Chapter 4 Infectious diseases, tropical medicine and sexually transmitted infections
Infection and infectious disease
‘Infection’ is defined as the process of foreign organisms invading and multiplying in or on a host. In practice, the term is usually reserved for situations in which this results in harm, rather than an infectious agent simply colonizing the host without ill effect. Infectious diseases remain the main cause of morbidity and mortality in man, particularly in developing areas where they are associated with poverty and overcrowding.
In the developed world increasing prosperity, universal immunization and antibiotics have reduced the prevalence of infectious disease. However, antibiotic-resistant strains of microorganisms and diseases such as human immunodeficiency virus (HIV) infection, variant Creutzfeldt–Jakob disease (vCJD), avian influenza and pandemic H1N1 influenza have emerged. There is increased global mobility, both enforced (as a result of war, civil unrest and natural disaster) and voluntary (for tourism and economic benefit). This has aided the spread of infectious disease and allowed previously localized pathogens such as dengue and West Nile virus to establish themselves across much wider territories. An increase in the movement of livestock and animals has enabled the spread of zoonotic diseases like monkeypox, while changes in farming and food-processing methods have contributed to an increase in the incidence of food- and water-borne diseases. Deteriorating social conditions in the inner city areas of our major conurbations have facilitated the resurgence of tuberculosis and other infections. Prisons and refugee camps, where large numbers of people are forced to live in close proximity, often in poor conditions, are providing a breeding ground for devastating epidemics of infectious disease. There are new concerns about the deliberate release of infectious agents such as smallpox or anthrax by terrorist groups or national governments.
In the developing world successes such as the eradication of smallpox have been balanced or outweighed by the new plagues. Infectious diseases cause nearly 25% of all human deaths (Table 4.1), rising to more than 50% in low income countries. Two billion people – one-third of the world’s population – are infected with tuberculosis (TB), up to 400 million people catch malaria every year and 200 million are infected with schistosomiasis. Some 500 million people are chronically infected with a hepatitis virus (either HBV or HCV) and 34 million people are living with HIV/AIDS, with 2.6 million new HIV infections in 2008 (65% in sub-Saharan Africa). Infections are often multiple and there is synergy both between different infections and between infection and other factors such as malnutrition. Many of the infectious diseases affecting developing countries are preventable or treatable, but continue to thrive owing to lack of money and political will.
Table 4.1 Worldwide mortality from infectious diseases
| Disease | Estimated deaths (annual) |
|---|---|
Acute lower respiratory infection |
3.5 million |
HIV/AIDS |
2 million |
Tuberculosis |
2 million |
Diarrhoeal disease |
1.8 million |
Malaria |
1 million |
Measles |
350 000 |
Whooping cough |
301 000 |
Tetanus |
292 000 |
Meningitis |
175 000 |
Leishmaniasis |
51 000 |
Trypanosomiasis |
10 000 |
The WHO has set eight Millennium Development Goals (MDGs), to be achieved by 2015: these include combating HIV/AIDS, malaria and other diseases. Currently, nine African and 29 non-African countries are on course to meet the malaria targets and the global incidence of TB is slowly falling. New HIV infections fell by 16% between 2000 and 2008 and antiretroviral treatment provision in low and middle income countries increased 10-fold between 2003 and 2008. A public/private partnership, the Global Fund, was established to combat AIDS, tuberculosis and malaria and has achieved much by providing the means for treatment for TB, insecticide-treated bed nets for malaria and antivirals for HIV. Several other funding streams (governmental, non-governmental and charitable) have also contributed to the fight against infection.
The impact of global warming on the spread of infection remains uncertain but may be significant. Both natural climatic events and the gradual global change in weather conditions can affect the spread and transmission of infectious diseases. Changes in temperature may directly influence the behaviour of insect vectors, while changes in rainfall may have an effect on water-borne disease. Climate change may also trigger population movement and migration, indirectly affecting infection transmission.
Infectious agents
The causative agents of infectious diseases can be divided into four groups:
Prions are the most recently recognized and the simplest infectious agents, consisting of a single protein molecule. They contain no nucleic acid and therefore no genetic information: their ability to propagate within a host relies on inducing the conversion of endogenous prion protein PrPc into an abnormal protease-resistant isoform referred to as PrPSc.
Viruses contain both protein and nucleic acid and so carry the genetic information for their own reproduction. However, they lack the apparatus to replicate autonomously, relying instead on ‘hijacking’ the cellular machinery of the host. They are small (usually less than 250 nanometres (nm) in diameter) and each virus possesses only one species of nucleic acid (either RNA or DNA).
Bacteria are usually, though not always, larger than viruses. Unlike the latter they have both DNA and RNA, with the genome encoded by DNA. They are enclosed by a cell membrane and even bacteria which have adopted an intracellular existence remain enclosed within their own cell wall. Bacteria are capable of fully autonomous reproduction and the majority are not dependent on host cells.
Eukaryotes are the most sophisticated infectious organisms, displaying subcellular compartmentalization. Different cellular functions are restricted to specific organelles, e.g. photosynthesis takes place in the chloroplasts, DNA transcription in the nucleus and respiration in the mitochondria. Eukaryotic pathogens include unicellular protozoa, fungi (which can be unicellular or filamentous) and multicellular parasitic worms.
Other higher classes, notably the insects and the arachnids, also contain species which can parasitize man and cause disease: these are discussed in more detail on page 160.
Host–organism interactions
Each of us is colonized with huge numbers of microorganisms (1014 bacteria, plus viruses, fungi, protozoa and worms) with which we co-exist. The relationship with some of these organisms is symbiotic, in which both partners benefit, while others are commensals, living on the host without causing harm. Infection and illness may be due to these normally harmless commensals and symbiotes evading the body’s defences and penetrating into abnormal sites. Alternatively, disease may be caused by exposure to exogenous pathogenic organisms which are not part of our normal flora.
The symptoms and signs of infection are a result of the interaction between host and pathogen. In some cases, such as the early stages of influenza, symptoms are almost entirely due to killing of host cells by the invading organism. Usually, however, the harmful effects of infection are due to a combination of direct microbial pathogenicity and the body’s response to infection. In meningococcal septicaemia, for example, much of the tissue damage is caused by cytokines released in an attempt to fight the bacteria. The molecular mechanisms underlying host-pathogen interactions are discussed in more detail on page 78.
Sources of infection
The endogenous skin and bowel commensals can cause disease in the host, either because they have been transferred to an inappropriate site (e.g. bowel coliforms causing urinary tract infection) or because host immunity has been attenuated (e.g. candidiasis in an immunocompromised host). Many infections are acquired from other people, who may be symptomatic themselves or be asymptomatic carriers. Some bacteria, like the meningococcus, are common transient commensals, but cause invasive disease in a small minority of those colonized. Infection with other organisms, such as the hepatitis B virus, can be followed in some cases by an asymptomatic but potentially infectious carrier state.
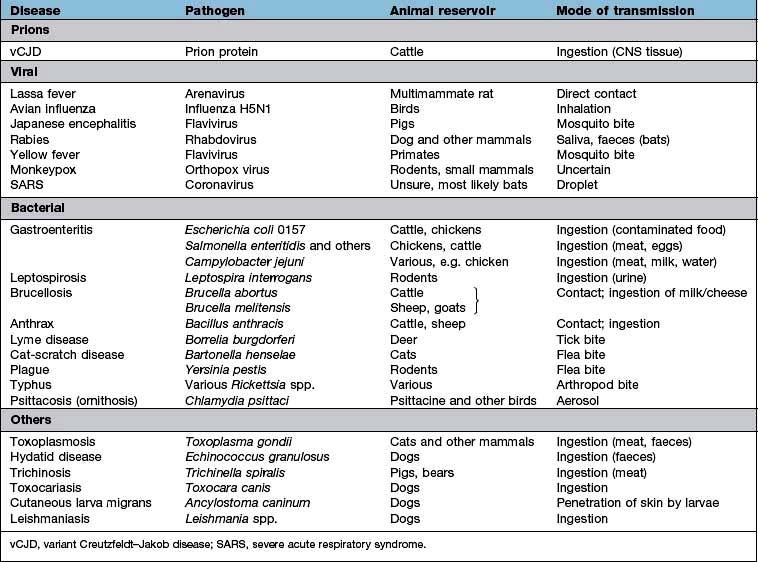
Zoonoses are infections that can be transmitted from wild or domestic animals to man. Infection can be acquired in a number of ways: direct contact with the animal, ingestion of meat or animal products, contact with animal urine or faeces, aerosol inhalation, via an arthropod vector or by inoculation of saliva in a bite wound. Many zoonoses can also be transmitted from person to person. Some zoonoses are listed in Table 4.2.
Most microorganisms do not have a vertebrate or arthropod host but are free-living in the environment. The vast majority of these environmental organisms are non-pathogenic, but a few can cause human disease (Table 4.3). Person-to-person transmission of these infections is rare. Some parasites may have a stage of their life cycle which is environmental (e.g. the free-living larval stage of Strongyloides stercoralis and the hookworms), even though the adult worm requires a vertebrate host. Other pathogens can survive for periods in water or soil and be transmitted from host to host via this route (see below): these should not be confused with true environmental organisms.
Table 4.3 Environmental organisms which can cause human infection
| Organism | Disease (most common presentations) |
|---|---|
Bacteria |
|
Burkholderia pseudomallei |
Melioidosis |
Burkholderia cepacia |
Lung infection in cystic fibrosis |
Pseudomonas spp. |
Various |
Legionella pneumophila |
Legionnaires’ disease (pneumonia) |
Bacillus cereus |
Gastroenteritis |
Listeria monocytogenes |
Various |
Clostridium tetani |
Tetanus |
Clostridium perfringens |
Gangrene, septicaemia |
Mycobacteria other than tuberculosis (MOTT) |
Pulmonary infections |
Fungi |
|
Candida spp. |
Local and disseminated infection |
Cryptococcus neoformans |
Meningitis, pulmonary infection |
Histoplasma capsulatum |
Pulmonary infection |
Coccidioides immitis |
Pulmonary infection |
Mucor spp. |
Mucormycosis (rhinocerebral, cutaneous) |
Sporothrix schenckii |
Lymphocutaneous sporotrichosis |
Blastomyces dermatitidis |
Pulmonary infection |
Aspergillus fumigatus |
Pulmonary infections |
Routes of transmission
The body’s own endogenous flora can cause infection if the organism gains access to an inappropriate area of the body. This can happen by simple mechanical transfer, e.g. colonic bacteria entering the female urinary tract. The nonspecific host defences may be breached, for example, by cutting or scratching the skin and allowing surface commensals to gain access to deeper tissues; this is frequently the aetiology of cellulitis. There may be more serious defects in host immunity owing to disease or chemotherapy, allowing normally harmless skin and bowel flora to produce invasive disease.
Many respiratory tract pathogens are spread from person to person by aerosol or droplet transmission. Secretions containing the infectious agent are coughed, sneezed or breathed out and are then inhaled by a new victim. Some enteric viral infections may also be spread by aerosols of faeces or vomit. Environmental pathogens such as Legionella pneumophila and zoonoses such as psittacosis, are also acquired by aerosol inhalation, while rabies virus may be inhaled in the dust from bat droppings.
Transmission of organisms by the faeco-oral route can occur by direct transfer (usually in small children), by contamination of clothing or household items (usually in institutions or conditions of poor hygiene) or most commonly via contaminated food or water. Human and animal faecal pathogens can get into the food supply at any stage. Raw sewage is used as fertilizer in many parts of the world, contaminating growing vegetables and fruit. Poor personal hygiene can result in contamination during production, packaging, preparation, or serving of foodstuffs. In the western world, the centralization of food supply and increased processing of food has allowed the potential for relatively minor episodes of contamination to cause widely disseminated outbreaks of food-borne infection.
Water-borne faeco-oral spread is usually the result of inadequate access to clean water and safe sewage disposal and is common throughout the developing world. Worldwide, 1.1 billion people have no access to clean water and 2.6 billion do not have basic sanitation.
Many tropical infections, including malaria, are spread from person to person or from animal to person by an arthropod vector. Vector-borne diseases are also found in temperate climates, but are relatively uncommon. In most cases part of the parasite life cycle takes place within the body of the arthropod and each parasite species requires a specific vector. Simple mechanical transfer of infective organisms from one host to another can occur, but is rare. Some vector-borne diseases are shown in Table 4.4.
