Spinal Cord Injury
After studying this chapter, the student or practitioner will be able to do the following:
1 Understand the difference between complete and incomplete spinal cord injury and the classification system used to describe such levels of injury.
2 Recognize and identify the various spinal cord injury syndromes.
3 Briefly describe the medical and surgical management of the individual who has experienced a traumatic spinal cord injury.
4 Identify some of the complications that can limit optimal functional potential.
5 Describe the changes in sexual functioning in males and females after spinal cord injury.
6 Identify the specific assessment tools that must be considered before developing intervention objectives.
7Analyze the critical issues in factors to consider when developing intervention objectives during the acute, active, and discharge phases of the rehabilitation process.
8 Identify in detail the functional outcomes, including equipment considerations and personal and home care needs, that can be reached at each level of complete injury under optimal circumstances.
9 Analyze how the effects of spinal cord injury accelerate the normal aging process, and explain how functional status may change.
Rehabilitation of the client with a spinal cord injury (SCI) is a lifelong process that requires readjustment to nearly every aspect of life. Occupational therapists and occupational therapy (OT) assistants play a significant role in physical and psychosocial restoration and help the client achieve maximal independence. Through accurate evaluation, retraining, and adaptive techniques and equipment, occupational therapists provide their clients with the tools and resources needed to resume engagement in occupation to support participation in life situations to their maximal physical and functional potential.
SCIs have many causes, trauma being the most common. Trauma can result from motor vehicle accidents, violent injuries such as gunshot and stab wounds, falls, sports accidents, and diving accidents.5,12 Normal spinal cord function may also be disturbed by diseases such as tumors, myelomeningocele, syringomyelia, multiple sclerosis, cancer, and amyotrophic lateral sclerosis. Some of the intervention principles outlined in this chapter may apply to these conditions; however, the emphasis is on rehabilitation of the individual with a traumatic SCI.
Results of Spinal Cord Injury
SCI results in quadriplegia (labeled tetraplegia by the American Spinal Cord Injury Association) or paraplegia. Tetraplegia, which will be referred to as quadriplegia throughout the remainder of the chapter, is any degree of paralysis of the four limbs and trunk musculature. There may be partial upper extremity (UE) function, depending on the level of the cervical lesion. Paraplegia is paralysis of the lower extremities (LEs) with involvement of the trunk and hips, depending on the level of the lesion.5,12
SCIs are referred to in terms of the regions (cervical, thoracic, and lumbar) of the spinal cord in which they occur and the numerical order of the neurologic segments. The level of SCI designates the last fully functioning neurologic segment of the cord. For example, C6 refers to the sixth neurologic segment of the cervical region of the spinal cord as the last fully intact neurologic segment.3,5 Complete lesions result in the absence of motor or sensory function of the spinal cord below the level of the injury.
Incomplete lesions may involve several neurologic segments, and some spinal cord function may be partially or completely intact.2,3
Complete versus Incomplete Neurologic Classifications
The extent of neurologic damage depends on the location and severity of the injury (Figure 36-1). In a complete injury, total paralysis and loss of sensation result from a complete interruption of the ascending and descending nerve tracts below the level of the lesion. In an incomplete injury, there is some degree of preservation of the sensory or motor nerve pathways below the level of the lesion. Segments at which normal function is found often differ in the side of the body and in terms of sensory versus motor testing.
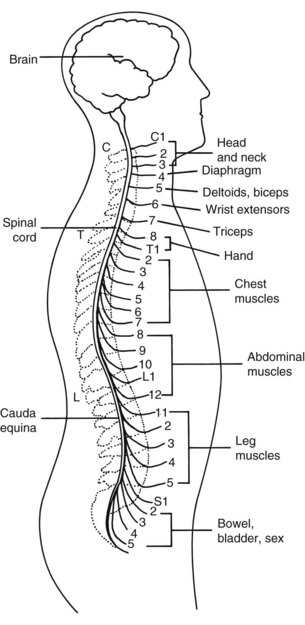
FIGURE 36-1 Spinal nerves and major areas of body they supply. (From Paulson S, editor: Santa Clara Valley Medical Center spinal cord injury home care manual, ed 2, San Jose, CA, 1994, Santa Clara Valley Medical Center.)
It is essential that a very careful neurologic examination be done before determining whether an injury is complete or incomplete.
The American Spinal Injury Association (ASIA) uses the findings from the neurologic examination to classify injury types to further objectify specific clinical findings:
• ASIA impairment scale classification A indicates a complete lesion; there is no motor or sensory function preserved in the sacral segments S4 through S5. Any preservation of strength without sensory sparing in the sacral segments of S4 through S5 is considered a zone of partial preservation (ZPP) and still considered a complete (ASIA A) neurologic classification.
• ASIA classification B indicates an incomplete lesion in which sensory but not motor function is preserved below the neurologic level and must include the sacral segments S4 through S5.
• ASIA classification C indicates an incomplete lesion in which motor function is preserved below the neurologic level and more than half of the key muscles below the neurologic level have a muscle grade of less than 3 (Fair).
• ASIA classification D indicates an incomplete lesion in which motor function is preserved below the neurologic level and at least half of the key muscles below the neurologic level have a muscle grade of 3 or more.
• ASIA classification E indicates that motor and sensory functions are normal.1
• Incomplete injuries are categorized according to the area of damage: central, lateral, anterior, or peripheral.
After thorough muscle and sensory testing, Laurence’s neurologic diagnosis was C7 ASIA A. Key musculature innervated by the C7 nerve root (triceps) was graded at 4 (Good). He had 2 (Poor) strength in his finger flexors, extensors, and thumb flexors. Because sensation was intact to the C7 dermatome level and completely absent below and in the sacral segments, his diagnosis was clearly ASIA A with a ZPP at C8.
Clinical Syndromes
After SCI, the individual enters a stage of spinal shock that may last from 24 hours to 6 weeks. This period is one of areflexia, in which reflex activity ceases below the level of the injury.3 The bladder and bowel are atonic or flaccid. Deep tendon reflexes are decreased, and sympathetic functions are disturbed. This disturbance results in decreased constriction of blood vessels, low blood pressure, a slower heart rate, and no perspiration below the level of injury.10,16
The spinal cord is usually not damaged below the level of the lesion. Therefore, muscles that are innervated by the neurologic segments below the level of injury usually develop spasticity, because the monosynaptic reflex arc is intact but separated from higher inhibitory influences. Deep tendon reflexes become hyperactive, and spasticity may be evident. Sensory loss continues, and the bladder and bowel usually become spastic (“upper motor neuron” bladder) in clients whose injuries are above T12. The bladder and bowel usually remain flaccid (“lower motor neuron” bladder) in clients whose lesions are at L1 and below. Sympathetic functions become hyperactive. Spinal reflex activity (mass muscle spasms) usually becomes evident in the areas below the level of the lesion.2,12,14
Four weeks after his injury, Laurence began to develop spasticity in his LEs and abdominal muscles. When he was assisted into bed, he said, he felt as if “the breath was knocked out of me” as a result of abdominal tightness. This sensation created a considerable amount of anxiety for him until he learned more about the effects of abdominal spasms and how the involuntary tightness of the abdominal muscles would make it difficult for him to exhale—hence, the sensation of shortness of breath. His LEs were very tight and difficult to manage during his morning dressing program with the occupational therapist because of the extensor spasms that he was experiencing upon exertion. His therapist discussed this challenge with Laurence’s doctor, who prescribed spasticity medication to inhibit the spasms that were interfering with LE dressing and pretransfer and posttransfer setup. Because his therapist could observe firsthand the effect of Laurence’s spasticity on his daily activities, this therapist’s feedback to Laurence’s physician considerably influenced the dosage of his spasticity medications.
Central Cord Syndrome
Central cord syndrome occurs when there is more cellular destruction in the center of the cord than in the periphery. Paralysis and sensory loss are greater in the UEs because these nerve tracts are more centrally located than those of the LEs. Central cord syndrome is often seen in older people in whom arthritic changes have caused a narrowing of the spinal canal; in such cases, cervical hyperextension without vertebral fracture may precipitate central cord damage.
Brown-Séquard Syndrome (Lateral Damage)
Brown-Séquard syndrome results when only one side of the cord is damaged, as in a stabbing or gunshot injury. Below the level of injury, there is motor paralysis and loss of proprioception on the ipsilateral side and loss of pain, temperature, and touch sensation on the contralateral side.
Anterior Spinal Cord Syndrome
Anterior spinal cord syndrome results from injury that damages the anterior spinal artery or the anterior aspect of the cord. This syndrome involves paralysis and loss of pain, temperature, and touch sensation. Proprioception is preserved.
Cauda Equina (Peripheral)
Cauda equina injuries involve peripheral nerves rather than directly involving the spinal cord. This type of injury usually occurs with fractures below the L2 level and results in a flaccid-type paralysis. Because peripheral nerves possess a regenerating capacity that the cord does not, this injury is associated with a better prognosis for recovery. Patterns of sensory and motor deficits are highly variable and asymmetrical.
Prognosis for Recovery
The prognosis for substantial recovery of neuromuscular function after SCI depends on whether the lesion is complete or incomplete. If there is no sensation or return of motor function below the level of lesion 24 to 48 hours after the injury in carefully assessed complete lesions, motor function is less likely to return. However, partial to full return of function to one spinal nerve root level below the fracture can be gained and may occur in the first 6 months after injury. In incomplete lesions, progressive return of motor function is possible, yet it is difficult to determine exactly how much and how quickly return will occur.14 Frequently, the longer it takes for recovery to begin, the less likely it is that it will occur.
The following statements can be used as guidelines to predict and assist therapists and their clients in understanding the recovery process after a new SCI:11
• The severity of the original injury determines whether recovery will occur. Unfortunately, no test to measure this severity exists at this time, and predictions must be based on what has happened to others in the past with similar neurologic findings.
• Incomplete injuries are associated with a better chance of further recovery than are complete injuries, but even with incomplete injuries there is no guarantee that further recovery will occur.
• Most of the recovery that will occur starts within the first few weeks. Therefore, each day that goes by without any return of function means that the likelihood of recovery is reduced.
• No amount of hard work will cause nerve function to return. If hard work were all it took, very few people would end up with permanent paralysis.
• Rehabilitation will not affect the degree of recovery. The purpose of rehabilitation is to prevent further medical complications through education, to maintain and improve the strength and skills that are present, to maximize function in self-care activities, to facilitate mobility, and to optimize lifestyle options for the patient and their family, therefore, maintaining the body and the individual’s general well being in a “recovery ready” state.
Medical and Surgical Management of the Person with Spinal Cord Injury
After a traumatic event in which SCI is likely, the conscious client should be carefully questioned about cutaneous numbness and skeletal muscle paralysis before being moved. Emergency medical technicians, paramedics, and air transport personnel are trained in SCI precautions and extrication techniques for moving a person who has sustained a possible SCI from an accident site. Movement of the spine must be prevented during the transfer procedures. A firm stretcher or board to which the person’s head and back can be strapped should be procured before moving the person. After the patient is transferred to the stretcher or board, he or she should be strapped to the board or stretcher and carefully transferred via air or ground transport to the nearest hospital emergency room. Axial traction on the neck should be maintained, and any movement of the spine and neck prevented during this process. Careful examination, stabilization, and transportation of the patient may keep a temporary or minimal SCI from becoming more severe or permanent. Initial care is directed toward preventing further damage to the spinal cord and reversing neurologic damage, if possible, by stabilization or decompression of the injured neurologic structures.5,10,12 Anti-inflammatory and steroidal drugs are administered immediately after injury in an effort to minimize swelling to the specific lesion and therefore minimize neurologic damage, although the significance of their effect on neurologic recovery remains unclear.
