Nutrition in Weight Management
Sections of this chapter were written by Molly Gee, MED, RD for the previous edition of this text.
Body weight is the sum of bone, muscle, organs, body fluids, and adipose tissue. Some or all of these components are subject to normal change as a reflection of growth, reproductive status, variation in physical activity, and the effects of aging. Consistent body weight is orchestrated by neural, hormonal, and chemical mechanisms as well as individual genetic polymorphisms that balance energy intake and expenditure within fairly precise limits (de Luis et al., 2006). Abnormalities of these complex mechanisms can result in weight fluctuations, most commonly overweight and obesity.
On the other end of the weight spectrum is underweight. Although the inability to gain weight can also be a primary problem, low body weight is usually secondary to a disease state, an eating disorder, or a psychological problem (see Chapter 23). In the elderly or in children, unintentional weight loss can be especially detrimental and should be addressed early to prevent malnutrition or other undesirable consequences.
Body Weight Components
Body weight is often described in terms of its composition, and different models have been advanced to estimate body fat. Body composition is discussed in detail in Chapter 6. Traditionally, a two-compartment model divides the body into fat mass, the fat from all body sources including the brain, skeleton, and adipose tissue, and fat-free mass (FFM), which includes water, protein, and mineral components (Figure 22-1). The proportions of FFM are relatively constant from person to person.
Although FFM is often used interchangeably with the term lean body mass, it is not exactly the same. Lean body mass (LBM) is muscle. LBM is higher in men than in women, increases with exercise, and is lower in older adults. It is the major determinant of the resting metabolic rate (RMR). It follows that a decrease in LBM could hinder the progress of weight loss. Therefore, to achieve long-term weight-loss, the loss of fat mass while maintaining FFM and RMR is desirable (Stiegler and Cunliffe, 2006). Water, which makes up 60% to 65% of body weight, is the most variable component of LBM, and the state of hydration can induce fluctuations of several pounds.
Body Fat
Total body fat is the combination of “essential” and “storage” fats, usually expressed as a percentage of total body weight that is associated with optimum health. Muscle and even skeletal mass adjust to some extent to support the burden of adipose tissue.
Essential fat, necessary for normal physiologic functioning, is stored in small amounts in the bone marrow, heart, lung, liver, spleen, kidneys, muscles, and the nervous system. In men, approximately 3% of body fat is essential. In women, essential fat is higher (12%) because it includes body fat in the breasts, pelvic regions, and thighs that support the reproductive process.
Storage fat is the energy reserve, primarily as triglycerides (TGs) in adipose tissue. This fat accumulates under the skin and around the internal organs to protect them from trauma. Most storage fat is “expendable.” The fat stores in adipocytes are capable of extensive variation. This allows for the changing requirements of growth, reproduction, aging, environmental and physiologic circumstances, the availability of food, and the demands of physical activity. Total body fat (essential fat plus storage fat) as a percentage of body weight that is associated with optimal health is 10% to 25% in men and 18% to 30% in women, although professional and elite athletes have body fat levels much lower than those of the average person, with an average for optimal fitness of 12% to 18% for men and 16% to 25% for women (Wilmore et al., 1986).
Adipose Tissue Composition
Adipose tissue exerts a profound influence on whole-body homeostasis. Adipose tissue is located primarily under the skin, in the mesenteries and omentum, and behind the peritoneum. Although it is primarily fat, it also contains small amounts of protein and water. White adipose tissue (WAT) stores energy as a repository for TGs, serves as a cushion to protect abdominal organs, and insulates the body to preserve heat. Carotene gives it a slight yellow color. Brown adipose tissue (BAT) is a rapid source of energy for infants, found primarily in the scapular and subscapular areas as 5% of their body weight. The brown color is due to extensive vascularization for energy and heat production. Its function in humans remains poorly understood, and by adulthood BAT is no longer available (Hansen and Kristiansen, 2006).
Adipocyte Size and Number
The mature fat cell (adipocyte) consists of a large central lipid droplet surrounded by a thin rim of cytoplasm, which contains the nucleus and the mitochondria. These cells can store fat equal to 80% to 95% of their volume. Gains in weight and adipose tissue occur by increasing the number of cells, the size of cells as lipid is added, or a combination of the two.
Hyperplasia (increased number of cells) occurs as a normal growth process during infancy and adolescence. Cell number increases in both lean and obese children into adolescence, but the number increases faster in obese children. In teens and adults, increases in fat cell size are more common, but hyperplasia can also occur after the fat content of existing cells has reached capacity.
During normal growth, the greatest percentage of body fat (approximately 25%) is set by 6 months of age. In lean children, fat cell size then decreases; this decrease does not occur in obese children. At the age of 6 years in lean children, adiposity rebound occurs, especially in girls, with an increase in body fat. An early adiposity rebound occurring before 5.5 years is predictive of a higher level of adiposity at 16 years of age and in adulthood; a period of later rebound is correlated with normal adult weight (Rolland-Cachera, 2005).
With hypertrophy (increased cell size), fat depots can expand as much as 1000 times at any age as long as space is available. With weight loss as a result of trauma, illness, or starvation, fat cell size decreases but cell numbers remain the same (Bjorntorp and Sjostrom, 1971). Although weight loss of any amount in severely obese individuals improves basic adipocyte physiology, a weight loss of at least 5% is required to decrease fat cell size (de Luis et al., 2006; Varady et al., 2009).
Fat Storage
Most depot fat comes directly from dietary TGs. The fatty acid composition of adipose tissue mirrors the fatty acid composition of the diet. Even excess dietary carbohydrate and protein are converted to fatty acids in the liver by the comparatively inefficient process of lipogenesis. Under normal conditions, little dietary carbohydrate is used to produce adipose tissue; it requires three times more energy to convert excess energy from carbohydrate to fat storage as that from dietary fat. Recommendations simply to reduce dietary fat are ineffective; total reduction of calories is needed for weight loss to occur.
Semivolatile organic compounds (SVOCs) accumulate in adipose tissues from exposure to toxins, chemicals, and pesticides.
When adipose tissue is mobilized during weight loss, SVOCs are released. See Clinical Insight: What’s in That Fat When You Lose It? Obese women should lose weight before becoming pregnant because the effect of SVOCs on the developing fetal brain is not yet known (see Chapter 16).
Lipoprotein Lipase
Dietary TG is transported to the liver by chylomicrons. Endogenous TGs, synthesized in the liver from free fatty acids, travel as part of very-low-density lipoprotein particles. The enzyme lipoprotein lipase (LPL) moves lipid from the blood into the adipose cell where it hydrolyzes TG into free fatty acids and glycerol. Glycerol proceeds to the liver; fatty acids enter the adipocyte and are reesterified into TGs. When needed by other cells, TGs are hydrolyzed once again to fatty acids and glycerol by hormone-sensitive lipase (HSL) within the adipose cell; they are then released into the circulation.
Hormones affect LPL activity in different adipose tissue regions. Estrogens stimulate LPL activity in the gluteofemoral adipocytes and thus promote fat storage in this area for childbearing and lactation. In the presence of sex steroid hormones, a normal distribution of body fat exists. With a decrease in sex steroid hormones, as occurs with menopause or gonadectomy, there is a tendency to increase central obesity.
Regulation of Body Weight
Regulatory systems such as neurochemicals, body-fat stores, protein mass, hormones, and postingestion factors all play a role in regulating intake and weight. Regulation takes place on both a short- and a long-term basis. Short-term regulation governs consumption of food from meal to meal; long-term regulation is controlled by the availability of adipose stores and hormone responses.
Metabolic Rate and Voluntary Activity
The RMR explains 60% to 70% of total energy expenditure. RMR declines with age or with restriction of energy intake. When the body is suddenly deprived of adequate energy from involuntary or deliberate starvation, the RMR conserves energy by dropping rapidly, by as much as 15% in 2 weeks.
Activity thermogenesis (AT) is the energy expended in voluntary activity, the most variable component of energy expenditure. Under normal circumstances physical activity accounts for 15% to 30% of total energy expenditure. Yet all activity counts. Nonexercise activity thermogenesis (NEAT) is the energy expended for everything that is not sleeping, eating, or sportslike exercise. It includes going to work, typing, doing yard work, toe-tapping, even fidgeting (see Chapter 2). NEAT and a sedentary lifestyle may have profound importance in weight management. NEAT varies as much as 2000 kcal/day between individuals (Levine et al., 2007). To reverse obesity, individual strategies should promote standing and ambulating for 2.5 hours per day and should also reengineer work, school, and home environments to support a more active lifestyle (Levine, 2007).
Short- and Long-Term Regulation
Short-term controls are concerned primarily with factors governing hunger, appetite, and satiety. Satiety is associated with the postprandial state when excess food is being stored. Hunger is associated with the postabsorptive state when those stores are being mobilized. Physical triggers for hunger are much stronger than those for satiety, and it is easier to override the signals for satiety.
When either overfeeding or underfeeding occurs, younger individuals exhibit spontaneous hypophagia (undereating) or hyperphagia (overeating) accordingly. Older individuals do not have the same responsiveness; they are more vulnerable to unexplained weight losses or gains because they are unable to control spontaneous, short-term changes in food intake.
Long-term regulation seems to involve a feedback mechanism in which a signal from the adipose mass is released when “normal” body composition is disturbed, as when weight loss occurs. Adipocytokines are proteins released by the adipose cell into the bloodstream that act as signaling molecules. Younger persons have more responsiveness to this feedback than do older adults. See Table 22-1 and Focus On: Signals from a Host of Hormones.
