The Child with Integumentary Dysfunction

Impetigo contagiosa. (From Weston WL, Lane AT, Morelli JG: Color textbook of pediatric dermatology, ed 3, St Louis, 2002, Mosby.)

FIG. 30-4 Cellulitis of cheek from puncture wound. (From Weston WL, Lane AT, Morelli JG: Color textbook of pediatric dermatology, ed 4, St Louis, 2007, Mosby.)
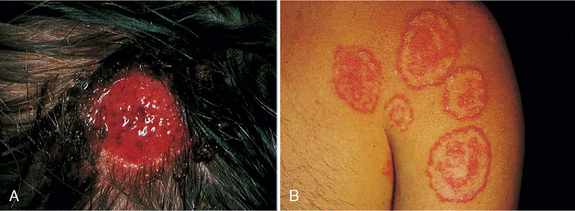
FIG. 30-5 A, Tinea capitis. B, Tinea corporis. Both infections are caused by Microsporum canis, the “kitten” or “puppy” fungus. (From Habif TP: Clinical dermatology: a color guide to diagnosis and therapy, ed 4, St Louis, 2004, Mosby.)
SKIN DISORDERS RELATED TO CHEMICAL OR PHYSICAL CONTACTS
SKIN DISORDERS RELATED TO ANIMAL CONTACTS
On completion of this chapter the reader will be able to:
 Describe the distribution and configuration of various skin lesions.
Describe the distribution and configuration of various skin lesions.
 List the benefits of a moist environment for wound healing.
List the benefits of a moist environment for wound healing.
 Discuss the nursing care related to therapies for skin disorders.
Discuss the nursing care related to therapies for skin disorders.
 Contrast the manifestations of and therapies for bacterial, viral, and fungal infections of the skin.
Contrast the manifestations of and therapies for bacterial, viral, and fungal infections of the skin.
 Compare the skin manifestations related to age in children.
Compare the skin manifestations related to age in children.
 Outline a care plan to prevent and treat diaper dermatitis.
Outline a care plan to prevent and treat diaper dermatitis.
 Outline a care plan for a child with atopic dermatitis.
Outline a care plan for a child with atopic dermatitis.
 Formulate a teaching plan for an adolescent with acne.
Formulate a teaching plan for an adolescent with acne.
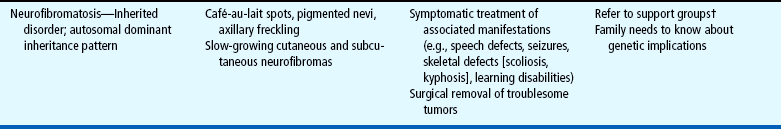
 Describe the methods for assessing a burn wound.
Describe the methods for assessing a burn wound.
 Discuss the physical and emotional care of a child with a severe burn wound.
Discuss the physical and emotional care of a child with a severe burn wound.
INTEGUMENTARY DYSFUNCTION
Lesions of the skin result from a variety of etiologic factors. Skin lesions originate from (1) contact with injurious agents (infective organisms, toxic chemicals, and physical trauma), (2) hereditary factors, (3) external factors (e.g., allergens), or (4) systemic diseases (e.g., measles, lupus erythematosus, nutritional deficiency diseases). Responses to these agents or factors are highly individualized. An agent that is harmless to one individual may be damaging to another, and a single agent may produce varying degrees of response.
An important factor in the etiology of skin manifestations is the child’s age. Infants are subject to “birthmark” malformations and atopic dermatitis (AD) that appear early in life; the school-age child is susceptible to ringworm of the scalp; and acne is a characteristic skin disorder of puberty. Contact dermatitis, such as poison ivy, is seen only when the noxious agent is found in the environment. Tension and anxiety may produce, modify, or prolong skin conditions.
Skin of Younger Children
The major skin layers arise from different embryologic origins. Early in the embryonic period, a single layer of epithelium forms from the ectoderm, while simultaneously the corium develops from the mesenchyme. In the infant and small child the epidermis is loosely bound to the dermis. This poor adherence causes the layers to separate easily during an inflammatory process to form blisters. This is especially true in preterm infants, who have a propensity to blister formation and separation of the skin with minor trauma such as the removal of adhesive tape. In contrast, the skin of the older child is thinner, and the cells of all the strata are more compressed.
Pathophysiology of Dermatitis
More than half of the dermatologic problems in children are forms of dermatitis. This implies a sequence of inflammatory changes in the skin that are grossly and microscopically similar but diverse in course and causation. Acute responses produce intercellular and intracellular edema, the formation of intradermal vesicles, and an initial infiltration of inflammatory cells into the epidermis. In the dermis there is edema, vascular dilation, and early perivascular cellular infiltration. The location and manner of these reactions produce the lesions characteristic of each disorder. The changes are usually reversible, and the skin ordinarily recovers without blemish unless complicating factors such as ulceration from the primary irritant, scratching, and infection are introduced or underlying vascular disease develops. In chronic conditions permanent effects are seen that vary according to the disorder, the general condition of the affected individual, and the available therapy.
Diagnostic Evaluation
Although the history and subjective symptoms of skin lesions are explored first, the obvious objective characteristics of the lesions are often noted simultaneously. Many skin lesions are easily diagnosed after careful inspection.
History and Subjective Symptoms.: Many cutaneous lesions are associated with local symptoms. The most common local symptom is itching (pruritus), which varies in intensity. Pain or tenderness often accompanies some skin lesions. Other skin sensations such as burning, prickling, stinging, or crawling are also described. Alterations in local feeling include absence of sensation (anesthesia); excessive sensitiveness (hyperesthesia); diminished sensation (hypesthesia or hypoesthesia); or abnormal sensation, such as burning or prickling (paresthesia). These symptoms may remain localized or migrate; may be constant or intermittent; and may be aggravated by a specific activity, such as exposure to sunlight.
It is important to determine whether the child has an allergic condition such as asthma or hay fever or history of a previous skin disease. AD, often associated with allergies, frequently begins in infancy. Important questions for the parent include when the lesion or symptom first appeared; whether it occurred with ingestion of a food or other substance, including any medication; and whether the condition was related to activity such as contact with plants, insects, or chemicals.
Objective Findings.: The distribution, size, morphology, and arrangement of skin lesions provide significant information. Extrinsic causes usually result from physical, chemical, or allergic irritants or from an infectious agent such as bacteria, fungi, viruses, or animal parasites. Skin manifestations are also produced by intrinsic causes such as an infection (measles or chickenpox), drug sensitization, or other allergic phenomena.
Types of Lesions.: Skin lesions assume distinct characteristics that are related to the pathologic process. Nurses should become familiar with the common terms that are applied to skin lesions because these terms are used in the processes of record keeping and communication. These terms include:
Erythema—A reddened area caused by increased amounts of oxygenated blood in the dermal vasculature
Ecchymoses (bruises)—Localized red or purple discolorations caused by extravasation of blood into dermis and subcutaneous tissues
Petechiae—Pinpoint, tiny, and sharp circumscribed spots in the superficial layers of the epidermis
Primary lesions—Skin changes produced by a causative factor; common primary lesions in pediatric skin disorders are macules, papules, and vesicles (Fig. 30-1)
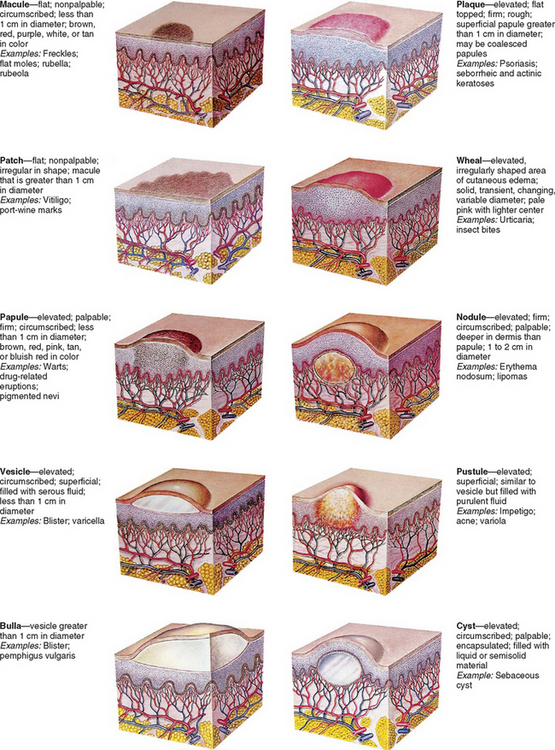
FIG. 30-1 Primary skin lesions. (From Seidel HM, Ball JW, Dains JE, and others: Mosby’s guide to physical examination, ed 6, St Louis, 2006, Mosby.)
Secondary lesions—Changes that result from alteration in the primary lesions, such as those caused by rubbing, scratching, medication, or involution and healing (Fig. 30-2)
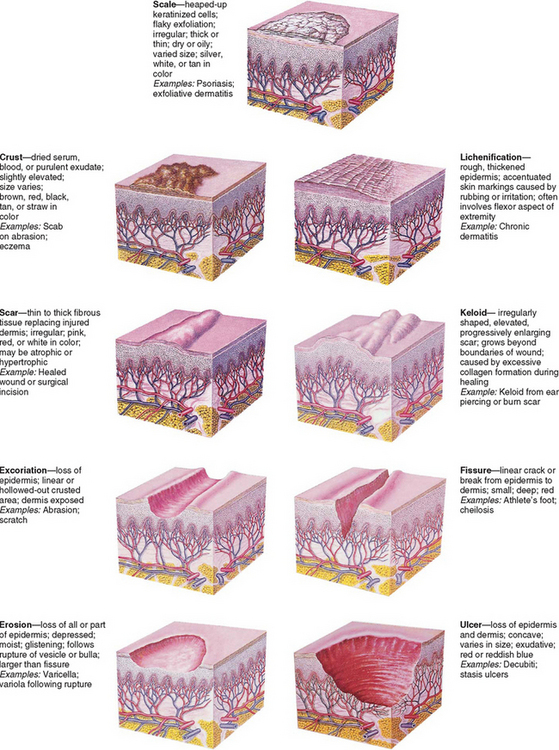
FIG. 30-2 Secondary skin lesions. (From Seidel HM Ball JW, Dains JE, and others: Mosby’s guide to physical examination, ed 6, St Louis, 2006, Mosby.)
Distribution pattern—The pattern in which lesions are distributed over the body, whether local or generalized, and the specific areas associated with the lesions
Configuration and arrangement—The size, shape, and arrangement of a lesion or groups of lesions (e.g., discrete, clustered, diffuse, or confluent)
Laboratory Studies.: If a skin problem is related to a systemic disease (e.g., collagen or immunodeficiency disease), laboratory studies are performed to identify these conditions. Diagnostic techniques include microscopic examination, cultures, skin scrapings or biopsy, cytodiagnosis, patch testing, Wood light examination, allergic skin testing, and other laboratory tests such as blood count and sedimentation rate.
WOUNDS
Wounds are structural or physiologic disruptions of the skin that activate normal or abnormal tissue repair responses. Wounds are classified as acute or chronic. Acute wounds are those that heal uneventfully within 2 to 3 weeks. Chronic wounds are those that do not heal in the expected time frame or are associated with complications. Cofactors that disrupt or delay wound healing include compromised perfusion, malnutrition, and infection. In children, most wounds are acute and can be prevented from becoming chronic wounds through appropriate nursing care. Wounds are also classified as surgical and nonsurgical and then further classified in the same manner as burns: superficial, partial thickness, or full thickness (complex wounds that include muscle or bone).
Epidermal Injuries
Abrasions are the most common epidermal wounds in children, usually in the form of a skinned knee or elbow. In most injuries the margins of the abraded area are superficial, involving only the outer layers of epidermis, although the central portion may extend into the dermis. Epithelial tissue is composed of labile cells, which are constantly destroyed and replaced throughout the life span. Therefore epidermal injuries usually result in rapid, uneventful healing and recovery.
Injury to Deeper Tissues
Tissues composed of permanent cells such as muscle and nerve cells are unable to regenerate. These tissues repair themselves by substituting fibrous connective tissue for the injured tissue. This fibrous tissue, or scar, serves as a patch to preserve or restore the continuity of the tissue. Wounds involving permanent cells include surgical incisions, lacerations, ulcers, evulsions, and full-thickness burns.
Process of Wound Healing
When the skin is injured, its normal protective barrier function is broken. In the healthy immunocompetent individual, acute traumatic abrasions, lacerations, and superficial skin and soft-tissue injuries heal spontaneously without complications. The process of tissue healing involves complex cellular interactions and biochemical reactions. The healing process is segregated into four phases that are characterized by the particular cells involved and the chemicals produced. The four stages of wound healing are hemostasis, inflammation, proliferation, and remodeling (Krasner, Rodeheaver, and Sibbald, 2001). Some authorities combine the first two phases.
In the hemostasis phase, platelets act to seal off the damaged blood vessels and to form a stable clot. Hemostasis occurs within minutes of the initial injury to the skin unless there is an underlying clotting disorder.
Inflammation, the second stage of wound healing, presents a clinical picture that involves erythema, swelling, and warmth, often associated with pain at the wound site. This stage usually lasts up to 4 days after injury. The inflammation phase involves white blood cells such as the neutrophils, monocytes, and macrophages. These cells mount an initial defense against microbial invasion and secrete proteolytic enzymes that destroy nonviable tissue and microorganisms in the wound area.
The proliferative phase, which includes granulation and contracture, is the third stage of healing. This phase lasts from 4 to 21 days in acute wounds, depending on the size of the wound. The phase involves the replacement of dermal tissues and subdermal tissues in deep wounds, as well as the contraction of the wound. The phase is characterized clinically by the presence of granulation tissue, the “beefy,” pebbled red tissue in the wound base. Fibroblasts, or immature connective tissue cells, secrete collagen, which provides the foundation for dermal regeneration. Angiocytes regenerate the outer layers of capillaries, and endothelial cells produce the lining in a process called angiogenesis. The formation of granulation tissue, which provides the foundation for the wound, depends on angiogenesis. The keratinocytes are responsible for epithelialization. In the final stage of epithelialization, contracture occurs as the keratinocytes differentiate and form the protective outer layer, or stratum corneum, of the skin.
Remodeling, or maturation, is the final phase of the healing process. This phase occurs in the dermis as fibroblasts increase the tissue tensile strength and gradually replace type 3 collagen in the scar tissue with type 1 collagen, thicken the collagen fibers, and reorient the collagen fibers along the lines of tissue tension. Fibroblasts disappear as the wound becomes stronger. The wound edges are brought closer together, and a mature scar is formed. Children heal aggressively with abundant scar tissue, especially during growth spurts. The highly elastic quality of children’s skin pulls on the wound, and the wound defends against this pull by forming scar tissue. Remodeling and maturation occur over several months and can take up to 2 years. Thus some wounds that appear to be completely healed can break down suddenly if attention is not paid to the initial causative factors.
The phases of wound healing are complex and may be interrupted by disease conditions, medications, and other systemic and local factors that influence the healing process. When a wound does not follow the “normal wound healing trajectory,” it may become stuck in one of the stages and become a chronic wound. It is important that health care providers understand and address the factors that influence wound healing and prevent the development of chronic wounds.
Factors That Influence Healing
Wound care management has shifted from interventions aimed at maintaining a dry environment to those that promote a moist, crust-free environment that enhances the migration of epithelial cells across the wound and facilitates remodeling. An acute full-thickness wound kept in a moist environment usually reepithelializes in 12 to 15 days, whereas the same wound when kept open to the air heals in about 25 to 30 days.
Numerous factors can delay healing (Table 30-1). For example, traditional practices, such as the use of antiseptics (hydrogen peroxide and povidone-iodine [Betadine] solutions), which were once thought to prevent infection, are now known to have a cytotoxic effect on healthy cells and minimal effect on controlling infections. Povidone-iodine may also be absorbed through the skin in neonates and young children.
GENERAL THERAPEUTIC MANAGEMENT
Some skin disorders demand aggressive therapy, but by and large the major aim of treatment is to prevent further damage, eliminate the cause, prevent complications, and provide relief from discomfort while tissues undergo healing (McCord and Levy, 2006). Factors that contribute to the development of dermatitis and that prolong the course of the disease should be eliminated when possible. The most common causative agents of dermatitis in infants, children, and adolescents are environmental factors (soaps, bubble baths, shampoos, rough or tight clothing, wet diapers, blankets, and toys) and the natural elements (such as dirt, sand, heat, cold, moisture, and wind). Dermatitis may also result from home remedies and medications.
Dressings
No one dressing meets the needs of all wounds. The traditional dry gauze dressing should not be used on open wounds, since it allows the wound surface to dry, does little to prevent bacterial invasion, and adheres to the dried scab so that removal disturbs the newly regenerating epithelial cells. In most instances, traditional gauze dressings have been replaced by dressings that promote moist wound healing (Table 30-2). Moist wound healing increases the rate of collagen synthesis and reepithelialization and decreases pain and inflammation. It also creates an environment for autolytic débridement of necrotic tissue, which creates a clean wound bed and enhances granulation. However, a balance must be achieved between creating a moist wound bed and maintaining a dry periwound area that protects the skin and wound from maceration. The dressing type and frequency of dressing changes help to achieve this balance. The frequency of dressing changes is based on the presence of infection, the type of dressing, the location of the wound, and the amount of drainage. Dressings should always be changed when they are loose or soiled. They should be changed more frequently in areas where contamination is likely (e.g., the sacral area, the buttocks, the tracheal area) or when wound infection is suspected or present.
Topical Therapy
Several agents and methods are available for treatment. In selecting a therapeutic regimen, the practitioner considers (1) the choice of active ingredient, (2) the proper vehicle or base, (3) the cosmetic effect, (4) the cost, and (5) instructions for use. Several basic concepts must also be considered. Overtreatment is avoided. For example, when the dermatitis is acute, topical applications should be mild and bland to avoid further irritation. Broken or inflamed skin, especially in children, is more absorbent than intact skin, and chemicals that are nonirritating to intact skin may be quite irritating to inflamed skin.
Topical applications may be applied to treat the disorder, reduce itching, decrease external stimuli, or apply external heat or cold. The emollient action of soaks, baths, and lotions provides a soothing film over the skin surface that reduces external stimuli. Ordinarily, lukewarm, tepid, or cool applications offer the greatest relief.
Ointments in a petrolatum base provide protection from moisture. Therefore this type of ointment is indicated around gastrostomy tubes, in skinfolds, and in the diaper area. Creams are absorbed by the skin and are used for areas where a nongreasy “feel” is desired (e.g., face, hands).
Topical Corticosteroid Therapy.: Glucocorticoids are the therapeutic agents used most frequently for skin disorders. Their local antiinflammatory effects are merely palliative, so the medication must be applied until the condition undergoes a remission or the causative agent is eliminated. Corticosteroids are applied directly to the affected area, are essentially nonsensitizing, and have only minor side effects. As with the use of any steroids, their use in large amounts may mask signs of infection, and symptoms may be exacerbated after termination of the drug. Families are cautioned that the medication cannot be used for all skin disorders. The concentrations available without prescription are not adequate for stubborn skin conditions (e.g., psoriasis) and may further aggravate inflammation caused by fungus or bacteria. Most parents and children apply too much topical hydrocortisone; therefore they should be counseled that it is both effective and economical to apply only a thin film and to massage it into the skin. Parents and children should also be advised to use the application for no more than 5 to 7 days because these agents may cause depigmentation and other changes in the skin.
Other Topical Therapies.: Other topical treatments include chemical cautery (especially useful for warts), cryosurgery, electrodesiccation (chiefly used for warts, granulomas, and nevi), ultraviolet (UV) therapy (primarily used in psoriasis and acne), laser therapy (especially for birthmarks), and acne therapies such as dermabrasion and chemical peels. New drugs called topical immunomodulators are effective in reducing the itching of AD (eczema) and preventing the recurrence of “flares.”
Systemic Therapy
Systemic drugs may be used as an adjunct to topical therapy in some dermatologic disorders. The drugs most frequently used are corticosteroids, antibiotics, and antifungal agents. Corticosteroids are valuable because of their capacity to inhibit inflammatory and allergic reactions. Dosage is carefully adjusted and gradually tapered to the minimum dosage that is effective and tolerated. In infants and children, the dosage is larger than is usually calculated from body weight ratios. However, prolonged use may temporarily suppress growth.
Antibiotics are used in severe or widespread skin infections. However, because these drugs tend to produce hypersensitivity in some patients, they are used with caution. Antifungal agents are the only means for treating systemic fungal infections.
