chapter 7 Trunk control: supporting functional independence
After completing this chapter, the reader will be able to accomplish the following:
1. Understand the functional anatomy of the trunk.
2. Understand the control requirements for various movement patterns and activities.
3. By activity analysis, understand key components of trunk control required for independence in various activities of daily living.
4. Comprehensively evaluate trunk control and its effect on function.
5. Implement interventions to improve and compensate for loss of trunk control.
Loss of trunk control commonly occurs in patients who have had a stroke and persists into the chronic stage of recovery.52 The recovery of trunk control is varied, but during the first month after stroke, significant improvements may be observed. In contrast to common beliefs, the time course of recovery of the trunk is similar to the recovery of arm, leg, and functional ability.51
Impairments in trunk control include weakness (both contralesional and, to a lesser extent, ipsilesional), loss of stability, stiffness, and loss of proprioception, and may lead to the following:
 Dysfunction in upper and lower limb control
Dysfunction in upper and lower limb control
 Potential for spinal deformity and contracture
Potential for spinal deformity and contracture
 Impaired ability to interact with the environment
Impaired ability to interact with the environment
 Visual dysfunction resulting from head/neck malalignment
Visual dysfunction resulting from head/neck malalignment
 Symptoms of dysphagia because of proximal malalignment
Symptoms of dysphagia because of proximal malalignment
 Decreased independence in activities of daily living (ADL) and other meaningful tasks
Decreased independence in activities of daily living (ADL) and other meaningful tasks
 Decreased sitting and standing tolerance, balance, and function
Decreased sitting and standing tolerance, balance, and function
For a comprehensive review of this topic, see Chapters 4 and 5 for incorporating task-oriented, learning and environmental strategies into treatment plans focused on improving trunk control, Chapter 8 for a complete overview of the multiple variables that affect balance skills, Chapter 10 for a review on the interdependence of trunk control and upper extremity function, and Chapter 14 for an overview of mobility impairments.
Regaining trunk control has been a major focus of stroke rehabilitation for many years. Until more recently, the majority of the literature focusing on trunk control/postural control was based on expert clinicians’ observations of and treatment philosophies about trunk dysfunction after stroke. The traditional approaches to treatment7,8,17,22,40 have emphasized improved trunk control as a key element of focus in the stroke population, and this focus continues as therapists integrate current models of motor control and learning (see Chapters 4 and 6).
An overview of common trunk impairments that may interfere with daily function
While motor control studies after stroke focus primarily on upper extremity function and/or gait (see Chapters 10 and 15), there is a body of descriptive evidence that aims to give clinicians insight into the various specific trunk impairments observed after stroke.
Dickstein and colleagues20 examined anticipatory postural adjustment in trunk muscles during the performance of upper and lower limb flexion tasks in patients with hemiparesis secondary to stroke. The researchers recorded electromyographic activity of the lumbar erector spinae and of the latissimus dorsi muscles bilaterally during flexion of either arm and from the two rectus abdominis and obliquus externus muscles during flexion of either hip. The authors documented impairments in the activity of trunk muscles in the hemiparetic subjects. This was manifested in the reduced activity level of the lateral trunk muscles, in delayed onset, and in reduced synchronization between activation of pertinent muscular pairs. Further, they documented that these impairments were associated with motor and functional deficits.
Bohannon, Cassidy, and Walsh11 have studied trunk muscle strength impairments after stroke (specifically forward and lateral trunk flexion strength). Their study included 20 patients with stroke and resultant hemiparesis and 20 control subjects. Trunk strength was measured with a handheld dynamometer; subjects were seated upright during the study. Results indicated that trunk strength, whether lateral or forward, was significantly decreased in the patients relative to controls. The greatest difference in strength was in forward flexion strength. The patients demonstrated trunk weakness on the paretic side relative to the nonparetic side. The conclusion was that trunk muscle strength was impaired multidirectionally in the stroke population.
Bohannon10 studied 11 stroke patients and evaluated lateral trunk flexion strength and the effect of trunk muscle strength on sitting balance and ambulation. His results indicated that the mean lateral flexion force on the paretic side was 32.1%, which was significantly less than the mean lateral flexion force on the nonparetic side. His study further demonstrated a statistically significant correlation between sitting balance and strength of the lateral trunk flexors.
Bohannon9 also studied the recovery of trunk muscle strength after stroke in 28 subjects. Subjects’ strength was tested in a variety of directions, including forward flexion, movement toward the paretic side, and movement toward the nonparetic side. Statistical analysis demonstrated that trunk muscle strength increased significantly over time. The greatest recovery was in the direction of forward flexion. This study again verified a strong correlation between trunk muscle strength and sitting balance at the initial and final assessments.
Esparza and colleagues23 examined hemispheric specialization and the coordination of arm and trunk movements during pointing in subjects with strokes. They concluded that arm and trunk timing was disrupted compared with healthy controls, temporal coordination of trunk and arm recruitment is mediated bilaterally by each hemisphere, and that the differences they found in the range of trunk displacement between subjects with right and left lesions suggest that left hemisphere plays a greater role than the right in controlling complex arm-trunk movements.
Ryerson and colleagues43 documented trunk position sense impairments in those with poststroke hemiparesis. Specifically, individuals exhibited greater trunk repositioning error than age-matched controls. Based on this finding, the authors recommended trunk position sense retraining emphasizing sagittal and transverse movements as a potential poststroke intervention strategy to improve trunk balance and control.
In addition to the mentioned studies, several studies have focused on documenting electromyographic activity in normal subjects during a variety of tasks including trunk displacements.1,5,19,25,50,58 See Basmajian’s and DeLuca’s5 classic text for a comprehensive review of electromyographic studies performed during functional tasks.
Functional trunk anatomy
Skeletal system
This section reviews the bony components of trunk anatomy, including articulations and range of motion (ROM).
Vertebral column.
The vertebral column is made up of 26 vertebrae, which are classified as follows:
As a whole, the vertebral column from sacrum to skull is equivalent to a joint with three degrees of freedom33 in the directions of flexion and extension, right and left lateral flexion, and axial rotation. Kapandji33 has documented the ROM throughout the vertebral column (Table 7-1).
Table 7-1 Range of Motion of the Vertebral Column
| MOVEMENT | RANGE OF MOTION |
|---|---|
| Flexion | Cervical: 40 degrees Thoracolumbar: 105 degrees Total: 145 degrees |
| Extension | Cervical: 75 degrees Thoracolumbar: 60 degrees Total: 135 degrees |
| Lateral flexion | Cervical: 35 to 45 degrees Thoracic: 20 degrees Lumbar: 20 degrees Total: 75 to 85 degrees |
| Rotation | Cervical: 45 to 50 degrees Thoracic: 35 degrees Lumbar: 5 degrees Total: 85 to 90 degrees |
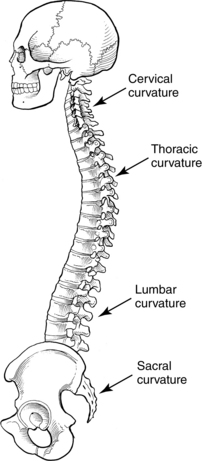
An understanding of spinal alignment is necessary for effective evaluation and treatment planning. Normal alignment of the vertebral column implies that the appropriate spinal curvatures are present. In the sagittal plane, the vertebral column shows four curvatures33 (Table 7-2 and Fig. 7-1).
| POSTERIOR MOVEMENT | |||
|---|---|---|---|
| CURVATURE | CONVEX | CONCAVE | |
| Sacral (fixed) | X | ||
| Lumbar | X | ||
| Thoracic | X | ||
| Cervical | X | ||
Pelvis
According to Kapandji,33 “The bony pelvis constitutes the base of the trunk. It supports the abdomen and links the vertebral column to the lower limbs. It is a closed osteo-articular ring made up of three bony parts and three joints.” The three bony parts include the two iliac bones and the sacrum. The three joints of the pelvis include two sacroiliac joints and the symphysis pubis. It is critical to remember that because of the firmness of the sacroiliac and lumbosacral junctions, every pelvic movement is accompanied by a realignment of the spine predominantly in the lumbar region.47
Pelvic tilt can occur anteriorly or posteriorly. In an anterior tilt, the anterior superior iliac spines of the ilia migrate anteriorly to the foremost part of the symphysis pubis. This pelvic motion accentuates the lumbar curve and results in increased hip flexion. In contrast, posterior pelvic tilt results in a “flattening” of the lumbar curve and an increase in hip extension. Lateral pelvis tilting results in a height discrepancy of the iliac crests and is accompanied by lateral spine flexion and a lateral rib cage displacement.
Rib cage
The rib cage is formed by the sternum, costal cartilage, ribs, and the bodies of the thoracic vertebrae. The rib cage protects the organs in the thoracic cavity, assists in respiration, and provides support for the upper extremities. During inspiration the ribs are elevated, and during expiration the ribs are depressed.
Although each rib has its own ROM (occurring primarily at the costovertebral joint), rib cage shifts occur with movement of the vertebral column. During column extension, the rib cage migrates anteriorly, and the ribs are elevated. During spinal flexion, the rib cage moves posteriorly, and the ribs are depressed. Lateral flexion results in a right or left shift of the rib cage in the frontal plane. Finally, rotation of the vertebral column results in one side of the rib cage moving posteriorly and movement of the opposite side anteriorly in the transverse plane.
Muscular system
Muscles of the abdominal wall
The general functions of the abdominal muscles are as follows:
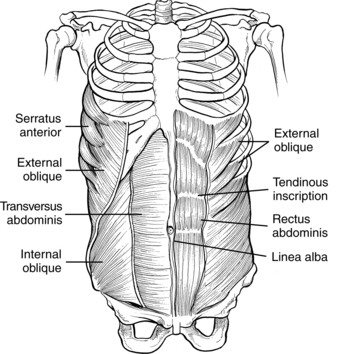
Although these muscles are situated primarily on the anterior aspect of the trunk, they also are situated laterally and slightly posteriorly, forming a girdle around the abdomen. The abdominal muscles consist of three groups: the rectus abdominis, the obliques (internal and external), and the transversus abdominis (Fig. 7-2).
Rectus abdominis.
The rectus abdominis consists of right and left sides that are separated by a fibrous band called the linea alba, which runs from the xiphoid process to the pubis.
The proximal attachment is the xiphoid process of the sternum and adjacent costal cartilage, whereas the distal attachments are the pubic bones near the pubic symphysis.47
The muscle is palpated easily in the following two cases:
1. When the subject is supine and is asked to lift the head and shoulders off the support surface in a straight plane (sit-up)
When this muscle is activated and not opposed by the extensors, the pelvis and sternum are approximated, the pelvis is pulled into a posterior tilt, and the lumbar curves flatten. Because of its multisegmental arrangement, the rectus abdominis can contract in part or as a whole, making a variety of postures possible. De Troyer’s work19 demonstrated that “abdominal muscle recruitment which naturally occurs in response to posture in most individuals does not uniformly involve the whole of the muscles.”
The rectus abdominis (and the other muscles of the trunk) require a stable origin to function efficiently.17 This stable origin can be the pelvis or thorax, depending on the posture and which part of the trunk is moving. Davies17 further explains, “The pelvis is stabilized in lying, sitting, and standing by the activity of the muscles around the hips, and in sitting and lying the stabilization is helped by the weight of the legs themselves. Stabilization of the thoracic origin for activities in which the abdominals contract to move or prevent movements of the pelvis requires selective extension of the thoracic spine.” Davies further points out that the abdominal muscles cannot function effectively when their origin and insertion are approximated (e.g., in patients with an exaggerated thoracic kyphosis). Winzeler-Mercay and Mudie57 noted weakness based on electromyographic recordings in the rectus abdominis after stroke during dynamic trunk movements such as donning shoes. The weakness was noted particularly on the involved side. Similarly, Tanaka, Hachisuka, and Ogata49 found that peak torque of the flexors was significantly less than in healthy controls.
The rectus abdominis can be self-palpated by assuming a recumbent posture in a chair (slumping in the chair) and then pulling up and forward to an aligned position. One should notice that the burst of activity diminishes when leaning forward (shoulders move in front of hips).
Obliques.
The obliques consist of three interwoven muscles: internal obliques, external obliques, and transversus abdominis.
External obliques.
The external oblique forms the superficial layer of the abdominal wall. Its fibers run an oblique course superoinferiorly and lateromedially.33 The muscle is lateral to the rectus abdominis and covers the anterior and lateral regions of the abdomen. The attachments are as follows:47
 Proximal attachment: Anterolateral portions of ribs where the muscle interdigitates with serratus anterior and slips from latissimus dorsi
Proximal attachment: Anterolateral portions of ribs where the muscle interdigitates with serratus anterior and slips from latissimus dorsi
 Distal attachment: Upper fibers run down and forward and attach to an aponeurosis that connects them to the linea alba; lower fibers attach to the crest of the ilium
Distal attachment: Upper fibers run down and forward and attach to an aponeurosis that connects them to the linea alba; lower fibers attach to the crest of the ilium
If the external oblique contracts unilaterally, the trunk rotates to the opposite side. Therefore, if one rotates to the left, the right external oblique is active and vice versa. Bilateral contraction assists in trunk flexion and a resultant posterior pelvic tilt. This muscle is also active during straining and coughing.47 The muscle is palpated easily while rotating the trunk to the opposite side.
Internal obliques.
The internal obliques also are located laterally and are covered by the external obliques. In essence, the internal obliques constitute the second layer of muscles on the abdominal wall. This muscle covers the same area as the external oblique, but its fibers cross those of the external oblique. Attachments are as follows:47
 Proximal attachment: Inguinal ligament, crest of ilium, and thoracolumbar fascia
Proximal attachment: Inguinal ligament, crest of ilium, and thoracolumbar fascia
 Distal attachments: Pubic bone, an aponeurosis connecting to linea alba, and last three or four ribs
Distal attachments: Pubic bone, an aponeurosis connecting to linea alba, and last three or four ribs
This muscle groups is activated during trunk rotation, but contraction occurs toward the same side (i.e., rotation to the left occurs following contraction of the left internal oblique). Clearly the external and internal obliques are synergists in the action of trunk rotation. The right external and left internal oblique work together to rotate the trunk to the left and vice versa. “The efficient action of the muscles of one side of the abdominal wall is therefore very much dependent upon the fixation or anchorage provided by the activity of the muscles on the other side, particularly for activities involving rotation of the trunk.”16
Tanaka, Hachisuka, and Ogata49 examined trunk rotation performance in poststroke hemiplegic subjects and found significantly lower muscle performance in the subjects compared with the health controls. No differences were found when comparing right and left rotation in terms of angular velocities, the side of hemiplegia, or gender, but muscle performance in both directions was decreased compared with controls.
The internal obliques are difficult to palpate. However, the therapist may feel tension under the fingertips when palpating the lateral abdominal wall on the side toward which the trunk is rotating. This tension is due in part to activation of the internal obliques.
Transversus abdominis.
