The Child with Musculoskeletal or Articular Dysfunction
http://evolve.elsevier.com/wong/ncic
Adolescents: Intentional and Unintentional Injury, Ch. 19
Birth Injuries, Ch. 9
Care of the Family Experiencing Unexpected Childhood Death, Ch. 23
Childhood Injuries, Ch. 1
Compliance, Ch. 27
Congenital Clubfoot, Ch. 11
Developmental Dysplasia of the Hip, Ch. 11
Family-Centered Care of the Child with Chronic Illness or Disability, Ch. 22
Family-Centered Home Care, Ch. 25
Head Injury, Ch. 37
Injury Prevention: Infant, Ch. 12; Toddler, Ch. 14; Preschooler, Ch. 15; School-Age Child, Ch. 17
Maintaining Healthy Skin, Ch. 27
Pain Assessment; Pain Management, Ch. 7
Physical Abuse, Ch. 16
Physical Activity, Ch. 17
Physical Examination: Back and Extremities, Ch. 6
The Child and Trauma
Epidemiology of Trauma
Trauma is a leading cause of death in children older than age 1 year (see Chapter 1) and an important cause of disability during childhood and adolescence. In many ways, childhood trauma differs little from trauma in adults. However, the child’s developmental stage affects many aspects of injury, including the type of injury incurred and the physiologic response to injury. The Centers for Disease Control and Prevention estimated that 9.2 million children ages 0 to 19 years visited an emergency department annually between 2000 and 2006 for treatment of an unintentional injury (Borse, Gilchrist, Dellinger, et al, 2008).
Unintentional Injury: Among the leading causes of morbidity in children are medical problems resulting from traumatic injury that occurs at home or at school, in an automobile, or in association with recreational activities. Children’s everyday activities include vigorous play that may involve such things as climbing, falling, running into immovable objects, and receiving blows to any part of the body. All of these activities make them prone to injury. School-age children and adolescents are vulnerable to multiple and severe trauma because they are mobile on bikes and motorcycles and in automobiles; they are also active in sports. Speed and congested surroundings often increase the chance of injury.
Young children and adolescents usually do not calculate risks as they learn to manipulate their environment and achieve developmental goals. Therefore accidents are a part of many childhood experiences. Fortunately, when children fall or are hit, their body’s resilience protects them from serious damage to soft tissue, the musculoskeletal system, or other body organs. Their bones are more flexible than those of adults and therefore do not offer the rigid resistance to external forces that are likely to cause fractures (as occurs in more mature bones).
Child Abuse Injury: Unfortunately, careless handling of an infant or child (in some instances intentional physical abuse) is not uncommon. A multitude of different types of bone and soft tissue injury are inflicted on children by adults, and smaller children who are unable to protect themselves are most vulnerable. It is estimated that 25% to 50% of fractures in children younger than 3 years of age are the result of child abuse.
A traumatic incident that produces physical injury to an infant or child may be the outcome of an accident that was no one’s fault, or it may be associated with child abuse. A well-documented history and a careful examination are essential to determine the cause of the injury. Emergency department and pediatric office personnel should be alert to situations in which the child’s injuries are not congruent with the parent’s description of the incident; in which the child’s behaviors, such as fearful mannerisms or lack of crying, are not the expected ones; or in which radiographs show multiple healed fractures. Accounts of injury inconsistent with developmental abilities can alert the provider to possible abuse. For example, a 6-month-old infant cannot “climb out of the crib and break her leg.” Reporting these incidents will aid in securing help for the child and family. (See Community Focus box; also see Physical Abuse, Chapter 16.)
Childhood Characteristics: Certain developmental characteristics of children at various ages render them more susceptible to injury. For example, the large head of infants and toddlers predisposes them to head injury, especially in falls or motor vehicle injuries. Also, the relatively large spleen and liver and the broad costal arch make these structures prone to direct trauma. Because of their light weight and small size, infants and small children are easily thrown around in a moving vehicle. Their natural curiosity and their propensity for using large muscles lure them to attempt potentially hazardous activities.
Later, in school-age children and adolescents, whose bone growth outstrips muscle growth, difficulty controlling movement can contribute to physical injury. This is also a time when many children attempt to engage in activities beyond their physical capabilities to keep up with more agile companions and to meet the expectations of adults and older siblings. They are also vulnerable to a “dare.” Risk taking compounded by a feeling of invulnerability is also characteristic of adolescence. Children of school-age and early adolescence may also be encouraged to continue engaging in sports activities after suffering a contusion or sprain and are therefore subject to repetitive sprain injuries.
Prevention of Injury
Increasingly, health care providers are recognizing the importance of injury prevention efforts in preserving the health and well-being of children. Nurses have an important role to play in these efforts.
Leading causes of injury to children include falls, being struck by or against an object, motor vehicle accidents, fires, pedestrian-vehicle accidents, drowning, and firearms. Falls were the leading cause of nonfatal injury among children ages 0 to 15 years. Motor vehicle collisions were the leading cause of nonfatal injury in adolescents ages 15 to 19 years of age (Borse, Gilchrist, Dellinger, et al, 2008). Poisonings also occur in young children, especially those between 1 and 4 years of age, and sports injuries occur in school-age children and adolescents.
Unintentional, preventable injury is the primary cause of pediatric mortality and a significant contributor to morbidity, including permanent disability. Both morbidity and mortality could be reduced dramatically by improved efforts at injury prevention. Studies have indicated a general lack of public awareness regarding risks, causes, and prevention of injury to children. Studies also show that injury prevention counseling is effective both in reducing hazards in the home and in increasing car seat use. Nurses can be active in legislative efforts, public awareness campaigns, group classes on injury prevention, and individual prevention counseling with children and families.
Many injury prevention strategies have been suggested for nurses. Nursing history or hospital admission forms can include screening questions about safety issues. Discharge planning or primary care visits might be a time to provide a family with information on safety practices. Well-child visits to the practitioner for physicals and immunizations are an excellent time to visit with children and parents about injury prevention in the home and the community. Home health care nurses can easily assist a family in conducting a home safety assessment. School nurses can develop safety education programs for different age-groups and discuss injury prevention with children that is applicable to their specific age-group. Additional resources for discussing injury prevention with adolescents include automobile insurance companies and the police and first-rescue personnel.* Nurses in emergency department and outpatient clinic settings can provide instructions related to injury prevention on an individual basis as developmentally appropriate.
Accident prevention among adolescents presents a unique challenge to all health care workers. For accident prevention to be effective, adolescents must perceive the specific interventions as having an impact on their lives. Adolescents are concerned with body image and often feel indestructible unless their own life or the life of a close friend is touched by a catastrophic debilitating injury or death. With increased emphasis in society on having fun and enjoying life to its fullest (today) regardless of the consequences (tomorrow), it is difficult for adolescents to understand the need to follow the rules laid down by authority figures.
Concern is also increasing about injuries to older school-age children and adolescents from the use of all-terrain motor vehicles (for which many states have no laws on minimum age for riders), snowmobiles, personal water craft such as wave runners, in-line skates, trampolines, scooters, and motor vehicles. Activities involving such vehicles and equipment, although safe in and of themselves when conducted according to safety guidelines (of the manufacturer), may be dangerous for children and adolescents who are unable to appreciate the risks involved, not only to self but to others as well.
Assessment of Trauma
The site of the injury usually influences the order of priority of interventions when emergency care is being instituted. Consider the safety of both the victim and the “Good Samaritan” rescuers to prevent further injury.
For example, removing a child from a burning building or the bottom of a swimming pool is an obvious, logical action, but anxious rescuers may not consider their own safety to be of prime importance. The major reason for thinking through the steps to be taken in an emergency before an incident actually occurs is to have preplanned actions available at a stimulus-response level.
Emergency Management
The Emergency Treatment box outlines guidelines for care of the child at the scene of an injury. After level of consciousness is assessed, the concerns are for airway, breathing, and circulation (ABC), after which other injuries are managed as indicated by the assessment. When spinal trauma is a possibility, open the airway using the modified jaw thrust maneuver, which is accomplished by grasping the angles of the victim’s lower jaw and lifting with both hands, one on each side, and displacing the mandible upward and outward (without head tilt or chin lift). Otherwise a head tilt–chin lift maneuver is effective in opening the victim’s airway. (See Cardiopulmonary Resuscitation, Chapter 31.)
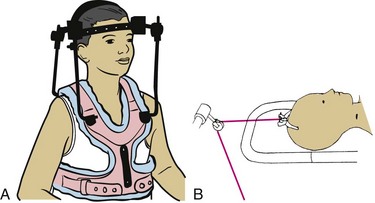
Spinal cord injury cannot be assessed adequately in the prehospital setting. Radiography, computed tomography (CT), or magnetic resonance imaging (MRI) is required for diagnosis. Spinal cord injury is always suspected in a patient with head, trunk, or multisystem trauma. Only in a fully equipped trauma center with radiography and other diagnostic testing can spinal cord injury be ruled out. Therefore the patient is treated as if injury were present. Immobilize the cervical spine by maintaining the head in a neutral position and not allowing movement of the head or body in any direction.
Breathing is assessed after the airway is opened. If the child is not breathing, rescue breaths are given at a rate of 20 breaths/min. Oxygen should be provided when possible. Circulation is assessed only after the airway has been maintained and breathing is established. In children younger than 1 year of age, a brachial pulse is assessed. In those older than 1 year of age, a carotid pulse is palpated. Chest compressions should be initiated if necessary. (See Cardiopulmonary Resuscitation, Chapter 31.)
Control of bleeding is first attempted by application of direct pressure with a gloved hand. If this does not work, a pressure dressing is applied. The next step is to elevate the body part and then attempt to control hemorrhage by pressing on arterial pressure points. A tourniquet is used only when the bleeding cannot be controlled with a pressure dressing (Laskowski-Jones, 2002). If used, the tourniquet should be applied only to control bleeding. Once applied, it should not be removed or loosened. Below the tourniquet site, skin and tissue necrosis begins. If the tourniquet is loosened or removed, the toxins can be released into the circulation in high concentrations and may induce a systemic, deadly, tourniquet shock. With the tourniquet in place, the patient has a better chance of survival, even though it may mean the loss of a limb. Tourniquet use in prehospital settings has been shown to be safe (Doyle and Taillac, 2008; Lee, Porter, and Hodgetts, 2007).
Assessment of the child involves observation from head to toe, since infants and young children are unable to communicate except by crying and other behaviors. Therefore pinpointing areas of pain is difficult. To check for any motor or sensory dysfunction in the extremities, the nurse should note any spontaneous movement, which provides the best clue in infants and young children. Older children are able to follow directions to wiggle toes or fingers, demonstrate a grasp, “push down on the gas pedal,” or lift legs off the bed. The child is identified as soon as feasible by anyone who knows the child. It is important to determine whether the child has any existing health problems that might have implications for the circumstances of the injury and for therapeutic management. Ask any witnesses for details about the incident to aid in assessment of the child’s emotional responses.
In the prehospital setting the nurse’s role consists of contacting emergency medical services (EMS) and providing basic life support until EMS personnel arrive on the scene. The nurse’s role is limited to basic life support because the nurse has no standing orders or protocols under which to work in the prehospital setting (see Emergency Treatment box). Call EMS as soon as possible so that the patient can receive advanced life support before and during transport. A pediatric trauma triage system with personnel designated to care for an injured child is essential to provide excellent trauma patient care.
A paramedic-level ambulance provides at least one paramedic with skills in advanced cardiac life support, pediatric advanced life support, and neonatal resuscitation. A paramedic’s skills include electrocardiogram interpretation and defibrillation, advanced airway management (including endotracheal intubation, as well as intravenous [IV] and pharmacologic therapy), placement of a pneumatic antishock garment (PASG), pleural decompression (with a chest tube), and placement of a nasogastric tube and Foley catheter. Other advanced life support skills include expertise in spinal immobilization, extrication, management of fractures and bleeding, and emergency scene management. The paramedic remains in constant contact with the emergency department physician by means of a radio or cellular telephone for situations requiring medical control. Attempting to transport a child by automobile wastes valuable time in obtaining help. Transportation by EMS is recommended. Services in most large communities can institute advanced life support immediately or en route to a medical facility.
Systematic Assessment
Several factors can affect a child’s response to trauma. An undetected congenital anomaly can contribute to a complicated injury. Acute gastric distention occurs frequently in children because of the crying and screaming that accompany an injury. The temperature of young children is unstable because of their large surface area in relation to body mass, and temperature maintenance is critical in trauma management. Children also experience rapid metabolic changes. When they are ill, children are really ill; but as they recover, they change very rapidly. In addition, children have a small volume of blood in absolute terms. Whereas blood volume is 60% of total body weight in the adult, it is 70% to 85% in the child.
The first priority on admission to an emergency facility is rapid assessment of ABC status. Because the overwhelming majority of childhood injuries are the result of blunt-impact trauma, multiple organ involvement is a common finding. Therefore it is essential to perform a systematic assessment of the trauma victim.
The secondary survey is a systematic head-to-toe search for any additional injuries not originally addressed in the primary survey. However, children are often an exception to the head-to-toe approach. It may be preferable to complete the secondary survey on the injured child in a toe-to-head direction. This approach may allow the rescuer to gain the child’s trust as the survey progresses and the rescuer moves gradually into the child’s personal space. The Nursing Care Guidelines box gives an example of a complete secondary survey. Throughout the assessment, the nurse observes for areas of deformity, edema, ecchymosis, bleeding, hematoma, paralysis, or pain.
