Chapter 18 Environmental medicine
Disease and the environment
The incidence and prevalence of disease and causes of death within a community are a reflection of interrelated factors:
 Nutrition, poverty and affluence
Nutrition, poverty and affluence
 Purity of water sources, sanitation and atmospheric pollution
Purity of water sources, sanitation and atmospheric pollution
 Environmental disasters and accidents
Environmental disasters and accidents
 Background ionizing radiation and man-made radiation exposure, deliberate or accidental
Background ionizing radiation and man-made radiation exposure, deliberate or accidental
 Political forces determining levels of healthcare, preventative strategies and effects of war on civilian populations.
Political forces determining levels of healthcare, preventative strategies and effects of war on civilian populations.
Some of these environmental effects have been clearly documented within the last decade, e.g. the massive civilian mortality and morbidity during the current Afghan and previous Iraq wars, and loss of life and disease prevalence following the 2006 tsunami, the earthquakes in Sechuan (2008) and Haiti (2010) and cyclone Nargris in the Irawaddy delta. Flooding caused by El Niño in East Africa not only resulted in an increase in breeding sites for mosquito vectors but a major outbreak of Rift Valley fever due to the enforced close proximity of cattle with humans.
Smoking (active and passive), obesity and excess alcohol consumption also play a significant role in disease. Worldwide health programmes have been established in most countries to reduce their effects.
Environmental temperature
The effect of environmental temperature (TEnv) is paramount in infective diseases; changes as small as 1°C cause major changes in disease vectors. Climate change is an unquestionable phenomenon. Patterns of infective disease are likely to change radically within the next 20 years. There are suggestions that climate effects are already becoming apparent, e.g.:
 Patterns of malaria in South-east Asia
Patterns of malaria in South-east Asia
 The occurrence of dengue fever in southern Italy
The occurrence of dengue fever in southern Italy
 Outbreaks of cholera, and seasonal variation in diarrhoea and vomiting.
Outbreaks of cholera, and seasonal variation in diarrhoea and vomiting.
Research into the effect of climate change on the changing patterns of infective diseases will point to potential ways in which national and international efforts can be targeted.
Heat
Body core temperature (TCore) is maintained at 37°C by the thermoregulator centre in the hypothalamus.
Heat is produced by cellular metabolism and is dissipated through the skin by both vasodilatation and sweating and in expired air via the alveoli. When the environmental temperature (TEnv) is >32.5°C, profuse sweating occurs. Sweat evaporation is the principal mechanism for controlling TCore following exercise or in response to an increase in TEnv.
Heat acclimatization. Acclimatization to heat takes place over several weeks. The sweat volume increases and the sweat salt content falls. Increased evaporation of sweat reduces TCore.
Heat cramps. Painful muscle cramps, usually in the legs, often occur in fit people when they exercise excessively, especially in hot weather. Cramps are probably due to low extracellular sodium caused by excess intake of water over salt. Cramps can be prevented by increasing dietary salt. They respond to combined salt and water replacement, and in the acute stage to stretching and muscle massage. TCore remains normal.
Heat illness. At any environmental temperature (especially with TEnv of >25°C), and with a high humidity, strenuous exercise in clothing that inhibits sweating such as a wetsuit can cause an elevation in TCore in <15 minutes. Weakness/exhaustion, cramps, dizziness and syncope, with TCore >37°C, define heat illness (heat exhaustion). Elevation of TCore is more critical than water and sodium loss. Heat illness may progress to heat injury, a serious emergency.
Management of heat illness
Reduce (TEnv) if possible. Cool with sponging and fans. Give O2 by mask. Other causes of high TCore, e.g. malaria, should be ruled out if appropriate.
Oral rehydration with both salt and water (25 g of salt per 5 L of water/day) is given in the first instance, with adequate replacement thereafter. In severe heat illness, i.v. fluids are needed; 0.9% saline is given; monitor serum sodium and correct secondary potassium loss.
Heat injury
Heat injury (heat stroke) is an acute life-threatening situation when TCore rises above 41°C. There is headache, nausea, vomiting and weakness, progressing to confusion, coma and death. The skin feels intensely hot to the touch. Sweating is often absent, but not invariably.
Heat injury can develop in unacclimatized people in hot, humid windless conditions, even without exercise. Sweating may be limited by prickly heat (plugging or rupture of the sweat ducts, leading to a pruritic papular erythematous rash). Excessive exercise in inappropriate clothing, e.g. exercising on land in a wetsuit, can lead to heat injury in temperate climates. Diabetes, alcohol and drugs, e.g., antimuscarinics, diuretics and phenothiazines, can contribute. Heat injury can lead to a fall in cardiac output, lactic acidosis and intravascular coagulation.
