Health Problems of Middle Childhood
Systemic Disorders Related to Skin Lesions
Skin Disorders Related to Chemical or Physical Contacts
Skin Disorders Related to Drug Sensitivity
http://evolve.elsevier.com/wong/ncic
Acne, Ch. 20
Autism, Ch. 24
Birthmarks, Ch. 9
Bullous Impetigo, Ch. 9
Burns, Ch. 29
Candidiasis, Ch. 9
Communicable Diseases, Ch. 16
Dental Health: Infant, Ch. 12; Toddler, Ch. 14; Preschooler, Ch. 15; School-Age Child, Ch. 17
Maintaining Healthy Skin, Ch. 27
Pain Assessment; Pain Management, Ch. 7
Physical Assessment (Newborn), Ch. 8
Physical Examination: Skin, Ch. 6
Preparation for Diagnostic and Therapeutic Procedures, Ch. 27
Restraining Methods and Therapeutic Holding, Ch. 27
Sexually Transmitted Infections, Ch. 20
Skin Disorders (Infancy), Ch. 13
Suicide, Ch. 21
Disorders Affecting the Skin
Skin of Younger Children
The major skin layers arise from different embryologic origins. Early in the embryonic period, a single layer of epithelium forms from the ectoderm, while simultaneously the corium develops from the mesenchyme. In the infant and small child the epidermis is still loosely bound to the dermis, partly because the rete pegs are flat. This poor adherence causes the layers to separate readily and form blisters during an inflammatory process. This is especially true in preterm infants, who have an even greater propensity to blister formation and separation during careless handling (such as removal of adhesive tape). The skin is thinner than in older children, and the cells of all strata are more compressed.
Several characteristics influence skin responses in infants and young children. Their skin is far more susceptible to superficial bacterial infection compared with older children and adults. They are more likely to have associated systemic symptoms with some infections and are more apt to react to a primary irritant than to a sensitizing allergen. Infants and young children are more frequently affected by chronic atopic dermatitis (eczema). The infant’s skin is much more prone to develop a toxic erythema as a result of skin eruptions or drug reactions and is subject to maceration, infection, and the moisture retention associated with diaper rash.
Lesions of the skin can result from a variety of etiologic factors. In general, skin lesions originate from (1) contact with injurious agents such as infectious organisms, toxic chemicals, and physical trauma; (2) hereditary factors; (3) an external factor that produces a reaction in the skin (e.g., allergens); or (4) a systemic disease in which the lesions are a cutaneous manifestation (e.g., measles, lupus erythematosus, nutritional deficiency diseases). Responses are highly individual. An agent that may be harmless to one individual may be damaging to another, and a single agent may produce various types of responses in different individuals.
Another factor involved in the etiology of skin manifestations is the child’s age. For example, infants are subject to “birthmark” malformations and atopic dermatitis that appear early in life, the school-age child is susceptible to ringworm of the scalp, and acne is a characteristic skin disorder of puberty. Contact dermatitis, such as that caused by poison ivy, occurs only where the noxious agent is touched. Similarly, insect bites are associated with life-cycle and seasonal activities. Tension and anxiety may produce, modify, or prolong many skin conditions, although this is less common in children.
Pathophysiology of Dermatitis
More than half of dermatologic problems are various forms of dermatitis. This implies a sequence of inflammatory changes in the skin that are grossly and microscopically similar but diverse in course and causation. Acute responses produce intercellular and intracellular edema, the formation of intradermal vesicles, and an initial minimum infiltration of inflammatory cells into the epidermis. In the dermis there is edema, vascular dilation, and early perivascular cellular infiltration. The location and manner of these reactions produce the lesions characteristic of each disorder. The changes are reversible, and the skin ordinarily recovers without blemish and completely intact unless complicating factors such as ulceration from the primary irritant, scratching, and infection are introduced or underlying vascular disease develops. In chronic conditions permanent effects are seen that vary according to the disorder, the general condition of the affected individual, and available therapy.
Clinical Manifestations and Diagnostic Evaluation
The following discussion first explores the history and symptoms, but also notes some objective findings simultaneously. One of the more advantageous aspects of skin lesions is that often the diagnosis is readily established after simple, careful inspection.
History and Symptoms: Many cutaneous lesions are associated with local symptoms, the most common of which is itching (pruritus) that varies in kind and intensity. Pain or tenderness often accompanies some skin lesions, and other sensations may be described as burning, prickling, stinging, or crawling. Alterations in local feeling or sensation include absence of sensation (anesthesia); excessive sensitiveness (hyperesthesia); diminished sensation (hypesthesia); and abnormal sensation, such as burning or prickling (paresthesia). These symptoms may remain localized or may migrate. They may also be constant or intermittent and may be aggravated by a specific activity or circumstance, such as exposure to sunlight.
Determining whether the child has had an allergic condition such as asthma or hay fever or has had previous skin disease is also important. Atopic dermatitis, often associated with allergies, frequently begins in infancy. It should be determined when the lesion or symptom first became apparent and whether it is related to ingestion of a food or other substance, including any medication the child might be taking. Keep in mind that the condition may be related to an activity such as contact with plants, insects, or chemicals.
Objective Findings: The skin lesion’s distribution, size, and morphologic characteristics provide significant information. The usual extrinsic causes are physical, chemical, or allergic irritants or infectious agents such as bacteria, fungi, viruses, or animal parasites. Intrinsic causes such as a specific infection (e.g., measles or chickenpox), drug sensitization, or other allergic phenomena can produce skin manifestations. Other diagnostic tools include medical and laboratory studies.
Laboratory Studies: When it is suspected that a skin problem might be related to a systemic disease, such as one of the collagen diseases or an immunodeficiency disease, studies are needed to rule out these possibilities. Diagnostic modalities include microscopic examination, cultures, skin scrapings or biopsy, cytodiagnosis, patch testing, and Wood light examination. Allergic skin testing and various other laboratory tests (blood count, sedimentation rate) are used when indicated.
Wounds
Wounds are structural or physiologic disruptions of the integument that call for normal or abnormal tissue repair responses. All wounds can be classified as acute or chronic. Acute wounds are those that heal uneventfully within the usual time frame. Chronic wounds are those that do not heal in the expected time frame or are associated with many complications. In children most wounds are acute and can be prevented from becoming chronic through appropriate nursing care. Wounds are classified in the same manner as burns: partial-thickness, full-thickness, and complex wounds that include muscle and/or bone. Wounds that often become chronic are burns and pressure ulcers, localized areas of cellular necrosis that develop when soft tissue is compressed between a bony prominence and a firm surface. (See Burns, Chapter 29, and Maintaining Healthy Skin, Chapter 27.)
Some types of acute wounds are the following:
Abrasion—Removal of the superficial layers of skin by rubbing or scraping
Avulsion—Forcible pulling out or extraction of tissue
Laceration—Torn or jagged wound; accidental cut wound
Incision—Division of the skin made with a sharp object; cut
Penetrating wound—Disruption of the skin surface that extends into underlying tissue or into a body cavity
Puncture—Wound with a relatively small opening compared with the depth
Process of Wound Healing
Epidermal Injuries: Abrasions are the most common epidermal wounds of childhood, usually in the form of a skinned knee or elbow. In most injuries the margins of the abraded area are superficial, involving only the outer layers of epidermis, although the central portion may extend into the dermis. Initially the defect is filled by a blood clot and necrotic debris, which subsequently dehydrate to form a scab. Epithelial tissue is composed of labile cells, which are constantly destroyed and replaced throughout life. Injury to these tissues results in regeneration (i.e., rapid replacement by similar cells).
The epithelial wound heals by migration and proliferation of epithelial cells from the wound margin and from cells surviving in transected skin appendages. This response begins within 24 to 48 hours after the wound is incurred. Cell migration ceases when migrating cells make contact with epithelial cells migrating from all other sites. Fixed basal cells adjacent to the wound edge and in skin appendages begin to divide rapidly to replace the migrated cells. As resurfacing is accomplished, the migrated cells begin to divide and thicken the new epithelial layer.
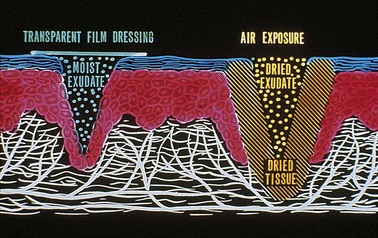
Epithelial cells advance over the wound surface by “flowing.” The first cell advances, anchors, and then moves no more. Instead, a cell from behind advances over it, anchors, and subsequently is overridden by other cells that advance over both of the primary cells—similar to a leapfrog movement. Epithelial cells move most rapidly in moist environments, such as when the wound is covered with a transparent or other occlusive-type dressing, and the rate of epithelialization depends on a variety of factors, particularly the amount of oxygen supplied to the wound. Allowing the skin to dry and form an eschar or crust (scab) impedes the migration of epithelial cells (Fig. 18-1). In addition, fluid may collect and infection may occur under the eschar.
Injury to Deeper Tissues: Tissues composed of permanent cells, such as muscle and some nerve cells, are unable to regenerate. Therefore these tissues repair themselves by substituting fibrous connective tissue for the injured tissue. This fibrous tissue, or scar, serves as a patch to preserve or restore the continuity of the tissue. Wounds involving permanent cells include surgical incisions, lacerations, ulcers, evulsions, and full-thickness burns. Injured cells of glandular organs and bones, composed of stable cells, multiply less vigorously and heal more slowly. (See Bone Healing and Remodeling, Chapter 39.) With some wounds an overgrowth of nerve endings may occur, resulting in allodynia, or the sensation of pain from normally nonpainful stimuli, such as light touch.
Mechanism of Wound Healing: The nonspecific repair mechanism of wound healing with scar formation involves the processes of inflammation, fibroplasia, scar contraction, and scar maturation. The initial response at the site of injury is inflammation, a vascular and cellular response that prepares the tissues for the subsequent repair process. There is a transient constriction of transected blood vessels, lasting 5 to 10 minutes, followed by active vasodilation of all local small vessels and increased blood flow to the area. This is accompanied by increased permeability of small venules, which allows plasma to leak into surrounding tissues (edema). A blood clot is formed along wound edges, providing a framework for future growth of capillaries (angiogenesis) and epithelial cells.
At the same time, vessel walls become lined with leukocytes, primarily neutrophils, which pass through the walls and concentrate at the injured site, where they ingest bacteria and debris (phagocytosis). Neutrophils are superseded by macrophages, which continue phagocytosis, and also by growth factors needed for skin repair and angiogenesis. Fibroblasts attracted to the area from blood vessels deposit fibrin throughout the clot. Adjacent capillaries begin to form buds that stretch across the supporting fibrin threads, and epithelial cells secrete a fibrolytic enzyme that allows their advancement across the wound. This initial phase of wound healing takes place during the first 3 to 5 days after injury. The wound is weakest at this time.
Fibroplasia (granulation or proliferation), the second phase of healing, lasts from 5 days to 4 weeks. Fibroblasts, immature connective tissue cells, migrate to the healing site and begin to secrete collagen into the meshwork spaces. Granulation tissue is highly vascular, “beefy” red, shiny connective tissue that organizes and restructures, forming thicker, stronger fibers arranged in orderly layers. A thin layer of epithelial tissue is regenerated over the surface of the wound, and leukocytes gradually disappear from the area. The wound is fragile at this time, and granulation tissue bleeds profusely if disturbed.
During contraction and maturation, the third and fourth phases of wound healing, collagen continues to be deposited and organized into layers, compressing the new blood vessels and gradually stopping blood flow across the wound. Fibroblasts disappear as the wound becomes stronger. Fibroblast movement causes contraction of the healing area, which helps to bring wound edges closer together. A mature scar is then formed. Initially the scar is pink and raised. With maturation, the scar becomes pale, does not tan when exposed to sunlight, will not sweat or produce hair, and may cause itching. The maturation process may continue for years, and the extent to which the scar remodels and matures varies among individuals.
