Health Promotion of the Adolescent and Family
Promoting Optimum Growth and Development
Promoting Optimum Health During Adolescence
Adolescents’ Perspectives on Health
Factors That Promote Adolescent Health and Well-Being
Health Concerns of Adolescence
Parenting and Family Adjustment
Intentional and Unintentional Injury
Dietary Habits, Eating Disorders, and Obesity
Sexual Behavior, Sexually Transmitted Infections, and Unintended Pregnancy
Use of Tobacco, Alcohol, and Other Substances
Physical, Sexual, and Emotional Abuse
Infectious Diseases and Immunizations
http://evolve.elsevier.com/wong/ncic
Adolescent Pregnancy, Ch. 20
Eating Problems and Disorders, Ch. 21
Health Problems of the Female Reproductive System, Ch. 20
Health Problems of the Male Reproductive System, Ch. 20
Health Problems Related to Sexuality, Ch. 20
Hyperlipidemia, Ch. 34
Immunizations, Ch. 12
Injury Prevention, Ch. 17
Obesity, Ch. 21
Precocious Puberty, Ch. 38
Problems Related to Sports Participation, Ch. 39
Sexually Transmitted Infections, Ch. 20
Substance Abuse, Ch. 21
Suicide, Ch. 21
Systemic Hypertension, Ch. 34
Promoting Optimum Growth and Development
Adolescence is a period of transition between childhood and adulthood, a time of profound biologic, intellectual, psychosocial, and economic change. During this period individuals reach physical and sexual maturity, develop more sophisticated reasoning abilities, and make educational and occupational decisions that will shape their adult careers. The changes of adolescence have important implications for understanding the kinds of health risks to which young people are exposed, the health-enhancing and risk-taking behaviors in which they engage, and the major opportunities for health promotion among this population.
In the process of examining widely accepted theories of adolescent development, researchers have challenged many popular notions. For example, a common belief is that teenagers’ behaviors are overwhelmingly determined by “raging hormones,” and that adolescence is a period when rebellious and risky behavior is the norm. Both notions are misguided, but these mistaken beliefs are not benign. They may have detrimental effects on attitudes and interactions with individual adolescents and on policy and program development. Although current research supports a more positive view of this life period, it also confirms that adolescence involves a complex interplay of biologic, cognitive, psychologic, and social change, perhaps more so than at any other time of life. Unfortunately, some perceive that the United States as a society often has provided little help to individuals as they try to cope with the normal changes of adolescence.
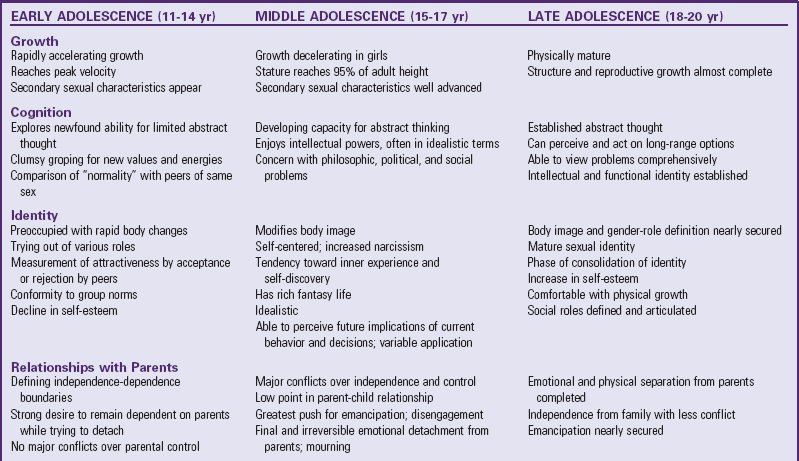
Change during adolescence occurs on multiple levels. On the individual level, changes include biologic maturation, cognitive development, and psychologic development. Change also occurs in the social contexts of adolescents’ families, peer groups, schools, and workplaces. Adolescence involves three distinct subphases: early adolescence (ages 11 to 14), middle adolescence (ages 15 to 17), and late adolescence (ages 18 to 20). The changes, opportunities, pressures, skills, and resources available to young people differ during these subphases. For example, early adolescence is characterized primarily by the changes of puberty and responses to those changes. Middle adolescence is characterized by transition to a dominant peer orientation, with all the stereotypic adolescent preoccupations of music, technology, dress and appearance, language, and behavior. Late adolescence involves transition into adulthood, including taking on adult work roles and developing adult relationships (Table 19-1).
Biologic Development
![]() Neuroendocrine Events of Puberty
Neuroendocrine Events of Puberty
The fundamental biologic changes of adolescence are collectively referred to as puberty. Puberty involves a predictable sequence of hormonal and physical changes that occur universally over a defined period of time. It encompasses both sexual maturation and physical growth. It is generally accepted that the events of puberty are triggered by hormonal influences and are controlled by the anterior pituitary gland in response to a stimulus from the hypothalamus.
![]() Animation—Ovarian Growth in the Child
Animation—Ovarian Growth in the Child
Puberty begins as some not completely understood cluster of events triggers the production of gonadotropin-releasing hormone (GnRH) by the hypothalamus (Fig. 19-1). GnRH travels through a network of capillaries to the anterior pituitary gland, where it stimulates the production and secretion of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Increasing levels of FSH and LH in the blood stimulate gonadal response. For females, FSH stimulates growth of ovarian follicles and production of estrogen. LH initiates ovulation, the formation of the corpus luteum, and progesterone production. For males, LH acts on testicular Leydig cells, prompting maturation of the testicles and testosterone production. FSH, acting with LH, stimulates sperm production. The sex steroids—estrogen, progesterone, and testosterone and other androgens—are released from the gonads and effect biologic changes in various organs, including muscles, bones, skin, and hair follicles. Increasing serum levels of sex steroids also provide feedback to the hypothalamus, causing decreases in GnRH secretion. When serum sex hormone levels decrease, the hypothalamus is stimulated to increase GnRH secretion, again initiating the sequence that produces the appropriate gonadal responses.
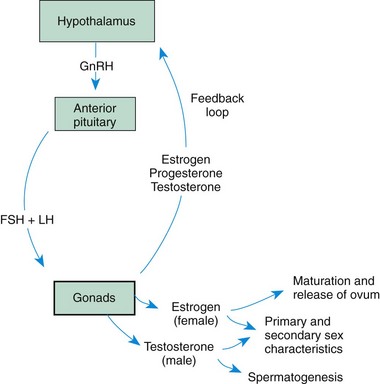
Fig. 19-1 Hormonal interaction between hypothalamus, pituitary, and gonads. GnRH, Gonadotropin-releasing hormone; FSH, follicle-stimulating hormone; LH, luteinizing hormone.
Initiation of Puberty: The precise mechanism that institutes the changes at puberty is not completely understood. Although the pituitary gland and gonads are capable of mature function and can respond to stimuli at any age, the hypothalamic-pituitary-gonadal system is kept in a dormant state throughout childhood by some central nervous system inhibitory mechanism in the region of the hypothalamus. It is believed that the receptor sites in the hypothalamus are so highly sensitive that the most minute quantities of circulating sex hormones are sufficient to inhibit the secretion of GnRH during childhood. The hypothalamus loses this negative sensitivity at puberty, which allows the hypothalamic-pituitary-gonadal mechanism to attain full secretory function. As puberty progresses, the pituitary and gonads become increasingly sensitive to positive hormonal stimulation.
Changes in Reproductive Hormones
Females: The primary sexual characteristic in girls is the development and release of an egg, or ovum, from the ovaries approximately every 28 days. Beginning in early puberty, FSH stimulates estrogen production by the ovaries. However, concentrations of estrogen do not reach levels high enough to cause ovulation. By the time girls reach midpuberty, the body produces estrogen in larger amounts. This quantity of estrogen production results in the building of an endometrial lining of the uterus and first menstruation, or menarche. At menarche, ova still do not generally mature enough to be released. However, as puberty progresses, usually one ovarian follicle becomes dominant during each menstrual cycle and produces increasing amounts of estrogen during the early-cycle, follicular phase. This follicle then releases an ovum, a process termed ovulation, around day 14 of the menstrual cycle. After ovulation the follicle involutes and its estrogen production decreases. This leads to a drop in serum estrogen and progesterone. The pituitary gland responds to the drop in these hormone levels with increased production of FSH, initiating the start of a new menstrual cycle.
By direct action, estrogens cause growth and development of the vagina, uterus, and fallopian tubes. The skin of the labia majora, as well as that of the breast areola and nipples, grows and darkens under the influence of estrogen. Estrogen is responsible for breast enlargement. Estrogen also promotes the growth of pubic and axillary hair, and widening of the hips. At low levels estrogen tends to stimulate skeletal growth in both boys and girls, but at higher levels it inhibits growth.
Males: The primary male sexual characteristic is the development of viable sperm. During puberty, FSH acts on testicular cells, stimulating the production of viable sperm. FSH and LH also act on a different group of testicular cells, resulting in increased production and secretion of testosterone. In this process of sexual development, boys do not experience a discrete event analogous to menstruation or ovulation in girls. However, just as the production of a mature ovum tends to occur 1 year or more after menarche in girls, the production of viable sperm tends to follow boys’ first ejaculations. The capacity to ejaculate appears relatively early in boys’ sexual development, approximately 1 year after initial testicular enlargement and the appearance of pubic hair. From a clinical perspective, however, an adolescent should be considered potentially fertile with a first menstrual period or a first ejaculation.
Testosterone and other androgens have a direct impact on growth of the penis, scrotum, prostate, and seminal vesicles of the testicles. The tremendous growth-promoting properties of these hormones also result in rapid increases in muscle mass, skeletal growth, bone age, and bone density. In both sexes androgens are responsible for the development of pubic, axillary, facial, and body hair. Clinically, increased activity of androgens is associated with pubertal conditions such as acne, body odor, deepening of the voice, a spurt in height, and an increase in red blood cell levels.
Pubertal Sexual Maturation
Increases in reproductive hormones are responsible for dramatic changes in secondary sexual characteristics that occur during puberty. As with general growth, development of secondary sexual characteristics occurs in a predictable sequence. This sequence has been divided into a series of five phases termed the Tanner stages (Box 19-1 and Figs. 19-2 to 19-6). Although the sequence of sexual development is predictable, the ages at which these changes occur and the rate of developmental progression vary considerably among individuals. Over the course of pubescence, many young people have questions about the timing, rate, and normalcy of their body changes. These concerns provide nurses with a prime opportunity to discuss health-related topics such as puberty, sexuality, birth control, prevention of sexually transmitted infections (STIs), nutrition, exercise, and safe methods of weight control.
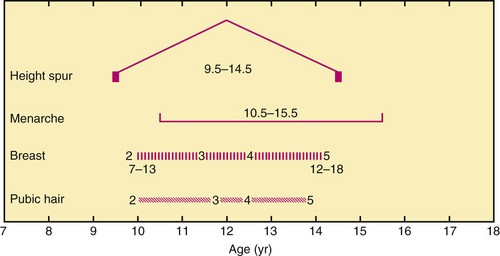
Fig. 19-2 Approximate timing of developmental changes in girls. Numbers indicate stages of development. Range of ages during which some of the changes occur is indicated by inclusive numbers below them. See Figs. 19-3 and 19-4 for explanation. (Based on revised data from Herman-Giddens M, Slora EJ, Wasserman RC, et al: Secondary sexual characteristics and menses in young girls seen in office practice: a study from the Pediatric Research in Office Settings Network, Pediatrics 99(4):505-512, 1997.)
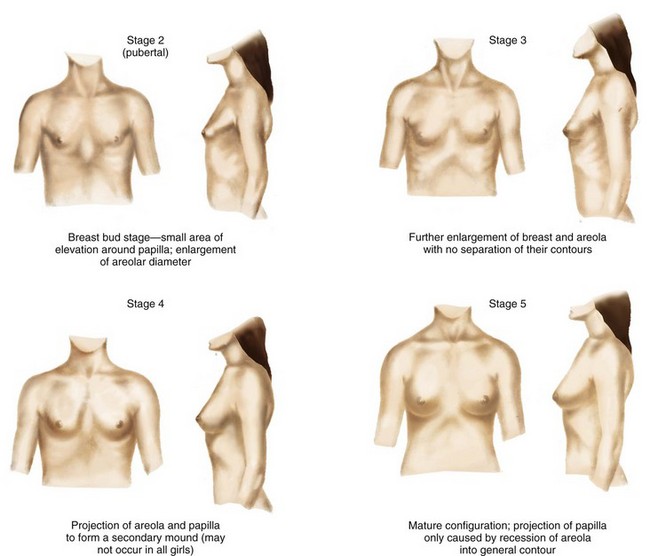
Fig. 19-3 Development of breasts in girls. Average age span is 6 to 13 years. Stage 1 (prepubertal—elevation of papilla only) is not shown. (Modified from Marshall WA, Tanner JM: Variations in pattern of pubertal changes in girls, Arch Dis Child 44(235):291-303, 1969; and Daniel WA, Paulshock BZ: A physician’s guide to sexual maturity, Patient Care 13:122-124, 1979.)
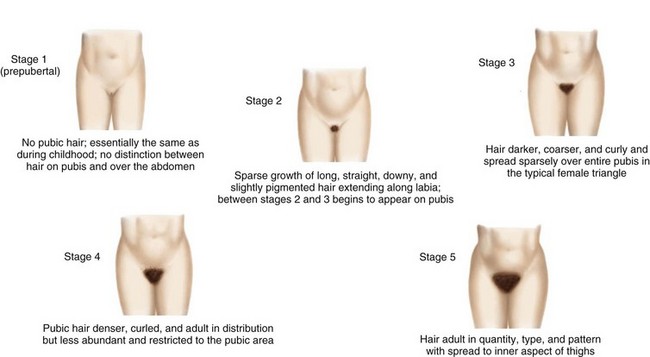
Fig. 19-4 Growth in pubic hair in girls. Average age span for stages 2 through 5 is 11 to 14 years. (Modified from Marshall WA, Tanner JM: Variations in pattern of pubertal changes in girls, Arch Dis Child 44(235):291-303, 1969; and Daniel WA, Paulshock BZ: A physician’s guide to sexual maturity, Patient Care 13:122-124, 1979.)
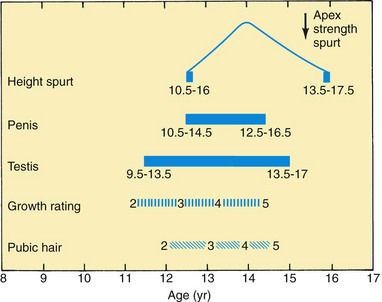
Fig. 19-5 Approximate timing of developmental changes in boys. Numbers indicate stages of development. Range of ages during which some of the changes occur is indicated by inclusive numbers below them. See Fig. 19-6 for explanation. (From Marshall WA, Tanner JM: Variations in the pattern of pubertal changes in boys, Arch Dis Child 45(239):13-23, 1970.)
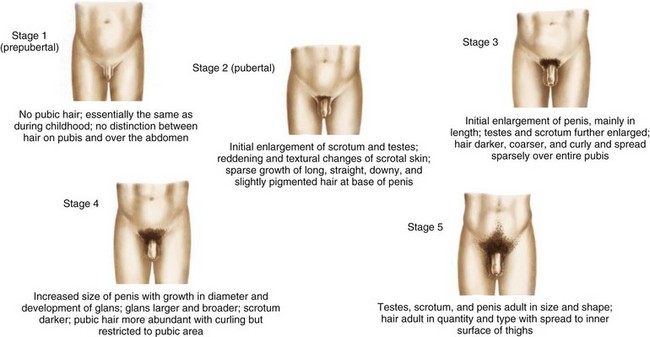
Fig. 19-6 Developmental stages of secondary sexual characteristics and genital development in boys. Average age span is 12 to 16 years. (Modified from Marshall WA, Tanner JM: Variations in the pattern of pubertal changes in boys, Arch Dis Child 45(239):13-23, 1970; and Daniel WA, Paulshock BZ: A physician’s guide to sexual maturity, Patient Care 13:122-124, 1979.)
Sexual Maturation in Girls: In four out of five girls, changes in the nipple and areola and development of a small bud of breast tissue (thelarche) are the earliest, most easily visible changes of puberty. The average age of thelarche for Caucasian girls is 10 years, with a range of 8 to 12.75 years; for African-American girls, the average age of thelarche is earlier, around 9 years, with a range of 7 to 11 years (Herman-Giddens, Slora, Wasserman, et al, 1997; Herman-Giddens, 2006). The appearance of pubic hair (pubarche) usually follows initial breast development by about 2 to 6 months; however, in a minority of normally developing girls, pubic hair may precede breast development. Early in puberty there is often an increase in normal vaginal discharge (physiologic leukorrhea), associated with uterine development. Girls or their parents may be concerned that this vaginal discharge is a sign of infection. The nurse can reassure them that the discharge is normal and a sign that the uterus is preparing for menstruation.
During midpuberty, breast enlargement occurs, and pubic hair progresses to adult-type sexual hair covering the mons pubis and labia majora. Most girls reach their peak height velocity and peak weight velocity in midpubescence.
The hallmark of late puberty is the first menstrual period, or menarche. Initial menstrual periods are usually scanty and irregular and may not be accompanied by ovulation. Ovulation and regular menstrual periods usually begin 6 to 14 months after menarche. Menarche occurs about 2 years after the appearance of breast buds, approximately 9 months after attainment of peak height velocity, and 3 months after attainment of peak weight velocity. The mean age of menarche in the United States is 12.55 years for non-Hispanic Caucasian, 12.06 for African-American, and 12.25 for Mexican-American girls, with a normal age range of  to
to  years (Chumlea, Schubert, Roche, et al, 2003). Menarche has been reported to occur at about 17% body fat, with 22% body fat reported to be required to maintain menstruation. Girls may be considered to have precocious puberty if breast development or pubic hair occurs before age 7 years for Caucasian girls or age 6 years for African-American girls, or if menarche occurs before age 10 years (Kaplowitz and Oberfield, 1999). Girls may be considered to have pubertal delay if breast development has not occurred by age 13 or if menarche has not occurred within 2 to
years (Chumlea, Schubert, Roche, et al, 2003). Menarche has been reported to occur at about 17% body fat, with 22% body fat reported to be required to maintain menstruation. Girls may be considered to have precocious puberty if breast development or pubic hair occurs before age 7 years for Caucasian girls or age 6 years for African-American girls, or if menarche occurs before age 10 years (Kaplowitz and Oberfield, 1999). Girls may be considered to have pubertal delay if breast development has not occurred by age 13 or if menarche has not occurred within 2 to  years of the onset of breast development.
years of the onset of breast development.
In the United States and most developed countries, the mean age of menarche has gradually decreased over the past century, corresponding to population improvements in nutrition, sanitation, and control of infectious diseases. This decline in the average age of menarche appears to have leveled off in recent years (Patton and Viner, 2007). Internationally, a decline in the average age at first menses has not been seen in countries where children are more likely to be malnourished and suffer from chronic illness.
Sexual maturation influences young peoples’ satisfaction with their appearance, but the effects appear to differ for girls and boys. For girls, physical maturation can lead to greater dissatisfaction with their appearance. For example, recent studies indicate that adolescent girls are more dissatisfied with their appearance and significantly more likely to identify themselves as being overweight than adolescent boys, even when they are at a normal weight for height (Smith, Stewart, Peled, et al, 2009). Normal increases in weight and fat deposition that accompany puberty among girls conflict with cultural norms that emphasize a slender look. Early-maturing girls suffer most because they begin to develop at a time when their age-mates still exemplify prepubertal slimness. Unfortunately, an all-too-common response to changes in body shape among teenage girls is to engage in extensive dieting at a time when nutritional requirements are at a peak. For some, the focus on slimness and dieting may trigger the development of eating disorders. (See Chapter 21.) Consequently, health promotion efforts related to pubertal growth, eating behaviors, and body image are important for adolescent girls, especially early-maturing girls.
