, which is activated to an allergen or hapten by radiation. The immune system is involved and when the photosensitiser reacts with UVR a delayed hypersensitivity reaction occurs, presenting as severe pruritus and a rash that can spread to skin areas that were not exposed to sunlight.
Ultraviolet radiation damage
Extended exposure to the sun, whether from sunbathing or as a normal consequence of an outdoor occupation or lifestyle, can lead to sunburn, premature ageing of the skin (photoageing), immunosuppression and skin disorders including cancers. The damage is caused by solar ultraviolet radiation (UVR), which comprises the part of the spectrum of electromagnetic radiation with wavelengths shorter than those of visible light (at the violet end of the colour spectrum) and longer than those of X-rays.
Effects of UVR
UVR has useful effects in activating sterols to vitamin D compounds and has been used to treat acne and neonatal jaundice (and thus prevent kernicterus and permanent brain damage). UVR can also damage DNA strands by causing thymine bases to link in dimers, and may activate or inactivate viruses. Excessive exposure to UVR can result in skin damage that progresses from minor irritations, blistering, skin darkening (tanning) and thickening, through severe sunburn to a precancerous skin condition and skin cancer later in life. Cutaneous malignant melanoma has been associated with excessive sun exposure, especially during childhood, whereas large cumulative UVR doses over a lifetime appear to increase the incidence of non-melanoma skin cancers (see Clinical Interest Box 48-3). UVR has been shown to cause mutations in the tumour-suppressor gene p53. Actinic (solar) keratoses, lesions that are potential precursors of squamous cell carcinomas, are sometimes treated with topical cytotoxic drugs, the anti-proliferative agent imiquimod (also used against warts) or with diclofenac gel (an NSAID).
Clinical Interest Box 48-3 Sunburn, skin cancer and SPF
Incidence
Skin cancers mainly comprise malignant melanomas and nonmelanocytic cancers (basal [BCC] and squamous cell [SCC] carcinomas). The incidence of skin cancers in Australia is now more than three times the incidence of all other can cers combined. Two out of three people who live their lives in Australia will require treatment for at least one skin cancer, and about 1000 Australians die each year from skin cancer, mainly melanomas. Because of excessive sun exposure and the largely fair-skinned populations, Australia and New Zealand have by far the highest rates of both incidence and mortality of melanoma in the world.
Statistics on the incidence of non-melanocytic cancers are not easy to ascertain, as the cancers are very common and may be treated by general practitioners without numbers being notified to a central cancer registry. BCCs make up around 80% of skin cancers, SCCs 15%, and melanomas about 5%. BCC and SCC are almost twice as common in men as in women, as they are closely related to sun exposure. In the 15–24 age group in Australia, melanomas are the most common cancers. The annual incidence of melanomas in Australia in 2001 was about 55 per 100,000 for males and 37 per 100,000 for females.
Preventive measures
Sun protection is necessary, as sunlight is the major external cause of skin cancer. Childhood exposure to sunlight is important in development of all types of skin cancers, with episodic high exposure causing burning a significant factor in later melanomas. There is a 10–20-year delay between the UVR exposure (especially UVB) and the appearance of skin cancer.
The primary means of protection is avoiding sunburns, especially in childhood and adolescence. If possible, avoid outdoor activities when the sun is strongest (‘from 11 to 3, stay under a tree’), wear protective clothing (broad-brimmed hat and long sleeves) and stay in the shade. A broad-spectrum sunscreen that blocks exposure to UVA and UVB light (sun protection factor [SPF] 15 or 30) should be applied liberally and reapplied every 2 hours and after swimming, vigorous activity and towelling dry. UVR can also affect the eyes, increasing the risk for cataracts and other eye disorders, and it can suppress the immune system. It is recommended that sunglasses that block 99%–100% of UVR be worn, especially by people with light-coloured eyes.
Treatment measures
Choice of treatment is based on assessment of type of tumour, site, size and stage; age and condition of the patient; and facilities and skills of the physician. Surgical excision is most common for all skin cancers and the only treatment for melanomas. Non-melanocytic cancers, if inaccessible by surgery, may be treated with radiotherapy, curettage and cryotherapy. Topical treatment with retinoids, antibiotics, powerful keratolytics and cytotoxic agents is being trialled. Lifelong follow-up is required for all patients who have been treated for a skin cancer, as they are at greater than normal risk of recurrence and of developing another primary tumour. Actinic (solar) keratoses, which can potentially develop into squamous cell carcinomas, are sometimes treated topically with diclofenac 3% gel, fluorouracil or imiquimod 5% cream or methyl aminolevulinate 16% cream plus red light photosensitisation.
Sources: Anti-Cancer Council of Victoria 1999; AIHW 2008; Australian Medicines Handbook 2010.
Most age-associated changes in skin appearance are due to UV-induced effects via mitochondrial damage, protein oxidation, reduction in transforming growth factor and DNA damage. Clinical signs include dryness, irregular darkened pigmentation, deep furrows, leathery appearance and reduced elasticity of skin and amount of collagen.
UVR spectrum
UVA, or long-wave radiation, has wavelengths in the range 400–320 nm and is the closest to visible light; it can pass through glass and penetrate into the dermis. It produces darkening of preformed melanin in the basal layer of the epidermis, results in a light suntan and contributes to skin cancer via immunosuppression. UVA is responsible for many photosensitivity reactions. (This is the wavelength used in commercial solariums.)
UVB has wavelengths of 320–290 nm. It causes erythema, sunburn and photoageing and is associated with vitamin D3 synthesis. UVB is responsible for skin cancer induction, and the carcinogenic properties of UVB appear to be augmented by UVA. Around 90% of UVB has in the past been blocked by the Earth’s ozone layer, hence the worldwide concern that ‘holes’ in the ozone layer (caused mainly by environmental pollutants and ‘greenhouse gases’ such as chlorofluorocarbons) will allow passage of greater proportions of solar UVB and increase the incidence of skin cancers.
Most of the UVC from the sun (wavelength 290–200 nm) does not reach the earth’s surface. Exposure to this type of radiation is usually from artificial sources such as mercury lamps and arc-welding. UVC can cause some erythema but will not stimulate tanning; it is very damaging to the retina.
In this context, ‘broad spectrum’ refers to sunscreens that block both UVA and UVB. Very little UVR is blocked by cloud cover, although infrared radiation that contributes to the sensation of heat is usually reduced, which can give a person a false sense of security against sunburn. The sun’s rays can be reflected onto skin from water, concrete, snow and sand, but are deflected by the Earth’s atmosphere and by sweat; hence sunburn is worse at high altitudes and in dry desert conditions.
Sunscreens
Absorbers or reflectors
Sunscreen preparations are applied to absorb and/or to reflect UVR, in order to reduce the risks of photo-ageing, sunburn and skin cancers. It should be noted that sunscreens may be more effective at preventing sunburn than preventing skin cancers.
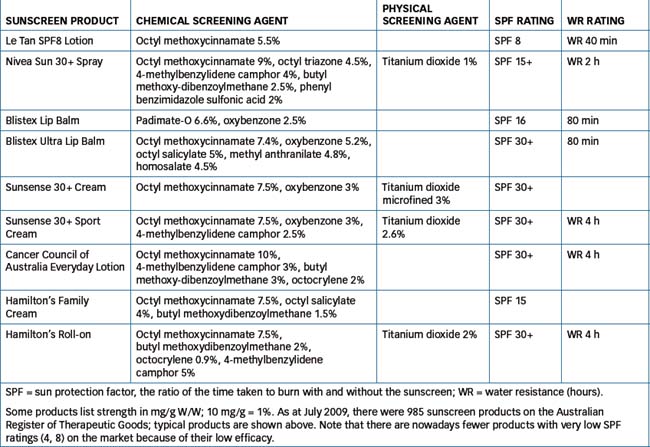
Absorbing chemicals absorb and block at least 85% of the UVB. Absorbing agents are chemicals such as p-aminobenzoic acid (PABA) derivatives, benzophenones (which absorb both UVA and UVB), cinnamates, some salicylates, camphors and anthranilates (see Table 48-2).
Physical or opaque sun blocks contain agents that reflect and scatter UVB and UVA but do not absorb it. Reflectors include chemicals such as titanium dioxide and zinc oxide. These agents are opaque (e.g. zinc creams, which look like thick white paste) and must be applied heavily to physically block out the UVR, thus they are not cosmetically acceptable to most people.
Nanoparticle sunscreens
Both types of agents are now also being prepared as nano-sized particles in sunscreens; these ‘micronised’ products are less opaquely white, but their long-term safety has yet to be established. At present, it appears that insoluble nanoparticles, such as titanium and zinc oxides, do not penetrate human skin and so are non-toxic (see Clinical Interest Box 42-4, and reviews by Nohynek et al [2008], Baron et al., 2008Baron et al [2008] and Lautenschlager et al [2007]). Consequently, the Australian Therapeutic Goods Administration (TGA) does not require that warnings about nanoparticles be placed on labels of such products. The TGA will continue to monitor the scientific literature with respect to safety concerns about nanoparticle products.
Sun protection factors
The sun protection factor (SPF) is a value given to a sunscreen preparation to indicate its effectiveness. It is largely determined by the sunscreening agents (whether chemical or physical) present in the preparation. The SPF for a product is the ratio between the exposures to UVB required to cause erythema (reddening) with and without the sunscreen. This is expressed as the MED, or the minimal erythemal dose: if a person experiences 1 MED with 25 units of UVR (in an unprotected state) and if after application of a sunscreen the person requires 250 units of radiation to produce the same amount of reddening, then this product will be given an SPF rating of 10. The higher the SPF, the longer it takes to burn or develop a tan. However, ‘SPF numbers should not be translated into burn times for individuals’ (Dermatology Expert Group 2009).
The SPF scale is a logarithmic scale rather than an arithmetic one, thus a sunscreen with SPF 2 gives a 50% reduction in UVB passage (50% penetration), SPF 4 gives 75% reduction (25% penetration) etc. Hence it can be calculated that SPF 16 (i.e. 15+) reduces UVB passage by about 94% of UVB, whereas a screen with SPF 32 (30+) reduces it by 97%. Thus, although they sound much more effective, there is little useful difference between preparations with very high SPF values. A more important consideration is the water-resistance time of the product, because this period may be much shorter than the ‘SPFallowed’ time.
