Chapter 38The Carpus
Anatomy
The carpus consists of the antebrachiocarpal, middle carpal, and carpometacarpal joints. The antebrachiocarpal and middle carpal joints are considered ginglymi, but they are not typical of hinge joints; the carpometacarpal joint is arthrodial.1 Arthrodial joints also exist between carpal bones in each respective row. Effective movement of the carpus originates from the antebrachiocarpal and middle carpal joints. The carpometacarpal joint does not open, but it is subject to shear stress. The antebrachiocarpal joint lies between the distal aspect of the radius and the proximal row of carpal bones. The distal, dorsal aspect of the radius has deep grooves in which run the tendons of the extensor carpi radialis and common digital extensor muscles. In flexion the tendons compress the dorsal aspect of the antebrachiocarpal joint, limiting visibility when arthroscopic examination is performed. The proximal row of carpal bones includes the accessory carpal bone, which articulates with the distal aspect of the radius and the ulnar carpal bone. The accessory carpal bone forms the lateral border of the carpal canal. From lateral to medial, the ulnar carpal, the intermediate carpal, and the radial carpal bones complete the proximal row.
The middle carpal joint lies between the proximal and distal rows of carpal bones. The number of bones in the distal row varies but always includes, from medial to lateral, the second, third, and fourth carpal bones. A first carpal bone is present unilaterally or bilaterally in approximately 50% of horses1 and should not be mistaken on radiographs for an osteochondral fragment. The first carpal bone articulates with the second metacarpal bone (McII) and the second carpal bone, and its presence is often associated with radiolucent areas in the McII. A fifth carpal bone is rare, but if present is small, articulates with the fourth carpal bone and the proximal aspect of the fourth metacarpal bone (McIV), and can be confused with an osteochondral fragment. The second, third, and fourth carpal bones articulate with the McII, the third metacarpal bone (McIII), and the McIV, respectively. The articulation of the second carpal bone and the McII is broader than is that of the fourth carpal bone and the McIV, and hence the McII receives greater load, an important fact to consider with fractures of the McII and the McIV. The third carpal bone, the largest bone in the distal row, has two fossae separated by a distinct ridge, the intermediate (lateral) and radial (medial). The radial fossa is largest, receives greater load, and is more commonly injured. The third carpal bone is L shaped and has a large, dense palmar portion that is rarely injured.
The carpal bones are held together by intercarpal ligaments including the dense palmar carpal ligament from which the accessory ligament of the deep digital flexor tendon arises. The strong intercarpal ligaments play a major role in stability, and the palmar intercarpal ligaments have been shown to provide more resistance to extension of the carpus than does the palmar carpal ligament.2 When large medial and lateral corner osteochondral fragments of the third carpal bone are removed, the intercarpal ligaments and capsular attachments must be incised. These dense attachments provide stability, which can be advantageous when slab fractures are repaired. The dorsomedial intercarpal ligament courses between the medial aspect of the second carpal bone and the dorsomedial aspect of the radial carpal bone,3 but during arthroscopic examination it appears to blend with the joint capsule. A theory was proposed that the dorsomedial intercarpal ligament became hypertrophied and impinged on the articular surface of the radial carpal bone, causing secondary modeling in young racehorses and lameness.4 Recent studies of normal carpi found that the dorsomedial intercarpal ligament was neither hypertrophied nor impinging on the radial carpal bone. A definite relationship exists between the development of pathological conditions on the distal aspect of the radial carpal bone and the attachment of the dorsomedial intercarpal ligament, but I have not observed hypertrophy or impingement. The majority of radial carpal bone osteochondral fragments occur within or just lateral to the attachment site of the dorsomedial intercarpal ligament. Because the dorsomedial intercarpal ligament resists dorsomedial displacement of the radial carpal bone,3 this site is prone to develop osteochondral fragments. In abnormal carpi, hypertrophy of the dorsomedial intercarpal ligament has been found to be apparent, but no correlation existed between hypertrophy and cartilage or subchondral bone damage.5
The medial and lateral palmar intercarpal ligaments resist displacement and dissipate axial forces by allowing abaxial translation of carpal bones.6,7 The long and short medial and lateral collateral ligaments originate on the radius and attach to the proximal aspects of the McII and the McIV, and the abaxial surface of the carpal bones, respectively. The collateral ligaments provided the major resistance to dorsal displacement of the proximal row of carpal bones during experimental loading, but the small but important palmar intercarpal ligaments contributed 23% resistance.2 The lateral palmar intercarpal ligament mostly attaches proximally on the ulnar carpal bone and distally on the third carpal bone and may be divided,3 findings different from those previously reported—that the distal attachment was mostly on the fourth carpal bone.8 The medial palmar intercarpal ligament has four bundles that vary in size, and it courses between the radial carpal bone proximally and the palmaromedial surface of the third carpal bone and palmarolateral surface of the second carpal bone distally.3 Tearing of the medial palmar intercarpal ligament and to a lesser extent the lateral palmar intercarpal ligament was observed in horses with carpal disease and was recently proposed to be associated with cartilage and subchondral bone damage (see the following discussion).8,9