TABLE 22-1
Regulatory Factors Involved in Feeding and Weight Management
| Brain Neurotransmitters | Characteristics and Function |
| Norepinephrine and dopamine | Released by the SNS in response to dietary intake; mediate the activity of areas in the hypothalamus that govern feeding behavior. Fasting and semistarvation lead to decreased SNS activity and increased adrenal medullary activity with a consequent increase in epinephrine, which fosters substrate mobilization. Dopaminergic pathways in the brain play a role in the reinforcement properties of food. |
| Serotonin, neuropeptide Y, and endorphins | Decreases in serotonin and increases in neuropeptide Y have been associated with an increase in carbohydrate appetite. Neuropeptide Y increases during food deprivation; it may be a factor leading to an increase in appetite after dieting. Preferences and cravings for sweet, high-fat foods observed among obese and bulimic patients involve the endorphin system. |
| CRF | Involved in controlling adrenocorticotropic hormone release from the pituitary gland, CRF is a potent anorexic agent and weakens the feeding response produced by norepinephrine and neuropeptide Y. CRF is released during exercise. |
| Gut Hormones | |
| Incretins | Gastrointestinal peptides increase the amount of insulin released from the beta cells of the pancreas after eating, even before blood glucose levels become elevated. They also slow the rate of absorption by reducing gastric emptying and may directly reduce food intake. Incretins also inhibit glucagon release from the alpha cells of the pancreas. (See GLP-1 and GIP.) |
| CCK | Released by the intestinal tract when fats and proteins reach the small intestine, receptors for CCK have been found in the gastrointestinal tract and the brain. CCK causes the gallbladder to contract and stimulates the pancreas to release enzymes. At the brain level, CCK inhibits food intake. |
| Bombesin | Released by enteric neurons; reduces food intake and enhances the release of CCK. |
| Enterostatin | A portion of pancreatic lipase involved specifically with satiety following the consumption of fat. |
| Adiponectin | An adipocytokine secreted by the adipose tissue that modulates glucose regulation and fatty acid catabolism. Levels of this hormone are inversely correlated with BMI. The hormone plays a role in metabolic disorders such as type 2 diabetes, obesity, and atherosclerosis. Levels drop after gastric bypass surgery for up to 6 months (Couce et al., 2006). |
| Glucagon | Increased secretion of glucagon is caused by hypoglycemia, increased levels of norepinephrine and epinephrine, increased plasma amino acids, and cholecystokinin. Decreased secretion of glucagon occurs when insulin or somatostatin is released. |
| Apolipoprotein A-IV | Synthesized and secreted by the intestine during lymphatic secretion of chylomicrons. After entering the circulation, a small portion of apolipoprotein A-IV enters the CNS and suppresses food consumption. |
| Fatty acids | Free fatty acids, triglycerides, and glycerol are factors that also affect uptake of glucose by peripheral tissues. |
| GLP-1 and GIP | Released by intestinal mucosa in presence of meals rich in glucose and fat; stimulate insulin synthesis and release; GLP-1 decreases glucagon secretion, delays gastric emptying time, and may promote satiety; examples of incretin hormones. |
| Insulin | Acts in the CNS and the periphery nervous system to regulate food intake. Insulin is involved in the synthesis and storage of fat. Impaired insulin activity may lead to impaired thermogenesis. It is possible that obese persons with insulin resistance or deficiency have a defective glucose disposal system and a depressed level of thermogenesis. The greater the insulin resistance, the lower the thermic effect of food. Fasting insulin levels increase proportionately with the degree of obesity; however, many obese persons demonstrate insulin resistance because of a lack of response by insulin receptors, impaired glucose tolerance, and associated hyperlipidemia. These sequelae can usually be corrected with weight loss. |
| Leptin | An adipocytokine secreted by the adipose tissue, correlated with percent of body fat. Primary signal from energy stores; in obesity loses the ability to inhibit energy intake or to increase energy expenditure (Enriori et al., 2006). Compared with men, women have significantly higher concentrations of serum leptin. |
| Resistin | An adipocytokine expressed primarily in adipocytes; antagonizes insulin action (Goldstein and Scalia, 2007). |
| Ghrelin | Produced primarily by the stomach; acts on the hypothalamus to stimulate hunger and feeding. Ghrelin levels are highest in lean individuals and lowest in the obese. Increased levels are seen in people who are dieting, and suppressed levels are noted after gastric bypass, possibly counteracted by adiponectin (Couce et al., 2006). |
| PYY3-36 | Secreted by endocrine cells lining the small bowel and colon in response to food; a “middle man” in appetite management. PYY seems to work opposite from ghrelin; it induces satiety. |
| IL-6 and TNF-α | Both are gut hormones. Cytokines secreted by adipose tissue and participate in metabolic events. Impair insulin signals in muscle and liver. Levels are proportional to body fat mass (Thomas et al., 2010). |
| Other Hormones | |
| Thyroid hormones | Modulate the tissue responsiveness to the catecholamines secreted by the SNS. A decrease in triiodothyronine lowers the response to SNS activity and diminishes adaptive thermogenesis. Women should be tested for hypothyroidism, particularly after menopause. Weight regain after weight loss may be a function of a hypometabolic state; energy restriction produces a transient, hypothyroid, hypometabolic state. |
| Visfatin | An adipocytokine protein secreted by visceral adipose tissue that has an insulin-like effect; plasma levels increase with increasing adiposity and insulin resistance (Stevens and Vidal-Puig, 2006). |
| Adrenomedullin | A new regulatory peptide secreted by adipocytes as a result of inflammatory processes. |
BMI, Body mass index; CCK, cholecystokinin; CNS, central nervous system; CRF, corticotropin-releasing factor; GIP, glucose-dependent insulinotropic peptide; GLP-1, glucagon-like peptide 1; IL-6, interleukin-6; PYY3-36, peptide YY3-36; SNS, sympathetic nervous system; TNF-α, tumor necrosis factor–α.
Set Point Theory
Fat storage in nonobese adults appears to be regulated in a manner that preserves a specific body weight. In both animals and humans, deliberate efforts to starve or overfeed are followed by a rapid return to the original body weight, a “set point.” Body weight remains remarkably stable from internal regulatory mechanisms that are genetically determined. Some studies suggest that body weight can be displaced only temporarily and that RMR lowers, resulting in a regain of lost weight; other studies have not shown this adaptive metabolic response.
Weight Imbalance: Overweight and Obesity
Overweight occurs as a result of an imbalance between food consumed and physical activity. Obesity is a complex issue related to lifestyle, environment, and genes. Environmental and genetic factors have a complex interaction with psychological, cultural, and physiologic influences. Over the years, many hypotheses have evolved to explain why some people become fat and others remain lean, and why it is so difficult for reduced-obese persons to maintain weight loss. No single theory can completely explain all manifestations of obesity or apply consistently to all persons.
Prevalence
The United States has the highest prevalence of obesity among the developed nations. However, increases in the prevalence of overweight and obesity have been observed throughout the world. The international trend is often called “globesity.”
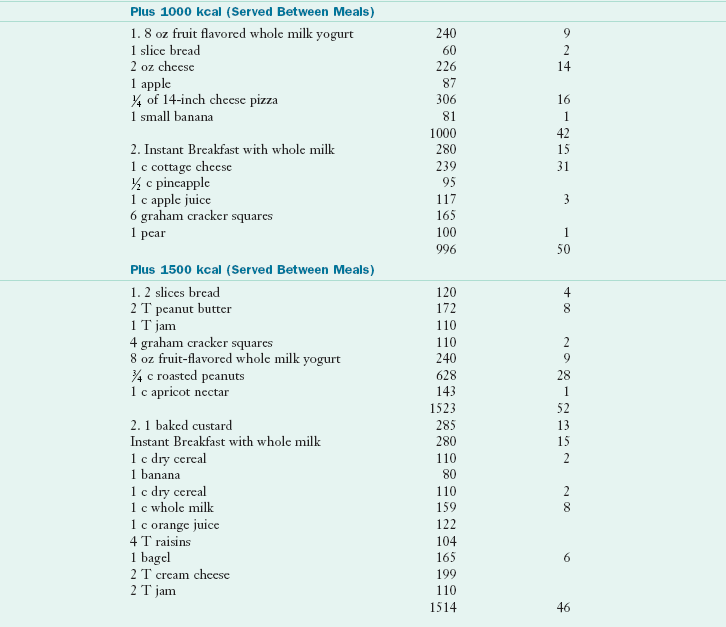
The estimates of overweight and obesity among children and adults are based on measured weights and heights from the National Health and Nutrition Examination Survey (NHANES), conducted by the National Center for Health Statistics (Centers for Disease Control and Prevention [CDC], 2007). An estimated 66% of U.S. adults are overweight, and 32% are obese. In Canada 36% of adults are overweight and another 23% are obese (Statistics Canada, 2010). In Europe between 15% and 25% of adults are obese. In the United States, prevalence of obesity is higher in black and Hispanic populations, especially among Mexican-American women (CDC, 2007; Figure 22-2).
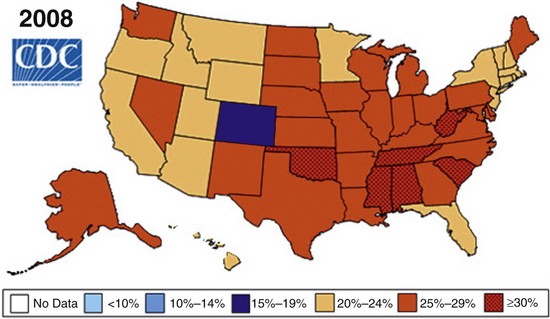
FIGURE 22-2 Prevalence of obesity among U.S. adults in 2008. (Centers for Disease Control and Prevention (CDC) Behavioral Risk Factor Surveillance System Survey, June 13, 2010.)
Unfortunately, children are not immune to the epidemic. Obesity is now the most common pediatric nutritional problem in the United States. Nearly 1/3 of children and adolescents between ages 2 and 19 years are overweight. See New Directions: Organizing to Solve the Childhood Obesity Problem “Within a Generation.”
Causes of Overweight and Obesity
Many hormonal and neural factors involved in weight regulation are determined genetically. These include the short- and long-term signals that determine satiety and feeding activity. Small defects in their expression or interaction could contribute significantly to weight gain.
The number and size of fat cells, regional distribution of body fat, and RMR are also influenced by genes. Studies of twins confirm that genes determine 50% to 70% of the predisposition to obesity (Prentice, 2005). Although numerous genes are involved, several have received much attention—the Ob gene, the adiponectin (ADIPOQ) gene, the FTO gene, and the β3-adrenoreceptor gene. The Ob gene produces leptin. Mutations in the Ob gene, leptin receptor (LEPR), or ADIPOQ genes can result in obesity or metabolic syndrome (MetS), especially if diet provides too much saturated fat (Ferguson et al., 2010). The β3-adrenoreceptor gene, located primarily in the adipose tissue, is thought to regulate RMR and fat oxidation in humans. The FTO gene predisposes to diabetes by its effect on body mass (Frayling et al., 2007).
Nutritional or lifestyle choices can activate or deactivate those obesity-triggering genes. Thus the answer to successful long-term weight management is likely to include behavioral application of individual genetics. One day soon, specific deoxyribonucleic acid tests may give accurate predictions about an individual’s response to a low-fat diet, a low-carbohydrate diet, or a balanced diet (Ashley et al., 2010). Nutritional counseling can truly be personalized (see Chapter 5).
Inadequate Physical Activity
Lack of exercise and a generally sedentary lifestyle, compounded by chronic overeating, are also causes of weight gain. The sedentary nature of society is a factor in the growing problem of obesity. Fewer people are exercising, and more time is being spent in low-energy, screen-watching activities such as watching television or movies, using the computer, playing video games, and sitting in cars driving to work or events.
Inflammation
Adipose tissue actively secretes a wide range of pro- and antiinflammatory cytokines that are influenced by single-nucleotide polymorphisms in the cytokine genes; effects include insulin insensitivity, hyperlipidemia, muscle protein loss, and oxidant stress (Grimble, 2010). Scientists have found a direct relationship between obesity and inflammatory diseases such as cardiovascular disorders, some cancers, and type 2 diabetes.
Metabolic signals are triggered in the hypothalamus of obese individuals, laying the groundwork for chronic inflammation and tissue damage during a prolonged period. In mice fed a high-fat diet, the “master switch” of inflammation turns on the hypothalamus. In humans, chronic overeating “flips on” the inflammation switch, leading to weight gain and insulin resistance. In insulin-resistant individuals on a weight-loss diet, ezetimibe (Zetia) reduces hepatic steatosis and inflammatory markers (Chan et al., 2010).
A combined approach of diet and drug is likely to improve health outcomes. Simple diet and lifestyle changes can alter obesity-related inflammation. Foods such as oranges are antiinflammatory, whereas cream may be proinflammatory and red wine is neutral. Genotypic factors influence the effectiveness of immunonutrients; antioxidants and ω-3 polyunsaturated fatty acid decrease the intensity of the inflammatory process (Grimble, 2010). For further information on inflammation, see Chapter 6.
Sleep, Stress, and Circadian Rhythms
Shortened sleep alters the endocrine regulation of hunger and appetite. Hormones that affect appetite take over and may promote excessive energy intake. Thus recurrent sleep deprivation can modify the amount, composition, and distribution of food intake and may contribute to the obesity epidemic. It is estimated that more than 50 million Americans suffer from sleep deprivation. Others may have shift work or exposure to bright light at night, increasing the disruption of circadian rhythms and enhancing the prevalence of adiposity (Garaulet et al., 2010).
There is also a relationship between sleep, disrupted circadian rhythm, genes, and the metabolic syndrome. The cellular lipid membrane content of monounsaturated fatty acids from the diet may be protective against development of metabolic syndrome (Garaulet et al., 2009). Stress is another factor. Cortisol is released under stress; it stimulates insulin release to maintain blood glucose levels in the “fight-or-flight” response. Thus an increase in appetite occurs. Cortisol levels are typically high in the early morning and low around midnight. Individuals with night-eating syndrome (NES) have a delayed circadian rhythm of meal intake as a result of genetically programmed neuroendocrine factors, including altered cortisol levels (Stunkard and Lu, 2010).
