Chapter 41The Hind Foot and Pastern
The contribution of the hind foot and pastern to hindlimb lameness is considerably less important than that of the digit to forelimb lameness. Extensive information regarding lameness of the foot and pastern in the forelimb is found in Chapter 26Chapter 27Chapter 28Chapter 29Chapter 30Chapter 31Chapter 32Chapter 33Chapter 34Chapter 35Chapter 82. This information is directly applicable to the hindlimb. During lameness examination, the hind foot and pastern are easily overlooked because they are in a potentially dangerous place to examine. Other regions of the hindlimb have been presumed to be more important, and, historically, little has been taught about the distal part of the limb. Without a commitment to performing diagnostic analgesic techniques in the distal aspect of the hindlimb, there is little way to discover whether the digit is the authentic source of pain unless the problem is severe or obvious. Subtle primary or compensatory lameness problems of this region are likely to go unnoticed daily. However, in certain sports horses, such as the draft horse, lameness of the hind foot and pastern is so common that this region cannot be overlooked. I am curious as to why infectious osteitis of the distal phalanx is more common in the hind feet. Of 26 affected limbs in 21 lame foals with infectious osteitis of the distal phalanx, most likely hematogenous in origin, 18 (69%) were hindlimbs.1 Infectious arthritis in foals occurs more commonly in hindlimb joints, specifically the femoropatellar and tarsocrural joints, than in forelimb joints, a finding that is equally difficult to explain.2
Anatomy and Innervation of the Hind Foot and Pastern
The bones are essentially the same as in the forelimb. The hind distal phalanx is narrower compared with the forelimb and has a steeper dorsal angle. The plantar surface is more concave, and the plantar processes are closer together.1 In external appearance, the hind foot usually is more upright than the fore foot, but abnormal wear and shoeing practices can produce a common pathological condition of a low, underrun heel (see Chapter 6). The hind middle phalanx is narrower and longer, and the hind proximal phalanx is slightly shorter than the corresponding bones in the forelimb.3 The ligaments, tendons, digital flexor tendon sheath (DFTS), and distal interphalangeal and proximal interphalangeal joints are the same as in the forelimb. Innervation of the foot is derived primarily from the medial and lateral plantar nerves, which originate from the tibial nerve (see Chapter 10). The medial and lateral plantar metatarsal nerves, which originate from the deep branch of the lateral plantar nerve, become superficial just distal to the “bell” of the second and fourth metatarsal bones. Unlike the palmar metacarpal nerves, the hindlimb medial and lateral plantar metatarsal nerves supply sensation to the pastern region and coronary band, a fact that can complicate interpretation of perineural analgesia in the hind digit.4
Examination, Clinical Signs, and Diagnosis
The clinical examination of the hind foot and pastern was described in Chapter 6, and a detailed description of the clinical investigation of the foot and shoeing is found in Chapter 27Chapter 28Chapter 30Chapter 31Chapter 32Chapter 33Chapter 34. A conscientious effort must be made during every lameness examination to evaluate the hind foot with the limb in both the standing and flexed positions. The type of shoeing and shoe wear are important in understanding potential lameness conditions of the foot, but perhaps more important, study of hind foot balance and shoeing can provide important clues in the diagnosis of lameness located more proximally in the limb. Dramatic abnormalities in balance and shoe additives, such as calks, grabs, trailers, and bars, can place added forces of shear and torsion on hindlimb bones and joints. Therapeutic recommendations cannot be made unless the clinician is aware of the type of shoes that are currently in place. Hoof imbalance has not been studied extensively in the hindlimb, but dorsal to plantar and medial to lateral hoof imbalance is a likely contributor to lameness in the proximal interphalangeal and metatarsophalangeal joints. Palpation for signs of inflammation, such as increased digital pulse amplitude, heat, swelling, and pain, must be performed but can be difficult in fractious horses. Palpation is difficult in the hindlimb because of the stay apparatus, which causes the digit to flex involuntarily. Palpation of the plantar pastern soft tissue structures is difficult, and subtle swelling and pain associated with the distal sesamoidean ligaments or other structures can be easily overlooked. In draft horses, signs of inflammation can be obscure (Figure 41-1). Examination with hoof testers is important, but normally horses show considerable sensitivity across the heel (see Chapter 6). Because the foot is incorporated in the rigid hoof capsule and swelling may not be apparent, even severe lameness conditions, such as abscesses or fractures, can go unnoticed. Commonly lameness of the hind foot is misinterpreted as originating high up in the limb, because clinical signs are not prominent and are easy to overlook.