Table 4.4 Infections transmitted by arthropod vectors
| Vector | Disease | Microorganism |
|---|---|---|
Mosquito |
Malaria |
Plasmodium spp. |
Lymphatic filariasis |
Wuchereria bancrofti, Brugia malayi |
|
Yellow fever |
Flavivirus |
|
West Nile fever |
Flavivirus |
|
Dengue |
Flavivirus |
|
Sandfly |
Leishmaniasis |
Leishmania spp. |
Blackfly |
Onchocerciasis |
Onchocerca volvulus |
Tsetse fly |
Sleeping sickness |
Trypanosoma brucei |
Flea |
Plague |
Yersinia pestis |
Endemic typhus |
Rickettsia typhi |
|
Carrion’s disease |
Bartonella bacilliformis |
|
Reduviid bug |
Chagas’ disease |
Trypanosoma cruzi |
Louse |
Epidemic typhus |
Rickettsia prowazekii |
Louse-borne relapsing fever |
Borrelia recurrentis |
|
Hard tick |
Lyme disease |
Borrelia burgdorferi |
Typhus (spotted fever group) |
Rickettsia spp. |
|
Babesiosis |
Babesia spp. |
|
Tick-borne relapsing fever |
Borrelia duttonii |
|
Tick-borne encephalitis |
Flavivirus |
|
Congo-Crimean haemorrhagic fever |
Nairovirus (Bunyavirus) |
Direct person-to-person spread
Organisms can be passed on directly in a number of ways. Sexually transmitted infections are dealt with on page 160. Skin infections such as ringworm, and ectoparasites such as scabies and head lice, can be spread by simple skin-to-skin contact. Other organisms are passed on by blood- (or occasionally other body fluid) to-blood transmission. Blood-to-blood transmission can occur during sexual contact, from mother to infant either transplacentally or in the peripartum, between intravenous drug users sharing any part of their injecting equipment, when infected medical or other (e.g. tattoo needles) equipment is reused, if contaminated blood or blood products are transfused, or in any sporting or accidental contact when blood is spilled. Ingestion of infected breast milk is another route of person-to-person spread for some infections (e.g. HIV).
Infection can occur when pathogenic organisms breach the normal mechanical defences by direct inoculation. Some of the circumstances in which this can occur are covered under endogenous infection and blood-to-blood transmission above. Some environmental organisms may be inoculated by accident: this is a common mode of transmission of tetanus and certain fungal infections. Rabies virus may be inoculated by the bite of an infected animal.
Consumption of infected material
Although many food-related zoonotic infections are due to contamination of food with animal faeces (and are thus, strictly speaking, faeco-oral), several diseases are transmitted directly in animal products. These include some strains of Salmonella (eggs, chicken meat), brucellosis (unpasteurized milk) E. coli and the prion diseases kuru and vCJD (neural tissue).
Prevention and control
Methods of preventing infection depend upon the source and route of transmission, as described above.
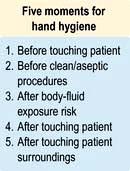
 Infection control measures. Poor infection control practice in hospitals and other healthcare environments can cause the transfer of infection from person to person. This may be air-borne, via fomites or a direct contact route. It is essential that all healthcare workers wash or clean their hands before and after patient contact and whenever necessary they should wear gloves, aprons and other protective equipment. This is particularly necessary when performing invasive procedures, or manipulating indwelling devices such as cannulae.
Infection control measures. Poor infection control practice in hospitals and other healthcare environments can cause the transfer of infection from person to person. This may be air-borne, via fomites or a direct contact route. It is essential that all healthcare workers wash or clean their hands before and after patient contact and whenever necessary they should wear gloves, aprons and other protective equipment. This is particularly necessary when performing invasive procedures, or manipulating indwelling devices such as cannulae.
 Eradication of reservoir. In a few diseases, for which man is the only natural reservoir of infection, it may be possible to eliminate disease by an intensive programme of case finding, treatment and immunization. This has been achieved in the case of smallpox. If there is an animal or environmental reservoir, complete eradication is unlikely, but local control methods may decrease the risk of human infection (e.g. killing of rodents to control plague, leptospirosis and other diseases).
Eradication of reservoir. In a few diseases, for which man is the only natural reservoir of infection, it may be possible to eliminate disease by an intensive programme of case finding, treatment and immunization. This has been achieved in the case of smallpox. If there is an animal or environmental reservoir, complete eradication is unlikely, but local control methods may decrease the risk of human infection (e.g. killing of rodents to control plague, leptospirosis and other diseases).
 Immunization (see p. 94).
Immunization (see p. 94).
Healthcare-associated infections (HCAI)
In recent years, the burden of morbidity, mortality and cost attributed to healthcare-associated infection has been highlighted in many developed countries. Although data from low income countries are lacking the impact of HCAI is likely to be even greater. Clostridium difficile, Staphylococcus aureus (especially MRSA), vancomycin-resistant enterococci and multiresistant Gram-negative organisms are all strongly associated with healthcare contact and are an increasing problem in hospitals worldwide. In the UK, the Department of Health estimates the risk of acquiring HCAI in a healthcare facility to be 6–10%, with HCAIs costing the NHS up to £1 billion per year. The response to HCAIs needs to be multifaceted. High standards of basic infection control (isolation, barrier precautions, hand hygiene and cleaning) need to be combined with decreased use of invasive devices such as vascular cannulae and urinary catheters, with better insertion and care standards when these are used. Antibiotic stewardship, with reduced overall usage and restriction of broad-spectrum agents, is essential to minimize antimicrobial resistance. There are already data to suggest that reduction in the use of cephalosporins has reduced the incidence of C. difficile. Often a combination of different methods can be used together to reduce a particular risk (e.g. ventilator-associated pneumonia): the so-called ‘care bundle’ approach.
Classification of outbreaks
The type of outbreak has a bearing on public health measures that need to be instituted for its control.
 Person to person where infection is passed from one infected individual to another and outbreaks of infection are separated by the incubation period.
Person to person where infection is passed from one infected individual to another and outbreaks of infection are separated by the incubation period.
 ‘Point source’ is where there is a single source of infection, e.g. food eaten at a social function. All those infected will develop symptoms at the same time, around the expected incubation period.
‘Point source’ is where there is a single source of infection, e.g. food eaten at a social function. All those infected will develop symptoms at the same time, around the expected incubation period.
 Common source where there is a single source of infection but over a period of time, e.g. a symptomatic carrier of infection working with food preparation. Many people will be exposed over a long period of time.
Common source where there is a single source of infection but over a period of time, e.g. a symptomatic carrier of infection working with food preparation. Many people will be exposed over a long period of time.
 Epidemic. An increased unusual widespread infection in the community, causing waves of infection. These spread through communities and affect all people who have no active immunity to that infection.
Epidemic. An increased unusual widespread infection in the community, causing waves of infection. These spread through communities and affect all people who have no active immunity to that infection.
Cases of some infectious diseases should be notified to the public health authorities so that they are aware of cases and outbreaks. Diseases that are notifiable in England and Wales are listed in Table 4.5.
Table 4.5 Diseases notifiable (to Local Authority Proper Officers) in England and Wales, under the Health Protection (Notification) Regulations 2010
FURTHER READING
Cardo D, Dennehy PH, Halverson P et al. Moving toward elimination of healthcare-associated infections: a call to action. Am J Infect Control 2010; 38:671–675.
Chomel B, Belotto A, Meslin FX. Wildlife, exotic pets and emerging zoonoses. Emerg Infect Dis 2007; 13:6–11.
Horton R, Das P. Indian health: the path from crisis to progress. Lancet 2011; 377:181–183.
Relman DA. Microbial genomics and infectious diseases. N Engl J Med 2011; 365: 347–357.
Shurman EK. Global climate change and infectious disease. N Engl J Med 2010; 282:1061–1063.
SIGNIFICANT WEBSITES
Health Protection Agency: http://www.hpa.org.uk
WHO Infectious Diseases: http://www.who.int/topics/infectious_diseases/en/
Principles and basic mechanisms
Man constantly interacts with the world of microorganisms from birth to death. The majority cause no harm and some play a role in the normal functioning of the mouth, vagina and intestinal tract. However many microorganisms have the potential to produce disease. This may result from inoculation into damaged tissues, tissue invasion, a variety of virulence factors, or toxin production.
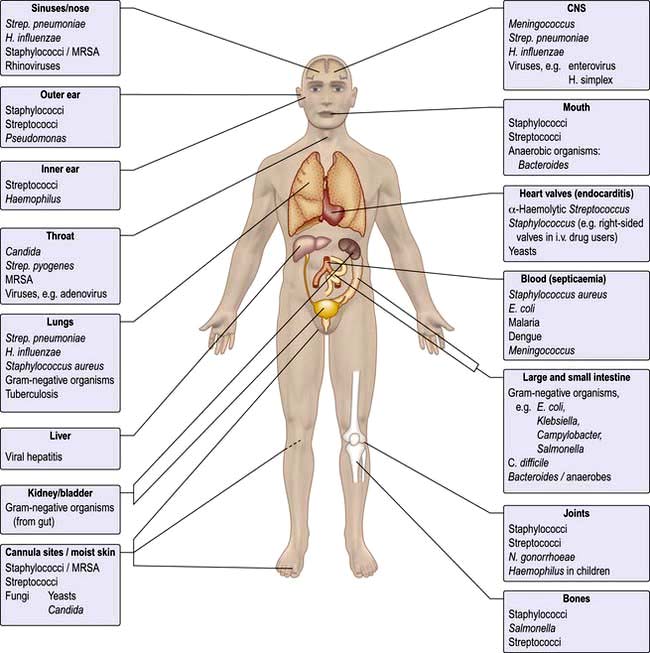
Specificity
Microorganisms are often highly specific with respect to the organ or tissue they infect (Fig. 4.1). For example, a number of viruses are hepatotropic, such as those responsible for hepatitis A, B, C and E and yellow fever. This predilection for specific sites in the body relates partly to the presence of appropriate receptors on different cell types and partly to the immediate environment in which the organism finds itself; e.g. anaerobic organisms colonize the anaerobic colon, whereas aerobic organisms are generally found in the mouth, pharynx and proximal intestinal tract. Other organisms that show selectivity include:
Even within a species of bacterium such as E. coli, there are clear differences between strains with regard to their ability to cause gastrointestinal disease (see p. 110), which in turn differ from uropathogenic E. coli responsible for urinary tract infection.
Within an organ a pathogen may show selectivity for a particular cell type. In the intestine, for example, rotavirus predominantly invades and destroys intestinal epithelial cells on the upper portion of the villus, whereas reovirus selectively enters the body through the specialized epithelial cells, known as M cells that cover the Peyer’s patches (see p. 262).
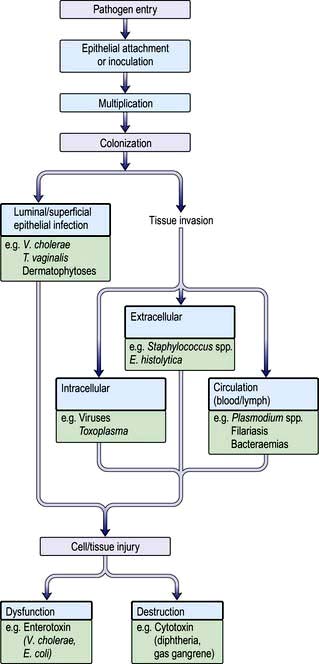
Pathogenesis
Figure 4.2 summarizes some of the steps that occur during the pathogenesis of infection. In addition, pathogens have developed a variety of mechanisms to evade host defences. For example, some pathogens produce toxins directed at phagocytes: Staphylococcus aureus (α-toxin), Streptococcus pyogenes (streptolysin) and Clostridium perfringens (α-toxin), while others such as Salmonella spp. and Listeria monocytogenes can survive within macrophages. Several pathogens possess a capsule that protects against complement activation (e.g. Strep. pneumoniae). Antigenic variation is an additional mechanism for evading host defences that is recognized in viruses (antigenic shift and drift in influenza), bacteria (flagella of salmonella and gonococcal pili) and protozoa (surface glycoprotein changes in Trypanosoma).
Epithelial attachment
Many bacteria attach to the epithelial substratum by specific organelles called pili (or fimbriae) that contain a surface lectin(s) – a protein or glycoprotein that recognizes specific sugar residues on the host cell. This family of molecules is known as adhesins (see p. 23). Following attachment, some bacteria, such as species of coagulase-negative staphylococci, produce an extracellular slime layer and recruit additional bacteria, which cluster together to form a biofilm. These biofilms can be difficult to eradicate and are a frequent cause of medical device-associated infections which affect prosthetic joints and heart valves as well as indwelling catheters. Many viruses and protozoa (e.g. Plasmodium spp., Entamoeba histolytica) attach to specific epithelial target-cell receptors. Other parasites such as hookworm have specific attachment organs (buccal plates) that firmly grip the intestinal epithelium.
Colonization
Following epithelial attachment pathogens may remain either on the surface epithelium or within the lumen of the organ they have colonized. Tissue invasion may follow.
 an intracellular location for the pathogen (e.g. viruses, Mycobacterium spp., Toxoplasma gondii, Plasmodium spp.)
an intracellular location for the pathogen (e.g. viruses, Mycobacterium spp., Toxoplasma gondii, Plasmodium spp.)
 an extracellular location for the pathogen (e.g. pneumococci, E. coli, Entamoeba histolytica)
an extracellular location for the pathogen (e.g. pneumococci, E. coli, Entamoeba histolytica)
 invasion directly into the blood or lymph circulation (e.g. schistosome schistosomula and trypanosomes).
invasion directly into the blood or lymph circulation (e.g. schistosome schistosomula and trypanosomes).
Once the pathogen is firmly established in its target tissue, a series of events follows that usually culminates in damage to the host.
Tissue dysfunction or damage
Microorganisms produce disease by a number of well-defined mechanisms:
The presence of replicating viruses within a cell may interfere with host cell metabolism such that the cell dies – so-called cytolytic or cytocidal infection.
