Chapter 88 The Newborn Infant (See Also Chapter 7)
The neonatal period is a highly vulnerable time for an infant, who is completing many of the physiologic adjustments required for extrauterine existence. The high neonatal morbidity and mortality rates attest to the fragility of life during this period; of all deaths occurring in the 1st yr of life in the USA, two thirds are in the neonatal period. The annual rate of deaths during the 1st yr is unequaled by the rate in any other period of life until the 7th decade.
An infant’s transition from intrauterine to extrauterine life requires many biochemical and physiologic changes. Many of a newborn infant’s special problems are related to poor adaptation because of asphyxia, premature birth, life-threatening congenital anomalies, or the adverse effects of delivery.
88.1 History in Neonatal Pediatrics
The perinatal history should include the following information:
88.2 Physical Examination of the Newborn Infant
Many physical and behavioral characteristics of a normal newborn infant are described in Chapters 7 and 584.
The initial examination of a newborn infant should be performed as soon as possible after delivery. Temperature, pulse, respiratory rate, color, type of respiration, tone, activity, and level of consciousness of infants should be monitored frequently until stabilization. For high-risk deliveries, this examination should take place in the delivery room and should focus on congenital anomalies, maturation and growth, and pathophysiologic problems that may interfere with normal cardiopulmonary and metabolic adaptation to extrauterine life. Congenital anomalies of varying degrees of severity may be present in 3-5% of infants. After a stable delivery room course, a 2nd and more detailed examination should be performed within 24 hr of birth. If an infant remains in the hospital longer than 48 hr, a discharge examination should be performed within 24 hr of discharge. For a healthy infant, the mother should be present during this examination; even minor, seemingly insignificant anatomic variations may worry a family and should be explained. The explanation must be careful and skillful so that otherwise unworried families are not unduly alarmed. Infants should not be discharged from the hospital without a final examination because certain abnormalities, particularly heart murmurs, often appear or disappear in the immediate neonatal period; in addition, evidence of disease that has just been acquired may be noted. The pulse (normal, 120-160 beats/min), respiratory rate (normal, 30-60 breaths/min), temperature, weight, length, head circumference, and dimensions of any visible or palpable structural abnormality should be assessed. Blood pressure is determined if a neonate appears ill or has a heart murmur. Pulse oximetry is performed by some clinicians to screen for serious ductus arteriosus–dependent congenital heart disease.
Examining a newborn requires patience, gentleness, and procedural flexibility. Thus, if the infant is quiet and relaxed at the beginning of the examination, palpation of the abdomen or auscultation of the heart should be performed 1st, before other, more disturbing manipulations are attempted.
General Appearance
Physical activity may be absent during normal sleep, or it may be decreased by the effects of illness or drugs; an infant may be either lying with the extremities motionless, to conserve energy for the effort of difficult breathing, or vigorously crying, with accompanying activity of the arms and legs. Both active and passive muscle tone and any unusual posture should be noted. Coarse, tremulous movements with ankle or jaw myoclonus are more common and less significant in newborn infants than at any other age. Such movements tend to occur when an infant is active, whereas convulsive twitching usually occurs in a quiet state. Edema may produce a superficial appearance of good nutrition. Pitting after applied pressure may or may not be noted, but the skin of the fingers and toes lacks the normal fine wrinkles when filled with fluid. Edema of the eyelids commonly results from irritation caused by the administration of silver nitrate. Generalized edema may occur with prematurity, hypoproteinemia secondary to severe erythroblastosis fetalis, nonimmune hydrops, congenital nephrosis, Hurler syndrome, and from unknown causes. Localized edema suggests a congenital malformation of the lymphatic system; when confined to one or more extremities of a female infant, it may be the initial sign of Turner syndrome (Chapters 76 and 580).
Skin
Vasomotor instability and peripheral circulatory sluggishness are revealed by deep redness or purple lividity in a crying infant, whose color may darken profoundly with closure of the glottis preceding a vigorous cry, and by harmless cyanosis (acrocyanosis) of the hands and feet, especially when they are cool. Mottling, another example of general circulatory instability, may be associated with serious illness or related to a transient fluctuation in skin temperature. An extraordinary division of the body from the forehead to the pubis into red and pale halves is known as harlequin color change, a transient and harmless condition. Significant cyanosis may be masked by the pallor of circulatory failure or anemia; alternatively, the relatively high hemoglobin content of the 1st few days and the thin skin may combine to produce an appearance of cyanosis at a higher PaO2 than in older children. Localized cyanosis is differentiated from ecchymosis by the momentary blanching pallor (with cyanosis) that occurs after pressure. The same maneuver also helps in demonstrating icterus. Pallor may be due to anemia, asphyxia, shock, or edema. Early recognition of anemia may lead to a diagnosis of erythroblastosis fetalis, subcapsular hematoma of the liver or spleen, subdural hemorrhage, or fetal-maternal or twin-twin transfusion. Without being anemic, postmature infants tend to have paler and thicker skin than term or premature infants. The ruddy appearance of plethora is seen with polycythemia.
The vernix and common transitory macular capillary hemangiomas of the eyelids and neck are described in Chapter 639. Cavernous hemangiomas are deeper, blue masses that, if large, may trap platelets and produce disseminated intravascular coagulation or interfere with local organ function. Scattered petechiae may be seen on the presenting part (usually the scalp or face) after a difficult delivery. Slate-blue, well-demarcated areas of pigmentation are seen over the buttocks, back, and sometimes other parts of the body in more than 50% of black, Native American, and Asian infants and occasionally in white ones. These benign patches have no known anthropologic significance despite their name, Mongolian spots; they tend to disappear within the 1st year. The vernix, skin, and especially the cord may be stained brownish yellow if the amniotic fluid has been colored by the passage of meconium during or before birth.
