Health Problems of Toddlers and Preschoolers
INFECTIOUS DISORDERS, 453
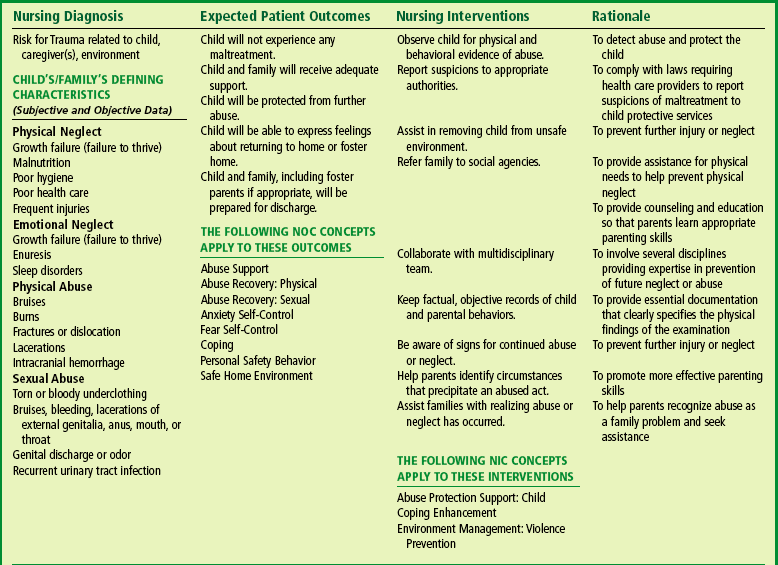
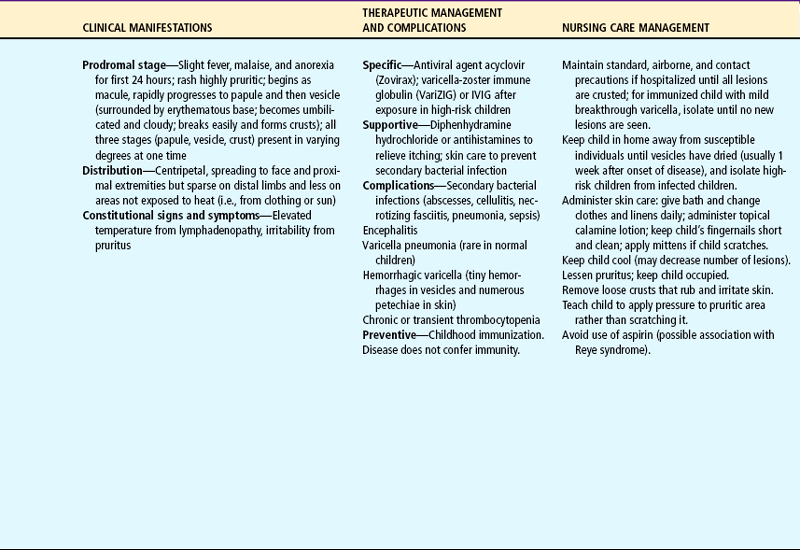
Chickenpox (varicella). A, Progression of disease. B, Simultaneous stages of lesions in chickenpox. C, Clinical view. (C, From Habif TP: Clinical dermatology: a color guide to diagnosis and therapy, ed 4, St Louis, 2004, Mosby.)

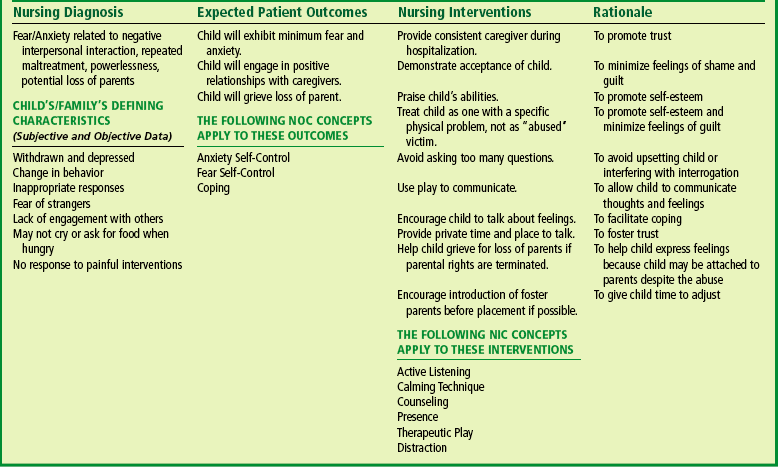
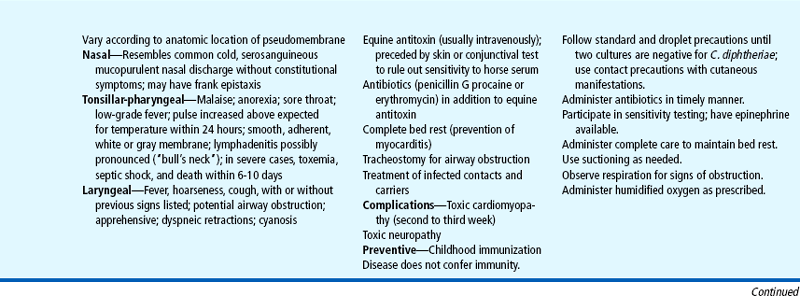
FIG. 14-2 Erythema infectiosum. (From Habif TP: Clinical dermatology: a color guide to diagnosis and therapy, ed 4, St Louis, 2004, Mosby.)
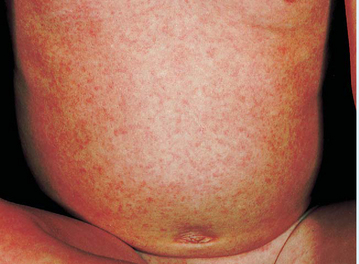
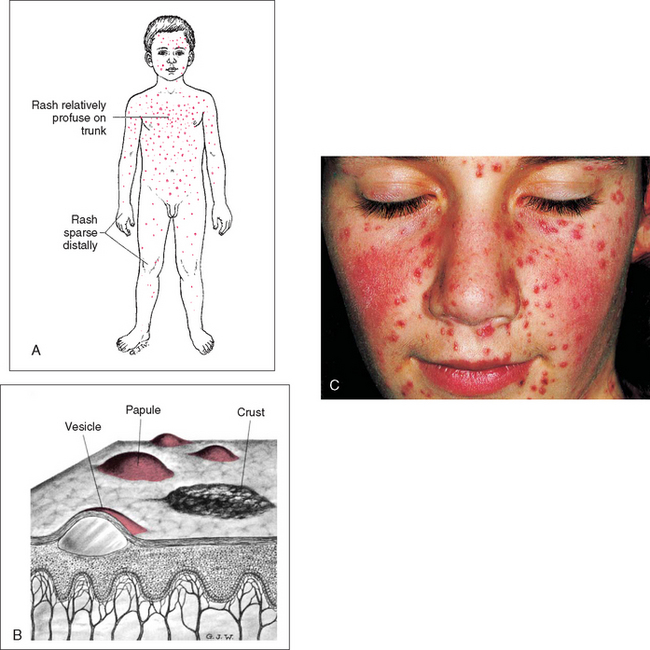
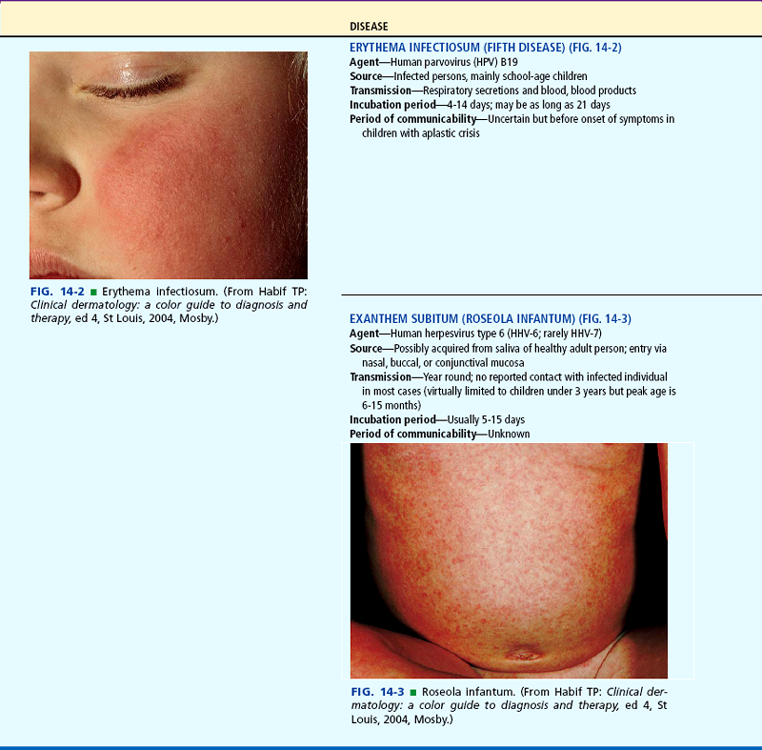
FIG. 14-3 Roseola infantum. (From Habif TP: Clinical dermatology: a color guide to diagnosis and therapy, ed 4, St Louis, 2004, Mosby.)
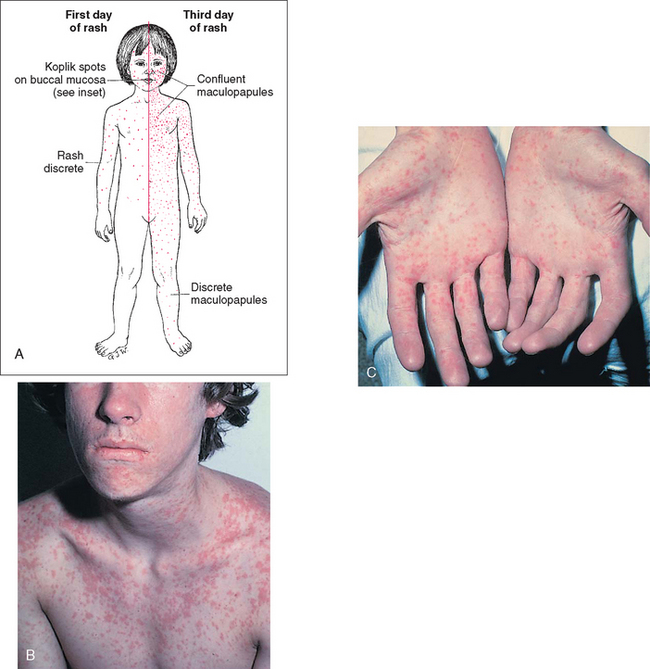
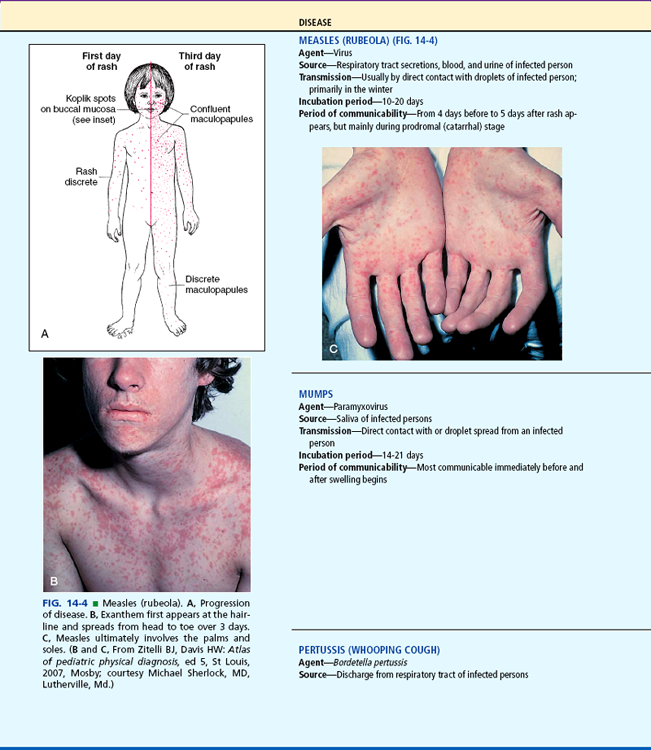
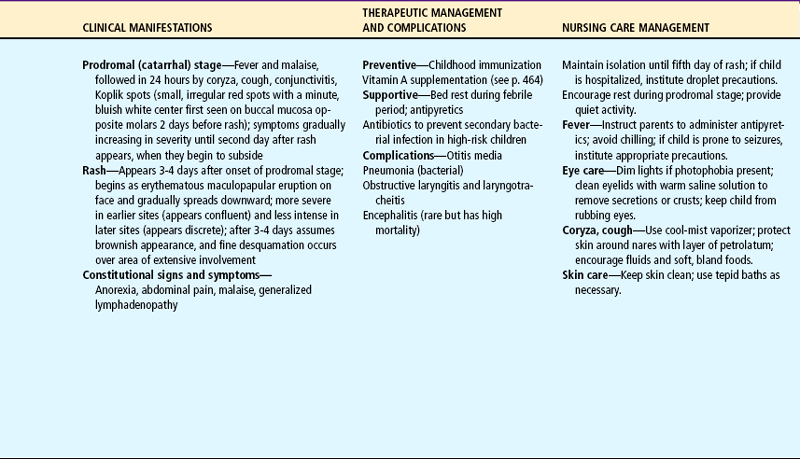
FIG. 14-4 Measles (rubeola). A, Progression of disease. B, Exanthem first appears at the hairline and spreads from head to toe over 3 days. C, Measles ultimately involves the palms and soles. (B and C, From Zitelli BJ, Davis HW: Atlas of pediatric physical diagnosis, ed 5, St Louis, 2007, Mosby; courtesy Michael Sherlock, MD, Lutherville, Md.)