NURSING CARE MANAGEMENT
The child’s subjective symptoms and the parent’s history provide valuable information to help establish a diagnosis. Older children often describe the condition as painful, itching, or tingling or in other descriptive terms. However, much can be determined by also observing the younger child’s behavior. Does the child scratch? Is the child restless or irritable? Does the child favor or avoid using a body part? A careful history provides important clues. Has the child had access to chemicals or been in the woods or around a woodpile? Has the child eaten a new food? Is the child taking medication? Has the child any known allergy? Do siblings or playmates have similar lesions? What soap or bubble bath is used for bathing?
It is important for nurses to not only describe but also assess skin lesions and wounds. The color, shape, and distribution of lesions and wounds are important. Individual lesions are described according to standard terminology. Sometimes two descriptors are used for a particular characteristic (e.g., maculopapular rash). To confirm or amplify the findings made by inspection, the nurse may gently palpate the skin to detect characteristics such as temperature, moisture, texture, elasticity, and edema. Wounds are assessed for depth of tissue damage, evidence of healing, and signs of infection.
The frequency of wound assessment depends on the severity and complexity of the wound. For example, simple or chronic wounds are assessed weekly; infected or complex wounds are assessed daily. Wounds are measured at least weekly (height, width, and depth). The wound bed is assessed for color, drainage, odor, necrosis, granulation tissue, fibrin slough, undermining and condition of the wound edges, and the color and condition of the surrounding skin.
Therapeutic programs are designed to include general measures such as rest, protection, and relief of discomfort and specific treatments such as medication and physical techniques. Only a few skin diseases are contagious; therefore it is usually not necessary to isolate the affected child, except from persons in danger of acquiring a secondary infection (e.g., a child receiving large doses of corticosteroids or other immunosuppressant drugs or a child with an immunologic deficiency disorder). However, if the skin manifestation is caused by a viral exanthema, such as measles or chickenpox, the child is prevented from exposing other susceptible children.
Wound Care
Parents can generally manage small skin lesions or wounds at home. The parents are instructed to wash their hands and then wash the wound gently with mild soap and water or normal saline. They are cautioned to avoid povidone-iodine, alcohol, and hydrogen peroxide because these products are toxic to wounds.
Open wounds are covered with a dressing, such as a commercial adhesive bandage, although larger wounds may benefit from the use of occlusive dressings (see Table 30-2). If occlusive dressings are applied, parents should learn how to apply and remove the dressings correctly. For example, hydrocolloid dressings adhere best if a wide margin is left around the wound and the dressing is pressed against intact skin until it adheres. If a dressing needs to be secured, a nonalcohol skin barrier can be applied to protect the skin, or the wound can be “picture framed” with hydrocolloid dressing and dressing tape can be secured to the hydrocolloid. This method of securing the dressing protects the skin when the tape is removed. Montgomery straps or stretch netting can also be used to secure dressings and to avoid the use of tape.
Dressings are removed carefully to protect intact skin and the epithelial surface of the wound. When removing transparent or hydrocolloid dressings, the nurse or parent should raise one edge of the dressing and pull parallel to the skin to loosen the adhesive. The longer the dressings are left on, the easier they are to remove. Less frequent dressing changes decrease wound contamination.
Lacerations present a special challenge. The injured child and family are usually distressed by the bleeding. In particular, scalp lacerations tend to bleed profusely. Parental guilt and shock usually accompany the injury. The initial nursing intervention is to apply pressure to the area and to attempt to calm the child before further examination. Unless there is bleeding from a severed artery, the wound is cleansed with a forced jet of sterile tepid water or saline (via syringe) and examined for extent; depth; and presence of foreign material such as dirt, glass, or fabric fragments.
The location of the wound facilitates assessment. Wounds over bony areas may contain bone chips, and clear fluid seeping from severe head wounds may indicate cerebrospinal fluid. A pressure dressing is applied for transfer to medical care. After the child is in a medical facility, he or she is prepared for suturing.
Puncture wounds that do not require a tetanus booster are soaked in warm water and soap for several minutes. Causing the wound to rebleed may be helpful. An adhesive bandage can be applied if desired. Puncture wounds of the head, chest, or abdomen or those that could still contain a portion of the puncturing object must be evaluated carefully.
Parents are cautioned against opening blisters or kissing a wound “to make it better.” The wound can easily become contaminated from germs in the human mouth. If scabs form, they are allowed to slough off without assistance; picking or early removal may cause scarring and secondary infection. Parents are advised to seek medical help if there is evidence of infection.
Relief of Symptoms
Most therapeutic regimens for skin lesions are directed toward relief of pruritus, the most common subjective complaint. Cooling the affected area and increasing the skin pH with cool baths or compresses and alkaline applications (e.g., baking soda baths) are helpful in reducing the itching. Clothing and bed linen should be soft and lightweight to decrease the irritation from friction and stimulation.
During treatment, both the affected and unaffected skin is protected from damage and secondary infection. Preventing scratching is important. Older children can cooperate, although they may need to be reminded to stop scratching or rubbing. However, small or uncooperative children may require the use of devices such as mittens (especially during sleep) or special coverings. Keeping fingernails clean, short, and trimmed reduces the risk of secondary infection.
Antipruritic medications, such as diphenhydramine (Benadryl) or hydroxyzine (Atarax), may be prescribed for severe itching, especially if it disturbs the child’s rest. Pain and discomfort are usually managed with nonpharmacologic measures and mild analgesia. Severe pain requires more potent medication. Occlusive dressings over wounds reduce pain. For suturing wounds a topical anesthetic or intradermal buffered lidocaine should be used (see Pain Management, Chapter 7).
Topical Therapy
The specific type of topical therapy and the mode of application depend on the nature and location of the lesion. It is especially important to wash the hands before and after application of any topical therapy. The skin is assessed before the application and reassessed after treatment. Any observed changes are noted and described.
Wet compresses or dressings cool the skin by evaporation, relieve itching and inflammation, and cleanse the area by loosening and removing crusts and debris. A variety of ingredients, such as plain water or Burow solution (available without a prescription), can be applied on Kerlix gauze; plain gauze; or (preferably) soft cotton cloths such as freshly laundered handkerchiefs or strips from diaper, sheeting, or pillowcase material.
Dressings immersed in the desired solution are wrung out slightly and applied to the affected area wet but not dripping. They are applied flat and smooth in such a way that motion is not totally restricted—fingers are wrapped separately, and arms and legs are wrapped so that elbows and knees can bend. Dressings are held in place by Kerlix or other cotton wrap, tubular stockinette, mittens, and socks (two pairs—one to hold the dressings in place, the other to protect from movement). When evaporation begins to dry them, the dressings are removed, rewet in the solution, and reapplied using aseptic technique. The solution is not poured or applied with a syringe directly over the dressings. As fluid evaporates, the solution becomes more concentrated, and this could damage sensitive lesions.
Fresh solution at room temperature is applied at 2-, 3-, or 4-hour intervals and allowed to remain on the lesion from 20 to 90 minutes. Wet dressings are seldom continued after about 48 hours. The child is protected against chilling during treatment, and no more than 20% of the body is covered with a dressing at one time to avoid the risk of hypothermia. After treatment, the skin is dried thoroughly by patting with a towel. Lotion or other medication (if prescribed) is applied at this time.
When children are uncooperative in the use of wet dressings, soaks are often used for removal of crusts and for their mild astringent action. The same solutions are used as for wet compresses. Gaining young children’s cooperation for hand or foot soaks is difficult unless the procedure is accompanied by play. Older infants and toddlers delight in playing with brightly colored objects or poker chips scattered over the bottom of the receptacle, and preschoolers can be challenged to hold a floating item beneath the water’s surface. However, these activities require supervision; infants and small children place items in their mouths, and children easily lose control with water play. Washing dishes, cars, dolls, or doll clothes will also occupy time during soaks.
Although older children can cooperate, they, too, need something to do during the procedure, such as listening to music or a story or watching television. Placing the solution and the extremity in a plastic sealable bag is an effective method to soak a hand or foot.
Baths are useful in the treatment of widespread dermatitis by evenly distributing the soothing antipruritic and antiinflammatory effects of the solution, usually oatmeal or mineral oil preparations. The solution is added to a tub of lukewarm water. The temperature of the bath is tepid, and the treatment usually lasts 15 to 30 minutes. Therapeutic baths are more interesting when toy boats or other items for water play accompany the procedure.
Topical applications are applied to skin lesions to ease discomfort, prevent further injury, and facilitate healing. A thin application of the ointment or cream may be covered with a plastic film and anchored with adhesive, covered with a commercial transparent dressing, or wrapped in Kerlix gauze and held in place by a stretchy net dressing. Topical preparations are applied systematically with the contour of the body surface (not simply up and down). Children love to be “painted,” and lotion applications can be fun when an ordinary paintbrush is used. Regardless of the type of preparation used, parents need detailed information on how to apply it and how long the preparation should remain on the skin.
HOME CARE AND FAMILY SUPPORT
Dermatologic conditions always involve the family, but few situations require hospitalization and most care is delivered at home. Because the family members must carry out the treatment plan, their cooperation is essential. Regimens that are simple to accomplish in the clinic, hospital, or primary care provider’s office may be frustrating and baffling at home. The family may also need assistance in adapting equipment available for home therapy.
It is important that the child and family be given as detailed explanations as possible about both the expected and unexpected results of treatment, including any ill effects that might occur. If unexplained reactions develop, the family is directed to discontinue treatment and report the reactions to the appropriate person. The use of over-the-counter medicines is discouraged unless the preparations have been discussed with the health care provider and have received approval.
Because the skin is the most visible portion of the body, defects in its surface alter its appearance and cause distress for the child. Skin problems may also result in rejection by others. Parents of other children may fear that their children will “catch” the disorder. Occasionally the affected child’s own family members reduce their interaction or physical contact with the child. This is seldom a problem with dermatitis of short duration, but chronic conditions can frequently create problems and affect the child’s self-esteem.
INFECTIONS OF THE SKIN
Normally, the skin harbors a variety of bacterial flora, including the major pathogenic varieties of staphylococci and streptococci. The degree of pathogenicity of the organism depends on its invasiveness and toxicity, the integrity of the skin, and the immune and cellular defenses of the host. Children with congenital or acquired immunodeficiency disorders (such as acquired immunodeficiency syndrome [AIDS]), those in a debilitated condition, those receiving immunosuppressant therapy, and those with a generalized malignancy such as leukemia or lymphoma are at risk for developing bacterial infections.
Because of the characteristic “walling-off” process of the inflammatory reaction (abscess formation), staphylococci are more difficult to treat, and the local infected area is associated with an increase in bacteria all over the skin surface that serves as a source of continuing infection. In previous years, methicillin-resistant Staphylococcus aureus (MRSA) infections were primarily seen in nursing homes and hospitals. In recent years, the number of MRSA community-acquired infections has risen (Kaplan, 2006). All these factors underline the importance of careful hand washing and cleanliness when caring for infected children and their lesions to prevent the spread of infection and as an essential prophylactic measure when caring for infants and small children. Common bacterial skin disorders are outlined in Table 30-3.
Nursing Care Management
The major nursing interventions related to bacterial skin infections are to prevent the spread of infection and to prevent complications. Impetigo contagiosa and MRSA infection can easily spread by self-inoculation; therefore the child must be cautioned against touching the involved area. Hand washing is mandatory before and after contact with an affected child, and this practice is emphasized to all those who care for the child. Many children with AD are colonized with MRSA in the nares and under the fingernails. For many bacterial infections, and for MRSA infection in particular, the child should be provided with washcloths and towels separate from those of other family members. Pajamas, underwear, and other clothes should be changed daily and washed in hot water. Razors used for shaving should be discarded after each use and not shared. To prevent recurrence, some infectious disease specialists recommend bathing in a chlorine bath twice weekly with 1 tsp of chlorine per gallon of water.
Children and parents are often tempted to squeeze follicular lesions. They must be warned that squeezing will not hasten the resolution of the infection and that there is a risk of making the lesion worse or spreading the infection. No attempt should be made to puncture the surface of the pustule with a needle or sharp instrument. A child with a sty may waken with the eyelids of the affected eye sealed shut with exudate. The child or the parents are instructed to gently wipe the lid from the inner to the outer edge with warm water and a clean washcloth until the exudate is removed.
The child with limited cellulitis of an extremity is usually managed at home on a regimen of oral antibiotics and warm compresses. The parents are taught the procedures and instructed in administration of the medication. Children with more extensive cellulitis, especially around a joint with lymphadenitis or on the face, are usually admitted to the hospital for parenteral antibiotics with continued treatment at home. Nurses are responsible for teaching the family to administer the medication and apply compresses.
VIRAL INFECTIONS
Viruses are intracellular parasites that produce their effect by using the intracellular substances of the host cells. Composed of only a deoxyribonucleic acid (DNA) or ribonucleic acid (RNA) core enclosed in an antigenic protein shell, viruses are unable to provide for their own metabolic needs or to reproduce themselves. After a virus penetrates a cell of the host organism, it sheds the outer shell and disappears within the cell, where the nucleic acid core stimulates the host cell to form more virus material from its intracellular substance. In a viral infection the epidermal cells react with inflammation and vesiculation (as in herpes simplex) or by proliferating to form growths (warts).
Many of the communicable viral diseases of childhood are associated with rashes, and each rash is characteristic. The type of lesion and the configuration of rubeola, rubella, and chickenpox are described in Table 14-1. Other common viral disorders of the skin are outlined in Table 30-4.
DERMATOPHYTOSES (FUNGAL INFECTIONS)
The dermatophytoses (ringworm) are infections caused by a group of closely related filamentous fungi that invade primarily the stratum corneum, hair, and nails. These are superficial infections that live on, not in, the skin. They are confined to the dead keratin layers and are unable to survive in the deeper layers. Because the keratin is desquamated constantly, the fungus must multiply at a rate that equals the rate of keratin production to maintain itself; otherwise the infection would be shed with the discarded skin cells. Common dermatophytoses are outlined in Table 30-5.
Dermatophytoses are designated by the Latin word tinea, with further designation related to the area of the body where they are found (e.g., tinea capitis [ringworm of the scalp]). Dermatophyte infections are most often transmitted from one person to another or from infected animals to humans. Diagnosis is made from microscopic examination of scrapings taken from the advancing periphery of the lesion, which almost always produces a scale.
Nursing Care Management
When teaching families how to care for ringworm, the nurse should emphasize good health and hygiene. Because of the infectious nature of the disease, affected children should not exchange grooming items, headgear, scarves, or other articles of apparel that have been in proximity to the infected area with other children. Affected children are provided with their own towels and directed to wear a protective cap at night to avoid transmitting the fungus to bedding, especially if they sleep with another person. Because the infection can be acquired by animal-to-human transmission, all household pets should be examined for the disorder. Other sources of infection are seats with headrests (theater seats), seats in public transportation vehicles, helmets, and gymnasium mats.
Both 2% ketoconazole and 1% selenium sulfide shampoos may reduce colony counts of dermatophytes. These shampoos can be used in combination with oral therapy to reduce the transmission of disease to others. The shampoo should be applied to the scalp for 5 to 10 minutes at least three times per week. The child may return to school once the therapy is initiated.
Alternately, if the child is treated with the drug griseofulvin, the therapy frequently continues for weeks or months, and because subjective symptoms subside, children or parents may be tempted to decrease or discontinue the drug. The nurse should emphasize to family members the importance of maintaining the prescribed dosage schedule and of taking the medication with high-fat foods for best absorption. They are also instructed regarding possible drug side effects, such as headache, gastrointestinal upset, fatigue, insomnia, and photosensitivity. For children who take the drug over many months, periodic testing is required to monitor leukopenia and assess liver and renal function. Newer antifungal medications such as terbinafine, itraconazole, and fluconazole may be used when there are adverse reactions to griseofulvin. Currently, these drugs are being studied to determine their efficacy and safety in treating tinea capitis in children but are not approved by the U.S. Food and Drug Administration (FDA) for this indication at this time.
SYSTEMIC MYCOTIC (FUNGAL) INFECTIONS
Mycotic (systemic or deep fungal) infections have the capacity to invade the viscera, as well as the skin. The most common infections are the lung diseases, which are usually acquired by inhalation of fungal spores. These fungi produce a variable spectrum of disease, and some are common in certain geographic areas. They are not transmitted from person to person but appear to reside in the soil, from which their spores are airborne. The cutaneous lesions caused by deep fungal infections are granulomatous and appear as ulcers, plaques, nodules, fungating masses, and abscesses. The course of deep fungal diseases is chronic with slow progression that favors sensitization (Table 30-6).
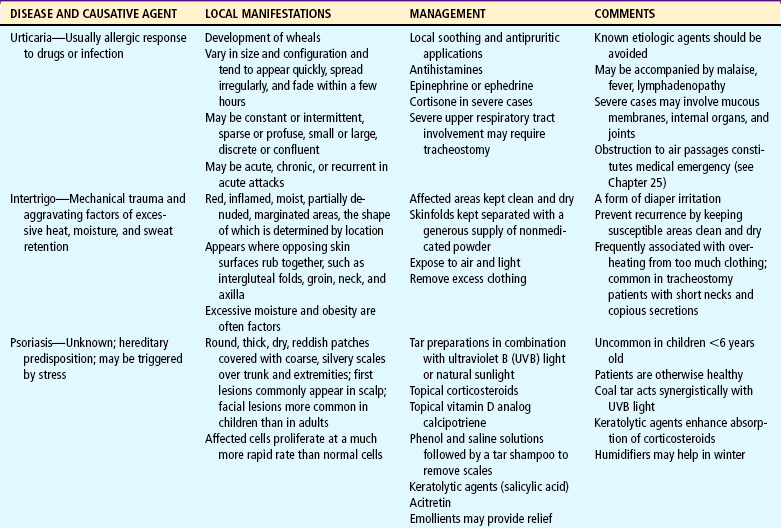
SKIN DISORDERS RELATED TO CHEMICAL OR PHYSICAL CONTACTS
Contact dermatitis is an inflammatory reaction of the skin to chemical substances, natural or synthetic, that evoke a hypersensitivity response or direct irritation. The initial reaction occurs in an exposed region, most commonly the face and neck, backs of the hands, forearms, male genitalia, and lower legs. Early in the reaction, there is usually a sharp delineation between inflamed and normal skin that ranges from a faint, transient erythema to massive bullae on an erythematous swollen base. Itching is a constant symptom.
The cause may be a primary irritant or a sensitizing agent. A primary irritant is one that irritates any skin. A sensitizing agent produces an irritation on those individuals who have met the irritant or something chemically related to it, have undergone an immunologic change, and have become sensitized. Prior exposure is not necessarily a factor in the reaction. A sensitizer irritates in relatively low concentrations only persons who are allergic to it.
In infants, contact dermatitis occurs on the convex surfaces of the diaper area (see Diaper Dermatitis, p. 1084). Other agents that produce contact dermatitis include plants (poison ivy, oak, or sumac), animal irritants (wool, feathers, and furs), metal (nickel found in jewelry and the snaps on sleepers and denim), vegetable irritants (oleoresins, oils, and turpentine), synthetic fabrics (e.g., shoe components), dyes, cosmetics, perfumes, and soaps (including bubble baths). The list is endless.
The major goal in treatment is to prevent further exposure of the skin to the offending substance. Provided there is no further irritation, the skin’s normal recuperative powers will often produce healing without treatment. Otherwise, treatment of contact dermatitis is based on severity. Mild cases are treated with topical steroids. Mild to moderately severe cases may require a 2-week course of strong topical corticosteroids. Very severe cases require systemic corticosteroids (Kronemyer, 2003).
Nursing Care Management
Nurses frequently detect evidence of contact dermatitis during routine physical assessments. Skin manifestations in specific areas suggest limited contact, such as around the eyes (mascara), areas of the body covered by clothing but not protected by undergarments (wool), or areas of the body not covered by clothing (UV injury). Generalized involvement is more likely to be caused by bubble bath or soap. Often nurses can determine the offending agent and counsel families regarding management. However, if the lesions persist, are extensive, or show evidence of infection, medical evaluation is indicated.
POISON IVY, OAK, AND SUMAC
Contact with the dry or succulent portions of any of three poisonous plants (ivy, oak, and sumac) produces localized, streaked or spotty, oozing, and painful impetiginous lesions. The offending substance in these plants is an oil, urushiol, that is extremely potent. Sensitivity to urushiol is not inborn but is developed after one or two exposures and may change over a lifetime. All parts of the plants contain the oil, including dried leaves and stems (Fig. 30-6). Even smoke from burning brush piles can produce a reaction.