The skin of premature infants is thin and delicate and tends to be deep red; in extremely premature infants, the skin appears almost gelatinous and translucent. Fine, soft, immature hair, lanugo, frequently covers the scalp and brow and may also cover the face of premature infants. Lanugo has usually been lost or replaced by vellus hair in term infants. Tufts of hair over the lumbosacral spine suggest an underlying abnormality such as occult spina bifida, a sinus tract, or a tumor. The nails are rudimentary in very premature infants, but they may protrude beyond the fingertips in infants born past term. Post-term infants may have a peeling, parchment-like skin (Fig. 88-1), a severe degree of which suggests ichthyosis congenita (Chapter 650).

Figure 88-1 Infant with intrauterine growth retardation as a result of placental insufficiency. Note the long, thin appearance with peeling, parchment-like dry skin, alert expression, meconium staining of the skin, and long nails.
(From Clifford S: Advances in pediatrics, vol 9, Chicago, 1962, Year Book.)
In many neonates, small, white papules on an erythematous base develop 1-3 days after birth. This benign rash, erythema toxicum, persists for as long as 1 wk, contains eosinophils, and is usually distributed on the face, trunk, and extremities (Chapter 639). Pustular melanosis, a benign lesion seen predominantly in black neonates, contains neutrophils and is present at birth as a vesiculopustular eruption around the chin, neck, back, extremities, and palms or soles; it lasts 2-3 days. Both lesions need to be distinguished from more dangerous vesicular eruptions such as herpes simplex (Chapter 244) and staphylococcal disease of the skin (Chapter 174.1).
Amniotic bands may disrupt the skin, extremities (amputation, ring constriction, syndactyly), face (clefts), or trunk (abdominal or thoracic wall defects). Their cause is uncertain but may be related to amniotic membrane rupture or vascular compromise with fibrous band formation. Excessive skin fragility and extensibility with joint hypermobility suggest Ehlers-Danlos syndrome, Marfan syndrome, congenital contractural arachnodactyly, and other disorders of collagen synthesis.
Skull
The head circumference of all infants should be charted. The skull may be molded, particularly if the infant is the first-born and if the head has been engaged in the pelvic canal for a considerable time. The parietal bones tend to override the occipital and frontal bones. The head of an infant born by cesarean section or from a breech presentation is characterized by its roundness. The suture lines and the size and fullness of the anterior and posterior fontanels should be determined digitally by palpation. Premature fusion of sutures (cranial synostosis) is identified as a hard nonmovable ridge over the suture and an abnormally shaped skull. Great variation in the size of the fontanels exists at birth; if small, the anterior fontanel usually tends to enlarge during the 1st few months of life. The persistence of excessively large anterior (normal, 20 ± 10 mm) and posterior fontanels has been associated with several disorders (Table 88-1). Persistently small fontanels suggest microcephaly, craniosynostosis, congenital hyperthyroidism, or wormian bones; presence of a 3rd fontanel suggests trisomy 21 but is seen in preterm infants. Soft areas (craniotabes) are occasionally found in the parietal bones at the vertex near the sagittal suture; they are more common in premature infants and in infants who have been exposed to uterine compression. Though such soft areas are usually insignificant, their possible pathologic cause should be investigated if they persist. Soft areas in the occipital region suggest the irregular calcification and wormian bone formation associated with osteogenesis imperfecta, cleidocranial dysostosis, lacunar skull, cretinism, and, occasionally, Down syndrome. Transillumination of an abnormal skull in a dark room followed by ultrasound or computed tomography will rule out hydranencephaly and hydrocephaly (Chapter 585). An excessively large head (megalencephaly) suggests hydrocephaly, storage disease, achondroplasia, cerebral gigantism, neurocutaneous syndromes, or inborn errors of metabolism, or may be familial. The skull of a premature infant may suggest hydrocephaly because of the relatively larger brain growth in comparison with growth of other organs. Depression of the skull (indentation, fracture, pingpong ball deformity) is usually of prenatal onset and due to prolonged focal pressure by the bony pelvis. Atrophic or alopecic scalp areas may represent aplasia cutis congenita, which may be sporadic or autosomal dominant or associated with trisomy 13, chromosome 4 deletion, or Johanson-Blizzard syndrome. Deformational plagiocephaly may be due to in utero positioning forces on the skull and manifests as an asymmetric skull and face with ear malalignment. It is associated with torticollis and vertex positioning. Any significant and persistent abnormality in shape or size of the skull should be evaluated by cranial CT.
Face
The general appearance of the face should be noted with regard to dysmorphic features, such as epicanthal folds, widely or narrowly spaced eyes, microphthalmos, asymmetry, long philtrum, and low-set ears, which are often associated with congenital syndromes. The face may be asymmetric as a result of a 7th nerve palsy, hypoplasia of the depressor muscle at the angle of the mouth, or an abnormal fetal posture (Chapter 102); when the jaw has been held against a shoulder or an extremity during the intrauterine period, the mandible may deviate strikingly from the midline. Symmetric facial palsy suggests absence or hypoplasia of the 7th nerve nucleus (Möbius syndrome).
