Physical Health Problems of Adolescence
http://evolve.elsevier.com/wong/ncic
Behavioral Health Problems of Adolescence, Ch. 21
Disorders Affecting the Skin, Ch. 18
Genitalia (Examination), Ch. 6
Health Promotion of the Adolescent and Family, Ch. 19
Infection Control, Ch. 27
Precocious Puberty, Ch. 38
Common Health Concerns of Adolescence
![]() Adolescents are subject to the same skin conditions that affect the school-age child, such as bacterial, viral, and fungal infections; contact dermatitis; and drug reactions. However, one skin disorder, although not limited to the adolescent age-group, appears predominantly at this time: acne vulgaris (common acne). Acne is the most common skin problem treated by physicians. Acne involves important anatomic, physiologic, biochemical, genetic, immunologic, and psychologic factors.
Adolescents are subject to the same skin conditions that affect the school-age child, such as bacterial, viral, and fungal infections; contact dermatitis; and drug reactions. However, one skin disorder, although not limited to the adolescent age-group, appears predominantly at this time: acne vulgaris (common acne). Acne is the most common skin problem treated by physicians. Acne involves important anatomic, physiologic, biochemical, genetic, immunologic, and psychologic factors.
More than half the adolescent population will have had acne by the end of the teenage years, and many children have evidence of the disorder before age 10. Acne usually occurs in middle to late adolescence, at age 16 to 17 years in girls and 17 to 18 years in boys. The disorder is more common in boys than in girls. After this age period the disease usually decreases in severity, but it may persist well into adulthood. Early acne occurs in the midface region (midforehead, nose, and chin) and later spreads to the lateral cheeks, lower jaw, back, and chest. The degree to which acne affects an individual may range from nothing more than a few isolated comedones to a severe inflammatory reaction. Although the disease is self-limiting and is not life threatening, its significance to the affected adolescent is great, and it is a mistake to underestimate its impact on teens.
Etiology
Numerous factors affect the development and course of acne. Research has shown a familial aspect to acne vulgaris, with a high occurrence of severe acne and increased sebum secretion among monozygotic twins. Forty-five percent of adolescent boys with acne have a positive family history, whereas only 8% of adolescent boys without acne have a positive family history. Premenstrual flares of acne occur in nearly 70% of girls, suggesting a hormonal cause. Scientific studies do not demonstrate a clear association between stress and acne; however, adolescents commonly cite stress as a cause for acne outbreaks. Cosmetics containing lanolin, petrolatum, vegetable oils, lauryl alcohol, butylstearate, and oleic acid can increase comedone production. Exposure to oils in cooking grease can be a precursor to acne in adolescents working in fast-food restaurants. There is no known link between dietary intake and the development or worsening of acne lesions.
Pathophysiology
Acne is a disease that involves the pilosebaceous unit, which consists of the sebaceous glands and hair follicles. Acne is most commonly found on the face, chest, upper back, and neck because of the large quantity of sebaceous glands on these skin areas. There are nearly 900 glands per square centimeter on the skin surfaces of the face, chest, neck, and upper back, compared with 100 glands per square centimeter on the rest of the body.
Three pathophysiologic factors have the greatest influence on acne development: excessive sebum production, comedogenesis, and the overgrowth of Propionibacterium acnes (Olutunmbi, Paley, and English, 2008). Increased sebum production begins at the time of adrenocortical maturation and subtly continues to increase until the late teens. Acne severity is proportional to the sebum secretion rate, which is genetically determined.
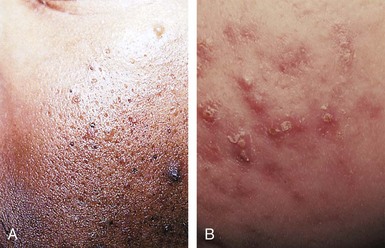
Comedogenesis (formation of comedones) results in a noninflammatory lesion that may be either an open comedone (blackhead) or a closed comedone (whitehead). Inflammation occurs with the proliferation of P. acnes, which draws in neutrophils, causing inflammatory papules, pustules, nodules, and cysts (Fig. 20-1). The traditional ice pick scarring results from macrophages that digest the inflamed skin along with the normal dermis in the process.
Psychosocial Ramifications
Adolescents are acutely aware of their physical appearance, and their cognitive development results in the feeling that they are constantly on stage. In one survey one third of teenagers reported that pimples were the first thing people noticed about them (Gupta and Gupta, 2003). A population-based study found that older adolescents with acne had lower self esteem, lower self-worth, and less body satisfaction than those without acne (Dalgard, Gieler, Holm, et al, 2008). The amount of psychologic stress does not directly correlate to the clinical severity of the acne. The importance of timely treatment has been underscored by research demonstrating the long-term psychologic impact of living with acne over critical developmental periods of life (Gupta and Gupta, 2003).
Therapeutic Management
Successful management of acne depends on a cooperative effort between the care provider, adolescent, and parents. The care provider must determine the adolescent’s goals and increase understanding of the cause and treatment of acne. Unlike many dermatologic conditions, the acne lesions resolve slowly, and improvement may not be apparent for at least 6 weeks. Individual comedones may take several weeks to months to resolve, and papules and pustules usually resolve in about 1 week.
The multifactorial causes of acne require a combined approach for successful treatment. Treatment consists of general measures of care and specific treatments determined by the type of lesions involved.
General Measures: The practitioner provides the adolescent with an overall explanation of the disease process, emphasizing the patient’s individual requirements. Parents should be present at the initial discussion to ensure their cooperation, understanding, and support. Remind adolescents that acne occurs, to some degree, in almost all teenagers.
Improvement of the adolescent’s overall health status is part of the general management. Adequate rest, moderate exercise, a well-balanced diet, reduction of emotional stress, and elimination of any foci of infection are all part of general health promotion. Review general skin care considerations, including limiting sun exposure and the use of noncomedogenic moisturizers and sunscreens.
Cleansing: Acne is not caused by dirt or oil on the surface of the skin. Gentle cleansing with a mild cleanser once or twice daily is usually sufficient. Antibacterial soaps are ineffective and may be drying when used in combination with topical acne medications. For some adolescents, hygiene of the hair and scalp appears to be related to the clinical activity of acne. Acne on the forehead may improve with brushing the hair away from the forehead and more frequent shampooing.
Medications
Treatment success depends on commitment from the adolescent. Before prescribing treatment, the clinician should determine the adolescent’s level of comfort and readiness to begin treatment. The teen should be reminded that clinical improvement may take weeks to months. Those who are impatient with speed of recovery may discontinue the medication or apply too much. Discussion about acne treatment should begin in early puberty. In young girls the early development of acne is the best predictor of future severe acne. Early intervention, most often with topical medications, may prevent the development of more severe acne.
Topical retinoids are the only drugs that effectively interrupt the abnormal follicular keratinization that produces microcomedones, the invisible precursors of the visible comedones. Retinoids are recommended as the first line of treatment for most forms of acne. Tretinoin has been the gold standard for topical retinoids and is available as a cream, gel, or liquid. The cream is less irritating than the gel, which is less irritating than the liquid. Newer formulations contain tretinoin trapped within porous copolymer microspheres that localize the medication to the follicle. These are less irritating to the skin because the medication is released over time, reducing the concentration on the skin (Guttman, 2009). The next-generation topical retinoids adapalene and tazarotene became available in the late 1990s. A comparison trial of the two medications found them to have similar efficacy, but adapalene gel 0.3% was better tolerated. After 12 weeks of treatment more than 50% of subjects in both treatment arms reported marked improvement or near clearing of acne (Thiboutot, Arsonnaud, and Pascale, 2008).
A gel combining 0.25% tretinoin and 1.2% clindamycin phosphate (Ziana gel) has been recently approved by the U.S. Food and Drug Administration (FDA). This gel has been shown to be more effective in treating acne than tretinoin or clindamycin monotherapy (Eichenfield and Wortzman, 2009).
Instruct the patient to begin with a pea-sized dot of medication, which is divided into the three main areas of the face and then gently rubbed into each area. The patient should not apply the medication until at least 20 to 30 minutes after washing to decrease the burning sensation. A daily moisturizer should be used along with retinoid treatment. Since sun exposure may easily result in severe sunburn, advise adolescents to avoid sun, apply the medication at night, and use a sunscreen with a sun protective factor (SPF) of at least 15 in the daytime.
Topical benzoyl peroxide is an antibacterial agent that inhibits the growth of P. acnes. Benzoyl peroxide is effective against both inflammatory and noninflammatory acne and is an effective first-line agent. The medication is available as a cream, lotion, gel, or wash. Using benzoyl peroxide is less likely to result in the development of antibiotic-resistant strains of P. acnes, which makes it an ideal adjunct when topical or oral antibiotic treatment is employed (Bowe and Shalita, 2008). Benzoyl peroxide soaps are convenient because they can be applied in the shower and assist in the treatment of acne on the chest and back. Benzoyl peroxide and salicylic acid are the most common ingredients in popular and effective acne treatment kits available over the counter. Patient education should include information regarding the bleaching effect of the peroxide on sheets, bedclothes, and towels. The adolescent can be reassured that skin bleaching will not occur. The drying effects of the medication can be accommodated with gradual increases in strength and frequency of application.
When inflammatory lesions accompany the comedones, a topical antibacterial agent may be prescribed. These agents are used to prevent new lesions and to treat preexisting acne. Clindamycin, erythromycin-metronidazole, and azelaic acid are currently available topical antibiotics. Side effects of these medications include erythema, dryness, and burning; using the medications every other day will decrease the adverse effects. Topical antimicrobials combined with benzoyl peroxide are more effective than either product alone. Retinoids in combination with antimicrobials also improve the penetration of these topical agents and are the only means to address three of the pathogenic causes of acne: keratinization, P. acnes, and inflammation. Combination therapy is usually more effective than either component alone (Krakowski, Stendardo, and Eichenfield, 2008).
Systemic antibiotic therapy is initiated when moderate to severe acne does not respond to topical treatments. The foundation for using systemic antibiotics in acne treatment has been the elimination of the inflammatory effects of P. acnes by suppressing the bacteria. Tetracycline, erythromycin, minocycline, doxycycline, and amoxicillin are systemic antibiotics used to treat acne (Olutunmbi, Paley, and English, 2008; Yan, 2006). They are relatively free of side effects with the exception of occasional gastrointestinal upset, photosensitivity, or vaginal candidiasis. Minocycline is more expensive but is less likely to cause gastrointestinal side effects and is very effective against severe inflammatory acne. Resistance to antibiotics may develop, especially with tetracycline and erythromycin. Judicious use of oral antibiotics and avoidance of topical antibiotics in combination with oral treatment can prevent resistance. Providers should avoid use of multiple antibiotic classes and shorten the course by using the full dose of systemic antibiotics for 1 month and then begin to taper the dosage. The adolescent can then be maintained on topical treatment (Krakowski, Stendardo, and Eichenfield, 2008).
Girls with mild to moderate acne may respond to topical treatment and the addition of an oral contraceptive pill (OCP). OCPs reduce the endogenous androgen production and decrease the bioavailability of the woman’s circulating androgens. Combination OCPs containing levonorgestrel, gestodene, and desogestrel as the progestin decrease acne in women. The FDA has approved multiple combination OCPs for the treatment of acne in girls. Visible improvement may take up to 4 months.
Isotretinoin 12-cis-retinoic acid (Accutane), a potent and effective oral agent, is reserved for severe, cystic acne that has not responded to other treatments. Isotretinoin is the only agent available that affects all factors in the development of acne. Only physicians who have taken a comprehensive educational program about the medication, necessary monitoring of patients, and parameters for pregnancy prevention may manage treatment with isotretinoin. Adolescents with multiple, active, deep dermal or subcutaneous cystic and nodular acne lesions are treated for 20 weeks. Long-term remissions occur with this highly effective drug. However, multiple cutaneous side effects can occur, which vary from mild to moderate in severity. Dry skin, dry eyes, dry mucous membranes, nasal irritation, decreased night vision, photosensitivity, arthralgia, headaches, mood changes, depression, and suicidal ideation may occur. There is some concern that isotretinoin may be associated with increased incidence of depression and suicide despite several findings to the contrary (Webster, 2009). Careful monitoring for signs of depression among all adolescents taking isotretinoin is recommended as part of all health visits for acne treatment (Hull and D’Arcy, 2003; Jacobs, Deutsch, and Brewer, 2001). The most significant side effects are the teratogenic effects, causing limb and skull abnormalities. Isotretinoin is absolutely contraindicated in pregnant women. Sexually active young women must use an effective contraceptive method during treatment and for 1 month after treatment. Providers should also monitor patients receiving isotretinoin for elevated cholesterol and triglyceride levels. Significant elevation may require discontinuation of the medication.
Scarring begins early in all types of acne, from papulopustular to nodulocystic. Most of the scarring is a result of loss of tissue rather than thickening. Chemical peels have been traditionally used for the treatment of scarring in acne. Only the mildest acne scarring will actually resolve with chemical peels. Fractional photothermolysis using laser technology is considered to be as effective as carbon dioxide lasers for treating acne scarring; some side effects are associated with carbon dioxide laser therapy (Chapas, Brightman, Sukai, et al, 2008; Walgrave, Ortiz, MacFalls, et al, 2009).
Nursing Care Management
The health screening interview should contain questions regarding the adolescent’s concern about acne. Because acne is so common and its appearance may seem so mild, the health care provider may underestimate the relative importance of the disease to the adolescent. The nurse should assess the individual adolescent’s level of distress, current management, and perceived success of any regimen before initiating a referral. If the adolescent does not perceive the acne to be a problem, he or she may lack motivation to follow the treatment plan. The primary care provider can manage most cases of acne without referral to a dermatologist.
The nurse can provide ongoing support for the adolescent when a treatment plan has been initiated. Encourage the family to support the adolescent in his or her efforts. Discuss the use of the medications and basic skin care information in detail with the adolescent. Written information to accompany the discussion is helpful. Inform patients that it will take 6 to 8 weeks to appreciate improvement in their skin. Information to dispel myths regarding the use of abrasive cleansing products as a means of removing blackheads can prevent unnecessary costs and trauma to the skin. Teenagers also need to be educated about factors that may aggravate acne and damage skin, such as too vigorous scrubbing. Picking, squeezing, and manual expression with fingernails breaks down ductal walls and causes acne to worsen. Mechanical irritation, such as vinyl helmet straps that rub areas predisposed to acne, can cause the development of lesions.
Vision Changes
Vision changes are common during the teenage years. The onset of refractory errors or worsening of previous errors peaks in adolescence as a result of the growth spurt. Other than myopia, new eye problems in this age-group are rare. Vision screening is usually performed in the school by nurses, and referrals are made as required to correct vision problems. The main goal is to detect new refractive errors. Adolescents with vision changes are referred for contacts or glasses as appropriate.
Health Problems of the Male Reproductive System
Common congenital anomalies of the penis are almost always detected and corrected in infancy or early childhood. In some cases boys who need an operative procedure to repair hypospadias (the most common congenital deformity of the penis) may reach adolescence with a penis that looks different from those of their friends. A few who have received no medical care have uncorrected deformities that can cause serious psychologic problems during this sensitive period of development. These young boys need to be identified for surgical repair of the defect.
Uncircumcised males may encounter some problems during adolescence related to a tight foreskin that cannot be retracted over the enlarging glans; some males may not cleanse the area properly. These boys are at risk for more frequent infections. Penile carcinoma is associated with human papillomavirus types 16 and 18 (HPV 16, 18). Although HPV is a common sexually transmitted infection (STI) among American males, penile carcinomas are rare in the United States and most Western countries.
Trauma to the penis, including burns and accidental injuries, can occur in various ways. The frenulum (the fold on the lower surface of the glans that connects it with the prepuce) can be torn after retraction of the foreskin, unusually rough masturbation, or coitus. It can be frightening to the young boy but usually heals spontaneously with minimum care. However, any extensive bleeding may require suturing of the tissues. Penile fracture is a rupture of the corpus cavernosum as a result of blunt trauma to the erect penis, usually during vigorous sexual intercourse or manipulation. The condition is considered a urological emergency, and surgical repair is recommended to prevent further complications (Al-Shaiji, Amann, and Brock, 2009; Maruschke, Lehr, and Hakenberg, 2008).
Drugs such as trazodone (Desyrel), taken alone or in combination with cocaine or Ecstasy (MDMA [3-4 methylenedioxymethamphetamine]), may cause a prolonged erection (priapism), which can be extremely uncomfortable and in some cases may require surgical intervention to release blood trapped in the corpus cavernosum. Drugs available to adults for erectile dysfunction or other drugs not intended for recreational uses may have unintentional and undesirable side effects (James and Mendelson, 2004).
