Chapter 9 Applied Anatomy of the Musculoskeletal System
It is beyond the scope of this book to describe all aspects of musculoskeletal anatomy in depth, yet a detailed knowledge of anatomy is fundamental to a lameness diagnostician, as highlighted in the chapters on observation and palpation (see Chapters 5 and 6). Some aspects of anatomy are considered in depth in individual chapters dealing with conditions of specific areas. This chapter considers some philosophical aspects of the importance of anatomical knowledge and describes some basic principles. It also provides illustrations that we hope will help the reader to understand better the three-dimensional aspects of anatomy.
Accurate interpretation of what we see and feel during an examination requires knowledge of what structures we are looking at and palpating. For example, a swelling is noted over the dorsal aspect of the carpus. Is the swelling diffuse and possibly related to a hygroma, periarticular edema, or cellulitis, or is there a discrete swelling, horizontally oriented, reflecting distention of the middle carpal joint? Or is it a longitudinal swelling reflecting distention of the common digital extensor tendon sheath or the tendon sheath of the extensor carpi radialis? If the swelling is longitudinal, are any compressions in the swelling caused by normal retinaculum or adhesions within the sheath (Figure 9-1)? If we examine the sheath by ultrasonography, is the echogenic band extending from the sheath wall to the enclosed tendon normal mesotendon, or is it an adhesion? If diffuse swelling is present around the dorsal aspect of the carpus associated with lameness, how can we tell if the middle carpal joint capsule is distended? We need to know that there is a palmar outpouching of the middle carpal joint on the palmarolateral aspect of the carpus, just distal to the accessory carpal bone. Thus during visual inspection and palpation the clinician should be constantly asking, “What structure am I seeing or palpating, what are its functions, and what would be the consequences of loss of function?” If it has abnormal contour or size, is this the result of swelling of that structure or of an adjacent or underlying structure? Having established what structure is abnormal, the clinician then must consider the best imaging modality. If it is a tendonous or ligamentous structure, ultrasonography probably will provide the most information, but we must remember that it has bony attachments, and damage at those attachments might best be assessed by either radiology or nuclear scintigraphy. So we need to know not only what each structure is, but also the structures to which it is attached.

Fig. 9-1 Sagittal anatomical section through the carpus, transecting the extensor carpi radialis tendon (ECRT). C3, Third carpal bone; ICB, intermediate carpal bone.
During visual inspection and palpation, we also need to think logically. We know that the superficial and deep digital flexor tendons (SDFT, DDFT), the accessory ligament of the DDFT (ALDDFT), and the suspensory ligament (SL) lie on the palmar aspect of the third metacarpal bone (McIII) (Figure 9-2). Swelling confined to just the medial aspect of the metacarpal region is far more likely to reflect direct trauma to the medial aspect of the limb than sprain or strain of any of the ligamentous or tendonous structures. We need to know that the proximal aspect of the SL lies between the bases (heads) of the second and fourth metacarpal bones and therefore is inaccessible to direct palpation, and that desmitis often may be present without discernible soft tissue swelling (Figure 9-3).
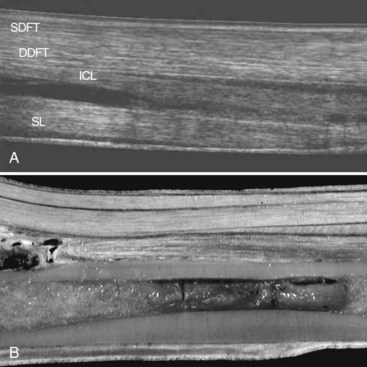
Fig. 9-2 Sagittal views of the palmar metacarpal region. Proximal is to the right. A, FreeStyle Extended Imaging (Sequoia model, Acuson, Mountain View, California, United States) ultrasonographic image of the palmar metacarpal region. B, Corresponding anatomical section. DDFT, Deep digital flexor tendon; ICL, accessory ligament of the DDFT (inferior check ligament); SDFT, superficial digital flexor tendon; SL, suspensory ligament.
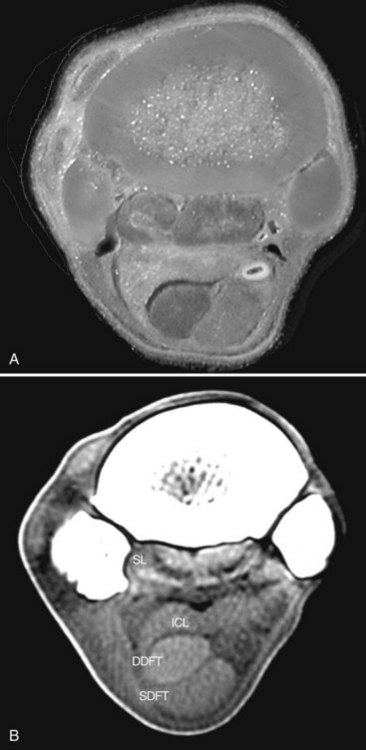
Fig. 9-3 Transverse sections through the proximal metacarpal region. Dorsal is to the top and lateral is to the left. A, Anatomical specimen. B, Computed tomographic scan using soft tissue windowing. DDFT, Deep digital flexor tendon; ICL, accessory ligament of the deep digital flexor tendon (inferior check ligament); SDFT, superficial digital flexor tendon; SL, suspensory ligament.