Choice of SPF
The best way to choose a sunscreen is according to skin type, the length of time spent in the sun, whether water resistance is important, the usual intensity of the sun’s rays in the geographic area and the type of preparation or formulation preferred. People who tan gradually and don’t burn easily may use an SPF 15+ preparation, while those who burn easily and tan only minimally need a 30+ formulation. An SPF 30+ sunscreen is recommended for use by all fair-skinned people in tropical areas.
Water resistance of sunscreens
The efficacy of a sunscreen agent depends on its ability to remain effective during vigorous exercise, sweating and swimming. Two categories established are ‘water-resistant’ and ‘very water-resistant’ (waterproof). Water-resistant products maintain sun protection for at least 40 minutes in water; very water-resistant products maintain sun protection for at least 80 minutes in water. Water resistance is largely dependent on the vehicle used in the product, in particular how water-soluble it is; thus oil-based lotions and creams are likely to remain on the skin longer while swimming than are O/W creams or lotions.
Application of sunscreens
Sunscreens should be liberally applied to all exposed body areas (except eyelids) and reapplied frequently to achieve the maximum effectiveness. It has been recommended that sun block be applied 30 minutes before exposure to allow adequate skin penetration, and reapplied every 2 hours depending on factors such as the product used (the SPF and water resistance category), activity and sweating levels, time of day, cloud cover and reflections. It is recommended that individuals stay out of the sun when the UVR is at the highest intensity, usually between 11 am and 3 pm, when two-thirds of the daily solar radiation occurs.
Logically, it can be seen that reapplication does not ‘allow’ another number of hours of sun—if a person has already had enough UVR to reach the MED, then any further exposure will cause more erythema, i.e. burning. Because the amount of sunscreen applied is often only one-third to half of what is necessary, the theoretical SPF is rarely achieved, which explains why people get sunburnt despite applying sunscreen. Generally, Australians do not use enough sunscreen—a family of four on a beach holiday should use a bottle of sunscreen every couple of days, but many families make a bottle last a year! Sunscreens are dated products and may lose efficacy if kept after their use-by date.
Infants should be kept out of the sun; children older than 6 months should always wear protective clothing, hats and sunscreens, with SPF 15 to SPF 30. It has been projected that consistent use of SPF 15 products from 6 months through to 18 years of age will result in about 80% reduction in the risk of skin cancer over a person’s lifetime.
Sunscreens and low vitamin D
There has been an increasing incidence of vitamin D deficiency in Australia in the last few years, causing rickets or osteomalacia (see Chapter 37). This has been explained partly by immigration of dark-skinned people who may wear long covering clothing and veils (preventing sun activation of vitamin D in the skin) and partly by increasing protection of skin from the sun by use of shade, hats and sunscreens. The prevalence is also high in institutionalised elderly people. The Dermatology Expert Group (2009) suggests that ‘fair-skinned Australians should be able to maintain adequate vitamin D concentrations with 10 minutes of sun exposure to the face, arms and hands on most days of the week during summer, and for 2–3 hours per week over winter ... Patients who receive little sunlight should be investigated for vitamin D deficiency and when present, supplemental vitamin D should be offered’.
Topical antimicrobial agents
General principles of antimicrobial chemotherapy of skin infections
Antimicrobial agents used on the skin or to treat skin infections include antibacterial, antiviral, antifungal and antiparasitic agents. There is an increasing problem worldwide with organisms developing resistance to antimicrobials, hence concerted efforts are being made to rationalise the prescribing of broad-spectrum antibiotics and use drugs specific to organisms that are sensitive to them.
Antimicrobials used topically are preferably not the same as those used systemically, both to minimise the risk of development of resistance and to utilise drugs that may be toxic systemically but not topically. Whenever possible, skin or nail infections are treated with topical antimicrobials; however, in some severe infections, e.g. fungal nail infections or acne resistant to topical treatment, systemic chemotherapy may be required with antimicrobial agents administered orally.
All the antimicrobial drug groups (except those used to treat parasitic infestations) have been covered in detail in earlier chapters (44–46), so only summaries will be given here.
Antiseptics
Many topical preparations are available OTC, labelled as first-aid products to help prevent infection in minor cuts, burns or injuries. These generally contain simple antiseptic or disinfectant-type products and are effective for first-aid treatment but not for specific bacterial infections. Antiseptics (skin disinfectants) are solutions or creams of antimicrobial agents applied topically to the skin; they usually contain chemicals that are very effective but too toxic to be administered internally. Many have simple detergent, solubilising actions. Examples include benza lkonium chloride, triclosan, chlorhexidine, cetrimide, povidone–iodine and hypochlorite solutions (see Appendix 2). Plant products such as aloes, benzoin and oils of melaleuca, lemon, clove, thyme and lemongrass have mild antiseptic properties.
Antibacterial agents
The most frequent organisms causing skin infections are the common body flora bacteria Streptococcus pyogenes and Staphylococcus aureus, causing folliculitis, impetigo, furuncles (boils), carbuncles (multi-headed boils of several adjacent hair follicles) and cellulitis. To treat these common skin disorders, topical antibacterials including bacitracin, neomycin, sodium fusidate, polymyxin B, silver sulfadiazine, framycetin, gramicidin, mupirocin and metronidazole may be applied. Clindamycin and erythromycin are used in acne and silver sulfadiazine in burns (see later sections). Antimicrobial agents are sometimes formulated in combination with a corticosteroid, for treatment of inflammatory conditions in which there is a major component of infection as well.
Common adverse effects
Sensitisation to many topical antibiotics can occur. Prolonged use can produce superinfection as an overgrowth of non-susceptible organisms such as fungi. Photosensitivity is reported with topical gentamicin. Chloramphenicol used topically can cause systemic adverse effects, including bone marrow hypoplasia and blood dyscrasias, as well as local effects such as itching, burning, urticaria and vesicular and maculopapular dermatitis. Topical fusidic acid is likely to induce resistance.
Antibiotics only used topically
Neomycin
Neomycin is a broad-spectrum aminoglycoside antibiotic, indicated for topical application in infections such as impetigo (‘school sores’) and boils. It is also used in an anti-acne lotion and in preparations for application to eye or ear infections. Overgrowth of resistant organisms can occur with prolonged use.
Applied topically, neomycin occasionally irritates the skin, and allergic contact dermatitis has been reported. For conditions where percutaneous absorption of neomycin can occur (including burns and trophic ulceration), there is the potential for nephrotoxicity, ototoxicity and neomycin hypersensitivity reactions. Use in pregnancy can lead to ototoxicity and renal toxicity in the fetus (Pregnancy Safety Category D).
An ointment that combines neomycin, bacitracin and polymyxin B (‘triple antibiotic’) may be more efficacious in mixed infections (e.g. in the ear) than when these agents are used singly; see Drug Monograph 32-1.
Mupirocin
Mupirocin is a topical antibiotic obtained from Pseudomonas species; it inhibits RNA and protein synthesis and is active mainly against Gram-positive aerobes. It is used in treatment of impetigo caused by S. aureus and beta-haemolytic streptococci and in eradicating the nasal carrier status for S. aureus. It is usually applied to affected areas three times daily.
Antiviral agents
Aciclovir and idoxuridine
Aciclovir and idoxuridine are used for treatment of cutaneous herpes simplex infections of the lips (‘cold sores’) or genital areas. Aciclovir is activated in herpesinfected cells to a metabolite that inhibits viral DNA polymerase, thus inhibiting further viral replication. Topical aciclovir is used for the treatment of herpes simplex (non-life-threatening) in immunocompromised patients; however, systemic aciclovir is much more effective. Another guanine analogue, penciclovir, is also formulated in a lip cream for labial herpes simplex.
Idoxuridine is an antimetabolite with a mechanism of action similar to those of the antitumour antimetabolites: its structure is very similar to that of the nucleic acid base thymidine, and it inhibits the incorporation of thymidine into viral DNA and hence blocks viral replication, analogous to the antimetabolites used in cancer chemotherapy (see Figure 42-1). It is available combined with lignocaine in a cream for use in herpes simplex infections (e.g. ‘cold sores’ on the lips).
Adverse reactions from topical application of aciclovir or idoxuridine include hypersensitivity reactions, pruritus and stinging. The dosage is enough for adequate covering of the lesions with ointment, from as early as possible in the infection, every 4 hours daily for 5 days.
Treatment of warts
Although warts are caused by a virus (human papillo mavirus, HPV), they are not treated with specific antiviral drugs. Warts usually resolve without treatment, as they are overcome by the body’s immune defences. In immunocompromised patients, however, they can become extensive. Anogenital warts are predominantly transmitted in young people by sexual intercourse. The condition can undergo malignant transformation, and in women there is a strong association with cervical cancer; there is now an effective vaccine against HPV.
Treatment for warts depends largely on the site involved and extent of spread. Topical application of keratolytics, such as salicylic acid and trichloroacetic acid, and topical antimicrobials, including podophyllotoxin and glutaraldehyde, have been used. Non-pharmacological treatments include curettage, electrosurgery and cryotherapy with liquid nitrogen or solid carbon dioxide.
A new drug, imiquimod, is used for treating external genital and perianal warts; it acts via agonist activity at toll-like receptor-7 to enhance the body’s immune response. (It has also been approved for use by topical application in treatment of solar keratoses and some non-melanocytic skin cancers such as superficial basal cell carcinomas when surgical removal is not appropriate.) For anogenital warts a 5% cream is applied topically at night 3 nights per week for a maximum of 16 weeks; severe inflammatory responses are possible.
Antifungal agents
Fungal skin infections
Three pathogenic fungi (dermatophytes) that can cause superficial fungal infections (dermatophytoses) without systemic infection are Microsporum, Trichophyton and Epidermophyton; there can also be mixed infections. Systemic mycoses usually occur only in severely immunocompromised patients.
Dermatophytes exist in moist, warm environments, such as skin areas covered by shoes and socks (tinea pedis, or athlete’s foot), or in the groin, scalp or trunk. The fungi invade the stratum corneum and cause inflammation and induce sensitivity when they penetrate the epidermis and dermis.
Because the stratum corneum is shed daily, spread of the fungi occurs by contact, commonly around swimming pools or in bathrooms. General hygiene measures such as wearing sandals in communal change-rooms and showers and drying skin well, especially between the toes, help reduce infection. Before starting treatment, skin or nail scrapings should be taken for microscopic identification of the causative organism. Treatment may be required for many months, and relapse after cessation is common.
Foot infections are particularly dangerous in people with diabetes, and fungal infections can lead to bacterial infections, gangrene and amputations (see Chapter 36). Onychomycosis (fungal infection of toenails) is a significant predictor of foot ulcers, so early intervention and good foot care are critical.
