Nursing Care of the Family During Pregnancy
• Describe the process of confirming pregnancy and estimating the date of birth.
• Summarize the physical, psychosocial, and behavioral changes that usually occur as the mother and other family members adapt to pregnancy.
• Evaluate the benefits of prenatal care and problems of accessibility for some women.
• Outline the patterns of health care used to assess maternal and fetal health status at the initial and follow-up visits during pregnancy.
• Select the typical nursing assessments, diagnoses, interventions, and methods of evaluation in providing care for the pregnant woman.
• Plan education needed by pregnant women to understand physical discomforts related to pregnancy and to recognize signs and symptoms of potential complications.
• Examine the effect of culture, age, parity, and number of fetuses on the response of the family to the pregnancy and on the prenatal care provided.
• Describe the options for health care providers and birth setting choices that are available.
![]() http://evolve.elsevier.com/Lowdermilk/MWHC/
http://evolve.elsevier.com/Lowdermilk/MWHC/
The prenatal period is a time of physical and psychologic preparation for birth and parenthood. Becoming a parent is considered one of the maturational milestones of adult life. It is a time of intense learning for parents and those close to them. The prenatal period provides a unique opportunity for nurses and other members of the health care team to influence family health. During this period essentially healthy women seek regular care and guidance. The nurse’s health promotion interventions can affect the well-being of the woman, her unborn child, and the rest of her family for many years.
Regular prenatal visits, ideally beginning soon after the first missed menstrual period, offer opportunities to ensure the health of the expectant mother and her infant. Prenatal health care enables discovery, diagnosis, and treatment of preexisting maternal disorders and any disorders that develop during the pregnancy. Prenatal care is designed to monitor the growth and development of the fetus and to identify abnormalities that will interfere with the course of normal labor. Prenatal care also provides education and support for self-management and parenting.
Pregnancy spans 9 months, but health care providers do not use the familiar monthly calendar to determine fetal age or to discuss the pregnancy. Instead, they use lunar months, which last 28 days, or 4 weeks. Normal pregnancy, then, lasts about 10 lunar months, which is the same as 40 weeks or 280 days. Health care providers also refer to early, middle, and late pregnancy as trimesters. The first trimester lasts from weeks 1 through 13; the second, from weeks 14 through 26; and the third, from weeks 27 through 40. A pregnancy is considered to be at term if it advances to the completion of 37 weeks. The focus of this chapter is on meeting the health needs of the expectant family over the course of pregnancy, which is known as the prenatal period.
Diagnosis of Pregnancy
Women suspect pregnancy when they miss a menstrual period. Many women come to the first prenatal visit after a positive home pregnancy test; however, the clinical diagnosis of pregnancy before the second missed period is difficult in some women. Physical variations, obesity, or tumors, for example, confound even the experienced examiner. Accuracy is important, however, because emotional, social, health, or legal consequences of an inaccurate diagnosis, either positive or negative, can be extremely serious.
Signs and Symptoms
The physical cues of pregnancy vary greatly; therefore, the diagnosis of pregnancy is uncertain for a time. Many of the indicators of pregnancy are clinically useful in the diagnosis of pregnancy, and they are classified as presumptive, probable, or positive (see Table 13-2).
Presumptive indicators of pregnancy include subjective symptoms and objective signs. Subjective symptoms are reported by the woman and include amenorrhea, nausea and vomiting (morning sickness), breast tenderness, urinary frequency, and fatigue. Quickening, the mother’s first perception of fetal movement, is noted between weeks 16 and 20. Objective signs that are validated by the examiner include elevation of basal body temperature (BBT), breast and abdominal enlargement, and changes in the uterus and vagina. Other visible changes occur in the skin, such as striae gravidarum, deeper pigmentation of the areolae, chloasma (mask of pregnancy), and linea nigra (pigmented line on the abdomen).
The presumptive indicators of pregnancy can be caused by conditions other than gestation; therefore, these signs alone are not reliable for diagnosis of pregnancy.
Probable indicators of pregnancy are detected by an examiner and are related mainly to physical changes in the uterus. Objective signs include uterine enlargement, Braxton Hicks contractions, placental souffle (sound of blood passing through the placenta), ballottement (examiner is able to feel the fetus float during a vaginal examination), and a positive pregnancy test. When combined with presumptive signs and symptoms, they strongly suggest pregnancy, but they are not conclusive.
The positive indicators of pregnancy are directly attributed to the fetus and include the presence of a fetal heartbeat distinct from that of the mother, fetal movement felt by someone other than the mother, and visualization of the fetus with a technique such as ultrasound examination.
Estimating Date of Birth
After the diagnosis of pregnancy the woman’s first question usually concerns when she will give birth. This date has traditionally been termed the estimated date of confinement (EDC), although estimated date of delivery (EDD) also has been used. To promote a more positive perception of both pregnancy and birth, however, the term estimated date of birth (EDB) is suggested. Accurate dating of pregnancy and calculation of the EDB have implications for timing of specific prenatal screening tests, assessing fetal growth and critical decisions for managing pregnancy complications. Ultrasound dating of gestational age is accurate; however, researchers in the Routine Antenatal Diagnostic Imaging with Ultrasound Study (RADIUS) concluded that the cost associated with the routine use of ultrasound screening in the absence of clear clinical indications is prohibitive (Hunter, 2009).
Several formulas have been suggested for calculating the EDB based on the LMP. These rules assume regular 28-day ovulatory cycles and rely on a woman’s accurate recall of her LMP. The most common of these methods is Nägele’s rule, which is as follows: after determining the first day of the LMP, subtract 3 calendar months and add 7 days; or alternatively, add 7 days to the LMP and count forward 9 calendar months (Box 15-1). Only about 5% of women give birth spontaneously on the EDB as determined by Nägele’s rule. Most women give birth during the period extending from 7 days before to 7 days after the EDB.
Adaptation to Pregnancy
Pregnancy affects all family members, and each family member must adapt to the pregnancy and interpret its meaning in light of his or her own needs. This process of family adaptation to pregnancy takes place within a cultural environment influenced by societal trends. Dramatic changes have occurred in Western society in recent years, and the nurse must be prepared to support not only traditional families in the childbirth experience but also single-parent families, reconstituted families, dual-career families, and alternative families.
Much of the research on family dynamics in pregnancy in the United States and Canada has been done with Caucasian, middle-class nuclear families. Therefore, the findings may not apply to families who do not fit the traditional North American model. Adaptation of terms is appropriate to avoid embarrassment to the nurse and offense to the family. Additional research is needed on a variety of families to determine if study findings generated in traditional families are applicable to others.
Maternal Adaptation
Women of all ages use the months of pregnancy to adapt to the maternal role, a complex process of social and cognitive learning. Early in pregnancy nothing seems to be happening, and a woman may spend much time sleeping secondary to the increased fatigue of this stage. With the perception of fetal movement in the second trimester, the woman turns her attention inward to her pregnancy and to relationships with her mother and other women who have been or who are pregnant.
Pregnancy is a maturational milestone that can be stressful but also rewarding as the woman prepares for a new level of caring and responsibility. Her self-concept changes in readiness for parenthood as she prepares for her new role. She moves gradually from being self-contained and independent to being committed to a lifelong concern for another human being. This growth requires mastery of certain developmental tasks: accepting the pregnancy, identifying with the role of mother, reordering the relationships between herself and her mother and between herself and her partner, establishing a relationship with the unborn child, and preparing for the birth experience. The partner’s emotional support is an important factor in the successful accomplishment of these developmental tasks. Single women with limited support may have difficulty making this adaptation.
Accepting the Pregnancy
The first step in adapting to the maternal role is accepting the idea of pregnancy and assimilating the pregnant state into the woman’s way of life. Mercer (1995) described this process as cognitive restructuring and credited Reva Rubin (1984) as the nurse theorist who pioneered our understanding of maternal role attainment. The degree of acceptance is reflected in the woman’s emotional responses. Many women are upset initially at finding themselves pregnant, especially if the pregnancy is unintended. Eventual acceptance of pregnancy parallels the growing acceptance of the reality of a child. However, do not equate nonacceptance of the pregnancy with rejection of the child, for a woman may dislike being pregnant but feel love for the child to be born.
Women who are happy and pleased about their pregnancy often view it as biologic fulfillment and part of their life plan. They have high self-esteem and tend to be confident about outcomes for themselves, their babies, and other family members. Despite a general feeling of well-being, many women are surprised to experience emotional lability, that is, rapid and unpredictable changes in mood. These swings in emotions and increased sensitivity to others are disconcerting to the expectant mother and those around her. Increased irritability, explosions of tears, and anger can alternate with feelings of great joy and cheerfulness apparently with little or no provocation.
Profound hormonal changes that are part of the maternal response to pregnancy may be responsible for mood changes. Other reasons such as concerns about finances and changed lifestyle contribute to this seemingly erratic behavior.
Most women have ambivalent feelings during pregnancy whether the pregnancy was intended or not. Ambivalence—having conflicting feelings simultaneously—is considered a normal response for people preparing for a new role. During pregnancy women may, for example, feel great pleasure that they are fulfilling a lifelong dream, but they also may feel great regret that life as they now know it is ending.
Even women who are pleased to be pregnant may experience feelings of hostility toward the pregnancy or unborn child from time to time. Such incidents as a partner’s chance remark about the attractiveness of a slim, nonpregnant woman or news of a colleague’s promotion can give rise to ambivalent feelings. Body sensations, feelings of dependence, or the realization of the responsibilities of child care also can generate such feelings.
Intense feelings of ambivalence that persist through the third trimester may indicate an unresolved conflict with the motherhood role (Mercer, 1995). After the birth of a healthy child, memories of these ambivalent feelings usually are dismissed. If the child is born with a defect, however, a woman may look back at the times when she did not want the pregnancy and feel intensely guilty. She may believe that her ambivalence caused the birth defect. She then will need assurance that her feelings were not responsible for the problem.
Identifying with the Mother Role
The process of identifying with the mother role begins early in each woman’s life when she is being mothered as a child. Her social group’s perception of what constitutes the feminine role can subsequently influence her toward choosing between motherhood or a career, being married or single, being independent rather than interdependent, or being able to manage multiple roles. Practice roles, such as playing with dolls, babysitting, and taking care of siblings may increase her understanding of what being a mother involves.
Many women have always wanted a baby, liked children, and looked forward to motherhood. Their high motivation to become a parent promotes acceptance of pregnancy and eventual prenatal and parental adaptation. Other women apparently have not considered in any detail what motherhood means to them. During pregnancy these women must resolve conflicts such as not wanting the pregnancy and child-related or career-related decisions.
Reordering Personal Relationships
Close relationships of the pregnant woman undergo change during pregnancy as she prepares emotionally for the new role of mother. As family members learn their new roles, periods of tension and conflict may occur. An understanding of the typical patterns of adjustment can help the nurse reassure the pregnant woman and explore issues related to social support. Promoting effective communication patterns between the expectant mother and her own mother and between the expectant mother and her partner are common nursing interventions provided during the prenatal visits.
The woman’s own relationship with her mother is significant in adaptation to pregnancy and motherhood. Important components in the pregnant woman’s relationship with her mother are the mother’s availability (past and present), her reactions to the daughter’s pregnancy, respect for her daughter’s autonomy, and the willingness to reminisce (Mercer, 1995).
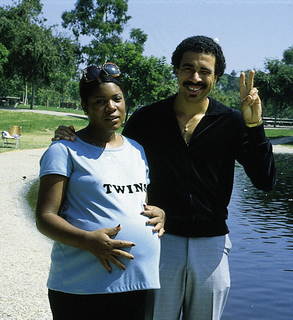
The mother’s reaction to the daughter’s pregnancy signifies her acceptance of the grandchild and of her daughter. If the mother is supportive, the daughter has an opportunity to discuss pregnancy and labor with a knowledgeable and accepting woman (Fig. 15-1). Reminiscing about the pregnant woman’s early childhood and sharing the prospective grandmother’s account of her childbirth experience help the daughter anticipate and prepare for labor and birth.

FIG. 15-1 A pregnant woman and her mother enjoying their walk together. (Courtesy Michael S. Clement, MD, Mesa, AZ.)
Although the woman’s relationship with her mother is significant in considering her adaptation to pregnancy, the most important person to the pregnant woman is usually the father of her child. Women express two major needs within this relationship during pregnancy: feeling loved and valued and having the child accepted by the partner.
The marital or committed relationship is not static but evolves over time. The addition of a child changes forever the nature of the bond between partners. This may be a time when couples grow closer, and the pregnancy has a maturing effect on the partners’ relationship as they assume new roles and discover new aspects of one another. Partners who trust and support each other are able to share mutual-dependency needs (Mercer, 1995).
Sexual expression during pregnancy is highly individual. The sexual relationship is affected by physical, emotional, and interactional factors, including misinformation about sex during pregnancy, sexual dysfunction, and physical changes in the woman. An individual may also inaccurately attribute anomalies, mental retardation, and other injuries to the fetus and mother to sexual relations during pregnancy. Some couples fear that the birth process will drastically change the woman’s genitals. Some couples do not express their concerns to the health care provider because of embarrassment or because they do not want to appear foolish.
As pregnancy progresses, changes in body shape, body image, and levels of discomfort influence both partners’ desire for sexual expression. During the first trimester the woman’s sexual desire may decrease, especially if she has breast tenderness, nausea, fatigue, or sleepiness. As she progresses into the second trimester, however, her sense of well-being combined with the increased pelvic congestion that occurs at this time may increase her desire for sexual release. In the third trimester, somatic complaints and physical bulkiness may increase her physical discomfort and again diminish her interest in sex.
Partners need to feel free to discuss their sexual responses during pregnancy with each other and with their health care provider (see later discussion).
Establishing a Relationship with the Fetus
Emotional attachment—feelings of being tied by affection or love—begins during the prenatal period as women use fantasizing and daydreaming to prepare themselves for motherhood (Rubin, 1975). They think of themselves as mothers and imagine maternal qualities they would like to possess. Expectant parents desire to be warm, loving, and close to their child. They try to anticipate changes that the child will bring into their lives and wonder how they will react to noise, disorder, reduced freedom, and caregiving activities. The mother-child relationship progresses through pregnancy as a developmental process that unfolds in three phases.
In phase 1 the woman accepts the biologic fact of pregnancy. She needs to be able to state, “I am pregnant” and incorporate the idea of a child into her body and self-image. The woman’s thoughts center around herself and the reality of her pregnancy. The child is viewed as part of herself, not a separate and unique person.
In phase 2 the woman accepts the growing fetus as distinct from herself, usually accomplished by the fifth month. She can now say, “I am going to have a baby.” This differentiation of the child from the woman’s self permits the beginning of the mother-child relationship that involves not only caring but also responsibility. Attachment of a mother to her child is enhanced by experiencing a planned pregnancy and it increases when ultrasound examination and quickening confirm the reality of the fetus.
With acceptance of the reality of the child (hearing the heartbeat and feeling the child move) and an overall feeling of well-being, the woman enters a quiet period and becomes more introspective. A fantasy child becomes precious to the woman. As the woman seems to withdraw and to concentrate her interest on the unborn child, her partner sometimes feels left out. If there are children in the family, they may become more demanding in their efforts to redirect the mother’s attention to themselves.
During phase 3 of the attachment process, the woman prepares realistically for the birth and parenting of the child. She expresses the thought, “I am going to be a mother” and defines the nature and characteristics of the child. She may, for example, speculate about the child’s sex (if unknown) and personality traits based on patterns of fetal activity.
Although the mother alone experiences the child within, both parents and siblings believe the unborn child responds in a very individualized, personal manner. Family members may interact a great deal with the unborn child by talking to the fetus and stroking the mother’s abdomen, especially when the fetus shifts position (Fig. 15-2). The fetus may have a nickname used by family members.