Sexual Maturation in Boys: The first pubescent changes in boys are testicular enlargement accompanied by thinning, reddening, and increasing looseness of the scrotum. These events usually occur between  and 14 years of age. Early puberty is also characterized by the initial appearance of pubic hair. Penile enlargement begins, and testicular enlargement and pubic hair growth continue throughout midpuberty. During this period boys also undergo increasing muscularity, early voice changes, and development of early facial hair. Gynecomastia (breast enlargement and tenderness) is common during midpuberty. It occurs in up to one third of boys and is usually temporary. The spurts in height and weight occur concurrently toward the end of midpuberty. For most boys, breast enlargement disappears within 2 years. By midpuberty, there is a definite increase in the length and width of the penis, testicular enlargement continues, and first ejaculation occurs. Axillary hair develops, and facial hair extends to cover the anterior neck. Final voice changes occur secondary to the growth of the larynx.
and 14 years of age. Early puberty is also characterized by the initial appearance of pubic hair. Penile enlargement begins, and testicular enlargement and pubic hair growth continue throughout midpuberty. During this period boys also undergo increasing muscularity, early voice changes, and development of early facial hair. Gynecomastia (breast enlargement and tenderness) is common during midpuberty. It occurs in up to one third of boys and is usually temporary. The spurts in height and weight occur concurrently toward the end of midpuberty. For most boys, breast enlargement disappears within 2 years. By midpuberty, there is a definite increase in the length and width of the penis, testicular enlargement continues, and first ejaculation occurs. Axillary hair develops, and facial hair extends to cover the anterior neck. Final voice changes occur secondary to the growth of the larynx.
Precocious puberty in boys may be a concern if secondary sexual characteristics occur before age 9. Concerns about pubertal delay should be considered for boys who exhibit no enlargement of the testes or scrotal changes by ages  to 14, or if genital growth is not complete 4 years after the testicles begin to enlarge.
to 14, or if genital growth is not complete 4 years after the testicles begin to enlarge.
Changes in the size and shape of the penis and testicles and changes in genital functioning can be areas of great concern for adolescent boys. Although the ability for penile erection is present at birth, only with pubertal maturation do boys have seminal emissions. Ejaculation may occur spontaneously as a nocturnal emission, or “wet dream”; as a result of self-stimulation (masturbation); or during sexual activity with others. Unless they are prepared, boys may find spontaneous ejaculations puzzling, troublesome, and embarrassing. Pubertal changes and related concerns create important opportunities for health promotion among young teenage boys. Health care professionals can be a resource for boys and provide appropriate information and guidance around issues related to sexual maturation.
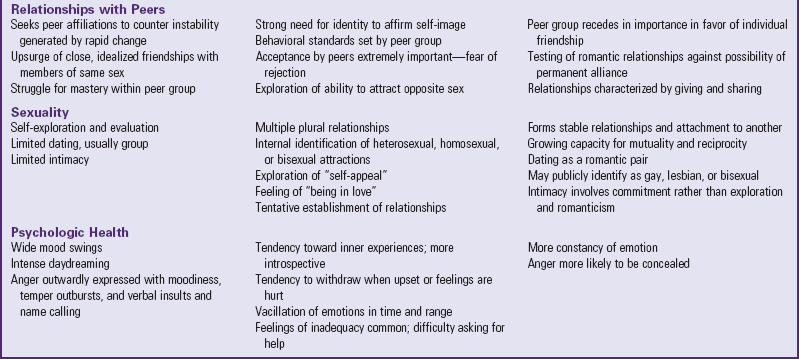
Physical Growth During Puberty
Along with increases in reproductive hormones and sexual maturation, major changes in skeletal and lean body mass occur during puberty. The final 20% to 25% of linear growth is achieved during puberty, and up to 50% of ideal adult body weight is gained during this time as well. The pubertal growth spurt refers to the general increase in growth of the skeleton, muscles, and internal organs, which reaches a peak rate at about 12 years of age in girls and about 14 years of age in boys. Although accelerated growth occurs in all adolescents, the age of onset, duration, and extent vary among individuals. Genetic endowment is the most important determinant of the onset, rate, and duration of pubertal growth, although adequate nutrition also plays a role.
Normal Patterns of Growth: Once the process of growth begins, the sequence of changes is progressive and usually predictable. Awareness of this sequence is not only important for reassuring concerned adolescents and parents but also useful in diagnosing conditions associated with abnormal growth. In general, girls begin puberty and reach maturity about  to 2 years earlier than boys. The pubertal growth spurt begins as early as
to 2 years earlier than boys. The pubertal growth spurt begins as early as  years or as late as
years or as late as  years in girls, and as early as
years in girls, and as early as  years and as late as 16 years in boys.
years and as late as 16 years in boys.
General growth includes accumulation of body mass, along with increases in height and weight. Lean body mass, primarily muscle mass, increases in both girls and boys during early puberty. For girls, the rate of muscle mass growth peaks at menarche and then slows. For boys, muscle mass continues to increase throughout puberty, resulting in the attainment of significantly higher lean body mass in boys than in girls. In girls, gain in fat mass increases markedly early in puberty and continues to increase after menarche. In boys there is a peak deceleration in the rate of fat mass accumulation at the time of their growth spurt, and thereafter a slower and much less dramatic increase than in girls.
The rate of linear growth (height) (Fig. 19-7) begins to increase in girls during early puberty, whereas in boys the rate does not increase until midpuberty. Peak height velocity (PHV) occurs at about 12 years of age in girls, around 6 to 12 months before menarche. PHV is used as a predictor of menarche; height at menarche is a predictor of ultimate adult height. Few girls grow more than 5 cm (2 inches) in height after menarche. Growth in girls’ height usually ceases 2 to  years after menarche. Boys typically reach PHV at about 14 years of age, after growth of the testicles and penis and the appearance of axillary and mature pubic hair. Among most boys, growth in height ceases at 18 or 20 years of age. Increases in leg length tend to precede growth of the trunk by about 6 to 9 months and that of the shoulders and chest by about 1 year. In short, teenagers tend to follow a linear growth pattern in which they outgrow their shoes first, then their pants, and finally their shirts. Peak weight velocity occurs about 6 months after PHV in girls. In contrast, weight and height spurts occur simultaneously for boys. On average, girls gain 5 to 20 cm (2 to 8 inches) in height and 7 to 25 kg (15.5 to 55 lb) in weight during adolescence, and boys gain 10 to 30 cm (4 to 12 inches) in height and 7 to 30 kg (15.5 to 66 lb) in weight during adolescence.
years after menarche. Boys typically reach PHV at about 14 years of age, after growth of the testicles and penis and the appearance of axillary and mature pubic hair. Among most boys, growth in height ceases at 18 or 20 years of age. Increases in leg length tend to precede growth of the trunk by about 6 to 9 months and that of the shoulders and chest by about 1 year. In short, teenagers tend to follow a linear growth pattern in which they outgrow their shoes first, then their pants, and finally their shirts. Peak weight velocity occurs about 6 months after PHV in girls. In contrast, weight and height spurts occur simultaneously for boys. On average, girls gain 5 to 20 cm (2 to 8 inches) in height and 7 to 25 kg (15.5 to 55 lb) in weight during adolescence, and boys gain 10 to 30 cm (4 to 12 inches) in height and 7 to 30 kg (15.5 to 66 lb) in weight during adolescence.
Other Physiologic Changes
In addition to the characteristic changes of puberty already discussed, numerous others occur. The size and strength of the heart, blood volume, and systolic blood pressure increase, whereas the heart rate decreases. Consistent with the general developmental timetable, these changes appear earlier in girls, who establish a slightly higher pulse rate and a slightly lower systolic blood pressure than boys. Blood volume, which has increased steadily during childhood, reaches higher levels in boys than in girls, a fact that may be related to the increased muscle mass in pubertal boys. Adult values are reached for all formed elements of the blood. For instance, there is a marked increase in serum iron, the number of red blood cells, hemoglobin, and hematocrit in boys, but not in girls.
The lungs increase in both diameter and length during puberty. The respiratory rate, decreasing steadily throughout childhood, reaches the adult rate in adolescence. Respiratory volume, vital capacity, and other physiologic properties related to respiratory function are increased, and to a greater extent in boys than in girls. The differences between the sexes are a result of the greater lung growth associated with boys’ increased shoulder and chest size.
The rate of steady decline in basal metabolic rate from birth to adulthood slows during puberty, coinciding with the growth spurt in both sexes, reflecting the increase in physiologic activities. A slightly higher metabolic rate in boys than in girls is probably a function of differences in androgenic hormones. Basal body temperature gradually decreases with age in both sexes, reaching adult values by 12 years of age in girls and somewhat later in boys.
Adolescence is also a time of continued brain growth. Although the number of neurons does not increase, there is a proliferation of the support cells that brace and nourish the neurons, and an increase in the number of neural connections. Development of these connections within the cortex of the brain continues during adolescence and may not reach adult levels until after age 20. In addition, the growth of the myelin sheath around the nerve cells continues through and beyond puberty, enabling faster neural processing. This “fine tuning” of the neural system coincides with development of the more advanced cognitive capacities of youth, but continues into early adulthood. Recent studies have shown, for example, that the frontal cortex areas of the brain, associated with executive functions, continue myelinization into the twenties, and may not be complete until as late as age 25.
Cognitive Development
Emergence of Formal Operational Thought (Piaget)
Jean Piaget (1972) described the shift from childhood to adolescence as a movement from concrete to formal operational thought. Children’s thinking is oriented to things and events that they can observe directly. Unable to think in terms of abstract possibilities, they process information based on what is directly observable. For most young people, emergence of formal operational thinking occurs between the ages of 11 and 14. Formal operational thought includes being able to think in abstract terms, think about possibilities, and think through hypotheses. Young people become able to think about abstractions; thus they can symbolically associate behaviors with abstract concepts such as attractiveness, adult status, or happiness. Adolescents also become capable of using a future time perspective rather than being tied to the here-and-now thinking of childhood. They are able to imagine possibilities, such as a sequence of future events that might occur, including college or occupational opportunities, or how current situations, such as relationships with parents or friends, could change to meet an imagined ideal.
Hypothetical reasoning is aligned with thinking about possibilities. To think through hypotheses, one needs to see beyond what is directly observable and reason in terms of what might be possible. Hypothetical thinking allows adolescents to systematically generate alternative possibilities and explanations and to compare what they actually observe with what they believe is possible. In practical terms, being able to plan ahead and identify future consequences of possible actions are skills dependent on being able to think hypothetically.
The health care provider’s ability to assess an adolescent’s level of cognitive development has important implications for health promotion. Older adolescents may be able to consider some of the symbolic and long-term implications of their behaviors. Thus they may respond to health promotion efforts that require a future time perspective or attention to symbolic rewards. For young people who primarily use concrete thinking (i.e., younger teenagers), health promotion efforts should emphasize immediate risks or benefits of the behavior.
Along with cognitive development, decision-making abilities increase over the adolescent period. Young people develop the ability to consider hypothetical risks and benefits of possible behaviors, along with potential consequences of such behaviors. In addition, the likelihood of teenagers consulting with adult experts, mentors, and role models increases over the junior and senior high school years. By middle adolescence, most teenagers are able to reason as well as adults. Health promotion efforts, especially those aimed at younger adolescents, should offer learning strategies that enhance decision-making skills. Such efforts might include discussions emphasizing health-promoting norms for behavior among young people and alternatives to unhealthy behaviors, along with opportunities to practice skills necessary to resist unhealthy behaviors.
Even with the best framework for health promotion, persons who are capable of formal operational thought and reasoned decision making do not use these processes all the time. When faced with time pressures, personal stress, or overwhelming peer pressure, young people are more likely to abandon rational thought processes. Thoughts about unfamiliar or emotionally arousing topics also tend to be less sophisticated and more vulnerable to the effects of stress and pressure. Unfortunately, many of the health-related decisions adolescents confront, such as those related to substance use or sexual behavior, involve issues that are personally stressful, emotion laden, or new. Under such conditions, people tend not to use their capacities for abstract formal reasoning, even if they typically use advanced decision-making skills.
Adolescent Conceptions of Self
With development of formal operational thought, adolescents become able to describe the self more abstractly. Compared with children, they are more psychologic in their self-descriptions, focusing on personal and interpersonal characteristics, beliefs, and emotional states. They also develop a more differentiated self-concept, recognizing that their behavior and performance vary from setting to setting. With time, they become able to integrate these disparate observations of self into abstract personal characterizations (e.g., “I am a sensitive person”).
Psychologic theories help explain how teens use these powerful new cognitive tools to make the transition to adult roles and relationships (Elkind, 1978; Lapsley, 1993). Being able to think about one’s own thoughts and emotions can lead to periods of extreme self-absorption, what Elkind called adolescent egocentrism. This self-absorption has also been described by Lapsley as a way of imagining and “trying on” various personas and practicing hypothetical interactions in an attempt to develop a separate sense of self.
Two common patterns of thinking help explain some of the health-related beliefs and behaviors of youth. The first, the imaginary audience, involves having such a heightened sense of self-consciousness that an adolescent imagines that everyone notices and is focused on his or her behavior. For example, a teen who has diabetes may worry about injecting insulin at school because “everybody will notice.” The second pattern of thinking, called the personal fable, is the belief that one’s feelings and experiences are completely unique, or that one is all-knowing or invulnerable. This helps explain the common accusation from younger teens towards adults, “You just don’t understand!” as well as some of their decisions around risk behaviors. For example, a sexually active adolescent may choose not to use condoms for safe sex, truly believing that “other people can get STIs, but not me,” or an adolescent who has been drinking may choose to drive home after a party, believing that he or she will not be affected by the alcohol.
There is growing evidence that the inward-focused or narcissistic egocentrism of early adolescence may be an important developmental mechanism that leads to positive mental health, but teens with a strong sense of invulnerability in their personal fable are more likely to engage in risky behaviors that can lead to injury, and teens whose personal fable is focused on their uniqueness may be at higher risk for depression and suicidal ideation (Aalsma, Lapsley, and Flannery, 2006).
Changes in Social Cognition
Gains in cognitive abilities also have an impact on perspective-taking capacities of young people. Adolescents are better able than children to “step into the shoes” of others. During elementary school, children begin to realize that other people have thoughts and feelings; however, they have difficulty understanding that what affects their own thoughts and feelings can also influence the thoughts and feelings of others. Preadolescents develop limited perspective-taking skills, first learning to step into the shoes of best friends, then peers and family members, and finally people of other ages and backgrounds.
Perspective-taking capacities develop further as adolescents become able to engage in mutual role taking. In other words, teenagers can both understand the perspectives of others and see how the thoughts or actions of one person can influence those of others. Role-taking capabilities continue to expand throughout adolescence. They are able to discuss various issues highlighting points of importance to people in various social roles (e.g., “From a parent’s perspective, having a curfew is important because …”). Older adolescents also realize that the perspectives people hold are complicated in that they are influenced by a range of intrapersonal, interpersonal, and sociocultural factors.
Ultimately, gains in perspective-taking skills that take place during adolescence lead to an increased capacity to learn from the experiences of others. Older adolescents are able to consider the choices, behaviors, and outcomes experienced by others in making their own health-related choices. This newfound capacity significantly expands the opportunities to learn health-promoting behaviors.
Development of Value Autonomy
With advances in cognitive development, adolescents’ beliefs become more abstract and increasingly rooted in general ideologic principles. At the same time, young people are gaining increasing emotional independence from parents, relying less on their parents’ beliefs and values than they did as children. Adolescents also progress toward greater behavioral independence, encountering situations and decisions they have not previously experienced. With these new capacities and experiences, young people face a variety of cognitive conflicts as they compare the advice of parents and friends and deal with competing pressures to behave in given ways. These conflicts may prompt young people to consider, in serious and thoughtful terms, what they themselves really believe. Whereas earlier in life they may have merely accepted the decisions or points of view of adults, adolescents begin to substitute a set of values distinct from those of significant adults in their lives. This struggle to clarify values, created in part by an expanded behavioral independence, is a large part of the process of developing what has been termed value autonomy (Steinberg, 1990). The development of a personal value system is a gradual process, with evidence that value autonomy occurs relatively late in adolescence, between the ages of 18 and 20 (Steinberg, 1990).
Moral Development
Moral development parallels advances in reasoning and social cognition. With the attainment of abstract thought and the realization that people’s perspectives and opinions may differ, the ways adolescents approach moral issues change. According to one theory of moral development (Kohlberg and Gilligan, 1972), older children and young adolescents function at a conventional level of moral reasoning in which absolute moral guidelines are seen to emanate from authorities such as parents or teachers. Thus judgments of right and wrong are made according to a set of concrete rules. A major concern is to act or behave in ways that will gain or maintain the approval of others. The correctness of society’s rules is not questioned—one “does one’s duty” by upholding and respecting the social order.
Elements of principled moral reasoning emerge during adolescence. With this level of reasoning, adolescents question absolutes and rules and view moral standards as subjective and based on points of view that are subject to disagreement. One may have a moral duty to abide by social standards for behavior, but only insofar as those standards support and serve human ends. Thus occasions arise in which social conventions ought to be questioned and when principles such as justice, caring, or quality of life take precedence over established social norms. Empirical research on Kohlberg’s theory has demonstrated that aspects of both conventional and principled reasoning are present during adolescence, and different levels of reasoning are used at different times and in different situations.
Kohlberg’s scheme of moral development focuses on an orientation to justice. This orientation holds as its ideal a morality based on reciprocity and equal respect. From this orientation the most important consideration in making moral decisions would be whether the individuals involved were treated “fairly” by the ultimate decision. Gilligan (1982) proposes that an equally valid alternative to the justice orientation is one that emphasizes caring. From this perspective, the ideal is a morality of attention to others and responses to human need. As opposed to the justice orientation, which assumes that moral decisions are best made from a detached position of objectivity, the caring orientation is rooted in the belief that moral decisions should be shaped by attachments and responsiveness to others. Studies have found that although both men and women are capable of approaching moral problems from the perspectives of justice and caring, women may be more likely to give caring-oriented responses before justice-oriented ones, whereas men are more likely to follow the opposite pattern (Gilligan, 1986; Walker, de Vries, and Trevethan, 1987).
Spiritual Development
Religious beliefs also become more abstract and principled during the adolescent years. Specifically, adolescents’ beliefs become more oriented toward spiritual and ideologic matters and less oriented toward rituals, practice, and the strict observance of religious customs. Compared with children, adolescents place more emphasis on the internal aspects of religious commitment, such as what a person believes, and less on the external manifestations, such as whether an individual attends religious worship (Elkind, 1978).
Generally, the stated importance of participation in organized religion declines somewhat during the adolescent years. More high school students than postsecondary school young people attend religious services regularly, and, not surprisingly, the younger the adolescents, the more likely they are to view religion as being important to them. Among older adolescents, the importance of organized religion declines more among college students than among those not in college. Late adolescence appears to be a time when individuals reexamine and reevaluate many of the beliefs and values of their childhood. Consistent with developmental changes in value autonomy, the religious beliefs of young people are likely to become more personalized and less bound to the traditional religious practices they may have been exposed to when they were younger.
Although religious cults and dramatic religious conversion have attracted a great deal of attention in the media, they remain rare phenomena among American adolescents and often reflect nonreligious concerns. Membership in a religious cult is often associated with a preceding period of psychologic stress, identity diffusion, rootlessness, and dissatisfaction with mainstream societal values.
Psychosocial Development
The task of identity formation is to develop a stable, coherent picture of oneself that includes integrating one’s past and present experiences with a sense of where one is headed in the future. Before adolescence the child’s identity is like pieces of a puzzle scattered on a table. Both cognitive development and social situations encountered during adolescence push individuals to combine puzzle pieces—to reflect on their place in society, the way others view them, their own sense of self-worth, and their options for the future. For most individuals, puzzle pieces first form a coherent whole sometime during late adolescence and early adulthood. Erik Erikson, one of the most influential theorists in the area of psychosocial development, describes identity achievement as one of the main psychosocial tasks of the adolescent years. According to Erikson (1968), “From among all possible and imaginable relations [the adolescent] must make a series of ever-narrowing selections of personal, occupational, sexual, and ideological commitments.”
Social forces play a large role in shaping an adolescent’s sense of self. Erikson (1968) argues that the key to identity achievement lies in adolescents’ interactions with others. The people with whom a young person interacts serve as mirrors that reflect information back to the adolescent about whom she or he is and who she or he ought to be. During the period of identity formation, adolescents also learn from others what they ought to keep doing and what they ought not to do. Society also plays an important role in determining the range of available alternatives open to young people involved in identity formation. Optimally, adolescents have the opportunity to explore a range of possible options related to ideologic, occupational, and interpersonal roles before making an identity commitment.