Antifungals
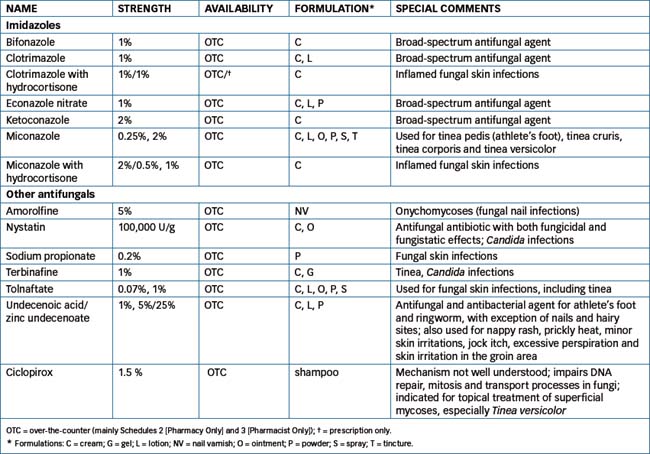
The primary topical antifungal agents include the imidazole group (clotrimazole, ketoconazole, bifonazole, miconazole etc), terbinafine and amorolfine, and miscellaneous antifungal agents, including undecylenic, benzoic, salicylic and propionic acid products, tolnaftate, the antibiotics nystatin and griseofulvin, povidone–iodine, a new antifungal ciclopirox and a variety of antifungal combination creams, ointments, powders, sprays, liquids and paints (see Chapter 45).
Fungal infections of the nails (onychomycoses) are particularly resistant to treatment by usual topical or oral formulations, so a medicated nail varnish has been developed (Drug Monograph 48-1). See Table 48-3 for the generic names, availability status (OTC or prescription) and comments on topical antifungal products. Adverse reactions with the use of the topical antifungals are generally mild and include local irritation, pruritus, erythema and stinging.
Drug Monograph 48-1 Amorolfine nail lacquer
Amorolfine is one of a pair of antifungal agents (the other is terbinafine) that have selective fungistatic and fungicidal actions against a broad spectrum of yeasts, dermatophytes and other fungi and moulds. They impair sterol synthesis in fungal cell membranes and are active both orally and topically. Amorolfine is the only antifungal agent that is sufficiently well absorbed through fingernails and toenails to be effective topically in treating fungal nail infections (onychomycoses); however, it is expensive and may have limited efficacy.
Indications
Amorolfine nail varnish is indicated for topical treatment of onychomycoses; it alleviates or cures 70%–80% of cases.
Pharmacokinetics
Amorolfine is very lipophilic but is virtually insoluble in intestinal fluids. After application to the nail, it permeates and diffuses through the nail plate and can reach measurable levels in the blood.
Adverse reactions
Because fungal sterols are different from those in mammalian cells, there are few adverse effects. Occasionally a slight burning sensation is felt after application; allergic reactions are rare.
Drug interactions
There are no known drug interactions; however, patients are advised not to use any other nail preparations (polishes, artificial nails) during treatment. If the fungal infection is too severe to be treated by amorolfine nail varnish as monotherapy, PO antifungals such as griseofulvin may be required concurrently.
Warnings and contraindications
Amorolfine is contraindicated if a previous hypersensitivity to it has occurred. Users are warned not to apply the varnish to the skin beside the nails. There is little information on the use of this product in pregnant or lactating women or in children, so its use in these people is not recommended.
Dosage and administration
Amorolfine is supplied as a 5% solution in a 5 mL nail lacquer base; also included in the kit are cleaning pads, nail files and spatulas to be used in applying the varnish. The varnish is applied 1–2 times weekly after first cleaning the nail and filing it down (including the nail surface) to remove as much as possible of the infected nail. Before the next application, the nail is cleaned to remove the remaining varnish and filed down again. Because nail infections are so difficult to eradicate, the process needs to be continued for about 6 months for fingernails and longer for toenails.
Ectoparasiticidal drugs
Ectoparasites are insects that live on the outer surface of the body; ectoparasiticides are drugs used against those parasites; they are referred to as pediculicides (against lice) and scabicides or acaricides (against mites), reflecting the type of parasite treated.
Treatment of pediculosis (lice infestation)
Pediculosis is a parasite infestation of lice on the skin of a human. Lice are transmitted from one person to the next by close contact with infested people, clothing, combs and towels. There are three types of infestations: (1) pediculosis pubis, caused by Phthirus pubis (pubic or crab louse); (2) pediculosis corporis, caused by Pediculus humanus corporis (body louse); and (3) pediculosis capitis, caused by Pediculus humanus capitis (head louse). In pediculosis corporis, except in heavily infested individuals, the parasite is often absent from the body but inhabits seams of clothing in the axillae, beltline or collar.
Common findings in a person who is infested include pruritus (itching), nits (eggs of lice) on hair shafts, lice on skin or clothes and, occasionally with pubic lice, blue macules on the inner thighs or lower abdomen. The drugs of choice are the pediculicides permethrin and maldison (malathion) in lotions or shampoos; local public health officers or school nurses usually recommend the optimal current treatment regimen, including use of medicated shampoo and combing of hair with a fine-tooth comb to remove nits. Affected family members may also require treatment, and hairbrushes, hats, clothing, bedding etc require cleaning.
Pediculicides
Permethrin acts on the nerve cell membranes of lice, ticks, mites and fleas. It disrupts the sodium channel depolarisation, thus paralysing the parasites. It has a high cure rate (up to 99%) in treating head lice after only a single application. The most common adverse reactions include pruritus, mild burning on application and transient erythema. Related compounds are the allethrins and the natural pyrethrins found in chrysanthemum flowers.
Maldison (also known as malathion) is an organophosphate cholinesterase inhibitor available for treating head lice and nits; it is relatively non-toxic to humans. This product is usually effective in lice-infested individuals within 24 hours and is well tolerated. Malathion lotion is rubbed into the scalp and left to air-dry. Because the drug is flammable, the individual must be warned to avoid open flames and smoking and not to use a hairdryer. The hair should be shampooed 8–12 hours after application; dead lice and nits are combed out.
Benzyl benzoate is an older type of pediculicide, also effective as an acaricide against mites. It is sometimes used as an insect repellent, and clothes or mosquito nets can be soaked in a solution and dried; the repellent effect outlasts some washings. Permethrin is used in a similar manner to impregnate clothing and nets with repellent.
Treatment of scabies (mite infestation)
Scabies is a parasitic infestation caused by the itch mite Sarcoptes scabiei. It is an obligate parasite of humans and is transmitted by close contact with an infested individual. It bores into the horny layers of the skin in cracks and folds (almost exclusively at night), causing irritation and pruritus. The infestation in adults is usually generalised over the body, especially in web spaces between fingers, wrists, elbows and buttocks.
The acaricide of choice is permethrin cream or lotion, two applications 1 week apart. This is considered more effective than crotamiton or benzyl benzoate. Family members and close contacts should also be treated, and items such as bedding, clothes and soft toys should be sprayed.
Anti-inflammatory and immunomodulating agents
As many conditions manifested in the skin involve inflammatory or autoimmune pathological processes, drugs that modify these responses are widely used in derm atology to target mediators such as cytokines, receptors and inflammatory cells. Most commonly used topically are the corticosteroids; other immunosuppressants include drugs such as cyclosporin and methotrexate, and newer ‘immunobiological agents’ such as pimecrolimus, infliximab and etanercept (see Chapter 47). For optimal efficacy the drugs should penetrate into the deeper layers of the skin, but not be absorbed into the systemic circulation (to avoid systemic adverse effects) (see review by Pariser [2009]). In severe cases of inflammatory or autoimmune dermatological conditions, the drugs may need to be administered systemically.
Corticosteroids
Actions and uses
Topical corticosteroids are generally indicated for direct relief of inflammatory and pruritic dermatoses, with fewer systemic effects than from oral or parenteral administration; these drugs are discussed in greater detail in Chapters 35 and 47 (see Drug Monograph 35-1). They are used topically for their anti-inflammatory, antipruritic, vasoconstrictor and immunosuppressant actions in various types of dermatitis (eczema) and psoriasis, and in skin reactions to insect bites and sunburn. Topical corticosteroids may also stabilise epidermal lysosomes in the skin, and fluorinated steroids have antiproliferative (antimitotic) actions.
Adverse drug reactions
Adverse reactions for topical corticosteroids include skin atrophy and striae, acneiform eruptions, burning sensations, dryness, itching, hypopigmentation, purpura and haemorrhage, hirsutism (usually facial), folliculitis, alopecia (usually of scalp) and masking or aggravation of fungal infections. Contact dermatitis can be precipitated as an allergic reaction to topical corticosteroids, which may be difficult to distinguish from the inflammatory condition for which the drug is being applied.
If a significant amount of the corticosteroid is absorbed, systemic adverse effects can occur, with suppression of the hypothalamic–pituitary–adrenal axis and the classical cushingoid effects of moon face, fluid retention, skin striae, weak skin and bones, hypertension, immunosuppression, overgrowth of microorganisms leading to secondary infections, glaucoma and poor wound healing.
Potencies
Fluorinated corticosteroids are particularly recommended for topical application to thickened skin because of their potency, lipid solubility (hence topical efficacy) and low tendency to cause sodium retention. In decreasing order of potency, some topical corticosteroids are: betamethasone dipropionatef> betamethasone valeratef, mometasone, triamcinolonef> clobetasonef, flumethasonef, methylprednisolone > desonidef, hydrocortisone. (Those marked f are fluorinated compounds; potencies can vary depending on ester form and strength of formulation.)
Acute inflammatory eruptions usually respond to the medium- and low-potency steroids, whereas chronic hyperkeratotic lesions require potent or highly potent drugs.
Formulations
Corticosteroids are available in a wide range of topical formulations that are stable, easy to apply and rapid-acting, causing no pain, discolouration or odour on application. Inhalation of corticosteroids (see Drug Monograph 28-4) in treatment and prevention of asthma is a specialised topical application, in this case to the mucous membranes and thence to the smooth muscle of the airways.
Types of formulations for topical application of corticosteroids include creams, ointments, lotions, sprays, gels and scalp lotions, at various strengths. Combination preparations with antifungal or antibacterial antibiotics are also available for use in inflammatory dermatitis with a large component of infection.