 Exotoxins have many diverse activities including inhibition of protein synthesis (diphtheria toxin), neurotoxicity (Clostridium tetani and C. botulinum) and enterotoxicity, which results in intestinal secretion of water and electrolytes (E. coli, Vibrio cholerae). Colonization and secretion in many classical diarrhoeal diseases is the result of virulence-associated genes which encode protein secretion systems (Fig. 4.3).
Exotoxins have many diverse activities including inhibition of protein synthesis (diphtheria toxin), neurotoxicity (Clostridium tetani and C. botulinum) and enterotoxicity, which results in intestinal secretion of water and electrolytes (E. coli, Vibrio cholerae). Colonization and secretion in many classical diarrhoeal diseases is the result of virulence-associated genes which encode protein secretion systems (Fig. 4.3).
 Endotoxin is a lipopolysaccharide (LPS) in the cell wall of Gram-negative bacteria. It is responsible for many of the features of septic shock (see p. 881), namely hypotension, fever, intravascular coagulation and, at high doses, death. The effects of endotoxin are mediated predominantly by release of tumour necrosis factor.
Endotoxin is a lipopolysaccharide (LPS) in the cell wall of Gram-negative bacteria. It is responsible for many of the features of septic shock (see p. 881), namely hypotension, fever, intravascular coagulation and, at high doses, death. The effects of endotoxin are mediated predominantly by release of tumour necrosis factor.
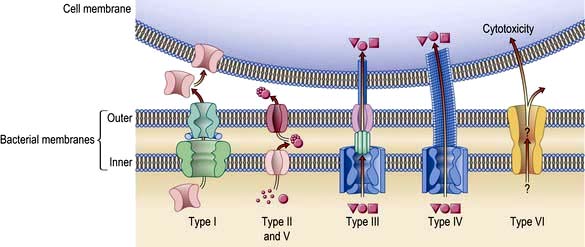
Figure 4.3 Protein secretion pathways for Gram-negative bacteria. These specialized pathways are necessary for virulence. Types I and II facilitate protein (toxin) secretion into the extracellular space (Type I). Type II does this in two stages. Types III and IV pathways secrete toxins as well as inject toxins directly into the host cells via multiprotein complexes across the bacterial cell envelope and host cell membrane. Type V is a minor variation of Type II. Type VI pathway is unclear but is involved in cytotoxicity.
(Reproduced with permission from Yarh TL. A critical new pathway for toxin secretion? New England Journal of Medicine 2006; 355:1171–1172.
Staphylococcus aureus presents an excellent example of the repertoire of microbial virulence. The clinical expression of disease varies according to site, invasion and toxin production and is summarized in Table 4.6. Furthermore, host susceptibility to infection may be linked to genetic or acquired defects in host immunity that may complicate intercurrent infection, injury, ageing and metabolic disturbances (Table 4.7).
Table 4.6 Clinical conditions produced by Staphylococcus aureus
|
|
Table 4.7 Examples of host factors that increase susceptibility to staphylococcal infections (predominantly Staphylococcus aureus)
|
Foreign bodiesa |
Host response to infection
The natural host defences to infection are those of an intact surface epithelium with local production of secretions, antimicrobial enzymes (e.g. lysozyme in the eye) and in the stomach, gastric acidity. The mucociliary escalator of the large airways is unique to the lung.
Antibody and cell-mediated immune mechanisms play a vital role in combating infection. All organisms can initiate secondary immunological mechanisms, such as complement activation, immune complex formation and antibody-mediated cytolysis of cells. The immunological response to infection is described in Chapter 3.
Metabolic and immunological consequences of infection
Body temperature is controlled by the thermoregulatory centre in the anterior hypothalamus in the floor of the third ventricle. Body temperature is maintained at 36.8°C in health, with a diurnal variation of ±0.5°C. Gram-negative bacteria contain lipopolysaccharide (LPS) and peptidoglycan, which is also a component of Gram-positive bacterial cell walls. Toll-like receptors (TLR, see p. 55) on monocytes and dendritic cells recognize these lipopolysaccharides and generate signals leading to formation of inflammatory cytokines, e.g. IL-1, -6, -12, TNF-α and many others. These cytokines act on the thermoregulatory centre by increasing prostaglandin (PGE2) synthesis. The antipyretic effect of salicylates is brought about, at least in part, through its inhibitory effects on prostaglandin synthase.
Fever production has a positive effect on the course of infection. However, for every 1°C rise in temperature, there is a 13% increase in resting metabolic rate and oxygen consumption. Fever therefore, leads to increased energy requirements at a time when anorexia leads to decreased food intake. The normal compensatory mechanisms in starvation (e.g. mobilization of fat stores) are inhibited in acute infections. This leads to an increase in skeletal muscle breakdown, releasing amino acids, which, via gluconeogenesis, are used to provide energy.
The inflammatory response is a fundamental biological response to a variety of stimuli including microorganisms or their products, such as endotoxin which acts on monocytes and macrophages. Non-phagocytic cells (lymphocytes, natural killer cells) are also involved. The release of cytokines, notably TNF-α, IL-1, IL-6 and interferon-γ, leads to the release of a cascade of other mediators involved in inflammation and tissue remodelling, such as interleukins, prostaglandins, leukotrienes and corticotropin. TNF is therefore responsible for many of the effects of an infection.
The biological behaviour of the pathogen and the consequent host response are responsible for the clinical expression of disease that often allows clinical recognition. The incubation period following exposure can be helpful (e.g. chickenpox 14–21 days). The site and distribution of a rash may be diagnostic (e.g. shingles), while symptoms of cough, sputum and pleuritic pain point to lobar pneumonia. Fever and meningismus characterize classical meningitis. Infection may remain localized or become disseminated and give rise to the sepsis syndrome and disturbances of protein metabolism and acid–base balance (see Ch. 16). Many infections are self-limiting and immune and non-immune host defence mechanisms will eventually clear the pathogens. This is generally followed by tissue repair, which may result in complete resolution or leave residual damage.
FURTHER READING
Eltzschig HK, Carmeliet P. Hypoxia and inflammation. N Engl J Med 2011; 364:656–665.
Fey PD, Olson ME. Current concepts in biofilm formation of Staphylococcus epidermidis. Future Microbiol 2010; 5:917–933.
Lemichez E, Lecuit M, Nassif X et al. Breaking the wall: targeting of the endothelium by pathogenic bacteria. Nat Rev Microbiol 2010; 8:93–104.
Yahr TL. A critical new pathway for toxin secretion? N Engl J Med 2006; 355:1171–1172.
Approach to the patient with a suspected infection
Infectious diseases can affect any organ or system and can cause a wide variety of symptoms and signs. Fever is often regarded as the cardinal feature of infection, but not all febrile illnesses are infections and not all infectious diseases present with a fever. History-taking and examination should aim to identify the site(s) of infection and also the likely causative organism(s).
History
A detailed history is taken with specific questions about epidemiological risk factors for infection. These are based on the sources of infection and routes of transmission discussed above.
 Travel history: some diseases are more prevalent in certain geographical locations and many infections common in the tropics are seen rarely, if at all, in the UK.
Travel history: some diseases are more prevalent in certain geographical locations and many infections common in the tropics are seen rarely, if at all, in the UK.
 Food and water history: systemic as well as gastroenteric infections can be caught via this route.
Food and water history: systemic as well as gastroenteric infections can be caught via this route.
 Animal contact: domestic, farm and wild animals can all be responsible for zoonotic infection.
Animal contact: domestic, farm and wild animals can all be responsible for zoonotic infection.
 Sexual activity: as well as the traditional sexually transmitted diseases, HIV, hepatitis B and occasionally other blood-borne infections can be transmitted sexually. Some enteric infections are more common among men who have sex with men.
Sexual activity: as well as the traditional sexually transmitted diseases, HIV, hepatitis B and occasionally other blood-borne infections can be transmitted sexually. Some enteric infections are more common among men who have sex with men.
 Intravenous drug use: as well as blood-borne viruses, drug injectors are susceptible to a variety of bacterial and fungal infections due to inoculation. Other needle exposures, such as tattooing and body piercing and receipt of blood products (especially outside the UK), are also risk factors for blood-borne viruses.
Intravenous drug use: as well as blood-borne viruses, drug injectors are susceptible to a variety of bacterial and fungal infections due to inoculation. Other needle exposures, such as tattooing and body piercing and receipt of blood products (especially outside the UK), are also risk factors for blood-borne viruses.
 Leisure activities: certain pastimes may predispose to water-borne infections or zoonoses.
Leisure activities: certain pastimes may predispose to water-borne infections or zoonoses.
Clinical examination
A thorough examination covering all systems is required. Skin rashes and lymphadenopathy are common features of infectious diseases and the ears, eyes, mouth and throat should also be inspected. Infections commonly associated with a rash are listed in Box 4.1. Rectal, vaginal and penile examination is required in sexually transmitted infections. The fever pattern may occasionally be helpful, e.g. the tertian fever of falciparum malaria, but too much weight should not be placed on the pattern or degree.
![]() Box 4.1
Box 4.1
Infections commonly associated with a rash
Petechial/haemorrhagic
 Any septicaemia with disseminated intravascular coagulation (DIC)
Any septicaemia with disseminated intravascular coagulation (DIC)
 Viruses (see Table 4.23)
Viruses (see Table 4.23)
Investigations
In some infections, such as chickenpox, the clinical presentation is so distinctive that no investigations are normally necessary to confirm the diagnosis. Other cases require further tests to determine the cause and site of the infection.
General investigations (to assess health and identify organ(s) involved)
These will vary depending on circumstances:
 Blood tests. Routine blood count, ESR and C-reactive protein (CRP), biochemical profile, urea and electrolytes are performed in the majority of cases. CRP is a nonspecific marker of inflammation and is raised in many different infections: it is more useful in monitoring response to treatment than in making a diagnosis. Procalcitonin may be a more specific marker of bacterial infection, but this remains to be confirmed (Box 4.2).
Blood tests. Routine blood count, ESR and C-reactive protein (CRP), biochemical profile, urea and electrolytes are performed in the majority of cases. CRP is a nonspecific marker of inflammation and is raised in many different infections: it is more useful in monitoring response to treatment than in making a diagnosis. Procalcitonin may be a more specific marker of bacterial infection, but this remains to be confirmed (Box 4.2).
 Imaging. X-ray, ultrasound, echocardiography, CT and MR scanning are used to identify and localize infections. Positron emission tomography (PET) and single photon emission tomography (SPECT) have proved useful in localizing infection, especially when combined with CT scanning. However, the sensitivity and specificity of these tests in diagnosing infection has yet to be determined and their use remains limited. Biopsy or aspiration of tissue for microbiological examination may also be facilitated by ultrasound or CT guidance.
Imaging. X-ray, ultrasound, echocardiography, CT and MR scanning are used to identify and localize infections. Positron emission tomography (PET) and single photon emission tomography (SPECT) have proved useful in localizing infection, especially when combined with CT scanning. However, the sensitivity and specificity of these tests in diagnosing infection has yet to be determined and their use remains limited. Biopsy or aspiration of tissue for microbiological examination may also be facilitated by ultrasound or CT guidance.
 Radionuclide scanning after injection of indium- or technetium-labelled white cells (previously harvested from the patient) may occasionally help to localize infection. It is most effective when the peripheral white cell count is raised and is of particular value in localizing occult abscesses.
Radionuclide scanning after injection of indium- or technetium-labelled white cells (previously harvested from the patient) may occasionally help to localize infection. It is most effective when the peripheral white cell count is raised and is of particular value in localizing occult abscesses.
![]() Box 4.2
Box 4.2
General investigations for a patient with suspected infection
| Investigation | Possible cause |
|---|---|
Full blood count |
|
Neutrophilia |
Bacterial infection |
Neutropenia |
Viral infection |
|
Brucellosis |
|
Typhoid |
|
Typhus |
|
Overwhelming sepsis |
Lymphocytosis |
Viral infection |
Lymphopenia |
HIV infection (not specific) |
Atypical lymphocytes |
Infectious mononucleosis |
Eosinophilia |
Invasive parasitic infection |
Thrombocytopenia |
Overwhelming sepsis |
|
Malaria |
ESR or C-reactive protein |
Elevated in many infections |
Urea and electrolytes |
Potentially deranged in severe illness from any cause |
Procalcitonin |
Elevated particularly in bacterial infection |
Liver enzymes |
|
Minor elevation of transferases |
Nonspecific feature of many infections |
|
Mild viral hepatitis |
High transferases, elevated bilirubin |
Viral hepatitis (usually A, B or E) |
Coagulation |
May be deranged in hepatitis and in overwhelming infection of any type |
Microbiological investigations (to identify causative organism)
Diagnostic services range from simple microscopy to molecular probes. It is often helpful to discuss the clinical problem with a microbiologist to ensure that appropriate tests are performed and that specimens are collected and transported correctly.
Direct tests
Some microbiological tests rely on direct examination of a tissue specimen (e.g. blood, CSF or urine) for the presence of microorganisms. Microscopy and electron microscopy fall into this category. Other direct tests identify specific microbial components such as nucleic acids, cell wall molecules and other antigens. Specific genes from many pathogenic microorganisms have been cloned and sequenced.