Management
 Cool: sponging, icepacks, fanning. Give O2 by mask
Cool: sponging, icepacks, fanning. Give O2 by mask
 Manage in intensive care: monitor cardiac output, respiration, biochemistry, clotting and muscle enzymes
Manage in intensive care: monitor cardiac output, respiration, biochemistry, clotting and muscle enzymes
 Give fluids intravenously so the intravascular volume can remain normal.
Give fluids intravenously so the intravascular volume can remain normal.
Prompt treatment is essential and can be curative even with TCore of >41°C. Delay can be fatal. Complications are hypovolaemia, intravascular coagulation, cerebral oedema, rhabdomyolysis, and renal and hepatic failure.
Cold
Hypothermia is defined as a core temperature of <32°C. It is frequently lethal when TCore falls below 30°C. Survival, with full recovery has however been recorded with TCore of <16°C. Cold injury includes:
 Frostbite: the local cold injury that follows freezing of tissue
Frostbite: the local cold injury that follows freezing of tissue
 Non-freezing cold injury: the damage – usually to feet – following prolonged exposure to TEnv between 0 and 5°C, usually in damp conditions.
Non-freezing cold injury: the damage – usually to feet – following prolonged exposure to TEnv between 0 and 5°C, usually in damp conditions.
Hypothermia
Hypothermia occurs in many settings.
At home. Hypothermia can occur when TEnv is below 8°C, when there is poor heating, inadequate clothing and poor nutrition. Depressant drugs, e.g. hypnotics, as well as alcohol, hypothyroidism or intercurrent illness also contribute. Hypothermia is commonly seen in the poor, frail and elderly. The elderly have diminished ability to sense cold and also have little insulating fat. Neonates and infants become hypothermic rapidly because of a relatively large surface area in proportion to subcutaneous fat.
Outdoors on land. Hypothermia is a prominent cause of death in climbers, skiers, polar travellers and in wartime. Wet, cold conditions with wind chill, physical exhaustion, injuries and inadequate clothing are contributory. Babies and children are at risk because they cannot take action to warm them themselves.
Cold water immersion. Dangerous hypothermia can develop following immersion for more than 30 min to 1 hour in water temperatures of 15–20°C. In TWater below 12°C limbs rapidly become numb and weak. Recovery takes place gradually, over several hours following rescue.
Clinical features
Mild hypothermia (TCore <32°C) causes shivering and initially intense discomfort. However, the hypothermic subject, though alert, may not act appropriately to rewarming, e.g. by huddling, wearing extra clothing or exercising. As the TCore falls below 32°C, severe hypothermia causes impaired judgement – including lack of awareness of cold – drowsiness and coma. Death follows, usually from ventricular fibrillation.
Diagnosis
Diagnosis is straightforward, if a low-reading thermometer is available. If not, rapid clinical assessment is reliable. Someone who feels icy to touch – abdomen, groin, axillae – is probably substantially hypothermic. If they are clammy, uncooperative or sleepy, TCore is almost certainly <32°C.
Sequelae
Pulse rate and systemic BP fall. Cardiac output and cerebral blood flow are low in hypothermia and can fall further if the upright position is maintained, the thorax restrained by a harness or by hauling during evacuation. This is why helicopter and lifeboat winch rescues are often carried out with a stretcher, rather than a chest harness.
Respiration becomes shallow and slow. Muscle stiffness develops; tendon reflexes become sluggish, then absent. As coma ensues, pupillary and other brainstem reflexes are lost; pupils are fixed and may be dilated in severe hypothermia. Metabolic changes are variable, with either metabolic acidosis or alkalosis. Arterial PO2 may appear normal, i.e. falsely high.
There is shift of the oxygen dissociation curve to the left because of the reduction in temperature of haemoglobin. Thus, if an arterial blood sample from a hypothermic patient is analysed at 37°C, the PO2 will be falsely high. Within the range 37–33°C this factor is around 7% per °C. Many blood gas machines also calculate the arterial saturation; this too will be falsely high. When a patient is monitored using a pulse oximeter, the level of arterial oxygen saturation (SaO2) will however be correct – but if SaO2 is then converted by calculation to PaO2, a downwards correction must be applied – simply due to hypothermia.
Bradycardia with ‘J’ waves (rounded waves above the isoelectric line at the junction of the QRS complex and ST segment) are pathognomonic of hypothermia. Prolongation of PR and QT intervals and QRS complex also occur. Ventricular dysrhythmias (tachycardia/fibrillation) or asystole are the usual causes of death.
Principles of hypothermia management
 Maintain the patient horizontal, or slightly head down.
Maintain the patient horizontal, or slightly head down.
 Correct metabolic abnormalities.
Correct metabolic abnormalities.
 Anticipate and treat dysrhythmias.
Anticipate and treat dysrhythmias.
 Check for hypothyroidism (see p. 962).
Check for hypothyroidism (see p. 962).