The vehicle (aerosol, cream, gel, lotion, ointment, solution or tape) in which the corticosteroid is placed can alter the therapeutic efficacy. Corticosteroid penetration of the skin is enhanced by (in decreasing order of effectiveness) ointments, gels, creams and lotions. As a result of their occlusive nature, ointments hydrate the stratum corneum, enhancing steroid penetration. Lotions, sprays and gels are well suited to hairy areas or for lesions that are oozing and wet. Creams and ointments are suited to dry, scaling, thickened and pruritic areas.
The rate of transcutaneous penetration after application also influences therapeutic efficacy. It is limited by three factors: the rate of dissolution of the drug in the vehicle, the rate of passive diffusion of the drug across membranes and the drug penetration rate through the stratum corneum. Inflamed or moist skin absorbs topical steroids to a greater degree than thick or lichenified skin. Occlusive dressings (e.g. using an occlusive ointment base or wrapping in plastic cling-wrap, see Figure 48-3) increase the hydration of the skin and penetration of the drug up to 100-fold, hence systemic adverse effects are possible.
Dosage and administration
For most topical formulations, the adult dosage is one or two applications daily as directed. Application frequency depends on the site, response of the cutaneous eruption to medication and application technique.
In some conditions resistant to milder treatment, intralesional injection of corticosteroids is used. Triamcinolone is most often used, injected for example into the lesions of keloid scars, acne cysts or alopecia areata.
Newer immunomodulators
Calcineurin inhibitors
Pimecrolimus is a new calcineurin inhibitor related to tacrolimus and sirolimus, which are used mainly to prevent transplant rejection, and temsirolimus, an mTOR inhibitor used as an anti-angiogenesis agent in renal cell cancer therapy. These agents block T-cell activation and thus prevent release of inflammatory mediators. Pimecrolimus is indicated for short-term or intermittent use in treatment of psoriasis and eczema, applied twice daily as a cream. It can be used safely in children over 3 months, which is a benefit in childhood dermatoses. Main adverse reactions are local stinging and erythema and secondary infections.
TNF-alpha antagonists
Tumour necrosis factor-alpha (TNF-α) is an important regulator of inflammation, and antagonists of its activity are some of the newer anti-inflammatory agents proving effective in treatment of psoriasis. Etanercept is a TNF-α receptor fusion protein, while adalimumab, infliximab and golimumab are monoclonal antibodies against TNF. They are given by injection, and reactions at the infusion or injection site are common. Serious adverse effects include opportunistic infections and reactivation of infections (especially tuberculosis). There may also be increased risk of multiple sclerosis and of malignancies.
Uses in eczema, psoriasis and urticaria
Eczema
Eczema, also known as dermatitis, is an inflammatory condition with genetic predisposition in which skin becomes red, itchy, scaly, moist and blistered. Emollient moisturisers are indicated to maintain skin hydration, tar preparations (coal tar, ichthammol) are used for their antipruritic effects and topical corticosteroids for antiinflammatory effects. The potent new immunosuppressant pimecrolimus is second-line therapy. Antibiotics may be required for infected patches of skin, and antihistamines, sedatives or analgesics for relief from itching. UVR therapy and avoidance of triggering factors such as soaps, perfumes and preservatives are also useful. Strategies with no proven benefit include homoeopathy, Chinese herbs, dietary restrictions, massage therapy, reduction of house dust and salt baths.
Atopic dermatitis is common in young children, with prevalence of 10%–20% in those under 10 years; itching and infections are likely. Prevention is best, with education of parents and avoidance of triggers and irritants such as harsh, perfumed or coloured bath additives. Topical corticosteroids are used short-term for flare-ups, and calcineurin inhibitors (e.g. pimecrolimus cream) can be administered to children over 2 years old with severe disease.
Psoriasis
Psoriasis is a common skin disease (with 2%–3% prevalence worldwide) characterised by abnormal immune response, epidermal proliferation and pink–red thickened patches of skin covered with silvery scales, with pain, itching and bleeding. Large areas of skin may be involved, with the elbows, knees, buttocks and scalp most frequently affected. There are various forms, mostly of the plaque variety; the abnormally thick lesions are packed with activated T cells causing chronic inflammation and impairing skin functions. There is a strong association with arthritis, liver disease, cardiovascular diseases and metabolic syndrome. Peak onset is in early adult years. The cause is unknown, although there appears to be an immunological involvement, and trigger factors include stress, injury, smoking, alcohol, infections and drugs such as some angiotensin-converting enzyme inhibitors, β-blockers, non-steroidal anti-inflammatory drugs (NSAIDs), quinine derivatives and lithium.
Drugs used in treatment include those administered for eczema (see above), plus the psoralens, vitamin D analogues (calcipotriol, calcitriol, which act as antiproliferative agents in the keratinocytes, see Chapter 37) and a retinoid (acitretin). In severe cases, systemic administration of the immunosuppressants cyclosporin and methotrexate (in considerably lower dose than that used in anticancer chemotherapy) may be required, with phototherapy. The new immunomodulators are also tried, especially the anti-TNF agents etanercept, infliximab and adalimumab and the new anti-interleukin antibody, ustekinumab. Adverse effects include infections, malignancies and induction of autoimmune conditions. Interestingly, some TNF inhibitors when used to treat autoimmune diseases such as rheumatoid arthritis and Crohn’s disease have actually induced psoriasis, a condition which they can be used to treat—this anomaly is being studied further. Tazarotene cream, a retinoid used in acne for its actions modifying cell proliferation and differentiation, is also indicated for use in plaque psoriasis.
Psoriasis can occur in children; it is estimated that about 27% of cases occur before the age of 16 years. Topical treatment is usually with corticosteroids or calcipotriol; more potent drugs such as methotrexate, acitretin and cyclosporin have more risks in children due to their greater potential toxicities.
Urticaria
Urticaria, or hives, is a common skin condition in which there is transient itchiness, reddening and swelling of the dermis or subcutaneous tissue; angio-oedema may be associated. In about 20% of cases, some precipitating factor may be identifiable, e.g. heat, cold, sun exposure, emotion, drugs or infection. Although a skin condition, urticaria is treated not with topical agents but with systemic antihistamines, corticosteroids, NSAIDs, tricyclic antidepressants or various other drugs. Acute severe angiooedema is a medical emergency, as airways can become obstructed, and requires treatment with parenteral adrenaline, hydrocortisone, antihistamine and fluids, together with airways support and oxygen.
Retinoids and treatment of acne
Pathology
Acne vulgaris is a skin disease that involves increased sebum production, abnormal keratinisation leading to the formation of a keratin plug at the base of the pilosebaceous follicle, proliferation of the bacterium Propionibacterium acnes and inflammation. It affects up to 90% of adolescents and is associated with high androgen levels. Mild acne involves skin comedones (‘blackheads’), papules and pustules, and severe acne involves extension of pustules to abscesses, cysts and widespread scarring. There may be significant psychological and emotional trauma associated with the disfigurement caused.
At the molecular level, it has been proposed that increased fibroblast growth factor receptor-2 (FGFR-2) signalling is involved in the pathogenesis of acne, and that many anti-acne agents act by downregulation of FGFR-2 signalling. Other aetiological factors implicated in women are androgens, oestrogens, growth hormone and insulinlike growth factor. Acne in women can be associated with polycystic ovary syndrome.
There is no clinical evidence of links between diet and acne, although some people note increased skin oiliness and acne flare-ups after eating particular foods, such as chocolate or high-fat dairy products. Excessive skin washing can in fact exacerbate acne by causing skin irritation, as can some oily cosmetics and exposure to industrial oils. Some drugs can produce or exacerbate acne, particularly androgenic hormones (in anabolic steroids), danazol, androgen-derived oral contraceptives, oral corticosteroids, phenytoin, isoniazid, iodides and lithium.
Treatment of acne
The reduction and removal of sebum and bacteria are the targets of acne therapy, along with improvement of the complexion, reduction in scarring and psychosocial benefits. Treatment of acne may include (1) removal of keratin plugs, (2) treatment and prevention of infection by P. acnes and (3) decreasing sebum production. There is no ‘quick fix’ for acne, which in many sufferers is a chronic disease, and most treatments need to be continued for many months for significant benefits to be achieved, and even years to prevent relapses.
Retinoids (vitamin A analogues)
Vitamin A, or retinol, is a carotenoid substance formed from β-carotene pigments in fruit and vegetables, and also present in some fish oils and animal foods. It is a fat-soluble vitamin required for normal growth, bone and teeth formation, retinal function, skin and membrane functions and reproduction. Vitamin A has long been known to be involved in skin physiology, as it has roles in shedding and repair of epithelial tissues, stability of membranes and maintenance of normal growth (see Clinical Interest Box 48-4).
Clinical Interest Box 48-4 Vitamin a, acne and antarctica
The recommended daily intake of vitamin A in adults is about 0.75 mg/day, with higher amounts needed by lactating women. Deficiency of vitamin A occurs during malnutrition, in food faddists and people on diets deficient in fats, and in people with disorders of fat absorption and storage. Signs of deficiency include night blindness, corneal opacity and damaged epithelium, with skin becoming dry and infected.
Overdosage and toxicity can occur, particularly in children and elderly people being given herbal remedies laced with vitamin A or taking ‘mega-doses’ of vitamin supplements. Chronic overdose causes irritability, itchiness, hypertrophy of bone, increased incidence of metaplasia and neoplasia and cardiotoxicity, whereas acute toxicity causes vomiting, peeling of skin and raised intracranial pressure; deaths have occurred. High doses of retinoids are mutagenic and teratogenic and are contraindicated in pregnancy (Category X).
During the Australian Antarctic expeditions of 1911–1914, Sir Douglas Mawson and his companion, Xavier Mertz, suffered from severe malnutrition after their sledge and supplies (and a third member of the team) were lost down a crevasse. Mawson and Mertz were forced to eat the meat from their husky dogs that had died. They became very ill, with layers of skin peeling off, severe diarrhoea, convulsions and headaches; Mertz succumbed but Mawson survived after months of illness. It is thought that they suffered from vitamin A toxicity from eating the livers and fat of the dogs, which had been fed fish and seal meat that had accumulated vitamin A from plankton in seawater. At the top of the food chain, the men received toxic overdoses of retinoids. Eskimos and Arctic explorers in the northern hemisphere knew from folklore that eating the livers of polar bears or seals was taboo; 100 g has been shown to contain toxic doses of vitamin A.