We must be aware of anatomy to realize the possible consequences of trauma to an area. The paucity of soft tissues over the cranial aspect of the stifle makes the patella and the tibial tuberosity vulnerable to direct trauma, hence the risk of fracture after hitting a fixed fence. The lack of soft tissues also means that if the horse hits a thorn hedge, the possibility of a thorn penetrating the femoropatellar joint capsule, resulting in contamination and infection, is quite high. We also need to think about how structures move relative to one another while the horse is in motion. If a steeplechase horse sustains an interference injury on the palmar aspect of the metacarpal region while galloping, the position of the skin laceration probably will not coincide with the level of the laceration in the SDFT (Figure 9-4). We also need to know the relative positions of the laceration and the digital flexor tendon sheath to be aware of the likelihood that the sheath may have been traumatized, and thus the risk of infectious tenosynovitis. Faced with a contaminated wound on the dorsal aspect of a hind fetlock and severe lameness, and the possibility of infection of the metatarsophalangeal joint, we need to know where to expect to see distention of the plantar pouch of the joint capsule and to know that this site is safely accessible for arthrocentesis.
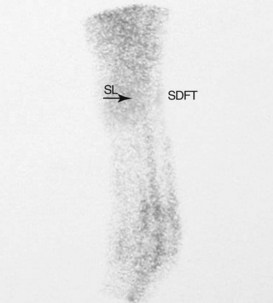
Fig. 9-4 Lateral scintigraphic image of the metacarpal region acquired before the end of the flow (vascular) phase and at the beginning of the pool phase. This jumper had a history of low-grade chronic desmitis of the proximal aspect of the suspensory ligament (SL), and mild diffuse superficial digital flexor (SDFT) tendonitis. An acute interference injury to the midmetacarpal region was evident on the skin. Note the proximal location of the acute injury to the SDFT. The linear area of uptake between the SL and SDFT is vascular artifact related to the time of acquisition.
A fundamental principle of lameness investigation is the identification of the source or sources of pain. Although this may be possible through detailed clinical examination, in many instances it is essential to perform diagnostic analgesia (see Chapter 10). A detailed knowledge of the anatomy of nerves, joint capsules and the various outpouchings, tendon sheaths, and bursae is fundamental to safe, accurate performance of perineural and intrasynovial injections.
Given the knowledge of the close relationship among the distal interphalangeal joint capsule, the distal sesamoidean impar ligament, the collateral sesamoidean ligaments and the distal phalanx, and the close proximity of branches of the palmar digital nerve, it is not surprising that intraarticular analgesia is not specific and that other structures can be affected, especially if interpretation of the response is delayed or an excessively large volume of local anesthetic solution is used. Knowledge that the medial and lateral femorotibial joints do not normally communicate and that the cruciate ligaments usually are extraarticular structures is crucial for an understanding of why these joint compartments must be injected separately, and why the response to intraarticular analgesia may be both incomplete and delayed if a cruciate ligament is damaged.
Knowledge of functional neuroanatomy also is important for interpretation of specific gait abnormalities. Inability to bear weight on a hindlimb after general anesthesia may be the result of myopathy, but in the absence of marked pain and distress, it is more likely that the horse has lost extensor function and is unable to extend any of the hindlimb joints because of femoral nerve paresis. Loss of ability to extend the elbow may result from loss of triceps function associated with a fracture of the olecranon but may also be caused by radial nerve paresis.
Vascular anatomy is important because many nerves lie close to vessels. With superficial nerves and vessels, identification of the vessel may facilitate palpation of the nerve and thus aid accurate perineural injection. Avoiding penetration of the vessel and causing hematoma formation also is desirable. With regard to deeper nerves the veterinarian may benefit by knowing that the needle must be in close proximity to the nerve if blood appears in the needle hub. This information can be helpful when performing perineural analgesia of the deep branch of the fibular nerve.
Assessment of digital pulse amplitudes is an integral part of palpation. Increased pulse amplitude usually signifies a site of inflammation at, or distal to, the region of palpation, especially in association with inflammatory conditions of the foot, such as subsolar abscessation or laminitis. Palpation of the pulse in the dorsal metatarsal artery and assessment of saphenous vein filling can be helpful in the evaluation of a horse with suspected aortoiliac thrombosis.
Knowledge of the sites of major vessels is important when considering the consequences of major laceration to an area and possible avascular areas, and in planning a surgical approach to an area. All bones have one or more nutrient foramina through which major vessels enter. These usually are in standard locations (Figure 9-5). Knowledge of these sites is critical for accurate radiological interpretation because a nutrient foramen appears as a radiolucent area, which should not be confused with a pathological lesion. The position of these intraosseous vessels also has important consequences in considering repair of major long bone fractures.