Preparing for Childbirth
Many women actively prepare for birth by reading books, viewing films, attending parenting classes, and talking to other women. They seek the best caregiver possible for advice, monitoring, and caring. The multiparous woman has her own history of labor and birth that influences her approach to preparation for this childbirth experience.
Anxiety can arise from concern about a safe passage for herself and her child during the birth process (Mercer, 1995; Rubin, 1975). Some women do not express this concern overtly, but they give cues to the nurse by making plans for care of the new baby and other children in case “anything should happen.” These feelings persist despite statistical evidence about the safe outcome of pregnancy for mothers and their infants. Many women fear the pain of childbirth or mutilation because they do not understand anatomy and the birth process. Education can alleviate many of these fears. Women also express concern over what behaviors are appropriate during the birth process and whether caregivers will accept them and their actions.
Toward the end of the third trimester, breathing is difficult, and fetal movements become vigorous enough to disturb the woman’s sleep. Backaches, frequency and urgency of urination, constipation, and varicose veins can become troublesome. The bulkiness and awkwardness of her body interfere with the woman’s ability to care for other children, perform routine work-related duties, and assume a comfortable position for sleep and rest. By this time, most women become impatient for labor to begin, whether the birth is anticipated with joy, dread, or a mixture of both. A strong desire to see the end of pregnancy, to be over and done with it, makes women at this stage ready to move on to childbirth.
Paternal Adaptation
The father’s beliefs and feelings about the ideal mother and father and his cultural expectation of appropriate behavior during pregnancy affect his response to his partner’s need for him. One man may engage in nurturing behavior. Another may feel lonely and alienated as the woman becomes physically and emotionally engrossed in the unborn child. He may seek friends and relationships outside the home or become interested in a new hobby or involved with his work. Some men view pregnancy as proof of their masculinity and their dominant role. To others, pregnancy has no meaning in terms of responsibility to either mother or child. However, for most men, pregnancy can be a time of preparation for the parental role with intense learning.
Accepting the Pregnancy
The ways fathers adjust to the parental role has been the subject of considerable research. In older societies the man enacted the ritual couvade; that is, he behaved in specific ways and respected taboos associated with pregnancy and giving birth so his new status was recognized and endorsed. Now some men experience pregnancy-like symptoms, such as nausea, weight gain, and other physical symptoms. This phenomenon is known as the couvade syndrome. Changing cultural and professional attitudes have encouraged fathers’ participation in the birth experience.
The man’s emotional response to becoming a father, his concerns, and his informational needs change during the course of pregnancy. Phases of the developmental pattern become apparent. May (1982) described three phases characterizing the developmental tasks experienced by the expectant father:
• The announcement phase may last from a few hours to a few weeks. The developmental task is to accept the biologic fact of pregnancy. Men react to the confirmation of pregnancy with joy or dismay, depending on whether the pregnancy is desired, unplanned, or unwanted. Ambivalence in the early stages of pregnancy is common. If pregnancy is unplanned or unwanted, some men find the alterations in life plans and lifestyles difficult to accept. Some men engage in extramarital affairs for the first time during their partner’s pregnancy. Others batter their wives for the first time or escalate the frequency of battering episodes (Krieger, 2008). Chapter 5 provides information about violence against women and offers guidance on assessment and intervention.
• The second phase, the moratorium phase, is the period when he adjusts to the reality of pregnancy. The developmental task is to accept the pregnancy. Men appear to put conscious thought of the pregnancy aside for a time. They become more introspective and engage in many discussions about their philosophy of life, religion, childbearing, and childrearing practices and their relationships with family members, particularly with their father. Depending on the man’s readiness for the pregnancy, this phase may be relatively short or persist until the last trimester.
• The third phase, the focusing phase, begins in the last trimester and is characterized by the father’s active involvement in both the pregnancy and his relationship with his child. The developmental task is to negotiate with his partner the role he is to play in labor and to prepare for parenthood. In this phase the man concentrates on his experience of the pregnancy and begins to think of himself as a father.
Identifying with the Father Role
Each man brings to pregnancy attitudes that affect the way in which he adjusts to the pregnancy and parental role. His memories of the fathering he received from his own father, the experiences he has had with child care, and the perceptions of the male and father roles within his social group will guide his selection of the tasks and responsibilities he will assume. Some men are highly motivated to nurture and love a child. They are excited and pleased about the anticipated role of father (Fig. 15-3). Others are more detached or even hostile to the idea of fatherhood.
Reordering Personal Relationships
The partner’s main role in pregnancy is to nurture and respond to the pregnant woman’s feelings of vulnerability. The partner also must deal with the reality of the pregnancy. The partner’s support indicates involvement in the pregnancy and preparation for attachment to the child.
Some aspects of a partner’s behavior may indicate rivalry, and it may be especially evident during sexual activity. For example, some men protest that fetal movements prevent sexual gratification or feel that they are being watched by the fetus during sexual activity. However, feelings of rivalry are often unconscious and not verbalized, but expressed in subtle behaviors.
The woman’s increased introspection may cause her partner to feel uneasy as she becomes preoccupied with thoughts of the child and of her motherhood, with her growing dependence on her health care provider, and with her reevaluation of the couple’s relationship.
Establishing a Relationship with the Fetus
The father-child attachment can be as strong as the mother-child relationship, and fathers can be as competent as mothers in nurturing their infants. The father-child attachment also begins during pregnancy. A father may rub or kiss the maternal abdomen; try to listen, talk, or sing to the fetus; or play with the fetus as he notes movement. Calling the unborn child by name or nickname helps to confirm the reality of pregnancy and promote attachment.
Men prepare for fatherhood in many of the same ways as women do for motherhood—by reading and by fantasizing about the baby. Daydreaming about their role as father is common in the last weeks before the birth; however, men rarely describe their thoughts unless they are reassured that such daydreams are normal.
Nurses can help fathers identify concerns and prepare for the reality of a baby by asking questions such as the following:
• What do you expect the baby to look and act like?
• What do you think being a father will be like?
• Have you thought about the baby’s crying? Changing diapers? Burping the baby? Being awakened at night? Sharing your partner with the baby?
Some fathers will not wish to answer such questions when they are asked but may need time to think them through or discuss them with their partners.
As the birth date approaches, men have more questions about fetal and newborn behaviors. Some men are shocked or amazed at the smallness of clothes and furniture for the baby. If an expectant father can imagine only an older child and has difficulty visualizing or talking about an infant, this situation must be explored. The nurse can tell the father about the unborn child’s ability to respond to light, sound, and touch and encourage him to feel and talk to the fetus. A tour of a newborn nursery or discussions with new fathers, as in childbirth classes, may be welcomed.
Some men become involved by choosing the child’s name and anticipating the child’s sex, if it is not already known. Some couples select the name of the child as early as the first month of pregnancy. Family tradition, religious customs, and the continuation of the parent’s name or names of relatives or friends are important in the selection process.
Preparing for Childbirth
The days and weeks immediately before the expected day of birth are characterized by anticipation and anxiety. Boredom and restlessness are common as the couple focuses on the birth process; however, during the last 2 months of pregnancy, many expectant fathers experience a surge of creative energy at home and on the job. They become dissatisfied with their present living space. If possible, they tend to act on the need to alter the environment (remodeling, painting, etc.). This activity is their way of sharing in the childbearing experience. They are able to channel the anxiety and other feelings experienced during the final weeks before birth into productive activities. This behavior earns recognition and compliments from friends, relatives, and their partners.
Major concerns for the man are getting the woman to a health care facility in time for the birth and not appearing ignorant. Many men want to be able to recognize labor and determine when it is appropriate to leave for the hospital or call the birth attendant. They fantasize different situations and plan what they will do in response to them, or rehearse taking various routes to the hospital, timing each route at different times of the day.
Some prospective fathers have questions about the labor suite’s furniture and equipment, nursing staff, and location, as well as the availability of the birth attendant and anesthesia provider. Others want to know what is expected of them when their partners are in labor. The man also may have fears concerning safe passage of his child and partner and the possible death or complications of his partner and child. It is important he verbalize these fears, otherwise he cannot help his mate deal with her own spoken or unspoken apprehension.
With the exception of childbirth preparation classes, a man has few opportunities to learn ways to be an involved and active partner in this rite of passage into parenthood. Mothers often sense the tensions and apprehensions of the unprepared, unsupportive father and it often increases their fears.
The same fears, questions, and concerns may affect birth partners who are not the biologic fathers. Birth partners need to be kept informed, supported, and included in all activities in which the mother desires their participation. Nurses can do much to promote pregnancy and birth as a family experience.
Sibling Adaptation
Sharing the spotlight with a new brother or sister may be the first major crisis for a child. The older child often experiences a sense of loss or feels jealous at being “replaced” by the new sibling. Some of the factors that influence the child’s response are age, the parents’ attitudes, the role of the father, the length of separation from the mother, the facility visitation policy, and the way the child has been prepared for the change.
A mother with other children must devote time and effort to reorganizing her relationships with them. She needs to prepare siblings for the birth of the baby (Fig. 15-4 and Box 15-2) and begin the process of role transition in the family by including the children in the pregnancy and being sympathetic to older children’s concerns about losing their places in the family hierarchy. No child willingly gives up a familiar position.

FIG. 15-4 A sibling class of preschoolers learns infant care using dolls. (Courtesy Marjorie Pyle, RNC, Lifecircle, Costa Mesa, CA.)
Siblings’ responses to pregnancy vary with their age and dependency needs. The 1-year-old infant seems largely unaware of the process, but the 2-year-old child notices the change in his or her mother’s appearance and may comment that “Mommy’s fat.” Toddlers’ need for sameness in the environment makes children aware of any change. They may exhibit more clinging behavior and sometimes regress in toilet training or eating.
By age 3 or 4 years, children like to be told the story of their own beginning and accept a comparison of their own development with that of the present pregnancy. They like to listen to the fetal heartbeat and feel the baby moving in utero (see Fig. 15-2). Sometimes they worry about how the baby is being fed and what it wears.
School-age children take a more clinical interest in their mother’s pregnancy. They may want to know in more detail, “How did the baby get in there?” and “How will it get out?” Children in this age-group notice pregnant women in stores, churches, and schools and sometimes seem shy if they need to approach a pregnant woman directly. On the whole, they look forward to the new baby, see themselves as “mothers” or “fathers,” and enjoy buying baby supplies and readying a place for the baby. Because they still think in concrete terms and base judgments on the here and now, they respond positively to their mother’s current good health.
Early and middle adolescents preoccupied with the establishment of their own sexual identity may have difficulty accepting the overwhelming evidence of the sexual activity of their parents. They reason that if they are too young for such activity, certainly their parents are too old. They seem to take on a critical parental role and may ask, “What will people think?” or “How can you let yourself get so fat?” or “How can you let yourself get pregnant?” Many pregnant women with teenage children will confess that the attitudes of their teenagers are the most difficult aspect of their current pregnancy.
Late adolescents do not appear to be unduly disturbed. They are busy making plans for their own lives and realize that they soon will be gone from home. Parents usually report they are comforting and act more as other adults than as children.
Grandparent Adaptation
Every pregnancy affects all family relationships. For expectant grandparents a first pregnancy in a child is undeniable evidence that they are growing older. Many think of a grandparent as old, white-haired, and becoming feeble of mind and body; however, some people face grandparenthood while still in their 30s or 40s. Some individuals react negatively to the news that they will be grandparents, indicating that they are not ready for the new role.
In some family units, expectant grandparents are nonsupportive and may inadvertently decrease the self-esteem of the parents-to-be. Mothers may talk about their terrible pregnancies; fathers may discuss the endless cost of rearing children; and mothers-in-law may complain that their sons are neglecting them because their concern is now directed toward the pregnant daughters-in-law.
However, most grandparents are delighted at the prospect of a new baby in the family. It reawakens the feelings of their own youth, the excitement of giving birth, and their delight in the behavior of the parents-to-be when they were infants. They set up a memory store of the child’s first smiles, first words, and first steps that they can use later for “claiming” the newborn as a member of the family. These behaviors provide a link between the past and present for the parents and grandparents-to-be.
In addition, the grandparent is the historian who transmits the family history, a resource person who shares knowledge based on experience; a role model; and a support person. The grandparent’s presence and support can strengthen family systems by widening the circle of support and nurturance (Fig. 15-5).
Care Management
The purpose of prenatal care is to identify existing risk factors and other deviations from normal so that pregnancy outcomes may be enhanced (Johnson, Gregory, & Niebyl, 2007). Major emphasis is placed on preventive aspects of care, primarily to motivate the pregnant woman to practice optimal self-management and to report unusual changes early so that problems can be prevented or minimized. If health behaviors must be modified in early pregnancy, nurses need to understand psychosocial factors that may influence the woman. In holistic care, nurses provide information and guidance about not only the physical changes but also the psychosocial impact of pregnancy on the woman and members of her family. The goals of prenatal nursing care, therefore, are to foster a safe birth for the infant and to promote satisfaction of the mother and family with the pregnancy and birth experience.
More than two thirds of women in the United States received care in the first trimester. African- American, Hispanic, and Native-American women were twice as likely to get late prenatal care or no care at all than were Caucasian women (Heron, Sutton, Xu, Ventura, Strobino, & Guyer, 2010). Although women of middle or high socioeconomic status routinely seek prenatal care, women living in poverty or who lack health insurance are not always able to use public health care services or gain access to private care. Lack of culturally sensitive care providers and barriers in communication resulting from differences in language also interfere with access to care (Darby, 2007). Likewise, immigrant women who come from cultures in which prenatal care is not emphasized may not know to seek routine prenatal care. Birth outcomes in these populations are less positive, with higher rates of maternal and fetal or newborn complications. Problems with low birth weight (LBW; less than 2500 g) and infant mortality have in particular been associated with lack of adequate prenatal care.
Barriers to obtaining health care during pregnancy include lack of transportation, unpleasant clinic facilities or procedures, inconvenient clinic hours, childcare problems, and personal attitudes (American College of Obstetricians and Gynecologists [ACOG] Committee on Health Care for Underserved Women, 2006; Daniels, Noe, & Mayberry, 2006; Johnson, Gregory, & Niebyl, 2007). The availability of advanced practice nurses (nurse practitioners and certified nurse-midwives) as independent providers of care or in collaborative practice with physicians improves the availability and accessibility of prenatal care. A regular schedule of home visiting by trained unlicensed health workers during pregnancy is effective in reducing barriers to prenatal care (Agency for Healthcare Research and Quality [AHRQ] Healthcare Innovations Exchange, 2009).
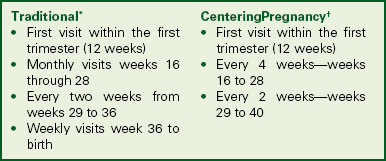
The current model for provision of prenatal care has been used for more than a century. The initial visit usually occurs in the first trimester, with monthly visits through week 28 of pregnancy. Thereafter, visits are scheduled every 2 weeks until week 36, and then every week until birth (American Academy of Pediatrics and ACOG, 2007) (Box 15-3). Research supports a model of fewer prenatal visits, and in some practices there is a growing tendency to have fewer visits with women who are at low risk for complications.
CenteringPregnancy is a care model that is gaining in popularity. This model is one of group prenatal care in which authority is shifted from the provider to the woman and other women who have similar due dates. The model creates an atmosphere that facilitates learning, encourages discussion, and develops mutual support. Most care takes place in the group setting after the first visit and continues for ten 2-hour sessions (Moos, 2006). At each meeting, the first 30 minutes is spent in completing assessments (by the woman herself and by the healthcare provider), and the rest of the time is spent in group discussion of specific issues such as discomforts of pregnancy and preparation for labor and birth. Families and partners are encouraged to participate (Massey, Rising, & Ickovics, 2006; Reid, 2007) (see Box 15-3).