Nucleic acid probes can be designed to detect these sequences, identifying pathogen-specific nucleic acid in body fluids or tissue. The use of nucleic acid amplification techniques (NAAT) such as the polymerase chain reaction (PCR) has increased the power of these tests to detect very small quantities of microbial material. Such techniques are not only exquisitely sensitive, but may also enable quantitation, e.g. viral load testing and sub-speciation, e.g. at the genotype level. However, the ability to detect tiny amounts of nucleic acid in a sample means that there is a significant potential for false-positive results due to contamination. This is less likely when looking for viral nucleic acid and it is in the area of virology that NAAT tests are most widely used. A recent development for bacterial identification is the introduction to clinical practice of PCR tools for amplifying bacterial ribosome 16S subunits. This allows ‘screening’ of clinical samples for a wide range of organisms, but because of the risk of contamination results must be interpreted carefully in the light of clinical findings.
Culture
Another way of ‘amplifying’ the yield of microorganisms to a detectable level is through culture. Culture techniques can be applied to a wide variety of bacteria, fungi and viruses. However, some organisms are difficult to grow and may require special culture media and conditions. Viruses are particularly difficult (and in many cases impossible) to culture in the laboratory.
Specimens to be sent for microscopy and culture (Box 4.3):
 Blood and urine should routinely be sent for bacterial culture if infection is suspected, regardless of whether fever is present at the time.
Blood and urine should routinely be sent for bacterial culture if infection is suspected, regardless of whether fever is present at the time.
 Cerebrospinal fluid, sputum and biopsy specimens are sent if clinically indicated.
Cerebrospinal fluid, sputum and biopsy specimens are sent if clinically indicated.
 Special culture techniques are required for fungi, mycobacteria and some other bacteria such as Brucella spp., and the laboratory must be informed if these are suspected.
Special culture techniques are required for fungi, mycobacteria and some other bacteria such as Brucella spp., and the laboratory must be informed if these are suspected.
 Faecal culture for viruses is not helpful in the investigation of gastroenteritis – the viruses responsible for this do not grow in routine tissue culture. Antigen or nucleic acid detection techniques (see below) are more appropriate, especially in the investigation of an outbreak of diarrhoea and vomiting. Protozoa should be considered as a cause of diarrhoea in returning travellers, immunocompromised patients, toddlers, men having sex with men, farm workers and in any cases of prolonged unexplained diarrhoea. Detection of a specific clostridial toxin is a more reliable test for diarrhoea caused by Clostridium difficile than culture of the organism itself. Stool culture is a costly routine test and is often requested unnecessarily.
Faecal culture for viruses is not helpful in the investigation of gastroenteritis – the viruses responsible for this do not grow in routine tissue culture. Antigen or nucleic acid detection techniques (see below) are more appropriate, especially in the investigation of an outbreak of diarrhoea and vomiting. Protozoa should be considered as a cause of diarrhoea in returning travellers, immunocompromised patients, toddlers, men having sex with men, farm workers and in any cases of prolonged unexplained diarrhoea. Detection of a specific clostridial toxin is a more reliable test for diarrhoea caused by Clostridium difficile than culture of the organism itself. Stool culture is a costly routine test and is often requested unnecessarily.
![]() Box 4.3
Box 4.3
Specimens and indications for microscopy, culture and other microbiological tests
| Specimen | Investigation | Indication |
|---|---|---|
Blood |
Giemsa stain for malaria |
Any symptomatic traveller returning from a malarious area |
Malaria antigen detection test |
||
Stains for other parasites |
Specific tropical infections |
|
Culture |
All suspected bacterial infections |
|
Urine |
Microscopy and culture |
All suspected bacterial infections |
Tuberculosis (TB) culture |
Suspected TB |
|
|
Unexplained leucocytes in urine |
|
NAAT |
STIs |
|
Faeces |
Microscopy ± iodine stain |
Suspected protozoal diarrhoea |
Culture |
All unexplained diarrhoea |
|
PCR/antigen detection (not usually necessary to do both) |
Suspected viral diarrhoea in children |
|
Clostridium difficile toxin |
Diarrhoea following hospital stay or antibiotic treatment |
|
Throat swabs |
Culture |
Suspected bacterial tonsillitis and pharyngitis |
PCR |
Viral meningitis |
|
PCR/antigen detection |
Viral respiratory infections where urgent diagnosis is considered necessary |
|
Sputum |
Microscopy and culture |
Unusual chest infections; pneumonia |
Auramine stain/TB culture (liquid culture, see p. 120) |
Suspected TB |
|
Other special stains/cultures |
Immunocompromised patients |
|
Cerebrospinal fluid |
Microscopy and culture |
Suspected meningitis |
Auramine stain/TB culture |
Suspected TB, meningitis |
|
Other special stains/cultures |
Immunocompromised patients |
|
Suspected fungal infections |
||
PCR |
Suspected encephalitis or viral or bacterial meningitis |
|
Rash aspirate: |
|
|
Petechial |
Microscopy and culture |
Meningococcal disease |
Vesicular |
PCR/antigen detection/viral culture |
Herpes simplex/zoster |
NAAT, nuclear acid amplification test; PCR, polymerase chain reaction; STI, sexually transmitted infection.
Immunodiagnostic tests
These can be divided into two types:
 Tests that detect microbial components, using a polyvalent antiserum or a monoclonal antibody
Tests that detect microbial components, using a polyvalent antiserum or a monoclonal antibody
 Tests that detect an antibody response to infection (serological tests).
Tests that detect an antibody response to infection (serological tests).
These investigations are valuable in the identification of organisms that are difficult to culture, especially viruses and fungi, and can also be helpful when antibiotics have been administered before samples were obtained. However, care is needed in the interpretation of serological tests. Elevated antibody titres on a single occasion (especially of IgG) are rarely diagnostic and in some infections it may be difficult to distinguish between past and acute infection. Paired serological tests a few weeks apart, or specific assays for IgM antibodies (indicating an acute infection), are more helpful. Avidity testing may also enable distinction between recent (low avidity antibodies) and historical (high avidity) infection. Numerous serological tests are available: they should only be used in the light of the clinical picture and not as a general ‘trawl’ for a diagnosis.
Treatment
Many infections, particularly those caused by viruses, are self-limiting and require no treatment. The mainstay of therapy for most infectious diseases that do require treatment is antimicrobial chemotherapy. The choice of antibiotic should be governed by:
Serious infections may require supportive therapy in addition to antibiotics. It is always preferable to have a definite microbial diagnosis before starting treatment, so that an antibiotic with the most appropriate spectrum of activity and site of action can be used. However, some patients are too unwell to wait for results (which in the case of culture may take days). In diseases such as meningitis or septicaemia delay in treatment may be fatal and therapy must be started on an empirical basis. Appropriate samples for culture should be taken before the first dose of antibiotic and an antibiotic regimen chosen on the basis of the most likely causative organisms. Usually patients are less unwell and specific therapy can be deferred pending results. (Antibiotic therapy is discussed in more detail on page 85.)
Returning travellers. A detailed travel itinerary, including any flight stopovers, should be taken from anyone who is unwell after arriving from another country. Previous travel should also be covered as some infections may be chronic or recurrent. It is necessary to find out not just which countries were visited but also the type of environment: a stay in a remote jungle village carries different health risks from a holiday in an air-conditioned coastal holiday resort. Food and water consumption, bathing and swimming habits, animal and insect contact and contact with human illness all need to be established. Enquiry should be made about sexual contacts, drug use and medical treatment (especially parenteral) while abroad. In some parts of the world, over 90% of professional sex workers are HIV-positive and hepatitis B and C are very common in parts of Africa and Asia. In addition to the investigations described in the previous section, special tests may be needed depending on the epidemiological risks and clinical signs and malaria films are mandatory in anyone who is unwell after being in a malarious area. Some of the more common causes of a febrile illness in returning travellers are listed in Table 4.8.
Table 4.8 Causes of febrile illness in travellers returning from the tropics and worldwide
WHO advises that fever occurring in a traveller 1 week or more after entering a malaria risk area and up to 3 months after departure is a medical emergency |
|
Developing countries |
Specific geographical areas (see text) |
Malaria |
Histoplasmosis |
Schistosomiasis |
Brucellosis |
Dengue |
Worldwide |
Tick typhus |
Influenza |
Typhoid |
Pneumonia |
Tuberculosis |
URTI |
Dysentery |
UTI |
Hepatitis A |
Traveller’s diarrhoea |
Amoebiasis |
Viral infection |
URTI, upper respiratory tract infection; UTI, urinary tract infection.
Immunocompromised patients. Advances in medical treatment over the past three decades have led to a huge increase in the number of patients living with immunodeficiency states. Cancer chemotherapy, the use of immunosuppressive drugs and the worldwide AIDS epidemic have all contributed to this. The presentation may be very atypical in the immunocompromised patient with few, if any, localizing signs or symptoms. Infection can be due to organisms which are not usually pathogenic, including environmental bacteria and fungi. The normal physiological responses to infection (e.g. fever, neutrophilia) may be diminished or absent. The onset of symptoms may be sudden and the course of the illness fulminant. A high index of suspicion for infections in people who are known to be immunosuppressed is required. These patients may need early and aggressive antibiotic therapy without waiting for the results of investigations. Samples for culture should be sent before starting treatment, but therapy should not be delayed if this proves difficult. The choice of antibiotics should be guided by the likely causative organisms: these are shown in Box 4.4.
![]() Box 4.4
Box 4.4
Common causes of infection in immunocompromised patients
| Deficiency | Causes | Organisms |
|---|---|---|
Neutropenia |
Chemotherapy |
Escherichia coli |
|
Myeloablative therapy |
Klebsiella pneumoniae |
|
Immunosuppressant drugs |
Staph. aureus |
|
|
Staph. epidermidis |
|
|
Aspergillus spp. |
|
|
Candida spp. |
Cellular immune defects |
HIV infection |
Respiratory syncytial virus |
|
Lymphoma |
Cytomegalovirus |
|
Myeloablative therapy |
Epstein–Barr virus |
|
Congenital syndromes |
Herpes simplex and zoster |
|
|
Salmonella spp. |
|
|
Mycobacterium spp. (esp. M. avium-intracellulare) |
|
|
Cryptococcus neoformans |
|
|
Candida spp. |
|
|
Cryptosporidium parvum |
|
|
Pneumocystis jiroveci |
|
|
Toxoplasma gondii |
Humoral immune deficiencies |
Congenital syndromes |
Haemophilus influenzae |
|
Chronic lymphocytic leukaemia |
Streptococcus pneumoniae |
|
Corticosteroids |
Enteroviruses |
Terminal complement deficiencies (C5–C9) |
Congenital syndromes |
Neisseria meningitidis |
|
|
N. gonorrhoeae |
Splenectomy |
Surgery |
Strep. pneumoniae |
|
Trauma |
N. meningitidis |
|
|
H. influenzae |
|
|
Malaria |
Injecting drug users. Parenteral drug use is associated with a variety of local and systemic infections. HIV, HBV and HCV can all be transmitted by sharing injecting equipment. Abscesses and soft tissue infections at the site of injection are common, especially in the groin, and may involve adjacent vascular and bony structures. Systemic infections are also common, most frequently caused by staphylococci and group A streptococci, but a wide variety of other bacterial and fungal pathogens may be implicated.
Highly transmissible infections. Relatively few patients with infectious disease present a serious risk to healthcare workers (HCW) and other contacts. However, the appearance of diseases like the ‘new’ strains of influenza (such as H5N1 avian influenza and pandemic H1N1), the occasional importation of zoonoses like Lassa fever and concerns about the bioterrorist use of agents such as smallpox mean that there is still the potential for unexpected outbreaks of life-threatening disease. During the worldwide SARS outbreak in 2003, scrupulous infection control procedures reduced spread of infection. However, in the ‘inter-epidemic’ period it is difficult to maintain the same level of alert. HCWs should remain vigilant because the early symptoms of many of these diseases are nonspecific. Many HCWs are developing multi-resistant TB from HIV patients with resistant TB organisms, which is becoming a very significant problem in Africa.
Pyrexia of unknown origin
History, clinical examination and simple investigation will reveal the cause of a fever in most patients. In a small number, however, no diagnosis is apparent despite continuing symptoms. The term pyrexia (or fever) of unknown origin (PUO) is sometimes used to describe this problem. Various definitions have been suggested for PUO: a useful one is ‘a fever persisting for >2 weeks, with no clear diagnosis despite intelligent and intensive investigation’. Patients who are known to have HIV or other immunosuppressing conditions are normally excluded from the definition of PUO, as the investigation and management of these patients is different.
Successful diagnosis of the cause of PUO depends on knowledge of the likely and possible aetiologies. These have been documented in a number of studies and are summarized in Box 4.5.
A detailed history and examination is essential, taking into account the possible causes, and the examination should be repeated on a regular basis in case new signs appear. Investigation findings to date should be reviewed, obvious omissions amended and abnormalities followed up. Confirm that the patient does have objective evidence of a raised temperature: this may require admission to hospital if the patient is not already under observation. Some people have an exaggerated circadian temperature variation (usually peaking in the evening), which is not pathological.