The examining physician carries out a careful neurologic examination to aid in determining the site and type of injury. The client is in a supine position for this procedure, with the neck and spine immobilized. A catheter is usually placed in the client’s bladder to drain urine. Anteroposterior and lateral x-ray films may be taken, with the individual’s head, neck, or spine immobilized, to help determine the type of injury. A computed tomography (CT) scan or magnetic resonance imaging (MRI) may be needed for further evaluation. In early medical treatment the goals are to restore normal alignment of the spine, maintain stabilization of the injured area, and decompress neurologic structures that are under pressure.
Bony realignment and stabilization can be achieved by placing the client on a rotating kinetic bed (Figure 36-2) that allows skeletal traction and immobilization. The bed’s constant rotation allows continuous pressure relief, mobilization of respiratory secretions, and easy access to the client’s entire body for bowel, bladder, and hygiene care. Open surgical reduction with internal fixation and spinal fusion may be indicated.

FIGURE 36-2 Kinetic bed with custom arm positioner. Designed and fabricated by the Occupational Therapy Department, Santa Clara Valley Medical Center, San Jose, California. (Courtesy of Luis Gonzalez, Media Resource Department, Santa Clara Valley Medical Center.)
The goals of surgery are to decompress the spinal cord and achieve spinal stability and normal bony alignment.5,12 Surgery is not always necessary, and adequate immobilization may allow the individual to heal. As soon as possible, a means of portable immobilization is provided—usually a cervical collar or halo vest for cervical injuries (Figure 36-3, A) and a thoracic brace or body jacket for thoracic injuries (Figure 36-3, B). This approach enables the client to be transferred to a standard hospital bed and, subsequently, to be upright in a wheelchair and involved in an active therapy program in as little as 1 to 2 weeks after injury. Initiating an upright sitting tolerance program shortly after injury can substantially reduce the incidence and severity of further medical complications, such as deep vein thrombosis, joint contractures, and the general deconditioning that can result from prolonged bed rest.
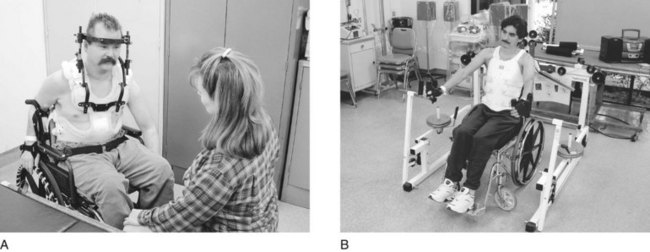
FIGURE 36-3 A, Halo vest. One type of neck immobilization device for individuals with quadriplegia and high-level paraplegia (T1 to T4). B, Body jacket. One type of immobilization device for paraplegia. (Courtesy of Luis Gonzalez, Media Resource Department, Santa Clara Valley Medical Center.)
The benefits of early transport to an SCI center have been documented.7 Clients treated initially in a spinal cord acute-care unit rather than a general hospital had shorter acute-care lengths of stay. Clients treated in general hospitals tended to have a higher incidence of skin problems and spinal instability. It has been found that individuals sent to rehabilitation centers specializing in the treatment of SCI made functional gains with greater efficiency.16 Spinal cord centers are equipped to offer a complete, multidisciplinary program executed by an experienced team of professionals who specialize in this unique and demanding disability.
Laurence was injured at his work site, which happened to be very close to a hospital in which a designated SCI center was located. In addition to his cervical spine injury, he sustained bilateral wrist fractures and facial lacerations as a result of the nature of the fall from the equipment on which he had been standing. Standard practice at this particular hospital is to contact the physiatrist on call for an immediate opinion regarding trauma care.
Complications of Spinal Cord Injury
Skin Breakdown, Pressure Sores, or Decubitus Ulcers
Sensory loss increases the risk of skin breakdown. Persons with sensory loss cannot feel the pressure and shearing of prolonged sitting or lying in one position or the presence of pain or heat against the body. Pressure causes the loss of blood supply to the area, which can ultimately result in necrosis. Heat can quickly burn and destroy tissues. Shearing can destroy underlying tissue. Any combination of the aforementioned factors will hasten skin breakdown. The areas most likely to develop skin breakdown are bony prominences over the sacrum, ischium, trochanters, elbows, and heels; however, other bony prominences, such as the iliac crest, scapula, knees, toes, and rib cage, are also at risk.
All rehabilitation personnel must be aware of the signs of developing skin problems. At first the area reddens and then blanches when pressed. Later, the reddened or abraded area does not blanch, which indicates that necrosis has begun. Finally, a blister or ulceration appears in the area. The problem is often more severe below the level of the skin surface. The visible sore may be only the tip of the iceberg. If allowed to progress, a sore can become severe, destroying underlying tissues even as deep as the bone.
Skin breakdown can be prevented by relieving and eliminating pressure points and protecting vulnerable areas from excessive shearing, moisture, and heat. Routine turning of clients in bed, specialized mattresses and wheelchair seat cushions, protection of bony prominences with various types of padding, and the performance of weight shifts are some of the methods used to prevent pressure sores.
The use of hand splints, body jackets, and other orthoses can also cause skin breakdown, particularly when protective sensation in those areas is impaired. The therapist must inspect the skin, and the client must be taught to examine his or her skin on a consistent, daily basis, using a mirror or caregiver assistance to watch for signs of developing problems. Skin damage can develop within 30 minutes; therefore, frequent weight shifting, repositioning, and vigilance are essential if skin breakdown is to be prevented.12,14
Decreased Vital Capacity
Decreased vital capacity is a problem among people who have sustained cervical and high thoracic lesions. Such individuals have markedly limited chest expansion and a decreased ability to cough because of weakness or paralysis of the diaphragm and the intercostal and latissimus dorsi muscles. This scenario can result in a tendency toward respiratory tract infections. Reduced vital capacity affects the overall endurance level for activity. Endurance can be improved by assisted breathing and by vigorous respiratory and physical therapy. Strengthening of the sternocleidomastoids and the diaphragm, manually assisted cough, and deep breathing exercises are essential to maintain optimal vital capacity.12,14
Laurence’s vital capacity was 50% of normal capacity for a man of his size. He required assistance to cough because he did not have the force to clear his secretions upon exhaling. His endurance was low during his 4- to 5-hour therapy program. He required much education in this area because he was previously a triathlete and in exceptional cardiovascular shape.
Osteoporosis
Osteoporosis is likely to develop in individuals with SCIs because of disuse of long bones, particularly of the LEs. Osteoporosis may be sufficiently advanced for pathologic fractures to occur a year after the injury. Pathologic fractures are most common in the supracondylar area of the femur, proximal tibia, and distal tibia, the intertrochanteric area of the femur, and the neck of the femur. Pathologic fractures are usually not seen in UEs. Daily standing with a standing frame may slow the onset of osteoporosis;12,14 however, this is a controversial method and not embraced in all rehabilitation programs. A standing program must fit into the patient’s activities of daily living (ADLs) after discharge to be effective on an ongoing basis. Not all reimbursement sources will cover the cost of standing equipment.
Orthostatic Hypotension
A lack of muscle tone in the abdomen and LEs leads to pooling of blood in these areas, with a resultant decrease in blood pressure (hypotension). This problem occurs when the patient moves from a supine to upright position or changes body position too quickly. Symptoms are dizziness, nausea, and loss of consciousness.4 The client must be reclined quickly and, if sitting in a wheelchair, should be tipped back with legs elevated until symptoms subside. With time, this problem can diminish as sitting tolerance and level of activity increase; however, some people continue to have hypotensive episodes. Abdominal binders, compression garments, antiembolism stockings, and medications can help reduce symptoms.
Autonomic Dysreflexia
Autonomic dysreflexia is a phenomenon seen in persons whose injuries are above the T4 to T6 level. It is caused by reflex action of the autonomic nervous system in response to some stimulus, such as a distended bladder, fecal mass, bladder irritation, rectal manipulation, thermal or pain stimuli, or visceral distention. The symptoms are immediate pounding headache, anxiety, perspiration, flushing, chills, nasal congestion, paroxysmal hypertension, and bradycardia.
Autonomic dysreflexia is a medical emergency and life threatening. The client should not be left alone.5,12,14 The condition is treated by placing the client in an upright position and removing anything restrictive, such as abdominal binders or elastic stockings, to reduce blood pressure. The bladder should be drained or leg bag tubing checked for obstruction. Blood pressure and other symptoms should be monitored until they return to normal. The occupational therapist must be aware of symptoms and treatment because autonomic dysreflexia can occur at any time after the injury.
Individuals who are susceptible to this condition are encouraged to carry an emergency card describing the condition and treatment because many emergency rooms and medical personnel may be unfamiliar with it.
Spasticity
Spasticity is a nearly universal complication of SCI.14 It is an involuntary muscle contraction below the level of injury that results from lack of inhibition from the brain. Patterns of spasticity change over the first year, gradually increasing in the first 6 months and reaching a plateau about 1 year after the injury. A moderate amount of spasticity can be helpful in the overall rehabilitation of the patient with an SCI. It helps to maintain muscle mass, assists in the prevention of pressure sores by facilitating blood circulation, and can be used to assist in range of motion (ROM) and bed mobility. A sudden increase in spasticity can alert the individual to other medical problems, such as bladder infections, skin breakdown, and fever.
Because it can interfere with function, severe spasticity can be quite frustrating to both the client and the therapist. It may be treated more aggressively with a variety of medications. In select instances, local injections of nerve blocks or Botox may benefit some individuals. In severe cases, neurosurgical procedures can be performed.5,12,14
Heterotopic Ossification
Heterotopic ossification (HO), also called ectopic bone, is bone that develops in abnormal anatomic locations.16 It most often occurs in the muscles around the hip and knee, but occasionally it can also be noted at the elbow and shoulder. The first symptoms are swelling, warmth, and decreased joint ROM. The onset of HO is usually 1 to 4 months after injury. Early diagnosis and initiation of treatment can minimize complications. Symptoms are often discovered during physical or occupational therapy treatments even when radiologic findings are negative. Treatment consists of medication and the maintenance of joint ROM during the early stage of active bone formation to preserve the functional ROM necessary for good wheelchair positioning, symmetrical position of the pelvis, and maximal functional mobility. If HO progresses to the phase of substantially limiting hip flexion, pelvic obliquity while in the sitting position is likely to occur. This problem contributes to trunk deformities such as scoliosis and kyphosis, with subsequent skin breakdown at the ischial tuberosities, trochanters, and sacrum.5,12
Sexual Function
The sexual drive and the need for physical and emotional intimacy are not altered by SCI. However, problems of mobility, functional dependency, and altered body image, as well as complicating medical problems and the attitudes of partners and society, affect social and sexual roles, access, and interest and satisfaction. Education is essential for the individual with an SCI as well as all clinicians and, as an important area of occupation (both in ADLs and social participation), is a critical part of the rehabilitation process. Lack of sensation over one part of the body is accompanied by increased or altered sensation over other parts of the body. The sexual response of the body after SCI needs to be explored in the same way a person learns what muscles are working and where he or she can feel.
In males, erections and ejaculations are often affected by SCI. However, because this problem is variable, it should be evaluated individually. The motility of sperm in men with SCI is frequently decreased, even when other function is near normal.1 Significant advances in treatment are identifying the possible sources of infertility caused by SCI and ways to reverse the problem.