The Immobilized Child
One of the most difficult aspects of illness is the immobility it often imposes on a child. Children’s natural tendency to be mobile influences all elements of growth and development—physical, social, psychologic, and emotional. Impaired physical mobility related to disability or imposed activity restrictions presents a definite challenge to the child, staff, and parents providing care.
Causes of Immobilization
The usual reason for immobilizing or restricting the activity of a child without disabilities is illness or injury. Bed rest or mechanical restraining devices are frequently prescribed to aid in the healing and restorative processes. When children are ill, they are content to remain quiet, and most of them instinctively reduce their activity. It is children who are forced to remain inactive because of physical limitations or therapy who display the multiple effects of restricted movement.
The most frequent reasons for immobility are congenital defects (e.g., spina bifida); neuromuscular conditions (e.g., muscular dystrophy, spinal muscular atrophy); the need for prolonged mechanical ventilation and sedation; and infections or injuries that impair the integumentary system (severe burns), the musculoskeletal system (complex fractures or osteomyelitis), or the neurologic system (spinal cord injury, Guillain-Barré syndrome, or traumatic brain injury and coma). Sometimes therapies such as traction and spinal fusion are responsible for prolonged immobilization, although the trend is toward early mobilization, early discharge, and outpatient care.
Physiologic Effects of Immobilization
Many clinical studies, including space program research, have documented predictable consequences that occur after immobilization and the absence of gravitational force. Functional and metabolic responses to restricted movement occur in most of the body systems. Each has a direct influence on the child’s growth and development, since homeostatic mechanisms thrive on normal use and need feedback to maintain dynamic equilibrium. Inactivity leads to a decrease in the functional capabilities of the whole body as dramatically as the lack of physical exercise leads to muscle weakness.
Although children usually become mobile once they feel well, the effects of immobility may be offset by a process termed prehabilitation, in which the individual’s functional capacity is enhanced before prolonged immobility to help withstand the stress on the body’s vital function. Prehabilitation has been implemented for adult patients in the intensive care unit and for those undergoing coronary artery bypass graft, knee arthroplasty, or orthopedic surgery who require prolonged immobilization; it could also be used for children anticipating immobility. Athletes use prehabilitation to decrease the incidence of injuries and increase vital functioning of the cardiorespiratory system, muscles, and metabolism.
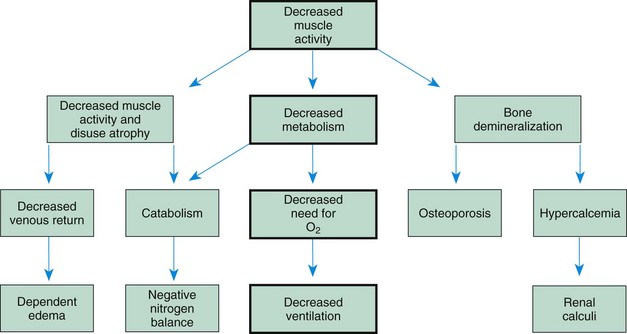
Most of the pathologic changes that take place during immobilization arise from decreased muscle strength and mass, decreased metabolism, and bone demineralization. The three are closely interrelated, with one change leading to or affecting another. Some results of immobilization are primary and produce a direct effect; other pathophysiologic consequences occur frequently but seem to be more indirect and are therefore secondary effects. Many pathophysiologic changes affect more than one body system, with the primary or secondary effect being demonstrated in multiple systems.
Children who are confined to bed during an illness or traumatic injury are usually restricted in movement for a relatively short time or are sufficiently active to avoid the physical consequences of immobility.
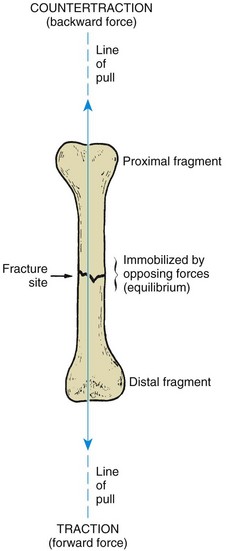
The major effects of immobilization (Fig. 39-1) are related directly or indirectly to decreased muscle activity, which produces numerous primary changes in both muscular and bone structures along with secondary alterations in the cardiovascular, respiratory, metabolic, and renal systems. The major consequences are:
• Significant loss of muscle strength, endurance, and muscle mass (atrophy)
The larger the portion of the body immobilized and the longer the immobilization, the greater the hazards of immobility.
Muscular System: Inactive muscle loses strength at the rate of 3% per day, and several weeks or months are sometimes required for function to be regained when there is no primary neuromuscular deficit. Stretching can occur as muscle loses its tone or as excessive strain is put on weakened muscle (e.g., stretching by tight bed covers or poor body position that produces footdrop as experienced by some children with disability). The disuse leads to tissue breakdown and loss of muscle mass (atrophy). The chief intracellular muscle enzyme, creatine, is released into the serum as the muscle atrophies; therefore serum levels provide an indication of the amount of muscle mass undergoing degeneration. Muscle inactivity also affects the cardiovascular system by decreasing venous return and cardiac output. In general, muscle atrophy causes decreased strength and endurance. Passive or active range-of-motion exercise and proper positioning can prevent joint stiffness and joint and intraarticular dysfunction.
Skeletal System: The daily stresses on bone created by motion and weight bearing maintain the balance between bone formation (osteoblastic activity) and bone resorption (osteoclastic activity). When these stresses are diminished, bone formation ceases, but bone destruction continues, so that the state of equilibrium is disrupted. Bone calcium becomes severely depleted, and secretion of phosphorus and nitrogen is increased. This demineralization of the bone (osteopenia) makes the skeletal structures prone to pathologic fractures and increases calcium ion concentration in the blood (hypercalcemia).
In children who have limited mobility, such as children who are unconscious or partially or fully paralyzed, joint mobility becomes restricted. In the absence of normal structural stretching, collagen fibers generated within the joint become fibrotic and further limit movement. This tissue fibrosis creates shortening of the muscles and contracture of the joint. Any decrease in circulation to the joint caused by edema, inflammation, or restrictive positioning contributes to further fibrotic changes. The problem rapidly becomes cyclic as the contracture leads to muscle fatigue and pain, which causes the child to protect the site, thus leading to more fibrosis. This process is further exaggerated because body flexor muscles are stronger than extensor muscles, and unless range of motion is reestablished within 3 to 7 days, contractures will develop. Frequent disabling contractures are hip flexion, knee flexion, shoulder stiffness, and plantar flexion of the feet.
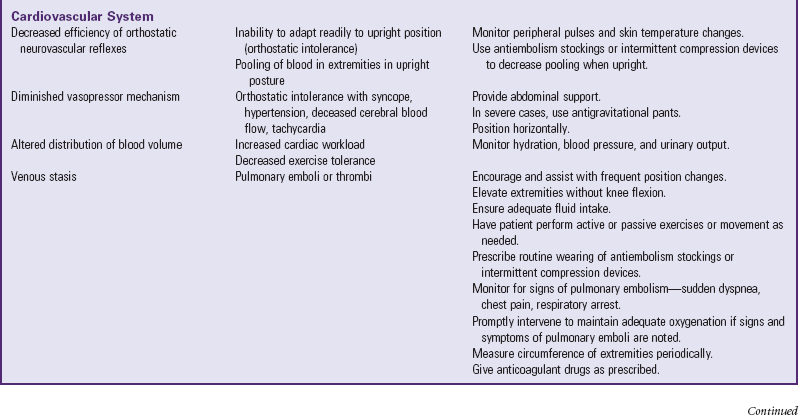
Cardiovascular System: Immobility has three major cardiovascular consequences: orthostatic intolerance, increased workload of the heart, and thrombus formation. During movement, muscle contraction causes pressure on peripheral veins, which in turn causes the venous valves to close and thus assists in return of the blood to the heart when the individual is in an upright position. In the absence of this assistance, blood tends to pool in the dependent areas, reducing the blood supply to the trunk and brain. In addition, direct reflex stimulation to the splanchnic and peripheral vessels causes them to constrict when a person is upright. Impairment of this neurovascular orthostatic reflex activity from lack of motion causes further interference with venous return. The individual displays signs of excessive autonomic activity (e.g., pallor, sweating, and restlessness, which are frequently followed by fainting). The child with a spinal cord injury has unique problems with orthostatic intolerance, which is discussed in Chapter 40.
Changes in vascular resistance caused by the horizontal position and immobility alter the distribution of blood within the body. The reduction in gravity pressure to the extremities causes much of the total blood volume to be redistributed from lower extremities to other parts of the body. Consequently there is an increase in the venous return and the volume of blood to be handled by the heart, which is reflected in elevated blood pressure. As a result, cardiac output and stroke volume are increased, and a progressive increase in heart rate occurs. When immobilization extends over time, there is a compensatory decrease in blood volume and a decrease in heart rate and blood pressure.
Without muscle contraction, venous stasis and increased intravascular pressure in the extremities often lead to dependent edema. If undue pressure is exerted on the major veins by positioning or mechanical devices, the likelihood of interstitial edema is increased. Edematous tissue, especially tissue located over an area that receives much of the body’s weight, is prone to skin breakdown.
Circulatory stasis combined with hypercoagulability of the blood, which results from factors such as damage to the endothelium of blood vessels (Virchow triad), can lead to thrombus and embolus formation. Deep vein thrombosis (DVT) involves the formation of a thrombus in a deep vein such as the iliac and femoral veins and can cause significant morbidity if it remains undetected and untreated. DVT may develop with prolonged venous stasis in conditions such as obesity, chronic heart failure, prolonged surgical procedure, long trips without exercise, or prolonged immobilization (Wipke-Tevis and Rich, 2007).
The state of deconditioned cardiac function, caused by skeletal muscle inactivity, can produce a variety of secondary problems in other systems. However, the major clinical manifestation is increased pulse and heart rate in response to an active exercise program. After prolonged immobility the child should build up activity tolerance slowly to allow the heart to regain optimum capabilities.
Respiratory System: Initially the effects of immobilization are compensatory or adaptive. The basal metabolic rate is decreased because with reduced expenditure of energy the cells require less oxygen and produce less carbon dioxide. Lessened demand for oxygen–carbon dioxide exchange causes the respirations to become slower and more shallow. Chest expansion may be limited by the supine posture; by abdominal distention caused by accumulation of feces, gas, or fluid; and by mechanical restriction such as from a body cast, brace, or tight binders. Reduced muscle power and coordination secondary to altered innervation can also hinder respiratory movement. More effort is required to expand the lungs in the supine position.
Prolonged immobility also reduces the normal movement of secretions from the tracheobronchial tree, particularly in the presence of impaired muscle function and without positional changes that normally facilitate removal of secretions. A weak and ineffectual cough reflex contributes to stasis of secretions and the possibility of airway obstruction in the smaller airways of children. Shallow respirations and obstruction of the airway with thick mucus are factors in the development of secondary complications such as atelectasis and pneumonia.
Gastrointestinal System: Prolonged immobility produces a state of negative nitrogen balance resulting from the increased catabolic activity related to muscle atrophy. This and the reduced energy requirements contribute to a diminished appetite and a resulting decrease in ingestion of nutrients (anorexia). Eating and feeding become more difficult with immobility, and the risk of aspiration is increased. Associated psychologic factors further influence intake.
The process of elimination depends on the integration of smooth and skeletal muscle activity and on visceral reflex patterns. Immobility may interfere with these mechanisms, as well as with the gravitational effect on stool passing through the intestines. Slowing of stool in the colon causes the feces to become hard, and the bowel wall is not stimulated to further its peristaltic movement down the tract to the rectum. Weakened muscles used in defecation (diaphragmatic and abdominal muscles) are unable to produce the intraabdominal pressure needed for elimination. Sometimes embarrassment in using a bedpan or bedside commode may be the cause of not responding to the urge to defecate.
Renal System: The urinary system is designed to function in an upright posture. When the gravitational force is altered by the reclining position, the peristaltic contractions of the ureters are insufficient to overcome gravitational resistance. Consequently there may be stasis of urine in the kidney pelves, and any particulate matter that settles in the calyces may serve as nuclei for calculi formation or as foci for infection.
In the horizontal position the individual has difficulty relaxing the perineal musculature and external sphincter sufficiently to initiate the integrated reflex micturition mechanism, which involves the external sphincter, the internal sphincter, and the detrusor muscle of the bladder wall. If adequate intraabdominal pressure is exerted, voiding can occur, but if the individual does not respond to the sensation to void, bladder distention leads to stasis, and its complications add to embarrassing overflow incontinence. In time, reflux and back pressure may impair renal function, and urinary tract infection is always a hazard with urine retention.
Normally the kidney is able to handle the increased metabolites from protein breakdown and bone demineralization. However, the increased level of calcium excreted may predispose the person to calculus formation. Formation of calculi (kidney stones) is further favored by urinary stasis, infection, and an alkaline urine caused by the decreased production of the acid by-products of metabolism. Hematuria may be the only clue to the diagnosis.
Metabolism: Immobility or severe restriction of activity is often accompanied by decreased or inappropriate nutritional intake, which frequently leads to a decreased basal metabolic rate, a negative nitrogen balance associated with catabolism, and a high serum calcium level.