The range of tests available is discussed above. Obviously investigation is guided by particular abnormalities on examination or initial test results, but in some cases ‘blind’ investigation is necessary. Some investigations, especially cultures, should be repeated regularly and serial monitoring of inflammatory markers such as C-reactive protein allows assessment of progress.
Improvements in imaging techniques have diminished the need for invasive investigations in PUO and scanning has superseded the blind diagnostic laparotomy. Ultrasound, echocardiography, CT, MRI, PET and labelled white cell scanning can all help in establishing a diagnosis if used appropriately: the temptation to scan all patients with PUO from head to toe as a first measure should be avoided. Biopsy of bone marrow (and less frequently liver) may be useful even in the absence of obvious abnormalities and temporal artery biopsy should be considered in the elderly (see p. 543). Bronchoscopy can be used to obtain samples for microbiological and histological examination if sputum specimens are not adequate. Molecular and serological tests have greatly improved the diagnosis of infectious causes of PUO, but these tests should only be ordered and interpreted in the context of the clinical findings and epidemiology.
Treatment of a patient with a persistent fever is aimed at the underlying cause and if possible only symptomatic treatment should be used until a diagnosis is made. Blind antibiotic therapy may make diagnosis of an occult infection more difficult and empirical steroid therapy may mask an inflammatory response without treating the underlying cause. In a few patients no cause for the fever is found despite many months of investigation and follow-up. In most of these the symptoms do eventually settle spontaneously and if no definite cause has been identified after 2 years, the long-term prognosis is good.
SIGNIFICANT WEBSITE
Non-commercial advice on available laboratory tests. http://www.labtestsonline.org.uk/
Antimicrobial chemotherapy
Principles of use
Antibiotics are among the safest of drugs, especially those used to treat community infections. They have had a major impact on the life-threatening infections and reduce the morbidity associated with surgery and many common infectious diseases. This in turn is, in part, responsible for the overprescribing of these agents which has led to concerns with regard to the increasing incidence of antibiotic resistance.
Most antibiotic prescribing, especially in the community, is empirical. Even in hospital practice, microbiological documentation of the nature of an infection and the susceptibility of the pathogen is generally not available for a day or two. Initial choice of therapy relies on a clinical diagnosis and, in turn, a presumptive microbiological diagnosis. Such ‘blind therapy’ is directed at the most likely pathogen(s) responsible for a particular syndrome such as meningitis, urinary tract infection, or pneumonia. Examples of ‘blind therapy’ for these three conditions are ceftriaxone, trimethoprim and amoxicillin (± macrolide), respectively. Initial therapy in the severely ill patient is often broad spectrum in order to cover the range of possible pathogens but should be targeted once microbiological information becomes available. In patients with less severe infections a narrower-spectrum agent can be used from the outset while awaiting culture results, as the potential consequences of initial inadequate coverage are less serious.
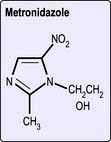
Combinations of drugs are occasionally required for reasons other than providing broad-spectrum cover. Tuberculosis is initially treated with three or four agents to avoid resistance emerging. Synergistic inhibition is achieved by using penicillin and gentamicin in enterococcal endocarditis or gentamicin and ceftazidime in life-threatening pseudomonas infection.
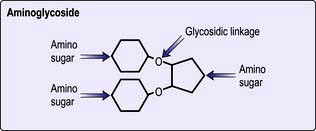
In the majority of infections, there is no firm evidence that bactericidal drugs (penicillins, cephalosporins, aminoglycosides) are more effective than bacteriostatic drugs (tetracyclines), but it is generally considered better to use the former in the treatment of bacterial endocarditis and in patients in whom host defence mechanisms are compromised, particularly in those with neutropenia.
Pharmacokinetic factors
To be successful, sufficient antibiotic must penetrate to the site of the infection. Knowledge of the standard pharmacokinetic considerations of absorption, distribution, metabolism and excretion for the various drugs is required. Difficult sites include the brain, eye and prostate, while loculated abscesses are inaccessible to most agents.
Many mild-to-moderate infections can be treated effectively with oral antibiotics provided that the patient is compliant. Parenteral administration is indicated in the severely ill patient to ensure rapid high and/or consistent blood and tissue concentrations of drug. Some antibiotics can only be administered parenterally, such as the aminoglycosides and extended-spectrum cephalosporins. Parenteral therapy is also required in those unable to swallow or where gastrointestinal absorption is unreliable.
Dose and duration of therapy
This will vary according to the nature, severity and response to therapy. The need to completely clear the infection must be balanced against the undesired effects of prolonged antibiotic therapy (e.g. promotion of antimicrobial resistance, drug toxicity, superinfection with organisms such as Candida spp. or Clostridium difficile and cost). For many infections 5–7 days of treatment is adequate, while for some (e.g. uncomplicated urinary tract infections and some forms of bacterial gastroenteritis) 1–3 days may be enough. However, other infections may require much longer: bacterial endocarditis normally needs 4–6 weeks, bone and prosthetic joint infections often need 12 weeks and mycobacterial infections require months or even years of therapy. In a few conditions such as HIV or chronic hepatitis B infection treatment is suppressive rather than curative so lifelong antimicrobial treatment is needed. Even within a course of treatment it may be possible to simplify or streamline therapy, e.g. change from intravenous to oral or from broad spectrum to narrow spectrum, as the patient improves.
FURTHER READING
McDonald LC. Trends in antimicrobial resistance in healthcare associated pathogens and effect on treatment. Clin Infect Dis 2006; 42: S65–S71.
Moellering RC Jr. NDM-1 – a cause for worldwide concern. N Engl J Med 2010; 363:2377–2379.
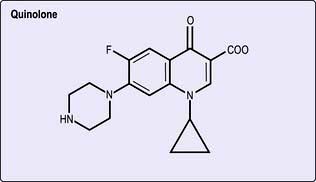
Robicsek A, Jacoby GA, Hooper DC. The worldwide emergence of plasmid-mediated quinolone resistance. Lancet Infect Dis 2006; 6:629–640.
Renal and hepatic insufficiency
Patients with renal impairment may require reduction in dose or increased dosing interval in order to avoid toxic accumulation of antibiotic. This applies to the β-lactams and especially the aminoglycosides and vancomycin. In those with hepatic insufficiency, dose reduction is often required for agents which rely on extensive hepatic metabolism for excretion. A full list of such drugs can be found in the British National Formulary (BNF).
Therapeutic drug monitoring
To ensure therapeutic yet non-toxic drug concentrations, serum concentrations of drugs such as the aminoglycosides and vancomycin should be monitored, especially in those with impaired or changing renal function. Specific monitoring algorithms are available for such drugs (general guidance is provided in the BNF, but local guidelines should be followed wherever possible).
Antibiotic chemoprophylaxis
The value of antibiotic chemoprophylaxis has been questioned as there are few controlled trials to prove efficacy (see p. 708). The evidence for chemoprophylaxis against infective endocarditis (IE) is an example. New English guidelines recognize that procedures can cause bacteraemia but without significant risk of infective endocarditis. Even patients at ‘high risk’, e.g. previous IE, prosthetic heart valves and surgical shunts, do not always require prophylaxis (Table 4.9). However, there are a number of indications for which the prophylactic use of antibiotics is still advised. These include surgical procedures where the risk of infection is high (colon surgery) or the consequences of infection are serious (post-splenectomy sepsis). The choice of agent(s) is determined by the likely infectious risk and the established efficacy and safety of the regimen.
Table 4.9 Antibiotic chemoprophylaxis
(a) General |
||
Clinical problem |
Aim |
Drug regimena |
Splenectomy/spleen malfunction |
To prevent serious pneumococcal sepsis |
Phenoxymethylpenicillin 500 mg 12-hourly |
Rheumatic fever |
To prevent recurrence and further cardiac damage |
Phenoxymethylpenicillin 250 mg × 2 daily or sulfadiazine 1 g if allergic to penicillin |
Meningitis: |
|
|
Due to meningococci |
To prevent infection in close contacts |
Adults: rifampicin 600 mg twice-daily for 2 days |
Due to H. influenzae type b |
To reduce nasopharyngeal carriage and prevent infection in close contacts |
Adults: rifampicin 600 mg daily for 4 days |
Tuberculosis |
To prevent infection in exposed (close contacts) tuberculin-negative individuals, infants of infected mothers and immunosuppressed patients |
Oral isoniazid 300 mg daily for 6 months (Children: 5–10 mg/kg daily) |
(b) Endocarditis (NICE guidelines for adults and children undergoing interventional procedures March 2008) |
||
Antibacterial prophylaxis and chlorhexidine mouthwash are not recommended for the prevention of endocarditis in patients undergoing dental procedures. |
||
Antibacterial prophylaxis is not recommended for the prevention of endocarditis in patients undergoing procedures of the: |
||
Upper and lower respiratory tract (including ear, nose and throat procedures and bronchoscopy) |
||
Genitourinary tract (including urological, gynaecological and obstetric procedures) |
||
Upper and lower gastrointestinal tract. |
||
Any infection in patients at risk of endocarditis should be investigated promptly and treated appropriately to reduce the risk of endocarditis. |
||
If patients at risk of endocarditis are undergoing a gastrointestinal or genitourinary tract procedure at a site where infection is suspected, they should receive appropriate antibacterial therapy that includes cover against organisms that cause endocarditis. |
||
Patients at risk of endocarditis should be: |
||
Advised to maintain good oral hygiene |
||
Told how to recognize signs of infective endocarditis and advised when to seek expert advice. |
||
a Unless stated, doses are those recommended in adults. For surgical procedure, see individual procedures in text.
Adapted from Joint Formulary Committee British National Formulary, 63rd edn. London: BMJ Group and RPS Publishing; 2012.
Mechanisms of action and resistance to antimicrobial agents
Antibiotics act at different sites of the bacterium, either inhibiting essential steps in metabolism or assembly or destroying vital components such as the cell wall.
Resistance to an antibiotic can be the result of:
 Impaired or altered permeability of the bacterial cell envelope, e.g. penicillins in Gram-negative bacteria
Impaired or altered permeability of the bacterial cell envelope, e.g. penicillins in Gram-negative bacteria
 Active expulsion from the cell by membrane efflux systems
Active expulsion from the cell by membrane efflux systems
 Alteration of the target site (e.g. single point mutations in E. coli or a penicillin-binding protein in Strep. pneumoniae leading to acquired resistance, see below)
Alteration of the target site (e.g. single point mutations in E. coli or a penicillin-binding protein in Strep. pneumoniae leading to acquired resistance, see below)
 Specific enzymes which inactivate the drug before or after cell entry (e.g. β-lactamases)
Specific enzymes which inactivate the drug before or after cell entry (e.g. β-lactamases)
The development or acquisition of resistance to an antibiotic by bacteria involves either a mutation at a single point in a gene or transfer of genetic material from another organism (Fig. 4.4).
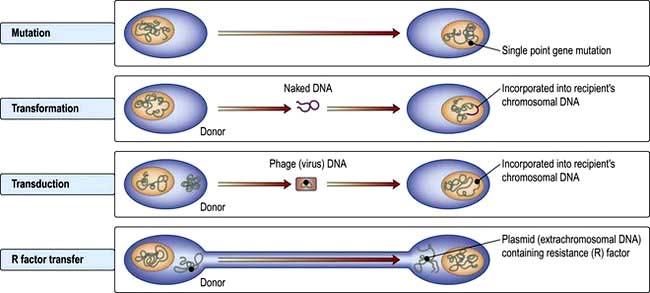
Figure 4.4 Some mechanisms for the development of resistance to antimicrobial drugs. These involve either a single point mutation or transfer of genetic material from another organism (transformation, transduction or R factor transfer).
Larger fragments of DNA may be introduced into a bacterium either by transfer of ‘naked’ DNA or via a bacteriophage (a virus) DNA vector. Both the former (transformation) and the latter (transduction) are dependent on integration of this new DNA into the recipient chromosomal DNA. This requires a high degree of homology between the donor and recipient chromosomal DNA.
Finally, antibiotic resistance can be transferred from one bacterium to another by conjugation, when extrachromosomal DNA (a plasmid) containing the resistance factor (R factor) is passed from one cell into another during direct contact. Transfer of such R factor plasmids can occur between unrelated bacterial strains and involve large amounts of DNA and often codes for multiple antibiotic resistance, e.g. as for the quinolones.
Transformation is probably the least clinically relevant mechanism, whereas transduction and R factor transfer are usually responsible for the sudden emergence of multiple antibiotic resistance in a single bacterium. Increasing resistance to many antibiotics has developed (Table 4.10).