In women, menstruation usually ceases for an interval of weeks to months after injury. It will usually start again and return to normal in time. There may also be changes in lubrication of the vagina during sexual activity. In contrast to males, however, there is no change in female fertility. Females with SCI can conceive and give birth. Special attention must be given to the interaction of pregnancy and childbirth with SCI, especially with regard to blood clots, respiratory function, bladder infections, autonomic dysreflexia, and the use of medications during pregnancy and breast-feeding.
To avoid pregnancy, women with SCI must take precautions, and the type of birth control used must be considered carefully. Birth control pills are associated with blood clots, especially when combined with smoking, and probably should not be used. The intrauterine device (IUD) is not recommended, even for able-bodied females. Diaphragms may be difficult to position properly when there is loss of sensation in the vagina or decreased hand function. Foams and suppositories are not very effective. The use of condoms by the male partner is probably the safest method.
Disabled individuals quickly sense the attitudes of professionals and caregivers toward their sexuality. Awareness and acceptance by professionals is increasing, and sexual counseling and education are a regular part of many rehabilitation programs for all types of physical disabilities. Some clients lack basic sex education. Others feel asexual because of their disability and altered self-esteem and are isolated from peers; thus, they may feel uncomfortable with any type of sexual interaction. For these reasons, sexual education and counseling must be geared to the needs of the individual client and his or her significant other. In some instances, social interaction skills require improvement before sexual activity can be considered, and occupational therapists play an important role in providing information and a forum to deal with these issues. (See Chapter 12 for more information on sexuality with physical dysfunction.)
Laurence was divorced at the time of his accident. He was very close to his stepdaughter and was having a difficult time dealing with the dissolution of his family. While in the hospital, his ex-wife and stepdaughter resumed their relationship with Laurence in hopes of resolving their conflicts. After acknowledging the permanency of his disability, Laurence felt considerable depression, anger, and low self-esteem. Even with the resumption of family support and the large professional community of support he was given, he could not imagine himself as a sexual person who could offer his family and friends the love and relationships he had known in the past.
Occupational Therapy Intervention
Evaluation of the client is an ongoing process that begins on the day of admission and continues long after discharge on an outpatient follow-up basis. Depending on whether the patient is in an acute inpatient rehabilitation, outpatient, or home setting, the occupational therapist should continually evaluate the client’s functional progress and the appropriateness of intervention and equipment. An accurate and comprehensive formal initial evaluation is essential. Initial data gathered from the medical chart will provide personal information, a medical diagnosis, and a history of other pertinent medical information. Input from the multidisciplinary team will enhance the occupational therapist’s ability to predict realistic optimal outcomes accurately.
Discharge planning begins during the initial evaluation. Therefore, the individual’s social and vocational histories, as well as personal contexts such as past and expected living situations, are necessary for planning an intervention program that meets the client’s ongoing needs. Intervention should begin as soon as possible. It is possible to quickly gather enough information to begin addressing high-priority areas such as splinting, positioning, and family training without having to wait for the evaluation to be completed.
Occupational and Psychosocial Status
The top-down and client-centered approaches recommended in the Occupational Therapy Practice Framework, Second Edition (OTPF-2), suggest that the evaluation process begin with an occupational profile, which includes obtaining an occupational history and ascertaining the goals of the client as they pertain to resuming performance of favored occupations. Frequently, given the acute nature and overwhelming impact of an SCI, some of the physical problems associated with client factors crucial to survival must initially be given priority for evaluation. Efforts may be directed toward determining baseline neurologic, clinical, and functional status from which to formulate an early intervention program. However, while the occupational therapist is initially addressing these critical physical client factors, he or she can be simultaneously engaging the client in an occupational profile, learning the client factors related to values, beliefs, and spirituality, along with the areas of occupation that comprise and give meaning to the client’s life. By involving the client as central to the intervention plan and identifying occupational goals as primary, the more physical aspects and client factors (body structure and body functions) are put into perspective as underlying and supportive to these occupational goals.
Through conducting the occupational profile and occupational history and beginning interventions, the occupational therapist has the opportunity to learn about and observe the client’s psychosocial adjustment to the disability and life in general through the nature of the activities and occupations in which the patient participates.12 The evaluation phase is important for establishing rapport and mutual trust, which will facilitate participation and progress in later and more difficult phases of rehabilitation. The client’s motivation, determination, and contexts—including socioeconomic background, education, family support, personal attitudes toward disability, problem-solving abilities, and financial resources—can prove to be invaluable assets or limiting factors in determining the outcome of rehabilitation. A therapist must carefully observe the client’s status in each of these areas before recommending the course of intervention.
Physical Status
Before evaluation of the client’s physical status (or “client factors: body functions and body structures”), specific medical precautions should be obtained from the primary and consulting physicians. Skeletal instability and related injuries or medical complications will affect the way in which the client is moved and the active or resistive movements allowed.
Passive range of motion (PROM) should be measured before specific manual muscle testing to determine available pain-free movement. This evaluation also identifies the presence of or potential for joint contractures, which could suggest the need for preventive or corrective splinting and positioning (see Chapter 21).
Shoulder pain, which ultimately causes decreased shoulder and scapular ROM, is extremely common in those individuals with C4 through C7 quadriplegia. Among the possible causes is scapular immobilization resulting from prolonged bed rest and nerve root compression subsequent to the injury. Shoulder pain should be thoroughly assessed and diagnosed so that proper intervention can be provided before the onset of chronic discomfort and functional loss.
Accurate assessment of the client’s muscle strength is critical in determining a precise diagnosis of neurologic level and establishing a baseline for physical recovery and functional progress. Because the occupational therapist’s skills with activity analysis greatly enhance his or her effectiveness in treating the client with SCI, a precise working knowledge of musculoskeletal anatomy and specific manual muscle testing techniques is essential. Use of accepted muscle testing protocols ensures accurate technique during performance of this complex evaluation. The muscle test should be repeated as often as is necessary to provide an ongoing picture of the client’s strength and progress (see Chapter 22).
Sensation is evaluated for light touch, superficial pain (pin prick), and kinesthesia, which determines areas of absent, impaired, and intact sensation. These findings are useful in establishing the level of injury and determining functional limitations (Figure 36-4).1
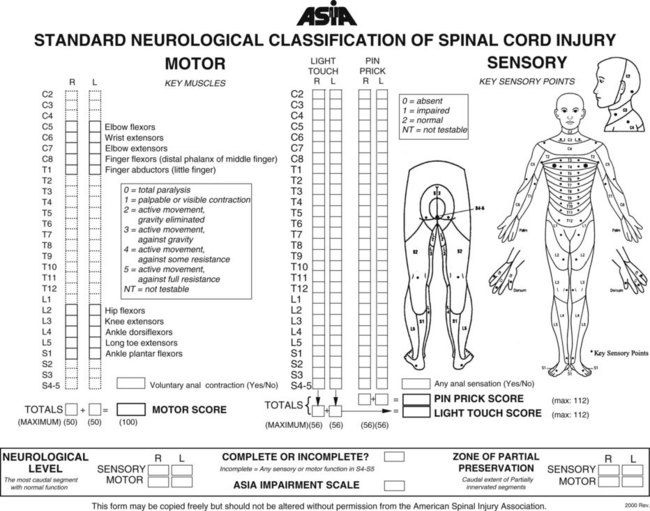
FIGURE 36-4 Standard neurologic classification of spinal cord injury. (Courtesy of the American Spinal Injury Association, 2000.)
If the client is evaluated in the acute stage, spasticity is rarely noted because the client is still in spinal shock. When spinal shock subsides, increased muscle tone may be present in response to stimuli. The therapist should then determine whether the spasticity interferes with or enhances function.
An evaluation of wrist and hand function determines the degree to which a client can manipulate objects. This information is used to suggest the need for equipment such as positioning splints or universal cuffs or, later, consideration of a tenodesis orthosis (wrist-driven flexor hinge splint). Gross grasp and pinch measurements indicate functional abilities and may be used as an adjunct to manual muscle testing to provide objective measurements of baseline status and progress for clients who have active hand musculature.8
Clinical observation is used to assess endurance, oral motor control, head and trunk control, LE functional muscle strength, and total body function. More specific assessment in any of these areas may be required, depending on the client’s specific needs.
An increased number of combined SCI and head-injury diagnoses suggests that a specific cognitive and perceptual evaluation may be necessary.9 Assessing a client’s ability to initiate tasks, follow directions, carry over learning day to day, and handle problem-solving tasks contributes to the information base necessary for appropriate and realistic goal setting (see Chapters 25 and 26). Understanding the client’s learning style, coping skills, and communication style is also essential.
In Laurence’s case, he had no memory of his fall and several hours of the time that elapsed after his accident. He also exhibited a slight memory deficit, as shown by his poor carryover of tasks from day to day during the first 2 weeks of his rehabilitation. He received a full cognitive assessment and was determined to be below his baseline for cognition and memory. His therapists helped him complete a memory book of his daily activities to assist in carryover. Because his therapists believed that his extreme depression contributed to his poor memory, he was seen daily for individual counseling. His memory and affect significantly improved over the next several weeks.
Functional Status
Observing as the client performs ADLs is an important part of the OT evaluation. The purpose of this observation is to determine present and potential levels of functional ability. If the client is cleared of bed-rest precautions, evaluation and simultaneous intervention should begin as soon as possible after injury. Light activities such as feeding, light hygiene at the sink, and object manipulation may be appropriate, depending on the level of injury (see Chapter 10).
Direct interaction with the client’s family and friends provides valuable information regarding the client’s support systems while in the hospital and, more important, after discharge. This information is relevant to later caregiver training in areas in which the client may require the assistance of others to accomplish self-care and mobility tasks
Establishing Intervention Objectives
Establishing intervention objectives in concert with the client and with the rehabilitation team is important. The primary objectives of the rehabilitation team may not be those of the client. Psychosocial factors, cultural factors, cognitive deficits, environmental limitations, and individual financial considerations must be identified and integrated into a comprehensive intervention program that will meet the unique needs of each individual. Every client is different; therefore, a variety of intervention approaches and alternatives may be necessary to address each factor that may affect goal achievement.7 Increased participation can be expected if the client’s priorities are respected to the extent that they are achievable and realistic.
The occupational therapist’s general objectives for intervention with the person with SCI are as follows:
1. To maintain or increase joint ROM and prevent problems associated with body functions and other body structures (skin) via preparatory activities such as active and passive ROM, splinting, positioning, and client education
2. To increase the strength of all innervated and partially innervated muscles and address problems associated with other body functions (e.g., sensation, higher level cognitive functions, emotional functions) through preparatory activities and engagement in purposeful activities and occupations
3. To increase physical endurance and other performance skills and performance patterns through engagement in purposeful activities and occupations
4. To maximize independence in performance in all areas of occupation, including ADLs, IADLs, rest and sleep, education, work, play, leisure, and social participation
5. To aid in the psychosocial adjustment to disability
6. To evaluate, recommend, and educate the client in the use and care of necessary durable medical and adaptive equipment
7. To ensure safe and independent home and environmental accessibility through consultation and safety and accessibility recommendations
8. To assist the client in developing the communication skills necessary for training caregivers to provide safe assistance
9. To educate the client and his or her family regarding the benefits and consequences of maintaining healthy and responsible lifestyle habits in relation to long-term function and the aging process
The client’s length of stay in the inpatient rehabilitation program and the ability to participate in outpatient therapy determine the appropriateness and priority of the aforementioned activities.
Intervention Methods
During the acute, or immobilized, phase of the rehabilitation program, the client may be in traction or wearing a stabilization device such as a halo brace or body jacket. Medical precautions must be in force during this period. Flexion, extension, and rotary movements of the spine and neck are contraindicated.