Animals do not seem to be affected by the oil; however, dogs or other animals that have run or played in the plants may carry the sap on their fur, and animals that eat the plants can transfer the oil in their saliva. Shoes, tools, and toys can transfer the oil. Golf balls that have been in the rough are another source of contact.
Urushiol takes effect as soon as it touches the skin. It penetrates through the epidermis and bonds with the dermal layer, where it initiates an immune response. The full-blown reaction is evident after about 2 days, with redness, swelling, and itching at the site of contact. Several days later, streaked or spotty blisters oozing serum from damaged cells produce the characteristic impetiginous lesions (Fig. 30-7). The lesions dry and heal spontaneously, and itching stops by 10 to 14 days.

FIG. 30-7 Poison ivy lesions. Note “streaked” blisters surrounding one large blister. (From Habif TP: Clinical dermatology: a color guide to diagnosis and therapy, ed 4, St Louis, 2004, Mosby.)
Therapeutic Management
As soon as an exposure is realized, there is no time to waste. The earlier the skin is cleansed, the greater the chance of removing the urushiol before it attaches to the skin. The exposed skin can be cleansed with isopropyl alcohol followed by water. A shower with soap and warm water should follow. Clothes, tools, shoes and any other objects that had contact with the plants should be cleaned with alcohol and then water.
Treatment of the lesions includes calamine lotion, soothing Burow solution compresses, or Aveeno baths to relieve discomfort. Topical corticosteroid gel is effective for prevention or relief of inflammation, especially when applied before blisters form. Oral corticosteroids may be needed for severe reactions, and a sedative such as diphenhydramine may be ordered.
Nursing Care Management
When it is known that the child has made contact with the plant, the area is immediately flushed (preferably within 15 minutes) with cold running water to neutralize the urushiol not yet bonded to the skin. If there is a stream nearby, an effective method is to have the child enter the water (clothes and all) and allow the water to rinse the oil from both skin and clothing. Harsh soap is contraindicated because it removes protective skin oils and dilutes the urushiol, allowing it to spread; hard scrubbing irritates the skin. All clothing that has come in contact with the plant is removed with care and thoroughly laundered in hot water and detergent. Every effort is made to prevent the child from scratching the lesions. Although the lesions do not spread by contact with the blister serum or from scratching, they can become secondarily infected (see Critical Thinking Exercise).
Prevention.: Prevention is best accomplished by avoiding contact and removing the plant from the environment. All children, especially those known to be sensitive, should be taught to recognize the plant. Information regarding means for destroying plants can be obtained from the U.S. Department of Agriculture or U.S. Forestry Service. If poisonous plants are growing in public community area, the local authorities should be contacted to remove the plants. A cream that protects exposed skin from poison oak and ivy is Ivy Block.
DRUG REACTIONS
Adverse reactions to drugs are seen more often in the skin than in any other organ, although any organ of the body can be affected. The reaction may be a result of toxicity related to drug concentration, individual intolerance to the average dosage of the drug, or an allergic or idiosyncratic response. The manifestations may be associated with side effects or secondary effects of a drug, either of which are unrelated to its primary pharmacologic actions.
Although any drug is capable of producing a reaction in the susceptible individual, some drugs have a tendency to produce a particular reaction consistently, and others are more likely to produce an untoward effect. Many are allergenic responses that occur after a previous administration of the drug, even a topical application. Other factors influence a drug response in a particular individual. For example, the incidence increases with the amount and number of drugs given.
Manifestations of drug reactions may be delayed or immediate. A period of 7 days is usually required for a child to develop sensitivity to a drug that has never been administered previously. With prior sensitivity the manifestations appear almost immediately. Rashes are the most common manifestation of adverse drug reactions in children. However, individual drug reactions may vary from a single lesion to extensive, generalized epidermal necrosis such as that seen in Stevens-Johnson syndrome (see Table 30-9). Cutaneous manifestations can resemble almost any skin disease and can be seen in almost any degree of severity. With few exceptions, the distribution of a drug eruption is widespread because it results from a circulating agent; appears as an inflammatory response with itching; is sudden in onset; and may be associated with constitutional symptoms such as fever, malaise, gastrointestinal upsets, anemia, or liver and kidney damage.
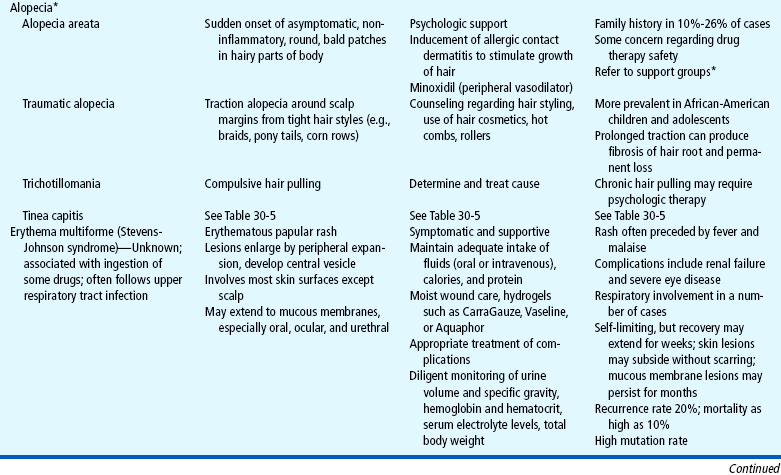
TABLE 30-9
*National Alopecia Areata Foundation, 14 Mitchell Blvd., San Rafael, CA 94903; (415) 472-3780; fax: (415) 472-5343; e-mail: info@naaf.org: http://www.naaf.org.
†Children’s Tumor Foundation, 95 Pine St., 16th Floor, New York, NY 10005; (800) 323-7938 or (212) 344-6633; fax: (212) 747-0004; e-mail:info@naaf.org: http://www.ctf.org.
In most cases treatment for simple cutaneous reactions consists of discontinuing the drug. Sometimes a decision is made to continue the drug (such as an antibiotic in an infant or small child) until the cause of the rash is clearly indicated. In urticarial-type eruptions antihistamines may be ordered, and for widespread and severe lesions corticosteroids are beneficial. Severe anaphylactic reactions are a medical emergency (see Anaphylaxis, Chapter 25).
Nursing Care Management
The most effective means of management is prevention. Parents always remember a severe reaction. A careful history will elicit evidence of a previous drug reaction. The history should include the name of the drug, nature of the reaction, drug dosage, and how soon after administration the reaction occurred (see Chapter 6).
Nurses who suspect that a rash is caused by a medication should withhold any further dose and report the eruption to the practitioner. Frequent offenders in drug reactions are penicillin and sulfonamides, and nurses must be alert to this possibility. However, even commonplace drugs, including aspirin, barbiturates, chemical agents in some foods, flavoring agents, and preservatives, are capable of producing an undesired response. Persons who have severe reactions should wear a medical identification bracelet or necklace in case of emergency or inadvertent administration of the offending drug.
FOREIGN BODIES
Parents can remove small wooden splinters with a needle and tweezers that have been sterilized with alcohol or a flame. The area around the sliver is washed with soap and water before removal is attempted. The sliver is exposed with the needle, then grasped firmly by the tweezers and pulled out. Some foreign bodies, such as a fishhook, pieces of glass, a difficult-to-see object, or a deeply embedded object (such as a needle in a foot or near a joint), require medical evaluation.
Small cactus prickles or spines are troublesome to remove, but the following methods may prove helpful:
SKIN DISORDERS RELATED TO ANIMAL CONTACTS
Bites and stings account for a significant amount of mild to moderate discomfort in children. Most bites and stings are managed by simple symptomatic measures, such as compresses, calamine lotion, and prevention of secondary infection. Arthropods include insects and arachnids, such as mites, ticks, spiders, and scorpions. Most arthropods in the United States, including tarantulas, are relatively harmless. Although all spiders produce venom that is injected via fangs, some are unable to pierce the skin and others produce venom that is insufficiently toxic to be harmful. Only scorpions and two spiders—the brown recluse and the black widow—inject venom deadly enough to require immediate attention. Children bitten by these arachnids must receive medical attention as soon as possible. Major offending creatures, their manifestations, and management are outlined in Table 30-7.
When a hymenopteran (bees in particular) stings, its barbed stinger penetrates the skin. As long as the stinger remains in the skin, the muscles push the stinger deeper and the venom is pumped into the wound. The best approach is to remove the stinger as quickly as possible and to get away from the vicinity of other insects to prevent further injury. Children who have become sensitized to hymenopteran bites may demonstrate a severe systemic response that can be life threatening. One sting can produce generalized urticaria, respiratory difficulty (from laryngeal edema), hypotension, and death. Intramuscular administration of epinephrine provides immediate relief and must be available for emergency use.
Hypersensitive children should wear a medical identification bracelet. They should also have a kit that contains epinephrine and a hypodermic syringe. Families are reminded to check the expiration date on the kit and to replace an outdated one. They should determine whether a nurse is available at the school and the school policy regarding administration of drugs. If a school nurse is not present, someone at the school should be designated to inject the epinephrine in case of an emergency.
SCABIES
Scabies is an endemic infestation caused by the scabies mite, Sarcoptes scabiei. Lesions are created as the impregnated female burrows into the stratum corneum of the epidermis (never into living tissue) to deposit her eggs and feces. The inflammatory response and intense itching occur after the host becomes sensitized to the mite, approximately 30 to 60 days after initial contact. If the person has been previously sensitized to the mite, the response occurs within 48 hours after exposure. After this time, the areas over which the mite has traveled will begin to itch and develop the characteristic eruption (Box 30-1). Consequently, mites will not necessarily be located at all sites of eruption.
There is great variability in the type of lesions. Infants often develop an eczematous eruption; therefore the observer must look for discrete papules, burrows, or vesicles.
Nursing Care Management
The treatment of scabies is the application of a scabicide. Currently, permethrin 5% cream (Elimite) is the drug of choice. Alternative drugs are 1% lindane cream or lotion and 10% crotamiton. Permethrin is preferred because it is safer, it avoids the risk of neurotoxicity, and it is more effective than lindane. Nurses instructing families in the use of scabicides should emphasize the importance of following directions carefully. Lindane should not be used immediately after a bath or shower. Permethrin is applied to all skin surfaces from the neck down to the toes (not just areas with rash, but also areas between the fingers and toes, the umbilicus, and the cleft of the buttocks). The cream should remain on the skin for 8 to 14 hours and then be removed by bathing. Lindane is removed by bathing after 8 to 12 hours. A second treatment with the same lotion may be required 7 to 10 days later. Lindane should not be used for preterm infants, young infants, people with known seizure disorders, people with hypersensitivity to the product, patients with crusted scabies, or patients with extensive dermatitis. Pregnant women and younger children are often treated with milder scabies medications. Crotamiton is applied once a day for 2 days, followed by a cleansing bath 48 hours after the last application. All clothes, bedding, and towels used by the infested person 3 days before treatment should be washed in hot water and dried in a hot dryer (Centers for Disease Control and Prevention, 2008).
Another prescription drug used to treat scabies is ivermectin (Frankowski and Weiner, 2002). Ivermectin is administered orally in a single dose for treatment of severe or crusted scabies. It should be considered for patients whose infestation is refractory or those who cannot tolerate topical scabicides. However, the safety and efficacy of ivermectin for pediatric patients younger than 5 years of age or children weighing less than 15 kg (33 pounds) is not established. This drug is not currently licensed for treatment of scabies by the FDA (American Academy of Pediatrics, 2006). Families need to know that although the mite that causes scabies will be killed with these treatments, the rash and the itch will not be eliminated until the stratum corneum is replaced in approximately 2 to 3 weeks. Soothing ointments or lotions can be applied for itching. Antibiotics may be given for secondary infection.
PEDICULOSIS CAPITIS
Pediculosis capitis (head lice) is an infestation of the scalp by Pediculus humanus capitis, a common parasite in school-age children. The adult louse lives only about 48 hours when away from a human host, and the life span of the average female is 1 month. The female lays her eggs at night at the junction of a hair shaft and close to the skin because the eggs need a warm environment. The nits, or eggs, hatch in approximately 7 to 10 days. Itching is usually the only symptom. Common areas involved are the occipital area, behind the ears, and the nape of the neck (Box 30-2).
Diagnostic Evaluation
Diagnosis is made by observation of the white eggs (nits) firmly attached to the hair shafts (Fig. 30-9). Because of their brief life span and mobility, adult lice are more difficult to locate. Nits must be differentiated from dandruff, lint, hair spray, and other items of similar size and shape. Scratch marks or inflammatory papules, caused by secondary infection, may also be found on the scalp in the vulnerable areas.
Therapeutic Management
Treatment consists of the application of pediculicides and manual removal of nit cases. The drug of choice for infants and children is permethrin 1% cream rinse (Nix), which kills adult lice and nits. This product and preparations of pyrethrin with piperonyl butoxide (RID or A-200 Pyrinate) can be obtained without a prescription and are more effective and safer than lindane (Strong and Johnstone, 2008). The FDA has issued a warning regarding the use of lindane because of the potential for neurotoxicity (US Food and Drug Administration, 2003). Although the FDA believes that the benefits of lindane outweigh the risks when used as directed, patients should be treated with these medications when other treatments are not tolerable or have failed. Another product approved for treatment of head lice, malathion 0.5% (Ovide), is available only by prescription. However, malathion contains flammable alcohol, must remain on the hair for 8 to 12 hours, and is not recommended for children younger than 6 years of age.
Because of concerns that head lice may be developing resistance to chemical shampoos and that repeated exposure of children to strong chemicals on the scalp may be unwise, effective nonchemical control measures are essential. Daily removal of nits from the child’s hair with a metal nit comb at least every 2 or 3 days is a control measure following treatment with a pediculicide (Mumcuoglu, Barker, Burgess, and others, 2007).
Nursing Care Management
An important nursing role is educating the parents about pediculosis. Nurses should emphasize that anyone can get pediculosis; it has no respect for age, socioeconomic level, or cleanliness. The louse does not jump or fly, but it can be transmitted from one person to another on personal items. Lice are more likely to infest Caucasian children, those with straight hair, and girls. Children are cautioned against sharing combs, hair ornaments, hats, caps, scarves, coats, and other items used on or near the hair. Children who share lockers are more likely to become infested, and slumber parties place children at risk. Lice are not carried or transmitted by pets.
Nurses or parents should carefully inspect children who scratch their head more than usual for bite marks, redness, and nits. The hair is systematically spread with two flat-sided sticks or tongue depressors, and the scalp is observed for any movement that indicates a louse. Nurses should wear gloves when examining the hair. Lice are small and grayish tan, have no wings, and are visible to the naked eye. The nits, or eggs, appear as tiny whitish oval specks adhering to the hair shaft about 6 mm (0.25 inch) from the scalp. The adherent nature of the nits distinguishes them from dandruff, which falls off readily. Empty nit cases, indicating hatched lice, are translucent rather than white and are located more than 6 mm from the scalp (see Fig. 30-9).
If evidence of infestation is found, it is important to treat the child according to the directions on the label of the pediculicide. Parents are advised to read the directions carefully before beginning treatment. The child is made as comfortable as possible during the application process because the pediculicide must remain on the scalp and hair for several minutes. Playing “beauty parlor” during the shampoo is a useful strategy. The child lies supine, with the head over a sink or basin, and covers the eyes with a dry towel or washcloth. This prevents medication, which can cause chemical conjunctivitis, from splashing into the eyes. If eye irritation occurs, the eyes must be flushed well with tepid water. It is not necessary to remove the nits after treatment because only live lice cause infestation. However, because none of the pediculicides is 100% effective in killing all the eggs, the makers of some pediculicides recommend manual removal of the nits after treatment (Centers for Disease Control and Prevention, 2005). An extra-fine-tooth comb that is included in many commercial pediculicides or is available at community pharmacies facilitates manual removal. If the comb is ineffective in removing the nit cases, the examiner should remove them by scraping them off the strands of hair with his or her fingernails.
Live lice survive for up to 48 hours away from the host, but nits are shed into the environment and are capable of hatching in 7 to 10 days; retreatment may be required (Centers for Disease Control and Prevention, 2005). Therefore measures must be taken to prevent further infestation (see Community Focus box). Spraying with insecticide is not recommended because of the danger to children and animals. Families should also be advised that the pediculicide is relatively expensive, especially when several members of the household require treatment. Families may be inclined to try home remedies to treat the lice. A recent study by Lee, Rios, Aten, and others (2004) showed that home remedies such as petroleum jelly, oils, vinegar, butter, alcohol, and mayonnaise did little to kill louse eggs but increased the risk for skin infection with Staphylococcus aureus. Another study by Pearlman (2004) showed that dry-on pediculicide lotions may effectively treat lice without the use of current shampoos with neurotoxins, nit removal, or extensive housecleaning. Another study (Goates, Atkin, Wilding, and others, 2006) demonstrated that one 3-minute application of hot air has the potential to eliminate lice infestations.
Prevention.: The increasing incidence of pediculosis in schoolchildren is a serious concern for school nurses, parents, and community health agencies. However, school head lice screening programs have not proven to have a significant effect on the incidence of head lice in the school setting; parent education programs may be more helpful in the management of head lice. Children with head lice should be allowed to return to school after proper treatment. Both the American Academy of Pediatrics and the National Association of School Nurses discourage a “no nit” policy for schools (Frankowski and Weiner, 2002) (see Evidence-Based Practice box).
RICKETTSIAL DISEASES
The organisms responsible for a number of disorders are transmitted to human beings via arthropods (Table 30-8). Mammals become infected only through the bites of infected lice, fleas, ticks, and mites, all of which serve as both infectors and reservoirs. Rickettsiae are intracellular parasites, similar in size to bacteria that inhabit the alimentary tract of a wide range of natural hosts. Rickettsial diseases are more common in temperate and tropical climates where humans live in association with arthropods. Infection in humans is incidental (except epidemic typhus) and not necessary for the survival of the rickettsial species. However, after the organism invades a human, it causes a disease that varies in intensity from a benign, self-limiting illness to a disease that is fulminating and fatal.
LYME DISEASE
Lyme disease is the most common tick-borne disorder in the United States. It is caused by the spirochete Borrelia burgdorferi, which enters the skin and bloodstream through the saliva and feces of ticks, especially the deer tick. Most cases of Lyme disease are reported in the Northeast from southern Maine to northern Virginia. The disease may initially appear in any of three stages:
Stage 1 consists of the tick bite at the time of inoculation, followed in 3 to 31 days by the development of erythema migrans at the site of the bite (Fig. 30-10).

FIG. 30-10 Lyme disease. Note annular red rings in erythema chronicum migrans. (From Weston WL, Lane AT: Color textbook of pediatric dermatology, ed 4, St Louis, 2007, Mosby.)
Stage 2, the most serious stage of the disease, is characterized by systemic involvement of neurologic, cardiac, and musculoskeletal systems that appears several weeks after the cutaneous phase is completed.
Stage 3, or the late stage, includes musculoskeletal pain that involves the tendons, bursae, muscles, and synovia. Arthritis may occur, and late neurologic problems include deafness and chronic encephalopathy.
Diagnostic Evaluation
Diagnosis is best made clinically during the early stages by recognizing the characteristic rash, erythema migrans. Serologic testing may be used to establish the diagnosis in later stages of the disease.
Therapeutic Management
Early and appropriate treatment is essential to prevent complications. Children older than 8 years of age are treated with oral doxycycline; amoxicillin is recommended for children younger than 8 years of age (American Academy of Pediatrics, 2006). For patients allergic to penicillin, alternative drugs include cefuroxime or erythromycin (Wade, 2000). Most experts treat individuals with early Lyme disease for 14 to 21 days. Persons who have removed ticks from themselves should be monitored closely for signs and symptoms of tickborne diseases for 30 days; in particular they should be monitored for erythema migrans, a red expanding skin lesion at the site of the tick bite that may suggest Lyme disease. People who develop a skin lesion or viral infection—like illness within 1 month of an attached tick should seek prompt medical attention (Wormser, Dattwyler, Shapiro, and others, 2006). Treatment of erythema migrans most often prevents development of later stages of Lyme disease.