The status of personal commitments in occupational, social, and ideologic domains can measure progress towards identity achievement. The status of personal commitments has four proposed levels: achievement, moratorium, foreclosure, and diffusion (Marcia, 1966). Individuals who demonstrate identity achievement have established a coherent identity after actively exploring possible alternatives; individuals currently engaged in this exploration are in moratorium. Foreclosure refers to making identity commitments without a period of exploration or experimentation, and identity diffusion refers to a lack of firm identity commitments, along with a lack of effort to make those commitments. During adolescence, many individuals progress from diffusion to moratorium to identity achievement, or, alternatively, from diffusion to foreclosure.
Experiences and opportunities within one’s social environment influence both the content of identity and progression toward identity achievement. Among ethnic minority adolescents, identity foreclosure may be more common than among teenagers from the majority culture because of restricted opportunities to explore alternative roles. Identity diffusion also appears to be more common among minority boys and men than among other groups. Possible barriers to identity formation among minority youth may include conflicting values between their minority ethnic group and the broader society, a lack of adult role models who exemplify positive ethnic identity, and inadequate preparation for stereotyping and prejudice that are frequently experienced. However, many ethnic minority adolescents develop effective bicultural identities and abilities to navigate the cultural expectations of home and society, and positive connections to cultural identities can foster healthy adolescent development.
Development of Autonomy
Becoming an autonomous, self-governing person is another of the fundamental psychosocial tasks of adolescence. Autonomy includes emotional, cognitive, and behavioral components. Emotional autonomy is that aspect of independence related to changes in an individual’s close relationships, and behavioral autonomy is the capacity to make independent decisions and follow through with them. Generally, emotional and behavioral autonomy are likely to surface as psychosocial concerns somewhat earlier during adolescence than value autonomy, which usually does not become a prominent concern until middle or late adolescence.
Individuals generally begin the process of emotional autonomy during early adolescence by becoming more emotionally independent from their parents but less separate from their friends. In the process of separating from their parents, younger adolescents often shift a portion of their emotional ties to other adults, often developing “crushes” on teachers, coaches, celebrities, or the parent of a best friend. By the end of adolescence, individuals are less emotionally dependent on their parents than they were as children. This emotional autonomy can be seen in several ways. First, older adolescents do not generally rush to their parents when they are worried or upset. Second, they no longer see their parents as all-knowing or all-powerful. Third, teenagers often have more emotional energy invested in relationships outside their families. Finally, older adolescents are able to see and interact with their parents as people, not just as their parents.
As adolescents increasingly find themselves in situations where adults are not present and where they must make decisions and take responsibility for their own actions, the extent to which they are capable of independent decision making and autonomous behavior takes on added importance. An individual who is behaviorally autonomous is able to turn to others for advice when it is appropriate, weigh alternative courses of action based on his or her own judgment and the suggestions of others, and reach an independent conclusion about how to behave. Behavioral autonomy includes the ability to make independent decisions based on one’s own choices rather than conforming to the opinions of others. Decision-making abilities improve over the adolescent years, with older adolescents being more likely than younger adolescents to be aware of risks and benefits involved with a particular decision, to consider future consequences, to turn to “experts” for advice, and to realize when vested interests may influence the advice of others. Conformity to parents’ opinions declines during early adolescence. However, conformity to peer influence increases during this time. During middle and late adolescence, conformity to both parent and peer opinions declines, allowing for genuine behavioral autonomy. Subjective feelings of self-reliance increase steadily over the adolescent years.
In contrast to popular stereotypes, the development of autonomy during adolescence does not typically involve rebellion, nor is it usually accompanied by strained or tense family relationships. In households where guidelines for adolescent behavior are clear and consistently enforced; where changes in guidelines are open to discussion; and where an atmosphere of interpersonal warmth, concern, and fairness exists, family relationships nurture a gradual and smooth maturational process over the course of the adolescent years. Problems in the development of autonomy are often understandable reactions to excessively controlling circumstances or to growing up in the absence of clear standards. In addition to dispelling the myths that major parent-child conflicts and adolescent rebellion are essential to the development of autonomy, research has shown that parent and peer influences are not necessarily opposing forces but can play complementary roles in the development of a healthy degree of individual independence.
Achievement
Another set of psychosocial tasks encountered during adolescence centers around achievement. Broadly speaking, achievement concerns the development of motives, capabilities, interests, and behaviors related to performance in evaluative situations. The study of achievement during adolescence has focused almost exclusively on young people’s performance in educational settings and on the development and implementation of plans for future scholastic and occupational careers. Various theories have attempted to explain why some young people achieve at higher levels in school. Some have focused on differences in individuals’ motivations to succeed. Others have examined young people’s beliefs about success and failure. Still others have pointed to differences in adolescents’ opportunities for success and to the roles of important adults and peers in their lives. Various indicators of achievement are highly interrelated. For example, success in school during the early elementary years leads to later success in school; doing well in school generally leads to higher levels of educational attainment, which in turn lead to more challenging forms of employment with greater earning power.
Although there are distinct differences among different occupations, the actual process leading toward occupational achievement can be a lengthy one in contemporary society. Because career options have expanded and changed so dramatically, and because increasing numbers of individuals enter college after completing high school, many people do not decide on a career until well into adulthood.
A definite relationship exists between social class and both educational and occupational achievement. A significant problem facing those interested in promoting achievement during adolescence is socioeconomic disparities in educational and occupational achievement. Beginning in early childhood, through no action of their own, many individuals find themselves on an educational course that directs them toward low levels of academic achievement, curtailed schooling, and limited occupational mobility. They reach adulthood with little hope and few dreams for their future. Understanding how this course is set in motion and identifying factors that help individuals from economically disadvantaged backgrounds succeed despite tremendous barriers are necessary steps in building interventions that promote the development and health of these young people.
Sexuality
Adolescence represents a critical time in the development of sexuality. Hormonal, physical, cognitive, and social changes that occur during adolescence all have an impact on sexual development. Of all the developmental changes that affect adolescent sexuality, none is more obvious than the impact of puberty. Adolescents must come to terms with hormonal influences, physiologic manifestations such as menstruation and ejaculation, and physical changes such as breast and genital development. All these changes have a profound impact on the way teenagers perceive their bodies (i.e., body image). In addition to transitions in body image, increasing levels of pubertal hormones contribute to increased levels of sexual motivation among both boys and girls. Evidence also suggests that early development of secondary sexual characteristics is associated with early sexual activity. For example, some early-maturing girls begin dating earlier and may have sexual intercourse at younger ages than their peers (Doswell, Millor, Thompson, et al, 1998). Even when physical development occurs at an average onset and pace, the degree to which adolescents feel comfortable with their bodies may affect sexual behaviors.
Changes in sexual motivations and feelings, happening at the same time as shifts in cognitive skills, contribute to painful conjectures (“Is what I’m feeling normal?”), self-conscious concern (“Am I good looking enough?”), and hypothetical thinking (“What if she wants to have sex?”). The emergence of formal operational thinking also increases adolescents’ decision-making capabilities concerning sexual issues. As they mature, teenagers become better able to think through potential risks and benefits of sexual behaviors before they engage in them. Older adolescents may also be able to conceptualize more long-term consequences of present behaviors. One of the important tasks of adolescence is to incorporate sexuality successfully into intimate relationships (Sullivan, 1953). This task is made possible by the advanced cognitive abilities that emerge over the course of adolescence.
Part of adolescent identity formation involves the development of sexual identity. As they begin to integrate changes involved with puberty, young adolescents also develop emotional and social identities separate from their families. For young adolescents, the process of sexual identity development usually involves forming close friendships with same-sex peers, with whom they may experiment sexually, often to satisfy curiosity. Sexual activity among young teenagers varies by gender. Masturbation provides an opportunity for sexual self-exploration; participation in this behavior is influenced by learned cultural attitudes and sex-role expectations. Boys typically begin masturbating during early adolescence; the age of first masturbation varies greatly for girls. Although some girls begin masturbating during early adolescence, many do not masturbate until after they have had intercourse. Similarly, a small number of teens may engage in oral sex during early adolescence, but the percentage of teens who report oral sex at each age is similar to the percentage of teens who report sexual intercourse, suggesting that oral sex does not necessarily precede intercourse (Brewster and Tillman, 2008; Smith, Stewart, Peled, et al, 2009). Although the age of initiating sexual intercourse has been getting older among teens in the past decade in the United States, about one third of teens have had sexual intercourse by age 15. These young people are at high risk for STIs and pregnancy.
Many teenagers begin to make a shift from relationships with same-gender peers to intimate relationships with opposite-gender partners during middle adolescence (Fig. 19-8). Opposite-gender relationships typically begin with peer activities involving both boys and girls. Pairing off as couples becomes more common as middle adolescence progresses. The type and degree of seriousness of partner relationships vary. Initial relationships are usually noncommittal, extremely mobile, and seldom characterized by any deep romantic attachments. Sexual activity (whether with same- or opposite-gender partners) becomes more common during middle to late adolescence. Nationally, approximately 38% of ninth-grade boys and 27% of girls report having had sexual intercourse. By twelfth grade, 62% of boys and 68% of girls report having had intercourse (Eaton, Kann, Kinchen, et al, 2008). Around 11% of girls and 5% of boys report same-gender sexual partners (Mulye, Park, Nelson, et al, 2009).
The relationship between love and sexual expression is brought into focus during middle adolescence. Most young people oppose exploitation, pressure, or force in sex as well as sex solely for the sake of physical enjoyment without a personal relationship. Many adolescents find it hard to believe that sex can exist without love; therefore they view each relationship as real love. However, some teen social groups have embraced norms that include sexual relationships with friends who are not considered exclusive romantic partners, but rather “friends with benefits.”
The meaning and implication of sexual activity as it affects psychosocial development may be quite different for adolescent boys and girls; that is, sexual socialization differs for males and females in our society. Typically, adolescent boys’ first sexual experiences are in early adolescence through masturbation. Before adolescent boys begin dating, they have generally already experienced orgasm and know how to arouse themselves sexually. For boys, the development of sexuality during adolescence revolves around efforts to integrate the formation of close relationships into an already existing sense of sexual capability. Girls’ first sexual experiences are likely to be different and to carry different meanings. Masturbation is a less prevalent activity among girls, and it is less regularly practiced. The adolescent girl, in contrast to the adolescent boy, is more likely to experience sexual intercourse for the first time in a perceived close relationship. For girls, the development of sexuality involves the integration of sexual activity into an existing capacity for emotional involvement.
An integrated sexual identity often emerges during late adolescence as individuals incorporate sexual experiences, feelings, and knowledge. For most, this identity is consistent with their own physical and mental capacities and with societal limits and expectations. Most older adolescents identify themselves as being predominantly heterosexual or mostly heterosexual, with a smaller number self-identifying as bisexual, or gay or lesbian; an even smaller group is still unsure of their sexual orientation, although this varies somewhat by ethnicity (Russell, Seif, and Truong, 2001; Saewyc, Poon, Wang, et al, 2007). Whatever their sexual orientation, most older teenagers possess the capacity to have intimate relationships that satisfy the emotional and sexual needs of both partners.
Sexual orientation is an important aspect of sexual identity. Sexual orientation is defined as a pattern of sexual arousal or romantic attraction toward persons of the opposite gender (heterosexual), of the same gender (homosexual, often called gay or lesbian), or of both genders (bisexual). Sexual orientation encompasses several dimensions, including attraction, fantasy, actual sexual behavior, and self-labeling or group affiliation. In individuals the direction and intensity of each dimension are not necessarily consistent with any of the others. For example, individuals may be attracted most strongly to their same gender, fantasize about both genders, have sexual activity only with the opposite gender, and identify as gay or lesbian. Other individuals may engage in same-gender sexual behavior, fantasize about both genders, but identify as heterosexual. As with all aspects of sexual identity, cultural meaning and expectation, gender, peer groups, opportunities for intimacy, and other environmental contexts all influence sexual orientation. Research has suggested that the trajectory of developing sexual orientation may be different for boys and girls, and that girls’ sexual behaviors and attractions may be more fluid (Diamond, 2000).
Adolescence is the period during which individuals commonly begin to identify their sexual orientation as part of their developing sexual identity. However, cultural beliefs and values, societal and family pressures, or a lack of similar peers can influence this identification process. The majority of adolescents eventually report an orientation toward exclusively heterosexual relationships. For adolescents whose orientation encompasses any same-gender dimensions, the identity process during adolescence can be complicated, especially when community norms disapprove of orientations other than heterosexual. Adolescents who have witnessed harassment or violence directed at gay, lesbian, and bisexual people, for example, may be reluctant to self-identify, even when their attractions and behaviors are exclusively same-gender or bisexual. In several population-based studies throughout the 1990s, researchers found approximately 1% to 5% of adolescents identify as gay, lesbian, or bisexual, whereas 3% to 12% report same-gender or bisexual orientation in one or more of the other dimensions of sexual orientation (Reis and Saewyc, 1999).
The development of sexual orientation as part of sexual identity includes several developmental milestones during late childhood and throughout adolescence. These milestones do not necessarily occur in the same order for everyone, nor are they completed in the same amount of time (Rosario, Meyey-Bahlburg, Hunter, et al, 1996). They include (1) the realization of romantic or erotic attraction to people of one (or both) genders; (2) erotic daydreaming about one or both genders; (3) romantic partners or dates without sexual activity; (4) sexual activity with people of the preferred gender or genders (also, for some teens, sexual activity with a nonpreferred gender, due to curiosity or social pressure); (5) self-identification of the orientation that best fits one’s current circumstances and understanding; (6) publicly self-identifying that orientation, usually to intimate friends and family first, then the wider social group; and (7) an intimate, committed sexual relationship with a person of the gender appropriate to one’s orientation.
The order of these milestones varies greatly among adolescents, but adolescents who identify as gay, lesbian, or bisexual tend to publicly self-identify later than their heterosexual peers. Without positive gay, lesbian, or bisexual role models or a supportive peer group, sexual minority teens can feel isolated, and they may not share their orientation with anyone for fear of rejection or violence (see Critical Thinking Exercise). When adolescents who would otherwise identify as bisexual can only find a peer group of gay and lesbian teens, they may focus on their same-gender dimensions of orientation and adopt the label of lesbian or gay; later, they may self-label as bisexual. Likewise, some gay and lesbian adolescents may first identify as heterosexual, then bisexual, before identifying as gay or lesbian. In studies among self-identified gay, lesbian, bisexual, and heterosexual adolescents, many of the adolescents report changing their self-labels one or more times during their adolescence and beyond (Rosario, Meyey-Bahlburg, Hunter, et al, 1996; Diamond, 2000).
Although only a few states in the United States, some European countries, and Canada legally recognize same-gender marriages at present, some religious faiths and social groups do celebrate committed same-gender couples’ relationships. There is no evidence that gay, lesbian, or bisexual adults are more or less likely to create long-term, stable relationships than are heterosexual couples. It should be noted that bisexual adolescents and adults do not generally engage in sexual relationships with both genders concurrently; self-identification as bisexual usually refers to the ability to be attracted to either gender but does not imply that such a person requires partners of both genders, or that one must be equally attracted to and have sexual experience with both genders in order to be bisexual.
Intimacy
Intimate relationships are emotional attachments between two people characterized by concern for each other’s well-being; a willingness to disclose private, possibly sensitive topics; and a sharing of common interests and activities. Intimate relationships are distinct from sexual relationships. It is possible for individuals to have close relationships without becoming sexually involved. At the same time, people can be involved in sexual relationships that are not particularly intimate.
It is not until adolescence—a time characterized by pubertal changes, advances in social cognitive abilities, and broadening of social worlds—that truly intimate relationships first emerge. Adolescents’ close friendships are more likely to include a strong emotional foundation in which individuals understand and care about each other. The development of intimacy during adolescence involves changes in the adolescent’s needs for intimacy and in the capacity and opportunities to have intimate friendships. Puberty and its resultant changes in sexual impulses often raise new issues and concerns requiring serious, intimate discussions. Over the course of the adolescent years, individuals become more capable of and interested in emotional closeness with other people. The greater degree of behavioral independence often accompanying the transition into adolescence provides more opportunities for teenagers to be alone with friends and to come into meaningful contact with adults outside their families. Although research on intimacy during adolescence has focused on peer friendships, intimate relationships are by no means limited to peers. Teenagers may also develop intimate relationships with parents, siblings, and adults who are not part of their immediate families.
Harry Stack Sullivan (1953) was among the first to describe the developmental course of intimacy. Usually adolescents develop the capacity for intimacy through preadolescent and early adolescent relationships with same-gender peers. Intimate relationships with opposite-sex peers develop relatively late during adolescence. Opposite-gender friendships may play a more important role in the development of intimacy among boys than among girls, who may develop and experience intimacy with other girls earlier in adolescence.
Individuals move through a series of stages in their close relationships with others. Many adolescents move into role-focused friendships, behaving in ways that are dominated by conventional norms. In their close relationships, individuals at this level attempt to avoid controversy and control their emotions. Role-focused persons are generally more concerned with conforming to the appropriate roles and norms in a relationship (e.g., what the “good” girlfriend does) than with a friend as an individual. It is not until later in adolescence that people develop the capacity for having individuated-connected friendships. With this level of friendship, individuals form intimate relationships with others that acknowledge the complexity and contradictions in close relationships. Differences in outlook between individuals are not only tolerated but encouraged as part of what makes the relationship vital.
Although teenagers may begin dating during early adolescence, these early dating relationships are not usually psychosocially intimate. Early dating relationships typically follow highly ritualized “scripts,” in which adolescents are more likely to play stereotypic roles than to really be themselves. Participating in mixed-gender group activities, such as going to parties or other events, may have a positive impact on young teenagers’ well-being. One-on-one dating during early adolescence, however, with a lot of time spent alone, may lead to sexual intimacy before a teen is ready. A moderate degree of dating, with serious relationships delayed until late adolescence, may be the ideal pattern of interpersonal involvement.
Social Environments
Although all adolescents experience similar biologic and cognitive changes and face similar psychosocial tasks, the health-related effects of these changes are not the same for all people. Why aren’t individuals affected in the same ways by puberty, by changes in thinking patterns, and by changes in social and legal status? The answer lies in the fact that biologic, cognitive, and social changes of adolescence are shaped by the social environment in which the changes take place (Bronfenbrenner, 1979). The social environment provides the opportunities, barriers, role models, and support for individuals’ development and health. Systems within the social environment, including family, peers, schools, community (including Internet-based community), and the larger society, all contribute uniquely to an adolescent’s development and health.
The nurse can use an ecologic model as a way of understanding adolescents’ social environments (Bronfenbrenner, 1979). In this model the social environment is divided into proximal and more distal systems. The social environment includes microsystems, mesosystems, exosystems, and macrosystems.
Microsystems are the most proximal social contexts in which adolescents participate directly, such as family, peer groups, school, and the workplace. All these contexts have substantial influences on the development and health-related behaviors of adolescents (Perry, Kelder, and Komro, 1993).
The next layer of social environment, mesosystems, is formed by linkages between microsystems. The extent to which individuals in one microsystem are involved in other systems determines the strength or “richness” of the mesosystem. For example, regular interactions between family members and school personnel, which have positive effects on student achievement and school performance, reflect a rich mesosystem.
The third layer of social environment, exosystems, consists of settings that influence adolescent behavior and development but in which they do not directly participate. Many community-level influences fall within this layer. These include opportunities within a community for health-enhancing or health-compromising behaviors, such as the availability of age-appropriate activities for young people that do not include alcohol, tobacco, or drugs.
The most distal social environment, macrosystems, consists of culturally based belief systems and economic and political systems. These systems can have profound effects on young people’s health-related behaviors and development, mostly through their influences on more proximal systems. Social systems are embedded within each other, and what happens within one system can influence what happens in others. To have the most impact on adolescent health promotion, interventions must address multiple environmental systems.