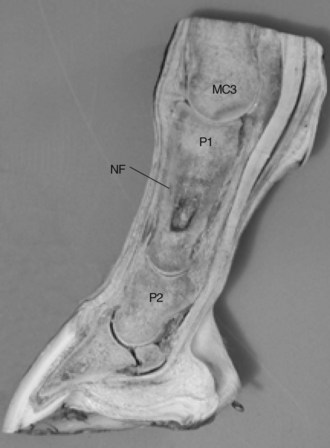
Fig. 9-5 Sagittal anatomical section through the pastern demonstrating a common location for the nutrient foramen (NF) entering the proximal phalanx (P1). MC3, Third metacarpal bone; P2, middle phalanx.
Thermography relies on the detection of surface heat and is obviously greatly influenced by the position of superficial vessels. Interpretation may be misleading without knowledge of location. Thus it should be absolutely clear that anatomy is a dynamic subject and is not merely a function of knowing the origins and insertions of numerous structures.
We also need to know some fundamentals of biomechanics. What is the biomechanical function of the SL? What are the implications of loss of function? For example, how may function be altered by a change in foot angle after application of a heel wedge? How is load in the distal limb joints affected by mediolateral foot imbalance? If the accessory ligament of the SDFT is cut (superior check desmotomy), how does this alter the function of not only the SDFT but also other tendonous and ligamentous structures? Does consequent overload of the SL predispose to an increased risk of suspensory desmitis? When orthopedic surgery is being considered, which is the tension side of the bone, to which a bone plate should be applied to take advantage of the tension band principle?
In more general terms, how will lameness in the left hindlimb alter forces in the other limbs, and does this vary with the gait? Given the reciprocal apparatus of the hindlimb and the inability to flex and extend the limb joints independently, it is not surprising that the gait characteristics of hindlimb lameness are so similar, irrespective of the source of pain causing lameness. Understanding the reciprocal apparatus in addition to the results of loss of its function (e.g., after damage to the fibularis tertius) is hugely important for an understanding of hindlimb lameness.
After the source of pain causing lameness has been isolated, then it is necessary to establish what is causing pain; this requires one of a number of imaging modalities: radiography, ultrasonography, nuclear scintigraphy, magnetic resonance imaging (MRI), computed tomography (CT), and exploratory arthroscopy, bursoscopy, or tenoscopy. Accurate interpretation of the findings from any of these techniques requires specialist anatomical knowledge. With radiographic images, various structures are superimposed, resulting in potentially confusing radiolucent lines that can mimic a fracture (e.g., in the relatively complex carpus and tarsus). A frog shadow superimposed over the navicular bone may mimic a fracture. We must be cognizant of anatomical variations, for example, the shape and size of the crena of the distal phalanx. We have to know how best to image a specific anatomical location, such as the sustentaculum tali of the calcaneus (fibular tarsal bone) using a skyline projection. For interpretation of the clinical significance of periosteal or entheseous new bone, detailed knowledge of the soft tissue structures that do (or do not) attach in that area is vital. Particularly in the fetlock and pastern areas, numerous ligamentous structures have discrete areas of attachment (Figure 9-6).
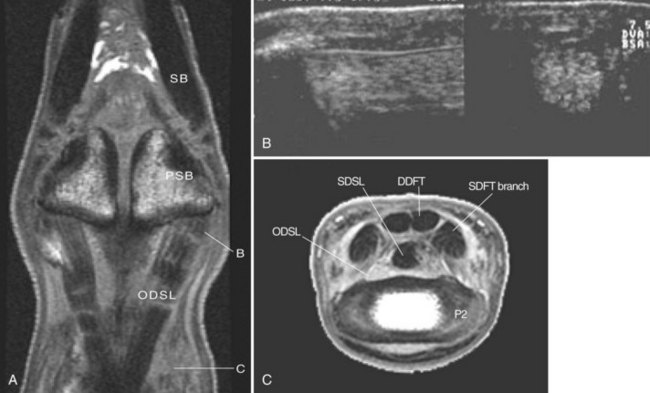
Fig. 9-6 The oblique distal sesamoidean ligaments. A, Frontal magnetic resonance image (MRI) of the pastern showing the origins and insertions of the oblique distal sesamoidean ligaments (ODSL). B, Frontal (left) and transverse (right) ultrasonographic images of the ODSLs obtained at point B in A. Proximal and dorsal are to the left. C, Transverse MRI scan obtained at point C in A. DDFT, Deep digital flexor tendon; P2, middle phalanx; PSB, proximal sesamoid bone; SB, suspensory branch; SDFT, superficial digital flexor tendon; SDSL, straight distal sesamoidean ligament.
(A Courtesy Alexia L. McKnight, University of Pennsylvania, Philadelphia, Pennsylvania, United States.)
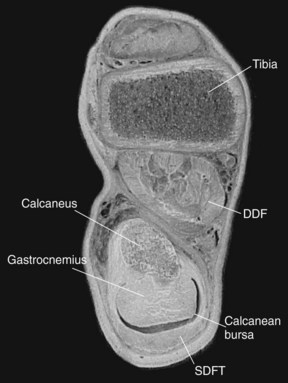
Radiography requires the awareness that we are looking at a three-dimensional structure in two dimensions, and thus images of the area must be obtained from several different angles. With ultrasonography, and more particularly with MRI and CT, structures can be imaged in three dimensions; this requires detailed knowledge of the shape, size, and relationships among structures. In the proximal metatarsal region the DDFT lies more medial than the SDFT and SL, and thus these structures cannot be imaged adequately by ultrasonography at the same time from the plantar aspect of the limb (Figure 9-7). The transducer must be moved to a plantaromedial site to evaluate the DDFT in its entirety. A large vessel on the plantarolateral aspect of the SL can cause shadowing artifacts in the SL.