Testicular Tumors
Tumors of the testes are not a common condition but are usually malignant when found in adolescence. Testicular carcinomas account for 7% of the malignancies that occur in 15- to 19-year-olds in the United States (Reaman and Bleyer, 2006). Testicular cancer is the most common solid tumor in males 15 to 34 years of age. The usual presenting symptom is a heavy, hard, painless mass that is palpable on the anterior or lateral aspect of a testis. The tumor may be smooth or nodular and does not transilluminate unless accompanied by a hydrocele. The involved testicle hangs lower and is therefore more susceptible to trauma. Although not all scrotal masses are malignant, any firm swelling of the testes demands immediate evaluation. If a firm swelling is noted, the adolescent should be evaluated by ultrasonography and immediately referred for direct biopsy if the mass is found to be solid.
Treatment for testicular cancer consists of surgical removal of the affected testicle (orchiectomy) and the adjacent lymph nodes if they are affected. If metastases are evident in more distant nodes or organs, chemotherapy and radiotherapy are implemented. (See Chapter 36.)
Nursing Care Management
To supplement routine health assessment, every adolescent boy should learn to perform monthly testicular self-examination (TSE). This provides an opportunity for the adolescent to familiarize himself with his own anatomy and to ensure early detection of any abnormality. In the TSE each testicle is examined individually, preferably after a warm bath or shower, when scrotal skin is more relaxed, using the thumbs and fingers of both hands and applying a small amount of firm, gentle pressure. The normal testicle is a firm organ with a smooth, egg-shaped contour. The epididymis can be palpated as a raised swelling on the superior aspect of the testicle and should not be confused with an abnormality. The nurse can play an important role in providing anticipatory guidance to all adolescent boys. This guidance includes an explanation of the rationale for TSE and how to perform this procedure (see Critical Thinking Exercise).
Varicocele
A varicocele is characterized by elongation, dilation, and tortuosity of the veins of the spermatic cord superior to the testicle. The finding is rare in prepubertal children, but the incidence increases dramatically at the onset of puberty. Idiopathic varicocele is the most common treatable cause of male-related impaired fertility, especially if caught and treated early (Zampieri, Mantovani, Ottolenghi, et al, 2009). Varicoceles occur most often on the left side because of the greater length of the left spermatic vein and its entry into the left renal artery; the right spermatic vein enters the vena cava directly and at a lesser angle, which may be a source of future difficulty. A varicocele can be palpated as a wormlike mass situated above the testicle that decreases in size when the male is recumbent and becomes distended and tense when he is upright. Some males may experience discomfort during sexual stimulation.
In pubertal boys the left testicle is usually larger than the right. However, when there is an associated varicocele, the left testicle is usually smaller than the right. Testicular size and levels of dihydrotestosterone in seminal plasma decrease with increasing duration of the varicocele. Varicocelectomy is indicated in adolescents when there is growth arrest of the affected testicle or when there is pain associated with the varicocele. Currently, improvement in testicular volume is the main outcome measure following varicocelectomy in children and adolescents. Several recent studies have shown significant catch-up growth after surgical treatment (Sakamoto, Ogawa, and Yoshida, 2008; Sakamoto, Saito, Ogawa, et al, 2008). Surgical repair of varicoceles in adult men is less successful than in children and adolescents. There is no statistical difference in catch-up growth postoperatively for males between 10 and 24 years of age (DeCastro, Shabsigh, Poon, et al, 2009). Whether there is a correlation between testicular catch-up growth and testicular function is still to be determined.
Epididymitis
Epididymitis is an inflammatory reaction of the epididymis of the testicle as a result of an infection (bacterial or viral), a chemical irritant (urine), or a nonspecific cause (local trauma). The clinical presentation is an insidious (slow) onset of unilateral scrotal pain, redness, and swelling. Associated symptoms include urethral discharge, dysuria, fever, and pyuria. Epididymitis is not associated with gastrointestinal symptoms as found in testicular torsion. The causative factor in males less than 35 years of age is thought to be predominantly Chlamydia trachomatis, although nearly 90% do not have laboratory evidence of the bacteria from urethral swab (Tracy, Steers, and Costabile, 2008). Mild presentation of symptoms may mimic testicular torsion, which requires immediate surgical intervention. Therefore immediate evaluation by a practitioner is indicated. Treatment consists of analgesics, scrotal support, bed rest, and appropriate antibiotic therapy. Conduct an assessment for other STIs, including human immunodeficiency virus (HIV), for adolescent males who test positive for chlamydia.
Testicular Torsion
Intravaginal torsion of the testicle is a condition in which the tunica vaginalis, which normally encases the testicle, fails to do so and the testis hangs free from its vascular structures. This condition can result in partial or complete venous occlusion with rotation around this vascular axis. In severe torsion the organ can become swollen and painful; the scrotum becomes red, warm, and edematous and appears to be immobile or fixed as a result of spasm of the cremasteric fibers.
Testicular torsion occurs in 1 in every 4000 males, with a peak onset at 13 years of age. Rapid growth and increasing vascularity of the testicle are thought to be precursors to torsion, accounting for the occurrence at puberty (Gatti and Murphy, 2008). Testicular torsion is the most common cause of testicular loss in young males (Adelman and Joffe, 2000; Mansbach, Forbes, and Peters, 2005). Typically, the adolescent complains of pain that was either acute or insidious in onset and that has radiated to the groin. Nausea, vomiting, and abdominal pain may accompany the pain; the cremasteric reflex is often absent. Fever and urinary symptoms are generally not present. The history often reveals that similar painful episodes have occurred previously, resolving spontaneously. Emergency surgery is often necessary to preserve the testicle.
Nursing Care Management
Nurses should be alert to the possibility of testicular torsion in adolescents who complain of scrotal pain. Because torsion often results from trauma to the scrotum, school nurses are likely to encounter such injuries and should refer the adolescent for medical evaluation immediately.
Gynecomastia
Some degree of bilateral or unilateral breast enlargement occurs frequently in young boys during puberty. Approximately half of adolescent boys have transient gynecomastia, which usually lasts less than 1 year. When gynecomastia has a prepubertal onset, the adolescent should be evaluated for rare adrenal or gonadal tumors, liver disease, or Klinefelter syndrome. Gynecomastia may also be drug induced; calcium channel blockers, cancer chemotherapeutic agents, histamine2-receptor blockers, and oral ketoconazoles have all been shown to cause the disorder. Some report that marijuana causes gynecomastia.
If gynecomastia persists or is extensive enough to cause embarrassment, plastic surgery is indicated for cosmetic and psychologic reasons. Administration of testosterone has no effect on breast development or regression and may even aggravate the condition.
Health Problems of the Female Reproductive System
Whether it is her first experience or one of many, adolescent girls are often apprehensive before a pelvic examination. Adolescents are self-conscious about their bodies and the changes taking place. The adolescent needs anticipatory guidance regarding what to expect and what she can do to help herself relax during the procedure. Many fears and apprehensions are a result of information she has obtained from family members and friends. The discussion should begin by addressing these anxieties.
The ideal time to begin preparing a girl for examination of the genitalia is as she is entering puberty. External genitalia examination should always be included as part of a routine physical assessment; excluding the genitalia reinforces the attitude that sexuality is something to be avoided.
The timing of the initial pelvic examination is controversial; the ultimate decision depends on the adolescent and the health care provider. Indications for a pelvic examination during adolescence are listed in Box 20-1. The advent of effective urine based STI tests has added to the controversy, since assessment for many STIs can be done without the use of the speculum.
The pelvic examination provides an excellent opportunity for teaching about hygiene, body functions, and sexuality. Encourage the girl to ask questions about changes in her body and the implications. The pelvic examination also allows an opportunity to discuss practicing safer sex, preventing STIs, and postponing sexual involvement. Lack of knowledge is a factor in risky sexual experimentation in adolescence.
The pelvic examination should be as nonstressful as possible. Nurses should attempt to make the initial pelvic examination a positive experience for the adolescent, since this can increase the likelihood of compliance with annual visits. The teenager should have the option of choosing a supportive person to be present during the examination. Suggested individuals might include a parent, best friend, boyfriend, or other health professional. The use of models and drawings and a display of equipment to be used facilitate understanding. Allowing the adolescent to handle the speculum may help decrease some of the fear. The adolescent is given the choice of wearing a gown or her own clothing during the examination. A description of the examination, including information about the procedure and words that describe anticipated feelings and sensations experienced during the examination, may reduce anxiety. Of major concern to the adolescent is fear of discovery of a pathologic pelvic condition. Reassurance regarding normal physical findings is extremely important.
Most girls favor a semisitting position, which has the additional advantage of allowing eye contact during the procedure. Sometimes a pillow helps the patient feel more comfortable and less vulnerable. The provision of a mirror for the girl to see what is taking place if she so desires helps the examiner explain various aspects of anatomy. When possible, it is important to respect the adolescent’s request for a female provider.
Numerous techniques have been described to teach women to relax during a pelvic examination, including breathing exercises, imagery, and other strategies for reducing stress. (See Pain Management, Chapter 7.) However, these techniques are not effective with all individuals. When the examination is finished, the provider discusses the findings with the adolescent and makes referrals if indicated. Written materials are useful educational materials.
Menstrual Disorders
The mean age of menarche in the United States is 12.55 years for non-Hispanic Caucasian, 12.06 for African-American, and 12.25 for Mexican-American girls, with 80% of girls beginning between 11 and 13.75 years of age (Chumlea, Schubert, Roche, et al, 2003). Pubertal development proceeds in a predictable sequence and tempo. When evaluating an adolescent with amenorrhea, the nurse requires an accurate history of the timing of development of secondary sexual characteristics. Primary amenorrhea is defined as no menses by age 15. An evaluation is necessary at age 13 if the girl has no secondary sexual characteristics or if menarche does not follow within 3 years of the onset of secondary sexual characteristics. Secondary amenorrhea is no menses for 6 months in a previously menstruating female when pregnancy has been excluded. Secondary amenorrhea is much more common than primary amenorrhea.
It is not unusual for an adolescent to have irregular menses when establishing ovulatory cycles. This is a result of an immature hypothalamic-pituitary-ovarian axis. In general, the later menarche occurs, the longer the period of anovulation. Two thirds of adolescent girls establish regular menstrual cycles by 2 years after menarche. Oligomenorrhea (abnormally light or infrequent menstruation) early after menarche is not uncommon. After a careful examination to rule out any physical abnormalities, including signs of androgen excess and congenital defects of the genital tract, the young girl and parent can be given reassurance with no additional evaluation.
Amenorrhea
The causes of amenorrhea can be divided into organ system and estrogen status. The most common cause of amenorrhea is pregnancy. A pregnancy test is an essential part of the evaluation for all females with amenorrhea, regardless of the sexual history. The next most prevalent causes of amenorrhea in adolescents are polycystic ovary syndrome and hypothalamic amenorrhea. For girls who are more than 2 or 3 years past menarche, the most common hypothalamic causes of amenorrhea are eating disorders, excessive exercise, medication, and stress (Wiksten-Almstromer, Hirschberg, and Hagenfeldt, 2007).
Polycystic ovary syndrome (PCOS) is a common endocrine disorder. There are no formal diagnostic criteria for teens with PCOS, and the cause is unclear. The characteristic findings are hyperandrogenism, chronic anovulation, and polycystic ovaries. Other ovarian causes of amenorrhea include gonadal dysgenesis; the most common form is Turner syndrome. Girls with Turner syndrome have delayed puberty, short stature, webbed neck, widely spaced nipples, and cardiac and kidney abnormalities. Premature ovarian failure, galactosemia, and ovarian tumor are other ovarian causes of amenorrhea.
Thyroid disease is not uncommon in adolescents and is more common in females than males. Both hypothyroidism and hyperthyroidism may result in menstrual irregularities, with the latter more likely to cause amenorrhea.
Adrenal causes of amenorrhea include congenital adrenal hyperplasia, which is an autosomal recessive disorder of steroidogenesis. Nonclassic adrenal hyperplasia is characterized in adolescents by hirsutism or amenorrhea. Pituitary causes of amenorrhea include prolactinoma, Cushing syndrome, and sarcoidosis.
Primary amenorrhea in an adolescent complaining of periodic (usually monthly) lower abdominal pain with evidence of estrogen production and sexual maturation may be related to an imperforate hymen, closed hymen from female circumcision, or transverse vaginal septum. The treatment is simple surgical perforation and drainage. Other anatomic causes of the amenorrhea include intrauterine adhesions and congenital absence of a uterus.
Menstrual Irregularities in the Female Athlete
The most common clinical indications of potentially adverse effects of exercise on an adolescent’s reproductive cycle include (1) delayed menarche, (2) anovulation associated with dysfunctional uterine bleeding, and (3) oligomenorrhea or amenorrhea with hypoestrogenic states. Researchers have not been able to identify the exact mechanism of these menstrual changes. The most probable cause is at the hypothalamic level as a result of an imbalance of the amount of energy in (food) compared to the energy out (exercise). Amenorrhea is so common among female athletes that it is misinterpreted as normal by athletes, coaches, and some health care providers. Prevalence of amenorrhea has been found to be as high as 69% among ballet dancers and 65% among distance runners. Eating disorders are often part of the syndrome with exercise-induced amenorrhea (Warren and Chua, 2008). Adolescents who exercise intensely and have menstrual bleeding more frequently than every 21 days or at intervals of 35 to 120 days are likely to have chronic anovulation. They usually produce estrogen but have inadequate levels of progesterone. Unopposed estrogen can lead to endometrial hyperplasia and theoretic risk of endometrial adenocarcinoma.
In addition to menstrual dysfunction, female athletes also may be at risk for eating disorders and decreased bone mineral density (Joy, Van Hala, and Cooper, 2009). Any adolescent athlete who becomes amenorrheic requires medical evaluation to rule out other causes of amenorrhea and to assess for disordered eating (Sherman and Thompson, 2004). Sometimes a trial of decreasing the intensity or duration of exercise and improving nutrition will relieve irregularities. Careful evaluation by a health care provider who specializes in the treatment of eating disorders and athletes is essential. (See Chapter 39.)
Dysmenorrhea
Dysmenorrhea is defined as painful menstrual flow. Primary dysmenorrhea is painful menses without any identifiable pathologic disorder. Primary dysmenorrhea is the most common cause of painful menses in adolescents. Secondary dysmenorrhea is defined as painful menses with a pathologic condition such as endometriosis, salpingitis, or congenital anomalies of the müllerian system. The incidence of dysmenorrhea increases as adolescents mature; at age 12 years the prevalence is reported at 38%, and it increases to 66% to 77% by age 17 (Slap, 2003). It is a leading cause of recurrent absence from work and school.
Etiology: The factor present in all instances of primary dysmenorrhea is the onset of ovulatory cycles. Although it is not invariable, the symptoms do not occur during the first few postmenarchal months or during months of irregular anovulatory menses. After the progesterone withdrawal before menstruation, prostaglandins and leukotrienes are released in the uterus, causing an inflammatory response. This response is the cause of cramping and the systemic symptoms of nausea, vomiting, bloating, and headaches. Levels of prostaglandins are higher in the menstrual fluid of women with dysmenorrhea (Harel, 2008).
Clinical Manifestations: Typical complaints of the adolescent with dysmenorrhea are lower abdominal cramping and pain or discomfort. About 50% of girls also have systemic symptoms, including nausea and vomiting, fatigue, nervousness, diarrhea, and headache. The pain usually begins several hours before the appearance of visible vaginal bleeding, is most severe on the first day of menstruation, and may last from a few hours to a day or more but seldom exceeds 2 or 3 days. The symptoms and degree of discomfort vary considerably from one individual to another and from one period to another in the same female. The pain may be only a mild, fleeting discomfort or so severe as to be incapacitating, requiring absence from school. After adolescence the menstrual discomfort decreases with age, and it may resolve completely after childbirth.
Therapeutic Management: A careful history, including a menstrual and sexual history, is necessary. In addition, a careful review of gastrointestinal and genitourinary systems is necessary to rule out problems. A thorough gynecologic examination is carried out to exclude any pelvic abnormalities. The pelvic examination may not be indicated in an adolescent who is not sexually active and who responds to medical therapy.
The treatment of choice for adolescents is the administration of nonsteroidal antiinflammatory drugs (NSAIDs). These drugs block the formation of prostaglandins, leading to a reduction in uterine activity and prevention of pain. Antiprostaglandins are taken for only 2 or 3 days of the menstrual cycle. Prophylactic use of NSAIDs has proved effective when begun a few days before the onset of the menses, approximately 11 days after ovulation. The relief appears to be a result of prostaglandin inhibition rather than analgesic effect.