Evaluation of total body positioning and hand splinting needs should be initiated at this time. In clients with quadriplegia/tetraplegia, scapular elevation and elbow flexion (as well as limited shoulder flexion and abduction while on bed rest) can cause pain in the shoulders and ROM limitations. UEs should be intermittently positioned in 80 degrees of shoulder abduction, external rotation with scapular depression, and full elbow extension to assist in alleviating this common problem. The forearm should be positioned in forearm pronation because the client is at risk for supination contractures, such as at the C5 level. At Santa Clara Valley Medical Center, the OT department has designed and fabricated a device that can be used to maintain the arm in an appropriate position while the patient is immobilized on a kinetic bed (see Figure 36-2).
Selection of appropriate splint style and accurate fabrication and fit of the splint by the occupational therapist enhance client acceptance and optimal functional gain. If musculature is not adequate to support the wrist and hands properly (radial wrist extensors—extensor carpi radialis longus [ECRL] and extensor carpi radialis brevis [ECRB]) below 3+ (F+) for functional or cosmetic reasons, splints should be fabricated to support the wrist properly in extension and the thumb in opposition and to maintain the thumb web space while allowing the fingers to flex naturally at the metacarpophalangeal (MP) and proximal interphalangeal (PIP) joints. Splints should be dorsal rather than volar in design to allow maximal sensory feedback while the patient’s hand is resting on any surface. If at least 3+ (F+) strength of wrist extension is present, a short opponens splint should be considered to maintain the web space and support the thumb in opposition. This splint can be used functionally while the client is trained to use a tenodesis grasp.
Active and active-assisted ROM of all joints should be performed within strength, ability, and tolerance levels. Muscle re-education techniques for wrists and elbows should be employed when indicated. Progressive resistive exercises for wrists may be carried out. The client should be encouraged to engage in self-care activities such as feeding, hygiene, and keyboard and writing activities if possible, using simple devices such as a universal cuff or a custom writing splint. Even though the client may be immobilized in bed, discussion of anticipated durable medical equipment (DME), home modifications, and caregiver training should be initiated to allow sufficient time to prepare for discharge. When indicated, bedside activities that might be of interest to the client, such as modified call systems, laptop computer setup on bed tables, and avocational activities can be explored.
During the immobilization phase of Laurence’s rehabilitation, he was given a U-cuff for self-feeding, which was fitted over his wrist cast. A typing splint was fabricated for him for page turning and computer use while he was lying on his side in bed.
Active Phase
During the active, or mobilization, phase of the rehabilitation program, the client can sit in a wheelchair and should begin developing upright tolerance. A high priority at this time is determining a method of relieving sitting pressure for the purpose of preventing decubitus ulcers, or pressure sores, on the ischial, trochanteric, and sacral bony prominences. If the client has quadriplegia yet has at least F+ (3+) shoulder and elbow strength bilaterally, pressure can be relieved on the buttocks by leaning the client forward over the feet. Simple cotton webbing loops are secured to the back frame of the wheelchair (Figure 36-5). A person with low quadriplegia (C7 with F+ or better triceps) or a person with paraplegia with intact UE musculature can perform a full depression weight shift off the arms or wheels of the wheelchair. Some clients with C6 quadriplegia can also perform this type of weight shift by mechanically locking the elbows in extension while simultaneously externally rotating the shoulders and using their strong shoulder muscles to support their weight. Weight shifts should be performed every 30 to 60 minutes until skin tolerance is determined.

FIGURE 36-5 Forward weight shift using loops attached to wheelchair frame. A client with C6-level quadriplegia with symmetrical grade 4 deltoids and biceps and wrist extensors.
Active and passive ROM exercises should be continued regularly to prevent undesirable contractures. Splinting or casting of the elbows may be indicated to correct contractures that are developing. Some clients will have active wrist extension, which will be used to substitute for absent grasp through tenodesis action of the long finger flexors. With these clients, it is desirable to develop some tightness in these tendons to give some additional tension to the tenodesis grasp. The desirable contracture is developed by ranging finger flexion with the wrist fully extended and finger extension with the wrist flexed, thus never allowing the flexors or extensors to be in full stretch over all of the joints that they cross (Figure 36-6).14
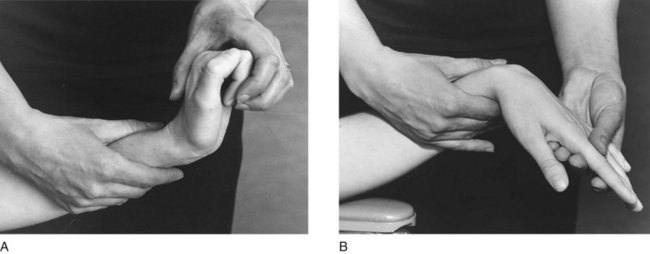
FIGURE 36-6 Tenodesis action. A, Wrist is extended when fingers are passively flexed. B, Wrist is flexed when fingers are passively extended.
Elbow contractures should never be allowed to develop. Full elbow extension is essential for allowing propping to maintain balance during static sitting and for assisting in transfers. With zero triceps strength, a person with C6-level quadriplegia can maintain forward sitting balance by shoulder depression and protraction, external rotation, full elbow extension, and full wrist extension (Figure 36-7).
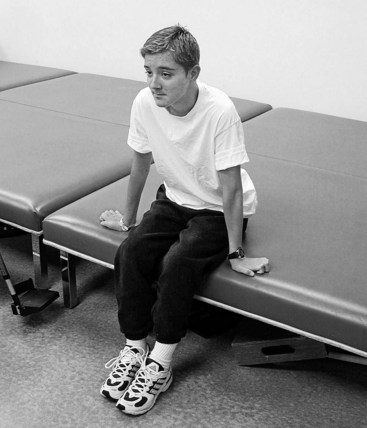
FIGURE 36-7 A client with C6-level quadriplegia; forward sitting balance is maintained (without triceps) by locking elbows. This is a valuable skill for maintaining sitting balance, bed mobility, and transfers. (Courtesy of Luis Gonzalez, Media Resource Department, Santa Clara Valley Medical Center.)
Progressive resistive exercise and resistive activities can be applied to innervated and partially innervated muscles. Shoulder musculature should be exercised so as to promote proximal stability, with emphasis on the latissimus dorsi (shoulder depressors), deltoids (shoulder flexors, abductors, and extensors), and the remainder of the shoulder girdle and scapular muscles. The triceps, pectoralis, and latissimus dorsi muscles are needed for transfers and for shifting weight when in the wheelchair. Wrist extensors should be strengthened to maximize natural tenodesis function, thereby maximizing the necessary prehension pattern in the hand for functional grasp and release. Strengthening wrist extensors also increases the client’s ability to use the tenodesis splint more effectively, mechanically transferring the strength of the wrist extensors to the finger pieces of the splint for a stronger pinch.
The intervention program should be graded to increase the amount of resistance that can be tolerated during activity. As muscle power and endurance improve, increasing the amount of time in wheelchair activities will help the patient participate in activities and occupation throughout the day.
Many assistive devices and equipment items can be useful to the person with SCI. However, every attempt should be made to have the client perform the task with no equipment or with as little as possible. Modified techniques are available that enable an individual to perform efficiently without the need for expensive or bulky equipment.
When appropriate, the universal cuff for holding eating utensils, toothbrushes, pens, and typing sticks is a simple and versatile device that offers increased independence. A wrist cock-up splint to stabilize the wrist with attachment of the universal cuff may be useful for clients with little or no wrist extension. A plate guard, cup holder, extended straw with straw clip, and nonskid table mat can facilitate independent feeding. A wash mitt, soap holder, or soap-on-a-rope appears to make bathing easier; however, the added difficulty of donning and doffing such equipment must be considered. A sliding board is a valuable option for safe transfers. Through intervention, optimal muscle strength and coordination can occur, enabling the client to outgrow the use of initially necessary equipment.
During the active phase, the ADL program may be expanded to include independent feeding with devices, oral and facial hygiene, upper-body bathing, bowel and bladder care (e.g., digital stimulation and intermittent catheterization), UE dressing, and transfers using the sliding board. Communication skills in writing and using the telephone, tape recorder, stereo equipment, computer, and calculator keyboard should be an important part of the intervention program (Figure 36-8). Training in the use of the mobile arm support and overhead slings (see Chapter 30, Section II), wrist-hand orthosis (flexor hinge or tenodesis splint), and assistive devices is also part of the OT program.
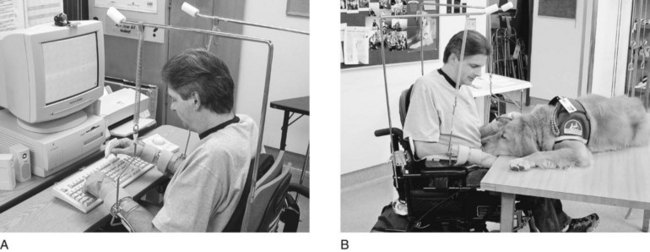
FIGURE 36-8 A, Individual with injury at C4 to C5 typing at keyboard with bilateral overhead slings, bilateral wrist splints, and typing splints. B, Use of a service dog as a treatment option to facilitate bilateral upper extremity use. (Courtesy of Luis Gonzalez, Media Resource Department, Santa Clara Valley Medical Center.)
The occupational therapist should continue to provide psychological support by allowing and encouraging the client to express frustration, anger, fears, and concerns.12 The OT clinic in an SCI center can provide an atmosphere where clients can establish support groups with other inpatients and outpatients who can share their experiences and problem-solving advice with those in earlier phases of their rehabilitation. Direct OT intervention to address psychosocial issues of SCI can include training in stress management; coping-skills training; and education regarding social connectedness, sexuality, and relationship-building strategies; and the connection between occupation and emotional health. Such intervention is particularly helpful when conducted by the occupational therapist in the supportive clinic atmosphere described previously. Occupational therapists have also found it beneficial to involve successful former clients as expert peer participants or co-leaders during such psychosocial intervention groups and individual sessions.13
The assessment, ordering, and fitting of DME such as wheelchairs, seating and positioning equipment, mechanical lifts, beds, and bathing equipment are extremely important parts of the rehabilitation program. Such equipment should be specifically evaluated, however, and ordered only when definite goals and expectations are known. Inappropriate equipment can impair function and cause further medical problems, such as skin breakdown or trunk deformity; the therapist must take into account all functional, positioning, environmental, psychological, and financial considerations in evaluating the client’s equipment needs. The desired equipment—especially wheelchairs, seat cushions, back supports, positioning devices, and bathing equipment—should be available for demonstration and trial by the client before final ordering. It is imperative that the therapist involved in the evaluation and ordering of this costly and highly individualized equipment be not only familiar but have considerable experience with currently available products and be knowledgeable in ordering equipment that will provide the client with optimal function and body positioning on a short- and long-term basis. A good working relationship with an experienced and certified assistive technology provider (ATP), a durable medical equipment vendor who assists in selection of custom assistive technology for the consumer’s needs, and provides training in the use of the selected device(s) is preferable. Advancements in technology and design have provided a wide variety of equipment from which to choose, and working with another professional specializing in such equipment will help ensure correct selection and fit. (See Chapter 11, Section II, for a more detailed discussion of wheelchairs, seating, and positioning equipment.)
In addition to enhancing respiratory function by supporting the client in an erect, well-aligned position that maximizes sitting tolerance and optimizes UE function, wheelchair seating must assist in the prevention of deformity and pressure sores. An appropriate and adequate wheelchair cushion helps distribute sitting pressure, assists in the prevention of pressure sores, stabilizes the pelvis as necessary for proper trunk alignment, and provides comfort. Whether it is the occupational therapist’s or the physical therapist’s role to evaluate and order the wheelchair and cushion, both should work closely together to ensure consistent training and use for the individual needs of each client.