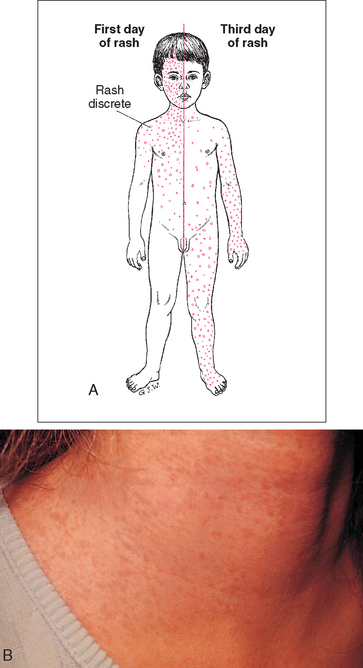
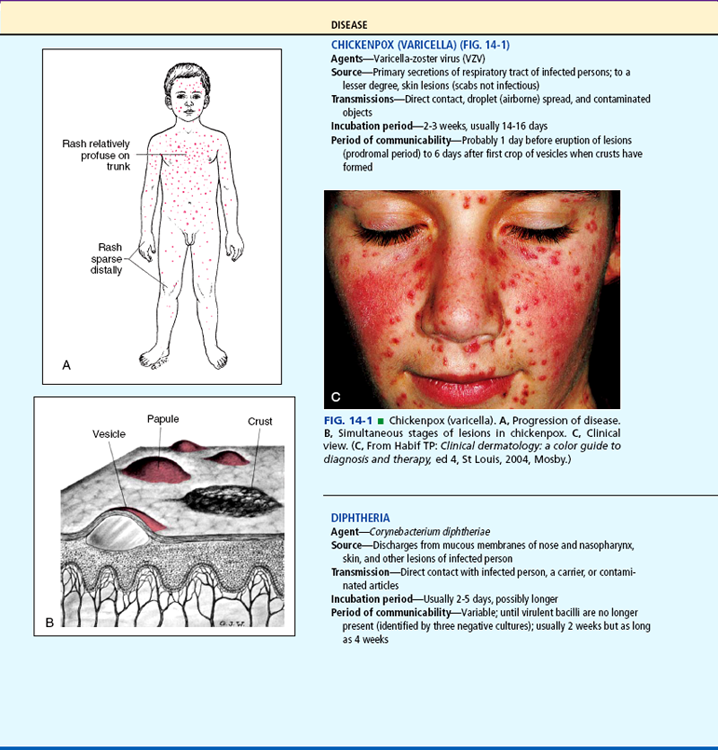
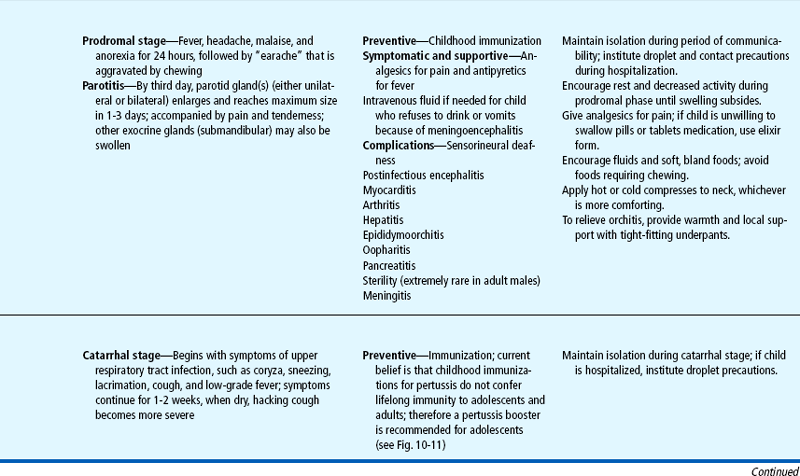
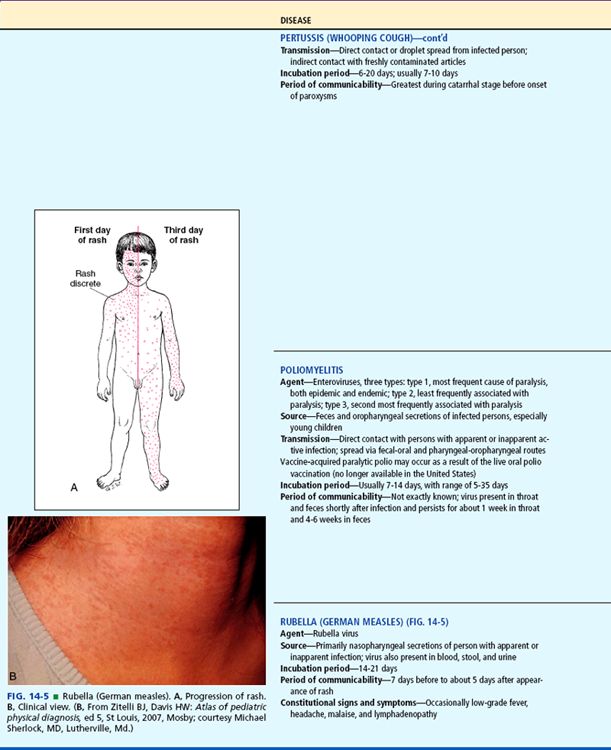
FIG. 14-5 Rubella (German measles). A, Progression of rash. B, Clinical view. (B, From Zitelli BJ, Davis HW: Atlas of pediatric physical diagnosis, ed 5, St Louis, 2007, Mosby; courtesy Michael Sherlock, MD, Lutherville, Md.)
On completion of this chapter the reader will be able to:
 Describe the major characteristics of communicable diseases of childhood.
Describe the major characteristics of communicable diseases of childhood.
 List three principles of nursing care of children with communicable disease.
List three principles of nursing care of children with communicable disease.
 Describe the nursing care of the child with conjunctivitis.
Describe the nursing care of the child with conjunctivitis.
 Distinguish between aphthous stomatitis and herpetic gingivostomatitis.
Distinguish between aphthous stomatitis and herpetic gingivostomatitis.
 Outline a teaching plan designed to prevent transmission of intestinal parasites.
Outline a teaching plan designed to prevent transmission of intestinal parasites.
 Identify the principles in the emergency treatment of poisoning.
Identify the principles in the emergency treatment of poisoning.
 Name four sources of lead in the environment.
Name four sources of lead in the environment.
 Describe the nursing care of the child with lead poisoning.
Describe the nursing care of the child with lead poisoning.
 State three factors thought to be associated with child abuse.
State three factors thought to be associated with child abuse.
 State four areas of the history that should arouse suspicion of abuse.
State four areas of the history that should arouse suspicion of abuse.
INFECTIOUS DISORDERS
The incidence of childhood communicable diseases has declined significantly since the advent of immunizations. Serious complications resulting from such infections have been further reduced with the use of antibiotics and antitoxins. However, infectious diseases do occur, and nurses must be familiar with the infectious agent to recognize the disease and to institute appropriate preventive and supportive interventions (Table 14-1). (See also Chapter 30 for a discussion of nursing care for dermatologic conditions.)
TABLE 14-1
Communicable Diseases of Childhood
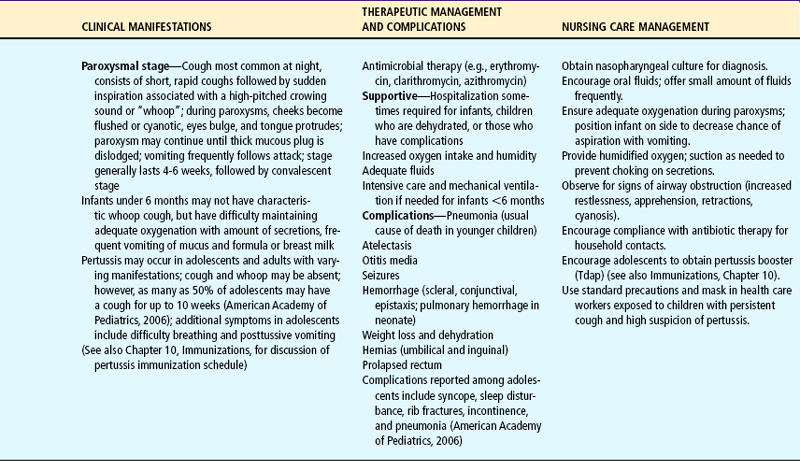
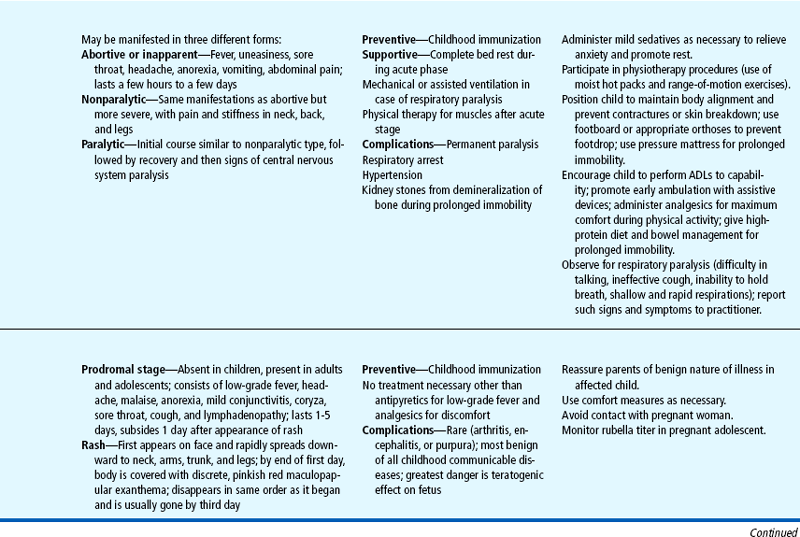
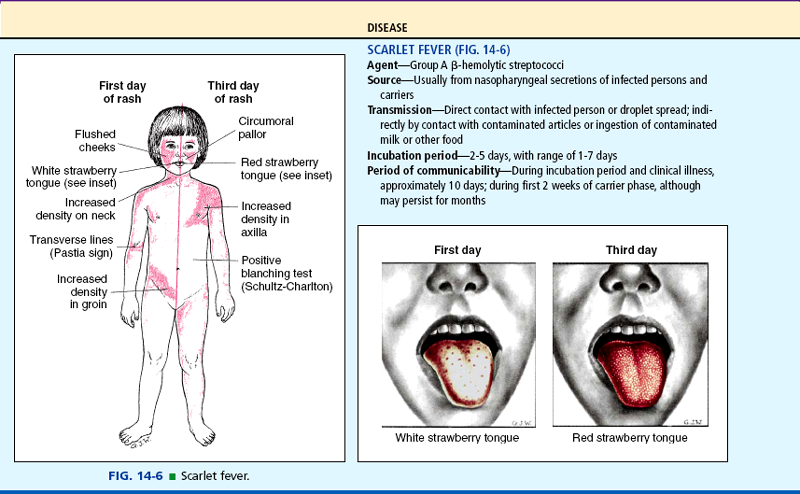
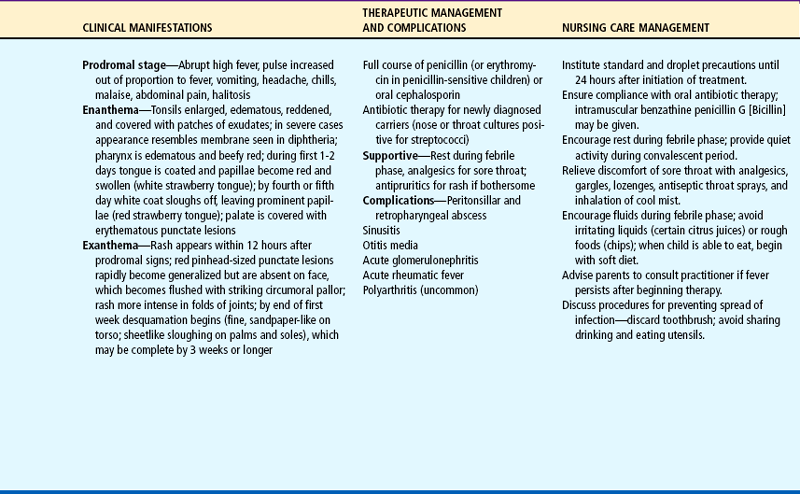
ADLs, Activities of daily living; IVIG, intravenous immune globulin.
Nursing Care Management
The more common communicable diseases of childhood, their therapeutic management, and specific nursing care are described in Table 14-1. The following is a general discussion of nursing care management for communicable diseases. The nursing process for care of the child with a communicable disease is outlined in the Nursing Process box.
Identification of the infectious agent is of primary importance to prevent exposure to susceptible individuals. Nurses in ambulatory care settings, child care centers, and schools are often the first persons to see signs of a communicable disease, such as a rash or sore throat. The nurse must operate under a high index of suspicion for common childhood diseases to identify potentially infectious cases and to recognize diseases that require medical intervention. An example is the common complaint of sore throat. Although most often a symptom of a minor viral infection, it can signal diphtheria or a streptococcal infection, such as scarlet fever. Each of these bacterial conditions requires appropriate medical treatment to prevent serious sequelae.
When a communicable disease is suspected, it is important to assess:
 Recent exposure to a known case
Recent exposure to a known case
 Prodromal symptoms (symptoms that occur between early manifestations of the disease and its overt clinical syndrome) or evidence of constitutional symptoms, such as a fever or rash (see Table 14-1)
Prodromal symptoms (symptoms that occur between early manifestations of the disease and its overt clinical syndrome) or evidence of constitutional symptoms, such as a fever or rash (see Table 14-1)
Immunizations are available for many diseases, and infection usually confers lifelong immunity; therefore the possibility of many infectious agents can be eliminated based on these two criteria.
Prevent Spread.: Prevention consists of two components: prevention of the disease and control of its spread to others. Primary prevention rests almost exclusively on immunization. (The nurse’s role in immunization of children is discussed in Chapter 10.)
Control measures to prevent spread of disease should include techniques to reduce risk of cross-transmission of infectious organisms between patients and to protect health care workers from organisms harbored by patients. If the child is hospitalized, the facility’s policies for infection control are followed (see Chapter 22). The most important procedure is hand washing. Persons directly caring for the child or handling contaminated articles must wash their hands and practice effective standard precautions in care of their patients.
The child is instructed to practice good hand-washing technique after toileting and before eating. For those diseases spread by droplets, the nurse instructs parents in measures to reduce airborne transmission. The child who is old enough should use a tissue to cover the face during coughing or sneezing; otherwise, the parent should cover the child’s mouth with a tissue and then discard it. The usual hygiene measures of not sharing eating and drinking utensils are stressed to the family.
Prevent Complications.: Although most children recover without difficulty, certain groups are at risk for serious, even fatal, complications from communicable diseases, especially the viral diseases chickenpox and erythema infectiosum (EI) (fifth disease) caused by human parvovirus (HPV) B19. Most healthy children are less likely to become infected from either of these viruses compared with children with immunodeficiency—those receiving steroid or other immunosuppressive therapy, those with a generalized malignancy such as leukemia or lymphoma, or those with an immunologic disorder—who are at risk for viremia from replication of the varicella-zoster virus (VZV)* in the blood. VZV is so named because it causes two distinct diseases: varicella (chickenpox) and zoster (herpes zoster or shingles). Varicella occurs primarily in children younger than 15 years of age. However, it leaves the threat of herpes zoster, an intensely painful varicella that is localized to a single dermatome (body area innervated by a particular segment of the spinal cord). In children the dermatomes most likely affected by herpes zoster are the cervical and sacral dermatomes (Leung, Robson, and Leong, 2006). Immunocompromised patients and healthy infants younger than 1 year of age (who also have reduced immunity) are at a higher risk for reactivation of VZV causing herpes zoster, probably as a result of a deficiency in cellular immunity (Chen, George, Woodruff, and others, 2002). Complications of herpes zoster virus in children include secondary bacterial infection, depigmentation, and scarring; postherpetic neuralgia in children is uncommon (Leung, Robson, and Leong, 2006).
Children with hemolytic disease, such as sickle cell disease, are at risk for aplastic anemia from EI. HPV B19 infects and lyses red blood cell precursors, thus interrupting the production of red blood cells. Therefore the virus may precipitate a severe aplastic crisis in patients who need increased red blood cell production to maintain normal red blood cell volumes; thrombocytopenia and neutropenia may also occur as a result of HPV B19 infection. The fetus has a relatively high rate of red blood cell production and an immature immune system; it may develop severe anemia and hydrops as a result of maternal HPV infection. Fetal death rates as a result of HPV B19 have been estimated to be between 2% and 6% (American Academy of Pediatrics, 2006).