Eyes
The eyes often open spontaneously if the infant is held up and tipped gently forward and backward. This maneuver, a result of labyrinthine and neck reflexes, is more successful for inspecting the eyes than is forcing the lids apart. Conjunctival and retinal hemorrhages are usually benign. Retinal hemorrhages are more common with vacuum-assisted deliveries (75%) than after cesarean section (7%). They resolve in most infants by 2 wk of age (85%) and in all infants by 4 wk. Pupillary reflexes are present after 28-30 wk of gestation. The iris should be inspected for colobomas and heterochromia. A cornea >1cm in diameter in a term infant (with photophobia and tearing) suggests congenital glaucoma and requires prompt ophthalmologic consultation. The presence of bilateral red reflexes suggests the absence of cataracts and intraocular pathology (Chapters 611, 619-625). Leukokoria (white pupillary reflex) suggests cataracts, tumor, chorioretinitis, retinopathy of prematurity, or a persistent hyperplastic primary vitreous and warrants an immediate ophthalmologic consultation.
Ears
Deformities of the pinnae are occasionally seen. Unilateral or bilateral preauricular skin tags occur frequently; if pedunculated, they can be tightly ligated at the base, resulting in dry gangrene and sloughing. The tympanic membrane, easily seen otoscopically through the short, straight external auditory canal, normally appears dull gray.
Nose
The nose may be slightly obstructed by mucus accumulated in the narrow nostrils. The nares should be symmetric and patent. Dislocation of the nasal cartilage from the vomerian groove results in asymmetric nares. Anatomic obstruction of the nasal passages secondary to unilateral or bilateral choanal atresia results in respiratory distress.
Mouth
A normal mouth may rarely have precocious dentition, with natal (present at birth) or neonatal (eruption after birth) teeth in the lower incisor position or aberrantly placed; these teeth are shed before the deciduous ones erupt (Chapter 299). Alternatively, such teeth occur in Ellis-van Creveld, Hallermann-Streiff, and other syndromes. Extraction is not usually indicated. Premature eruption of deciduous teeth is even more unusual. The soft and hard palate should be inspected and palpated for a complete or submucosal cleft, and the contour noted if the arch is excessively high or the uvula is bifid. On the hard palate on either side of the raphe, there may be temporary accumulations of epithelial cells called Epstein pearls. Retention cysts of similar appearance may also be seen on the gums. Both disappear spontaneously, usually within a few weeks of birth. Clusters of small white or yellow follicles or ulcers on erythematous bases may be found on the anterior tonsillar pillars, most frequently on the 2nd or 3rd day of life. Of unknown cause, they clear without treatment in 2-4 days.
Neonates do not have active salivation. The tongue appears relatively large; the frenulum may be short, but its shortness (tongue-tied or ankyloglossia) is rarely a reason for cutting it. If there are problems with feedings (breast or bottle) and the frenulum is short, frenulotomy may be indicated. The sublingual mucous membrane occasionally forms a prominent fold. The cheeks have fullness on both the buccal and the external aspects as a result of the accumulation of fat making up the sucking pads. These pads, as well as the labial tubercle on the upper lip (sucking callus), disappear when suckling ceases. A marble-sized buccal mass is usually due to benign idiopathic fat necrosis.
The throat of a newborn infant is hard to see because of the low arch of the palate; it should be clearly viewed because posterior palatal or uvular clefts are easy to miss. The tonsils are small.
Neck
The neck appears relatively short. Abnormalities are not common but include goiter, cystic hygroma, branchial cleft rests, teratoma, hemangioma, and lesions of the sternocleidomastoid muscle that are presumably traumatic or due to a fixed positioning in utero that produces either a hematoma or fibrosis, respectively. Congenital torticollis causes the head to turn toward and the face to turn away from the affected side. Plagiocephaly, facial asymmetry, and hemihypoplasia may develop if it is untreated (Chapter 672.1). Redundant skin or webbing in a female infant suggests intrauterine lymphedema and Turner syndrome (Chapters 76 and 580). Both clavicles should be palpated for fractures.
Chest
Breast hypertrophy is common, and milk may be present (but should not be expressed). Asymmetry, erythema, induration, and tenderness suggest mastitis or a breast abscess. Supernumerary nipples, inverted nipples, or widely spaced nipples with a shield-shaped chest may be seen; the last finding suggests Turner syndrome.
Lungs
Much can be learned by observing breathing. Variations in rate and rhythm are characteristic and fluctuate according to the infant’s physical activity, the state of wakefulness, or the presence of crying. Because fluctuations are rapid, the respiratory rate should be counted for a full minute with the infant in the resting state, preferably asleep. Under these circumstances, the usual rate for normal term infants is 30-60 breaths/min; in premature infants the rate is higher and fluctuates more widely. A rate consistently over 60 breaths/min during periods of regular breathing usually indicates pulmonary, cardiac, or metabolic disease (acidosis). Premature infants may breathe with a Cheyne-Stokes rhythm, known as periodic respiration, or with complete irregularity. Irregular gasping, sometimes accompanied by spasmodic movements of the mouth and chin, strongly indicates serious impairment of the respiratory centers.
The breathing of newborn infants at rest is almost entirely diaphragmatic, so during inspiration, the soft front of the thorax is usually drawn inward while the abdomen protrudes. If the baby is quiet, relaxed, and of good color, this “paradoxic movement” does not necessarily signify insufficient ventilation. On the other hand, labored respiration with retractions is important evidence of respiratory distress syndrome, pneumonia, anomalies, or mechanical disturbance of the lungs. A weak persistent or intermittent groaning, whining cry, or grunting during expiration signifies potentially serious cardiopulmonary disease or sepsis and warrants immediate attention. When benign, the grunting resolves between 30 and 60 min after birth. Flaring of the alae nasi and retraction of the intercostal muscles and sternum are common signs of pulmonary pathology.