Fig. 41-1 The defect in the coronary band of this draft horse was not detected until the long hair (or feathers) was shaved. Hoof tester examination yielded negative findings, but investigation of the foot was prompted by a positive response to perineural analgesia.
Degree of lameness varies greatly. Most recognized problems of the hind foot cause obvious, often severe lameness, but occasionally subtle or insidious problems occur. Horses with the most common problems, such as a hoof abscess and penetrating wounds, may not bear weight. If they are bearing weight, horses usually are severely lame at the trot. Horses with severe hind foot lameness, particularly of the toe region, may walk with a shortened caudal phase of the stride, similar to horses with pain in the coxofemoral region (see Chapter 7). Horses with most lameness conditions typically have a shortened cranial phase of the stride at both the walk and trot. Observing a paradoxical shortened caudal phase of the stride at the walk and the more typically seen shortened cranial phase of the stride at the trot can be an indication of hind foot pain. The horse may bear weight only on the toe. Turning may accentuate pain. At the trot, horses with hind foot and pastern lameness travel like horses with pain that originates anywhere distal to the distal aspect of the crus, and no typical alteration in limb flight is observed. When the horse is viewed from behind, limb flight is characterized by moving the foot straight ahead or slightly medial to the line of expected limb flight and then stabbing laterally during the later portion of the stride, just before impact.
Lameness associated with many conditions in this region worsens with a lower limb flexion test. Horses with osteoarthritis of the distal interphalangeal and proximal interphalangeal joints or tenosynovitis of the DFTS and tendonitis of the deep digital flexor tendon (DDFT) respond prominently. In general, hindlimb flexion tests have low specificity, and in horses that respond markedly to lower limb flexion, a source of pain located more proximal in the limb cannot be dismissed without using diagnostic analgesia.
Lameness must be localized using perineural or intraarticular analgesic techniques. Differentiation of sources of pain in the hind foot and pastern can be problematic because the same difficulties in interpretation of plantar digital and distal interphalangeal analgesic techniques occur as in the forelimb. When the plantar digital block is done with the limb elevated, it is difficult to inject local anesthetic solution just above the cartilages of the foot, so this block is usually performed in a more proximal location than in the forelimb. It may be difficult to remove all pain in horses with severe lameness. Pain associated with the proximal aspect of the proximal phalanx, such as from midsagittal fractures, or from other causes of pain in the metatarsophalangeal joint can easily be removed inadvertently during performance of plantar digital analgesia.5 Careful interpretation of analgesic techniques is necessary, particularly in racehorses, in which metatarsophalangeal joint region lameness is common (Figure 41-2).
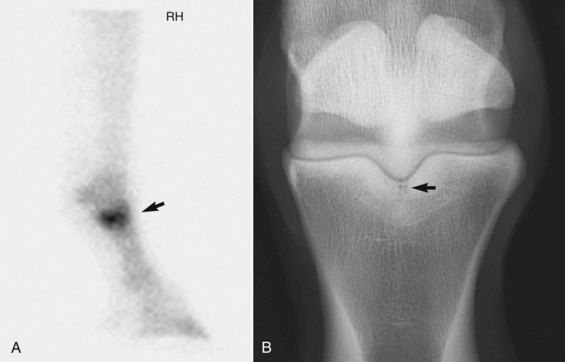
Fig. 41-2 A, Lateral delayed phase scintigraphic image of a 4-year-old Standardbred pacer with right hindlimb lameness thought to originate in the foot because the horse was sound after plantar digital analgesia. However, focal, intense increased radiopharmaceutical uptake of the proximal aspect of the proximal phalanx (arrow) is diagnostic for fracture. B, Dorsoplantar digital radiographic image documenting the presence of a short, midsagittal fracture of the proximal phalanx (arrow). Pain originating from the metatarsophalangeal joint can be desensitized by plantar digital analgesia.
Imaging considerations are similar to those described in the forelimb. It may be preferable to obtain plantarodorsal rather than dorsoplantar radiographic views of the foot. Many horses are reluctant to stand on a block with the foot bearing weight for lateromedial views. Satisfactory images can readily be obtained with the foot bearing weight only on the toe, provided that the foot is not rotated.6
Specific Lameness Conditions
Overall the most common conditions of the hind foot and pastern involve hoof abscesses and bruises, penetrating wounds into the hoof capsule and soft tissues of the pastern region, and cellulitis. Scratches can cause horses to appear lame at a walk and when severe, lame also at the trot. Management of these conditions is well described elsewhere.