In the past decade there has been an increase in the cases of pertussis, particularly in infants less than 6 months old and in children 10 to 14 years of age. Early clinical manifestations of pertussis in infants may include gagging, coughing, emesis, and apnea; the typical “whoop” associated with the disease is absent (American Academy of Pediatrics, 2006). In older children the disease may manifest as a common cold (see Table 14-1). There is now a recommendation that children ages 11 to 18 receive a booster pertussis vaccine (Tdap) to prevent the disease (see Immunizations, Chapter 10). Because pertussis is contagious, especially among close household members, pertussis should be identified early and treatment initiated for the child and those who have been exposed. Azithromycin (for infants under 1 month) and erythromycin are administered to infants and children with pertussis (American Academy of Pediatrics, 2006).
Prevention of complications from diseases such as diphtheria, pertussis, and scarlet fever requires compliance with antibiotic therapy. With oral preparations the need to complete the entire course of therapy is stressed (see Compliance, Chapter 22). The use of varicella-zoster immune globulin (VariZIG) or immune globulin intravenous (IGIV) is recommended for children who are immunocompromised, who have no previous history of varicella, and who are likely to contract the disease and have complications as a result (American Academy of Pediatrics, 2006). The antiviral agent acyclovir (Zovirax) may be used to treat varicella infections in susceptible immunocompromised persons; it is effective in decreasing the number of lesions; shortening the duration of fever; and decreasing itching, lethargy, and anorexia. Oral acyclovir should be considered for susceptible pregnant women, immunocompromised children without a history of varicella disease, newborns whose mother had varicella within 5 days before delivery or within 48 hours after delivery, and hospitalized preterm infants with significant varicella exposure (American Academy of Pediatrics, 2006).
Evidence suggests that vitamin A supplementation reduces both morbidity and mortality in measles and that all children with severe measles should be given vitamin A supplements. A single oral dose of 200,000 IU for children at least 1 year old (use half that dose for children 6 to 12 months of age) is recommended. The higher dose may be associated with vomiting and headache for a few hours. The dose should be repeated the next day and at 4 weeks for children with ophthalmologic evidence of vitamin A deficiency (American Academy of Pediatrics, 2006).
Provide Comfort.: Many communicable diseases cause skin manifestations that are bothersome to the child. The chief discomfort from most rashes is itching, and measures such as cool baths (usually without soap) and lotions (e.g., calamine) are helpful.
To avoid overheating, which increases itching, children should wear lightweight, loose, nonirritating clothing and keep out of the sun. If the child persists in scratching, the nails are kept short and smooth; mittens and clothes with long sleeves or legs may be needed. For severe itching, antipruritic medication, such as diphenhydramine (Benadryl) or hydroxyzine (Atarax), may be required, especially when the child has trouble sleeping because of itching. Loratadine, cetirizine, and fexofenadine do not cause drowsiness and may be preferred for urticaria during the day.
An elevated temperature is common, and both antipyretic medicine (acetaminophen or ibuprofen) and environmental manipulation are implemented (see Controlling Elevated Temperature, Chapter 22). The acetaminophen is effective in lowering the fever but does not significantly reduce the symptoms of itching, anorexia, abdominal pain, fussiness, or vomiting.
A sore throat, another frequent symptom, is managed with lozenges, saline rinses (if the child is old enough to cooperate), and analgesics. Because most children are anorectic during an illness, bland foods and increased liquids are usually preferred. During the early stages of the disease, children voluntarily curtail their activity, and although bed rest is beneficial, it should not be imposed unless specifically indicated. During periods of irritability, quiet activity (e.g., reading, music, television, video games, puzzles, coloring) helps distract children from the discomfort.
Support Child and Family.: Most communicable diseases are benign, but may produce considerable concern and anxiety for parents. Often the occurrence of a disease such as chickenpox is the first time the child is acutely uncomfortable. Parents need assistance to cope with manifestations of the illness, such as intense itching. The family and child need reassurance that recovery is generally rapid. However, visible signs of the dermatosis may be present for some time after the child is well enough to resume usual activities.
CONJUNCTIVITIS
Acute conjunctivitis (inflammation of the conjunctiva) occurs from a variety of causes that are typically age related. In newborns conjunctivitis can occur from infection during birth, most often from Chlamydia trachomatis (inclusion conjunctivitis) or Neisseria gonorrhoeae. These organisms, as well as herpes simplex virus (HSV), cause serious ocular damage. In infants recurrent conjunctivitis may be a sign of nasolacrimal (tear) duct obstruction. A chemical conjunctivitis may occur within 24 hours of instillation of neonatal ophthalmic prophylaxis; the clinical features include mild lid edema and a sterile, nonpurulent eye discharge (Fuloria and Kreiter, 2002). In children the usual causes of conjunctivitis are viral, bacterial, allergic, or related to a foreign body. Bacterial infection accounts for most instances of acute conjunctivitis in children. Diagnosis is made primarily from the clinical manifestations (Box 14-1), although cultures of purulent drainage may be needed to identify the specific cause.
Therapeutic Management
Treatment of conjunctivitis depends on the cause. Viral conjunctivitis is self-limiting, and treatment is limited to removal of the accumulated secretions. Bacterial conjunctivitis has traditionally been treated with topical antibacterial agents such as polymyxin and bacitracin (Polysporin), sodium sulfacetamide (Sulamyd), or trimethoprim and polymyxin (Polytrim). However, in one study of children with acute infective conjunctivitis treated by placebo vs topical chloramphenicol, there was little difference in cure rates; the authors concluded that most children will get better without antibiotic treatment (Rose, Harnden, Brueggemann, and others, 2005). Fluoroquinolones, approved for children ages 1 year and older, are viewed by ophthalmologists as the best ophthalmic antimicrobial agents available (Lichtenstein, Rinehart, and Levofloxacin Bacterial Conjunctivitis Study Group, 2003). Drops may be used during the day and an ointment at bedtime because the ointment preparation remains in the eye longer. Ointments are usually not used in the daytime because they blur vision. Corticosteroids are avoided because they reduce ocular resistance to bacteria.
Nursing Care Management
Nursing care includes keeping the eye clean and properly administering ophthalmic medication. Accumulated secretions are always removed by wiping from the inner canthus downward and outward, away from the opposite eye. Warm, moist compresses, such as a clean washcloth wrung out with hot tap water, are helpful in removing the crusts. Compresses are not kept on the eye because an occlusive covering promotes bacterial growth. Medication is instilled immediately after the eyes have been cleaned and according to correct procedure (see Chapter 22).
Prevention of infection in other family members is an important consideration with bacterial conjunctivitis. The child’s washcloth and towel are kept separate from those used by others. Tissues used to clean the eye are discarded. The child should refrain from rubbing the eye and is instructed in good hand-washing technique.
STOMATITIS
Stomatitis is inflammation of the oral mucosa, which may include the buccal (cheek) and labial (lip) mucosa, tongue, gingiva, palate, and floor of the mouth. It may be infectious or noninfectious and may be caused by local or systemic factors. In children aphthous stomatitis and herpetic stomatitis are typically seen. Children with immunosuppression and those receiving chemotherapy or head and neck radiotherapy are at high risk for developing mucosal ulceration and herpetic stomatitis.
Aphthous stomatitis (aphthous ulcer, canker sore) is a benign but painful condition whose cause is unknown. Its onset is usually associated with mild traumatic injury (biting the cheek, hitting the mucosa with a toothbrush, or a mouth appliance rubbing on the mucosa), allergy, or emotional stress. The lesions are painful, small, whitish ulcerations surrounded by a red border. They are distinguished from other types of stomatitis by healthy adjacent tissues, absence of vesicles, and no systemic illness. The ulcers persist for 4 to 12 days and heal uneventfully.
Herpetic gingivostomatitis (HGS) is caused by HSV, most often type 1, and may occur as a primary infection or recur in a less severe form known as recurrent herpes labialis (commonly called cold sores or fever blisters). The primary infection usually begins with a fever; the pharynx becomes edematous and erythematous; and vesicles erupt on the mucosa, causing severe pain (Fig. 14-7). Cervical lymphadenitis often occurs, and the breath has a distinctly foul odor. In the recurrent form the vesicles appear on the lips, usually singly or in groups. The precipitating factors for the cold sores include emotional stress, trauma (often related to dental procedures), immunosuppression, or exposure to excessive sunlight. The disease can last 5 to 14 days, with varying degrees of severity.
Stomatitis may occur as a manifestation of hand-foot-and-mouth disease and herpangina; both manifest with scattered vesicles on the buccal mucosa and are commonly caused by the nonpolio enteroviruses (primarily coxsackieviruses). Children with either hand-foot-and-mouth or herpangina often have poor intake as a result of the mouth sores.
Therapeutic Management
Treatment for all types of stomatitis is aimed at relief of symptoms, primarily pain. Acetaminophen and ibuprofen are usually sufficient for mild cases, but with more severe HGS, stronger analgesics such as codeine may be needed. Topical anesthetics are helpful and include over-the-counter preparations such as Orabase, Anbesol, and Kank-A. Lidocaine (Xylocaine Viscous) can be prescribed for the child who can keep 1 teaspoon of the solution in the mouth for 2 to 3 minutes and then expectorate the drug. A mixture of equal parts of diphenhydramine elixir and Maalox (aluminum and magnesium hydroxide) provides mild analgesia, antiinflammatory properties, and a protective coating for the lesions. Sucralfate can also be used as a coating agent for oral mucous membranes. Specific treatment for children with severe cases of HGS is the use of antiviral agents such as acyclovir (Faden, 2006).
Nursing Care Management
The chief nursing goals for children with stomatitis are relief of pain and prevention of spread of the herpes virus. Analgesics and topical anesthetics are used as needed to provide relief, especially before meals to encourage food and fluid intake. For younger infants and toddlers who cannot swish and swallow, the diphenhydramine and Maalox solution may be applied with a cotton-tipped applicator before feedings to minimize pain. Educating parents regarding the use of these medications is important to maintain adequate hydration in the child whose mouth is too sore to take liquids. Drinking bland fluids through a straw is helpful in avoiding the painful lesions. Mouth care is encouraged; the use of a very soft bristle toothbrush or disposable foam-tipped toothbrush provides gentle cleaning near ulcerated areas.
Careful hand washing is essential when caring for children with HGS. Because the infection is autoinoculable, children should keep their fingers out of the mouth; contaminated hands can infect other body parts. Very young children may require elbow restraints to ensure compliance. Articles placed in the mouth are cleaned thoroughly. Newborns and individuals with immunosuppression should not be exposed to infected children.
Because herpes infection is often associated with sexual transmission, the nurse should explain to parents and older children that HGS is usually caused by type 1 HSV, the type not associated with sexual activity.
INTESTINAL PARASITIC DISEASES
Intestinal parasitic diseases, including helminths (worms) and protozoa, constitute the most frequent infections in the world. In the United States the incidence of intestinal parasitic disease, especially giardiasis, has increased among young children who attend daycare centers. Young children are especially at risk because of typical hand-mouth activity and uncontrolled fecal activity.
Intestinal parasitic diseases in humans are caused by various infecting organisms. This discussion is limited to the two most common parasitic infections among children in the United States: giardiasis and pinworms. Table 14-2 describes the outstanding features of selected helminths that belong to the family of nematodes.
GENERAL NURSING CARE MANAGEMENT
Nursing responsibilities related to intestinal parasitic infections involve assistance with identification of the parasite, treatment of the infection, and prevention of initial infection or reinfection. Identification of the organism is accomplished by laboratory examination of substances containing the worm, its larvae, or ova. Most are identified by examining fecal smears from the stools of persons suspected of harboring the parasite. Fresh specimens are best for revealing parasites or larvae; therefore collected specimens should be taken directly to the laboratory for examination. If this is not feasible, the specimen is placed in a container with a preservative. Parents need clear instructions on obtaining an adequate sample and the number of samples required (see Stool Specimens, Chapter 22). In most parasitic infections, examination of other family members, especially children, may be carried out to identify those who are similarly affected.
After the diagnosis is confirmed and appropriate treatment is planned, parents need further explanation and reinforcement. Compliance in terms of drug therapy and other measures, such as thorough hand washing, is essential for eradication of the parasite. The family needs to understand the nature of transmission and that in some cases the medication must be repeated in 2 weeks to 1 month to kill organisms hatched since initial treatment.
The nurse’s most important function is preventive education of children and families regarding hygiene and health habits. Thorough hand washing before eating or handling food and after using the toilet is the most important precautionary method. Other preventive practices are listed in the Community Focus box.
GIARDIASIS
Giardiasis is caused by the protozoan Giardia lamblia (also called Giardia intestinalis, Giardia duodenalis, and Lamblia intestinalis). It is the most common intestinal parasitic pathogen in the United States. Child care centers and institutions providing care for persons with developmental disabilities are common sites for urban giardiasis, and the children may pass cysts for months. Giardiasis should also be considered in those with a history of recent travel to an endemic area (Pickering, 2004).
The potential for transmission is great, because the cysts—the nonmotile stage of the protozoa—can survive in the environment for months. Chief modes of transmission are person to person; contaminated water, especially in mountain lakes and streams and swimming or wading pools frequented by diapered infants; food; and animals, especially puppies. In children, person-to-person transmission is the most likely cause. Although individuals infected with giardiasis may be asymptomatic, common symptoms include abdominal cramps and diarrhea (Box 14-2).
Diagnosis of giardiasis may be made by microscopic examination of stool specimens or duodenal fluid, or by identification of G. lamblia antigens in these specimens by techniques such as enzyme immunoassay (EIA). Because the Giardia organisms live in the upper intestine and are excreted in a highly variable pattern, repeated microscopic examination of stool specimens may be required to identify trophozoites (active parasites) or cysts. Duodenal specimens are obtained by direct aspiration, biopsy, orthe string test. In the string test, the child swallows a gelatin capsule with a nylon string attached. Several hours later, the string is withdrawn and the contents are sent for laboratory analysis. With the availability of EIA techniques to identify Giardia antigens in stool specimens, other tests are being used less often.
Therapeutic Management
The drugs of choice for treatment of giardiasis are metronidazole (Flagyl), tinidazole (Tindamax), and nitazoxanide (Alinia). Tinidazole is said to have an 80% to 100% cure rate after a single dose (American Academy of Pediatrics, 2006). Metronidazole and tinidazole have a metallic taste as well as gastrointestinal side effects, including nausea and vomiting. Nitazoxanide has no bitter taste and should be taken with food to avoid gastrointestinal symptoms. Albendazole is also used to treat the disease and reportedly has fewer side effects than metronidazole (American Academy of Pediatrics, 2006).
Nursing Care Management
The most important nursing consideration is prevention of giardiasis and education of parents, child care center staff, and those who are entrusted with the daily care of small children. Attention to meticulous sanitary practices, especially during diaper changes, is essential (see Community Focus box and Fig. 14-8). Nurses can play an important role in educating parents of small children and daycare staff regarding appropriate sanitation practices (see Preschool and Kindergarten Experience, Chapter 13). In addition young children who are infected or who have diarrhea should be discouraged from swimming in community or private pools until they are infection-free. Lakes and streams may contain high numbers of Giardia spore cysts, which can be swallowed in the water. Children are discouraged from swimming in stagnant bodies of water, and in water where there are known infected children swimming when there is a high chance of swallowing water. Giardia organisms are said to be resistant to chlorine (Hlavsa, Watson, and Beach, 2005). Parents are encouraged to take small children to the restroom frequently when swimming, to avoid letting children in diapers in swimming areas, and to change diapers away from the water source (see also Centers for Disease Control information on recreational water illnesses*). After children are infected, family education regarding drug administration is essential.