A variety of drugs that are taken at the onset of symptoms are available without prescription, such as ibuprofen and naproxen. The fenamates have the additional benefit of antagonizing the action of already-formed prostaglandins. If NSAIDs are unsuccessful in relieving the pain or if the adolescent desires contraception, cyclic estrogen therapy to prevent ovulation can provide dramatic and predictable relief from pain. Oral contraceptives are effective in approximately 90% of cases.
Transcutaneous electrical nerve stimulation, which reduces the perception of pain, has been an effective nonpharmacologic source of relief of pain associated with dysmenorrhea but less effective than NSAIDs. Insufficient evidence is available to prove whether acupuncture is effective. Small clinical studies have demonstrated positive effects, but randomized, placebo-controlled trials are needed (Yang, Liu, Chen, et al, 2008). Exercise is widely believed to alleviate dysmenorrhea by improving pelvic blood flow and stimulating the release of β-endorphins, which have an analgesic effect.
Nursing Considerations: The nurse may be the person to whom a young woman turns for advice regarding menstrual problems. The nurse should provide anticipatory guidance concerning menstrual physiology and hygiene and the importance of a well-balanced diet, exercise, and general health maintenance. Adolescents need information regarding availability of effective treatment for dysmenorrhea. Only about 50% of females with dysmenorrhea take medication to relieve the symptoms, even though effective treatment is available. The nurse should review correct dosing, since many adolescents use subtherapeutic doses of medication. Timing of the onset of the treatment requires the use of a menstrual calendar.
Most of the prostaglandin inhibitors are available without prescription. Whatever drug the adolescent chooses, she needs to be told how the drug produces its effect, how to take the drug for maximum effect, and the side effects. The drug should be taken with food and a full glass of water. If no satisfactory relief is achieved, refer the adolescent for further evaluation.
Endometriosis
Dysmenorrhea that is not substantially relieved within 6 months of taking OCPs and NSAIDs requires an evaluation with laparoscopy to rule out endometriosis. The disease is much more common in adolescents than was previously thought, with incidence rates ranging from 47% to 67% (Templeman, 2009).
Endometriosis is defined as the presence of endometrial glands and stroma outside the normal intrauterine endometrial cavity. The etiology is still unclear; risk factors include early menarche and late menopause. Research now suggests there is a genetic component to the etiology. The use of OCPs is protective and decreases the risk of endometriosis for up to 1 year after the method is discontinued. The presentation of endometriosis is variable, but women with surgical diagnosis of endometriosis are more likely to have dysmenorrhea, dyspareunia, pelvic pain, and menorrhagia. In addition, women with endometriosis are likely to have subfertility or infertility (Ballard, Seaman, de Vries, et al, 2008).
Treatment is medical, surgical, or a combination. The goal of treatment is pain control and suppression of the disease. The patient and family need to understand that the recurrence rate is high and that currently no cure is available for the disease.
Premenstrual Syndrome
Although premenstrual syndrome (PMS) was first described in 1931, after several decades of research it remains poorly defined. The natural history of PMS is not known. It has more than 200 reported symptoms, and, with no confirmatory laboratory test, providers are hesitant to initiate treatment (Braverman, 2007). Research about PMS in adolescents is sparse; pharmacologic treatment trials have not included adolescent subjects. The symptoms are stable across cycles, occur regularly in the late luteal phase, and resolve within days of onset of menstrual bleeding. The manifestations most frequently cited are irritability, mood swings, headache, anxiety, and depression with the physical complaints of bloating, fatigue, and breast tenderness.
PMS is very common, occurring at some point in most women’s reproductive lives. When specific diagnostic criteria are used, about 30% of women are significantly affected by moderate to severe symptoms. Only 5% to 8% of women meet the criteria for premenstrual dysphoric disorder (PMDD) (Rapkin and Mikacich, 2008). PMDD is characterized by symptoms of marked and persistent anger, irritability, mood swings, anxiety, and affective lability sufficient to cause significant impairment in one’s ability to function occupationally or socially during the week preceding menses (Vigod, Ross, and Steiner, 2009).
Accurate diagnosis of PMS requires a thorough history and careful physical examination to exclude other medical or psychiatric conditions. A daily report form enables the young woman to pinpoint symptoms, which allows for monitoring during treatment. The diagnosis is made when at least one disabling physical or psychologic symptom is present up to 2 weeks before menses with remission when the menstrual flow begins (Rapkin and Mikacich, 2008). Currently, few well-controlled studies demonstrate effective treatment. Treatment options vary depending on the type and severity of symptoms.
Nutritional supplements have long been recommended as a treatment for PMS. Supplementation with 1200 mg/day of calcium and vitamin D has been demonstrated to reduce water retention, food craving, and pain (Bertone-Johnson, Hankinson, Bendich, et al, 2005). There is no clear evidence that dietary supplements such as vitamin B6, primrose oil, or multivitamins are effective in the treatment of PMS. High-intensity aerobic exercise improves symptoms of PMS in adult studies.
An OCP containing a new progestin called drospirenone in a regimen of 24 active and four inactive pills has been demonstrated to be effective in the treatment of PMDD (Rapkin and Mikacich, 2008). Case reports have shown that adolescents with PMDD respond well to fluoxetine given in the luteal phase (Hetrick, Merry, McKenzie, et al, 2007).
The nurse can provide information regarding direct-care measures, adequate rest, good nutrition, and regular exercise. Families often have questions about the myriad treatment options available. The nurse can provide information about current recommended therapies. The nurse can teach patients to cope with the psychosocial aspect of the syndrome through stress reduction techniques, counseling, and support groups.
Dysfunctional Uterine Bleeding
Dysfunctional uterine bleeding (DUB) is abnormal vaginal bleeding that occurs in the absence of pregnancy, infection, neoplasms, or any other demonstrable pathologic condition or disease. DUB is usually associated with anovulation and is the most frequent urgent gynecologic problem for adolescents. During adolescence, abnormalities in the menstrual flow’s timing (intervals of <20 or >40 days), length (>8 days’ duration), and amount (>80 ml) can occur frequently. This irregularity is usually attributed to immaturity of the positive feedback mechanism between the hypothalamic-pituitary-gonadal axis and absence of the luteinizing hormone surge late in the menstrual cycle. The result is anovulatory cycles in which the production of estrogen is unopposed because of a lack of progesterone. The effect of the estrogen is an increase in the thickness of the endometrial lining without structural integrity. Without progesterone, menstrual flow is not limited. Not all anovulatory females have DUB. One contributing factor is the amount of endogenous estrogen.
A comprehensive health history and physical examination, including a pelvic examination, are indicated to ascertain the cause of bleeding. The initial assessment should include the amount of blood loss and the possible need for hospitalization. Common causes of vaginal bleeding need to be ruled out before the diagnosis of DUB can be established. The most common reason for vaginal bleeding in adolescence is pregnancy. Other causes of vaginal bleeding can be related to anatomic anomalies, foreign bodies, endocrine disease, STIs, chronic illness, or previously undetected familial bleeding disorders (e.g., von Willebrand disease).
Treatment of vaginal bleeding depends on determination of the underlying mechanism. The initial management depends on the amount of blood lost and the patient’s symptoms. If the bleeding is infrequent and not associated with anemia, reassurance and a menstrual calendar for follow-up monitoring are often sufficient.
When moderate anemia occurs, hormonal therapy, in the form of OCPs or cyclic medroxyprogesterone, has been beneficial. The adolescent needs to know that, at completion of the recommended regimen, a heavy flow with cramping will probably occur for 3 or 4 days. Without this information, she may believe that her condition is worse and assume that the treatment was ineffective. Untreated patients are at increased risk for endometrial hyperplasia and adenocarcinoma from the persistent, unopposed estrogen stimulation of the endometrium. The OCPs are continued for several months, after which bleeding irregularities seldom recur. DUB may persist for up to 2 years in more than half the cases.
Dilation and curettage may be necessary to control hemorrhage in severe cases or in those that do not respond to more conservative management. Supplemental iron is sometimes needed to correct anemia. Normally menstruating females average a loss of 1 mg of iron daily; thus blood loss of more than 80 ml/month is a significant risk factor for the development of iron deficiency anemia and signifies the need for oral iron therapy (Ferrara, Coppola, Coppola, et al, 2006).
Nursing Care Management
Ordinarily, only reassurance and attention to general health status are needed, with emphasis on a well-balanced diet, adequate rest, and moderate exercise. The nurse should instruct the adolescent to use a menstrual calendar to track improvement and guide future interventions. When OCPs are prescribed, the adolescent and her parents need careful explanation of the use of these medications. The high-dose estrogen OCPs can result in nausea and vomiting. Anticipatory supportive care includes preparation for procedures if these are a possibility.
Vaginitis and Vulvitis (Vulvovaginitis)
A small quantity of vaginal mucus is normal and in adolescent girls usually increases at the time of ovulation and before the onset of menstruation. It is characteristically clear and, except in rare instances when it appears in large amounts, causes no discomfort. However, some teenagers mistakenly believe that the discharge is a sign of vaginal infection. After an examination the girl can generally be reassured and given anticipatory guidance about hygiene and the increased secretions associated with sexual excitement.
Leukorrhea is the term used to describe a glutinous, gray-white discharge, which can be caused by physical, chemical, or infectious agents. Physical causes include foreign bodies such as a forgotten tampon. Irritation from pinworms, bubble bath, douching, deodorant pads or tampons, or improper wiping after defecation can also cause leukorrhea. The resulting discharge may be purulent, blood tinged, or brown with an offensive odor. Removal of the offending material is usually all that is necessary.
The normal vaginal flora is predominantly composed of Lactobacillus acidophilus, which produces lactic acid and hydrogen peroxide to maintain an acidic environment. Vaginitis occurs when pathogens or changes in the environment disrupt this balance. Oral antibiotics, oral and vaginal contraceptive agents, sexual intercourse, douching, and stress may allow pathogen proliferation and the development of vaginitis.
Vulvovaginal candidiasis results when Candida organisms begin to proliferate, resulting in overgrowth and infection. The most common organism is Candida albicans, accounting for 80% to 90% of infections; Candida glabrata occurs in 10% to 20% of cases. Susceptibility to candidiasis can be increased by a number of factors, including estrogen status, presence of glycogen, and the loss of protective bacterial flora from broad-spectrum antibiotics. A small percentage of women have recurrent yeast infections, four or more episodes in a year, and would benefit from culture identification of the Candida species. The nurse should be alert to risk factors for HIV, since recurrent or persistent vulvovaginal candidiasis may be the first symptom of the infection.
The adolescent with vulvovaginal candidiasis generally has vaginal pruritus and sometimes dysuria. The presence of the classic thick “cottage cheese–like” discharge is seen in a minority of patients. Most females have a minimum amount of an uncharacteristic discharge. The diagnosis is easy to confirm with microscopic evaluation.
First-line treatment of candidiasis remains the administration of over-the-counter topical antifungal drugs. The medications are available in cream, lotion, suppository, and tablet formulations. Shorter treatment regimens are associated with increased compliance; those with recurrence may benefit from a longer course (7 to 14 days). Oral 1-day treatment regimens are safe and as effective as topical treatments but may result in more systemic side effects. Treatment of the male partner in sexually active adolescents is not necessary unless the glans penis is inflamed. The adolescent should be advised to expect decreased symptoms in 24 to 72 hours and complete resolution in 6 to 8 days, regardless of treatment type.
Trichomonas vaginalis is an anaerobic parasitic protozoan involved in 20% to 30% of all cases of vaginitis. It is the most prevalent nonviral STI in adolescents. The infection was once considered a nuisance infection but is now recognized to play a role in several poor health outcomes. Females with T. vaginalis are more likely to acquire HIV, herpes, and pelvic inflammatory disease (PID). Infection with T. vaginalis doubles the risk of persistent HPV infection in women and increases the shedding of HIV among both men and women with HIV infection (Pattullo, Griffeth, Ding, et al, 2009).
The infection is often asymptomatic and self-limiting in men. Women may be asymptomatic, but many have a vaginal discharge and vulvovaginal soreness. Dysuria and an odor may accompany the symptoms. T. vaginalis diagnosis has traditionally been made by microscopic visualization of the motile trichomonads from a vaginal wet mount specimen. This has low sensitivity depending on the clinician’s skills with microscopy and the length of time from specimen collection to observation. Culture is the gold standard but is expensive, is not widely available, and requires 4 days for a final reading. More commercially available tests for T. vaginalis are now offered; these are more sensitive than wet prep and less costly than culture.
Metronidazole or tinidazole is used for the treatment of T. vaginalis, in either a 2-g single dose or 500 mg twice daily for 7 days. Single-dose treatment is ideal in the adolescent population. Tinidazole has fewer gastrointestinal side effects than metronidazole. Sexual partners should also be treated and should abstain from sexual intercourse until 7 days after treatment is completed.
Bacterial vaginosis (BV) is a common vaginal infection in young women. The infection is noninflammatory and caused by an overgrowth of a variety of organisms. The symptoms include a thin, homogeneous, malodorous vaginal discharge. Providers commonly use the Amsel criteria for the diagnosis of bacterial vaginosis. It requires three out of four positive findings: homogeneous thin, gray vaginal discharge; pH more than 4.5; more than 20% clue cells on wet mount; and a positive Whiff test (fishy odor after application of potassium hydroxide). BV is associated with abnormal Papanicolaou (Pap) smears, PID, premature rupture of membranes, preterm labor, and postoperative infections. BV is not an STI; however, sexual transmission occurs as a result of disruption of normal vaginal flora. Other associated factors are smoking, oral receptive sex, and douching.
Treatment is recommended only for symptomatic women or those undergoing gynecologic surgery or abortion. The most effective treatment is metronidazole, 500 mg twice daily for 7 days, or as an intravaginal preparation for 5 days. Single-dose therapy is not recommended. Treatment of the male sexual partner is not necessary. Instruct the adolescent to abstain from sexual intercourse while taking the medication. Recurrence of BV is not uncommon.
Nursing Care Management
The adolescent who comes in for treatment of a vaginal discharge provides an opportunity for health teaching. Teach the young woman how to differentiate normal vaginal discharge from a potential infection. The discussion may elicit questions and concerns the adolescent has regarding other aspects of her developing body and sexuality. The nurse should stress the importance of an evaluation whenever the adolescent notices a change in her normal vaginal discharge.
When an infection is identified, the nurse can explain how the etiologic agents produced the irritation and the principles behind management. The prescription of a vaginal cream requires a careful explanation and demonstration of use. Girls who have never used a tampon will be less familiar with insertion of the vaginal applicator. Instruct the adolescent to apply the cream before bedtime to avoid leakage of the medication while in an upright position. The use of oil-based vaginal creams may break down the latex condom.
Health teaching should include the prevention of future infections. Teach girls at an early age to wipe front to back after toileting. Avoiding tight fitting clothes and nylon panties can assist in prevention. Douching is a common practice among adolescents and should be discouraged because it leads to changes in the normal vaginal microflora. Also, stress the use of condoms for prevention of T. vaginalis and other STIs.
Health Problems Related to Sexuality
The biologic maturation that forms the foundation of adolescent development and the transition to adulthood is accompanied by conflicting feelings, attitudes, and social practices related to developing sexuality. During adolescence the sexual drive emerges, and adolescents begin to explore their ability to attract a partner. The physical urges often precede emotional maturity.
The Youth Risk Behavior Surveillance System from the Centers for Disease Control and Prevention conducts a national school-based survey to monitor key health-risk behaviors among youth. The 2007 survey results found that 47.8% of students had had sexual intercourse, with 7.1% having their first sexual encounter before the age of 13. Not all young people who have ever had sexual intercourse are currently sexually active; in this survey 35% of the students had sexual intercourse with at least one person during the 3 months before the survey. Among those students, 61.5% used a condom during the last sexual intercourse (Centers for Disease Control and Prevention, 2008).
The causes of adolescent sexual risk taking are multifactorial. There is great social pressure to experiment with sex, and enticements by the media to enhance physical attractiveness conflict with traditional religious and societal expectations for chastity. Easy access to cars, unsupervised time at home, and changing family composition also contribute to the incidence of sexual experimentation among the adolescent population. Egocentrism and the concept of the personal fable (feelings of omnipotence, invulnerability, and immortality) lead to risk taking and experimentation. Past research has found that low self-esteem in females was associated with intercourse at an early age; more recent studies have reported similar findings for adolescent males (Spencer, Zimet, Aalsma, et al, 2002; Laflin, Wang, and Barry, 2008).
Family influences can delay the initiation of sexual activity. Adolescents who have at least one warm, supportive parent engage in less risky behavior. Effective parent-child communication about sexual topics can delay the onset of sexual intercourse. In addition, supervision of the adolescent’s social activities and peer group, frequently referred to as parental monitoring, has consistently been shown to postpone sexual involvement. However, parents often underestimate the level of risk for their child and may not provide the appropriate monitoring and communication to assist in postponing sexual involvement (O’Donnell, Stueve, Duran, et al, 2008).