Fractures of the Distal Phalanx
Fractures of the distal phalanx occur in any type of sports horse as the result of direct trauma from kicking a wall or trailer. Occasionally horses step on a hard object while turned out or during competition. In racehorses, fractures of the distal phalanx can occur as a result of maladaptive or nonadaptive remodeling, but this is much less common than in the forelimb. Because many fractures are the result of direct trauma, the distribution varies. Of 72 racehorses with fractures of the distal phalanx, only nine fractures involved a hindlimb, but eight involved the medial aspect of the distal phalanx.7 Distribution of hindlimb distal phalangeal fractures differs markedly from that seen in the forelimb of racehorses, in which left front (LF) lateral and right front (RF) medial fractures are most common.7 Medial location seems counterintuitive if hindlimb distal phalangeal fractures share a common cause with those seen in the forelimb. In the forelimb it is proposed that many distal phalangeal fractures are stress fractures that occur as a result of chronic repetitive bone injury, and the distribution reflects a counterclockwise direction of racing, making the lateral side of the LF and medial side of the RF (compression side of bone) prone to the development of fracture.7 It is the distal lateral aspect of the hindlimb that appears prone to the development of other stress-related subchondral bone injury (see Chapter 19Chapter 42Chapter 106Chapter 107Chapter 108Chapter 109), and why the distribution of distal phalangeal fractures is different is unknown. Articular plantar process fractures are most common, but incomplete (stress) fractures and midsagittal fractures also occur. Lameness is variable in degree, and it is important to recognize that lameness may be episodic in horses with a nonarticular plantar process fracture. Fractures often can be seen in lateromedial radiographic images, but special oblique images may be required. Comminuted fractures are rare but develop as the result of direct trauma. An unusual fracture near the insertion of the DDFT was found in a 2-year-old Thoroughbred colt referred for scintigraphic examination for undiagnosed right hindlimb lameness (Figure 41-3). This horse raced successfully with conservative management and corrective shoeing. Conservative management in most horses with fracture of the distal phalanx is quite successful. The decision to perform neurectomy is often made earlier than for injuries in a forelimb.
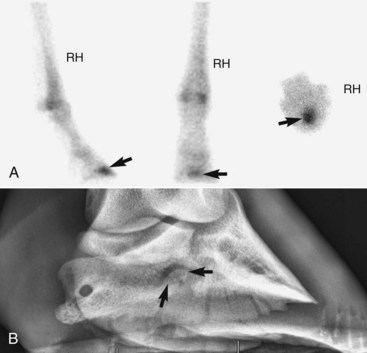
Fig. 41-3 A, Lateral (left image), plantar (middle image), and solar (right image) delayed phase scintigraphic images of a 2-year-old Thoroughbred colt in race training referred because of undiagnosed right hindlimb lameness. Lameness improved but did not abate completely after plantar digital and low plantar analgesia. Focal, intense increased radiopharmaceutical uptake (arrows) is seen in an unusual location, near the insertion of the deep digital flexor tendon on the distal, central aspect of the distal phalanx. B, Dorsal 45° lateral-plantaromedial oblique digital radiographic image showing an unusual lesion thought to be a small fracture fragment (arrow).
Laminitis
In horses with enterocolitis, pleuritis, metritis, or other systemic diseases, laminitis can develop in all four limbs, but rarely is the condition seen in only the hindlimbs. Even when hind feet are involved, clinical signs usually are most prominent in the front feet. Laminitis restricted to the hind feet has been seen only in overweight cob-type horses and ponies.8 Traumatic laminitis can occur from intense exercise on hard ground in unshod horses, but it most commonly develops in the contralateral limb of horses with severe unilateral hindlimb lameness. In the latter form, called orthopedic laminitis, distal displacement or rotation of the distal phalanx generally takes considerable time to develop (5 to 8 weeks) and can go unrecognized for several weeks (Figure 41-4). Often the first clinical sign that a problem is developing in the contralateral (laminitic) limb is that the lameness is observed to be inexplicably considerably improved in the original limb, or the horse starts to constantly shift weight between the two hindlimbs. Rarely, I have observed hindlimb laminitis as an apparently incidental finding in horses referred for scintigraphic examination for primary forelimb lameness or when whole-body scintigraphic examinations are performed. Marked increased radiopharmaceutical uptake (IRU) involving the distal or dorsal aspect of the distal phalanx and radiological evidence of rotation were seen. Primary lameness is found elsewhere, but laminitis in these horses may represent an unusual form of compensatory lameness.