Children heal aggressively with abundant scar tissue, especially during growth spurts. Because of its highly elastic quality, children’s skin pulls on wounds, which defend against the pull by aggressive scarring. Consequently, the child’s skin heals with more scar tissue than the less elastic skin of the adult.
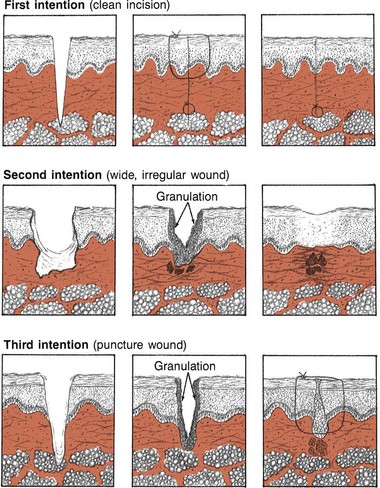
Types of Wound Healing: Repair healing takes place in one of three ways: by primary, secondary, or tertiary intention (Fig. 18-2). Primary intention healing takes place when all layers of the wound margins (skin, subcutaneous tissue, and muscle) are neatly approximated, as with a surgical incision. Unless infection interferes or the wound edges separate, these wounds heal with a minimum of scarring.
Repair by secondary intention takes place in wounds that occur from ulceration and lacerations in which the edges cannot be approximated, such as an avulsion or a third-degree burn. The inflammatory reaction may be greater, and the chance of infection is increased. Often debris, cells, and exudate must be cleaned away (débrided) before healing can take place. Healing takes place from the edges inward and from the bottom of the wound upward until the defect is filled. More granulation tissue and a larger scar are formed than in healing by primary intention.
Repair by tertiary intention takes place when suturing is delayed after injury or the wound later breaks down and is sutured or resutured when granulation is present. More granulation tissue is formed than in healing by primary intention, and there is a greater chance that microorganisms will invade the wound. Frequently, suturing of a contaminated wound is deliberately delayed to afford better removal of infection before closing. Healing of wounds by tertiary intention results in a larger and deeper scar than healing by primary intention.
Factors That Influence Healing
During the past two decades, understanding of wound healing has revolutionized the interventions used to promote healing. Emphasis has shifted from interventions directed at maintaining a dry environment that promotes eschar formation to those that promote a moist, crust-free environment that enhances the migration of epithelial cells across the wound and facilitates resurfacing. An acute full-thickness wound kept in a moist environment usually reepithelializes in 12 to 15 days, whereas the same wound kept open to the air heals in approximately 25 to 30 days (see Fig. 18-1).
Eschar (thick, fibrin-containing necrotic tissue) also interferes with healing by preventing wound contraction. In most situations it is best to remove eschar and other dead tissue from the wound. Repeated application of occlusive dressings mobilizes the body’s own enzymes to lyse the eschar, a process known as autolysis.
Adequate nutrition is essential for wound healing. In particular, sufficient protein, calories, vitamin C, and zinc are needed for healing of extensive wounds, such as burns. Supplemental nutrition is an integral aspect of treatment of severe wounds.
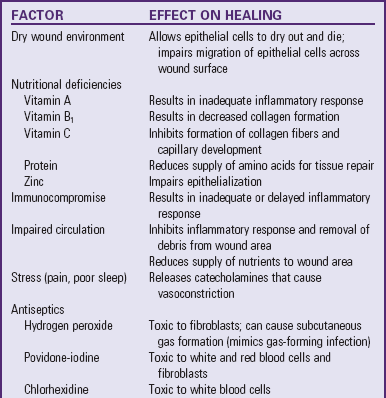
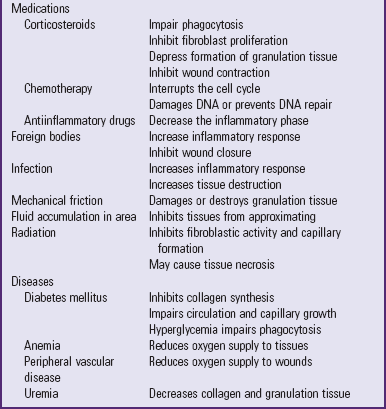
Numerous factors delay healing (Table 18-1). Some traditional practices are ineffective or even harmful; for example, antiseptics that were once used to help prevent infections (hydrogen peroxide and povidone-iodine [Betadine] solutions) are now known to have cytotoxic effects on healthy cells and minimal effect on controlling infections. Povidone-iodine may be absorbed through the skin in neonates and young children and must be used with caution in patients with thyroid or renal disease.
General Therapeutic Management
The human body tends to heal; therefore direct treatment is directed toward eliminating or ameliorating factors that interfere with normal healing processes. Some disorders may demand aggressive therapy, but by and large the major aim of any treatment is to prevent further damage, eliminate the cause, prevent complications, and provide relief from discomfort while tissues undergo healing. When possible, eliminate factors that contribute to the dermatitis and prolong the course of the disease. The most common offenders in pediatrics are environmental factors (such as soaps, bubble baths, shampoos, rough or tight clothing, wet diapers, blankets, and toys) and natural elements (such as dirt, sand, heat, cold, moisture, and wind). Dermatitis can also be aggravated by home remedies and medications.
Dressings
No one dressing meets the needs of all wounds. The traditional dry gauze dressing should not be used on open wounds, since it allows the wound surface to dry, does little to prevent bacterial invasion, and adheres to the dried scab so that removal disturbs the newly regenerating epithelial cells. In most instances, traditional gauze dressings have been replaced by moist wound healing dressings. Moist wound healing increases the rate of collagen synthesis and reepithelialization and decreases pain and inflammation. It also creates an environment for autolytic débridement of necrotic tissue, which creates a clean wound bed and enhances granulation. However, a balance must be achieved between creating a moist wound bed and maintaining a dry periwound area that protects the skin and wound from maceration. The dressing type and frequency of dressing changes help to achieve this balance. The frequency of dressing changes depends on the presence or absence of infection, the type of dressing, the location of the wound, and the amount of drainage. Dressings should always be changed when they are loose or soiled. They should be changed more frequently in areas where contamination is likely (e.g., the sacral area, the buttocks, the tracheal area) or when wound infection is suspected or confirmed.
Dressings serve the following functions: (1) provide a moist healing environment, (2) protect the wound from infection and trauma, (3) provide compression in the event of anticipated bleeding or swelling, (4) apply medication, (5) absorb drainage, (6) débride necrotic tissue, (7) reduce pain, and (8) control odor. To ensure a moist environment, cover wounds with an occlusive ointment or dressing (Table 18-2).
TABLE 18-2
DRESSING CATEGORY DEFINITIONS AND EXAMPLES OF PRODUCTS
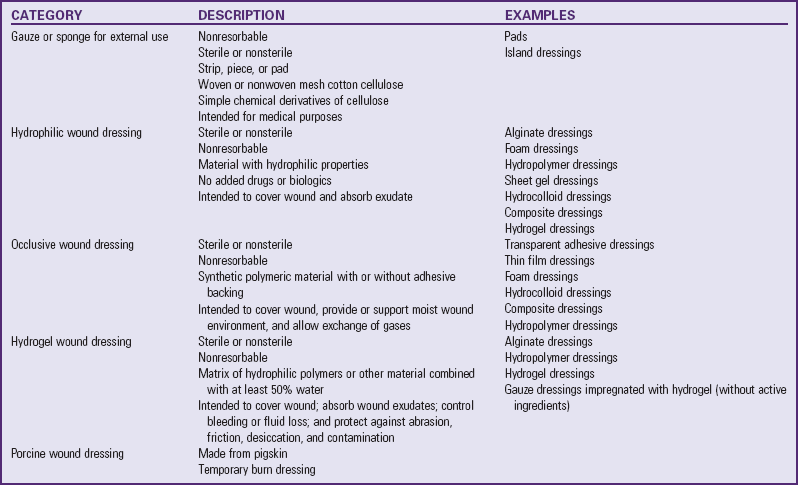
From van Rijswijk L: Recommendations to change the FDA classification of various wound dressings, Ostomy Wound Manage 45(3):31, 1999. Used with permission.
Occlusive dressings can be classified according to their degree of permeability. The term occlusive is synonymous with impermeable, semiocclusive is synonymous with semipermeable, and nonocclusive is synonymous with permeable. No one dressing meets the needs of all types of wounds. The traditional gauze dressing is a permeable dressing that reduces the moisture content in a wound by absorbing exudate and allowing it to evaporate. Traditional gauze dressings should not be used on open wounds because they allow wounds to dehydrate, are permeable to bacteria, increase the probability of wound sepsis, and adhere to the wound when removed, which causes additional trauma to newly regenerating epithelial cells. In many situations traditional gauze dressings have been replaced by new “active occlusive” dressings, which allow for moist wound healing. The use of silver in wound care has reemerged. Silver is impregnated in various dressing vehicles such as foam, hydrocolloid dressings, and wound gels. Several studies suggest that silver decreases the bacteria and bioburden in the wound, which allows optimal wound conditions for granulation and healing (Ovington, 2004). Since the absorption of these products in infants and children is unknown, use caution when applying these dressings in the pediatric population.
Topical Therapy
A variety of agents and methods are available for treatment of dermatologic problems. In selecting a therapeutic program, the practitioner considers (1) the active ingredient of the agent, (2) the vehicle or base, (3) the cosmetic effect, (4) the cost, and (5) instructions for the agent’s use. In addition, keep several basic concepts in mind. Avoid overtreatment. For example, when the dermatitis is acute, topical applications should be mild and bland to avoid further irritation. Broken or inflamed skin, especially in children, is more absorbent than intact skin, and chemicals that are nonirritating to intact skin may be quite irritating to inflamed skin.
Topical applications may be used to treat the disorder, reduce the itching associated with many diseases, decrease external stimuli, or provide external heat or cold. The emollient action of soaks, baths, and lotions provides a soothing film over the skin surface that reduces external stimuli. Ordinarily, tepid or cool applications offer the greatest relief.
Topical Corticosteroid Therapy: The glucocorticoids are the therapeutic agents used most widely for skin disorders. Their local antiinflammatory effects are merely palliative, so the medication must be applied until the disease state undergoes a remission or the causative agent is eliminated. Corticosteroids are applied directly to the affected area. Because they are essentially nonsensitizing and have only minor side effects, they can be applied over prolonged periods with continuing effectiveness. As with any steroids, their use in large amounts may mask signs of infection, and symptoms may be exacerbated after termination of the drug. Caution families that the medication cannot be used for all skin disorders. At the concentrations available without prescription, they are not adequate for some stubborn conditions (e.g., psoriasis) and may lead to worsening of inflammation caused by fungus or bacteria. Most parents and children apply too much topical hydrocortisone; therefore counsel them that it is both effective and economical to apply only a thin film and to massage it into the skin. Also advise parents and children to use the medication for no more than 5 to 7 days because these agents may cause depigmentation and other changes in the skin.
Other Topical Therapies: Other topical treatments include chemical cautery (especially useful for warts), cryosurgery, electrodesiccation (chiefly used for warts, granulomas, and nevi), ultraviolet therapy (primarily used in psoriasis and acne), laser therapy (especially for birthmarks), and special acne therapies such as dermabrasion and chemical peels. New drugs called topical immunomodulators are effective in reducing the itching of atopic dermatitis (eczema) and preventing flare-ups. Recently, chronic use of immunomodulators in transplant patients has been linked to possible skin cancer and lymphoma. The U.S. Food and Drug Administration (FDA) has issued a black box warning cautioning against the use of these topicals as first-line treatments in children younger than 2 years of age (Dohil and Eichenfield, 2005). A recent study by Papp, Breuer, Meurer, and colleagues (2005) on the use of pimecrolimus cream (Elidel) in infants and children concluded that there was no apparent effect on the antibody responses in these patients.
Systemic Therapy
Systemic therapeutic agents are often used as an adjunct to topical therapy in dermatologic disorders, and those most frequently used therapeutically are the corticosteroids and the antibiotics. The corticosteroid hormones, with their capacity to inhibit inflammatory and allergic reactions, are valuable in the treatment of severe skin disorders. Dosage is carefully adjusted and gradually tapered to the minimum that is effective and tolerated. In infants and children, the dosage is larger than is usually calculated from body weight ratios. However, prolonged use may temporarily suppress growth.