Prenatal care is ideally a multidisciplinary activity in which nurses work with nurse-midwives, nutritionists, physicians, social workers, and others. Collaboration among these individuals is necessary to provide holistic care. The case management model, which makes use of care maps and critical pathways, is one system that promotes comprehensive care with limited overlap in services. To emphasize the nursing role, care management for the initial visit and follow-up visits is organized around the central elements of the nursing process: assessment, nursing diagnoses, expected outcomes, plan of care and interventions, and evaluation (see the Nursing Process box).
In recent years the concept of preconception care has been recognized as an important contributor to good pregnancy outcomes (see Chapter 4). If women can be taught healthy lifestyle behaviors and then practice them before conception—specifically good nutrition, entering pregnancy with as healthy a weight as possible, adequate intake of folic acid, avoidance of alcohol and tobacco use, prevention of sexually transmitted infections (STIs) and other health hazards—a healthier pregnancy may result. Likewise, women who have health problems related to chronic diseases such as diabetes mellitus can be counseled regarding their special needs with the intent to minimize maternal and fetal complications.
Initial Visit
Once the presence of pregnancy has been confirmed and the woman’s desire to continue the pregnancy has been validated, prenatal care is begun. The assessment process begins at the initial prenatal visit and is continued throughout the pregnancy. Assessment techniques include the interview, physical examination, and laboratory tests. Because the initial visit and follow-up visits are distinctly different in content and process, they are described separately.
Prenatal Interview
The pregnant woman and family members who may be present should be told that the first prenatal visit is longer and more detailed than future visits. The initial evaluation includes a
comprehensive health history emphasizing the current pregnancy, previous pregnancies, the family, a psychosocial profile, a physical assessment, diagnostic testing, and an overall risk assessment. A prenatal history form (paper or electronic) is used to document information obtained.
The therapeutic relationship between the nurse and the woman is established during the initial assessment interview. Two types of data are collected: the woman’s subjective appraisal of her health status and the nurse’s objective observations.
One or more family members often will accompany the pregnant woman. With her permission, include those accompanying the woman in the initial prenatal interview. Observations and information about the woman’s family are then included in the database. For example, if the woman has small children with her, the nurse can ask about her plans for child care during the time of labor and birth. Note any special needs at this time (e.g., wheelchair access, assistance in getting on and off the examining table, and cognitive deficits).
Reason for Seeking Care: Although pregnant women are scheduled for “routine” prenatal visits, they often come to the health care provider seeking information or reassurance about a particular concern. When the woman is asked a broad, open-ended question such as, “How have you been feeling?” she may reveal problems that could otherwise be overlooked. The woman’s chief concerns should be recorded in her own words to alert other personnel to the priority of needs as identified by her. At the initial visit the desire for information about what is normal in the course of pregnancy is typical.
Current Pregnancy: The presumptive signs of pregnancy may be of great concern to the woman. A review of symptoms she is experiencing and how she is coping with them helps establish a database to develop a plan of care. Some early teaching may be provided at this time.
Childbearing and Female Reproductive System History: Data are gathered on the woman’s age at menarche, menstrual history, and contraceptive history; the nature of any infertility or reproductive system conditions; a history of any STIs; a sexual history; and a detailed history of all her pregnancies, including the present pregnancy, and their outcomes. The date of the last Papanicolaou (Pap) test and the result are noted. The date of her LMP is obtained to calculate the EDB.
Health History: The health history includes those physical conditions or surgical procedures that may affect the pregnancy or that may be affected by the pregnancy. For example, a pregnant woman who has diabetes, hypertension, or epilepsy requires special care. Because most women are anxious during the initial interview, the nurse’s reference to cues, such as a MedicAlert bracelet, prompts the woman to explain allergies, chronic diseases, or medications being taken (i.e., cortisone, insulin, or anticonvulsants).
The woman should also describe the nature of previous surgical procedures. If a woman has undergone uterine surgery or extensive repair of the pelvic floor, a cesarean birth may be necessary; appendectomy rules out appendicitis as a cause of right lower quadrant pain in pregnancy; and spinal surgery may contraindicate the use of spinal or epidural anesthesia. Note any injury involving the pelvis.
Women who have chronic or handicapping conditions often forget to mention them during the initial assessment because they have become so adapted to them. Special shoes or a limp may indicate the existence of a pelvic structural defect, which is an important consideration in pregnant women. The nurse who observes these special characteristics and inquires about them sensitively can obtain individualized data that will provide the basis for a comprehensive nursing care plan (Smeltzer, 2007). Observations are vital components of the interview process because they prompt the nurse and woman to focus on the specific needs of the woman and her family.
Nutritional History: The woman’s nutritional history is an important component of the prenatal history because her nutritional status has a direct effect on the growth and development of the fetus. A dietary assessment can reveal special dietary practices, food allergies, eating behaviors, the practice of pica, and other factors related to her nutritional status (see Box 14-7). Obese women should receive counseling about weight gain, nutrition and food choices. They should also be advised about their risk for complications for themselves and increased risk for congenital abnormalities (Davies, Maxwell, McLeod, Gagnon, Basso, Bos, et al., 2010). Pregnant women are usually motivated to learn about good nutrition and respond well to nutritional advice generated by this assessment. Women who receive specific written and verbal information regarding nutrition, weight gain expectations, and exercise as well as weight gain reminders at each prenatal visit, are less likely to gain weight in excess of the IOM recommendations during pregnancy (Polley, Wing, & Sims, 2002).
History of Drug and Herbal Preparations Use: A woman’s past and present use of drugs (legal over-the-counter [OTC] and prescription medications; herbal preparations; caffeine; alcohol; nicotine) and illegal (e.g., marijuana, cocaine, heroin) is assessed. This is because many substances cross the placenta and may therefore harm the developing fetus. See Chapter 32 for discussion of substance abuse during pregnancy. Increasing numbers of individuals are using herbal preparations, and this includes pregnant women. Therefore, it is important for health care providers to question prenatal women regarding the use of herbal preparations and document their responses.
Family History: The family history provides information about the woman’s immediate family, including parents, siblings, and children. These data help identify familial or genetic disorders or conditions that could affect the present health status of the woman or her fetus.
Social, Experiential, and Occupational History: Situational factors such as the family’s ethnic and cultural background and socioeconomic status are assessed while the history is obtained. The following information may be obtained in several encounters. The woman’s perception of this pregnancy is explored by asking questions such as the following:
• Is this pregnancy planned or not, wanted or not?
• Is the woman pleased, displeased, accepting, or nonaccepting?
• What problems related to finances, career, or living accommodations will occur as a result of the pregnancy?
The family support system is determined by asking the following questions:
• What primary support is available to her?
• Are changes needed to promote adequate support?
• What are the existing relationships among the mother, father or partner, siblings, and in-laws?
• What preparations are being made for her care and that of dependent family members during labor and for the care of the infant after birth?
• Is financial, educational, or other support needed from the community?
• What are the woman’s ideas about childbearing, her expectations of the infant’s behavior, and her outlook on life and the female role?
Other questions that should be asked include the following:
• What does the woman think it will be like to have a baby in the home?
During interviews throughout the pregnancy nurses should remain alert to the appearance of potential parenting problems, such as depression, lack of family support, and inadequate living conditions. Nurses must assess the woman’s attitude toward health care, particularly during childbearing, her expectations of health care providers, and her view of the relationship between herself and the nurse.
Coping mechanisms and patterns of interacting are identified. Early in the pregnancy the nurse should determine the woman’s knowledge in various areas: pregnancy, maternal changes, fetal growth, self-care, and care of the newborn, including feeding. Asking about attitudes toward unmedicated or medicated childbirth and about her knowledge of the availability of parenting skills classes is important. Before planning for nursing care, the nurse needs information about the woman’s decision-making abilities and living habits (i.e., exercise, sleep, diet, diversional interests, personal hygiene, clothing). Common stressors during childbearing include the baby’s welfare, labor and birth process, behaviors of the newborn, the woman’s relationship with the baby’s father and her family, changes in body image, and physical symptoms.
Explore attitudes concerning the range of acceptable sexual behavior during pregnancy by asking questions such as the following: What has your family (partner, friends) told you about sex during pregnancy? Give emphasis to the woman’s sexual self-concept by asking questions such as the following: How do you feel about the changes in your appearance? How does your partner feel about your body now? How do you feel about wearing maternity clothes?
Women should be questioned regarding their occupation—past and present—because this may adversely affect maternal and fetal health. For some women, heavy lifting and exposure to chemicals and radiation may be part of their daily work, and these activities may negatively affect the pregnancy. Standing for long periods of time at a retail checkout line or in front of a classroom are associated with orthostatic hypotension. For others long hours of sitting at a desk working on a computer can contribute to carpal tunnel syndrome or circulatory stasis in the legs.
History of Physical Abuse: All women should be assessed for a history or risk of physical abuse, particularly because the likelihood of abuse increases during pregnancy. Although visual cues from the woman’s appearance or behavior may suggest the possibility, no one profile of the battered woman exists. During pregnancy the target body parts change during abusive episodes. Women report physical blows directed to the head, breasts, abdomen, and genitalia. Sexual assault is common.
Battering and pregnancy in teenagers constitutes a particularly difficult situation. Adolescents may be trapped in the abusive relationship because of their inexperience. Routine screening for abuse and sexual assault is recommended for pregnant adolescents (Family Violence Prevention Fund, 2010). Because pregnancy in young adolescent girls is commonly the result of sexual abuse, the nurse should assess the desire to maintain the pregnancy (see Chapter 5 for further discussion).
Review of Systems: During this portion of the interview, ask the woman to identify and describe preexisting or concurrent problems in any of the body systems, and assess her mental status. Question the woman about physical symptoms she has experienced, such as shortness of breath or pain. Pregnancy affects and is affected by all body systems; therefore, information on the present status of the body systems is important in planning care. For each sign or symptom described, the following additional data should be obtained: body location, quality, quantity, chronology, aggravating or alleviating factors, and associated manifestations (onset, character, course) (Seidel, Ball, Dains, Flynn, Soloman, & Stewart, 2011).
Physical Examination
The initial physical examination provides the baseline for assessing subsequent changes. The nurse should determine the woman’s needs for basic information regarding reproductive anatomy and provide this information, along with a demonstration of the equipment that may be used and an explanation of the procedure itself. The interaction requires an unhurried, sensitive, and gentle approach with a matter-of-fact attitude.
The physical examination begins with assessment of vital signs and height and weight (for calculation of body mass index [BMI]) (see Chapter 14). The bladder should be empty before pelvic examination. A urine specimen may be obtained to test for protein, glucose, or leukocytes or other tests.
Each examiner develops a routine for proceeding with the physical examination; most choose the head-to-toe progression. Heart and lung sounds are evaluated, and extremities are examined. Distribution, amount, and quality of body hair are of particular importance because the findings reflect nutritional status, endocrine function, and attention to hygiene. The thyroid gland is assessed carefully. The height of the fundus is noted if the first examination is done after the first trimester of pregnancy. During the examination the nurse must remain alert to the woman’s cues that give direction to the remainder of the assessment and that indicate a potential threatening condition such as supine hypotension—low blood pressure (BP) that occurs while the woman is lying on her back, causing feelings of faintness. See Chapter 4 for a detailed description of the physical examination.
Whenever a pelvic examination is performed, the tone of the pelvic musculature and the woman’s knowledge of Kegel exercises is assessed. Particular attention is paid to the size of the uterus because this is an indication of the duration of gestation. During the examination the nurse can coach the woman in breathing and relaxation techniques, as needed. One vaginal examination during pregnancy is recommended, but another is usually not performed unless medically indicated.
Laboratory Tests
The laboratory data yielded by the analysis of the specimens obtained during the examination provide important information concerning the symptoms of pregnancy and the woman’s health status.
Specimens are collected at the initial visit so that the cause of any abnormal findings can be treated (Table 15-1). Blood is drawn for a variety of tests. A sickle cell screen is recommended for women of African, Asian, or Middle Eastern descent, and testing for antibody to the human immunodeficiency virus (HIV) is strongly recommended for all pregnant women (Centers for Disease Control and Prevention [CDC], Workowski, & Berman, 2006) (Box 15-4). In addition, pregnant women and fathers with a family history of cystic fibrosis and of Caucasian ethnicity may elect to have blood drawn for testing to ascertain if they are a cystic fibrosis carrier (Norton, 2008). A urine specimen is collected for cultures and metabolic function tests. A purified protein derivative (PPD) tuberculin test may be administered to assess exposure to tuberculosis. During the pelvic examination, cervical and vaginal smears can be obtained for cytologic studies and for diagnosis of infection (e.g., gonorrhea, chlamydia).
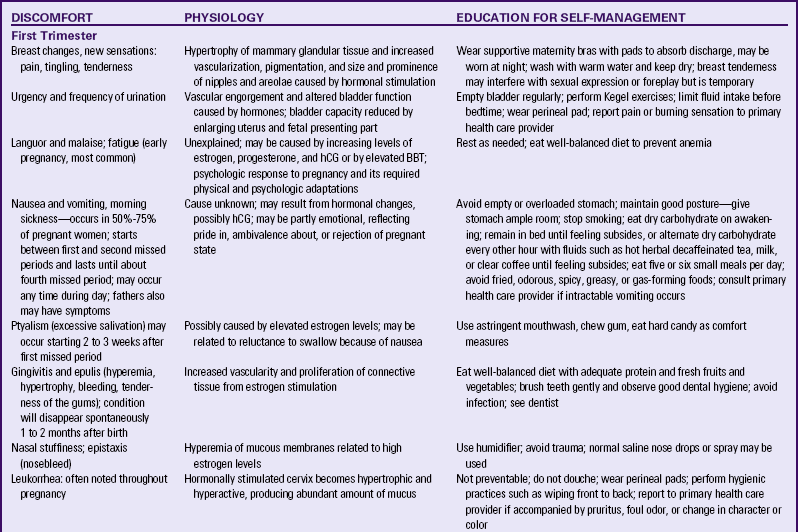
TABLE 15-1
LABORATORY TESTS IN PRENATAL PERIOD
| LABORATORY TEST | PURPOSE |
| Hemoglobin, hematocrit, WBC, differential | Detects anemia; detects infection |
| Hemoglobin electrophoresis | Identifies women with hemoglobinopathies (e.g., sickle cell anemia, thalassemia) |
| Blood type, Rh, and irregular antibody | Identifies those fetuses at risk for developing erythroblastosis fetalis or hyperbilirubinemia in neonatal period |
| Rubella titer | Determines immunity to rubella |
| Tuberculin skin testing; chest film after 20 weeks of gestation in women with reactive tuberculin tests | Screens for exposure to tuberculosis |
| Urinalysis, including microscopic examination of urinary sediment; pH, specific gravity, color, glucose, albumin, protein, RBCs, WBCs, casts, acetone; hCG | Identifies women with glycosuria, renal disease, hypertensive disease of pregnancy; infection; occult hematuria |
| Urine culture | Identifies women with asymptomatic bacteriuria |
| Renal function tests: BUN, creatinine, electrolytes, creatinine clearance, total protein excretion | Evaluates level of possible renal compromise in women with a history of diabetes, hypertension, or renal disease |
| Pap test | Screens for cervical intraepithelial neoplasia; if a liquid-based test is used, may also screen for HPV |
| Cervical cultures for Neisseria gonorrhoeae, Chlamydia | Screens for asymptomatic infection at first visit |
| Vaginal/anal culture | GBS test done at 35-37 weeks for infection |
| RPR, VDRL, or FTA-ABS | Identifies women with untreated syphilis, done at first visit |
| HIV antibody, hepatitis B surface antigen, toxoplasmosis | Screens for the specific infections |
| 1-hour glucose tolerance | Screens for gestational diabetes; done at initial visit for women with risk factors; done at 24-28 weeks for pregnant women at risk whose initial screen was negative; women with low risk usually not tested |
| 3-hour glucose tolerance | Tests for gestational diabetes in women with elevated glucose level after 1-hour test; must have two elevated readings for diagnosis |
| Cardiac evaluation: ECG, chest x-ray, and echocardiogram | Evaluates cardiac function in women with a history of hypertension or cardiac disease |
BUN, Blood urea nitrogen; ECG, electrocardiogram; FTA-ABS, fluorescent treponemal antibody absorption test; GBS, group B streptococci; hCG, human chorionic gonadotropin; HIV, human immunodeficiency virus; HPV, human papillomavirus; RBC, red blood cell; RPR, rapid plasma reagin; VDRL, Venereal Disease Research Laboratory; WBC, white blood cell.