Families
Over the past several decades, changes have taken place within the family microsystem that have important implications for adolescent health. Higher rates of divorce and remarriage, increasing numbers of single-parent or blended families, and greater percentages of working mothers have become characteristic of contemporary U.S. society. The “ideal” family consisting of an employed father, an at-home mother, and two or more school-age children is no longer the norm for American society. Higher rates of divorce and the decisions of single women to have children have increased the number of U.S. children spending at least part of their childhood in a single-parent family. Correspondingly, many young people find themselves in blended families, thus developing relationships with stepparents during their adolescent years. A growing number of same-gender couples are raising their own or adopted children as well; in the 2000 census, an estimated 250,000 households were headed by same-gender partners (Bennett and Gates, 2004). Changes in family structure have been accompanied by changes in parent work patterns and a dramatic increase in the percentage of mothers who work outside the home (Gottfried and Gottfried, 1994). (See Family Structure, Chapter 3.)
These changes in family structure and parent employment have resulted in young people having more time unsupervised by adults with increased time alone or with peers. Although for mature adolescents little risk may be involved with minimum supervision, for less competent teenagers, decreased adult supervision may result in more risk-taking behaviors, such as substance use and sexual intercourse. Poorly monitored teenagers may also socialize with peers who engage in risky behaviors. Lack of adult supervision also decreases adolescents’ opportunities for communication and intimacy with a parent or other supportive adults. Although quantity of time does not guarantee quality, sufficient quantity is necessary for communication and the development of intimate relationships.
Consistently, adolescents who feel close to their parents show more positive psychosocial development and behavioral competence, less susceptibility to negative peer pressure, and lower tendencies to be involved in risk-taking behaviors (Resnick, Bearman, Blum, et al, 1997; Smith, Stewart, Peled, et al, 2009). In many situations lack of direct adult supervision may be counterbalanced by parent monitoring and communication about adolescents’ activities during parental absence.
On the other hand, in dysfunctional or abusive families, spending greater amounts of time with parents may compromise the health of teenagers. In these situations the type and content of communication may be the most important factors to address.
In addition to adult supervision, the overall parenting style affects adolescent development. Both effective conflict resolution within families and family cohesion create environments conducive to healthy adolescent development. These two characteristics, along with parent expectations for mature behavior on the part of the adolescent and the practice of setting and enforcing reasonable limits for behavior, form the basis of effective parenting. This parenting style, termed authoritative parenting, is related to greater psychosocial maturity and school performance and less substance abuse among young people.
Adolescents from low-income households are more likely than other adolescents to spend less supervised time with adults, to have parents working at more than one job, to drop out of high school, and to experience violence in their homes and communities. Although disorder within their larger social environments often creates a need for a buffer, which could include spending quality time with adults, poor adolescents often experience fewer of these health-enhancing activities.
Nurses should be cautious, however, in attributing differences in adolescent risk behaviors to racial or ethnic group membership, socioeconomic status, or family structure.
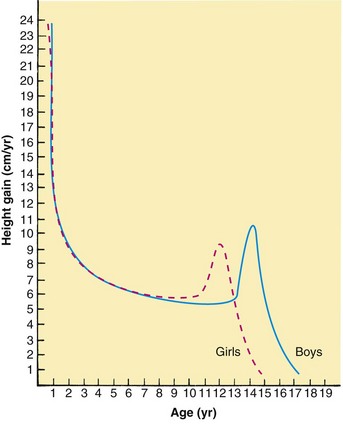
Peer Groups
One hallmark of adolescence is the increasing value young people place on friendships and relationships with peers (Fig. 19-9). Adolescents spend more time with their peers than do children. Compared with children, their peer groups are more autonomous and are more likely to include members of the opposite sex. Because of the changes that have taken place within family systems in contemporary society, peer groups play a significant role in the socialization of adolescents.
Peers serve as credible sources of information, role models of new social behaviors, sources of social reinforcement, and bridges to alternative lifestyles. Close and supportive peer friendships have beneficial effects for young people (Fig. 19-10). However, adolescents with greater peer identification than parental identification, especially when peers model and support problem behaviors, are more prone to negative and health-compromising behaviors. Thus the transition to greater peer involvement, like other developmental transitions of adolescence, is a process requiring guidance; skills; and, optimally, a prolonged time to complete the transition. At a time when they are developing interpersonal skills to deal with peer pressure, young adolescents who lack adult supervision and opportunities for communication with adults may be more susceptible to peer influences and at a higher risk for poor peer-group selection than teenagers who have close relationships with caring adults.
The heightened value placed on adolescent peer relationships leads to questions about the quality and nature of peer influence. Rather than thinking of all peer influence as either good or bad, it is important to recognize that the influence of peers varies from one adolescent to another, from one peer group to another, and across different societies and cultures. Adolescents’ selection of peer groups seems to be most strongly influenced by sociodemographic factors and by common patterns of behavior, including, for example, substance use, school achievement, and religious participation. Peers can have either positive or negative effects on adolescent behavior. Negative effects include increased substance use, gang membership, and violent behaviors. Positive effects include an orientation supporting academic achievement, an environmental commitment, or a commitment to religious or social youth groups.
Peers can also be a positive force in health promotion. Same-age and older adolescents can encourage healthy behavior by serving as positive role models and promoting positive health norms in the peer group (Rosenfeld, Keenan, Fox, et al, 2000; Tuttle, Bidwell-Cerone, Campbell-Heider, et al, 2000). For most adolescents, prosocial pressures from peers are greater than antisocial ones, and adolescents are influenced more by prosocial or neutral pressures than by pressures toward misconduct.
Schools
In contemporary society, schools play an increasingly important role in preparing young people for adulthood. Schooling is essential for a successful future for both boys and girls. Failure to complete high school reduces employment opportunities and the probability of earning an adequate income. Yet many schools in the United States do not meet the developmental needs of all young people.
Many minority-group members are not at appropriate grade levels for their age, and the dropout rate among minority students is higher than among nonminority students. However, gains have been made in educational attainment in the past 30 years; in 2004, 93% of Caucasian adults ages 25 to 29 years had graduated from high school, as had 88% of African-American young adults, and the number of African-Americans attending college and completing bachelor’s degrees doubled over the same time period (US Census Bureau, 2004). Dropout rates are still highest among Hispanic and Native American adolescents.
Another important problem is the lack of parental involvement in schools. Parental involvement increases the effectiveness of schools at all levels. However, with the larger number of single-parent and two–working parent families, parents have less time for involvement in schools.
The timing of school transition may be important, especially if the school environment is not appropriate to the adolescent’s developmental needs. In particular, the transition into a middle or junior high school at age 12 or 13 typically occurs at the same time as the rapid physical changes of puberty.
Another characteristic of school that may have negative effects is a system of grading that acknowledges few young people for their academic successes. Teenagers whose grades fall below average may spend much of their time in environments in which they perceive negative evaluations by adult authorities. As a result, they may feel alienated from school. Subgroups of adolescents may unite and develop countercultures or exhibit antisocial behavior. This process may be most intense for young people from poorer families who attend schools that include students from a broad range of socioeconomic classes.
In addition, students who repeat one or more grades exhibit greater emotional distress than those who do not repeat grades (Resnick, Bearman, Blum, et al, 1997). Students with below-average grades are more likely to be engaged in health-compromising behaviors such as tobacco and alcohol use, unprotected sexual intercourse, and suicide attempts.
The social environment of schools has an impact on student outcomes. Small classroom size and small school size are both related to higher-quality social environments within schools. Safety and respect for all students are critical issues, since students have difficulty learning in unsafe environments, where bullying occurs and is not addressed. In many schools, violence and harassment of students on the basis of race, gender, or sexual orientation is common, affecting more than half of all students (Saewyc, Singh, Reis, et al, 2000). Students targeted for repeated teasing and harassment are more likely to skip school, to report symptoms of depression, and to attempt suicide (Eisenberg and Aalsma, 2005). Equally troubling, teens who are regularly harassed or bullied are also more likely to bring weapons to school to feel safe. In 2007, 20% of adolescents nationwide reported carrying a weapon one or more days in the past month, which is a decline since 1991, when 27% of youth reported carrying a weapon (Mulye, Park, Nelson, et al, 2009). School practices and conditions that lead to better student outcomes stress the importance of supportive environments that foster positive peer group relationships, promote health and fitness, encourage family involvement in school, and strengthen connections between schools and communities.
Work
For the majority of young people in the United States, the workplace becomes a fourth microsystem. Most teenagers are employed in a relatively restricted array of jobs as restaurant workers, cashiers, sales clerks, clerical assistants, and unskilled laborers. The jobs tend to be monotonous, require little initiative or decision making, and rarely use skills learned in school. Furthermore, some are highly stressful, requiring work under extreme time pressure.
Adolescent work as it exists today may negatively affect development. The typical teenager’s job fails to provide continuity to adult employment or links to adults who could serve as vocational mentors. In addition, the monotonous nature of many adolescent jobs is neither intellectually stimulating nor related to role experimentation involved in identity development. Rather, involvement in work may take time away from other activities that could contribute to identity development. Greater involvement in work can also lead to fatigue, decreased interest in school, reduced extracurricular involvement, and poorer grades. Detrimental effects are especially likely for adolescents who work more than 20 hours a week.
Although much work done by teenagers may not contribute to healthy development, jobs that allow young people to develop intellectual and social skills, to have some autonomy, or to feel that their contributions matter can be positive experiences. Jobs that provide adolescents with experiences relevant to future employment or that link them to adults who can serve as vocational mentors may be especially valuable.
Technology as a Social Environment
In the past decade a number of emerging technologies have influenced adolescent social relationships and development. The widespread availability of the Internet and access to social networking websites such as FaceBook, chatrooms, free e-mail, blogs, and Twitter have created “virtual” communities and ways for young people to interact with others; web cameras even allow those interactions to include real-time video communication. Cellular telephones offer more mobile opportunities to talk on the phone, send text messages, send photos, or use video phone capabilities. Young people are no longer limited in their friendships or communities to those who live geographically close. But how do adolescents use these technologies, and how do they influence health and risk behaviors?
Recent studies show increasingly universal access to the Internet and computers. A study in 2004 found that nearly two thirds of urban youth in New York had computer access at home (Bleakley, Merzel, VanDevanter, et al, 2004), whereas a population study in 2008 found that 99% of students in a western Canadian province had access to a computer at home (Smith, Stewart, Peled, et al, 2009).
The Internet chatrooms and social networking sites have created a more public arena for trying out identities and developing interpersonal skills with a wider network of people, occasionally with anonymity. This can create opportunities for young people who have a limited access to friends (because of rural location, shyness, or rare chronic conditions) to interact with people like themselves. However, most adolescents appear to be using the online social environment to interact with the same peers they spend their day with at school.
Text messaging via cell phones has become a common activity and can sometimes be disruptive during school. In addition, both the online and text environment can create opportunities for cyberbullying, where teens engage in insults, harassment, and publicly humiliating statements online or on cell phones. These can evoke responses as distressing as those to bullying in the school setting; there are reports of youth committing suicide after being the target of cyberbullying, and estimates of the prevalence of cyberbullying are similar to reports of in-person bullying and harassment.
Another problematic form of technology use is “sexting,” or the electronic transmission of sexual comments, suggestive pictures, or even sexually explicit photos, primarily via cell phones. Although teens may intend to send the picture or comment only to a boyfriend or girlfriend, they cannot control what happens to the photo after that, whether it is shared with others or even posted online. Some states and countries have laws that consider the transmission of such photos of teens as distributing child pornography and have responded with criminal charges. It is important to help teens think about the possible consequences of posting images on websites or sending them to friends.
Studies have noted that teens are not only enthusiastic technology users, but frequently use multiple types of media at the same time. They may be listening to music on their digital music player while the television is on, and they are surfing the Internet to do their homework and texting friends on their cell phone or on their computer. It is unclear at present how this multitasking and multiple media exposure will affect development of the brain and attention, but frequent media use has been associated with late nights and sleep deprivation. In addition, there are some demonstrated affective and behavioral effects among adolescents who are exposed to high levels of violence or sexual content in the media they use, which can become a cause of concern for health promotion (Brown, L’Engle, Pardun, et al, 2006).
There is increased concern focusing on adolescent vehicle driving and concurrent handheld cellular phone usage. Studies have shown that drivers using handheld devices are considerably more distracted and spend less time looking at the road or paying attention to driving conditions (Hosking, Young, and Regan, 2009). Many states have outlawed the use of handheld mobile devices while actively operating a vehicle (McCartt, Hellinga, and Bratiman, 2006).
Community and Society
Society influences adolescent health and development indirectly through the structures of social institutions, division of economic wealth, and construction and implementation of public policies. Society also provides a dominant set of values and expectations for behavior to which adolescents are exposed. These values and expectations are transmitted through the mass media, local institutions, and social networks.
In the United States, adolescence is a time during which individuals are expected to make the transition from childhood to adulthood. Adolescents are given more autonomy than children and are also expected to show more responsible behavior. Young people are given more personal control over health-related behaviors but often fail to receive necessary guidance, support, or access to positive adult role models. At the same time, society seeks to limit adolescents’ involvement in some risk-taking behaviors that may convey adult status, such as alcohol and tobacco use or sexual behaviors. Many of these same behaviors are glamorized through media programming and advertising campaigns directed at teenagers. For some teenagers faced with societal expectations to “grow up,” risk-taking behaviors take on specific functional meanings. Behaviors such as substance use or unsafe sex may offer adolescents opportunities to challenge social authority, demonstrate autonomy, or gain social approval.
Local communities, as part of the broader societal context, also influence adolescents’ capacity for healthy development. The local community has a more proximal influence on adolescents’ motivations and opportunities to engage in health-enhancing or risk-taking behaviors. For example, adults within the community serve as direct role models, affecting adolescents’ expectations concerning their likely roles and activities as adults. Communities with a high proportion of employed, well-educated, financially successful adults provide a different array of models than impoverished neighborhoods predominated by poor households, chronic illness, and drug abuse, where the financially successful adults are those involved in illicit activities. Such environmental characteristics affect young people’s expectations for the future, their perceptions of how current behavior could jeopardize future chances, and, consequently, their motivation to avoid high-risk behavior.
A community’s economic resources play a significant role in the health and well-being of young people. Resources affect opportunities for health promotion (e.g., by influencing the quality of local schools and health-related services). Schools in wealthy areas can provide high-quality education that will enhance students’ interest in school and their chances of future success. Wealthy communities also provide opportunities for alternative, health-enhancing activities through community clubs and organizations. Thus community resources influence the type and number of health risks young people face and the local capacity for health promotion.
Promoting Optimum Health During Adolescence
Health promotion involves empowering individuals, families, and communities to take developmentally and contextually appropriate actions toward realizing their potential. It includes physical, cognitive, emotional, and social dimensions. For adolescents, health promotion involves helping youth acquire the power (including knowledge, attitudes, and skills), authority (permission to use their power), and opportunities to make choices that increase the likelihood of their creating positive expressions of health for themselves in their contexts.
A comprehensive approach to health promotion combines activities aimed at individuals with interventions focused on changing norms, attitudes, and behaviors of peer groups, families, communities, and society at large. For example, prevention of tobacco use involves more than a teacher’s lecture on the consequences of cigarette and smokeless tobacco use, a ban on tobacco use in schools, a parent’s admonition not to smoke, or a nurse’s question to an adolescent about smoking history. In reality, it requires all these components and more. Effective health promotion requires the support of many individuals and institutions that affect the lives of adolescents.
The rationale for focusing on these health issues becomes obvious when one examines the major sources of mortality and morbidity during adolescence. The primary causes of mortality during adolescence are injuries, homicide, and suicide; together these three causes are responsible for 75% of all adolescent deaths. Major causes of adolescent morbidity include the use of motor and recreational vehicles, sexual and physical abuse, sexual activity such as unwanted pregnancy and STIs, and substance use. Mental disorders, chronic illness, eating disorders, and oral health problems are other important sources of morbidity (Eaton, Kann, Kinchen, et al, 2008). Chapters 20 and 21 provide further information about threats to adolescent health and well-being.
A number of inequities exist in relation to health status among subsets of the U.S. population. Adolescents are one subgroup that experiences health inequities. For example, a substantial gap in life expectancy exists between African-American and Caucasian adolescents. African-American and Native American males have a higher risk of premature death than any other racial or ethnic group. Adolescent males die at a rate more than twice that of girls. Mortality rates increase by more than 200% between early and late adolescence. There are also age differences in the causes of death, with a shift toward more violent deaths occurring in late adolescence. Among Caucasian adolescents a dramatic increase in suicide occurs during later adolescence, making it the second leading cause of death in this group. For older African-American adolescents, homicide ranks as the most likely cause of death. Similar to mortality, patterns of morbidity vary within the adolescent population. For example, rates of vehicular injury are high among males, whereas for females morbidities associated with “quietly disturbed” behaviors such as eating disorders and emotional distress are common (Eaton, Kann, Kinchen, et al, 2008).
Adolescents’ Perspectives on Health
To be most effective, adolescent health promotion efforts must incorporate adolescents’ perspectives on what health means. Such efforts also must focus on adolescents’ concerns and priorities related to health and health care services. From a positive perspective, adolescents’ developmentally based sense of curiosity and movement toward autonomy provide opportunities for health promotion that should not be wasted.
Adolescents define health in much the same way as adults: health means being able to live up to one’s potential; being able to function physically, mentally, and socially; and experiencing positive emotional states. The content of their definitions often goes beyond an “absence of illness” and includes what can be done to maintain and enhance health.
Adolescents’ health-related interests and concerns include stress and anxiety, relationships with adults and peers, weight, acne, and feelings of sadness or depression. Health concerns are often consistent with the immediate developmental tasks that teenagers face. For example, younger adolescents—in the midst of the physical changes of puberty—have a particular interest in issues related to growth and development. In the process of making transitions from middle or junior high school to senior high school, middle adolescents have questions and concerns related to peer-group acceptance, relationships with friends, and physical appearance. Older adolescents focus increasingly on school performance, future career and employment plans, and emotional health issues.
Among the behaviors that adolescents view as risky are substance use, sexual activity, and the use of recreational and motor vehicles. Adolescents also identify health threats that primarily involve psychologic issues, such as clinical depression and eating or weight problems. Other perceived health threats include violence and pollution and threats within the more immediate social environment, including school problems and conflicts with parents, teachers, and friends. When adolescents are asked about general threats to youth, they respond differently than if asked about how their own personal behaviors produce certain risks. Like adults, adolescents tend to underestimate the potentially negative consequences of their own behaviors.
Although young people identify health risks and concerns that are primarily social and psychologic, many are reluctant to seek health services for problems they do not consider to be organic, despite the fact that they indicate they would like help with these problems. A variety of factors influence an adolescent’s reluctance to seek health care, including perceived availability of confidential services, characteristics of health care providers, geographic access, and financial limitations (Smith, Stewart, Peled, et al, 2009).
The availability of confidential services is particularly important to adolescents, especially when they have concerns related to sensitive issues such as sexual or substance use behaviors. Many teenagers are unwilling to seek health care related to sensitive topics if their parents will know about the visit (Reddy, Fleming, and Swain, 2002). Although most states have provisions for confidential care for problems related to substance abuse and sexual health, adolescents often do not know whether and where they can receive confidential health care. Laws also vary by state, and since 2001, a number of states have either enacted or are considering laws requiring parental notification for a variety of health care services for teens, including reproductive health care. Adolescents may be more likely to participate in health care services when such services are delivered by caring, respectful providers.
Factors That Promote Adolescent Health and Well-Being
Even when they are exposed to risk factors such as poverty, neighborhood violence, parental abuse or neglect, or divorce of parents, most adolescents become competent, healthy adults. It is important to understand how this group of young people succeeds despite odds against them. Health promotion efforts with adolescents should focus on nurturing such protective factors in addition to reducing risk factors. Indeed, a large body of research has shown that fostering protective factors can reduce a wide range of health risk behaviors, so it may be more effective than health promotion efforts solely focused on reducing the problem behavior.
A variety of protective factors characterize children and youth who cope successfully when faced with adverse life situations such as poverty, parental alcoholism or psychopathology, or poor relationships between parents. The protective factors include individual personal attributes, attributes of families, and attributes of the larger social environment (Resnick, 2000). One protective personal factor is the ability to adapt to new persons and situations.
Adolescents who cope successfully in the midst of adverse circumstances are often supported by caring, cohesive families in which the parents are concerned with the well-being of their children. This family support can also be provided by some other caring adult, such as a grandparent, in the absence of a supportive parent. Protective factors within the community include connections with adults outside the family, with the school, or with a church group (Resnick, 2000). For example, health care providers who are able to connect with adolescents help support successful coping. Schools that are comfortable, safe, and intellectually engaging can make a difference in the health and well-being of young people. Involvement with healthy peer groups, guided by caring adults who are good role models, also prevents poor outcomes. Community engagement where young people think their involvement is meaningful, and they are listened to, is associated with better adjustment during adolescence.