Antibiotics, which interfere with the growth of microorganisms, are used in cases of severe or widespread skin infection. However, because they tend to produce a hypersensitivity in the patient, they are used with caution. Antifungal agents are the only means for treating systemic fungal infections.
Nursing Care of the Child with a Skin Disorder
To help establish a diagnosis, it is important for nurses to accurately describe any deviation in the character of the skin, using both inspection and palpation. Note the color, shape, and distribution of the lesions or wounds. Describe the individual lesions using the accepted terminology and may consist of more than one type, such as a maculopapular rash. Assess wounds for depth of tissue damage, evidence of healing, and signs of infection.
To confirm or amplify the findings made by inspection, gently palpate the skin to detect characteristics such as temperature, moisture, texture, elasticity, and the presence of edema. Indicate whether the findings are restricted to the area of the lesion(s) or are generalized.
The child’s symptoms provide additional information. Older children are able to describe the condition as painful, itching, or tingling or in other descriptive terms. However, the nurse can determine much by noting the younger child’s behavior and the parents’ account of these reactions. Does the child scratch? Is the child restless or irritable? Does the child favor or avoid using a body part? A careful history may provide clues. Has the child had access to chemicals or been in the woods or around a woodpile? Has the child eaten a new food? Is the child taking medication? Does the child have any known allergy? Do any playmates have a similar lesion? An uncertain diagnosis is frequently confirmed on the basis of the history.
Therapeutic programs are usually designed to provide general measures, such as rest, protection, and relief of discomfort; and specific treatments, such as a definitive medication or physical technique. Because only a few skin diseases are contagious, it is usually not necessary to isolate the affected child unless there is a danger of the child’s acquiring a secondary infection (e.g., the child who is receiving large doses of corticosteroids or other immunosuppressant drugs or the child with an immunologic deficiency disorder). If the skin manifestation is a viral exanthem, such as measles or chickenpox, the child is prevented from exposing other susceptible children.
Wound Care
![]() Parents can generally manage small wounds to the skin at home. Instruct parents to wash their hands and then wash the wound gently with mild soap and water, or normal saline Caution them to avoid povidone-iodine, alcohol, and hydrogen peroxide because these products are toxic to wounds. To prevent possible tattooing, an abrasion from which the dirt cannot be removed requires wound cleaning with the patient receiving topical anesthesia. Wounds covering a very large area (>15% of the body) need medical attention with the child undergoing conscious sedation and analgesia. (See Chapter 7.) Open wounds are covered with a dressing, such as a commercial adhesive bandage, although larger wounds may benefit from the use of occlusive dressings (see Table 18-2). If occlusive dressings are applied, instruct the parents on their correct application and removal. For example, hydrocolloid dressings adhere best if a wide margin is left around the wound and the dressing is pressed against intact skin until it adheres. The edges of the dressing can be secured to the skin with waterproof tape. The dressings are removed if leakage occurs or after a specific time interval, usually 7 days.
Parents can generally manage small wounds to the skin at home. Instruct parents to wash their hands and then wash the wound gently with mild soap and water, or normal saline Caution them to avoid povidone-iodine, alcohol, and hydrogen peroxide because these products are toxic to wounds. To prevent possible tattooing, an abrasion from which the dirt cannot be removed requires wound cleaning with the patient receiving topical anesthesia. Wounds covering a very large area (>15% of the body) need medical attention with the child undergoing conscious sedation and analgesia. (See Chapter 7.) Open wounds are covered with a dressing, such as a commercial adhesive bandage, although larger wounds may benefit from the use of occlusive dressings (see Table 18-2). If occlusive dressings are applied, instruct the parents on their correct application and removal. For example, hydrocolloid dressings adhere best if a wide margin is left around the wound and the dressing is pressed against intact skin until it adheres. The edges of the dressing can be secured to the skin with waterproof tape. The dressings are removed if leakage occurs or after a specific time interval, usually 7 days.
![]() Evidence-Based Practice—Wound Care
Evidence-Based Practice—Wound Care
Dressings are removed carefully to protect intact skin and the epithelial surface of the wound from damage. To remove transparent or hydrocolloid dressings, raise one edge of the dressing and pull parallel to the skin to loosen the adhesive. The longer the dressings are left on, the easier they are to remove. Use of a nonalcohol skin barrier protects the skin from epidermal stripping on tape removal. Or the wound may be “picture-framed” with strips of a skin barrier dressing (DuoDERM, Coloplast) on the skin and the adhesive tape secured to the skin barrier. This technique protects the underlying skin with dressing changes. If a dressing sticks to the wound base when it is being removed, saturate the dressing with normal saline, water, or wound cleanser to loosen it.
Lacerations present a special challenge. The injured child and family are usually distressed by the bleeding and are in variable degrees of shock. Parental guilt usually accompanies the injury. Because scalp lacerations bleed so profusely, they are especially frightening. The initial nursing intervention is to apply pressure to the area and attempt to calm the child before further examination. Unless there is bleeding from a severed artery, the wound can be cleansed with a forced jet of sterile tepid water or saline (via syringe) and examined for extent; depth; and foreign material such as dirt, glass, or fabric fragments.
The location of the wound also dictates assessment. For example, wounds over bony areas may contain bone chips, and clear fluid seeping from severe head wounds may indicate cerebrospinal fluid leakage. Apply a pressure dressing for transfer to medical care; prepare the child in a medical facility for suturing. Soak puncture wounds that do not require a tetanus booster in warm water and soap for several minutes. Causing the wound to rebleed may be helpful. Apply an adhesive bandage if desired. Puncture wounds of the head, chest, or abdomen or those that could still contain a portion of the puncturing object must be evaluated.
Caution parents against opening blisters or kissing a wound “to make it better.” The wound can easily become contaminated from germs in the human mouth. If scabs form, they are allowed to slough off without assistance; picking or early removal may cause scarring. Advise parents to seek medical help if there is evidence of infection.
Relief of Symptoms
Most of the therapeutic regimens are directed toward relief of pruritus, the most common subjective complaint. Itching is believed to often result from stimulation of C fibers at the dermoepidermal junction. These fibers are similar to but distinct from pain fibers. Substances released within the skin, histamine and endopeptidases, also elicit itching, although their release triggers are unknown (Barnett, 2001).
Cooling the affected area and increasing the skin pH with measures such as cool baths or compresses to reduce external stimuli to the area, as well as alkaline applications such as baking soda baths to increase skin pH, help to prevent scratching. Clothing and bed linen should be soft and lightweight to decrease the irritation from friction and stimulation.
During any type of treatment, both affected and unaffected skin is protected from damage and secondary infection. Preventing scratching is of primary importance. Older children usually cooperate, although they may need to be reminded to stop scratching or rubbing. In smaller and uncooperative children, techniques and devices such as mittens (especially during sleep) or special coverings are required. Keeping fingernails short, well trimmed, and clean helps reduce the chance of secondary infection.
Antipruritic medications, such as diphenhydramine (Benadryl) or hydroxyzine (Atarax), may be prescribed for severe itching, especially if it disturbs the child’s rest. Pain and discomfort are usually managed with nonpharmacologic measures and mild analgesia. Severe pain requires more potent medication. Occlusive dressings over wounds reduce pain. For suturing wounds a topical anesthetic, tissue adhesive, or intradermal buffered lidocaine can be used. Pain medications should be given before dressing changes and cleansing, with adequate time allowed for the medicine to take effect. (See Pain Management, Chapter 7.)
Topical therapy usually involves application of some type of topical agent, and the mode of application depends on the nature and location of the lesion being treated. For example, soothing lotions, creams, and intermittent wet dressings or soaks help cool and moisten; ointments, lotions, and creams soften and lubricate dry, scaling areas. Nurses and parents are responsible for the application of topical therapeutic agents.
It is especially important to wash the hands before and after application of topical therapies. Assess the skin before the treatment or application of medication and reassess after the treatment is completed. Note any changes and describe them.
Wet compresses or dressings cool the skin by evaporation, relieve itching and inflammation, and cleanse the area by loosening and removing crusts and debris. Any of a variety of ingredients, such as plain water or Burow solution (available without a prescription), can be applied on Kerlix gauze, plain gauze, or (preferably) soft cotton cloths such as freshly laundered handkerchiefs or strips from cloth diaper, sheeting, or pillowcase material.
Dressings immersed in the desired solution are wrung out slightly and applied to the affected area wet but not dripping. They are applied flat and smooth and in such a way that motion is not totally restricted; fingers are wrapped separately, and arms and legs are wrapped so that elbows and knees can bend. Dressings are kept in place by Kerlix or other cotton wrap, tubular stockinette, mittens, or socks (two pairs—one to hold the dressings in place, the other to take up movement) but are left uncovered. When evaporation begins to dry them, the dressings are removed, rewet in the solution, and reapplied to the area using aseptic technique. The solution is not poured or syringed directly over the dressings. As fluid evaporates, the solution becomes increasingly concentrated and thus stronger, which may damage sensitive lesions.
Fresh solution at room temperature is applied at 2-, 3-, or 4-hour intervals and is allowed to remain on the lesion from 30 to 90 minutes. Wet dressings are seldom continued after about 48 hours. The child must be guarded against chilling during treatment, and no more than 20% of the body should be covered at one time to avoid the risk of hypothermia. After treatment, the skin is dried thoroughly by patting with a towel. Application of lotion or other medication may be ordered at this time.
When children are uncooperative in the use of wet dressings, soaks are often used for removal of crusts and for their mild astringent action. The same solution as for wet compresses is used. Gaining young children’s cooperation for hand or foot soaks is difficult unless the procedure is made attractive to them through play. Older infants and toddlers delight in playing with brightly colored objects or poker chips scattered over the bottom of the receptacle, and preschoolers can be challenged to hold a floating item beneath the water’s surface. These activities require supervision; infants and small children often place items in their mouths, and children can easily lose control with water play. Washing dishes, cars, dolls, or doll clothes will occupy many children for some time.
Although older children are able to cooperate, they need something to do during the procedure, such as listening to music or a story, or watching television or a video. A single extremity (a foot or a hand) can be easily soaked by placing the solution and the extremity in a sealable plastic bag. The closure is then zipped snugly around the limb.
Baths are especially useful in the treatment of widespread dermatitis because they evenly distribute the soothing antipruritic and antiinflammatory solution, usually an oatmeal or mineral oil preparation. The solution is added to a tub of water. The temperature of the bath is tepid, and the treatment usually lasts 15 to 30 minutes. Therapeutic baths are always more interesting when the child has toy boats or other items for water play.
Topical agents are applied to skin lesions to ease discomfort, prevent further injury, and facilitate healing. Most preparations are placed directly on the skin and left uncovered; some may be applied under an occlusive dressing. A thin application of the ointment or cream is covered with plastic film and anchored with adhesive or covered with a commercial transparent dressing. Occlusive dressings promote moisture retention and decrease evaporation of the preparation, which increases the penetration of the medication. Apply topical applications systematically with the contour of the body surface (not simply up and down). Children love to be “painted,” so lotion applications can be fun when an ordinary paintbrush is employed.
Regardless of the type of preparation used, parents need detailed information on how to apply it and how long the preparation should remain on the skin or under an occlusive dressing.
Recombinant growth factors are human platelet–derived growth factors that are engineered outside the body. They foster the formation of new granulation tissue by stimulating the migration of fibroblasts, macrophages, smooth muscle cells, and capillary endothelial cells to the wound site (Beaumont and Anderson-Dam, 1998). Becaplermin (Regranex) is the only recombinant growth factor currently approved by the FDA; however, the safety of this product has not been established for children under 16 years of age.