The transversus abdominis is the deepest layer of the abdominal wall. Its fibers run transversely, and the muscle has been called the corset muscle because it encloses the abdominal cavity like a corset. Attachments are as follows:47
 Proximal attachments: Lower ribs, thoracolumbar fascia, crest of the ilium, and inguinal ligament
Proximal attachments: Lower ribs, thoracolumbar fascia, crest of the ilium, and inguinal ligament
 Distal attachments: Via an aponeurosis fuses with other abdominal muscles into linea alba
Distal attachments: Via an aponeurosis fuses with other abdominal muscles into linea alba
The main action of the transversus abdominis is forced compression; the muscle acts like a girdle to flatten the abdominal wall and compress the abdominal viscera. Weakness of this muscle permits bulging of the anterior abdominal wall, thereby indirectly leading to an increase in lordosis.38 The therapist may palpate this muscle between the lower ribs and the crest of the ilium during forced expiration.
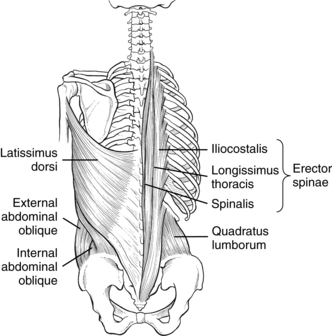
Posterior trunk muscles
The posterior trunk muscles include the quadratus lumborum, the erector spinae group, and latissimus dorsi (Fig. 7-3). The actions of this group of muscles include trunk extension, lateral flexion, rotation of the trunk, and assistance with balancing the vertebral column.
Quadratus lumborum.
The quadratus lumborum is lateral and posterior (i.e., on the posterior abdominal wall); it lies between the psoas major and the erector spinae group. The attachments are as follows:47
 Proximal attachment: Crest of ilium
Proximal attachment: Crest of ilium
 Distal attachments: Twelfth rib and transverse processes of first to third lumbar vertebrae
Distal attachments: Twelfth rib and transverse processes of first to third lumbar vertebrae
The main action of this muscle is to assist in “hip hiking.” Therefore, the muscle is active during lateral trunk flexion. The easiest way to palpate the quadratus lumborum is to have the subject prone, to palpate superior and lateral to the iliac crest, and to ask the subject to hike the hip.
Erector spinae group.
The erector spinae group of muscles is a large mass that fills the spaces between the transverse and spinous processes of the vertebrae and extends laterally covering a large portion of the posterior thorax. Multiple muscles make up this group, and they are named according to attachments, shape, and action. Muscles such as the transversospinales, the interspinales, the longissimus, and the iliocostalis are included in this group.
Collectively, these muscles connect the back of the skull to the posterior iliac crest and sacrum. Unopposed contraction of the back extensors approximates the head and the sacrum. The pelvis is pulled into an anterior tilt (accentuating the lumbar curve), and the ribs are forced to flare. These muscles also contract during lateral flexion (to balance the abdominals), and they may assist in trunk rotation during unilateral contraction (e.g., assist the trunk with rotating to the ipsilateral side). The therapist easily can palpate this muscle group with patients in the prone position if the head and shoulders are lifted from the support surface;47 palpation also is possible during forward sway in sitting or standing. The therapist easily can palpate the lower back extensors during low back extension (accentuating the lumbar curve) while the patient is sitting.
Winzeler-Mercay and Mudie57 found increased activity in the erector spinae on both sides during work activities (such as reaching and donning shoes) and at rest. This increased activity was particularly evident on the involved side. They hypothesized that this abnormal response might reflect a disruption of cortical influences on motor unit activity. Similarly, Tanaka, Hachisuka, and Ogata48 found that peak torque of the extensors was significantly less than in healthy controls.
Latissimus dorsi.
The latissimus dorsi is superficial and covers the posterior/lateral trunk. Its attachments include the following:47
 Proximal attachments: Spinous processes of T6 down, dorsolumbar fascia, posterior crest of ilium, lower ribs, interdigitations with external oblique; fibers converge toward axilla, passing over the inferior angle of the scapula.
Proximal attachments: Spinous processes of T6 down, dorsolumbar fascia, posterior crest of ilium, lower ribs, interdigitations with external oblique; fibers converge toward axilla, passing over the inferior angle of the scapula.
 Distal attachments: Tendon attaches to crest of lesser tubercle of humerus, proximal to the teres major.
Distal attachments: Tendon attaches to crest of lesser tubercle of humerus, proximal to the teres major.
Acting unilaterally, the latissimus dorsi adducts, extends, and internally rotates the humerus and laterally flexes the trunk (approximates the shoulder and the pelvis). Bilateral contraction helps hyperextend the spine and anteriorly tilt the pelvis.
Motor control considerations
Trunk muscle contractions
To achieve full trunk control and to use this control during functional tasks, patients must regain the ability to contract their trunk muscles under three different circumstances outlined by Davies.17 The task of lower extremity bathing from a seated position illustrates these points:
1. Contracting to move opposite the pull of gravity: When the trunk is moving in a direction that is opposite to gravitational pull, the muscles on the uppermost side of the trunk are contracting concentrically. For example, after washing feet, the trunk is straightened from a bent-over position by concentric contraction of the back extensors (the uppermost muscles). Therefore, the muscles are shortening actively. The one exception to the rule that the uppermost muscles are active during this type of contraction is bridging. In this case, movement does occur in a direction opposite the pull of gravity (back and buttocks moving away from the support surface), but the underside muscles (the extensors) are contracting concentrically and are responsible for the success of this task. Concentric contractions are used functionally to reposition the trunk during or after task completion.
2. Preventing movement that would occur because of gravitational pull: This type of muscle contraction (usually isometric) prevents falling toward the pull of gravity, stabilizes the trunk for successful completion of tasks, and forms the basis of many balance reactions. During lower extremity washing, the back extensors contract to stabilize (isometrically hold) the trunk as one washes the lower leg, allowing proximal stabilization for distal function. As a note, when one leans all of the way forward (extreme flexion), the back extensors become inactive, and the vertebral ligaments become responsible for holding the trunk in this posture.5
3. Controlling the speed of trunk movements in the direction of gravitational pull: In this type of contraction, the muscles are contracting eccentrically (in controlled and active elongation). The muscles responsible for this contraction are on the side of the trunk that is opposite the pull of gravity. When one leans forward to wash the feet during lower body washing, the back extensors contract eccentrically to control the speed and range of the forward trunk movement. This muscle contraction has a braking effect as the large mass of the trunk moves into the pull of gravity.
The previous examples show that functional independence requires control of all three trunk muscle contractions and combinations. Successful treatment plans must include activities that elicit a variety of trunk muscle contractions. Self-care training inherently challenges a variety of trunk postures and muscle contractions.
Musculoskeletal components
Control of the trunk depends on several musculoskeletal variables including ROM, biomechanical alignment, strength, and muscle length. These variables are interdependent and can create a vicious circle in stroke patients.
Postural malalignment
Stroke patients commonly assume postural malalignments that first must be identified via observations and palpations. After identification, the causative factors must be determined before determining the most appropriate intervention (Table 7-3).
Table 7-3 Common Postural Alignments and Potential Causes
| Posterior pelvic tilt/lumbar spine flexion (loss of the lumbar curve) | |
| Pelvic obliquity characterized by unequal weight-bearing through the ischial tuberosities | |
| Increased kyphosis | |
| Sitting off midline and/or lateral spine flexion | |
| Rib cage rotation | |
| Head/neck malalignment (rotation away from and lateral flexion toward the involved side) |
Prolonged postural malalignment results in muscle shortening on one side of the trunk and muscle overstretching on the opposite side. For example, a posterior pelvic tilt with lumbar flexion results in shortening of the anterior musculature and elongation (overstretching) of the posterior muscles. Lateral flexion on the right side results in muscle shortening on the right side and muscle elongation on the left side of the trunk.
Postural malalignment may occur because of unilateral weakness (specifically around the pelvis), unbalanced skeletal muscle activity, perceptual dysfunction and an inability to perceive midline, and soft-tissue shortening.
Prolonged postural malalignment can result in soft-tissue shortening, loss of ROM, and an inability to generate enough force to contract the muscle group in question. The total force of muscle (active tension) is high at the rest length of the muscle (i.e., when the trunk is aligned properly) and less when the muscle is tested at shorter lengths. Therefore, the force-generating mechanism within the muscle works optimally at the rest length of the muscle38 (i.e., a symmetrical and aligned trunk).
Managing stiffness and the degrees of freedom problem
Mohr40 states, “Normal control in any body part demands the ability to dissociate (separate) different parts of the body.” She gives the examples of dissociating the head from the body, one side of the body from the other, and the upper trunk from the lower trunk. Instead, patients often appear stiff, have nonfluid movements, and move their body segments as a unit
Examples of dissociation during functional tasks include upper trunk rotation with lower trunk stability while reaching for toilet paper, counterrotation of the trunk during ambulatory activities, and upper trunk rotation with concurrent lower trunk lateral flexion to increase the range of reach beyond the arm span when reaching for a phone positioned on the left side of a desk with the right hand.
Difficulty with dissociation/postural stiffness may result from soft-tissue tightness, bony contracture, or efforts by the patient to decrease the degrees of freedom in the trunk45 during functional activities. It is critical to determine why the person is not able to dissociate. A typical clinical problem is determining if trunk stiffness and lack of dissociation is due to soft-tissue tightness (which may require soft tissue stretching and mobilization) or if the person is freezing the degrees of freedom in an effort to maintain stability (which requires core stabilization activities). One method to differentiate the cause is to provide various levels of postural support, for example, sitting in a high back chair versus sitting unsupported on a therapy table, or side lying versus sitting unsupported. If the underlying cause of the stiffness is related to freezing the degrees of freedom, substantial differences will be noted for both passive and active movements under the various conditions of postural support. In the situations in which the patient has the most support (side lying and supported seating), he or she will be able to “free” the degrees of freedom and move with increased ease and fluidity, and will be able to separate body parts. If the same person is placed in a condition of decreased postural support, the system will respond by “freezing” the degrees of freedom, and stiffness will emerge.
Motor adaptation
Concerning motor adaptation, Smith, Weiss, and Lehmkuhl47 state, “Normal postural control requires the ability to adapt responses to changing tasks and environmental demands. This flexibility requires the availability of multiple movement strategies and the ability to select the appropriate strategy for the task and environment. The inability to adapt movements to changing task demands is a characteristic of many patients with neurological disorders. Patients become fixed in stereotypical patterns of movement, showing a loss of movement flexibility and adaptability.”
Motor adaptation can occur in response to an external perturbation or in anticipation of potentially destabilizing forces. Unexpected external perturbations include bumping into someone in a crowded lobby, being in a vehicle that unexpectedly turns or decelerates, and being on a moving platform, such as an escalator, that stops unexpectedly.
Activities that lead to trunk movements in anticipation of destabilizing forces (i.e., internal perturbations) include reaching for a heavy book on a shelf, reaching beyond the arm span, and preparing to push or pull a chair into place. Shumway-Cook and Woollacott46 point out that anticipatory postural control depends heavily on previous experience and learning. Research focusing on anticipatory postural responses during reach activities is presented in Chapter 10.
General considerations for evaluation and treatment of the trunk
Therapists should consider the following points during evaluation of the trunk and treatment planning:
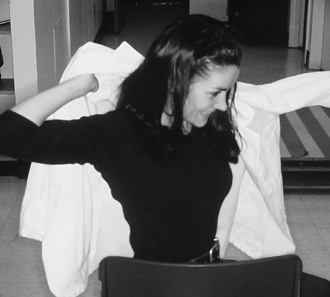
1. Proper evaluation and treatment of the trunk result from use of keen observational skills. Patients should be undressed (shirtless or in sports bra or bathing suit top), so that movements are more easily observed during functional tasks. Clothing folds, wrinkles, and crooked seams can lead to incorrect observations.
2. The therapist must realize that the slightest change in posture can change trunk muscle activity and alignment completely.16 For example, a subtle anterior shift of the shoulders results in extensor activation, whereas a subtle posterior shift of the shoulders results in trunk flexor activation.
3. The therapist should evaluate the trunk in a variety of postures that coincide with ADL. Trunk adjustments are task specific; therefore, a trunk evaluation of a patient who is supine should include activities such as rolling, assuming/maintaining side lying, bridging, and transitions to sitting (see Chapter 14). Evaluations of seated patients should include activities such as upper and lower extremity dressing, scooting, and bathing; evaluations of standing patients should include reaching for items in medicine cabinets, on bookshelves, and in kitchen cabinets (see Chapter 8).
Evaluation process
Subjective interview
Therapists should question patients about their perceived stability limits. Stability limits have been defined as the “boundaries of an area of space in which the body can maintain its position without changing the base of support.”47 Patients’ perceived stability limits may or may not be consistent with their actual limits. If patients’ perceived limits of stability are greater than their actual limits, they are at risk for falls. If their perceived limits of stability are less than their actual limits, they may be reluctant to attempt tasks with progressively greater demands on their postural system (e.g., lower extremity dressing without assistive devices and picking up objects from the floor without a reacher).
Perceived stability limits may have a direct correlation with observed neurobehavioral deficits. Body scheme disorders commonly occur in the stroke population. These deficits include body neglect, somatoagnosia, and impaired right/left discrimination.2 Ayres3 has defined body scheme as a postural model on which movements are based. Knowledge of body parts and their relationships are necessary for deciding what and where to move and in what way to perform.2 Spatial relation deficits including spatial neglect, depth perception, and spatial relation disorders also may have an effect on patients’ perceived stability limits (gaining and regaining midline orientation and position in space) (see Chapter 18).
Other components of the subjective interview include determining patients’ insights into their trunk malalignments and their ability to perceive and assume midline positions.43 The therapist’s goal in this interview is to gain insight into the patients’ ability to make accurate observations about their postural dysfunction. This is difficult for many patients because trunk control does not occur at a conscious level in the majority of daily tasks.
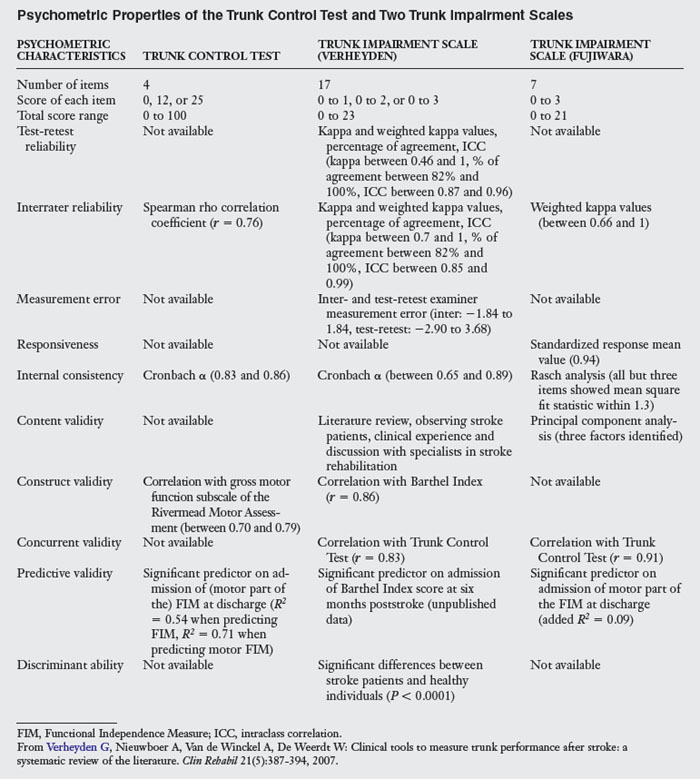
Standardized assessments
The use of valid and reliable tools is always recommended. The following section reviews available measurement instruments related to trunk control. The first three instruments specifically evaluate trunk control after stroke and are therefore highly recommend for this area of practice/research, while the others are comprehensive measures that include items related to the trunk. See Table 7-4 for a review of the psychometric properties of these three measures.