Nursing Care Management
The major thrust of nursing care should be educating parents to protect their children from exposure to ticks. Children should avoid tick-infested areas or wear light-colored clothing so that ticks can be spotted easily, tuck pant legs into socks, and wear a long-sleeved shirt tucked into pants when in wooded areas. Parents and children need to perform regular tick checks when they are in infested areas (with special attention to the scalp, neck, armpits, and groin areas). Parents should also be alert for signs of the skin lesion, especially if their children have been in tick-infested areas. Insect repellents containing diethyltoluamide (DEET) and permethrin can protect against ticks, but parents should use these chemicals cautiously. Although there have been reports of serious neurologic complications in children resulting from frequent and excessive application of DEET repellants, the risk is low when they are used properly. Products with DEET should be applied sparingly according to label instructions and not applied to a child’s face, hands, or any areas of irritated skin. After the child returns indoors, treated skin should be washed with soap and water. Information about Lyme disease can be obtained from the American Lyme Disease Foundation, Inc.*
PET AND WILD ANIMAL BITES
Animal bites are common in childhood. However, children are bitten more often by animals belonging to the family or to neighbors than by stray animals. The majority of victims of dog bites are boys between the ages of 5 and 9 years (Centers for Disease Control and Prevention, 2003; Bernardo, Gardner, O’Connor, and others, 2000). Most dog or cat injuries are to the upper extremities. Small children are likely to be bitten or scratched on the head, face, and neck because they tend to put their heads near the animal’s head and flail their arms rather than protecting their heads. Animal bites are potentially serious because of the likelihood of significant infection. Injuries vary in intensity from small puncture wounds to complete evulsion of tissue that is associated with significant crush injury.
Therapeutic Management
General wound care consists of rinsing the wound with copious amounts of saline or Ringer’s lactate under pressure via a large syringe and of washing the surrounding skin with mild soap. A clean pressure dressing is applied, and the extremity is elevated if the wound is bleeding. Medical evaluation is advised because of the danger of tetanus and rabies, although dogs in most urban areas must be immunized against rabies. Bites from wild animals, such as squirrels, bats, raccoons, foxes, and skunks, are also dangerous.
Prophylactic antibiotics are indicated for puncture wounds and wounds in areas that may prove to be cosmetically or functionally impaired if infected. Extensive lacerations are débrided and loosely sutured to allow drainage in the event of infection. Tetanus toxoid is administered according to standard guidelines (see Immunizations, Chapter 10), and rabies protocol is followed (see Rabies, Chapter 28). Injuries to poorly vascularized areas, such as the hands, are more likely to become infected than those in more vascularized areas, such as the face; puncture wounds are more likely to become infected than lacerations.
Nursing Care Management
The most important aspect related to animal bites is prevention. Children should understand animal behavior and develop respect for animals (see Community Focus box). Parents should monitor their children’s behavior with a dog and instruct them not to tease or surprise a dog, invade its territory, interfere with its feeding or sleeping, take its toy, or interact with a sick or injured dog or a dog with pups. Parents who are considering getting a pet, especially a dog, for themselves or their children should select a dog that has a high level of sociability with, and is unlikely to be a danger to, children.
HUMAN BITES
Children often acquire lacerations from the teeth of other humans in rough play, during fights, or as victims of child abuse. Many preschool children bite others out of frustration or anger. Because human dental plaque and gingiva harbor pathogenic organisms, all human bites should receive attention. Delayed treatment increases the risk of infection.
If the laceration is less than 6 mm (0.25 inch) in length, the wound can be treated at home. The wound is washed vigorously with soap and water, and a pressure dressing is applied to stop bleeding. Ice applications minimize discomfort and swelling. Increased pain or redness at the wound site is an indication that the child should receive medical attention for antibiotic therapy. Tetanus toxoid is needed if the child is insufficiently immunized. Wounds larger than 6 mm should receive medical attention.
CAT SCRATCH DISEASE
Cat scratch disease is the most common cause of regional lymphadenitis in children and adolescents. It usually follows the scratch or bite of an animal (a cat or kitten in 99% of cases). The disease is usually a benign, self-limiting illness that resolves spontaneously in about 2 to 4 months. Diagnosis is made on the basis of (1) history of contact with a cat or kitten, (2) the presence of regional lymphadenopathy for several days, and (3) serologic identification of the causative organism by indirect fluorescent antibody assay or polymerase chain reaction test. The disease may persist for several months before gradual resolution. In some children, especially those who are immunocompromised, the adenitis may progress to suppuration and serious complications. Treatment is primarily supportive, but antibiotic therapy may hasten the resolution of adenopathy in the disease (Centers for Disease Control and Prevention, 2002).
MISCELLANEOUS SKIN DISORDERS
A number of miscellaneous skin lesions occur in children. Some occur as a result of congenital disorders and are inherited as an autosomal dominant trait (Table 30-9). Ichthyoses are a heterogeneous group of disorders characterized by scaling that create challenging problems in treatment. These disorders are not discussed in detail here because of their wide variability.
SKIN DISORDERS ASSOCIATED WITH SPECIFIC AGE-GROUPS
Several common dermatologic conditions are confined to children in specific age-groups. These conditions include diaper, atopic, and seborrheic dermatitis, which occurs predominantly in infants, and acne, which is most common in adolescence.
DIAPER DERMATITIS
Diaper dermatitis is common in infants and one of several acute inflammatory skin disorders caused either directly or indirectly by wearing diapers. The peak age of occurrence is 9 to 12 months of age, and the incidence is greater in bottle-fed infants than in breast-fed infants.
Pathophysiology and Clinical Manifestations
Diaper dermatitis is caused by prolonged and repetitive contact with an irritant (e.g., urine, feces, soaps, detergents, ointments, friction). Although the irritant in the majority of cases is urine and feces, a combination of factors contribute to irritation.
Prolonged contact of the skin with diaper wetness produces higher friction, greater abrasion damage, increased transepidermal permeability, and increased microbial counts. Healthy skin is less resistant to potential irritants.
Although ammonia was once thought to cause diaper rash because of the association between the strong odor on diapers and dermatitis, ammonia alone is not sufficient. The irritant quality of urine is related to an increase in pH from the breakdown of urea in the presence of fecal urease. The increased pH promotes the activity of fecal enzymes, principally the proteases and lipases, which act as irritants. Fecal enzymes also increase the permeability of skin to bile salts, another potential irritant in feces.
The eruption of diaper dermatitis is manifested primarily on convex surfaces or in folds. The lesions represent a variety of types and configurations. Eruptions involving the skin in most intimate contact with the diaper (e.g., the convex surfaces of buttocks, inner thighs, mons pubis, scrotum) but sparing the folds are likely to be caused by chemical irritants, especially from urine and feces (Fig. 30-11). Other causes are detergents or soaps from inadequately rinsed cloth diapers or the chemicals in disposable wipes. Perianal involvement is usually the result of chemical irritation from feces, especially diarrheal stools. Candida albicans infection produces perianal inflammation and a maculopapular rash with satellite lesions that may cross the inguinal fold (Fig. 30-12). It is seen in up to 90% of infants with chronic diaper dermatitis and should be considered in diaper rashes that are recalcitrant to treatment.
Nursing Care Management
Nursing interventions are aimed at altering the three factors that produce dermatitis: wetness, pH, and fecal irritants. The most significant factor amenable to intervention is the moist environment created in the diaper area. Changing the diaper as soon as it becomes wet eliminates a large part of the problem, and removing the diaper to expose healthy skin to air facilitates drying. The use of a hair dryer or heat lamp is not recommended because these devices can cause burns.
Diaper construction has a significant impact on the incidence and severity of diaper dermatitis. Superabsorbent disposable paper diapers reduce diaper dermatitis. They contain an absorbent gelling material that binds water tightly to decrease skin wetness, maintains pH control by providing a buffering capacity, and decreases skin irritation by preventing mixing of urine and feces in the diaper. Another advance in diapers is the addition of an inner layer or top sheet that is impregnated with petrolatum (as in Pampers Swaddler with Absorb Away Liner).
Guidelines for controlling diaper rash are presented in the Family-Centered Care box. A common misconception about using cornstarch on skin is that it promotes the growth of C. albicans. Neither cornstarch nor talc promotes the growth of fungi under conditions normally found in the diaper area. Cornstarch is more effective in reducing friction and tends to cake less than talc when the skin is wet. On the basis of these properties and its safety in terms of inhalation injury, cornstarch is the preferred product. Talc should not be used.
ATOPIC DERMATITIS (ECZEMA)
Eczema or eczematous inflammation of the skin refers to a descriptive category of dermatologic diseases and not to a specific etiology. AD is a type of pruritic eczema that usually begins during infancy and is associated with allergy with a hereditary tendency (atopy). AD manifests in three forms based on the child’s age and the distribution of lesions:
1. Infantile (infantile eczema)—Usually begins at 2 to 6 months of age; generally undergoes spontaneous remission by 3 years of age.
2. Childhood—May follow the infantile form; occurs at 2 to3 years of age; 90% of children have manifestations by age 5 years.
3. Preadolescent and adolescent—Begins at about 12 years of age; may continue into the early adult years or indefinitely.
The diagnosis of AD is based on a combination of history and morphologic findings (Box 30-3). Children with AD have a lower threshold for cutaneous itching than do other children, and many authorities believe the dermatologic manifestations appear subsequent to scratching from the intense pruritus. For example, infants rub their faces against bed linen, and their crawling (a form of scratching) results in irritation of knees and elbows. Lesions disappear if the scratching is stopped.
The majority of children with infantile AD have a family history of eczema, asthma, food allergies, or allergic rhinitis, which strongly supports a genetic predisposition. The cause is unknown but appears to be related to abnormal function of the skin, including alterations in perspiration, peripheral vascular function, and heat tolerance. Manifestations of the chronic disease improve in humid climates and get worse in the fall and winter, when homes are heated and environmental humidity is lower. The disorder can be controlled but not cured.
Therapeutic Management
The major goals of management are to (1) hydrate the skin, (2) relieve pruritus, (3) reduce flare-ups or inflammation, and (4) prevent and control secondary infection. The general measures for managing AD focus on reducing pruritus and other aspects of the disease. Management strategies include avoiding exposure to skin irritants or allergens; avoiding overheating; and administrating medications such as antihistamines, topical immunomodulators, topical steroids, and (sometimes) mild sedatives as indicated.
Enhancing skin hydration and preventing dry, flaky skin are accomplished in a number of ways, depending on the child’s skin characteristics and individual needs. A tepid bath with a mild soap (Dove or Neutrogena), no soap, or an emulsifying oil, followed immediately by application of an emollient (within 3 minutes), assists in trapping moisture and preventing its loss. Bubble baths and harsh soaps should be avoided. The bath may need to be repeated once or twice daily, depending on the child’s status; excessive bathing without emollient application only dries out the skin. Some lotions are not effective, and emollients should be chosen carefully to prevent excessive skin drying. Aquaphor, Cetaphil, and Eucerin are acceptable lotions for skin hydration. A nighttime bath, followed by emollient application and dressing in soft cotton pajamas, may help alleviate most nighttime pruritus.
Sometimes colloid baths, such as the addition of 2 cups of cornstarch to a tub of warm water, provide temporary relief of itching and may help the child sleep if given before bedtime. Cool wet compresses are soothing to the skin and provide antiseptic protection.
Oral antihistamine drugs such as hydroxyzine or diphenhydramine usually relieve moderate or severe pruritus. Nonsedating antihistamines such as loratadine (Claritin) or fexofenadine (Allegra) may be preferred for daytime pruritus relief. Because pruritus increases at night, a mildly sedating antihistamine may be needed.
Occasional flare-ups require the use of topical steroids to diminish inflammation. Low-, moderate-, or high-potency topical corticosteroids are prescribed, depending on the degree of involvement, the area of the body to be treated, the child’s age, the potential for local side effects (striae, skin atrophy, and pigment changes), and the type of vehicle to be used (e.g., cream, lotion, ointment). Patients receiving topical corticosteroid therapy for chronic conditions should be evaluated for risk factors for suboptimal linear growth and reduced bone density (American Academy of Dermatology, 2003). Topical immunomodulators, a new nonsteroidal treatment for AD, are best used at the beginning of a “flare up” just as the skin becomes red and itches. Two new immunomodulator medications used in children with AD are tacrolimus and pimecrolimus (Kronemyer, 2003). Tacrolimus is available in two ointment strengths (0.03% and 0.1%); the 0.03% concentration has been approved for use in children 2 years of age and older. Tacrolimus is recommended for intermittent therapy in patients who are not adequately responsive to, or are intolerant of, conventional therapy (Yetman and Parks, 2002). Pimecrolimus is available in a 1% cream that has no systemic accumulation or effects. This drug is approved for use in children with mild to moderate AD. Both drugs can be used freely on the face without worrying about steroid side effects.
If secondary skin infections occur in children with AD, these infections are managed with appropriate systemic antibiotics.
Nursing Care Management
Assessment of the child with AD includes a family history for evidence of atopy, a history of previous involvement, and any environmental or dietary factors associated with the present and previous exacerbations. The skin lesions are examined for type, distribution, and evidence of secondary infection. Parents are interviewed regarding the child’s behavior, especially in relation to scratching, irritability, and sleeping patterns. Exploration of the family’s feelings and methods of coping is also important.
The nursing care of the child with AD is challenging. Controlling the intense pruritus is imperative if the disorder is to be successfully managed, since scratching leads to new lesions and may cause secondary infection. In addition to the medical regimen, other measures can be taken to prevent or minimize the scratching. Fingernails and toenails are cut short, kept clean, and filed frequently to prevent sharp edges. Gloves or cotton stockings can be placed over the hands and pinned to shirtsleeves. One-piece outfits with long sleeves and long pants also decrease direct contact with the skin. If gloves or socks are used, the child needs time to be free from such restrictions. An excellent time to remove gloves, socks, or other protective devices is during the bath or after receiving sedative or antipruritic medication.
Conditions that increase itching are eliminated when possible. Woolen clothes or blankets, rough fabrics, and furry stuffed animals are removed from the child’s environment. Because heat and humidity cause perspiration (which intensifies itching), proper dress for climatic conditions is essential. Pruritus is often precipitated by exposure to the irritant effects of certain components of common products such as soaps, detergents, fabric softeners, perfumes, and powders. Most children experience less itching when soft cotton fabrics are worn next to the skin. During cold months, synthetic fabrics (not wool) should be used for overcoats, hats, gloves, and snowsuits. Exposure to latex products, such as gloves and balloons, should also be avoided.
Clothes and sheets are laundered in a mild detergent and rinsed thoroughly in clear water (without fabric softeners or antistatic chemicals). Putting the clothes through a second complete wash cycle without using detergent reduces the amount of residue remaining in the fabric.
Preventing infection is usually accomplished by preventing scratching. Baths are given as prescribed, the water is kept tepid, and soaps (except as indicated) and bubble baths are avoided, as are oils or powders. Skinfolds and diaper areas need frequent cleansing with plain water. A room humidifier or vaporizer may benefit children with extremely dry skin. The skin lesions are examined for signs of infection—usually honey-colored crusts or pustules with surrounding erythema. Any signs of infection are reported to the practitioner.
Wet soaks and compresses are applied and medications for pruritus or infection are administered as directed. The family is given explicit instructions on the preparation and use of soaks, special baths, and topical medications, including the order of application if more than one is prescribed. It is important to emphasize that one thick application of topical medication is not equivalent to several thin applications, and that excessive use of an agent (particularly steroids) can be hazardous. If children have difficulty remaining still for a 10- or 15-minute soak, bath, or dressing application, these can be carried out at naptime or when the child is engrossed in watching television, listening to a story, or playing with tub toys.
Diet modification is another source of frustration to parents. When a hypoallergenic diet is prescribed, parents need help to understand the reason for the diet and the guidelines for avoiding hyperallergenic foods (see Nursing Care Guidelines box). Because hypoallergenic diets take time before visible effects are apparent, parents need reassurance that results may not be seen immediately. If airborne allergens make eczema worse, the family is counseled about “allergy proofing” the home (see Asthma, Chapter 23).
Family Support.: Parents are assured that the lesions will not produce scarring (unless secondarily infected) and that the disease is not contagious. However, the child may have repeated exacerbations and remissions. Spontaneous and permanent remission takes place at approximately 2 to 3 years of age in most children with the infantile disorder.
During acute phases, emotional stress can become intense for the family. They need time to discuss negative feelings and to be reassured that these feelings are normal. Stress tends to aggravate the severity of the condition. Therefore efforts to relieve as much anxiety as possible in both the parents and the child have a beneficial emotional and physical effect.
SEBORRHEIC DERMATITIS
Seborrheic dermatitis is a chronic, recurrent, inflammatory reaction of the skin. It occurs most commonly on the scalp (cradle cap) but may involve the eyelids (blepharitis), external ear canal (otitis externa), nasolabial folds, and inguinal region. The cause is unknown, although it is more common in early infancy, when sebum production is increased. The lesions are characteristically thick, adherent, yellowish, scaly, oily patches that may or may not be mildly pruritic. Unlike AD, seborrheic dermatitis is not associated with a positive family history for allergy and is common in infants shortly after birth and in adolescents after puberty. Diagnosis is made primarily on the basis of the appearance and the location of the crusts or scales.
Nursing Care Management
Cradle cap may be prevented with adequate scalp hygiene. Not infrequently, parents omit shampooing the infant’s hair for fear of damaging the “soft spots,” or fontanels. The nurse should discuss how to shampoo the infant’s hair and emphasize that the fontanel is like skin anywhere else on the body—it does not puncture or tear with mild pressure.
When seborrheic lesions are present, the treatment is directed at removing the crusts. Parents are taught the appropriate procedure to clean the scalp. Education may need to include a demonstration. Shampooing should be done daily with a mild soap or commercial baby shampoo; medicated shampoos are not necessary, but an antiseborrheic shampoo containing sulfur and salicylic acid may be used. Shampoo is applied to the scalp and allowed to remain on the scalp until the crusts soften. Then the scalp is thoroughly rinsed. A fine-tooth comb or a soft facial brush helps remove the loosened crusts from the strands of hair after shampooing.
ACNE
Acne vulgaris is the most common skin problem treated by physicians during patients’ adolescence. Acne is not caused by dirt but by testosterone, a hormone present in males and females that increases during puberty. It stimulates the sebaceous glands of the skin to enlarge, or produce oil, and plug the pores. Whiteheads, blackheads, and pimples are present in teenage acne (American Academy of Dermatology, 2006).
One half of the adolescent population experiences acne by the end of the teenage years. Although the disorder can appear before the age of 10 years, the peak incidence occurs in middle to late adolescence (at age 16 to 17 years in girls and 17 to 18 years in boys). It is more common in boys than in girls. The degree to which an individual is affected may range from nothing more than a few isolated comedones to a severe inflammatory reaction. Although the disease is self-limiting and not life threatening, it has great significance to the adolescent. Health professionals should not underestimate the impact that acne has on teens.
Numerous factors affect the development and course of acne. Its distribution in families and a high degree of concordance in identical twins suggest hereditary factors. Premenstrual flares of acne occur in nearly 70% of adolescent girls, suggesting a hormonal cause. Studies do not indicate a clear association between stress and acne, but adolescents commonly cite stress as a cause for acne outbreaks. Cosmetics containing lanolin, petrolatum, vegetable oils, lauryl alcohol, butyl stearate, and oleic acid can increase comedone production. Exposure to oils in cooking grease can be a precursor in adolescents who work over fast-food restaurant hot oils. There is no known link between dietary intake and the development or worsening of acne.
Pathophysiology
Acne is a disease that involves the pilosebaceous follicles (the hair follicle and sebaceous gland complex) of the face, neck, chest, and upper back. Three pathophysiologic factors are involved in the development of acne: excessive sebum production, comedogenesis, and the overgrowth of Propionibacterium acnes (Mancini, 2000).
Comedogenesis (formation of comedones) results in a noninflammatory lesion that may be either an open comedone (“blackhead”) or a closed comedone (“whitehead”). Inflammation occurs with the proliferation of P. acnes, which draws in neutrophils, causing inflammatory papules, pustules, nodules, and cysts (Fig. 30-14).
Therapeutic Management
Successful management of acne depends on a cooperative effort between the health care provider, the adolescent, and the parents. Unlike many other dermatologic conditions, acne lesions resolve slowly, and improvement may not be apparent for at least 6 weeks. Individual comedones can take several weeks to months to resolve, and papules and pustules usually resolve in about 1 week. The multifactorial causes of acne necessitate a combined approach for successful treatment. Treatment consists of general measures of care and specific treatments determined by the type of lesions involved.
General Measures.: Improvement of the adolescent’s overall health status is part of the general management. Adequate rest, moderate exercise, a well-balanced diet, reduction of emotional stress, and elimination of any foci of infection are all part of general health promotion.
Cleansing.: Dirt or oil on the surface of the skin does not cause acne. Gentle cleansing with a mild cleanser once or twice daily is usually sufficient. Antibacterial soaps are ineffective and may be too drying when used in combination with topical acne medications. For some adolescents hygiene of the hair and scalp appears to be related to the clinical activity of the acne. Acne on the forehead may improve with brushing the hair away from the forehead and more frequent shampooing.