Taste, Satiety, and Portion Sizes
Food and its taste elements evoke pleasure responses. The endless variety of food available at any time at a reasonable cost can contribute to higher calorie intake; people eat more when offered a variety of choices than when a single food is available. Normally, as foods are consumed, they become less desirable; this phenomenon is known as sensory-specific satiety. Overriding this principle is the “all-you-can-eat buffet” in which the diner reaches satiety for one food but has many choices for the “next course.” Although sensory-specific satiety can promote the intake of a varied or nutritionally balanced diet, it can also lead to overconsumption of energy.
Active overeating is partly the result of excessive portion sizes that are now accepted as normal. The portions and calories that restaurants and fast-food outlets offer in one meal often exceed a person’s energy needs for the entire day. High intake of energy-dense food can also be problematic.
Obesogens
Obesogens are chemical compounds foreign to the body that act to disrupt the normal metabolism of lipids, ultimately resulting in over fatness and obesity (Grun and Blumberg, 2006). Obesogens can be called “endocrine disruptors” in that they alter lipid homeostasis and fat storage, change metabolic set points, disrupt energy balance, or modify the regulation of satiety and appetite to promote accumulation of fat and obesity. Examples of suspected obesogens in the environment and food supply are bisphenol A and phthalates which are found in many plastics used in food packaging and which migrate into foods processed or stored in them (Grun, 2010). See Clinical Insight: What’s in That Fat When You Lose It?
Viruses and Pathogens
In the last two decades, at least ten adipogenic pathogens have been identified, including viruses, scrapie agents (spongiform encephalopathies from sheep or goats), bacteria, and gut microflora (Pasarica and Dhurandhar, 2007). Whether or not “infectobesity” is a relevant contributor to the obesity epidemic remains to be determined. A human adenovirus, adenovirus-36, is capable of inducing adiposity in experimentally infected animals by increasing the replication, differentiation, lipid accumulation, and insulin sensitivity in fat cells and reduces leptin secretion and expression (van Ginnekin et al., 2009).
Assessment
Overweight is a state in which the weight exceeds a standard based on height. Obesity is a condition of excessive fatness, either generalized or localized. Overweight and obesity usually parallel each other, but it is possible to be overweight according to standards, but not be overfat or obese. It is also possible to have excessive fatness, and yet not be overweight.
It is important to assess body fatness or adiposity to determine the health risks as explained in detail in Chapter 6. Clinically practical assessment tools are: 1) the body mass index (BMI) or W/H2, in which W= weight in kg and H = height in meters, 2) the waist circumference, 3) the waist-to-hip ratio, and 4) the Deurenberg equation which predicts body fat percentage (Deurenberg and Deurenberg-Yap, 2003).
The NIH guidelines classify individuals with a BMI of 25 as overweight and those with a BMI of 30 or more as obese (Table 22-2). Optimal BMI for longevity varies with race, gender, and age. BMI that increases over time have a substantial effect on health outcomes (Newby et al., 2006). See Chapter 6 and Appendix 23.
TABLE 22-2
Classification of Overweight and Obesity
| Classification | Body Mass Index (kg/m2) |
| Underweight | <18.5 |
| Normal | 18.5-24.9 |
| Overweight | 25.0-29.9 |
| Obesity, class I | 30.0-34.9 |
| Obesity, class II | 35.0-39.9 |
| Extreme obesity, class III | >40 |
From National Institutes of Health, National Heart, Lung, and Blood Institute: Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report, NIH Publication No. 98-4083, 1998.
Waist circumference of more than 40 inches in men and more than 35 inches in women signifies increased risk, equivalent to a BMI of 25 to 34. When waist circumference and percentage of fat are both high, they are significant predictors of heart failure and other risks associated with obesity (Nicklas et al., 2007). Waist circumference is a strong correlate of insulin sensitivity index in older adults; measurement of waist circumference is helpful to assess disease risk (Racette et al., 2006). Waist/hip ratio (WHR) is a measurement in which a ratio of more than 0.8 for women and 1 for men is also associated with high risk for cardiovascular events.
The Deurenberg equation using the BMI, age, and gender of an individual to determine body fatness is as follows (Deurenberg and Deurenberg-Yap, 2003):
For example if BMI = 28, age = 21 and G = female:
A body fat percentage of 20% to 25% or more in a male and 25% to 32% or more in a female is usually considered to be excessive and associated with the metabolic and health risks of obesity.
Health Risks and Longevity
In general, obesity can be viewed as metabolically unhealthy. Chronic diseases such as heart disease, type 2 diabetes, hypertension, stroke, gallbladder disease, infertility, sleep apnea, hormonal cancers, and osteoarthritis tend to worsen as the degree of obesity increases (Figure 22-3).
FIGURE 22-3 The medical complications of obesity are extensive. (Reprinted with permission from Delichatsios HK: Obesity assessment in the primary care office, Harvard Medical School. 23rd Annual International Conference-Practical approaches to the treatment of obesity, Boston, June 18-20 2009, GL Blackburn, course director.)
A subset of obese persons who are metabolically normal seems to exist. This subgroup has uncomplicated, early-onset obesity, hyperplastic adipocytes, and normal quantities of visceral fat. However, they are the exception and not the rule. Estimates using mortality data from the NHANES surveys show that thousands of deaths are related to obesity. Moderately high BMI in adolescence is correlated with premature death in younger and middle-age women (van Dam et al., 2006). Increased adiposity and reduced physical activity are strong independent risk factors for death in women.
A huge study of more than 100,000 U.S. men and women age 50 and older who took part in a 9-year Cancer Prevention Study II Nutrition Cohort found that obesity is linked to death. Those individuals with very large waists (at least 47 inches in men and 43 inches in women) had twice the risk of mortality compared with those with small waists (35 inches or less for men and 30 inches or less for women). This was true at all BMIs, but was strongest in women of normal weight, indicating the danger of waistline, abdominal, or visceral fat (Jacobs et al., 2010).
Several large studies have determined that the optimal BMI with the least risk for mortality is a BMI of 23 to 24.9. BMI above or below this range seems to increase mortality risk (Adams et al., 2006; Jee et al., 2006). The optimal range for longevity appears to be within the range of 20.5 to 24.9.
Nonalcoholic fatty liver disease (NAFLD) is associated with obesity and may progress to end-stage liver disease. Obesity is also a risk factor for cancer, infertility, poor wound healing, and poor antibody response to hepatitis B vaccine. Thus the costs of obesity are staggering. Health economists estimate costs of overweight and obesity to account for nearly 10% of total annual U.S. medical expenditures. The Internal Revenue Service issued a rule in 2002 qualifying obesity as a disease, allowing taxpayers to claim weight loss expenses as a medical deduction if undertaken to treat an existing disease.
The U.S. government recognizes the immense effect of obesity on the health and financial well-being of its citizens. Healthy People 2020 objectives also identify the implications of overweight and obesity (see Chapter 12). The objectives include targets to increase the proportion of adults who are at a healthy weight and to reduce the proportion of adults, children, and adolescents who are obese. Overweight adolescents often become obese adults; obese individuals are at increased risk for comorbidities of type 2 diabetes, hypertension, stroke, certain cancers, infertility, and other conditions.
Fat Deposition and the Metabolic Syndrome
Regional patterns of fat deposit are controlled genetically and differ between and among men and women. Two major types of fat deposition are currently recognized: excess subcutaneous truncal-abdominal fat (the apple-shaped android fat distribution) and excess gluteofemoral fat in thighs and buttocks (the pear-shaped gynoid fat distribution). The android shape is more common among men. The fat deposits support the demands of pregnancy and lactation. Women with the gynoid type of obesity do not develop the impairments of glucose metabolism in those with an android deposition. Postmenopausal women more closely follow the male pattern of abdominal fat stores.
Visceral obesity, or excessive visceral adipose tissue (VAT) under the peritoneum and in the intraabdominal cavity, is highly correlated with insulin resistance. Individuals diagnosed with the metabolic syndrome (MetS) have three or more of the following abnormalities: waist circumference of more than 102 cm (40 in) in men and more than 88 cm (35 in) in women, serum TGs of at least 150 mg/dL, high-density lipoprotein (HDL) level less than 40 mg/dL in men and less than 50 mg/dL in women, blood pressure 135/85 mm Hg or higher, or fasting glucose 100 mg/dL or higher. Increased visceral fat is a risk factor for coronary artery disease, dyslipidemia, hypertension, stroke, type 2 diabetes, and MetS (Goodpaster, 2005; Gower et al., 2006). By the same token, both VAT and low cardiorespiratory fitness (CRF) levels are associated with a deteriorated cardiometabolic risk profile. Achieving a low level of VAT and a high level of CRF are important targets for cardiometabolic health (Rheaume, 2011).
Calorie Restriction and Longevity
Balancing energy intake and energy expenditure is the basis of weight management throughout life. Lifestyle modification, becoming aware of eating behavior triggers to manage them more effectively, is vital for permanent change to occur. A key recommendation is to prevent gradual weight gain over time by making small decreases in overall calories and increasing physical activity. Patterns of healthful eating and regular physical activity should begin in childhood and continue throughout adulthood. The aging process with a lower RMR introduces special challenges. Energy balance must be maintained by adjusting or reducing caloric intake and increasing physical activity to prevent weight gain.
Prolonged calorie restriction (CR) increases life span and slows aging in animals. The apparent generality of the longevity-increasing effects of CR has prompted speculation that similar results could be obtained in humans. Two biomarkers of longevity (fasting insulin level and body temperature) are decreased by prolonged CR in humans (Heilbronn et al., 2006). Proponents of CR for antiaging believe that cutting calorie intake reduces aging and chronic disease development. In rodents with Alzheimer disease, heart disease, and stroke, decreased deterioration of nerves and increased nerve creation was also demonstrated (Mayo Clinic, 2010). Whether CR can slow the aging process, however, remains an important question (Fontana, 2009; Phelan, 2006). The Calorie Restriction (CR) Society International (www.crsociety.org) supports the efforts of people who practice CR for current health, future longevity, or other benefits; those curious about or interested in understanding the effects of the diet; and those interested in the development of related, science-based health-enhancing and life-extension technologies.
Weight Discrimination
Widespread bias and discrimination based on weight have been documented in education, employment, and health care. Like other forms of prejudice, this stems from a lack of understanding of the chronic disease of obesity and its medical consequences. Despite laws designed to prevent discrimination based on appearance, unfavorable attitudes and practices still persist. Overweight children experience adverse social, educational, and psychological consequences as a result of weight bias (Latner et al., 2005). There are automatic negative associations for obese people among health professionals, exercise science students, and obese individuals themselves (Brown, 2006; Carr and Friedman, 2005). It is essential to break down the barriers caused by ignorance and indifference. Patient support groups help to correct the negative effect of this type of discrimination.
Management of Obesity in Adults
The management of obesity has evolved over the years. Initially, clinicians focused entirely on weight loss, and little was known about weight maintenance. It soon became clear that focusing on weight loss without attention to weight maintenance was inappropriate, unfair, and possibly harmful to anyone trying to manage his or her weight.
Treatment has also evolved. Years ago, an energy-restricted diet was the only treatment. Eventually, lifestyle modifications were added. The importance of physical activity was recognized as an essential ingredient for weight maintenance after weight loss. Today, a chronic disease-prevention model incorporates both lifestyle interventions and interdisciplinary therapies from physicians, dietitians, exercise specialists, and behavior therapists. Weight-reduction programs with the most promise of success integrate healthier food choices, exercise, and lifestyle modification. Pharmacologic treatment and surgical intervention are appropriate in some circumstances but are not a substitute for the necessary changes in eating and physical activity pattern. The American Dietetic Association (ADA) Evidence Analysis Library (EAL) provides reliable treatment guidelines (Figure 22-4).