Normally, the breath sounds are bronchovesicular. Suspicion of pulmonary pathology because of diminished breath sounds, rales, retractions, or cyanosis should always be verified with a chest radiograph.
Heart
Normal variation in the size and shape of the chest makes it difficult to estimate the size of the heart. The location of the heart should be determined to detect dextrocardia. Transitory murmurs usually represent a closing ductus arteriosus. Although congenital heart disease may not initially produce a murmur, a substantial portion of infants in whom persistent murmurs are detected during routine neonatal examination have underlying malformation. Evaluation of the heart by echocardiography is essential when the possibility of a significant lesion exists. Oxygen saturation measurements can be used to screen for serious congenital heart disease. Oxygen saturation value < 96% 24 hours after birth has been used as a cutoff for suspicion of serious congenital heart disease.
The pulse may vary normally from 90 beats/min in relaxed sleep to 174 beats/min during activity. The still higher rate of supraventricular tachycardia (>220 beats/min) may be determined better with a cardiac monitor or electrocardiogram than by ear. Premature infants, whose resting heart rate is usually 140-150 beats/min, may have a sudden onset of sinus bradycardia. On both admission to and discharge from the nursery, the infant’s pulses should be palpated in the upper and lower extremities to detect coarctation of the aorta.
Blood pressure measurements may be a valuable diagnostic aid in ill infants (Chapter 419). The oscillometric method is the easiest and most accurate noninvasive method available. Continuous or intermittent direct measurement of blood pressure with an umbilical artery catheter may be indicated in special circumstances for infants who are under close observation in an intensive care unit (Fig. 88-2).
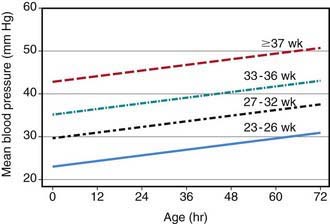
Figure 88-2 Nomogram for mean blood pressure (BP) in neonates with gestational ages of 23-43 wk derived from continuous arterial BP measurements obtained from 103 infants admitted to the neonatal intensive care unit. The graph shows the predicted mean BP of neonates of different gestational ages during the 1st 72 hours of life. Each line represents the lower limit of the 80% confidence interval (two-tail) of the mean BP for each gestational age group; 90% of infants for each gestational age group will be expected to have a mean BP value equal to or above the value indicated by the corresponding line, the lower limit of the confidence interval.
(From Nuntnarumit P, Yang W, Bada-Ellzey SB: Blood pressure measurements in the newborn, Clin Perinatol 26:976–996, 1999.)
Abdomen
The liver is usually palpable, sometimes as much as 2 cm below the rib margin. Less commonly, the tip of the spleen may be felt. The approximate size and location of each kidney can usually be determined on deep palpation. At no other period of life does the amount of air in the gastrointestinal tract vary so much, nor is it usually so great under normal circumstances. Gas should normally be present in the rectum on roentgenogram by 24 hr of age. The abdominal wall is normally weak (especially in premature infants), and diastasis recti and umbilical hernias are common, particularly among black infants.
Unusual masses should be investigated immediately with ultrasonography. Renal pathology is the cause of most neonatal abdominal masses. Cystic abdominal masses include hydronephrosis, multicystic-dysplastic kidneys, adrenal hemorrhage, hydrometrocolpos, intestinal duplication, and choledochal, ovarian, omental, or pancreatic cysts. Solid masses include neuroblastoma, congenital mesoblastic nephroma, hepatoblastoma, and teratoma. A solid flank mass may be caused by renal vein thrombosis, which becomes clinically apparent with hematuria, hypertension, and thrombocytopenia. Renal vein thrombosis in infants is associated with polycythemia, dehydration, maternal diabetes, asphyxia, sepsis, nephrosis, and hypercoagulable states such as antithrombin III and protein C deficiency.
Abdominal distention at birth or shortly afterward suggests either obstruction or perforation of the gastrointestinal tract, often as a result of meconium ileus; later distention suggests lower bowel obstruction, sepsis, or peritonitis. A scaphoid abdomen in a newborn suggests diaphragmatic hernia. Abdominal wall defects produce an omphalocele (Chapter 99) when they occur through the umbilicus and gastroschisis when they occur lateral to the midline. Omphaloceles are associated with other anomalies and syndromes such as Beckwith-Wiedemann, conjoined twins, trisomy 18, meningomyelocele, and imperforate anus. Omphalitis is an acute local inflammation of the periumbilical tissue that may extend to the abdominal wall, the peritoneum, the umbilical vein or portal vessels, or the liver and may result in later portal hypertension. The umbilical cord should have two arteries and one vein. A single umbilical artery increases the risk for an occult renal anomaly.
Genitals
The genitals and mammary glands normally respond to transplacentally acquired maternal hormones to produce enlargement and secretion of the breasts in both sexes and prominence of the genitals in females, often with considerable nonpurulent discharge. These transitory manifestations require no intervention.
An imperforate hymen may result in hydrometrocolpos and a lower abdominal mass. A normal scrotum at term is relatively large; its size may be increased by the trauma of breech delivery or by a transitory hydrocele, which is distinguished from a hernia by palpation and transillumination. The testes should be in the scrotum or should be palpable in the canals in term infants. Black male infants usually have dark pigmentation of the scrotum before the rest of the skin assumes its permanent color.
The prepuce of a newborn infant is normally tight and adherent. Severe hypospadias or epispadias should always lead one to suspect either that abnormal sex chromosomes are present (Chapter 76) or that the infant is actually a masculinized female with an enlarged clitoris, because this finding may be the 1st evidence of adrenogenital syndrome (Chapter 570). Erection of the penis is common and has no significance. Urine is usually passed during or immediately after birth; a period without voiding may normally follow. Most neonates void by 12 hr, and about 95% of preterm and term infants void within 24 hr.