All body systems are influenced by a decrease in metabolism. The altered energy level leads to further fatigue and lack of motivation for moving. Immobilized persons often feel sluggish and have a poor appetite, particularly for protein foods. The protein breakdown in the body related to a loss of muscle and other tissues is more apt to be severe after injury or surgery. Protein breakdown produces nitrogenous wastes, and on the fifth or sixth day of catabolic protein metabolism, an increase in urinary nitrogen level develops that contributes to anemia and delayed healing.
Another metabolic problem is hypercalcemia associated with bone catabolism. Completely immobilized children or adolescents are especially prone to hypercalcemia. Symptoms, which include nausea and vomiting, polydipsia, polyuria, and lethargy, usually appear 4 to 8 weeks after immobilization. In tetraplegia, symptoms may occur within 10 days and last for as long as 6 months. The accelerated rate of bone metabolism in children makes the bone demineralization a greater hazard. Larger amounts of calcium are released into the blood than the kidney can excrete, and calcium continues to accumulate in serum. High levels of serum calcium decrease neuronal permeability, which can lead to a depression of the central and peripheral nervous systems. Symptoms, including smooth and skeletal muscle fatigue, diminished reflexes, and atony of the gastrointestinal tract, are a result of the depressed nervous system.
A child with bone demineralization may not develop hypercalcemia, but the excess amount of calcium that the kidneys are required to excrete may produce a negative calcium balance, with more calcium than citric acid lost in the urine. This imbalance causes the urine to become alkaline, with the potential danger of renal calculi, especially if there is an accompanying retention of urine.
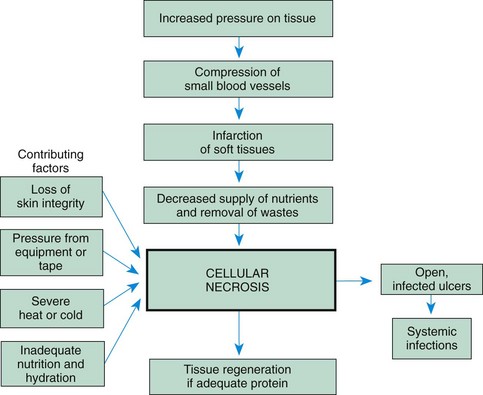
Integumentary System: Circulation to the skin is reduced during inactivity and may be further impeded by dependent edema. Circulation is especially compromised in places where the bone surface is near the skin, such as areas over the sacrum, occiput, trochanter, and ankle, and continued impairment causes rapid necrosis with ulcer formation. Friction and mechanical irritation from appliances, such as straps, rods, and ropes, and the friction of bedclothes during turning or other movement can produce skin breakdown. Healing capacity is also impaired by poor circulation, negative nitrogen balance, and anemia. Immobilization often makes it difficult to carry out adequate cleansing and hygienic measures, which may also contribute to tissue breakdown in areas that are difficult to reach. Guard children with neurologic deficit against extremes of heat and cold in direct contact with the skin.
Cellular breakdown caused by prolonged pressure has several characteristics. Normally when pressure is applied to the skin, the skin appears pale but becomes very red, or hyperemic, after the pressure is removed. This reactive hyperemia should disappear within 5 to 15 minutes. Prolonged redness (>30 minutes) indicates that a pressure area is developing and treatment should begin. Other manifestations of tissue ischemia include an increase in temperature in the area, blistering, swelling, and dark purple or black areas. The pressure area may be limited to the skin and subcutaneous layers or may be deeper and more extensive. The skin changes observed may represent the top of a cone-shaped area with widespread tissue destruction, beneath which tissue rapidly ulcerates and creates a large pressure ulcer that sometimes extends to the bone. Fig. 39-2 illustrates the sequence of events in tissue breakdown. (See also Maintaining Healthy Skin, Chapter 27.)
Neurosensory System: Studies indicate that immobilization does not produce neurosensory consequences directly; however, two occurrences—loss of innervation and sensory and perceptual deprivation—are common.
Peripheral nerves, in contrast to skeletal muscles, do not degenerate with disuse, but loss of innervation takes place if nerves are damaged by pressure or if their blood supply is disrupted. Improper body positioning, poorly applied casts or restraints, or fluid buildup within a compartment (compartment syndrome) can place excessive pressure on nerves and blood vessels that can lead to ischemia and nerve degeneration. Frequent sites of nerve compression phenomenon are the peroneal nerve, where pressure results in footdrop, and the radial nerve, where pressure leads to wristdrop. These complications significantly interfere with attempts to regain functional use of the extremities, but they can be prevented by conscientious nursing assessment and intervention. Preventing pressure on vulnerable areas and avoiding extreme positions of flexion and extension that apply inappropriate pressure on nerves and blood vessels reduce the likelihood of compression injury. Periodic plantar flexion and dorsiflexion of the feet and hands by passive or active range of motion will stimulate circulation and keep nerves from becoming pinched. Numbness, tingling, change in sensation, and loss of motion are symptoms of neurologic impairment and should be evaluated immediately.
Psychologic Effects of Immobilization
For children, one of the most difficult aspects of illness is immobilization. Throughout childhood, physical activity is an integral part of daily life and is essential for physical growth and development. It also serves children as an instrument for communication and expression and as a means for learning about and understanding their world. Activity helps them deal with a variety of feelings and impulses and provides a mechanism by which they can exert control over inner tensions. Children respond to anxiety with increased activity. Removal of this power deprives them of necessary input and a natural outlet for their feelings and fantasies. Through movement children also gain sensory input, which provides an essential element for developing and maintaining a body image.
Active children have many opportunities for input from a wide variety of settings. When they are immobilized by disease or as a part of a treatment regimen, they experience diminished environmental stimuli with a loss of tactile, vestibular, and proprioceptive input and an altered perception of themselves and their environment. Sudden or gradual immobilization narrows the amount and variety of environmental stimuli they receive by means of all their senses: touch, sight, hearing, taste, smell, and proprioception. This sensory deprivation frequently leads to feelings of isolation, boredom, and being forgotten, especially by peers. Nursing interventions involving the use of diversional activities, schoolwork, structured television viewing, computer games, or interactive video programs can assist the child in maintaining usual activities. (See Chapter 26.)
The struggle for independence is thwarted by imposed immobility. For toddlers, exploration and imitative behaviors are essential to developing a sense of autonomy; preschoolers’ expression of initiative is evidenced by their penchant for vigorous physical activity; school-age children’s development is strongly influenced by physical achievement and competition; and adolescents rely on mobility to achieve independence. The quest for mastery at every stage of development is related to mobility. To children, the inability to move is threatening to self-preservation and reactivates the struggle between activity and passivity, and between dependence and independence.
Behavioral changes occur when children experience prolonged sensory deprivation. Some of these behaviors are indications of a higher-than-normal level of anxiety (Box 39-1). Children are likely to become depressed over their loss of ability to function or the marked changes in body image. Significant others often notice regressive behavior and a greater reliance on them for tasks the children are able to perform. Children seek their attention by reverting to earlier developmental behaviors, such as wanting to be fed, bed-wetting, and baby talk. In many ways immobilized children are realistically dependent on others; therefore intelligent and sensitive care is required to prevent major developmental regressions during the period of immobility.
Limbs that are immobilized by casts, traction, or paralysis transmit less sensory data than normally. Sensory impairment may be a concomitant problem of the involved part. Numbness or loss of feeling markedly alters proprioception. Children who have limited ability to feel others touching them not only experience less tactile stimulation in a physical sense but are also deprived of warm, loving feelings that arise from being touched. The loss of feeling from touch can further add to their sense of being isolated and unwanted.
Children often react to immobility with active protest, anger, and aggressive behavior, or they may become quiet, passive, and submissive. Often children believe that the immobilization is a justified punishment for misbehavior. Children should be allowed to express their anger, but this expression should be within the limits of safety to their self-esteem and not damaging to the integrity of others. For example, providing an object to attack rather than a person or a valued possession is safe and therapeutic.
Adults may be confused by, resent, and find it difficult to deal with the acting-out behavior of children. Too often this behavior is considered “bad” even when it is a release of tension. In some cases, such as with a paralyzed child, parents and nurses may feel inadequate to cope with the child’s profound distress and feelings of hopelessness, and the professional help of a mental health specialist is necessary.
The most difficult situations are those involving major injuries and diseases that produce a disfigurement or a severe loss of function that directly affects a child’s self-image, such as burns; amputation; or the sudden, catastrophic effects of an accident that leaves a healthy, active child paralyzed for life. Children have difficulty expressing feelings of anger and hostility when they are at the mercy of the environment. They dare not speak out against or defy the authorities on whom they depend so completely. Consequently their aggression may be masked by cheerfulness or rigidity. When they are unable to express their anger, the aggression is often displayed inappropriately through regressive behavior and outbursts of crying or temper tantrums over insignificant irritations. Adolescents and older school-age children should vary their daily routine to fit their needs for independence; allowing this age-group to stay up late at night and sleep in during the daytime (within reasonable limits to accommodate treatment needs) may help decrease struggles over other inconsequential matters and at the same time allow a daily pattern of life. Encourage parents to continue setting limits and not abandon disciplinary measures with children who are confined to bed due to trauma or illness.
Effects of Immobilization on Families
Brief periods of child immobilization have few effects on the family; however, a child’s catastrophic illness or disability may severely tax their resources. The need for instruction concerning medical and nursing care, community resources to contact, and emotional support are paramount. Many families have unmet needs, operate from crisis to crisis, and are unable to use outside help appropriately. For these families the new situation can be disruptive; therefore the rehabilitation team must help the family members identify unmet needs and solve problems. The following are commonly occurring problems:
• Financial strains may decrease or totally eliminate the family’s resources.
• Attention is focused, at least temporarily, on the affected member; therefore other members of the family, especially siblings, may feel that they are being neglected or that their needs may not be met.
• The family may have difficulty accepting the child’s altered body condition.
• Individual family members may be unable to express their feelings and may have difficulty coping with the crisis.
• Parents often experience guilt over their child’s condition and need for immobilization. Their perception of failing to protect the child forms the basis for their difficulty coping.
The family’s needs often must be met through the services of a multidisciplinary team, and nurses play a key role in anticipating the services the family will need and in coordinating appropriate care. In preparation for the child’s discharge from the hospital, home visits are recommended, and home management is frequently planned weeks in advance of the actual discharge, including special provisions for meeting cultural, economic, physical, and psychologic needs. A child with a severe disability is dependent, and caregivers need rest periods to revitalize themselves. Individual and group counseling is beneficial for problem-solving situations and provides an emotional support system. Parent groups are also helpful and often allow nonthreatening social contact. The families of children with permanent disabilities need long-term resources, since some of the most difficult problems arise as they try to sustain high-quality care for many years. (See Chapters 25 and 22.)
Nursing Care Management
Assessment: Physical assessment of the child who is immobilized as a result of an injury or a degenerative disease includes a focus not only on the injured part (e.g., fracture or damaged joint), but also on the functioning of other systems that may be affected secondarily—the circulatory, renal, respiratory, muscular, and gastrointestinal systems.
Encourage children to be as active as their condition and restrictive devices allow. This usually poses few problems for children, whose innate ingenuity and natural inclination toward mobility provide them with the impetus for physical activity. They need the opportunity, the materials or objects to stimulate activity, and the encouragement and participation of others. Those who are unable to move will need passive exercise and movement, often in consultation with a physical therapist. An occupational therapist and child life specialist may also assist in planning activities to decrease boredom and to help regain lost skills such as self-feeding. A child psychologist may be consulted to discuss with the child and family issues such as depression, anger management, and the effects of the illness on family function.
Children who require prolonged total immobility and are unable to move themselves in bed should be placed on a pressure reduction mattress to prevent skin breakdown. Frequent position changes also help prevent dependent edema and stimulate circulation, respiratory function, gastrointestinal motility, and neurologic sensation. Children at higher risk for skin breakdown include those with prolonged immobilization; those who use orthotic and prosthetic devices, including wheelchairs; those who have plaster casts; and children requiring intensive care. Additional risk factors include poor nutrition, friction (from bed linen with traction), and moist skin (from urine or perspiration) (Fig. 39-3). Nursing care of children at risk includes proactive strategies for preventing skin breakdown when such conditions are present. The Modified Braden Q Scale is a reliable, objective tool the nurse can use in assessing for pressure ulcer development in children who are acutely ill or who are at risk for skin breakdown from neurologic conditions and immobilization (Curley, Razmus, Roberts, et al, 2003).
Circulatory stasis and DVT development are prevented by instructing patients to change positions frequently, dorsiflex their feet and rotate the ankles, sit in a bedside chair periodically, or ambulate several times daily. The use of antiembolism stockings or intermittent compression devices prevents circulatory stasis and dependent edema in the lower extremities and the development of DVT. Anticoagulant therapy may also be implemented with low-molecular-weight heparin, vitamin K antagonists, or unfractionated heparin. Children who are unable to move should have passive range-of-motion exercises of the upper and lower extremities to increase circulation and minimize stasis.
Transporting the child by stretcher, wheelchair, stroller, or wagon outside the confines of the room whenever possible increases environmental stimuli and provide social contact with others. While hospitalized, the child benefits from frequent visitors, accessibility of clocks and calendars, and a program of diversional therapy to help the child function more normally. A child life specialist should be consulted for recreational planning. An activity center or slanting tray can be helpful for the child with limited mobility to use for drawing, coloring, writing, and playing with small toys such as trucks and cars. A child is able to express frustration, displeasure, and anger through play, which is helpful in the child’s recovery. As soon as possible, the child should wear street clothes and resume school and preinjury hobbies. Play is the most useful tool of nursing (see Chapter 26), and activities should be selected on the basis of interest, ability, and limitations. They should include some form of physical activity that encourages the use of uninvolved muscles and joints. Any activity that is tolerated (e.g., turning in bed or changing the position of the bed in the room) helps to alter the monotony of immobilization and dissipates tension and frustration. Allow a parent or siblings to room in with the hospitalized child to prevent the effects of family disruption from hospitalization. Make every effort to minimize family disturbance resulting from the hospitalization. Although most of the suggestions discussed relate to hospital care, the same consultations (physical therapist, occupational therapist, child life specialist, speech/language pathologist) and environment may be considered in the home as well to help the child to gain independence and the family to achieve normalization.