Table 4.10 Some bacteria that have developed resistance to common antibiotics
| Pathogen | Previously fully sensitive to: |
|---|---|
Enterobacteria |
Amoxicillin, trimethoprim, ciprofloxacin, gentamicin, glycopeptide (GRE), vancomycin (VRE) |
Helicobacter pylori |
Metronidazole, clarithromycin |
Haemophilus influenzae |
Amoxicillin, chloramphenicol |
E. coli |
Quinolones |
Neisseria gonorrhoeae |
Penicillin, ciprofloxacin |
Pseudomonas aeruginosa |
Gentamicin |
Salmonella spp. |
Amoxicillin, sulphonamides, ciprofloxacin |
Shigella spp. |
Amoxicillin, trimethoprim, tetracycline |
Staphylococcus aureus |
Penicillin, meticillin (MRSA), vancomycin (VRSA), ciprofloxacin |
Streptococcus pneumoniae |
Penicillin, erythromycin, cefotaxime |
Streptococcus pyogenes |
Erythromycin, tetracycline |
Vibrio cholerae |
Quinolones, azithromycin |
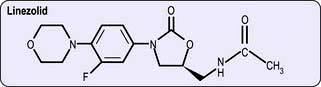
Antibacterial drugs
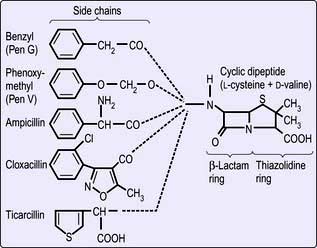
β-Lactams (penicillins, cephalosporins and monobactams)
Penicillins
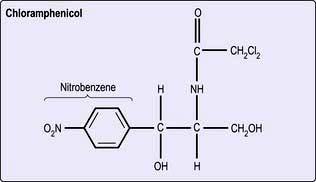
Structure. The β-lactams share a common ring structure (Fig. 4.5). Changes to the side-chain of benzylpenicillin (penicillin G) render the phenoxymethyl derivative (penicillin V) acid resistant and allow it to be orally absorbed. The presence of an amino group in the phenyl radical of benzylpenicillin increases its antimicrobial spectrum to include many Gram-negative and Gram-positive organisms. More extensive modification of the side-chain (e.g. as in flucloxacillin) renders the drug insensitive to bacterial penicillinase. This is useful in treating infections caused by penicillinase (β-lactamase)-producing staphylococci.
Mechanisms of action. β-lactams block bacterial cell wall mucopeptide formation by binding to and inactivating specific penicillin-binding proteins (PBPs), which are peptidases involved in the final stages of cell wall assembly and division. Meticillin-resistant Staph. aureus (MRSA) (see p. 115) produce a low-affinity PBP which retains its peptidase activity even in the presence of high concentrations of meticillin. Many bacteria have developed the ability to produce penicillinases and beta-lactamases, which inactivate antibiotics of this class. Recent years have seen the emergence of Gram-negative organisms producing extended-spectrum beta-lactamases (ESBLs), rendering the bacteria potentially resistant to all β-lactam antibiotics.
Indications for use. Benzylpenicillin can only be given parenterally and is still the drug of choice for some serious infections. However due to increasing antimicrobial resistance it should not be used as monotherapy in serious infections without laboratory confirmation that the organism is penicillin sensitive. Uses include serious streptococcal infections (including infective endocarditis), necrotizing fasciitis and gas gangrene, actinomycosis, anthrax and spirochaetal infections (syphilis, yaws).
Phenoxymethylpenicillin (penicillin V) is an oral preparation that is used chiefly to treat streptococcal pharyngitis and as prophylaxis against rheumatic fever.
Flucloxacillin is used in infections caused by β-lactamase (penicillinase)-producing staphylococci and remains the drug of choice for serious infections caused by meticillin-sensitive S. aureus (MSSA).
Ampicillin is susceptible to β-lactamase, but its antimicrobial activity includes streptococci, pneumococci and enterococci as well as Gram-negative organisms such as Salmonella spp., Shigella spp., E. coli, H. influenzae and Proteus spp. Drug resistance has, however, eroded its efficacy against these Gram-negatives. It is widely used in the treatment of respiratory tract infections. Amoxicillin has similar activity to ampicillin, but is better absorbed when given by mouth.
The extended-spectrum penicillin, ticarcillin, is active against pseudomonas infections, as is the acylureidopenicillin piperacillin in combination with sulbactam.
Clavulanic acid is a powerful inhibitor of many bacterial β-lactamases and when given in combination with an otherwise effective agent such as amoxicillin (co-amoxiclav) or ticarcillin can broaden the spectrum of activity of the drug. Sulbactam acts similarly and is available combined with ampicillin, while tazobactam in combination with piperacillin is effective in appendicitis, peritonitis, pelvic inflammatory disease and complicated skin infections. The penicillin β-lactamase combinations are also active against β-lactamase-producing staphylococci.
Pivmecillinam has significant activity against Gram-negative bacteria including E. coli, Klebsiella, Enterobacter and Salmonella but not against Pseudomonas.
Temocillin is active against Gram-negative bacteria, including β-lactamase producers. It is not active against Pseudomonas or Acinetobacter spp.
Interactions. Penicillins inactivate aminoglycosides when mixed in the same solution.
Toxicity. Generally, the penicillins are very safe. Hypersensitivity (skin rash (common), urticaria, anaphylaxis), encephalopathy and tubulointerstitial nephritis can occur. Ampicillin also produces a hypersensitivity rash in approximately 90% of patients with infectious mononucleosis who receive this drug. Co-amoxiclav causes a cholestatic jaundice six times more frequently than amoxicillin, as does flucloxacillin.
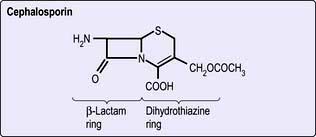
Cephalosporins
The cephalosporins (Fig. 4.6) have an advantage over the penicillins in that they are resistant to staphylococcal penicillinases (but are still inactive against meticillin-resistant staphylococci) and have a broader range of activity that includes both Gram-negative and Gram-positive organisms, but excludes enterococci and anaerobic bacteria. Ceftazidime and cefpirome are active against Pseudomonas aeruginosa.
Indications for use (Table 4.11). These potent broad-spectrum antibiotics are useful for the treatment of serious systemic infections, particularly when the precise nature of the infection is unknown. They may be used for serious sepsis in postoperative and immunocompromised patients, as well as for meningitis and intra-abdominal sepsis, but are increasingly being replaced by other agents because of their link with Clostridium difficile associated diarrhea (CDAD).
Table 4.11 Some examples of cephalosporins
| Activity | Use | |
|---|---|---|
First generation |
Gram-positive cocci and Gram-negative organisms |
Urinary tract infections |
Cefalexin (oral) |
|
Penicillin allergy |
Cefradine (oral) |
|
|
Cefadroxil (oral) |
|
|
Second generation |
Extended spectrum |
Prophylaxis and treatment of Gram-negative infections and mixed aerobic-anaerobic infections |
Cefuroxime |
More effective than first generation against E. coli, Klebsiella spp. and Proteus mirabilis, but less effective against Gram-positive organisms |
|
Cefoxitina |
Includes Bacteroides fragilis |
Peritonitis |
Cefaclor (oral) |
|
|
Cefuroxime (oral) |
|
|
Cefprozil (oral)a |
|
|
Third generation |
|
|
Cefotaxime |
Broad-spectrum |
Especially severe infection with Enterobacteriaceae, Pseudomonas aeruginosa (ceftazidime, cefpirome) and Neisseria gonorrhoeae, N. meningitidis, Lyme disease (ceftriaxone) |
Ceftazidime |
More potent against aerobic Gram-negative bacteria than first or second generation |
|
Cefpiromea |
|
Urinary tract infections and infections with neutropenia |
Ceftriaxone |
|
Once daily. Septicaemia, pneumonia, meningitis |
Cefpodoxime (oral) |
|
|
Cefixime (oral) |
|
|
Fourth generation |
Aerobic Gram-negative bacteria including P. aeruginosa |
Febrile, neutropenic patients |
Cefepimea |
|
|
Fifth generation |
Similar to third generation but active against MRSA |
Not yet in widespread use |
Ceftarolinea |
|
|
Ceftobiprolea |
|
|
Interactions. There are relatively few interactions.
Toxicity. The toxicity is similar to that of the penicillins but is less common. Some 10% of patients are allergic to both groups of drugs. The early cephalosporins caused proximal tubule damage, although the newer derivatives have fewer nephrotoxic effects. Second and third generation cephalosporins are strongly associated with CDAD and alternative antibiotics should be used when possible.
Monobactams
Aztreonam is currently the only member of this class available. It is a synthetic β-lactam and, unlike the penicillins and cephalosporins, has no ring other than the β-lactam, hence its description as a monobactam.
Its mechanism of action is by inhibition of bacterial cell wall synthesis. It is resistant to most β-lactamases and does not induce β-lactamase production.
Indications for use. Aztreonam’s spectrum of activity is limited to aerobic Gram-negative bacilli. It is a useful alternative to aminoglycosides in combination therapy, largely for the treatment of intra-abdominal sepsis, and is also used in pseudomonas infection (including lung infection in cystic fibrosis).
Carbapenems
The carbapenems are semisynthetic β-lactams and include imipenem, meropenem, doripenem and ertapenem. They are currently the broadest spectrum of antibiotics, being active against the majority of Gram-positive and Gram-negative as well as anaerobic bacterial pathogens. Ertapenem, unlike the others, is not active against Pseudomonas or Acinetobacter spp. They differ in their dosage and frequency of administration. Imipenem is partially inactivated in the kidney by enzymatic inactivation and is therefore administered in combination with cilastatin.
Indications for use. They are used for serious nosocomial infections when multiple-resistant Gram-negative bacilli or mixed aerobe and anaerobe infections are suspected.
Toxicity. This is similar to that of β-lactam antibiotics. Nausea, vomiting and diarrhoea occur in less than 5% of cases. Imipenem may cause seizures and should not be used to treat meningitis; meropenem is safe for this indication.
Aminoglycosides
Structure. These antibiotics are polycationic compounds of amino sugars (Fig. 4.7).
Mechanism of action. Aminoglycosides interrupt bacterial protein synthesis by inhibiting ribosomal function (messenger and transfer RNA).
Indications for use. Streptomycin is bactericidal and is rarely used except for the treatment of tularaemia or plague. Neomycin is used only for the topical treatment of eye and skin infections. Even though it is poorly absorbed, prolonged oral administration can produce ototoxicity.
Gentamicin and tobramycin are given parenterally. They are highly effective against many Gram-negative organisms including Pseudomonas spp. They are synergistic with a penicillin against Enterococcus spp. Netilmicin and amikacin have a similar spectrum but are more resistant to the amino-glycoside-inactivating enzymes (phosphorylating, adenylating or acetylating) produced by some bacteria. Their use should be restricted to gentamicin-resistant organisms.
Interactions. Enhanced nephrotoxicity occurs with other nephrotoxic drugs, ototoxicity with some diuretics and neuromuscular blockade with curariform drugs.
Toxicity. This is dose-related. Aminoglycosides are nephrotoxic and ototoxic (vestibular and auditory), particularly in the elderly. Therapeutic drug monitoring is necessary in ensuring therapeutic and non-toxic drug concentrations.
Tetracyclines and glycylcyclines
Structure. These are bacteriostatic drugs possessing a four-ring hydronaphthacene nucleus (Fig. 4.8). Included among the tetracyclines are tetracycline, oxytetracycline, demeclocycline, lymecycline, doxycycline and minocycline. Tigecycline is an injectable glycylcycline, which is structurally related to the tetracyclines.
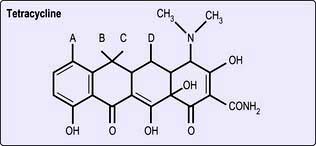
Figure 4.8 The structure of a tetracycline. Substitution of CH3, OH or H at positions A–D produces variants of tetracycline.
Mechanism of action. Tetracyclines inhibit bacterial protein synthesis by interrupting ribosomal function (transfer RNA).
Indications for use. Tetracyclines are active against Gram-positive and Gram-negative bacteria but their use is limited, partly owing to increasing bacterial resistance Tetracyclines are active against V. cholerae, Rickettsia spp., Mycoplasma spp., Coxiella burnetii, Chlamydia spp. and Brucella spp.
Tigecycline, the only currently available glycylcycline, is active against many organisms resistant to tetracycline and other antibiotics. This includes vancomycin-resistant enterococci, MRSA and multidrug-resistant Gram-negative bacilli including Acinetobacter spp. Its indications include complicated skin and soft tissue infections and intra-abdominal sepsis. However a recent FDA alert has raised concern about the efficacy of tigecycline in some serious infections (notably ventilator-associated pneumonia, VAP) and it should be used only on expert advice.
Interactions. The efficacy of tetracyclines is reduced by antacids and oral iron-replacement therapy.
Toxicity. Tetracyclines are generally safe drugs, but they may enhance established or incipient renal failure, although doxycycline is safer than others in this group. They cause brown discoloration of growing teeth and thus these drugs are not given to children or pregnant women. Photosensitivity can occur. Nausea and vomiting are the most frequent adverse effects of tigecycline.
Macrolides
Erythromycin and clarithromycin
Structure. Erythromycin and clarithromycin both consist of a lactone ring with two sugar side-chains, one of which is an aminosugar.
Mechanism of action. Macrolides inhibit protein synthesis by interrupting ribosomal function.