Trunk control test
The Trunk Control Test14 examines four functional movements: roll from supine to the weak side, roll from supine to the strong side, sitting up from supine, and sitting on the edge of the bed for 30 seconds (feet off the ground). Each of the four tasks are scored as follows: 0, unable to perform with assistance; 12, able to perform but in an abnormal manner; and 25, able to complete movement normally. The range of scores is 0 to 100.
The Trunk Control Test has been shown to be sensitive to change in assessing recovery of stroke patients, to correlate with the Functional Independence Measure, and to predict motor Functional Independence Measure items at discharge better than motor Functional Independence Measure Scores.12,14 In addition, Duarte and colleagues21 found that the Trunk Control Test significantly correlated with length of stay, discharge motor Functional Independence Measure scores, gait velocity, walking distance, and the Berg Balance Scale. They also found that the Trunk Control Test predicted 52% of the variance in length of stay and 54% of the discharge Functional Independence Measure (Table 7-5).
| TESTS (ON BED) | SCORING 0—UNABLE TO 12—ABLE TO DO WITH NONMUSCULAR HELP 25—NORMAL |
|---|---|
From Collin C, Wade D: Assessing motor impairment after stroke: a pilot reliability study. J Neurol Neurosurg Psychiatry 53(7):576-579, 1990.
Trunk impairment scale (a)
This scale evaluates motor impairment of the trunk after stroke. The tool scores static (3 items), dynamical sitting balance (10 items), and trunk coordination (4 items). It also aims to score the quality of trunk movement and to be a guide for treatment. The scores range from a minimum of 0 to a maximum of 2353 (Table 7-6).
Table 7-6 Trunk Impairment Scale (A)
| The starting position for each item is the same. The patient is sitting on the edge of a bed or treatment table without back and arm support. The thighs make full contact with the bed or table, the feet are hip width apart and placed flat on the floor. The knee angle is 90°. The arms rest on the legs. If hypertonia is present the position of the hemiplegic arm is taken as the starting position. The head and trunk are in a midline position. If the patient scores 0 on the first item, the total score for the TIS is 0. Each item of the test can be performed three times. The highest score counts. No practice session is allowed. The patient can be corrected between attempts. The tests are verbally explained to the patient and can be demonstrated if needed. |
||
| ITEM | ||
| Static sitting balance | ||
| Patient falls or cannot maintain starting position for 10 seconds without arm support | h0 | |
| Patient can maintain starting position for 10 seconds If score = 0, then Trunk Impairment Scale (TIS) total score = 0 |
h2 | |
| Patient falls or cannot maintain starting position for 10 seconds without arm support | h0 | |
| Therapist crosses the unaffected leg over the hemiplegic leg | Patient can maintain starting position for 10 seconds | h2 |
| Patient falls | h0 | |
| Patient crosses the unaffected leg over the hemiplegic leg | Patient cannot cross legs without arm support on bed or table | h1 |
| Patient crosses the legs but displaces the trunk more than 10 cm backward or assists crossing with the hand | h2 | |
| Patient crosses the legs without trunk displacement or assistance | h3 | |
| Total static sitting balance | /7 | |
| Dynamical sitting balance | ||
| Patient falls, needs support from an upper extremity, or the elbow does not touch the bed or table | h0 | |
| Patient is instructed to touch the bed or table with the hemiplegic elbow (by shortening the hemiplegic side and lengthening the unaffected side) and return to the starting position | Patient moves actively without help, elbow touches bed or table | h1 |
| If score = 0, then items 2 and 3 score = 0 | ||
| Patient demonstrates no or opposite shortening/lengthening | h0 | |
| Patient demonstrates appropriate shortening/lengthening | h1 | |
| If score = 0, then item 3 scores = 0 | ||
| Patient compensates. Possible compensations are: (1) use of upper extremity, (2) contralateral hip abduction, (3) hip flexion (if elbow touches bed or table further than proximal half of femur), (4) knee flexion, (5) sliding of feet | h0 | |
| Patient moves without compensation | h1 | |
| Patient falls, needs support from an upper extremity, or the elbow does not touch the bed or table | h0 | |
| Patient is instructed to touch the bed or table with the unaffected elbow (by shortening the unaffected side and lengthening the hemiplegic side) and return to the starting position | Patient moves actively without help, elbow touches bed or table | h1 |
| If score = 0, then items 5 and 6 score = 0 | ||
| Patient demonstrates no or opposite shortening/lengthening | h0 | |
| Patient demonstrates appropriate shortening/lengthening | h1 | |
| If score = 0, then item 6 scores = 0 | ||
| Patient compensates. Possible compensations are: (1) use of upper extremity, (2) contralateral hip abduction, (3) hip flexion (if elbow touches bed or table further than proximal half of femur), (4) knee flexion, (5) sliding of feet | h0 | |
| Patient moves without compensation | h1 | |
| Patient demonstrates no or opposite shortening/lengthening | h0 | |
| Patient is instructed to lift pelvis from bed or table at the hemiplegic side (by shortening the hemiplegic side and lengthening the unaffected side) and return to the starting position | Patient demonstrates appropriate shortening/lengthening | h1 |
| If score = 0, the item 8 scores = 0 | ||
| Patient compensates. Possible compensations are: (1) use of upper extremity, (2) pushing off with the ipsilateral foot (heel loses contact with the floor) | h0 | |
| Patient moves without compensation | h1 | |
| Patient demonstrates no or opposite shortening/lengthening | h0 | |
| Patient is instructed to lift pelvis from bed or table at the unaffected side (by shortening the unaffected side and lengthening the hemiplegic side) and return to the starting position | Patient demonstrates appropriate shortening/lengthening If score = 0, then item 10 scores = 0 |
h1 |
| Patient compensates. Possible compensations are: (1) use of upper extremity, (2) pushing off with the ipsilateral foot (heel loses contact with the floor) | h0 | |
| Patient moves without compensation | h1 | |
| Total dynamical sitting balance | /10 | |
| Coordination | ||
| Hemiplegic side is not moved three times | h0 | |
| Patient is instructed to rotate upper trunk 6 times (every shoulder should be moved forward 3 times), first side that moves must be hemiplegic side, head should be fixated in starting position | Rotation is asymmetrical | h1 |
| Rotation is symmetrical | h2 | |
| If score = 0, then item 2 scores = 0 | ||
| Rotation is asymmetrical | h0 | |
| Rotation is symmetrical | h1 | |
| Hemiplegic side is not moved three times | h0 | |
| Patient is instructed to rotate lower trunk 6 times (every knee should be moved forward 3 times), first side that moves must be hemiplegic side, upper trunk should be fixated in starting position | Rotation is asymmetrical | h1 |
| Rotation is symmetrical | h2 | |
| If score = 0, then item 4 scores = 0 | ||
| Rotation is asymmetrical | h0 | |
| Rotation is symmetrical | h1 | |
| Total coordination | /6 | |
| Total trunk impairment scale | /23 | |
From Verheyden G, Nieuwboer A, Mertin J, et al: The Trunk Impairment Scale: a new tool to measure motor impairment of the trunk after stroke, Clin Rehabil 18(3):326-334, 2004.
Trunk impairment scale (b)
This tool consists of seven items. Abdominal muscle strength and verticality items were derived from the Stroke Impairment Assessment Set, and the other five items consist of the perception of trunk verticality, trunk rotation muscle strength on the affected and the unaffected sides, and righting reflexes both on the affected and the unaffected sides. The seven items are scored on four-point scale with 0 indicated poor performance and 3 indicated best performance28 (Box 7-1 and Table 7-7).
Box 7-1 Trunk Impairment Scale (B) Trunk Impairment Scale Items and Criteria for Scoring
Perception of trunk verticality
While the patient is sitting on the edge of a bed or on a chair without a backrest, with the feet off the ground, the examiner holds both sides of the patient’s shoulders and makes the patient’s trunk deviate to the right and left. The examiner asks the patient to indicate when he or she feels the trunk is in a vertical position. The examiner then records the degree of trunk angle deviation from the vertical line drawn from the midpoint of the Jacoby line.
Trunk rotation muscle strength on the affected side
The patient is asked to roll the body from the supine position to the unaffected side. The arms should be crossed in front of the chest and legs kept extended. The patient is asked to roll his or her body without pushing the floor with his or her limbs or pulling on the bed clothes. Isometric contractions for stabilization and other muscles than external oblique (e.g., pectoralis major) activation during rolling are allowed.
Trunk rotation muscle strength on the unaffected side
The patient is asked to roll the body from the supine position to the affected side. Scoring is the same as for the trunk rotation muscle strength on the unaffected side.
Right reflex on the affected side
The patient sits on the edge of a bed or a chair without a backrest. The examiner pushes the patient’s shoulder laterally (about 30 degrees) to the unaffected side and scores according to the degree of the reflex elicited on the affected side of the patient’s trunk.
1 = The reflex is poorly elicited, and the patient cannot bring his or her body back to the erect position as before.
2 = The reflex is not strong, but the patient can bring his or her body back to the erect position almost as before.
3 = The reflex is strong enough, and the patient can immediately bring his or her body back to the erect position as before.
Righting reflex on the unaffected side
The examiner pushes the patient’s shoulder laterally (about 30 degrees) to the affected side. Scoring is the same as for the righting reflex on the affected side.
Stroke impairment assessment set verticality
Stroke impairment assessment set abdominal muscle strength
Stroke Impairment Assessment Set abdominal muscle strength is evaluated with the patient resting in a 45-degree semireclining position in either a wheelchair or a high-back chair. The patient is asked to raise the shoulders off the back of the chair and assume a sitting position.
From Fujiwara T, Liu M, Tsuji T, et al: Development of a new measure to assess trunk impairment after stroke (trunk impairment scale): its psychometric properties. Am J Phys Med Rehabil 83(9):681-688, 2004.
Table 7-7 Comparison of the Trunk Impairment Scale (B) and the Trunk Control Test
| CONTENT | TRUNK IMPAIRMENT SCALE | TRUNK CONTROL TEST |
|---|---|---|
| Practicality | ||
| No. of items | 7 | 4 |
| Score of each item | 0 to 3 | 0, 12, 25 |
| Score range | 0 to 21 | 0 to 100 |
| Reliability | ||
| Interrater reliability | Yes, weighted kappa | Yes, Spearman rank correlation |
| Internal consistency | Yes, Rasch analysis (mean square fit index) | Yes, Cronbach α |
| Validity | ||
| Content validity | Yes, principal component analysis | No |
| Construct validity | Yes, Rasch analysis (logits) | Yes, correlation of individual items |
| Concurrent validity | Yes, with TCT | Yes, with RMA GF |
| Predictive validity | Yes, discharge Functional Independence Measure motor score | Yes, discharge FIM motor score |
FIM, Functional Independence Measure.
RMA GF, Rivermead Motor Assessment gross function scores.
From Fujiwara T, Liu M, Tsuji T, et al: Development of a new measure to assess trunk impairment after stroke (trunk impairment scale): its psychometric properties. Am J Phys Med Rehabil 83(9):681-688, 2004.
Postural assessment scale for stroke patients
The Postural Assessment Scale for Stroke Patients includes items related to trunk control. Overall, the scale contains 12 four-point items graded from 0 to 3. Higher scores indicate better performance. Items include sitting without support, standing with and without support, standing on the nonparetic leg, standing on the paretic leg, supine to affected side, supine to nonaffected side, supine to sit, sit to supine, sit to stand, stand to sit, and standing and picking up a pencil from the floor. The Postural Assessment Scale for Stroke Patients has been found to be highly valid and reliable during the first three months after stroke.6
Five items have been suggested31 to measure trunk control: sitting without support, supine to affected side, supine to nonaffected side, supine to sitting on the edge of the bed, and sitting to supine. Recent work on this instrument has demonstrated that while the tool can predict performance in ADL at one year poststroke, a ceiling effect was noted at various points in recovery indicating a limited discriminative ability between individuals and a limited responsiveness over the first six months after stroke.56
Chedoke-mcmaster stroke assessment
The Chedoke-McMaster Stroke Assessment is used to assess physical impairment and disability in clients with stroke. It has two components including the Impairment Inventory (which determines the presence and severity of physical impairments in the six dimensions of shoulder pain, postural control, arm, hand, foot, and leg quantified in a seven-point staging system) and the Activity Inventory (which measures the client’s functional ability). The Activity Inventory has two components: the Gross Motor Function Index (with items including moving in bed and transferring to a chair) and the Walking Index (with items including walking on rough ground and climbing stairs). The maximum score that a client can obtain is 100 as there are 14 items with a seven-point scale and a two-point score awarded for age-appropriate walking distance.30
Motor assessment scale
The Motor Assessment Scale12 is a comprehensive assessment of motor behavior and includes items related to trunk control. Overall, the scale consists of eight items: supine to side-lying (onto intact side), supine to sit, balanced sitting, sit to stand, walking, upper arm function, hand movements, and advanced hand activities. Each item is scored on seven-point scale from 0 to 6. Higher scores indicate better performance.
Fugl-meyer assessment
The Fugl-Meyer Assessment27 evaluates five areas: joint motion and pain, balance, sensation, upper extremity motor function, and lower extremity motor function. The balance subscale includes seven functions related to postural control: sit without support, protective reactions on affected and nonaffected sides, stand with support, stand without support, stand on nonaffected leg, and stand on affected leg.
Mao and colleagues39 compared the psychometric properties of the balance subscale of the Fugl-Meyer Assessment, the Berg Balance Scale (see Chapter 8), and the Postural Assessment Scale for Stroke Patients. They concluded that all three tests showed acceptable levels of reliability, validity, and responsiveness with the Postural Assessment Scale for Stroke Patients showing slightly better psychometric characteristics. The reader is referred to Chapter 8 for a review of other standardized assessments of postural control. In addition, the reader should review Chapter 21 concerning use of the Assessment of Motor and Process Skills. The assessment includes motor skill items such as stabilizes, aligns, and positions. The Assessment of Motor and Process Skills is unique and highly recommended, for the therapist can gather information related to motor skills during ADL performance.
Observations of trunk alignment/malalignment
For the purposes of this chapter, observations concern the seated posture. The patient’s trunk should be exposed as much as possible, and the patient should be asked to “sit up nice and straight and gently rest your hands in your lap.” (Table 7-8 outlines the ideal alignment of the trunk and extremities and common asymmetries observed after stroke during static sitting.)