Using dolls or a stuffed animal such as a bear to illustrate and explain the restraining method is a valuable tool for small children. Placing a cast, tubing, or other restraining device on the doll or stuffed animal offers the child a nonthreatening opportunity to express, through the doll, feelings concerning the restrictions and feelings toward the nurse and other health care providers.
Children typically dislike hospital food, which is usually not tailored to their age. In some institutions food services are geared toward children’s preferences with child-friendly menus and smaller food portions served. Allow parents and friends to bring in favorite foods from home or other sources such as fast food places, provided they meet necessary requirements for the illness. This enables children to have more control of their environment and will decrease resistance to treatments and schedules, which is common behavior evidenced when adults and children are not given any choices in an acute care setting.
One of the most useful interventions to help children cope with immobility is participation in their own care. Self-care to the maximum extent possible is usually well received by children. They can help plan their daily routine; select their diet (when possible); and choose the clothes they are to wear, including innovative adornment, such as a baseball cap, brightly colored stockings, or other items that express their autonomy and individuality. Encourage them to do as much for themselves as they are able to keep muscles active and their interest alive. If feasible, they should be placed where they can benefit from the company of other children, which assures them that they are not being singled out for this medical treatment.
It is important for children to understand behavioral limitations or rules. Their questions should be answered. For example, children need to know the reasons for medical, nursing, occupational, and physical therapy and to know that some schedules are necessary. In some areas they have a choice; in others they do not. They may or may not be permitted to sleep late, but they can choose their own clothing. Most of children’s activities of daily living are play; therefore therapies that incorporate play are more apt to gain their cooperation.
Visits from significant persons, such as family members and friends from school or the neighborhood, offer occasions for emotional support and also provide opportunities for learning how to care for the child. If a traumatic incident caused the child’s disability, guilt feelings may be displayed overtly or masked behind regressive or aggressive behavior. The feeling that “I must have been bad to receive this fate” is common, and honest feedback, such as “It just happened—it was an accident,” needs repeating many times. Additional aspects of grieving are involved if there was a loss of another person or if permanent disability occurred as a result of the accident. All these feelings need to be brought out and dealt with. In addition, professionals working with these children must not “baby” or overprotect them but must help them to cope with their altered body image and reestablish their self-esteem.
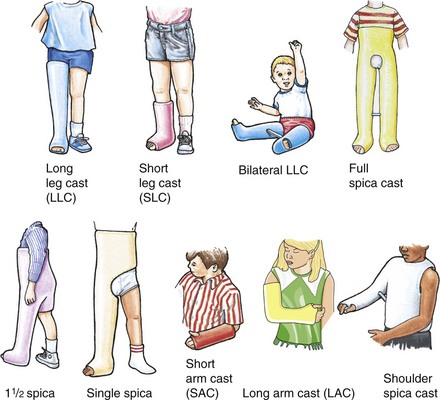
For a child with greatly restricted movement (e.g., a child with tetraplegia or a child with a large bilateral hip spica cast), creativity in nursing care is often required to keep the child stimulated and prevent the effects of immobilization. These situations may require long-term care in the hospital, a rehabilitation center, or, increasingly, at home. Wherever the care occurs, consistent planning and coordination of activities with professionals and significant others is vital.
Nursing assessment includes gathering psychosocial data, in addition to assessing physical manifestations, since long-term immobilization has a profound effect on the child and the family. Nursing approaches are evaluated frequently and continued, discontinued, or modified to meet the changing problems and goals. Table 39-1 summarizes the physical effects of immobilization and appropriate nursing care management. With the increased trend toward early mobilization, early discharge, and home health care, many children are discharged home after a few days of hospitalization. Follow-up treatment may take place in the home or in an outpatient ambulatory facility.
TABLE 39-1
SUMMARY OF PHYSICAL EFFECTS OF IMMOBILIZATION WITH NURSING INTERVENTIONS*
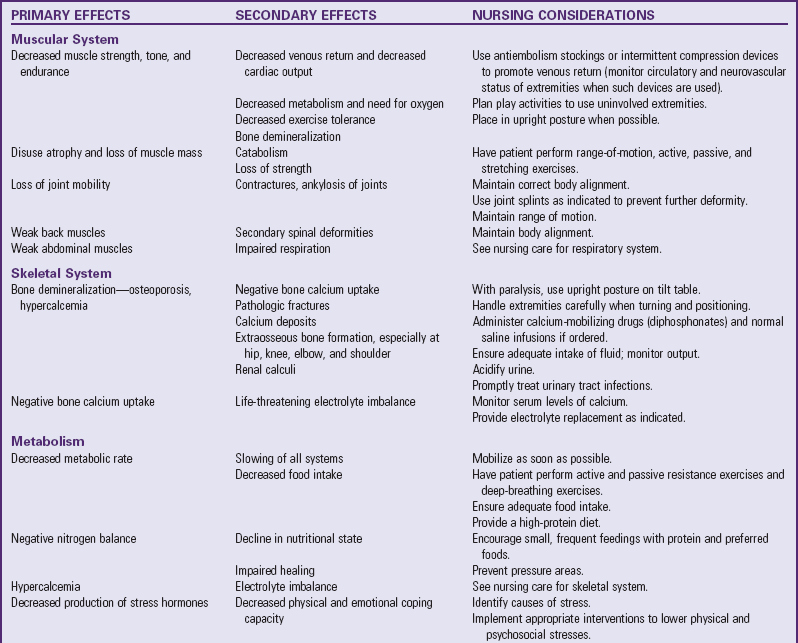
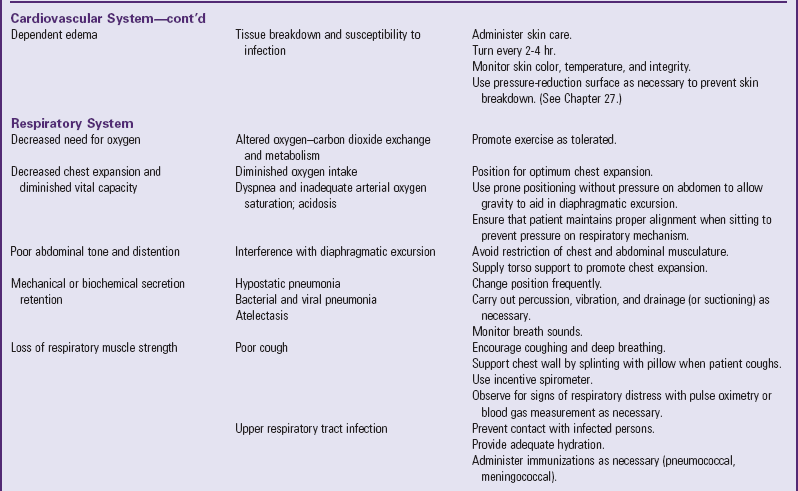
*Individualize care according to child’s needs; interventions may vary in different institutions.
Mobilization Devices
Developments in the fields of orthotics (fabrication and fitting of braces) and prosthetics (fabrication and fitting of artificial limbs) have resulted in lighter and better-fitting devices and thus greater patient compliance in using them. Orthoses are often used to prevent deformity, increase the energy efficiency of the gait, and control alignment. Braces that facilitate walking can sometimes stabilize paralyzed or markedly weakened extremities. Special joint hinges permit the hip, knee, and ankle to flex while sitting, whereas the leg is held rigid during ambulation. Well-fitted orthoses promote ambulation, whereas ill-fitting braces throw off the child’s balance and frequently cause muscle stress and tissue breakdown. In the growing child braces need frequent adjustment and replacement by the orthotist if long-term use is necessary.
A standing frame or a parapodium (a standing frame on a circular base) helps small children to assume an upright position and begin mobilization. Children learn to use their arms and shift their weight to swivel the base of the parapodium to mobilize. Four common types of orthoses are used in older children and are described based on the joints controlled by the orthosis. The ankle-foot orthosis (AFO) is used to prevent footdrop due to bed rest, trauma to the foot, or paralysis of muscles that flex the foot; to prevent heel cord tightening after heel cord–lengthening surgery; or to support the foot in proper position for standing and walking (Fig. 39-4). AFOs are now available in patterns and colors.

Fig. 39-4 Left to right: Supramalleolar ankle-foot orthosis (AFO), solid ankle AFO, articulating ankle AFO, floor reaction AFO.
The knee-ankle-foot orthosis (KAFO) is used to prevent buckling of the knee, to support the extremity when there is paralysis or marked weakness of the knee extension or quadriceps muscle, or to protect the limb when the bone structure is weak (Fig. 39-5). The hip-knee-ankle-foot orthosis (HKAFO) is used to provide various types of control for the knee and ankle joints (as described earlier), as well as the hip (e.g., flail lower limb and paralysis). The reciprocal gait orthosis (RGO) is a type of HKAFO that has a mechanism allowing children with significant paraplegia to walk in a reciprocal fashion on a flat surface. RGOs are used in children with spinal cord injury, sacral agenesis, and spina bifida.
The thoracolumbosacral orthosis (TLSO) is custom molded and fits snugly around the trunk of the body to exert pressure on the ribs and back to support the spine in a straight position (Fig. 39-6). The Boston brace is an underarm orthosis customized from prefabricated plastic shells, with corrective forces for each patient supplied by lateral pads. These braces may prevent the progression of curves in the spine, such as scoliosis, or provide needed torso support in a child with paraplegia. The Jewett-Taylor brace is sometimes used to support the spine and trunk during ambulation to prevent compression after fracture of the spinal column.
An orthosis must fit each body curvature to avoid undue pressure on tissues and imbalance between muscle groups. Bony prominences where a brace has contact, such as along the spine, chin, and iliac crests, are observed closely for pressure or irritation and are padded as necessary.
When prostheses are prescribed, the provider considers many factors: level of amputation, age, weight, activity, agility, and skin condition. Each prosthesis is custom made or fabricated of various plastic and foam materials. The style of the prosthesis depends on the most distal joint involved in the amputation or prosthetic fitting. Common abbreviations used to describe types of amputations are listed in Box 39-2.
Advances are constantly occurring in both the fabrication and fitting of prosthetics. Development of myoelectric devices, use of new cosmetic materials in terminal gloves and feet, and socket construction using computer-aided design and computer-aided manufacturing are but a few of the recent changes with positive effects for patients who require prostheses.
Nursing Care Management
Meticulous skin care under a brace is necessary. At times, protective clothing should be worn under braces to protect the skin from friction and pressure. Assessment of all areas that make contact with the brace every 2 to 4 hours for the first few days after application is recommended. If any area is reddened, the brace should be removed for  to 1 hour. If the redness does not disappear, the nurse should notify the practitioner or orthotist (see Family-Centered Care box).
to 1 hour. If the redness does not disappear, the nurse should notify the practitioner or orthotist (see Family-Centered Care box).
Before a prosthesis is applied, the condition of the skin must be assessed, with special note taken of areas of redness or breaks in the integrity of the skin. Prevention of skin breakdown is best accomplished through good hygiene of the residual limb, proper fitting of the artificial limb, and prosthetic training (see Family-Centered Care box).
Safety is another important consideration. Parallel bars provide secure hand rails on both sides as the child learns to walk again with or without braces or a prosthesis. As the child becomes more proficient, a walker with or without wheels is substituted for the bars, and the child is no longer confined to a limited territory. The child then progresses to crutches if age and condition permit it.
Crutches and Canes
Crutches are used when children are not allowed to bear weight; need support for balance while walking in braces; or can place only part of their body weight on an extremity, such as with most lower leg injuries. There are many types of crutches, and the selection depends on the child’s individual needs. Axillary swing-through crutches are used most frequently as temporary assistance. Forearm crutches (Fig. 39-7) are the usual selection for children who anticipate permanent use, such as paraplegic children who are able to use braces. In children with limited hand and arm strength or function, the use of trough crutches allows the weight to be assumed by the elbow. For habilitating small children who have not yet learned to walk or who are unsteady, front- or rear-rolling walkers are typically used until the children can progress to crutches (Fig. 39-8).

Fig. 39-7 Adolescent using forearm crutches for ambulation. (Courtesy Texas Children’s Hospital, Houston.)

Fig. 39-8 Young child with rear-rolling walker. (Courtesy Paul Vincent Kuntz, Texas Children’s Hospital, Houston.)
Children must be properly fitted with a crutch or cane to prevent both poor posture and crutch pressure on the axilla during ambulation. A physical therapist usually measures the child for crutches and teaches crutch and cane use; however, nurses in some areas such as the emergency department do teach children crutch walking. Nurses also supervise the use of crutches and canes in pediatric units and in the home. The type of crutch gait taught to a child depends on how stable the child is on crutches, whether or not the knees can be flexed, how much weight bearing is allowed, and what specific goal is established for the child.