Medications.: Treatment success depends on commitment from the adolescent. Before prescribing treatment, the practitioner should determine the adolescent’s level of comfort and readiness to begin treatment.
Tretinoin (Retin-A) is the only drug that effectively interrupts the abnormal follicular keratinization that produces microcomedones, the invisible precursors of the visible comedones. Tretinoin alone is usually sufficient for management of comedonal acne (Russell, 2000). Tretinoin is available as a cream, gel, or liquid. This drug can be extremely irritating to the skin and requires careful patient education for optimal usage. The patient should be instructed to begin with a pea-sized dot of medication, which is divided into the three main areas of the face and then gently rubbed into each area. The medication should not be applied for at least 20 to 30 minutes after washing to decrease the burning sensation. The avoidance of sun and the daily use of sunscreen must be emphasized, since sun exposure can result in severe sunburn. Adolescents should be advised to apply the medication at night and to use a sunscreen with a sun protection factor (SPF) of at least 15 in the daytime.
Topical benzoyl peroxide is an antibacterial agent that inhibits the growth of P. acnes organisms. It is effective against both inflammatory and noninflammatory acne and is an effective first-line agent. This medication is available as a cream, lotion, gel, or wash. The patient should be informed that the medication may have a bleaching effect on sheets, bedclothes, and towels. The adolescent can be reassured that skin bleaching will not occur. Accommodation to the medication can be gained with a gradual increase in the strength and frequency of application.
When inflammatory lesions accompany the comedones, a topical antibacterial agent may be prescribed. These agents are used to prevent new lesions and to treat preexisting acne. Clindamycin, erythromycin, metronidazole, azelaic acid, and the combination of either benzoyl peroxide and erythromycin (Benzamycin) or benzoyl peroxide and glycolic acid are all choices for topical antibacterial therapy. The combination of 5% benzoyl peroxide and 3% erythromycin is especially beneficial, although the exact mechanism of action is not understood (Burkhart, Specht, and Neckers, 2000). Tretinoin improves the penetration of other topical agents, and combination therapy with tretinoin and an antibacterial treatment is the only way to address three of the pathogenic causes of acne: keratinization, P. acnes, and inflammation (Laude, 2000).
Systemic antibiotic therapy is used when moderate to severe acne does not respond to topical treatments. Oral antibiotics such as tetracycline, erythromycin, minocycline, and doxycycline are considered safe to use (American Academy of Dermatology, 2006).
Females with mild to moderate acne may respond well to topical treatment and the addition of an oral contraceptive pill (OCP). OCPs reduce the endogenous androgen production and decrease the bioavailability of the woman’s circulating androgens. Both of these actions result in decreased acne.
Isotretinoin, 13-cis-retinoic acid (Accutane), is a potent and effective oral agent that is reserved for severe cystic acne that has not responded to other treatments. Isotretinoin is the only agent available that affects factors involved in the development of acne. However, treatment with isotretinoin should be managed only by a dermatologist. Adolescents with multiple, active, deep dermal or subcutaneous cystic and nodular acne lesions are treated for 20 weeks. Multiple side effects can occur, including dry skin and mucous membranes, nasal irritation, dry eyes, decreased night vision, photosensitivity, arthralgia, headaches, mood changes, aggressive or violent behaviors, depression, and suicidal ideation. Adolescents on this drug should be monitored for depression, depressive symptoms, and suicidal ideation (Jacobs, Deutsch, and Brewer, 2001). The drug should be given only at the recommended doses for no longer than the recommended duration. The most significant side effects of this drug are the teratogenic effects. Isotretinoin is absolutely contraindicated in pregnant women. Sexually active young women must be using an effective contraceptive method during treatment and for 1 month after treatment. Patients receiving isotretinoin should also be monitored for elevated cholesterol and triglyceride levels. Significant elevation may require discontinuation of the medication.
Nursing Care Management
Because acne is so common and its appearance may seem so mild, the health care provider may underestimate the relative importance of the disease to the adolescent. The nurse should assess the individual adolescent’s level of distress, current management, and perceived success of any regimen before initiating a referral. If adolescents do not perceive the acne to be a problem, they may lack motivation to follow the treatment plan.
The nurse can provide ongoing support for the adolescent when a treatment plan is initiated. The family is also encouraged to support the adolescent in his or her efforts. Use of medications and basic skin care information should be discussed in detail with the adolescent. Written instructions should accompany the verbal discussion. Information to dispel myths regarding the use of abrasive cleansing products can prevent unnecessary costs and trauma to the skin.
Teenagers need education about the factors that aggravate and damage the skin, such as too vigorous scrubbing. In addition, picking, squeezing, and manual expression with fingernails break down the ductal walls of lesions and cause the acne to worsen. Mechanical irritation, such as vinyl helmet straps that rub areas predisposed to acne, can also cause the development of lesions.
THERMAL INJURY
Burn injuries are usually attributed to extreme heat sources but may also result from exposure to cold, chemicals, electricity, or radiation. Most burns are relatively minor and do not require definitive medical treatment. However, burns involving a large body surface area, critical body parts, or the geriatric or pediatric population often benefit from treatment in specialized burn centers. The American Burn Association has established criteria to guide decisions regarding the severity of injury and the need for transfer for specialized care.* Burn prevention is also discussed in Chapters 10, 12, 15, and 16.
When burns are characterized by patients’ age and type of injury, the following patterns become apparent: (1) hot-water scalds are most frequent in toddlers, (2) flame-related burns are more common in older children, (3) 10% to 20% of documented cases of child abuse include burn injuries (Herndon, 2007), and (4) children playing with matches or lighters account for 1 in 10 house fires.
The extent of tissue destruction is determined by the intensity of the heat source, the duration of contact or exposure, the conductivity of the tissue involved, and the rate at which the heat energy is dissipated by the skin. A brief exposure to high-intensity heat from a flame can produce burn injuries similar to those induced by long exposure to less intense heat in hot water.
Characteristics of Burn Injury
The physiologic responses, therapy, prognosis, and disposition of the injured child are all directly related to the amount of tissue destroyed. Therefore the severity of the burn injury is assessed on the basis of the percentage of total body surface area (TBSA) burned and depth of the burn. Among children in the school age—group or younger age-groups, a burn that is 10% TBSA can be life threatening if not treated correctly. Other important factors in determining the seriousness of the injury are the location of the wounds, the child’s age and general health, the causative agent, the presence of respiratory involvement, and any associated injury or condition.
Type of Injury.: The majority of burns result from contact with thermal agents such as a flame, hot surfaces, or hot liquids. Electrical injuries caused by household current have the greatest incidence in young children, who insert conductive objects into electrical outlets and bite or suck on connected electrical cords (Herndon, 2007). These burns occur most commonly during the spring and summer months and are also associated with risk-taking behaviors in boys. Direct contact with high- or low-voltage current, as well as lightning strikes, is the most frequent mechanism of injury. The resistance of the tissue and the path of the electric current are responsible for the damage incurred. Electric current travels through the body following the path of least resistance, which involves the tissues, fluid, blood vessels, and nerves. A more localized burn is produced if skin resistance is high at the area of contact, and a more systemic pattern of injury is produced if skin resistance is low. Often compared with a crush injury, serious electrical trauma results from current passing through vital organs, muscle compartments, and nerve or vascular pathways. Loss of limbs, cardiac fibrillation, respiratory collapse, and burns are common occurrences after exposure to electrical energy. Criteria for admission, as derived from evidence-based practice for electrical burn injuries, includes a history of loss of consciousness, electrocardiographic (ECG) changes, 10% TBSA affected, or the need for monitoring an affected extremity. Cardiac monitoring is therefore included in standard burn care when ECG changes are identified on admission (Arnoldo, Klein, and Gibran, 2006).
Chemical burns are seen in the pediatric population and can cause extensive injury. The severity of injury is related to the chemical agent (acid, alkali, or organic compound) and the duration of contact. The mechanism of injury differs from that in other burns in that there is a chemical disruption and alteration of the physical properties of the exposed body area. Noxious agents exist in many cleaning products commonly found in the home. In addition to concern for localized damage, the potential for systemic toxicity must be addressed. Of particular concern is the exposure of the eyes to chemical agents, the ingestion of caustic substances, and inhalation of toxic gases produced from chemicals.
Extent of Injury.: The extent of a burn is expressed as a percentage of the TBSA. This is most accurately estimated by using specially designed age-related charts (Fig. 30-15). It is more efficient to use a chart designed to assign body proportions to children of different ages.
Depth of Injury.: A thermal injury is a three-dimensional wound that is also assessed in relation to depth of injury. Traditionally the terms first-, second-, and third-degree have been used to describe the depth of tissue injury. However, with the current emphasis on wound healing, these have been replaced by more descriptive terms based on the extent of destruction to the epithelializing elements of the skin (Fig. 30-16).
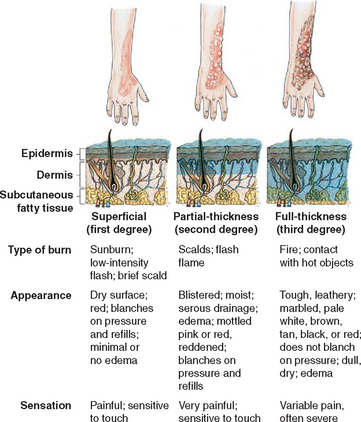
FIG. 30-16 Classification of burn depth. (Redrawn from Grant HD, Murray RH: Emergency care, ed 7, Upper Saddle River, NJ, 1995, Prentice-Hall.) Prentice-Hall
Superficial (first-degree) burns are usually of minor significance. With these burns, there is often a latent period followed by erythema. Tissue damage is minimal, the protective functions of the skin remain intact, and systemic effects are rare. Pain is the predominant symptom, and the burn heals in 5 to 10 days without scarring. Mild sunburn is an example of a superficial burn.
Partial-thickness (second-degree) injuries involve the epidermis and varying degrees of the dermis. These wounds are painful, moist, red, and blistered. Superficial partial-thickness burns involve the epidermis and part of the dermis. Dermal elements are intact, and the wound should heal in approximately 14 days with variable amounts of scarring (Fig. 30-17). The wound is extremely sensitive to temperature changes, exposure to air, and light touch. Although classified as second-degree or partial-thickness burns, deep dermal burns resemble full-thickness injuries in many respects. Sweat glands and hair follicles remain intact. The burn may appear mottled, with pink, red, or waxy white areas exhibiting blisters and edema formation. Systemic effects are similar to those encountered with full-thickness burns. Although many of these wounds heal spontaneously, healing time may be extended beyond 14 days. These burn wounds often heal with extensive scarring.
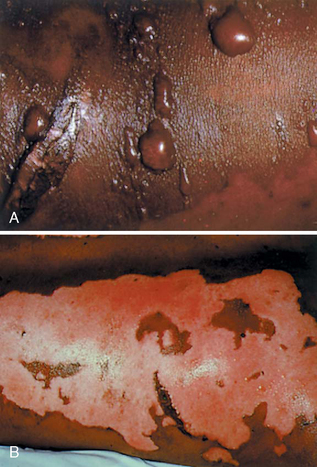
FIG. 30-17 Superficial partial-thickness burns on an African-American child. A, Blisters intact. B, Blisters removed. (Courtesy Hillcrest Medical Center, Tulsa, Oklahoma.)
Full-thickness (third-degree) burns are serious injuries that involve the entire epidermis and dermis and extend into subcutaneous tissue (see Fig. 30-16). Nerve endings, sweat glands, and hair follicles are destroyed. The burn varies in color from red to tan, waxy white, brown, or black and is distinguished by a dry, leathery appearance (Fig. 30-18). Normally, full-thickness burns lack sensation in the area of injury because of the destruction of nerve endings. However, most full-thickness burns have superficial and partial-thickness burned areas at the periphery of the burn, where nerve endings are intact and exposed. Excised eschar and donor sites also cause exposed nerve fibers. As the peripheral fibers regenerate, painful sensations return. Consequently, children often experience severe pain related to the size and depth of the burn. Full-thickness wounds are not capable of reepithelialization and require surgical excision and grafting to close the wound.

FIG. 30-18 Bottom to top: Deep partial-thickness burn (red area); full-thickness burn (white area); full-thickness burn with eschar (brown area). (Courtesy Hillcrest Medical Center, Tulsa, Oklahoma.)
Fourth-degree burns are full-thickness injuries that involve underlying structures such as muscle, fascia, and bone. The wound appears dull and dry, and ligaments, tendons, and bone may be exposed (Fig. 30-19).
Severity of Injury.: Burns are classified as minor, moderate, or major, which is useful in determining the disposition of the patient for treatment. Burn patients are categorized as (1) those with a major burn injury, who require the services and facilities of a specialized burn center; (2) those with a moderate burn, who may be treated in a hospital with expertise in burn care; and (3) those with minor injuries, who may be treated on an outpatient basis. The extent and depth of the burn (Table 30-10), the causative agent, the body area involved, the patient’s age, and concomitant injuries and illnesses determine the severity of the injury.
TABLE 30-10
Severity Grading System Adopted by the American Burn Association
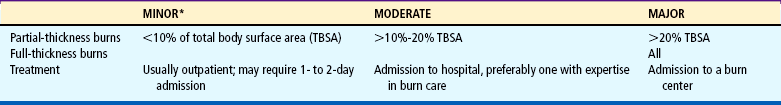
*Minor burns exclude any burn involving the face, hands, feet, perineum, or crossing joints; electrical burns; any injury complicated by the presence of inhalation injury or concomitant trauma; children with psychosocial factors affecting the injury.
From Vaccaro P, Trofino RB: Care of the patient with minor to moderate burns. In Trofino RB, editor: Nursing care of the burn-injured patient, Philadelphia, 1991, Davis.
Because the skin of infants is so thin, it is likely to sustain deeper injuries compared with older children. Children younger than 2 years of age, especially 6 months or younger, have a significantly higher mortality rate than older children with burns of similar magnitude. Acute or chronic illnesses or superimposed injuries also complicate burn care and response to treatment.
Inhalation Injury.: Trauma to the tracheobronchial tree often follows inhalation of the heated gases and toxic chemicals produced during combustion. Although direct thermal injury to the upper airway may occur, heat damage below the vocal cords is rare. Inspired heated air is cooled in the upper airway before reaching the trachea. Reflex closure of the cords and laryngospasm also prevent full inhalation. However, evidence of direct thermal injury to the upper airway includes burns of the face and lips, singed nasal hairs, and laryngeal edema. Clinical manifestations may be delayed as long as 24 to 48 hours. Wheezing, increasing secretions, hoarseness, wet rales, and carbonaceous secretions are signs of respiratory tract involvement. Upper airway obstruction is often associated with burn shock and fluid resuscitation. In such situations, endotracheal intubation may also be necessary to preserve a patent airway.
Inhalation of carbon monoxide is suspected when the injury has occurred in an enclosed space. Mucosal erythema and edema followed by sloughing of the mucosa are manifestations of respiratory tract injury. A mucopurulent membrane replaces the mucosal lining and seriously compromises respiration and ventilation.
Early in the postburn period most pulmonary infections result from nosocomial exposure, immobility, and abdominal distention. The hematogenous variety occurs later and is related to the septic burn wound or other foci, such as phlebitis at the site of an invasive IV line. A significant increase in mortality has been observed when inhalation injury and pneumonia are both present.
Deep burns, especially those circling the thorax, may cause restriction of chest excursion as a result of edema and inelastic eschar formation. Young children are particularly at risk because of the pliability of the skeletal structure. Restriction of the chest is relieved by an escharotomy incision, which allows expansion of the chest wall to facilitate ventilation.
Pathophysiology
Thermal injuries produce both local and systemic effects that are related to the extent of tissue destruction. In superficial burns the tissue damage is minimal. In partial-thickness burns there is considerable edema and more severe capillary damage. With a major burn greater than 30% TBSA, there is a systemic response involving an increase in capillary permeability, allowing plasma proteins, fluids, and electrolytes to be lost. Maximum edema formation in a small wound occurs about 8 to 12 hours after injury. After a larger injury, hypovolemia, associated with this phenomenon, will slow the rate of edema formation, with maximum effect at 18 to 24 hours.
Another systemic response is anemia, caused by direct heat destruction of red blood cells, hemolysis of injured red blood cells, and trapping of red blood cells in the microvascular thrombi of damaged cells. A long-term decrease in the number of red blood cells may occur as a result of increased red blood cell fragility. Initially there is an increased blood flow to the heart, brain, and kidneys, with decreased blood flow to the gastrointestinal tract. There is an increase in metabolism to maintain body heat, providing for the increased energy needs of the body.
Complications.: Thermally injured children are subject to a number of serious complications, both from the wound and from systemic alterations resulting from the injury. The immediate threat to life is related to airway compromise and profound shock. During healing, infection—both local and systemic sepsis—is the primary complication. Mortality associated with thermal trauma in children increases with the severity of injury and decreases as age advances. In children older than 3 years, the mortality rate is similar to that of adults. Below this age, the survival rate with burns and their associated complications lessens considerably.
A less apparent respiratory tract injury is inhalation of carbon monoxide. Carbon monoxide has a greater affinity for hemoglobin than does oxygen, thereby depriving peripheral tissues and oxygen-dependent organs (such as the heart and brain) of the oxygen needed for survival. Treatment for either of these two problems is 100% oxygen, which reverses the situation rapidly.
Pulmonary problems are a major cause of fatality in children with either thermal burns or complications in the respiratory tract. Respiratory problems include inhalation injuries, aspiration in unconscious patients, bacterial pneumonia, pulmonary edema, pulmonary embolus, posttraumatic pulmonary insufficiency, and atelectasis. The most common cause of respiratory failure in the pediatric age-group is bacterial pneumonia, which requires prolonged intubation and sometimes a tracheostomy. Tracheostomies increase the incidence of serious complications and are performed only in extreme cases.
A less common complication is pulmonary edema resulting from fluid overload or acute respiratory distress syndrome (ARDS) in association with gram-negative sepsis. ARDS results from pulmonary capillary damage and leakage of fluid into the interstitial spaces of the lung. A loss of compliance and interference with oxygenation are the consequences of pulmonary insufficiency in conjunction with systemic sepsis.
Wound Sepsis.: Sepsis is a critical problem in the treatment of burns and an ever-present threat following the shock phase. Initially, burn wounds are relatively pathogen free unless they are contaminated with potentially infectious material, such as dirt or polluted water. However, dead tissue and exudate provide a fertile field for bacterial growth. On approximately the third postburn day, early colonization of the wound surface by a preponderance of gram-positive organisms (primarily staphylococci) changes to predominantly gram-negative opportunistic organisms, particularly Pseudomonas aeruginosa. By the fifth postburn day, bacterial invasion is well under way beneath the surface of the burn wound. Early surgical excision of eschar together with placement of autograft reduces the incidence of sepsis.
Therapeutic Management
Emergency Care.: The initial management of the burn patient begins at the scene of injury. The first priority is to stop the burning process (see Emergency Treatment box). The child should then be transported immediately to the nearest medical facility for treatment and evaluation. The child and the family are usually extremely frightened and anxious; sensitivity to their emotional state and reassurance should be provided during the transport process.
Stop the Burning Process.: The chief aim of rescue in flame burns is to smother the fire, not fan it. Children tend to panic and run, which spreads the flames and makes assistance more difficult. The injured child should be placed in a horizontal position and rolled in a blanket, rug, or similar article, with care taken not to cover the head and face because of the danger of inhalation of toxic fumes. If nothing is available, the victim should lie down and roll over slowly to extinguish the flames. Remaining in the vertical position may cause the hair to ignite or the inhalation of flames, heat, or smoke.
Major burns with large amounts of denuded skin should not be cooled. Heat is rapidly lost from burned areas, and additional cooling leads to a drop in core body temperature and potential circulatory collapse. Wet dressings also promote vasoconstriction because of cooling, resulting in impaired circulation to the burned area and increased tissue damage. Chemical burns require continuous flushing with large amounts of water before transport to a medical facility. The use of neutralizing agents on the skin is contraindicated, since a chemical reaction is initiated and further injury may result. If the chemical is in powder form, the addition of water may spread the caustic agent. The powder should be brushed off if possible.
Burned clothing is removed to prevent further damage from smoldering fabric and hot beads of melted synthetic materials. Jewelry is removed to eliminate the transfer of heat from the metal and constriction resulting from edema formation. This also provides access to the wound and prevents painful removal later.
Assess the Victim’s Condition.: As soon as the flames are extinguished, the child is assessed. Airway, breathing, and circulation are the primary concerns. Cardiopulmonary complications may result from exposure to electric current, inhalation of toxic fumes and smoke, hypovolemia, and shock. Emergency measures are instituted as appropriate.