Table 7-8 Typical Alignment and Common Malalignments after Stroke
| NORMAL ALIGNMENT | COMMON MALALIGNMENT | |
|---|---|---|
| Pelvis | Equal weight-bearing through both ischial tuberosities Neutral to slight anterior tilt Neutral rotation |
Asymmetrical weight-bearing Posterior pelvic tilt Unilateral retraction |
| Vertebral column | Straight from posterior view Appropriate curves from lateral view |
Scoliosis Loss of lumbar curve; increased thoracic kyphosis Shortening on one side; elongation on opposite side |
| Rib cage | Neutral in terms of lateral tilt Neutral rotation Alignment over pelvis and under shoulders |
Lateral tilt Flaring on one side Unilateral retraction |
| Shoulders | Symmetrical height Alignment over pelvis |
Asymmetrical height Unilateral retraction |
| Head/neck | Neutral | Protraction Flexion to weak side Rotation away from weak side |
| Upper extremities | Resting in lap; if weight-bearing, effortless and symmetrical | Use of stronger extremity as postural support to maintain alignment Too little or too much activity in more involved extremity |
| Lower extremities | Hips at 90 degrees Knee aligned with hips Feet in full contact with floor, accepting weight; feet under knees |
Hips toward extension because of posterior pelvic tilt Hip adduction resulting in knee contact “Windswept” hips Feet not equally bearing weight, or “pushing”; foot placed in front of knee |
Following the evaluation of postural malalignments during static sitting, the therapist should begin to hypothesize the cause of these malalignments. Causes may include increased skeletal muscle activity on one side of the trunk, inability to recruit muscle activity or weakness, soft-tissue shortening, fixed deformity, body scheme disorder, and inability to perceive midline.
The therapist must remember that observed postures may be caused by more than one impairment (see Table 7-3). For example, stroke patients tend to sit in a posterior pelvic tilt position with resultant hip extension and thoracic spine flexion. This posture may result from one of or a combination of the following:
 Weakness or lack of activity in the trunk extensors, especially in the lower back
Weakness or lack of activity in the trunk extensors, especially in the lower back
 Fixed contracture of the hamstrings and/or thoracic spine
Fixed contracture of the hamstrings and/or thoracic spine
 Abdominal weakness: The mentioned posture changes the center of gravity and decreases the potential to fall backward. The abdominal muscles are primarily responsible for preventing backward sway, therefore assuming a flexed posture reduces the chance of having to activate the abdominals to prevent falls.
Abdominal weakness: The mentioned posture changes the center of gravity and decreases the potential to fall backward. The abdominal muscles are primarily responsible for preventing backward sway, therefore assuming a flexed posture reduces the chance of having to activate the abdominals to prevent falls.
Another example of a commonly observed malalignment is trunk shortening on the side affected by the stroke. The patient may assume this posture for several reasons:
 Inactive shoulder elevators on the side affected by the stroke that let the shoulder depress16
Inactive shoulder elevators on the side affected by the stroke that let the shoulder depress16
 Increased muscle activity of the scapula depressors that pull the shoulder down on the affected side
Increased muscle activity of the scapula depressors that pull the shoulder down on the affected side
 Perceptual dysfunction resulting in an inability to find midline, bearing the most weight on the stronger side and resulting in a shortening of the affected side
Perceptual dysfunction resulting in an inability to find midline, bearing the most weight on the stronger side and resulting in a shortening of the affected side
 Increased muscle activity or shortening of the affected lateral flexors resulting in a shortening response
Increased muscle activity or shortening of the affected lateral flexors resulting in a shortening response
 Fear of shifting weight to the affected side, with the majority of weight on stronger side, resulting in shortening of the affected side
Fear of shifting weight to the affected side, with the majority of weight on stronger side, resulting in shortening of the affected side
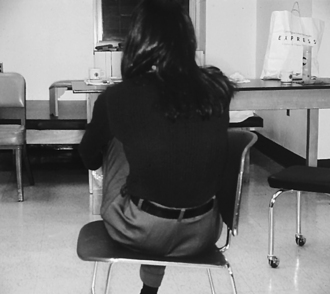
Following the observation of the patient in a static posture, the occupational therapist must observe trunk responses during functional activities. The two most effective methods of making these observations are observing patients during self-care and mobility in a variety of positions and controlled reach pattern activities (Table 7-9). During functional reach patterns, trunk responses are required to provide proximal stability for distal function, enhance the ability to interact with the environment by increasing reaching distance (i.e., extend the arm span with an appropriate trunk response), and prevent falls.
Table 7-9 Effects of Object Positioning on Trunk Movements and Weight Shifts during Reaching Activities*
| POSITION OF OBJECT | TRUNK RESPONSE/WEIGHT SHIFT |
|---|---|
| Straight ahead at forehead level, past arm’s length |
Trunk extension, anterior pelvic tilt Anterior weight shift |
| On floor, between feet |
Trunk flexion Anterior weight shift |
| To side at shoulder level, past arm’s length |
Left trunk shortening, right trunk elongation, left hip hiking Weight shift to right |
| On floor, below right hip |
Right trunk shortening, left trunk elongation Weight shift to right |
| Behind right shoulder, at arm’s length |
Trunk extension and rotation (right side posteriorly) Weight shift to right |
| At shoulder level, to left of left shoulder |
Trunk extension and rotation (left side posteriorly) Weight shift to left |
| On floor, to left of left foot |
Trunk flexion and rotation (left side posteriorly) Weight shift to left |
| Above head, directly behind |
Trunk extension, shoulders move behind hips Posterior weight shift |
* These examples are for a patient with left hemiplegia. The left-hand column indicates where to position objects during a reaching task (using the right upper extremity). The right-hand column indicates the resultant trunk position and weight shift.
An individual’s reaching ability is limited to within the arm span by static trunk postures. When an object is placed beyond arm’s length (e.g., on a floor, across a dining table, or under a sink), a trunk response is required to pick up the object successfully.
In general, picking up an object from the floor or from in front of an individual requires an anterior trunk shift. Picking up objects placed beyond the arm span to the right or left of the individual requires a lateral weight shift from the trunk primarily onto one of the ischial tuberosities. Retrieving objects placed behind the trunk requires a posterior weight shift. Rotational trunk responses result from reaching across the midline or for objects posterior to the shoulders or hips.
The therapist’s goals while observing the patient perform functional reach patterns are the following:
 Ensure that trunk and upper extremity patterns are coordinated to result in successful task completion.
Ensure that trunk and upper extremity patterns are coordinated to result in successful task completion.
 Note asymmetries during reaching.
Note asymmetries during reaching.
 Objectively evaluate the perceived and actual stability limits of the patient.
Objectively evaluate the perceived and actual stability limits of the patient.
 Note in which directions the patient is or is not able to reach beyond the arm span.
Note in which directions the patient is or is not able to reach beyond the arm span.
Evaluation of specific trunk movement patterns
In addition to performing each movement pattern, the reader should refer to the appropriate figures while reading this section. The following evaluation procedures are based on the work of Mohr,40 Boehme,8 Davies,16 and Basmajian and DeLuca.5
Trunk flexor control
The trunk flexors are evaluated by the five different methods that follow:
1. Patients assume a seated, upright position. The therapist asks them to move their shoulders behind their hips slowly and with control (Fig. 7-4, A); this movement pattern occurs in the sagittal plane, is initiated from the upper trunk,40 and elicits an eccentric contraction of the trunk flexors.25,50 Holding the end range of this posture results in an isometric contraction of the trunk flexors. Observations should include resistance to movement, fall potential, and symmetry of the posterior weight shift. Unilateral weakness causes the weak side to become posterior to the stronger side (i.e., it results in rotation of the trunk).
2. From the end position of the first movement pattern, the therapists asks patients to move their shoulders forward so that they are sitting in proper alignment within the sagittal plane (see Fig. 7-4, B); this movement pattern is achieved by a concentric contraction of the trunk flexors.25 The therapist should note symmetry during the movement pattern. Unilateral weakness causes the stronger side to lead the pattern.
3. In an aligned, seated position, patients assume a controlled lumbar flexion posture (posterior tilt with flattening of the lumbar curve and spinal flexion) (see Fig. 7-4, C). Mohr40 states that this movement pattern is initiated by the lower trunk and pelvis. If this pattern is performed actively, the final posture is assumed by concentric flexor contraction. Patients also may achieve this posture by a relaxation response of the low back extensors, so the therapist should palpate the flexors to ensure the pattern is due to active movement. At the end range of this pattern—posterior tilt and spinal flexion (a recumbent posture)—little to no muscle activity exists, and patients maintain this posture by support of their vertebral ligaments.5
4. The therapist also should evaluate control of the trunk flexors when the patient is supine (during rolling and bed mobility activities). While the patient is in a supine position, the therapist asks the patient to sit up in a straight plane. This movement pattern, which is controlled primarily by the rectus abdominis, allows the therapist to evaluate antigravity control of the trunk flexors. The therapist also can ask the patient to roll by lifting one shoulder up and across the trunk in a position of trunk flexion and rotation. This movement pattern also gives the therapist insight into the antigravity control of the flexors (primarily the obliques).38
5. Although the first four movement patterns to test flexor control were initiated by the patient, testing the response of the flexors to being moved by the therapist also is useful. The therapist lifts the lower legs of the patient into a position of increased hip flexion. For the patient to refrain from falling backward, the trunk flexors must be activated isometrically (see Fig. 7-4, D).
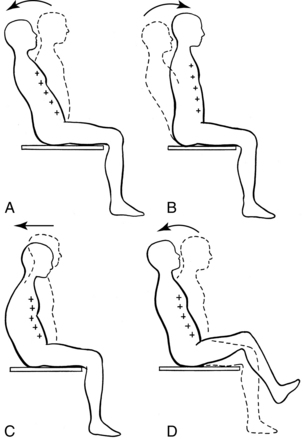
Figure 7-4 Trunk flexor control. Dotted lines indicate trunk starting position, solid lines indicate trunk final position, arrows indicate movement direction, and plus signs indicate muscle groups primarily responsible for control of pattern.
(Skeletal muscle activity occurs on both sides of the trunk; that is, reciprocal innervation.)
As a rule of thumb the trunk flexors are activated in the seated position when the shoulders move posterior to the hips (backward sway), when the trunk is moving away from the support surface (supine starting point), and during rotational activities.
Trunk extensor control
The following four movement patterns are used to evaluate trunk extensor control during seated activities and bridging.
1. To start this movement pattern, the patient assumes a flexed spine posture with a posterior pelvis tilt (the resting posture for many stroke survivors). The patient initiates the movement with the lower trunk and pelvis40 and assumes an extended spine posture with a neutral to slight anterior tilt, which accentuates the lumbar curve (Fig. 7-5, A). The patient completes the movement pattern by a concentric contraction of the trunk extensors, which is the trunk pattern required for forward reach.
2. Patients assume an aligned, seated starting position and are asked to keep their spine straight as they lean forward, keeping the shoulders in front of the hips in the sagittal plane (see Fig. 7-5, B). They assume this posture by an eccentric contraction of the trunk extensors,5,25,50 and if they hold the posture between the middle to end range, the back extensors isometrically contract. The patient has unilateral weakness if the trunk moves forward asymmetrically. Unilateral weakness causes the weaker side to lead the movement pattern (e.g., to fall into gravity). If the movement continues in a forward direction (e.g., patient reaches down to the floor), the back extensors become inactive at the end range, and the tension of the vertebral ligaments maintains the position.5
3. While patients are in the end posture of the second movement pattern, the therapists asks them to move their shoulders back to assume a seated, aligned position (see Fig. 7-5, C). To assume this posture, the trunk extensors contract concentrically, although the hip extensors initiate the movement;5,50 this movement occurs in the sagittal plane.
4. The therapist also should test the back extensors by observing the patient in a bridge posture. While the patient is in a supine position with the hips and knees flexed, the therapist asks the patient to assume a bridge position, which is accomplished by a concentric contraction of the back and hip extensors16 and is maintained by an isometric contraction of the same muscles. The release of the posture is controlled by eccentric contraction of the back and hip extensors.
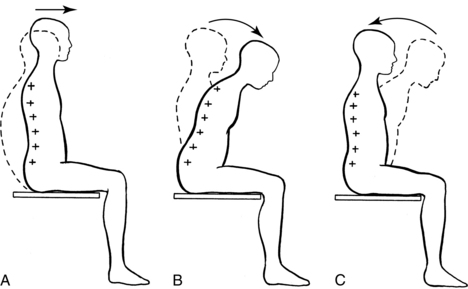
Figure 7-5 Trunk extensor control. Dotted lines indicate trunk starting position, solid lines indicate trunk final position, arrows indicate movement direction, and plus signs indicate muscle groups primarily responsible for control of pattern.
(Skeletal muscle activity occurs on both sides of the trunk; that is, reciprocal innervation.)
As a rule of thumb, in the seated posture the back extensors are active during anterior weight shifts (in which the shoulders move in front of the hips), during correction of posture to a position of alignment from an anterior weight shift, and during bridging activities.
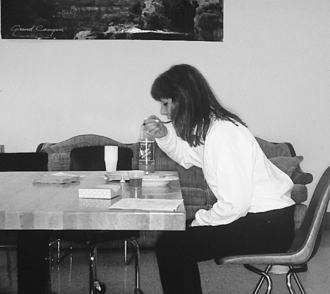
Control of the lateral flexors
Lateral flexion occurs in the coronal plane; therefore, a balance of control between the flexors and extensors is required to maintain movement. Electromyographic studies have demonstrated that dorsal and ventral muscles coactivate during lateral flexion.50 Electromyographic activity of the right and left erector spinae has been documented during lateral trunk flexion.5,25
Mohr40 states, “Two different movement strategies occur when you reach down to the side: (1) the initiation may occur in the upper trunk and the ipsilateral spine shortens, or (2) the movement can be initiated with your lower trunk and pelvis, resulting in ipsilateral elongation.” Three movement patterns are used to evaluate control of lateral trunk flexion:
1. The first movement pattern is initiated from an aligned, seated position. The pelvis remains stable, and the upper trunk initiates lateral flexion toward the floor with the shoulder approximating the hip (Fig. 7-6A). The end posture (one of ipsilateral trunk shortening) occurs by an eccentric contraction of the side of the elongating trunk.40,50 In Fig. 7-6, A, the right side of the trunk is shortening, but the predominant control is on the left side, which is elongating eccentrically. Holding this posture between the middle and end ranges allows evaluation of isometric lateral flexion control. Therapists should evaluate both sides of the trunk using this movement pattern.
2. While patients are in the end position of the first movement pattern, the therapist asks them to realign themselves by sitting up straight (see Fig. 7-6, B). The trunk is realigned by a concentric contraction of the lateral flexors38 (the left lateral flexors in Fig. 7-6, B).
3. The last movement pattern evaluates lateral flexion, which initiates the movement from the lower trunk and pelvis.40 This movement pattern allows reach beyond the arm span in the frontal plane. During this movement, the majority of weight is shifted to one ischial tuberosity; the shoulder and hip approximate in this pattern. In the resulting posture the trunk is elongated on the weight-bearing side, and trunk shortening occurs on the nonweight-bearing side (see Fig. 7-6, C). The predominant control comes from concentric contraction of the lateral flexors on the shortening side. Fig. 7-6, C, illustrates the contraction on the right side of the trunk. The therapist must evaluate both sides of the trunk.