Performing upper body strengthening exercises to condition and strengthen arms and shoulders before crutch use is important if immobilization has been prolonged. The child gains confidence in ambulating by wearing a safety belt held by the therapist. The types of gaits used and instructions given to children are similar to those for adults. Instructions are conveyed in language children understand and with a demonstration. Most children adapt to the techniques readily.
Wheelchairs
Wheelchairs are used temporarily or permanently as a means of transportation. A wheelchair for temporary use should fit the child and contain any adaptations needed, such as an elevating leg rest or reclining back. The child learns how to transfer in and out of the chair and how to move it safely. Prescribing a wheelchair for permanent use is the joint responsibility of the physician and therapist after an assessment of home and surroundings. A wheelchair should be neither too small nor too large and preferably should be adaptable as the child grows (Fig. 39-9).

Fig. 39-9 Child in wheelchair, which should be scaled appropriately to child’s size. Note ankle-foot orthoses and left wrist splint to prevent contractures. (Courtesy Texas Children’s Hospital, Houston.)
Detachable or rotating armrests, which permit easy transfer in and out, are needed for children with spinal cord injuries. Other desirable features are detachable and swing-away footrests and detachable desk arms. Elevating leg rests are required for children who are prone to contractures, and a reclining back rest is needed for those who may have poor trunk balance. A pressure-relief cushion should be provided for a child who has decreased sensation. Hand-rim and brake-lever projections are helpful for children with upper extremity weakness. For children who have the use of only one arm, a special “one-arm drive” wheelchair is available. Children with paraplegia require upper arm strengthening exercises and instruction on transfer techniques before wheelchair mobilization (Fig. 39-10). Often a tilt table is used to overcome the problem of orthostatic intolerance before the child is able to tolerate wheelchair sitting.

Fig. 39-10 Wheelchair allows adolescent mobility and independence. (Courtesy Texas Children’s Hospital, Houston.)
Various motorized chairs are available for children with marked upper extremity weakness, and mouth- or cheek-operated models are obtainable for children who do not have the use of upper extremities so that they can operate the wheelchairs independently. Very small children who have permanent paralysis of the lower extremities are provided with specially designed units that allow independent mobility. A detachable handle on these units permits their conversion to strollers.
Bicycles and tricycles (Figs. 39-11 and 39-12) can be modified for children with limited ambulatory mobility; these also promote muscle strengthening and prevent disuse contractures. Gait training may be accomplished with a number of special devices (Fig. 39-13).

Fig. 39-11 Tricycle used to provide mobility and to strengthen leg muscles. (Courtesy Texas Children’s Hospital, Houston.)
The Child with a Fracture
The process of ossification, the gradual conversion of precursor substances (i.e., cartilage) to bony structures, begins in the embryo and continues until the child is 18 to 21 years of age. In long bones this process progresses outward from the diaphysis, the hard, shaftlike portion that constitutes the major part of the bone. Within this hard, compact shaft is the hollow medullary canal composed of the bone marrow.
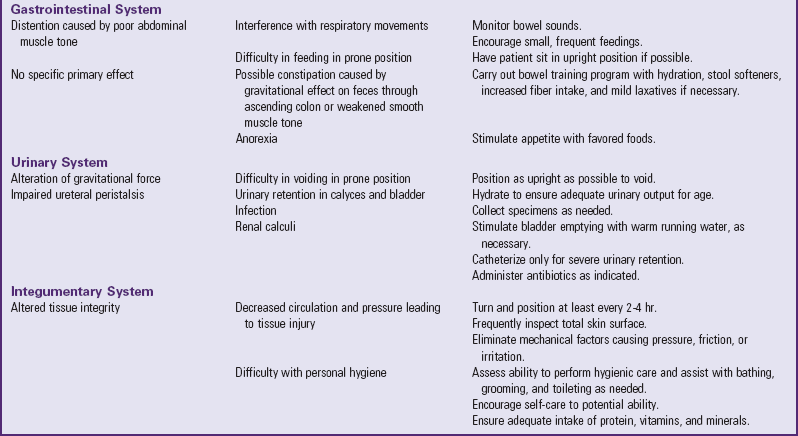
The epiphyses, located at the ends of long bones, consist of layers of cartilage, subchondral bone, and spongelike cancellous bone. Situated between the diaphysis and the epiphysis is the epiphyseal plate, which plays a major role in the longitudinal growth of the developing child (Fig. 39-14). The periosteum, the thin, tough membrane covering all bones, contains blood vessels that nourish the living bone. Damage to this thin membrane can be a major problem in bone growth and healing.
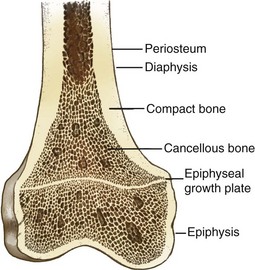
Fig. 39-14 Diagram of bone showing relationships of compact and cancellous bone, epiphysis, epiphyseal plate, and diaphysis. (From Thompson JM, McFarland GK, Hirsch JE, et al: Mosby’s clinical nursing, ed 4, St Louis, 1997, Mosby.)
Fractures
![]() Bones fracture when the resistance of the bone against the stress being exerted yields to the stress force. Fractures are a common injury at any age but are more likely to occur in children and the elderly. Their natural tendency toward active mobility and their limited gross motor coordination make children susceptible to physical injury.
Bones fracture when the resistance of the bone against the stress being exerted yields to the stress force. Fractures are a common injury at any age but are more likely to occur in children and the elderly. Their natural tendency toward active mobility and their limited gross motor coordination make children susceptible to physical injury.
Etiology
The causes of fracture injuries in children are those described for general traumatic injuries in childhood. Fractures in infancy are more often the result of birth trauma, injury, or child abuse. Aside from motor vehicle injuries, true accidents causing fracture are uncommon in infancy; therefore injuries in children in this age-group warrant further investigation. Most often, early bone trauma in infants consists of periosteal bleeding in the long bones of the arms and legs, usually caused by rough handling, twisting, and pulling, which is not evident on radiographic examination until 3 to 6 weeks after the injury. Any investigation of fractures in infants, particularly multiple fractures, should include the suspicion of osteogenesis imperfecta (OI) (see p. 1675). In any small child, radiographic evidence of fractures at various stages of healing, with few exceptions, indicates physical abuse (see Community Focus box, on p. 1620).
Fractures of the forearm are common bone injuries in childhood and are usually caused when the child extends the palm of the hand to break a fall. The force resulting from a fall on the outstretched hand progresses up the length of the extremity with the possibility of injury to the finger, wrist, elbow, shoulder, or clavicle (Fig. 39-15). DiFazio and Atkinson (2005) report that upper extremity fractures are more common in children than in adults. The radius is the most commonly fractured bone of the upper extremity, followed by the bones in the hand. The clavicle is another frequently broken bone in children; approximately half of clavicle fractures occur in children younger than 10 years of age. Many such fractures occur at birth. Hip fractures are uncommon in children and require a great deal of force to produce. A femoral neck fracture may be sustained in children 6 or 7 years of age as a result of pedestrian-automobile accidents because in these children the hip is at the same level as an automobile bumper. In older children the femur is the most likely target; in adolescents knee injuries are common.
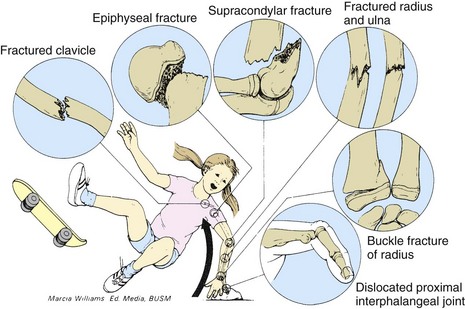
Fig. 39-15 Trauma resulting from progression of force in fall on outstretched hand. (From Segal D: Pediatric orthopedic emergencies, Pediatr Clin North Am 26(4):793-802, 1979.)
Children fall from heights (e.g., trees, roofs, playground equipment) as their insatiable curiosity and immature judgment lure them to places of danger. Fractures in school-age children are often the result of bicycle-automobile collisions or skateboard injuries. Sports are a frequent cause of injury in the school-age child and adolescent.
At all ages motor vehicle mishaps are a frequent cause of bone injury. Most children who are hit by an automobile are between 4 and 7 years of age and sustain a triad of injuries, which must be kept in mind when making an assessment: (1) the child’s femur, which is at the level of the bumper, is fractured; (2) the hood of the automobile produces injuries to the child’s trunk; and (3) a contralateral head injury is usually sustained when the child is thrown to the ground by the impact. Therefore a child with any one of these injuries who was struck by an automobile should be examined for evidence of the other two.
Pathophysiology
![]() The anatomic, biomechanical, and physiologic nature of children’s skeletons causes differences from adults in the patterns of fracture, the problems of diagnosis, and the methods of treatment. The bones of the adult are strong and require a violent traumatic force to fracture, which is accompanied by massive injury to surrounding soft tissues. In children the bones are more easily injured, and fractures may result from minor falls or twists and are less likely to be accompanied by soft tissue damage. Features of children’s fractures not observed in adults are listed in Box 39-3.
The anatomic, biomechanical, and physiologic nature of children’s skeletons causes differences from adults in the patterns of fracture, the problems of diagnosis, and the methods of treatment. The bones of the adult are strong and require a violent traumatic force to fracture, which is accompanied by massive injury to surrounding soft tissues. In children the bones are more easily injured, and fractures may result from minor falls or twists and are less likely to be accompanied by soft tissue damage. Features of children’s fractures not observed in adults are listed in Box 39-3.
Types of Fracture: A fractured bone consists of fragments: the fragment closest to the midline, or the proximal fragment, and the fragment farthest from the midline, or the distal fragment. When fracture fragments are separated, the fracture is complete; when fragments remain attached, the fracture is said to be incomplete. The fracture line can be any of the following:
Transverse—Crosswise, at right angles to the long axis of the bone
Oblique—Slanting but straight, between a horizontal and a perpendicular direction
Spiral—Slanting and circular, twisting around the bone shaft
All fractures affect the entire cross section of the bone. The twisting of an extremity while the bone is breaking results in a spiral fracture. If the fracture injury does not produce a break in the skin, it is a simple, or closed, fracture. Open, or compound, fractures are those with an open wound through which the bone protrudes. If the bone fragments cause damage to other organs or tissues (e.g., the lung or bladder), the injury is said to be complicated. When small fragments of bone are broken from the fractured shaft and lie in the surrounding tissue, the fracture is called comminuted. This type of fracture is rare in children. The types of fracture that occur most often in children are shown in Box 39-4.
Epiphyseal (or Physeal) Injuries: The weakest point of long bones is the cartilage growth plate, or epiphyseal plate. Consequently, this is a frequent site of damage during trauma. Under most conditions, fractures in this area proceed along the zone of degenerating cartilage cells, before the cartilage begins to ossify, without injury to the growth plate and thus cause little damage. Healing is usually prompt. When fracture lines deviate from a transverse direction through the degenerating cells, more serious damage to the epiphysis and the plate may occur. Fig. 39-16 illustrates the types of epiphyseal injury in order of increasing risk of permanent epiphyseal damage and possible growth disturbance. The Salter-Harris classification is typically used to describe epiphyseal injuries, as indicated in Fig. 39-17.
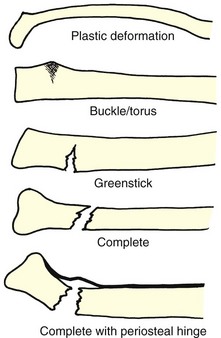
Fig. 39-16 Common types of fracture in children. Note that there are subclassifications of complete fractures based on characteristics of the fracture line.
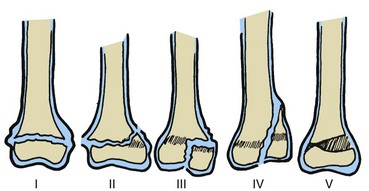
Fig. 39-17 Types of epiphyseal injury in order of increasing risk. The injuries are classified as follows: type I, separation or slip of growth plate without fracture of the bone; type II, separation of growth plate and breaking off of section of metaphysis; type III, fracture of epiphysis extending through joint surface; type IV, fracture of growth plate, epiphysis, and metaphysis; type V, crushing injury of epiphysis (can be diagnosed only in retrospect). This classification of epiphyseal injuries was developed by orthopedists RB Salter and WR Harris. (First published in Salter RB, Harris WR: Injuries involving the physeal plate, J Bone Joint Surg Am 45[3]:587-622, 1963.)
Detection of epiphyseal injuries is sometimes difficult, and they may be mistaken for dislocations or ligamentous injuries. Fractures involving the epiphysis or epiphyseal plate present special problems in determining whether bone growth will be affected. Early and correct assessment is essential to prevent longitudinal growth problems and angular deformities. The medical and surgical management of these injuries is different from that for other fractures because open reduction and internal fixation are often employed to prevent complications. If the affected limb is shorter, epiphyseal surgery is performed either to stimulate the involved epiphysis or to restrict growth in the unaffected leg.
Associated Problems: Immediately after a fracture occurs, the muscles contract and physiologically splint the injured area. This phenomenon accounts for the muscle tightness observed over a fracture site and the deformity that is produced as the muscles pull the bone ends out of alignment. This muscle response must be overcome by traction or complete muscle relaxation (i.e., anesthesia) in order for the distal bone fragment to be realigned to the proximal bone fragment.