If the patient is awake, with a core temperature of >32°C, place them in a warm room, use a foil wrap and give warm fluids orally. Outdoors, add extra dry clothing, huddle together and use a warmed sleeping bag. Rewarming may take several hours. Avoid alcohol: this adds to confusion, boosts confidence factitiously, causes peripheral vasodilatation and further heat loss, and can precipitate hypoglycaemia.
Severe hypothermia
In severe hypothermia, people look dead. Always exclude hypothermia before diagnosing brainstem death (see p. 897). Warm gradually, aiming at a 1°C/hour increase in TCore. Direct mild surface heat from an electric blanket can be helpful. Treat any underlying condition promptly, e.g. sepsis. Monitor all vital functions. Correct dysrhythmias. Check for sedative drugs.
Give warm i.v. fluids slowly. Correct metabolic abnormalities. Hypothyroidism, if present, should be treated with liothyronine. Various methods of artificial rewarming exist – inhaled warm humidified air, gastric or peritoneal lavage, and haemodialysis. These are rarely used.
Prevention
Hypothermia in the field can often be prevented by forethought and action. For the elderly, improved home heating and insulation, central heating in bedrooms and electric blankets are helpful in cold spells. This can be expensive and unaffordable for some people, so supplemental finance is required.
Cold injury
Frostbite
Ice crystals form within skin and superficial tissues when the temperature of the tissue (TTissue) falls to −3°C: TEnv generally must be below −6°C. Wind chill is frequently a factor. Typically, fingers, toes, nose and ears become frostbitten.
Frostbitten tissue is pale, greyish and initially doughy to touch. Later, tissue freezes hard, looking like meat from a freezer. Frostbite can easily occur when working or exercising in low temperatures and typically develops without the patient’s knowledge. Below TEnv 5°C, hands or feet that have lost their feeling are at risk of cold injury.
Management
Transport the patient – or if this is impossible, make them walk, even on frostbitten feet – to a place of safety before commencing warming. Warm the frozen part by immersion in hand hot water at 39–42°C, if feasible. Assess hypothermia. Continue warming until obvious thawing occurs; this can be painful. Vasodilator drugs have no part in management. Blisters form within several days and, depending on the depth of frostbite, a blackened shell – the carapace – develops as blisters regress or burst. Dry, non-adherent dressings and aseptic precautions are essential, though hard to achieve. Frostbitten tissues are anaesthetic and at risk from further trauma and infection. Recovery takes place over many weeks, and may be incomplete. Surgery may be needed, but should be avoided in the early stages.
Chilblains
These are small, purplish itchy inflammatory lesions, occurring on toes and fingers. They occur in cold, wet conditions. They are more common in women and heal in 7–14 days. Prevention is by keeping warm and wearing gloves and warm footwear.
Non-freezing cold injury (NFCI)
NFCI (trench foot) describes tissue damage following prolonged exposure, usually for several hours or more, at TEnv around or slightly above freezing, but without frostbite. Wet socks and boots are the usual cause. There is severe vasoconstriction, blotchiness of the lower limbs, with pain and oedema on rewarming. Recovery usually follows over several weeks. There may be prolonged late susceptibility to cold. NFCI is a prominent cause of morbidity in troops operating in low temperatures, and a subsequent cause of litigation.
Prevention of frostbite and NFCI is largely by education and common sense: avoid damp feet and wet boots. Always carry spare dry socks, gloves and headgear.
High altitudes
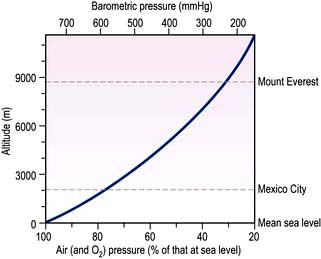
The partial pressure of atmospheric oxygen – and hence alveolar and arterial oxygen – falls in a near-linear relationship as barometric pressure falls with increasing altitude (Fig. 18.1).
Commercial aircraft are pressurized to 2750 m (lowering the oxygen saturation by 3–4%). The incidence of deep venous thrombosis and pulmonary embolism is slightly greater in sedentary passengers on long-haul flights than in a similar population at sea level. Dehydration and alcohol probably contribute. Prophylactic aspirin is not recommended.
On land, below 3000 m there are few clinical effects. The resulting hypoxaemia causes breathlessness only in those with severe cardiorespiratory disease. Above 3000–3500 m hypoxia causes a spectrum of related syndromes that affect high-altitude visitors, principally climbers, trekkers, skiers and troops (Table 18.1), especially when they exercise. These conditions occur largely during acclimatization, a process that takes several weeks and once completed can enable man to live – permanently if necessary – up to about 5600 m. At greater heights, although people can survive for days or weeks, deterioration due to chronic hypoxia is inevitable.