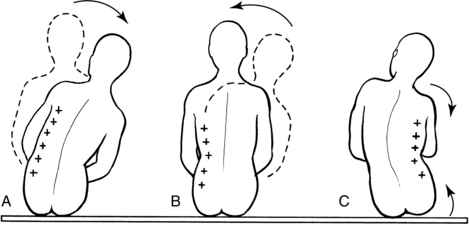
Figure 7-6 Lateral flexor control. Dotted lines indicate trunk starting position, solid lines indicate trunk final position, arrows indicate movement direction, and plus symbols indicate muscle groups primarily responsible for control of pattern.
(Skeletal muscle activity occurs on both sides of the trunk; that is, reciprocal innervation.)
Rotation control
Concerning rotation control, Kapandji33 states, “Rotation of the vertebral column is achieved by the paravertebral muscles and the lateral muscles of the abdomen. Unilateral contraction of the paravertebral muscles causes only weak rotation... During rotation of the trunk, the main muscles involved are the oblique muscles. Their mechanical efficiency is enhanced by their spiral course around the waist and by their attachments to the thoracic cage away from the vertebral column, so that both the lumbar and lower thoracic vertebral columns are mobilised.” During rotation of the trunk to the left, the right external and left internal obliques are activated (Fig. 7-7). The fibers of both of these muscles run in the same direction and are synergistic. Basmajian’s4 review of the literature on electromyography demonstrates that bilateral activity in the extensors at the thoracic level is evident during rotation.
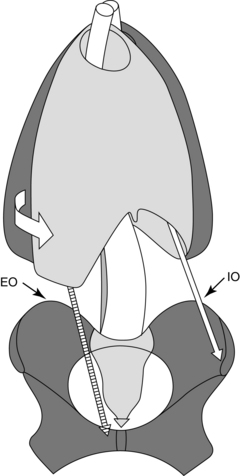
Figure 7-7 Rotation control. IO, Internal oblique; EO, external oblique.
(From Kapandji IA: The physiology of the joints, vol 3, The trunk and vertebral column, New York, 1974, Churchill Livingstone.)
Mohr40 states, “Stroke patients will very rarely rotate because normal rotation requires extensors and flexors to be active simultaneously on opposite sides of the trunk.” Rotational trunk control depends on muscle fixation on one side of the trunk, resulting in efficient muscle action on the opposite side.
Trunk rotation can occur in two positions: flexion with rotation and extension with rotation.7 Mohr40 points out that rotation can be initiated by the upper trunk or the lower trunk/pelvis. Rotation control is evaluated by five movement patterns:8,40
1. In the first movement pattern, the patient sits upright, and the pelvis remains stable on the support surface. The patient reaches across midline so that the shoulder moves toward the opposite hip (e.g., reaching with the right arm across the body toward the floor). The result is a position of flexion and rotation. The primary control is by concentric contraction of the obliques and contraction of the back extensors (especially at the thoracic level). The therapist must evaluate both sides of the trunk.
2. In the second movement pattern, the upper trunk remains stable, and the lower trunk and pelvis initiate a forward movement on one side (e.g., scooting forward). The result is a position of extension with rotation.
3. In the third movement pattern the patient reaches behind at the shoulder level (upper trunk initiation), and the resulting posture is rotation and extension.
4. The fourth movement pattern involves initiating a backward shift with the lower trunk and pelvis (scooting backward) while shifting to one side and rotating the opposite side posteriorly; this posture is flexion with rotation.
5. The final movement pattern is similar to a pattern reviewed in the section on trunk flexion control. The patient is supine and initiates a segmental roll by lifting the shoulders up from the support surface and toward the opposite side of the body. This pattern is controlled by a concentric contraction of the abdominal muscles (the obliques).
Trunk control during activities of daily living
There is a clear relationship between the loss of trunk control and the loss of functional independence. Conclusions from empirical research include:
 Franchignoni, Tesio, and Ricupero26 stated that trunk control appears to be an obvious prerequisite for the control of more complex limb activities that, in turn, constitute a prerequisite for complex behavioral skills.
Franchignoni, Tesio, and Ricupero26 stated that trunk control appears to be an obvious prerequisite for the control of more complex limb activities that, in turn, constitute a prerequisite for complex behavioral skills.
 Hsieh and colleagues31 affirmed that strong evidence exists for the predictive value of trunk control on comprehensive ADL, and they recommended early assessment and management of trunk control after stroke.
Hsieh and colleagues31 affirmed that strong evidence exists for the predictive value of trunk control on comprehensive ADL, and they recommended early assessment and management of trunk control after stroke.
 Karatkas and colleagues34 concluded that trunk flexion and extension muscle weakness in unihemispheric stroke patients can interfere with balance, stability, and functional disability.
Karatkas and colleagues34 concluded that trunk flexion and extension muscle weakness in unihemispheric stroke patients can interfere with balance, stability, and functional disability.
 Verheyden and colleagues52 asserted that measures of trunk performance are significantly related with values of balance, gait, and functional ability.
Verheyden and colleagues52 asserted that measures of trunk performance are significantly related with values of balance, gait, and functional ability.
The previous section focused on select movement patterns of the trunk. Evaluating the trunk in this manner is useful for identifying specific problem areas and focusing treatment plans. However, the impact that impaired trunk control has on functional tasks is more relevant to all rehabilitation professionals. Most, if not all, of the reviewed movement patterns (and combinations of them) are used during ADL performance. Therefore, the evaluation of trunk control can take place during skilled observations of ADL.
For clarification, an infinite number of variations are observed in movement patterns during task performance. Therefore, the focus of evaluation and treatment should be on observing, evaluating, and treating the patient in a variety of different environments and with tasks that include multiple variables. The situational context and task demands determine which components of trunk control are necessary for successful task performance. Box 7-2 has an example of task variables that affect trunk control patterns.
Box 7-2 Variables of Eating That Affect Required Trunk Control Patterns
 Type of seating surface (e.g., presence of armrests or backrest, cushions, chair height, distance person is from table)
Type of seating surface (e.g., presence of armrests or backrest, cushions, chair height, distance person is from table)
 Placement of items such as condiments, utensils, and serving bowls (e.g., near or far, right or left)
Placement of items such as condiments, utensils, and serving bowls (e.g., near or far, right or left)
 Type of food (e.g., hot soup, cold fruit)
Type of food (e.g., hot soup, cold fruit)
 Solitary or group dining (e.g., may get assistance with passing needed items)
Solitary or group dining (e.g., may get assistance with passing needed items)
The list of trunk control variations during ADL performance in the following section are not considered exhaustive, but are guidelines for observing trunk patterns and inherent variations during various tasks. The reader should mimic performing each task to ensure understanding of the posture descriptions (Table 7-10).
Table 7-10 Trunk Control to Support Participation
| ACTIVITY | POSSIBLE NECESSARY MOVEMENTS | ||
|---|---|---|---|
| Bridging | Bridging requires trunk extension, which is necessary at the trunk and hips to assume a functional bridge position. (The height of the bridge depends on the task. For example, bridging to use a bedpan requires more extension than bridging to don/doff pants.) See Chapter 14. | ||
| Scooting | Scooting requires the following movement:
|
||
| Toileting | Using the toilet requires the following movements:
|
||
| Bathing (seated on a tub seat or bench). | Bathing requires the following movements:
|
||
| Grooming | Oral care | Hygiene of the mouth requires the following movements:
|
|
| Hair care | Hair care requires the following movements:
|
||
| Dressing | Upper extremity | Pullover shirt Putting on a pullover shirt requires the following movements:
|
|
| Button-down shirt Putting on a button-down shirt requires the following movements:
|
|||
| Lower extremity (seated) | Putting on pants, underwear, shoes, and socks requires the following movements:
|
||
| Eating | Eating requires the following movements: | ||
|
|
|||
Upper extremity dressing
Pullover shirt.
Putting on a pullover shirt requires the following movements:
 Trunk flexion: Required for the patient to manipulate the shirt in the lap and reach down toward the lap to insert an arm into the sleeve
Trunk flexion: Required for the patient to manipulate the shirt in the lap and reach down toward the lap to insert an arm into the sleeve
 Trunk extension: Observed as the patient realigns the trunk, continues to pull up the sleeve, and inserts the head into the shirt
Trunk extension: Observed as the patient realigns the trunk, continues to pull up the sleeve, and inserts the head into the shirt
 Trunk rotation with extension: May be necessary for reaching posteriorly and adjusting the orientation of the shirt and/or tucking the shirt into the pants
Trunk rotation with extension: May be necessary for reaching posteriorly and adjusting the orientation of the shirt and/or tucking the shirt into the pants
Button-down shirt.
Putting on a button-down shirt requires the following movements:
 Trunk flexion: Used to orient the shirt correctly on the lap for preparation of donning and to guide the arm into the sleeve when the trunk is inclined forward
Trunk flexion: Used to orient the shirt correctly on the lap for preparation of donning and to guide the arm into the sleeve when the trunk is inclined forward
 Trunk extension: Required to realign the trunk from the previous position
Trunk extension: Required to realign the trunk from the previous position
 Trunk rotation with extension: Used to reach with the more functional arm behind the head and to the opposite shoulder to grasp the collar of the shirt and pull it to the opposite side (Fig. 7-8); also used to move the second arm through the sleeve and tuck the shirt into the pants
Trunk rotation with extension: Used to reach with the more functional arm behind the head and to the opposite shoulder to grasp the collar of the shirt and pull it to the opposite side (Fig. 7-8); also used to move the second arm through the sleeve and tuck the shirt into the pants
 Trunk flexion: Used as the patient attempts to button the shirt; more often used as relaxation position (a slumped posture) rather than an active flexion pattern
Trunk flexion: Used as the patient attempts to button the shirt; more often used as relaxation position (a slumped posture) rather than an active flexion pattern
Lower extremity dressing (seated).
Putting on pants, underwear, shoes, and socks requires the following movements:
 Trunk flexion: Required to reach down toward the feet (Fig. 7-9)
Trunk flexion: Required to reach down toward the feet (Fig. 7-9)
 Trunk rotation with flexion: Required to reach the more functional arm toward the opposite foot
Trunk rotation with flexion: Required to reach the more functional arm toward the opposite foot
 Trunk extension: Required to realign the trunk from the previous positions
Trunk extension: Required to realign the trunk from the previous positions
 Lateral flexion: Required when using a crossed-leg method to don/doff pants, underwear, or footwear (the crossed-leg position shifts the patients’ center of gravity posteriorly, placing increased demand on the abdominal muscles [i.e., controlling the trunk in flexion while preventing a posterior fall]) (Fig. 7-10); also required to pull pants and underwear up or down over the buttocks and hips successfully
Lateral flexion: Required when using a crossed-leg method to don/doff pants, underwear, or footwear (the crossed-leg position shifts the patients’ center of gravity posteriorly, placing increased demand on the abdominal muscles [i.e., controlling the trunk in flexion while preventing a posterior fall]) (Fig. 7-10); also required to pull pants and underwear up or down over the buttocks and hips successfully
Grooming
Oral care.
Hygiene of the mouth requires the following movements:
 Trunk flexion: Isometric control commonly used to position the head over the sink to preventing spillage of toothpaste and saliva onto clothing; increased trunk flexion for expectorating (toothpaste and mouthwash) after completion of tooth brushing
Trunk flexion: Isometric control commonly used to position the head over the sink to preventing spillage of toothpaste and saliva onto clothing; increased trunk flexion for expectorating (toothpaste and mouthwash) after completion of tooth brushing
 Trunk extension: Used to realign body from previous position; also used to reach for supplies in a medicine cabinet over a sink and during gargling
Trunk extension: Used to realign body from previous position; also used to reach for supplies in a medicine cabinet over a sink and during gargling
 Trunk rotation with flexion: May be used to reach toward and adjust the faucet opposite the arm being used
Trunk rotation with flexion: May be used to reach toward and adjust the faucet opposite the arm being used
Hair care.
Hair care requires the following movements:
 Trunk flexion or extension: May be used isometrically during hair washing; trunk flexion is used if patients prefer to lean forward and allow the lather to be rinsed off in front of them; trunk extension (and head/neck extension) is used if patients prefer to lean back and allow the lather to be rinsed off behind them; both may be used during hair combing to accentuate the position of the head and optimally position the brush or comb to make contact with the scalp
Trunk flexion or extension: May be used isometrically during hair washing; trunk flexion is used if patients prefer to lean forward and allow the lather to be rinsed off in front of them; trunk extension (and head/neck extension) is used if patients prefer to lean back and allow the lather to be rinsed off behind them; both may be used during hair combing to accentuate the position of the head and optimally position the brush or comb to make contact with the scalp
 Lateral flexion: May be used during hair washing or combing (initiated by upper trunk) as the head is tilted to the right or left side; also may be used for optimal head placement
Lateral flexion: May be used during hair washing or combing (initiated by upper trunk) as the head is tilted to the right or left side; also may be used for optimal head placement
Eating
Eating requires the following movements:
 Trunk flexion and extension: Used in varying degrees with a hand-to-mouth pattern in which an anterior weight shift of the trunk toward the table occurs (Fig. 7-11) to position the mouth over the plate as food enters. (The degree to which this weight shift occurs depends on the type of food being eaten. Food that is hot or liquid requires increased flexion toward the plate or bowl. The increased flexion reduces the distance the food must be transported, thereby reducing spillage opportunities.)
Trunk flexion and extension: Used in varying degrees with a hand-to-mouth pattern in which an anterior weight shift of the trunk toward the table occurs (Fig. 7-11) to position the mouth over the plate as food enters. (The degree to which this weight shift occurs depends on the type of food being eaten. Food that is hot or liquid requires increased flexion toward the plate or bowl. The increased flexion reduces the distance the food must be transported, thereby reducing spillage opportunities.)
 Trunk rotation: May be used in flexion and extension to reach for condiments that are across the midline of the trunk
Trunk rotation: May be used in flexion and extension to reach for condiments that are across the midline of the trunk
 Lateral flexion: Lower trunk initiation may be used in reaching for condiments that are positioned to the side of the place setting and beyond arm’s length and also may be used with trunk rotation postures (Fig. 7-12); upper trunk initiation may be used when reaching for an object that drops on the floor to the side of the patient.
Lateral flexion: Lower trunk initiation may be used in reaching for condiments that are positioned to the side of the place setting and beyond arm’s length and also may be used with trunk rotation postures (Fig. 7-12); upper trunk initiation may be used when reaching for an object that drops on the floor to the side of the patient.
Bathing (seated on a tub seat or bench).
Bathing requires the following movements:
 Trunk flexion and extension: Required to reach toward the lower extremities and then realign
Trunk flexion and extension: Required to reach toward the lower extremities and then realign
 Trunk rotation: Trunk rotation with flexion is used to reach down toward the opposite lower extremity for lower leg and foot washing; trunk rotation with extension may be used when reaching posteriorly to wash back and neck. (In general, trunk rotation is used when reaching across the midline of the trunk. The amount of flexion and extension depends on the area of the body being washed [e.g., flexion for lower body washing; extension for upper body washing].)