The finding of risk factors during pregnancy may indicate the need to repeat some tests at other times. For example, exposure to tuberculosis or an STI would necessitate repeat testing after treatment. STIs are common in pregnancy and may have negative effects on mother and fetus. Careful assessment and screening are essential.
Follow-up Visits
In traditional prenatal care, monthly visits are scheduled routinely during the first and second trimesters, although clients can make additional appointments as the need arises. During the third trimester, however, the possibility for complications increases, and closer monitoring is necessary. Starting with week 28, maternity visits are scheduled every 2 weeks until week 36 and then every week until birth, unless the health care provider individualizes the schedule. Visits can occur more or less frequently, often depending on individual needs, complications, and risks of the pregnant woman. The pattern of interviewing the woman first and then assessing physical changes and performing laboratory tests continues.
In prenatal care models that use a reduced frequency screening schedule or in CenteringPregnancy, the timing of follow-up visits will be different, but assessments and care will be similar.
Interview
Follow-up visits are less intensive than the initial prenatal visit. At each of these follow-up visits, the woman is asked to summarize relevant events that have occurred since the previous visit. She is asked about her general emotional and physiologic well-being, complaints, problems, and questions she may have. Personal and family needs also are identified and explored (Fig. 15-6).
Emotional changes are common during pregnancy, and therefore asking whether the woman has experienced any mood swings, reactions to changes in her body image, bad dreams, or worries is reasonable. Note any positive feelings (her own and those of her family). Record the reactions of family members to the pregnancy and the woman’s emotional changes.
During the third trimester, assess current family situations and their effect on the woman. For example, assess siblings’ and grandparents’ responses to the pregnancy and the coming child. In addition, assess of the woman and her family’s knowledge of warning signs of emergencies; signs of preterm and term labor; the labor process and concerns about labor; and fetal development and methods to assess fetal well-being. The nurse should ask if the woman is planning to attend childbirth preparation classes and what she knows about pain management during labor.
A review of the woman’s physical systems is appropriate at each prenatal visit, and any suspicious signs or symptoms are assessed in depth. Identify any discomforts reflecting adaptations to pregnancy. Inquire about success with self-care measures as well as outcomes of prescribed therapy.
Physical Examination
Reevaluation is a constant aspect of a pregnant woman’s care. Physiologic changes are documented as the pregnancy progresses and reviewed for possible deviations from normal progress.
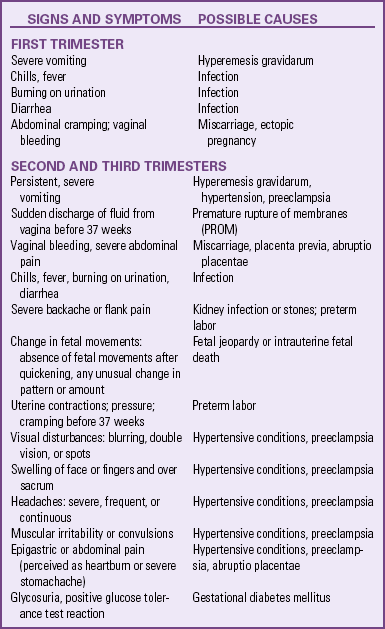
At each visit physical parameters are measured. BP is measured using the same arm at every visit (see Box 13-1). The woman’s weight is assessed, and the appropriateness of the gestational weight gain is evaluated in relationship to her BMI. Urine may be checked by dipstick, and the presence and degree of edema are noted. For examination of the abdomen, the woman lies on her back with her arms by her side and head supported by a pillow. The bladder should be empty. Abdominal inspection is followed by measurement of the height of the fundus (see Fig. 15-7). While the woman lies on her back, the nurse should be alert for the occurrence of supine hypotension. When a pregnant woman is lying in this position, the weight of the abdominal contents may compress the vena cava and aorta, causing a decrease in BP and a feeling of faintness (see the Emergency box).
The information provided through the interview and the physical examination reflects the status of maternal adaptations. When any of the findings are suspicious, an in-depth examination is performed. For example, careful interpretation of BP is important in the risk factor analysis of all pregnant women. Signs and symptoms other than hypertension also may be present that indicate potential complications (see the Signs of Potential Complications box).
Fetal Assessment
Listening for Fetal Heart Tones: Toward the end of the first trimester, before the uterus is an abdominal organ, the fetal heart tones (FHTs) can be heard with an ultrasound fetoscope or an ultrasound stethoscope (see Fig. 15-8). To hear the FHTs, place the instrument in the midline, just above the symphysis pubis, and apply firm pressure. Offer the woman and her family the opportunity to listen to the FHTs.
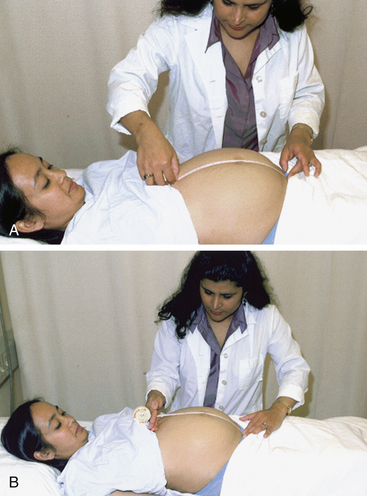
Measuring Fundal Height: During the second trimester the uterus becomes an abdominal organ. The fundal height (measurement of the height of the uterus above the symphysis pubis) is used as one indicator of fetal growth. The measurement also provides a gross estimate of the duration of pregnancy. From gestational weeks (GW) 18 to 32, the height of the fundus in centimeters is approximately the same as the number of weeks of gestation (± 2 GW), if the woman’s bladder is empty at the time of measurement. As much as a 3-cm variation is possible if the bladder is full (Cunningham, Leveno, Bloom, Hauth, Rouse, & Spong, 2010). For example, a woman of 28 weeks of gestation, with an empty bladder, would measure from 26 to 30 cm. In addition, the fundal height measurement may aid in the identification of high risk factors. A stable or decreased fundal height
may indicate the presence of intrauterine growth restriction (IUGR); an excessive increase could indicate the presence of multifetal gestation (more than one fetus) or polyhydramnios.
A disposable paper metric tape measure is preferred for measuring fundal height; plastic retractable tape measures should be cleaned after use and prior to retraction. To increase the reliability of the measurement, the same person examines the pregnant woman at each of her prenatal visits, but often this is not possible. All clinicians who examine a particular pregnant woman should be consistent in their measurement technique. Ideally, a protocol should be established for the health care setting in which the measurement technique is explicitly set forth, and the woman’s position on the examining table, the measuring device, and method of measurement used are specified. Conditions under which the measurements are taken also can be described in the woman’s records, including whether the bladder was empty and whether the uterus was relaxed or contracted at the time of measurement.
Various positions for measuring fundal height have been described. The woman can be supine, have her head elevated, have her knees flexed, or have both her head elevated and knees flexed. Measurements obtained with the woman in the various positions differ, making it even more important to standardize the fundal height measurement technique.
Placement of the tape measure also can vary. The tape can be placed in the middle of the woman’s abdomen and the measurement made from the upper border of the symphysis pubis to the upper border of the fundus, with the tape measure held in contact with the skin for the entire length of the uterus (Fig. 15-7, A). In another measurement technique, the upper curve of the fundus is not included in the measurement. Instead, one end of the tape measure is held at the upper border of the symphysis pubis with one hand, and the other hand is placed at the upper border of the fundus. The tape is placed between the middle and index fingers of the other hand, and the point where these fingers intercept the tape measure is taken as the measurement (see Fig. 15-7, B).
Gestational Age: In an uncomplicated pregnancy fetal gestational age is estimated after the duration of pregnancy and the EDB are determined. Fetal gestational age is determined from the menstrual history, contraceptive history, pregnancy test result, and the following findings obtained during the clinical evaluation:
• First uterine evaluation: date, size
• Fetal heart first heard: date, method (Doppler stethoscope, fetoscope)
• Current fundal height, estimated fetal weight (EFW)
• Current week of gestation by history of LMP and/or ultrasound examination
• Ultrasound examination: date, week of gestation, biparietal diameter (BPD)
Quickening usually occurs between 16 and 20 weeks of gestation and is initially experienced as a fluttering sensation. The mother’s report should be recorded. Multiparas often perceive fetal movement earlier than primigravidas.
The use of ultrasound examination (also called a sonogram) in early pregnancy has become routine, and many health care providers have this equipment available in the office. This procedure may be used to establish the duration of pregnancy if the woman cannot give a precise date for her LMP or if the size of the uterus does not conform to the EDB as calculated by Nägele’s rule. Ultrasound also provides information about the well-being of the fetus (see Chapter 26 for further discussion). However, the routine use of ultrasound has not been found to substantively improve fetal outcome (Hunter, 2009).
Health Status: The assessment of fetal health status includes consideration of fetal movement. The mother is instructed to note the extent and timing of fetal movements and to report immediately if the pattern changes or if movement ceases. Regular movement has been found to be a reliable indicator of fetal health (Frøen, Heazell, Tveit, Saastad, Fretts, & Flenday, 2008) (see Chapter 26).
The fetal heart rate (FHR) is checked on routine visits once it has been heard (Fig. 15-8). Early in the second trimester, the heartbeat may be heard with a Doppler stethoscope (see Fig. 15-8, B). To detect the heartbeat before the fetal position can be palpated by Leopold maneuvers (see Chapter 19), the scope is moved around the abdomen until the heartbeat is heard. Each nurse develops a set pattern for searching the abdomen for the heartbeat—for example, starting first in the midline about 2 to 3 cm above the symphysis, then moving to the left lower quadrant, and so on. The heartbeat is counted for 1 minute, and the quality and rhythm noted. Later in the second trimester, the FHR can be determined with a fetoscope or a Pinard fetoscope (see Fig. 15-8, A and C). A normal rate and rhythm are other good indicators of fetal health. Once the heartbeat is noted, its absence is cause for immediate investigation.
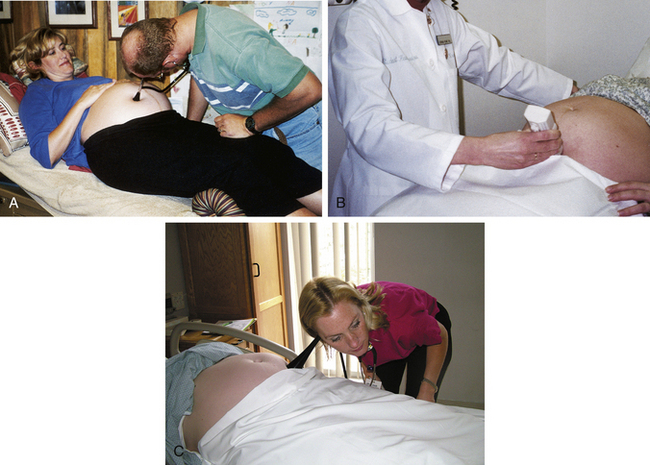
FIG. 15-8 Detecting fetal heart rate. A, Father listens to the fetal heart (first detectable around 18 to 20 weeks) with a fetoscope. B, Doppler ultrasound stethoscope (fetal heartbeat detectable at 12 weeks). C, Pinard fetoscope. Note: Hands should not touch fetoscope while listening. (A, Courtesy Shannon Perry, Phoenix, AZ; B, courtesy Dee Lowdermilk, Chapel Hill, NC; C, courtesy Julie Perry Nelson, Loveland, CO.)
Fetal health status is investigated intensively if any maternal or fetal complications arise (e.g., gestational hypertension, IUGR, premature rupture of membranes [PROM], irregular or absent FHR, or decreased/absent fetal movements after quickening). Careful, precise, and concise recording of client responses and laboratory results contributes to the continuous supervision vital to ensuring the well-being of the mother and fetus.
Laboratory Tests
The number of routine laboratory tests done during follow-up visits in pregnancy is limited. A clean-catch urine specimen is obtained to test for glucose, protein, nitrites, and leukocytes at each visit. Urine specimens for culture and sensitivity are obtained, and cervical and vaginal smears and blood tests are repeated as necessary.
First-trimester screening for chromosomal abnormalities is offered as an option between 11 and 14 weeks. This multiple marker screen includes sonographic evaluation of nuchal translucency (NT) and biochemical markers—pregnancy-associated placental protein (PAPP-A) and free beta-human chorionic gonadotropin (β-hCG).
Maternal serum alpha-fetoprotein (MSAFP) screening is recommended between 15 and 22 GW, ideally between 16 and 18 weeks of gestation. Elevated levels are associated with open neural tube defects and multiple gestations, whereas low levels are associated with Down syndrome. The multiple-marker, or triple-screen, blood test is also recommended. Done between 16 and 18 weeks of gestation, it measures the MSAFP, hCG, and unconjugated estriol, the levels of which are combined to yield one value. Maternal serum marker levels that are higher or lower than normal are associated with chromosomal abnormalities (see Chapter 26). If not done earlier in pregnancy, a glucose screen is obtained for women at high risk for gestational diabetes between 24 and 28 weeks of gestation. GBS testing is done between 35 and 37 weeks of gestation; cultures collected earlier will not accurately predict GBS status at time of birth (Van Dyke, Phares, Lynfield, Thomas, Arnold, Craig, et al., 2009).
Other diagnostic tests, such as amniocentesis, are available to assess the health status of both the pregnant woman and the fetus (See Chapter 26 for further discussion).
Collaborative Care
After obtaining information through the assessment process, the data are analyzed to identify deviations from the norm and unique needs of the pregnant woman and her family.
The nurse-client relationship is critical in setting the tone for further interaction. The techniques of listening with an attentive expression, touching, and using eye contact have their place, as does recognizing the woman’s feelings and her right to express these feelings. The interaction may occur in various formal or informal settings. A clinical setting, home visits, or telephone conversations all provide opportunities for contact and can be used effectively.
In supporting a woman, the nurse must remember that both the nurse and the woman are contributing to the relationship. The nurse has to accept the woman’s responses as a factor in trying to be of help. An example of one nurse-client relationship is as follows:
Keisha has been very forthright in saying that this pregnancy was unplanned but had countered this observation with comments such as, “All things happen for the best,” and “Children bring their own love.” Over time, as our relationship developed to one of mutual trust, she complained increasingly of her fear of pain, of hating to wear maternity clothes, and of having to give up helping the family. Finally I ventured to say, “Sometimes when a pregnancy is unplanned, women resent it and are angry about it.” Her relief was evident. She said, “You don’t know how angry I’ve been.” As a result, the whole tenor of support being offered changed, and the plan was adjusted to meet her real needs.