Anus
Some passage of meconium usually occurs within the 1st 12 hr after birth; 99% of term infants and 95% of premature infants pass meconium within 48 hr of birth. Imperforate anus is not always visible and may require evidence obtained by gentle insertion of the examiner’s little finger or a rectal tube. Radiographic study is required. Passage of meconium does not rule out an imperforate anus if a rectal-vaginal fistula is present. The dimple or irregularity in skinfold often normally present in the sacrococcygeal midline may be mistaken for an actual or potential neurocutaneous sinus.
Extremities
During examination of the extremities, the effects of fetal posture (Chapter 664) should be noted so that their cause and usual transitory nature can be explained to the mother. Such explanations are particularly important after breech presentations. A fracture or nerve injury associated with delivery can be detected more commonly by observation of the extremities in spontaneous or stimulated activity than by any other means. The hands and feet should be examined for polydactyly, syndactyly, and abnormal dermatoglyphic patterns such as a simian crease.
The hips of all infants should be examined with specific maneuvers to rule out congenital dislocation (Chapter 670.1).
Neurologic Examination (Chapters 7 and 584)
In utero neuromuscular diseases associated with limited fetal motion produce a constellation of signs and symptoms that are independent of the specific disease. Severe positional deformation and contractures produce arthrogryposis. Other manifestations of fetal neuromuscular disease include breech presentation, polyhydramnios, failure to breathe at birth, pulmonary hypoplasia, dislocated hips, undescended testes, thin ribs, and clubfoot. Many congenital disorders manifest as hypotonia, hypertonia, or seizures.
Deshpande SA, Jog S, Watson H, et al. Do babies with isolated single umbilical artery need routine postnatal renal ultrasonography? Arch Dis Child Fetal Neonatal Ed. 2009;94:F265-F267.
Meberg A, Brugmann-Pieper S, Due RJr, et al. First day of life pulse oximetry screening to detect congenital heart defects. J Pediatr. 2008;152:761-766.
Mullany LC, Katz J, Khatry SK, et al. Incidence and seasonablity of hypothermia among newborns in Southern Nepal. Arch Pediatr Adolesc Med. 2010;164:71-77.
Nuntnarumit P, Yang W, Bada-Ellzey SB. Blood pressure measurements in the newborn. Clin Perinatol. 1999;26:981-996.
88.3 Routine Delivery Room and Initial Care
Low-risk infants may initially be placed head downward after delivery to allow gravity to clear the mouth, pharynx, and nose of fluid, mucus, blood, and amniotic debris; wiping of the mouth with a cloth or gentle suction with a bulb syringe or soft catheter may also be helpful if there is an excessive amount of fluid in the mouth or nares. Most healthy infants who appear to be in satisfactory condition should be given directly to their mothers for immediate bonding and nursing. If respiratory distress is a concern, infants should be placed under warmers for observation.
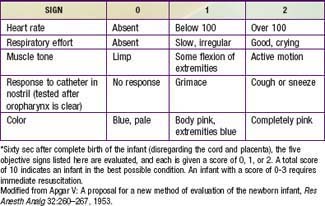
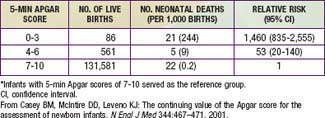
The Apgar score is a practical method of systematically assessing newborn infants immediately after birth (Table 88-2). A low score may be due to fetal distress but may also be due to a number of factors, including prematurity and drugs given to the mother during labor (Table 88-3). The Apgar score was not designed to predict neurologic outcome. Indeed, the score is normal in most patients in whom cerebral palsy subsequently develops, and the incidence of cerebral palsy is low in infants with Apgar scores of 0-3 at 5 min (but higher than in infants with Apgar scores of 7-10). Low Apgar scores and umbilical artery blood pH predict neonatal death. An Apgar score of 0-3 at 5 min is uncommon but is a better predictor of neonatal death (in both term and preterm infants) than an umbilical artery pH ≤ 7.0; the presence of both variables increases the relative risk of neonatal mortality in term and preterm infants (Table 88-4). Infants who fail to initiate respiration should receive prompt resuscitation and close observation (Chapter 94).
Table 88-3 FACTORS AFFECTING THE APGAR SCORE*
FALSE-POSITIVE (NO FETAL ACIDOSIS OR HYPOXIA; LOW APGAR SCORE)
FALSE-NEGATIVE (ACIDOSIS; NORMAL APGAR SCORE)
* Regardless of the etiology, a low Apgar score because of fetal asphyxia, immaturity, central nervous system depression, or airway obstruction identifies an infant needing immediate resuscitation.
Table 88-4 INCIDENCE OF NEONATAL DEATH IN 132,228 SINGLETON INFANTS BORN AT TERM (37TH WEEK OF GESTATION OR LATER) IN RELATION TO APGAR SCORES AT 5 MINUTES OF AGE*
Maintenance of Body Heat
Newborn infants are at risk for heat loss and hypothermia for several reasons. Relative to body weight, the body surface area of a newborn infant is approximately three times that of an adult. Generation of body heat depends in large part on body weight, but heat loss depends on surface area. In low birthweight and preterm infants, the insulating layer of subcutaneous fat is thin. The estimated rate of heat loss in a newborn is approximately four times that of an adult. Under the usual delivery room conditions (20-25°C), an infant’s skin temperature falls approximately 0.3°C/min and deep body temperature decreases approximately 0.1°C/min during the period immediately after delivery; these rates generally result in a cumulative loss of 2-3°C in deep body temperature (corresponding to a heat loss of approximately 200 kcal/kg). The heat loss occurs by four mechanisms: (1) convection of heat energy to the cooler surrounding air, (2) conduction of heat to the colder materials touching the infant, (3) heat radiation from the infant to other nearby cooler objects, and (4) evaporation from skin and lungs.