The potential positive impact of social interactions suggests guidelines for making changes in adolescent environments that support overall health and well-being. Nurses involved with adolescents can develop interventions that shift the balance for young people from vulnerability to resilience by decreasing exposures to health risks or stressful life events (i.e., the impact of parental alcoholism or threats of violence) and by increasing the number of protective factors (i.e., communication and problem-solving skills or sources of emotional support).
Contexts for Adolescent Health Promotion
A consensus is growing that the most effective adolescent health promotion efforts involve multiple systems and address multiple issues. Interventions integrating programs and expertise from health care, school, and community-based settings can effectively increase adolescents’ prevention skills, improve their access to health care services, build adult motivation and support for adolescent prevention practices, and change physical environments and social norms to support healthy behavior. Such a comprehensive approach to health promotion requires a great deal of cooperation and coordination on the part of complex institutions. On the other hand, by not limiting the responsibility for adolescent health to one person or one setting, multiple opportunities for health promotion arise. Individual efforts reinforce important themes and become an integral part of an overall health promotion strategy. For example, a plan for smoking cessation devised by a teenager with the help of a nurse is most likely to be successful if the teenager is encouraged by peers and family members to abstain, and if use and access to tobacco products are discouraged through policy interventions such as smoke-free schools and bans on cigarette vending machines.
Schools: Schools are a primary site for adolescent health promotion and disease prevention. Large numbers of young people can be affected by school-based health promotion efforts, since virtually all teenagers attend school at least through the early adolescent years. Group interventions offer adolescents a sense of anonymity, which they prefer when obtaining information about sensitive topics. School personnel often have special expertise and experience with health education. Through daily contact, school staff can develop supportive relationships with a limited number of students. Parent-teacher associations and school boards also link schools with the larger community in ways that can be used to expand the scope of adolescent health promotion efforts.
School-based health promotion interventions include classroom health education, school-level policies, and environmental changes. Classroom programs often include components that focus on building students’ knowledge and skills and establishing peer support for health-enhancing behaviors. Some programs effectively use classroom peer leaders as positive role models and social support for healthy behaviors. Out-of-class assignments often involve parents or other admired adults, emphasizing the roles that adults play as resources regarding health issues. Classroom programs have been designed to address health-related issues, including healthy eating and exercise habits (Fig. 19-11), nonviolent conflict resolution, substance use and abuse prevention, and responsible sexual behavior.

Fig. 19-11 Adolescents should be encouraged to participate in activities that contribute to lifelong physical fitness.
Other school-level interventions involve changing the school environment itself, including improving physical education and food service programs or adopting tobacco-free school policies. School-wide environmental changes reinforce classroom programs aimed at promoting health-enhancing behavior.
School-Based and School-Linked Health Services: Another avenue for health promotion is school-based and school-linked clinics. School-based clinics (SBCs) are located on school grounds and serve adolescents within a specific school. School-linked clinics (SLCs) may be located off school grounds or on school campuses but serve more than one school. Originally designed to address issues related to adolescent pregnancy, SBCs and SLCs have expanded to address a broad range of health problems and psychosocial issues. In combination, school-linked health services and traditional school-based health promotion efforts provide a comprehensive approach to health promotion that integrates health care, education, and environmental support.
Several private foundations, as well as state and local governments, have provided considerable resources to initiate school-linked health services that offer adolescents confidential services at minimum cost. Parental consent for services is usually obtained on a blanket basis before adolescents seek services. These services increase adolescents’ access to preventive and primary care services through highly visible locations, convenient hours, affordability, and confidential care. SLCs have made a concerted effort to provide the services of a multidisciplinary team of health professionals—which may include nurses, nurse practitioners, health educators, medical assistants, physicians, psychologists, nutritionists, and social workers—skilled in meeting both the mental and physical health needs of adolescents. Adolescents are receptive to services offered by SLCs, especially when they address emotionally charged issues such as depression.
Communities: Community-level approaches to adolescent health promotion, involving both media campaigns and initiatives on the part of community groups, offer the advantage of reaching a broad audience. Specifically, community-based approaches can reach adolescents who do not attend school or have no source of preventive health care. This type of approach directly addresses changing social environments where high-risk behaviors occur. For example, violence prevention may be more effectively addressed by changing community-wide standards related to issues such as conflict resolution than by focusing on the individual. Community-based approaches have the potential to be most effective when they involve various sectors of the community (including adolescents) and include persons representing a variety of youth-serving agencies. With the involvement of multiple sectors, adolescents have the opportunity to hear consistent health messages across a variety of social contexts.
Media campaigns can be an effective but somewhat costly way to reach adolescents in community-level health promotion efforts. Adolescents receive considerable information from sources such as television, the Internet, radio, and magazines. Messages can also be targeted to appeal to parents and other adults who have an impact on the health-related behavior of youth. Media campaigns use brief images and provide short, superficial coverage of specific issues. Podcasts and youth-created videos uploaded to public websites such as YouTube are other ways of using media for health promotion efforts (see The Internet and Other Technologies, below).
Coalitions and task forces are another setting in which nurses can raise awareness about health issues or influence the larger environments for health promotion. This is an opportunity to partner with parents, community agencies, and concerned community groups. The goal of initiatives launched by parent and community groups is often to build climates within communities that support health-enhancing behaviors. Such initiatives create social contexts in which teenagers encounter more health-promoting messages and norms.
Health Care Settings: Consistent, supportive, one-on-one interactions over time between adolescents and members of the health care team provide significant opportunities for health promotion. These relationships can create “safe environments” in which adolescents can disclose sensitive information related to health risk. In turn, this information should be incorporated into preventive interventions specific to individual adolescent needs.
Health care settings offer the advantage of being able to provide confidential services, which are especially important in sensitive situations such as those involving substance use and sexual behavior. Interventions provided through health care settings can include parents and help to create social environments that support adolescents’ health-enhancing behaviors. Another advantage is that health care settings have resources available to address various components of health, including physical, emotional, and social needs.
However, health promotion interventions provided in health care settings have limitations. Individual care is time-consuming, limiting the number of adolescents who can be reached in one-on-one encounters. Although one-on-one interventions can foster health-enhancing attitudes and behaviors of individual adolescents, they do not address changes in social environments, such as peer groups and communities, that may be necessary to support these attitudes and behaviors.
To be effective, health care services for adolescents must be accessible and appropriate. To be accessible, services must be available, affordable, and approachable. Services must include outreach to adolescents and their parents, informing them of the availability of services. Mechanisms for low- or no-cost services must be developed, since cost is a major barrier to adolescents receiving appropriate care. Locating health care services in places such as schools, youth services centers, shopping malls, and detention facilities and offering convenient clinical hours are two strategies that increase accessibility for teenagers who may not use traditional services.
Research has shown that adolescent-focused care can be cost-effective and improve health outcomes (Bensussen-Walls and Saewyc, 2001). To be appropriate, services must take into consideration the cultural contexts and adolescents’ needs for confidential, developmentally appropriate care that addresses their specific health concerns.
The Internet and Other Technologies: A growing number of health promotion activities use the communication technologies that adolescents surround themselves with. Health-related websites designed to appeal to youth (often designed with youth) offer extensive information on nearly every topic that can affect adolescent health, although the accuracy and quality of such websites varies greatly. Programs for helping youth manage their chronic conditions can include a web-based or electronic “health passport,” with information about their condition, their medications, and their health regimen. Social networking sites have been created to help youth with specific health issues. For example, Beyond Blue is a website in Australia about depression that includes therapist-monitored online support groups (see www.beyondblue.org). Some youth clinics offer text message reminders of appointments and cell phone calls to return for STI testing results. Other programs even offer text message or e-mail encouragements for youth who are trying to quit smoking; reminders about safer sex practices; or tips to improve nutrition, exercise, and weight management. Although clinicians need to consider carefully the levels of privacy and confidentiality in the use of different forms of technology, there is growing evidence of effectiveness in engaging youth through the technology they use to communicate.
Adolescent Health Screening
One vehicle for health promotion used by nurses and other professionals in health care settings is one-on-one health screening. Through information gained during a health screening interview, the health professional can identify both assets and threats to an adolescent’s health and well-being. The health screening interview also offers an opportunity for health professionals to build trusting relationships with adolescents. This sense of trust may be critical for adolescents to act on information, attitudes, and skills that are shared to help them successfully negotiate particular stressors.
In addition, the health screening interview provides an opportunity for teaching adolescents self-advocacy skills. Nurses in schools and clinic settings can use several specific strategies to promote self-advocacy skills. These strategies include (1) maintaining an up-to-date file of handouts, pamphlets, and websites to show adolescents during “teachable moments”; (2) directing adolescents to resources in their community and to appropriate, accurate sources of health information on the Internet; and (3) teaching adolescents how the health care system works, how to schedule their health care appointments, and how to keep their own personal health records of immunizations, allergies, and health care encounters.
Interview Process: The development of trust between the adolescent and the health professional is vital to a health screening interview. Within the context of trusting relationships, adolescents are able to disclose sensitive and personal information, and nurses are able to transmit information, attitudes, and skills necessary for adolescents to take health-promoting actions. Three critical elements in establishing trusting relationships are active listening, responding to the adolescent’s emotions, and ensuring confidentiality and privacy.
Active listening involves seeking to understand what is being said without imposing judgment. It includes paying attention to teenagers’ nonverbal cues and noting inconsistencies between verbal and nonverbal communication. Finally, active listening requires listening for understanding rather than truth. For example, when an adolescent states, “My mother hates me,” a nurse who is listening for understanding may reply, “That must be very hard for you,” rather than “What does your mother do to make you think that?” Listening to understand the psychoemotional context of situations can be a difficult skill to master because the cultural milieu in which health care services are provided often encourages getting “just the facts.” However, in noncrisis situations this approach is a critical element in encouraging communication and establishing trusting relationships.
Responding to an adolescent’s emotions includes verbalizing concern about nonverbal cues that are observed. It also involves expressing empathy and support. Furthermore, it includes respecting adolescents’ rights and abilities to make decisions and acknowledging potential issues related to developmental stage, cultural and religious values, beliefs and practices, gender, and sexual orientation.
A third critical element in establishing trusting relationships is ensuring confidentiality and privacy. In general, adolescents have the right to confidential communication with providers unless they are being abused or a life-threatening situation arises. Health care providers need to become familiar with the legal rights of adolescent patients in their state and their obligations to adolescent patients and families.
The nurse should establish the boundaries around confidentiality and privacy at the beginning of the interview so that adolescents feel they can discuss sensitive topics. A brief, clear explanation of confidentiality can clarify that the nurse will not share most things discussed during the interview with others and that life-threatening issues that need to be shared (e.g., report of ongoing abuse, suicidal or homicidal plans) will not be shared without the adolescent’s prior knowledge. To allow for private conversation, complete most of the health screening interview with parents out of the room (Fig. 19-12).

Fig. 19-12 Most of the health screening interview with the adolescent can be completed with parents out of the room.
The Nursing Care Guidelines box lists several other considerations related to the interview process. To convey an interest in adolescents’ perspectives, nurses can begin interviews by asking teenagers to explain their reasons for the visit. At the beginning of the interview, give adolescents a nonthreatening explanation of why questions are asked, such as “I’ll be asking you questions, including some that some people find personal or even embarrassing, so that I can better understand your health.” To increase adolescents’ comfort in disclosing sensitive information, nurses should avoid lectures and questions that convey judgmental attitudes. Asking open-ended questions and avoiding assumptions (e.g., all teenagers have supportive families, all teenagers are heterosexual) give adolescents opportunities to share more of their psychosocial contexts. Any medical language used during the interview should be clarified, and adolescents should be asked to explain any terms they use that are unfamiliar. Restating issues that adolescents may verbalize during an interview allows for a mutual understanding of their concerns.
Interview Content: Reviewing the major morbidities and mortalities of youth reveals that many threats to adolescent health are psychosocial and behavioral. Therefore, given the limited time available during routine clinical encounters, place emphasis on assessment of social, personal, and behavioral factors that underlie the major threats to the health and well-being of adolescents. This approach to assessment will help to identify the majority of adolescents who are coping well, those who require simple health information or counseling, and those who have significant psychosocial problems requiring referral to appropriate resources.
The mnemonic device SAFE TIMES can be used to guide interview questions. As shown in Box 19-2, each letter represents an important issue in preventive care. The less sensitive issues are toward the bottom (i.e., safety, education). It is best to begin the interview with less sensitive topics, ending with more sensitive areas such as sexuality.
Health Concerns of Adolescence
Several professional organizations have published guidelines aimed at improving and maintaining health care for adolescents and young adults. The American Academy of Pediatrics, American Academy of Family Physicians, American Medical Association, Bright Futures, and U.S. Preventive Services Task Force have similar guidelines for health supervision of adolescents. These guidelines emphasize the need to provide health services to adolescents that meet their physical and emotional needs. They place great import on provision of health care by health care providers who are trained in meeting the adolescents’ needs (Jenkins, 2007). The American Medical Association issued a comprehensive set of recommendations, the Guidelines for Adolescent Preventive Services (GAPS), intended to provide a framework for providers who have one-on-one contact with adolescents in clinical settings (American Medical Association, 1997). The following discussion is an overview of the GAPS topics and provides specific recommendations related to screening, guidance, and immunizations.
Parenting and Family Adjustment
Having family members who are emotionally available and appropriately involved in their lives has proved to be a key factor in adolescents’ well-being. On the other hand, family dysfunction can be a strong contributor to many adolescent problems, including depression, alcohol and other drug abuse, eating disorders, and school failure. A wide variety of family disorders, including parental discord, alcohol or drug abuse, mental illness, and sexual and physical abuse, can lead to additional stresses in teenagers coping with the tasks of adolescence.
Screening questions such as “Who is in your family?” “How are things going at home?” and “Who in your family could you talk with about problems you are having?” help to give a general sense of family relationships. More directed questions that give insight into family functioning include “How does your family generally solve disagreements?” “What are some of the rules in your family related to (issues such as underage drinking, curfew, friends)?” “Who sets these rules?” and “Are you currently having conflicts with your family?”
Many parents are interested in, concerned about, and involved in the lives of their adolescent. Parents who are appropriately involved serve as an important protective influence, and efforts to exclude parents from adolescent health services are both unrealistic and unwise. In providing health care, a balance must be sought between the individual adolescent’s growing autonomy and the parents’ diminishing control over, and responsibility for, the adolescent.
Offer parents health guidance at least once during their child’s early adolescence, once during middle adolescence, and once during late adolescence. Such guidance can include information about normative adolescent development, along with signs and symptoms of troubled adolescents. Engage parents in discussion of parenting behaviors that promote healthy adolescent adjustment, including maintaining open communication, setting age-appropriate limits, monitoring their child’s social and recreational activities, and acting as role models for health-enhancing behaviors. Encourage parents to discuss health-related behaviors with their adolescents (see Family-Centered Care and Community Focus boxes and the Family-Centered Care box, p. 772).
Generally, if an adolescent is doing well in school, relates well to peers, and is able to resolve areas of conflict with family members, family intervention is not necessary. Nurses can support positive conflict resolution around minor issues between adolescents and their families, such as curfew hours and appropriate limit setting. Families dealing with major conflicts or dysfunctional relationships should be referred to a family therapist or other mental health professional.
Psychosocial Adjustment
As adolescents experience the many changes of adolescence, they redefine who they are and what they want out of life. Most individuals progress through the changes of their adolescent years with minimum emotional upheaval, countering the belief that this period in life is one of “storm and stress.” Some adolescents, however, do have difficulty coping and exhibit emotional distress, especially when multiple normative events happen simultaneously and are combined with nonnormative life events.
Adolescence is characterized by change within multiple domains. Changes associated with pubertal development typically take place during the early adolescent years. Early- and late-maturing adolescents, who feel they are “out of synch” with their age-mates’ growth patterns, may have a more difficult time emotionally than those who develop “on time” with their peers. Another normative change, typically occurring during middle adolescence, is the transition from middle or junior high school to high school. With this transition, adolescents often are increasingly concerned about same- and opposite-sex peer relationships. School transitions may also expose teenagers to social environments that are larger, less individualized, and less capable of providing adult support and supervision. During older adolescence, psychosocial concerns focus on school achievement and future career plans.
Questions such as “Do you think that your development is going too fast, too slow, or at about the right speed?” may allow young adolescents to discuss issues related to physical development. Questions about feeling cared for and connected to teachers, counselors, students, and others at school, along with questions about their involvement in school-related activities, give teenagers an opportunity to talk about strengths and deficits they experience within their school environments. Questions about the quality of peer relationships may help identify teenagers who feel socially isolated. Finally, questions about future plans related to education and employment or career choices may give older youths the chance to talk through significant sources of stress.
As sources of credible information, support, and encouragement, nurses can help adolescents cope with the changes and challenges they face. To promote both emotional health and psychosocial adjustment, nurses and other health care professionals can encourage adolescents to develop (1) skills to cope with stress and change and (2) skills to become involved in personally meaningful activities.
Intentional and Unintentional Injury
Injuries kill more U.S. adolescents than any other single cause, with unintentional injury, homicide, and suicide accounting for 70% of deaths among teens 10 to 24 years old in 2005 (Mulye, Park, Nelson, et al, 2009). (See Childhood Mortality, Chapter 1.) Motor vehicle crashes are the single greatest source of unintentional injury and death in young people. Many factors contribute to the higher rate of crashes among teen drivers, including lacking driving experience and maturity, following too closely, driving too fast, having other teen passengers in the car, and using alcohol. Homicide, a form of intentional injury, is the second leading cause of death among all U.S. adolescents; for African-American teenagers it is the most likely cause of death. In the United States, homicides among teenagers are most likely to involve firearms and to occur among friends or gangs. In 2007, 82% of all homicides for persons 13 through 19 years of age were firearm related (Mulye, Park, Nelson, et al, 2009).
In addition to being the leading cause of death, injuries also account for substantial morbidity among youth. The leading causes of injury-related morbidity include vehicular crashes, firearms, drownings, poisonings, burns, and falls. Certain behaviors increase the risk of unintentional injury. For example, 11% of high school students nationwide report rarely or never using seat belts. When asked about their practices over the past 30 days, nearly one third (30%) of U.S. high school students reported riding with a driver who had been drinking, and 3.5% of students had driven a vehicle after drinking alcohol (Mulye, Park, Nelson, et al, 2009). The majority of adolescents who use in-line skates or ride bicycles, skateboards, and snowboards do not wear helmets, despite the risk of traumatic brain injury that accidents can cause with these forms of recreation or transportation.
Behaviors that contribute to intentional injury are also prevalent among young people. For example, in 2007, 18% of U.S. high school students reported carrying a weapon (e.g., a gun, knife, or club) at some point during the previous month, with 6% noting that they carried a weapon on school property during that same time period. Nationwide, 36% of students reported being in a physical fight during the year (Mulye, Park, Nelson, et al, 2009). Many adolescents have easy access to a gun in their home, and such accessibility is significantly associated with involvement in violent behavior and with fatal suicide attempts among adolescents.
During an interview, the segment addressing injury prevention should include screening and counseling related to motor vehicle crashes, firearm use, and suicide. In relation to prevention of motor vehicle injury, one might initially ask how the adolescent “gets around town.” Further questions and health education might focus on seat belt or helmet use and the practice of drinking and driving or riding with drivers who have been drinking. Ask adolescents whether they have access, at home or elsewhere, to firearms; whether they carry a gun; and whether they ever use alcohol or other substances in combination with handling guns.
Health education related to firearm injury prevention should include advising parents to limit their children’s household access to firearms, counseling on nonviolent ways to resolve conflicts, and discouraging use of weapons. Family members and acquaintances are a common source of guns for young people. Having a gun in the home increases the risk of adolescent suicide and homicide. Assess all families for the presence of a gun in the home and inform them of the increased risk for suicide and homicide. Gun availability in the general population is linked to increased gun death among children (Glatt, 2005; Miller, Azrael, and Hemenway, 2002). When guns are present in the home, families must take preventive action to be certain that the guns are never loaded, that they are locked up in a safe place, and that ammunition is locked up in a separate location accessible only to appropriate adults.