Cover the Burn.: The burn wound should be covered with a clean cloth to prevent contamination, decrease pain by eliminating air contact, and prevent hypothermia. No attempt should be made to treat the burn. Application of topical ointments, oils, or other home remedies is contraindicated.
Transport the Child to Medical Aid.: The child with an extensive burn is not given anything by mouth to avoid aspiration in the presence of paralytic ileus and upper airway edema and to prevent water intoxication. The child is transported to the nearest medical facility. If this cannot be accomplished within a relatively short period, IV access should be established, if possible, with a large-bore catheter. Oxygen is administered, if available, at 100%. A report of the initial assessment and any interventions implemented is given to the medical facility assuming care of the child.
Minor Burns.: Treatment of burns classified as minor can usually be managed adequately on an outpatient basis when it is determined that the parent can be relied on to carry out instructions for care and observation. Patients with less than optimum circumstances may require close follow-up to ensure adherence with treatment.
The wound is cleansed with a mild soap and tepid water. Débridement of the wound includes removal of any embedded debris, chemicals, and devitalized tissue. Removal of intact blisters remains controversial. Some authorities argue that blisters provide a barrier against infection; others maintain that blister fluid is an effective medium for the growth of microorganisms. However, blisters should be broken if the injury is due to a chemical agent to control absorption. Most practitioners favor covering the wound with an antimicrobial ointment to reduce the risk of infection and to provide some form of pain relief. The dressing consists of nonadherent fine-mesh gauze placed over the ointment and a light wrap of gauze dressing that avoids interference with movement. This helps keep the wound clean and protect it from trauma. The caregiver is instructed to wash the wound, reapply the dressing, and return the child to the office or clinic as directed for wound observation. The frequency of dressing changes may vary from every other day to once a day.
Some practitioners prefer an occlusive dressing, such as a hydrocolloid, which is placed over the wound after cleansing. Hydrogel dressings, which are soothing and nonadherent, may also be used. The dressing is changed when leakage occurs—at regular intervals or at least weekly. This method eliminates the discomfort associated with frequent dressing changes but impairs visualization of the wound surface.
If there is a high probability of infection or other complications or if there is doubt about the ability to carry out instructions, the caregiver may be directed to bring the patient in daily for dressing changes and inspection. Another option is have a nurse make a home visit to inspect the wound and perform the dressing change. Frequent removal of the dressing is an effective mode of débridement. Soaking the dressing in tepid water or normal saline before removal helps loosen the dressing and debris and reduce discomfort. Burns of the face are usually treated by an open method. The wound is washed and débrided in the same manner, and a thin film of antimicrobial ointment is applied.
A tetanus history is obtained on admission. If there is no history of immunization, or if more than 5 years have passed since the last immunization, tetanus prophylaxis is administered. There is no evidence that systemic antibiotic prophylaxis decreases the incidence of infection in small burn wounds (Herndon, 2007). Therefore antibiotics should be used only when there is evidence of infection. A mild analgesic such as acetaminophen is usually sufficient to relieve discomfort; the antipyretic effect of the drug also alleviates the sensation of heat.
Most minor burns heal without difficulty, but if the wound margin becomes erythematous, gross purulence is noted, or the child develops evidence of systemic reaction, such as fever or tachycardia, hospitalization is indicated. The child should also be evaluated for functional impairment, and the caregiver should be instructed in the exercise and ambulation program. After wound healing, an evaluation of scar maturation and range of motion will indicate any need for further therapy.
Major Burns.: The first priority is airway maintenance. The inhalation of noxious agents or respiratory burns is suggested when there is a history of injury in an enclosed space; edema of the oral and nasal membranes; thermal injury to the face, nares, and upper torso; hyperemia; and blisters or evidence of trauma to the upper respiratory passages. When respiratory involvement is suspected or evident, 100% oxygen is administered and blood gas values, including carbon monoxide levels, are determined.
If the child exhibits changes in sensorium, air hunger, or other signs of respiratory distress, an endotracheal tube is inserted to maintain the airway. When severe edema of the face and neck is anticipated, intubation is performed before swelling makes intubation difficult or impossible. Controlled intubation is preferred to an emergency procedure. Intubation allows for the delivery of humidified oxygen, the removal of secretions from respiratory passages, and the provision of ventilatory support.
When full-thickness burns encircle the chest, constricting eschar may limit chest wall excursion, and ventilation of the child becomes more difficult. Escharotomy of the chest relieves this constriction and improves ventilation.
Fluid Replacement Therapy.: The objectives of fluid therapy are to (1) compensate for water and sodium lost to traumatized areas and interstitial spaces, (2) reestablish sodium balance, (3) restore circulating volume, (4) provide adequate perfusion, (5) correct acidosis, and (6) improve renal function.
Fluid replacement is required during the first 24 hours because of fluid shifts that occur after the injury. Various formulas are used to calculate fluid needs, and the one adopted depends on practitioner preference. Crystalloid solutions are used during this initial phase of therapy. Parameters such as vital signs (especially heart rate), urinary output volume, adequacy of capillary filling, and state of sensorium determine adequacy of fluid resuscitation.
After the initial 24-hour period, theoretically there is a capillary seal, and capillary permeability is restored. Colloid solutions such as albumin, Plasma-Lyte, or fresh frozen plasma are useful in maintaining plasma volume. However, children with burn injuries usually require fluids in excess of their calculated maintenance and replacement volume. Reasons for this may include underestimation of burn size (particularly in pediatric patients), pulmonary injury that sequesters resuscitation fluid in the lung, electrical injury with greater tissue destruction than that which is visible, and a delay in the initiation of fluid resuscitation. Irreversible burn shock that persists despite aggressive fluid resuscitation remains a significant cause of death in the immediate postburn period. Fluid balance may continue to be a problem throughout the course of treatment, especially during periods in which there may be considerable evaporative loss from the wound.
Nutrition.: The enhanced metabolic requirements and catabolism in severe burns make nutritional needs of paramount importance and often difficult to satisfy. The diet must provide sufficient calories to meet the increased metabolic needs and enough protein to avoid protein breakdown. Hypoglycemia can result from the stress of the burn injury because the liver glycogen stores are rapidly depleted.
A high-protein, high-calorie diet is encouraged. Many children have poor appetites and are unable to meet energy requirements solely by oral feeding. Most children with burns in excess of 25% TBSA require supplementation with tube feeding. Early and continued nutritional support is an important part of therapy for seriously burned patients. Enteral feeding provides direct nourishment to the gastrointestinal tract and helps reverse the defective gut barrier that accompanies burn shock (Purdue, 2007).
If nutritional requirements cannot be met entirely by the enteral route, parenteral hyperalimentation is used to supplement intake. However, enteral feeding increases blood flow in the intestinal tract, preserves gastrointestinal function, and minimizes bacterial translocation by decreasing mucosal atrophy of the intestines. These factors make enteral feeding the preferred route of nutritional support (Herndon, 2007).
To facilitate growth and proliferation of epithelial cells, administration of vitamins A and C is begun early in the postburn period. Zinc is also supplemented because of its important role in wound healing and epithelialization.
Medication.: Antibiotics are usually not administered prophylactically. The administration of systemic antibiotics to control wound colonization is not indicated, since decreased circulation to the injured area prevents delivery of the medication to areas of deepest injury. Surveillance cultures and monitoring of the clinical course provide the most reliable indicators of developing infection. Appropriate antibiotics are instituted to treat the specific identified organism. Otitis media should not be overlooked as a source of fever in the pediatric population.
Some form of sedation and analgesia is required in the care of burned children. Morphine sulfate is the drug of choice for severe burn injuries. Morphine has extensive distribution but is metabolized rapidly; continuous infusion or frequent administration is needed for pain management in burns. Morphine is administered intravenously and titrated to individual need. The unstable circulatory status and edema formation preclude intramuscular or subcutaneous administration. When combined, midazolam (Versed) and fentanyl (Sublimaze) also provide excellent IV sedation and analgesia to control procedural pain in children with burns (Herndon, 2007). The oral form of fentanyl, Oralet, provides effective analgesia in a convenient form that the child can suck. Dosage monitoring is important because tolerance to opioids may develop. IV analgesics are most effective when they are administered just before the onset of procedural pain.
The use of short-acting anesthetic agents, such as propofol (Diprivan) and nitrous oxide, has proved beneficial in eliminating procedural pain. Pharyngeal reflexes remain intact, thus ensuring a patent airway. Propofol is an IV sedative hypnotic agent that produces sedation in less than 1 minute and lasts only a few minutes. Nitrous oxide is a useful short-term analgesic when given in a mixture of gases on a fixed ratio of 50% nitrous oxide and 50% oxygen (Annequin, Carbajal, Chauvin, and others, 2000). Initiation of action is approximately 1 minute, with peak effect reached in 3 to 5 minutes. Nitrous oxide is useful to alleviate anxiety and raise the threshold of pain during procedures. The child may self-administer the nitrous oxide mixture with assistance. For any conscious or unconscious sedation, the child must be monitored continuously during the procedure (see Preoperative Care, Chapter 22; and Pain Assessment and Pain Management, Chapter 7).
Management of the Burn Wound.: After the initial period of shock and the restoration of fluid balance, the primary concern is the burn wound. The objectives of wound management include prevention of infection, removal of devitalized tissue, and closure of the wound. The application of dressings and topical antimicrobial therapy reduce pain by minimizing the exposure to air.
Primary Excision.: In children with large, full-thickness burn wounds, excision is performed as soon as the patient is hemodynamically stable after initial resuscitation. Because the burn wound precipitates an exaggerated physiologic response, many complications do not resolve until the eschar is excised and the wound is closed. Early excision of deep partial- and full-thickness burns reduces the incidence of infection and the threat of sepsis.
Débridement.: Partial-thickness wounds require débridement of devitalized tissue to promote healing. Débridement is painful and requires analgesia and a sedative before the procedure. Medications given for pain need to be readily available during this procedure and may need to be titrated up during the procedure. Hydroxyzine and diphenhydramine are often needed for itching that occurs after whirlpool and débridement. The itching becomes particularly bothersome as the burns heal.
Hydrotherapy is employed to cleanse the wound and involves soaking in a tub or showering at least once a day for no more than 20 minutes. The water acts to loosen and remove sloughing tissue, exudate, and topical medications. Hydrotherapy helps to cleanse not only the wound but the entire body and aids in maintenance of range of motion. Mesh gauze serves to entrap the exudative slough and is readily removed during hydrotherapy. Any loose tissue is carefully trimmed away before the wound is redressed.
Topical Antimicrobial Agents.: Methods used for managing the burn wound include:
Exposure—Wounds are left open to air; crust forms on partial-thickness wounds, and eschar forms on full-thickness burns.
Open—Topical antimicrobial agent is applied directly to the wound surface and the wound is left uncovered.
Modified—Antimicrobial agent is applied directly or impregnated into thin gauze and applied to the wound; gauze or net secures the area.
Occlusive—Antimicrobial agent is impregnated in gauze or applied directly to the wound; multiple layers of bulky gauze are placed over the primary layer and secured with gauze or net.
All these methods provide wound coverage and employ some type of topical agent. Topical agents do not eliminate organisms from the wound but can effectively inhibit bacterial growth. To be effective, a topical application must be nontoxic, capable of diffusing through eschar, harmless to viable tissue, inexpensive, and easy to apply. A topical ointment should not encourage the development of resistant strains of bacteria and should produce minimal electrolyte derangement. A comparison of commonly used agents is summarized in Table 30-11.
Biologic Skin Coverings.: Permanent coverage of extensive burns is a prolonged process that requires repeated operative procedures using general anesthesia for atraumatic care in débridement and grafting. Early closure shortens the period of metabolic stress and decreases the likelihood of burn wound sepsis. In the acute phase, biologic dressings cover and protect the wound from contamination, reduce fluid and protein loss, increase the rate of epithelialization, reduce pain, and facilitate movement of joints to retain range of motion.
Allograft (homograft) skin is obtained from human cadavers that are screened for communicable diseases. Allograft is particularly useful in the coverage of surgically excised deep partial- and full-thickness wounds in extensive burns when available donor sites are limited. Severe immunosuppression occurs in massively burned children, and the allograft becomes adherent. The allograft can remain in place until suitable donor sites become available. Typically, rejection is seen approximately 3 to 4 weeks after application (Herndon, 2007). The availability of tissue banks and a supply of suitable donors limit the use of allografts.
Xenograft from a variety of species, most notably pigs, is commercially available. In large burns, the porcine xenograft is commonly applied when extensive early débridement is indicated to cover a partial-thickness burn; this provides a temporary covering for the wound until an available autograft can be applied to the full-thickness areas (Herndon, 2007). Pigskin dressings are replaced every 1 to 3 days. They are particularly effective in children with partial-thickness scald burns of the hands and face because they allow relatively pain-free movement, which reduces contracture formation and has the added benefit of improving appetite and morale.
When applied early to a superficial partial-thickness injury, biologic dressings stimulate epithelial growth and faster wound healing. However, biologic dressings must be applied to clean wounds. If the dressing covers areas of heavy microbial contamination, infection occurs beneath the dressing. In the case of partial-thickness burns, such infection may convert the wound to a full-thickness injury.
Synthetic skin coverings are available for the management of partial-thickness burn wounds. Ideally, the dressing should provide the properties of human skin: adherence, elasticity, durability, and hemostasis. Synthetic skin substitutes are readily available, have an indefinite shelf life, and are relatively inexpensive.
Synthetic dressings are composed of a variety of materials and can be used successfully in the management of superficial partial-thickness burns and donor sites. Examples include adherent elastic films; hydroactive materials; or colloidal suspensions that are usually permeable to air, vapor, and fluids.
Biobrane is a flexible silicone-nylon membrane bonded to collagenous peptides of porcine skin. Calcium alginate is another treatment for donor sites. As with biologic dressings, it is important that the wound be free of debris before the dressing is applied. Body temperature elevation or evidence of purulence, erythema, or cellulitis around the wound edges may indicate that the wound has become infected beneath the dressing. If this occurs, prompt discontinuance of the synthetic dressing is indicated. All synthetic dressings are reputed to hasten wound healing and reduce discomfort.
Permanent Skin Coverings.: Permanent coverage of deep partial- and full-thickness burns is usually accomplished with a split-thickness skin graft. This graft consists of the epidermis and a portion of the dermis removed from an intact area of skin by a special instrument, the dermatome (Fig. 30-20). With extensive burns it is often difficult to find enough viable skin to cover the wounds; therefore available donor sites and special techniques are used. Split-thickness skin grafts may be sheet graft or mesh graft.
Sheet Graft.: A sheet of skin, removed from the donor site, is placed intact over the recipient site and sutured in place; this is used in areas where cosmetic results are most visible (Fig. 30-21).
Mesh Graft.: A sheet of skin is removed from the donor site and passed through a mesher, which produces tiny slits in the skin that allow the skin to cover 1.5 to 9 times the area of the sheet graft; this results in a less desirable cosmetic and functional outcome (Fig. 30-22).
The donor site is dressed with synthetic wound coverings or fine-mesh gauze until the dressing separates at 10 to 14 days, when the wound is healed. Dressings are not changed on donor sites to avoid damage to newly healed, delicate epithelium. Healed donor sites are available for reharvesting in patients with extensive burns and limited undamaged skin, but the quality of skin is decreased when multiple grafts are taken.
Artificial Skin.: The development of Integra, a product that allows the dermis to regenerate, has produced significant improvement in burn wound healing and decreased scar formation. It is applied to partial- and full-thickness burns. The two-layer membrane is made of collagen (a fibrous protein from animal tendons and cartilage) and silicone rubber (i.e., Silastic). The Silastic layer is peeled off after the dermis is formed. The application of artificial skin does not replace the grafting procedure, but it prepares the burn wound to accept an ultrathin autograft. Advantages include faster healing of the burn wound when integrity of the dermis is restored, faster healing of donor sites with the use of ultrathin grafts, and restoration of sweat glands and hair follicles. A disadvantage is its high cost.
Cultured Epithelium.: When burns are extensive and donor sites for split-thickness skin grafting are limited, it is possible to culture cells from a full-thickness skin biopsy and produce coherent sheets that can be applied to clean, excised full-thickness wounds. Epithelial cell culture grafts offer the possibility of an unlimited source of autografts in patients with extensive burns. Cultured epithelial autografts are effective in early wound closure. The child’s own skin is fractionated and cultured in a porcine media to form a thin epithelial layer that is applied to the burn wound. This technique offers an improved rate of survival in patients with extensive burns and limited donor sites.
Prognosis.: Children differ from adults in their responses to thermal injury, and the mortality rates in young children are significantly higher than those in older children and adults. Mortality is greatest for children younger than 48 months of age. Many children who do survive have long-term functional and cosmetic impairments.
Nursing Care Management
Because the care of burned children encompasses a broad range of skills, nursing care has been divided into segments that correspond with the major phases of burn treatment. The acute phase, also referred to as the emergent or resuscitative phase, involves the first 24 to 48 hours. The management phase extends from the completion of adequate resuscitation through wound coverage. The rehabilitative phase begins once the majority of the wounds have healed and rehabilitation has become the predominant focus of the care plan. This phase continues until all reconstructive procedures and corrective measures are accomplished (often a period of months or years).
Acute Phase.: The primary emphasis during the emergent phase is the treatment of burn shock and the management of pulmonary status. Monitoring vital signs, output, fluid infusion, and respiratory parameters are ongoing activities in the hours immediately after injury. IV infusion is begun immediately and is regulated to maintain a urinary output of at least 1 to 2 ml/kg in children weighing less than 30 kg (66 pounds); an output of 30 to 50 ml/hr is expected in children weighing more than 30 kg. Urinary output and specific gravity, vital signs, laboratory data, and objective signs of adequate hydration guide the rate of fluid administration.
Children who are hospitalized with burns require constant observation and assessment for complications. Alterations in electrolyte balance produce clinical symptoms of confusion, weakness, cardiac irregularities, and seizures. Changes in respiratory function and gas exchange are reflected clinically by restlessness, irritability, increased work of breathing, and alterations in blood gas values. The loss of protective function of the skin exposes burned children to increased risk of hypothermia. Edema formation and circulatory impairment result in the loss of sensation and deep throbbing pain.
Burn units maintain a pictorial record of the wound to record progress and for legal purposes (if child abuse is suspected). The burn wound is treated according to the protocol of the specific burn facility. The burn team monitors infection control procedures and ensures that staff and visitors comply with established protocols to prevent cross-contamination in the burn unit.
Throughout the acute phase of care, the psychosocial needs of the children and their families should not be overlooked. The child is frightened, uncomfortable, and often confused. Children may be isolated from familiar persons and surroundings; the overwhelming physical needs at this time are the primary focus of the staff and parents. In addition to feeling concern for their child, the family experiences guilt, which may be related to the fact that the parents did not or could not protect their child from injury. Consistency in the information presented and in the attitude of the staff creates a sense of familiarity and stability during the acute phase of care. Consistent caregivers can also help decrease the patient’s and family’s anxiety and provide coordination of care. For example, when many teams of consultants and specialists are involved in the child’s care, appointing one “spokesperson” decreases the confusion and enhances communication regarding the child’s care.
Management and Rehabilitative Phases.: After the patient’s condition is stabilized, the management phase begins. The multidisciplinary team concentrates on preventing wound infections, closing the wound as quickly as possible, and managing the numerous complications. Although the rehabilitative phase begins when permanent wound closure has been achieved, rehabilitation issues are identified on admission and are included in the care plan throughout the hospital course.
Comfort Management.: The severe pain of the wound and resultant therapies, the anxiety generated by these experiences, sleep deprivation, itching related to wound healing, and the conscious and unconscious interpretations of traumatic events contribute to the psychologic behaviors commonly observed in children with burns. It is always difficult to deal with a child in pain, and inflicting pain on a helpless child is contrary to the empathic nature of nursing. Interventions to promote comfort may include medications (including IV morphine or midazolam and short-term anesthetics such as propofol), relaxation techniques, distraction therapy, behavioral techniques, operant conditioning (e.g., tokens, star chart), and family participation.
Children need age-appropriate explanations before all procedures. When children appear to accept pain with little or no response, psychologic consultation may be needed. Consistency in caregivers is important. If this is not possible, a carefully developed, multidisciplinary care plan is necessary to provide consistency.
Care of the Burn Wound.: The nurse has a major responsibility for cleansing, débriding, and applying topical medications and dressings to the burn wound. Pain medication should be administered so that the peak effect of the drug coincides with the procedure. Children who have an understanding of the procedure to be performed and some perceived control demonstrate less maladaptive behavior. Children also respond well to participating in decisions (see Atraumatic Care box).