Table 18.1 Conditions caused by sustained hypoxia
| Condition | Incidence (%) | Usual altitude (m) |
|---|---|---|
Acute mountain sickness |
70 |
3500–4000 |
Acute pulmonary oedema |
2 |
4000 |
Acute cerebral oedema |
1 |
4500 |
Retinal haemorrhage |
50 |
5000 |
Deterioration |
100 |
6000 and above |
Chronic mountain sickness |
Rare |
3500–4000 |
The world’s highest railway is to Lhasa, reaching altitudes over 5000 m. Emergency oxygen is provided in the carriages. Roads at similar altitudes in central Asia are used extensively but since road passengers do not exercise, serious altitude-related illnesses are unusual. Climbing the world’s highest summits is just possible without supplementary oxygen, though it is often used on peaks above 7500 m. At the summit of Everest (8848 m) the barometric pressure is 34 kPa (253 mmHg). An acclimatized mountaineer has an alveolar PO2 of 4.0–4.7 kPa (30–35 mmHg) – near man’s absolute physiological limit.
Acute mountain sickness (AMS)
AMS describes malaise, nausea, headache and lassitude and affects the majority of people for a few days, above 3500 metres. Following arrival at this altitude there is usually a latent interval of 6–36 hours before symptoms begin. Treatment is rest, with analgesics if necessary. Recovery is usually spontaneous over several days.
Prophylactic treatment with acetazolamide, a carbonic anhydrase inhibitor and a respiratory stimulant, is of some value in preventing AMS. Acclimatizing, i.e. ascending gradually, provides better and more natural prophylaxis.
In the minority, more serious sequelae – high-altitude pulmonary oedema and high-altitude cerebral oedema develop.
High-altitude pulmonary oedema
Predisposing factors include youth, rapidity of ascent, heavy exertion and severe AMS. Breathlessness, occasionally with frothy blood-stained sputum, indicates established oedema. Unless treated rapidly this leads to cardiorespiratory failure and death. Milder forms are common. Breathlessness at rest should raise the suspicion of pulmonary oedema.
High-altitude cerebral oedema
Cerebral oedema is the result of abrupt increase in cerebral blood flow that occurs even at modest altitudes of 3500–4000 metres. It is unusual below 4500 metres, and occurs typically in the first 2 weeks, during acclimatization. Cerebral oedema can also develop suddenly in well-acclimatized climbers above 7000 metres. Headache is followed by drowsiness, ataxia and papilloedema, with coma and death if brain oedema progresses.
Treatment
Any but the milder forms of AMS require urgent treatment. Oxygen should be given by mask if available, and descent should take place as quickly as possible. Nifedipine reduces pulmonary hypertension and is used in pulmonary oedema. Dexamethasone is effective in reducing brain oedema. Portable pressure bags inflated by a foot pump are widely used; the patient is enclosed in the bag.
Retinal haemorrhages
Small flame haemorrhages within the retinal nerve fibre layer are common above 5000 metres, and usually symptomless. Rarely a haemorrhage will cover the macula, causing painless loss of central vision. Recovery is usual.
Deterioration
Prolonged residence between 6000 and 7000 metres leads to weight loss, anorexia and listlessness after several weeks. Above 7500 metres, the effects of deterioration become apparent over several days, although it is possible to survive for a week or more at altitudes near 8000 metres without supplementary oxygen.
Chronic mountain sickness
Chronic mountain sickness occurs in long-term residents at high altitudes, usually after several decades and is seen in the Andes and in central Asia.
Headache, polycythaemia, lassitude, cyanosis, finger clubbing, congested cheeks and ear lobes, and right ventricular enlargement develop. Chronic mountain sickness is gradually progressive.
Coronary artery disease and hypertension are rare in high-altitude native populations.
FURTHER READING
Clarke C. High altitude and mountaineering expeditions. In: Warrell D, Anderson S (eds). Expedition Medicine, 2nd edn. London: Royal Geographical Society; 2008.
Grocott MP, Martin DS, Levett DZ et al. Arterial blood gases and oxygen content in climbers on Mount Everest. N Engl J Med 2009; 360:140–149.
SIGNIFICANT WEBSITES
Wilderness Medical Society Information, PO Box 2463, Indianapolis, Indiana 462206, USA: http://www.wms.org
UIAA Mountain Medicine Data Centre leaflets, available from British Mountaineering Council, 177–179 Burton Road, Manchester M20 2BB, UK: http://www.thebmc.co.uk
Diving
Free diving by breath-holding is possible to around 5 metres, or with practice to greater depths. Air can be supplied to divers by various methods. With a snorkel, providing air to a depth of c. 0.5 metres, inspiratory effort is the limiting factor. At depths >0.5 metres, i.e. with a longer snorkel tube, forced negative-pressure ventilation can cause pulmonary capillary damage with haemorrhagic alveolar oedema. Scuba divers, i.e. recreational sports divers descending to 30 metres, carry bottled compressed air, or a nitrogen–oxygen mixture. Divers who work at great depths commercially breathe helium–oxygen or nitrogen–oxygen mixtures, delivered by hose from the surface. Ambient pressures at various depths are shown in Table 18.2.
| Water depth (m) | Pressure | |
|---|---|---|
| Atmospheres | mmHg | |
0 |
1 |
760 |
10 |
2 |
1520 |
50 |
6 |
4560 |
90 |
10 |
7600 |
Problems during descent
Middle ear barotrauma (squeeze) is common and caused by inability to equalize pressure in the middle ear – Eustachian tube blockage is the usual cause. Pain and hearing loss occur, sometimes with tympanic membrane rupture and acute vertigo.