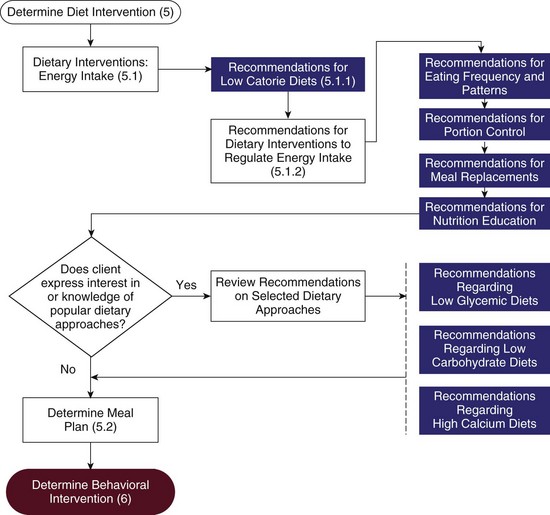
FIGURE 22-4 Algorithm for managing obesity using nutrition care process intervention terms. (© American Dietetic Association. Reprinted with permission.)
Goals of Treatment
The goal of obesity treatment should focus on weight management, attaining the best weight possible in the context of overall health. Achieving an “ideal” body weight or percentage of body fat is not always realistic; under some circumstances, it may not be appropriate at all. Depending on the type and severity of the obesity and the age and lifestyle of the individual, successfully reducing body weight varies from a being relatively simple to being virtually impossible.
Maintaining present body weight or achieving a moderate loss is beneficial. Obese persons who lose even small amounts of weight (5% to 10% of initial body weight) are likely to improve blood glucose, blood pressure, and cholesterol levels.
Despite the recognition that modest weight loss is beneficial and may be more achievable, obese persons usually have self-defined goal weights that differ considerably from the goals suggested by professionals. Therefore health professionals must help their patients accept more modest, realistic weight-loss goals.
Rate and Extent of Weight Loss
Reduction of body weight involves the loss of both protein and fat, in amounts determined to some degree by the rate of weight reduction. A drastic reduction in calories resulting in a high rate of weight loss can mimic the starvation response. Tissue response to starvation is one of adaptation to an anticipated period of deprivation. The classic starvation studies done by Keys (1950) found that during the first 10 days of a fast and after use of glycogen stores, approximately 8% to 12% of the energy expenditure is from protein and the balance is from fat. As starvation progresses, up to 97% of energy expenditure is from stored TG. Metabolic aberrations during starvation include bradycardia, hypotension, dry skin and hair, easy fatigue, constipation, nervous system abnormalities, depression, and even death.
Mobilizing fat, with more than twice the kilocalories of protein, is more efficient and also spares vital LBM. Steady weight loss over a longer period favors reduction of fat stores, limits the loss of vital protein tissues, and avoids the sharp decline in RMR that accompanies rapid weight reduction. Calorie deficits that result in a loss of approximately 0.5 to 1 lb per week for persons with a BMI of 27 to 35, and 1 to 2 lb per week for those with BMIs greater than 35, should continue for approximately 6 months for a reduction of 10% of body weight (American Dietetic Association [ADA], 2010). For the next 6 months the focus changes from weight loss to weight maintenance. Following this phase, further weight loss may be considered.
Even with the same caloric intake, rates of weight reduction vary. Men reduce weight faster than women of similar size because of their higher LBM and RMR. The heavier person expends more energy than one who is less obese, and loses faster on a given calorie intake than a lighter person. Many obese persons who fail to lose weight on a diet actually consume more energy than they report and overestimate their physical activity levels.
Weight goals should be individualized and realistic, with reduction of body fat as the focus. For example, neither the morbidly obese nor the gynoid types will be able to maintain a large weight loss. Female models of dress sizes 6 to 10 and male models with 30-inch to 34-inch waists are not appropriate role models for the obese population; even BMIs of 25 are unreasonable goals for many dieters. See Focus On: The Influence of Fashion on Societal Food Patterns.
Lifestyle Modification
Behavior modification is the cornerstone of lifestyle intervention. It focuses on restructuring a patient’s environment, nutritional intake, and physical activity by using goal setting, stimulus control, problem solving, cognitive restructuring, self-monitoring, and relapse prevention (Berkel et al., 2005). It also provides feedback on progress and places the responsibility for change and accomplishment on the patient.
In goal setting, most behavioral programs try to achieve a 0.5- to 1-lb weight loss per week by providing calorie, fat grams, and physical activity targets. It is important to identify goals that support a client’s sense of self-efficacy.
Stimulus control involves modification of (1) the settings or the chain of events that precede eating, (2) the kinds of foods consumed when eating does occur, and (3) the consequences of eating. Patients are taught to slow their rate of eating to become mindful of satiety cues and reduce food intake. Strategies such as putting down the utensils between bites, pausing during meals, and chewing for a minimum number of times are some ways to slow the eating process.
Problem solving is the process of defining the intake problem, generating possible solutions, evaluating and choosing the best solution, implementing the new behavior, evaluating outcomes, and reevaluating alternative solutions if needed.
Cognitive restructuring teaches patients to identify, challenge, and correct the negative thoughts that frequently undermine their efforts (see Chapter 15). Some lifestyle modification strategies are listed in Box 22-1.
Self-monitoring with daily records of place and time of food intake, as well as accompanying thoughts and feelings, helps identify the physical and emotional settings in which eating occurs. Physical activity is typically recorded in minutes or calories expended. Self-monitoring also gives clues to the occurrence of relapses and consequent guilt and how they can be prevented.
A comprehensive program of lifestyle modification produces a loss of approximately 10% of initial weight in 16 to 26 weeks, as revealed by a review of recent randomized controlled trials (RCTs), including the Diabetes Prevention Program. Long-term weight control is facilitated by continued patient-therapist contact, whether provided in person or by telephone, mail, or e-mail. Multiple strategies for behavioral therapy are often needed (ADA, 2010).
Technology shows promise as a delivery mechanism. Both e-mail and phone consults appear to be viable methods for contact and support as part of structured behavioral weight loss programs. Future treatment methods may include augmenting behavioral interventions with specific stimulus controls, self-monitoring with pharmacotherapy, targeted interventions available from the Internet, meal replacements, and telephone interventions. Nontraditional behavioral interventions for children and culturally sensitive interventions for racial and ethnic minority populations are needed (Berkel et al., 2005).
Dietary Modification Recommendations
Weight-loss programs with any degree of success integrate food-choice changes with exercise, behavior modification, nutrition education, and psychological support. When these approaches fail to bring about the desired reduction in body fat, medication may be added. For morbid obesity (BMI of 40 or greater), surgical intervention may be required.
Weight-loss programs should combine a nutritionally balanced dietary regimen with exercise and lifestyle modification at the least possible expense. Selecting the appropriate treatment strategy depends on the goals and health risks of the patient. Treatment options include:
• A low-calorie diet, increased physical activity, and lifestyle modification
• The preceding plus pharmacotherapy
• Surgery plus an individually prescribed dietary regimen, physical activity, and lifestyle modification program
Restricted-Energy Diets
A balanced, restricted-energy diet is the most widely prescribed method of weight reduction. The diet should be nutritionally adequate except for energy, which is decreased to the point at which fat stores must be mobilized to meet daily energy needs. A caloric deficit of 500 to 1000 kcal daily usually meets this goal. The energy level varies with the individual’s size and activities, usually ranging from 1200 to 1800 kcal daily. Regardless of the level of CR, healthful eating should be taught and recommendations for increasing physical activity should be included.
The low-calorie diet should be individualized for carbohydrates (50% to 55% of total kilocalories), using sources such as vegetables, fruits, beans, and whole grains. Generous protein, approximately 15% to 25% of kilocalories, is needed to prevent conversion of dietary protein to energy. Fat content should not exceed 30% of total calories. Extra fiber is recommended to reduce caloric density, to promote satiety by delaying stomach-emptying time, and to decrease to a small degree the efficiency of intestinal absorption. New food products made from oats and beverages with coconut oil may promise to enhance satiety by intake before a meal, with the expectation of reduced overall caloric intake. There are no current studies that suggest that coconut oil is effective for weight loss and it may contribute to weight gain with its 120 kcal and 13 g of fat per tablespoon. Otherwise, by combining oats with other fiber-rich foods, satiety may be increased.
Calculating fat as a percentage of calories is useful. A simple rule is to divide ideal calorie level by 4 for a 25% fat intake (e.g., an 1800-kcal intake needs 450 kcal from fat, or, at approximately 9 kcal/g, approximately 50 g of fat). Giving the person license to distribute fat grams throughout the day makes the approach more appealing, involves the person in the process, and decreases energy intake without hunger. Total calories must also be considered.
Alcohol and foods high in sugar should be limited to small amounts for palatability. Alcohol makes up 10% of the diet for many regular drinkers and contributes 7 kcal/g. Heavy drinkers who consume 50% or more of daily calories from alcohol may have a depressed appetite, whereas moderate users tend to gain weight with the added alcohol calories. Habitual use of alcohol may result in lipid storage, weight gain, or obesity.
Artificial sweeteners and fat substitutes improve the acceptability of limited food intakes for some people. There is no evidence that using artificial sweeteners reduces food intake or results in weight loss.
Vitamin and mineral supplements that meet age-related requirements are usually recommended with less than 1200 kcal for women or 1800 kcal for men. It is difficult to choose foods to maintain this calorie level and meet all nutritional requirements every day.
Formula Diets and Meal Replacement Programs
Formula diets are commercially prepared, ready-to-use, portion-controlled meal replacements. These meal replacements can be found over the counter (OTC) in drug stores, supermarkets, and franchised weight loss centers or in a clinical setting as drinks, prepackaged meals (entrees), or meal bars. The goal is to provide structure and replace other higher calorie foods. Per serving, most meal replacements include 0 to 5 g of fiber, 10 to 14 g of protein, various amounts of carbohydrate, 0 to 10 g of fat, and 25% to 30% of recommended dietary allowances for vitamins and minerals. Usually shakes are milk or soy based and are high in calcium with 150 to 250 kcal/8 oz. Some shakes are prepared using a blender at home and are made with a purchased powder. People who have difficulty with self-selection or portion control may use meal replacements as part of a comprehensive weight management program. Substituting one or two daily meals or snacks with meal replacements is a successful weight loss and weight maintenance strategy (ADA, 2010).
Commercial Programs
Millions of Americans turn to commercial weight-loss or self-help programs in search of permanent weight loss. The more caloric-restricted programs are usually medically supervised in a health care setting. As Table 22-3 illustrates, the programs vary considerably. Some require the use of proprietary prepackaged low-fat meals. Prepackaged diets appeal to some people because they allow them to avoid making choices about food. Some provide classes on self-introspection, behavior modification, and nutrition.