Metabolic acidosis, hypoxemia, hypoglycemia, and increased renal excretion of water and solutes may develop in term infants exposed to cold after birth because of their effort to compensate for heat loss. Heat production is augmented by increasing the metabolic rate and oxygen consumption in part by releasing norepinephrine, which results in nonshivering thermo-genesis through oxidation of fat, particularly brown fat. In addition, muscular activity may increase. Hypoglycemic or hypoxic infants cannot increase their oxygen consumption when exposed to a cold environment, and their central temperature decreases. After labor and vaginal delivery, many newborn infants have mild to moderate metabolic acidosis, for which they may compensate by hyperventilating, a response that is more difficult for infants with central nervous system depression (asphyxia, drugs) and infants exposed to cold stress in the delivery room. Therefore, to reduce heat loss, it is desirable to ensure that infants are dried and either wrapped in blankets or placed under radiant warmers. Skin-to-skin contact with the mother is the optimal method of maintaining temperature in the stable newborn. Because carrying out resuscitative measures on a covered infant or one enclosed in an incubator is difficult, a radiant heat source should be used to warm the baby during resuscitation.
Antiseptic Skin and Cord Care
Careful removal of blood from the skin shortly after birth may reduce the risk of infection with blood-borne agents. Once a healthy infant’s temperature has stabilized, the entire skin and cord should be cleansed with warm water or a mild nonmedicated soap solution and rinsed with water to reduce the incidence of skin and periumbilical colonization with pathogenic bacteria and subsequent infectious complications. To avoid heat loss, the infant is then dried and wrapped in clean blankets. To reduce colonization with Staphylococcus aureus and other pathogenic bacteria, the umbilical cord may be treated daily with a bactericidal or antimicrobial agents such as triple dye or bacitracin. One application of triple dye followed by twice-daily alcohol swabbing (until the cord falls off) reduces colonization, exudates, and foul odor of the umbilicus in comparison with dry care (soap and water when soiled). Alternatively, chlorhexidine washing or, on rare occasion during S. aureus epidemics, a single hexachlorophene bath may be used. Topical ointments should not be applied to preterm infants in neonatal intensive care units because this treatment increases the risk of bacterial sepsis. Routine or repeated total body exposure to hexachlorophene may be neurotoxic, particularly in low-birthweight infants, and is thus contraindicated. Nursery personnel should use chlorhexidine or iodophor-containing antiseptic soaps for routine handwashing before caring for each infant. Rigid enforcement of hand-to-elbow washing for 2 min in the initial wash and 15-30 sec in the 2nd wash is essential for staff and visitors entering the nursery. Equally thorough washes between handling infants are also required.
Other Measures
The eyes of all infants, including those born by cesarean section, must be protected against gonococcal ophthalmia neonatorum by instillation of 1% silver nitrate drops or erythromycin (0.5%) or tetracycline (1.0%) sterile ophthalmic ointments. This procedure may be delayed during the initial short-alert period after birth to promote bonding, but once applied, drops should not be rinsed out (Chapters 185 and 218.3).
Although hemorrhage in newborn infants can be due to factors other than vitamin K deficiency, an intramuscular injection of 1 mg of water-soluble vitamin K1 (phytonadione) is recommended for all infants immediately after birth to prevent hemorrhagic disease of the newborn (Chapter 97.4). Oral vitamin K may also be useful but is not as effective as the parenteral dosage. Administration of vitamin K to the mother during labor is not recommended because of unpredictable placental transfer.
Hepatitis B immunization before discharge from the nursery is recommended for newborns with weight >2 kg irrespective of maternal hepatitis status.
Neonatal screening is available for various genetic, metabolic, hematologic, and endocrine disorders. All states in the USA have neonatal screening programs, although the specific tests required vary (Chapter 78). The expanded newborn screening, which consists of a panel of approximately 29 disorders, is estimated to increase by 32% the number of affected children identified. The most commonly identified disorders (and their rates) include hypothyroidism (52/100,000 births), cystic fibrosis (30/100,000), hemoglobinopathies (26/100,000), medium-chain acyl–coenzyme A dehydrogenase deficiency (6/100,000), galactosemia (5/100,000), and phenylketonuria (5/100,000), and adrenal hyperplasia (5/100,000). To be effective in the timely identification and prompt management of treatable diseases, screening programs must include not only high-quality laboratory tests but also follow-up of infants with abnormal test results; education, counseling, and psychologic support for families; and prompt referral of the identified neonate for accurate diagnosis and therapy.
Hearing impairment, a serious morbidity that affects speech and language development, may be severe in 2/1,000 births and overall affects 5/1,000 births. Universal screening of infants is recommended to ensure early detection of hearing loss and appropriate, timely intervention.
Routine measurement of the hematocrit or blood glucose value is not necessary in the absence of risk factors. Screening for hyperbilirubinemia should include risk assessment in all infants with measurement of serum or transcutaneous bilirubin levels as indicated.
American Academy of Pediatrics Committee on Fetus and Newborn. The Apgar score. Pediatrics. 2006;117:1444-1447.
Casey BM, McIntire DD, Leveno KJ. The continuing value of the Apgar score for the assessment of newborn infants. N Engl J Med. 2001;344:467-471.