Trunk rotation: Trunk rotation with flexion is used to reach down toward the opposite lower extremity for lower leg and foot washing; trunk rotation with extension may be used when reaching posteriorly to wash back and neck. (In general, trunk rotation is used when reaching across the midline of the trunk. The amount of flexion and extension depends on the area of the body being washed [e.g., flexion for lower body washing; extension for upper body washing].)
 Lateral flexion: Lower trunk initiation is required to wash the perineum and rectal areas; upper trunk initiation may be used to wash the sides of the lower legs or to pick up a bar of soap from the bottom of the tub. (Bathing activities place extra demands on trunk control because of the slippery nature of the support surface.)
Lateral flexion: Lower trunk initiation is required to wash the perineum and rectal areas; upper trunk initiation may be used to wash the sides of the lower legs or to pick up a bar of soap from the bottom of the tub. (Bathing activities place extra demands on trunk control because of the slippery nature of the support surface.)
Toileting.
Using the toilet requires the following movements:
 Lateral flexion: Lower trunk initiation may be used depending on the sequence of clothing management for toileting and the type of transfer being used (for example, if patients are performing a sit-pivot transfer, clothing usually is managed from the seated position. Therefore, lateral flexion is necessary so that pants and underwear can clear the hips/buttocks.); may also be used for wiping after toileting.
Lateral flexion: Lower trunk initiation may be used depending on the sequence of clothing management for toileting and the type of transfer being used (for example, if patients are performing a sit-pivot transfer, clothing usually is managed from the seated position. Therefore, lateral flexion is necessary so that pants and underwear can clear the hips/buttocks.); may also be used for wiping after toileting.
 Trunk rotation with extension: Used to reach across the body for toilet paper
Trunk rotation with extension: Used to reach across the body for toilet paper
 Trunk flexion: May be used for self-catheterization, application of a condom-style catheter, management of feminine hygiene products, and wiping after toileting
Trunk flexion: May be used for self-catheterization, application of a condom-style catheter, management of feminine hygiene products, and wiping after toileting
Bridging.
Bridging requires trunk extension, which is necessary at the trunk and hips to assume a functional bridge position. (The height of the bridge depends on the task. For example, bridging to use a bedpan requires more extension than bridging to don/doff pants.) See Chapter 14.
Scooting.
Scooting requires the following movement:
 Trunk flexion and extension: Must be balanced for successful scooting (The efficiency of the scooting pattern is compromised if the patient maintains a flexed trunk with a posterior pelvic tilt or a hyperextended trunk.)
Trunk flexion and extension: Must be balanced for successful scooting (The efficiency of the scooting pattern is compromised if the patient maintains a flexed trunk with a posterior pelvic tilt or a hyperextended trunk.)
 Lateral flexion: Lower trunk initiation is used to clear the buttocks from the support surface, which is required to advance the hip forward.
Lateral flexion: Lower trunk initiation is used to clear the buttocks from the support surface, which is required to advance the hip forward.
 Trunk rotation with extension: Lower trunk initiation allows the patient to achieve the goal of scooting forward.
Trunk rotation with extension: Lower trunk initiation allows the patient to achieve the goal of scooting forward.
Treatment techniques to enhance trunk control during task performance
Assuming an appropriate starting posture
Before initiation of tasks and retraining of trunk control, the trunk must be in a proper biomechanical alignment. Therapists should observe patients anteriorly, posteriorly, and laterally to detect deviations from normal alignment (see Table 7-8).
Physically or verbally cueing patients to assume an appropriate starting posture should place them in a position of readiness for function-optimal symmetry in the trunk that is usually in midline, depending on the task (Box 7-3).
This neutral starting posture is similar to the position the trunk and lower extremities assume when a person begins a typing task.
An aligned and upright trunk posture has been shown to recruit muscle activity in the trunk. Floyd and Silver’s electromyographic studies25 demonstrated that a “slumped” position while sitting (simultaneous trunk flexion and extension of the hip joint) resulted in trunk extensor relaxation. In contrast, sitting upright in a chair without a backrest resulted in increased activity of the erector spinae muscle group. This muscle activity persisted as long as the trunk remained in extension, despite adjustments of the head and shoulders. A “slumped” posture, which consists of trunk flexion, posterior pelvic tilt, and resulting hip extension, is observed commonly during evaluation of posture in the stroke population; the position requires minimal skeletal muscle activity.
Andersson and Ortengren’s review of the literature1 demonstrated that the position of the feet had an effect on the myoelectric activity of the trunk extensors. Knee flexion (causing the feet to come toward the chair) increased muscle activity in the trunk, whereas knee extension resulted in a decrease in muscle activity. Stroke patients commonly assume a seated posture in which their feet (especially the more affected lower extremity) are positioned on the floor in front of their knees (e.g., in knee extension). The position of the feet tends to have an effect on pelvic tilt and resultant trunk postures. When the feet are positioned under the knees and toward the chair, an anterior pelvic tilt and trunk extension are enhanced. The opposite is also true: when the feet are positioned in front of the knees and the knees are extended, a posterior pelvic tilt and resulting trunk flexion are enhanced.
More recently, there is further empirical evidence that a neutral spine/starring position should be encouraged from both a neuromuscular and functional perspective. Cholewicki and colleagues13 demonstrated that antagonistic trunk flexor-extensor muscle coactivation was present around the neutral spine posture in healthy individuals, and this coactivation increased with added mass to the torso. Gillen and colleagues29 examined the effects of various seated trunk postures on upper extremity function. Fifty-nine adults were tested using the Jebsen Taylor Hand Function Test while in three different trunk postures. Significant mean differences between the neutral versus the flexed and laterally flexed trunk postures were noted during selected tasks. Specifically, dominant hand performance during the tasks of feeding and lifting heavy cans was significantly slower while the trunk was flexed and laterally flexed than when performed in the neutral trunk position. Performance of the nondominant hand during the tasks of picking up small objects, page turning, and the total score was slower while the trunk was flexed compared with performance in the neutral trunk position. These findings support the assumption that neutral trunk posture improves upper extremity performance during daily activities, although the effect is not consistent across tasks.
Patients should be encouraged to feel the difference between an aligned and a malaligned posture. The patient should be able to assume an appropriate posture automatically. Demonstration of the effect that a slumped posture has on reaching activities performed with the side less affected by the stroke may be helpful. Patients may realize that the distance and quality of their reach is enhanced when they are sitting in a proper alignment.
Although the use of mirrors for visual feedback may be appropriate for some patients, mirrors should be used with caution for patients with neurobehavioral deficits. Another technique for assisting patients with gaining symmetry is to have the therapist positioned in front of the patient and to assume the patient’s postures to provide feedback for the patient. Therapists should slowly correct their posture, instructing the patient to mimic the movement. The therapist may state, “Keep your shoulders in line with mine” or “Keep your forehead at the same level as mine.”
Mohr40 emphasizes use of activities that encourage rotation and lateral flexion to gain midline control: “the active movements of the trunk into rotation and lateral flexion are caused by the same muscles that flex and extend the trunk. The different movements occur as a result of different interactions of these muscles with each other . . . In order for patients to achieve midline postural control, the therapist must work with the patient in the higher levels of lateral and rotational planes of movement.”
Maintaining or increasing trunk range of motion through mobilization and movement
Concerning ROM in the trunk, Mohr40 states, “If there is not full range in all trunk movements (flexion extension, lateral flexion, and rotation), it will be more difficult to gain full control of the trunk. Any lack of ROM in the trunk will lead to decreased function.”
Although limited ROM in the extremities is commonly evaluated and treated, the ROM in the spine often is overlooked. After acute strokes, patients lose the ability to shift their weight and make postural adjustments. Evaluating patients who have trunks influenced completely by gravity and who demonstrate only static trunk postures is common. In these cases, prolonged immobilization of the trunk because of loss of control can result in loss of softtissue elasticity, joint play, and ultimately function. These problems, compounded by inappropriate trunk positioning and support in upright postures, lead to a cycle of immobility, soft-tissue changes, loss of range, and impaired functional abilities.
Specific trunk mobilization techniques are beyond the scope of this chapter but are discussed in the literature.8,16,22,40 Just as therapists train patients to perform self-ROM activities for their extremities, therapists must promote patient awareness of trunk mobility and educate them about specific movement patterns that maintain and/or increase their trunk ROM. Following are examples of movement patterns that patients can perform to meet this goal:
1. While supine, patients flex their hips and knees as if preparing to bridge. Patients are instructed to keep their shoulders flat on the bed and simultaneously allow their knees to fall slowly from one side and then the other. This movement pattern encourages dissociation from the upper and lower trunk (rotation).
2. While supine, patients keep their hips and knees straight while cradling their more affected upper extremity. The goal is to lift and rotate the upper trunk as if initiating a roll with the upper trunk (rotation).
3. While sitting, patients cradle their more affected upper extremity against their chest. The therapist encourages patients to move the upper trunk in a twisting motion without letting the pelvis move (rotation).
4. While sitting, patients practice moving from an upright posture to a posture of lateral flexion on one side so that they are bearing weight on their forearm to the side of their trunk. The pelvis should remain stable on the support surface for optimal stretch (lateral flexion).
5. While sitting, patients hold their more affected wrist and reach to the floor between their feet. The therapist also encourages them to allow their head to drop and dangle (flexion).
6. While supine, patients assume a bridge posture and hold the position as able (extension).
7. While sitting, patients practice lifting their hip from the support surface. This movement can be enhanced by having the patient reach up and to the side with the opposite upper extremity. Reaching beyond the arm span in this posture requires lateral flexion for the reach pattern to be successful (lateral flexion).
Using various postures
Therapists may use various postures as an adjunct treatment during patients’ performance of functional tasks. Therapists should select postures based on specific patient needs. The chosen posture should accentuate and challenge the movement and control patterns interfering with independent performance of life activities. If the patient is not engaging in a specific activity (self-care tasks, games, and adapted sports), the use of these postures in isolation is not encouraged. Examples of varying postures include the following:
 Seated with legs crossed: Use of this posture is appropriate for patients whose inability to control lateral flexion and flexion patterns and to shift their weight is preventing functional independence. Working with patients in this posture encourages weight transference to one ischial tuberosity and has the added effect of challenging abdominal control. This occurs because the crossed leg is in a position of hip flexion. When the hips are flexed, the traction on the hamstrings tends to tilt the pelvis posteriorly,33 resulting in a posterior shift in the center of gravity. Abdominal control therefore is required to prevent a posterior loss of balance. Participation in tasks such as lower extremity dressing, lower body washing, and activities such as modified volleyball place extra demands on patients who are in this position.
Seated with legs crossed: Use of this posture is appropriate for patients whose inability to control lateral flexion and flexion patterns and to shift their weight is preventing functional independence. Working with patients in this posture encourages weight transference to one ischial tuberosity and has the added effect of challenging abdominal control. This occurs because the crossed leg is in a position of hip flexion. When the hips are flexed, the traction on the hamstrings tends to tilt the pelvis posteriorly,33 resulting in a posterior shift in the center of gravity. Abdominal control therefore is required to prevent a posterior loss of balance. Participation in tasks such as lower extremity dressing, lower body washing, and activities such as modified volleyball place extra demands on patients who are in this position.
 Sitting in front of a table while bearing weight on both forearms: Ryerson and Levit44 recommend this posture during the acute stage of hemiplegia when little postural control is evident. In this posture, patients use their upper extremities as a point of proximal stability. The therapist should stress that the arm should be active and the trunk should not be allowed to “hang” on an inactive arm. Patients are encouraged to practice anterior, posterior, and lateral shifting in this posture to reestablish postural control; coordinate trunk, scapula, and humerus patterns; and to establish weight-bearing of the upper extremities. Because both arms are engaged in a weight-bearing activity, patient participation in functional tasks is difficult. Immediately following use of this posture, the therapist must engage the patient in a follow-up activity such as reaching to ensure the postures can be incorporated into ADL.
Sitting in front of a table while bearing weight on both forearms: Ryerson and Levit44 recommend this posture during the acute stage of hemiplegia when little postural control is evident. In this posture, patients use their upper extremities as a point of proximal stability. The therapist should stress that the arm should be active and the trunk should not be allowed to “hang” on an inactive arm. Patients are encouraged to practice anterior, posterior, and lateral shifting in this posture to reestablish postural control; coordinate trunk, scapula, and humerus patterns; and to establish weight-bearing of the upper extremities. Because both arms are engaged in a weight-bearing activity, patient participation in functional tasks is difficult. Immediately following use of this posture, the therapist must engage the patient in a follow-up activity such as reaching to ensure the postures can be incorporated into ADL.
 Prone on elbows: Although effective for gaining trunk extension, this position should be used with caution. The position may compromise respiratory status, cause shoulder pain if upper extremity alignment is not considered, and be generally uncomfortable for older stroke patients. The position may be effective for some patients and may be a required posture for some transitional movements such as floor-to-chair transfers.
Prone on elbows: Although effective for gaining trunk extension, this position should be used with caution. The position may compromise respiratory status, cause shoulder pain if upper extremity alignment is not considered, and be generally uncomfortable for older stroke patients. The position may be effective for some patients and may be a required posture for some transitional movements such as floor-to-chair transfers.
 Kneeling: This posture is appropriate for patients having trouble in gaining trunk/hip extension. Patients also may find this posture uncomfortable, but it may be necessary for transitional patterns.
Kneeling: This posture is appropriate for patients having trouble in gaining trunk/hip extension. Patients also may find this posture uncomfortable, but it may be necessary for transitional patterns.
 Variations on the degree of hip flexion while seated: Changing the position of the lower extremities can challenge the performance of specific trunk patterns. Being in a position with the knees below the hips, such as sitting on a high stool, decreases the amount of hip flexion and has a tendency to place the trunk in increased extension.
Variations on the degree of hip flexion while seated: Changing the position of the lower extremities can challenge the performance of specific trunk patterns. Being in a position with the knees below the hips, such as sitting on a high stool, decreases the amount of hip flexion and has a tendency to place the trunk in increased extension.
Conversely, positioning the patient with the knees above the hips (increasing the amount of hip flexion) results in a position of trunk flexion and a posterior weight shift, which places greater demands on the trunk flexors.
Treating the “pusher syndrome” or contraversive pushing
The “pusher syndrome” is a phrase coined by Davies,19 who derived the name from what she felt was the most striking aspect of this syndrome: the patient pushes heavily toward the hemiplegic side in all positions and resists any attempt at passive correction (i.e., a correction that would bring the weight toward or over the midline of the body to the unaffected side). This phenomenon has been documented in patients with both right and left hemispheric lesions. Further analysis has revealed that the brain structure typically damaged in patients with pusher syndrome is the left or right posterolateral thalamus.36
Danells and colleagues15 defined pushing as “resistant to accepting weight on and actively ‘push’ away from the nonparetic side.” The authors identified pushers (n=65) from stroke patients with moderate to severe hemiparesis and examined longitudinal changes in symptoms, level of impairment, and functional independence. Assessments were performed within 10 days postonset, at six weeks, and at three months. The authors found:
 At one week after stroke, 63% of patients demonstrated features of pushing.