FIG. 14-8 Prevention of giardiasis, especially in daycare centers, requires sanitary practices during diaper changes, such as discarding paper diapers in a covered receptacle, changing paper covers on the diaper-changing surface, and having facilities for hand washing nearby. NOTE: Soiled cloth diapers and clothing should be stored in a plastic bag for transport home.
ENTEROBIASIS (PINWORMS)
Enterobiasis, or pinworms, caused by the nematode Enterobius vermicularis, is the most common helminthic infection in the United States. It is universally present in temperate climatic zones and may infect more than 30% of all children at any one time. Crowded conditions, such as in classrooms and daycare centers, favor transmission.
Infection begins when the eggs are ingested or inhaled (the eggs float in the air). The eggs hatch in the upper intestine, then mature and migrate through the intestine. After mating, adult females migrate out the anus and lay eggs (American Academy of Pediatrics, 2006). The movement of the worms on skin and mucous membrane surfaces causes intense itching. As the child scratches, eggs are deposited on the hands and underneath the fingernails. The typical hand-to-mouth activity of young children makes them especially prone to reinfection. Pinworm eggs persist in the indoor environment for 2 to 3 weeks, contaminating anything they contact, such as toilet seats, doorknobs, bed linen, underwear, and food. Except for the intense rectal itching associated with pinworms, the clinical manifestations are nonspecific (Box 14-3).
Diagnostic Evaluation
Diagnosis is most commonly made from the tape test (see Nursing Care Management). Repeated tests to collect eggs may be necessary, and if there is a possibility that other family members may be infected, a tape test should be performed on them.
Therapeutic Management
The drugs available for treatment of pinworms include mebendazole (Vermox), pyrantel pamoate (Pin-Rid, Antiminth), and albendazole. The drug of choice is mebendazole, which is safe, effective, and convenient, with few side effects. However, it is not recommended for children younger than 2 years of age. If pyrvinium pamoate is prescribed, parents are advised that the drug stains stool and vomitus bright red, as well as clothing or skin that comes in contact with the drug; it is available without prescription and should not be used in children under 2 years without consulting the primary practitioner. Because pinworms are easily transmitted, all household members are treated. The dose of antiparasitic medication should be repeated in 2 weeks to completely eradicate the parasite and prevent reinfection.
Nursing Care Management
Nursing care is directed at identifying the parasite, eradicating the organism, and preventing reinfection. Parents need clear, detailed instructions for the tape test. A loop of transparent (not “frosted” or “magic”) tape, sticky side out, is placed around the end of a tongue depressor, which is then firmly pressed against the child’s perianal area. A convenient, commercially prepared tape is also available for this purpose. Pinworm specimens are collected in the morning as soon as the child awakens and before the child has a bowel movement or bathes. The procedure may need to be performed on 3 or more consecutive days before eggs are collected. Parents are instructed to place the tongue blade in a glass jar or loosely in a plastic bag so that it can be brought in for microscopic examination. For specimens collected in the hospital, practitioner’s office, or clinic, the tape is placed smoothly on a glass slide, sticky side down, for examination.
Adherence to the drug regimen is usually excellent because the duration of treatment is typically only one dose. However, the family is reminded of the need to take a second dose in 2 weeks to ensure eradication of the eggs.
To prevent reinfection, washing all clothes and bed linens in hot water and vacuuming the house may be recommended. However, there is little documentation on the effectiveness of these measures, since pinworms survive on many surfaces. Helpful suggestions include hand washing after toileting and before eating, keeping the child’s fingernails short to minimize the chance of ova collecting under the nails, dressing children in one-piece sleeping outfits, and daily showering rather than tub bathing. Families should be informed that recurrence is common. Repeated infections should be treated in the same manner as the first one.
INGESTION OF INJURIOUS AGENTS
Since the passage of the Poison Prevention Packaging Act of 1970, which requires that certain potentially hazardous drugs and household products be sold in child-resistant containers, the incidence of poisonings in children has decreased dramatically. However, despite these advances, poisoning remains a significant health concern, with most cases (51% in 2004) occurring in children younger than 6 years of age. Although pharmaceuticals such as analgesics, cough and cold preparations, topical preparations, antibiotics, vitamins, gastrointestinal preparations, hormones, and antihistamines are frequently the agents of poisonings, children may be poisoned by a variety of substances. The most frequently ingested poisons include (Watson, Litovitz, Rodgers, and others, 2005; Litovitz, Klein-Schwartz, White, and others, 2000; Powers, 2000):
 Cosmetics and personal care products (perfume, cologne, aftershave)*
Cosmetics and personal care products (perfume, cologne, aftershave)*
 Cleaning products (hypochlorite [“household”] bleach, pine oil disinfectants)
Cleaning products (hypochlorite [“household”] bleach, pine oil disinfectants)
 Plants (nontoxic gastrointestinal irritants, oxalates) (Box 14-4)
Plants (nontoxic gastrointestinal irritants, oxalates) (Box 14-4)
 Foreign bodies, toys, and miscellaneous substances (desiccants, thermometers, bubble-blowing solutions)
Foreign bodies, toys, and miscellaneous substances (desiccants, thermometers, bubble-blowing solutions)
Many poisonings reflect the ready accessibility of the product in the home, where more than 90% of poisonings occur, although a significant number take place elsewhere, such as in a grandparent’s or friend’s home, in a school, or in a health care facility.
The developmental characteristics of young children predispose them to poisoning by ingestion. Infants and toddlers explore their environment through oral experimentation. Because the sense of taste is not discriminating at this age, many unpalatable substances are ingested. In addition, toddlers and preschoolers are developing autonomy and initiative, which increase their curiosity and noncompliant behavior. Imitation is also a powerful motivator, especially when combined with lack of awareness of danger.
This section is primarily concerned with the immediate emergency treatment of ingestion of injurious agents. Specific management of corrosive, hydrocarbon, acetaminophen, salicylate, iron, and plant poisoning is summarized in Box 14-5. Because of the importance of lead poisoning among young children, ingestion of lead is discussed separately. Appropriate suggestions for poison prevention are discussed on p. 474 and in Chapter 12.
PRINCIPLES OF EMERGENCY TREATMENT
A poisoning may or may not require emergency intervention, but in every instance medical evaluation is necessary to initiate appropriate action. Parents are advised to call the poison control center (PCC) before initiating any intervention. The local PCC telephone number (usually listed in the front of the telephone directory) should be posted near each phone in the house* (see Critical Thinking Exercise and Emergency Treatment box).
Based on the initial telephone assessment, the PCC counsels the parents to begin treatment at home or to take the child to an emergency facility. When a call is taken, the name and telephone number of the caller is recorded to reestablish contact if the connection is interrupted. Because most poisonings are managed in the home, expert advice is essential in minimizing adverse effects. When the exact quantity or type of ingested toxin is not known, admission to a health care facility with pediatric emergency treatment services for laboratory evaluation and surveillance is critical during the time after ingestion.
Assessment
The first and most important principle in dealing with a poisoning is to treat the child first, not the poison. This requires an immediate concern for life support. Vital signs are taken, and respiratory or circulatory support is instituted as needed. The child’s condition is routinely reevaluated. Because shock is a complication of several types of household poisons, particularly corrosives, measures to reduce the effects of shock, beginning with the ABCs (airway, breathing, circulation) of resuscitation, are important. Establishing and maintaining vascular access for rapid intravascular volume expansion is vital in the treatment of pediatric shock.
The emergency department nurse’s responsibility is to be prepared for immediate intervention with all of the necessary equipment. Because time and speed are critical factors in recovery from serious poisonings, anticipation of potential problems and complications may mean the difference between life and death.
Gastric Decontamination
In general, the immediate treatment is to remove the ingested poison by adsorbing the toxin with activated charcoal, performing gastric lavage, or increasing bowel motility (catharsis). Because of continuing controversy regarding the use of these methods, each toxic ingestion should be treated individually (Abruzzi and Stork, 2002). Specific antidotes may be administered for certain poisonings. Syrup of ipecac, an emetic that exerts its action through irritation of the gastric mucosa and by stimulation of the vomiting center, is no longer recommended for immediate treatment of poison ingestion (American Academy of Clinical Toxicology and European Association of Poisons Centres and Clinical Toxicologists, 2004b; American Academy of Pediatrics, 2003). The American Academy of Pediatrics (2003) recommends that existing ipecac in the home be disposed of safely and that the first action for a caregiver of a child who may have ingested a toxic substance is to consult the local PCC. If the PCC cannot be reached, the child should be taken to the nearest emergency department.
Ipecac is contraindicated because it may cause prolonged vomiting (up to 12 hours), which makes it relatively contraindicated in ingestions that may cause sedation, coma, or seizures (Powers, 2000). Medications such as calcium channel blockers and benzodiazepines either produce a rapid onset of adverse symptoms (e.g., sedation, seizures, coma) or exaggerate the vagal response induced by gagging, which can lead to significant bradycardia. Under either circumstance, uncontrolled vomiting becomes an undesirable and unsafe event.
No emetic or other substance should be given at home without consultation with a PCC or physician.
If the child is admitted to an emergency facility, gastric lavage may be performed to empty the stomach of the toxic agent; however, this procedure is associated with serious complications (gastrointestinal perforation, hypoxia, aspiration) and it is no longer recommended in all cases of ingestion. There is no conclusive evidence that gastric lavage decreases morbidity (Criddle, 2007; Heard, 2005). In addition, gastric lavage may be of little use if used beyond 1 hour of ingestion (Heard, 2005). Conditions that may be appropriate for the use of gastric lavage include presentation within 1 hour of ingestion of a toxin, ingestion in patient who has decreased gastrointestinal motility, the ingestion of a toxic amount of sustained-release medication, and a massive or life-threatening amount of poison (Criddle, 2007). When gastric lavage is used, the patient requires a protected airway, possible sedation, and the largest-diameter tube that can be inserted to facilitate passage of gastric contents.
A more commonly used method of gastrointestinal decontamination is the use of activated charcoal, an odorless, tasteless, fine black powder that adsorbs many compounds, creating a stable complex. Activated charcoal may replace ipecac as the home remedy of choice (Bond, 2002), but the American Academy of Pediatrics (2003) suggests it is premature to recommend the administration of activated charcoal in the home. Activated charcoal is mixed with water or a saline cathartic to form a slurry. Slurries are neither gritty nor distasteful but resemble black mud. To increase the child’s acceptance of activated charcoal, the nurse should mix it with diet soda and serve it through a straw in an opaque container with a cover (such as a disposable coffee cup and lid) or an ordinary cup covered with aluminum foil or placed inside a small paper bag. In one small study, healthy adolescents preferred the taste of activated charcoal mixed with Coca-Cola or chocolate milk mixture instead of water (Cheng and Ratnapalan, 2007). For small children a nasogastric tube may be required to administer activated charcoal.
Potential complications from the use of activated charcoal include aspiration (usually in patients with impaired gag reflexes), constipation, and intestinal obstruction (in multiple doses). Superactivated charcoal products for gastric decontamination are reported to be more palatable and just as effective (Criddle, 2007; Heard, 2005). Cathartics, such as sorbitol, sodium, or magnesium, may be administered to stimulate evacuation of the bowel, thus decreasing systemic absorption of the poison and aiding in the removal of the charcoal. Many commercial preparations of activated charcoal contain cathartics. However, the use of cathartics is controversial, and the American Academy of Clinical Toxicology and European Association of Poisons Centres and Clinical Toxicologists (2004a) do not recommend their use in children. The Evidence-Based Practice box reviews recent literature on the use of gastric lavage in comparison to activated charcoal when a child has ingested poison.
In a minority of poisonings, specific antidotes are available to counteract the poison. They are highly effective and should be available in all emergency facilities. The supply of antidotes should be checked routinely and replaced as used or according to expiration dates. Antidotes available to treat toxin ingestion include N-acetylcysteine for acetaminophen poisoning, oxygen for carbon monoxide inhalation, naloxone for opioid overdose, flumazenil (Romazicon) for benzodiazepines (diazepam [Valium], midazolam [Versed]) overdose, digoxin immune Fab (Digibind) for digoxin toxicity, amyl nitrate for cyanide, and antivenin for certain poisonous bites.
Prevention of Recurrence
The ultimate objective is to prevent poisonings from occurring or recurring. One effective counseling method is first to discuss the difficulties of constantly watching and safeguarding young children (see Family Focus box). In this way the challenging task of raising children can lead to a discussion of injury prevention as part of the parental role. This approach also incorporates contributory causes for the incident, such as inadequate support systems; marital discord; discipline techniques (especially use of physical punishment); parental distress; or any disruption in the family or family activities, such as vacations, moves, visitors, illnesses, or births. A visit to the home, especially after repeat poisonings, is recommended as part of the follow-up care to assess hazards, including family factors, and to evaluate appropriate injury-proofing measures. One method of identifying risk areas is to ask specific questions or to have the parent complete a questionnaire designed to isolate factors that predispose children to poisoning. Another approach is to encourage parents to bend down to the child’s eye level and survey the home environment for potential hazards. Have the parents try to open cabinets and reach shelves to access poisons.
Passive measures (those that do not require active participation) have been the most successful in preventing poisoning and include using child-resistant closures and limiting the number of tablets in one container. However, these measures alone are not sufficient to prevent poisoning, since most toxic agents in the home do not have safety closures. Therefore, active measures (those that require participation) are essential. Guidelines for preventing the occurrence or recurrence of a poisoning are listed in the Community Focus box.
HEAVY METAL POISONING
Heavy metal poisoning can occur from the ingestion of a variety of substances, the most common being lead. Other sources that are important in terms of children are iron and mercury. Mercury toxicity, a rare form of heavy metal poisoning, has occurred in children from a variety of sources, such as broken thermometers or thermostats, broken fluorescent light bulbs, disk batteries, topical medications, gas regulators, cathartics, and interior latex house paint (Clifton, 2007; Etzel, 2001). Elemental mercury (also called metallic mercury or quicksilver) is nontoxic if ingested and if the gastrointestinal tract is healthy (e.g., has no fistulas). However, mercury is volatile at room temperature and enters the bloodstream after it is inhaled, causing toxicity (tremors, memory loss, insomnia, gingivitis, diarrhea, anorexia, weight loss). The classic form of mercury poisoning is called acrodynia (or “painful extremities”).
Heavy metals have an affinity for certain essential tissue chemicals, which must remain free for adequate cell functioning. When metals are bound to these substances, cellular enzyme systems are inactivated. Treatment involves chelation, use of a chemical compound that combines with the metal for rapid and safe excretion.