The nurse also must accept that the woman must be a willing partner in a purely voluntary relationship. As such, the relationship can be refused or terminated at any time by the pregnant woman or her family.
Supportive care involves developing, augmenting, or changing the mechanisms used by women and their families in coping with stress. The nurse tries to promote active participation by the family in the solution of their own problems. The nurse can help a woman gather pertinent information, explore options, decide on a course of action, and assume responsibility for the outcomes. These outcomes may include living with a problem as it is, easing the effects of a problem so that it can be accepted more readily, or eliminating the problem by effecting change.
At other times a successful outcome can be documented readily. For example, a woman who early in her pregnancy had predicted a severe depressive state in the post-birth period was elated when such a state did not materialize. She remarked to the nurse who had provided support during the labor and birth, “You’re the best nerve medicine I’ve ever had!”
Education About Maternal and Fetal Changes
Expectant parents are typically curious about the growth and development of the fetus and the subsequent changes that occur in the mother’s body. Mothers in particular are sometimes more tolerant of the discomforts related to the continuing pregnancy if they understand the underlying causes. Educational literature that describes fetal and maternal changes is available and can be used in explaining changes as they occur. The nurse’s familiarity with any material shared with pregnant families is essential to effective client education. Educational material may include electronic and written materials appropriate to the pregnant woman’s or couple’s literacy level and experience and the agency’s resources. It is important that available educational materials reflect the pregnant woman’s or couple’s ethnicity, culture, and literacy level to be most effective.
Education for Self-Management
The expectant mother needs information about many subjects. The nurse who is observant, listens, and knows typical concerns of expectant parents can anticipate questions that will be asked and prompt mothers and partners to discuss what is on their minds. Many times, printed literature can be given to supplement the individualized teaching the nurse provides, and women often avidly read books and pamphlets related to their own experience. When nurses read the literature before they distribute it, they can point out areas that may not correspond with local health care practices. Because family members are common sources for health information, it is also important to include them in the health education endeavors (Yamashita, 2009). In addition, as more individuals use the computer for information, the pregnant woman or couple may have questions from their Internet reviews. Nurses may also share recommended electronic sites from reliable sources.
Pregnant women who receive conflicting advice or instruction are likely to grow increasingly frustrated with members of the health care team and the care provided. Several topics that may cause concerns in pregnant women are discussed in the following sections.
Nutrition: Good nutrition is important for the maintenance of maternal health during pregnancy and the provision of adequate nutrients for embryonic and fetal development (American Dietetic Association [ADA], 2008). Assessing a woman’s nutritional status and providing information on nutrition are part of the nurse’s responsibilities in providing prenatal care. This includes assessment of weight gain during pregnancy as well as prenatal nutrition. Teaching may include discussion about foods high in iron, encouragement to take prenatal vitamins, and recommendations to moderate or limit caffeine intake. In some settings a registered dietitian conducts classes for pregnant women on the topics of nutritional status and nutrition during pregnancy, or interviews them to assess their knowledge of these topics. Nurses can refer women to a registered dietitian if a need is revealed during the nursing assessment. (For detailed information concerning maternal and fetal nutritional needs and related nursing care, see Chapter 14.)
Personal Hygiene: During pregnancy the sebaceous (sweat) glands are highly active because of hormonal influences, and women often perspire freely. They may be reassured that the increase is normal and that their previous patterns of perspiration will return after the postpartum period. Baths and warm showers can be therapeutic because they relax tense, tired muscles, help counter insomnia, and make the pregnant woman feel fresh. Tub bathing is permitted even in late pregnancy because little water enters the vagina unless under pressure. However, late in pregnancy, when the woman’s center of gravity lowers, she is at risk for falling. Tub bathing is contraindicated after rupture of the membranes.
Prevention of Urinary Tract Infections: Because of physiologic changes that occur in the renal system during pregnancy (see Chapter 13), urinary tract infections (UTIs) are common but they may be asymptomatic. Women should be instructed to inform their health care provider if blood or pain occurs with urination. UTIs pose a risk to the mother and fetus; therefore, the prevention or early treatment of these infections is essential.
The nurse can assess the woman’s understanding and use of good handwashing techniques before and after urinating and the importance of wiping the perineum from front to back. Soft, absorbent toilet tissue, preferably white and unscented, should be used; harsh, scented, or printed toilet paper may cause irritation. Bubble bath or other bath oils should be avoided because these may irritate the urethra. Women should wear cotton-crotch underpants and pantyhose and avoid tight-fitting slacks or jeans for long periods; anything that allows a buildup of heat and moisture in the genital area may foster the growth of bacteria.
Some women do not consume enough fluid and food. After discovering the woman’s food preferences, the nurse should advise her to drink at least 2 L (eight glasses) of liquid a day, preferably water, to maintain an adequate fluid intake that ensures frequent urination. Pregnant women should not limit fluids in an effort to reduce the frequency of urination. Women need to know that if urine looks dark (concentrated), they must increase their fluid intake. The consumption of yogurt and acidophilus milk may help prevent urinary tract and vaginal infections. The nurse should review healthy urination practices with the woman. Women are told not to ignore the urge to urinate because holding urine lengthens the time bacteria are in the bladder and allows them to multiply. Women should plan ahead when they are faced with situations that may normally require them to delay urination (e.g., a long car ride). They always should urinate before going to bed at night. Bacteria can be introduced during intercourse; therefore, women are advised to urinate before and after intercourse, and then drink a large glass of water to promote additional urination. Although frequently recommended, there is conflicting evidence regarding the effectiveness of cranberry juice and, in particular, the effective dosage in the prevention of urinary tract infections (Jepson & Craig, 2008).
Kegel Exercises: Kegel exercises (deliberate contraction and relaxation of the pubococcygeus muscle) strengthen the muscles around the reproductive organs and improve muscle tone. Many women are not aware of the muscles of the pelvic floor until it is pointed out that these are the muscles used during urination and sexual intercourse that can be consciously controlled. The muscles of the pelvic floor encircle the vaginal outlet, and they need to be exercised because an exercised muscle can then stretch and contract readily at the time of birth. Practice of pelvic muscle exercises during pregnancy also results in fewer complaints of urinary incontinence in late pregnancy and postpartum (Lentz, 2007).
Several ways of performing Kegel exercises have been described. The method described in the Teaching for Self-Management box on p. 91. demonstrates evidence-based nursing care. This method was developed by nurses involved in a research utilization project for continence in women. Teaching has been effective if the woman reports an increased ability to control urine flow and greater muscular control during sexual intercourse.
Preparation for Breastfeeding: Pregnant women are usually eager to discuss their plans for feeding the newborn. Breast milk is the food of choice, in part because breastfeeding is associated with a decreased incidence of perinatal morbidity and mortality. The American Academy of Pediatrics recommends breastfeeding for at least a year. However, a deep-seated aversion to breastfeeding on the part of the woman or partner, the woman’s need for certain medications or use of street drugs, and certain life-threatening illnesses and medical complications, such as HIV infection, are contraindications to breastfeeding (Lawrence & Lawrence, 2005). Although hepatitis B surface antigen (HBsAg) has not been shown to be transmitted through breast milk, as an added precaution, it is recommended that infants born to HBsAg-positive women receive the hepatitis B vaccine and hepatitis B immune globulin (HBIg) immediately after birth. In developed countries, women who are HIV positive are discouraged from nursing because the risk of HIV transmission outweighs the risk of the infant dying from another cause (Lawrence & Lawrence).
A woman’s decision about the method of infant feeding often is made before pregnancy; therefore, educating women of childbearing age about the benefits of breastfeeding is essential. If undecided, the pregnant woman and her partner are given information about the advantages and disadvantages of bottle feeding and breastfeeding so they can make an informed choice. Health care providers support their decisions and provide any needed teaching,
Women with inverted nipples need special consideration if they are planning to breastfeed. The pinch test is done to determine whether the nipple is everted or inverted (Fig. 15-9). The nurse shows the woman the way to perform the pinch test. It involves having the woman place her thumb and forefinger on her areola and gently press inward. This action will cause her nipple either to stand erect or to invert. Most nipples will stand erect.
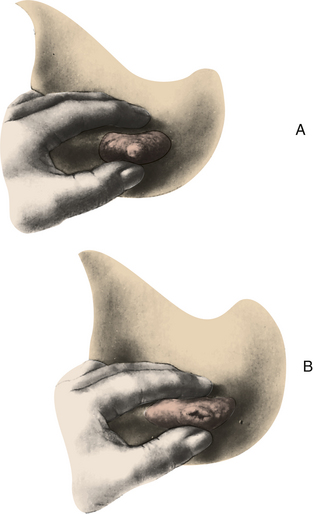
FIG. 15-9 A, Normal nipple everts with gentle pressure. B, Inverted nipple inverts with gentle pressure. (Modified from Lawrence, R., & Lawrence, R. [2005]. Breastfeeding: A guide for the medical profession [6th ed.]. Philadelphia: Mosby.)
Exercises to break the adhesions that cause the nipple to invert do not work and may precipitate uterine contractions (Lawrence & Lawrence, 2005). Breast shells, small plastic devices that fit over the nipples, may be recommended for women who have flat or inverted nipples (Fig. 15-10). Breast shells work by exerting a continuous, gentle pressure around the areola that pushes the nipple through a central opening in the inner shield. The shells should be worn for 1 to 2 hours daily during the last trimester of pregnancy and for gradually increasing lengths of time (Lawrence & Lawrence). Breast stimulation is contraindicated in women at risk for preterm labor; therefore, the decision to suggest the use of breast shells to women with flat or inverted nipples must be made judiciously.

FIG. 15-10 Breast shell in place inside bra to evert nipple. (Courtesy Michael S. Clement, MD, Mesa, AZ.)
The woman is taught to cleanse the nipples with warm water to keep the ducts from being blocked with dried colostrum. Soap, ointments, alcohol, and tinctures should not be applied because they remove protective oils that keep the nipples supple. The use of these substances may cause the nipples to crack during early lactation (Lawrence & Lawrence, 2005).
The woman who plans to breastfeed should purchase a nursing bra that will accommodate her increased breast size during the last few months of pregnancy and during lactation. If her breasts are very heavy, or if the woman feels uncomfortable with the weight unsupported, the bra can be worn day and night.
Dental Care: Dental care during pregnancy is especially important because nausea during pregnancy may lead to poor oral hygiene, allowing dental caries to develop. A fluoride toothpaste should be used daily. Inflammation and infection of the gingival and periodontal tissues may occur (Russell & Mayberry, 2008). Research links periodontal disease with preterm births and LBW (Lopez, 2005) and an increased risk for preeclampsia (Boggess & Edelstein, 2006; Dasanayake, Gennaro, Hendricks-Munoz, & Chhun, 2008).
Because calcium and phosphorus in the teeth are fixed in enamel, the old adage “for every child a tooth” is not true. There is no scientific evidence to support the belief that filling teeth or even dental extraction involving the administration of local or nitrous oxide–oxygen anesthesia precipitates miscarriage or premature labor. However, antibacterial therapy should be considered for sepsis, especially in pregnant women who have had rheumatic heart disease or nephritis. Emergency dental surgery is not contraindicated during pregnancy. However, explain the risks and benefits of dental surgery to the woman. The American Dental Association (2006) recommends that elective dental treatment not be scheduled in the first trimester or last half of the third trimester. The woman will be most comfortable during the second trimester because the uterus is now outside the pelvis but not so large as to cause discomfort while she sits in a dental chair (Russell & Mayberry, 2008).
Physical Activity: Physical activity promotes a feeling of well-being in the pregnant woman. It improves circulation, promotes relaxation and rest, and counteracts boredom, as it does in the nonpregnant woman (ACOG, 2002). Detailed exercise tips for pregnancy are presented in the Teaching for Self-Management box: Exercise Tips for Pregnant Women. Exercises that help relieve the low back pain that often arises during the second trimester because of the increased weight of the fetus are demonstrated in Figure 15-11.
Posture and Body Mechanics: Skeletal and musculature changes and hormonal changes (relaxin) in pregnancy may
predispose the woman to backache and possible injury. As pregnancy progresses, the pregnant woman’s center of gravity changes, pelvic joints soften and relax, and stress is placed on abdominal musculature. Poor posture and body mechanics contribute to the discomfort and potential for injury. To minimize these problems, women can learn good body posture and body mechanics (Fig. 15-12). Strategies to prevent or relieve backache are presented in the Teaching for Self-Management box: Posture and Body Mechanics.
Rest and Relaxation: Nurses encourage women to plan regular rest periods, particularly as pregnancy advances. The side-lying position is recommended because it promotes uterine perfusion and fetoplacental oxygenation by eliminating pressure on the ascending vena cava and descending aorta, which can lead to supine hypotension (Fig. 15-13). Show the woman how to rise slowly from a side-lying position to prevent placing strain on the back and to minimize the orthostatic hypotension caused by changes in position common in the latter part of pregnancy. To stretch and rest back muscles at home or work, the nurse can show the woman the way to do the following exercises:

FIG. 15-13 Side-lying position for rest and relaxation. Some women prefer to support upper part of leg with pillows. (Courtesy Julie Perry Nelson, Loveland, CO.)
• Stand behind a chair. Support and balance self by using the back of the chair (Fig. 15-14). Squat for 30 seconds; stand for 15 seconds. Repeat 6 times, several times per day, as needed.

FIG. 15-14 Squatting for muscle relaxation and strengthening and for keeping leg and hip joints flexible. (Courtesy Julie Perry Nelson, Loveland, CO).
• While sitting in a chair, lower head to knees for 30 seconds. Raise head. Repeat 6 times, several times per day, as needed.
Conscious relaxation is the process of releasing tension from the mind and body through deliberate effort and practice. The ability to relax consciously and intentionally is beneficial for the following reasons:
• To relieve the normal discomforts related to pregnancy
• To reduce stress and therefore diminish pain perception during the childbearing cycle
• To heighten self-awareness and trust in one’s own ability to control responses and functions
• To help cope with stress in everyday life situations, whether the woman is pregnant or not
The techniques for conscious relaxation are numerous and varied. Box 15-5 gives some guidelines.
Employment: Employment of pregnant women usually has no adverse effects on pregnancy outcomes. Job discrimination that is based strictly on pregnancy is illegal. However, some job environments pose potential risk to the fetus (e.g., dry-cleaning plants, chemistry laboratories, parking garages). Excessive fatigue is usually the deciding factor in the termination of employment. Strategies to improve safety during pregnancy are described in the Teaching for Self-Management box: Safety During Pregnancy.
Women with sedentary jobs need to walk around at intervals to counter the usual sluggish circulation in the legs. They also should neither sit nor stand in one position for long periods, and they should avoid crossing their legs at the knees, because all of these activities can foster the development of varices and thrombophlebitis. Standing for long periods also increases the risk of preterm labor. The pregnant woman’s chair should provide adequate back support. Use of a footstool can prevent pressure on veins, relieve strain on varicosities, minimize edema of feet, and prevent backache.
Clothing: Some women continue to wear their usual clothes during pregnancy as long as they fit and feel comfortable. If maternity clothing is needed, outfits may be purchased new or found at thrift shops or garage sales in good condition. Comfortable, loose clothing is recommended. Tight bras and belts, stretch pants, garters, tight-top knee socks, panty girdles, and other constrictive clothing should be avoided because tight clothing over the perineum encourages vaginitis and miliaria (heat rash), and impaired circulation in the legs can cause varicosities.
Maternity bras are constructed to accommodate the increased breast weight, chest circumference, and the size of breast tail tissue (under the arm). These bras also have drop-flaps over the nipples to facilitate breastfeeding. A good bra can help prevent neckache and backache.