At one week after stroke, 63% of patients demonstrated features of pushing.
 In 62% of pushers, symptoms resolved by six weeks, whereas in 21%, pushing symptoms persisted at three months.
In 62% of pushers, symptoms resolved by six weeks, whereas in 21%, pushing symptoms persisted at three months.
 Motor recovery and functional abilities at three months were significantly lower among the pushers compared with the nonpushers.
Motor recovery and functional abilities at three months were significantly lower among the pushers compared with the nonpushers.
 Pushers also had a significantly longer hospital length of stay (89 days versus 57 days).
Pushers also had a significantly longer hospital length of stay (89 days versus 57 days).
 Motor and functional recovery improved significantly over the three-month study period for both pushers and nonpushers.
Motor and functional recovery improved significantly over the three-month study period for both pushers and nonpushers.
 Although the pushers had greater lengths of stay in both acute care and rehabilitation facilities, they were discharged home with similar frequency to the nonpushers.
Although the pushers had greater lengths of stay in both acute care and rehabilitation facilities, they were discharged home with similar frequency to the nonpushers.
Perennou and colleagues42 investigated whether the pusher syndrome affects only the trunk for which gravitational feedback is given by somesthetic information, or the head as well (gravitational information given by the vestibular system). The results of their pilot study indicated that that the pusher syndrome does not result from disrupted processing of vestibular information but from a higher-order disruption in the processing of somesthetic information originating in the left hemibody, which could be an extinction phenomenon. The authors felt that this disruption leads pushers actively to adjust their body posture to a subjective vertical bias to the side opposite the lesion.
Pedersen and colleagues41 also examined the pusher syndrome. The study examined the incidence of the syndrome, the relation of this syndrome to neurobehavioral deficits, and the effect of the syndrome on the rehabilitation process in 327 patients. The study revealed a 10% incidence and found no significant differences in hemineglect or anosognosia in patients with and without ipsilateral pushing. The study discovered that patients who demonstrated ipsilateral pushing required 3.6 weeks longer to reach the same outcome as patients who did not demonstrate ipsilateral pushing. Of note in this study are the Barthel index scores at admission and discharge. On admission, patients who demonstrated ipsilateral pushing scored an average of 13.7 on the Barthel index compared with 46.8 for patients without evidence of pushing. On discharge, the average score for pushers was 43.9 compared with 66.8 for patients without pushing. The discharge scores (in terms of ADL function) of the patients who were pushers were still below the admission scores for patients who did not push.
Davies17 summarizes the typical signs of the pusher syndrome as the following:
 Head turned away from affected side and laterally flexed toward stronger side
Head turned away from affected side and laterally flexed toward stronger side
 Decreased ability to perceive stimuli from affected side
Decreased ability to perceive stimuli from affected side
 Poor breath control with monotone, hypophonic voice
Poor breath control with monotone, hypophonic voice
 Evidence of pushing with stronger leg while supine
Evidence of pushing with stronger leg while supine
 Holding onto side of bed or mat as if falling
Holding onto side of bed or mat as if falling
 Shortening of stronger side of trunk with elongation of hemiplegic side while sitting
Shortening of stronger side of trunk with elongation of hemiplegic side while sitting
 Marked resistance to attempts to transfer weight to stronger side
Marked resistance to attempts to transfer weight to stronger side
 Pushing with stronger arm and leg to more affected side
Pushing with stronger arm and leg to more affected side
 Difficulty transferring, especially to stronger side
Difficulty transferring, especially to stronger side
 All weight shifted to affected side while standing; leaning against therapist’s supporting arm or flexing forward at hips
All weight shifted to affected side while standing; leaning against therapist’s supporting arm or flexing forward at hips
 Hemiplegic leg adduction (scissors) when walking; difficulty taking a step with affected leg because of an inability to shift weight to stronger side
Hemiplegic leg adduction (scissors) when walking; difficulty taking a step with affected leg because of an inability to shift weight to stronger side
Pushing can be quantified via the Scale for Contraversive Pushing (SCP).35 It is scored 0 to 6 with higher the scores indicating a greater severity of pushing. There are three domains (posture, extension, and resistance) that are assessed for both sitting and standing positions (i.e., six scored items) (Box 7-4). Using a cut score of greater than 0 in each section appears to increase the agreement of clinical and SCP observations and has been suggested.4
Box 7-4 The Scale for Contraversive Pushing
| (A) Posture (symmetry of spontaneous posture) | Sitting | Standing |
| Score 1 = severe contraversive tilt with falling to the contralesional side | h | h |
| Score 0.75 = severe contraversive tilt without falling | h | h |
| Score 0.25 = mild contraversive tilt without falling | h | h |
| Score 0 = no tilt/upright body orientation | h | h |
| Total (max = 2): | ||
| (B) Extension (use of the arm/leg to extend the area of physical contact to the ground) | ||
| Score 1 = performed already in rest | h | h |
| Score 0.5 = performed not until position is changed | h | h |
| Score 0 = no extension | h | h |
| Total (max = 2): | ||
| (C) Resistance (resistance to passive correction of posture to an upright position) | ||
| Score 1 = resistance is shown | h | h |
| Score 0 = resistance is not shown | h | h |
| Total (max = 2): |
Note: For section B: For sitting, ask the patient to glide the buttocks on the mattress toward the nonparetic side, to transfer from bed to wheelchair toward the nonparetic side, or both. For standing, ask the patient to start walking. If pushing already occurs when the patient is rising from the sitting position, section B is given the value of 1 for standing.
For section C: Touch the patient at the sternum and the back. Give the following instructions: “I will move your body sideward. Please permit this movement.”
Translated from Karnath HO, Ferber S, Dichgans J: The origin of contraversive pushing. Neurology 55(9):1298-1304, 2000.
Unfortunately at this point, specific interventions are based on anecdotal evidence only, but they may still be helpful to clinicians. Davies17 recommends the following specific treatments for the pusher syndrome:
 Restore head movements: maintain full passive ROM, stretch, and encourage active ROM by scanning activities.
Restore head movements: maintain full passive ROM, stretch, and encourage active ROM by scanning activities.
 Activate the side flexors (see activities described in previous sections).
Activate the side flexors (see activities described in previous sections).
Karnath and Broetz37 recommend the following intervention sequence:
 Realize the disturbed perception of erect body position.
Realize the disturbed perception of erect body position.
 Visually explore the surroundings and the body’s relation to the surroundings. Ensure that the patient sees whether he or she is oriented upright. The therapist should use visual aids that give feedback about body orientation (i.e., the therapist’s arm) and work in a room containing many vertical structures, such as door frames, windows, pillars, and so on.
Visually explore the surroundings and the body’s relation to the surroundings. Ensure that the patient sees whether he or she is oriented upright. The therapist should use visual aids that give feedback about body orientation (i.e., the therapist’s arm) and work in a room containing many vertical structures, such as door frames, windows, pillars, and so on.
 Learn the movements necessary to reach a vertical body position.
Learn the movements necessary to reach a vertical body position.
 Maintain the vertical body position while performing other activities.
Maintain the vertical body position while performing other activities.
A hands-on approach does not seem to be effective with patients who have the pusher syndrome; therapists’ attempts to assist patients with gaining midline by handling is met by further patient resistance. Manipulating the environment and providing external cues (verbal) seem to be more effective. Examples include the following:
 Have patients reach with their stronger upper extremity for objects beyond their arm span to encourage a weight shift to the stronger side.
Have patients reach with their stronger upper extremity for objects beyond their arm span to encourage a weight shift to the stronger side.
 Provide verbal cues to realign the trunk, such as, “Bring your head toward mine” and “Bring your left shoulder toward the wall.”
Provide verbal cues to realign the trunk, such as, “Bring your head toward mine” and “Bring your left shoulder toward the wall.”
 Provide a target toward which patients can move their trunk and maintain the position as long as possible. For example, place a bolster on patients’ stronger side, and cue them to lean against the bolster and hold the position.
Provide a target toward which patients can move their trunk and maintain the position as long as possible. For example, place a bolster on patients’ stronger side, and cue them to lean against the bolster and hold the position.
 Remove surfaces from which to push. For example, raise the hospital bed or therapy table, so that the person’s foot is not on the floor and place a movable surface (e.g., small ball) under the less affected foot to prevent pushing.
Remove surfaces from which to push. For example, raise the hospital bed or therapy table, so that the person’s foot is not on the floor and place a movable surface (e.g., small ball) under the less affected foot to prevent pushing.
Further empirical intervention studies are needed in this area of practice.
Engaging in reaching tasks
Therapists can use placement of objects in reaching activities as a way to place a variety of demands on the trunk. The key to eliciting a trunk response is to place the object slightly beyond the arm’s reach. Fisher24 observes that when subjects without brain injuries reach, they anteriorly tilt the pelvis, slightly extend the upper back, and move the trunk in the direction of the arm. Patients with brain injuries do not incorporate trunk movements into arm movements and reach only to arm’s length as they maintain a slumped posture.
Therapists have the ability to control the desired response by the way they set up the activity. Setting up the activity includes placing items required during ADL in specific places, choosing the appropriate environment (e.g., kitchen with upper and lower shelves, bookcase, desk space, meal table), deciding how far beyond the arm span the activity should be placed, and deciding on the characteristics of the objects the patient is reaching for (number of objects, weight of the objects, and whether objects require one or two hands). Table 7-11 includes examples of activity placement and resulting trunk response.
Table 7-11 Examples of Grading Activities during Reaching Tasks
| EASIER | MORE DIFFICULT | |
| Sitting surface | Firm and stable surface | Cushioned or unstable surface |
| Full thigh support | Partial thigh support | |
| Object | Within arm’s reach | Beyond arm’s reach |
| Light (e.g., a pencil) | Heavy (e.g., bag of flour) | |
| Use of arms | Reach with one arm | Reach with both arms |
| External support | Maximum via therapist, bolsters, and so on | None |
| Prediction | Predictable (e.g., lift stationary object) | Unpredictable (e.g., catch a ball) |
Dean and Shepard18 investigated, via a randomized placebo-controlled trial of task-related training after stroke, the effect of a training program designed to improve the ability to balance in sitting after stroke. The training program was designed to improve sitting balance and involved emphasis on appropriate loading of the affected leg while at the same time practicing reaching tasks using the unaffected hand to grasp objects located beyond arm’s length. The reaching tasks were performed under varied conditions. Changing the location of the object that the subject was reaching for varied the distance and direction of reach. Seat height, movement speed, object weight, and extent of thigh support were also varied. Increasing the number of repetitions and complexity of the tasks advanced the training. The authors found that after training, subjects were able to reach faster and farther, increase load through the affected foot, and increase activation of affected leg muscles compared with the control group (highlighting the critical contribution of the lower extremities in promoting sitting balance). The experimental group also improved in sit to stand. The control group did not improve in reaching or sit to stand, and finally, neither group improved in walking. See Tables 7-9 and 7-11 for suggestions to grade reaching tasks.
Using movable surfaces
Several authors have advocated the use of movable surfaces to challenge trunk control.8,16,32 Movable surfaces used in treatment include items such as therapy balls, bolsters, and rocker boards. Movable surfaces can be used in treatment in a variety of ways, including the following:
 To grade the difficulty of the task
To grade the difficulty of the task
 To challenge the patient to maintain control of the surface without outside assistance (challenge isometric patterns)
To challenge the patient to maintain control of the surface without outside assistance (challenge isometric patterns)
 To allow the patient to respond to the therapist’s perturbation of the movable surface
To allow the patient to respond to the therapist’s perturbation of the movable surface
 To allow the patient to initiate moving the surface
To allow the patient to initiate moving the surface
 To enhance stretching and mobilization of the trunk by using a particular surface such as a large ball
To enhance stretching and mobilization of the trunk by using a particular surface such as a large ball
Use of movable surfaces may be appropriate for patients who are experiencing difficulty controlling their trunk in environments with external perturbations (e.g., trains, automobiles, and buses). Although movable surfaces are used commonly in the clinic, research concerning the effectiveness of this type of treatment compared with other types is lacking. One may argue that when patients master trunk control on a movable surface (a difficult situation), their control will improve on less demanding surfaces (surfaces that do not move). Unfortunately, this argument is not supported by current research that advocates task-specific training.
Handling
Handling is a common technique used in the clinic. This intervention commonly is associated with neurodevelopmental therapy7 and may allow the patient to feel the desired movement pattern, gain range, assist weak movement patterns, and provide external support to prevent falls. To be effective, the patient must be aware of the goal associated with handling, and the therapist should use handling within the context of a functional task. In addition, the handling from the therapist should be graded to allow the patient to perform as much of the movement pattern as possible. A variety of texts that review specific techniques of handling are available.7,8,16,17,22,32 Although handling is commonly used, research does not support use of this technique (see Chapter 6).
Using activities of daily living and mobility tasks
Clearly the most effective tools that occupational therapists can use to help patients regain trunk control are self-care, instrumental ADL, and mobility tasks.
The therapist first must perform a thorough evaluation as described in previous sections. Following the evaluation, therapists and patients should identify the most problematic movement patterns that occur during the patients’ daily activities. At this point, therapists use their activity analysis skills to choose appropriate tasks that incorporate the desired patterns and postures as described previously. For example, if the identified problematic patterns are lateral flexion and lateral weight shifts, therapists may choose the following activities for the patient to practice:
 Weight shifting for pressure relief
Weight shifting for pressure relief
 Assuming a sitting position from side-lying position
Assuming a sitting position from side-lying position
 Reaching for objects that are positioned above and to the side of the patient opposite the side where lateral flexion is desired
Reaching for objects that are positioned above and to the side of the patient opposite the side where lateral flexion is desired
 Reaching for objects on the floor that are on the side of the patient
Reaching for objects on the floor that are on the side of the patient
The majority of ADL and mobility tasks encompass a variety of postures and movements. For the mentioned strategies to be effective, therapists should initially focus patients’ attention on the desired components of trunk movements. As the patient progresses, the obvious goal is for the trunk responses to be relearned and become automatic.
Therapeutic exercise
A recent pilot randomized controlled trial55 (N = 33) documented that conventional occupational and physical therapy combined with additional trunk exercises aimed at improving sitting balance and selective trunk movements has a positive effective on the selective performance of lateral flexion after stroke. Specifically, the experimental group received 10 hours of additional trunk exercises that included:
 Supine exercises with legs bent and meet on the therapy table: anterior/posterior pelvic movements, bridging, and trunk rotation, initiated from the upper and lower trunk
Supine exercises with legs bent and meet on the therapy table: anterior/posterior pelvic movements, bridging, and trunk rotation, initiated from the upper and lower trunk
 In sitting: flexion and extension of the trunk without moving the trunk forward or backward, flexion/extension of the lumbar spine, flexion/extension of the hips with the trunk extended, lateral flexion of the trunk initiated from the shoulder and pelvic girdle, upper and lower trunk rotation, and scooting forward and backwards.
In sitting: flexion and extension of the trunk without moving the trunk forward or backward, flexion/extension of the lumbar spine, flexion/extension of the hips with the trunk extended, lateral flexion of the trunk initiated from the shoulder and pelvic girdle, upper and lower trunk rotation, and scooting forward and backwards.