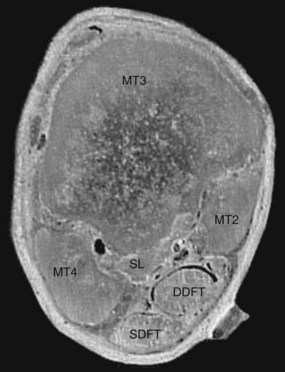
Fig. 9-7 Transverse anatomical section of the proximal metatarsal region demonstrating the lateral position of the superficial digital flexor tendon (SDFT) relative to the deep digital flexor tendon (DDFT). Lateral is to the left and dorsal to the top of the image. This arrangement is the opposite of that seen in the forelimb (compare with Figure 9-3). MT2, MT3, and MT4, Second, third, and fourth metatarsal bones, respectively; SL, suspensory ligament.
The internal architecture of the joint becomes important during exploratory arthroscopy. What are the normal variations in cartilage thickness? Where do you expect to see a synovial fossa? Which parts of the synovial membrane are usually more vascular? Is it normal that the cranial cruciate ligament can be seen without synovial covering from the medial femoral tibial joint?
A textbook of this type cannot possibly provide detailed descriptions of all aspects of anatomy, functional anatomy, and biomechanics, nor answer all of the questions posed earlier in this chapter. It is hoped that this overview will stimulate readers to have a thirst for more knowledge of these subjects, in the understanding of their huge importance.
Lameness clinicians are encouraged to acquire a set of boiled-out bones for reference and perform detailed dissections of cadaver limbs to improve knowledge of anatomy. Practicing nerve block techniques on cadaver limbs is very important for inexperienced clinicians or those performing a new block for the first time. If a lame horse must be humanely destroyed, clinicians should take the opportunity, whenever possible, to perform a postmortem examination to correlate clinical findings with the actual lesions and revise anatomy at the same time. Each time a dissection is performed, new anatomical detail becomes apparent that previously may have been missed.
The remainder of this chapter provides some basic definitions of anatomical terms used elsewhere in the book, describes the reciprocal apparatus of the forelimb and hindlimb, and presents correlative illustrations of anatomical specimens and images of those areas to assist in the understanding of three-dimensional anatomy.
The Language of Anatomy
The system described in the Nomina Anatomica Veterinaria (NAV) according to the guidelines of the International Committee on Veterinary Anatomical Nomenclature has been used so that anatomical terminology is universal. English translations of NAV terms have been used whenever possible according to these guidelines.
Forces
The interaction of anatomical structures allows for the conversion of chemical energy into purposeful movement. It is often useful to think of complex anatomical structures in terms of interactions between simplified structural units. The interaction of forces within these anatomical units dictates the abilities and the potential weaknesses of the equine athlete. In simple terms, the stresses acting on the body are compression, tension, shear, torsion, and bending.
Compression is the force applied between two points to move them together. Examples of compression are seen in joints, such as within the middle carpal joint at the interface between the radial and third carpal bones, or the compression sustained by the digital cushion between the sole, frog, and the distal phalanx. Compression also is sustained within most bones, such as the third carpal bone or the dorsal cortex of the McIII.
Tension is the force that tends to stretch or elongate a structure. Examples of tension are most obvious in tendons and ligaments, but bones such as the olecranon or within the palmar cortex of the McIII also sustain tensile strain.
Shear is a stress at the interface between two structures moving in opposite directions. Examples of shear are seen in the femoropatellar and tarsocrural joints, within bone, and within the hoof capsule.
Torsion is the stress produced when a twisting motion is applied to an object. Examples of torsional stress are seen within joints, such as the distal hock joints, or within individual bones, such as the McIII.
Bending is a combination of compression on one side of a structure and tension on the other side. Structures subjected to bending are long bones such as the McIII, where the dorsal cortex is subjected to compression, whereas the palmar cortex is subjected to tension.
Specialized Structures
Synovial Structures
Synovial bursae, tendon sheaths, and joints have a similar function and generally similar structure. All are sacs containing synovial fluid produced by the lining of the sac. In simple terms, synovial structures facilitate the movement between independent structures by providing a hydraulic cushion of viscous fluid that limits the effects of friction to help dissipate compressive and shear forces. (For a more complete discussion on synovial structures, see Chapter 61Chapter 62Chapter 63Chapter 64Chapter 65Chapter 66Chapter 67Chapter 74Chapter 75Chapter 76Chapter 77Chapter 78Chapter 79.)
A diarthrosis is a mobile joint containing a synovial membrane. This membrane is flexible enough to allow for movement of the joint. The synovial fluid lubricates, hydraulically equalizes pressure between cartilage plates, and nourishes the articular cartilage.