The social environment also has an effect on sexual risk-taking behavior. Adolescents who attend schools where they feel connected and involved in the programming are more likely to postpone sexual involvement. Youth with high academic achievement are more likely to postpone sexual involvement as well (Laflin, Wang, and Barry, 2008). Community support, resources, and supervision will also decrease risk taking among adolescents. Current data suggest that personal and perceived peer norms about sexual intercourse, condom use, and oral sex along with the use of alcohol and other drugs are strong predictors of initiation of sexual intercourse among adolescents (Santelli, Kaiser, Hirsch, et al, 2004; Potard, Courtois, and Rusch, 2008).
Prevention strategies must be comprehensive to decrease high-risk sexual behaviors. Delaying sexual intercourse, using condoms, choosing partners carefully, limiting sexual partners, and using reliable contraception help to reduce the impact of sexual activity on the adolescent. Nurses working with individual adolescents benefit from taking a sexual history so that prevention strategies are appropriate for the level of risk. Questioning adolescents who have not initiated sexual intercourse about their intention to initiate it is helpful, since their intentions are positively associated with actual sexual initiation in boys and girls (Gray, Austin, Huang, et al, 2008). Instruction in the skills needed to resist sexual intercourse has a stronger influence on reducing sexual activity than simply providing information on acquired immunodeficiency syndrome (AIDS) or birth control methods.
Adolescent Pregnancy
In recent years the teenage pregnancy rate has shown a continual downward trend. Between 1990 and 2004, birth rates for teenagers 15 to 19 years of age declined nationally for all races and Hispanic-origin populations. The rates for younger teens have declined more than the rate for older teens (Ventura, Abma, Mosher, et al, 2008). However, adolescent birth rates still remain high in the United States compared with those in other developed countries (American Academy of Pediatrics, 2005).
Contraception use among adolescents is variable, with decisions made within the context of the relationship. The less familiar an adolescent is with his or her partner, the less likely it is that they will use contraception during intercourse. Contraception use increases among girls as the duration of the relationship increases. A hormonal method (OCPs, contraceptive patch, injectable progesterone) is more likely to be used in later relationships than in first sexual relationships. Discontinuation of contraception is common; 46% of women have discontinued at least one method because of dissatisfaction (Moreau, Cleland, and Trussell, 2007).
In most cases, with early prenatal care, teenage pregnancy is no longer considered to be biologically disadvantageous to the child. However, teenage parenting is still regarded as socially, educationally, psychologically, and economically disadvantageous to both mother and child. Poverty is often the result of teenage childbearing (Aquilino and Bragadottir, 2000). African-American and Hispanic adolescents were more likely to become pregnant than their Caucasian counterparts. Eighty-two percent of all teenage pregnancies are unplanned (Alan Guttmacher Institute, 2006). Many of these social risk factors can be improved if a second pregnancy is prevented during the adolescent years or if the second pregnancy does not occur until 26 months postpartum. Other predictors of maternal success include participation in a program for pregnant teens, a social support system, and a sense of control over one’s life (American Academy of Pediatrics, 2001).
Medical Aspects
Adolescents often receive delayed or inadequate prenatal care. Prenatal care may be delayed because the adolescent does not realize she is pregnant or denies the pregnancy until the second or third trimester. Health care providers working with adolescents should have a high index of suspicion for pregnancy. She may or may not have considered the possibility of pregnancy no matter how at risk for pregnancy she is. A pregnant adolescent may give vague reports of irregular periods or missed periods; the bleeding that occurs with implantation may be mistaken for a period, further delaying the diagnosis. Lacking adequate care, adolescent mothers and their unborn infants are at greater risk for low-birth-weight infants and infant deaths. It remains unclear whether this is a result of biologic immaturity or sociodemographic factors.
The obstetric risk and risk to the infant during a second pregnancy for the teenager is much higher. An adolescent with a poor outcome in the first pregnancy has a threefold risk of repeating the poor outcome in the second pregnancy. In teenagers the risk for a preterm delivery recurring is double the rate found in mature women. However, the mean birth weight for second deliveries is higher, related to an increase in the maternal prepregnancy body mass index (BMI).
Diagnosis of Pregnancy
A detailed menstrual and sexual history should be a routine part of health care for adolescents. Review specific symptoms of pregnancy, including amenorrhea, breast tenderness, urinary frequency, fatigue, and nausea. Absence of these symptoms does not exclude pregnancy. It is best not to perform a pregnancy test without the adolescent’s knowledge. Before the pregnancy test, discuss with the adolescent what she will do if the test is positive and determine who else is aware she is sexually active and possibly pregnant.
After confirming that a pregnancy test is positive, inform the adolescent privately. Common reactions are ambivalence, shock, fear, or apparent apathy. The nurse should be supportive at this time and assure her the feelings are normal. Review the facts about the pregnancy, including the duration of pregnancy and anticipated due date. The next step is to determine who she plans to inform and, if she is under 18, how she would like to tell her parents. Some girls may want to take some time before notifying their parent. The nurse should schedule a follow-up appointment in 24 to 48 hours to assist with parental notification. Usually, the adolescent informs her parent on her own terms during this period. The nurse can assist with notification by offering to tell the parent for the teen or to be present when she tells her parent. Nonjudgmental support is critical at this time for the safety of the teen and her pregnancy.
Complications of Pregnancy
Bleeding is common in early pregnancy (occurring in 20% to 25% of cases), and about half of these pregnancies end in spontaneous abortion. Most spontaneous abortions occur in the first trimester as a result of abnormal chromosomal complement, uterine or cervical abnormalities, maternal systemic illness, or infection. Ultrasound evaluation can assist in determining the prognosis for the pregnancy. Bed rest is usually recommended when bleeding occurs; however, there is little evidence to demonstrate its effectiveness in preventing spontaneous abortions (Sotiriadis, Papatheodorou, and Makrydimas, 2004).
When a young woman is seen with bleeding and abdominal pain, an ectopic pregnancy must be ruled out. Ectopic pregnancy occurs when the fertilized egg implants outside of the uterus, usually in the fallopian tube. Damage to the fallopian tube is the most frequent cause of ectopic pregnancy. This damage occurs as a result of tubal surgery, PID, and previous ectopic pregnancy. Smoking is another risk factor for ectopic pregnancy; however, the mechanism is not known (Vichnin, 2008). When ectopic pregnancy is suspected, prompt evaluation and treatment are necessary. If the adolescent is seen with hypotension and abdominal pain, the ectopic pregnancy may have ruptured and emergency surgery is indicated.
Structural Factors: Labor may be prolonged in younger teenagers, particularly those 12 to 16 years of age; this is directly related to fetopelvic incompatibility and is a reflection of the teenager’s smaller stature and incomplete growth process. The incidence of prolonged labor is highest in girls younger than age 14. Girls who are 12 to 13 years old have the highest rate of cesarean births, primarily because of cephalopelvic disproportion. However, older adolescents, 15 to 21 years of age, and especially those who have previously delivered a baby, often have labors that are shorter than average. The transition between pelvic disproportion and pelvic adequacy appears to occur around 15 years of age in the average adolescent.
Nutritional Needs: Caloric requirements during adolescence closely parallel the growth curve, and the need for protein, calcium, and iron is increased. Young adolescents tolerate caloric restriction poorly, and the anabolic need for calories during pregnancy places an added burden on their bodies. The preconception weight is a major determinant of birth weight for infants born to adolescents. Weight gain recommendations for pregnant girls should be based on their weight-for-height percentile or BMI, not on their age. Primiparous adolescents are more likely than first time adult pregnant women to gain more than 18 kg (40 lb). Excessive weight gain during pregnancy is associated with labor and delivery complications, preterm labor, maternal anemia, and infant mortality. Excessive weight gain during pregnancy is also linked with postpartum obesity and the associated health risks (American Academy of Pediatrics, 2009). Recommended weight gain in pregnancy varies according to the woman’s prepregnancy BMI; a higher weight gain is recommended for thin women and a lower weight gain for women who are overweight or obese (American Academy of Pediatrics, 2009).
Because of the marked variation in the dietary needs of individual teenagers, there are no hard-and-fast rules to describe an adequate diet for all pregnant girls. The diet must provide sufficient nutrients to meet growth needs of both the prospective mother and the unborn child without the threat of excessive weight gain or fetal malnutrition. An additional 340 kcal/day (second trimester) to 452/day kcal (third trimester) are recommended for nutritional intake (American Academy of Pediatrics, 2009). The best guides for determining nutritional needs for the adolescent and pregnant adolescent are the Recommended Dietary Allowances and the Dietary Guidelines for Americans; the dietary reference intakes (DRIs) from the Institute of Medicine include recommended intakes of vitamins, minerals, and macronutrients for women of all ages and for those who are pregnant.* (See also Nutritional Assessment, Chapter 6.) Pregnant teenagers exhibit food preferences, eating behaviors, and lifestyle habits that are similar to those of their nonpregnant peers. Frequent snacking on foods high in fat and sugar and low in essential nutrients results in less than the recommended intake of calcium; iron; zinc; folic acid; and vitamins B6, A, and C—nutrients of special concern during pregnancy.
Social and Economic Aspects
Poor school performance usually precedes adolescent pregnancy. Unable to achieve academically, the girl views motherhood as a rite of passage into adult status. Adolescents with high educational expectations are less likely than others to become pregnant. Another significant aspect of school dropout and accelerated maturity is the girl’s alienation and isolation from her peers during a stage of development when identity formation is closely allied with peer identification. She is deprived of the interrelationship with the adolescent social system that is so essential to the development of a sense of identity. The girl may believe that she no longer “belongs” to the peer group and does not qualify for membership in the older peer group of mothers. On the other hand, the pregnancy may give the adolescent an entrance into a peer group. One study found that absenteeism and dropout rates were lower when adolescents received prenatal care in a school-based health center in an alternative school. Programs such as this can help reduce the long-term negative outcomes of adolescent parenting (Barnet, Arroyo, Devoe, et al, 2004).
Mother-Infant Relationship
Adolescents often have unrealistic expectations for the child. The young mother may view the infant as a plaything or a love object for herself. Children of adolescent mothers experience more developmental problems than children of adult mothers. The amount of cognitive stimulation in the child’s early home environment is associated with the child’s level of cognitive attainment. Many children of adolescents are raised by a grandparent. Although living with a grandparent may have positive effects on child outcomes, coresidence with the grandmother may have negative effects if the mother and grandmother are in conflict. Nurses need to stress the importance of the adolescent caring for the child even when other adults (e.g., mother or grandmother) are involved. The other adults present need education and support to allow optimum development of the infant and adolescent mother.
Several factors influence the mother-infant relationship. Maternal stresses, including changes in circumstances, influence coping ability and sensitivity to the infant’s needs. Teenage mothers may consider an argument with a parent, boyfriend, or husband stressful, whereas adult mothers focus on problems directly involving the infant. Vocational and educational disadvantages of both teenage mothers and fathers further affect their coping abilities. It is important to recognize that not all adolescent mothers are alike. Some teenagers adjust well to the stresses and responsibilities of parenting, whereas others may lack the maturity or confidence to nurture optimally.
When socioeconomic status is controlled for, it has been found that younger adolescent mothers have lower acceptance of their children compared with older adolescent mothers. Studies in the literature indicate that specific family variables, including the mother’s age (<19 years), are risk indicators for child abuse and neglect (Lounds, Borkowski, and Whitman, 2006; Murray, Baker, and Lewin, 2000).
A positive correlation exists between the total amount of social support and the frequency of appropriate maternal behavior. An assessment of whom the adolescent thinks she receives the most support from (her family, her partner, his family, or a close friend) allows the nurse to help the young mother benefit from this support (see Family-Centered Care box).
The cognitive development of the adolescent influences the development of attitudes and realistic expectations regarding childbearing. To cope effectively and solve situational dilemmas, pregnant teenagers must be able to use the problem-solving approach to assess and evaluate consequences. The concrete thought and egocentrism of early adolescence can influence the mother’s ability to evaluate the infant’s needs. Adolescent mothers lack knowledge of normal infant growth and development. This deficit may directly affect their perception, interpretation, and responsiveness to infant cues.
Infant characteristics also influence parental behavior. Teenage parents view their children as more temperamentally difficult than do adult parents. Temperamentally difficult infants have an adverse effect on the parents’ sensitivity and responsiveness. Parent-infant interaction that is not mutually satisfying can also alter the parents’ feelings of effectiveness and self-worth.
Adolescent Fathers
Little information is available about adolescent fathers. Most studies have small sample sizes and rely on reporting from the mother rather than the young man himself. Most teen fathers are involved with and interested in their children (Savio Beers, and Hollo, 2009). This involvement has positive effects on the mother’s self-esteem and decreases her level of distress and depression. The teen mother and her mother largely influence the level of participation a teen father has with his children. Social supports and parenting classes are often lacking for adolescent fathers. The nurse should take advantage of opportunities to involve young fathers in educational programs.
Nursing Care Management
It is evident from the preceding discussion that nurses play a central role in meeting the needs of pregnant teenagers. The nurse may be the one to whom the young girl turns for help and guidance in her dilemma and on whom she relies for support and reassurance.
The first goal in nursing care of the pregnant teenager is to help her obtain health care whether she elects to continue or terminate the pregnancy. Typically, adolescents are reluctant to seek medical help, in part because of anxiety but more often because of a tendency to deny the pregnancy. Early prenatal care is essential for the welfare of both mother and infant. For guidelines, teaching, and general support measures during pregnancy, the reader is directed to the excellent textbooks available on nursing care throughout the maternity cycle.
Basic to the implementation of any care program is communication and the establishment of a trusting relationship. Initially the adolescent may appear apathetic and display little interest in discussing her pregnancy. The nurse must make every effort to put the adolescent at ease and avoid undue pressure. The young girl may have encountered rejection and open criticism from authority figures and peers. Conveying a nonjudgmental and genuine caring acceptance of the adolescent and her goals will assist the nurse in gaining the adolescent’s confidence and trust.
Communication takes time and patience. Asking open-ended questions and listening for cues will help identify physical, emotional, social, and cultural influences that might affect the adolescent’s progress through the maternity cycle. Factors that might affect her physical status, such as smoking, drug use, and nutritional state and habits, need to be explored and confronted. Each teenager represents a unique situation in terms of background, lifestyle, support structure, and coping mechanisms. Listening to the teenager and understanding the situation from her perspective are essential for a trusting relationship and effective communication.
Nutrition assessment should focus on the dietary adequacy of iron and calcium; multivitamins with folic acid are prescribed. Refer the adolescent for food supplement programs and other financial assistance, such as Women, Infants, and Children; Medicaid; Temporary Assistance for Needy Families (formerly Aid to Families with Dependent Children); and housing. Social work referral for thorough psychosocial assessment and planning may be initiated. Programs that have been most successful are comprehensive and use an interdisciplinary team concept.
The adolescent needs to know what is happening to her, what is expected of her, and how she can help in developing a care plan. Adolescents have their own ideas about the type of help and support they need. Nurses should consult with them and provide them an opportunity to share their ideas. It is important to jointly choose goals that the adolescent believes are beneficial, attainable, and able to be maintained over time. When developing a plan with a teen parent, the nurse should include the family, school, and community; involve the young father early in the relationship; and respect and understand the grandmothers’ role.
The adolescent needs help to improve her altered self-image, a crucial factor in adolescence. Giving her as much individual attention as possible; being a sympathetic listener; providing the opportunity for her to know, support, and be supported by other girls in the same situation; and helping her experience success will facilitate progress toward achieving this goal.
The nurse should involve the family whenever possible. The parents of the adolescent mother and the father of the child need to express feelings and attitudes about the situation. The nurse should not make assumptions about whether the girl wishes to have these persons involved in her decisions and care.
Direct postpartum care of adolescents to prevent subsequent pregnancies and enhance life outcomes for the teen parents and child. Health care programs that provide contraceptive services for the young mother at the time of her child’s appointment are helpful. Merely dispensing contraception is not enough. Comprehensive programs to promote positive parenting, self-esteem, vocational or academic assessment, career goals, and family cohesiveness are necessary.
Adolescent Abortion
In 1973 the landmark U.S. Supreme Court case Roe v. Wade concluded that individuals had the right to a first-trimester abortion. This right was not absolute but subject to certain state restrictions. Abortion is one of the most controversial moral issues in the United States. For example, many Americans believe that a pregnant woman should be able to obtain an abortion if her own life is endangered, if there is a strong chance that the fetus has a serious defect, or if the pregnancy is a result of a rape. However, some Americans do not believe that a woman should be able to have an abortion for any reason. The right to an abortion is also legally determined by the stage of pregnancy.