Retinoids have found important new medical uses in acne and psoriasis, and in cancer. Given orally or topically, retinoids act as keratolytics, enhance discharge and drainage of acne pustules and reduce epithelial proliferation in psoriasis. Retinoids have been shown to have effective anticancer actions in some leukaemias and renal cancers, and are being studied to determine the mechanism of their antineoplastic action, thought to be via inhibition of telomerase enzymes.
Tretinoin emollient cream has been released in the USA to treat facial wrinkles and photo-ageing caused by the sun. This product contains 0.05% tretinoin and is the first prescription drug with this indication.
Information on Mawson’s expedition from: Howell & Ford 1985.
Retinoids (analogues of vitamin A) are now drugs of choice in treatment of acne because of their actions modifying cell proliferation, differentiation and apoptosis. There are various vitamin A look-alikes available, for oral or topical administration in acne, psoriasis, hyperpigmentation and keratinisation disorders. Two examples are tretinoin, which is all-trans retinoic acid (RA), and isotretinoin, which is the 13-cis-RA form. Another analogue, acitretin, may also be prescribed by specialists as prophylactic therapy against skin cancers in transplant patients treated with immunosuppressant agents.
Mechanism of action
The mechanism of action of retinoids is a field of active research, as retinoids are now known to be involved in a wide range of cellular functions, including in tissue repair and in regulation of growth in cancers. There are two main types of receptors for retinoids in cell nuclei: RA receptors and retinoid X receptors. Activation of RA receptors mediates steps in many biochemical pathways, including liberation of proteolytic enzymes, breakdown of cartilage, synthesis of mucopoly saccharides and steroids, morphogenesis, differentiation and proliferation of epithelial tissues, induction of neural growth factors, regulation of the immune system and development of the kidneys.
In acne, retinoids facilitate the extrusion of fatty material from existing comedones and prevent the reblocking of plugs and formation of new lesions, and have antiinflammatory actions.
Topical retinoids
Topical retinoids are used for treating mild acne vulgaris; examples of topical preparations are isotretinoin gel 0.05%, tretinoin gel and cream 0.05% (Drug Monograph 48-2), adapalene cream and gel 0.1% and tazarotene 0.05%, 0.1% cream. Gels are preferred for oily skins, and creams for those with dry skin. A useful combination product is a gel containing 0.1% adapalene and 2.5% benzoylperoxide. These medications are contraindicated in pregnancy because of the possibility of birth defects if absorbed. In severe cases of acne, retinoids may be prescribed for oral administration, with or without an oral antibiotic.
Drug Monograph 48-2 Tretinoin acne cream
Tretinoin, aka all-trans retinoic acid, is the active metabolite of vitamin A. It is an irritant that stimulates epidermal cell turnover, causing skin peeling; this reduces the free fatty acids and horny cell adherence within the comedone. It also causes changes in cellular differentiation and reduces keratinisation.
Indications
Tretinoin cream is used in the treatment of acne vulgaris in which comedones, pustules and papules predominate.
Pharmacokinetics
Topical application of the tretinoin cream to normal skin does not lead to significant absorption of tretinoin. Repeated application over a prolonged period to inflamed skin may cause some transcutaneous absorption.
Adverse reactions
Adverse reactions of topical tretinoin are all reversible. They include skin irritation with red and oedematous blisters; crusted, stinging or peeling skin; temporary alterations in skin pigmentation; and increased sensitivity to sunlight.
Drug interactions
Concomitant topical use with drying or peeling agents such as benzoyl peroxide, resorcinol, salicylic acid, sulfur, strong soaps and astringents can result in excessive keratolytic and peeling effects. There are additive adverse effects if used with oral retinoids or with other photosensitising agents, so these combinations should be avoided.
Warnings and contraindications
Use of tretinoin cream is contraindicated in eczematous skin or if there have been previous hypersensitivity reactions. Because of the risk of birth defects, it rates Pregnancy Safety Classification D. In women of childbearing age, a negative pregnancy test must be confirmed in the 2 weeks before starting treatment. Patients using the cream should be warned about the risk of excessive sunburning effects and advised to use a sunscreen and protective clothing. Contact of the cream with mucous membranes and skin around the eyes and mouth should be avoided.
Dosage and administration
The cream is available in strength 0.05%; an amount of 0.5 g is estimated to contain the equivalent of 250 mcg vitamin A. The cream is applied to the affected areas before retiring at night, then washed off in the morning to reduce sun sensitivity. A slight exacerbation of the condition may occur at first, but improvement should be noted within 2–3 weeks. Treatment is prolonged for several months to achieve remission of acne.
Tretinoin is also available as 0.025% and 0.1% creams and a 0.01% gel; and as 10 mg capsules (Pregnancy Safety Category X) for treating promyelocytic leukaemia.
Oral retinoids
For treatment of severe cystic acne resistant to milder therapies, systemic drugs may be required. Isotretinoin 10-mg or 20-mg and acitretin 10-, 20- or 40-mg oral capsules are available. These products inhibit sebaceous gland activity and thus decrease sebum formation and secretion, and have keratolytic and anti-inflammatory effects. They are reserved to treat severe acne and have induced prolonged remissions in severe cystic acne.
Women who are pregnant or are planning to become pregnant should not use these preparations. Many spontaneous abortions have been reported, as well as major abnormalities (hydrocephalus, microcephalus and external ear and cardiovascular problems) in the fetus at birth in women who have taken retinoids during pregnancy. Because of this risk, prescription of oral retinoids is restricted to specialist dermatologists and authorised physicians. Sexually-active women of child-bearing age who are prescribed these drugs must use efficient contraceptive methods for 1 month before starting the treatment, continuously during treatment, and for 1 month (isotretinoin) or 2 years (acitretin) after cessation of treatment. The latter requirement is due to the long halflives of acitretin (>2 days) and its active metabolite etretinate (>3 months). The use of oral retinoids with topical retinoids is not recommended because additive toxicity may result.
Other adverse reactions are as described in Clinical Interest Box 48-4 for overdose and toxicity of vitamin A. In addition, there are isolated reports of acquired hearing loss after oral isotretinoin.
Other acne products
Keratolytics and antiseptics
In mild acne, topical keratolytics and antibacterials are the treatments of first choice. Creams and lotions containing salicylic acid, benzoyl peroxide or azelaic acid are recommended, to unblock pores by removing keratin plugs. Benzoyl peroxide slowly and continuously liberates active oxygen, producing an antibacterial, keratolytic and drying effect. The release of oxygen into the pilosebaceous and comedone area creates unfavourable growth conditions for P. acnes and reduces the release of the fatty acids from sebum. The drying vehicle also aids in shrinking the papules or pustules. There is no problem of development of resistance by the bacteria.
Azelaic acid, a straight-chain 9-carbon dicarboxylic acid, is a relatively new topical agent useful in acne. It has anti bacterial activity against P. acnes and reduces keratinisation. It has also been tried in hyperpigmentary skin disorders and in malignant melanoma. As an acid, it can cause skin irritation (burning, stinging or pruritus) if it is applied on broken skin.
Other measures include avoidance of oil- or alcoholbased cleansers or harsh soaps, and avoidance of vigorous scrubbing of the skin, as these tend to increase oiliness of the skin. Older medications include formulations with sulfur, bentonite, silica, zinc, lactic acid, urea and resorcinol as keratolytics and mild antimicrobial agents, and antiseptic washes including cetrimide, chlorhexidine, lactoferrin, alpha-hydroxy-acids or triclosan. Treatment ‘kits’ combining a keratolytic and an antiseptic cleanser can help improve compliance with therapy.
Antibiotics
The exact mechanism of action of topical and systemic antibiotics used in the treatment of acne is unknown, as acne is not mainly an infection nor is it contagious, but P. acnes appears to convert comedones to inflamed pustules or papules. Antibiotics may decrease the colonisation of P. acnes, thus decreasing the formation of sebaceous fatty acid byproducts and preventing the formation of new acne lesions. The antibiotics used include clindamycin, erythromycin and minocycline or doxycycline. Topical erythromycin and clindamycin gels are most commonly prescribed for mild to moderate acne, whereas oral antibiotics (tetracyclines) are generally reserved for individuals with severe acne, and for those who are intolerant or whose acne did not respond to topical agents. Antibiotic resistance can lead to treatment failures.
Hormones
Because acne is sometimes associated with excess androgen production, women with acne can be treated with antiandrogen agents, which reduce sebum secretion. Drugs with antiandrogenic activity include cyproterone acetate, spironolactone and flutamide (see Chapter 39) and oestrogens, usually prescribed in a combined oral contraceptive pill (Chapter 40). It is important that the preparation not contain an oestrogen with significant androgenic activity.
Treatment of burns
Pathophysiology of burns
Burn injuries range from mild and superficial to very severe with extensive skin loss associated with systemic and metabolic complications. Burns can be caused by heat, chemical agents (strong acids or bases) or electricity. Burns cause lesions of the skin accompanied by pain; however, the chief cause of death after burning is shock, which must be anticipated in any effective plan of treatment.
At first, capillary permeability is altered in the injured area: permeability is increased, resulting in a loss of plasma and weeping of the surface tissues. If the burn is extensive, considerable amounts of plasma fluid can be lost in a relatively short time. This depletes the blood volume and causes decreased cardiac output and diminished blood flow. Unless the situation is rapidly brought under control, irreversible shock can result from rapidly developing tissue anoxia, with damage extending to tissues remote from those suffering the initial injury. One of the aims of the treatment of burns is therefore to stop the loss of plasma and to replenish that which is lost as quickly as possible.
Extent and depth of burns
The proportion of body surface area affected is estimated by the ‘rule of nines’ for adults (see Figure 48-4A). If large areas of skin are burnt, there is great danger of infection to the patient; it is estimated that about 75% of people suffering 30% burns or more are likely to die of infection and its consequences.