LEAD POISONING
Poisoning from lead has been a problem throughout history and throughout the world. In the United States the problem began in the early 1900s, when white lead was added to paints and when tetraethyl lead was added to gasoline as an antiknock compound. Lead content in paint was decreased in 1950, and in 1978 the use of lead in household paint was banned. The use of lead in paint and leaded gasoline has been banned in the United States. After this change in policy, the average blood lead level (BLL) in the United States for people ages 1 to 74 years dropped from 12.8 mcg/dl in 1980 to 1.9 mcg/dl in 1999 (American Academy of Pediatrics, 2005). Yet because lead does not decompose or break down into smaller particles, lead deposited in the past is still present in soil near heavily trafficked areas. Coupled with deteriorating lead-based paint falling from the exterior of nearby houses, soil becomes a significant pathway by which lead poisoning can occur. Bare soil used as a play area contributes to the lead exposure of young children, since lead-contaminated dust is tracked into the home.
A child does not need to eat loose paint chips to be exposed to the toxin; normal hand-to-mouth behavior, coupled with the presence of lead dust in the environment, is the usual method of poisoning (American Academy of Pediatrics, 2005; Erickson and Thompson, 2005). Cultural practices may also lead to pediatric ingestion of substances containing lead, especially when these are brought in from other countries. Children of Hispanic origin are believed to be at higher risk for lead poisoning as a result of exposure to culturally related items that contain lead (Erickson and Thompson, 2005). Other risk factors for having an elevated BLL include poverty, age less than 6 years, dwelling in urban areas, and living in older rental homes where lead decontamination may not be a priority. Children of immigrants and internationally adopted children may have been exposed to sources of lead before arrival in the United States and should also be carefully evaluated for lead exposure (Woolf, Goldman, and Bellinger, 2007). Any child, however, is at risk for becoming lead poisoned if hazardous conditions for lead are present in their environment.
Causes of Lead Poisoning
Although there are numerous sources of lead (Box 14-6), in most instances of acute childhood lead poisoning, the source is nonintact lead-based paint in an older home or lead-contaminated bare soil in the yard. Microparticles of lead gain entrance into a child’s body through ingestion or inhalation and, in the case of an exposed pregnant woman, by placental transfer. When measured, a mother’s lead level is nearly the same as that of her unborn child. A level of lead not harmful to an adult woman can be harmful to the fetus.
Inhalation exposure usually occurs during renovation and remodeling activities in the home, whereas ingestion happens during normal day-to-day play and mouthing activities. Sometimes a child will actually swallow loose chips of lead-based paint because it has a sweet taste. Water and food may also be contaminated with lead.
Because of family, cultural, or ethnic traditions, a source of lead may be a routine part of life for a child. Nurses must educate themselves about the practices of their patients and identify when such products may be a source of lead. The use of pottery or dishes containing lead may be an issue, as may the use of folk remedies for stomachaches or the use of some cosmetics (see Cultural Awareness box). Some hobbies and occupations of adult family members may contribute to lead hazards carried into the household on clothes, shoes, or skin (American Academy of Pediatrics, 2005). Nurses are often in a position to observe or elicit information about these practices and educate families about their potential harm.
Pathophysiology and Clinical Manifestations
Lead can affect any part of the body, including the renal, hematologic, and neurologic systems (Fig. 14-9). Of most concern for young children is the developing brain and nervous system, which are more vulnerable than those of an older child or adult. Lead in the body moves via an equilibration process between the blood, the soft tissues and organs, and the bones and teeth. Lead ultimately settles in the bones and teeth, where it remains inert and in storage. This makes up the largest portion of the body burden, approximately 75% to 90%. At the cellular level it competes with molecules of calcium, interfering with the regulating action of calcium.
The neurologic system is of most concern when young children are exposed to lead. The developing brain is especially vulnerable. Lead disrupts the biochemical processes and may have a direct effect on the release of neurotransmitters, may cause alterations in the blood-brain barrier, and may interfere with the regulation of synaptic activity (Lidsky and Schneider, 2006).
There is a relationship between anemia and lead poisoning. Children who are iron deficient absorb lead more readily than those with sufficient iron stores. Lead can interfere with the binding of iron onto the heme molecule. This sometimes creates a picture of anemia, even though the child is not iron deficient. Lead toxicity to the erythrocytes leads to the release of the enzyme erythrocyte protoporphyrin (EP). Because EP is not sensitive to BLLs of less than about 16 to 25 mcg/dl, it is no longer used as a screening test. Therefore the BLL test is currently used for screening and diagnosis. However, elevation of the EP level (above 35 mcg/dl of whole blood) is a good indicator of toxicity from lead and reflects the length of exposure and body burden of lead in the individual child.
Although adults have been shown to suffer adverse renal effects from occupational lead exposure, few studies document renal effects in children at other than extremely high lead levels. One can hypothesize that lead can affect the renal integrity of children as well as adults. Therefore the renal system of a child is still considered a potential target for the harmful effects of lead.
The lead levels identified in children have declined since the initiation of screening for children at risk for lead poisoning. With earlier intervention, the most prevalent effects have changed. Since the late 1960s, children have rarely died of lead poisoning, and seizures or mental retardation have become less likely. However, even mild and moderate lead poisoning can cause a number of cognitive and behavioral problems in young children, including aggression, hyperactivity, impulsivity, delinquency, disinterest, and withdrawal. Long-term neurocognitive signs of lead poisoning include developmental delays, lowered intelligence quotient (IQ), reading skill deficits, visual-spatial problems, visual-motor problems, learning disabilities, and lower academic success. Physical growth and reproductive efficiency may also be adversely affected by chronic lead toxicity (Woolf, Goldman, and Bellinger, 2007).
Diagnostic Evaluation
Children with lead poisoning rarely have symptoms, even at levels requiring chelation therapy. A diagnosis of lead poisoning is based only on the lead testing of a venous blood specimen from a venipuncture. The collection process is important. Blood must be collected carefully to avoid contamination by lead on the skin. The level of concern for an elevated BLL has dropped from 80 mcg/dl in 1950 to 10 mcg/dl today (American Academy of Pediatrics, 2005).
Anticipatory Guidance
Anticipatory guidance lends support to primary prevention efforts. The Centers for Disease Control and Prevention (2005) recommends that the following information be made available to families beginning during prenatal care, at 3 to 6 months, and at 1 year of age:
 Hazards of lead-based paint in older housing
Hazards of lead-based paint in older housing
 Ways to control lead hazards safely
Ways to control lead hazards safely
 Hazards accompanying repainting and renovation of homes built before 1978
Hazards accompanying repainting and renovation of homes built before 1978
 Other exposure sources, such as traditional remedies, that might be relevant for a family
Other exposure sources, such as traditional remedies, that might be relevant for a family
There has been recent concern regarding imported toys and other items children play with that have been found to contain lead. Parents should carefully evaluate the source (manufacturer) of every toy or item and not assume it is safe just because it is sold on the U.S. market. The U.S. Consumer Product Safety Commission* is an excellent resource for parents and caretakers concerned about the safety of a given toy or product.
Screening for Lead Poisoning
When primary prevention fails, the secondary prevention effort of screening for elevated BLLs can identify children much earlier than in the past. Guidelines from the Centers for Disease Control and Prevention (2005) recommend universal or targeted screening on the basis of each state’s determination of need. This need is established using blood lead surveillance and other risk factor data collected over time to establish the status and risk of children throughout the state. In areas without available data, universal screening is recommended.
Universal screening should be done at ages 1 and 2 years. Any child between the ages of 3 and 6 years who has not been previously screened should also be tested. Any child with risk factors should be screened more often.
Targeted screening is acceptable when an area has been determined by existing data to have less risk. Children should be screened when they live in a high-risk geographic area or are members of a group determined to be at risk (e.g., Medicaid recipients), or if their family cannot answer “no” to the following personal risk questions:
 Does your child live in or regularly visit a house that was built before 1950?
Does your child live in or regularly visit a house that was built before 1950?
 Does your child live in or regularly visit a house built before 1978 with recent or ongoing renovations or remodeling within the past 6 months?
Does your child live in or regularly visit a house built before 1978 with recent or ongoing renovations or remodeling within the past 6 months?
 Does your child have a sibling or playmate who has or did have lead poisoning?
Does your child have a sibling or playmate who has or did have lead poisoning?
Therapeutic Management
The degree of concern, urgency, and need for medical intervention changes as the lead level increases. Education is one of the most important elements of the treatment process. The Centers for Disease Control and Prevention (2005) has identified several areas that should be discussed with the family of every child who has an elevated BLL (10 mcg/dl):
 The child’s BLL and what it means
The child’s BLL and what it means
 Potential adverse health effects of an elevated BLL
Potential adverse health effects of an elevated BLL
 Sources of lead exposure and suggestions on how to reduce exposure, such as importance of wet cleaning to remove lead dust on floors, window sills, and other surfaces
Sources of lead exposure and suggestions on how to reduce exposure, such as importance of wet cleaning to remove lead dust on floors, window sills, and other surfaces
 Importance of good nutrition in reducing the absorption and effects of lead; for persons with poor nutritional patterns, adequate intake of calcium and iron and importance of regular meals
Importance of good nutrition in reducing the absorption and effects of lead; for persons with poor nutritional patterns, adequate intake of calcium and iron and importance of regular meals
 Need for follow-up testing to monitor the child’s BLL
Need for follow-up testing to monitor the child’s BLL
 Results of an environmental investigation if applicable
Results of an environmental investigation if applicable
 Hazards of improper removal of lead paint (dry sanding, scraping, or open-flame burning)
Hazards of improper removal of lead paint (dry sanding, scraping, or open-flame burning)
Treatment actions vary depending on the child’s BLL. Based on a diagnosis from a venous BLL test, the Centers for Disease Control and Prevention (2002) recommends the following actions:
| BLL (mcg/dl) | Action |
| <10 | Reassess or rescreen in 1 year. If exposure status changes, do this sooner. |
| 10-14 | Provide family with lead poisoning education, follow-up testing, and social service referral if necessary. |
| 15-19 | Provide family with lead poisoning education (dietary and environmental), follow-up testing, and social service referral as needed; if BLL persists, initiate actions for BLL of 20 to 44 mcg/dl. |
| 20-44 | Provide coordination of care, clinical management, environmental investigation, and lead hazard control. |
| 45-69 | Within 48 hours, provide coordination of care and clinical management, including treatment, environmental investigation, and lead hazard control. The child must not remain in a lead-hazardous environment if resolution is to occur. |
| ≥ 70 | Immediately provide medical treatment and begin coordination of care, clinical management, environmental investigation, and lead hazard control. |
Chelation Therapy.: Chelation is the term used for removing lead from circulating blood and, theoretically, some lead from organs and tissues. It is unclear whether chelation affects lead stores in bones. Although not an antidote in the truest sense, it does serve a similar purpose in that the toxic substance or poison is removed from the body. However, chelation does not counteract any effects of the lead. Because lead in circulating blood (the compartment most readily accessed by the chelator) is such a small part of the total body burden, the equilibration process will cause blood lead to rise again after treatment.
Historically two chelating agents have been used consistently: calcium disodium edetate (CaNa2EDTA or calcium EDTA) and succimer (Chemet, meso-2,3 dimercaptosuccinic acid [DMSA]). British antilewisite (BAL, dimercaprol, dimercaptopropanol) is used in conjunction with EDTA. All the agents have potential toxic side effects and contraindications. Renal, hepatic, and hematologic parameters must be monitored.
Because of the equilibration process between blood, soft tissues, and other sites in the body, there is often a rebound of the BLL after chelation. After the body burden of lead is reduced enough to stabilize the BLL, rebound will cease. Multiple chelation treatments may be necessary. Adequate hydration is essential during therapy because the chelates are excreted via the kidneys.
BAL must not be used in the presence of a glucose 6-phosphate dehydrogenase (G6PD) deficiency or peanut allergy, nor should it be given in conjunction with iron. It is never used as a single-agent therapy, only in conjunction with EDTA. It must be given only at a deep intramuscular site. EDTA should be given intravenously over several hours or, when necessary to restrict fluids, may be given intramuscularly.
Succimer is given orally over a 19-day course of treatment. The capsule is opened and sprinkled on a small amount of food or may be swallowed whole. Adverse effects include nausea, vomiting, diarrhea, loss of appetite, rash, elevated liver function tests, and neutropenia. Because the chelates are excreted via the kidneys, adequate hydration is essential.
An oral chelating agent, d-penicillamine, is sometimes used to treat lead poisoning, but low doses should be used in children and monitoring of renal function and blood counts during administration is essential (Woolf, Goldman, and Bellinger, 2007).
Prognosis.: Although most of the pathophysiologic effects of lead are reversible, the most serious consequences of both high and low lead exposure are the effects on the central nervous system. In children with lead encephalopathy, permanent brain damage can result in mental retardation, behavior changes, possible paralysis, and seizures. However, moderate- to low-dose exposure may also cause permanent neurologic deficits. Increased distractibility, short attention span, impulsivity, reading disabilities, and school failure have been associated with lead exposure (Markowitz, 2000). There is some evidence that treatment of moderate levels of lead poisoning can result in cognitive improvement (American Academy of Pediatrics, 2005).
Nursing Care Management
The primary nursing goal in lead poisoning is to prevent the child’s initial or further exposure to lead. For children with low-level exposure, this requires identifying the sources of lead in the environment. Careful history taking is the most useful and most valuable tool and should concentrate on the personal risk questions (see p. 478). Suggestions for reducing lead in the child’s environment are listed in the Community Focus box.
Children who must undergo chelation therapy are prepared for the injections, and all efforts are made to reduce injection pain. Chelating agents are administered deeply into a large muscle mass (see Atraumatic Care box). To lessen the pain from EDTA, the local anesthetic procaine is injected with the drug. Rotation of sites is essential to prevent the formation of painful areas of fibrotic tissue. Because EDTA and lead are toxic to the kidneys, records are kept of intake and output, and the results of urinalysis are assessed to monitor renal functioning.
Discharge planning for children with lead poisoning must include thorough education of families regarding safety from lead hazards, clear instructions regarding medication administration and follow-up, and confirmation that the child will be discharged to a home without lead hazards. Although caution must be used to avoid alarming parents unnecessarily, it is important that they know the risk implications for their child’s behavior and cognitive functions. Nurses should observe the development and behavior of children who are hospitalized. Any concerns that are identified should be thoroughly evaluated. Referral to a child development or speech and language specialist may be indicated.
As in any situational crisis, parents need support and understanding if their child is treated for lead poisoning. Many families at the highest risk for lead poisoning have the fewest resources to comply with measures such as relocation or removing lead from the environment where the child experiences exposure.
CHILD MALTREATMENT
The broad term child maltreatment includes intentional physical abuse or neglect, emotional abuse or neglect, and sexual abuse of children, usually by adults. It is one of the most significant social problems affecting children. In 2005, Child Protective Services (CPS) agencies in the United States confirmed that an estimated 900,000 children were victims of child maltreatment. Of the confirmed cases, 17% suffered physical abuse, 9% sexual abuse, 63% neglect, and 7% emotional abuse. In 2005, estimates indicated that 1460 children died as a result of child abuse and neglect (US Department of Health and Human Services, 2007). Reported statistics only partially represent the actual incidence of child maltreatment, since many cases are believed to go unreported.*
CHILD NEGLECT
Child neglect is the most common form of maltreatment. More than half of all reported cases are associated with deprivation of necessities, and 40% of deaths from maltreatment are in this group (US Department of Health and Human Services, 2007). Neglect is generally defined as the failure of a parent or other person legally responsible for the child’s welfare to provide for the child’s basic needs and an adequate level of care.