The vacuum-assisted closure (VAC) device uses a subatmospheric technique that involves placing an open-cell foam dressing into the wound, covering with an occlusive dressing, and applying suction. The negative force of the suction is applied from the foam dressing to the wound surfaces. The mechanical force removes excess fluids from the wound, stimulates formation of granulation tissue, restores capillary flow, and fosters closure of the wound (Patel, Kinsey, Koperski-Moen, et al, 2000). VAC has been used to prepare wounds for a skin graft and to treat surgical wounds, burns, and pressure ulcers (Kinetic Concepts, 2003). Recently, VAC therapy has been used in pediatrics. Despite case reports indicating this therapy is beneficial in infants and children, prospective, randomized trials are needed to determine the safety and efficacy of the VAC technique for these age-groups (McCord, Naik-Mathuria, Murphy, et al, 2007; Bookout, McCord, and McLane, 2004).
Home Care and Family Support
Dermatologic conditions always involve the family. Because few situations require hospitalization and children who are hospitalized will complete a therapy program at home, the family must carry out the treatment plan; therefore their cooperation is essential. Regimens that are simple to accomplish in the hospital or office may be frustrating and baffling at home. The family often needs assistance in adapting equipment available in the home to the therapy.
It is important to give the child and family as detailed explanations as possible about both the expected and the unexpected results of treatment, including any ill effects that might occur. Direct the family to discontinue treatment and report the reactions to the appropriate person(s) if unexplained reactions do develop. Discourage the use of over-the-counter medicines unless these have first been approved by the attending practitioner.
Because the skin is the most visible portion of the body, defects in its surface that alter its appearance are sometimes a source of distress to the child and a source of revulsion and rejection by others. Parents of other children may fear that their children will “catch” the disorder. Occasionally the affected child’s own family members reduce their interaction with the child, especially close physical contact, or otherwise demonstrate a distaste for the condition, which the child may interpret as rejection. This is seldom a difficulty with dermatitis of short duration, but chronic conditions can create problems and affect the child’s self-concept (see Family-Centered Care box).
Infections of the Skin
Normally, the skin harbors a variety of bacterial flora, including the major pathogenic varieties of staphylococci and streptococci. The degree of their pathogenicity depends on the invasiveness and toxigenicity of the specific organism, the integrity of the skin (the host’s barrier), and the host’s immune and cellular defenses. Children with congenital or acquired immune disorders such as acquired immunodeficiency syndrome (AIDS), children in a debilitated condition, those receiving immunosuppressive therapy, and those with a generalized malignancy such as leukemia or lymphoma are at risk for developing bacterial infections.
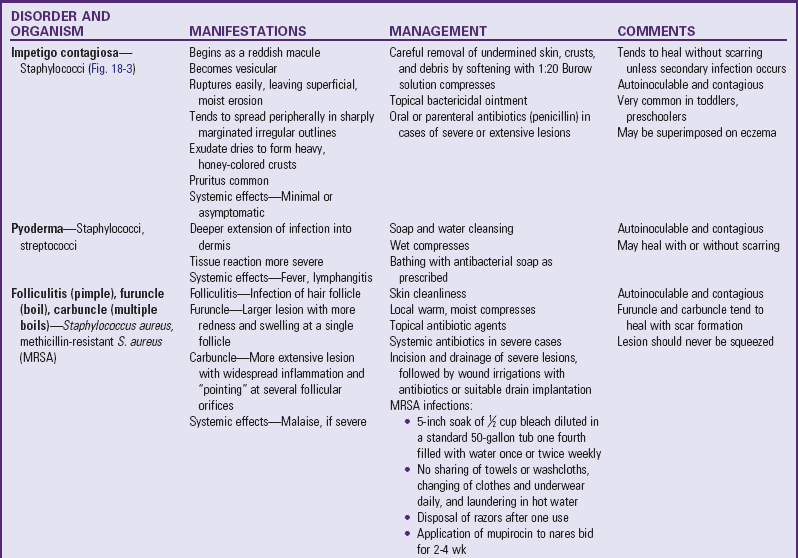
The characteristic “walling-off” process of the inflammatory reaction (abscess formation) makes staphylococci more difficult to attack, and the local infected area is associated with an increase in the numbers of bacteria all over the skin surface, which serves as a source of continuing infection. Staphylococcal infections occur most often in children in the younger age-groups; the incidence decreases with advancing age. All these factors point up the importance of careful hand washing and cleanliness when caring for infected children and their lesions to prevent spread of the infection and as an essential prophylactic measure when caring for infants and small children. ![]() Table 18-3 outlines common bacterial skin disorders.
Table 18-3 outlines common bacterial skin disorders.

Fig. 18-3 Impetigo contagiosa. (From Weston WL, Lane AT: Color textbook of pediatric dermatology, ed 4, St Louis, 2007, Mosby.)

Fig. 18-4 Cellulitis of the cheek from a puncture wound. (From Weston WL, Lane AT: Color textbook of pediatric dermatology, ed 4, St Louis, 2007, Mosby.)
Nursing Care Management
The major nursing functions related to bacterial skin infections are to prevent the spread of infection and to prevent complications. Impetigo contagiosa and methicillin-resistant Staphylococcus aureus (MRSA) infection can easily spread by self-inoculation; therefore caution the child against touching the involved area. Hand washing is mandatory before and after contact with an affected child. Also emphasize hand washing to both the child and the family. Many children with atopic dermatitis are colonized with MRSA in the nares and under the fingernails (Rosenthal, 2004). For many bacterial infections and for MRSA infection in particular, the child should be provided with washcloths and towels separate from those of other family members. The child’s pajamas, underwear, and other clothes should be changed daily and washed in hot water. Razors used for shaving should be discarded after each use and not shared. To prevent recurrence, some infectious disease specialists recommend bathing in a chlorine bath once or twice weekly. A 5-minute soak of 2.5 ml of bleach diluted in 13 gallons of water, or  cup of bleach diluted in a standard 50-gallon tub one fourth filled with water, could decrease community-acquired MRSA colonies by more than 99.9% (Fisher, Chan, Hair, et al, 2008; Kaplan, 2008). In addition, mupirocin can be applied to the nares of patients and families twice daily for 2 to 4 weeks to prevent reinfection (Lee, Rios, Aten, et al, 2004; Dohil and Eichenfield, 2005).
cup of bleach diluted in a standard 50-gallon tub one fourth filled with water, could decrease community-acquired MRSA colonies by more than 99.9% (Fisher, Chan, Hair, et al, 2008; Kaplan, 2008). In addition, mupirocin can be applied to the nares of patients and families twice daily for 2 to 4 weeks to prevent reinfection (Lee, Rios, Aten, et al, 2004; Dohil and Eichenfield, 2005).
Children and parents are often tempted to squeeze follicular lesions. They must be warned that squeezing will not hasten the resolution of the infection and that there is a risk of making the lesion worse or spreading the infection. Children should not puncture the surface of the pustule with a needle or sharp instrument. A child with a stye may waken with the eyelids of the affected eye sealed shut with exudate. Instruct the child or the parents to gently wipe the lid from the inner to the outer edge with warm water and a clean washcloth until the exudate has been removed.
The child with limited cellulitis of an extremity is usually managed at home on a regimen of oral antibiotics and warm compresses. Teach the parents the procedures and instruct them in administration of the medication. Children with more extensive cellulitis, especially around a joint with lymphadenitis or on the face, or with lesions larger than 5 cm (2 inches), may be admitted to the hospital for parenteral antibiotics, incision, and drainage (Fisher, Chan, Hair, et al, 2008; Kaplan, 2008). Nurses are responsible for teaching the family to administer the medication and to apply compresses.
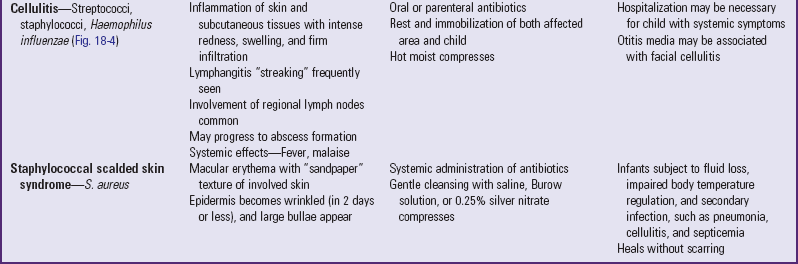
Viral Infections
Viruses are intracellular parasites that produce their effect by using the intracellular substances of the host cells. Composed of only a deoxyribonucleic acid or ribonucleic acid core enclosed in an antigenic protein shell, viruses are unable to provide for their own metabolic needs or to reproduce themselves. After a virus penetrates a cell of the host organism, it sheds the outer shell and disappears within the cell, where the nucleic acid core stimulates the host cell to form more virus material from its intracellular substance. In a viral infection the epidermal cells react with inflammation and vesiculation (as in herpes simplex) or by proliferating to form growths (warts).
Most of the communicable diseases of childhood are associated with rashes, and each rash is characteristic. The type of lesion and the configuration of the viral exanthems of rubeola, rubella, and chickenpox are described in Table 16-1. Other common viral disorders of the skin are in Table 18-4.
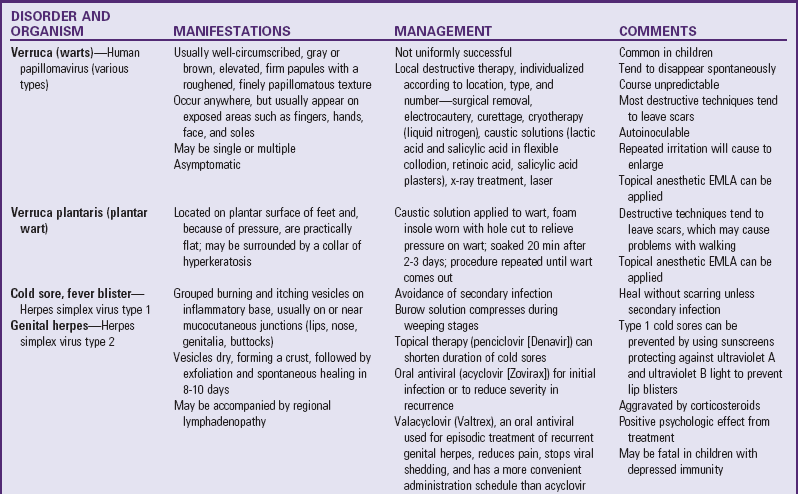
Dermatophytoses (Fungal Infections)
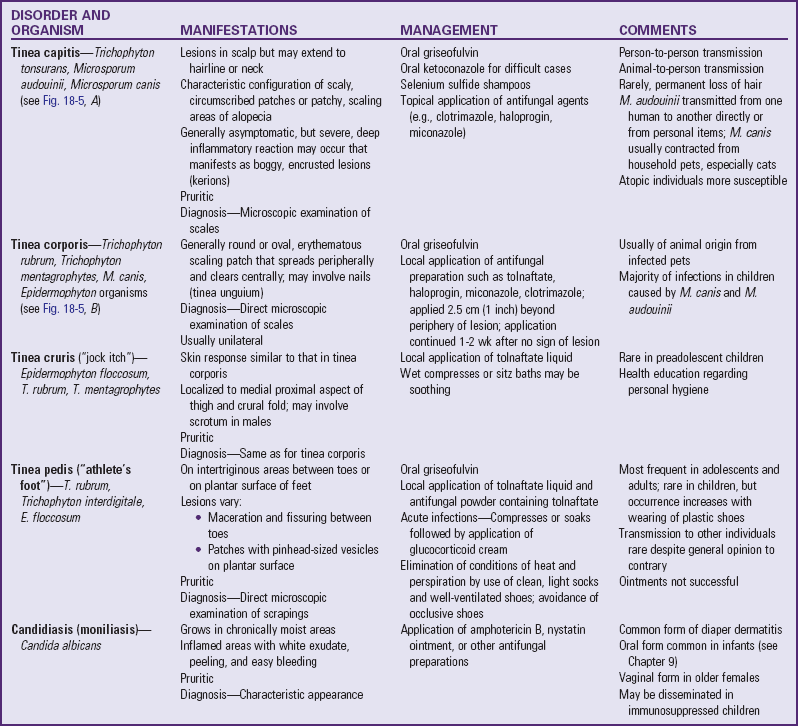
![]() The dermatophytoses (ringworm) are infections caused by a group of closely related filamentous fungi that invade primarily the stratum corneum, hair, and nails. These are superficial infections by organisms that live on, not in, the skin. These microbes are confined to the dead keratin layers and are unable to survive in the deeper layers. Because keratin is being shed constantly, the fungus must multiply at a rate that equals the rate of keratin production to maintain itself; otherwise the organism would be shed with the discarded skin cells. Table 18-5 outlines common dermatophytoses.