Sinus squeeze is intense local pain due to blockage of the nasal and paranasal sinus ostia.
Treatment is by holding the nostrils closed and swallowing, or similar manoeuvres – and decongestants. Diving with a respiratory or sinus infection should be avoided.
Oxygen narcosis
Pure oxygen is not used for diving because of oxygen toxicity. Lung atelectasis, endothelial cell damage and pulmonary oedema occur when alveolar oxygen pressure exceeds 1.5 atmospheres, at depths around 5 metres. At around 10 metres the CNS becomes affected: apprehension, nausea and sweating are followed by muscle twitching and generalized convulsions.
Nitrogen narcosis
When compressed air is breathed below 30 metres, narcotic effects of nitrogen begin to impair brain function. Poor judgement is hazardous; this also occurs with nitrogen–oxygen mixtures in recreational diving. Nitrogen narcosis is avoided by replacing air with helium–oxygen mixtures, enabling descent to 700 metres. At these extreme depths, direct effect of pressure on neurones can cause tremor, hemiparesis and cognitive impairment.
Problems during and following ascent
Free divers who breath-hold often hyperventilate deliberately prior to plunging in. This drives off CO2 – reducing the stimulus to inspire. During the subsequent breath-hold PaCO2 rises; PaO2 falls. On surfacing, decompression lowers PaO2 further. This can lead to syncope, known as a shallow water blackout. Since loss of consciousness can take place in the water, this can lead to fatalities.
FURTHER READING
Bennett P, Elliot D. The Physiology and Medicine of Diving, 5th edn. London: WB Saunders; 2002.
Edmonds C, Thomas B, McKewzie B, Pennefather J. Diving Medicine for Scuba Divers, 2012 edn. Available at: www.divingmedicine.info.
Melamed Y, Shupak A, Bitterman H. Medical problems associated with underwater diving. N Engl J Med 1992; 326:30–36.
Decompression sickness
Decompression sickness (the bends) are caused by release of bubbles of nitrogen or helium and follow returning too rapidly to the surface. Decompression tables indicate the duration for safe return from a given depth to the surface.
The bends can be mild (type 1, non-neurological bends), with skin irritation and mottling and/or joint pain. Type 2, neurological bends, are more serious – cortical blindness, hemiparesis, sensory disturbances or cord lesions develop.
If bubbles form in pulmonary vessels, divers experience retrosternal discomfort, breathlessness and cough, known as the chokes. These develop within minutes or hours of a dive. Decompression problems do not only occur immediately on reaching the surface, they may take some hours to become apparent. Over the subsequent 24 h, further ascent, e.g. air travel, can occasionally provoke the bends.
Other problems during ascent include paranasal sinus pain and nosebleeds – medically minor but dramatic, with excruciating pain and a mask full of bloody fluid. Toothache can be caused by gas bubbles within rotten fillings.
Management. All but the mildest forms of decompression sickness, e.g. skin mottling alone, require recompression in a pressure chamber, following strict guidelines. Recovery is usual. A long-term problem is aseptic necrosis of the hip due to nitrogen bubbles causing infarction. Focal neurological damage may persist, but complaints of fatigue and poor concentration are issues compounded by litigation that commonly follows diving accidents. Objective, evidence-based assessments are essential.
FURTHER READING
Lynch JH, Bove AA. Diving medicine: a review of current evidence. J Am Board Fam Med 2009; 22:399–407 (available at: http://www.jabfm.org/content/22/4/399.long).
SIGNIFICANT WEBSITES
Divers Alert Network (DAN): http://www.diversalertnetwork.org/
Diving Medicine for Scuba Divers: http://www.divingmedicine.info/
Lung rupture, pneumothorax and surgical emphysema
These emergencies occur when divers breath-hold during emergency ascents after gas supplies become exhausted. There is dyspnoea, cough and haemoptysis. Pneumothorax and surgical emphysema resolve with 100% oxygen. Air embolism can also occur and is treated with recompression.
Drowning and near-drowning
Drowning is a common cause of accidental death worldwide. In the UK, some 40% of drownings occur in children under 5 years of age. Drowning can also follow a seizure or a myocardial infarct. Exhaustion, alcohol, drugs and hypothermia all contribute to deaths following immersion.
Dry drowning
Between 10% and 15% of drownings occur without water aspiration into the lungs. Laryngeal spasm develops acutely, followed by apnoea and cardiac arrest.