Important contributing factors for child neglect are lack of knowledge of child’s needs, lack of resources, and caretaker substance abuse. For example, neglectful parents often demonstrate poor parenting skills. They may be unaware that an infant needs to be fed every 3 to 4 hours, may not know what to feed the child, and may have insufficient funds to buy food. An equally serious lack of knowledge is failure to recognize emotional nurturing as an essential need of children. (See also Growth Failure [Failure to Thrive], Chapter 11.)
Types of Neglect
Neglect takes many forms and can be classified broadly as physical or emotional maltreatment. Physical neglect involves the deprivation of necessities, such as food, clothing, shelter, supervision, medical care, and education. Emotional neglect generally refers to failure to meet the child’s needs for affection, attention, and emotional nurturance. Neglect may also include lack of intervention for or fostering of maladaptive behavior, such as delinquency or substance abuse.
EMOTIONAL ABUSE
Emotional abuse, an even more difficult aspect of maltreatment to define, refers to the deliberate attempt to destroy or significantly impair a child’s self-esteem or competence. Emotional abuse may take the following forms: rejecting, isolating, terrorizing, ignoring, corrupting, verbally assaulting, or overpressuring the child (Nelms, 2001).
PHYSICAL ABUSE
The deliberate infliction of physical injury on a child, usually by the child’s caregiver, is termed physical abuse. Legal definitions of physical abuse are defined in state and federal statutes. The federal definition of abuse is “any recent act or failure to act that results in imminent risk of serious harm, death, serious physical or emotional harm of a child (less than 18 years of age) by a parent or caretaker who is responsible for the child’s welfare” (Child Abuse Prevention and Treatment Act, 1996, Public Law 104-235). Minor physical injury is responsible for more reported cases of maltreatment than major physical injury, but major physical abuse causes more deaths. Despite the importance of the problem, a universally accepted definition of what constitutes minor and major physical abuse does not exist. Rather, each state in the United States defines abuse according to its individual reporting laws.
Shaken Baby Syndrome
Shaken baby syndrome (SBS) is a serious form of child abuse caused by violent shaking of infants and young children. This violent shaking would be easily recognized by others as dangerous (American Academy of Pediatrics, 2001) and is most often a result of the caregiver’s frustration with crying (Castiglia, 2001). Every year in America an estimated 1200 to 1400 children are shaken; of these victims, 25% to 30% die as a result of their injuries and the rest have life-long complications (National Center on Shaken Baby Syndrome, 2007).
It is important to understand what happens in SBS. Infants have a large head-to-body ratio, weak neck muscles, and a large amount of water in the brain. Violent shaking causes the brain to rotate within the skull, resulting in shearing forces tearing blood vessels and neurons. The characteristic injuries that occur are intracranial bleeding (subdural and subarachnoid hematomas) and retinal hemorrhages, but they may also include fractures of the ribs and long bones. Most often there are no signs of external injury. SBS is often not an isolated event. In one study 45% of the children with inflicted traumatic brain injury caused by shaking showed some evidence of prior injury (Ewing-Cobb, Kramar, Prasad, and others, 1998).
Victims of SBS can be seen with a variety of symptoms, from generalized flulike symptoms to unresponsiveness with impending death (Miehl, 2005). Many of the presenting symptoms, such as vomiting, irritability, poor feeding, and listlessness, are often mistaken for common infant and childhood ailments. In more severe forms, presenting symptoms may include seizures, posturing, alterations in level of consciousness, apnea, bradycardia, or death. The long-term outcomes of SBS include seizure disorder; visual impairments, including blindness; developmental delays; hearing loss; cerebral palsy; and mild to profound mental, cognitive, and motor impairments (Walls, 2006). Nurses can take an active role in prevention of SBS by teaching all caregivers about crying and techniques to cope with inconsolable crying (Carbaugh, 2004).
Munchausen Syndrome by Proxy
Munchausen syndrome by proxy (MSBP), also known as factitious disorder by proxy or medical child abuse, is a rare but serious form of child abuse in which caretakers deliberately exaggerate or fabricate histories and symptoms or induce symptoms. This form of child maltreatment may include physical, emotional, and psychologic abuse for the gratification of the caretaker. In most cases the perpetrator is the biologic mother, with some degree of health care knowledge and training. Health care providers can become easily misled and unknowingly enable the perpetrator (Leider, Irving, Mauricio, and others, 2005). As a result of the history of symptoms provided by the caretaker, the child endures painful and unnecessary medical testing and procedures. Common symptoms reported by the caretaker include seizures, nausea and vomiting, diarrhea, and altered mental status; they are usually witnessed only by the perpetrator.
Considerations when determining whether a child is a victim of MSBP include:
 Is the child’s condition consistent with the reported history?
Is the child’s condition consistent with the reported history?
 Does diagnostic evidence support reported history?
Does diagnostic evidence support reported history?
 Has anyone other than the caretaker witnessed the symptoms?
Has anyone other than the caretaker witnessed the symptoms?
 Is treatment being provided primarily because of the caretaker’s demands?
Is treatment being provided primarily because of the caretaker’s demands?
The resolution of symptoms after separation from the perpetrator confirms the diagnosis.
Factors Predisposing to Physical Abuse
The causes of child abuse are multifaceted. Child maltreatment occurs across all socioeconomic, religious, cultural, racial, and ethnic groups (Goldman, Salus, Wolcott, and others, 2003). Three risk factors are commonly identified in child abuse: parental characteristics, characteristics of the child, and environmental characteristics. However, no single factor or group of factors is predictive of abuse. Rather, the interaction of these factors is thought to increase the risk of abuse occurring in a particular family.
Parental Characteristics.: Certain identified characteristics occur more frequently in parents who abuse their children and are therefore considered risk factors. Younger parents more often are abusers of their children. One-parent families are at higher risk for abuse, and in single-parent families that include an unrelated partner, the partner is frequently the abuser.
Abusive families are often more socially isolated and have fewer supportive relationships. These parents are often from low-income circumstances, with concurrent undereducation and substance abuse problems. With little or no available support system and concurrent stressors imposed by the child or environment, these parents are vulnerable to additional crises of any nature and may strike out at the child to release their increasing frustration and anxiety.
Other factors identified in abusive parents include low self-esteem and little knowledge of appropriate parenting skills. Parenting skills are learned behaviors, and parents who grew up with poor parental role models may have difficulty parenting their own children. Approximately, one third of parents who were maltreated as children will subject their children to similar maltreatment (Gara, Allen, Herzog, and others, 2000).
Characteristics of the Child.: The onus for child abuse is always on the abuser; however, some characteristics are common in children who are abused. Children from birth to 3 years of age are at highest risk for being abused (US Department of Health and Human Services, 2007). Infants and small children require constant attention and must have all their needs met by others. This can result in parental or caretaker fatigue with resultant striking out at the child with physical force, shaking the child, or ignoring the child’s needs.
The physical and emotional demands placed on the parents or caretaker of an unwanted, brain-damaged, hyperactive, or physically disabled child may overwhelm them, resulting in abuse. Disabled children may not understand that abusive behaviors are not appropriate, so do not tell others or defend themselves. Preterm infants may be at risk for maltreatment because of failure of parent-child bonding during early infancy, increased physical needs, or irritability. One child in the family may be singled out in an abusive family. Removing that child from the home often places the other siblings at risk for abuse. Therefore no child is safe if left in the abusive environment unless the parents can be helped to learn new parenting skills and to meet their needs and release their frustration through alternatives other than attacking their children.
Environmental Characteristics.: The environment is a significant part of the potential abusive situation. A typical environment is one of chronic stress, including problems of divorce, poverty, unemployment, poor housing, frequent relocation, alcoholism, and drug addiction. Increased exposure between children and parents, such as that which occurs in crowded living conditions, also increases the likelihood of abuse.
Although most reporting of abuse has been from lower socioeconomic populations, as stated before, child abuse is not a problem of any one societal group. Stresses imposed by poverty predispose lower socioeconomic families to abusive situations, and abuse in these groups is more apt to be reported. However, concealed crises may also be present in upper-class families. Families who have substitute caregivers such as daycare providers and baby-sitters may also be at risk for child abuse, especially if the family has not fully evaluated the caregiver. Nurses need to be aware of all these factors to identify the less obvious examples of child abuse and neglect.
SEXUAL ABUSE
Sexual abuse is one of the most devastating types of child maltreatment, and estimates indicate that it has increased significantly during the past decade (US Department of Health and Human Services, 2007). Child sexual abuse constitutes approximately 10% of officially substantiated child maltreatment cases. Some of the apparent increase can be attributed to increased awareness (Putnam, 2003).
As with all forms of child maltreatment, no universal definition for sexual abuse exists. Definitions of sexual abuse cover a range of acts, including involvement of children in sexual acts they do not understand, that they cannot give consent to, or that violate social taboos (Finkel and DeJong, 2001). The Child Abuse and Prevention Act (Public Law 93-247) defines sexual abuse as “the use, persuasion, or coercion of any child to engage in sexually explicit conduct (or any simulation of such conduct) or producing any visual depiction of such conduct, or rape, molestation, prostitution, or incest with children.”
Sexual abuse includes the following types of sexual maltreatment (see also Sexual Assault [Rape], Chapter 17):
Incest—Any physical sexual activity between family members; blood relationship is not required (abusers can include step-parents, unrelated siblings, grandparents, uncles, and aunts); does not include sexual relations between legally sanctioned partners, such as spouses
Molestation—A vague term that includes “indecent liberties,” such as touching, fondling, kissing, single or mutual masturbation, or oral-genital contact
Exhibitionism—Indecent exposure; usually exposure of the genitalia by an adult male to children or women
Child pornography—Arranging and photographing, in any media, sexual acts involving children, alone or with adults or animals, regardless of consent by the child’s legal guardian; also may denote distribution of such material in any form, with or without profit
Child prostitution—Involving children in sex acts for profit and usually with changing partners
Pedophilia—Literally means “love of child” and does not denote a type of sexual activity but the preference of an adult for prepubertal children as the means of achieving sexual excitement
Characteristics of Abusers and Victims
Anyone, including siblings and mothers, can be sexual abusers, but a typical abuser is a man whom the victim knows. Offenders come from all levels of society. Adults comprise 80% of offenders of sexual abuse, with the remaining 20% being adolescents and preadolescents (Johnson, 2003). Most sexual abuse is committed by men and by persons known to the child, with family members constituting up to two thirds of the perpetrators (Christian, Lavell, and DeJong, 2000). Many offenders hold full-time jobs, are active in community affairs, and do not have prior criminal records (Finkel and DeJong, 2001). Offenders often are employed in or volunteer for positions that will bring them into contact with young girls and boys such as teaching or coaching. Child sexual abuse may be generational unless discovered and stopped (Johnson, 2003). Offenders may commit many assaults before being caught.
Incestuous relationships between father or stepfather and daughter are generally prolonged, and the victims are usually reluctant to report the situation because of fear of retaliation and fear that they will not be believed. Typically, incestuous relationships begin later than other forms of child abuse. The eldest daughter is usually abused, but in her absence another sister may be substituted. Sibling incest may also occur. Sexual abuse by relatives with a strong emotional bond with the victim is the most devastating to the child.
Boys are also victims of both intrafamilial and extrafamilial abuse. Male victims are much less likely to report abuse, and they may suffer much greater emotional harm from incestuous relationships, especially between mother and son, than female victims. Boys are likely to be subjected to anal penetration and oral-genital contact; to have subtle physical findings; and to be abused by a father, stepfather, or mother’s boyfriend.
Considerable evidence exists to show that at least 20% of American women and 5% to 10% of American men experienced some form of sexual abuse as children. Race and socioeconomic status do not seem to be major risk factors. Significant risk factors for child sexual abuse include parental unavailability, lack of emotional closeness and flexibility, social isolation, emotional deprivation, and communication difficulties. Approximately 20% to 25% of child sexual abuse cases involve penetration or oral-genital contact. The mean age of vulnerability is 9 years, with a range from infancy to 17 years of age (Berlinger and Elliott, 2002).
Initiation and Perpetuation of Sexual Abuse
The cycle of sexual abuse often starts insidiously, unless it involves an isolated attack, such as rape. Often offenders spend time with the victims to gain their trust before initiating any sexual contact. Most victims are then pressured into being an accessory to the sexual activity through various means (Box 14-7) and may be unaware that sexual activity is part of the offer. Children may not reveal the truth for fear that their parents would not believe them, especially if the offender is a trusted member of the family. Some fear they will be blamed for the situation, and many young children with limited vocabulary have difficulty describing the activity when they do have the courage or opportunity to reveal the abuse.
Incest most frequently occurs between fathers and daughters, but may be between grandfather and granddaughter or brother and sister. Brother-sister incest has been found to be just as damaging as father-daughter abuse (Cyr, Wright, McDuff, and others, 2002). Victims may take years to disclose this abuse. However, not all incestuous relationships follow this pattern of silence. Reports of father-daughter incest during child custody conflicts have become more common and have raised serious concerns regarding the possibility of false accusation. Rather than tolerating or denying the child’s sexual abuse, the other parent (usually the mother) is typically the chief accuser.
NURSING CARE OF THE MALTREATED CHILD
A critical responsibility of health professionals is identifying abusive situations as early as possible. The characteristics that may predispose members of some families to commit abuse can serve as a framework for assessing vulnerability but are never predictive of actual abuse. A careful, detailed history and interview combined with a thorough physical examination are the diagnostic tools needed to identify abuse. Nurses have a special role because they may be the first person to see the child and parent and are the consistent caregivers if the child is hospitalized (see Nursing Care Guidelines box).
During the interview with the child and family, the nurse must be careful to avoid biasing the child’s retelling of the events. Some experts suggest that health professionals limit the interview to the child’s physical and mental health concerns and leave topics of the family’s social, legal, or other problems to the police or CPS (McClain, Giardet, Lahoti, and others, 2000). If this is not possible, an effort should be made to coordinate the interview process so that all pertinent health care professionals can be present.
Recognition of abuse or neglect necessitates a familiarity with both physical and behavioral signs that suggest maltreatment (Boxes 14-8 and 14-9). No one indicator can be used to diagnose maltreatment. It is a pattern or combination of indicators that should arouse suspicion and further investigation. It is important to note that some situations may be misinterpreted as abuse; for example, bleeding disorders, osteogenesis imperfecta, sudden infant death syndrome (SIDS), and cultural practices such as cupping or coin rubbing (see Health Practices, Chapter 4) may mimic physical abuse. Unintentional injuries, such as burns from metal buckles on car seats, bruising from seat belts, or spiral fractures from a twist and fall injury, may also be wrongly diagnosed as abuse. Normal variants, such as Mongolian spots and congenital anomalies of genitalia, can be mistaken for abuse.