TABLE 22-3
Popular Commercial Diet Programs
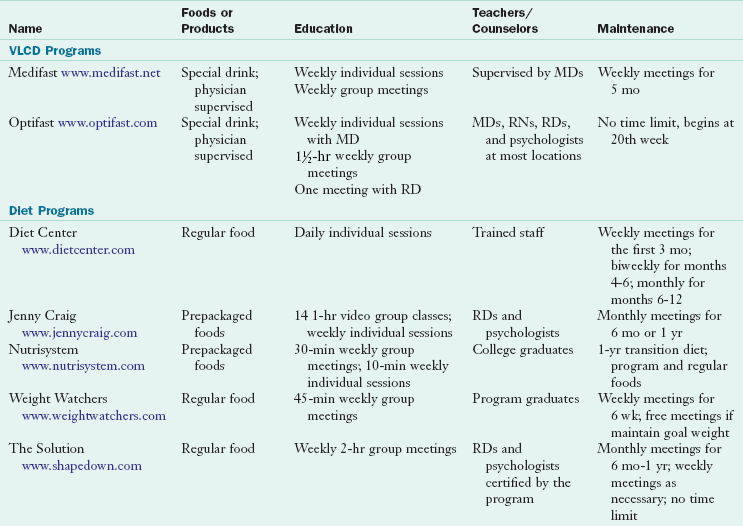
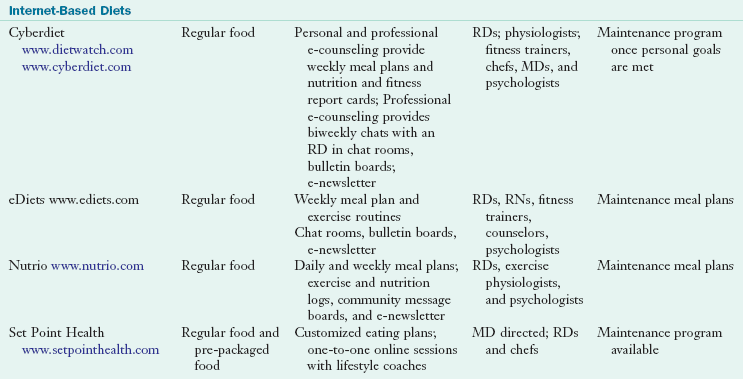
MD, Medical doctor; RD, registered dietitian; VLCD, very-low-calorie diet.
Use of the Internet has spawned a new generation of commercial programs. The importance of a tailored approach was the conclusion of an RCT comparing an Internet-based tailored weight management program with an information-only Internet weight management program based in an integrated health care setting (Rothert, 2006).
With the exception of Weight Watchers, the evidence to support the use of the major commercial and self-help weight loss programs is suboptimal. The reported results are probably a best-case scenario because many studies do not control for high attrition rates. More controlled trials are needed to assess the efficacy and cost-effectiveness of commercial programs. Thus it is important to evaluate all weight loss programs for sound nutritional practices. Consumers are savvy, and many programs have begun to report data on dropout or success rates, as well as weight maintenance.
Extreme Energy Restriction and Fasting
Extreme energy-restricted diets provide fewer than 800 kcal per day, and starvation or fasting diets provide fewer than 200 kcal per day. Fasting is seldom prescribed as a treatment; however, it is frequently invoked as a part of religious or protest regimen or in a personal effort to lose weight. Under these circumstances it is seldom continued long enough to produce the serious neurologic, hormonal, and other side effects that accompany prolonged starvation. More than 50% of the rapid weight reduction is fluid, which often leads to serious hypotension. Accumulation of uric acid can precipitate episodes of gout; gallstones can also occur. Also, as fat stores diminish, molecules are released that can affect further weight loss. See Clinical Insight: What’s in That Fat When You Lose It? Sometimes what starts as extreme energy restriction to lose weight leads to more disordered eating patterns (see Chapter 23).
Very-Low-Calorie Diets
Diets providing 200 to 800 kcal are classified as very-low-calorie diets (VLCDs). Little evidence suggests that intakes of fewer than 800 calories daily are of any advantage. Most VLCDs are hypocaloric but relatively rich in protein (0.8-1.5 g/kg IBW per day). They are designed to include a full complement of vitamins, minerals, electrolytes, and essential fatty acids, but not calories; they are given in a form that completely replaces usual food intake; and they are usually given for a period of 12 to 16 weeks. Their major advantage is rapid weight loss. Because of potential side effects, prescription of these diets is reserved for persons with a BMI of more than 30 for whom other diet programs with psychotherapy have been unsuccessful. Occasionally VLCDs may be indicated for persons with a BMI of 27 to 30 who have comorbidities or other risk factors.
The VLCD that first became popular in the early 1970s resulted in several deaths; however, improved protein formulations have increased acceptability and safety for those with morbid obesity. The VLCDs can lead to an increase of urinary ketones that interfere with the renal clearance of uric acid, resulting in increased serum uric acid levels or gout. Higher serum cholesterol levels resulting from mobilization of adipose stores pose a risk of gallstones. Additional adverse reactions include cold intolerance, fatigue, light-headedness, nervousness, euphoria, constipation or diarrhea, dry skin, anemia, and menstrual irregularities; some of these are related to triiodothyronine (thyroid) deficiency.
Even though there are significantly greater weight losses with VLCDs in the short term, there are no significant differences in the weight losses in the long term (Gilden and Wadden, 2006). Thus there does not seem to be reason to recommend these VLCDs over more moderate CR except rarely. For those who have lost weight on a VLCD, limiting dietary fat intake and maintaining physical activity are both important factors for the prevention of weight regain. To promote better weight loss, patients should limit their fat intake to less than 30% of calories and increase activity levels.
Popular Diets and Practices
Each year, new approaches to weight loss find their way to the consumer through the popular press and media. Some of the programs are sensible and appropriate, whereas others emphasize fast results with minimum effort. Some of the proposed diets would lead to nutritional deficiencies over an extended period; however, the potential health risks are seldom realized because the diets are usually abandoned after a few weeks. Diets that emphasize fast results with minimum effort encourage unrealistic expectations, setting the dieter up for failure, subsequent guilt, and feelings of helplessness at ever managing the weight problem.
The low-carbohydrate, high-fat diet restricts carbohydrates to less than 20% of calories (and often less than 10% in the beginning), and fat constitutes 55% to 65% of calories, with protein making up the balance. Protein obtained from animal sources means that fat, saturated fat, and cholesterol intakes are high. Although these diets feature high ketone production, they suppress appetite to only a minor degree. The initial rapid weight loss from diuresis is secondary to the carbohydrate restriction. Examples of severe carbohydrate-restricted diets include Dr. Atkins’ New Diet Revolution and The Carbohydrate Addict’s Diet. The Zone and the South Beach Diet both restrict carbohydrates to no more than 40% of total calories, with fat and protein providing 30% of calories each. This diet composition is claimed to keep insulin in check, which is blamed for fat storage. The diet includes generous amounts of fiber and fresh fruits and vegetables. There is attention to the kind of fat, with emphasis on monounsaturated and polyunsaturated fat and limitation of saturated fat. Weight loss ensues not because insulin is kept in a narrow range, but because calories are restricted.
The EAL examined 14 studies on the effectiveness of the low-carbohydrate diets (Atkins, South Beach). Consumption of ad libitum low-carbohydrate diets (only limiting carbohydrate) and reduced-calorie diets both lower total caloric intake. However, ad libitum low-carbohydrate diets often result in greater body weight loss and fat loss in the first 6 months. After 1 year the differences are no longer significant (ADA, 2010).
Very-low-fat diets contain less than 10% of calories from fat, such as Dr. Dean Ornish’s Program for Reversing Heart Disease and The Pritikin Program. These diets produce rapid weight loss and are very restrictive. A more popular variation limits fat to 20% of total energy intake. Because fat provides more than two times the energy per gram as protein or carbohydrate (9 kcal versus 4 kcal), an effective diet can be one that includes extensive controls on this nutrient.
Moderate-fat, balanced-nutrient reduction diets contain 20% to 30% of calories from fat, 15% to 20% of calories from protein, and 55% to 60% of calories from carbohydrate. Volumetrics, a program in this category, focuses on the energy density of foods (Rolls et al., 2005). Foods high in water content have a low energy density. These include fruits, vegetables, low-fat milk, cooked grains, lean meats, poultry, fish, and beans. Low–water containing foods that are energy dense such as potato chips, crackers, and fat-free cookies are restricted.
The U.S. Department of Agriculture (USDA) supported a scientific review of popular diets to assess their efficacy for weight loss and weight maintenance, as well as their effect on metabolic parameters, psychological well being, and reduction of chronic disease. A summary is shown in Table 22-4.
Physical Activity
Physical activity is the most variable component of energy expenditure. Increases in energy expenditure through exercise and other forms of physical activity are important components of interventions for weight loss and its maintenance. By increasing LBM in proportion to fat, physical activity helps to balance the loss of LBM and reduction of RMR that inevitably accompany intentional weight reduction. Other positive side effects of increased activity include strengthening cardiovascular integrity, increasing sensitivity to insulin, and expending additional energy and therefore calories.
Adequate levels of physical activity appear to be 60 to 90 minutes daily, as recommended by the USDA. This is also the amount of activity reported by those in the National Weight Control Registry (NWCR) who have kept off at least 10% of their weight for at least a year. Overweight and obese adults should gradually increase to these levels of physical activity. There is evidence that, even if an overweight or obese adult is unable to achieve this level of activity, significant health benefits can be realized by participating in at least 30 minutes of daily activity of moderate intensity (ADA, 2010). Therefore it is important to target these levels of physical activity to improve health-related outcomes and to facilitate long-term weight control (Jakicic, 2006).
Both aerobic and resistance training should be recommended. Resistance training increases LBM, adding to the RMR and the ability to use more of the energy intake, and it increases bone mineral density, especially for women (see Chapter 24). Aerobic exercise is important for cardiovascular health through elevated RMR, calorie expenditure, energy deficit and loss of fat. In addition to the physiologic benefits of exercise are relief of boredom, increased sense of control, and improved sense of well-being. The whole family can get involved in pleasurable activities (Figure 22-5).

FIGURE 22-5 Jogging is an excellent aerobic activity for the whole family. (Photo printed with permission from Dr. David Rivera, 2010.)
Consistency is the key to realizing the health and weight-management benefits of exercise. Previous exercise recommendations for health called for 20 to 60 minutes of moderate- to high-intensity endurance exercise performed three or more times weekly. It now appears that most health benefits can be gained by physical activity of moderate intensity (enough to expend 200 kcal daily) accumulated in intermittent short bouts, such as 20 to 30 minutes of high-intensity activity 4 to 7 days per week (Institute of Medicine, 2002). High-intensity activity is not required. Contrary to popular belief, spot reduction (i.e., reducing fat in one area of the body) is not possible with exercise; fat is burned from the largest concentrations of adipose tissue.
Pharmaceutical Management
Appropriate pharmacotherapy can augment diet, physical activity, and behavior therapy as treatment for patients with a BMI of 30 or higher or patients with 27 or higher who also have significant risk factors or disease. These agents can decrease appetite, reduce absorption of fat, or increase energy expenditure. As with any drug treatment, physician monitoring for efficacy and safety is necessary. Pharmacotherapy is not a “magic pill”; dietitians should collaborate with other health professionals regarding the use of Food and Drug Administration (FDA)–approved pharmacotherapy. Not all individuals respond, but for patients who do respond, clinical trials suggest that a weight loss of approximately 2 to 20 kg can be expected usually during the first 6 months of treatment. Medication without lifestyle modification is less effective.
Medications currently available can be categorized as central nervous system (CNS)–acting agents and non–CNS-acting agents. The CNS-acting agents fall into the categories of catecholaminergic agents, serotoninergic agents, and combination catecholaminergic-serotoninergic agents. Common side effects of CNS-acting agents are dry mouth, headache, insomnia, and constipation. Only sibutramine (Meridia) and orlistat are approved by the FDA for long-term use in the treatment of obesity (Food and Drug Administration, 2009).
Catecholaminergic drugs act on the brain, increasing the availability of norepinephrine. Drug Enforcement Agency Schedule II anorexic agents such as amphetamines have a high potential for abuse and are not recommended for obesity treatment.
Serotoninergic agents act by increasing serotonin levels in the brain. Two drugs in this category, fenfluramine (commonly used in combination with phentermine, known as “fen-phen”) and dexfenfluramine, were removed from the market in 1997 after concerns were raised regarding the possible side effects of cardiac valvulopathy, regurgitation, and primary pulmonary hypertension.
Sibutramine is a combination of catecholaminergic and serotoninergic agents, which inhibit the reuptake of serotonin and norepinephrine in the CNS to increase satiety, reduce hunger, and lessen the drop in metabolic rate that often occurs with weight loss. Because it stimulates the sympathetic nervous system, patients taking sibutramine may experience cardiovascular side effects; it is not appropriate for patients with a history of cardiovascular disorders. Sibutramine should not be used in combination with certain antidepressant agents such as monoamine oxidase inhibitors, selective serotonin reuptake inhibitors or other central-acting agents such as pseudoephedrine (Ephedra). The interaction may cause a hypertensive crisis.