Contusions of the soft tissues often accompany a fracture, especially of the femur or pelvis, and severe hemorrhage into the tissues is not uncommon. Both the bleeding and the pain are major contributors to shock associated with this injury; therefore suspected musculoskeletal injury should be treated as a fracture until radiographic confirmation can be obtained. The surrounding tissue will be swollen, and a hematoma is usually present. The soft tissue injury must be treated as any other contusion. Because the injury may cause damage to essential structures, the circulatory and neurologic status of tissues distal to the fracture is carefully assessed, especially for fractures of the femur and supracondylar fractures of the elbow.
Clinical Manifestations
Children demonstrate the usual signs of injury: generalized swelling, pain or tenderness, and diminished functional use of the affected part. There may be bruising, severe muscular rigidity, and sometimes crepitus (a grating sensation at the fracture site), which are also frequent signs in adults. More often the fracture is remarkably stable because of the usually intact periosteum. The child may even be able to use an affected arm or walk on a fractured leg.
Although neurologic and vascular damage is much less frequent in children than in adult patients, the integrity of these structures must be thoroughly assessed. This is often difficult in infants and young children, who are unable to cooperate. Vascular injury is most likely to occur with supracondylar fractures of the humerus and femur. Femoral and popliteal vessels and the sciatic nerve are prone to trauma in femoral fractures. Humeral fractures may cause damage to the medial, ulnar, or radial nerves and to the brachial artery.
During the assessment, include examination for the five Ps of ischemia from a vascular injury: pain, pallor, pulselessness, paresthesia, and paralysis.
Nursing Assessment
Nurses often conduct the initial assessment of a child with a suspected fracture (see Emergency Treatment box). The child and the parents are frightened and upset; the child is in pain; and, because some fractures are obvious, the parents and frequently the child are already convinced of the diagnosis. As a first step, the injured limb should be supported in some manner. Then, if the child is alert and there is no evidence of hemorrhage, direct the initial nursing interventions toward calming and reassuring the child and parents so that a thorough assessment is easier to accomplish.
Maintaining a calm manner, the nurse can ask the parents to describe what happened and what they think about it. As long as the limb is supported in some manner, this minute or two does not delay or endanger the treatment. It is best not to touch children initially but to ask them to point to the painful area and wiggle their fingers or toes distal to the injury. Previous experiences with injury and health care personnel will influence a child’s anxiety. However, children need to be told what will happen and what they can do to help. The affected limb need not be palpated and should not be moved unless properly splinted. A temporary splint should be applied carefully if the child must be transported to a hospital or clinic or to the radiology department.
Diagnostic Evaluation
A history of the injury or events leading up to the injury may be lacking for childhood injuries. Infants and toddlers are unable to clearly communicate the details of what occurred. Older children may not be reliable informants or volunteer information (even under direct questioning) if the injury occurred during questionable activities. In cases of child abuse, parents or caregivers may deliberately give false information to protect themselves. Whenever possible, it is helpful to get information from someone who witnessed the injury.
Radiography: Radiographic examination is the most useful diagnostic tool for assessing skeletal trauma. The calcium deposits in mature bone make the entire structure radiopaque. However, during normal growth and development, much of the skeleton of infants and young children is composed of radiolucent growth cartilage that does not appear on radiographs. In addition, the epiphyseal cartilage and undisplaced separations of the epiphysis (which are common) are not easily detected on x-ray films. Radiographs are sometimes less reliable than gross deformity and point tenderness in predicting extremity fractures.
Practitioners often obtain a film of the uninjured limb for a direct comparison to help identify minor alterations in alignment and configuration of the epiphysis and associated injuries that might be missed. Radiographic films are also taken after fracture reduction and in some situations may be taken during the healing process to confirm satisfactory progress.
Therapeutic Management
The goals of fracture management are:
• To reestablish alignment and length of the bony fragments (reduction)
• To retain alignment and length (immobilization)
Some conditions may require immediate medical attention. These include open fractures, compartment syndrome with and without fracture, fractures associated with vascular or nerve injuries, and joint dislocations that cannot be reduced (DiFazio and Atkinson, 2005). Some fractures may be splinted to immobilize and protect the fractured (or suspected fractured) extremity (see Research Focus box), and pain management is initiated with nonsteroidal antiinflammatory drugs (NSAIDs) such as ibuprofen, oxycodone, or acetaminophen with codeine (Friday, Kanegaye, McCaslin, et al, 2009; Koller, Myers, Lorenz, et al, 2007). In one study ibuprofen was as effective as acetaminophen with codeine for the treatment of musculoskeletal trauma in children (Clark, Plint, Correll, et al, 2007), whereas another study reported no difference among these agents in reducing pain in a group of children with fractures (Drendel, Lyon, Bergholte, et al, 2006).
In children the bone fragments are usually realigned and immobilized by traction or by closed manipulation and casting until adequate callus is formed. Internal and external fixation is also used. Weight bearing and active movement for the purpose of regaining function can begin after the fracture site is stable. The child’s natural tendency to be active is usually sufficient to restore normal mobility, and physical therapy is usually required only with more complex traumatic injuries. Open reduction is seldom required and is limited to fractures that cannot be maintained by conservative methods and cases in which there is interposed tissue or injury to arteries or nerves, such as in a motor vehicle accident or other major trauma. In the majority of cases children’s fractures can be managed by closed reduction and immobilization with plaster or fiberglass; this is often done on an outpatient basis with reevaluation in 7 to 10 days.
For many fractures closed reduction may be carried out in the emergency department with administration of procedural sedation drugs such as midazolam (Versed), fentanyl (Sublimaze), and morphine (Cimpello, Khine, and Avner, 2004); a local or regional nerve block; fentanyl and midazolam; ketamine (Ketalar) and midazolam; or a combination of nitrous oxide and local or regional anesthesia (Kennedy, Luhmann, and Luhmann, 2004). Etomidate is a rapid-acting sedative that induces unconsciousness and is cleared rapidly from the system. This hypnotic drug may be used for procedural sedation; however, it does not have analgesic properties (Meredith, O’Keefe, and Galwankar, 2008). With any fracture appropriate pain management should be implemented in all children. Studies have shown that historically children have been inadequately treated for pain during procedures in the emergency department and pain scores have been underused (Brown, Klein, Lewis, et al, 2003).
Children are most frequently hospitalized for fractures of the femur and the supracondylar area of the distal humerus. If simple reduction cannot be achieved or a neurovascular problem is detected after injury, observation in a hospital unit is indicated. Severe contusions with profound swelling cannot be treated with a cast, which would act as a tourniquet on the extremity, and badly malaligned fractures may require traction for a time before a cast is applied. The trend, however, is to avoid hospitalization. Some malaligned fractures respond to treatment with external pinning and traction or, more commonly, the use of an Ilizarov external fixator (see p. 1650). Several factors determine the method of fracture reduction (Box 39-5).
Medical interventions to manage a fracture injury involve the physician, the nurse, and the family (Box 39-6). Specific interventions and nursing responsibilities associated with the care of a child with a fracture are discussed later in the chapter.
Bone Healing and Remodeling
Bone healing follows a patterned sequence. Fig. 39-18 shows three broad overlapping phases: inflammatory, restorative, and remodeling. Bone healing can be described more definitively in terms of five stages (Table 39-2). When the bone breaks, the envelope of subcutaneous tissue, muscle, and periosteal tissue surrounding the site is torn, blood vessels rupture, and a hematoma forms. The ends of the fractured bone segments, deprived of circulation, die as far back as the nearest collateral circulation. Necrotic tissue accumulates, and an inflammatory response takes place at the site, with its characteristic vasodilation, plasma exudation, and edema. The organization and reabsorption of the hematoma proceeds, and the restorative phase begins with the reestablishment of local circulation. Repair requires an adequate blood supply and immobilization of the fracture fragments.
TABLE 39-2
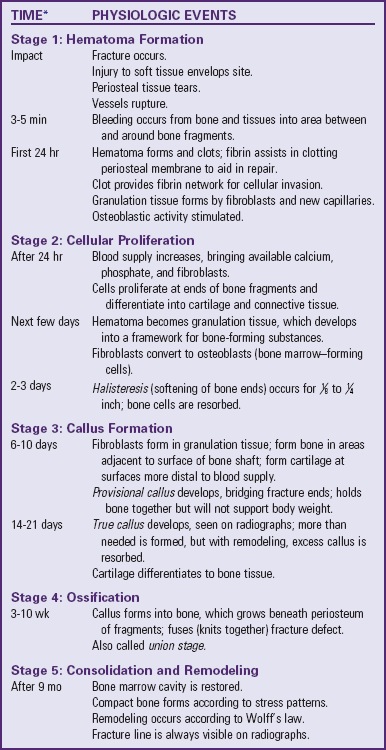
*Healing time more rapid in infants and in cancellous (spongy) bone; may be delayed if complications occur.
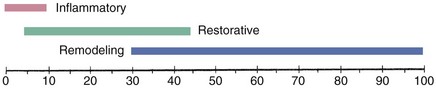
Fig. 39-18 Approximate time spent in inflammatory, restorative, and remodeling phases of bone healing. Scale indicates percentage of healing time.
When there is a break in the continuity of bone, the periosteal and intraosseous osteoblasts are in some way stimulated to maximum activity. New osteoblasts are formed in immense numbers almost immediately after the injury and begin building a bridge, as evidenced by a bulging growth of osteoblastic tissue and new bone matrix between the fractured bone fragments. This is followed by deposition of calcium salts to form callus, which provides stability (Fig. 39-19, B).
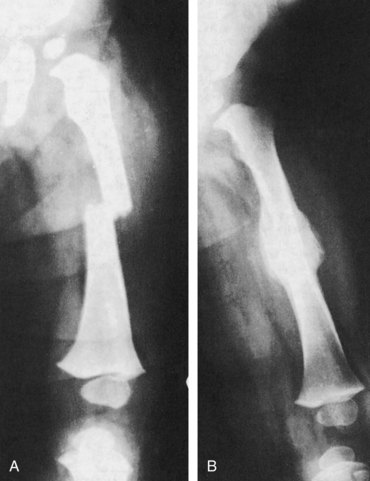
Fig. 39-19 Fractured femur. Most fractured femurs in childhood are of the spiral type shown here. Note comparison of A, original x-ray film, with B, 6-month postfracture film showing callus formation. (Courtesy Henrietta Egleston Hospital for Children, Atlanta. From Hilt NE, Schmitt EW: Pediatric orthopedic nursing, St Louis, 1975, Mosby.)
Bone healing is characteristically rapid in children because of the thickened periosteum and generous blood supply. In the young child, for example, there is frequently a solid union of the femoral shaft in 3 to 4 weeks, whereas in the adult, callus sufficient to avoid deformities from the constant muscle contraction associated with movement may not form in fewer than 10 to 16 weeks. The approximate healing times for a femoral shaft fracture are as follows:
Remodeling is a unique process that occurs in the healing of long bone fractures before epiphyseal closure. When a bone remodels, the irregularities produced by the fracture become indistinct because hollows are filled in and angles are rounded off in the healing process, which gives the bone a straighter appearance. It does not alter the alignment of the bone. The buildup of new bone or callus restores a portion of the normal bone structure in most cases despite observable malalignment. The younger the child and the closer the proximity of the fracture to the growth plate, the more likely that spontaneous correction will take place. In some instances a 90-degree angle will straighten in a year, but rotational deformities do not correct themselves. Various factors such as the type and location of the fracture, the child’s age, and the amount of fragment angulation or rotation influence the degree of correction in alignment that can be obtained by remodeling.
The position of the bone fragments in relation to one another influences the rapidity of healing and the residual deformity. For example, a gap between fragments delays (or prevents) healing (Fig. 39-20, A). Healing is prompt and complete with end-to-end apposition (Fig. 39-20, B), but the fracture stimulates accelerated growth of the neighboring epiphysis, which causes bony overgrowth and increased length of the extremity. Angulation deformity caused by an incomplete fracture (Fig. 39-20, C) may remodel in the young child, but the degree of residual deformity depends on the relationship of the angulation of the bone fragments to the angle of the joint. This requires careful evaluation and reduction to prevent permanent deformity.
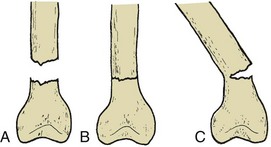
Fig. 39-20 Relationships of fracture fragments. A, Gap between fragments. B, End-to-end apposition. C, Angulation of incomplete fracture.
Wolff’s law is applied in treating children with orthopedic problems. Paraphrased, it states that bone will grow in the direction in which stress is placed on it. Examples of the use of this law are the hip spica cast with an abduction bar for treating developmental hip dysplasias and application of casts or traction at a selected angle to influence the direction of bone healing.
Bone healing in any age-group is greatly influenced by the traumatized person’s general health. The child with a fracture requires adequate nutrition for optimum bone healing. When nutritional intake is insufficient, vitamin and mineral supplementation may be necessary. No special dietary changes need to be made except to correct any existing nutritional deficiencies. Monitoring for fluid and electrolyte balance, renal function, and possible anemia is equally important to promote the child’s wellness.
The Child in a Cast
The completeness of the fracture, the type of bone involved, and the amount of weight that can be placed on the limb influence how much of an extremity must be included in a cast to immobilize the fracture site completely. In most situations the joints above and below the fracture are immobilized to eliminate the possibility of movement that might cause displacement at the fracture site. Three major types of cast are used for immobilization of fractures: upper extremity to immobilize the wrist or elbow, lower extremity to immobilize the ankle or knee, and spica to immobilize the hip and knee (Fig. 39-21). Fig. 39-22 shows a full spica cast with a hip abductor, and Fig. 39-23 shows a single spica cast.