Caregiver-Child Interaction
The nurse can use the initial contact with the family to assess the interaction between the caregiver and the child. Caregivers who seem indifferent to or unsupportive of the child should cause concern. Observations of the caregivers should include emotional support for the child, attentiveness to the child’s needs, and concern for the child’s injury. Although caregivers and children may vary in responses to a stressful event, an unusual caregiver-child relationship should be noted and factored into the overall evaluation of the child. Certain behavioral responses of the parents to their child and to the interviewer should alert the nurse to the possibility of maltreatment. Abusive parents may have difficulty showing concern toward their child. They may be unable or unwilling to comfort the child. Abusers may blame the child for the injuries or belittle him or her for being clumsy or stupid. When interacting with the health care workers, the parents may become hostile or uncooperative. During the child’s hospitalization they may not participate in the child’s care and may show little concern for his or her progress, eventual discharge, or need for follow-up care.
Abused children’s responses to their parents or the injury may also support the suspicion of abuse. Although no one pattern is typical, extremes of behavior may be observed. Children may be unresponsive to the parent or excessively clinging and intolerant of separation. They may be overly attached to the abusive parent, possibly in the hope of preventing any upset that may precipitate anger and another attack. During care of the injury, children may be passive and accepting of the discomfort or uncooperative and fearful of any physical contact. They may avoid eye contact. Some children maintain a wary watchfulness of all strangers; some shy away from strangers as if frightened; others are unusually affectionate and outgoing.
History and Interview
Child Physical Abuse.: It is often difficult to differentiate child maltreatment from accidental injuries. Caregivers whose history of events may be deceptive or incomplete or children who are nonverbal may make the assessment more complex. A purposeful, skilled history and appropriate interview questions will help the nurse to ensure the right course of action. Knowledge of mechanism of injury and child development is essential. Cases of abuse are often detected because the child or caregiver history of events is inconsistent with physical findings. Children who are verbal can often give a history of the injury. Separating the child from the caregiver may provide a more reliable history. It is important to ask nonleading, open-ended questions. The history should include a narrative of the injury from both caregiver and child (if verbal). Date, time, and location where injury took place along with who was present at time of the injury are essential questions. Family history for bleeding or bone disorders is important. Areas of history that are concerning for abuse are outlined in Box 14-8.
Neglect and Emotional Abuse.: Each child may manifest different responses to neglect depending on the situation and developmental age. The goal of the interview is to determine if the child is in a safe environment and if the caregiver has the skills and resources to care for the child. It is often difficult to determine whether the circumstances constitute poor parenting skills or true neglect. Behaviors suggestive of abuse or neglect are found in Box 14-9.
Sexual Abuse.: An essential component to identifying sexual abuse is the interview. Several dynamics may impede the child’s revelation of sexual abuse. Child sexual abuse is often perpetrated by someone known to the children, including family members. In some cases the children may have been sworn to secrecy. They may have been told that no one will believe them or their family would be harmed if they tell someone about the abuse. Small children may imitate behaviors they have had perpetrated on themselves or have seen others do. The nurse must be able to recognize normal, age-related sexual curiosity and self-stimulating behaviors. Typically, children do not act out specific details of the sexual act or perform intrusive acts on others unless they have sexual knowledge beyond their normal age-related development (Johnson, 2003).
Children’s reports of sexual abuse may vary from contradictory stories to unwavering versions of the experience. Stories that sound contradictory may reflect the child’s experiences in several instances of abuse. Also, children who repeatedly tell identical facts may have been prompted to do so. Increasing evidence suggests that the types of interrogation children are exposed to after reports of sexual abuse shape their thinking. To avoid biasing the interaction, nurses must be skillful interviewers when questioning children who may be victims of abuse. Medical records should include verbatim statements made by the child and interviewer that reflect appropriate nonleading questions and statements (Hornor, 2001; McClain, Giradet, Lahoti, and others, 2000). The child may not be emotionally ready to discuss the abuse. Establishing rapport with the child is essential to gaining his or her trust. Interviews should not be rushed. Engaging the child in play activities while encouraging conversation may help the child discuss the abuse. It may take several interviews or psychologic counseling for the child to be forthcoming about the abuse. Information regarding the last sexual contact is important because it determines the need for a forensic evaluation. Forensic testing should be considered for children who have been sexually abused within the past 72 to 96 hours.
Unfortunately, there is no typical profile of the victim, and there must be a high index of suspicion to identify these children. Physical signs vary and may include any of those listed for sexual abuse. The victim may exhibit various behavioral manifestations, but none of these behaviors is diagnostic. When abused children exhibit these behaviors, the signs may be incorrectly attributed to the normal stresses of childhood, especially in older school-age children or adolescents. Even signs considered most predictive of sexual abuse, such as certain genital findings, sexually inappropriate behavior for age, enactment of adult sexual activity, and intense focus on sexual activity (e.g., masturbation), do not always indicate that sexual abuse has occurred. Conversely, abused children may not demonstrate more knowledge of sexual activity than nonabused children. However, one difference in the abused children’s explanation of sexual activity may be unusual affective responses. For example, abused children may have an increased incidence of sleep disorders, temper tantrums, and depression (Calam, Horne, Glasgow, and others, 1998).
Physical Assessment
Child Physical Abuse.: The goal of the physical assessment for child physical abuse is identification of all injuries. A systems approach ensures the whole body is evaluated. In instances of severe abuse and injuries, the assessment should begin with a rapid assessment of airway, breathing, circulation, and neurologic systems. A systematic head-to-toe examination follows. Attention to areas often overlooked, such as the scalp, behind the ears, and the lingual frenulum, is essential. An exterior examination of the genitalia and the child’s posterior surface should be completed.
Record the location and a detailed description of all injuries. Note color, size, and location of all bruising. Burn documentation should include location, pattern, demarcation lines, and presence of eschar or blisters. Diagrams of the injuries using a body diagram form are helpful. If available, photographs of the injuries using a measurement tool should be obtained.
Not all forms of physical abuse have obvious signs. Intraabdominal organ injury from blunt trauma to the abdomen can occur without signs of external abdominal bruising. Nurses should consider intraabdominal injury in infants and children who have any other signs of abuse.
All evidence collected must adhere to strict guidelines for legal purposes; chain of custody must be appropriately maintained with local law enforcement personnel. Documentation on the chain of custody form should include names of persons collecting or receiving evidence (such as photographs and DNA samples), type of evidence collected or received, and date of receipt (Kaczor, Pierce, Makoroff, and others, 2006).
Neglect and Emotional Abuse.: Neglect from deprivation of necessities is easier to identify than emotional neglect or abuse because physical signs are usually evident. Assessment of the child’s height, weight, nutritional status, hygiene, and age-appropriate interactions is important for the overall picture of potential neglect. Emotional maltreatment may be readily suspected, but it is difficult to substantiate. Physical signs are often nonspecific, and nurses must rely on behavioral indicators, which range from depression to acting-out behavior, to help identify a possibly abusive situation. Any persistent and unexplained change in the child’s behavior is an important clue to possible emotional abuse.
Sexual Abuse.: Identifying instances of sexual abuse is particularly difficult because, often, few if any obvious physical indications of the activity exist. Physical signs vary and may include any of those listed in Box 14-9 for sexual abuse. The goal of the physical examination is to document genital findings. In most cases, the genital examination is normal, which does not mean that sexual abuse did not occur. Fondling or genital-to-genital contact without penetration may leave no physical findings. Forensic evidence collection should be considered for any child with known or suspected sexual contact within 72 hours. Forensic evidence obtained directly from a prepubertal victim’s body diminishes greatly after 24 hours, with the best chance for evidence collection coming from bed linens or the child’s underwear (Christian, Lavelle, DeJong, and others, 2000). The female genital examination should include a description of the vulva, hymen, and surrounding tissue. Abnormal findings of concern are injuries to the posterior vulva or the lower half of the hymeneal ring, or abrasions, bruising, or bleeding of the genital or anal tissue. It is often helpful to use a magnifying instrument (colposcope) to detect subtle injuries. There are many variants of normal findings for female genital anatomy, so it is recommended that the examination be done by a practitioner experienced with these types of cases. Contrary to popular myth, the size of the hymenal opening is not predictive of the likelihood of sexual abuse (Christian and Rubin, 2002). For male victims, presence of swelling, abrasions, or bruising of the genital tissue is of concern for abuse. The anal area should be examined for symmetry, tone, fissures, or scars. Genital tissue heals quickly and most often without scars. Therefore, unless seen within a few days of injury, the genital tissue may appear normal. In addition, the vaginal and anal mucosa is elastic; therefore penetration without disruption of tissue is possible. This defies another myth that there is always evidence of female virginity. Consideration should be given to the collection of specimens for determining the presence of sexually transmitted diseases, which may have been contracted during the sexual contact.
A number of nursing diagnoses are prominent in the nursing care of the maltreated child and family, and others specific to individual cases become evident. The most common nursing diagnoses are outlined in the Nursing Process box. The expected outcomes are described in the Nursing Care Plan on p. 489.
Nursing Care Management
Protect Child from Further Abuse.: Initially, identification of instances of suspected abuse or neglect is essential. The nurse may come in contact with abused children in an emergency department, practitioner’s office, home, daycare center, or school.
All states and provinces in North America have laws for mandatory reporting of child maltreatment. Suspected child abuse is reported to the local authorities.* Referrals usually come to the state child welfare department and are assigned to a caseworker in an agency such as CPS. After a referral has been made, a caseworker is assigned to investigate the report. Based on the findings, the child is left in the home or temporarily removed.
A court proceeding may be necessary before the child can be placed outside the home or when parental rights are to be terminated. When the courts are involved, they usually require firsthand testimony by the referring parties. Nurses may be subpoenaed to appear in court, or their notes may be introduced as evidence in court hearings. Accurate and factual documentation is essential. Behaviors are described, not interpreted, and are recorded daily to establish a progress record (see Nursing Care Guidelines box). Conversations among the nurse, child, and parent are recorded verbatim as much as possible.
Support Child.: Children suspected of being abused are often hospitalized for medical management of their injuries and to allow further assessment of their safety needs. The needs of these children are the same as those of any hospitalized child. The child should be treated as a child with the usual physical needs, developmental tasks, and play interests—not as a victim of abuse. The goal of the nurse-child relationship is to provide a role model for the parents in helping them to relate positively and constructively to their child and to foster a therapeutic environment for the child in his or her reprieve from the abusing situation.
Support Family.: The nurse also encourages the child’s relationship with nonoffending parents. The nurse does not become a substitute parent, but rather acts as a role model for parents in helping them to relate positively and constructively to their child. When parental ignorance of childrearing practices has played a part in the abuse, the nurse can educate the parent regarding children’s physical and emotional needs. Because of the parents’ own childrearing, they may not be aware of nonviolent methods of discipline, such as time-out. They may also need help in dealing with their frustration so that they do not vent anger on the child. Because these parents may be sensitive to criticism, teaching is implemented through demonstration and example rather than through lecturing. Any competent parenting abilities they demonstrate are praised to promote their sense of parental adequacy.
Family members are advised to encourage the child to resume normal activities and observe the child for signs of distress (see Posttraumatic Stress Disorder, Chapter 17). Children express their feelings primarily through behavior. Parents should be alert for changes in behavior that indicate distress resulting from the incident, such as remaining in the house, refusing to go to school, changing sleeping patterns, and increasing frequency of nightmares. Children are encouraged to talk about these feelings and nightmares because the more they talk about the experience, the more they are able to gain control over it.
Referral to appropriate social service agencies is also essential. Many abusive parents live in poverty, and the daily stresses imposed by their circumstances are overwhelming. Resources for financial aid, improved housing, and child care should be sought. Self-help groups also provide important services. Groups such as Parents Anonymous* (a group for parents who have abused or fear that they may abuse their child, but only in terms of physical abuse, not sexual abuse) and Parents United International, Inc.† (a group devoted to helping sexually abused families), are accepting and nonjudgmental.
Plan for Discharge.: Discharge planning should begin as soon as possible after the legal disposition for placement, which may be temporary foster home placement, return to the parents, or permanent termination of parental rights. The latter is the most drastic solution, but it is necessary in situations of life-threatening abuse. Whenever children are sent to a foster home or juvenile institution, they must be allowed an opportunity to express their feelings. No matter how severe the abuse, they usually mourn the loss of their parents. They need help to understand why they must not return home and that this new home is in no way a punishment. Whenever possible, foster parents are encouraged to visit in the hospital, and the nurse should take an active role in helping these new parents understand the child. It is unfortunate that some abused children live in torment as they are sent from one foster home to another, sometimes enduring worse circumstances than those that existed in their original home. Only through constant evaluation of the placement residence and the child’s adjustment to a new environment can the vicious circle of abuse, abandonment, and neglect be stopped.
Prevent Abuse.: Prevention of child maltreatment has been an extremely difficult goal. Programs aimed at identifying potential abusers and instituting supportive intervention before the occurrence of an abusive act have met with variable success. However, nurses have played an important role in such programs. For example, home visiting by nurses to primiparas who were either teenagers, unmarried, or of low socioeconomic status was noted to be an effective preventive measure (Eckenrode, Ganzel, Henderson, and others, 2000; McMillian, 2000). The nurses provided information on normal child growth and development and routine health care needs, served as informal support persons, and referred families to appropriate services when a need for assistance was identified.
Such programs provide models for reducing factors that increase the risk of abuse. Nurses in a variety of settings can implement similar activities. For example, nurses in prenatal clinics can prepare expectant families for parenthood. Nursery and postpartum nurses can foster the attachment process by encouraging parents to hold and look at their infant, as well as teaching coping mechanisms for prolonged crying. Nurses in neonatal intensive care units can minimize the effects of separation by encouraging parents to visit and can help parents become comfortable caring for their child. Nurses in ambulatory settings can teach parents appropriate methods of bathing, feeding, toileting, disciplining, and preventing injuries, while stressing the normal needs and developmental characteristics of children. Nurses must be sensitive to parental needs for attention, reassurance, and reinforcement, and refer parents to community services and self-help groups.
Unlike preventive efforts for neglect and physical abuse, which have been aimed at the potential offender, prevention of child sexual abuse has centered on education of children to protect themselves. Materials are available for parents that describe sexual abuse and its prevention.* Supporting parental qualities of respect, affection, empathy, and ability to set boundaries and providing high-quality child care and education comprise the true preventive approach to sexual abuse. Helpful games such as “What if the baby-sitter wants to wrestle and hug but tells you to keep it a secret?” can be used to explore dangerous situations in advance and help children learn the importance of saying “no.” They need reassurance that no matter what the other person says or does, the parents want to know about it and will not punish them. Even if children participate in the activity before telling the parents, they must be reassured that it was not their fault.
It is equally important to teach children safety in terms of potential risk situations. Several suggestions for parents regarding protecting and educating children against possible molestation are presented in the Family-Centered Care box. The nurse is frequently in a position to discuss the topic of abuse with parents and to provide guidance. In addition, parents need to be made aware that “nice” people, including friends and relatives, can be offenders; parents should carefully observe how others act toward the child. A sudden change in the child’s behavior and a response such as “I don’t like Uncle anymore” are clues to investigate the relationship. In the event of any doubt, further solitary encounters with this person and the child should be prevented. It is sometimes to the child’s great misfortune that parents do not take certain comments seriously, such as “He hugs me too tight” or “I don’t want to go with him.” Casual parental statements such as “He just loves you” or “You do whatever adults tell you to do” can place children in jeopardy. Health professionals must alert parents to such dangers and guide them toward an appreciation of the problem, providing concrete guidelines toward child education and protection (see Nursing Care Plan).