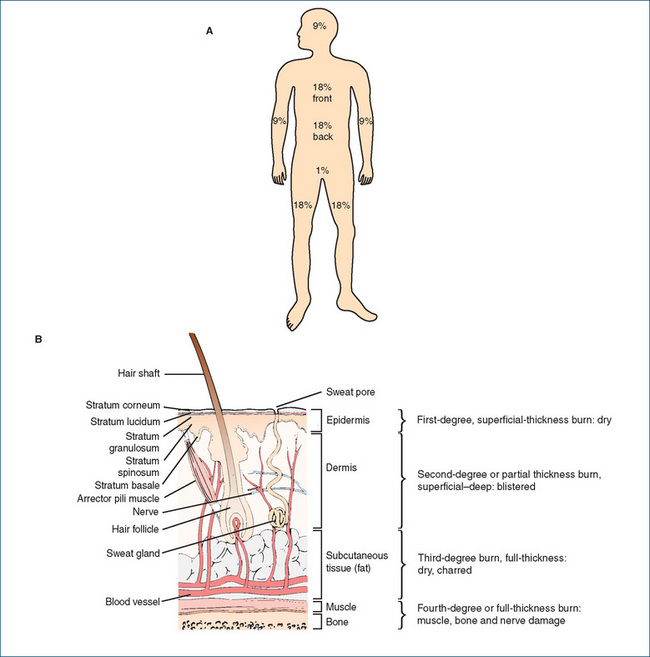
Figure 48-4 Extent of body burns: percentage and thickness. A The ‘rule of nines’ in describing percentage of adult body burned: the head (front and back) and the arms each count as 9%, the front and back of the trunk each count as 18%, each leg as 18%, and the groin area as the remaining 1% of body surface area. B Diagram of layers of skin and subcutaneous tissue, showing definition of burn depth. Thus second-degree burns are those in which the superficial or deep layers of the dermis are damaged, causing blistering.
Burns are classified by degree, which is determined by the depth of skin involved within a local area (see Figure 48-4B). First-degree or superficial-thickness burns involve only the epidermis, causing erythema with characteristic dry, painful reddening and inflammation (e.g. overexposure to sun or flash burn). Second-degree or partial-thickness burns involve the epidermis extending into the dermis and may be superficial or involve deep dermal necrosis. Epithelial regeneration may extend from the deep skin appendages, such as hair follicles and sebaceous glands, which penetrate the dermis. This burn is characterised by a moist, blistered, very painful surface (e.g. flash or scald burns from non-viscous liquids). Third-degree or fullthickness burns involve destruction of the entire epidermis and dermis and adnexal structures, and are characterised by white, opaque, dry, leathery skin or coagulated, charred skin without sensation as a result of the destruction of nerve endings (e.g. flame burns or hot viscous liquids). Fourth-degree burns extend into subcutaneous fat, muscle or bone, appear black and dry and cause scarring.
Partial- or full-thickness burns must be thought of as open wounds with the accompanying danger of infection. Normal body flora organisms including Staphylococcus, Candida and Pseudomonas become pathogenic. If the tissue becomes anoxic and necrotic, anaerobic organisms such as Clostridium tetani and C. perfringens can grow. Mixed infections with multiple organisms occur frequently. The immune system can become suppressed because of injury and shock, with resulting poor defence mechanisms. Infection must be prevented or treated.
The severity of electrical burns depends on the current received, the condition of the skin (e.g. cuts, abrasions and moisture, which lower resistance) and duration of contact, which can be affected by flexor muscles contracting and inhibiting release from the power source. Electrical burns result in necrosis of more tissue than thermal burns. Chemical burns occur after contact with strong acid or alkali; the initial treatment is water irrigation of the affected area followed by neutralisation.
Management of burns
First-aid treatment of burns
An important first-aid treatment for minor and major burns regardless of cause (chemical, electrical or thermal) is to cool the wound immediately to remove irritants, decrease inflammation and constrict blood vessels; this reduces the permeability of the blood vessels and reduces oedema formation. Recommended first aid is to flush the burned area and hot clothing with cool running water (10–15̊C) for 20–30 minutes. The more quickly the wound is cooled, the less tissue damage there is likely to be and the less subsequent morbidity and need for surgery. No greasy ointments, butter or dressings should be applied, because these agents inhibit loss of heat from the burn, which increases both discomfort and tissue damage. After prolonged cool washing, the burn can be covered with cling wrap or sterile sheet until the person can be transported for medical attention. Major burns need referral to a burns unit (see Clinical Interest Box 48-5).
Clinical Interest Box 48-5 Spray-on skin, a great western australian invention
Dr Fiona Wood, Clinical Professor in the School of Paediatrics and Child Health at the University of Western Australia, and plastic surgeon and Head of Royal Perth Hospital’s Burns Unit, came to prominence when a large proportion of the survivors of the 2002 Bali bombings arrived at Royal Perth Hospital. Professor Wood led a courageous and committed team to save 28 patients suffering severe burns (from 2% to 92% of body surface area), life-threatening infections and delayed shock.
In her research, Dr Wood had discovered that scarring after burns is markedly reduced if replacement skin can be provided within 10 days; however, previous techniques of skin culturing took 21 days to produce enough cells. With her colleague Dr Marie Stoner, Dr Wood extended the technique from growing sheets of skin cells to culturing a suspension of cells that could be sprayed onto the damaged area, after only 5 days. Pressure bandaging is also important for protection and to reduce hypertrophy of subsequent scars.
Her vision in having developed a plan to cope with large-scale disasters 5 years before the first Bali tragedy, and her exceptional leadership, research and surgical skills, led to Dr Wood’s being honoured as Australian of the Year for 2005.
Source: http://www.australianoftheyear.org.au/; Silla et al 2006.
Drugs used in management of burns patients
Burned patients treated in an emergency room or burns unit are stabilised with intravenous fluids, given analgesics for pain and sedated if necessary; they may require immunisation against tetanus. Catheterisation may be necessary to measure urinary output, depending on the patient’s status. After stabilisation, the burn wound is cleaned with a mild soap and water, and a sterile, non-adherent dressing is applied to the wound.
Burned patients have a sustained increase in release of stress hormones, including corticosteroids and catecholamines, leading to a prolonged hypermetabolic state with greatly increased metabolic rate and increased requirements for energy, carbohydrates, proteins, fats, vitamins, minerals and antioxidants. Depending on the state of the patient, these may have to be supplied by parenteral nutrition. Beta-blockers have been used to help reduce the catabolic effects of burn injury and reverse protein breakdown.
Small, uncontaminated burns that can be adequately dressed do not require topical or oral antimicrobials. Silver sulfadiazine is usually preferred because of its broad-spectrum activity and because it is easy to apply to the burned site (see Drug Monograph 48-3). There is some concern about potential toxicity of silver to various host (patient) cells. New formulations with nanocrystalline silver particles are proving to have stronger antimicrobial activity with reduced frequency of dressing changes.
Drug Monograph 48-3 Silver sulfadiazine
Silver sulfadiazine is the antimicrobial agent of choice in treatment and prevention of infection in burns, leg ulcers and pressure sores: it has broad antimicrobial activity against many Gram-negative and Gram-positive bacteria, and some yeasts and anaerobic bacteria. It combines the antibacterial actions of silver nitrate with those of sulfonamides. It has bacteriostatic actions through actions on cell membranes and cell walls, as well as inhibition of enzymes involved in folic acid synthesis. Silver sulfadiazine is formulated 1% in an O/W cream, combined with the broad-spectrum antiseptic chlorhexidine at 0.2%.
Indications
Silver sulfadiazine is used for prophylaxis and treatment of infections associated with second- and thirddegree burns, leg ulcers, pressure sores and other chronic wounds with extensive denuded areas of skin. It softens eschar, facilitating its removal and preparation of the wound for grafting.
Pharmacokinetics
Silver sulfadiazine in contact with exudates is slowly metabolised. When applied to extensive areas of the body, significant amounts of the drug may be absorbed, reaching therapeutic plasma concentrations and producing adverse reactions characteristic of both the sulfonamides and of silver. Renal function in these patients should be monitored, and adequate hydration supplied.
Adverse reactions
Pain, burning and itching occur infrequently after application of the silver sulfadiazine cream. Hypersensitivity to sulfonamides can occur; if so, the drug should be discontinued. Resistance can develop.
Drug interactions
The cream should not be used concurrently with anionic surfactants (as chlorhexidine is cationic) or with enzymatic debriding agents, which may be inactivated by silver.
Warnings and contraindications
Caution should be observed with extensive use in patients with renal or liver impairment. The cream (initially white) darkens on exposure to light. Sulfonamides can cause kernicterus in babies if used extensively by pregnant women, so silver sulfadiazine is in Pregnancy Category C. It retards re-epithelialisation, so should be discontinued once the wound starts healing.
Dosage and administration
Silver sulfadiazine is available as a 1% cream to be applied topically to cleansed, debrided burn wounds once or twice daily until healing is adequate. It should be applied with a spatula or gloved hand to a thickness of about 2–3 mm. Burn wounds should be continuously covered with the cream. Daily bathing and debriding are important and a dressing may or may not be used.
Povidone–iodine has been used in some centres, and it also penetrates eschar (the dead, separated, damaged skin). Povidone–iodine causes pain on application, however, and hardens the eschar area when dry. An ancient remedy that is regaining popularity is honey: in some studies of treatments for superficial or partial-thickness burns, honey covered by sterile gauze showed favourable results in terms of rate of healing compared with silver sulfadiazineimpregnated gauze (Clinical Interest Box 32-3). Other pharmacological management includes adequate pain relief, especially during dressing changes, and relief of severe itching in rehabilitating patients.
Treatment of pressure sores and leg ulcers
Pressure sores
Pathophysiology
The pressure sore (bedsore or decubitus ulcer) is a break in the skin and underlying subcutaneous and muscle tissue caused by abnormal, sustained pressure or friction exerted over the bony prominences of the body by the object on which the body part rests. It results in vascular insufficiency and ischaemic necrosis, and most frequently affects debilitated, immunosuppressed, comatose, immobilised or paralysed patients. The prevalence of pressure ulcers ranges from about 9% in acute care facilities to 33% in critical care patients and those with spinal injuries, and up to 23% in nursing homes. In addition to the suffering of patients, the total cost to the health-care system of treating such wounds is enormous.
Local and systemic causes include local circulatory impairment, oedema or hypertension; trauma, pressure and shearing force on the lower body if the head of the bed is raised more than 30̊; loss of sensation of pressure or pain; debilitation, muscle atrophy and motor paralysis; reduction in the amount of adipose tissue between skin and underlying bone; dehydration, poor nutrition with inadequate intake of vitamins (especially vitamin C) and minerals (such as copper and zinc); obesity, infection and septicaemia; and heat and moisture (maceration), e.g. from incontinence.