The dermatophytoses (ringworm) are infections caused by a group of closely related filamentous fungi that invade primarily the stratum corneum, hair, and nails. These are superficial infections by organisms that live on, not in, the skin. These microbes are confined to the dead keratin layers and are unable to survive in the deeper layers. Because keratin is being shed constantly, the fungus must multiply at a rate that equals the rate of keratin production to maintain itself; otherwise the organism would be shed with the discarded skin cells. Table 18-5 outlines common dermatophytoses.
![]() Critical Thinking Case Study—Tinea Capitis
Critical Thinking Case Study—Tinea Capitis
Three principal types of fungi are responsible for dermatophyte infections: Trichophyton, Microsporum, and Epidermophyton. They are designated by the Latin word tinea, with further designation relating to the area of the body where they are found (e.g., tinea capitis [ringworm of the scalp]) (Fig. 18-5, A). Dermatophyte infections are most often transmitted from one person to another or from infected animals to humans. Atopic individuals (those with a tendency to develop allergy) are more susceptible to dermatophyte infections. Fungi exert their effect by means of an enzyme that digests and hydrolyzes the keratin of hair, nails, and the stratum corneum. Dissolved hair breaks off to produce the bald spots characteristic of tinea capitis. In the annular lesions the fungi principally appear in the edge of the inflamed border as they move outward from the inflammation. Diagnosis is made from microscopic examination of scrapings taken from the advancing periphery of the lesion, which almost always produces scale.
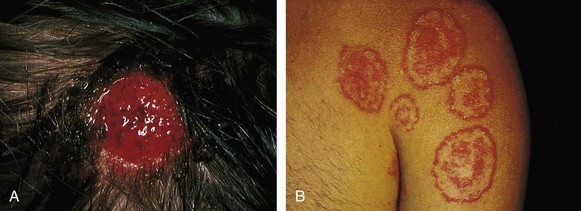
Fig. 18-5 A, Tinea capitis. B, Tinea corporis. Both infections are caused by Microsporum canis, the “kitten” or “puppy” fungus. (From Habif TP: Clinical dermatology: a color guide to diagnosis and therapy, ed 4, St Louis, 2004, Mosby.)
Nursing Care Management
When teaching families about the care of children with ringworm, the nurse should emphasize good health and hygiene. Both 2% ketoconazole and 1% selenium sulfide shampoos may reduce colony counts of dermatophytes. These shampoos can be used in combination with oral therapy to reduce the transmission of the disease to others. The shampoo should be applied to the scalp for 5 to 10 minutes at least three times per week (Roberts and Friedlander, 2005). The child may return to school once therapy is initiated. Because of the infectious nature of the disease, affected children should not exchange with other children any grooming items, headgear, scarves, or other articles of apparel that have been in proximity to the infected area. Infected children should use their own towels and wear a protective cap at night to avoid transmitting the fungus to bedding, especially if they sleep with another person. Because the infection can be acquired by animal-to-human transmission, all household pets should be examined for the disorder. Other sources of infection are seats with headrests (e.g., airplane seats), seats in public transportation, helmets, and gymnasium mats.
Treatment with the drug griseofulvin frequently continues for weeks or months, and because symptoms subside, children or parents may be tempted to decrease or discontinue the drug. The nurse should emphasize to family members the importance of maintaining the prescribed dose and schedule and of taking the medication with high-fat foods for best absorption. Also inform them about possible side effects of the drug, such as headache, gastrointestinal upset, fatigue, insomnia, and photosensitivity. For children who take the drug over many months, periodic testing is required to monitor for leukopenia and assess liver and renal function. Newer antifungal drugs such as terbinafine, itraconazole, and fluconazole may be used when there are adverse reactions to griseofulvin. Currently, these drugs are being studied to determine their efficacy and safety in treating tinea capitis in children but are not approved by the FDA for this indication at this time.
Scabies
Scabies is an endemic infestation caused by the scabies mite, Sarcoptes scabiei. Lesions are created as the impregnated female scabies mite burrows into the stratum corneum of the epidermis (never into living tissue), where she deposits her eggs and feces.
Clinical Manifestations
The inflammatory response causes intense pruritus that leads to punctate discrete excoriations secondary to the itching. Maculopapular lesions are characteristically distributed in intertriginous areas: interdigital surfaces, the axillary-cubital area, popliteal folds, and the inguinal region. There is variability in the lesions. Infants often develop an eczematous eruption; therefore the observer must look for discrete papules, burrows, or vesicles (Fig. 18-6). A mite is identified as a black dot at the end of a minute, linear, grayish brown, threadlike burrow. In children older than 2 years of age, most eruptions are on the hands and wrists. In children younger than 2 years, they are often on the feet and ankles. Children with Down syndrome may not complain of itching; therefore they can get a severe infestation before it is recognized.

Fig. 18-6 Scabies. (From McCance K, Huether S: Pathophysiology: the biological basis for disease in adults and children, ed 6, St Louis, 2010, Mosby.)
The inflammatory response and itching occur after the host becomes sensitized to the mite, approximately 30 to 60 days after initial contact. (In persons previously sensitized to the mite, the inflammatory response occurs within 48 hours after exposure.) After this time, anywhere the mite has traveled will begin to itch and develop the characteristic eruption. Consequently, mites will not necessarily be located at all sites of eruption. A person needs prolonged contact with the mite to become infested. It takes about 45 minutes for the mite to burrow under the skin; consequently, transient body contact is less likely to cause transfer of the mite. The diagnosis is made by microscopic identification from scrapings of the burrow.
Therapeutic Management
The treatment of scabies is the application of a scabicide. The drug of choice in children and infants older than 2 months is permethrin 5% cream (Elimite). Alternative drugs are 10% crotamiton, ivermectin, or 1% lindane cream or lotion. Lindane can be neurotoxic and is contraindicated in several age-groups. Lindane should be reserved for treatment of patients who fail to respond to other preparations (American Academy of Pediatrics, 2009).
Ivermectin, an oral medication, may be used to treat scabies in patients with secondary excoriations for whom topical scabicides are irritating and not well tolerated or whose infestation is refractory (American Academy of Pediatrics, 2009). However, the safety and efficacy of ivermectin for children younger than 5 years of age or children weighing less than 15 kg (33 lb) has not been established.
Because of the length of time between infestation and physical symptoms (30 to 60 days), all persons who were in close contact with the affected child need treatment. This may include boyfriends or girlfriends, baby-sitters, grandparents, and immediate family members. The objective is to treat as thoroughly as possible the first time. Enough medication for the entire family should be prescribed, with 2 oz allowed for each adult and 1 oz for each child.
Nursing Care Management
Nurses instructing families in the use of the scabicide should emphasize the importance of following the directions carefully. If lindane lotion is prescribed, it is applied to cool, dry skin—not following a hot bath. It is applied over the entire cutaneous surface from the neck down and is left on for the recommended time, usually 4 hours for infants and 6 hours for older children and adults. Because scabies is a superficial skin disorder, penetration need not be promoted. One liberal application is sufficient.
When permethrin 5% is used, the cream should be thoroughly and gently massaged into all skin surfaces (not just the areas that have a rash) from the head to the soles of the feet. Skin surfaces between the fingers and toes, the folds of the wrist and waist, the umbilicus, and the cleft of the buttocks should not be missed. A toothpick can be used to apply permethrin cream beneath the fingernails and toenails. Take care to avoid contact with the eyes. If permethrin cream accidentally gets into the eyes, they should be flushed immediately with water. Permethrin cream should remain on the skin for 8 to 14 hours, after which time it can be removed by bathing and shampooing.
Touching and holding the child should be minimized until treatment is completed, and the hands should be washed carefully after contact is made. Nurses should wear gloves when caring for the child. Following treatment, freshly laundered bed linen and clothing should be used, and bedclothes and previously worn clothing should be washed in very hot water and dried at the high setting in the dryer. Aggressive housecleaning is not necessary. Families need to know that although the mite will be killed, the rash and the itch will not be eliminated until the stratum corneum is replaced, which takes approximately 2 to 3 weeks. Soothing ointments or lotions, antihistamines, and topical corticosteroids can be used for itching. Antibiotics may be given for secondary infection.
Pediculosis Capitis
Pediculosis capitis (head lice) is an infestation of the scalp by Pediculus humanus capitis, a common parasite in school-age children. These lice infestations create embarrassment and concern in the family and community. They can also cause a child to be ridiculed by other children.
The louse is a blood-sucking organism that requires approximately five meals a day. The adult louse lives only about 48 hours when away from a human host, and the life span of the average female is 1 month. The female lays her eggs at night at the junction of a hair shaft and close to the skin because the eggs need a warm environment. The nits, or eggs, hatch in approximately 7 to 10 days.
Clinical Manifestations and Diagnostic Evaluation
Itching, caused by the crawling insect and insect saliva on the skin, is usually the only symptom. Common sites of involvement are the occipital area, behind the ears, and at the nape of the neck. Observation of the white eggs (nits) firmly attached to the hair shafts confirms the diagnosis. Because of their brief life span and mobility, adult lice are difficult to locate. Nits must be differentiated from dandruff, lint, hair spray, and other items of similar size and shape. On inspection, nits are seen attached to the hair shaft. Scratch marks and/or inflammatory papules caused by secondary infection may be found on the scalp in the vulnerable areas (Fig. 18-7).
Therapeutic Management
Treatment consists of the application of pediculicides and manual removal of nit cases. Because of its efficacy and lack of toxicity, the drug of choice for infants and children is permethrin 1% cream rinse (Nix), which kills adult lice and nits (American Academy of Pediatrics, 2009). This product and preparations of pyrethrin with piperonyl butoxide (RID or A-200 pyrinate) can be obtained without a prescription and are more effective and safer than lindane. Most experts advise a second treatment at 7 to 10 days to ensure a cure (America Academy of Pediatrics, 2009; Leung, Fong, and Pinto-Rojas, 2005). However, pyrethrin products are contraindicated for individuals with contact allergy to ragweed or turpentine. If neither permethrin nor pyrethrin products are effective, the prescription drug 0.5% malathion, which has been approved for treatment of head lice, can be used. However, malathion contains flammable alcohol, must remain in contact with the scalp for 8 to 12 hours, and is not recommended for children younger than 2 years of age.
Because of concerns that head lice may be developing resistance to chemical shampoos and that repeated exposure of children to strong chemicals on the scalp may be unwise, effective nonchemical control measures are essential. Daily removal of nits from a child’s hair with a metal nit or flea comb is an essential control measure following treatment with the pediculicide. The child’s entire head should be completely combed every day until no more nits are found. In most instances, a nit comb removes most of the nits. However, in some instances, nits need to be removed by scraping them off strands of hair with the fingernail or using tweezers. Several nit combs are currently available at community pharmacies.
Lice are small and grayish tan, have no wings, and are visible to the naked eye. The nits, or eggs, appear as tiny whitish oval specks adhering to the hair shaft about 6 mm (0.25 inch) from the scalp. The adherent nature of the nits distinguishes them from dandruff, which falls off readily. Empty nit cases, which indicate hatched lice, are translucent rather than white and are located more than 0.25 inch from the scalp (Fig. 18-8).
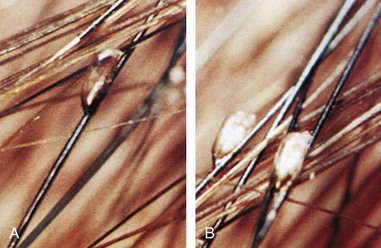
Fig. 18-8 A, Empty nit case. B, Viable nits. (From The contemporary approach to the control of head lice in schools and communities, Pittsburgh, 1991, SmithKline Beecham.)