A synovial sheath is a sac that completely surrounds a tendon, forming a synovial lining on the surface of the tendon and the lining of the sheath. The synovial reflection between these visceral and parietal layers is termed the mesotendon. This structure is similar to the mesentery in the abdominal cavity. Nerve and blood supply to the tendon is found within the mesotendon. In areas of great mobility within the synovial sheaths, the nerve and blood supply to the tendons is through a vinculum, which is a modified mesotendon in the form of a narrow band connecting visceral and parietal layers.
A synovial bursa is a simple sac lying between a tendon or muscle and an adjacent bony prominence. A bursa does not surround the tendon but acts as a cushion at the interface where pressure is concentrated (Figure 9-8).
Intercalated Bones
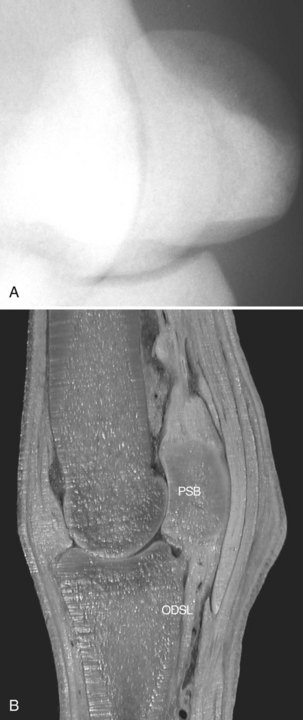
Intercalated bones are bones that arise within tendons or ligaments allowing for the interface between the tendonous structure and the underlying bone at an area of focal pressure, typically at the level of a joint. The interface between these bones is within a synovial sac. The navicular bone, proximal sesamoid bones (PSBs), and patella are intercalated bones. These bones allow for smooth movement and dissipation of focal pressure between the tendon or ligament and the underlying joint (Figure 9-9).
Fibrocartilaginous Structures
In general terms, there are four functional arrangements of fibrocartilage: interarticular, connecting, circumferential, and stratiform.
Interarticular Fibrocartilage
Menisci are fibrocartilaginous structures located between the articular cartilages of a diarthrosis. Menisci are not directly attached to the joint surfaces but are held in place by ligaments immediately adjacent to the articular surfaces. They provide congruency between the condyles, allow for a greater range of movement of the joint, and absorb concussion. Menisci are found in the stifle and temporomandibular joints of the horse.
Connecting Fibrocartilage
A symphysis is a fibrocartilaginous joint that allows minimal movement. The pelvic symphysis and intersternebral and intervertebral joints are examples of fibrocartilaginous joints.
Circumferential Fibrocartilage
In the coxofemoral joint the acetabular lip (labrum acetabulare) is a fibrocartilaginous ring extending the articular surface in a firm, semiflexible manner. The transverse acetabular ligament is the portion of the labrum crossing the acetabular notch. The glenoid labrum seen in other species is a poorly developed fibrous band in the shoulder of the horse.
Stratiform Fibrocartilage
Stratiform fibrocartilages arise within ligamentous structures at an interface with high focal pressure between soft tissue and bone, either within a ligament or as an extension of a bony surface. These structures are similar to intercalated bones in that they typically provide rigidity to help dissipate compressive forces, but the moderate elasticity allows for some flexibility of the structures.
The parapatellar fibrocartilage on the medial aspect of the patella, portions of the biceps brachii tendon of origin within the intertubercular (bicipital) bursa, the manica flexoria, and portions of the DDFT adjacent to the proximal aspect of the middle phalanx are examples of stratiform cartilage formation within tendonous structures. The proximal, middle, and distal scuta are stratiform fibrocartilaginous structures associated with the intersesamoidean ligament, the palmar aspect of the middle phalanx, and the collateral sesamoidean ligaments, respectively. These structures serve as semirigid pulleys primarily for the DDFT.
Passive Stay Apparatus
Distal Limb
The horse is uniquely equipped to be able to stand at rest while expending minimal muscular effort. In the forelimb and hindlimb the fetlock is prevented from overextension by a combination of structures providing passive resistance. The suspensory apparatus is the main contributor, forming a sling that maintains the fetlock in extension. In addition, the SDFT, DDFT, and the associated accessory (check) ligaments (in the forelimb) act as tension bands providing passive support. The suspensory apparatus consists primarily of the SL and branches, PSBs, and distal sesamoidean ligaments. The intercalated PSBs provide a broad face at the point where focal pressure is high at the palmar or plantar aspect of the fetlock joint, enabling the ligamentous tension band to support the fetlock. Dorsal branches of the SL join with the common or long digital extensor tendon, helping to stabilize the dorsal aspect of the digit. The axial and abaxial palmar and plantar ligaments of the proximal interphalangeal joint, the SDFT branches, and the straight sesamoidean ligament support the palmar or plantar aspect of the proximal interphalangeal joint. The navicular bone and its suspensory apparatus, in combination with the distal sesamoidean impar ligament, stabilize the palmar or plantar aspect of the distal interphalangeal joint.