Dietary Habits, Eating Disorders, and Obesity
Puberty marks the beginning of accelerated physical growth, which can as much as double adolescents’ nutritional requirements for iron, calcium, zinc, and protein. At the same time, growing independence, the need for peer acceptance, concern with physical appearance, and an active lifestyle may affect eating habits, food choices, nutrient intake, and thus nutritional status. Although problems related to overt nutritional deficiencies (excluding iron deficiencies) have decreased since the 1940s, they have been replaced by problems of dietary imbalances and excess. Excess intake of calories, sugar, fat, cholesterol, and sodium is common among adolescents and is found in all income and racial or ethnic groups and both genders (Fig. 19-13). Inadequate intake of certain vitamins (folic acid, vitamin B6, vitamin A) and minerals (iron, calcium, zinc) is also evident, particularly among girls and teenagers of low socioeconomic status. In combination with other factors, these dietary patterns could result in increased risk for obesity and chronic diseases such as heart disease, osteoporosis, and some types of cancer later in life. Girls, in particular, may be susceptible to iron deficiency at menarche. Maximum bone mass is also acquired during adolescence; therefore the calcium deposited during these years determines the risk of osteoporosis.
In terms of weight concerns and weight control behaviors, the number of adolescents who are overweight has increased significantly over the past decade, with 18% of 12- to 19-year-olds qualifying as overweight (Mulye, Park, Nelson, et al, 2009). Female adolescents who are normal weight are also more likely to be currently attempting to lose weight, whereas male adolescents are more often trying to gain weight (Smith, Stewart, Peled, et al, 2009). Although most teens trying to lose weight exercise or diet, a small percent of students (around 5%) engage in risky weight-loss practices such as vomiting after meals or taking laxatives (Smith, Stewart, Peled, et al, 2009).
Currently in the United States, obesity and overweight among adolescents are increasing. Adolescent obesity poses both immediate and long-term problems for adolescents. Anorexia nervosa and bulimia nervosa also commonly occur during the adolescent and young adult years. If left untreated, these disorders, like obesity, can lead to considerable morbidity and mortality. (See Obesity and Eating Disorders, Chapter 21.)
Routine nutrition screening for all adolescents should include questions about meal patterns, dieting behaviors, consumption of high-fat and high-salt foods, and recent changes in weight. In 2007, one third of adolescents reported drinking sweetened soda daily, and only 22% ate the recommended five or more servings of fruits and vegetables (Mulye, Park, Nelson, et al, 2009). Discuss healthy dietary habits with all adolescents, including the benefits of a healthy diet; ways to consume foods rich in calcium, iron, and other vitamins and minerals; and safe weight management.
A screening hemoglobin or hematocrit is recommended at the first encounter with an adolescent, at the end of puberty, or at both screening visits and at the end of pubertal development. The American Academy of Pediatrics (2007) recommends annual measures of weight and height, along with calculation and plotting of body mass index (BMI [weight in kilograms divided by height in meters squared]). Reference BMI values for adolescent males and females are given in Table 19-2. Along with height and weight measurements, an appropriate screening or interview question related to obesity and eating disorders might be, “Do you feel that you are too heavy, too thin, or about the right weight?”
TABLE 19-2
Adolescent Body Mass Index Percentile Rankings
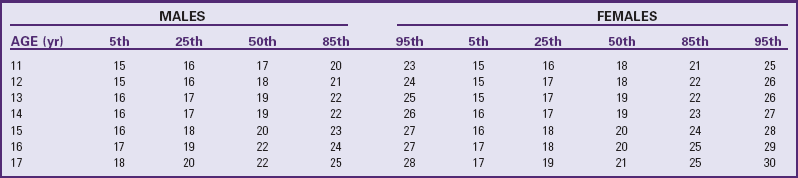
Data from Centers for Disease Control and Prevention: Body mass index–for-age percentiles growth charts, Atlanta, 2000, The Centers, available at www.cdc.gov/growthcharts/clinical_charts.htm (accessed January 29, 2010).
The American Medical Association Expert Committee on the Assessment, Prevention, and Treatment of Child and Adolescent Overweight and Obesity recently published recommendations for the assessment and management of children and adolescents who are either at risk for or are overweight or obese (Rao, 2008). These recommendations include a comprehensive assessment and review of the child or adolescent’s lifestyle habits, family history, physical examination, and laboratory evaluation. Adolescents with a family history of obesity, type 2 diabetes, hypertension, or cardiovascular disease should be carefully screened for risk or presence of health habits that place them at further risk for overweight and obesity (Rao, 2008). Adolescents with a BMI between the 85th and 94th percentiles are considered overweight, whereas adolescents with a BMI equal to or greater than the 95th percentile for age and gender are considered obese. Adolescents who are overweight should have an in-depth dietary and health assessment to determine psychosocial effects and risk for future cardiovascular and metabolic disease. (See Chapter 21 for a comprehensive discussion of the management of obesity.)
Physical Fitness
Nationwide, in 2007 nearly two thirds (64%) of all high school students reported that they had participated in activities that made them “sweat and breathe hard for at least 20 minutes” (i.e., vigorous physical activity) three or more times in the past week. Male students were more likely than female students to engage in vigorous physical activity (Mulye, Park, Nelson, et al, 2009). Participation in school physical education classes declines with age, since schools often do not have mandatory requirements past grade 9 or 10.
High levels of physical activity and fitness may reduce cardiovascular disease risk factors during adolescence, including obesity, high blood pressure, and hyperlipidemia. In addition, routine exercise may reduce adolescents’ risk for depression and emotional distress. Although only some evidence supports a positive relationship between a person’s level of physical activity and fitness during adolescence and this level as an adult, the association between exercise and physical fitness and reduced risk for cardiovascular disease during adulthood is well documented.
Routine screening related to exercise should include questions about frequency, intensity, and type of physical activity. Health care organizations such as the American Academy of Pediatrics (2006) recommend discussing the emotional, social, and physical benefits of exercise with all adolescents. Furthermore, encourage all adolescents to engage in safe exercise on a regular basis. Nurses should encourage all adolescents to be physically active daily, or nearly every day, as part of play, games, sports, work, transportation, recreation, physical education, or other planned exercise.
Sedentary activities, such as watching television, playing video games, and using a computer to surf the Internet or engage with friends, can also contribute to obesity and cardiovascular health problems in later life. Youth should limit their “screen time” in order to get enough exercise. Some new forms of video games include equipment for more active involvement, such as dance or musical performance video games or “virtual” sports. It is unclear if these will offer levels of aerobic activity equivalent to those of more traditional forms of sports and exercise, or if they are temporary fads among youth.
Sexual Behavior, Sexually Transmitted Infections, and Unintended Pregnancy
Sexual activity significantly decreased among U.S. youth in the 1990s through 2005, and among those who are sexually active, responsible sexual behavior had increased until recently. As a result, unintended pregnancy and birth among teens reached the lowest rates ever measured in the United States in 2005, although birth rates increased between 2005 and 2006 and increased again between 2006 and 2007 (Santelli, Orr, Lindberg, et al, 2009). Nationwide, in 2007 less than half (45.9%) of ninth through twelfth graders reported having had sexual intercourse ever during their lifetime, and 35.6% of students reported having had sexual intercourse in the previous 3 months. Rates of STIs and human immunodeficiency virus (HIV) infection among teens have increased, although this may be partly due to increased testing and better sensitivity of STI testing.
Many sexually active young people engage in behaviors that put them at risk for STIs or pregnancy, such as having sex with multiple partners and having sex without using condoms or other forms of contraception. Approximately 14% of U.S. high school students reported having had four or more sexual partners during their lifetime. Among the sexually active students, nearly two thirds reported using a condom during their most recent experience of intercourse, and 16% reported using birth control pills at the time of their most recent experience of intercourse. Since 2003, however, rates of oral contraceptive use have been declining, especially among Hispanic and African-American adolescents, and condom use appears to be decreasing as well, which helps explain the reversing trend in teen pregnancy (Santelli, Orr, Lindberg, et al, 2009).
Obtaining a sexual history can be an important step in promoting sexual health and preventing STIs and unintended pregnancies among young people. Given their sensitive nature, questions about sexuality should be prefaced by an explanation of their purpose and the limits of confidentiality. Initial questions can cover less sensitive topics, such as milestones in pubertal development and, for girls, the menstrual history (including the age at menarche, timing of menstrual cycles, duration of menstrual flow, and symptoms of dysmenorrhea). Questions should also address dating behavior, same- and opposite-gender attractions, and same- and opposite-gender sexual behavior (e.g., “There are many ways people can be sexual with others, such as kissing; touching; and having oral, vaginal, and anal sex. In what ways have you been sexual with others?”). Adolescents should be asked about a history of uninvited or nonconsensual sexual contact (e.g., “Has anyone ever touched you in a sexual way that felt uncomfortable or when you did not want them to? Has anyone ever forced you to have sex?”).
Sexually active youth should be asked about their consistency and motivation to use condoms or other barrier methods for preventing STIs; use of birth control pills or other forms of hormonal contraception; the number of sexual partners they have had over the past 6 months; and the use of alcohol or other substances in connection with sexual activity. Sexually active adolescents should also be asked about any history of pregnancies or STIs. Adolescents who reveal a history of physical or sexual abuse, who admit to heavy use of alcohol or other drugs, or who have unstable social or economic support systems should also be asked whether they have ever exchanged sex for money, shelter, or drugs.
Sexually active adolescents should be screened for STIs with laboratory tests for gonorrhea, chlamydia, and, for females, a Papanicolaou (Pap) test to detect human papillomavirus (HPV) infection or other cervical dysplasia. Both males and females should be evaluated for HPV by visual inspection and should also be asked about whether they have received the HPV vaccine series. Sexually active teenagers should have a serologic test for syphilis if they have lived in an area endemic for syphilis, have had other STIs, have had more than one sexual partner within the past 6 months, have exchanged sex for drugs or money, or are males who have had sex with other males.
One of the newly proposed goals for Healthy People 2020 is to increase the number of adolescents who have been tested for HIV (US Department of Health and Human Services, 2009). Adolescents at risk for HIV infection should be offered confidential HIV screening tests. HIV risk status includes having a history of injecting drug use (including anabolic steroid injections), having sexual intercourse in an area with a high prevalence of HIV infection, having other STIs, having more than one sexual partner in the past 6 months, exchanging sex for drugs or money, being a male and engaging in sex with other males, or having a sexual partner who is at risk for HIV infection. The frequency of laboratory screening for STIs and HIV depends on the sexual practices and STI history of individual adolescents.
All adolescents should receive medically accurate health guidance regarding responsible sexual behaviors, including abstinence. Adolescents should receive information on how STIs, including HIV, are transmitted and on possible consequences of infection. Counsel sexually active adolescents about ways to reduce their risk of STIs and unwanted pregnancy, including limiting the number of sexual partners, using condoms and barrier methods consistently, using appropriate methods of birth control, and avoiding substance use in connection with sexual activity. Counseling should include instruction on how to use condoms and other methods of birth control effectively. Despite extensive government funding available to provide “abstinence-only” sexual health education over the past decade, research evidence shows most such programs are not effective in delaying sexual behavior and may actually increase unprotected sex among adolescents once they become sexually active (Kirby, 2008). Adolescents should receive positive reinforcement for responsible sexual behaviors, including abstinence, consistent condom use, and appropriate use of birth control. Adolescents should also be counseled on ways to reduce their risk of sexual exploitation. Techniques for counseling adolescents to reduce risky sexual behaviors are discussed in detail in Chapter 20.
Gay, lesbian, and bisexual teens are as likely to be sexually active as their heterosexual peers, although the age of sexual debut is more likely to be during early adolescence, in part because of a higher risk for sexual abuse (Saewyc, Skay, Reis, et al, 2006). These youths may engage in heterosexual intercourse as a way to blend in with their peers. This strategy can even include pregnancy and teen parenting in an attempt to avoid detection as gay, lesbian, or bisexual. Recent studies have found sexual minority teens are more likely to be involved in a pregnancy during their adolescent years than their heterosexual peers (Saewyc, Poon, Homma, et al, 2008) and may be more likely to be a teen parent (Forrest and Saewyc, 2004).
Nurses need to acknowledge the possibility of same-gender and bisexual attractions and relationships in their work with adolescents. Screening questions regarding sexual attractions and experiences should be phrased in ways that allow adolescents to discuss same- and opposite-gender attractions, such as using the term partner rather than boyfriend or girlfriend. Gay, lesbian, and bisexual adolescents need the same sexuality education and information on pregnancy prevention and STI transmission and prevention that is appropriate for all other adolescents.
Use of Tobacco, Alcohol, and Other Substances
Statistically, experimentation with substances is common among U.S. adolescents. By the twelfth grade, the majority of students have used alcohol, just under half have smoked, a similar percentage have tried cannabis, and much smaller proportions have tried other illicit drugs. Substance use increases with age, with older teens more likely to use alcohol and cannabis than younger teens, but the rates have generally declined over the past 15 years. Among twelfth graders, for example, 43% used alcohol in the past month, but this is a decline since the early 1990s. One in five smoked cigarettes in the past month, 10% report smoking daily (Mulye, Park, Nelson, et al, 2009), and 5% use cannabis daily. Heavy use of alcohol and tobacco is not uncommon, although the prevalence of binge drinking and tobacco use among high school students is declining. Only about 10% of high school students ages 12 to 17 report binge drinking (having had five or more drinks in a row) at least once in the past month, while among twelfth graders, 25% have done so. However, rates among late adolescents and young adults (ages 18 to 24) increase dramatically compared to teens.
In contemporary U.S. society, adolescents may use tobacco, alcohol, and marijuana because these substances provide an opportunity to challenge authority, demonstrate autonomy, gain entry into a peer group, or simply relieve the stress of growing up. Although use may be accepted among many U.S. teenagers, there are substantive, documented consequences of early experimentation with alcohol, tobacco, and other drugs. Drinking and driving is the leading cause of death among teenagers. Persons who begin smoking at younger ages are more likely to become heavier smokers and are at increased risk for illness and death attributable to smoking (Rojas, Killen, Haydel, et al, 1998). Substance use has also been associated other health-challenging behaviors, such as delinquency, absenteeism, dropping out of school, lower academic achievement, and early sexual behavior.
In terms of health screening, the nurse can ask adolescents whether they or their friends have ever used tobacco, alcohol, marijuana, or other substances. They should also be asked about their current use and current use patterns among peers. The nurse should assess practices of drinking and driving or riding with someone who has been drinking. If answers to these initial questions indicate some problem use, the nurse should ask about the amount and frequency of use; frequency of getting “high” or “wasted”; use in relation to sexual activity; and difficulties with peers, school, parents, or the law in relation to use.
Adolescents who have begun experimenting or who engage in low-level use need to be made aware of other options that can help them achieve the same goals, and of the risks of higher-level use. Furthermore, they need to know the short-term effects of alcohol, tobacco, or other drugs, particularly in relation to driving and school or work performance. Offer cessation plans to adolescents who use tobacco products. Adolescents whose substance use patterns endanger their health should be referred to an appropriate mental health provider. Chapter 21 includes an in-depth discussion of etiology, prevention strategies, and nursing considerations related to adolescent substance use.
Depression and Suicide
A national survey of ninth through twelfth grade students found that 34% of the boys and 22% of girls reported feeling sad or hopeless almost every day for greater than or equal to 2 weeks in a row (Fig. 19-14). Nearly 15% of high school students reported seriously considering suicide during the past year, with female students (19%) being more likely than male students (10%) to have considered a suicide attempt. Around 7% of U.S. high school students reported actually having attempted suicide during the previous 12 months, with girls (9%) being more likely than boys (5%) to have attempted suicide (Mulye, Park, Nelson, et al, 2009).

Fig. 19-14 Adolescents use being alone as a method of coping with stress. Health care professionals need to assess whether this also indicates an attempt to cope with depression.
A brief psychologic screening is necessary during the course of a routine health visit. Screening for depression or suicidal risk should be done with adolescents who note declining school grades; chronic melancholy; family dysfunction; alcohol or other drug use; gay, lesbian, or bisexual orientation; a history of abuse; or previous suicide attempts. Most adolescents who are depressed respond affirmatively to the question, “Have you been feeling down or blue lately?” although they may not necessarily “look” depressed. Refer nonsuicidal adolescents who report commonly feeling “blue,” “down,” or “depressed” to a psychologist, psychiatrist, or other mental health professional who works with young people (Shain and Committee on Adolescence, 2007).
It is crucial to explore thoughts about and possible plans for suicidal acts with all troubled adolescents. Once an assessment of the immediate risk of suicide is completed, the nurse can construct a management scheme. If the adolescent has a specific plan, immediate referral for acute intervention with a psychiatrist or other mental health professional is indicated. (See Chapter 21 for further discussion of suicide.)
Physical, Sexual, and Emotional Abuse
Adolescents who have been physically, sexually, or emotionally abused during childhood or adolescence face challenges to healthy development. Over the past 2 decades, reported cases of physical and sexual abuse first increased dramatically, then declined in the late 1990s, and have remained fairly stable between 2001 and 2003 (US Department of Health and Human Services, 2005). In anonymous school-based surveys of adolescents, the proportion of teens reporting abuse appears to have been declining from the 1990s, although in some recent surveys, rates have plateaued or begun to increase again (Smith, Stewart, Peled, et al, 2009). Around one in four adolescents reports having been physically abused by family members. Approximately 3% to 5% of boys and 10% to 15% of girls report experiencing sexual abuse, most often by someone outside the family, less commonly by incest (sexual abuse by a family member), or both types of abuse (Saewyc, Pettingell, and Magee, 2003). Certain groups of adolescents, such as gay, lesbian, or bisexual youth (Saewyc, Skay, Hynds, et al, 2007) or those who are developmentally delayed, may be especially vulnerable to abuse.
A common constellation of symptoms among adolescents who have been victims of sexual abuse includes substance abuse, depression, withdrawn mood, suicidal ideation, and somatic complaints (Frederickson, 1999). Adolescents who have been abused are more likely than nonabused adolescents to engage in health-compromising behaviors such as self-mutilation, suicide attempts, injection drug use, and early sexual activity (Saewyc, Pettingell, and Magee, 2003) and are at higher risk of being sexually exploited (Widom and Kuhns, 1996). Adolescents with a history of sexual abuse are also more likely to become pregnant or father a child during their teen years (Saewyc, Pettingell, Skay, et al, 2004).
Early identification of abuse can protect adolescents who have been victims of physical, sexual, and emotional trauma. For this reason, questions about abuse should be part of routine adolescent health visits. Ensure privacy before inquiring about abuse. If an adolescent reports a history of sexual or physical abuse, further questions should be directed toward any ongoing abuse; the circumstances surrounding the abuse incident; and the presence of physical, emotional, or behavioral sequelae, including involvement in risk-taking behaviors. Once a history of maltreatment is suspected or disclosed, health care providers have a legal responsibility to report the case to the appropriate child protection agency. The more acute the problem, the more quickly the report must be made. Adolescents reporting abuse should always be informed about steps in the reporting process before information is disclosed to local authorities.
Adolescents who live in homes where there is constant conflict may run away, sometimes to a friend’s home. The conflict may be real (interpersonal) or perceived (intrapersonal), and escalation to abuse or the fear of abuse may prompt the adolescent to leave home. In addition, an adolescent who encounters difficulty with authority figures in the home may leave home believing this will solve the problem. The adolescent may stay in school and maintain close ties with less threatening family members and friends; the term couch surfing is used in some circles to refer to the adolescent who spends time at different friends’ houses sleeping on the couch or in an available spare room to “crash” temporarily. Such adolescents are often at higher risk for further abuse and neglect.
School and Learning Problems
In 2007, 16% of U.S. youth between the ages of 16 and 24 years of age (almost 6.2 million persons) dropped out before completing high school (Center for Labor Market Studies, 2009). Dropout rates vary by ethnicity. In 2007, 30% of dropouts were Hispanic, 18.8% were African-Americans, and 12% were Caucasians (Center for Labor Market Studies, 2009). Among in-school adolescents, a low grade point average has been associated with higher levels of emotional distress; cigarette, alcohol, and marijuana use; and earlier onset of sexual activity. School problems and dropping out of school can also be markers for difficulties such as learning disabilities, language barriers, family problems, lack of supportive relationships at school, and employment needs. In contemporary U.S. society, education is critical to economic self-sufficiency. Teenagers who drop out of school can expect to earn approximately $400,000 less over a lifetime (ages 18 to 64 years) than those who graduate. Males who drop out of school may earn $500,000 less over the same time period (Center for Labor Market Studies, 2009).