Wet drowning
Fresh or seawater aspiration destroys pulmonary surfactant, leading to alveolar collapse, ventilation/perfusion mismatch and hypoxaemia. Aspiration of hypertonic seawater (5% NaCl) pulls additional fluid into the alveoli with further ventilation/perfusion mismatch. In practice, there is little difference between saltwater and freshwater aspiration. In both, severe hypoxaemia develops rapidly. Severe metabolic acidosis develops in the majority of survivors.
Treatment and prognosis
Cardiopulmonary resuscitation should be started immediately (see p. 691). Patients have survived for up to 30 minutes underwater without suffering brain damage – and sometimes for longer periods if TWater is near 10°C. Survival is probably related to the protective role of the diving reflex; submersion causes bradycardia and vasoconstriction. Oxygen consumption is also decreased by hypothermia.
Resuscitation should always be attempted, even with absent pulse and fixed dilated pupils. Patients frequently make a dramatic recovery. All survivors should be admitted to hospital for intensive monitoring – lung injury can develop during the subsequent 48 hours.
Recovery is frequently complete if consciousness is regained within several minutes of commencing resuscitation but poor if a patient remains stuporose or in coma at 30 minutes.
Ionizing radiation
Ionizing radiation is either penetrating (X-rays, γ-rays or neutrons) or non-penetrating (α- or β-particles). Penetrating radiation affects the skin and deeper tissues, while non-penetrating radiation affects the skin alone. All radiation effects depend on the type of radiation, the distribution of dose and the dose rate.
Dosage is measured in joules per kilogram (J/kg); 1 J/kg = 1 gray (1 Gy) = 100 rads.
Radioactivity is measured in becquerels (Bq). 1 Bq is defined as the activity of a quantity of radioactive material in which one nucleus decays per second; 3.7 × 1010 Bq = one curie (Ci), the older, non-SI unit.
Radiation differs in the density of ionization it causes. Therefore a dose-equivalent called a sievert (Sv) is used. This is the absorbed dose weighted for the damaging effect of the radiation. The annual background radiation is approximately 2.5 mSv. A chest X-ray delivers 0.02 mSv, and CT of the abdomen/pelvis about 10 mSv (see Table 9.5). A cumulative risk of cancer following repeated imaging procedures has been established and reduction of X-ray exposures should be made if possible.
Excessive exposure to ionizing radiation follows accidents in industry, nuclear power plants and hospitals and deliberate nuclear explosions designed to eliminate populations – and exceptionally, by poisoning, e.g. with polonium.
Mild acute radiation sickness
Nausea, vomiting and malaise follow doses of approximately 1 Gy. Lymphopenia occurs within several days, followed 2–3 weeks later by a fall in all white cells and platelets.
Acute radiation sickness
Many systems are affected; the extent depends on the dose of radiation (Table 18.3).
Table 18.3 Systemic radiation effects
| Acute effects | Delayed effects |
|---|---|
Haemopoietic syndrome |
Infertility |
Gastrointestinal syndrome |
Teratogenesis |
CNS syndrome |
Cataract |
Radiation dermatitis |
Neoplasia: |
|
Acute myeloid leukaemia |
|
Thyroid |
|
Salivary glands |
|
Skin |
|
Others |
Haemopoietic syndrome
Absorption of 2–10 Gy is followed by transient vomiting in some individuals, followed by a period of improvement. Lymphocytes are particularly sensitive to radiation damage; severe lymphopenia develops over several days. A decrease in granulocytes and platelets follows 2–3 weeks later, since no new cells are formed in the marrow. Thrombocytopenia with bleeding develops and frequent overwhelming infections, with a high mortality.
Gastrointestinal syndrome
Doses >6 Gy cause vomiting several hours after exposure. This then stops, only to recur some 4 days later accompanied by diarrhoea. The villous lining of the intestine becomes denuded. Intractable bloody diarrhoea follows, with dehydration, secondary infection and sometimes death.
Late effects of radiation exposure
Survivors of the nuclear bombing of Hiroshima and Nagasaki in 1945 provided data on long-term radiation effects. Risks of acute myeloid leukaemia and cancer, particularly of skin, thyroid and salivary glands, increase. Infertility, teratogenesis and cataract are also late sequelae, developing years after exposure.
The sequelae of therapeutic radiation – early, early-delayed and late-delayed radiation effects are discussed on page 448. Focussing techniques are used to target radiation towards the field being treated; radiosensitive structures such as the ovaries are protected by shielding.
Treatment
Acute radiation sickness is an emergency. Absorption of the initial radiation dose can be reduced by removing contaminated clothing.
Treatment is largely supportive – prevention and treatment of infection, haemorrhage and fluid loss. Harvesting of blood products is sometimes carried out.