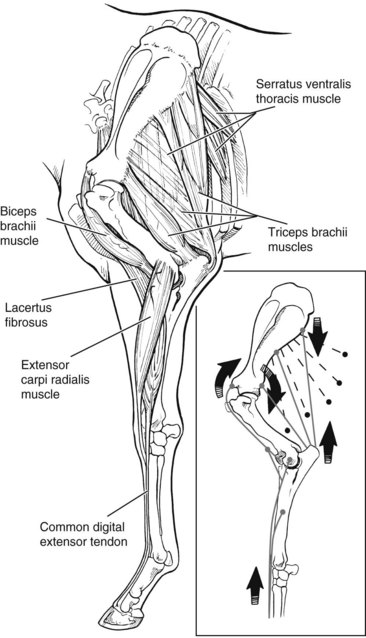
Forelimb
In the forelimb the fibrous portion of the serratus ventralis thoracis acts as a sling suspending the thorax from the forelimb by its attachment to the scapula. The downward force applied by the serratus ventralis on the caudal aspect of the scapula causes slight flexion of the scapulohumeral joint, applying tension to the biceps brachii. A fibrous band of the biceps brachii extends from the supraglenoid tubercle of the scapula and continues as the lacertus fibrosus, which joins with the extensor carpi radialis to passively extend the carpus. Minimal muscular effort by the triceps on the olecranon maintains the elbow in extension (Figure 9-10).
Hindlimb
The stifle is maintained in extension by the patellar locking mechanism with minimal muscular effort. Slight muscular effort by the quadriceps and tensor fasciae latae rotates the patella medially, where the cartilaginous process of the patella is caught caudal to the large prominence of the medial trochlear ridge of the femur. Slight relaxation of the quadriceps as a whole allows slight flexion of the stifle, which “locks” the patella in place by applying tension primarily to the medial and middle patellar ligaments (Figure 9-11). When the stifle is extended, the hock is passively extended by the superficial digital flexor and the fibrous component of the lateral head of the gastrocnemius muscles, which extend from the femur to the tuber calcis.
The reciprocal apparatus forces the hock to flex and extend in unison with the stifle. The reciprocal apparatus transfers mechanical energy to the distal aspect of the limb from the massive muscular structures of the upper limb without adding mass to the lower limb. The superficial digital flexor and the fibrous portion of the gastrocnemius muscles serve as the caudal component of the reciprocal apparatus, along with the long plantar ligament, which acts as a tension band to make the calcaneus, distal aspect of the tarsus, and metatarsal region a single functional lever arm. The fibularis (peroneus) tertius serves as the cranial component of the reciprocal apparatus, extending from the femur to the dorsal and lateral aspects of the tarsus (Figure 9-12). Although the fibularis tertius is important as part of the reciprocal apparatus, it is not essential for function of the passive stay apparatus, because its function is flexion of the tarsus.
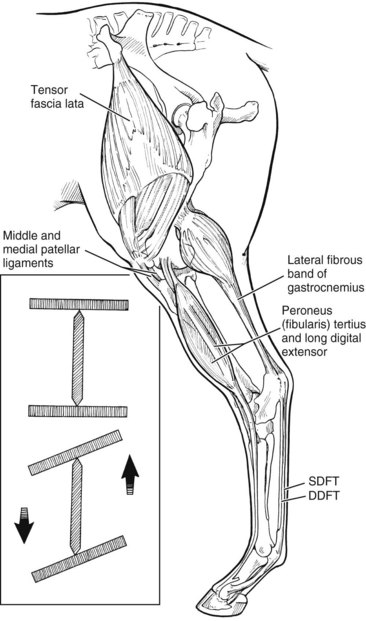
Fig. 9-12 The reciprocal apparatus. DDFT, Deep digital flexor tendon; SDFT, superficial digital flexor tendon.
A second reciprocal mechanism has been described for the lower hindlimb, where the fetlock and digit are flexed at the same time as the stifle and hock. The long digital extensor tendon and DDFT were the dorsal and plantar components suggested, but the SDFT probably also contributes.
Three-Dimensional Anatomy
Major advances in lameness diagnosis are being made with the assistance of advanced imaging techniques. Radiography, nuclear scintigraphy, and ultrasonography are well established, whereas CT and MRI are growing in importance. CT and MRI in particular require a detailed knowledge of three-dimensional anatomy. It is beyond the scope of this text to provide detailed correlative images of the entire musculoskeletal system. Figures 9-13 through 9-18 give a flavor of what is possible. Figures 9-13 through 9-16 highlight the complex anatomy of the navicular bone region, showing the close relationship between the collateral sesamoidean ligaments, the distal sesamoidean impar ligament, the DDFT, and the navicular bursa and distal interphalangeal joint capsule. Figures 9-17 and 9-18 demonstrate the relationship among some aspects of the complex anatomy of the carpal region.