If evidence of infestation is found, it is important to perform the treatment according to the directions on the label of the pediculicide. Advise parents to read the directions carefully before beginning treatment. Instructions indicate that dead lice and remaining nits are to be removed with an extra-fine-tooth comb (included with many preparations).
Make the child as comfortable as possible during the pediculicide application process, since the agent must remain on the scalp and hair for several minutes. Playing “beauty parlor” during the shampoo is a useful strategy. The child lies supine, with the head over a sink or basin, and covers the eyes with a dry towel or washcloth. This prevents medication, which can cause chemical conjunctivitis, from splashing into the eyes. If eye irritation occurs, flush the eyes well with tepid water.
Live lice survive for up to 48 hours away from the host, but nits are shed into the environment and are capable of hatching in 7 to 10 days. Therefore parents must take measures to prevent further infestation (see Community Focus box). Spraying with insecticide is not recommended because of the danger to children and animals. Families should also be advised that the pediculicide is relatively costly, especially when several members of the household require treatment. Families may be inclined to try home remedies to treat the lice (see Research Focus box).
The psychologic effects of lice infestations are stressful to children. They are influenced by the reactions of others, including their parents, school nurses, and officials. Some children feel ashamed or guilty. Parents are strongly cautioned against cutting a child’s hair or, worse, shaving a child’s head. Lice infest short hair as readily as long hair, and these actions only compound the child’s distress and serve as a continual reminder to their peers, who are prone to taunt children who have a different appearance.
Nursing Care Management
Nurses should emphasize that anyone can get pediculosis; it has no respect for age, socioeconomic level, or cleanliness. The louse does not jump or fly, but it can be transmitted from one person to another on personal items. Children are cautioned against sharing combs, hair ornaments, hats, caps, scarves, coats, and other items used on or near the hair. Children who share lockers are more likely to contract an infestation, and slumber parties place children at risk. Lice are not carried or transmitted by pets.
Nurses or parents should carefully inspect a child who scratches the head more than usual for bite marks, redness, and nits. The hair is systematically spread with two flat-sided sticks or tongue depressors, and the scalp is observed for any movement that indicates a louse. Nurses should wear gloves when examining the hair and use new tongue depressors or examining sticks for each child.
Prevention: The increasing incidence of pediculosis in schoolchildren has become a serious concern for school nurses, parents, and community health agencies. School nurses usually coordinate school-community prevention and control programs for pediculosis (see Research Focus box). The National Pediculosis Association* offers education and advocates a “no-nit” policy for the reentry of treated children into school (see Evidence-Based Practice box).
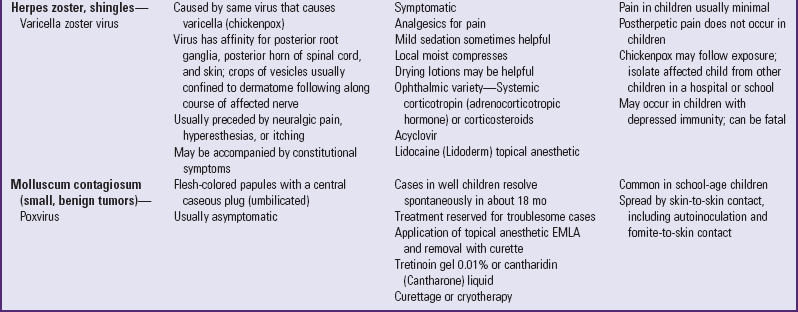
Systemic Disorders Related to Skin Lesions
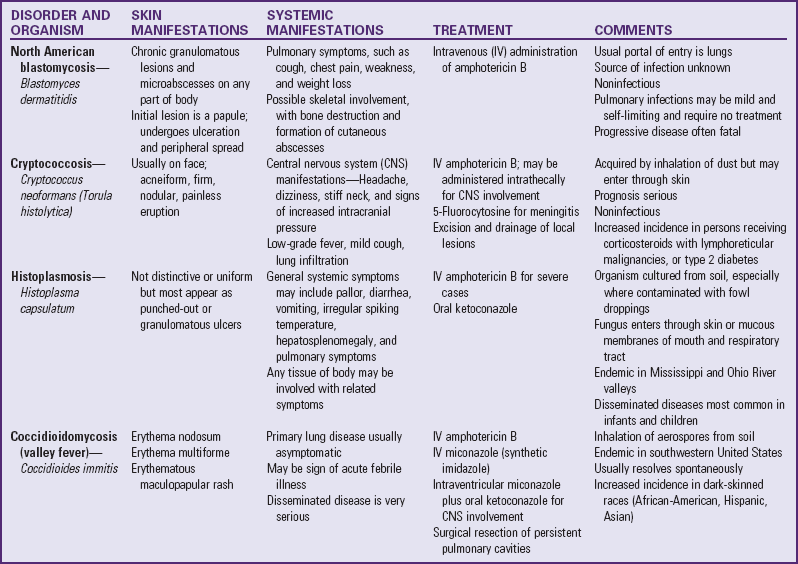
Systemic Mycotic (Fungal) Infections
Systemic mycotic (or deep fungal) infections have the capacity to invade the viscera as well as the skin. The best known of these are primarily lung diseases, which are usually acquired by inhalation of fungal spores. The fungi produce a variable spectrum of disease, and some are common in certain geographic areas. They are not transmitted from person to person but appear to reside in the soil, from which their spores are airborne. The cutaneous lesions are granulomatous and appear as ulcers, plaques, nodules, fungating masses, and abscesses. The course of deep fungal diseases is chronic, with slow progression that favors sensitization (Table 18-6).
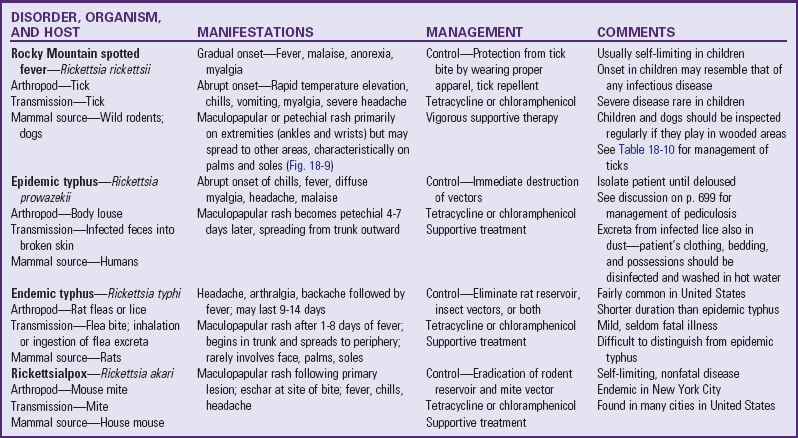
Rickettsial Infections
Rickettsiae are intracellular parasites, similar in size to bacteria that inhabit the alimentary tract of a wide range of natural hosts. Except in Q fever, mammals become infected only through the bites of infected insects (lice and fleas) or arachnids (ticks and mites), which serve as both infectors and reservoirs. Rickettsial diseases are more common in temperate and tropical climates and in areas where humans live in association with arthropods. Infection in humans is incidental (except in epidemic typhus) and is not necessary for the survival of the rickettsial species. However, once the organism invades a human, it causes a disease that varies in intensity from a benign self-limiting illness to a fulminating and frequently fatal one. Table 18-7 outlines some rickettsial infections.
Lyme Disease
Lyme disease is the most common tick-borne disorder in the United States. It is caused by the spirochete Borrelia burgdorferi, which enters the skin and bloodstream through the saliva and feces of ticks, especially the deer tick Ixodes dammini (also known as Ixodes scapularis) in the Midwest and Northeast and Ixodes pacificus in the Pacific Northwest regions of the United States. The ticks are clear to light brown and are very small, 2 to 4 mm (0.08 to 0.16 inch) in length (the size of a sesame seed), which makes detection difficult.
Clinical Manifestations
The disease may be initially seen in any of three stages. Stage 1, early localized disease, consists of the tick bite at the time of inoculation, followed in 3 to 30 days by the development of erythema migrans at the site of the bite. The lesion begins as a small erythematous papule that enlarges radially up to 30 cm (12 inches) over a period of days to weeks. It results in a large circumferential ring with a raised, edematous doughnut like border resulting in a bull’s eye appearance (Fig. 18-10). The thigh, groin, and axilla are common sites. The lesion is described as “burning,” feels warm to the touch, and occasionally is pruritic. The single annular rash may be associated with fever, myalgia, headache, or malaise.

Fig. 18-10 Lyme disease. Note annular red rings in erythema chronicum migrans. (From Weston WL, Lane AT: Color textbook of pediatric dermatology, St Louis, 1991, Mosby.)
Stage 2, early disseminated disease, occurs 3 to 10 weeks after inoculation. Many patients develop multiple smaller, secondary annular lesions without the indurated center. They may occur anywhere except on the palms and soles, and in untreated patients they disappear in 3 to 4 weeks. Constitutional symptoms, including fever, headache, malaise, fatigue, anorexia, stiff neck, generalized lymphadenopathy, splenomegaly, conjunctivitis, sore throat, abdominal pain, and cough, are often observed. A focal neurologic finding of cranial nerve palsy (seventh nerve palsy) occurs in 3% to 5% of cases.
Stage 3, the most serious stage of the disease, is characterized by systemic involvement of neurologic, cardiac, and musculoskeletal systems that appears 2 to 12 months after inoculation. Lyme arthritis is the most common manifestation with pain, swelling, and effusion. In children the arthritis is characterized by intermittently painful swollen joints (primarily the knees), with spontaneous remissions and exacerbations. Rare neurologic features of pediatric Lyme disease may include chronic demyelinating encephalitis, polyneuritis, and memory problems (Kest and Pineda, 2008).
Cardiac complications, which may appear in a small percentage of persons 4 to 5 weeks after erythema chronicum migrans, are commonly acute atrioventricular conduction abnormalities and may result in severe heart block (Wormser, Dattwyler, Shapiro, et al, 2006). Patients may be asymptomatic but can develop syncope, palpitations, dyspnea, chest pain, and severe bradycardia.
Diagnostic Evaluation
The diagnosis is based primarily on the history, observation of the lesion, and clinical manifestations. Serologic testing for Lyme disease at the time of a recognized tick bite is not recommended (Fix, Strickland, and Grant, 1998). Serologic testing is not standardized, and there is a high frequency of false-negative and false-positive results (Seltzer and Shapiro, 1996), which may lead to unnecessary treatments. Laboratory diagnosis can be established in later stages with a two-step approach that includes the enzyme-linked immunosorbent assay (ELISA) screening test and, if it is positive, Western Blot testing, as outlined by the Centers for Disease Control and Prevention (2009a) and adopted by the American Academy of Pediatrics.
Therapeutic Management
At the time the rash appears or shortly thereafter, children over 8 years of age are treated with oral doxycycline or amoxicillin, and children under 8 years of age are given amoxicillin. For patients who are allergic to penicillin, alternative drugs include cefuroxime and erythromycin (Wade, 2000; Centers for Disease Control and Prevention, 2009a).
The length of treatment depends on the clinical response and other disease manifestations, but it usually lasts from 14 to 21 days (American Academy of Pediatrics, 2009). The treatment is effective in preventing second-stage manifestations in most cases. Neurologic, cardiac, and arthritic manifestations are managed with intravenous or intramuscular antibiotics, such as ceftriaxone or penicillin G. For patients in whom tetracycline is contraindicated or who have allergies to penicillin, parenterally administered ceftriaxone is as effective as doxycycline in the treatment of acute disseminated Lyme disease (Dattwyler, Luft, Kunkel, et al, 1997). Follow-up care is important in ensuring that treatment is initiated or terminated as needed.
Nursing Care Management
The major thrust of nursing care should be educating parents to protect their children from exposure to ticks. In endemic areas tick habitats can include yards and parks, in addition to wooded areas.