Lie KK, Grøholt EK, Eskild A. Association of cerebral palsy with Apgar score in low and normal birthweight infants: population based cohort study. BMJ. 2010;341:817.
Paneth N. Apgar score and risk of cerebral palsy. BMJ. 2010;341:788-789.
88.4 Nursery Care
Non–high-risk, healthy infants may be taken to the “regular” (normal) newborn nursery or may be placed in the mother’s room if the hospital has rooming-in facilities.
The bassinet, preferably of clear plastic to allow for easy visibility and care, should be cleaned frequently. All professional care should be given to the infant in the bassinet, including the physical examination, clothing changes, temperature taking, skin cleansing, and other procedures that, if performed elsewhere, would establish a common contact point and possibly provide a channel for cross infection. The clothing and bedding should be minimal, only enough needed for an infant’s comfort; the nursery temperature should be kept at approximately 22-26°C (72-78°F). The infant’s temperature should be taken by axillary measurement. Although the interval between temperature measurements depends on many circumstances, it need not be shorter than 4 hr during the 1st 2-3 days and 8 hr thereafter. Axillary temperatures of 36.4-37.0°C (97.0-98.5°F) are within normal limits. Weighing at birth and daily thereafter is sufficient. Healthy infants should be placed supine to reduce the risk of sudden infant death syndrome.
Vernix is spontaneously shed within 2-3 days, much of it adhering to the clothing, which should be completely changed daily. The diaper should be checked before and after feeding and when the baby cries; it should be changed when wet or soiled. The perineal area can be cleaned with baby wipes or with mild soap and warm water. Meconium or feces should be cleansed from the buttocks with sterile cotton moistened with sterile water. The foreskin of a male infant should not be retracted. Circumcision is an elective procedure. Circumcision may decrease phimosis, urinary tract infections in infancy, penile cancer, and acquisition of some sexually transmitted infections, including HIV. Parents should make a determination in the interest of the baby until firm recommendations are provided.
Early discharge (<48 hr) or very early discharge (<24 hr) of a neonate may increase the risk of rehospitalization for hyperbilirubinemia, sepsis, failure to thrive, dehydration, and missed congenital anomalies. Early discharge requires careful ambulatory follow-up at home (by a visiting nurse) or in the office within 48 hr. Additional criteria for the early discharge of term neonates have been developed by the American Academy of Pediatrics and American College of Obstetrics and Gynecology (Table 88-5).
Table 88-5 RECOMMENDATIONS FOR EARLY DISCHARGE FROM THE NORMAL NEWBORN NURSERY*
* It is not likely that all these criteria will be met before 48 hr of age.
Adapted from American Academy of Pediatrics, American College of Obstetricians and Gynecologists: Guidelines for perinatal care, ed 5, Elk Grove Village, IL, 2002, American Academy of Pediatrics.
American Academy of Pediatrics Committee on Fetus and Newborn. Hospital discharge of the high-risk neonate. Pediatrics. 2008;122:1119-1126.
American Academy of. Pediatrics and The American College of Obstetricians and Gynecologists: Care of the neonate. Guidelines for perinatal care, ed 6. American Academy of Pediatrics, Elk Grove Village, IL., 2007.
Centers for Disease Control and Prevention. Impact of expanded newborn screening—United States, 2006. MMWR Morb Mortal Wkly Rep. 2008;57:1012-1015.
Conner JM, Soll RF, Edwards WH: Topical ointment for preventing infection in preterm infants, Cochrane Database Syst Rev (1):CD001150, 2004.
de-Wahl Granelli A, Wennergren M, Sandberg K, et al. Impact of pulse oximetry screening on the detection of duct dependent congenital heart disease: a Swedish prospective screening study in 39,821 newborns. BMJ. 2009;338:145-149.
Friedman MA, Spitzer AR. Discharge criteria for the term newborn. Pediatr Clin North Am. 2004;51:599-618.
Janssen PA, Selwood BL, Dobson SR, et al. To dye or not to dye: a randomized, clinical trial of a triple dye/alcohol regime versus dry cord care. Pediatrics. 2003;111:15-20.
Mally P, Bailey S, Hendricks-Muñoz KD. Clinical issues in the management of late preterm infants. Curr Prob Pediatr Adolesc Health Care. 2010;40(9):217-234.
Puckett RM, Offringa M: Prophylactic vitamin K for vitamin K deficiency bleeding in neonates, Cochrane Database Syst (4):CD002776, 2000.
Wilcken B, Haas M, Joy P, et al. Expanded newborn screening: outcome in screened and unscreened patients at age 6 years. Pediatrics. 2009;124:e241-e248.
88.5 Parent-Infant Bonding (See Also Chapter 7)
Normal infant development depends partly on a series of affectionate responses exchanged between a mother and her newborn infant that binds them psychologically and physiologically. This bonding is facilitated and reinforced by the emotional support of a loving family. The attachment process may be important in enabling some mothers to provide loving care during the neonatal period and subsequently during childhood. The power of this attachment is so great that it enables the mother and the father to make unusual sacrifices necessary for the day-to-day care of the infant, care night after night, giving feedings 24 hours a day, attending to crying, and so on. The sacrifices continue for many years as parents dedicate much of their lives to their children.