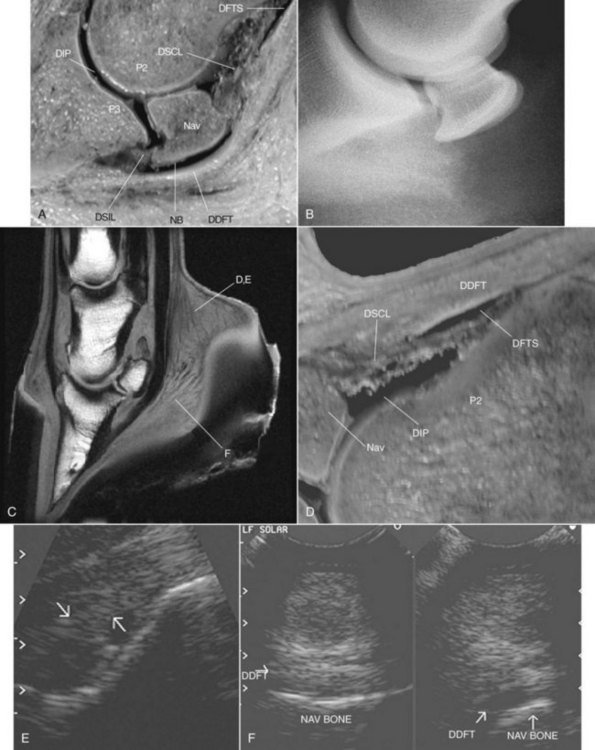
Fig. 9-13 Comparisons of the lateral view of the navicular bone and its relationship to neighboring structures. A, Sagittal anatomical section showing the digital flexor tendon sheath (DFTS), navicular bursa (NB), and distal interphalangeal (DIP) joint surrounding the navicular bone. B, Lateromedial radiographic image centered on the navicular bone. C, Sagittal magnetic resonance imaging scan of the foot. D and E, Sagittal anatomical section and corresponding ultrasonographic image of the palmar aspect of the distal aspect of the pastern obtained at points D and E in panel C. Proximal is to the right. The arrows outline the distal sesamoidean collateral ligament. F, Frontal (left) and sagittal (right) ultrasonographic images obtained through the frog at point F in panel C. The hypoechoic appearance of the portion of the deep digital flexor tendon (DDFT) is caused by the off-incidence artifact because the fibers are not perpendicular to the line of the ultrasound beam. Lateral and proximal are to the right. DSIL, Distal sesamoidean impar ligament; DSCL, distal sesamoidean collateral ligament (axial union forming fibrous portion of T ligament); Nav, navicular bone; P2, middle phalanx; P3, distal phalanx.
(B Courtesy Alexia L. McKnight, University of Pennsylvania, Philadelphia, Pennsylvania, United States.)
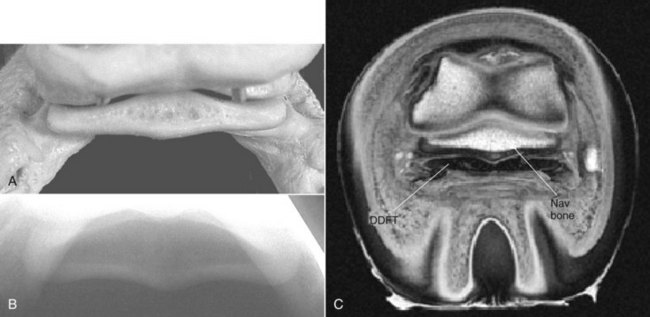
Fig. 9-14 Transverse sections through the navicular bone. A, Anatomical specimen, palmar view. B, Palmaroproximal-palmarodistal oblique radiographic image of a normal navicular bone. C, Transverse magnetic resonance image. The deep digital flexor tendon (DDFT) is nearly as broad at this point as the navicular bone.
(Courtesy Alexia L. McKnight, University of Pennsylvania, Philadelphia, Pennsylvania, United States.)
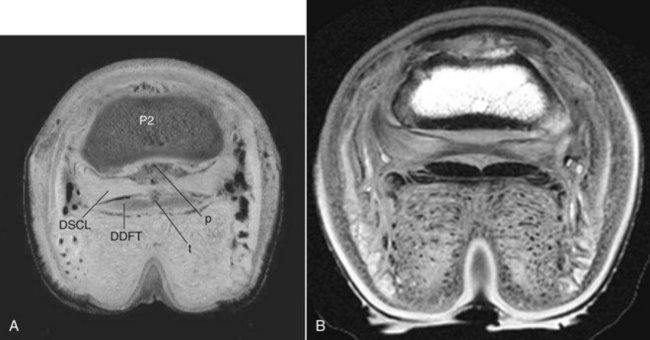
Fig. 9-15 Transverse sections through the foot at the level of the distal sesamoidean collateral ligaments (DSCL). A, Anatomical section showing the attachments of the DSCL to the deep digital flexor tendon (DDFT) marked at point t, and to the middle phalanx (P2) at point p. These attachments form the so-called “T ligament,” which forms the boundaries between the navicular bursa, distal interphalangeal joint, and digital flexor tendon sheath. B, Corresponding magnetic resonance image.
(Courtesy Alexia L. McKnight, University of Pennsylvania, Philadelphia, Pennsylvania, United States.)