Orlistat inhibits gastrointestinal lipase, which reduces approximately one third the amount of fat that is absorbed from food. Depending on the fat content of a person’s diet, this lowered absorption can represent 150 to 200 kcal/day. With lowered fat-soluble vitamin absorption, supplements are typically recommended, separated by 2 hours or more. Weight loss of 3 to 5 kg in orlistat-treated patients is common. Side effects are gastrointestinal: oily spotting, fecal urgency, and flatus with discharge. Health benefits include reduced low-density lipoprotein (LDL) cholesterol and elevated HDL cholesterol, improved glycemic control, and reduced blood pressure.
Other drugs targeting weight loss and obesity through the CNS pathways or peripheral adiposity signals are in early-phase clinical trials. Currently, the only FDA-approved OTC weight-loss product is Alli, which contains 50% of the prescription dose of orlistat. OTC and natural weight-loss products hold varying degrees of efficacy (Table 22-5).
TABLE 22-5
Nonprescription Weight Loss Products
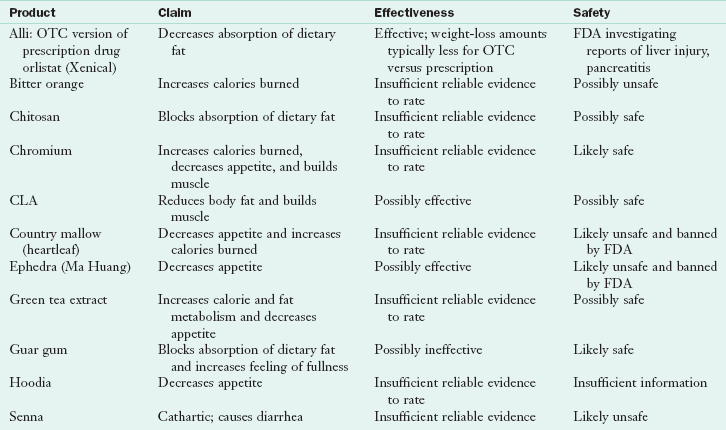
CLA, Conjugated linoleic acid; FDA, Food and Drug Administration; OTC, over the counter.
Data from Natural Medicines in the Clinical Management of Obesity, Natural Medicines Comprehensive Database, http://naturaldatabase.therapeuticresearch.com:80/ce/ceCourse.aspx?s=ND&cs=&pc=09%2D32&cec=1&pm=5, Accessed on April 19, 2011.
Other Nonsurgical Approaches
The “non-diet” paradigm maintains that the body will attain its natural weight if the individual eats healthfully, becomes attuned to hunger and satiety cues, and incorporates physical activity. This approach focuses on achieving health rather than attaining a certain weight. Advocates for this approach promote size acceptance and respect for the diversity of body shapes and sizes. Given the evidence that a 5% to 10% loss of initial weight can result in health benefits, that many persons set weight-loss goals that are unrealistic, and that fat discrimination continues to plague society, this approach may help some persons to develop a better relationship with food and a healthier perspective about their bodies.
Bariatric Surgery
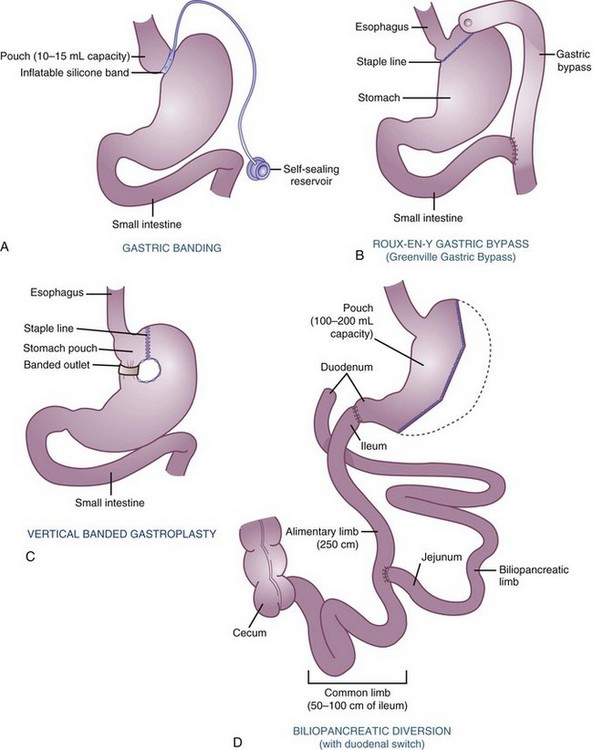
Bariatric surgery is an accepted form of treatment for extreme or class III obesity with a BMI of 40 or greater, or a BMI of 35 or greater with comorbidities. Gastroplasty procedures are restrictive because they decrease the amount of food entering the gastrointestinal tract. Other surgical procedures, such as Roux-en-Y, are restrictive and cause malabsorption because they also prevent food from being absorbed from the gastrointestinal tract.
Before any extremely obese person is considered for surgery, failure of a comprehensive program that includes CR, exercise, lifestyle modification, psychological counseling, and family involvement must be demonstrated. Failure is defined as an inability of the patient to reduce body weight by one third and body fat by one half and an inability to maintain any weight loss achieved. Such patients have intractable morbid obesity and should be considered for surgery.
If surgery is chosen, the patient is evaluated extensively with respect to physiologic and medical complications, psychological problems such as depression or poor self-esteem, and motivation. Counseling sharply improves the outcomes for dieting and drug therapy in this population (Wadden and Sarwer, 2006). Postoperative follow-up requires evaluation at regular intervals by the surgical team and a registered dietitian. In addition, behavioral or psychological support is necessary. Generally, bariatric surgery improves self-image and may alleviate depression.
Gastric Bypass, Gastroplasty, and Gastric Banding
Both gastroplasty and gastric bypass procedures reduce the amount of food that can be eaten at one time and produce early satiety (Figure 22-6). The new stomach capacity may be as small as 1 oz (20 to 30 mL) or approximately 2 tablespoons. After surgery the patient’s diet progresses from clear liquid, to full liquid, to puree, soft, and finally to a regular diet as tolerated, with emphasis on protein intake (Table 22-6). The results of gastric surgery are more favorable than those from the intestinal bypass surgery practiced during the 1970s. On average the reduction of excess body weight after gastric restriction surgery correlates to approximately 30% to 40% of initial body weight. In addition to the greater absolute weight loss observed, the gastric bypass tends to have sustainable results with significant resolution of hypertension, type 2 diabetes mellitus, osteoarthritis, back pain, dyslipidemia, cardiomyopathy, nonalcoholic steatohepatitis, and sleep apnea. However, late complications may be seen, such as vitamin deficiency, electrolyte problems or even intestinal failure.
TABLE 22-6
Diet Progression After Gastric Bypass
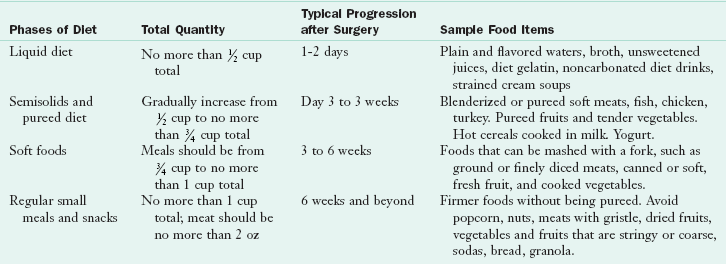
Adapted from Mayo Clinic, Gastric bypass diet. Accessed 11 July 2010 from http://www.mayoclinic.com/health/gastric-bypass-diet/my00827.
Gastroplasty reduces the size of the stomach by applying rows of stainless-steel staples to partition the stomach and create a small gastric pouch, leaving only a small opening (0.8-1 cm) into the distal stomach. This opening may be banded by a piece of mesh to prevent it from enlarging during the years after surgery. Vertical-banded gastroplasty is the most popular surgery. In the lap-band procedure, also called gastric banding, the band creating the reduced stomach pouch can be adjusted so that the opening to the rest of the stomach can be made smaller or enlarged. The band, filled with saline, has a tube exiting from it to the surface of the belly just under the skin; this allows for the injection of additional fluid or reduction of fluid into the lap band. Patients who undergo the banding procedures will not require folic acid, iron, or vitamin B12 replacements
Gastric bypass involves reducing the size of the stomach with the stapling procedure, but then connecting a small opening in the upper portion of the stomach to the small intestine by means of an intestinal loop. The original operation in the late 1960s evolved into the Roux-en-Y gastric bypass. Because use of the lower part of the stomach is omitted, the gastric bypass patient may have dumping syndrome as food empties quickly into the duodenum (see Chapter 28). The tachycardia, sweating, and abdominal pain are so negative that they motivate the patient to make the appropriate behavioral changes and refrain from overeating. However, patients tend to choose liquids; weight loss can be deterred by drinking too much calorically dense liquid such as milk shakes and soft drinks. Eventually the pouch expands to accommodate 4 to 5 oz at a time. Frequently, gastric bypass surgery leads to bloating of the pouch, nausea, and vomiting. A postsurgical food record noting the tolerance for specific foods in particular amounts helps in devising a program to avoid these episodes.
Completion of bypass surgery leads to malnutrition, which requires lifelong follow-up and monitoring by the multidisciplinary team. Nutritional status should be evaluated periodically by a dietitian. Monitoring should include an assessment of total body-fat loss, potential anemia, and deficiencies of potassium, magnesium, folate, and vitamin B12. Ice-cube pica and iron deficiency anemia are possible (Kushner and Shanta Retelny, 2005). Supplementation is necessary. An adult vitamin-mineral supplement (one liquid or chewable tablet twice daily) containing 1200-1500 mg calcium citrate,1000-2000 IU vitamin D, 500 mcg vitamin B12, 400 mcg folic acid, and 65-80 mg elemental iron with vitamin C is suggested (Kuluck et al., 2010; Snyder-Marlow et al., 2010.)
Liposuction
Liposuction (or liposculpture) involves aspiration of fat deposits by means of a 1- to 2-cm incision through which a tube is fanned out into the adipose tissue. The most successful operations are performed on younger persons with only small amounts of fat to be removed, where the elastic properties of the skin are able to allow tightening over the aspirated areas. It is not usually a weight-reduction technique but rather a cosmetic surgery because usually only approximately 5 lb of fat are removed at a time. Deaths, severe infections, cellulitis, and hemorrhage have occurred.
Common Problems in Obesity Treatment
Prognosis for maintaining reduced weight is typically poor. Continued dieting, with repeated ups and downs, leads gradually to a net increase in body fat and thus to a health risk for hyperlipidemia, hypertension, diabetes, and even osteoarthritis. Women having bariatric surgery had lower serum 25-hydroxyvitamin D (s25D) and higher parathyroid hormone (sPTH). The major determinant of s25D and sPTH was weight. Hyperparathyroidism in obesity did not indicate vitamin D insufficiency. Low s25D was not associated with comorbid conditions, apart from osteoarthritis (Grethen, 2011).
Maintaining Reduced Body Weight
Energy requirements for weight maintenance after weight reduction appear to be 25% lower than at the original weight. The net effect is that reduced-obese persons are faced with the necessity of maintaining a reduced energy intake even after the desired weight has been lost. Whether this reduced intake must be maintained indefinitely is not known.