Children should avoid tick-infested areas or wear light-colored clothing so that ticks can be spotted easily, tuck pant legs into socks, and wear a long-sleeved shirt tucked into pants when in wooded areas. Children should avoid grass and shrubbery where ticks may be lurking, and children and adults should walk in the center of trails. Parents and children need to perform regular tick checks when they are in infested areas. After a hike, a bare skin check (with special attention to the scalp, neck, armpits, and groin areas) is important to spot any ticks and remove them (see Table 18-10).
Parents should also be alert for signs of the skin lesion, especially if their children are known to have been exposed to the tick vector.
The use of insect repellents such as those containing diethyltoluamide (DEET) or permethrin can protect against insects. Advise parents to use them cautiously. DEET is absorbed through the skin and can cause toxicity in infants and children. These preparations can be used as directed by product insert in children as young as 2 months of age (American Academy of Pediatrics, 2009). The preparation should be sprayed on the child’s clothing, not directly on the skin. Information about Lyme disease is available from the Centers for Disease Control and Prevention.*
Cat Scratch Disease
Cat scratch disease is the most common cause of regional lymphadenitis in children and adolescents. It usually follows the scratch or bite of an animal (a cat or kitten in 90% of cases) and is caused by Bartonella henselae, a gram-negative bacterium (Margileth, 2000; Rombaux, M’Bilo, Badr-el-Din, et al, 2000). The disease is usually a benign, self-limiting illness that resolves spontaneously in 2 to 4 months.
The usual manifestations are a painless, nonpruritic erythematous papule at the site of inoculation, followed by regional lymphadenitis. The lymph nodes most commonly involved are axillary epitrochlear, cervical, submandibular, inguinal, and preauricular. The disease may persist for several months before gradual resolution. In some children, especially those who are immunocompromised, the adenitis may progress to suppuration. Some children may develop serious complications that include encephalitis, hepatitis, and Parinaud oculoglandular syndrome. This syndrome is characterized by granulomatous lesions on the palpebral conjunctiva associated with swelling of the ipsilateral preauricular nodes.
Diagnosis is made on the basis of (1) a history of contact with a cat or kitten, (2) the presence of regional lymphadenopathy for several days, and (3) serologic identification of the causative organism by indirect fluorescent antibody assay or polymerase chain reaction test (St. Geme, Haslam, and Ditmar, 1997).
Treatment is primarily supportive. Antibiotics do not shorten the duration or prevent progression to suppuration, but may be helpful in severe forms of the disease. Trimethoprim-sulfamethoxazole, ciprofloxacin, gentamicin, and rifampin have shown some benefit in uncontrolled clinical studies (St. Geme, Haslam, and Ditmar, 1997).
Activity is limited to prevent trauma to the large lymph nodes, and bed rest is indicated for children with fever. Analgesics are given for discomfort. Most children can continue normal activities during the disease. The animals are not ill during the time they transmit the disease, and most authorities do not recommend disposal of a cherished pet.
Skin Disorders Related to Chemical or Physical Contacts
Contact dermatitis is an inflammatory reaction of the skin to chemical substances, natural or synthetic, that evoke a hypersensitivity response or to those agents that cause direct irritation. The initial reaction occurs in an exposed region, most commonly the face and neck, backs of the hands, forearms, male genitalia, and lower legs. There is characteristically a sharp delineation between inflamed and normal skin early in the reaction that ranges from a faint, transient erythema to massive bullae on an erythematous swollen base. Itching is a constant symptom.
The cause may be a primary irritant or a sensitizing agent. A primary irritant is one that irritates any skin. A sensitizing agent produces an irritation on those who have encountered the irritant or something chemically related to it, have undergone an immunologic change, and have become sensitized. A sensitizer irritates in relatively low concentrations only persons who are allergic to it.
The clinical course is relatively short (1 to 4 weeks) if the causative agent is eliminated. Whether or not there are complications from secondary invasion or reactions to topical therapy depends on the severity of the original reaction.
Sensitizing reactions are acquired by repeated or prolonged exposure, and the sensitizing capacity of different substances varies widely. Strong sensitizers require only one or two exposures and provoke sensitivity reactions in a higher percentage of individuals; weak sensitizers require numerous exposures, and a smaller percentage of those exposed will be sensitized. The length of time from exposure to development of sensitivity varies and may be as short as a week or much longer. Sometimes with repeated exposure and reactions the skin loses its capacity to return to normal, or secondary factors become predominant and produce a chronic inflammatory process.
The major goal in treatment is to prevent further exposure of the skin to the offending substance. Provided there is no further irritation, the skin’s normal recuperative powers will produce satisfactory results without treatment.
The most frequent offenders are plant and animal irritants, the prototype of which is poison ivy (see discussion later). In infants the most common contact dermatitis occurs on the convex surfaces of the diaper area as a result of chemical irritation from putrefactive fecal enzymes acting on urine or laundry products. (See Diaper Dermatitis, Chapter 13.) Other agents that frequently produce dermatologic responses from contact are animal irritants such as wool, feathers, lanolin, and furs and vegetable irritants such as oleoresins, oils, and turpentine. Chemicals of all kinds, including synthetic fabrics (e.g., shoe components), dyes, metals, cosmetics, perfumes, soaps (including bubble baths), baby wipes, and moist towelettes, are also irritants (Nijhawan, Matiz, and Jacob, 2009).
Several cosmetic products advertised as safe for children may be responsible for skin irritation. These include a cream hair relaxer marketed especially for children that contains lye and must be used with extreme care. Because children’s hair is more resistant to artificial curling or straightening, pediatric preparations contain chemicals as strong as or stronger than those intended for use on adults.
Nursing Care Management
A thorough history is necessary to determine the causative agent or allergen associated with the patient’s dermatitis. Nurses frequently detect evidence of contact dermatitis during routine physical assessments. Skin manifestations in specific areas suggest limited contact, such as around the eyes (mascara), areas of the body covered by clothing but not protected by undergarments (wool), or areas of the body not covered by clothing (ultraviolet injury). Generalized involvement is more likely to be caused by bubble bath or soap. Often nurses are able to identify the offending agent and counsel families regarding management. If the lesions persist, are extensive, or show evidence of infection, medical evaluation is indicated.
Poison Ivy, Oak, and Sumac
![]() Contact with the dry or succulent portions of any of three poisonous plants (ivy, oak, or sumac) produces localized, streaked or spotty, oozing, and painful impetiginous lesions. Poison ivy grows almost everywhere east of the Rockies, poison oak is found primarily west of the Rockies, and poison sumac is usually restricted to swamp areas of the Southeast. Only Nevada, Hawaii, and Alaska (and regions above 4000 feet) appear to be free of the plants.
Contact with the dry or succulent portions of any of three poisonous plants (ivy, oak, or sumac) produces localized, streaked or spotty, oozing, and painful impetiginous lesions. Poison ivy grows almost everywhere east of the Rockies, poison oak is found primarily west of the Rockies, and poison sumac is usually restricted to swamp areas of the Southeast. Only Nevada, Hawaii, and Alaska (and regions above 4000 feet) appear to be free of the plants.
The offending substance in these plants is an oil, urushiol, that is extremely potent. Sensitivity to urushiol is not inborn but is developed after one or two exposures and may change over a lifetime. Repeated exposures appear to lower the reaction; exposure after long periods away from it may elicit a heightened response. Some highly sensitive persons may suddenly become resistant, whereas resistant persons may become sensitive. All parts of the plants, including dried leaves and stems, contain urushiol. Even smoke from burning brush piles can produce a reaction. There is widespread contact with the skin from the smoke of burning plants, and lung reactions from smoke inhalation can be life threatening.
Animals do not seem to be affected by the oil; dogs or other animals that have run or played in the plants may carry the sap on their fur, and animals that eat the plants can transfer the oil in saliva. Shoes, tools, and toys can transfer the oil. Golf balls that have been in the rough can be sources of contact.
Clinical Manifestations
Urushiol has an effect as soon as it touches the skin. It penetrates through the epidermis as a mixture of compound molecules called catechols. These catechols bond skin proteins, where it initiates an immune response (Fig. 18-11, A). The full-blown reaction is evident after about 2 days, with redness, swelling, and itching at the site of contact. Several days later, streaked or spotty blisters oozing serum from damaged cells produce the characteristic impetiginous lesions (Fig. 18-11, B). The lesions dry and heal spontaneously, and itching stops by 10 to 14 days.
Pathophysiology Reviewv
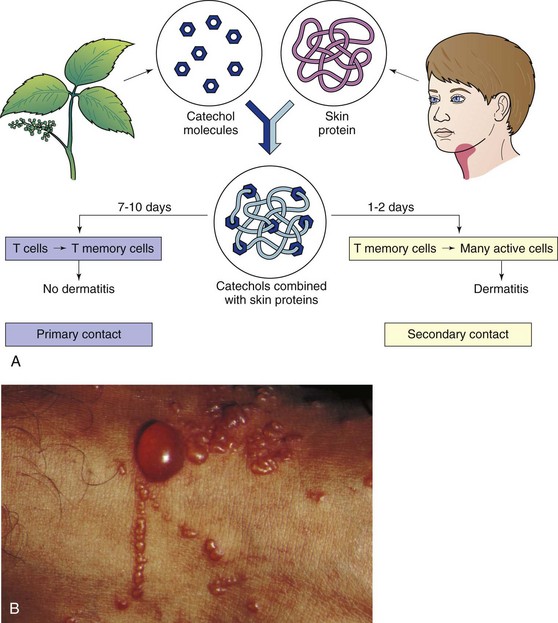
Fig. 18-11 A, Development of allergic contact dermatitis. B, Poison ivy lesions; note “streaked” blisters surrounding one large blister. (A, From McCance K, Huether S: Pathophysiology: the biological basis for disease in adults and children, ed 6, St Louis, 2010, Mosby. B, From Habif TP: Clinical dermatology: a color guide to diagnosis and therapy, ed 4, St Louis, 2004, Mosby.)
Therapeutic Management
Treatment of the lesions includes application of calamine lotion, soothing Burow solution compresses, and/or Aveeno baths to relieve discomfort. Topical corticosteroid gel is effective for prevention or relief of inflammation, especially when applied before blisters form. Oral corticosteroids may be needed for severe reactions, and a sedative such as diphenhydramine may be ordered.
Nursing Care Management
When the child has made contact with the plant, flush the area immediately (preferably within 15 minutes) with cold running water to neutralize the urushiol not yet bonded to the skin. If there is a stream nearby, an effective method is to have the child enter the water (clothes and all) and allow the water to rinse the oil from both skin and clothing. Use of harsh soap is contraindicated because it removes protective skin oils and dilutes the urushiol, allowing it to spread. Hard scrubbing irritates the skin. All clothing that has come in contact with the plant is removed with care and thoroughly laundered in hot water and detergent. Every effort is made to prevent the child from scratching the lesions. Although the lesions do not spread by contact with the blister serum or by scratching, the lesions can become secondarily infected (see Critical Thinking Exercise).
Prevention: Prevention is best accomplished by avoiding contact and removing the plant from the environment. Teach all children, especially those known to be sensitive, to recognize the plant. Information regarding means for destroying plants can be obtained from the U.S. Department of Agriculture or Forestry Service. Home garden sprays that kill broad-leaf plants or all vegetation (e.g., Roundup or Spectracide) are ineffective. If poisonous plants are growing in public community areas, the local authorities should be contacted to remove the plants.
Foreign Bodies
Small wooden splinters can be removed with a needle and tweezers that have been sterilized with alcohol or a flame. The area around the sliver is washed with soap and water before removal is attempted. The sliver is exposed with the needle and then grasped firmly by the tweezers and pulled out. Some foreign bodies, such as fishhooks, pieces of glass, difficult-to-see objects, or deeply embedded objects (such as a needle in a foot or near a joint), require medical evaluation.