The intervention and equipment needs of clients with high-level SCI (C4 and above) are unique and extremely specialized, ranging from mouthsticks and assistive technology to ventilators and sophisticated power wheelchairs and drive systems (see Table 36-1, levels C1-C3, and C3-C4). Commercially available products such as cell phones, electronic readers, and notebook computers have greatly enhanced the options available to high-level quadriplegics.
TABLE 36-1
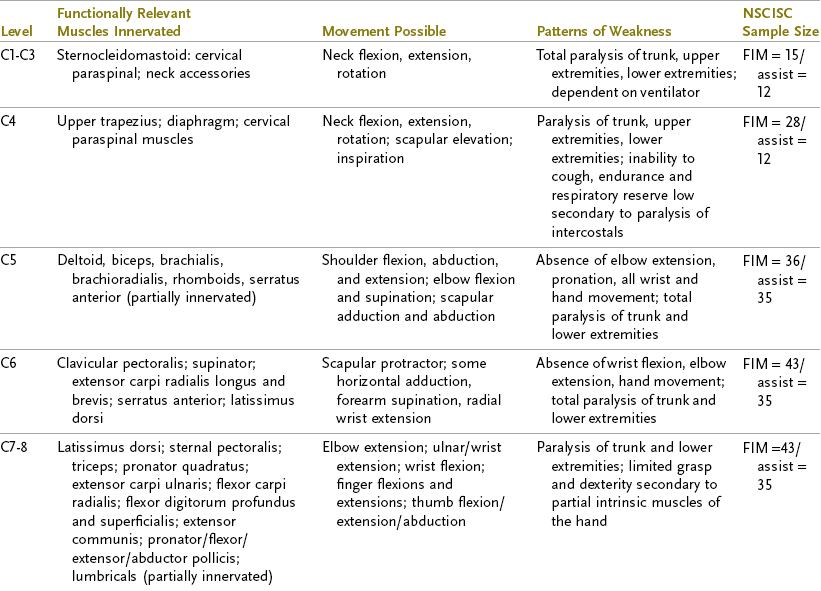
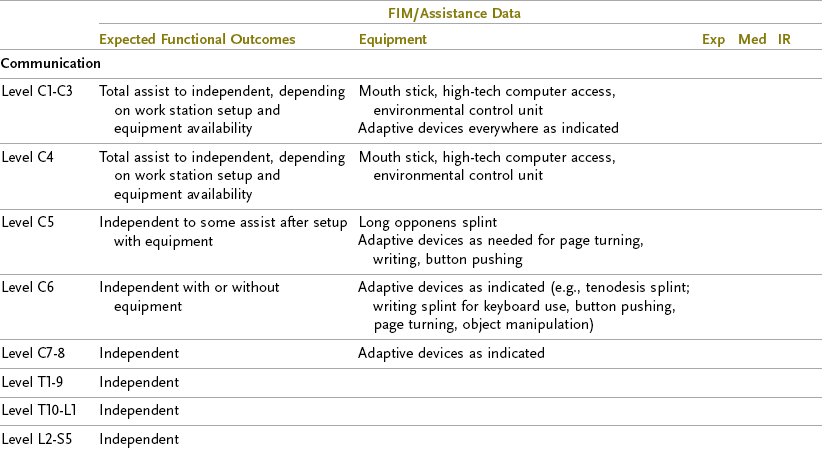
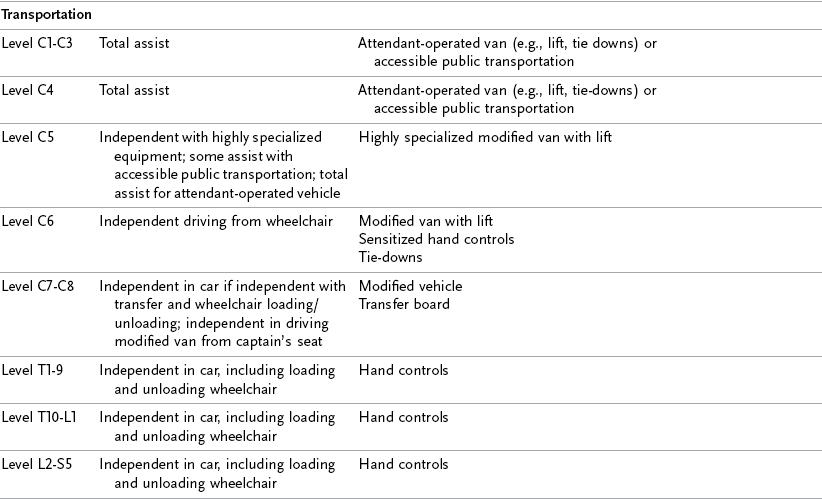
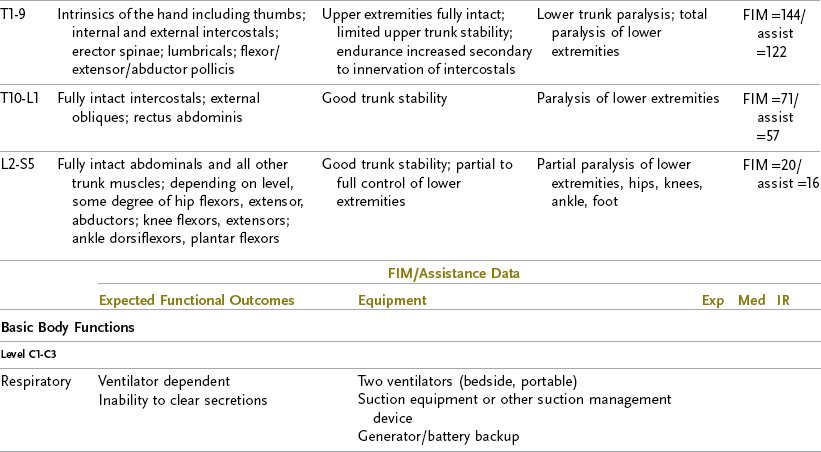