Questions about recent grades, school absences, suspensions, and any history of repeating a grade in school can be used to screen for school-related problems. Specific management plans for youth who note school problems should be coordinated with school personnel and with the adolescent’s parents or caregivers if possible.
Hypertension
As adolescents experience sexual maturation, along with increases in height and weight, blood pressure increases from the onset of adolescence and continues to rise until the end of pubertal growth. This trend is especially apparent among males. Approximately 1% of adolescents have sustained hypertension, defined as a blood pressure greater than the 95th percentile of standards. (See inside back cover for blood pressure tables and Chapter 34 for an in-depth discussion of hypertension in children and adolescents.) The detection of hypertension during adolescence is important because hypertension is one of the major preventable risk factors for adult cardiovascular disease. With increasing levels of obesity, there have been reports of increasing incidence of hypertension among adolescents (Hansen, Gunn, and Kaelber, 2007). To detect early hypertension, all adolescents should have blood pressure taken annually (American Academy of Pediatrics, 2007).
Hyperlipidemia
Along with hypertension, smoking, and obesity, elevated serum cholesterol and triglyceride levels are major risk factors for the development of adult cardiovascular disease. Results of several studies suggest that 23% to 35% of young adolescents have at least one cardiovascular disease risk factor; approximately 5% to 10% have two or more risk factors.
The American Academy of Pediatrics (Daniels, Greer, and Committee on Nutrition, 2008) recommends that children and adolescents with a family history of dyslipidemia or premature cardiovascular disease be screened for total blood cholesterol level (nonfasting) at least once after 2 years of age but no later than 10 years of age. The American Heart Association (McCrindle, Urbina, Dennison, et al, 2007) recommends that adolescents with borderline elevated total cholesterol (170 to 200 mg/dl) have a fasting cholesterol level repeated to monitor low-density lipoprotein (LDL) and high-density lipoprotein (HDL). Diet therapy is recommended for adolescents with elevated LDL levels (borderline high, 110 to 129 mg/dl; high, ≥130 mg/dl). LDL cholesterol–lowering drug therapy is recommended for children and adolescents whose LDL remains elevated after 6 months to 1 year on a restricted fat diet (Daniels, Greer, and Committee on Nutrition, 2008; McCrindle, Urbina, Dennison, et al, 2007; Zapalla and Gidding, 2009).
Infectious Diseases and Immunizations
Immunization updates are a significant part of adolescent preventive care. Adolescents 11 to 18 years of age should receive a single tetanus-diphtheria–acellular pertussis (Tdap) vaccine if they have received the recommended childhood series of DTaP immunizations. This vaccine is now required because of the increased incidence of pertussis seen in adolescents and adults who were previously immunized with the DTaP series yet developed the condition as adolescents. The adolescent who has received Td but not Tdap vaccine should also receive a single dose of the Tdap vaccine, provided 5 years have elapsed between the Td and Tdap vaccination (American Academy of Pediatrics, 2009). Meningococcal vaccine (MCV4) should be given to adolescents 11 to 12 years of age or at 15 years of age if previous immunization with MPSV4 occurred in childhood and at least 3 to 5 years have passed since primary immunization. The MCV4 vaccine is now preferred over the MPSV4 vaccine. College students living in dormitories are at increased risk for meningococcal disease and should therefore be immunized with MCV4 (American Academy of Pediatrics, 2009).
Two HPV vaccines are currently licensed for use in the United States. HPV4 (Gardasil) is recommended in females starting at ages 11 to 12 years for the prevention of cervical, vaginal, and vulvar cancers, and in males ages 9 to 18 for the prevention of genital warts. HPV2 (Cervacil) is recommended for females starting at age 11 or 12 years to prevent cervical cancers. Both are given in a series of three vaccines.
With the exception of pregnant teenagers, all adolescents should receive a second measles-mumps-rubella (MMR) vaccine unless they have documentation of two MMR vaccinations during childhood.
All adolescents who have not previously received three doses of hepatitis B vaccine should be vaccinated against hepatitis B virus. The hepatitis A vaccine should be given to all adolescents as part of the routine immunization schedule; the two-dose series may be completed in childhood, and a catch-up schedule for those who have not been previously immunized is recommended. Annual influenza vaccination with either the live attenuated influenza vaccine or trivalent influenza vaccine is now encouraged for all children and adolescents. All adolescents should also be assessed for previous history of varicella infection or vaccination. Vaccination with the varicella vaccine is recommended for those with no previous history; for adolescents 13 years or older with no previous infection or history, the varicella vaccine may be given in two doses 4 or more weeks apart (American Academy of Pediatrics, 2009). Any adolescent who has not completed the immunization series for hepatitis A, hepatitis B, poliovirus, and influenza should receive these immunizations according to the latest catch-up schedule. (See also Immunizations, Chapter 12.)
Adolescents should receive a tuberculin skin test if they have been exposed to active tuberculosis (TB), have lived in a homeless shelter, have been incarcerated, have lived in or come from an area with a high prevalence of TB, or currently work in a health care setting. Among adolescents who are at high risk for infection, an induration of 10 mm or more at the skin test site is considered positive. Adolescents with a positive skin test should be referred for evaluation for active TB. The frequency of TB testing depends on the risk factors for the individual adolescent. (See Tuberculosis, Chapter 32.)
H1N1 influenza (also called swine flu) became widespread throughout the world and the United States, reaching pandemic status by late summer of 2009, with adolescents and young adults appearing to have no previously acquired immunity to the new strain. The H1N1 vaccine was distributed in the United States beginning in late fall of 2009; the live-attenuated H1N1 influenza vaccine (LAIV) is available as nasal spray given once, whereas the inactivated influenza (H1N1) monovalent vaccine is administered by intramuscular route. Targeted candidates to receive the first supplies of vaccine available included pregnant women and persons aged 6 months to 24 years, health care and emergency workers, persons living with or providing care for infants less than 6 months of age, and persons aged 25 to 64 years who have medical conditions that place them at higher risk for influenza-related complications (Centers for Disease Control and Prevention, 2009). Nurses should provide general health teaching about preventing the spread of influenza through regular hand washing; staying out of public places when one has flulike symptoms; and sneezing or coughing into one’s sleeve, rather than the hand.
Body Art
Body art (piercing and tattooing) has become a major factor in some adolescents’ identity formation. The skin has become one of the latest sources of parent-adolescent conflict. The adolescent often seeks body art as an expression of his or her personal identity and style. Tattoos are often obtained to mark significant life events such as new relationships, births, and deaths. Piercing the ear, nose, nipple, navel, genitalia, or tongue may sometimes create a health problem in the uninformed teenager. It is a nursing responsibility to caution girls and boys against having piercing performed by friends, parents, or themselves. In addition, health education regarding the health risks of tattoos must be provided to youth and their families during routine health care visits (Betz, 2009). Although most cases of piercing are accompanied by few if any serious side effects, there is always a danger of complications such as infection, abscess formation, cyst or keloid formation, bleeding, dermatitis, or metal allergy. Using the same unsterilized needle to pierce body parts of multiple teenagers presents the same risk of HIV, hepatitis C, and hepatitis B virus transmission as with other needle-sharing activities.
A qualified operator using proper sterile technique should perform the procedure. This is especially important if the individual has a history of diabetes, allergies, or skin disorders. Adolescents should be informed about the approximate time for healing after body piercing and the care of the pierced area during and after healing. Some body sites need extra precautions. For example, cartilage (ear, nose) has a poor blood supply and heals slowly and scars easily; nipple piercing puts the adolescent at risk for breast abscess. Finally, migration of the piercing is common with naval and other flat skin surface piercing. Piercing guns should not be used for piercing anything other than the earlobe because guns place the piercing too deeply.
Studies of distinct populations of young adults and adolescents report body art rates as high as 23% (Braverman, 2006). Professional and amateur artists administer tattoos. The risk to the adolescent receiving a tattoo is low. The greatest risk is for the tattoo artist who comes in contact with the client’s blood. Adolescents who are amateur tattoo artists benefit from discussions about Standard Precautions and the hepatitis B vaccination. Many states either have no regulations or do not enforce existing regulations of piercing and tattooing facilities. The local health department is a source of information about local regulatory requirements. The Centers for Disease Control and Prevention has an excellent website that outlines safety concerns for persons performing and receiving body art (www.cdc.gov/Features/BodyArt).
Sleep Deprivation and Insomnia
The changing social environment of adolescents can often change their sleep patterns, at a time when their growth and development requires additional sleep for health. Although adolescents should generally get around 9 hours of sleep each night, early morning school scheduling, extracurricular activities, homework, employment, and desired social time with peers or on the Internet can make it difficult for them to get sufficient sleep. Recent studies into sleep among adolescents have shown that nearly half may not get the recommended amounts of sleep, and as many as 1 in 4 is regularly sleep-deprived, that is, reports 6 hours or less of sleep per night (Roberts, Roberts, and Duong, 2009). Sleep deprivation can affect physical and mental health and has been associated with higher rates of depression, somatic complaints such as headaches and stomachaches, fatigue, and difficulties with concentration. These physical and psychologic effects of inadequate sleep can also affect school performance and thus contribute to school problems.
Homeless and street-involved youth, youth who go to bed hungry because of insufficient access to food, and those with anxiety disorders are all more likely to experience sleep disturbances. However, the high rate of young people who do not get enough sleep, and the health consequences of inadequate sleep, suggest that nurses should regularly assess all adolescents for the amount and quality of sleep they are getting. Health teaching and health promotion should include information to promote sufficient sleep.
Tanning
The desire to be attractive leads many teenagers to excessive sunbathing and artificial means for tanning. However, this practice has serious long-term risks, and the adolescent should be educated regarding the detrimental effects of sunlight on the skin. (See Sunburn, Chapter 18.) Long-term effects include premature aging of the skin, increased risk of skin cancer, and, in susceptible individuals, phototoxic reactions.
The increasing popularity of artificial tanning has prompted concern among health professionals regarding the use of sunlamps and tanning machines. The long-term effects of tanning machines are similar to those of the sun; dermatologists do not recommend tanning by these means. Those who insist on using tanning equipment should be warned that goggles must be worn in tanning booths to prevent serious corneal burning. Education on the use of sunscreens, including hypoallergenic products, with a sun protective factor (SPF) of at least 15 and a nonalcohol base without lanolin, parobens, or fragrance is important. Broad-spectrum sunscreens that protect against both ultraviolet A and B are the most effective. Self-tanning creams safely simulate the appearance of a tan; however, teens using these products should be cautioned that sun protection is still required. Targeting health education messages to adolescents and incorporating information on sun protection behaviors in school health curricula and in health care visits will increase adolescent knowledge and awareness.
A large cross-sectional study of 12- to 18-year-olds in the United States found that teens are not following these recommendations; only 34% used sunscreen routinely in the past summer and 14% used a tanning bed at least once (Geller, Colditz, Oliveira, et al, 2002). Cutaneous melanoma, the most common fatal form of skin cancer, is associated with ultraviolet light exposure and continues to affect a significant amount of individuals yearly (Geller and Annas, 2003; Leiter and Garbe, 2008; Rigel, 2008).
Health Promotion Among Special Groups of Adolescents
Certain groups of adolescents—including adolescents of color; gay, lesbian, and bisexual youth; and adolescents living in rural areas—experience health problems at disproportionate rates and face barriers to health care because of a lack of financial resources, limited availability of appropriate resources, or other factors.
Minority Adolescents
Minority children (i.e., children of African-American, Latino-Hispanic, Asian, Native American, and Alaskan Native descent) are the fastest-growing population within the United States. It is estimated that by 2020 roughly 40% of the U.S. child population will be made up of minorities. In 2003, 34% of African-American children and 30% of Hispanic children lived in families with incomes below the poverty level (ChildTrends Data Bank, 2003). Large numbers of Native American children also live in poverty; unemployment on some reservations is estimated at 80%. The disproportionate levels of health problems experienced by adolescents from these racial, ethnic, and tribal groups can be attributed, at least in part, to the effects of poverty and the lack of access to health care that is associated with being poor.
Most of these children grow and develop normally and successfully meet the challenges of adolescence and young adulthood. Research has begun to identify factors that promote resiliency among minority adolescents from disadvantaged backgrounds, including those who grow up in poverty. Often these young people have come from families and communities that provide nurturing, supportive, and culturally rich environments (Isaacs, 1993). To be most effective, future health promotion interventions must include strategies that increase these protective factors in the lives of other adolescents growing up in high-risk environments.
However, too many minority adolescents experience predictable outcomes associated with living in environments where risk factors outweigh protective factors. Compared with nonminority children, higher percentages of minority children and adolescents have learning, emotional, or physical disabilities. They are more likely to drop out of school and have limited opportunities for higher education, become parents at an early age, are incarcerated in youth detention facilities, or die as a result of homicide or unintentional injuries before reaching adulthood. The increase in health risk behaviors during adolescence, in combination with limited access to health care and effective preventive services, places these adolescents at significantly higher risk for adolescent pregnancy, STIs, HIV infection and acquired immunodeficiency syndrome, chronic or other infectious diseases (i.e., hypertension, TB, and hepatitis), substance abuse, emotional problems, and violence. All these health problems, which often lead to premature death or chronic disorders, are preventable.
Effective health promotion programs can make important contributions to the prevention of health problems among minority adolescents. A consensus is growing that health promotion programs will be most effective if they are culturally competent. A culturally competent approach is one that both recognizes the importance of culture and incorporates—at all levels—the assessment of relations across cultures, with attention to dynamics that result from cultural differences, the expansion of cultural knowledge, and the adaptation of programs to meet culture-specific needs (Schorr, 1997). Nurses, working with other health care professionals and community leaders, can develop or adapt culture-specific health promotion interventions (see Cultural Competence box).
Several basic principles can guide the development of culturally appropriate health promotion efforts (Isaacs, 1993):
• Health promotion messages are most effective when they are conveyed through multiple community institutions. The content of these messages should be consistent across agencies, culturally appropriate, and couched in terms that deal with health-destructive behaviors in a pragmatic rather than a judgmental manner.
• Health promotion efforts should involve peer groups, schools, communities, and families. In particular, families must be recognized as a positive source of cultural strength and a primary source of information, education, and support for young people. Because “family” is defined differently by different cultures, a culture-specific definition of family must be the basis of developing interventions involving families. For example, prevention strategies that involve concerned relatives and friends have proved highly successful in reaching Hispanic youth involved in high-risk behavior. The willingness of family and friends to be involved is rooted in Hispanic values of familialism and community.
• Those who develop strategies for minority adolescents and communities must draw on community-based values, traditions, and customs and work with knowledgeable persons from the community in developing focused interventions and communication channels. The challenge for professionals, whose culture may be different from that of the target audience, is to develop collaborative relationships with community members that enable communities to identify health problems and their underlying causes and to design and evaluate programs that address identified needs.
• Health promotion interventions focused on minority adolescents may be most effective if they provide a generic framework and skills for developing relationships and problem solving that can be applied to any health-related decision. There is an emerging belief that this type of generic approach can be more effective than interventions focused on specific problems (i.e., STIs, pregnancy, or substance use), since the behaviors that lead to many adolescent health problems are highly interrelated.
• Health promotion and prevention strategies must be developed and implemented in places where these adolescents are found. Adolescents who have left the school system are often at greater risk for health problems than those who remain in school. Health promotion messages must be incorporated into shelters for homeless and runaway youth, detention centers, residential programs, and community recreation centers to reach young people at highest risk.
To date, there has been little systematic evaluation of the effectiveness of health promotion interventions among minority adolescents. Interventions that work must be documented so that these efforts can be disseminated and adapted for other communities of color.
Gay, Lesbian, and Bisexual Adolescents
The population of gay, lesbian, and bisexual adolescents has unique developmental issues and health challenges. Although adolescents may participate in same-gender sexual activity or have same-gender attractions, they do not necessarily become gay, lesbian, or bisexual adults. Assigning sexual orientation labels to adolescents is complex and should be approached cautiously, but most studies conclude that between 3% and 10% of adolescents are lesbian or gay and a larger percentage are bisexual in orientation (Saewyc, Skay, Hynds, et al, 2007).
Most of the health challenges of sexual minority teens are responses to negative societal attitudes and messages about homosexual or bisexual orientation. The stigma associated with gay, lesbian, or bisexual identity makes adolescents reluctant to acknowledge or identify their orientation to themselves and others. For those who try to manage this stigma by keeping their same-gender attractions hidden, the isolation and fear of disclosure can create emotional distress. They may use alcohol and other substances to escape their anxieties, and they are at much greater risk for suicidal behaviors than their heterosexual peers. In several population-based studies, nearly one third of gay, lesbian, and bisexual adolescents report attempting suicide one or more times (Saewyc, Skay, Hynds, et al, 2007). Although nurses should screen all youth about suicidal thoughts and history of suicide attempts, it is especially critical for an adolescent who identifies as gay, lesbian, or bisexual or one who is questioning his or her orientation.
Publicly disclosing a gay, lesbian, or bisexual orientation during adolescence (“coming out”) brings additional challenges. Many adolescents face hostility and even violence from their families when they first come out. Some families physically or sexually assault the adolescent, whereas others seek psychologic counseling or treatment to “change” their teen’s orientation (D’Augelli, Hershberger, and Pilkington, 1998). The American Psychological Association (2006) and the American Academy of Pediatrics have both issued statements that “reparative therapy,” or treatment designed to alter sexual orientation, shows no evidence of effectiveness but does show evidence of psychologic harm and is therefore unethical.
Some families are so distressed and angry after their teen’s disclosure of a homosexual or bisexual identity that they throw the adolescent out of the house. A disproportionate number of homeless and street youth are gay, lesbian, or bisexual (Smith, Saewyc, Albert, et al, 2007). Others are rejecting in more subtle ways, but even these nonsupportive responses can have an effect on adolescents’ healthy development; those who are rejected by their families are at increased risk for suicide attempts and substance abuse (Ryan, Huebner, Diaz, et al, 2008).
Nurses should not encourage teens to disclose their sexual orientation to their families without first forming a safety plan in case the reaction is not supportive. For teenagers who question their sexual orientation, the nurse should not reassure them that these feelings are only a passing phase. For the majority of young people, referral to an agency providing support services or social opportunities for gay, lesbian, and bisexual adolescents is appropriate. In many high schools, Gay Straight Alliances (GSAs), after-school advocacy and social groups, can be a source of peer and social support as well. Parents who seek assistance in adjusting to their son or daughter’s disclosure can be referred to a local chapter of Parents, Families and Friends of Lesbians and Gays (www.pflag.org), which provides information and support for parents and family members.
Teens who acknowledge same-gender attractions or relationships are also at risk for violence and harassment from schoolmates, neighbors, and even strangers. Gay, lesbian, and bisexual adolescents who are homeless face additional risks of physical and sexual violence. They may be forced to exchange sex for shelter or food or to avoid assault and may not be able to negotiate safer sex practices. As a result, they may be at increased risk for sexual abuse, STIs, and pregnancy.
Given their pervasive experiences of negative attitudes and potential violence, sexual minority adolescents may fear similar uncaring attitudes among health care providers and might avoid disclosing their orientation during health assessments. Many gay, lesbian, and bisexual adolescents have experienced insensitive behaviors from health care providers, and they may avoid needed health care as a result (Ryan and Futterman, 1997). To provide sensitive, professional care for gay, lesbian, and bisexual adolescents, nurses should be sensitive in their choice of language and be nonjudgmental and caring in their communication. Placing a poster or brochure about local services for gay, lesbian, and bisexual youth in a prominent position in the clinic setting sends the message it is safe to talk about such issues at the clinic. Health professionals who work with teenagers regarding sexual orientation issues are encouraged to seek out additional information and resources that address health needs and services for gay, lesbian, and bisexual adolescents (Ryan and Futterman, 1997).