Many pregnant adolescents choose to continue their pregnancies and parent the child. The abortion rate has fallen more quickly than the drop in the pregnancy rate for adolescents. There are many possible explanations for this trend, including the possibility that access to abortion services for teens has decreased, that those who truly do not want to parent are abstaining from intercourse or using more effective methods of contraception, and that there is more social support for parenting among adolescents (Henshaw and Feivelson, 2000).
Under current federal constitutional law, minors have the right to obtain first-trimester abortions without parental consent unless otherwise specified by state law. (See the concept of “mature minor” and informed consent in Chapter 27. See also the Alan Guttmacher Institute website [www.guttmacher.org] for an update on state policies regarding adolescent abortion and state notification.) Legislation that mandates parental involvement as a requirement for adolescents who seek an abortion has generated considerable controversy. U.S. Supreme Court rulings have held that it is not unconstitutional for states to impose parental notification requirements as long as pregnant adolescents who believe that this involvement would not be in their best interests are allowed to go to court without involving their parents and are legally permitted to make their own decisions. The American Academy of Pediatrics (1996) and several other health care organizations have reached a consensus that minors should not be compelled or required to involve their parents in this decision but should be encouraged to discuss their pregnancies with their parents and other responsible adults.
Abortion is a controversial and emotional issue and one that frequently confronts health care professionals involved in delivery of services to pregnant adolescents. Because the law in this area is unsettled and varies by state, nurses must stay informed of legal changes as they relate to reproductive rights of minors in the state in which they practice (Tillett, 2005).
Other barriers to receiving an abortion include distance to the clinic, cost, and antiabortion harassment. Abortion services in the United States are offered primarily at freestanding abortion clinics, usually in major population centers. Abortions are not covered by many insurers, and the cost may be prohibitive to many women, especially adolescents.
The medical safety of a legal abortion has been well established. The mortality rate associated with teenage full-term pregnancy is much higher than the rate with abortion. A discussion of surgical procedures available is beyond the scope of this text. First-trimester abortions are performed as outpatient procedures and require local anesthesia or mild sedation only. Complication rates have been reported to be 1% or less. Problems that arise after abortion are endometritis, hemorrhage, Rh sensitization, genital tract injury, retained fetal elements, and (in rare cases) pulmonary embolism or death. Second-trimester abortions are more complicated and are associated with greater risk from hemorrhage. Women who have an induced abortion are no more likely than other women to experience problems in bearing a healthy baby in subsequent pregnancies.
In 2000 the FDA approved mifepristone for medical abortion. This oral medication provides women the option of a nonsurgical abortion procedure at 49 days or less of pregnancy. The drug prevents receptor binding of endogenous or exogenous progesterone, which causes an abortion. The cervix is softened and the myometrium is sensitized to the contraction-inducing activity of prostaglandins. The medication can be used from the time of detection of pregnancy up to 49 days since the last menstrual period (Meier, 2000). The abortion completion rate is 92% to 95% in pregnancies less than 49 days (Grimes, 2000).
Numerous studies have examined the mental health risks associated with obtaining an abortion. There is no empirical evidence that women of any age who choose to have a legal first-trimester abortion experience psychologic problems or regret. Most of the studies have examined the effects up to 2 years after the abortion (Major, Cozzarelli, Cooper, et al, 2000).
Nursing Care Management
Early identification of pregnancy is essential, and nurses are in an optimum position to provide counseling on pregnancy options. Whatever option the adolescent chooses, initiate referral as quickly as possible to eliminate risk. Pelvic ultrasound may be indicated to assess gestational age correctly for those adolescents who cannot recall the date of their last menstrual period and when a bimanual examination is inconclusive.
Patient education regarding the medical aspects of the abortion should be conducted verbally, and the patient should be provided with written instructions before the procedure. Reviewing relaxation strategies that can be used during the procedure is helpful. Encourage the parents or other significant adults to be present during the medical procedure.
Conduct discussions about future contraceptive needs before the abortion. The adolescent may be started on a hormonal method of contraception immediately after the abortion. The young woman should be seen 3 weeks after an abortion to receive medical, contraceptive, and psychologic follow-up care.
Contraception
Family planning services have developed and expanded during recent years. Contraceptive use among adolescents continues to increase. Contraceptive options have expanded over the past decade as well. Although all teenagers need sexuality education, not all of them are candidates for contraception. Among the large adolescent population, some have made the decision to postpone sexual involvement, some are in exclusively same-sex relationships, and some also may wish to have a child.
Confidentiality is a critical issue when discussing contraception with adolescents. Privacy is important to adolescents as they struggle to forge a personal identity and establish social relationships. Adolescents are particularly concerned about the judgments of others. The American Medical Association, Society for Adolescent Medicine, American Academy of Pediatrics, and American College of Obstetricians and Gynecologists have written policy statements in support of a minor’s right to confidential health care. All agree that, although parental involvement is desirable, confidentiality may be central to encouraging teens to access needed health advice and treatment. Health delivery systems must be structured to allow confidentiality, including methods for appointment scheduling, billing, record keeping, and follow-up, that ensures privacy rights for adolescents. Family-centered care and parental involvement in contraceptive choice are ideal for patient compliance. However, there are adolescents who need confidential care. The predominant belief among many health professionals is that parental notification is important but that the “parents’ rights” view is not necessarily sensitive to the health needs and basic rights of youth. No evidence substantiates the belief that providing contraceptive guidance contributes to sexual irresponsibility and promiscuity. In fact, a request for contraceptive information indicates a responsible effort on the part of the teenager to avoid an unplanned pregnancy.
Contraceptive Methods
To be safe and effective, a contraceptive method must be suited to the individual. The choice is based on the adolescent’s preference after being informed of all the benefits and disadvantages of the methods available. The adolescent must be motivated to use whatever method is chosen. Factors associated with successful use of contraception include education, expectations, availability, cost, parent education level, perception of high likelihood of pregnancy, perception of disadvantages of having a pregnancy, and low rate of disadvantages of birth control methods.
Providing a birth control device is only part of a comprehensive sex education program. Partner involvement, when possible, is important to enhance user compliance. To make truly informed choices about contraception, adolescents need to know not only the efficacy of methods as they are actually used but also their efficacy when used consistently. Contraceptive efficacy is a representation of the number of unintended pregnancies that occur per year while using a particular method. Sexual intercourse with no protection is estimated to result in 85% of the women becoming pregnant. Table 20-1 outlines the advantages and disadvantages of various contraceptive methods recommended for use in adolescents.
TABLE 20-1
ADVANTAGES AND DISADVANTAGES OF CONTRACEPTIVE METHODS IN ADOLESCENTS
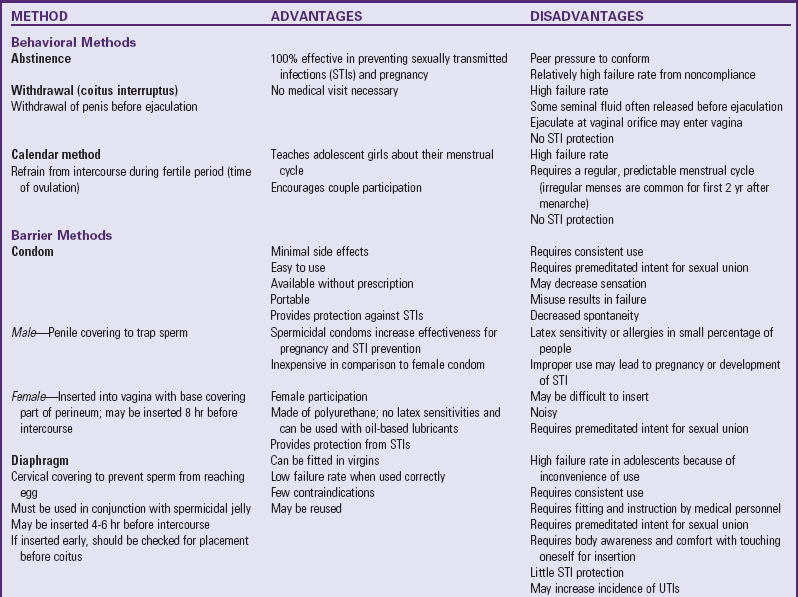

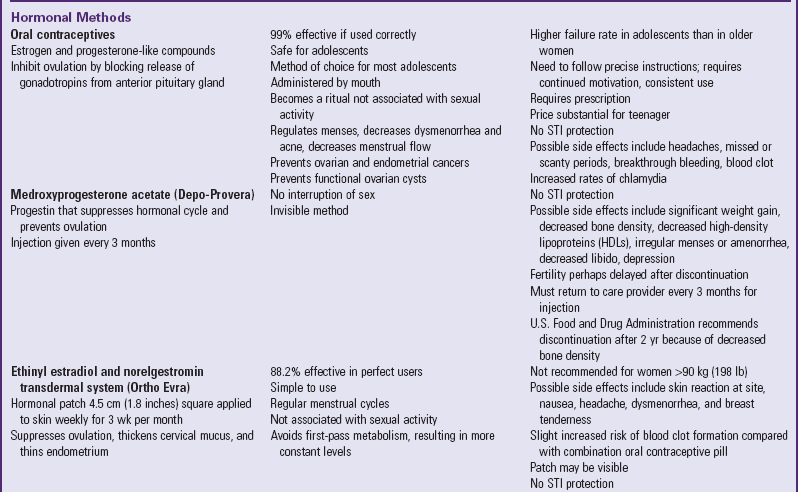
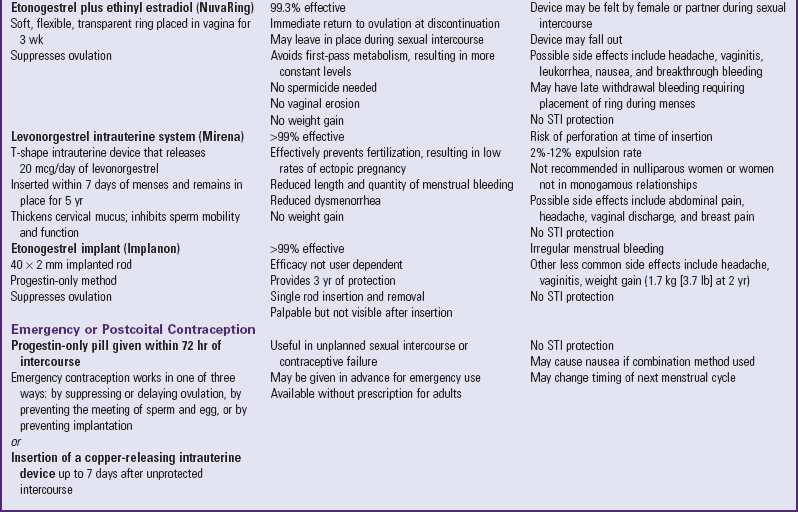
HIV, Human immunodeficiency virus; UTIs, urinary tract infections.
Nonprescription Methods: Sometimes, despite the effectiveness of prescription methods, teenagers use less effective methods to avoid side effects and the necessity for medical screening and supervision inherent in the use of prescription methods. Adolescents may report the use of withdrawal and reliance on “safe” periods in the menstrual cycle as their current method of contraception. Using the method of periodic abstinence, or the rhythm method, is very risky. When the couple breaks the rules in this method, they are having unprotected sexual intercourse at times during the menstrual cycle when pregnancy is most likely to occur. Providing factual information about condoms and clarifying myths and misinformation about pregnancy prevention helps reduce the incidence of unwanted pregnancy.
Because of the high incidence of STIs in the adolescent population, discuss condom use with all adolescents seeking contraceptive advice. The adolescent can then be assisted in choosing an additional method to prevent pregnancy.
The lack of female-controlled barrier methods known to protect against infection with STIs has led to the development of the female condom. The contraceptive efficacy of the female condom during typical use is similar to that of the diaphragm or cervical cap. The female condom is nearly as effective in preventing pregnancy as the male condom without spermicidal lubricant. The female condom appears to have great potential for giving a woman control in reducing her risk of HIV infection; however, there is no scientific evidence to prove this because efficacy studies of HIV transmission are unethical. Currently only one female condom is approved by the FDA for use in the United States. The female condom has been poorly used because of expense, problems with insertion, and slippage during sexual intercourse. A new female condom has been developed and is in the final stages of testing before potential acceptance by the FDA. Research has found that the PATH (Program for Appropriate Technology in Health) Woman’s condom is preferred over the current female condom in a comparative crossover study with both methods (Schwartz, Barnhart, Creinin, et al, 2008).
The spermicide nonoxynol-9 does not protect against STIs, including HIV, and may actually increase the risk of HIV transmission because of the irritation it causes to the vagina and rectum. The Centers for Disease Control and Prevention (2006a) recommends not using spermicides and condoms with nonoxynol-9.
Prescription Methods: The recommendation of a prescription method of contraception requires a careful medical history and assurance that the adolescent understands the method. A discussion of the pros and cons of each method helps dispel myths and helps the adolescent find the right method for her current situation. The clinician should provide accurate, unbiased information about the benefits and risks, effectiveness, and return to fertility for each contraceptive method.
Use of Contraception
The birth control pill and condoms remain the most popular methods for adolescents. Adolescents commonly delay seeking contraceptive information. The typical interval from onset of sexual intercourse until the first visit for contraception is 1 year. A pregnancy scare is usually the precipitating event for the contraception appointment. Fear of the pelvic examination is a common reason that girls postpone seeking contraception. The World Health Organization, American College of Obstetricians and Gynecologists, and Planned Parenthood Federation of America have all recommended unbundling these services. Box 20-2 lists additional reasons adolescents give for not making better use of contraception.
Emergency contraception (ECP) is the administration of an effective contraceptive method after sexual intercourse. It is appropriate to use after any unprotected sexual intercourse, after condom breakage, when it is too late for injectable contraception, after missed pills, or after rape. The FDA has approved a progestin-only method for ECP (levonorgestrel [Plan B]) with high effectiveness and low rates of side effects. ECP must be given within 3 days (72 hours) of unprotected sexual intercourse, with highest efficacy closest to the time of sexual intercourse. There are no contraindications to use of the progestin-only method. Plan B is available to adult women over the counter without a prescription.
Compliance in contraceptive use is related to many factors, including those discussed in the following sections.
Lack of Information: Sometimes health professionals have a tendency to confuse a teenager’s sophistication with knowledge. Although adolescents are acutely aware of their sexuality, their understanding of reproductive anatomy and physiology is often incomplete. If they are using contraception, they often do so with little or no instruction and with only vague understanding. Misinformation is commonplace. Lacking a fundamental understanding of fertility, they often believe they are too young or have sex too infrequently to become pregnant.
Anxiety Regarding Contraception: Some adolescents are concerned that their parents will be notified. Many have exaggerated ideas about the hazards of prescription methods, which correlate with misguided fears in the adult population. Myths about undesirable side effects prevail even after educational courses about contraception.
Conflict About Sexual Activity: Many teenagers feel ambivalent regarding their sexual activity and avoid many contraceptives because their use seems too premeditated and implies that sex is planned rather than a spontaneous activity. Most of these girls believe that sex is all right if it is not planned. This may also play a role in those adolescents who delay contraception, waiting for a relationship that is “close enough.” A close relationship would allow the adolescents to accept and acknowledge their sexual activity.
Desire for Pregnancy: Some teens are seeking pregnancy and fail to use an effective method of contraception or use a prescribed method improperly. Some adolescents seek pregnancy as a rite of passage into adulthood or as a misdirected attempt to have someone to love them. Careful counseling and assistance with decision-making skills are essential when counseling the adolescent desiring pregnancy.
Nursing Care Management
Much of contraceptive education and service are delivered by nurses as part of sex education programs, family planning services, or postpartum health services. The introduction of contraceptive methods should ideally be associated with ongoing sex education. When they are included in this education process, sexually active adolescents will consider contraceptives as a natural and logical part of intercourse. Education about sexuality, conception, and contraception should be accurate, straightforward, and nonjudgmental.
Although sexual abstinence is highly desirable as a form of contraception, it is difficult for many adolescents to “just say no.” Postponing sexual involvement requires effective communication and decision-making skills. Adolescents benefit from role-playing refusal skills in a safe environment. The nurse should also discuss with the adolescent how to introduce condoms into an existing or new relationship. Young women who have asked a partner to use a condom are more likely to use a condom consistently than women who have never made the request. The nurse plays an important role in offering appropriate education, helping build confidence in adolescents’ ability to make requests of their partners, and providing social support to the sexually active adolescent.