Sunburn
Sunburn is a common skin injury caused by overexposure to ultraviolet (UV) light waves—either sunlight or artificial light in the UV range. The sun emits a continuous spectrum of visible and nonvisible light rays that range in wavelength from very short to very long. The shorter, higher-frequency wavelengths are more damaging than longer wavelengths, but much of the light is filtered out as it travels through the atmosphere. Of the light that does get through, ultraviolet A (UVA) waves are the longest and cause only minimum burning but play a significant role in photosensitive and photoallergic reactions. They are also responsible for premature aging of the skin and potentiate the effects of ultraviolet B (UVB) waves, which are shorter and responsible for tanning; burning; and most of the harmful effects attributed to sunlight, especially skin cancer.
Numerous factors influence the amount of UVB exposure. Maximum exposure occurs at midday (10 am to 3 pm), when the distance from the sun to a given spot on the earth is shortest. Solar intensity also varies with the seasons, time zones, and altitude. Exposure is greater at higher altitudes and near the equator and less when the sky is hazy (although its effect is easily underestimated). Window glass effectively screens out UVB but not UVA. Fresh snow, water, and sand reflect UV rays, especially when the sun is directly overhead.
Some persons are more susceptible to sunburn than others. The fibrous keratin of the outer epidermis and the pigment melanin, produced by the melanocytes of the innermost, or basal, layer of the epidermis, provide protection from the sun. Areas of the body with thick keratin layers (palms and soles) enjoy the greatest protection. The protective pigment layer decreases the intensity of all UV light by physically blocking and scattering the radiation. UV rays stimulate the melanocytes to produce more melanin, which turns the skin darker. After several days of exposure, the dark melanin absorbs most of the incoming UV radiation before the rays can cause further damage.
Persons with light skin and eyes produce melanin slowly and are more prone to burning, whereas those with very dark skin are able to tolerate more rays without damage. People with certain diseases (e.g., porphyria, lupus erythematosus) are more sensitive to the sun’s rays. Some substances increase the skin’s sensitivity; these include numerous medications (e.g., barbiturates, oral contraceptives, sulfonamides, antiepileptics), topical products (e.g., retinoic acid [Retin-A], antiseptic soap, aftershave lotions, perfumes, colognes), and certain foods containing photosensitizing chemicals (e.g., carrots, parsley, limes).
UV rays penetrate the skin surface, precipitate a chemical change in the cell molecules, and produce toxic by-products that irritate surrounding tissues. The result is redness, tissue swelling, increased capillary permeability, and the tenderness characteristic of superficial (first-degree) burns and the coagulation, necrosis, and blistering of partial-thickness (second-degree) burns. (See Burns, Chapter 29.) Sunburned skin is exquisitely sensitive, and severe sunburn may be accompanied by nausea, chills, fever, abdominal cramping, and headache. Dehydration may occur.
Excessive or long-term exposure to the sun permanently damages the skin. Ninety percent of skin cancers occur in areas of the skin that are exposed to sunlight, and rates of skin cancers are higher in parts of the world where sunlight is more intense. Studies have also shown that childhood is a crucial time for sun exposure. Children who immigrate to sunny climates after 10 years of age develop cancer at lower rates than native-born children. In general, children receive three times as much sun exposure as adults. Teenagers spend even more time in the sun than school-age children, and their desire for the “perfect tan” places their skin at high risk for sun damage.
Nursing Care Management
Treatment involves stopping the burning process, decreasing the inflammatory response, and rehydrating the skin. Local application of cool tap water soaks or immersion in a tepid water bath (temperature slightly below 36.7° C [98° F]) for 20 minutes or until the skin is cool limits tissue destruction and relieves the discomfort. After the cool applications, a bland oil-in-water moisturizing lotion can be applied, but petrolatum-based products that trap radiant heat in the tissues should be avoided. Acetaminophen is recommended for relief of discomfort. Partial-thickness burns are treated the same as those from any heat source.
Prevention: Protection from sunburn is the major goal of management, and the harmful effects of the sun on the delicate skin of infants and children have been receiving increased attention. Protection can be achieved by physical means (e.g., protective clothing and a hat) or by chemical means. Two types of products are available for sun protection: topical sunscreens, which partially absorb UV light, and sun blockers, which block out UV rays by reflecting sunlight. The most frequently recommended sun blockers are zinc oxide and titanium dioxide ointments.
Sunscreens are products with a sun protective factor (SPF) based on evaluation of effectiveness against UV rays. The SPF is indicated by a number such as 15. If individuals normally burn in 10 minutes without a sunscreen, use of a sunscreen with an SPF of 15 allows them to remain in the sun for 15 times 10, or 150 minutes ( hours), before acquiring the same degree of burn. Most sunscreens have an SPF ranging from 2 to more than 30; the higher the number, the greater the protection. Waterproof sunscreens with a minimum SPF of 15 are recommended. The SPF provides information primarily in relation to the effects of UVB, not UVA. Claims such as “broad spectrum” or “UVA-UVB sun block” are usually unsubstantiated. One agent that affords protection against UVA is Parsol 1789, found in Photoplex and Shade UVA Guard.
hours), before acquiring the same degree of burn. Most sunscreens have an SPF ranging from 2 to more than 30; the higher the number, the greater the protection. Waterproof sunscreens with a minimum SPF of 15 are recommended. The SPF provides information primarily in relation to the effects of UVB, not UVA. Claims such as “broad spectrum” or “UVA-UVB sun block” are usually unsubstantiated. One agent that affords protection against UVA is Parsol 1789, found in Photoplex and Shade UVA Guard.
The most effective sunscreens against UVB contain p-aminobenzoic acid (PABA) and PABA esters. PABA is more effective than PABA esters. It penetrates the outer layer of skin and may accumulate with repeated use; thus it provides protection even when the child is swimming or sweating. PABA may stain clothing; PABA esters are less likely to do so. However, PABA can cause an allergic response in sensitive persons, manifested as redness and itching 24 hours after application. Benzophenones also offer protection against UVA but are less effective than the PABA preparations and wash off easily. For best results, the sunscreen should be effective against both UVA and UVB.
The range of sunscreens available offers the consumer access to a type and combination to meet any need. Sunscreens are applied evenly to all exposed areas, with special attention to skinfolds and areas that might become exposed as clothing shifts. The FDA recommends a layer of sunscreen that is 2 mg/cm2. Direct parents to read labels of sunscreen products carefully for the SPF and follow the manufacturer’s directions for application.
Individuals who work in the community, such as teachers, daycare workers, coaches, youth group leaders, and children’s relatives, should all be made aware of sun safety for children. Sunscreens must be applied liberally.
It is wise to avoid direct sun exposure when solar radiation is at maximum intensity. The strongest radiation occurs when the sun is at its highest (directly overhead). Earlier or later in the day, when the sun is at a 45-degree angle, the earth’s atmosphere provides protection equivalent to an SPF of 2.4.
Sun damage is cumulative. Although most long-term effects (cancer, wrinkling) are not evident until adulthood, skin care must begin in childhood. Nurses should teach skin care as a basic practice that becomes a part of the child’s life, much the same as tooth brushing (see Community Focus box). Sun-protection behaviors should also be included in existing school health curricula and result in knowledge and a potential change in behavior (Geller, Rutsch, Kenausis, et al, 2003).
Cold Injury
Cold injuries are most commonly seen in very cold regions. The nature of the heat-regulating mechanisms of the body are such that the inner portion of the body, or core, produces heat and the periphery, or outer area, conserves or dissipates the heat. When the body attempts to conserve heat, the outer tissues are subjected to low temperatures, and local trauma may result.
Chilblain, redness and swelling of the skin, occurs when extremities, usually the hands, are exposed intermittently to temperatures of 1.1° to 15.5° C (30° to 60° F). The response may vary but is characterized by intense vasodilation that increases the temperature of involved tissues above that of unaffected tissue and produces edematous, reddish blue patches that itch and burn. As warming takes place, the sensations become more intense but ordinarily subside in a few days.
Frostbite is the term used to describe tissue damage caused when excessive heat loss to local tissues allows ice crystals to form in tissues. The mechanisms of slow and rapid freezing differ. Slow freezing causes ice crystals to form in the extracellular fluid, which leads to increased osmolality and movement of water from the cells. This causes cellular dehydration and destruction. Rapid freezing produces both extracellular and intracellular freezing and immediate cellular destruction. Rapid freezing takes place at high altitudes or with high conductivity from cold water immersion.
When frozen tissues thaw, the tissue damage is like that from a high-temperature burn—red blood cell aggregation, stasis, venous thrombosis, tissue edema and ischemic damage, increased tissue pressure, and death and necrosis of surrounding tissues. The frostbitten part appears white or blanched, feels solid, and is without sensation.
Rapid rewarming is associated with less tissue necrosis than slow thawing. It restores blood flow and shortens the period of cellular damage. Rewarming produces a flush (sometimes deep purple) and a return of sensation, which is extremely painful. Large blisters may appear 24 to 48 hours after rewarming and begin to resorb within 5 to 10 days, followed by the formation of a hard black eschar. Superficial injury often heals satisfactorily.
Therapeutic Management
Rewarming is accomplished by immersing the part in well-agitated water at 37.8° to 42.2° C (100° to 108° F). Discomfort is managed with analgesics and sedatives. Care of blistered skin is similar to that described for burns. It is seldom possible to estimate the extent of tissue loss until new skin layers are revealed after the eschar layer separates. Therefore amputation of extremities is usually delayed for 60 to 90 days unless there is evidence of gangrene.
Nursing Care Management
Transfer the frostbite victim to the nearest emergency treatment center. Protect injured parts from trauma and handle gently. Prevent the patient from ambulating on injured feet. Rubbing injured tissues is contraindicated and can cause damage by rupture of crystallized cells. After rewarming, apply a loose dressing. Dry heat is not applied. (See Burns, Chapter 29, and Pain Management, Chapter 7.)
Hypothermia
Hypothermia is defined as the cooling of the body’s core temperature (pulmonary artery or esophageal temperature) to injurious levels, usually identified as below 35° C (95° F). Hypothermia occurs in environmental settings when heat production by exercise and metabolism is less than heat lost by convection, conduction, or radiation. There is a 6% drop in blood flow for each 1° C (1.8° F) decrease in core temperature. Very young children with a large surface area relative to body mass and thin persons are at the greatest risk for hypothermia.
The body in positive heat balance conserves heat by alternating vasoconstriction and vasodilation in extremities. Threat of prolonged or severe cold exposure causes the body to conserve core temperature at the expense of the extremities by shunting warm blood to the core after it passes through the muscles of the extremities. Shivering contributes to warming by raising the metabolic rate to increase the heat of blood before it returns to the core. Clinical manifestations related to degree of hypothermia are listed in Table 18-8.
TABLE 18-8
PHYSICAL EFFECTS OF HYPOTHERMIA
| TEMPERATURE | CHARACTERISTICS |
| 35° C (95° F) | Increased respiratory rate, decreased intestinal motility; vigorous shivering; may be conscious and alert; task performance often impaired |
| 32° C (90° F) | May continue uncontrollable shivering or may begin to show muscular rigidity; decreased respiratory rate; atrial fibrillation; may still be conscious but sensorium changes evident; impaired cognition, reasoning, and speech; loss of manual skills and dexterity; brief vasodilation that causes flushes and warm sensation and possible confusion |
| 30° C (86° F) | Decreased cerebral blood flow; may show increased blood pressure (may be difficult to measure), tachycardia, and tachypnea; may have supraventricular arrhythmia, premature ventricular contractions, and T-wave inversion; usually conscious, but a loss of consciousness is preceded by irritability |
| 27° C (80.6° F) | Bradycardia and slowed respiratory rate; metabolic rate decreased by 50%; decreased oxygen uptake, CO2 production; ventricular fibrillation; rigid extremities |
| 25° C (77° F) | Hypotension; glomerular filtration and blood flow to kidneys reduced by 30% |
| 20° C (68° F) | Unconscious; nonfunctioning reflexes; unresponsive pupils; respirations barely detectable or undetectable; extremities and trunk cold to touch; abnormal electrocardiogram; pulse may decrease to 4 per min, progressing to cardiac standstill; flat electroencephalogram; dead appearance |
| 18° C (64.4° F) | Injury to peripheral tissue |