Maternal support hose give considerable comfort and promote greater venous emptying in women with large varicose veins. Ideally, support stockings should be put on before the woman gets out of bed in the morning. Figure 15-15 demonstrates a position for resting the legs and reducing swelling and varicosities.

FIG. 15-15 Position for resting legs and for reducing edema and varicosities. Encourage woman with vulvar varicosities to include pillow under her hips. (Courtesy Julie Perry Nelson, Loveland, CO.)
Comfortable shoes that provide firm support and promote good posture and balance also are advisable. Very high heels and platform shoes are not recommended because of the changes in the pregnant woman’s center of gravity, and the hormone relaxin, which softens pelvic joints in later pregnancy, all of which can cause her to lose her balance. In addition, in the third trimester, the woman’s pelvis tilts forward, and her lumbar curve increases. The resulting leg aches and cramps are aggravated by nonsupportive shoes. Exercises to relieve leg cramps are depicted in Figure 15-16.
Travel: Travel is not contraindicated in low risk pregnant women. However, women with high risk pregnancies are advised to avoid long-distance travel after fetal viability has been reached to avert possible economic and psychologic consequences of giving birth to a preterm infant far from home. Travel to areas in which medical care is poor, water is untreated, or malaria is prevalent should be avoided if possible. Women who contemplate foreign travel should be aware that many health insurance carriers do not cover a birth in a foreign setting or even hospitalization for preterm labor. In addition, vaccinations for foreign travel may be contraindicated during pregnancy.
Pregnant women who travel for long distances should schedule periods of activity and rest. While sitting, the woman can practice deep breathing, foot circling, and alternately contracting and relaxing different muscle groups. She should avoid becoming fatigued. Although travel in itself is not a cause of adverse outcomes such as miscarriage or preterm labor, certain precautions are recommended while traveling in a car. For example, women riding in a car should wear automobile restraints and stop to walk every hour.
Maternal death as a result of injury is the most common cause of fetal death. The next most common cause is placental separation that occurs because body contours change in reaction to the force of a collision. The uterus as a muscular organ can adapt its shape to that of the body, but the placenta is not resilient. At the impact of collision, placental separation can occur. A combination lap belt and shoulder harness is the most effective automobile restraint, and both should be used (Fig. 15-17). The lap belt should be worn low across the pelvic bones and as snug as is comfortable. The shoulder harness should be worn above the gravid uterus and below the neck to prevent chafing. The pregnant woman should sit upright. The headrest should be used to prevent whiplash injury. Airbags if present should remain engaged, but the steering wheel should be tilted upward, away from the abdomen and the seat moved back away from the steering wheel as much as possible (Cesario, 2007).

FIG. 15-17 Proper use of seat belt and headrest. (Courtesy Brian and Mayannyn Sallee, Anchorage, AK.)
A pregnant woman traveling in high-altitude regions has lowered oxygen levels that may cause fetal hypoxia, especially if she is anemic. However, the current information on this condition is limited, and recommendations are not standardized.
Airline travel in large commercial jets usually poses little risk to the pregnant woman, but policies vary from airline to airline. The pregnant woman is advised to inquire about restrictions or recommendations from her carrier. Most health care providers allow air travel up to 36 weeks of gestation in women without health or pregnancy complications. Metal detectors used at airport security checkpoints are not harmful to the fetus. The 8% humidity at which the cabins of commercial airlines are maintained may result in some water loss; hydration (with water) should therefore be maintained under these conditions. Sitting in the cramped seat of an airliner for prolonged periods may increase the risk of superficial and deep thrombophlebitis; therefore, the woman is encouraged to take a walk around the aircraft during each hour of travel to minimize this risk. A review of the literature reveals that cosmic radiation exposure for flight crews is well below the annual limit recommended by the International Commission on Radiological Protection (Health Physics Society, 2009).
Medications and Herbal Preparations: Although much has been learned in recent years about fetal drug toxicity, the possible teratogenicity of many medications, both prescription and OTC, is still unknown. This is especially true for new medications and combinations of drugs. Moreover, certain subclinical errors or deficiencies in intermediate metabolism in the fetus may cause an otherwise harmless drug to be converted into a hazardous one. The greatest danger of drug-caused developmental defects in the fetus extends from the time of fertilization through the first trimester, a time when the woman may not realize she is pregnant. Self-treatment must be discouraged.
Immunizations: Some individuals have raised concern over the safety of various immunization practices during pregnancy. Immunization with live or attenuated live viruses is contraindicated during pregnancy because of its potential teratogenicity but should be part of postpartum care. Live-virus vaccines include those for measles (rubeola and rubella), chickenpox, and mumps, as well as the Sabin (oral) poliomyelitis vaccine (no longer used in the United States). Vaccines that can be administered during pregnancy include tetanus, diphtheria, recombinant hepatitis B, and influenza (inactivated) vaccines (CDC, 2008; www.cdc.gov/vaccines).
Alcohol, Cigarette Smoke, Caffeine, and Drugs: A safe level of alcohol consumption during pregnancy has not been established. Complete abstinence is strongly advised in order to avoid any risk of pregnancy complications. Maternal alcoholism is associated with high rates of miscarriage and fetal alcohol spectrum disorders (FASD); the risk for miscarriage in the first trimester is dose related (three or more drinks per day) (CDC, 2009). Cigarette smoking or continued exposure to secondhand smoke (even if the mother does not smoke) is associated with IUGR and an increase in perinatal and infant morbidity and mortality. Smoking is associated with an increased frequency of preterm labor, PROM, abruptio placentae, placenta previa, and fetal death, possibly resulting from decreased placental perfusion. Smoking cessation activities should be incorporated into routine prenatal care (ACOG Committee on Obstetric Practice, 2005). All women who smoke should be strongly encouraged to quit or at least reduce the number of cigarettes they smoke. Most studies of human pregnancy have revealed no association between caffeine consumption and birth defects or LBW. Some studies have documented an increased risk for miscarriage with caffeine intake greater than 200 mg/day (Weng, Odouli, & Li, 2008).
Because other effects are unknown, however, pregnant women are advised to limit their caffeine intake, particularly coffee intake because it has high caffeine content per unit of measure.
Any drug or environmental agent that enters the pregnant woman’s bloodstream has the potential to cross the placenta and harm the fetus. Marijuana, heroin, and cocaine are common examples. Although the problem of substance abuse in pregnancy is considered a major public health concern and comprehensive care of drug-addicted women improves maternal and neonatal outcomes, few facilities are available for treatment of these women (see Chapters 32 and 35).
Normal Discomforts: Pregnant women have physical symptoms that would be considered abnormal in the nonpregnant state. Women pregnant for the first time have an increased need for explanations of the causes of the discomforts and for advice on ways to relieve them. The discomforts of the first trimester are fairly specific. Information about the physiology and prevention of and self-management for discomforts experienced during the three trimesters is given in Table 15-2. Box 15-6 lists alternative and complementary therapies and why they might be used in pregnancy (see also Fig. 15-18). Nurses can do much to allay a first-time mother’s anxiety about such symptoms by
telling her about them in advance and using terminology that the woman (or couple) can understand. Understanding the rationale for treatment promotes their participation in their care. Interventions should be individualized, with attention given to the woman’s lifestyle and culture (see Nursing Care Plan: Discomforts of Pregnancy and Warning Signs).
Recognizing Potential Complications: One of the most important responsibilities of care providers is to alert the pregnant woman to signs and symptoms that indicate a potential complication of pregnancy. The woman needs to know how and to whom to report such warning signs. Therefore, the pregnant woman and her family can be reassured if they receive and use a printed form written at the appropriate literacy level, in their language and reflective of their culture,
listing the signs and symptoms that warrant an investigation and the telephone numbers to call if they have questions or an emergency.
The nurse must answer questions honestly as they arise during pregnancy. Pregnant women often have difficulty deciding when to report signs and symptoms. The mother is encouraged to refer to the printed list of potential complications and to listen to her body. If the woman senses that something is wrong, she should call her care provider. Several signs and symptoms must be discussed more extensively. These include vaginal bleeding, alteration in fetal movements, symptoms of gestational hypertension, rupture of membranes, and preterm labor.
Recognizing Preterm Labor: Teaching each expectant mother to recognize preterm labor is necessary for early diagnosis and treatment. Preterm labor occurs after the twentieth week but before the thirty-seventh week of pregnancy and consists of uterine contractions that if untreated cause the cervix to open earlier than normal and result in preterm birth. Warning signs and symptoms of preterm labor are discussed in Chapter 33.
Sexual Counseling
Sexual counseling of expectant couples includes countering misinformation, providing reassurance of normality, and suggesting alternative behaviors. The uniqueness of each couple is considered within a biopsychosocial framework (see the Teaching for Self-Management box: Sexuality in Pregnancy). Nurses can initiate discussion about sexual adaptations that must be made during pregnancy, but they themselves need a sound knowledge base about the physical, social, and emotional responses to sex during pregnancy. Not all maternity nurses are comfortable dealing with the sexual concerns of their clients. Be aware of your personal strengths and limitations in dealing with sexual content and be prepared to make referrals if necessary.
Many women merely need permission to be sexually active during pregnancy. Many other women, however, need to be given information about the physiologic changes that occur during pregnancy, have the myths that are associated with sex during pregnancy dispelled, and participate in open discussions of positions for intercourse that decrease pressure on the gravid abdomen. Such tasks are within the purview of the nurse and should be an integral component of the health care rendered.
Some couples need to be referred for sex therapy or family therapy. Couples with long-standing problems with sexual dysfunction that are intensified by pregnancy are candidates for sex therapy. Whenever a sexual problem is a symptom of a more serious relationship problem, the couple would benefit from family therapy.
Using the History: The couple’s sexual history provides a basis for counseling, but history taking also is an ongoing process. The couple’s receptivity to changes in attitudes, body image, partner relationships, and physical status are relevant topics throughout pregnancy. The history reveals the woman’s knowledge of female anatomy and physiology and her attitudes about sex during pregnancy, as well as her perceptions of the pregnancy, the health status of the couple, and the quality of their relationship.
Countering Misinformation: Many myths and much of the misinformation related to sex and pregnancy are masked by seemingly unrelated issues. For example, a discussion about the baby’s ability to hear and see in utero may be prompted by questions about the baby being an “unseen observer” of the couple’s lovemaking. The counselor must be extremely sensitive to the questions behind such questions when counseling in this highly charged emotional area.
Suggesting Alternative Behaviors: Research has not demonstrated that coitus and orgasm are contraindicated at any time during pregnancy for the obstetrically and medically healthy woman (Cunningham et al., 2010). However, a history of more than one miscarriage; a threatened miscarriage in the first trimester; impending miscarriage in the second trimester; and PROM, bleeding, or abdominal pain during the third trimester warrant caution when it comes to coitus and orgasm.
Solitary and mutual masturbation and oral-genital intercourse may be used by couples as alternatives to penile-vaginal intercourse. Partners who enjoy cunnilingus (oral stimulation of the clitoris or vagina) may feel “turned off” by the normal increase in the amount and odor of vaginal discharge during pregnancy. Couples who practice cunnilingus should be cautioned against the blowing of air into the vagina, particularly during the last few weeks of pregnancy when the cervix may be slightly open. An air embolism can occur if air is forced between the uterine wall and the fetal membranes and enters the maternal vascular system through the placenta.
Showing the woman or couple pictures of possible variations of coital position often is helpful (Fig. 15-19). The female-superior, side-by-side, rear-entry, and side-lying are possible alternative positions to the traditional male-superior position. The woman astride (superior position) allows her to control the angle and depth of penile penetration, as well as to protect her breasts and abdomen. The side-by-side position or any position that places less pressure on the pregnant abdomen and requires less energy may be preferred during the third trimester.
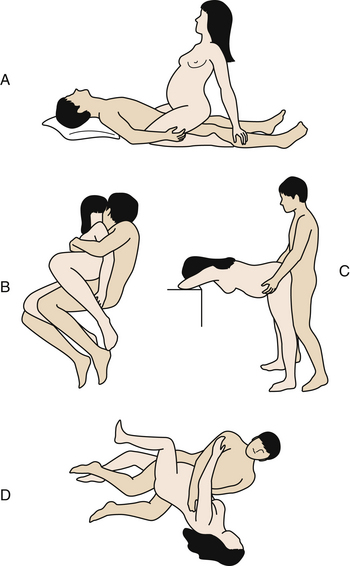
FIG. 15-19 Positions for sexual intercourse during pregnancy. A, Female superior. B, Side by side. C, Rear entry. D, Side-lying, facing each other.
Multiparous women sometimes have significant breast tenderness in the first trimester. A coital position that avoids direct pressure on the woman’s breasts and decreased breast fondling during love play can be recommended to such couples. The woman also should be reassured that this condition is normal and temporary.
Some women complain of lower abdominal cramping and backache after orgasm during the first and third trimesters. A back rub can often relieve some of the discomfort and provide a pleasant experience. A tonic uterine contraction, often lasting up to a minute, replaces the rhythmic contractions of orgasm during the third trimester. Changes in the FHR without fetal distress also have been reported.
The objective of risk-reduction measures is to provide prophylaxis against the acquisition and transmission of STIs (e.g., herpes simplex virus [HSV], HIV). Because these diseases may be transmitted to the woman and her fetus, the use of condoms is recommended throughout pregnancy if the woman is at risk for acquiring an STI.
Psychosocial Support
Esteem, affection, trust, concern, consideration of cultural and religious responses, and listening are all components of the emotional support given to the pregnant woman and her family. The woman’s satisfaction with her relationships—partner and familial—and their support, her feeling of competence, and her sense of being in control are important issues to be addressed in the third trimester. A discussion of fetal responses to stimuli, such as sound and light, as well as patterns of sleeping and waking, can be helpful. Other issues of concern that may arise for the pregnant woman and couple include fear of pain, loss of control, and possible birth of the infant before reaching the hospital; anxieties about parenthood; parental concerns about the safety of the mother and unborn child; siblings and their acceptance of the new baby; social and economic responsibilities; and parental concerns arising from conflicts in cultural, religious, or personal value systems. In addition, the father’s or partner’s commitment to the pregnancy and to the couple’s relationship and concerns about sexuality and its expression are topics for discussion for many couples. Providing the prospective parents with an opportunity to discuss their concerns and validating the normality of their responses can meet their needs to varying degrees. Anticipatory guidance and health promotion strategies can help partners cope with their concerns. Health care providers can stimulate and encourage open dialogue between the expectant mother and her partner.
Variations in Prenatal Care
The course of prenatal care described thus far may seem to suggest that the experiences of childbearing women are similar and that nursing interventions are uniformly consistent across all populations. Although typical patterns of response to pregnancy are easily recognized and many aspects of prenatal care indeed are consistent, pregnant women enter the health care system with individual concerns and needs. The nurse’s ability to assess unique needs and to tailor interventions to the individual is the hallmark of expertise in providing care. Variations that influence prenatal care include culture, age, and number of fetuses.
Cultural Influences
Prenatal care as we know it is a phenomenon of Western medicine. In the U.S. biomedical model of care, women are encouraged to seek prenatal care as early as possible in their pregnancy by visiting a physician and/or a nurse-midwife. This model not only is unfamiliar but also seems strange to women of other cultures.
Many cultural variations are found in prenatal care. Even if the prenatal care described is familiar to a woman, some practices may conflict with the beliefs and practices of a subculture group to which she belongs. Because of these and other factors, such as lack of money, lack of transportation, and language barriers, women from diverse cultures may not participate in the prenatal care system, for instance by keeping prenatal appointments. Such behavior may be misinterpreted by nurses as uncaring, lazy, or ignorant.