To make an informed decision, the adolescent needs a careful review of all methods available, including their advantages and disadvantages. Discontinuation rates of prescription methods are high among all women, particularly adolescents. A critical aspect of counseling about a contraceptive method is education about use, noncontraceptive benefits, and expected side effects. Clear verbal explanations and demonstrations with the actual methods assist the concrete thinker in understanding the complicated instructions. Whenever possible, the parent or partner should be included in the teaching. Provide written instructions and a phone number for questions. When adolescents choose hormonal methods, they should also use condoms for the prevention of STIs (see Community Focus box). The nurse should demonstrate the correct use of condoms to all sexually active adolescents. Frequent follow-up with a review of side effects, usage patterns, and an opportunity to voice concerns increases the likelihood that the adolescent will continue to use contraception effectively.
An organization that provides education and services for adolescents, including both individual and group counseling, is the Planned Parenthood Federation of America.* It has branches in most cities in the United States.
Rape
Adolescents and young adults have the highest rates of rape and other sexual assaults of any age-group. The majority of sexual assaults in the adolescent age-group are perpetrated by an acquaintance or relative of the teen (Kaufman and American Academy of Pediatrics, 2008). Females are more likely to report these experiences than males. In each instance the victim is potentially subjected to serious physical or emotional harm. There is no typical victim. Sexual assault victims are of all ages, ethnic groups, and economic groups and are of either gender, although adolescents and children with a physical or developmental disability are more vulnerable to sexual abuse than their peers.
Legal definitions of rape vary from state to state but include the following categories: completed rape, attempted rape, and statutory rape. Many current definitions of rape have been expanded to include all forms of sexual victimization, including anal, oral, and genital penetration. Sexual assault is not restricted to vaginal or anal penetration but includes every form of sexual activity, including voyeurism.
Statutory rape may be charged when the victim is unable to give consent legally by virtue of age (age varies from state to state but is usually <16 years); mental deficiency; psychosis; or an altered state of consciousness caused by sleep, drugs, or illness.
Assailants
Three relationships are identified for assault: stranger, nonstranger, and incest. Although all can have serious and long-lasting effects, they are presumed to be different in a number of important ways: in the nature of the dominant psychologic and cognitive behaviors they provoke, in the issues they raise for service providers and other potential helpers, and in the techniques that may be helpful for treating existing and new cases.
Nonstranger Rapist: The majority of rapes are committed by a nonstranger. This is often referred to as acquaintance rape. The acquaintance may be a date, someone who lives near the adolescent, someone who has contact with the victim through recreational activities, or someone in an official association with the teenager. Some assailants wait for an opportunity when the victim is defenseless, such as the teenager at home alone with an uncle or cousin or the baby-sitter being driven home.
The assailant may be another teenager known through social activity. The nature of sex-role learning in most cultures associates females with softness, nonassertiveness, and dependence on men. Young women are socialized to be alluring yet sexually unavailable and to assume the role of pacesetter in sexual situations. Males are conditioned to be strong, powerful, and aggressive (measures of masculinity) and to be aggressors in sexual situations.
Stranger Rapist: It is believed that stranger rapes probably account for nearly 50% of all rapes reported to the police. Victims are frequently selected at random because they are apparently helpless.
Incest: The most commonly reported incestuous relationships are between a daughter and a father or stepfather (or other man in a caretaking role). The victim’s participation is gained through the application of authority, subtle pressure, persuasion, or misrepresentation of moral standards. (For a further discussion of sexual abuse, see Child Maltreatment, Chapter 16.)
Clinical Manifestations
Adolescents who have been raped arrive at the emergency department or practitioner’s office under a variety of circumstances. They are usually brought in by parents, friends, or the police, but some girls may seek medical help on their own. They may display a variety of manifestations, such as hysterical crying or giggling; agitation; feelings of degradation, rage, or helplessness; nervousness; and rapid mood swings. Adolescents may alternately appear calm and controlled, masking inner turmoil; they may be angry, confused, and filled with self-blame.
The rape victim may manifest evidence of physical force, including roughness, nonbrutal beating (slapping), brutal beating (slugging, kicking), and choking or gagging. The predominant reaction of the victim is fear of the rape and of injury. Thus the victim is faced with the dilemma of submission or resistance. Resistance increases the victim’s chance of escape but also increases the likelihood of violence against the victim.
Therapeutic Management
It is advisable to obtain parental consent for examination, but the examination may be performed without consent if the adolescent is legally mature or the parents are unavailable. A female observer should be present during the history taking and examination of female victims who are examined by a male practitioner. Whether a parent should be present during the examination is determined on an individual basis. The parent’s presence is usually encouraged, but only if the parent is supportive. Often the presence of a parent or a police officer inhibits the person’s ability to describe the incident.
The medical assessment of the sexual assault victim includes the assessment and treatment of physical injury with focus on the genitalia. Pregnancy assessment and prevention, as well as evaluation and treatment for STIs, are performed. Obtaining forensic evidence requires training and should be conducted as soon after the incident as possible. Psychologic assessment and ongoing support are essential.
Initial Contact: The interrogation and associated activities, including the initial medical evaluation, have the potential to add to the trauma of the sexual assault. The initial contact with the rape victim must be supportive, and the fundamental goal is to do no further harm. Establishing a trusting relationship is an important step to decrease the victim’s anxiety. The victim needs to know that she is (1) all right and (2) not being blamed for the situation. The first approach is not one of repeated interrogation but an attempt to reduce the victim’s stress.
History: Although it is important to obtain a clear account of the circumstances of an alleged rape, it is also essential to minimize any further psychologic trauma that might occur if the adolescent is forced to relive a painful experience. The adolescent has probably been questioned by family and the police. If the person is too upset, the detailed history may be delayed. The adolescent should not be further victimized by insensitive care and unnecessary trauma.
The history should be as complete as possible and must be taken and presented in the patient’s own words, including any account of force or threats. Information includes the date, time, location, and an accurate description of all types of sexual contact. All related activities are included. For example, evidence can be altered if the victim has bathed, urinated, defecated, douched, or changed clothing; therefore these activities are recorded. Use of a condom by the assailant can alter evidence. For adequate care, other important data include the date of the last menstrual period, the date of last intercourse, use of contraception, and any possibility of a preexisting pregnancy or STI. Also record the victim’s behavior and emotional state.
Examination: The physical examination and collection of evidence are carried out as soon as possible because physical evidence deteriorates rapidly. Practitioners specially trained for rape examination should be used when possible. Nurses are often members of this group and are known as sexual assault nurse examiners (SANEs) (Stermac, Dunlap, and Bainbridge, 2005). The adolescent is always told in advance in understandable terms exactly what to expect in the way of tests and procedures, and the explanation is accompanied by emotional support. The victim is examined thoroughly, including nongenital areas, for evidence of injury that might substantiate the use of force. Photographs are taken of bruises, lacerations, or scratches for evidence, and rips or tears in clothing and the presence of dirt or grass stains are noted and recorded. Perineal, vaginal, or rectal lacerations suggest rape.
It is not uncommon for adolescent rape victims to delay seeking help, especially in cases of acquaintance or date rape. Nurses can be most supportive by acknowledging the painful and sometimes confusing feelings that surround such experiences and by focusing on the fact that the victim is seeking assistance now.
Treatment: Assessment of injury and management of pain are the first steps. Any injuries sustained by the victim that require surgical treatment are repaired. Most care providers prescribe prophylactic antibiotics at the initial examination. Pregnancy prophylaxis with ECPs is offered to the victim who was not previously pregnant or using a contraceptive method.
Nursing Care Management
Many of the approaches described for the sexually abused child apply to the adolescent. (See Chapter 16.) Sexual assault is a devastating experience with long-lasting effects. The primary goal of nursing care is to not inflict further stress on the victim, who is often angry, confused, frightened, embarrassed, and filled with self-blame. Young rape victims fear pregnancy, bodily injury, and the reactions of their parents and peers. Some believe that their bodies are permanently damaged and may even fear death as a consequence of the experience.
The nurse must do everything possible to reduce the stress of the interrogation and examination. Application of stress reduction techniques during the process can help the adolescent manage the immediate experience. Although most health professionals and law enforcement officers are sensitive to the needs of the victim and attempt to make the process as nonstressful as possible, the nurse acts as the advocate for the adolescent and is alert for cues that the victim is being overstressed.
Follow-up care of the rape victim extends over a long time. Rape victims typically show high levels of distress within the first week, which peak in severity by 3 weeks after the assault, continue at high levels for the next month, and then begin to decrease by 2 to 3 months after the assault. Make a referral to a public health agency or mental health agency as soon as possible. Victims who live in areas with established rape crisis centers are referred to these facilities.*
Aside from the universal need for emotional support, no firm guidelines exist for meeting the needs of rape victims. Trauma-focused cognitive behavioral therapy has been shown to be helpful for adolescents who have been abused or assaulted (Kaufman and American Academy of Pediatrics, 2008). In general, their needs vary widely and depend on the nature of the incident, when it took place, the physical and emotional injuries sustained, actions being considered as a result, resources available for informal support, and anticipated reactions of persons in the informal support network (see Family-Centered Care box). Posttraumatic stress disorder occurs in many victims of rape. (See Chapter 18.) Acquaintance rape is as devastating to the victim as stranger rape. There are few reliable predictors of positive readjustment among rape survivors. In general, a young age at the time of assault is associated with increased distress. Women victimized in childhood are more likely than nonvictims to be assaulted as adults.
Prevention: With the increasing incidence of rape in some communities in the United States, many professionals are looking for additional means for preventing rape at all ages. Many schools and organizations arrange for classes on how to avoid an attack and how to behave in the event of an attempted rape. Rape trauma centers and most law enforcement agencies provide this service to groups. Every effort should be made to protect children and adolescents from injury and to teach them how to avoid situations that may promote an attack and how to behave in a threatening situation.
Nurses can be advocates for improving the community environment and street lighting, providing safe housing and transportation, and improving the effectiveness of the criminal justice system. They can work to educate adolescents about the relationship of risk-taking behaviors and sexual attack. These behaviors include drinking, taking drugs, and hitchhiking.
Nurses can also play a role in identifying intimate partner violence. Only a small percentage of victims initiate a discussion about partner violence with their health care provider. One step toward increasing safety is to begin to ask adolescents about safety in their current relationship. Offer adolescents antiviolence information as routinely as other messages about pregnancy prevention, driving safety, and prevention of STIs.
Display information about dating violence in the waiting room, examining room, and bathroom. Awareness of local resources for adolescents who experience violence allows the nurse to assist in referring those teens in need of help. At a broader level, nurses can also provide community education about intimate partner violence, including antiviolence presentations that target young men.
Sexually Transmitted Infections
STIs represent one of the major causes of morbidity during adolescence and young adulthood and annually afflict approximately 10 million persons under the age of 25 years. Teenagers represent one of the groups at highest risk. The actual prevalence rates among adolescents is underestimated, since the most prevalent STIs in adolescents, chlamydial infection and HPV infection, are not required to be reported to the Centers for Disease Control and Prevention.
Several unique characteristics—biologic, developmental, and environmental—place adolescents at risk for acquisition of STIs. Biologically, the immature adolescent female cervix is composed of columnar epithelium on the exocervix (cervical ectopia). The thin layer of columnar cells appears to favor attachment of infectious agents (especially C. trachomatis and HPV), which accounts in part for the increased prevalence of these infections in adolescents. The unchallenged immune system does not provide localized antibody response at the cervical level when exposed repeatedly to infectious agents. During anovulatory cycles, estrogen predominates, as demonstrated by the clear and watery cervical discharge. This may facilitate the transport of pathogens to the upper genital tract.
Developmentally, teenagers experience biologic discontinuities when pubertal maturation precedes psychologic and cognitive maturity. As the average age of menarche has declined, the age of sexual debut has also declined. An earlier age at sexual initiation results in increased numbers of sexual partners. The absence of planning is often evident in the failure to see the implications of current behavior on future outcome, such as condom use to prevent an STI or pregnancy or the need to return for follow-up visits for contraceptive refill or STI treatment.
Adolescents lack the knowledge that many STIs can be asymptomatic, or they fail to recognize the symptoms when they occur. Adolescents also fail to recognize that oral or rectal sex may be a source of STIs. A substantial number of adolescents engage in sexual intercourse other than penile-vaginal intercourse.
Adolescents perceive themselves as at low risk for acquiring STIs, even when infected with the disease. Young people who do not perceive a risk are not likely to use condoms to protect themselves or seek testing for diseases (Ford, Jaccard, Millstein, et al, 2004). Studies have shown that as young women have more sexual partners, their use of hormonal contraception increases; at the same time, the use of condoms declines. Adolescents diagnosed with an STI have a 40% risk of acquiring another STI in the same year (Orr, Johnston, Brizendine, et al, 2001; Peterman, Tian, Metcalf, et al, 2006). Without behavioral changes, these adolescents are at significant risk for additional STIs.
Designing health care systems and providing in-service education for all health care personnel are essential to providing services that meet the needs of adolescents. Environmental barriers to health care use by teenagers include high cost, lack of insurance, inconvenient timing of appointments, and inconvenient location of health facilities. Services need to be easily accessible and sensitive to the adolescent’s developmental needs and desire for confidentiality.
Gonorrhea
Epidemiology: Several demographic factors place teenagers at risk for acquiring gonorrhea. Adolescents 15 to 19 years of age have the highest overall incidence of gonococcal infection compared with any other age-group when rates are adjusted for sexual activity. Gonorrhea among non-Caucasians is 10 times more frequent than among Caucasians. Part of this discrepancy is due to the fact that non-Caucasians are more likely to attend public health clinics, where reporting of the disease is better than in the private sector. Other known risk factors are low socioeconomic status, urban residence, early onset of sexual activity, single marital status, previous history of gonorrhea, and multiple sexual partners.
Epidemiologic evidence suggests the existence of a core group, or cluster of individuals, who are never treated or are inadequately treated and thus serve as a reservoir for reinfection. This emphasizes the need for partner identification and appropriate treatment to interrupt this cycle of reinfection. Prior infection is an important marker and should alert the clinician that the individual is at risk for reinfection.
Gonorrhea is almost always sexually transmitted, except when it appears in the conjunctiva, in which case vertical transmission from the maternal cervix to the newborn’s conjunctiva is the usual mode of infection. The incidence of gonococcal ophthalmia has decreased in developed countries as a result of the routine application of prophylactic antibiotics to the eyes of newborn infants. (See Chapter 8.) Gonococcal infections do not confer lifelong immunity; therefore individuals are subject to reinfection.
Pathophysiology: The causative organism is Neisseria gonorrhoeae, a gram-negative diplococcus. The organisms have specific survival requirements, preferring a moist, alkaline environment (pH 7.2 to 7.6) and a temperature of 35° to 36° C (95° to 96.8° F). The gonococci survive only on the columnar and transitional epithelium; stratified epithelium is resistant to the onslaught. The organism spreads along the mucosa from the point of entry. It penetrates between the epithelial cells and, when dead, liberates an irritant that produces the inflammatory response, characterized by localized capillary dilation, edema, and leukocytosis. This process accounts for the purulent discharge and erosive balanitis and cervicitis sometimes observed in affected persons.
Clinical Manifestations: Symptoms can appear as early as 1 day or as late as 2 weeks after sexual contact. Gonococcal infection can manifest in many diverse ways, with four basic presentations: asymptomatic, uncomplicated symptomatic, complicated symptomatic, and disseminated disease. The infection can involve a number of organs and a wide range of manifestations (Table 20-2). PID in females simulates the inflammatory process caused by other bacterial infections, and differential diagnosis is made for more definitive medical treatment. Because a large percentage of affected persons are asymptomatic, consider gonorrhea in the evaluation of all sexually active adolescents. Lack of clinical symptoms is especially characteristic of rectal and pharyngeal infections.
Diagnostic Evaluation: Diagnosis has traditionally been made by culture taken from the urethra in males or the cervix in females. The development of nucleic acid amplification tests (NAATs) has given clinicians the ability to provide sensitive testing from a variety of collection methods with rapid return of results, although these are more expensive than the traditional Gram stain or culture (Swygard, Seña, and Cohen, 2005). A pelvic examination is no longer the only option for testing females. Urine testing is highly sensitive although slightly less sensitive than cervical testing for women. Another valid alternative is a self-collected vaginal swab. For males a urine sample is adequate for diagnosis; the male should obtain a freshly voided urine sample without prepping the urethra before obtaining the specimen. A large array of tests are available for gonorrhea and chlamydia; they differ in requirements for storage and specimen source (urine, urethra, throat, vagina, cervix), and the nurse should follow labeling instructions.
Therapeutic Management: Uncomplicated gonorrhea is treated with a single dose of cefixime, 400 mg orally, or ceftriaxone may be administered as a one-time intramuscular dose of 125 mg (Centers for Disease Control and Prevention, 2006a). Azithromycin is added to cover chlamydial infection if a reliable test for chlamydia has not ruled out a coexisting chlamydial infection. Treatment failure is rare, and a test of cure after completion of antibiotics is not necessary. Sexual partners must be treated, and instruct the teen to abstain from sexual intercourse for 7 days after treatment (Centers for Disease Control and Prevention, 2006a).