Indications for use. Erythromycin has a similar (but not identical) antibacterial spectrum to penicillin and may be useful in individuals with penicillin allergy, especially in the management of bacterial respiratory infections. It can be given orally or parenterally, but oral intake is associated with significant gastrointestinal side-effects, while the i.v. formulation is very irritant and causes phlebitis. For these reasons, clarithromycin (which has similar antimicrobial properties but fewer side-effects) is often preferred. These drugs are the preferred agent in the treatment of pneumonias caused by Legionella spp. and Mycoplasma spp. They are also effective in the treatment of infections due to Bordetella pertussis (whooping cough), Campylobacter spp. and Chlamydia spp.
Other macrolides
These include azithromycin and telithromycin. They have a broad spectrum of activity that includes selective Gram-negative organisms, mycobacteria and Toxoplasma gondii. Compared with erythromycin, they have superior pharmacokinetic properties with enhanced tissue and intracellular penetration and longer half-life that allows once daily dosage. Azithromycin is also used for trachoma and cholera (see p. 136). Fidaxomicin is useful in C. difficile.
Interactions. Erythromycin and other macrolides interact with theophyllines, carbamazepine, digoxin and ciclosporin, occasionally necessitating dose adjustment of these agents.
Toxicity. Diarrhoea, vomiting and abdominal pain are the main side-effects of erythromycin (less with clarithromycin and azithromycin) and are, in part, a consequence of the intestinal prokinetic properties of the macrolides. Macrolides may also rarely produce cholestatic jaundice after prolonged treatment. QTc prolongation is a recognized cardiac effect of the macrolides. This may have serious consequences if the syndrome of ‘torsades de pointes’ is induced.
Chloramphenicol
Structure. Chloramphenicol is the only naturally occurring antibiotic containing nitrobenzene (Fig. 4.9). This structure probably accounts for its toxicity in humans and for its activity against bacteria.
Mechanism of action. Chloramphenicol competes with messenger RNA for ribosomal binding. It also inhibits peptidyl transferase.
Indications for use. Chloramphenicol is now little used in developed countries, although it remains an effective and useful antibiotic in some situations. In developing countries, it has been invaluable in the treatment of meningitis and severe infections caused by Salmonella typhi and S. paratyphi (enteric fevers) and is also active against H. influenzae (meningitis and acute epiglottitis) and Yersinia pestis (plague). It is used topically for the treatment of purulent conjunctivitis. Drug resistance is currently eroding the efficacy of chloramphenicol.
Interactions. Chloramphenicol enhances the activity of anticoagulants, phenytoin and some oral hypoglycaemic agents.
Toxicity. Severe irreversible bone marrow suppression is rare but nevertheless now restricts the usage of this drug where alternatives exist. Chloramphenicol should not be given to premature infants or neonates because of their inability to conjugate and excrete this drug; high blood levels lead to circulatory collapse and the often fatal ‘grey baby syndrome’.
Sodium fusidate
Structure. Sodium fusidate has a structure resembling that of bile salts (see p. 78).
Mechanism of action. It is a potent inhibitor of bacterial protein synthesis. Its entry into cells is facilitated by the detergent properties inherent in its structure.
Indications for use. Sodium fusidate is mainly used for penicillinase-producing Staph. aureus infections such as osteomyelitis (it is well concentrated in bone) or endocarditis and for other staphylococcal infections accompanied by septicaemia. The drug is well absorbed orally (i.v. preparations are also available) but is relatively expensive and should be used in combination with another staphylococcal agent to prevent resistance emerging.
Resistance. Resistance may occur rapidly and is the reason why sodium fusidate is given in combination with another antibiotic.
Toxicity. Sodium fusidate may occasionally be hepatotoxic but is generally a safe drug and if necessary can be given during pregnancy.
Sulphonamides and trimethoprim
Structure. The sulphonamides are all derivatives of the prototype sulphanilamide. Trimethoprim is a 2,4-diaminopyrimidine.
Mechanism of action. Sulphonamides block thymidine and purine synthesis by inhibiting microbial folic acid synthesis. Trimethoprim prevents the reduction of dihydrofolate to tetrahydrofolate (see Fig. 8.12).
Indications for use. Sulfamethoxazole is mainly used in combination with trimethoprim (as co-trimoxazole). Its use is now largely restricted to the treatment and prevention of Pneumocystis jiroveci infection and listeriosis in developed countries, although it is still in widespread use in developing countries. It may also be used for toxoplasmosis and nocardiosis and as a second-line agent in acute exacerbations of chronic bronchitis and in urinary tract infections. Trimethoprim alone is often used for urinary tract infections and acute-on-chronic bronchitis, as the side-effects of co-trimoxazole are most commonly due to the sulphonamide component. Sulfapyridine in combination with 5-aminosalicylic acid (i.e. sulfasalazine) is now less widely used in inflammatory bowel disease.
Resistance. Resistance to sulphonamides is often plasmid-mediated and results from the production of sulphonamide-resistant dihydropteroate synthase from altered bacterial cell permeability to these agents.
Interactions. Sulphonamides potentiate oral anticoagulants and some hypoglycaemic agents.
Toxicity. Sulphonamides cause a variety of skin eruptions, including toxic epidermal necrolysis, the Stevens–Johnson syndrome, thrombocytopenia, folate deficiency and megaloblastic anaemia with prolonged usage. It can provoke haemolysis in individuals with glucose-6-phosphate dehydrogenase deficiency and therefore should not be used in such people.
Quinolones
The quinolone antibiotics, such as ciprofloxacin, norfloxacin, ofloxacin and levofloxacin, are useful oral broad-spectrum antibiotics, related structurally to nalidixic acid. The latter achieves only low serum concentrations after oral administration and its use is limited to the urinary tract where it is concentrated. Newer quinolones, including moxifloxacin, gemifloxacin and gatifloxacin, have greater activity against Gram-positive pathogens. The structure is shown in Figure 4.10.
Mechanism of action. The quinolone group of bactericidal drugs inhibits bacterial DNA synthesis by inhibiting topoisomerase IV and DNA gyrase, the enzyme responsible for maintaining the superhelical twists in DNA.
Indications for use. The extended-spectrum quinolones such as ciprofloxacin have activity against Gram-negative bacteria, including some Pseudomonas aeruginosa and some Gram-positive bacteria (e.g. anthrax, p. 132). They are useful in Gram-negative septicaemia, skin and bone infections, urinary and respiratory tract infections, meningococcal carriage, in some sexually transmitted diseases such as gonorrhoea and nonspecific urethritis due to Chlamydia trachomatis and in severe cases of travellers’ diarrhoea (see p. 122). The newer oral quinolones provide an alternative to β-lactams in the treatment of community-acquired lower respiratory tract infections.
Resistance. In many countries 30–40% of E. coli are resistant. Resistance is also a growing problem among Salmonella, Vibrio cholerae and Staphylococcus aureus, including MRSA strains.
Interactions. Ciprofloxacin can induce toxic concentrations of theophylline.
Toxicity. Gastrointestinal disturbances, photosensitive rashes and occasional neurotoxicity can occur. Avoid in childhood and pregnancy and in patients taking corticosteroids. Tendon damage, including rupture, can occur within 48 h of use and the drug should be stopped immediately; it should not be used in patients with tendonitis. MRSA and Clostridium difficile infection in hospitals have been linked to high prescribing rates of quinolones and use is now discouraged where an effective alternative is available.
Oxazolidinones
Structure. The oxazolidinones are a novel class of antibacterial agents, of which linezolid (Fig. 4.11) is the first to be available.
Mechanism of action. The oxazolidinones inhibit protein synthesis by binding to the bacterial 23S ribosomal RNA of the 59S subunit, thereby preventing the formation of a functional 70S complex essential to bacterial translation.
Indications for use. Linezolid is active against a variety of Gram-positive pathogens including vancomycin-resistant Enterococcus faecium (although unfortunately resistant organisms have already been reported), meticillin-resistant Staph. aureus and penicillin-resistant Strep. pneumoniae. It is also active against group A and group B streptococci. Clinical experience has demonstrated efficacy in a variety of hospitalized patients with severe to life-threatening infections, such as bacteraemia, hospital-acquired pneumonia and skin and soft tissue infections. It can be given both intravenously and by mouth.
Interactions. Linezolid interacts reversibly as a non-selective inhibitor of monoamine oxidase and has the potential for interacting with serotoninergic and adrenergic agents.
Toxicity. Side-effects include gastrointestinal disturbances, headache, rash, hypertension, reversible but potentially severe cytopenias and occasional reports of optic neuropathy. Safety has not yet been shown in pregnancy.
Nitroimidazoles
Structure. These agents are active against anaerobic bacteria and some pathogenic protozoa. The most widely used drug is metronidazole. Others include tinidazole and nimorazole.
Mechanism of action. After reduction of their ‘nitro’ group to a nitrosohydroxyl amino group by microbial enzymes, nitroimidazoles cause strand breaks in microbial DNA.
Indications for use. Metronidazole plays a major role in the treatment of anaerobic bacterial infections, particularly those due to Bacteroides spp. It is also used prophylactically in colonic surgery. It may be given orally, by suppository (well absorbed and cheap) or intravenously (very expensive). It is also the treatment of choice for mild and moderate CDAD, amoebiasis, giardiasis and infection with Trichomonas vaginalis.
Interactions. Nitroimidazoles can produce a disulfiram-like reaction with ethanol and enhance the anticoagulant effect of warfarin.
Toxicity. Nitroimidazoles are tumorigenic in animals and mutagenic for bacteria, although carcinogenicity has not been described in humans. They cause a metallic taste and polyneuropathy with prolonged use. They should be avoided in pregnancy.
Glycopeptides
The glycopeptides are antibiotics active against Gram-positive bacteria and act by inhibiting cell wall synthesis.
Vancomycin
Vancomycin is given intravenously for meticillin-resistant Staph. aureus and other multiresistant Gram-positive organisms. It is also used for treatment and prophylaxis against Gram-positive infections in penicillin-allergic patients. It is used for Strep. pneumoniae meningitis when caused by penicillin-resistant strains. By mouth, it is an alternative to metronidazole for CDAD. Glycopeptide-resistant enterococci (GRE) are now seen, as well as vancomycin-resistant Staphylococcus (see p. 116).
Toxicity. Vancomycin can cause ototoxicity and nephrotoxicity and thus serum levels should be monitored. Care must be taken to avoid extravasation at the injection site as this causes necrosis and thrombophlebitis. Too rapid infusion can produce symptomatic release of histamine (red man syndrome).
Other antibiotics
Clindamycin is not widely used because of its strong association with CDAD. It is active against Gram-positive cocci including some penicillin-resistant staphylococci and is a useful agent for severe streptococcal or staphylococcal cellulitis. It has the added effect of inhibiting staphylococcal TSST-1 and alpha toxin production and has a role in infections caused by Staph. aureus secreting Panton Valentine leucocidin (PVL). It is also active against anaerobes, especially bacteroides. It is well concentrated in bone and used for osteomyelitis.
Streptogramins. A combination of quinupristin and dalfopristin is used for Gram-positive bacteria which have failed to respond to other antibacterials. It has found only limited use and is not available in the UK. Virginiamycin and pristinamycin are also available.
Daptomycin is a lipopeptide with a similar spectrum to vancomycin and is given by i.v. infusion. It is particularly used for complicated skin and soft tissue infections including those caused by MRSA. It is also useful for endocarditis of the right heart there is increasing evidence of efficacy in other types of carditis and systemic infection.
Fosfomycin, which is a relatively old antibiotic and is not currently licensed in the UK, is effective against many Gram-negative bacteria. It retains activity against the majority of ESBL-producing organisms and is therefore the subject of renewed interest.
Antituberculosis drugs
These are described on page 842. Rifampicin is also used in other infections apart from tuberculosis.
Antifungal drugs (Table 4.12)
Polyenes
Polyenes react with the sterols in fungal membranes, increasing permeability and thus damaging the organism. The most potent is amphotericin, which is used intravenously in severe systemic fungal infections. Nephrotoxicity is a major problem and dosage levels must take background renal function into account. Liposomal amphotericin is less toxic but very expensive. Nystatin is not absorbed through mucous membranes and is therefore useful for the treatment of oral and enteric candidiasis and for vaginal infection. It can only be given orally or as pessaries.
|
|
Azoles
Imidazoles such as ketoconazole, miconazole and clotrimazole are broad-spectrum antifungal drugs. They are predominantly fungistatic and act by inhibiting fungal sterol synthesis, resulting in damage to the cell wall. Ketoconazole is active orally but can produce liver damage. It is effective in candidiasis and deep mycoses including histoplasmosis and blastomycosis but not in aspergillosis and cryptococcosis.
Clotrimazole and miconazole are used topically for the treatment of ringworm and cutaneous and genital candidiasis. Econazole is used for the topical treatment of cutaneous and vaginal candidiasis and dermatophyte infections while tioconazole is indicated for fungal nail infections.
Triazoles. These include fluconazole, voriconazole and itraconazole. Fluconazole is noted for its ability to enter CSF and is used for candidiasis and for the treatment of central nervous system (CNS) infection with Cryptococcus neoformans. Itraconazole fails to penetrate CSF. It is the agent of choice for non-life-threatening blastomycosis and histoplasmosis. It is also moderately effective in invasive aspergillosis. Toxicity is mild. Voriconazole has broad-spectrum activity that includes Candida, Cryptococcus and Aspergillus spp. and other filamentous fungi. It is available for oral and intravenous use. Adverse effects include rash, visual disturbance and abnormalities of liver enzymes. It is indicated for invasive aspergillosis and severe candida infections unresponsive to amphotericin and fluconazole, respectively.