Pressure sores are classified into four stages or grades (Figure 48-5):
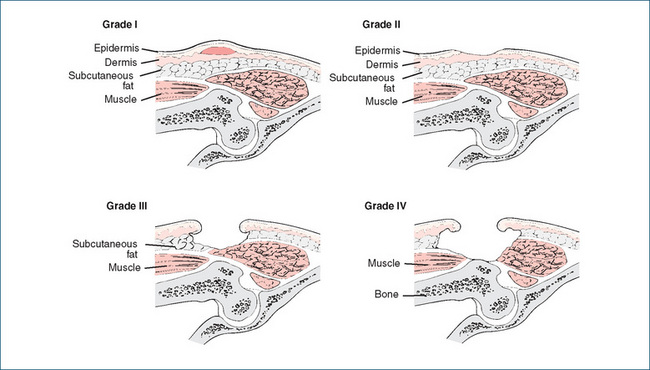
Figure 48-5 The four grades of pressure sore (decubitus ulcer or bedsore). In grade IV, the underlying muscle and bone are affected, with the consequent risk of osteomyelitis.
The bacterial flora of pressure sores are both Gramnegative and Gram-positive organisms, which include Staphylococcus aureus, Streptococcus groups A and D, Escherichia coli, Clostridium tetani and Bacteroides, Proteus, Pseudomonas, Klebsiella and Citrobacter organisms. Chronic ulcers may be complicated by increased risk of extension to bone, causing osteomyelitis, and of development of squamous cell carcinomas.
Physical management
Pressure sores, like leg ulcers, are notoriously difficult to treat, and if possible should be prevented by watchful nursing care with frequent turning of bedridden patients and ambulation whenever possible. If ulcers do develop, maximum activity is even more essential to relieve pressure, optimise the muscle pump and venous return and stimulate circulation. Wound management has become a specialised area of nursing and podiatry, with many techniques and dressings available (see Heyneman et al [2008]; Dermatology Expert Group [2009]).
A treatment plan for pressure sores should take into consideration four basic principles:
A person with a full-thickness loss of skin may require surgical intervention either to debride and cover the ulcer area or to stabilise the wound. Physical therapies that have been tried include electrical stimulation, infrared and UV radiation, laser therapy and ultrasound.
Pharmacological management
Systemic antibiotics are not usually indicated, as adequate drug levels are not reached in granulating wounds, but may be needed in difficult-to-treat infected pressure sores; for sepsis, osteomyelitis, bacteraemia and advancing cellulitis; and as an adjunct to surgical management. Metronidazole is an antibacterial agent used systemically to treat grade III and IV decubitus ulcers infected with anaerobic bacteria. (A topical metronidazole gel is used to treat acne rosacea in adults.)
Topical cleaning of pressure sores
Saline solutions are safe and effective for cleaning most pressure sores. Less mild antiseptics such as povidone–iodine, other iodophors, potassium permanganate and hydrogen peroxide are usually contraindicated because they are reported to be cytotoxic to fibroblasts and thus interfere with the granulation process. Antimicrobials similar to those used in burns (silver sulfadiazine) and bacterial skin infections (mupirocin) may be required.
An ancient therapeutic technique gaining renewed interest is that referred to euphemistically as ‘biosurgery’: the use of living maggots (larvae of insects) as debriding agents. Applied to the wound (e.g. in an upturned plastic container), the larvae clean wounds by gently removing necrotic devitalised tissue, thus decreasing the risk of infection and improving healing. This technique is gaining acceptance around the world and is considered safe, efficacious and simple.
Medicated dressings
Sterile, non-stick dressings are applied to the ulcer or wound to keep it moist, as moist wounds heal more effectively and faster than dry wounds. Antiseptic dressings include those impregnated with chlorhexidine, povidone–
iodine, silver, collagen, collagenase, honey or triclosan; there is also a dressing impregnated with the antibiotic framycetin. Finely powdered sterile gelatin is available for dusting into wounds, where it stimulates the growth of granulation tissue and healing of ulcers; the gelatin protein is gradually resorbed naturally. Packs of sterile calcium alginate fibres are used in bleeding or exuding wounds to act as haemostatics by releasing calcium, filling wounds and aiding coagulation. Unless pain or exudation occurs, dressings can be left on the wound for days or weeks, as constant removal of dressings delays healing. Bioengineered tissue substitutes such as epidermal cells or artificial fibres can help protect wounds and encourage healing.
Debriding agents
Debridement means the cleaning of wounds and removal of eschar, or slough, which may be retarding healing and providing a medium for bacterial infection. Before the application of debriding agents, the wound should be thoroughly but gently cleansed to flush away necrotic debris and exudates, with a solution that does not inactivate enzymes (preferably normal saline or sterile distilled water). All previously applied topical preparations should be removed before the new agent is applied. Slough may need to be removed surgically.
Dextranomers are hydrophilic beads placed in the wound to absorb exudate, bacteria and other matter. The preparation is used for cleansing a wet or secreting wound (not dry wounds) and the action continues until all the beads are saturated. The assumption of a greyish-yellow colour by the beads indicates that they are saturated and ready for removal. Therapy with dextranomer is continued until healthy granulation is evident. Patients who have diabetes mellitus or immunosuppression need to be closely monitored as they are more susceptible to the development of severe infections.
Active enzymes can also be used as debriding agents: ointments containing collagenase or papain (a protease enzyme preparation) are effective in removing necrotic material from pressure ulcers, leg ulcers and partial thickness wounds.
Leg ulcers
Skin ulcers on the legs (and on the feet, particularly in diabetes patients) cause many of the same problems as do burns and pressure sores: pain, chronic inflammation, risk of infection and prolonged requirement for nursing care and dressing changes. Similar treatment methods have been tried, but management is not simple. Physical methods include compression bandages or stockings, bioengineered skin substitutes and/or surgical recon struction, ablation or ligation of incompetent veins (see reviews by O’Meara et al [2008]; Coleridge-Smith [2009]). Any method that effectively promotes wound healing may be advantageous in reducing the development of necrosis and gangrene, and subsequent requirement for amputation.
Pharmacological treatments
Dressings similar to those used in pressure sores may be used, such as those impregnated with antiseptics (iodine, povidone–iodine, peroxides, ethacridine, levamisole, prop ylene glycol) or with adsorbents (alginates, carmellose, cadexomers, foam, hydrocolloids) or other medicaments (zinc oxide, glycerol).
Key points
 The skin, combined with its exocrine glands, hair and nails, forms the integumentary system; skin consists of two main layers (the epidermis and dermis) plus the subcutaneous tissue.
The skin, combined with its exocrine glands, hair and nails, forms the integumentary system; skin consists of two main layers (the epidermis and dermis) plus the subcutaneous tissue. The main function of the skin is defence: it serves as a barrier to the external environment. It also contains sensory nerve endings, synthesises vitamin D and helps in body temperature regulation.
The main function of the skin is defence: it serves as a barrier to the external environment. It also contains sensory nerve endings, synthesises vitamin D and helps in body temperature regulation. The skin serves as the site for topical drug application for the treatment of a variety of dermatological problems and can be used as the site of administration of lipid-soluble drugs intended for transcutaneous absorption and systemic actions.
The skin serves as the site for topical drug application for the treatment of a variety of dermatological problems and can be used as the site of administration of lipid-soluble drugs intended for transcutaneous absorption and systemic actions. Penetration of topical drugs into the skin, and absorption through the skin, are affected by the age, condition, hydration and site of skin; the metabolism and skin circulation; the lipid-solubility of the drug and the vehicle in which the drug is formulated.
Penetration of topical drugs into the skin, and absorption through the skin, are affected by the age, condition, hydration and site of skin; the metabolism and skin circulation; the lipid-solubility of the drug and the vehicle in which the drug is formulated. A wide variety of pathological conditions affect the skin; most are due to infection, excessive inflammatory or immune responses or reactions to sun exposure. Examples are fungal and viral infections, acne vulgaris, eczema and dermatitis, psoriasis, urticaria, sunburn and skin cancers.
A wide variety of pathological conditions affect the skin; most are due to infection, excessive inflammatory or immune responses or reactions to sun exposure. Examples are fungal and viral infections, acne vulgaris, eczema and dermatitis, psoriasis, urticaria, sunburn and skin cancers. Drugs, given either topically or systemically, can cause adverse reactions in the skin such as urticaria, purpura, fixed eruptions, dermatitis or eczema and photosensitisation.
Drugs, given either topically or systemically, can cause adverse reactions in the skin such as urticaria, purpura, fixed eruptions, dermatitis or eczema and photosensitisation. There are numerous formulations available as vehicles for administration of drugs to the skin; such preparations include creams and ointments, lotions and solutions, skin protectants and emollients, wet dressings and soaks, rubs and liniments, pastes, patches, powders and sprays. Many are available over the counter, contain several ingredients and may have little clinically proven efficacy.
There are numerous formulations available as vehicles for administration of drugs to the skin; such preparations include creams and ointments, lotions and solutions, skin protectants and emollients, wet dressings and soaks, rubs and liniments, pastes, patches, powders and sprays. Many are available over the counter, contain several ingredients and may have little clinically proven efficacy. Therapeutic agents applied topically for actions on or in the skin include sunscreens, antimicrobials (antibiotics, antivirals, antifungals and ectoparasiticidal drugs), corticosteroids and other immunosuppressants, keratolytics, acne products, burn products, antipruritics and wound dressings and treatments for skin ulcers and pressure sores.
Therapeutic agents applied topically for actions on or in the skin include sunscreens, antimicrobials (antibiotics, antivirals, antifungals and ectoparasiticidal drugs), corticosteroids and other immunosuppressants, keratolytics, acne products, burn products, antipruritics and wound dressings and treatments for skin ulcers and pressure sores. Exposure to the sun, in particular to ultraviolet radiation in the UVA and B wavelength ranges, causes major harm to the skin, ranging from sensitisation, allergies, ageing, reddening and burning through to benign and malignant skin cancers.
Exposure to the sun, in particular to ultraviolet radiation in the UVA and B wavelength ranges, causes major harm to the skin, ranging from sensitisation, allergies, ageing, reddening and burning through to benign and malignant skin cancers. Chemicals used in sunscreens may act by either absorbing particular UVR (e.g. aminobenzoates and benzophenones) or reflecting UVR (zinc and titanium oxides). Sunscreens are given SPF numbers, indicating their protective capacities; people who burn easily should use a product with SPF15+ or 30+.
Chemicals used in sunscreens may act by either absorbing particular UVR (e.g. aminobenzoates and benzophenones) or reflecting UVR (zinc and titanium oxides). Sunscreens are given SPF numbers, indicating their protective capacities; people who burn easily should use a product with SPF15+ or 30+. Antimicrobials used topically for skin infections should be those that are not administered systemically; antibacterial antibiotics frequently prescribed for topical use include neomycin and mupirocin. For herpes simplex viral infections, aciclovir and idoxuridine are available topically.