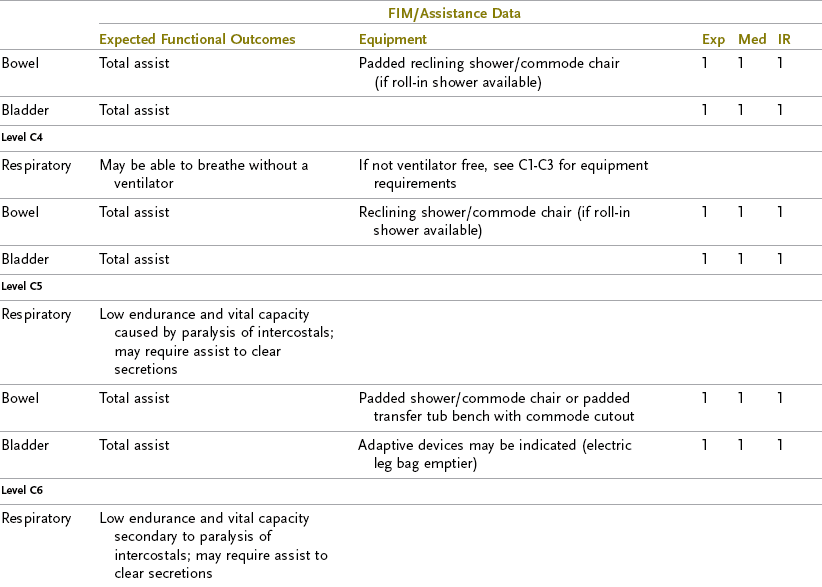
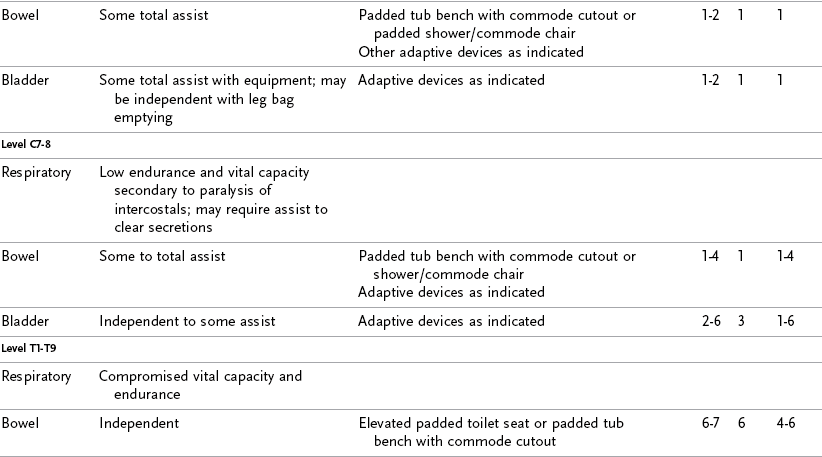
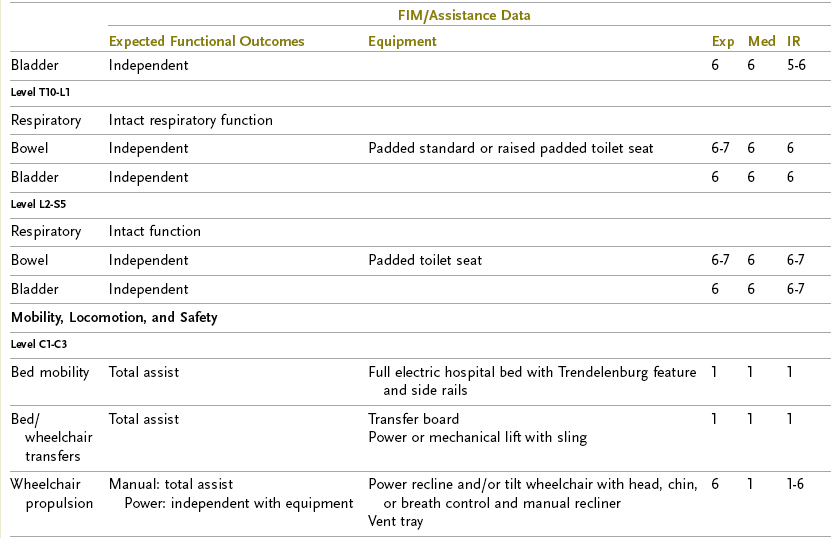
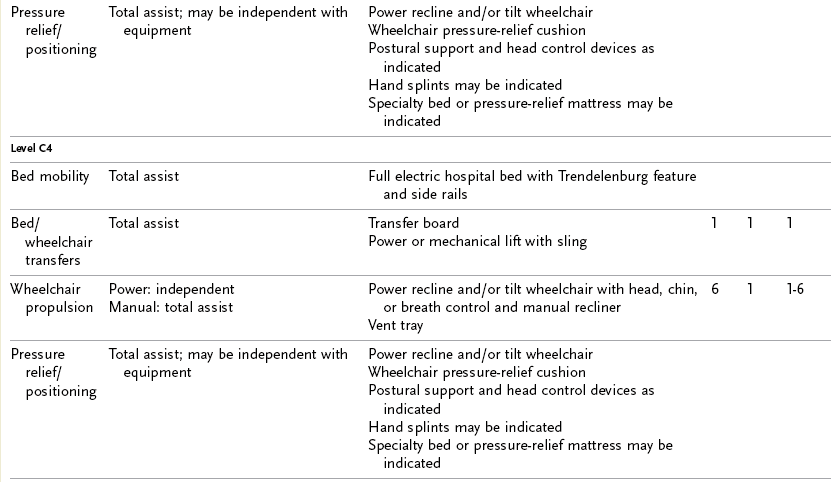
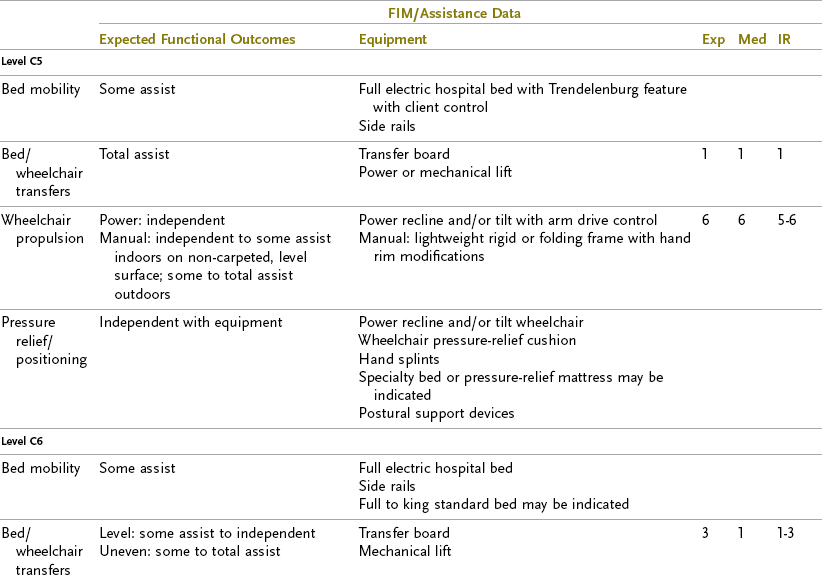

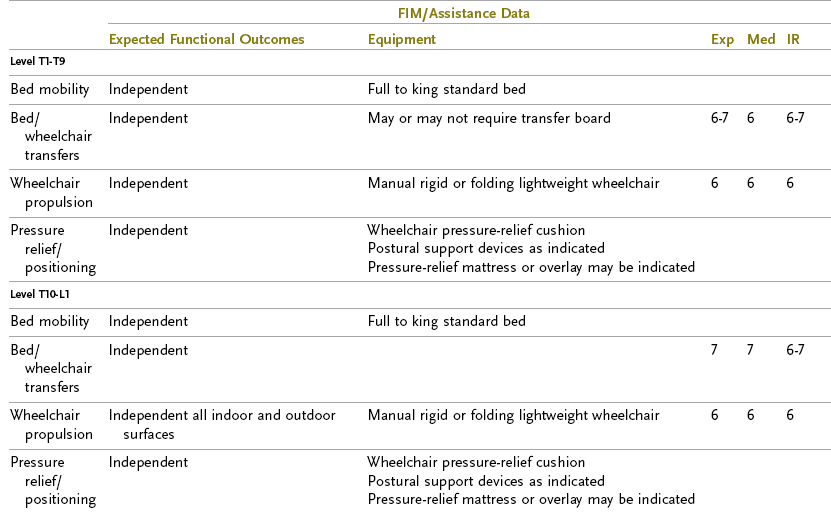
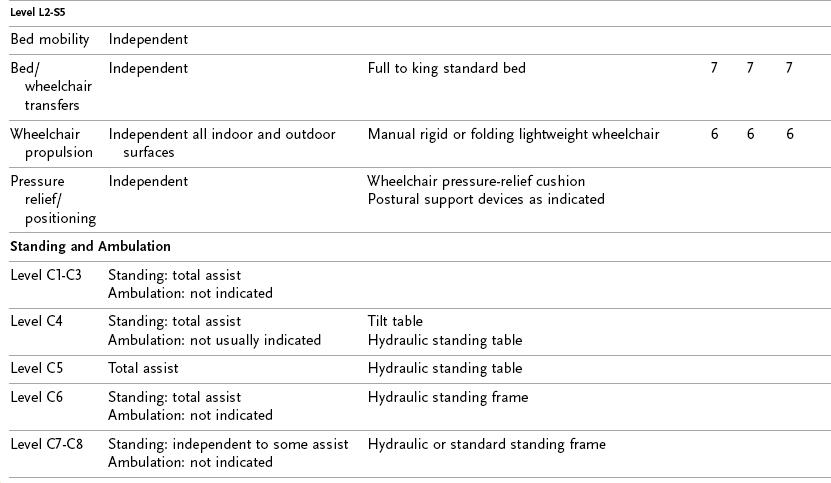
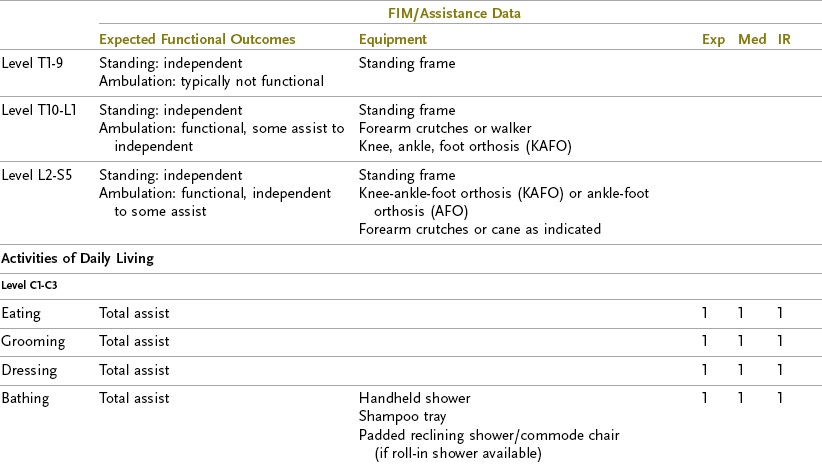
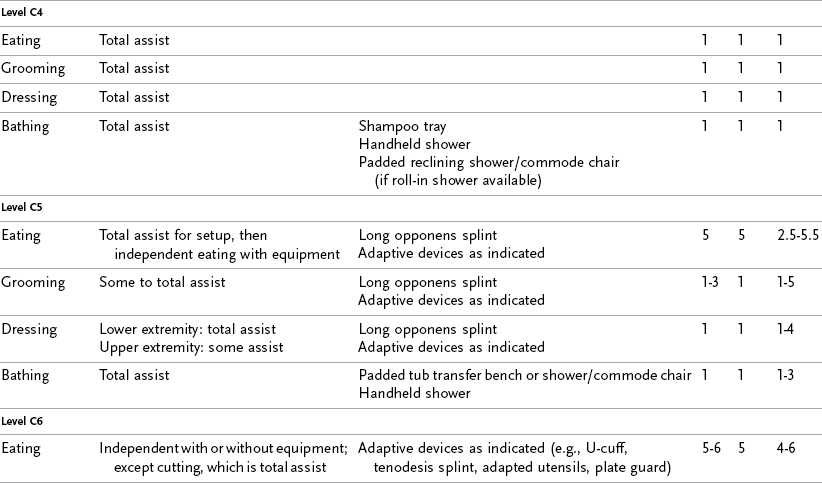
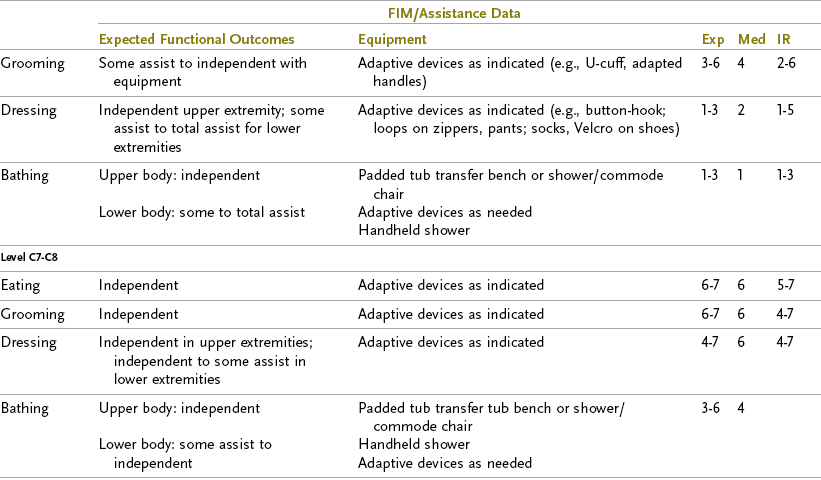
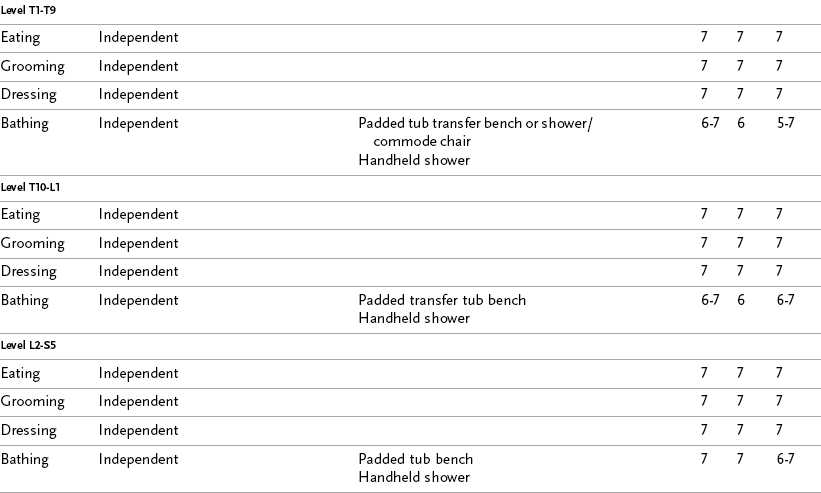
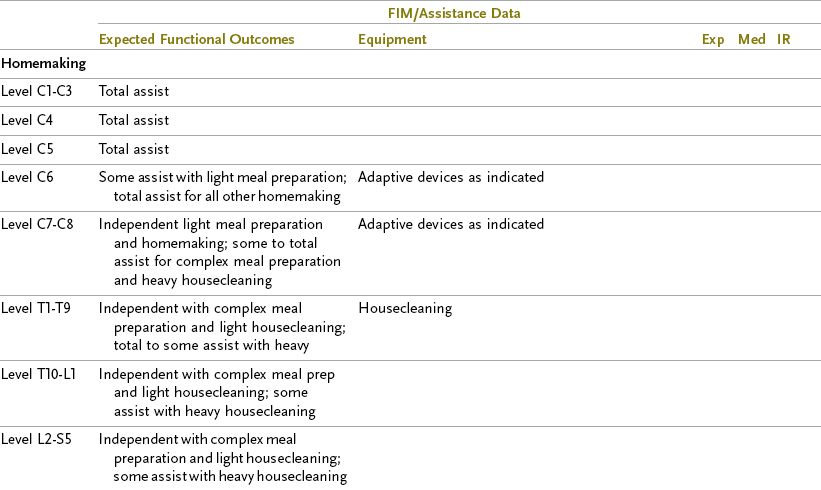
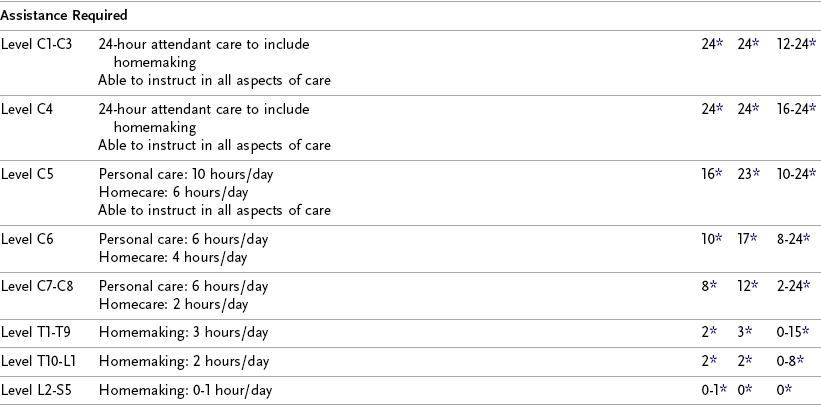
FIM/assistance data: Exp, expected FIM score; Med, NSCISC median; IR, NSCISC Interquartile Range.