REFERENCES
Abruzzi, G, Stork, CM. Pediatric toxicological concerns. Emerg Med Clin North Am. 2002;20(1):223–247.
American Academy of Clinical Toxicology, European Association of Poisons Centres and Clinical Toxicologists. Position paper: cathartics. J Toxicol. 2004;42(3):243–253.
American Academy of Clinical Toxicology, European Association of Poisons Centres and Clinical Toxicologists. Position paper: ipecac syrup. J Toxicol. 2004;42(2):133–143.
American Academy of Pediatrics, Committee on Infectious Diseases, Pickering L, eds. Red book: 2006 report of the Committee on Infectious Diseases, ed 27, Elk Grove Village, Ill: The Academy, 2006.
American Academy of Pediatrics, Committee on Environmental Health. Lead exposure in children: prevention, detection, and management. Pediatrics. 2005;116(4):1036–1046.
American Academy of Pediatrics, Committee on Injury, Violence, and Poison Prevention. Poison treatment in the home. Pediatrics. 2003;112(5):1182–1185.
American Academy of Pediatrics, Committee on Child Abuse and Neglect. Shaken baby syndrome: rotational cranial injuries (technical report). Pediatrics. 2001;108(1):206–210.
Berlinger, L, Elliott, D. Sexual abuse of children. In Myers J, Berliner L, Briere J, et al, eds.: APSAC handbook on child maltreatment, ed 2, Thousand Oaks, Calif: Sage Publications, 2002.
Bond, GR. Activated charcoal in the home: helpful and important or simply a distraction? Pediatrics. 2002;109(1):145–146.
Calam, R, Horne, L, Glasgow, D, et al. Psychological disturbances and child sexual abuse: a follow-up study. Child Abuse Negl. 1998;22(9):901–913.
Carbaugh, SF. The long road home: understanding shaken baby syndrome. Adv Neonatal Care. 2004;4:105–117.
Castiglia, R. Shaken baby syndrome. J Pediatr Health Care. 2001;15(2):78–80.
Centers for Disease Control and Prevention. Deaths associated with hypocalcemia from chelation therapy—Texas, Pennsylvania, and Oregon, 2003-2005. MMWR. 2006;55(08):204–207.
Centers for Disease Control and Prevention. Statewide plan for childhood blood lead screening. Atlanta: The Centers, 2005.
Centers for Disease Control and Prevention. Managing elevated blood lead levels among young children: recommendations from the Advisory Committee on Childhood Lead Poisoning Prevention. Atlanta: The Centers, 2002.
Chen, TM, George, S, Woodruff, CA, et al. Clinical manifestations of varicella-zoster virus infection. Dermatol Clin. 2002;20(2):267–282.
Cheng, A, Ratnapalan, S. Improving the palatability of activated charcoal in pediatric patients. Pediatr Emerg Care. 2007;23(6):384–386.
Christian, C, Lavelle, J, DeJong, A, et al. Forensic evidence findings in prepubertal victims of sexual assault. Pediatrics. 2000;106:100–104.
Christian, CW, Rubin, DM. Sexual abuse. In: Giardino AP, Giardino ER, eds. Recognition of child abuse for the mandated reporter. St Louis: G.W. Medical Publishing, 2002.
Clifton, JC. Mercury exposure and public health. Pediatr Clin North Am. 2007;54(2):237–269.
Criddle, LM. An overview of pediatric poisonings. AACN Adv Crit Care. 2007;18(2):109–118.
Cyr, M, Wright, J, McDuff, P, et al. Intrafamilial sexual abuse: brother-sister incest does not differ from father-daughter incest and stepfather-stepdaughter incest. Child Abuse Neglect. 2002;26(9):957–973.
Eckenrode, J, Ganzel, B, Henderson, C, et al. Preventing child abuse and neglect with a program of nurse home visitation: the limiting effects of domestic violence. JAMA. 2000;284(11):1385–1391.
Erickson, L, Thompson, T. A review of a preventable poison: pediatric lead poisoning. J Soc Pediatr Nurs. 2005;10(4):171–182.
Etzel, RA. Indoor air pollutants in homes and schools. Pediatr Clin North Am. 2001;48(5):1153–1165.
Ewing-Cobb, L, Kramer, L, Prasad, M, et al. Neuroimaging, physical, and developmental findings after inflicted and noninflicted traumatic brain injury in young children. Pediatrics. 1998;102:300–307.
Faden, H. Management of primary herpetic gingivostomatitis in young children. Pediatr Emerg Care. 2006;22(4):268–269.
Finkel, MA, DeJong, AR. Medical findings in child sexual abuse. In: Reece RM, Ludwig S, eds. Child abuse medical diagnosis and management. Philadelphia: Lippincott Williams & Wilkins, 2001.
Fuloria, M, Kreiter, S. The newborn examination, part I, Emergencies and common abnormalities involving the skin, head, neck, chest, and respiratory and cardiovascular systems. Am Fam Physician. 2002;65(1):61–68.
Gara, MA, Allen, LA, Herzog, EP, et al. The abused child as parent: the structure and content of physically abused mothers’ perceptions of their babies. Child Abuse Negl. 2000;24(5):627–639.
Goldman, J, Salus, MK, Wolcott, D, et al, What factors contribute to child abuse and neglect?. A coordinated response to child abuse and neglect: the foundation for practice. Child Welfare Information Gateway: ***, 2003. retrieved June 4, 2007, from http://www.childwelfare.gov/pubs/usermanuals/foundation/foundatione.cfm
Heard, K. Gastrointestinal decontamination. Med Clin North Am. 2005;89(6):1067–1078.
Hlavsa, MC, Watson, JC, Beach, MJ. Giardiasis surveillance—United States, 1998-2002. MMWR. 2005;54(SS1):9–16.
Hornor, G. Repeated sexual abuse allegations: a problem for primary care providers. J Pediatr Health Care. 2001;15(2):71–76.
Johnson, M. Child sexual abuse. In: Thomas DO, Bernardo LM, Herman B, eds. Core curriculum for pediatric emergency nursing. Sudbury, Mass: Jones & Bartlett, 2003.
Kaczor, K, Pierce, MC, Makoroff, K, et al. Bruising and physical child abuse. Clin Pediatr Emerg Med. 2006;7(3):153–160.
Lederman, C, Lederman, M. Ophthalmologic emergencies. In Crain EF, Gershel JC, eds.: Clinical manual of emergency pediatrics, ed 4, New York: McGraw-Hill, 2003.
Leider, HS, Irving, SY, Mauricio, R, et al. Munchausen syndrome by proxy: a case report. AACN Clin Issues. 2005;16(2):178–184.
Leung, AK, Robson, WL, Leong, AG. Herpes zoster in childhood. J Pediatr Health Care. 2006;20(5):1783–1785.
Lichtenstein, SJ, Rinehart, M, Levofloxacin Bacterial Conjunctivitis Study Group. Efficacy and safety of 0.5% levofloxacin ophthalmic solution for the treatment of bacterial conjunctivitis in pediatric patients. J AAPOS. 2003;7(5):317–324.
Lidsky, TI, Schneider, JS. Adverse effects of childhood lead poisoning: the clinical neuropsychological perspective. Environ Res. 2006;100(1):284–293.
Litovitz, T, Klein-Schwartz, W, White, S, et al. 1999 Annual report of the American Association of Poison Control Centers toxic exposure surveillance system. Am J Emerg Med. 2000;18(5):517–574.
Markowitz, M. Lead poisoning. Pediatr Rev. 2000;21(10):327–335.
McClain, N, Giardet, R, Lahoti, S, et al. Evaluation of sexual abuse in the pediatric patient. J Pediatr Health Care. 2000;14(3):93–102.
McMillian, H. Child maltreatment: what we know in the year 2000. Can J Psychiatry. 2000;45(8):702–709.
Miehl, NJ. Shaken baby syndrome. J Forensic Nurs. 2005;1(3):111–117.
National Center on Shaken Baby Syndrome. Shaken baby syndrome: medical facts. http://www.dontshake.com/Audience.aspx?categoryID=58&PageName=5MedicalFactsAnswers.htm, 2007. [retrieved July 12, 2007, from].
Nelms, BC. Emotional abuse: helping prevent the problem. J Pediatr Health Care. 2001;15(3):103–104.
Pickering, LK. Giardiasis and balantidiasis. In Behrman RE, Kliegman R, Jenson HB, eds.: Nelson textbook of pediatrics, ed 17, Philadelphia: Saunders, 2004.
Powers, K. Diagnosis and management of common toxic ingestions and inhalations. Pediatr Ann. 2000;29(6):330–342.
Putnam, FW. Ten year update review: child sexual abuse. J Am Acad Child Adolesc Psychiatry. 2003;42(3):269–278.
Rose, PW, Harnden, A, Brueggemann, AB, et al. Chloramphenicol treatment for acute infective conjunctivitis in children in primary care: a randomized double-blind placebo-controlled trial. Lancet. 2005;366(9479):37–43.
US Department of Health and Human Services, Administration on Children, Youth and Families Child maltreatment 2005 Washington, DC: US Government Printing Office; 2007. retrieved June 4, 2007, from http://www.acf.hhs.gov/programs/cb/pubs/cm05/index.htm
Walls, C. Shaken baby syndrome education: a role for nurse practitioners working with families of small children. J Pediatr Health Care. 2006;20(5):304–310.
Watson, WA, Litovitz, TL, Rodgers, GC, et al. 2004 Annual report of the American Association of Poison Control Centers Toxic Exposure Surveillance System. Am J Emerg Med. 2005;23(5):589–666.
Woolf, AD, Goldman, R, Bellinger, DC. Update on clinical management of childhood lead poisoning. Pediatr Clin North Am. 2007;54(2):271–294.
*Educational materials may be obtained from the VZV Research Foundation, 1201 Lexington Ave., Suite 204, New York, NY 10028; (212) 222–3390; http://www.vzvfoundation.org; or GlaxoSmithKline, 3030 Cornwallis Road, Research Triangle Park, NC 27709; (800) 825–5249; http://us.gsk.com.
*http://www.cdc.gov/healthyswimming.
*The most common substances in each category are in parentheses. Substances ingested are not necessarily most toxic but often readily available.
*Also available by calling (800) 222–1222 or online at American Association of Poison Control Centers, http://www.aapcc.org.
*Additional information is available from the Child Welfare Information Gateway, Children’s Bureau/ACYF, 1250 Maryland Ave. SW, Eighth Floor, Washington, DC 20024; (703) 835-7565 or (800) 394-3366; http://www.childwelfare.gov.
*Telephone numbers are usually listed under Child Abuse in the business white pages of the local directory, or call the emergency child abuse hotline: (800) 422-4453 ([800] 4-A-CHILD).
*675 West Foothill Blvd., Suite 220, Claremont, CA 91711; (909) 621-6184; http://www.parentsanonymous.org.
†615 15th Street, Modesto, CA, 95354; (209) 572-3446; http://www.parentsunited.info.
*Sources of information are Prevent Child Abuse America, 500 N. Michigan Ave., Suite 200, Chicago, IL 60611; (312) 663-3520 or (800) Children; http://www.preventchildabuse.org; Kempe Children’s Center, 1825 Marion St., Denver, CO 80218; (303) 864-5300, http://www.kempecenter.org; American Humane, 63 Inverness Drive East, Englewood, CO 80112; (303) 792-9900; http://www.americanhumane.org; and Child Welfare Information Gateway, Children’s Bureau/ACYF, 1250 Maryland Ave. SW, Eighth Floor, Washington, DC 20024; (703) 835-7565 or (800) 394-3366; http://www.childwelfare.gov.
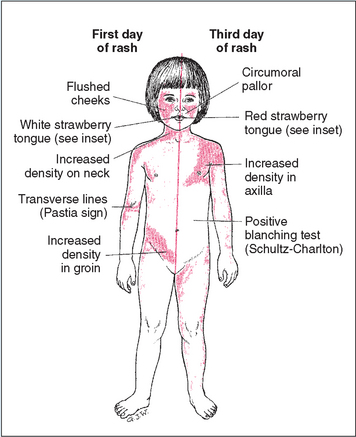
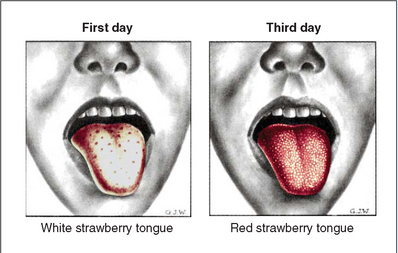
 IN TEXT
IN TEXT
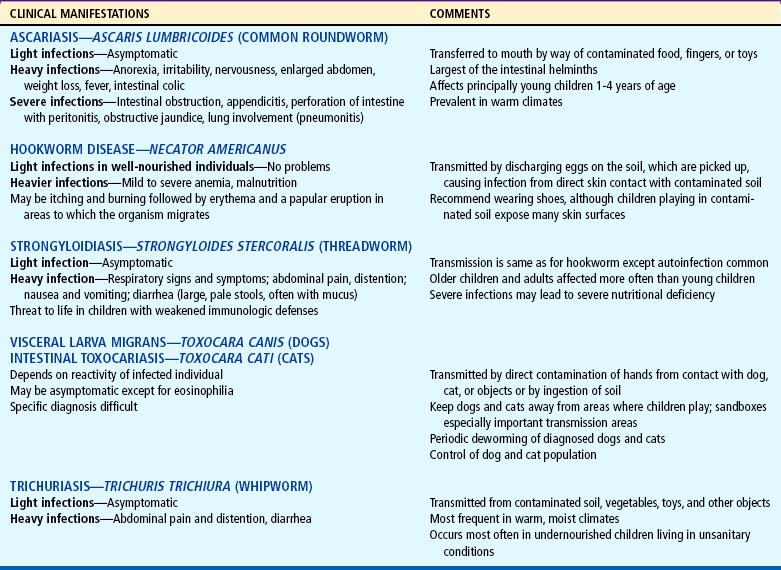
 COMMUNITY FOCUS
COMMUNITY FOCUS CRITICAL THINKING EXERCISE
CRITICAL THINKING EXERCISE FAMILY FOCUS
FAMILY FOCUS CULTURAL AWARENESS
CULTURAL AWARENESS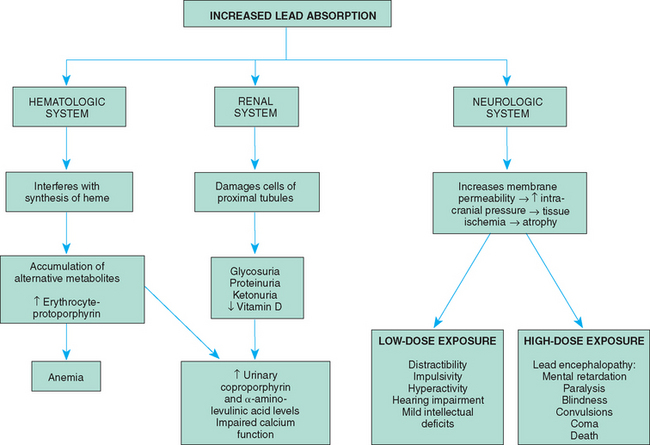
 ATRAUMATIC CARE
ATRAUMATIC CARE