Fig. 39-23 Single spica cast. Note diaper to maintain dryness. (Courtesy Texas Children’s Hospital, Houston.)
The Cast
Casting Materials: Casts are constructed from gauze strips and bandages impregnated with plaster of Paris or synthetic lighter-weight, water-resistant materials (e.g., fiberglass and polyurethane resin). The lightweight casts are being used more often for casting in children. They are available in colors and prints. Plaster casts are usually reserved for situations that require close conformity, such as “total contact” casting for wounds or small, irregularly shaped areas such as the hand. Table 39-3 compares the relative merits of plaster and synthetic casts.
Cast Application: A nurse may assist in cast application by holding the extremity in alignment. Special cast tables that hold the child’s body are used for applying large hip spica casts.
Consider the child’s developmental age before the cast is applied. For preschoolers who fear bodily harm and fantasize the loss of an extremity, use a plastic doll or stuffed animal to explain the procedure beforehand. Toddlers and preschoolers do not have easily defined body boundaries. If an extremity is wrapped in a bandage, cast, or splint, to the young child the extremity ceases to exist. Explain to the child that some synthetic cast material will become warm but will not burn. During the application of the cast, use various distraction methods, including discussing favorite pets or activities at school and blowing bubbles. In this age-group explanations such as “This will help your arm get better” are futile because the child has no concept of causality.
Before the cast is applied, check the extremities for any abrasions, cuts, or other alterations in the skin surface and for the presence of rings or other items that might cause constriction with swelling; such objects are removed.
To apply a plaster cast, a tube of stockinette is stretched over the area to be casted, and bony prominences are padded with soft cotton sheeting. Some practitioners use a special plastic material or Gore-Tex under a spica cast to prevent skin breakdown. Dry rolls of gauze impregnated with plaster of Paris are immersed in a pail of tepid water with the open end of the roll angled downward to allow soaking of the bandage. The wet plaster rolls are applied in bandage fashion and molded to the extremity. A heat-producing chemical reaction occurs between the plaster and water as the plaster becomes a crystalline gypsum. During application of the cast, the underlying stockinette is pulled over the raw edges of the cast and secured with a layer of wet plaster 1 to 2.5 cm (0.5 to 1 inch) below the rim to form a smooth, padded edge to protect the skin.
If the operator does not form such a protective edge with the stockinette, the raw edges of the cast can be protected by creating a “petaled” edge. Small pieces approximately 5 to 7.5 cm (2 to 3 inches) long are cut from moleskin or adhesive tape 2.5 to 4 cm (1 to 1.5 inches) wide. The edges are rounded with scissors, and the individual “petals” are placed over the edge of the cast, with each petal slightly overlapping the previous one to form a smooth, neat edge. It is easier to apply the petal to the underside of the cast first and then bring the unadhered edge to the front, pressing firmly so the edges remain securely attached. Adhesive strip bandages can be used instead of tape petals for quicker preparation and a slightly padded cast edge.
Nursing Care Management
The complete evaporation of the water from a hip spica cast can take 24 to 48 hours when plaster materials are used. Drying occurs within minutes with fiberglass materials. The cast must remain uncovered to allow it to dry from the inside out. Turning the child in a plaster cast at least every 2 hours will help to dry a body cast evenly and prevent complications related to immobility. Use of a regular fan or a hair dryer on the cool setting to circulate air may be helpful when the humidity is high.
Handle a wet plaster cast using the palms of the hands to avoid indenting the cast and creating pressure areas, and support it with a pillow covered with plastic. A dry plaster of Paris cast produces a hollow sound when tapped with the finger.
During the first few hours after a cast is applied, the chief concern is that the extremity may continue to swell to the extent that the cast becomes a tourniquet, shutting off circulation and producing neurovascular complications. One measure to reduce the likelihood of this problem is to elevate the body part and thereby increase venous return. If edema is excessive, casts are bivalved (i.e., cut to make anterior and posterior halves that are held together with an elastic bandage). The cast and the involved extremity are observed frequently to assess neurovascular integrity and detect any signs of compromise. Within 6 to 8 hours permanent muscle and tissue damage can occur, for which nurses can be held liable. Once the cast has dried, “hot spots” felt on the cast surface or foul-smelling areas of the cast may indicate infection underneath and should be further evaluated. Often the cast is windowed over the area of suspicion to directly observe and treat the area if necessary.
When a cast is applied to an extremity that has sustained an open fracture, a window is often left over the wound area to allow for observation and dressing of the wound.
Usually the child is discharged to home care after a cast is applied in the emergency department or clinic. Parents need instructions on drying and caring for the cast and checking for signs and symptoms that indicate the cast is too tight (see Family-Centered Care box). They should also know to take the child to the health care professional for attention if the cast becomes too loose, since a loose cast no longer serves its purpose. A cast may represent a badge of honor for the child and serves as visible evidence of an otherwise invisible injury.
Cast Removal: Cutting the cast to remove it or to relieve tightness is frequently a frightening experience for children. They fear the sound of the cast cutter and are terrified that their flesh, as well as the cast, will be cut. Because it works by vibration, a cast cutter cuts only the hard surface of the cast. This can be demonstrated by the person removing the cast. The oscillating blade vibrates back and forth very rapidly and will not cut when placed lightly on the skin. Children have described it as producing a “tickly” sensation. The vibration also generates heat that the child may feel. Explain both of these sensations to the child.
Preparation for the procedure helps reduce anxiety, especially if the nurse has established a trusting relationship with the child. Many young children come to regard the cast as part of themselves, which intensifies their fear of removal (Fig. 39-24). They need continual reassurance that all is going well and that their behavior is accepted.

Fig. 39-24 Young children come to regard a cast as part of their body. They usually adapt well but may fear its removal.
Home care of children in casts can create problems, especially with large casts (e.g., a hip spica cast). Common situations (e.g., returning the child home safely and comfortably) become problematic. Standard seat belts and car seats are not readily adapted for use by children in casts. (See Developmental Dysplasia of the Hip, Chapter 11.) Sitting can be impossible in a spica cast, and leg casts require extra space in a small room, under a table, and in a bathroom. Children in spica casts may experience difficulty with feeding, and the bed or wheelchair may need to be elevated for feeding; alternatively, they may manage a semisitting position in bed or in a wheelchair (see Figs. 39-22 and 39-23). Use of a conventional toilet is almost impossible for a child in a spica cast. Small bedpans or other containers offer alternatives for elimination. The use of a Gore-Tex pantaloon, a protective skin barrier, and absorbent pads is a way of reducing urine burns and heat rash and improving hygiene with a hip spica cast.
Nurses can help families adapt the child’s environment to accommodate the temporary encumbrance of a cast (e.g., devise plastic wraps for waterproofing casts for a shower). Baths are possible only if the plaster cast is kept out of the water and covered to prevent it from becoming wet from splashes. Some synthetic casts are waterproof, but skin can become irritated if water collects beneath the cast.
After the cast is removed, the skin surface is caked with desquamated skin and sebaceous secretions. Simple soaking in a bathtub is usually sufficient for their removal, but it may take several days to completely eliminate accumulation. The parents and child should not pull or forcibly remove this material with vigorous scrubbing, since this may cause excoriation and bleeding.
The Child in Traction
When bone fragments cannot be reduced with simple traction and stabilization with a cast, the extended pulling force obtained with continuous traction may be required. Traction is also used for other purposes (Box 39-7).
With the increased emphasis on outpatient treatment of acute and chronic illnesses to cut health care costs, developmental and social considerations, immobilization problems, and newer surgical techniques, traction is used with decreasing frequency. Skeletal fixation (internal or external) and early ambulation of the child have replaced the use of traction in many instances.
Purposes of Traction
When two forces of given direction and magnitude act on an object at the same point simultaneously from opposite directions, the object either changes its state of rest or motion or remains in equilibrium. The use of traction in the management of fractures is the direct application of such forces to produce equilibrium at the fracture site. A forward force (traction) is produced by attaching weight to the distal bone fragment. This force is balanced by the backward force of the muscle pull (countertraction) and the frictional force between the patient and the bed (Fig. 39-25).
To reduce or realign a fracture site, traction is provided by weights applied to the distal bone fragment; body weight provides countertraction. By adjusting the line of pull upward or downward or by adducting or abducting the extremity, the operator uses these forces to align the distal and proximal bone fragments. To attain equilibrium, the amount of forward force is adjusted by adding weight to or subtracting weight from the traction, or countertraction is increased by elevating the foot of the bed to create a greater gravitational pull in the backward force.
The three primary purposes of traction for reduction of fractures are:
1. To fatigue the involved muscle and reduce muscle spasm so that bones can be realigned
2. To position the distal and proximal bone ends in the desired realignment to promote satisfactory bone healing
3. To immobilize the fracture site until realignment has been achieved and sufficient healing has taken place to permit casting or splinting
In some cases traction may be used to treat a pathologic joint condition such as developmental hip dysplasia. The muscle is fatigued by applying constant stress to the muscle so that the buildup of lactic acid will produce muscle relaxation. The all-or-none law, which characterizes muscle contractility, applies to muscle relaxation as well. When the muscle is stretched, muscle spasm ceases, which permits the realignment of the bone ends. The continuous maintenance of traction is important during this phase, since releasing the traction allows the muscle to contract normally and again cause malpositioning of the bone ends.
The realignment of the bone fragments is a gradual process that is achieved more rapidly in infants, who have limited muscle tone, than in muscular teenagers. The line of pull and callus formation are checked periodically by radiographic examination. The traction pull to some degree immobilizes the fracture site; however, adjunct immobilizing devices such as splints or casts are sometimes used with skeletal traction. In injuries in which there is severe soft tissue swelling or vascular and nerve damage, it is customary to use traction until these complications have been resolved and it is safe to apply a cast. Immobilization with traction is maintained until the bone ends are in satisfactory realignment, after which a less-confining type of immobilization, usually a cast, is applied.
Types of Traction (General)
The two main types of traction are skin traction and skeletal traction. The pull needed for traction can be applied to the distal bone fragment in several ways (Box 39-8). The type of traction applied is determined primarily by the child’s age, the condition of the soft tissues, and the type and degree of displacement of the fracture. Fractures most commonly treated by application of traction are those involving the humerus, femur, and vertebrae.
Upper extremity traction is rarely used because of the urgency in management. Fractures of the humerus, which are usually the result of a fall with the arm in extension, frequently involve the supracondylar portion. Three major complications are associated with this injury: Volkmann contractures (p. 1651); traumatic injury to the median, ulnar, or radial nerve; and angulation deformities. The fracture must be carefully reduced with the child sedated or under anesthesia. Because of the danger of complications, children with closed reduction of supracondylar fractures are often hospitalized for observation.
In cases of upper extremity fracture the child is sedated, and treatment by closed reduction is attempted in the emergency department. Closed reduction with percutaneous pinning or open reduction with internal fixation is performed in the operating room as indicated.
The common site for a femoral fracture is the middle one third of the shaft (see Fig. 39-19, A). With such a fracture there is significant overriding but minimal displacement. In a fracture in the lower one third of the shaft, the pull of the gastrocnemius muscle causes the distal fragment to become downwardly displaced. The severity of the fracturing force and the ability of the muscles to hold the fracture out of alignment determine the fracture type and the amount of overriding of the fragments. The periosteum may remain intact, which helps maintain alignment.
Buck extension traction is a type of skin traction applied with the legs in an extended position (Fig. 39-26). Buck extension traction is used primarily for short-term immobilization, such as preoperative management of a child with a dislocated hip, or for correction of contractures or bone deformities, such as in Legg-Calvé-Perthes disease. A side-lying position may be permissible if the leg is stable.
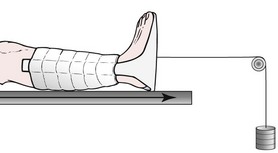
Fig. 39-26 Buck traction. (From Lewis SL, Heitkemper MM, Dirksen S, et al, editors: Medical-surgical nursing: assessment and management of clinical problems, ed 7, St Louis, 2007, Mosby.)
Russell traction uses skin traction on the lower leg and a padded sling under the knee. Two lines of pull, one along the longitudinal axis of the lower leg and one perpendicular to the leg, are produced. This combination of pulls allows realignment of the lower extremity and immobilizes the hip and knee in a flexed position. The hip flexion must remain at the prescribed angle to prevent fracture malalignment, since there is no direct support under the fracture and the skin traction may slip. Because the traction is set up to have two ropes pulling in the same direction at the foot plate, the traction pull is twice the amount of weight at the end of the bed.
A common skeletal traction is 90-degree–90-degree traction (90-90 traction). The lower leg is put in a boot cast or supported in a sling, and a skeletal Steinmann pin or Kirschner wire is placed in the distal fragment of the femur. From a nursing standpoint, this type of traction facilitates position changes, toileting, and prevention of traction complications. This traction also:
• Achieves the desired line of pull for reducing the fracture by means of the skeletal traction
• Allows a 90-degree flexion of both the hip and the knee
• Supports the lower extremity in a desired position with good venous return
Balanced suspension traction may be used with or without skin or skeletal traction. Unless it is combined with another type of traction, balanced suspension traction merely holds the leg in a desired flexed position to relax the hip and hamstring muscles and does not exert any traction directly on a body part. A Thomas splint extends from the thigh to midair above the foot, and a Pearson attachment supports the lower leg. Towels or pieces of felt covered with stockinette are clipped or pinned to the splints for leg support. Ropes are attached to create a balanced traction. When the child is lifted from the bed, the traction lifts as well, with no loss of alignment (see Fig. 39-3).