Outer dressings are removed. Any dressings that have adhered to the wound can be more easily removed by applying tepid water or normal saline. Loose or easily detached tissue is débrided during the cleansing process. In dressing the wound, it is important that all areas be clean, that medication be amply applied, and that no two burned surfaces touch each other (e.g., fingers or toes; ears touching the side of the head). If they are touching, the burned surfaces will heal together, causing deformity or dysfunction.
Topical medications may be applied directly to the wound with a tongue blade or gloved hand or impregnated into fine-mesh gauze before application. Dressings are then applied to assist in exudate absorption, wound débridement, and increased patient comfort. All dressings applied circumferentially should be wrapped in a distal-to-proximal manner. The dressing is applied with sufficient tension to remain in place but not so tightly as to impair circulation or limit motion. Elastic bandages are applied over dressings to prevent epithelial breakdown, decrease edema, stimulate circulation, and improve mobility. A stable dressing is especially important when the child is ambulatory.
Standard precautions, including the use of protective garb and barrier techniques, should be followed when caring for patients with thermal injuries. Frequent hand and forearm washing is the single most important element of the infection control program. Strict policies for cleaning the environment and patient care equipment should be implemented to minimize the risk of cross-contamination. All visitors and members of other departments should be oriented to the infection control policies, including the importance of hand and forearm washing and use of protective garb. Visitors should be screened for infection and contagious diseases before patient contact.
Nutrition.: Oral feedings are encouraged unless the child is intubated or paralytic ileus persists. Because children with burns often lack an appetite, the child needs encouragement, help, and patience. Consultation between the caregiver and the dietitian helps determine food preferences. Children who are old enough to participate should be included in meal planning. In addition, many children prefer an atmosphere more nearly like that provided at home. Therefore, when possible, many children enjoy sitting at a table and interacting with other children at mealtimes. Painful procedures should not be scheduled near mealtimes, since most children will be too physically exhausted and emotionally upset to eat.
Children who require enteral supplementation must be monitored for feeding intolerance and tube malposition. The nurse should also monitor and report any abdominal distention, diarrhea, or electrolyte and metabolic deviations.
Prevention of Complications
Acute Care.: The maintenance of body temperature is important to the child with burns. Core body temperature is supported when energy is conserved with an environmental temperature of 28° to 33° C (82.4° to 91.4° F). Large areas of the body should not be exposed simultaneously during dressing changes. Warmed solutions, linens, occlusive dressings, heat shields, a radiant warmer, and warming blankets assist in preventing hypothermia.
The chief danger during acute care is infection—wound infection, generalized sepsis, or bacterial pneumonia. Accurate and ongoing assessments of all parameters that provide clues to the early diagnosis and treatment of infection are essential. Symptoms of sepsis include a change in the level of consciousness, a rising or falling white blood cell count, hypothermia or hyperthermia, a loss of the progression of wound healing, increasing fluid requirements, hypoactive or absent bowel sounds, a rising or falling blood glucose level, tachycardia, tachypnea, and thrombocytopenia.
Children are reluctant to move if movement causes pain, and they are likely to assume a position of comfort. Unfortunately, the most comfortable position often encourages the formation of contractures and loss of function. Ongoing efforts to prevent contractures include maintaining proper body alignment, positioning and splinting involved extremities in extension, providing active and passive physical therapy, and encouraging spontaneous movement when feasible. Frequent position changes are important to promote adequate bronchopulmonary hygiene and capillary perfusion to common pressure areas. Low—air loss beds are beneficial for the morbidly obese or children with posterior grafts. Special attention should be given to areas at risk for increased pressure, such as the posterior scalp, heels, sacrum, and areas exposed to mechanical irritation from splints and dressings.
Long-Term Care.: The rehabilitative phase of care begins once wound coverage is achieved. Scar formation becomes a major problem as burn wounds heal (Fig. 30-23). Contractile properties of the scar tissue can result in disabling contractures, deformity, and disfigurement.

FIG. 30-23 Extensive scars from flame burn. (Courtesy The Paul and Carol David Foundation Burn Institute, Akron, Ohio.)
Uniform pressure applied to the scar decreases the blood supply. When pressure is removed, blood supply to the scar is immediately increased; therefore periods without pressure should be brief to avoid nourishment of the hypertrophic tissue. Continuous pressure to areas of scarring can be achieved by elastic bandages or commercially available pressure garments. Because these custom-made garments are often worn for months, revisions may be required as the child grows. It is much easier to prevent scarring and contracture of the wound than to resolve an existing problem. Splints and appliances may also be needed until wound maturation is achieved (Fig. 30-24).
Scar tissue has certain significant properties, particularly for growing children. Intense itching occurs in healing burn wounds and scar tissue until the scar is no longer active. Itching is usually treated with a combination of H1 and H2 antagonists such as cetirizine (Zyrtec) and cimetidine (Tagamet) (Baker, Zeller, Klein, and others, 2001); an H1 antagonist alone; and frequent applications of a moisturizer, such as Vaseline, Cetaphil, Aquaphor, Eucerin, cocoa butter, or Nivea. Petrolatum-based ointments (Vaseline, Aquaphor) seem to spread more easily on friable skin than thick creams do. Massage therapy during the application of moisturizers is also beneficial to stretch scar tissue and aid in contracture prevention. Scar tissue has no sweat glands, and children with extensive scarring may experience difficulty during hot weather. Caregivers should be alerted to this possibility and be prepared to institute alternate methods of cooling when necessary.
Scar tissue does not grow and expand, as does normal tissue, which may create difficulties, especially in functional areas such as on the hands and over joints. Additional surgery is sometimes required to allow independent functioning in daily activities, to improve cosmetic appearance, or to restore anatomic integrity.
The nursing activities in the rehabilitative phase of treatment focus on the child’s and family’s adaptation to the burn injury and their ability to reintegrate into the community. The psychologic pain and sequelae of severe burn injury are as intense as the physical trauma. The impact of severe burns taxes the coping mechanisms at all ages. Very young children, who suffer acutely from separation anxiety, and adolescents, who are developing an identity, are probably the most affected psychologically. Toddlers cannot understand why the parents they love and who have protected them can leave them in such a frightening and unfamiliar place. Adolescents, in the process of achieving independence from the family, find themselves in a dependent role with a damaged body. Being different from others at a time when conformity with peers is so important is difficult to accept.
Anticipation of the return to school can be overwhelming and frightening. It is essential that health care professionals recognize the importance of preparing teachers and classmates for the child’s return. Teachers need to be provided with information to assist the child and family and to promote the child’s optimal adjustment. Hospital-sponsored school reentry programs use a variety of methods to provide education and information about the implications of the injury, the garments and appliances, and the need for support and acceptance. Telephone calls, videotapes, information packets, and visits by members of the health care team offer opportunities to help with reintegration into the school environment’a focal point of the child’s life.
Psychosocial Support of the Child.: Children should begin early to do as much for themselves as possible and to be active participants in their care. Loss of control and perceived helplessness may result in acting-out behaviors. During illness, children regress to a previous developmental level that allows them to deal with stress. As children begin to participate in their care, they gain confidence and self-esteem. Fears and anxieties diminish with accomplishment and self-confidence. If the child demonstrates nonadherence in the rehabilitative phase, a behavior modification program can be initiated to promote or reward the child’s accomplishment in care.
Children need to know that their injury and the treatments are not punishment for real or imagined transgressions and that the nurse understands their fear, anger, and discomfort. They also need body contact. This is often difficult to arrange for the child with massive burns. Stroking areas of unburned skin is comforting. Even older children enjoy sitting on the parent’s lap and being cuddled and hugged. This can be a reward or a comfort in times of stress, but most of all it should be kept in mind that it is a natural part of childhood.
Psychosocial Support of the Family.: Recognizing and respecting each family’s strengths, differences, and methods of coping allow the nurse to respond to their unique needs by implementing a family-centered approach to care. In the acute phase, all attention is focused on the child, and the parents feel powerless and ineffectual. Most parents feel overwhelming guilt, whether or not the guilt is justified. They feel responsible for the injury. These feelings may impede the child’s rehabilitation. Parents may indulge the child and allow nonadherent behaviors that affect physical and emotional recovery. Parents need to be informed of the child’s progress and helped to cope with their feelings while providing support to their child. The nurse can help them understand that it is not selfish to look after themselves and their own needs to meet their child’s needs. It is important to recognize the parents’ need to grieve the change in their child’s normal appearance as part of the grieving process. Definitive professional help may be needed for parents whose response to the injury is severe or whose response to stress is manifested in destructive behavior.
The parents are members of the multidisciplinary team and participate in the development of the care plan. It is important to facilitate their input; to consider all aspects of the physical, emotional, social, and cultural factors affecting the child and family; and to establish a realistic home therapy program. The family’s willingness to assume responsibility for care and their ability to implement the therapeutic regimen are assessed. Home, school, and other environmental factors are explored; financial concerns and available community resources are discussed; and a specific care plan for the child, with an anticipated follow-up program, is developed.
Prevention of Burn Injury.: The best intervention is to prevent burns from occurring. Hot liquids in the kitchen and bathroom most commonly injure infants and toddlers. Hot liquids should be kept out of reach; tablecloths and dangling appliance cords are often pulled by toddlers, who spill hot grease and liquids on themselves. Electrical cords and outlets represent a potential risk to small children, who may chew on accessible cords and insert objects into outlets.
The Consumer Product Safety Commission recommends a reduction of water heater thermostats to a maximum of 48.9° C (120° F). The “dial-down” recommendation has been suggested by utility companies, burn treatment centers, medical personnel, and others interested in public safety. However, many water heaters continue to remain set at levels well above the safe level. Small children are especially at risk for scald injuries from hot tap water because of their decreased reaction time and agility, their curiosity, and the thermal sensitivity of their skin. Caregivers should never leave a child unattended in a bath and without adult supervision. Water should always be tested before a child is placed in the tub or shower.
The increased use of microwave ovens has resulted in burn injuries from the extremely hot internal temperatures generated in heated items. Baby formula, jelly-filled pastries, and hot liquids and dishes may result in cutaneous scalds or the ingestion of overheated liquids. Parents should use caution when removing items from the microwave oven and should always test the food before giving it to children.
As children mature, risk-taking behaviors increase. Matches and lighters are dangerous in the hands of the young. Adults must remember to keep potentially hazardous items out of the reach of children; a lighter, like a match, is a tool for adult use.
Education related to fire safety and survival should begin with the very young. They can practice “stop, drop, and roll” to extinguish a fire. The fire escape route, including a safe meeting place away from the home in case of fire, also should be practiced.
Community activities are also helpful in supporting burn survivors and preventing burns. The Aluminum Cans for Burned Children (ACBC) is an exemplary effort based at the Paul and Carol David Foundation Burn Institute, Akron, Ohio.* Activities funded by ACBC include Burn Survivors Support Group, Burn Camp, and meetings of Juvenile Firestoppers (for children with fire-setting behavior). Adult weekend retreats and school and family education sessions are a part of this program. The burn center and fire department provide the personnel to present programs.
Additional information on burn care and prevention can be obtained from the American Burn Association* and the National Safety Council.† The Alisa Ann Ruch Burn Foundation‡ provides assistance to burn victims and burn centers. The Shriners Burn Institutes are staffed to treat pediatric patients after acute burn injuries and those requiring rehabilitative and reconstructive services as a result of scarring and functional impairment. Information can be obtained from local Shrine Temples and Shrine Clubs, from Shriners Hospitals, or by contacting the International Shrine Headquarters.§ The Alisa Ann Ruch Foundation and Shriners Hospitals for Crippled Children support research to improve burn care and treatment and promote public education in burn prevention.
SUNBURN
Sunburn is a common skin injury caused by overexposure to UV light waves. The sun emits a continuous spectrum of visible and nonvisible light rays that range in length from very short to very long. The shorter, higher-frequency waves are more damaging than longer wavelengths, but much of the light is filtered out as it travels through the atmosphere. Of the light that does filter through, ultraviolet A (UVA) waves are the longest and cause only minimum burning, but play a significant role in photosensitive and photoallergic reactions. They are also responsible for premature aging of the skin and potentiate the effects of ultraviolet B (UVB) waves. UVB waves are shorter and are responsible for tanning, burning, and most of the harmful effects attributed to sunlight, especially skin cancer.
Numerous factors influence the amount of UVB exposure. Maximum exposure occurs at midday (10 am to 3 pm), when the distance from the sun to a given spot on the earth is shortest. There is more exposure at higher altitudes and near the equator, and less when the sky is hazy (although the amount of UV radiation that does penetrate is easily underestimated). Window glass effectively screens out UVB but not UVA rays. Fresh snow, water, and sand reflect UV rays, especially when the sun is directly overhead.
Sunburn is usually an epidermal burn, although severe sunburn can be a partial-thickness burn with blister formation. Treatment of sunburn involves stopping the burning process, decreasing the inflammatory response, and rehydrating the skin. Local application of cool tap water soaks, or immersion in a tepid-water bath (temperature slightly below 36.7° C [98° F]) for 20 minutes or until the skin is cool, limits tissue destruction and relieves the discomfort. After the cool applications, a bland oil-in-water moisturizing lotion can be applied. Partial-thickness burns are treated the same as those from any heat source (see earlier discussion on burns).
Nursing Care Management
Protection from sunburn is the major goal of management, and the harmful effects of the sun on the delicate skin of infants and children are currently receiving increased attention. To protect skin exposed to the sun for extended periods, skin should be covered with clothing, and FDA-approved sun protection agents should be applied.
Two types of products are available for sun protection: topical sunscreens, which partially absorb UV light, and sun blockers, which block out UV rays by reflecting sunlight. The most frequently recommended sun blockers are zinc oxide and titanium dioxide ointments. Sunscreens are products containing an SPF based on evaluation of effectiveness against UV rays. The SPF is a number, such as 15, which indicates that if individuals normally burn in 10 minutes without a sunscreen, use of a sunscreen with SPF 15 allows them to remain in the sun 15 times 10, or 150 minutes (2½ hours) before acquiring the same degree of burns. The most effective sunscreens against UVB are p-aminobenzoic acid (PABA) and PABA-esters. However, many individuals are allergic to PABA, and sunscreens without PABA are encouraged to prevent these reactions in children.
Sunscreens are applied evenly to all exposed areas, with special attention to skinfolds and areas that might become exposed as clothing shifts. Parents are directed to read labels of sunscreen products carefully for the SPF and follow the manufacturer’s directions for application.
Individuals who work in the community, such as teachers, daycare workers, coaches, and youth-group leaders, and relatives, should all be made aware of sun safety for children. Sunscreens must be applied liberally.
COLD INJURY
Cold injuries are most commonly seen in very cold regions. The nature of the heat-regulating mechanisms of the body are such that the inner portion of the body, or core, produces heat, and the periphery, or outer area, conserves or dissipates heat. When the body attempts to conserve heat, the outer tissues are subjected to low temperatures, and local trauma may result.
Chilblain, redness and swelling of the skin, occurs when extremities, usually the hands, are exposed intermittently to temperatures of 21.1° to 15.5° C (30° to 60° F). The response may vary but is characterized by intense vasodilation that increases the temperature of involved tissues above that of unaffected tissue and produces edematous, reddish blue patches that itch and burn. As warming takes place, the sensations become more intense, but ordinarily they subside in a few days.
Frostbite is the term used to describe tissue damage caused when excessive heat loss to local tissues allows ice crystals to form in tissues. The frostbitten part appears white or blanched, feels solid, and is without sensation. Rapid rewarming is associated with less tissue necrosis than slow thawing. It restores blood flow and shortens the period of cellular damage. Rewarming produces a flush (sometimes deep purple) and a return of sensation, which is extremely painful. Large blisters may appear in 24 to 48 hours after rewarming and begin to reabsorb within 5 to 10 days, followed by the formation of a hard black eschar. Superficial injury often heals without incident. Rewarming is accomplished by immersing the part in well-agitated water at 37.8° to 42.2° C (100° to 108° F). Discomfort is managed with analgesics and sedatives. Care of blistered skin is similar to that described for burns. It is seldom possible to estimate the extent of tissue loss until new skin layers are revealed after the eschar layer separates.
References
American Academy of Pediatrics, Committee on Infectious Diseases, Pickering L, eds. Red book: 2006 report of the Committee on Infectious Diseases, ed 27, London: Sounders, 2006.
American Academy of Pediatrics, Committee on Environmental Health. Ultraviolet light: a hazard to children. Pediatrics. 1999;104(2):328–333.
American Academy of Dermatology. Acne. http://www.aad.org/public/Publications/pamphlets/Acne.htm, 2006. [retrieved Feb 1, 2007, from].
American Academy of Dermatology. Guidelines for the care of atopic dermatitis. http://www.aad.org/professionals/guidelines/AtopicDermatitis.htm, 2003. [retrieved Feb 2, 2007, from].
Annequin, D, Carbajal, R, Chauvin, P, et al. Fixed 50% nitrous oxide oxygen mixture for painful procedures: a French survey. Pediatrics. 2000;105(4):E47.
Arnoldo, B, Klein, M, Gibran, NS. Practice guidelines for the management of electrical injuries. J Burn Care Res. 2006;27(4):439–447.
Baker, RAU, Zeller, RA, Klein, RL, et al. Burn wound itch control using H1 and H2 antagonists. J Burn Care Rehabil. 2001;22(4):263–268.
Bernardo, LM, Gardner, MJ, O’Connor, J, et al. Dog bites in children treated in a pediatric emergency department. J Spect Pediatr Nurs. 2000;5(2):87–95.
Burkhart, CN, Specht, K, Neckers, D. Synergistic activity of benzoyl peroxide and erythromycin. Skin Pharmacol Appl Skin Physiol. 2000;13(5):292–296.
Centers for Disease Control and Prevention. Division of Parasitic Diseases Scabies. http://www.cdc.gov/ncidod/dpd/parasites/scabies/factsht_scabies.htm, 2008. [retrieved April 22, 2008, from].
Centers for Disease Control and Prevention, Division of Parasitic Diseases. Treating head lice infestation. http://www.cdc.gov/ncidod/dpd/parasites/lice/factsht_head_lice_treating.htm, 2005. [retrieved April 22, 2008, from].
Centers for Disease Control and Prevention. Nonfatal dog bite—related injuries treated in hospital emergency departments—United States, 2001. MMWR. 2003;52(26):605–610.
Centers for Disease Control and Prevention. Cat-scratch disease in children—Texas, September 2000–August 2001. MMWR. 2002;51(10):212–214.
Food and Drug Administration. FDA issues health advisory regarding labeling changes for lindane products, April 2003, HealthInfo Tx Rep. http://www.fda.gov/bbs/topics/ANSWERS/2003/ANS01205.html. [retrieved March 4, 2007, from].
Goates, BM, Atkin, JS, Wilding, KG, et al. An effective nonchemical treatment for head lice: a lot of hot air. Pediatrics. 2006;188(5):1962–1970.
Frankowski, BL, Weiner, LB. Head lice. Pediatrics. 2002;110(3):638–643.
Herndon DN, ed. Total burn care, ed 3, London: Saunders, 2007.
Jacobs, DG, Deutsch, NL, Brewer, M. Suicide, depression, and isotretinoin: is there a causal link? J Am Acad Dermatol. 2001;45(5):S168–S175.
Kaplan, SL. Community-acquired methicillin-resistant Staphylococcus aureus infections in children. Semin Pediatr Infect Dis. 2006;17(3):113–119.
Krasner, DL, Rodeheaver, GT, Sibbald, RG. Chronic wound care: a clinical source book for healthcare professionals, ed 3. Wayne, Penn: HMP Communications, 2001.
Kronemyer, B. Scratching the surface of atopic and contact dermatitis. Infect Dis Child. 2003;16(3):40.
Laude, TA. Acne in childhood and adolescence: update on treatment choices. Consultant. 2000;3:457–465.
Lee, MC, Rios, Am, Aten, MF, et al. Management and outcome of children with skin and soft tissue abscesses caused by community-acquired methicillin-resistant Staphylococcus aureus. Pediatr Infect Dis J. 2004;23(2):123–127.
Mancini, AJ. Acne vulgaris: a treatment update. Contemp Pediatr. 2000;17(12):122–133.
McCord, SS, Levy, ML. Practical guide to pediatric wound care. Semin Plast Surg. 2006;20(3):92–199.
Mumcuoglu, KY, Barker, SC, Burgess, IE, et al. International guidelines for effective control of head louse infestations. J Drugs Dermatol. 2007;6(4):409–414.
Pearlman, DL. A simple treatment for head lice: dry on, suffocation based pediculicide. Pediatrics. 2004;114(3):e275–e279.