*Hours per day.
The use of experienced resources in determining appropriate short- and long-term goals and equipment needs enhances the quality and functional ability of a client who otherwise would be quite dependent. Rehabilitation centers specializing in the care of persons with high-level quadriplegia should be sought for their expertise in addressing all aspects of care for this unique client population.
When the discharge location is determined and the individual can tolerate leaving the hospital for a few hours, a home evaluation should be performed. The therapist, client, and family members can then view and attempt activities in the home in anticipation of return to a safe and accessible environment.
Accompanied by his occupational therapist, Laurence went to his new rental home to determine its safety and accessibility in light of his mobility and ADL needs. Modifications to both the front and rear entrances, as well as bathroom modifications, were recommended. He and his therapist discussed the recommendations with the contractor who would be performing the work on the house to determine the feasibility of door widening and ramping in terms of the house’s structural stability. It was important that Laurence participate in the plans not only because he needed to manage this part of his life but also because he needed to learn about regulations related to the Americans with Disabilities Act (ADA) and his rights as a renter (see Chapter 15). Laurence took control of managing his housing needs, as well as his discharge supplies and follow-up services. His sense of helplessness was subsiding as he began to assume control of his life again.
After Discharge from Acute Rehabilitation
Decreases in the amount of time devoted to inpatient rehabilitation have moved the extended phase of intervention to an outpatient basis or home therapy context. Adaptive driving, home management, leisure activities, and work skill assessments using hand- or power-based tools are feasible and appropriate intervention modalities for evaluating and increasing UE strength, coordination, and trunk balance; however, they may not be a priority during inpatient hospitalization. OT training in such activities can improve the client’s socialization skills and can also assess and improve problem-solving skills and potential work habits.
OT services can offer valuable evaluation and exploration of the vocational potential of persons with SCI. Because of the sheer magnitude of the physical disability, vocational possibilities for clients with high levels of SCI are limited. Many clients must change their vocation or alter former vocational goals. Decreased motivation, threat of loss of health benefits, and lack of perseverance on the part of many patients make vocational rehabilitation challenging.
The occupational therapist can assess the client’s level of motivation, functional aptitudes, attitudes, interests, and personal vocational aspirations during the process of the intervention program and through the use of ADLs, IADLs, mobility, and work simulation occupations. The therapist can observe the client’s attention span, concentration, problem-solving ability, judgment, and other high-level cognitive functions, as well as his or her manual ability with splints and devices, accuracy, speed, perseverance, work habits, and work tolerance level. The therapist can serve as a liaison between the client and the vocational rehabilitation counselor by offering valuable information gleaned from observation during the client’s performance of activities and occupations. When suitable vocational objectives have been selected, they may be pursued in an educational setting or in a work setting, usually out of the realm of OT.
Aging with Spinal Cord Injury
Following survival of acute SCI, the primary goal of rehabilitation is independence. Independence as the measure of quality of life for people with disabilities is a concept accepted and often perpetuated by professionals and survivors alike.15
Occupational therapists work in concert with these clients to identify and prioritize their favored and meaningful occupations and provide intervention to enable them to resume their engagement in these occupations for participation in a satisfying life. Occupational therapists treating clients with SCI have considerable responsibility in influencing the level of independence, whether in the acute setting, during active rehabilitation, or in follow-up care throughout the life of the client. Understanding the aging process in both able-bodied individuals and those with disabilities is necessary for providing appropriate options and fostering attitudes that enhance the quality of the client’s life at any age.
Physical aging is a natural, inevitable process. The signs of the process can occur at varying rates for each individual, and aging affects most systems of the body (see Chapter 46). In individuals with SCI, aging is usually accelerated by the secondary effects of the disability, such as the presence of muscle imbalance, infections (urinary and respiratory), deconditioning, pain, and joint degeneration secondary to overuse.12,17 Issues to be considered at an age much earlier than normal are urinary problems brought on by years of catheterization, bladder infections, and urinary retention. Also to be considered are osteoporosis, arthritis and joint degeneration, constipation, weakening of already precarious skin, substance abuse, and the need for an increasing amount of personal care over time.
Approximately 20 years after injury appears to be a point at which some of the aging problems begin to increase. Because at least one of four SCI survivors experienced an SCI more than 20 years ago,15 a significant portion of SCI survivors are prematurely experiencing the problems of aging. Individuals with SCI onset in their later years have very different patterns of functional outcomes, program needs, and financial resources than do those with onset in their earlier years. For someone who acquired quadriplegia in his or her 20s, when the majority of SCIs occur, the degenerating conditions of normal aging become evident prematurely, usually before the 40s.4 Thus, someone who was independent during transfers at home and the loading of a wheelchair in and out of the car may now require assistance getting in and out of bed; because his or her shoulders have deteriorated, this person may have to trade the car for a van that requires costly modifications. Similarly, someone who is at a level normally associated with functional independence (e.g., T10-level paraplegia) may, in fact, need personal care assistance and possibly a power wheelchair because of degenerative changes in shoulders, elbows, and wrists. The occupational therapist should make good trunk alignment and seating a priority from the onset to prevent fixed trunk and pelvic deformities such as kyphosis and scoliosis, which can lead to considerable skin problems and uncorrectable cosmetic deformities years later. In addition, it is necessary to be aware of how the lightest possible weight of a manual wheelchair and the optimal distance from shoulder to push rim when propelling a chair can positively affect a weak or imbalanced shoulder complex. Also to be considered is the advantage of the cardiopulmonary conditioning that such an activity can provide. The occupational therapist must simultaneously consider those benefits while weighing the benefit of a power wheelchair for joint and energy conservation.
When SCI is compounded by the increased fatigue and weakness often associated with normal aging, the functional status of the individual with SCI may decline. Occupational therapists may cite this change to justify additional services or equipment. Many considerations must be weighed to make appropriate short- and long-term decisions. Consulting experienced experts, who have a perspective on both acute and long-term injuries and issues, can provide valuable insight into intervention decisions.
Research
Current research conducted in clinical settings and scientific laboratories around the world focuses on understanding the nature of SCI and defining the nervous system’s response to this injury. There is now a sense of optimism in the scientific community that it will be possible someday to restore function after SCI. This optimism is based on the combined research efforts of scientists in many disciplines. It is important for occupational therapists treating SCI to be aware of the scientific and technological advances so as to better educate clients, while at the same time providing them with the most realistic and comprehensive rehabilitation interventions for their immediate and long-term needs.
Summary
SCI can result in substantial paralysis of the limbs and trunk. The degree of residual motor and sensory dysfunction depends on the level of the lesion, whether the lesion was complete or incomplete, and the area of the spinal cord that was damaged.
After an SCI, bony realignment and stabilization are established surgically, by way of an external immobilization device, or through a combination of both methods. The many possible complications of SCI include skin breakdown, rapid loss of bone density, and spasticity.
The goal of OT is to facilitate the client’s achievement of optimal independence and functioning. Areas of focus are physical restoration of available musculature; self-care; independent living skills; short- and long-term equipment needs; environmental accessibility; and educational, work, and leisure activities. The psychosocial adjustment of the client is instrumental, and the occupational therapist offers emotional support and intervention toward this end in every phase of the rehabilitation program.
Table 36-1 presents expectations of functional performance of SCI at 1 year after injury and at each of the eight levels of injury (C1-C3, C4, C5, C6, C7-C8, T1-T9, T10-L1, L2-S5). The outcomes reflect a level of independence that can be expected of a person with motor-complete SCI, given optimal circumstances.
The categories presented reflect expected functional outcomes in the areas of mobility, ADLs, instrumental activities of daily living (IADLs), and communication skills. The guidelines are based on the consensus of clinical experts, available literature on functional outcomes, and data compiled from Uniform Data Systems (UDS) and the National Spinal Cord Injury Statistical Center (NSCISC).
Within the functional outcomes for people with SCI listed in Table 36-1, essential ADLs and IADLs, including the attendant care likely to be needed to support the predicted level of independence at 1 year after injury, have been identified. These outcome areas include the following categories of ADLs and IADLs:
• Respiratory, bowel, and bladder function. The neurologic effects of SCI may result in deficits in the ability to perform basic body functions. Respiratory function includes the ability to breathe with or without mechanical assistance and to adequately clear secretions. Bowel and bladder function includes the ability to manage elimination, maintain perineal hygiene, and adjust clothing before and after elimination. Adapted or facilitated methods of managing these bodily functions may be required to attain expected functional outcomes.
• Bed mobility, bed/wheelchair transfers, wheelchair propulsion, and positioning/pressure relief. The neurologic effects of SCI may result in deficits in the ability of the individual to perform the activities required for mobility, locomotion, and safety. Adapted or facilitated methods of managing these activities may be required to attain expected functional outcomes in standing and ambulation.
• Standing and ambulation. SCI may result in deficits in the ability to stand for exercise or psychological benefit or to ambulate for functional activities. Adapted or facilitated methods of management may be outcomes in standing and ambulation.
• Eating, grooming, dressing, and bathing. The neurologic effects of SCI may result in deficits in the ability of the individual to perform these ADLs. Adapted or facilitated methods of managing ADLs may be necessary to attain expected functional outcomes.
• Communication (keyboard use, handwriting, and telephone use). The neurologic effects of SCI may result in deficits in the ability to communicate. Adapted or facilitated methods of communication may be required to attain expected functional outcomes.
• Transportation (driving, attendant-operated vehicle, and public transportation). Transportation activities are critical for individuals with SCI to become maximally independent in their community. Adaptations may be required to help the individual meet the expected functional outcomes.
• Homemaking (meal planning and preparations and home management). Adapted or facilitated methods of managing homemaking skills may be required to attain expected functional outcomes. Individuals with complete SCI at any level will require some level of assistance with some homemaking activities. The hours of assistance required for homemaking activities are presented in Table 36-1.
• Assistance required. Table 36-1 lists the number of hours that may be required from a caregiver to assist with personal care and homemaking activities. Personal care includes hands-on delivery of all aspects of self-care and mobility, as well as safety interventions. Homemaking assistance is also included in the recommendation for hours of assistance and includes activities previously presented. The number of hours presented in both the panel recommendations and the self-reported Craig Handicap Assessment and Reporting Technique (CHART) data is representative of skilled and unskilled and paid and unpaid hours of assistance. The 24-hour-a-day requirement noted for the C1 through C3 and C4 levels includes the expected need for unpaid attendant care to provide safety monitoring.
• Adequate assistance is required to ensure that the individual with SCI can achieve the outcomes set forth in Table 36-1. The hours of assistance recommended do not reflect changes in assistance required over time, as reported by long-term survivors of SCI, nor do they take into account the wide range of individual variables that may affect the required hours of assistance. The Functional Independence Measure (FIM) estimates are widely variable in several of the categories. Whether the representative individuals with SCI in the individual categories attained the expected functional outcomes for their specific level of injury is unclear, as is whether there were mitigating circumstances, such as age, obesity, or concomitant injuries, that would account for variability in assistance reported. An individualized assessment of needs is required in all cases.