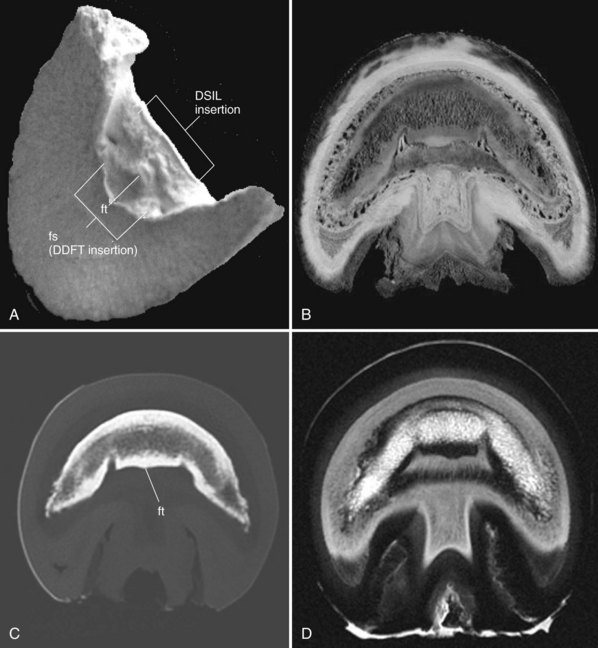
Fig. 9-16 The insertions of the deep digital flexor tendon (DDFT) and distal sesamoidean impar ligament (DSIL). A, Isolated distal phalanx solar view, showing the point of insertion of the DDFT on the flexor surface (fs). The flexor tubercle (see ft in panel C) is relatively smaller than in other species but should be recognized as a normal structure as seen on computed tomographic (CT) imaging. B, Transverse anatomical section through the insertion of the DDFT. This slice is slightly distal to the site of insertion of the distal sesamoidean impar ligament. C, Transverse CT image showing a normal flexor tubercle (ft). Avulsions here are difficult to demonstrate radiologically. Nuclear scintigraphy and ultrasonography can be helpful, but this area is best imaged using CT or magnetic resonance imaging (MRI). D, Transverse MRI scan.
(D courtesy Alexia L. McKnight, University of Pennsylvania, Philadelphia, Pennsylvania, United States.)
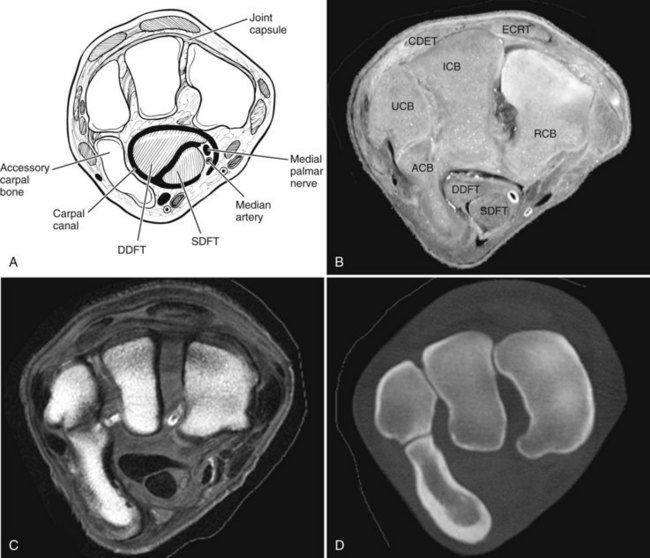
Fig. 9-17 Transverse slices through the proximal row of carpal bones. All images are oriented with dorsal to the top and lateral to the left. A, Diagram of carpal bones. B, Anatomical section. C, Magnetic resonance imaging image. D, Computed tomographic image. ACB, Accessory carpal bone; CDET, common digital extensor tendon; DDFT, deep digital flexor tendon; ECRT, extensor carpi radialis tendon; ICB intermediate carpal bone; RCB, radial carpal bone; SDFT, superficial digital flexor tendon; UCB, ulnar carpal bone.
(C Courtesy Alexia L McKnight, University of Pennsylvania, Philadelphia, Pennsylvania, United States.)
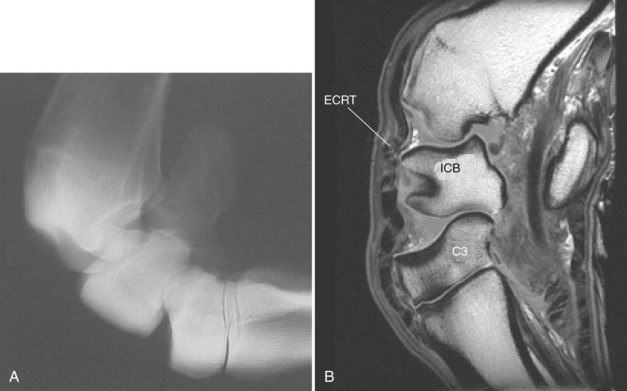
Fig. 9-18 Lateral views of the carpus. Compare with Figure 9-1. A, Flexed lateromedial radiographic image. B, Flexed sagittal magnetic resonance imaging image through the extensor carpi radialis tendon (ECRT). C3, Third carpal bone; ICB, intermediate carpal bone.
(Courtesy Alexia L McKnight, University of Pennsylvania, Philadelphia, Pennsylvania, United States.)