Accidental ingestion of, or exposure to, bone-seeking radioisotopes (e.g. strontium-90 and caesium-137) are treated with chelating agents, e.g. EDTA and massive doses of oral calcium. Radioiodine contamination should be treated immediately with potassium iodide to block radioiodine absorption by the thyroid.
Electric shock
 Pain and psychological sequelae. The common domestic electric shock is typically painful, rarely fatal or followed by serious sequelae. Nevertheless, it is an unpleasant and intensely frightening experience. A brief immediate jerking episode can occur, that is not an epileptic seizure. There is usually no lasting neurological, cardiac or skin damage. More serious effects are distinctly rare following accidents in the home or in industry, but claims by survivors following industrial accidents are frequently made.
Pain and psychological sequelae. The common domestic electric shock is typically painful, rarely fatal or followed by serious sequelae. Nevertheless, it is an unpleasant and intensely frightening experience. A brief immediate jerking episode can occur, that is not an epileptic seizure. There is usually no lasting neurological, cardiac or skin damage. More serious effects are distinctly rare following accidents in the home or in industry, but claims by survivors following industrial accidents are frequently made.
 Cardiac, neurological and muscle damage. Ventricular fibrillation, muscular contraction and spinal cord damage can follow a major shock. These are seen typically following lightning strikes with exceedingly high voltage and amperage.
Cardiac, neurological and muscle damage. Ventricular fibrillation, muscular contraction and spinal cord damage can follow a major shock. These are seen typically following lightning strikes with exceedingly high voltage and amperage.
 Electrical burns. These are commonly restricted to the skin – non-fatal lightning strikes cause fern-shaped burns. Muscle necrosis and spinal cord damage can also occur.
Electrical burns. These are commonly restricted to the skin – non-fatal lightning strikes cause fern-shaped burns. Muscle necrosis and spinal cord damage can also occur.
 Electrocution. This means death following ventricular fibrillation, either accidentally, or deliberately as a method of execution. In the USA, at executions an initial voltage of >2000 volts was applied for some 15 seconds in the electric chair, causing loss of consciousness and ventricular fibrillation before the voltage was lowered. The TCore during the execution process would sometimes reach >50°C, leading to severe damage to internal organs.
Electrocution. This means death following ventricular fibrillation, either accidentally, or deliberately as a method of execution. In the USA, at executions an initial voltage of >2000 volts was applied for some 15 seconds in the electric chair, causing loss of consciousness and ventricular fibrillation before the voltage was lowered. The TCore during the execution process would sometimes reach >50°C, leading to severe damage to internal organs.
Smoke
Smoke is air containing toxic and/or irritant gases and carbon particles, coated with organic acids, aldehydes and synthetic materials. Carbon monoxide, sulphur dioxide, sulphuric and hydrochloric acids and other toxins may also be present. The highly toxic polyvinyl chloride is no longer used in household goods. Air pollution is discussed on page 807.
On smoke inhalation, patients become breathless and tachypnoeic immediately. Choking and stridor may require intubation. Pulmonary oedema and hypoxia can be fatal.
Breathing through a wet towel or clothing is the best emergency treatment. Remove the victim from the scene as rapidly as possible. Give oxygen, and arrange ITU support.
Noise
Sound intensity is expressed as the square of sound pressure. The bel is the ratio equivalent to a 10-fold increase in sound intensity; a decibel (dB) is one-tenth of a bel. Sound is made up of a number of frequencies ranging from 30 Hz to 20 kHz, with most being between 1 and 4 kHz. In practice, a scale known as A-weighted sound is used; sound levels are reported as dB(A). A hazardous sound source is defined as one with an overall sound pressure of >90 dB(A).
Repeated prolonged exposure to loud noise, particularly between 2 and 6 kHz, causes first temporary and later permanent hearing loss, by physically destroying hair cells in the organ of Corti and, eventually, auditory neurones. Noise-induced hearing loss is a common occupational problem, not only in industry and the armed forces, but also in the home (drills and sanders), in sport (motor racing) and in entertainment (musicians, DJs and their audiences).
Serious noise-induced hearing loss is almost wholly preventable by personal protection (ear muffs, ear plugs). Little can be offered once hearing loss has become established.
Bioterrorism/biowarfare
Interest in biological warfare and bioterrorism intensified during the 1991 Iraq war and later following the destruction of the Twin Towers in New York in 2001. The potential of bacteria as weapons is illustrated by a suggestion that several kilograms of anthrax spores might kill as many people as a Hiroshima-sized nuclear weapon.
Potential pathogens
The US Centers for Disease Control and Prevention in Atlanta, Georgia, have developed a classification of potential biological agents (Table 18.4).