Antimicrobials used topically for skin infections should be those that are not administered systemically; antibacterial antibiotics frequently prescribed for topical use include neomycin and mupirocin. For herpes simplex viral infections, aciclovir and idoxuridine are available topically. Fungal skin infections, particularly of moist areas of skin or of finger- and toenails, can be difficult to eradicate. Many topical preparations of antifungals are available; examples are the imidazoles and terbinafine and amorolfine. Severe infections may require systemic antifungal therapy.
Fungal skin infections, particularly of moist areas of skin or of finger- and toenails, can be difficult to eradicate. Many topical preparations of antifungals are available; examples are the imidazoles and terbinafine and amorolfine. Severe infections may require systemic antifungal therapy. Skin infections with insects (lice and mites) cause severe itching; permethrin or maldison can be applied as a shampoo, lotion or cream.
Skin infections with insects (lice and mites) cause severe itching; permethrin or maldison can be applied as a shampoo, lotion or cream. Because many dermatological conditions such as dermatitis and urticaria have an inflammatory or immune component, the corticosteroids are commonly used topically for their anti-inflammatory and immunosuppressant effects, in ointments, creams and lotions. Fluorinated steroids such as betamethasone are particularly effective. Hydration of skin, e.g. by use of occlusive dressings or ointments, markedly enhances absorption of corticosteroids, which improves actions but increases the risk of systemic adverse effects.
Because many dermatological conditions such as dermatitis and urticaria have an inflammatory or immune component, the corticosteroids are commonly used topically for their anti-inflammatory and immunosuppressant effects, in ointments, creams and lotions. Fluorinated steroids such as betamethasone are particularly effective. Hydration of skin, e.g. by use of occlusive dressings or ointments, markedly enhances absorption of corticosteroids, which improves actions but increases the risk of systemic adverse effects. New immunomodulators such as calcineurin inhibitors and TNF antagonists are being used in eczema and psoriasis. Psoriasis may require treatment with potent immunosuppressants, including the cytotoxic agents cyclosporin and methotrexate.
New immunomodulators such as calcineurin inhibitors and TNF antagonists are being used in eczema and psoriasis. Psoriasis may require treatment with potent immunosuppressants, including the cytotoxic agents cyclosporin and methotrexate. Acne vulgaris may be alleviated by topical treatment with skin cleansers, keratolytics and antibiotics, or topical retinoids such as isotretinoin. Severe cases of acne may require systemic hormones or oral retinoids, which carry the risk of teratogenesis and must not be prescribed in women of childbearing age without adequate contraception being assured.
Acne vulgaris may be alleviated by topical treatment with skin cleansers, keratolytics and antibiotics, or topical retinoids such as isotretinoin. Severe cases of acne may require systemic hormones or oral retinoids, which carry the risk of teratogenesis and must not be prescribed in women of childbearing age without adequate contraception being assured. When large areas of skin are burned, there is severe risk of infection, shock and hypermetabolic syndrome. Fluid replacement is critical, and topical silver sulfadiazine is the antibacterial agent of choice in early stages of treatment.
When large areas of skin are burned, there is severe risk of infection, shock and hypermetabolic syndrome. Fluid replacement is critical, and topical silver sulfadiazine is the antibacterial agent of choice in early stages of treatment. The best treatment for pressure sores (decubitus ulcers) is prevention, as when they do occur they are painful, may cause necrosis and osteomyelitis, and may require prolonged extensive care. Wound dressings impregnated with antimicrobial agents or adsorbent particles are used, as are also proteolytic enzyme preparations or insect larvae.
The best treatment for pressure sores (decubitus ulcers) is prevention, as when they do occur they are painful, may cause necrosis and osteomyelitis, and may require prolonged extensive care. Wound dressings impregnated with antimicrobial agents or adsorbent particles are used, as are also proteolytic enzyme preparations or insect larvae.Review exercises
References and further reading
Anti-Cancer Council of Victoria. Cancer in Victoria 1996. Melbourne: Anti-Cancer Council of Victoria; 1999. Canstat 28. Sept 1999
Arowojolu A.O., Gallo M.F., Lopez L.M., et al. Combined oral contraceptive pills for treatment of acne. Cochrane Database of Systematic Reviews. 2009;3:CD004425..
Australian Drug Evaluation Committee. Prescribing Medicines in Pregnancy: An Australian Categorisation of Risk of Drug Use in Pregnancy, 4th edn. Canberra: Therapeutic Goods Administration; 1999.
Australian Institute of Health and Welfare (AIHW) & Australasian Association of Cancer Registries (ACCR). Cancer in Australia: An Overview 2008. AIHW cat. No. CAN 42. Canberra: AIHW (Cancer Series No. 46), 2008. Available: http://www.aihw.gov.au/publications/index.cfm/title/10607.[29 October 2009].
Australian Medicines Handbook 2010. Adelaide: AMH, 2010.
Baron E.D., Kirkland E.B., Santo Domingo D. Advances in photoprotection. Dermatology Nursing. 2008;20(4):265-272.
Beare P.G., Myers J.L. Adult Health Nursing, 3rd edn. St Louis: Mosby; 1998.
Bellamy D., Pfister A. World Medicine: Plants, Patients and People. Oxford: Blackwell; 1992.
Bowe W.P., Shalita A.R. Effective over-the-counter acne treatments. Seminars in Cutaneous Medicine and Surgery. 2008;27(3):170-176.
Braun L., Cohen M. Herbs and Natural Supplements: An Evidence-Based Guide, 2nd edn. Sydney: Elsevier Mosby; 2007.
Buys L.M. Treatment options for atopic dermatitis. American Family Physician. 2007;75(4):523-528.
Coleridge-Smith P.D. Leg ulcer treatment. Journal of Vascular Surgery. 2009;49(3):804-808.
Demling R.H. Burns: what are the pharmacological treatment options? Expert Opinion on Pharmacotherapy. 2008;9(11):1895-1908.
Dermatology Expert Group. Therapeutic Guidelines: Dermatology. Melbourne: Therapeutic Guidelines Limited; 2009. version 3
Dorland’s Illustrated Medical Dictionary. 30th edn. Philadelphia: Elsevier Saunders, 2003.
Fields A.L., Soprano D.R., Soprano K.J. Retinoids in biological control and cancer. Journal of Cellular Biochemistry. 2007;102(4):886-898.
George R., Clarke S., Thiboutot D. Hormonal therapy for acne. Seminars in Cutaneous Medicine and Surgery. 2008;27(3):188-196.
Ghali F., Kang S., Leyden J., et al. Changing the face of acne therapy. Cutis. 2009;83(2 Suppl):4-15.
Gupta A.K., Cooper E.A. Update in antifungal therapy of dermatophytosis. Mycopathologia. 2008;166(5–6):353-367.
Habif T.P., Campbell J.L., Dinulos J.G.H., Chapman M.S., Zug K.A. Skin Disease: Diagnosis and Treatment, 2nd edn. Philadelphia: Elsevier Mosby; 2005.
Helfrich Y.R., Sachs D.L., Voorhees J.J. Overview of skin aging and photoaging. Dermatology Nursing. 2008;20(3):177-183.
Heyneman A., Beele H., Vanderwee K., Defloor T. A systematic review of the use of hydrocolloids in the treatment of pressure ulcers. Journal of Clinical Nursing. 2008;17(9):1164-1173.
Howell M., Ford P. Medical Mysteries. London: Viking; 1985.
Jull A.B., Rodgers A., Walker N.. Honey as a topical treatment for wounds. Cochrane Database of Systematic Reviews. 2008;4:CD005083..
Kircik L.H., Del Rosso J.Q. Anti-TNF agents for the treatment of psoriasis. Journal of Drugs in Dermatology. 2009;8(6):546-559.
Lautenschlager S., Wulf H.C., Pittelkow M.R. Photoprotection. The Lancet. 2007;370(9586):528-537.
Mason A.R., Mason J., Cork M., et al. Topical treatments for chronic plaque psoriasis. Cochrane Database of Systematic Reviews. 2009;2:CD005028..
Mayser P., Freund V., Budihardja D. Toenail onychomycosis in diabetic patients: issues and management. American Journal of Clinical Dermatology. 2009;10(4):211-220.
Nohynek G.J., Dufour E.K., Roberts M.S. Nanotechnology, cosmetics and the skin: is there a health risk? Skin Pharmacology and Physiology. 2008;21(3):136-149.
O’Meara S., Al-Kurdi D., Ovington L.G.. Antibiotics and antiseptics for venous leg ulcers. Cochrane Database of Systematic Reviews. 2008;1:CD003557..
Pariser D. Topical corticosteroids and topical calcineurin inhibitors in the treatment of atopic dermatitis: focus on percutaneous absorption. American Journal of Therapeutics. 2009;16(3):264-273.
Ramos-e-Silva M., Carneiro S.C. Acne vulgaris: review and guidelines. Dermatology Nursing. 2009;21(2):63-67.
Roth J.J. The Essential Burn Unit Handbook. St Louis: Quality Medical Publishers; 2004.
Sauder D.N. Mechanism of action and emerging role of immune response modifier therapy in dermatologic conditions. Journal of Cutaneous Medicine and Surgery. 2004;8(Suppl 3):3-12.
Sherman R.A., Hall M.J., Thomas S. Medicinal maggots: an ancient remedy for some contemporary afflictions. Annual Review of Entomology. 2000;45:55-81.
Silla R.C., Fong J., Wright J., Wood F. Infection in acute burn wounds following the Bali bombings: a comparative prospective audit. Burns. 2006;32(2):139-144.
Sullivan J.R. Treatments for severe psoriasis. Australian Prescriber. 2009;32(1):14-18.
Thiboutot D., Gollnick H., Bettoli V., et al. New insights into the management of acne: an update from the Global Alliance to Improve Outcomes in Acne group. Journal of the American Academy of Dermatology. 2009;60(5 Suppl):S1-S50.
Wijesinghe M., Weatherall M., Perrin K., Beasley R. Honey in the treatment of burns: a systematic review and meta-analysis of its efficacy. New Zealand Medical Journal. 2009;122(1295):47-60.
Nursing aspects: www.dermatologynursing.net
TGA Factsheet on sunscreens: www.tga.gov.au/npmeds/sunscreen-zotd.htm
Website for checking NZ drugs: www.medsafe.govt.nz/
More weblinks at: http://evolve.elsevier.com/AU/Bryant/pharmacology