Purdue, GF. American Burn Association presidential address 2006 on nutrition: yesterday, today, and tomorrow. J Burn Care Res. 2007;28(1):1–5.
Russell, JJ. Topical therapy for acne. Am Fam Physician. 2000;61(2):357–366.
Strong, M, Johnstone, PW. Interventions for treating scabies. Cochrane Database Syst Rev. 2008;18(3):CD000320.
Wade, CF. Keeping Lyme disease at bay: an integrated approach to prevention. Am J Nurs. 2000;100(7):26–31.
Wormser, GP, Dattwyler, RJ, Shapiro, ED, et al. The clinical assessment, treatment, and prevention of Lyme disease, human granulocytic anaplasmosis, and babesiosis: clinical practice guidelines by the Infections Diseases Society of America. Clin Infect Dis. 2006;43:1089–1134.
Yetman, RJ, Parks, D. Diagnosis and management of atopic dermatitis. J Pediatr Health Care. 2002;16(3):143–145.
*PO Box 466, Lyme, CT 06371; e-mail: inquire@aldf.com; http://www.aldf.com.
*The American Burn Association offers an Advanced Burn Life Support Program; http://www.ameriburn.org/ablsnow.php.
*Akron Children’s Hospital, One Perkins Square, Akron, OH 44308-1062; (330) 543-1000; fax: (330) 543-9998; http://www.akronchildrens.org.
*625 North Michigan Ave., Suite 2550, Chicago, IL 60611; (312) 642-9260; fax: (312) 642-9130; e-mail: info@ameriburn.org; http://www.ameriburn.org.
†1121 Spring Lake Drive, Itasca, IL 60143-3201; (630) 285-1121, e-mail: info@nsc.org; http://www.nsc.org.
‡2501 W. Burbank Blvd., Suite 201, Burbank, CA 91505; (800) 242-BURN; http://www.aarbf.org.
§2900 Rocky Point Drive, Tampa, FL 33607; Shriners International Headquarters website: http://www.shrinershq.org; Shriners Hospitals for Children website: http://www.shriners.com/Hospitals/_Hospitals_for_Children.
 IN TEXT
IN TEXT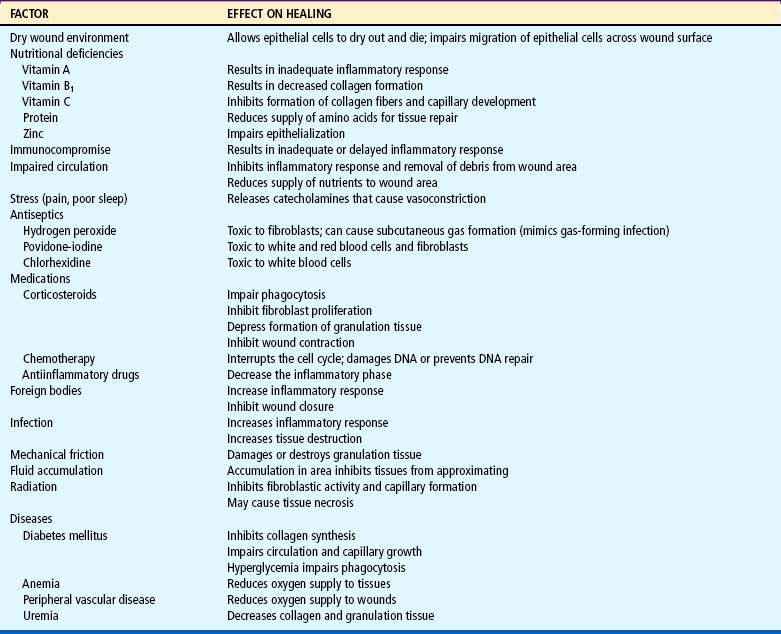
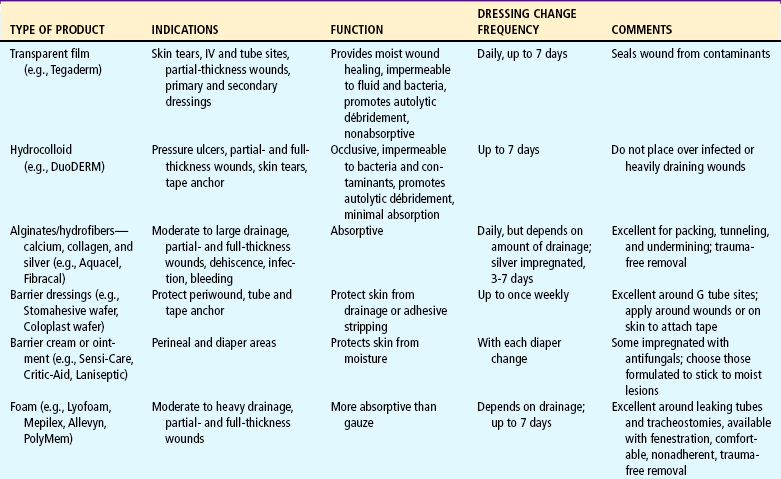
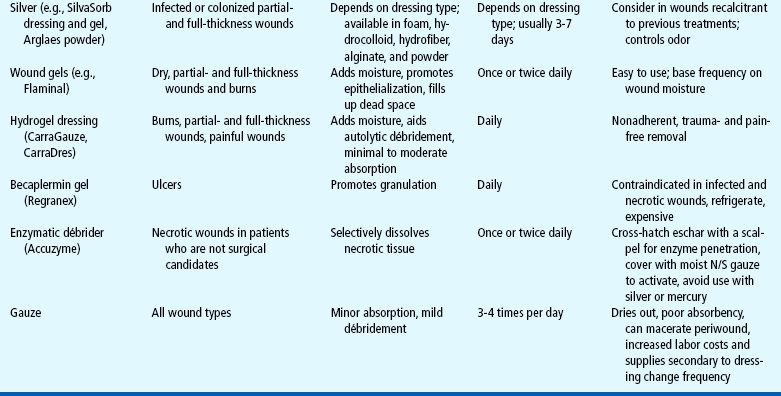
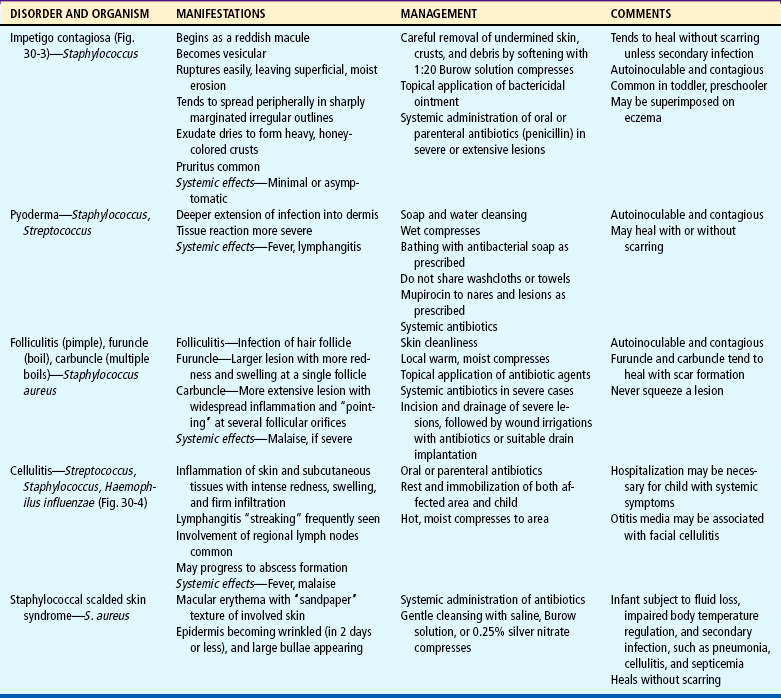
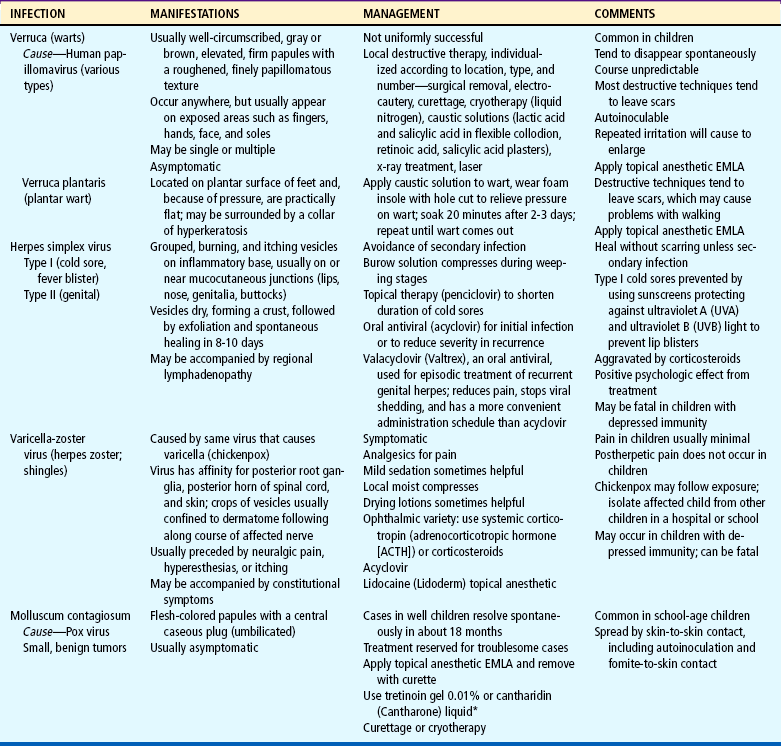
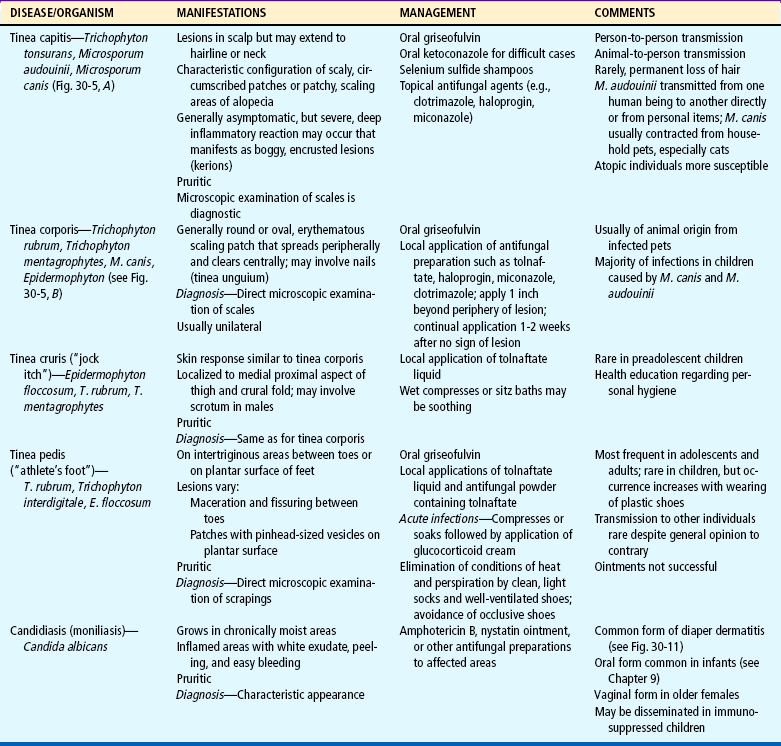
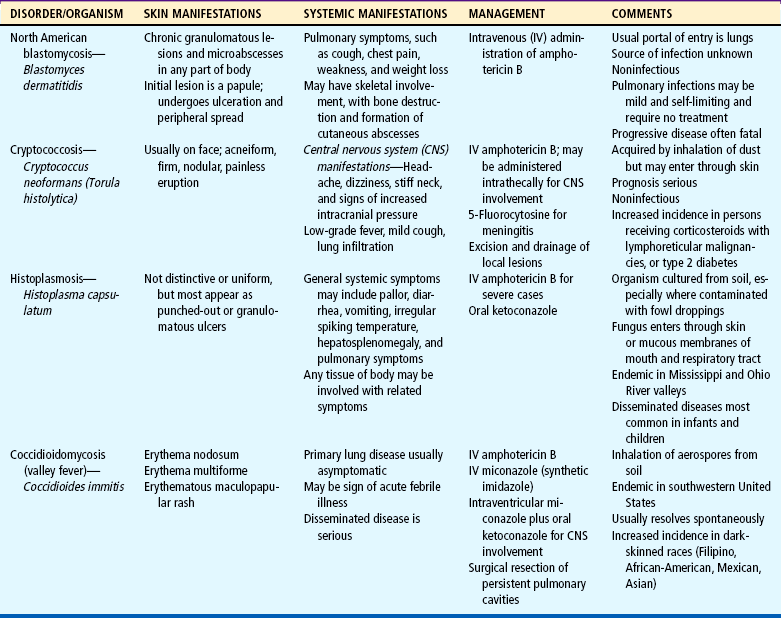

 CRITICAL THINKING EXERCISE
CRITICAL THINKING EXERCISE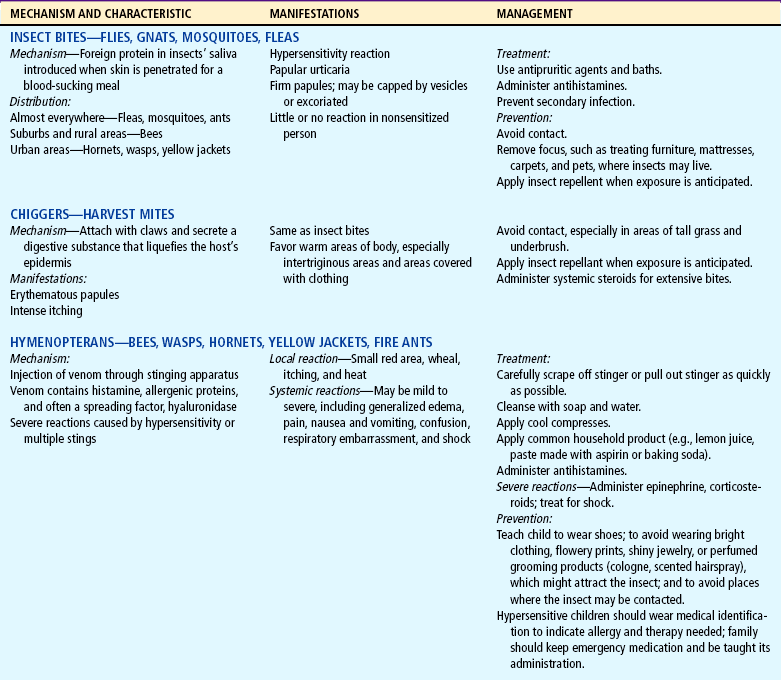
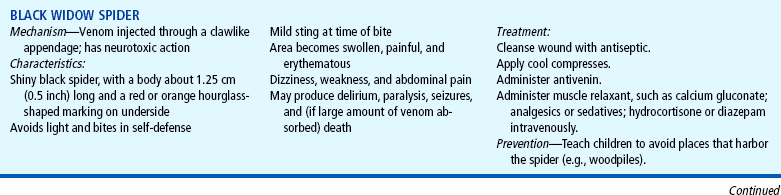
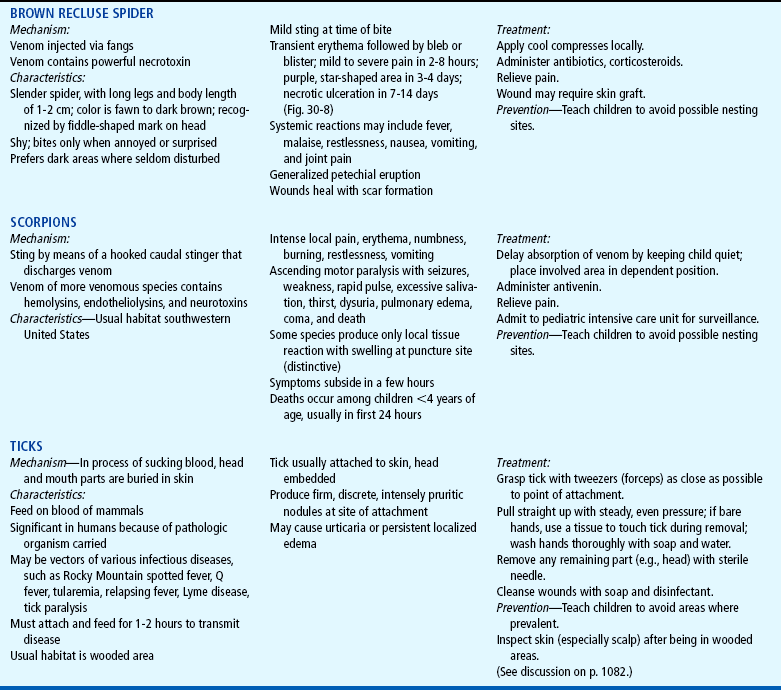
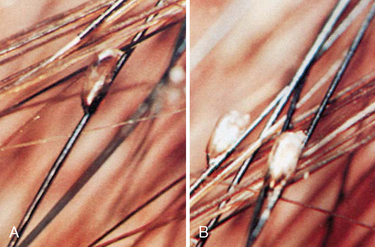
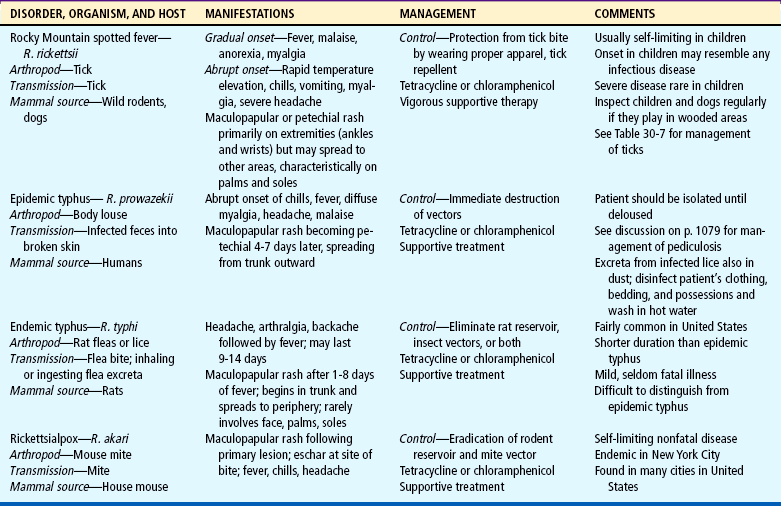


 FAMILY-CENTERED CARE
FAMILY-CENTERED CARE

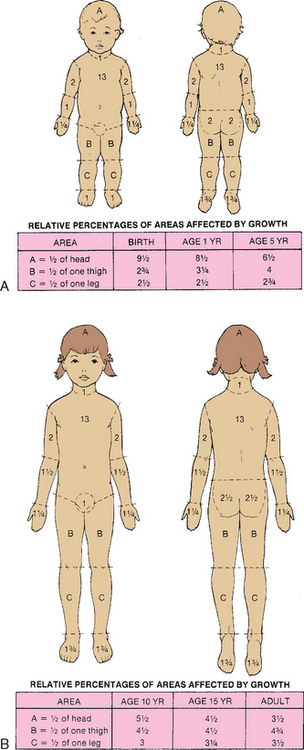

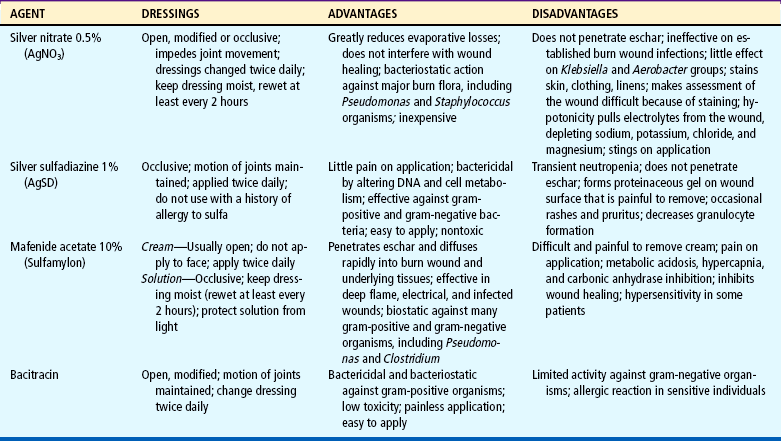



 ATRAUMATIC CARE
ATRAUMATIC CARE