A concern for modesty also is a deterrent to many women seeking prenatal care. For some women, exposing body parts, especially to a man, is considered a major violation of their modesty. For many women, invasive procedures, such as a vaginal examination, may be so threatening that they cannot be discussed even with their own husbands; therefore, many women prefer a female health care provider. Too often, health care providers assume women lose this modesty during pregnancy and labor, but actually most women value and appreciate efforts to maintain their modesty.
For many cultural groups a physician is deemed appropriate only in times of illness. Because pregnancy is considered a normal process and the woman is in a state of health, the services of a physician are considered inappropriate. Even if what are considered problems with pregnancy by standards of Western medicine develop, they may not be perceived as problems by members of other cultural groups.
Although pregnancy is considered normal by many, certain practices are expected of women of all cultures to ensure a good outcome. Cultural prescriptions tell women what to do, and cultural proscriptions establish taboos. The purposes of these practices are to prevent maternal illness resulting from a pregnancy-induced imbalanced state and to protect the vulnerable fetus. Prescriptions and proscriptions regulate the woman’s emotional response, clothing, activity and rest, sexual activity, and dietary practices. Exploration of the woman’s beliefs, perceptions of the meaning of childbearing, and health care practices may help health care providers foster her self-actualization, promote attainment of the maternal role, and positively influence her relationship with her partner.
To provide culturally responsive care, nurses must be knowledgeable about practices and customs, although it is not possible to know all there is to know about every culture and subculture or the many lifestyles that exist. It is important to learn about the varied cultures in the community where you practice (Cooper, Grywalski, Lamp, Newhouse, & Studlien, 2007). When exploring cultural beliefs and practices related to childbearing, the nurse can support and nurture those beliefs that promote physical or emotional adaptation. However, if you identify potentially harmful beliefs or activities, provide education and propose modifications.
Emotional Response
Virtually all cultures emphasize the importance of maintaining a socially harmonious and agreeable environment for a pregnant woman. A lifestyle with minimal stress is important in ensuring a successful outcome for the mother and baby. Harmony with other people must be fostered, and visits from extended family members may be required to demonstrate pleasant and noncontroversial relationships. If discord exists in a relationship, it is usually dealt with in culturally prescribed ways.
Besides proscriptions regarding food, other proscriptions involve forms of magic. For example, some Mexicans believe that pregnant women should not witness an eclipse of the moon because it may cause a cleft palate in the infant. They also believe that exposure to an earthquake may precipitate preterm birth, miscarriage, or even a breech presentation. In some cultures a pregnant woman must not ridicule someone with an affliction for fear her child might be born with the same handicap. A mother should not hate a person lest her child resemble that person, and dental work should not be done because it may cause a baby to have a “harelip.” A widely held folk belief in some cultures is that the pregnant woman should refrain from raising her arms above her head, because such movement ties knots in the umbilical cord and may cause it to wrap around the baby’s neck. Another belief is that placing a knife under the bed of a laboring woman will “cut” her pain.
Clothing
Although most cultural groups do not prescribe specific clothing to be worn during pregnancy, modesty is an expectation of many. Some Mexican women of the Southwest and women of Central America wear a cord beneath the breasts and knotted over the umbilicus. This cord, called a muñeco, is thought to prevent morning sickness and ensure a safe birth (Fig. 15-20). Amulets, medals, and beads also may be worn to ward off evil spirits.
Physical Activity and Rest
Norms that regulate the physical activity of mothers during pregnancy vary tremendously. Many groups, including Native Americans and some Asian groups, encourage women to be active, to walk, and to engage in normal, although not strenuous, activities to ensure that the baby is healthy and not too large. Conversely, other groups such as Filipinos believe that any activity is dangerous, and others willingly take over the work of the pregnant woman. Some Filipinos believe that this inactivity protects the mother and child. The mother is encouraged simply to produce the succeeding generation. If health care providers do not know of this belief, they could misinterpret this behavior as laziness or nonadherence with the desired prenatal health care regimen. It is important for the nurse to find out the way each pregnant woman views activity and rest.
Sexual Activity
In most cultures sexual activity is not prohibited until the end of pregnancy. Some Hispanics view sexual activity as necessary to keep the birth canal lubricated. Conversely, some Vietnamese may have definite proscriptions against sexual intercourse, requiring abstinence throughout the pregnancy because it is thought that sexual intercourse may harm the mother and fetus.
Diet
Nutritional information given by Western health care providers also may be a source of conflict for many cultural groups. Such a conflict commonly is not known by health care providers unless they understand the dietary beliefs and practices of the people for whom they are caring. For example, Muslims have strict regulations regarding preparation of food, and if meat cannot be prepared as prescribed, they may omit meats from their diets. Many cultures permit pregnant women to eat only warm foods.
Age Differences
The age of the childbearing couple may have a significant influence on their physical and psychosocial adaptation to pregnancy. Normal developmental processes that occur in both very young and older mothers are interrupted by pregnancy and require a different type of adaptation to pregnancy than that of the woman of typical childbearing age. Although the individuality of each pregnant woman is recognized, special needs of expectant mothers 15 years of age or younger or those 35 years of age or older are summarized.
Adolescents
Teenage pregnancy is a worldwide problem. About 1 million adolescent females in the United States, or 4 out of every 10 girls, become pregnant each year. Most of the pregnancies are unintended. Adolescents are responsible for almost 450,000 births in the United States annually. Hispanic adolescents currently have the highest birth rate, although the rate for African-American adolescents also is high (Heron et al., 2010). Most of these young women are unmarried, and many are not ready for the emotional, psychosocial, and financial responsibilities of parenthood.
Numerous adolescent pregnancy-prevention programs have had varying degrees of success. Characteristics of programs that make a difference are those that have sustained commitment to adolescents over a long time, involve the parents and other adults in the community, promote abstinence and personal responsibility, and assist adolescents to develop a clear strategy for reaching future goals such as a college education or a career.
When adolescents do become pregnant and decide to give birth, they are much less likely than older women to receive adequate prenatal care, with many receiving no care at all. These young women also are more likely to smoke and less likely to gain adequate weight during pregnancy. As a result of these and other factors, babies born to adolescents are at greatly increased risk of LBW, of serious and long-term disability, and of dying during the first year of life (Chedraui, 2008).
Delayed entry into prenatal care may be the result of late recognition of pregnancy, denial of pregnancy, or confusion about the available services. Such a delay in care may leave an inadequate time before birth to attend to correctable problems. The very young pregnant adolescent is at higher risk for each of the variables associated with poor pregnancy outcomes (e.g., socioeconomic factors) and for those conditions associated with a first pregnancy regardless of age (e.g., gestational hypertension). The role of the nurse in reducing the risks and consequences of adolescent pregnancy is very important as adolescents often see the nurse as trustworthy and someone who will keep their confidence as well as provide them with accurate information. Therefore, effective communication is essential in providing care to the pregnant adolescent (King-Jones, 2008) (Fig. 15-21) (see Nursing Care Plan: Adolescent Pregnancy).
Women Older Than 35 Years
Two groups of older parents have emerged in the population of women having a child late in their childbearing years. One group consists of women who have many children or who have an additional child during the menopausal period. The other group consists of women who have deliberately delayed childbearing until their late 30s or early 40s.
Multiparous Women: Multiparous women may have never used contraceptives because of personal choice or lack of knowledge concerning contraceptives. They also may be women who have used contraceptives successfully during the childbearing years, but as menopause approaches they may cease menstruating regularly or stop using contraceptives and consequently become pregnant. The older multiparous woman may feel that pregnancy separates her from her peer group and that her age
is a hindrance to close associations with young mothers. Other parents welcome the unexpected infant as evidence of continuing maternal and paternal roles.
Primiparous Women: The number of first-time pregnancies in women between the ages of 35 and 40 years has increased significantly over the past three decades (Heron et al., 2010). Seeing women in their late 30s or 40s during their first pregnancy is no longer unusual for health care providers. Reasons for delaying pregnancy include a desire to obtain advanced education, career priorities, and use of better contraceptive measures. Women who are infertile do not delay pregnancy deliberately but may become pregnant at a later age as a result of fertility studies and therapies.
These women choose parenthood. They often are successfully established in a career and a lifestyle with a partner that includes time for self-attention, the establishment of a home with accumulated possessions, and freedom to travel. When asked the reason they chose pregnancy later in life, many reply, “Because time is running out.”
The dilemma of choice includes the recognition that being a parent will have positive and negative consequences. Couples should discuss the consequences of childbearing and childrearing before committing themselves to this lifelong venture. Partners in this group seem to share the preparation for parenthood, planning for a family-centered birth, and desire to be loving and competent parents; however, the reality of child care may prove difficult for such parents.
First-time mothers older than 35 years select the “right time” for pregnancy; this time is influenced by their awareness of the increasing possibility of infertility or of genetic defects in the infants of older women. Such women seek information about pregnancy from books, friends, and electronic resources. They actively try to prevent fetal disorders and are careful in searching for the best possible maternity care. They identify sources of stress in their lives. They have concerns about having enough energy and stamina to meet the demands of parenting and their new roles and relationships.
If older women become pregnant after treatment for infertility, they may suddenly have negative or ambivalent feelings about the pregnancy. They may experience a multifetal pregnancy that may create emotional and physical problems. Adjusting to parenting two or more infants requires adaptability and additional resources.
During pregnancy parents explore the possibilities and responsibilities of changing identities and new roles. They must prepare a safe and nurturing environment during pregnancy and after birth. They must integrate the child into an established family system and negotiate new roles (parent roles, sibling roles, grandparent roles) for family members.
Adverse perinatal outcomes are more common in older primiparas than in younger women, even when they receive good prenatal care. Suplee and associates (2007) reported that women ages 35 years and older are more likely than are younger primiparas to have LBW infants, premature birth, and multiple births. The occurrence of these complications is quite stressful for the new parents, and nursing interventions that provide information and psychosocial support are needed, as well as care for physical needs. In addition, in women ages 35 years or older there is an increased risk of maternal mortality. Pregnancy-related deaths are from hemorrhage, infection, embolisms, hypertensive disorders of pregnancy, cardiomyopathy, and strokes (Johnson et al., 2007).
Multifetal Pregnancy
When the pregnancy involves more than one fetus, both the mother and fetuses are at increased risk for adverse outcomes. The maternal blood volume is increased, resulting in an increased strain on the maternal cardiovascular system. Anemia often develops because of a greater demand for iron by the fetuses. Marked uterine distention and increased pressure on the adjacent viscera and pelvic vasculature and diastasis of the two rectus abdominis muscles (see Fig. 13-13) may occur. Placenta previa develops more commonly in multifetal pregnancies because of the large size or placement of the placentas (Gilbert, 2011). Premature separation of the placenta may occur before the second and any subsequent fetuses are born.
Twin pregnancies often end in prematurity. Spontaneous rupture of membranes before term is common. Congenital malformations are twice as common in monozygotic twins as in singletons, although there is no increase in the incidence of congenital anomalies in dizygotic twins. In addition, two-vessel cords—that is, cords with a vein and a single umbilical artery instead of two—occur more often in twins than in singletons, but this abnormality is most common in monozygotic twins. The clinical diagnosis of multifetal pregnancy is accurate in about 90% of cases. The likelihood of a multifetal pregnancy is increased if any one or a combination of the following factors is noted during a careful assessment:
• History of dizygotic twins in the female lineage
• More rapid uterine growth for the number of weeks of gestation
• Palpation of more than the expected number of small or large parts
• Asynchronous fetal heartbeats or more than one fetal electrocardiographic tracing
The diagnosis of multifetal pregnancy can come as a shock to many expectant parents, and they may need additional support and education to help them cope with the changes they face. The mother needs nutrition counseling so that she gains more weight than that needed for a singleton birth, counseling that maternal adaptations will probably be more uncomfortable, and information about the possibility of a preterm birth.
If the presence of more than three fetuses is diagnosed, the parents may receive counseling regarding selective reduction to reduce the incidence of premature birth and improve the opportunities for the remaining fetuses to grow to term gestation (Cleary-Goldman, Chitkara, & Berkowitz, 2007). This situation may pose an ethical dilemma for many couples, especially those who have worked hard to overcome problems with infertility and have strong values regarding right to life. Initiating a discussion to identify what resources could help the couple (e.g., a minister, priest, or mental health counselor) to make the decision is important because the decision-making process and the procedure itself may be stressful. Most women will have feelings of guilt, anger, and sadness but most will come to terms with the loss and will bond with the remaining fetus or fetuses (Cleary-Goldman, et al.).
The prenatal care given women with multifetal pregnancies includes changes in the pattern of care and modifications in other aspects such as the amount of weight gained and the nutritional intake necessary. The prenatal visits of these women are scheduled at least every 2 weeks in the second trimester and weekly thereafter. Ultrasound evaluations are scheduled at 18 to 20 weeks and then every 3 to 4 weeks to monitor the fetal growth and amniotic fluid volume (Cleary-Goldman, et al., 2007). In twin gestations the recommended weight gain is 16 to 20 kg. Iron and vitamin supplementation is desirable. As the risk for preeclampsia and eclampsia increases in multifetal pregnancies, nurses aggressively work to identify and treat these complications of pregnancy.
The considerable uterine distention involved can cause the backache commonly experienced by pregnant women to be even worse. Maternal support hose may be worn to control leg varicosities. If risk factors such as premature dilation of the cervix or bleeding are present, abstinence from orgasm and nipple stimulation during the last trimester is recommended to help avert preterm labor. Frequent ultrasound examinations, nonstress tests, and FHR monitoring will be performed. Some practitioners recommend bed rest beginning at 20 weeks in women carrying multiple fetuses to prevent preterm labor. Other practitioners question the value of prolonged bed rest. If bed rest is recommended, the mother assumes a lateral position to promote increased placental perfusion. If birth is delayed until after the thirty-sixth week, the risk of morbidity and mortality decreases for the neonates.
Multiple newborns will likely place a strain on finances, space, workload, and the woman’s and family’s coping capability. Lifestyle changes may be necessary. Parents will need assistance in making realistic plans for the care of the babies (e.g., whether to breastfeed and whether to raise them as “alike” or as separate persons). Parents should be referred to national organizations such as Parents of Twins and Triplets (www.potatonet.org), Mothers of Twins (www.nomotc.org), and the La Leche League (www.lalecheleague.org) for further support.
Childbirth and Perinatal Education
The goal of childbirth and perinatal education is to assist individuals and their family members to make informed, safe decisions about pregnancy, birth, and early parenthood. It also is to assist them to comprehend the long-lasting potential that empowering birth experiences have in the lives of women and that early experiences have on the development of children and the family. The perinatal education program is an expansion of the earlier childbirth education movement that originally offered a set of classes in the third trimester of pregnancy to prepare parents for birth. Today perinatal education programs consist of a menu of class series and activities from preconception through the early months of parenting.
Health-promoting education should be provided in a context that emphasizes how a healthy body is best able to adapt to the changes that accompany pregnancy. Without this context of health, routine care and testing for risks may contribute to a mindset of families that pregnancy is a pathologic as opposed to a healthy mind-body-spirit event.
Some of the decisions the childbearing family must consider are the decision to have a baby, followed by choices of a care provider and type of care (a midwifery model [natural oriented] versus a medical [intervention oriented] model); the place for birth (hospital, birthing center, home); and the type of infant feeding (breast or bottle) and infant care. If a woman has had a cesarean birth, she may consider having a vaginal birth. Perinatal education can provide information to help childbearing families make informed decisions about these issues.
Previous pregnancy and childbirth experiences are important elements that influence current learning needs. The woman’s (and support person’s) age, cultural background, personal philosophy with regard to childbirth, socioeconomic status, spiritual beliefs, and learning styles are assessed to develop the best plan to help the woman meet her needs.