Prevention: Until a genuine prophylaxis against gonorrheal infections is available, direct preventive efforts toward finding and treating affected persons, locating and examining contacts of affected persons, and educating young people regarding the facts of the disease and its spread. Latex condoms prevent transmission of the infection.
Chlamydial Infection
Chlamydial infection is the most common bacterial STI in the United States. Rates are highest among adolescents and young adults. The sequelae of untreated chlamydial infections include PID, ectopic pregnancy, epididymitis, and infertility. Infants born to infected mothers may be born prematurely and develop conjunctivitis and pneumonia. Annual screening of all sexually active adolescent females for chlamydia is recommended (American College of Obstetricians and Gynecologists, 2006; US Preventive Services Task Force, 2007).
Pathophysiology: The disease is caused by the bacterium C. trachomatis. Like viruses, chlamydiae are intracellular parasites during part of their life cycle. The organisms consist of alternating forms: the extracellular, or elementary, body and the intracellular, or initial, body. The elementary body attaches to the host cell, where it induces active phagocytosis and is ingested in a vesicle that serves as a setting for the next stage of the cycle.
Unlike other phagocytosed organisms, C. trachomatis is able to circumvent host cell defenses and become a part of the cell. Within the host cell the elementary body reorganizes into the larger initial body, which uses the cell’s synthetic functions and energy sources for its own metabolic needs. It divides to produce microcolonies of chlamydiae. After 18 to 24 hours the initial bodies again reorganize into elementary bodies and exit from the disrupted host cell to infect new cells. The entire process takes about 40 hours, and the result is a slow, steady accumulation of intracellular inclusions that are diagnostic of the infection.
Clinical Manifestations: The most common symptoms for females are vaginal discharge or dysuria. As the infection ascends to the endometrium and fallopian tubes, menstrual irregularities and lower abdominal pain may develop. Symptomatic males have a urethral discharge or dysuria. Rectal infections are generally asymptomatic; however, symptoms of proctitis may occur.
Diagnostic Evaluation: The diagnosis has traditionally been confirmed by culture media; the emergence of NAATs has improved the testing options and sensitivity for chlamydia as well as for gonorrhea.
Therapeutic Management: The recommended treatment for uncomplicated chlamydial infections is azithromycin, 1 g by mouth as a single dose. The alternate therapy is doxycycline, 100 mg by mouth twice daily for 7 days. The single-dose treatment is preferred for compliance. A test of cure is not necessary. All sexual partners must be treated, and the adolescent should abstain from sexual intercourse for 7 days after treatment. Females should be rescreened in 3 months because recurrent chlamydial infections are more likely to result in PID (Centers for Disease Control and Prevention, 2006a).
Pelvic Inflammatory Disease
![]() PID is an infection of the upper genital tract (endometrium, fallopian tubes, and ovaries), most commonly caused by sexually transmitted bacteria, such as N. gonorrhoeae, C. trachomatis, and a variety of other anaerobic bacteria.
PID is an infection of the upper genital tract (endometrium, fallopian tubes, and ovaries), most commonly caused by sexually transmitted bacteria, such as N. gonorrhoeae, C. trachomatis, and a variety of other anaerobic bacteria.
![]() Animation—Pelvic Inflammatory Disease
Animation—Pelvic Inflammatory Disease
The long-term effects of PID include infertility because of tubal scarring, ectopic pregnancy, and chronic abdominal pain. It is estimated that each year 1 million females of reproductive age experience an episode of PID, with approximately 20% of cases occurring in teenagers. Women under the age of 25 years have a one in eight chance of experiencing PID, compared with a 1 in 8 risk in those over age 25 years. Menstruation at the time of initial infection can increase the risk for the development of PID. The loss of the mucous plug allows the infecting organism to ascend to the upper tract more readily. The blood itself acts as a culture medium for growth of the infecting organisms. Other mechanical factors such as douching may increase the risk of PID; sperm and motile Trichomonas organisms may also carry other infections up the genital tract. Another risk factor for adolescents is lack of access to health care that is affordable, convenient, and confidential. Lack of access results in delays of diagnosis and treatment of abdominal pain, which increases the risk for severe PID (Banikarim and Chacko, 2004).
PID can have acute complications, such as tubo-ovarian abscess and the Fitz-Hugh–Curtis syndrome. This syndrome occurs in about 5% to 20% of women who have acute salpingitis (infection of the fallopian tubes). The same organisms that cause the salpingitis produce an acute inflammation of the covering surrounding the liver (the hepatic capsule) and the peritoneum in contact with the hepatic capsule. The Fitz-Hugh–Curtis syndrome causes acute or chronic right upper quadrant abdominal pain and can lead to chronic adhesions between the hepatic capsule and the peritoneum. In some individuals the pain and tenderness associated with this syndrome may be more pronounced than the pelvic signs and symptoms.
Symptoms in the adolescent may be generalized, with lower abdominal pain; urinary tract symptoms; and vague influenza-like manifestations, such as malaise, nausea, diarrhea, or constipation. A pelvic examination to evaluate the possibility of PID is indicated for every sexually active female who complains of lower abdominal pain.
The diagnosis of PID is based on clinical findings. The 2006 STI guidelines (Centers for Disease Control and Prevention, 2006a) list the minimum criteria for diagnosis as uterine or adnexal tenderness and cervical motion tenderness. Additional criteria to support the diagnosis include oral temperature of 38° C (100.4° F), abnormal cervical discharge, presence of white blood cells on wet mount, elevated erythrocyte sedimentation rate or elevated C-reactive protein, and laboratory documentation of chlamydia or gonorrhea.
The potential for sequelae even after one episode of PID is as high as 25%. The adolescent with PID is at increased risk for infertility, ectopic pregnancy, and recurrent PID. Chronic pelvic pain and dyspareunia are not uncommon after an episode of PID.
The risk of sequelae requires aggressive management of PID in the adolescent. The two outpatient treatment recommendations are ofloxacin, 400 mg twice daily for 14 days, or levofloxacin, 500 mg once daily for 14 days, with or without metronidazole, 500 mg twice daily for 14 days; an alternative is ceftriaxone, 250 mg given intramuscularly, or cefoxitin, 2 g given intramuscularly, plus doxycycline, 100 mg orally twice daily for 14 days, with or without metronidazole. Inpatient therapy includes intravenous antibiotics such as cefoxitin, cefotetan, doxycycline, clindamycin, or gentamicin. On discharge, the adolescent receives a 14-day course of oral doxycycline or metronidazole.
Adolescents with PID need counseling to prevent future infections. Partner notification and treatment are necessary to avert recurrent infection. The adolescent should be instructed to abstain from sexual intercourse while taking the medication and until after her partner is treated. A discussion of negotiating condom usage is beneficial for the prevention of future infections.
Human Papillomavirus
Anogenital warts, caused by HPV infection, are the most common STI in the United States. The highest prevalence of HPV is among women 18 to 24 years of age. Persistent HPV infection is associated with cervical dysplasia and cervical cancer. HPV deoxyribonucleic acid (DNA) has been found in 99.7% of cervical cancer tissues (Kahn and Hillard, 2004). HPV types are classified by genomes with almost 120 genotypes described, 40 of which infect the genital tract. The HPV types are classified as low risk or high risk based on their potential for causing cancer. Either of the risk types may regress spontaneously. Risk factors for HPV infection include sexual behavior (multiple partners), lack of condom use, young age at first sexual intercourse, and history of prior infection (Kahn, Rosenthal, Succop, et al, 2002).
The most visible type of wart is condyloma acuminatum, a raised, polypoid mass with an irregular fingerlike surface and fissures, commonly described as having a “cauliflower” appearance. In females these warts are most commonly seen on the external genitalia or the vagina, cervix, or rectum. The shaft of the penis is the most common site in males, but warts may also appear on the meatus, anus, and scrotum. The presence of warts on the rectum or anus of males is frequently associated with anal intercourse; anal warts in females can be associated with autoinoculation.
Subclinical genital HPV infection is much more common than the warts that are exophytic (growing outward from surface). The previously common practice of treating areas that give a white appearance after application of acetic acid is no longer recommended. Acetowhitening is not a specific test for HPV. Subclinical infections often regress spontaneously without treatment.
Cytologic screening techniques provide high sensitivity in the diagnosis of cervical dysplasia, especially high-grade dysplasia. These liquid-based screening tests filter out the noncellular debris, thus allowing a single layer of cells on the slide. The liquid supernatant may be used to test for HPV DNA. Screening guidelines from the American Cancer Society recommend initiating Pap screening in adolescents 3 years after initiation of sexual intercourse or by age 21; thereafter it is recommended women have annual screening with traditional Pap smears or every 2 years with liquid-based cervical cytologic screening (Saslow, Runowicz, Solomon, et al, 2002). Recent American College of Obstetricians and Gynecologists guidelines recommend that women receive their first cervical cancer screening at age 21 instead of 3 years after initiation of sexual intercourse. In addition, women aged 21 to 30 years should be screened once every 2 years, and women aged 30 years and older who have had three negative cervical cancer tests may be screened once every 3 years (American College of Obstetricians and Gynecologists, 2009).
Therapeutic Management: The treatment of external warts on females and males consists of both patient-applied and provider-administered options. The patient-applied option includes (1) podofilox, 0.5% solution applied with a cotton swab twice daily for 3 days followed by 4 days without therapy; this cycle is repeated as needed for a total of four cycles; or (2) imiquimod, 5% cream applied every day for 3 days a week for 16 weeks. The provider-administered option includes (1) cryotherapy with liquid nitrogen every 1 to 2 weeks; (2) podophyllin resin, 10% to 25% in benzoin, repeated weekly; or (3) 80% to 90% trichloroacetic acid applied weekly (Centers for Disease Control and Prevention, 2006a).
Patient education regarding the use of medication and the importance of follow-up care is essential and should be ongoing. When parents are aware of the infection, their participation in the education may be beneficial to the adolescent. The concrete aspects of HPV and cervical dysplasia may be more easily understood by the adolescent; however, the abstract concepts of asymptomatic infections and the relationship of cigarette smoking to cervical cancer are more difficult to comprehend. The nurse plays an important role in educating the adolescent about the disease process, assisting with smoking cessation, and providing information regarding procedures and treatments. Vaccination against HPV is an important addition to the prevention education for females and males. Current immunization guidelines recommend initiating HPV vaccine at the 11- or 12-year-old well-child visit (see Immunizations, Chapter 12).
Human Immunodeficiency Virus Infection and Acquired Immunodeficiency Syndrome
Preliminary surveillance data from the Centers for Disease Control and Prevention (2006b) indicate that the number of deaths from AIDS in U.S. children younger than 13 years declined from 945 in 1992 to 55 in 2004; preliminary data show a further decrease to an estimated 28 cases in 2007 (Centers for Disease Control and Prevention, 2009). In 2006 a study of 50 states estimated that 56,300 new cases of HIV were diagnosed in adolescents and adults, for an overall rate of 22.8 per 100,000. The most significant increase in new HIV cases was reported among African-Americans males (Centers for Disease Control and Prevention, 2009). In 2006 estimates indicated that the rate of new HIV infections in African-Americans was seven times the rate in Caucasians. Seventy-three percent of all newly diagnosed cases were in men, and 27% were in women; 53% of the new cases were transmitted via males having sex with males, and 31% were transmitted through high-risk heterosexual contact (Hall, Song, Rhodes, et al, 2008). (See Human Immunodeficiency Virus Infection and Acquired Immunodeficiency Syndrome, Chapter 35.)
HIV Diagnostic Testing: Since 2006, the Centers for Disease Control and Prevention has recommended universal testing for everyone 13 to 64 years of age regardless of risk factors in all health care settings, unless the patient opts out. Retesting should be done when the patient has a new partner and with any STI assessment (Centers for Disease Control and Prevention, 2006c). Traditional enzyme immunoassay venipuncture testing, rapid testing from fingerstick, and oral swab home testing kits are available. Nurses in traditional health care office settings can assist in implementing universal testing in primary care.
Hepatitis B Virus
Hepatitis B virus (HBV) is an infection of the liver that affects 300,000 persons annually, 10,000 of whom require hospitalization. (See Chapter 33.) Major concerns have been voiced because of the increased rate of infection, particularly among high-risk populations: intravenous drug users, sexual partners of HBV-infected individuals, homosexual males, and infants of HBV-infected pregnant women. It is estimated that infants whose mothers are positive for HBV have a 70% to 90% chance of becoming infected, and nearly all these infants develop chronic HBV carrier status. Another area of concern is transmission of HBV through contaminated body fluids to health care workers.
Many potential negative outcomes can be avoided through immunization. Current immunization guidelines recommend beginning the hepatitis B vaccine series at birth or, in unimmunized children, at 11 to 12 years of age. (See Immunizations, Chapter 12.) The immunization consists of a series of three intramuscular injections. The goal of universal immunization is to target uninfected infants and adolescents before the onset of high-risk behaviors.
Other Sexually Transmitted Genital Infections
Many sores or lesions that appear on the genitalia are the result of STIs. Experienced clinicians can correctly diagnose these lesions by visual examination only about half of the time. A complete health history, physical examination, and appropriate diagnostic cultures are needed to determine the causative factors. Nurses who interact with adolescents are in a primary position to obtain a health history and refer any sexually active adolescent for appropriate evaluation. Follow-up health education regarding any treatment regimen and prevention strategies is a major nursing role. Because many of the lesions are viral, nurses can assist the adolescent with communication techniques to inform future sexual partners about the potential for infection with an STI. Table 20-3 summarizes the most common genital lesions seen in adolescents.
Nursing Care Management
Nursing responsibilities encompass all aspects of STI education, prevention, and treatment. Primary prevention by avoiding exposure is the least expensive and most effective approach. The nurse can play a role in offering this education to young people before they initiate sexual intercourse. Sexuality education should include information about these diseases, such as their symptoms or lack of symptoms and treatment, and information dispelling the myths associated with their mode of transmission. These diseases are not contracted from toilet seats, drinking glasses, or bath towels. Most teens are uninformed or misinformed about STIs.
Promoting the inclusion of STI information, access to care, and interpersonal and social skill building in school sexuality education programs is an important function of the nurse. No matter what their area of practice, nurses are in a position to disseminate information, identify probable cases of STIs, and refer these cases for treatment.
The increasing incidence of STIs in young people is influenced to a great extent by the number of adolescents who engage in sexual activity. Improvements in testing methods and availability of testing for diseases will result in increased reporting of STIs. The hormonal contraceptive methods provide no protection against STIs. Unfortunately, many girls using these methods mistakenly believe they are also protected against STIs. To decrease the likelihood of infection, encourage sexually active adolescents to always use a condom.
Essential measures for control of the disease include treating the disease, reporting it promptly, and tracking and treating contacts. When working with adolescents, nurses need highly developed interviewing skills and a nonjudgmental approach to elicit an accurate sexual history. Several characteristics of teenagers influence the way health professionals address specific issues related to STIs. Teenagers are often concrete thinkers, which affects the way they process information. Teenagers also have limited coping mechanisms to draw on to assist in dealing with such information. To gain the adolescent’s cooperation and trust, the nurse must convey acceptance and assure the adolescent of confidentiality. The nurse should always consider the early involvement of parents with permission from the adolescent. Family support may make access to health services easier and decrease the emotional stressors associated with acquiring an STI.
For additional information on STIs and abortion, refer to a women’s health or maternity text such as Perry, Hockenberry, Lowdermilk, and colleagues (2010).
Key Points
• Adolescent health-seeking behaviors center on skin problems, abdominal discomfort, menstrual symptoms, and anxieties about physical development and sexual changes.
• Acne is prevalent in the adolescent years; medication and gentle facial cleansing are the treatments of choice.
• The most frequent problems related to the male reproductive system are infections, scrotal conditions, and gynecomastia.
• The most frequent problems of the female reproductive system involve menstruation delays, irregularities, discomfort, and infections.
• Adolescent pregnancy has profound social, educational, psychologic, and economic ramifications. The pregnancy necessitates special attention to nutrition and psychologic and emotional support for the mother and father.
• Abortion as an alternative to birth is a highly controversial issue; there is evidence that it has no long-term psychologic sequelae for most women.
• Adolescents often do not use contraception because of lack of information, anxiety regarding use, conflict over sexual activity, or desire for pregnancy.
• Rape is a serious problem among adolescents; common forms are rape by a nonstranger, rape by a stranger, and incest.
• STIs are the most frequently occurring infectious diseases and a major cause of adolescent morbidity. HIV infection is an increasingly important adolescent health problem.