• Equipment requirements. Minimum recommendations for DME and adaptive devices are identified in each of the functional categories. The most commonly used equipment is listed, with the understanding that variations exist among SCI rehabilitation programs and that use of such equipment may be necessary to achieve the identified functional outcomes. Additional equipment and devices that are not critical for the majority of individuals at a specific level of injury may nonetheless be required for some individuals. The equipment descriptions are generic to allow for variances in program philosophy and financial resources. Rapid changes and advances in equipment and technology will be made and therefore must be considered.
• Healthcare professionals should remember that the recommendations set forth in Table 36-1 are not intended to be prescriptive; rather, they should serve as a guideline. The importance of completing an individual functional assessment of people with SCI before making equipment recommendations cannot be overemphasized. All DME and adaptive devices must be thoroughly assessed and tested to determine medical necessity, to prevent medical complications (e.g., postural deviations, skin breakdown, pain), and to foster optimal functional performance. Environmental control units and telephone modifications may be needed for safety and maximal independence, and each person must be individually evaluated to determine the need for this equipment. Recommendations for disposable medical products are not included in this document.
• FIM. Evidence for the specific levels of independence provided in Table 36-1 relies both on expert consensus and on data from FIM in large-scale, prospective, and longitudinal research conducted by NSCISC. FIM is the most widely used disability measure in rehabilitation medicine, and although it may not incorporate all of the characteristics of disability in individuals recovering from SCI, it captures many basic disability areas.
• FIM consists of 13 motor and five cognitive items that are individually scored from 1 to 7. A score of 1 indicates complete dependence, and a score of 7 indicates complete independence (Box 36-1). The sum of the 13 FIM motor score items can range from 13, indicating complete dependence for all items, to 91, indicating complete independence for all items. FIM is a measure usually completed by health care professionals; different observers, including the client, family members, and caregivers, can contribute information to the ratings. Each of these reporters may represent a different type of potential bias.
• Although the sample sizes of FIM data for certain neurologic level groups are quite small, the consistency of the data suggests that the interpretation is reliable. Other pertinent data regarding functional independence must be factored into outcome analyses, including medical information, patient factors, social role participation, quality of life, and environmental factors and supports.
• In Table 36-1, FIM data, when available, are reported in three areas. First, the expected FIM outcomes are documented on the basis of expert clinical consensus. The second number reported is the median FIM score, as compiled by NSCISC. The interquartile range for NSCISC FIM data is the third set of numbers. In total, the FIM data represent 1-year postinjury FIM assessments of 405 survivors with complete SCI and a median age of 27 years. The NSCISC sample size for FIM and Assistance Data is provided for each level of injury. Different outcome expectations should clearly apply to different client subgroups and populations. Some populations are likely to be significantly older than the referenced one. Functional abilities may be limited by advancing age.14,17
• Home modifications. To provide the best opportunity for individuals with SCI to achieve the identified functional outcomes, a safe and architecturally accessible environment is necessary. An accessible environment must take into consideration, but not be limited to, entrance and egress, mobility in the home, and adequate setup to perform personal care and homemaking tasks.
1. List three causes of SCI. Which is most common?
2. Describe the patterns of weakness in quadriplegia and paraplegia.
3. Describe the functional and prognostic differences between complete and incomplete lesions.
4. When reference is made to C5 in quadriplegia, what is meant in terms of level of injury and functioning muscle groups?
5. What are the characteristics of spinal shock?
6. What physical changes occur after the spinal shock phase?
7. What is the prognosis for recovery of motor function in complete lesions and incomplete lesions?
8. What are the purposes of surgery in management of SCI?
9. What are some medical complications common among clients with SCI that can limit achievement of functional potential?
10. How should postural hypotension be treated?
11. How should autonomic dysreflexia be treated?
12. What is the role of the occupational therapist in the prevention of pressure sores?
13. Why is vital capacity affected in individuals with SCI?
14. What effect does reduced vital capacity have on the rehabilitation program?
15. Which level of injury features full innervation of the rotator cuff musculature, biceps, and extensor carpi radialis and partial innervation of the serratus anterior, latissimus dorsi, and pectoralis major?
16. What additional muscle power does the client with C6-level quadriplegia have over the client with C5-level quadriplegia? What is the major functional advantage of this additional muscle power?
17. What are the additional critical muscles that the client with C7-level quadriplegia has, as compared with the client with C6-level quadriplegia?
18. What additional functional independence can be achieved because of this additional muscle power?
19. What is the first spinal cord lesion level that features full innervation of the UE musculature?
20. Which assessments do occupational therapists use to evaluate the client with SCI? What is the purpose of each?
21. List five goals of OT for the client with SCI.
22. How is wrist extension used to affect grasp by the individual with quadriplegia?
23. How does the individual with C6-level quadriplegia substitute for the absence of elbow extensors?
24. What contracture is encouraged in clients with SCI? Why? How is it developed?
25. What splint allows the client with C6-level quadriplegia to achieve functional prehension?
26. What are some of the first self-care activities that the client with a C6-level SCI should be expected to accomplish?
27. List four assistive devices commonly used by persons with quadriplegia, and tell the purpose of each.
28. How can ordering an ill-fitting wheelchair affect the UE function and skin care of someone with C6-level quadriplegia?
29. Describe the role of OT in the vocational evaluation of a client with SCI.
30. What are two considerations when predicting the future functional outcomes for a 25-year-old client with T4-level paraplegia?
31. Why would a person with paraplegia require homemaking assistance if he is independent in all self-care and mobility activities?
References
1. Amador, J. Contemporary information regarding male infertility following spinal cord injury. SCI Nursing. 1998;15(3):61.
2. Bromley, I. Tetraplegia and paraplegia: a guide for physiotherapists, ed 5. New York: Churchill Livingstone; 1998.
3. Consortium for Spinal Cord Medicine, Paralyzed Veterans of America. Outcomes following traumatic spinal cord injury: clinical practice guidelines for health-care professionals. Washington, DC: The Consortium; 1999.
4. Frankel, H, et al. The value of postural reduction in the initial management of closed injuries to the spine with paraplegia and tetraplegia. Paraplegia. 1969;7:179.
5. Freed, MM. Traumatic and congenital lesions of the spinal cord. In: Kottke FJ, Lehmann JF, eds. Krusen’s handbook of physical medicine and rehabilitation. Philadelphia: WB Saunders, 1990.
6. Gerhart, KA, et al. Quality of life following spinal cord injury: knowledge and attitudes of emergency care providers. Ann Emerg Med. 1994;23(4):807.
7. Hanak, M, Scott, A. An illustrated guide for health care professionals, ed 2. New York: Springer-Verlag; 1993.
8. Heinemann, AW, et al. Mobility for persons with spinal cord injury: an evaluation of two systems. Arch Phys Med Rehabil. 1987;68(2):90.
9. Hill JP, ed. Spinal cord injury: a guide to functional outcomes in occupational therapy. Rockville, MD: Aspen, 1987.
10. Institute for Medical Research, Santa Clara Valley Medical Center: Severe head trauma, a comprehensive medical approach, Project 13-9-59156/9 (Report to National Institute for Handicapped Research), Nov 1982.
11. Lammertse, D. Why some injured people get better and others don’t. In: Maddox S, ed. Spinal network. Boulder, CO: Spinal Network, 1987.
12. Paulson S, ed. Santa Clara Valley Medical Center spinal cord injury home care manual, ed 3, San Jose, CA: Santa Clara Valley Medical Center, 1994.
13. Pendleton, HMcH, Schultz-Krohn, W. Psycho-social issues of physical disability. In: Cara EM, MacRae A, eds. Psychosocial occupational therapy in clinical practice. New York: Delmar, 2005.
14. Penrod, LE, Hegde, SK, Ditunno, JFJr. Age effect on prognosis for functional recovery in acute traumatic central cord syndrome (CCS). Arch Phys Med Rehabil. 1990;71(12):963.
15. Pierce, DS, Nickel, VH. The total care of spinal cord injuries. Boston: Little, Brown; 1977.
16. Spencer, EA. Functional restoration. In Hopkins HL, Smith HD, eds.: Willard and Spackman’s occupational therapy, ed 8, Philadelphia: JB Lippincott, 1993.
17. Yarkony, GM, et al. Spinal cord injury rehabilitation outcomes: the impact of age. J Clin Epidemiol. 1988;41(2):173.
Suggested Key Words and Websites
pva.org. Consortium for Spinal Cord Injury: A resource guide for veterans who are paralyzed; the site includes information about support groups, activities, and sporting events
spinalcord.uab.edu. Spinal Cord Injury Information Network: Provides links to educational resources, government agencies, national organizations, and commercial products for those with SCI
disaboom.com. Provides resources, including information on rights, advocacy, and wellness, for people with disabilities
sciinfopages.com. Contains a resource directory for people with SCI. Topics include adaptive technology, travel and leisure, SCI organizations, and more
aparalyzed.com. Contemporary forums and online library for people with spinal cord injuries
spinalinjury.net. Explains basic anatomy, physiology, and complications associated with spinal cord injury. Topics such as rehabilitation and living with a spinal cord injury are discussed
christopherreeve.org. Christopher and Dana Reeve Association: The association promotes research in the area of SCI. The website includes information on current research. The association provides research grants, information, and advocacy for those living with SCI
Adler, C. Equipment considerations. In: Whiteneck GG, Adler C, Carter E, eds. The management of high quadriplegia. New York: Demos, 1989.
Baer, RW. Is Fred dead? A manual on sexuality for men with spinal cord injuries. Pittsburgh, PA: Dorrance; 2003.
Bergen, A, Presperin, J, Tallman, T. Positioning for function. Valhalla, NY: Valhalla Rehabilitation; 1990.
Field-Fote, EC. Spinal cord injury rehabilitation (contemporary perspectives in rehabilitation). Philadelphia: FA Davis; 2009.
Ford, JR, Duckworth, B. Physical management for the quadriplegic patient. Philadelphia: FA Davis; 1974.
Gerhart, KA, Koziol-McLain, J, Lowenstein, SR, Whiteneck, GG. Quality of life following spinal cord injury: knowledge and attitudes of emergency care providers. Ann Emerg Med. 1994;23(4):807–812.
Hill, JP. Spinal cord injury: a guide to functional outcomes in occupational therapy. Rockville, MD: Aspen; 1986.
Klein, SD, Karp, G. From there to here: stories of adjustment to spinal cord injury. Baltimore, MD: No Limits Communications; 2004.
Mayo Clinic. Guide to living with a spinal cord injury: moving ahead with your life. New York: Demos Health; 2009.
Palmer, S, Kriegsman, KH, Palmer, JB. Spinal cord injury: a guide for living, ed 2. Baltimore: The John Hopkins University Press; 2000.
Paralyzed Veterans of America. Outcomes following traumatic spinal cord injury: clinical practice guidelines for health-care professionals. Washington, DC: Paralyzed Veterans of America; 1999.
Paralyzed Veterans of America. Preservation of upper limb function following spinal cord injury: a clinical practice guideline for health-care professionals. Washington, DC: Paralyzed Veterans of America; 2005.
Sisto, SA, Druin, E, Sliwinski, MM. Spinal cord injuries: management and rehabilitation, St. Louis. Mosby; 2009.
Somer, MF. Spinal cord injury: functional rehabilitation, ed 3. Upper Saddle River, NJ: Prentice Hall; 2009.