The NWCR consists of more than 5000 individuals who have been successful in long-term weight loss maintenance. The purpose of establishing the NWCR is to identify the common characteristics of those who succeed in long-term weight loss maintenance. There is very little similarity in how these individuals lost weight but there are some common behaviors they all have for keeping their weight off. Lifestyle modification and a sense of self-efficacy appear to be essential. To maintain their weight loss, NWCR participants report:
1. Eating a relatively low-fat (24%) diet
2. Eating breakfast almost every day
3. Weighing themselves regularly, usually once per day to once per week
4. Engaging in high levels (60 to 90 minutes/day) of physical activity
Weight loss maintenance may get easier over time; after individuals have successfully maintained their weight loss for 2 to 5 years, the chance of longer-term success greatly increases (Wing and Phelan, 2005). Support groups are valuable for reduced-obese persons who are maintaining a new lower weight; they help individuals facing similar problems. Two self-help support groups are Overeaters Anonymous and Take Off Pounds Sensibly. These groups are inexpensive, continuous, include a “buddy system,” and encourage participation on a regular basis or as often as needed. Weight Watcher programs offer free lifelong maintenance classes for those who have reached and are maintaining their goal weights.
Interestingly, boring and monotonous diets can be a management strategy. Diets that are repetitious without change from meal to meal are one consideration because people tend to overeat when they have many mealtime choices. Overall, a common sense approach is needed. Some phrases can be shared with individuals who are trying to maintain their weight loss, including:
Plateau Effect
A common experience for the person in a weight-reduction program is arrival at a weight plateau, when weight remains at the same level for a long period. Eventually weight loss halts completely. One theory is that interim plateaus reflect a reduction of lipid in individual adipocytes to some level that signals metabolic adjustment and weight maintenance. Another theory is that there is a release of toxins from adipose tissue that act as endocrine disruptors and inflammatory agents and affect subsequent weight loss. See Clinical Insight: What’s in That Fat When You Lose It? To move out of this phase usually requires increasing the activity level.
Any weight loss, whether fast or slow, results in a loss of the extra muscle that has developed to support the excess adipose tissue. Because this extra LBM has contributed to an increased metabolic rate, RMR decreases as LBM is lost. The fact that RMR decreases rapidly at the onset of a weight-reduction diet, by as much as 15% within 2 weeks, indicates that other adaptations to the lower weight and the threat of deprivation are taking place.
Other factors join to decrease RMR and limit effectiveness of the restricted energy intake. A decrease in the total kilocalories ingested results in a decrease in total energy expenditure. Because a body that weighs less requires less energy expenditure to move around, the cost of physical activity is also less. A state of equilibrium is eventually reached at which the energy intake is equal to energy expenditure. Unless a change is made in either nutritional intake or physical activity, weight loss stops at this point.
Weight Cycling
Repeated bouts of weight loss and regain, known as weight cycling or the yo-yo effect, occurs in men and women and is common in both overweight and nonoverweight individuals. The effect of weight cycling appears to result in increased body fatness and weight with the end of each cycle. There are metabolic and psychological effects that are undesirable.
Weight Management in Children
Almost 32% of US children ages 2-19 are overweight or obese (Ogden et al, 2010). Obese children are often the targets of discrimination. Childhood obesity increases the risk of obesity in adulthood. For the child who is obese after 6 years of age, the probability of obesity in adulthood is significantly greater if either the mother or the father is obese.
The BMI tables for determining childhood obesity are available for use by health care practitioners (see Appendixes 12 and 16). Children whose BMI is greater than the 85th percentile are six times more likely to be overweight later (Nadir et al., 2006). In addition, children who have growth failure and undernutrition in utero or in the early years of life tend to become overweight in later childhood with subsequent risks of elevated blood pressure, lipid, and glucose levels (Stein et al., 2005). Obesity that begins in childhood tends to lead to hypertension, elevated LDL cholesterol, and TGs in adults (Thompson et al., 2007).
Children with a body mass index (BMI) in the 85th percentile or higher with complications of obesity, or with a BMI in the 95th percentile or higher with or without complications, should be carefully assessed for genetic, endocrinologic, and psychologic conditions, and secondary complications such as hypertension, dyslipidemias, sleep apnea, and orthopedic problems. If the complications cause serious morbidity and require rapid weight loss, referral to a pediatric obesity specialist may be necessary. Otherwise, parent and child readiness to make changes should be evaluated and eating and activity patterns carefully assessed.
Once assessment is complete, treatment can begin. The primary goal of treatment is to achieve healthy eating and activity, not to achieve an IBW. For children 7 years of age and younger the goal is prolonged weight maintenance or slowing of the rate of weight gain, which allows for a gradual decline in BMI as children grow in height. This is an appropriate goal in the absence of any secondary complications of obesity. However, if secondary complications are present, children in this age group may benefit from weight loss if their BMI is at the 95th percentile or higher. For children older than 7 years, prolonged weight maintenance is appropriate if their BMI is between the 85th and 95th percentile and if they have no secondary complications. If a secondary complication is present or if BMI is at the 95th percentile or above, weight loss (about 1 lb per month) is advised. If the weight appropriate for the child’s anticipated adult height has already been reached, maintenance at that weight should be the lifetime goal. The child who already exceeds an optimal adult weight can safely experience a slow weight loss of 10 to 12 lb per year until the optimal adult weight is reached. Balanced micronutrient intake for children includes 45% to 60% of kcal from carbohydrate, 25% to 40% from fat, and 10% to 35% from protein.
The child who needs to reduce weight is going to require more attention from family and health professionals. This attention should be directed to all the areas mentioned previously, with family modification of eating habits and increased physical activity. The program should be long term over the entire growth period and perhaps longer.
Inactivity is often coupled with sedentary hobbies, excessive TV watching, or prolonged sitting in front of a computer or game screen. However, there is a new theory that physical inactivity appears to be the result of fatness rather than its cause (Metcalf et al., 2010). This requires further research, but does suggest that factors other than inactivity may be more important in obesity development in children. See New Directions—Organizing to Solve the Childhood Obesity Problem “Within a Generation.”
Weight Imbalance: Excessive Leanness or Unintentional Weight Loss
Almost eclipsed by the attention focused on obesity is the need for some people to gain weight. The term underweight is applicable to those who are 15% to 20% or more below accepted weight standards. Because underweight is often a symptom of disease, it should be assessed medically. A low BMI (<18.5) is associated with greater mortality risk than that of individuals with optimal BMI (18.5-24.9), especially with aging and in the elderly. Undernutrition may lead to underfunction of the pituitary, thyroid, gonads, and adrenals. Other risk factors include loss of energy and susceptibility to injury and infection, as well as a distorted body image and other psychological problems (see Chapter 21).
Cause
Underweight or unintentional weight loss can be caused by (1) inadequate oral food and beverage intake, with insufficient quantities to match activity; (2) excessive physical activity, as in the case of compulsive athletic training; (3) inadequate capacity for absorption and metabolism of foods consumed; (4) a wasting disease that increases the metabolic rate and energy needs, as in cancer, acquired immune deficiency syndrome (AIDS), or hyperthyroidism; or (5) excess energy expenditure during psychological or emotional stress (see Chapter 23).
Assessment
Assessing the cause and extent of underweight before starting a treatment program is important. A thorough history and pertinent medical tests usually determine whether underlying disorders are causing the underweight. From anthropometric data such as arm muscle and fat areas, it is possible to determine whether health-endangering underweight really exists. Assessment of body fatness is useful, especially in dealing with the patient who has an eating disorder (see Chapter 23). Biochemical measurements will indicate whether malnutrition accompanies the underweight (see Chapter 8). Use of an eating inventory questionnaire can identify persons at risk of unintentional weight loss (Hays et al., 2006).
Management
Any underlying cause of unintentional weight loss or low BMI must be the first priority. A wasting disease or malabsorption requires treatment. Nutrition support and dietary changes are effective along with treatment of the underlying disorder (Table 22-7).
TABLE 22-7
Nutrition Management of Unintentional Weight Loss
| Concern | Tips |
| Anxiety, stress, depression | Antidepressants can help; monitor choice to be sure they do not contribute to weight loss. |
| Cancer | Gastrointestinal cancers are especially detrimental. Some treatments and medications can cause loss of appetite, as can the cancer itself. |
| Celiac disease | Ensure that all gluten-containing foods and ingredients are eliminated from the diet. |
| Changes in activity level or dietary preparation methods | Avoid skipping meals; prepare foods with high energy density. |
| Diabetes, new onset | See a physician; monitor medications and meals accordingly. |
| Dysphagia or chewing difficulties | Alter food and liquid textures accordingly to improve chewing and swallowing capability. |
| Hyperthyroidism | Too much thyroxine can cause weight loss. |
| Inflammatory bowel disease | Check medications and treatments to determine if new choices are in order. |
| Intestinal ischemia | See a physician. |
| Medications | Some medications can cause weight loss; check with the physician; add snacks or enhanced meals if needed. |
| Nausea and vomiting | Infections, other illnesses, hormonal changes, and some medications cause nausea and vomiting; small, frequent meals are useful; serve liquids between meals instead of with meals to reduce fullness. |
| Pancreatitis and cystic fibrosis | Monitor for sufficiency of pancreatic enzyme replacement. |
If the cause of the underweight is inadequate oral food and beverage intake, activity should be modified and psychological counseling started if necessary.
Appetite Enhancers
The FDA has approved orexigenic agents that include corticosteroids, cyproheptadine, loxiglumide (cholecystokinin antagonist), megestrol acetate, mirtazapine, dronabinol, oxoglutarate, anabolic agents (testosterone or Anadrol), oxandrin, and growth hormone. Use of orexigenic agents for weight loss in seniors is saved for those whose conditions are refractory to usual treatments. One third of older adults, especially women, exhibit weight loss in combination with depression. Mirtazapine is an effective antidepressant that is well tolerated and increases appetite. Dronabinol is used for chemotherapy-induced nausea and vomiting in cancer and AIDS patients; it has been shown to induce weight gain in patients with dementia.
High-Energy Diets
A careful history may reveal inadequacies in dietary habits and nutritional intakes. Meals should be scheduled and relaxed instead of hastily planned or quickly eaten. The underweight person frequently must be encouraged to eat, even if not hungry. The secret is to individualize the program with readily available foods that the individual really enjoys, with a plan for regular eating times throughout the day. In addition to meals, snacks are usually necessary to adequately increase the energy intake. Often a liquid supplement taken with meals or between meals is effective; it is nutritious as well as easy to prepare and consume.
The energy distribution of the diet should be approximately 30% of the kilocalories from fat, with the majority from monounsaturated or polyunsaturated sources and at least 12% to 15% of the kilocalories from protein. A basic vitamin and mineral supplement may be encouraged. In addition to an intake according to estimated energy requirements for the present weight, 500 to 1000 extra kilocalories per day should be planned. If 2400 kcal maintains the current weight, 2900 to 3400 kcal would be required for weight gain. The intake should be increased gradually to avoid gastric discomfort, discouragement, electrolyte imbalances, and heart dysfunction. Step-up plans are outlined in Table 22-8.
In underweight children, nonnutritional factors, insufficient caloric intake, excessive nutrient losses, and abnormal energy metabolism may contribute to growth failure and morbidity. Thus adequate nutritional support should be an integral part of the management plan. Lipid-based nutrient supplements are fortified products that are often ready-to-use therapeutic foods or highly concentrated supplements that can be administered at “point of service” or emergency settings (Chaparro and Dewey, 2010).
http://www.americaonthemove.org
American Society of Bariatric Surgery
Calorie Restriction Society International
Centers for Disease Control and Prevention (CDC)
International Association for the Study of Obesity
International Obesity Task Force
National Heart, Lung, and Blood Institute: Identification, Evaluation, and Treatment of Overweight and Obesity in Adults
http://www.nhlbi.nih.gov/guidelines/obesity/ob_home.htm
Weight Control Network: National Institute of Diabetes and Digestive and Kidney Disease
References
Adams, KF, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355:763.
American Dietetic Association. Evidence-based nutrition practice guideline on adult weight management, dietary intervention algorithm. www.adaevidencelibrary.com/topic.cfm?cat=2849. [and copyrighted by the American Dietetic Association. Accessed 10 July 2010].