For the most part, the pregnant woman and her partner attend childbirth education classes, although sometimes a friend, teenage daughter, or parent is the designated support person (Fig. 15-22). There are also classes for grandparents and siblings to prepare them for their attendance at birth and/or the arrival of the baby. Siblings often see a film about birth and learn ways they can help welcome the baby. They also learn to cope with changes that include a reduction in parental time and attention. Grandparents learn about current child care practices and how to help their adult children adapt to parenting in a supportive way.
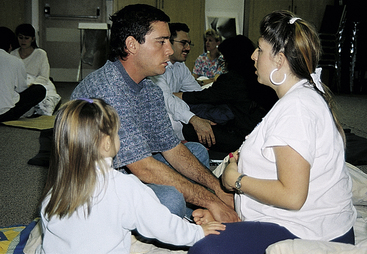
FIG. 15-22 Learning relaxation exercises with the whole family. (Courtesy Marjorie Pyle, RNC, Lifecircle, Costa Mesa, CA.)
Childbirth Education Programs
Childbirth, when one is prepared and well supported, presents to women a unique and powerful opportunity to find their core strength in a manner that forever changes their self-perception. Expectant parents and their families have different interests and information needs as the pregnancy progresses.
Early pregnancy (“early bird”) classes provide fundamental information. Classes are developed around the following areas: (1) early fetal development, (2) physiologic and emotional changes of pregnancy, (3) human sexuality, and (4) the nutritional needs of the mother and fetus. The classes often address environmental and workplace hazards. Exercises, nutrition, warning signs, drugs, and self-medication also are topics of interest and concern.
Mid-pregnancy classes emphasize the woman’s participation in self-management. Classes provide information on preparation for breastfeeding and formula feeding, infant care, basic hygiene, common complaints and simple safe remedies, infant health, parenting, and updating and refining the birth plans.
Late pregnancy classes emphasize labor and birth. There are different methods of coping with labor and birth and these are often the basis for various prenatal classes. These include Lamaze, Bradley, and Dick-Read. These classes usually include a hospital tour.
Current Practices in Childbirth Education
A variety of approaches to childbirth education have evolved as childbirth educators attempt to meet learning needs. In addition to classes designed specifically for pregnant adolescents, their partners, and/or parents, classes exist for other groups with special learning needs. These include classes for first-time mothers older than age 35, single women, adoptive parents, and parents of multiples or women with handicaps such as those who are visually impaired or deaf. Refresher classes for parents with children not only review coping techniques for labor and birth but also help couples prepare for sibling reactions and adjustments to a new baby. Cesarean birth classes are available for couples who have this kind of birth scheduled because of breech presentation or other risk factors. Other classes focus on vaginal birth after cesarean (VBAC) because many women can successfully give birth vaginally after previous cesarean birth.
Throughout the series of classes there is discussion of support systems that people can use during pregnancy and after birth. Such support systems help parents function independently and effectively. During all the classes the open expression of feelings and concerns about any aspect of pregnancy, birth, and parenting is welcomed.
Pain Management
Fear of pain in labor is a key issue and the reason many women give for attending childbirth education classes. Numerous studies show that women who have received childbirth preparation later report no less pain but do report greater ability to cope with the pain during labor and birth and more birth satisfaction than unprepared women. Therefore, although pain management strategies are an essential component of childbirth education, total pain eradication is not the primary source of birth satisfaction or a goal. Eliminating suffering is a realistic goal. Control in childbirth, meaning participation in decision making, has repeatedly been the primary source of birth satisfaction.
Couples need information about the advantages and disadvantages of pain medication and about other techniques for coping with labor. An emphasis on nonpharmacologic pain management strategies helps couples manage the labor and birth with dignity and increased comfort. Most instructors teach a flexible approach, which helps couples learn and master many techniques to use during labor (see Chapter 17 for further discussion).
Perinatal Care Choices
Often the first decision the woman makes is who will be her primary health care provider for the pregnancy and birth. This decision is doubly important because it usually affects where the birth will take place. The nurse can provide information about the different types of health care providers and what kind of care to expect from each type.
The Coalition to Improve Maternity Services (CIMS, 2000), a group of more than 50 nursing and maternity care–oriented organizations, produced a document to assist women in selecting their perinatal care. After some explanation of choices, encourage women to ask potential care providers the following questions:
• Who can be with me during labor and birth?
• What happens during a normal labor and birth in your setting?
• How do you allow for differences in culture and beliefs?
• May I walk and move around during labor? What position do you suggest for birth?
• How do you make sure everything goes smoothly when my nurse, doctor, nurse-midwife, or agency works with one another?
• What things do you normally do to a woman in labor?
• How do you help mothers stay as comfortable as they can be? Besides drugs, how do you help mothers relieve the pain of labor?
Physicians
Physicians (obstetricians, family medicine physicians) attend 91.6% of births in the United States and Canada (Heron et al., 2010). They see low and high risk clients. Care often includes pharmacologic and medical management of problems as well as use of technologic procedures. Family medicine physicians may need backup by obstetricians if a specialist is needed for a problem (e.g., a cesarean birth). Most physicians manage births in a hospital setting.
Nurse-Midwives
Most midwives are certified nurse midwives (CNMs). They provide care for more than 8% of the births in the United States and Canada (Martin, Hamilton, Sutton, Ventura, Menacker, Kirmeyer, et al., 2009). They usually see low risk obstetric clients. Care is often noninterventionist, and they often encourage the woman and her family to be active participants in the care. Nurse-midwives refer patients to physicians for complications. Most births (about 94%) are managed in hospital settings or alternative birth centers; a small number are managed in a home setting.
Direct-Entry Midwives
Direct-entry midwives and independent (lay) midwives manage slightly less than 1% of births in the United States; most are in the home setting.
Doulas
A doula is professionally trained to provide labor support, including physical, emotional, and informational support to women and their partners during labor and birth. The doula does not become involved with clinical tasks (Doulas of North America [DONA], 2008). Today many couples, no matter which type of childbirth classes they take, also employ a doula for labor support.
A Cochrane synopsis of 16 trials involving 13,391 women found that “continuous labor support like that provided by doulas reduces a woman’s likelihood of having pain medication, increases her satisfaction and chances for spontaneous birth, and has no known risks” (Hodnett, Gates, Hofmeyr, & Sakala, 2007).
A doula typically meets with the woman and her husband or partner before labor. At this meeting she ascertains the woman’s expectations and desires for the birth experience. With this information as her guide during labor and birth, the doula focuses her efforts on assisting the woman to achieve her goals. Doulas work collaboratively with other health care providers and the husband or other supportive individuals, but their primary goal is to assist the woman.
Doulas may be found through community contacts, other health care providers, or childbirth educators; a number of organizations offer information or referral services. It is important that the expectant mother be comfortable with the doula who will be attending her. See Box 15-7 for a list of questions to ask when arranging for a doula. Doulas of North America (DONA) is an organization that certifies doulas (www.dona.org). Although the doula role originally developed as an assistant during labor, some women benefit from assistance during the postpartum period. There are small but growing numbers of postnatal doulas who provide assistance to the new mother as she develops competence with infant care, feeding, and other maternal tasks.
Birth Plans
Once the maternity care provider is chosen, there are numerous other decisions to be made over the course of the perinatal year. Many prenatal care providers and childbirth educators encourage expectant parents to develop a birth plan to identify their options and set priorities. The birth plan is a tool with which parents can explore their childbirth options and choose those that are most important to them. The plan must be viewed as tentative because the realities of what is feasible may change as the actual labor and birth unfold. It is understood to be a preference list based on a best case scenario (see Chapter 19).
Birth Setting Choices
With careful thought, the concept of natural or family- or woman-centered maternity care can be implemented in any setting. The three primary options for birth settings are the hospital, birth center, and home. Women consider several factors in choosing a setting for childbirth, including the preference of their health care provider, characteristics of the birthing unit, and preference of their third-party payer. Approximately 99% of all births in the United States take place in a hospital setting (Martin et al., 2009). However, the types of labor and birth services vary greatly, from the traditional labor and delivery rooms with separate postpartum and newborn units, to in-hospital birthing centers, where all or almost all care takes place in a single unit.
Labor, Delivery, Recovery, Postpartum (Birthing) Rooms
Labor, delivery, and recovery (LDR), and labor, delivery, recovery, and postpartum (LDRP) rooms offer families a comfortable, private space for childbirth (Fig. 15-23). Women are admitted to LDR units, labor and give birth, and spend the first 1 to 2 hours postpartum there for immediate recovery and to have time with their families to bond with their newborns. After this period of recovery, the mothers and newborns move to a postpartum unit and nursery or mother-baby unit for the duration of their stay.
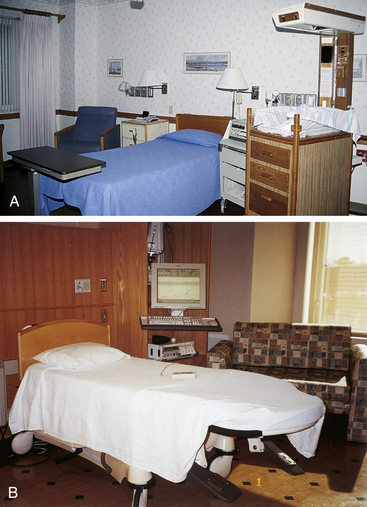
FIG. 15-23 A, Labor, delivery, and recovery (LDR) unit. B, Labor, delivery, recovery, and postpartum (LDRP) unit. Note sofa in background that converts to a bed. (A, Courtesy Julie Perry Nelson, Loveland, CO; B, Courtesy Dee Lowdermilk, Chapel Hill, NC.)
In LDRP units, the same nursing staff usually provides total care from admission through postpartum discharge. The woman and her family may stay in this unit for 6 to 48 hours after giving birth. The units are furnished to provide a homelike atmosphere, as LDR units are, but have accommodations for family members to stay overnight.
Both units have fetal monitors, emergency resuscitation equipment for mother and newborn, and heated cribs or warming units for the newborn. Often this equipment is out of sight in cabinets or closets when it is not being used.
Birth Centers
Free-standing birth centers are usually built in locations separate from the hospital but are often located nearby in case transfer of the woman or newborn is needed. These birth centers offer families a safe and cost-effective alternative to hospital or home birth. About one fourth of the 1% of out-of-hospital births are in birthing centers (Martin et al., 2009). The centers are usually staffed by nurse-midwives or physicians who also have privileges at the local hospital. Only women at low risk for complications are included for care. Attendance at childbirth and parenting classes is required of all clients. The family is admitted to the birth center for labor and birth and will remain there until discharge, which often takes place within 6 hours of the birth.
Birth centers typically have homelike accommodations, including a double bed for the couple and a crib for the newborn (Fig. 15-24). Emergency equipment and drugs are usually in cabinets, out of view but easily accessible. Private bathroom facilities are incorporated into each birth unit. There may be an early labor lounge or a living room and small kitchen.
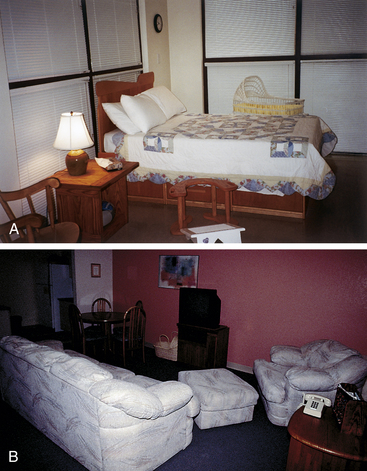
FIG. 15-24 Birth center. A, Note double bed, baby crib, and birthing stool. B, Lounge and kitchen. (A, Courtesy Dee Lowdermilk, Chapel Hill, NC. Photo location: The Women’s Birth and Wellness Center, Chapel Hill, NC; B, Courtesy Michael S. Clement, MD, Mesa, AZ. Photo location: Bethany Birth Center, Phoenix, AZ.)
Services provided by the free-standing birth centers include those necessary for safe management during the childbearing cycle. Clients must understand that some situations require transfer to a hospital, and they must agree to abide by those guidelines.
Birth centers as well as a hospital with a comprehensive birthing program may have resources for parents such as a lending library that includes books and videotapes; reference files on related topics; recycled maternity clothes, baby clothes, and equipment; and supplies and reference materials for childbirth educators. The centers may also have referral files for community resources that offer services relating to childbirth and early parenting, including support groups (e.g., for single parents, for postbirth support, and for parents of twins), genetic counseling, women’s issues, and consumer action.
A birth center should be located close to a major hospital so that quick transfer to that institution is possible if necessary for the birth. Ambulance service and emergency procedures must be readily available. Fees vary with the services provided by birthing centers but typically are less than or equal to those charged by local hospitals. Some base fees on the ability of the family to pay (a reduced-fee sliding scale). Several third-party payers, as well as Medicaid and the Civilian Health and Medical Programs of the Uniformed Services (TRICARE/CHAMPUS), recognize and reimburse these centers.
Home Birth
Home birth has always been popular in certain countries, such as Sweden and The Netherlands. In developing countries, hospitals or adequate lying-in facilities often are unavailable to most pregnant women, and home birth is a necessity. In North America home births account for about two thirds of the less than 1% of births outside the hospital setting (Martin et al., 2009).
Although home births are considered countercultural by many in the United States, there is no evidence base to discourage low risk couples who desire a carefully planned out-of-the-hospital birth (Johnson & Daviss, 2005). National groups supporting home birth are the Home Oriented Maternity Experience (HOME) and the National Association of Parents for Safe Alternatives in Childbirth (NAPSAC). These groups work to foster more humane childbearing practices at all levels, integrating the alternatives for childbirth to meet the needs of the total population.
One advantage of home birth is that the family is in control of the experience. Another is that the birth may be more physiologically normal in familiar surroundings. The mother may be more relaxed than she would be in the hospital environment. Care providers who participate in home births tend to be more support oriented and less intervention oriented. The family can assist in and be a part of the happy event, and contact with the newborn is immediate and sustained. In addition, home birth may be less expensive than a hospital confinement. Serious infection may be less likely, assuming strict aseptic principles are followed, because people generally are relatively immune to their own home bacteria.
KEY POINTS
• The prenatal period is a preparatory one both physically, in terms of fetal growth and parental adaptations, and psychologically, in terms of anticipation of parenthood.
• Pregnancy affects parent-child, sibling-child, and grandparent-child relationships.
• Discomforts and changes of pregnancy can cause anxiety to the woman and her family and require sensitive attention and a plan for teaching self-management measures.
• Education about healthy ways of using the body (e.g., exercise, body mechanics) is essential given maternal anatomic and physiologic responses to pregnancy.
• Important components of the initial prenatal visit include detailed and carefully recorded findings from the interview, a comprehensive physical examination, and selected laboratory tests.
• Follow-up visits are shorter than the initial visit and are important for monitoring the health of the mother and fetus and providing anticipatory guidance as needed.
• Even in normal pregnancy the nurse must remain alert to hazards such as supine hypotension, signs and symptoms of potential complications, and signs of family maladaptations.
• Blood pressure is evaluated based on absolute values and length of gestation and interpreted in light of modifying factors.
• Each pregnant woman needs to know how to recognize and report signs of potential complications such as preterm labor.
• The likelihood of physical abuse increases during pregnancy.
• Culture, age, parity, and multiple pregnancy can have a significant effect on the course and outcome of the pregnancy.
• Nurses must be knowledgeable about practices and customs related to childbearing to provide culturally sensitive care.
• Childbirth education teaches tuning in to the body’s inner wisdom and coping strategies that enhance women’s ability to know how to give birth.
• Childbirth education strives to promote healthier pregnancies and family lifestyles.
![]() Audio Chapter Summaries Access an audio summary of these Key Points on
Audio Chapter Summaries Access an audio summary of these Key Points on ![]()