Allylamines
Terbinafine has broad-spectrum antifungal and also anti-inflammatory activity. It is well absorbed orally and accumulates in keratin. It is useful for the treatment of superficial mycoses such as dermatophyte infections, onychomycosis and cutaneous candidiasis. A topical formulation is also available to treat fungal skin infections.
Echinocandins
These act by inhibiting the cell wall polysaccharide, glucan. Caspofungin, which is administered intravenously, is active against Candida spp. and Aspergillus spp. and is indicated for invasive candidiasis and invasive aspergillosis unresponsive to other drugs. Other echinocandins include micafungin and anidulafungin, approved for the treatment of disseminated candidiasis.
Antiviral drugs
Drugs for HIV infection are discussed on page 182.
Nucleoside analogues
Aciclovir. Aciclovir (also known as acycloguanosine) is an acyclic nucleoside analogue which acts as a chain terminator of herpesvirus DNA synthesis. This drug is converted to aciclovir monophosphate by a virus-encoded thymidine kinase produced by alpha herpesviruses, herpes simplex types 1 and 2 and varicella zoster virus (Table 4.13). Conversion to the triphosphate is then achieved by cellular enzymes. Aciclovir triphosphate acts as a potent inhibitor of viral (but not cellular) DNA polymerase and also competes with deoxyguanine triphosphate for incorporation into the growing chains of herpesvirus DNA, thereby resulting in chain synthesis termination due to its acyclic structure. This highly specific mode of activity, targeted only to virus-infected cells, means that aciclovir has very low toxicity. Crystallization in the renal tubules is a well-recognized adverse effect. Intravenous, oral and topical preparations are available for the treatment of herpes simplex and varicella zoster virus infections (Table 4.13). Treatment does not eliminate the virus so relapses do occur.
Table 4.13 Antiviral agents (for drugs used in HIV, see Table 4.53)
| Drug | Use |
|---|---|
Nucleoside analogues |
|
Aciclovir |
Topical – HSV infection |
Oral and intravenous – VZV and HSV |
|
Famciclovir |
Oral – VZV and HSV |
Valaciclovir |
Oral – VZV and HSV |
Ganciclovir |
Intravenous – CMV |
Valganciclovir |
Oral – CMV |
Lamivudine |
Oral – HBV infection |
Emtricitabine |
Oral – HBV infection |
Telbivudine |
Oral – HBV infection |
Entecavir |
Oral – HBV |
Nucleotide analogues |
|
Tenofovir |
Oral – HBV infection |
Adefovir |
Oral – HBV infection |
Cidofovir |
Intravenous – CMV |
Pyrophosphate analogues |
|
Foscarnet |
Intravenous – CMV |
Adamantanes |
|
Amantadine |
Oral – influenza A |
Neuraminidase inhibitors |
|
Zanamivir |
Topical (inhalation) – influenza A and B |
Oseltamivir |
Oral – influenza A and B |
Other drugs |
|
Ribavirin |
Topical (inhalation) – RSV |
Oral – Lassa fever, hepatitis C |
|
Pegylated INF-α |
HBV, HCV, some malignancies (e.g. renal cell carcinoma) (Given once weekly) |
Palivizumab |
Prevention in RSV |
Protease inhibitors |
|
Telaprevir |
Oral – HCV |
Boceprevir |
Oral – HCV |
Valaciclovir is an oral pro-drug of aciclovir. Coupling of the amino acid valine to the acyclic side-chain of aciclovir allows better intestinal absorption. The valine is removed by enzymic action and aciclovir is released into the circulation. A similar pro-drug of a related nucleoside analogue (penciclovir) is the antiherpes drug, famciclovir. The mode of action and efficacy of famciclovir are similar to those of aciclovir.
Ganciclovir. This guanine analogue is structurally similar to aciclovir, with extension of the acyclic side-chain by a carboxymethyl group. It is active against herpes simplex viruses and varicella zoster virus by the same mechanism as aciclovir. In addition, phosphorylation by a protein kinase encoded by the UL97 gene of cytomegalovirus renders it potently active against this virus. Thus, ganciclovir is currently the first-line treatment for cytomegalovirus disease. Intravenous and oral preparations are available as is an oral pro-drug, valganciclovir. Unlike aciclovir, ganciclovir has a significant toxicity profile including neutropenia, thrombocytopenia and rarely, sterilization by inhibition of spermatogenesis. It is therefore reserved for the treatment or prevention of life- or sight-threatening cytomegalovirus infection in immunocompromised patients.
Lamivudine is a reverse transcriptase inhibitor active against both HIV and hepatitis B. Drug resistance is a problem (see pp. 81, 184).
Entecavir is a more potent inhibitor of hepatitis B and is active against lamivudine-resistant strains. Telbivudine and emtricitabine are also nucleoside analogue inhibitors of HBV DNA polymerase activity.
Nucleotide analogues
Cidofovir is a phosphonate derivative of an acyclic nucleoside which is a DNA polymerase chain inhibitor. It is administered intravenously for the treatment of severe cytomegalovirus (CMV) infections in patients with AIDS for whom other drugs are inappropriate. It is given with probenecid and as it is nephrotoxic, particular attention should be given to hydration and to monitoring renal function.
Adefovir dipivoxil has activity against hepatitis B virus DNA polymerase. However, tenofovir disoproxil is much more potent, has a much higher barrier to resistance and has therefore largely superseded adefovir in use (see p. 322).
Pyrophosphate analogues
Foscarnet (sodium phosphonoformate) is a simple pyrophosphate analogue which inhibits viral DNA polymerases. It is active against herpesviruses and its main roles are as a second-line treatment for severe cytomegalovirus disease and for the treatment of aciclovir-resistant herpes simplex infection. It is given intravenously and the potential for severe side-effects, particularly renal damage, limits its use.
Adamantanes
Amantadine. Amantadine (and its derivative rimantadine) is a synthetic symmetrical amine, which is active prophylactically and therapeutically against influenza A virus (it is inactive against influenza B virus). Its prophylactic efficacy is similar to that of influenza vaccine and it is occasionally used to prevent the spread of influenza A in institutions such as nursing homes. CNS side-effects such as insomnia, dizziness and headache may occur (it is also used as a treatment for Parkinson’s disease) and the drug is poorly tolerated, especially in the elderly.
Neuraminidase inhibitors
Zanamivir (administered by inhalation) and oseltamivir (an oral preparation) inhibit the action of the neuraminidase of influenza A and B. Both have been shown to be effective in reducing the duration of illness in influenza. Oseltamivir is also available for the prophylaxis of influenza among household contacts of an index case. Intravenous peramivir and zanamivir were both reported to be effective in treating patients during the 2010 influenza pandemic, but neither are currently licensed for routine use in this way.
Protease inhibitors
Two new protease inhibitors, bocepravir and telapravir, have recently become available for treating chronic hepatitis C infection (in combination with ribavirin and interferon) (see p. 304).
Other drugs
Ribavirin. This synthetic purine nucleoside derivative which interferes with 5′-capping of messenger RNA, is active against several RNA and DNA viruses, at least in vitro. Its major use is in the treatment of chronic hepatitis C infection in combination with pegylated interferon-α, although it has no effect when given alone (see p. 324). It is administered orally. Haemolytic anaemia is the most frequent adverse reaction. It is also administered by a small-particle aerosol generator (SPAG) to infants with acute respiratory syncytial virus (RSV) infection. Another indication is in the treatment of Lassa fever virus infection.
Palivizumab. This monoclonal antibody is specifically indicated to prevent seasonal respiratory syncytial virus (RSV) infection in infants at high risk of this infection. It is administered by intramuscular injection.
Interferons
These are naturally occurring proteins with a multiplicity of actions, including antiviral, immunomodulatory and antiproliferative effects. Interferons are produced by virus-infected cells, macrophages and lymphocytes. They induce an antiviral state in uninfected cells, through activation of a complex set of biochemical pathways. They have been synthesized commercially by either culture of lymphoblastoid cells or by recombinant DNA technology and are licensed for therapeutic use.
The potency of INF-α has been enhanced by coupling the protein with polyethylene glycol. The resulting PEG interferon given once weekly has been shown to improve the response to, and reduce the side-effects from, treatment for hepatitis B and C.
Immunization against infectious diseases
Although effective antimicrobial chemotherapy is available for many diseases, the ultimate aim of any infectious disease control programme is to prevent infection occurring. This is achieved either by:
 eliminating the source or mode of transmission of an infection (see p. 75);
eliminating the source or mode of transmission of an infection (see p. 75);
Immunization, immunoprophylaxis and immunotherapy
Immunization has changed the course and natural history of many infectious diseases. Passive immunization by administering preformed antibody, either in the form of immune serum or purified normal immunoglobulin, provides short-term immunity and has been effective in both the prevention (immunoprophylaxis) and treatment (immunotherapy) of a number of bacterial and viral diseases (Table 4.14). The active immunization schedule currently recommended is summarized in Box 4.6. Long-lasting immunity is achieved only by active immunization with a live attenuated or an inactivated organism or a subunit thereof (Table 4.15). Active immunization may also be performed with microbial toxin (either native or modified) – that is, a toxoid. Immunization should be kept up to date with booster doses throughout life. Travellers to developing countries, especially if visiting rural areas, should in addition enquire about further specific immunizations.
Table 4.14 Examples of passive immunization available
![]() Box 4.6
Box 4.6
Recommended immunization schedules: (i) in the UK; (ii) WHO model schedule for developing countries
| Time of immunization | Vaccine |
|---|---|
(i) UK |
|
2 months |
DTaP, IPV, Hib + PCV (BCGa) |
3 months |
DTaP, IPV, Hib + MenC |
4 months |
DTaP, IPV, Hib + MenC + PCV |
12 months |
Hib, MenC |
13 months |
MMR + PCV |
3 years 4 months – 5 years |
DTaP, IPV, MMR |
12–13 years |
HPV |
13–18 years |
Td, IPV |
(ii) Developing countriesb |
|
Birth (or first contact) |
PV, BCG |
6 weeks |
DPT, PV, HBV |
10 weeks |
DPT, PV, HBV |
14 weeks |
DPT, PV, HBV |
9 months |
Measles, YFc |
DTaP, adsorbed diphtheria, tetanus triple vaccine, acellular pertussis; DPT, adsorbed diphtheria, whole cell pertussis, tetanus triple vaccine; Hib, Haemophilus influenzae type b vaccine; IPV, inactivated polio vaccine; PV, polio vaccine; MenC, meningococcus group C conjugate vaccine; aP, acellular pertussis; MMR, measles, mumps, rubella triple vaccine; T, tetanus; d, adsorbed low-dose diphtheria; HBV, hepatitis B vaccine; HPV, human papillomavirus vaccine; YF, yellow fever vaccine; PCV, pneumococcal conjugate vaccine.
Mumps vaccine is given in many developing countries.
a Children at high risk of contact with tuberculosis. For more detailed advice about childhood BCG immunization, see The Green Book (see Significant Websites for details).
b Model scheme, adapted locally depending on need and availability of vaccines.
Table 4.15 Preparations available for active
BCG, bacille Calmette–Guérin.
a Individual vaccines for measles, mumps and rubella are not licensed in the UK.
In 1974, the World Health Organization introduced the Expanded Programme on Immunization (EPI). By 1994, more than 80% of the world’s children had been immunized against tuberculosis, diphtheria, tetanus, pertussis, polio and measles. Poliomyelitis should shortly be eradicated worldwide, which will match the past success of global smallpox eradication. Introduction of conjugate vaccines against Haemophilus influenzae type b (Hib) has proved highly effective in controlling invasive H. influenzae infection, notably meningitis (see p. 1130).
Immunization e.g. tetanus, HBV, should be kept up to date in adults.
FURTHER READING
Chaves SS, Gargiullo P, Zhang JX et al. Loss of vaccine-induced immunity to varicella over time. N Engl J Med 2007; 356:1121–1129.
Crowcroft NS, Pebody RG. Recent developments in pertussis. Lancet 2006; 367:1926–1936.
Gardner P. Prevention of meningococcal disease. N Engl J Med 2006; 355:1466–1473.
Pallansch MA, Sandhu HS. The eradication of polio – progress and challenges. N Engl J Med 2006; 355:2508–2511.
SIGNIFICANT WEBSITES
NHS Immunisation Information: http://www.immunisation.nhs.uk
The Green Book – Immunisation against Infectious Disease: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_079917
Protection for travellers to developing/tropical countries
There has been a huge increase in the number of people travelling to developing countries, mainly for recreation and leisure. The risk of infection depends on the area to be visited, the type of activity and the underlying health of the traveller. Advice should therefore always be based on an individual assessment.
Protection for travellers against infection can be divided into three categories:
Because situations and risks can change rapidly, websites (which can be regularly updated) are often the best source of advice on travel health.
SIGNIFICANT WEBSITES
CDC Travel Health Site: http://www.cdc.gov/travel
National Travel Health Network and Centre: http://www.nathnac.org