Parent-infant bonding is initiated before birth with the planning and confirmation of the pregnancy. Subsequently, there is a growing awareness of the baby as an individual, starting usually with the remarkably powerful event of “quickening” or sensation of fetal movements. After delivery and during the ensuing weeks, sensory (visual, auditory, olfactory) and physical contact between the mother and baby triggers various mutually rewarding and pleasurable interactions, such as the mother touching the infant’s extremities and face with her fingertips and encompassing and gently massaging the infant’s trunk with her hands. Touching an infant’s cheek elicits responsive turning toward the mother’s face or toward the breast with nuzzling and licking of the nipple, a powerful stimulus for prolactin secretion. An infant’s initial quiet alert state provides the opportunity for eye-to-eye contact, which is particularly important in stimulating the loving and possessive feelings of many parents for their babies. An infant’s crying elicits the maternal response of touching the infant and speaking in a soft, soothing, higher-toned voice. Initial contact between the mother and infant should take place in the delivery room, and opportunities for extended intimate contact and breast-feeding should be provided within the 1st hours after birth. Delayed or abnormal maternal-infant bonding, as occurs because of prematurity, infant or maternal illness, birth defects, or family stress, may harm infant development and maternal caretaking ability. Hospital routines should be designed to encourage parent-infant contact. Open nurseries, rooming-in arrangements, care by parents, and family-centered care increase the opportunities for better parent-infant interaction.
Nurseries and Breast-Feeding
See Chapter 42 for full discussions of breast-feeding and formula feeding. Hospital practices that encourage successful breast-feeding include antepartum education and encouragement, immediate postpartum mother-infant contact with suckling, rooming-in arrangements, demand feeding, inclusion of fathers in prenatal breast-feeding education, and support from experienced women. Nursing at first for least 5 min at each breast is reasonable, allows a baby to obtain most of the available breast contents, and provides effective stimulation for increasing the milk supply. Nursing episodes should then be extended according to the comfort and desire of the mother and infant. A confident and relaxed mother, supported by an encouraging home and hospital environment, is likely to nurse well. The Baby-Friendly Hospital Initiative, a global effort (sponsored by the World Health Organization and the United Nations Children’s Fund) to promote breast-feeding, recommends 10 steps to successful breast-feeding (Table 88-6). Some hospital practices contribute to difficulties in breast-feeding by enforcing 4-hr feeding schedules, limiting nursing time, using only one breast at a feeding, washing nipples with substances other than water, delaying the 1st feeding, providing formula supplements, and using heavy intrapartum sedation.
Table 88-6 TEN STEPS TO SUCCESSFUL BREAST-FEEDING
From Protecting, promoting and supporting breastfeeding: the special role of maternity services. A joint WHO/UNICEF statement. Geneva, 1989, World Health Organization.
Drugs and Breast-Feeding
Maternal medications may affect the production and safety of breast milk (Table 88-7). Although most commonly used medications are safe, the safety of any new drug to be used while a woman is breast-feeding must be confirmed before the drug is initiated and/or breast-feeding is continued. Maternal sedatives may result in sedation of the infant. Maternal drugs that are weak acids, composed of large molecules, plasma bound, or poorly absorbed from the maternal or neonatal intestine are less likely to affect a neonate.
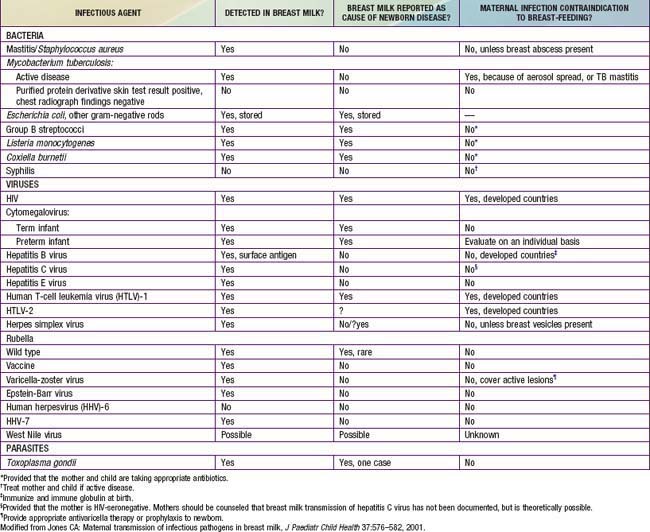
Medical contraindications to breast-feeding in the USA include infection with HIV, human T-cell leukemia virus types 1 and 2, cytomegalovirus (preterm infants), active tuberculosis (until appropriately treated ≥2wk and not considered contagious), and hepatitis B virus (until an infant receives hepatitis B immune globulin and vaccine) (Table 88-8).
American Academy of Pediatrics Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics. 2005;115:496-506.
Briggs GG, Freeman RK, Sumner JY. Drugs in pregnancy and lactation: a reference guide to fetal and neonatal risk. Philadelphia: Lippincott Williams & Wilkins; 2005.
Fortinguerra F, Clavenna A, Bonati M. Psychotropic drug use during breastfeeding: a review of the evidence. Pediatrics. 2009;124:e547-e556.
Hampton T. FDA warns against breast milk drug. JAMA. 2004;292:322.
Kennell JH, Klaus MH. Bonding: recent observations that alter perinatal care. Pediatr Rev. 1998;19:4-12.
Lawrence RM, Lawrence RA. Breast milk and infection. Clin Perinatol. 2004;31:501-528.
Nicoll A, Williams A. Breast feeding. Arch Dis Child. 2002;87:91-92.
Ostrea EMJr, Mantaring JB, Silvestre MA. Drugs that affect the fetus and newborn infant via the placenta or breast milk. Pediatr Clin North Am. 2004;51:539-579.
Philipp BL, Merewood A. The baby-friendly way: the best breastfeeding start. Pediatr Clin North Am. 2004;51:761-783.