Rural Adolescents
Except for higher rates of accidental injuries (related in part to farm accidents) and lower rates of delinquency among rural adolescents compared with urban ones, few known differences in health problems exist. Research on the health status of rural adolescents is limited, but rural adolescents experience many of the same health problems as adolescents in metropolitan areas. However, rural adolescents face barriers to health promotion, since they have more limited access to appropriate health care services.
Rural adolescents’ access to health care is limited by shortages of professionally staffed mental and physical health services, inadequately trained providers, transportation problems, and less access to Medicaid in rural states. Rural communities often lack adequately trained nurses, physicians, dentists, psychologists, social workers, and allied health professionals, in addition to modern equipment. Rural health professionals often feel inadequately prepared to address adolescents’ physical and psychosocial health issues. In metropolitan areas providers who are unwilling or unable to address adolescents’ concerns can refer to colleagues with expertise in adolescent health issues. The absence of adolescent health specialists, combined with a limited network of agencies focused on adolescent health promotion, exacerbates rural youths’ problems in obtaining appropriate services. Finally, rural adolescents who live in poverty are less likely than their low-income urban counterparts to be covered by Medicaid and to have financial coverage for health care services.
In addition to health promotion topics addressed with other populations of adolescents, prevention efforts focused on rural adolescents must include efforts to improve the safety of farm machinery and farming practices. Innovative efforts are needed to increase rural adolescents’ access to health care services, including development and funding for school-linked health services, improvements in transportation, use of nonprofessionals and adult community members, better dissemination of information about availability of local health services, and access to further education in adolescent health for health care providers.
Nursing Care Management
With continued increases in the numbers of adolescents in the United States and rising rates of health-related problems of youth, there is an unprecedented need for adolescent health promotion. Nursing professionals can make significant contributions to health promotion among adolescents and their families. Because nurses understand the biologic, cognitive, psychosocial, and social transitions of adolescence and their impact on health behavior, they can address adolescents’ developmental and health needs. Working with colleagues from other disciplines, community members, parents, and adolescents themselves, nurses must become part of a comprehensive approach that delivers consistent messages across clinical, school, and community-based settings. Nurses should be at the forefront of developing and disseminating culturally appropriate health promotion interventions among special populations, including adolescents of color; gay, lesbian, and bisexual youths; and rural teenagers.
Parents are often confused and perplexed about the changes and behaviors of adolescence. They need support and guidance to help them through this time. They need to understand the changes taking place and to accept the expected behaviors that accompany the process of detachment, to be prepared to “let go,” and to promote the changed relationship from one of dependency to one of mutuality. Suggestions for anticipatory guidance of parents of adolescents are listed in the Family-Centered Care box.
Key Points
• Adolescence is characterized by important biologic, cognitive, psychologic, and social change.
• The biologic events of puberty result in hormonal changes; changes in height, weight, strength, and endurance; and development of secondary sexual characteristics.
• During adolescence most individuals move from patterns of concrete thinking to abstract, hypothetical thinking.
• Major psychologic tasks of adolescence involve establishing a sense of identity along with behavioral, emotional, and value autonomy.
• According to Kohlberg’s theory of moral development, adolescents begin to question existing moral values and learn to make choices. Gilligan observed differences in the way males and females make moral decisions.
• Spiritual development is characterized by the questioning of family values and ideals, a move to more philosophic thinking, and emphasis on personal religion.
• As adolescents establish identities separate from those of parents and families, relationships with peers often become more important.
• Biologic, cognitive, and psychosocial changes all affect sexual activity and sexual identity development of adolescents.
• Gay, lesbian, and bisexual youth have unique issues to cope with in identity formation.
• The three primary causes of death during adolescence are injuries, homicide, and suicide.
• Motor vehicle injuries are the greatest causes of mortality from unintentional injuries in this age-group.
• Major causes of adolescent morbidity include injury; STIs; unintended pregnancy; and mental health problems, including depression, chronic illness, and eating disorders.
• To be most effective, adolescent health promotion efforts must actively involve teenagers at all stages.
• The availability of confidential health services is particularly important to adolescents.
• Certain groups of adolescents—including youth of color; rural youth; and gay, lesbian, and bisexual youth—experience health problems at disproportionate rates and face barriers to health care because of limited access to appropriate, affordable resources.
Answers to Critical Thinking Exercise
Discussing Sexual Orientation with Adolescents
1. Yes. There is sufficient information to arrive at a conclusion about John’s sexual orientation.
2. a. Studies of gay, lesbian, and bisexual people indicate that adolescence is the time when individuals become aware of same-gender attraction. Gay and bisexual youths are at risk for health-damaging behaviors such as early initiation of sexual behavior, substance abuse, suicide, and running away from home.
b Gay, lesbian, and bisexual youths are often confronted with anti-gay attitudes and values in society. This reaction makes it difficult for these youths to grow up and become healthy physically and mentally.
c Health care professionals who work with adolescents should consider the adolescent’s increasing independence and responsibility while ensuring confidentiality.
3. The nurse’s first priority in this situation is to give John permission to discuss his feelings about this topic. He has come to the nurse practitioner to discuss this matter, and he probably feels comfortable sharing this information with her. The nurse practitioner needs to be open and nonjudgmental in her interactions with John. He needs to know that the nurse practitioner will maintain confidentiality, appreciate his feelings, and remain sensitive to his need to talk about this topic. An example of an appropriate response for the nurse practitioner might be, “John, tell me more about how you came to this conclusion.”
4. Yes. The information about sexual orientation in adolescence and the role of the health care professional support this conclusion.
References
Aalsma, MC, Lapsley, DK, Flannery, DJ. Personal fables, narcissism, and adolescent adjustment. Psychol Schools. 2006;43:481–491.
American Academy of Pediatrics, Committee on Infectious Diseases. Pickering L, ed. 2009 Red book: report of the Committee on Infectious Diseases, ed 28, The Academy: Elk Grove Village, Ill, 2009.
American Academy of Pediatrics. Recommendations for preventive health care. Pediatrics. 2007;120(6):1376–1377.
American Academy of Pediatrics. Active healthy living: prevention of childhood obesity through increased physical activity. Pediatrics. 2006;117(5):1834–1842.
American Medical Association, Guidelines for adolescent preventive services. ed 4. Chicago: The Association; 1997. available at www.ama-assn.org/ama/upload/mm/39/gapsmono.pdf [(accessed January 29, 2010)].
American Psychological Association, Just the facts about sexual orientation and youth: a primer for principals, educators and school personnel. APA Online, 2006, available at www.apa.org/pi/lgbc/publications/justthefacts.html [(accessed February 18, 2006)].
Bennett, L, Gates, GJ. The cost of marriage inequality to children and their same-sex parents. Human Rights Campaign Foundation, available at www.hrc.org, 2004. [(accessed March 2005)].
Bensussen-Walls, W, Saewyc, EM. Teen-focused vs adult-focused prenatal care models for high-risk pregnant adolescents. Pub Health Nurs. 2001;18(6):424–435.
Betz, C. To tattoo or not: that is the question. J Pediatr Nurs. 2009;24(4):241–243.
Bleakley, A, Merzel, CR, VanDevanter, NL, et al. Computer access and Internet use among urban youths. Am J Pub Health. 2004;94:744–746.
Braverman, PK. Body art: piercing, tattooing, and scarification. Adolesc Med. 2006;17:505–519.
Brewster, KL, Tillman, KH. Who’s doing it? Patterns and predictors of youths’ oral sexual experiences. J Adolesc Health. 2008;42(1):73–80.
Bronfenbrenner, U. The ecology of human development. Cambridge, Mass: Harvard University Press; 1979.
Brown, JD, L’Engle, KL, Pardun, CJ, et al. Sexy media matter: exposure to sexual content in music, movies, television and magazines predicts black and white adolescents’ sexual behavior. Pediatrics. 2006;117:1018–1027.
Center for Labor Market Studies. Left behind in America: the nation’s dropout crisis. Northeastern University, available at www.clms.neu.edu/publication/documents/CLMS_2009_Dropout_Report.pdf, 2009. [(accessed September 11, 2009)].
Centers for Disease Control and Prevention, 2009 H1N1 monovalent influenza vaccine dosage, administration, and storage. Atlanta: The Centers; 2009. available at www.cdc.gov/h1n1flu/vaccination/dosage.htm [(accessed December 2009)].
ChildTrends Data Bank. Children in poverty, 2003. available at www.childtrensdatabank.org, 2003. [(accessed January 5, 2010)].
Chumlea, WC, Schubert, CM, Roche, AF, et al. Age at menarche and racial comparisons in US girls. Pediatrics. 2003;111(1):110–115.
Daniels, SR, Greer, FR, Committee on Nutrition. Lipid screening and cardiovascular health in childhood. Pediatrics. 2008;122(1):198–208.
D’Augelli, AR, Hershberger, SL, Pilkington, NW. Lesbian, gay, and bisexual youth and their families: disclosure of sexual orientation and its consequences. Am J Orthopsychiatry. 1998;68(3):361–371.
Diamond, LM. Sexual identity, attractions, and behavior among young sexual minority women over a 2 year period. Dev Psychol. 2000;36(2):241–250.
Doswell, WM, Millor, GK, Thompson, H, et al. Self-image and self-esteem in African-American preteen girls: implications for mental health. Issues Mental Health Nurs. 1998;19(1):71–94.
Eaton, DK, Kann, L, Kinchen, S, et al. Youth risk behavior surveillance—United States, 2007. MMWR Surv Summ. 2008;57(SS04):1–131.
Eisenberg, M, Aalsma, M. Bullying and peer victimization: position paper of the Society for Adolescent Medicine. J Adolesc Health. 2005;36(1):88–91.
Elkind, D. Understanding the young adolescent. Adolescence. 1978;13(49):128–134.
Erikson, E. Identity: youth in crisis. New York: Norton; 1968.
Forrest, R, Saewyc, E. Sexual minority teen parents: demographics of an unexpected population. J Adolesc Health. 2004;34(2):122.
Frederickson, D. Maltreatment of children. Child Family Nurs. 1999;2(6):393–401.
Geller, AC, Annas, GD. Epidemiology of melanoma and nonmelanoma skin cancer. Semin Oncol Nurs. 2003;19(1):2–11.
Geller, AC, Colditz, G, Oliveira, S, et al. Use of sunscreen, sunburning rates and tanning bed use among more than 10,000 U.S. children and adolescents. Pediatrics. 2002;109(6):1009–1014.
Gilligan C: Adolescent development reconsidered, paper presented at Invitational Conference on Health Futures of Adolescents, Daytona Beach, Fla, 1986.
Gilligan, C. In a different voice, 1982. Cambridge, Mass: Harvard University Press; 1982.
Glatt, K. Child-to-child unintentional injury and death from firearms in the United States: what can be done? J Pediatr Nurse. 2005;20(6):448–452.
Gottfried, AE, Gottfried, AW. Redefining families: implications for children’s development. New York: Plenum Press; 1994.
Hansen, ML, Gunn, PW, Kaelber, DC. Underdiagnosis of hypertension in children and adolescents. JAMA. 2007;298(8):874–879.
Herman-Giddens, ME. Recent data on pubertal milestones in United States children: the secular trend toward earlier development. Int J Androl. 2006;29(1):241–246.
Herman-Giddens, M, Slora, EJ, Wasserman, RC, et al. Secondary sexual characteristics and menses in young girls seen in office practice: a study from the Pediatric Research in Office Settings Network. Pediatrics. 1997;99(4):505–512.
Hosking, SG, Young, KL, Regan, MA. The effects of text messaging on young drivers. Hum Factors. 2009;51(4):582–592.
Isaacs, M. Developing culturally competent strategies for adolescents of color. In: Elster A, Panzarine S, Holt K, eds. American Medical Association State of the Art Conference on Adolescent Health Promotion: proceedings. Arlington, Va: National Center for Education in Maternal and Child Health, 1993.
Jenkins, RR. Adolescent medicine. In Kliegman RM, Behrman RE, Jenson HB, et al, eds.: Nelson textbook of pediatrics, ed 18, Philadelphia: Saunders, 2007.
Kaplowitz, P, Oberfield, SE. Reexamination of the age limit for defining when puberty is precocious in girls in the United States: implications for evaluation and treatment: Drug and Therapeutics and Executive Committees of the Lawson Wilkins Pediatric Endocrine Society. Pediatrics. 1999;104(4 Pt 1):936–941.
Kirby, D. The impact of abstinence and comprehensive sex and STI/HIV education programs on adolescent sexual behavior. Sexual Res Soc Policy. 2008;5(3):18–27.
Kohlberg, L, Gilligan, C. The adolescent as philosopher: the discovery of the self in a post-conventional world. In: Kagan J, Coles R, eds. Twelve to sixteen: early adolescence. New York: Norton, 1972.
Lapsley, DK. Toward an integrated theory of adolescent ego development: the “new look” at adolescent egocentrism. Am J Orthopsychiatry. 1993;63(4):562–571.
Leiter, U, Garbe, C. Epidemiology of melanoma and nonmelanoma skin cancer—the role of sunlight. Adv Exp Med Biol. 2008;624(1):89–103.
Marcia, J. Development and validation of ego identity status. J Perspec Soc Psychol. 1966;3(5):551–558.
McCartt, AT, Hellinga, LA, Bratiman, KA. Cell phones and driving: a review of research. Traffic Inj Prev. 2006;6(2):89–106.
McCrindle, BW, Urbina, EM, Dennison, BA, et al. AHA scientific statement: drug therapy of high-risk lipid abnormalities in children and adolescents: a scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee, Council of Cardiovascular Disease in the Young, with the Council on Cardiovascular Nursing. Circulation. 2007;115(14):1948–1967.
Miller, M, Azrael, D, Hemenway, D. Firearm availability and unintentional firearm deaths, suicide and homicide among 5-14 year olds. J Trauma. 2002;52:267–275.
Mulye, TP, Park, MJ, Nelson, CD, et al. Trends in adolescent and young adult health in the United States. J Adolesc Health. 2009;45:8–24.
Patton, GC, Viner, R. Adolescent health, part 1, Pubertal transitions in health. Lancet. 2007;369:1130–1139.
Perry, C, Kelder, S, Komro, K. The social world of adolescents: family, peers, schools, and the community. In: Millstein S, Petersen A, Nightingale E, eds. Promoting the health of adolescents: new directions for the twenty-first century. New York: Oxford University Press, 1993.
Piaget, J. Intellectual evolution from adolescence to adulthood. Hum Dev. 1972;15:1–12.
Rao, G. Childhood obesity: highlights of AMA Expert Committee recommendations. Am Acad Fam Physician. 2008;78(1):56–63. [65-66].
Reddy, DM, Fleming, R, Swain, C. Effect of mandatory parental notification on adolescent girls’ use of sexual health care services. JAMA. 2002;288(6):710–714.
Reis, E, Saewyc, EM. 83,000 youth: selected findings of eight population-based studies as they pertain to anti-gay harassment and the safety and well-being of sexual minority students. Seattle: Safe Schools Coalition of Washington; 1999.
Resnick, MD. Protective factors, resiliency and healthy youth development. Adolesc Med. 2000;11(1):157–165.
Resnick, MD, Bearman, PS, Blum, RW, et al. Protecting adolescents from harm: findings from the National Longitudinal Study of Adolescent Health. JAMA. 1997;278(10):823–831.
Rigel, DS. Cutaneous ultraviolet exposure and its relationship to the development of skin cancer. J Am Acad Dermatol. 2008;58(5 Suppl 2):S129–S132.
Roberts, RE, Roberts, CR, Duong, HT. Sleepless in adolescence: prospective data on sleep deprivation, health and functioning. Adolescence. 2009;23:1045–1057.
Rojas, NL, Killen, JD, Haydel, KF, et al. Nicotine dependence among adolescent smokers. Arch Pediatr Adolesc Med. 1998;152(2):151–156.
Rosario, M, Meyey-Bahlburg, H, Hunter, J, et al. The psychosexual development of urban lesbian, gay, and bisexual youth. J Sex Res. 1996;33(2):113–126.
Rosenfeld, SL, Keenan, PM, Fox, DJ, et al. Youth perceptions of comprehensive adolescent health services through the Boston HAPPENS program. J Pediatr Health Care. 2000;14(2):60–67.
Russell, ST, Seif, H, Truong, N. School outcomes of sexual minority youth in the United States: evidence from a national study. J Adolesc Health. 2001;24(1):111–127.
Ryan, C, Futterman, D. Lesbian and gay youth: care and counseling. New York: Columbia University Press; 1997.
Ryan, C, Huebner, D, Diaz, R, et al. Family rejection as a predictor of negative health outcomes in white and Latino lesbian, gay, and bisexual young adults. Pediatrics. 2008;123:346–352.
Saewyc, EM, Pettingell, S, Magee, LL. The prevalence of sexual abuse among adolescents in school. J School Nurs. 2003;19(5):266–272.
Saewyc, EM, Pettingell, S, Skay, C, et al. Teen pregnancy among sexual minority youth in population-based surveys of the 1990s: countertrends in a population at risk. J Adolesc Health. 2004;34(2):125–126.
Saewyc, EM, Poon, C, Homma, Y, et al. Stigma management? The links between enacted stigma and teen pregnancy trends among gay, lesbian and bisexual students in British Columbia. Can J Hum Sex. 2008;17(3):123–131.
Saewyc, E, Poon, C, Wang, N, et al. Not yet equal: the health of lesbian, gay, and bisexual youth in BC. Vancouver: McCreary Centre Society; 2007.
Saewyc, EM, Singh, N, Reis, E, et al. The intersection of racial, gender and orientation harassment in school and health risk behaviors among adolescents (abstract). J Adolesc Health. 2000;26(2):148.
Saewyc, EM, Skay, CL, Hynds, P, et al. Suicidal ideation and attempts among adolescents in North American school-based surveys: are bisexual youth at increasing risk? J LGBT Health Res. 2007;3:25–36.
Saewyc, EM, Skay, CL, Reis, E, et al. Hazards of stigma: the sexual and physical abuse of gay, lesbian, and bisexual adolescents in the U.S. and Canada. Child Welfare. 2006;58(2):196–213.
Santelli, JS, Orr, M, Lindberg, LD, et al. Changing behavioral risk for pregnancy among high school students in the United States, 1991-2007. J Adolesc Health. 2009;45(1):25–32.
Schorr, LB. Common purpose: strengthening families and neighborhoods to rebuild America. New York: Anchor Books; 1997.
Shain, B, Committee on Adolescence. Suicide and suicide attempts in adolescents. Pediatrics. 2007;120(3):669–676.
Smith, A, Saewyc, E, Albert, M, et al. Against the odds: a profile of marginalized and street-involved youth in BC. Vancouver: McCreary Centre Society; 2007.
Smith, A, Stewart, D, Peled, M, et al. A picture of health: highlights of the 2008 British Columbia Adolescent Health Survey. Vancouver: McCreary Centre Society; 2009.
Steinberg, L. Autonomy, conflict and harmony in the family relationship. In: Feldman S, Elliot G, eds. At the threshold: the developing adolescent. Cambridge, Mass: Harvard University Press, 1990.
Sullivan, H. The interpersonal theory of psychiatry. New York: Norton; 1953.
Tuttle, J, Bidwell-Cerone, S, Campbell-Heider, N, et al. Teen club: a nursing intervention for reducing risk-taking behavior and improving well-being in female African-American adolescents. J Pediatr Health Care. 2000;14(3):103–108.
US Census Bureau. Educational attainment in the United States, 2004, detailed tables: Table 1a. available at www.census.gov/population/www/socdemo/education/cps2004.html, 2004. [(accessed January 5, 2010)].
US Department of Health and Human Services, Administration on Children, Youth, and Families. Child maltreatment 2003. Washington, DC: US Government Printing Office; 2005.
US Department of Health and Human Services, Healthy people 2020: the road ahead. Washington, DC: The Department; 2009. available at www.healthypeople.gov/HP2020/default.asp [(accessed December 2009)].
Walker, L, de Vries, B, Trevethan, S. Moral stages and moral orientations in real-life and hypothetical dilemmas. Child Dev. 1987;58:842–858.
Widom, C, Kuhns, J. Childhood victimization and subsequent risk for promiscuity, prostitution and teen pregnancy: a prospective study. Am J Pub Health. 1996;86(11):1607–1611.
Zapalla, FR, Gidding, SS. Lipid management in children. Endocrinol Metab Clin North Am. 2009;38(1):171–183.