Table 18.4 Critical biological agents
| Category | Pathogens |
|---|---|
A.Very infectious and/or readily disseminated organisms: high mortality with a major impact on public health |
Smallpox, anthrax, botulinism, plague |
B.Moderately easy to disseminate organisms causing moderate morbidity and mortality |
Q fever, brucellosis, glanders, food-/water-borne pathogens, influenza |
C.Emerging and possible genetically engineered pathogens |
Viral haemorrhagic fevers, encephalitis viruses, drug-resistant TB |
Adapted from Khan AS, Morse S, Lillibridge S. Public health preparedness for biological terrorism in the USA. Lancet 2000; 356:1179–1182, reprinted with permission from Elsevier.
Smallpox
Smallpox is a highly infectious disease with a mortality >30%. There is no proven therapy, but there is an effective vaccine. Universal vaccination was stopped in the early 1970s: the vast majority of the world’s population is now unprotected against the variola virus (see p. 101). The potential exists for a worldwide epidemic of smallpox, possibly initiated by a bioterrorist act.
Smallpox has an incubation period of around 12 days, allowing any initial source of infection to go undetected until the rash (Fig. 18.2), similar to chickenpox, develops on the 2nd or 3rd day of the illness. Infection is transmitted by the airborne route; the patient becomes infectious to others 12–24 hours before the rash appears, thus allowing a potential infected volunteer to pass infection to others before being recognized as suffering from smallpox. If vaccines were to be administered widely to those potentially infected within 3 days of contact, an epidemic might well be prevented. Smallpox virus is stored in two secure laboratories – in Russia and in the USA. Supplies of vaccine are potentially available worldwide.
Anthrax
In late 2001, anthrax organisms (see p. 132) were sent through the US mail and infected 22 individuals. Of these, 11 developed pulmonary anthrax, five of whom died; 11 suffered from cutaneous anthrax.
A simulated anthrax attack postulated release of anthrax powder from a truck passing a sports stadium with 74 000 spectators; 16 000 were estimated to have become infected, with a death rate of 25%. In Russia, following accidental release of anthrax from a bioweapons factory, the death rate was substantial in those nearby, especially downwind.
Botulism
The toxin produced by Clostridium botulinum is one of the most potent poisons known (see p. 86).
As a bioweapon, botulinum toxin could be transmitted in food or by air, e.g. from a crop-spraying light aircraft. The toxin is inactivated by chlorine in domestic water supplies. There is no vaccine available.
Plague
Plague (see p. 136) could be transmitted as a bioweapon either by air-borne dissemination or by infected rats. Immunization is of limited value.
Other potential infective agents are listed in Table 18.4.
Travel
Motion sickness
This common problem is caused by repetitive stimulation of the labyrinth. Motion sickness occurs frequently at sea and in cars (especially in children), but also with less usual forms of transport such as camels or elephants. Nowadays, motion sickness is rare during commercial flights, but it is a problem during space travel, and on airships – one reason why the airship industry has not flourished.
Nausea, sweating, dizziness, vertigo and profuse vomiting occur, accompanied by an irresistible desire to stop moving. Prostration and intense incapacitating malaise can develop, e.g. in seasickness.
Prophylactic antihistamines, vestibular sedatives (hyoscine or cinnarizine) and stem ginger are of some value.
Jet-lag
Jet-lag (circadian dyschronism) is the well-known phenomenon that follows travelling through time-zones, particularly from West to East. Intense insomnia, fatigue, poor concentration, irritability and loss of appetite are common. Headaches may occur. Symptoms last several days.
Mechanisms relate to the hypothalamic body clock within the suprachiasmatic nuclei. The clock is regulated by various zeitgebers (time-givers), e.g. light and melatonin.
Management of jet-lag includes its acceptance as a phenomenon causing poor performance – and thus waiting for 3–5 days to recover. Drink plenty of fluid, avoiding alcohol. Various hypnotics can help insomnia, but their value is disputed. Oral melatonin is widely used to reduce jet-lag but is not available on prescription in the UK. Melatonin probably hastens resetting the body clock.
Building-related illnesses
Nonspecific building-related illness
Multi-storey buildings typically have a controlled environment, often with automated heating and air-conditioning, and without ready access to external ventilation. More than half the adult workforce in developed countries work in such offices.
Headache, fatigue and difficulty concentrating, sometimes in epidemics, are the main complaints – but have become less frequent. Psychological factors are thought to have a substantial role. Temperature, humidity, dust, volatile organic compounds, e.g. paints and solvents, and even low level carbon monoxide toxicity have all been blamed, none with any scientific foundation.
Specific building-related illnesses
Legionnaires’ disease (see p. 836) can follow contamination of air-conditioning systems.
Humidifier fever (see p. 854) is also due to contaminated systems, probably by fungi, bacteria and protozoa. Many common viruses are potentially transmissible in an enclosed environment, e.g. the common cold, influenza and rarely pulmonary TB. Allergic disorders, e.g. rhinitis, asthma and dermatitis, also occur following exposure to indoor allergens such as dust mites and plants. Office equipment, e.g. fumes from photocopiers, has also been implicated. Passive smoking (see p. 807) is no longer an issue in Europe and North America, following legislation against smoking.