The Pearson attachment stays wherever it is positioned. Many times the practitioner puts a rope between the end of the Pearson attachment and the end of the Thomas splint to prevent any alteration in knee flexion when the child is moved. This type of traction requires very careful checking of splints and ropes to make certain that no slippage or fraying has occurred. This mode of traction is of great value when lifting the older and heavier child for care.
The cervical area is a vulnerable site for flexion or extension injuries to muscles, vertebrae, or the spinal cord. Cervical muscle trauma without other complications is treated with a cervical soft or hard collar to relieve the weight of the head on the fracture site. Intermittent cervical skin traction using a head halter and weight might be employed to decrease muscle spasms. Injuries limited to cervical muscles can be uncomfortable but, with prompt medical care, usually resolve with conservative treatment.
When a child’s cervical vertebra is displaced or fractured, the site must be reduced and immobilized with cervical skeletal traction. The spinal cord runs through the intravertebral canal, and dislocation or fracture of the vertebrae can also cause spinal cord trauma. Physical examination, especially a neurologic assessment, and radiographic studies are essential diagnostic aids to determine:
• The presence of a vertebral fracture
• The degree of vertebral dislocation
• Displacement of an intervertebral disk
• Compression of the spinal cord and other neurologic structures
Cervical traction may be accomplished with halo ring traction, a halo vest (Fig. 39-27, A), or Gardner-Wells tongs (Fig. 39-27, B) (Fisher, Williams, and Levine, 2008). Gardner-Wells tongs are spring loaded, so making burr holes and shaving hair are not required; a local anesthetic may be used during application. The head is placed in a hyperextended position, and, as the neck muscles fatigue with constant traction pull, the vertebral bodies gradually are pulled apart and the cord is no longer pinched between the vertebrae. Immobilization until fracture healing can occur is an essential goal of cervical traction. If the injury has been limited to a vertebral fracture without neurologic deficit, a halo vest permits earlier ambulation (see Fig. 39-27, A). Halo vest devices are also used preoperatively and postoperatively to stabilize the cervical spine.
Nursing Care Management
To assess the child in traction, it is essential to know the purpose for which the traction is being applied. Regular assessment of both the child and the traction apparatus is required (see Nursing Care Guidelines box). The nurse also assesses the child for evidence of adverse effects of immobilization (see pp. 1624-1629).
Evaluating the therapeutic effects and possible negative consequences of traction is essential to good patient care. Many of the nursing problems associated with traction in a child are related to immobility. However, a number of physical needs related to traction require attention and vigilance.
In addition to routine skin observation and care (see The Immobilized Child, p. 1623), children in skeletal traction need special skin care at the pin site according to hospital policy or practitioner preference. In a review of pin site care in children and adults, it was concluded that pin sites should be frequently assessed and cleaned to prevent infection; after the first 48 to 72 hours pin site care may be performed once daily or weekly for mechanically stable pins (Holmes, Brown, and Pin Site Care Expert Panel, 2005). Use of a 2 mg/ml chlorhexidine solution has been proposed as best-practice care for skeletal pin sites by the National Association of Orthopaedic Nurses (Holmes, Brown, and Pin Site Care Expert Panel, 2005). Before the child’s discharge, teach parents and family pin site care, including how to observe for infection or pin instability, using a return demonstration method (Holmes, Brown, and Pin Site Care Expert Panel, 2005). A pressure reduction device, such as a foam overlay or an alternating-pressure mattress placed beneath the hips and back, reduces the chance of skin breakdown in these vulnerable areas.
When the child is first placed in traction, discomfort commonly increases because the traction pull fatigues the muscle. Muscle relaxants may be administered for muscle spasms. Orthopedic conditions are associated with a higher-than-average number of painful events and a higher percentage of bodily symptoms than other common conditions. Analgesics, including opioids, and muscle relaxants help during this phase of care and should be administered liberally.
Helping children cope with the confinement and new experience requires more than medications. Give an explanation about what is happening and why the child must remain in the device according to each child’s level of development. Reassure children that someone will always be available to aid them in adjusting to the traction and coping with the problems of immobilization.
Some devices assist children in performing activities independently. An overhead trapeze, which children can use to help lift themselves, facilitates hygiene and repositioning and provides exercise for uninvolved muscles. Encourage the child to move in bed as much as possible while maintaining the primary function of the device. Encourage active range of motion on unaffected joints and extremities and frequent repositioning.
Later, when traction is released, muscle spasms can be quite severe. Pain assessment and pain management should be a part of care at this phase. (See Chapter 7.)
Distraction
Unlike traction, which helps bones realign and fuse properly, distraction is the process of separating opposing bone to encourage generation of new bone in the created space. Distraction can be used when limbs are of unequal lengths and new bone is needed to elongate the shorter limb.
External Fixation
The Ilizarov external fixator (Fig. 39-28) is the most common external fixation device. It uses a system of wires, rings, and telescoping rods that permits limb lengthening to occur by manual distraction. In addition to lengthening bones, the device can be used to correct angular or rotational defects or to immobilize fractures. It allows earlier mobilization and earlier hospital discharge, and it obviates the need for traction. The device is attached surgically by securing a series of external full or half rings to the bone with wires. External telescoping rods connect the rings to each other. Manual distraction is accomplished by manipulating the rods to increase the distance between the rings. A percutaneous osteotomy is performed when the device is applied to create a false growth plate. In a special osteotomy or corticotomy, only the cortex of the bone is cut, and its blood supply, bone marrow, endosteum, and periosteum are preserved. Capillary blood flow to the transected area is essential for proper bone growth. Cut bone ends typically grow at a rate of 1 cm (0.4 inch) per month. Use of the external fixator can result in a gain in length of up to 15 cm (5.9 inches).

Fig. 39-28 Child with Ilizarov external fixator (on right leg) during physical therapy on parallel bars.
Other types of external fixation are used in the management of certain types of fractures—for example, fracture of a distal radius or a tibia in an adolescent. Mandibular distraction may be used within external fixation for Pierre Robin sequence. (See Chapter 11.)
Nursing Care Management
Successful use of external fixation depends on the child’s and family’s cooperation; therefore, before surgery, they must be fully informed about the appearance of the device, the way it accomplishes bone growth, required alterations in activities, and home and follow-up care. Children are involved in learning to adjust the device to accomplish distraction. Children who participate actively in their own care report less discomfort. With lower extremity fixation such as an Ilizarov fixator, partial weight bearing is allowed, and the child needs to learn to walk with crutches. Alterations in activity include modifications at school and in physical education. Full weight bearing is not allowed until the distraction is completed and bone consolidation has occurred. Instruct parents in pin care, including observation for infection and loosening of pins. Follow-up care is essential to maintain appropriate distraction until the desired leg length is achieved. The child may need to use crutches or have a cast for 4 to 6 weeks after removal of the device.
Internal Fixation
Internal fixation methods require surgery and include screw and plate fixation and intramedullary fixation. When surgical intervention is necessary to realign a fracture, the child needs physical and psychologic preparation. The preoperative teaching is the same as for any other surgical procedure, except that orthopedic surgery uses a variety of rods, screws, staples, and plates, and the child and family need to know that these objects will allow proper bone growth and repair to occur. The fixating devices are made of substances that do not act as proteins foreign to the body and therefore are not rejected.
Usually rods are driven down the shaft of the long bones, whereas screws and plates are attached to the sides of the bone shaft. Postoperatively the bone healing takes place with callus formation, as it does in a new fracture. Generally, after placement of an internal fixation device, the child sits in a chair and walks with a walker or crutches within a few hours or days. The most common postoperative complication is infection. The nurse’s responsibility includes close monitoring of neurovascular changes in the involved extremity and the prevention of postanesthesia problems. Alert the family to signs of infection and instruct them regarding appropriate weight-bearing and activity plans. Occasionally, supplemental casting or bracing is needed.
Fracture Complications
![]() If the trauma or immobilizing device restricts blood flow in veins or arteries of the affected extremity, bone healing will be seriously impaired. Careful assessment of the pulses, capillary refill, skin color, and temperature is an important nursing responsibility. After injury, swelling of tissues occurs more rapidly in the child than in the adult. In the upper extremity, brachial, radial, ulnar, and digital pulses are felt. In the leg, femoral, popliteal, posterior tibial, and dorsalis pedis pulses are checked.
If the trauma or immobilizing device restricts blood flow in veins or arteries of the affected extremity, bone healing will be seriously impaired. Careful assessment of the pulses, capillary refill, skin color, and temperature is an important nursing responsibility. After injury, swelling of tissues occurs more rapidly in the child than in the adult. In the upper extremity, brachial, radial, ulnar, and digital pulses are felt. In the leg, femoral, popliteal, posterior tibial, and dorsalis pedis pulses are checked.
![]() Skill—Monitoring Neurovascular Status
Skill—Monitoring Neurovascular Status
Closely associated with an inadequate blood supply is a low hematocrit value, which can result from the initial blood loss or surgically induced anemia. Although the blood flow may be adequate, a lowered amount of hemoglobin will not provide a sufficient supply of oxygen for tissue repair.
Nerve Compression Syndromes
Nerve damage can occur at the time of injury, develop in the process of realignment, or arise as a complication of use of an immobilizing apparatus. The syndromes are classified according to the anatomic area affected and can involve the median nerve (carpal tunnel syndrome), ulnar nerve (at wrist or elbow), radial nerve, posterior tibial nerve (tarsal tunnel syndrome), common peroneal nerve, or sciatic nerve. Peroneal nerve damage can result in footdrop, and radial nerve impairment produces wristdrop. Both these disabilities can significantly interfere with activities of daily living.
Sensory testing with touch and pinprick and evaluation of motor strength by asking the child to move the unaffected joint distal to the injury are common means of determining neurologic involvement. Subjective symptoms are pain or discomfort, muscular weakness, a burning sensation, limitation of motion, and altered sensation. Because the fear of pain limits the child’s cooperation, play can be the nurse’s most valuable tool.
Treatment is alleviation of pressure on the nerve. The practitioner determines whether correcting the alignment will alleviate pressure on the nerve or whether surgical intervention is necessary. At times sensory or motor changes indicate ischemia, and the treatment is correction of the vascular disturbance.
Compartment Syndromes
A compartment is a group of muscles surrounded by tough, inelastic fascial tissue. Compartment syndrome occurs when pressure within this closed space increases and compromises circulation to the muscles and nerves within the space. Muscles and nerves of both upper and lower extremities are enclosed within such compartments. The most frequent causes of compartment syndrome are tight dressings or casts, skin traction, hemorrhage, trauma, burns, and surgery. Other causes include an increase in compartment contents (hemorrhage, venous obstruction, infiltrated IV infusion, exudate) and externally applied pressure, such as lying on the affected limb. Intraarterial medication administration through an arterial line and prolonged operation time may also contribute to compartment syndrome (Green and Swiontkowski, 2008).
Signs and symptoms of compartment syndrome reflect a deficit in or deterioration of neuromuscular status in the anatomic area surrounding the involved structures. These include motor weakness and pain that is out of proportion to the injury and requires opioids for control (Lucas and Davis, 2005). Clinical manifestations may be difficult to recognize in small children or in those who have a head injury. A palpable peripheral pulse and brisk capillary refill may be present despite increasing compartmental pressure. Sensory deficit in the affected limb is reported to be the most reliable physical finding in compartment syndrome (Green and Swiontkowski, 2008). Clinical manifestations of compartment syndrome may occur as early as 30 minutes after the ischemia develops. Tenseness may be noted on palpation of the area. Because early detection is important in preventing permanent damage to tissues, in certain high-risk situations specialists may recommend continuous monitoring of compartment pressures by way of a small, slit-tip catheter; Wick catheter; or needle inserted into the compartment. Treatment of compartment syndrome is immediate relief of pressure, which sometimes requires fasciotomy.
Volkmann contracture (ischemic muscular atrophy) is a serious, persistent flexion contraction of the forearm and hand caused by massive infarction of muscle. Pressure caused by a cast or tight bandage or by swelling from the injury in the area of the elbow begins with arterial occlusion and then progresses to muscle anoxia and reflex vasospasms. Finally, the lack of blood supply leads to muscle necrosis and replacement with fibrous tissue, which produces paralysis and a clawlike hand contracture. Any fracture that requires excessive traction can be complicated by Volkmann contracture; however, it occurs most often in the elbow.
The neuromuscular symptoms are severe pain (although pain is not always a manifestation), pallor or cyanosis, edema, absence of pulses in the extremity, and loss of sensitivity. Unrelieved, the occlusive hypoxic process can cause some contracture if ischemia lasts as little as 6 hours. A great deal of muscle damage occurs after 12 to 24 hours; 48 hours of ischemia produces severe deformity, with muscle fibrosis and contractures in 5 to 10 days. If not treated, the contracture leads to severe deformity and paralysis.
The immediate treatment is to remove any mechanically obstructive materials, such as tight bandages, and extend the joint to free blood vessels. If the symptoms do not improve within a few hours, arteriography is done in anticipation of a possible need for surgical intervention (fasciotomy) to decrease arterial spasms and to improve the blood supply by separation of the fascial sheaths of the involved muscles. Elevation of the affected extremity is not recommended and may further decrease blood flow to the area (Green and Swiontkowski, 2008).