Answers to Critical Thinking Exercises
1. Yes. Although testicular cancer is not common in adolescence, when it does occur, it is generally malignant. Testicular cancer is very curable if detected early.
2. a. The best way to detect testicular tumors is by performing TSE every month.
b The usual presenting symptom for testicular cancer is a heavy, hard painless mass (either smooth or nodular) that is palpated on the testis.
c Adolescent boys are often self-conscious about their genital anatomy. Adolescent boys may joke about their genital anatomy because of peer influence, but many adolescent males will not admit that they have limited knowledge of their actual genital anatomy and its relation to health.
d As a pediatric nurse practitioner at the school-based clinic, Paul is in an excellent position to teach young men how to perform this examination. It is highly probable that he has already won their trust and confidence through his routine daily nursing activities, such as providing sports physicals and treating their episodic illnesses. Paul will be able to present the class in a manner that is respectful of the boys, while also allaying their anxieties and providing them with an important health skill. The class should be presented in a matter-of-fact way, with an explanation of both the characteristics of the normal testicle and a description of abnormal findings.
3. The first priority is to make certain that all adolescent boys with health problems feel comfortable visiting the health suite and sharing their concerns with the nurse practitioner. The ultimate goal is to ensure that no adolescent boy with a potential testicular tumor fails to get an immediate assessment and referral for treatment.
4. Yes. The information about testicular cancer and the importance of detecting it early provide a definite rationale for the class.
References
Adelman, WP, Joffe, A. The adolescent with a painful scrotum. Contemp Pediatr. 2000;17(3):111–127.
Alan Guttmacher Institute. In brief: facts on American teens’ sexual and reproductive health. New York: The Institute; 2006.
Al-Shaiji, TF, Amann, J, Brock, GB. Fractured penis: diagnosis and management. J Sex Med. 2009;6(12):3231–3234.
American Academy of Pediatrics. Pediatric nutrition handbook, ed 6. Elk Grove Village, Ill: The Academy; 2009.
American Academy of Pediatrics, Committee on Adolescence. Adolescent pregnancy: current trends and issues. Pediatrics. 2005;116(1):281–286.
American Academy of Pediatrics. Care of adolescent parents and their children. Pediatrics. 2001;107(2):429–434.
American Academy of Pediatrics, Committee on Adolescence. The adolescent’s right to confidential care when considering abortion. Pediatrics. 1996;97(5):746–751.
American College of Obstetricians and Gynecologists. Practice Bulletin No. 109: Cervical cytology screening. Obstet Gynecol. 2009;114(6):1409–1420.
American College of Obstetricians and Gynecologists, Committee on Gynecologic Practice. Primary and preventive care: periodic assessments. Obstet Gynecol. 2006;108:1615–1622.
Aquilino, ML, Bragadottir, H. Adolescent pregnancy. MCN. 2000;25(4):192–197.
Ballard, KD, Seaman, HE, de Vries, CS, et al. Can symptomatology help in the diagnosis of endometriosis? Findings from a national case-control study. BJOG. 2008;115:1382–1391.
Banikarim, C, Chacko, MR. Pelvic inflammatory disease in adolescents. Adolesc Med. 2004;15(2):273–285.
Barnet, B, Arroyo, C, Devoe, M, et al. Reduced school dropout rates among adolescent mothers receiving school-based prenatal care. Arch Pediatr Adolesc Med. 2004;138:262–268.
Bertone-Johnson, ER, Hankinson, SE, Bendich, A, et al. Calcium and vitamin D intake and risk of incident premenstrual syndrome. Arch Intern Med. 2005;165:1246–1252.
Bowe, WP, Shalita, AR. Effective over the counter acne treatments. Semin Cutan Med Surg. 2008;27(3):170–176.
Braverman, PK. Premenstrual syndrome and premenstrual dysphoric disorder. J Pediatr Adolesc Gynecol. 2007;20(1):3–12.
Centers for Disease Control and Prevention, HIV/AIDS surveillance report, 2007. Atlanta: The Centers; 2009. available at www.cdc.gov/hiv/topics/surveillance/resources/reports/2007report/cover.htm [(accessed January 31, 2010)].
Centers for Disease Control and Prevention. Youth risk behavior surveillance—United States. MMWR. 2008;7(SS-4):1–131.
Centers for Disease Control and Prevention. 2006 STD treatment guidelines. MMWR. 2006;55(RR11):1–94.
Centers for Disease Control and Prevention, Cases of HIV infection and AIDS in the United States, 2004. HIV/AIDS Surv Rep 2006;16. available at www.cdc.gov/hiv/topics/surveillance/resources/reports/2004report/default.htm [(accessed March 8, 2006)].
Centers for Disease Control and Prevention. Updated guidelines for HIV testing. MMWR. 2006;55(RR44):1–17.
Chapas, AM, Brightman, L, Sukai, S, et al. Successful treatment of acneiform scarring with CO2 ablative fractional resurfacing. Lasers Surg Med. 2008;40(6):381–386.
Chumlea, WC, Schubert, CM, Roche, AF, et al. Age at menarche and racial comparisons in US girls. Pediatrics. 2003;111(1):110–115.
Dalgard, F, Gieler, U, Holm, JO, et al. Self-esteem and body satisfaction among late adolescents with acne: results from a population survey. J Am Acad Dermatol. 2008;59(5):746–751.
DeCastro, GJ, Shabsigh, A, Poon, SA, et al. Adolescent varicocelectomy: is the potential for catch-up growth related to age and/or Tanner stage? J Urology. 2009;181(1):322–327.
Eichenfield, LF, Wortzman, M. A novel gel formulation of 0.25% tretinoin and 1.2% clindamycin phosphate: efficacy in acne vulgaris patients aged 12 to 18 years. Pediatr Dermatol. 2009;26(3):257–261.
Ferrara, M, Coppola, L, Coppola, A, et al. Iron deficiency in childhood and adolescence: retrospective review. Hematology. 2006;11(3):183–186.
Ford, CA, Jaccard, J, Millstein, SG, et al. Perceived risk of chlamydial and gonococcal infection among sexually experienced young adults in the United States. Perspect Sexual Reprod Health. 2004;36(6):258–264.
Gatti, JM, Murphy, JP. Acute testicular disorders. Pediatr Rev. 2008;29(7):235–240.
Gray, SH, Austin, SB, Huang, B, et al. Predicting sexual initiation in a prospective cohort study of adolescents. J Arch Pediatr Adolesc Med. 2008;162(1):55–59.
Grimes, DA. FDA approval of mifepristone: an overview. Contracep Rep. 2000;11(4):4–11.
Gupta, MA, Gupta, AK. Psychiatric and psychological co-morbidity in patients with dermatologic disorders. Am J Clin Dermatol. 2003;4(12):833–842.
Guttman, C. The future is now: nanotechnology creates promising new tretinoin formulation. Dermatol Times. 2009;30(11):39.
Hall, HI, Song, R, Rhodes, P, et al. Estimation of HIV incidence in the United States. JAMA. 2008;300(5):520–529.
Harel, Z. Dysmenorrhea in adolescents. Ann NY Acad Sci. 2008;1135:185–195.
Henshaw, SK, Feivelson, DJ. Teenage abortion and pregnancy statistics by state, 1996. Fam Plan Perspect. 2000;32(6):272–280.
Hetrick S, Merry S, McKenzie J, et al: Selective serotonin reuptake inhibitors for depressive disorders in children and adolescents, Cochrane Database Syst Rev 3:CD004851, 2007.
Hull, PR, D’Arcy, C. Isotretinoin use and subsequent depression and suicide. Am J Clin Dermatol. 2003;4:493–505.
Jacobs, DG, Deutsch, NL, Brewer, M. Suicide, depression, and isotretinoin: is there a causal link? J Am Acad Dermatol. 2001;45(5):S168–S175.
James, SP, Mendelson, WB. The use of trazodone as a hypnotic: a critical review. J Clin Psychiatry. 2004;65(6):752–755.
Joy, EA, Van Hala, S, Cooper, L. Health-related concerns of the female athlete: a lifespan approach. Am Fam Physician. 2009;79(6):489–495.
Kahn, JA, Hillard, PA. Human papillomavirus and cervical cytology in adolescents. Adolesc Med Clin. 2004;15(2):301–321.
Kahn, JA, Rosenthal, SL, Succop, PA, et al. Mediators of the association between age of first sexual intercourse and subsequent human papillomavirus infection. Pediatrics. 2002;109(1):e5.
Kaufman, M, American Academy of Pediatrics. Care of the adolescent sexual assault victim. Pediatrics. 2008;122(2):462–470.
Krakowski, AC, Stendardo, S, Eichenfield, LF. Practical considerations in acne treatment and the clinical impact of topical combination therapy. Pediatr Dermatol. 2008;25(Suppl 1):1–14.
Laflin, MT, Wang, J, Barry, M. A longitudinal study of adolescent transition from virgin to nonvirgin status. J Adolesc Health. 2008;42(3):228–236.
Lounds, JJ, Borkowski, JG, Whitman, TL. The potential for child neglect: the case of adolescent mothers and their children. Child Maltreat. 2006;11(3):281–294.
Major, B, Cozzarelli, C, Cooper, ML, et al. Psychological responses of women after first-trimester abortion. Arch Gen Psychiatry. 2000;57(8):777–784.
Mansbach, JM, Forbes, P, Peters, C. Testicular torsion and risk factors for orchiectomy. Arch Pediatr Adolesc Med. 2005;159(12):1167–1171.
Maruschke, M, Lehr, C, Hakenberg, OW. Traumatic penile injuries—mechanisms and treatment. Urol Int. 2008;81(3):367–369.
Meier, E. RU-486 and implications for use among adolescents seeking an abortion. Pediatr Nurs. 2000;26(1):93–94.
Moreau, C, Cleland, K, Trussell, J. Contraception discontinuation attributed to method dissatisfaction in the United States. Contraception. 2007;76(4):267–272.
Murray, SK, Baker, AW, Lewin, L. Screening families with young children for child maltreatment potential. Pediatr Nurs. 2000;26(1):47–54. [65].
O’Donnell, L, Stueve, A, Duran, R, et al. Parenting practices: parents’ underestimation of daughters’ risks and alcohol and sexual behaviors of urban girls. J Adolesc Health. 2008;42(5):496–502.
Olutunmbi, BA, Paley, K, English, JC. Adolescent female acne: etiology and management. J Pediatr Adolesc Gynecol. 2008;21(4):171–176.
Orr, DP, Johnston, K, Brizendine, E, et al. Subsequent sexually transmitted infection in urban adolescents and young adults. Arch Pediatr Adolesc Med. 2001;155(8):947–953.
Pattullo, L, Griffeth, S, Ding, L, et al. Stepwise diagnosis of Trichomonas vaginalis infection in adolescent women. J Clin Microbiol. 2009;47(1):59–63.
Perry, SE, Hockenberry, MJ, Lowdermilk, D, et al. Maternal child nursing care, ed 4. St Louis: Mosby; 2010.
Peterman, TA, Tian, LH, Metcalf, CA, et al. High incidence of new sexually transmitted infections in the year following a sexually transmitted infection: a case for rescreening. Ann Intern Med. 2006;145(8):564–572.
Potard, C, Courtois, R, Rusch, E. The influence of peers on risky sexual behaviour during adolescence. Eur J Contracept Reprod Health Care. 2008;13(3):264–270.
Rapkin, AJ, Mikacich, JA. Premenstrual syndrome and premenstrual dysphoric disorder in adolescents. Curr Opin Obstet Gynecol. 2008;20:455–463.
Reaman, GH, Bleyer, WA. Infants and adolescents with cancer: special considerations. In Pizzo PA, Poplack DG, eds.: Principles and practice of pediatric oncology, ed 5, Philadelphia: Lippincott Williams & Wilkins, 2006.
Sakamoto, H, Ogawa, Y, Yoshida, H. Relationship between testicular volume and varicocele in patients with infertility. Urology. 2008;71:104–109.
Sakamoto, H, Saito, K, Ogawa, Y, et al. Effects of varicocele repair in adults on ultrasonographically determined testicular volume and on semen profile. Urology. 2008;71:485–489.
Santelli, JS, Kaiser, J, Hirsch, L, et al. Initiation of sexual intercourse among middle school adolescents: the influence of psychosocial factors. J Adolesc Health. 2004;34(3):200–208.
Saslow, D, Runowicz, CD, Solomon, D, et al. American Cancer Society guideline for the early detection of cervical neoplasia and cancer. Cancer J Clin. 2002;52:342–362.
Savio Beers, LA, Hollo, RE. Approaching the adolescent-headed family: a review of teen parenting. Curr Probl Pediatr Adolesc Health Care. 2009;39(9):216–233.
Schwartz, JL, Barnhart, K, Creinin, MD, et al. Comparative crossover study of the PATH woman’s condom and the FC female condom. Contraception. 2008;78(6):465–473.
Sherman, RT, Thompson, RA. The female athlete triad. J Sch Nurs. 2004;20(4):197–202.
Slap, GS. Menstrual disorders in adolescence, Best Pract Res. Clin Obstet Gynecol. 2003;17(1):75–92.
Sotiriadis, A, Papatheodorou, S, Makrydimas, G. Threatened miscarriage: evaluation and management. BMJ. 2004;329(7458):152–155.
Spencer, JM, Zimet, GD, Aalsma, MC, et al. Self-esteem as a predictor of initiation of coitus in early adolescents. Pediatrics. 2002;109(4):581–584.
Stermac, L, Dunlap, H, Bainbridge, D. Sexual assault services delivered by SANEs. J Forensic Nurs. 2005;1(3):124–128.
Swygard, H, Seña, AC, Cohen, MC, Neisseria gonorrhoeae infections in men. UpToDate. 2005. available at www.uptodate.com [(accessed July 1, 2005)].
Templeman, C. Adolescent endometriosis. Obstet Gynecol Clin North Am. 2009;36(1):177–185.
Thiboutot, D, Arsonnaud, S, Pascale, S. Efficacy and tolerability of adapalene 0.3% gel compared to tazarotene 0.1% gel in the treatment of acne vulgaris. J Drugs Dermatol. 2008;4(5):S3–S10.
Tillett, J. Adolescents and informed consent: ethical and legal issues. J Perinat Neonatal Nurs. 2005;19(2):112–121.
Tracy, CR, Steers, WD, Costabile, R. Diagnosis and management of epididymitis. Urol Clin North Am. 2008;35:101–108.
US Preventive Services Task Force. Screening for chlamydia infection: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2007;147:128–134.
Ventura, SJ, Abma, JC, Mosher, WD, et al. Estimated pregnancy rates by outcome for the United States, 1990-2004. Natl Vital Stat Rep. 2008;56(15):1–25.
Vichnin, M. Ectopic pregnancy in adolescents. Curr Opin Obstet Gynecol. 2008;20(5):475–478.
Vigod, SN, Ross, LE, Steiner, M. Understanding and treating premenstrual dysphoric disorder: an update for the women’s health practitioner. Obstet Gynecol Clin North Am. 2009;36(4):907–924.
Walgrave, SE, Ortiz, AE, MacFalls, HT, et al. Evaluation of a novel fractional resurfacing device for treatment of acne scarring. Lasers Surg Med. 2009;41(2):122–127.
Warren, MP, Chua, AT. Exercise-induced amenorrhea and bone health in the adolescent athlete. Ann NY Acad Sci. 2008;1135:244–252.
Webster, GF. Acne: tips and tricks for the pediatrician. Pediatr Ann. 2009;38(2):80–83.
Wiksten-Almstromer, M, Hirschberg, AL, Hagenfeldt, K. Menstrual disorders and associated factors among adolescent girls visiting a youth clinic. Acta Obstet Gynecol Scand. 2007;86:65–72.
Yan, AC. Current concepts in acne management. Adolesc Med Clin. 2006;17(3):613–637.
Yang, H, Liu, CZ, Chen, X, et al. Systematic review of clinical trials of acupuncture related therapies for primary dysmenorrhea. Acta Obstet Gynecol Scand. 2008;87(11):1114–1122.
Zampieri, N, Mantovani, A, Ottolenghi, A, et al. Testicular catch up growth after varicocelectomy: does surgical technique make a difference? Urology. 2009;73:289–292.
*See DRIs at www.nal.usda.gov/fnic/etext/000105.html, or access the Institute of Medicine home page, www.iom.edu.
*434 W. 33rd St., New York, NY 10001; 212-541-7800 or 800-230-7526; www.plannedparenthood.org.
*For information about local organizations, contact National Organization for Victim Assistance, 510 King St., Suite 424, Alexandria, VA 22314; 800-879-6682 or 703-535-6682; e-mail: NOVA@trynova.org; www.trynova.org.