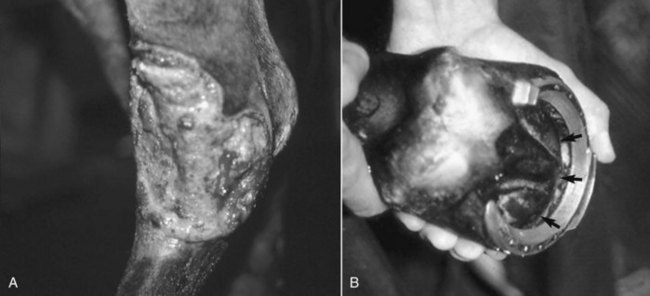
Fig. 41-4 A, Large wound in the left tarsal region as a result of inappropriate application of a topical counterirritant that caused chronic, severe lameness and eventually caused infectious arthritis of the distal hock joints. B, Photograph of the contralateral hind foot showing a noticeable convexity of the sole (arrows), the result of rotation and distal displacement of the distal phalanx (orthopedic laminitis).
I have examined two pleasure horses with primary bilateral hindlimb laminitis (without forelimb involvement) in which an unusual hindlimb gait was observed. At the walk horses had a goose-stepping gait like that seen in horses with fibrotic myopathy. The horses appeared to be attempting to land with an exaggerated heel-to-toe hoof strike. Both horses had a marked shortening of the caudal phase of the stride. At the trot horses had a short, choppy gait, but because lameness was bilateral, overt unilateral signs could not be seen.
Keratoma
Keratoma involving the hind feet is rare. An unusual radiolucent defect thought to be a keratoma that caused lameness and poor racing performance and was associated with IRU has been seen in the distal phalanx of a Thoroughbred racehorse.9
Navicular Syndrome
Navicular disease, osseous cystlike lesions, fractures, and malformations of the navicular bone are unusual in the hindlimb but do occur in all types of horses and ponies (see Chapters 30 and 31). In fact, in young racehorses, odd conditions of the navicular bone seem more common in the hindlimb than in the forelimb. The foot should never be discounted as a potential source of lameness (Figures 41-5 and 41-6). Degree of lameness is variable; lameness is usually unilateral and improved by perineural analgesia of the plantar digital nerves. Lesions are usually readily detectable radiologically. Lesions may occur bilaterally; therefore radiographic examination of both hind feet is recommended. It may be more difficult to obtain a skyline image of the navicular bone in a hindlimb than in a forelimb. Scintigraphy can be helpful in some horses, particularly in those suspected of having pain originating more proximal in the limb and fractious horses in which diagnostic analgesia to properly localize pain is dangerous.
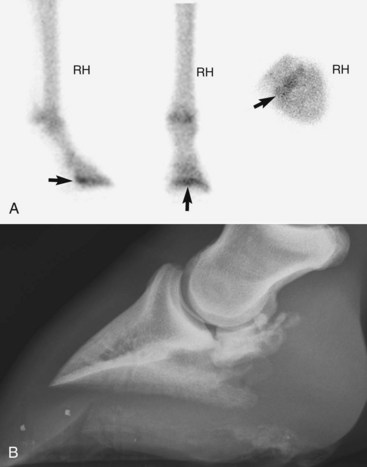
Fig. 41-5 A, Lateral (left image), plantar (middle image), and solar (right image) delayed (bone) phase scintigraphic images showing focal, moderately increased radiopharmaceutical uptake of the navicular bone in a 2-year-old, unraced Thoroughbred filly, admitted for examination of chronic right hindlimb lameness. B, Corresponding lateromedial digital radiographic image showing extensive degeneration of the navicular bone, with both bony proliferation and radiolucent defects present. There was no history of a penetrating wound or other traumatic incident, and an unusual malformation of the navicular bone was diagnosed. Note the close proximity of the distal aspect of the navicular bone to the distal phalanx, the abnormal orientation of the distal phalanx, and the abnormal shape of the hoof capsule.