Adapting the environment
Some patients may have little improvement in trunk control. Environmental adaptations are necessary for these patients to enhance independent performance. Examples include
 Use of outside supports can help maintain trunk stability while the extremities are engaged in functional tasks. Supports such as lateral supports, anterior chest straps, arm chairs, pillows and cushions for propping, and lap trays are examples of equipment used to compensate for compromised trunk control (see Chapter 26).
Use of outside supports can help maintain trunk stability while the extremities are engaged in functional tasks. Supports such as lateral supports, anterior chest straps, arm chairs, pillows and cushions for propping, and lap trays are examples of equipment used to compensate for compromised trunk control (see Chapter 26).
 Rearrangement of the environment can decrease demands on the trunk. Placing required equipment within the patient’s reach (arm reach) not only increases independence but also may prevent falls. Storing dishes on the counter instead of in a cabinet, placing utensils in front of the patient, and keeping grooming items on top of the sink instead of in a medicine cabinet are examples of this strategy.
Rearrangement of the environment can decrease demands on the trunk. Placing required equipment within the patient’s reach (arm reach) not only increases independence but also may prevent falls. Storing dishes on the counter instead of in a cabinet, placing utensils in front of the patient, and keeping grooming items on top of the sink instead of in a medicine cabinet are examples of this strategy.
 Provision of adaptive equipment is a common strategy to increase independent performance and minimize safety risks. ADL equipment issued to compensate for poor trunk control may include the following: long-handled shoe horns, elastic laces, adapted bath brushes, soap on a rope, reachers, tub seats, and commodes. See Chapter 28 for more information on adaptive devices.
Provision of adaptive equipment is a common strategy to increase independent performance and minimize safety risks. ADL equipment issued to compensate for poor trunk control may include the following: long-handled shoe horns, elastic laces, adapted bath brushes, soap on a rope, reachers, tub seats, and commodes. See Chapter 28 for more information on adaptive devices.
 Home modifications such as grab bars and bed rails also may be indicated. See Chapter 27 for a full review of home adaptations and equipment recommendations.
Home modifications such as grab bars and bed rails also may be indicated. See Chapter 27 for a full review of home adaptations and equipment recommendations.
CASE STUDY Regaining Trunk Control after a Stroke
S.G. is a 64-year-old female who came to the rehabilitation unit after a right middle cerebral artery cerebrovascular accident. The following data were collected from the initial evaluation (specific to the trunk):
 Static postural malalignments included posterior pelvic tilt, retracted left rib cage, and increased weight-bearing on left ischial tuberosity.
Static postural malalignments included posterior pelvic tilt, retracted left rib cage, and increased weight-bearing on left ischial tuberosity. Dynamical posture was difficult to assess because the patient was afraid to move. The patient could not reach beyond her arm span when reaching with her right arm. She had a tendency to fall backward and to the left during lower extremity dressing and when reaching for objects behind her.
Dynamical posture was difficult to assess because the patient was afraid to move. The patient could not reach beyond her arm span when reaching with her right arm. She had a tendency to fall backward and to the left during lower extremity dressing and when reaching for objects behind her. S.G.’s personal occupational therapy goals were to be able independently to don her shoes, be able to reach for objects she had dropped without falling, and decrease the amount of spillage that occurred during meals.
S.G.’s personal occupational therapy goals were to be able independently to don her shoes, be able to reach for objects she had dropped without falling, and decrease the amount of spillage that occurred during meals.The initial treatment plan included adapting her wheelchair with lateral supports (which were removed when she was supervised by friends, family, and staff) and a lumbar roll to maintain optimal alignment while functioning in the wheelchair, trunk mobilizations (specifically in the directions of extension and lateral flexion to both sides), activities to recruit abdominal activity (rolling, games that encouraged trunk rotation, reaching for objects positioned overhead and behind her), and activities that presented unexpected challenges to her trunk control (e.g., balloon volleyball and catch). During the initial stages of treatment, the therapist sat behind S.G. in a straddle position, which increased feelings of security and allowed the therapist to provide outside assistance with difficult patterns and to prevent falls. S.G. was observed while eating, and the therapist noted that she did not shift her weight anteriorly when bringing food to her mouth. Instead she kept her trunk supported against the back of the chair. Because of the increased distance the food had to travel to reach her mouth, spillage was considerable, especially of liquids on a spoon (e.g., soup and cereal milk). S.G. was trained to shift her weight forward as she brought food to her mouth. Although spillage still occurred, it happened less frequently, with the food falling to the plate or table and not in her lap.
As S.G. progressed, the therapist was able to sit next to or in front of her during activities. She engaged in graded reaching activities in which the distance S.G. was required to reach was increased progressively. Activities included reaching to lower shelves in the refrigerator and reaching for objects positioned at specific levels (e.g., knee level, midshin level, and floor level).
On discharge from inpatient rehabilitation, S.G. was able to perform all basic ADL with distant supervision and without assistive devices, reach to the floor when she propped her upper trunk with her more affected forearm against her knees, and eat independently by using a rocker knife to cut her food, with spillage occurring only 10% of the time.
Review questions
1. What is considered an aligned posture in preparation for engagement in functional tasks? What are the common deviations from this posture after stroke?
2. Name three ADL tasks that require control in the rotation plane.
3. What are advantages and disadvantages of using movable surfaces in trunk control treatment?
4. What are appropriate treatment activities for patients who lack trunk extensor control?
5. Explain the reason an appropriate starting alignment is considered a prerequisite for initiating functional activities.
6. Which trunk patterns are required for donning a button-down shirt?
1. Andersson BJ, Ortengren R. Myoelectric back activity during sitting. Scand J Rehabil Med. 1974;3:73-90. Suppl
2. Árnadóttir G. The brain and behavior. assessing cortical dysfunction through activities of daily living. St. Louis: Mosby. 1990.
3. Ayres AJ. Developmental dyspraxia and adult onset apraxia. Torrance, CA: Sensory Integration International; 1985.
4. Baccini M, Paci M, Rinaldi LA. The Scale for Contraversive Pushing. a reliability and validity study. Neurorehabil Neural Repair. 2006:20;4:468-472.
5. Basmajian JV, DeLuca CJ. Muscles alive. their functions revealed by electromyography, ed 5. Baltimore: Williams & Wilkins. 1985.
6. Benaim C, Perennou DA, Villy J, et al. Validation of a standardized assessment of postural control in stroke patients. Stroke. 1999;30(9):1862-1868.
7. Bobath B. Adult hemiplegia. evaluation and treatment, ed 3. London: Butterworth-Heinemann. 1990.
8. Boehme R. Improving upper body control. an approach to the treatment of tonal dysfunction. Tucson: Therapy Skill Builders. 1988.
9. Bohannon RW. Recovery and correlates of trunk muscle strength after stroke. Int J Rehabil Res. 1995;18(2):162-167.
10. Bohannon RW. Lateral trunk flexion strength. impairment, measurement reliability and implications following unilateral brain lesion. Int J Rehabil Res. 1992:15;3:249-251.
11. Bohannon RW, Cassidy D, Walsh S. Trunk muscle strength is impaired multidirectionally after stroke. Clin Rehabil. 1995;9(1):47.
12. Carr JH, Shepherd RB, Nordholm L, et al. Investigation of a new motor assessment scale for stroke patients. Phys Ther. 1985;65(2):175-180.
13. Cholewicki J, Panjabi M, Khachatryan A. Stabilizing function of trunk flexor and extensor muscles around a neutral spine posture. Spine. 1997;22(19):2207-2212.
14. Collin C, Wade D. Assessing motor impairment after stroke. a pilot reliability study. J Neurol Neurosurg Psychiatry. 1990:53;7:576-579.
15. Danells CJ, Black SE, Gladstone DJ, et al. Poststroke “pushing”. natural history and relationship to motor and functional recovery. Stroke. 2004:35;12:2873-2878.
16. Davies PM. Right in the middle. selective trunk activity in the treatment of adult hemiplegia. New York: Springer-Verlag. 1990.
17. Davies PM. Steps to follow. a guide to the treatment of adult hemiplegia. New York: Springer-Verlag. 1985.
18. Dean CW, Shepard RB. Task-related training improves performance of seated reaching tasks after stroke. a randomized controlled trial. Stroke. 1997:28;4:722-728.
19. De Troyer A. Mechanical role of the abdominal muscles in relation to posture. Respir Physiol. 1983;53(3):341-353.
20. Dickstein R, Sheffi S, Markovici E, et al. Anticipatory postural adjustment in selected trunk muscles in post stroke hemiparetic patients. Arch Phys Med Rehabil. 2004;85(2):261-267.
21. Duarte E, Marco E, Muniesa JM, et al. Trunk control test as a functional predictor in stroke patients. J Rehabil Med. 2002;34(6):267-272.
22. Eggers O. Occupational therapy in the treatment of adult hemiplegia. New York: Springer-Verlag; 1983.
23. Esparza DY, Archambault PS, Winstein CJ, et al. Hemispheric specialization in the co-ordination of arm and trunk movements during pointing in patients with unilateral brain damage. Exp Brain Res. 2003;148(4):488-497.
24. Fisher B. Effect of trunk control and alignment on limb function. J Head Trauma Rehabil. 1987;2(2):72.
25. Floyd WF, Silver PHS. The function of the erector spinae muscles in certain movements and postures in man. J Physiol. 1955;129(1):184.
26. Franchignoni FP, Tesio L, Ricupero C, et al. Trunk control as an early predictor of stroke rehabilitation outcome. Stroke. 1997;28(7):1382-1385.
27. Fugl-Meyer AR. Post-stroke hemiplegia. assessment of physical properties. Scand J Rehabil Med. 1980;7:85-93. suppl
28. Fujiwara T, Liu M, Tsuji T, et al. Development of a new measure to assess trunk impairment after stroke (trunk impairment scale). its psychometric properties. Am J Phys Med Rehabil. 2004:83;9:681-688.
29. Gillen G, Boiangiu C, Neuman M, et al. Trunk posture affects upper extremity function of adults. Percept Mot Skills. 2007;104(2):371-380.
30. Gowland C, Stratford P, Ward M, et al. Measuring physical impairment and disability with the Chedoke-McMaster Stroke Assessment. Stroke. 1993;24;1:58-63.
31. Hsieh CL, Sheu CF, Hsueh IP, et al. Trunk control as an early predictor of comprehensive activities of daily living function in stroke patients. Stroke. 2002;33(11):2626-2630.
32. Hypes B. Facilitating development and sensorimotor function. treatment with the ball. Hugo, MN: PDP Press. 1991.
33. Kapandji IA. The physiology of the joints, vol 3, The trunk and vertebral column. New York: Churchill Livingstone; 1974.
34. Karatas M, Cetin N, Bayramoglu M, et al. Trunk muscle strength in relation to balance and functional disability in unihemispheric stroke patients. Am J Phys Med Rehabil. 2004;83(2):81-87.
35. Karnath HO, Ferber S, Dichgans J. The origin of contraversive pushing. Neurology. 2000;55(9):1298-1304.
36. Karnath H-O, Ferber S, Dichgans J. The neural representation of postural control in humans. Proc Natl Acad Sci USA. 2000;97(25):13931-13936.
37. Karnath HO, Broetz D. Understanding and treating “pusher syndrome. Phys Ther. 2003;83(12):1119-1125.
38. Kendall FP, McCreary EK, Provance P. Muscles testing and function, ed 4. Baltimore: Lippincott Williams & Wilkins; 1993.
39. Mao HF, Hsueh IP, Tang PF, et al. Analysis and comparison of the psychometric properties of three balance measures for stroke patients. Stroke. 2002;33(4):1022-1027.
40. Mohr JD. Management of the trunk in adult hemiplegia. the Bobath concept. Top Neurol. 1990:1;1:1-12.
41. Pedersen PM, Wandel A, Jorgensen HS, et al. Ipsilateral pushing in stroke. incidence, relation to neuropsychological symptoms, and impact on rehabilitationthe Copenhagen stroke study. Arch Phys Med Rehabil. 1996:77;1:25-28.
42. Perennou DA, Amblard B, Laassel el M, et al. Understanding the pusher behavior of some stroke patients with spatial deficits. a pilot study. Arch Phys Med Rehabil. 2002:83;4:570-575.
43. Ryerson S, Byl NN, Brown DA, et al. Altered trunk position sense and its relation to balance functions in people post-stroke. J Neurol Phys Ther. 2008;32(1):14-20.
44. Ryerson S, Levit K. The shoulder in hemiplegia. In Donatelli RA, editor: Physical therapy of the shoulder, ed 2, New York: Churchill Livingstone, 1991.
45. Sabari JS. Motor learning concepts applied to activity-based intervention with adults with hemiplegia. Am J Occup Ther. 1991;45(6):523-530.
46. Shumway-Cook A, Woollacott M. Motor control. theory and practical applications. Baltimore: Williams & Wilkins. 1995.
47. Smith LK, Weiss EL, Lehmkuhl LD. Brunnstrom’s clinical kinesiology, ed 5. Philadelphia: FA Davis; 1996.
48. Tanaka S, Hachisuka K, Ogata H. Muscle strength of trunk flexion-extension in post-stroke hemiplegic patients. Am J Phys Med Rehabil. 1998;77(4):288-290.
49. Tanaka S, Hachisuka K, Ogata H. Trunk rotary muscle performance in post-stroke hemiplegic patients. Am J Phys Med Rehabil. 1997;76(5):366-369.
50. Thorstensson A, Oddsson L, Carlson H. Motor control of voluntary trunk movements in standing. Acta Physiol Scand. 1985;125(2):309.
51. Verheyden G, Nieuwboer A, De Wit L, et al. Time course of trunk, arm, leg, and functional recovery after ischemic stroke. Neurorehabil Neural Repair. 2008;22(2):173-179.
52. Verheyden G, Vereeck L, Truijen S, et al. Trunk performance after stroke and the relationship with balance, gait and functional ability. Clinical Rehabilitation. 2006;20(5):451-458.
53. Verheyden G, Nieuwboer A, Mertin J, et al. The Trunk Impairment Scale. a new tool to measure motor impairment of the trunk after stroke. Clin Rehabil. 2004:18;3:326-334.
54. Verheyden G, Nieuwboer A, Van de Winckel A, et al. Clinical tools to measure trunk performance after stroke. a systematic review of the literature. Clinical Rehabilitation. 2007:21;5:387-394.
55. Verheyden G, Vereeck L, Truijen S, et al. Additional exercises improve trunk performance after stroke. a pilot randomized controlled trial. Neurorehabil Neural Repair. 2009:23;30:281-286.
56. Wang CH, Hsueh IP, Sheu CF, et al. Discriminative, predictive, and evaluative properties of a trunk control measure in patients with stroke. Phys Ther. 2005;85(9):887-894.
57. Winzeler-Mercay U, Mudie H. The nature of the effects of stroke on trunk flexor and extensor muscles during work and rest. Disabil Rehabil. 2002;24(17):875-886.
58. Woodhull-McNeal AP. Activity in torso muscles during relaxed standing. Eur J Appl Physiol. 1986;55(4):418-424.