Anschultz, DJ, et al. Susceptibility for thin ideal media and eating styles. Body Image. 2008;5:70.
Ashley, EA, et al. Clinical assessment incorporating a personal genome. Lancet. 2010;375:1497.
Barber, N. The evolutionary psychology of physical attractiveness: sexual selection and human morphology. Evol Hum Behav. 1995;16:395.
Barouki, R. Linking long-term toxicity of xeno-chemicals with short-term biological adaptation. Biochimi. 2010;99:1222.
Bonafini, BA, Pozzilli, P. Body weight and beauty: the changing face of the ideal female body weight. Obes Rev. 2010. [[Epub ahead of print.] 19 May].
Berkel, LA, et al. Behavioral interventions for obesity. J Am Diet Assoc. 2005;105:S35.
Bjorntorp, P, Sjostrom, L. Number and size of adipose fat cells in relation to metabolism in human obesity. Metabolism. 1971;20:703.
Blackburn, GL. Break through your set point. New York: Harper-Collins; 2008.
Brown, I. Nurses’ attitudes toward adult patients who are obese: literature review. J Adv Nurs. 2006;55:265.
Carr, D, Friedman, MA. Is obesity stigmatizing? Body weight, perceived discrimination, and psychological well-being in the United States. J Health Soc Behav. 2005;46:264.
Centers for Disease Control and Prevention (CDC). Overweight and obesity trends. www.cdc.gov/nccdphp/obesity/trend/index.htm, 2007. [Accessed 12 May 2010 from].
Chan, DC, et al. Effect of ezetimibe on hepatic fat, inflammatory markers, and apolipoprotein B-100 kinetics in insulin-resistant obese subjects on a weight loss diet. Diab Care. 2010;33:1134.
Chaparro, CM, Dewey, KG. Use of lipid-based nutrient supplements (LNS) to improve the nutrient adequacy of general food distribution rations for vulnerable sub-groups in emergency settings. Matern Child Nutr. 2010;6:1S.
Couce, ME, et al. Is ghrelin the culprit for weight loss after gastric bypass surgery? A negative answer. Obes Surg. 2006;16:870.
De Luis, DA, et al. Influence of ALA54THR polymorphism of fatty acid binding protein 2 on lifestyle modification response in obese subjects. Ann Nutr Metab. 2006;50:354–360.
Deurenberg, P, Deurenberg-Yap, M. Validity of body composition methods across ethnic population groups. Acta Diabetol. 2003;40:2465.
Enriori, JP, et al. Leptin resistance and obesity. Obesity. 2006;14:254s.
Food and Drug Administration (FDA). FDA approves orlistat for over-the-counter use. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2007/ucm108839.htm, 2009. [Accessed 11 July 2010 from].
Ferguson, JF, et al. Gene-nutrient interactions in the metabolic syndrome: single nucleotide polymorphisms in ADIPOQ and ADIPOR1 interact with plasma saturated fatty acids to modulate insulin resistance. Am J Clin Nutr. 2010;91:794.
Fontana L: Calorie restriction, endurance exercise, and successful aging. 62nd Annual Scientific Meeting of the Gerontological Society of America, Atlanta, Ga, 21-22 November 2009.
Frayling, TM, et al. A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science. 2007;316:389.
Garaulet, M, et al. CLOCK genetic variation and metabolic syndrome risk: modulation by monounsaturated fatty acids. Am J Clin Nutr. 2009;90:1466.
Garaulet, M, et al. The chronobiology, etiology and pathophysiology of obesity. Int J Obes (Lond). 22 June 2010. [[Epub ahead of print.]].
Gilden, TA, Wadden, TA. The evolution of very-low-calorie diets: an update and meta-analysis. Obesity. 2006;14:1283.
Goldstein, BJ, Scalia, R. Adipokines and vascular disease in diabetes. Curr Diab Rep. 2007;7:25.
Goodpaster, BH, et al. Obesity, regional fat distribution, and the metabolic syndrome in older men and women. Arch Int Med. 2005;165:777.
Gower, BA, et al. Changes in intra-abdominal fat in early postmenopausal women: effects of hormone use. Obesity. 2006;14:1046.
Grethen, E, McClintock, R, Gupta, CE, Jones, R, Cacucci, BM, Diaz, D, Fulford, AD, Perkins, SM, Considine, RV, Peacock, M. Vitamin D and Hyperparathyroidism in Obesity. Clin Endocrinol Metab. 2011. [Feb 16].
Grimble, RF. The true cost of in-patient obesity: impact of obesity on inflammatory stress and morbidity. Proc Nutr Soc. 2010;69:511.
Grun, F. Obesogens. Curr Opin Endocrinal Diabetes Obes. 2010;17:453.
Grun, F, Blumberg, B. Environmental obesogens: organotins and endocrine disruption via nuclear receptor signaling. Endocrinology. 2006;147:s50.
Hansen, JB, Kristiansen, K. Regulatory circuits controlling white versus brown adipocyte differentiation. Biochem J. 2006;398:153.
Hays, NP, et al. Eating behavior and weight change in healthy postmenopausal women: results of a 4-year longitudinal study. J Gerontol A Biol Sci Med Sci. 2006;61:608.
Heilbronn, LK, et al. Effect of 6-month calorie restriction on biomarkers of longevity, metabolic adaptation, and oxidative stress in overweight individuals: a randomized, controlled trial. JAMA. 2006;295:1539.
Hyman M: Systems biology, toxins, obesity, and functional medicine. The Proceedings From the 13th International Symposium of The Institute for Functional Medicine, 2006.
Imbeault, P, et al. Weight loss-induced rise in plasma pollutant is associated with reduced skeletal muscle oxidative capacity. Am J Physiol Endocrinol Metab. 2002;282:E574.
Institute of Medicine, Food and Nutrition Board. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. Washington, DC: National Academies Press; 2002.
Jacobs, EJ, et al. Waist circumference and all-cause mortality in a large US cohort. Arch Intern Med. 2010;170:1293.
Jakicic, JM. Treatment and prevention of obesity: what is the role of exercise? Nutr Rev. 2006;64:S57.
Jee, SH, et al. Body-mass index and mortality in Korean men and women. N Engl J Med. 2006;355:779.
Keys, A. The biology of human starvation. Minneapolis: University of Minnesota Press; 1950.
Kuluck, D, et al. The bariatric surgery patient: a growing role for registered dietitians. J Am Diet Assoc. 2010;110:593.
Kushner, RF, Shanta Retelny, V. Emergence of pica (ingestion of non-food substances) accompanying iron deficiency anemia after gastric bypass surgery. Obes Surg. 2005;15:1491.
Latner, JD, et al. Stigmatized students: age, sex, and ethnicity effects in the stigmatization of obesity. Obes Res. 2005;13:1226.
Levine, JA. Nonexercise activity thermogenesis—liberating the life-force. J Intern Med. 2007;262:273.
Mayo Clinic. Calorie restriction for anti-aging. Accessed 16 April 2010 from http://www.mayoclinic.com/.
Metcalf, BS, et al. Fatness leads to inactivity, but inactivity does not lead to fatness: a longitudinal study in children (EarlyBird 45). Arch Dis Child. 2010. [[Epub ahead of print.] 23 June].
Nadir, PR, et al. Identifying risk for obesity in early childhood. Pediatrics. 2006;118:e594.
Newby, PK, et al. Longitudinal changes in food patterns predict changes in weight and body mass index and the effects are greatest in obese women. J Nutr. 2006;136:2580.
Nicklas, B. Polymorphisms of angiotensinogen and angiotensin-converting enzyme associated with lower extremity arterial disease in the health, aging and body composition study. J Hum Hypertens. 2007;1(8):673.
Ogden, CL, et al. Prevalence of high body mass index in US children and adolescents, 2007-2008. JAMA. 2010;303:242.
Ogden, CL, et al. Prevalence and trends in overweight among US children and adolescents, 1999-2000. JAMA. 2002;288:1728.
Pasarica, M, Dhurandhar, NV. Infectobesity: obesity of infectious origin. Adv Food Nutr Res. 2007;52:61.
Phelan, JP, Rose, MR. Calorie restriction increases longevity substantially only when the reaction norm is steep. Biogerontology. 2006;7:161.
Prentice, AM. Early influences on human energy regulation: thrifty genotypes and thrifty phenotypes. Physiol Behav. 2005;86:640.
Racette, SB, et al. Abdominal adiposity is a stronger predictor of insulin resistance than fitness among 50-95 year olds. Diabetes Care. 2006;29:673.
Rhéaume, C, Arsenault, BJ, Dumas, MP, Pérusse, L, Tremblay, A, Bouchard, C, Poirier, P, Després, JP. Contributions of Cardiorespiratory Fitness and Visceral Adiposity to Six-Year Changes in Cardiometabolic Risk Markers in Apparently Healthy Men and Women. Clin Endocrinol Metab. 2011. [Feb 16].
Rolland-Cachera, MF. Rate of growth in early life: a predictor of later health? Adv Exp Med Biol. 2005;569:35.
Rolls, BJ, et al. Provision of foods differing in energy density affects long-term weight loss. Obes Res. 2005;13:1052.
Rothert, K, et al. Web-based weight management programs in an integrated health care setting: a randomized controlled trial. Obesity. 2006;14:266.
Snyder-Marlow, G, et al. Nutrition care for patients undergoing laparoscopic sleeve gastrectomy for weight loss. J Am Diet Assoc. 2010;110:6000.
Statistics Canada. Accessed 7 July 2010 from http://www.statcan.gc.ca/pub/82-620-m/2005001/pdf/4224906-eng.pdf.
Stein, AD, et al. Childhood growth and chronic disease: evidence from countries undergoing nutrition transition. Matern Child Nutr. 2005;1:177.
Stevens, JM, Vidal-Puig, AJ. An update on visfatin/pre-B cell colony-enhancing factor, an ubiquitously expressed, illusive cytokine that is regulated in obesity. Curr Opin Lipidol. 2006;17:128.
Stiegler, P, Cunliffe, A. The role of diet and exercise for the maintenance of fat-free mass and resting metabolic rate during weight loss. Sports Med. 2006;36:239.
Stunkard, A, Lu, XY. Rapid changes in night eating: considering mechanisms. Eat Weight Disord. 2010;15:e2.
Task Force on Childhood Obesity, Domestic Policy Council: Solving the Problem of Childhood Obesity Within a Generation—White House Task Force on Childhood Obesity—Report to the President, May, 2010.
Thomas, S, et al. Bariatric surgery and the gut hormone response. Nutr Clin Pract. 2010;25:2.
Thompson, DR, et al. Childhood overweight and cardiovascular disease risks: the National Heart, Lung and Blood Institute Growth and Health Study. J Pediatr. 2007;150:18.
Tremblay, A, et al. Thermogenesis and weight loss in obese individuals: a primary association with organochlorine pollution. Int J Obes Relat Metab Disord. 2004;228:936.
Van Dam, RM, et al. The relationship between overweight in adolescence and premature death in women. Ann Intern Med. 2006;145:91.
Van Ginnekin, V, et al. Infectobesity: viral infections (especially with human adenovirus-36: Ad-36) may be a cause of obesity. Med Hypotheses. 2009;72:383.
Varady, KA, et al. Degree of weight loss required to improve adipokine concentrations and decrease fat cell size in severely obese women. Metabolism. 2009;58:1096.
Wadden, T, Sarwer, DB. Behavioral assessment of candidates for bariatric surgery: a patient-oriented approach. Surg Obes Relat Dis. 2006;2:171.
Wilmore, JH, et al. Body composition: a round table. The Physician and Sportsmedicine. 1986;14(3):144.
Wing, RR, Phelan, S. Long-term weight loss maintenance. Am J Clin Nutr. 2005;82:222S.