Fig. 41-6 Dorsal 65° proximal-plantaro(palmaro)distal oblique digital radiographic images of the left hind (LH) (A) and left fore (LF) (B) feet showing unusual, coexistent navicular bone fractures in a 3-year-old Standardbred filly pacer. Baseline 3 to 4 out of 5 LH lameness resolved after plantar digital analgesia, but the filly then showed marked LF lameness. Acute LH navicular bone fracture (arrows) with mild displacement and chronic LF navicular bone fracture or bipartite navicular bone anomaly (arrows) were diagnosed.
Distal Interphalangeal Joint
Primary osteoarthritis of the hind distal interphalangeal joint is rare. Osteophytes involving the extensor process of the distal phalanx are commonly seen but are usually incidental radiological findings. Osteoarthritis occurs as a result of instability or incongruity caused by articular fractures of the distal phalanx. Occasionally subchondral bone damage of the articular surface of the distal phalanx occurs and is recognized as radiolucent defects and secondary osteoarthritic changes; this damage usually is seen in older nonracehorse sports horses. Chronic, undiagnosed hindlimb lameness is followed by acute, prominent lameness. Diagnosis may be difficult, thus prompting scintigraphic examination. Focal areas of IRU in the subchondral bone of the distal phalanx should be differentiated from those in horses with incomplete fracture.
Extensor process fragments or fractures are rare. Osseous cystlike lesions as a result of osteochondrosis of the distal phalanx are seen occasionally. Some small lesions restricted to the subchondral bone of the distal phalanx are difficult to identify radiologically but usually result in intense, focal IRU scintigraphically. Definitive diagnosis may be possible only with magnetic resonance imaging (MRI) or at postmortem examination.8 Other fractures involving the distal aspect of the middle phalanx and comminuted fractures of this bone occur. Involvement of the distal interphalangeal joint in horses with comminuted fractures of the middle phalanx is a negative prognostic finding.
Collateral ligament injury of the distal interphalangeal joint is an uncommon cause of hindlimb lameness but does occur, usually with no localizing clinical signs. Although occasionally lesions can be identified using ultrasonography, diagnosis usually requires MRI.
Deep Digital Flexor Tendonitis
Primary injuries of the DDFT are an unusual cause of hindlimb lameness but have been identified in show jumpers and event horses. There has been an acute onset of moderate-to-severe unilateral lameness, usually with no localizing clinical signs. Diagnosis usually requires MRI.
The Hind Pastern
Lameness of the hind pastern region includes osteoarthritis of the proximal interphalangeal joint, osseous cystlike lesions of the distal aspect of the proximal phalanx, osteochondral fragmentation of the proximal interphalangeal joint, subluxation of the proximal interphalangeal joint, tenosynovitis of the DFTS, tendonitis of the DDFT and the branches of the superficial digital flexor tendon, injury of the distal sesamoidean ligaments, penetrating wounds, and cellulitis (see Chapters 35, 70, 74, and 82). Fractures of the proximal and middle phalanges are discussed in detail in Chapter 35. One fracture type, Salter-Harris type II fractures of the proximal aspect of the proximal phalanx, occurs most commonly in the hindlimb. Because physeal fractures are inherently more stable than those of the diaphyseal region of long bones, it is compelling to simply apply external coaptation such as a fiberglass cast incorporating the foot. However, prolonged cast immobilization quickly causes flexor laxity in foals and can predispose to osteoarthritis and sesamoiditis. Invariably, even with inherent stability, fracture displacement occurs. The metaphyseal component is usually plantaromedial, and even with external coaptation the proximal fracture fragment shifts distally and plantarolaterally and a gap opens on the dorsomedial aspect. Internal fixation using screws placed from the plantaromedially located metaphyseal portion improves stability, but alignment of the fracture is hard to maintain. An alternative approach is to apply a dorsolateral dynamic compression plate, a technique that takes advantage of the tension band principle, because the tension side of the proximal phalanx appears to be dorsolateral when this fracture occurs (Figure 41-7). Rigid internal fixation obviates the need to maintain foals in external coaptation. Because the epiphysis is narrow, care must be taken when placing the proximal screw.

Fig. 41-7 Dorsal 45° medial-plantarolateral oblique digital radiographic images before (A) and immediately after (B) repair and 3 months after repair and implant removal (C) in a weanling Warmblood foal with a Salter-Harris type II fracture of the proximal aspect of the right hind proximal phalanx. Using the tension band principle, a three-hole, limited-contact dynamic compression plate was applied to the dorsolateral aspect of the proximal phalanx; the middle screw was placed in lag fashion through the metaphyseal component. Rigid internal fixation obviated the need for prolonged external coaptation and maintained fracture alignment.