The carpus has a dense joint capsule dorsally that blends with the overlying fascia and retinaculum. Synovium in young horses is often thickened or folded dorsally in the middle carpal joint and can interfere with visibility during arthroscopic surgery. This fold appears to smooth as horses age or as osteoarthritis develops. The antebrachial fascia blends with the retinaculum that functions to restrain extensor tendons. Retinaculum thickens and forms the medial and palmar borders of the carpal canal. The palmar retinaculum is sometimes severed in horses with carpal tenosynovitis and tendonitis (see Chapter 75). Anatomical considerations and flexor and extensor tendon injuries are discussed elsewhere (see Chapters 69 and 77). The sheathed extensor carpi radialis and common digital extensor tendons, located dorsally and dorsolaterally, respectively, limit carpal palpation and restrict access. Cul-de-sacs of distended antebrachiocarpal and middle carpal joint capsules can be palpated medial to the extensor carpi radialis tendon or between the extensor carpi radialis and common digital extensor tendons in a standing horse. Arthrocentesis and arthroscopic examination require careful placement of needles and instruments in these portals to avoid injury to tendons and sheaths. These portals can be easily felt as distinct depressions when the carpus is flexed. The sheathed lateral digital extensor tendon, located on the lateral aspect, should be avoided during arthrocentesis of the palmarolateral pouches. The sheathed extensor carpi obliquus tendon is small and passes obliquely over the antebrachiocarpal joint from lateral to medial to attach to the McII. This tendon can readily be seen medially during arthroscopic examination of the antebrachiocarpal joint. Extensor tenosynovitis must be differentiated from middle carpal and antebrachiocarpal joint effusion and hygroma. The antebrachiocarpal and middle carpal joints each have a palmarolateral and a palmaromedial outpouching through which arthrocentesis and arthroscopic evaluation can be performed. Unless greatly distended, the palmarolateral outpouchings are larger than the corresponding palmaromedial outpouchings. The palmarolateral outpouching of the antebrachiocarpal joint is in close proximity to the carpal sheath, and inadvertent penetration of the carpal sheath can occur during arthrocentesis or arthroscopic examination even when the palmarolateral outpouching is distended.
Knowledge of the communications and boundaries of the carpal joints is important in understanding the extent of disease processes and the results of diagnostic analgesia (see Chapter 10). The antebrachiocarpal joint is considered solitary, although in a single specimen in a cadaver study the joint communicated with the middle carpal and carpometacarpal joints.10 In some horses a communication appears between the antebrachiocarpal joint and the carpal sheath. The middle carpal and carpometacarpal joints always communicate (see Figure 10-8Figure 10-9Figure 10-10). Communication between the middle carpal and carpometacarpal joints and the carpal sheath is rare. The carpometacarpal joint has distinct distopalmar outpouchings located axial to the McII and the McIV that have secondary pouches interdigitating within the proximal aspect of the suspensory ligament (SL). These outpouchings explain inadvertent analgesia of the carpometacarpal and middle carpal joint while performing high palmar analgesia and possibly why lameness abates during middle carpal analgesia in horses with avulsion fractures of the proximopalmar aspect of the McIII or proximal suspensory desmitis.11
Conformation
Racehorses, especially Thoroughbreds (TBs), with offset-knee (bench-knee) and back-at-the-knee (calf-knee) conformation are predisposed to develop carpal lameness. Mild in-at-the-knee (carpus valgus) deformity is common and of little concern, but if the deformity is severe, it can predispose to carpal lameness similar to that in horses with out-at-the-knee (carpus varus) conformation (see Chapter 4).
Clinical Characteristics and Diagnosis of Carpal Lameness
Carpal lameness is a common finding in many sports horses, but it is most common in racehorses. Former racehorses used in other disciplines may have chronic osteoarthritis (OA) or recurrence of osteochondral fragmentation. Primary carpal lameness in nonracehorses occurs from trauma such as from falls, kick wounds, and hitting fences; hyperextension injury resulting in fractures of the accessory carpal bone; and occasionally primary OA. Old horses, in particular Arabian horses, appear prone to develop inexplicable chronic, often severe OA of the carpometacarpal joint. Palmar carpal injury occurs in horses that fall or during recovery from general anesthesia and can result in moderate to severe lameness and subsequent OA. Palmar carpal injury most commonly involves the antebrachiocarpal joint, and clinical signs may not develop until hours or a few days after recovery from general anesthesia. Injury may result from trauma when the affected carpus is hyperextended or flexed and usually occurs in horses during rough recoveries but can occur, inexplicably, in horses with seemingly uneventful recoveries.
Few historical facts are pathognomonic for carpal lameness unless severe swelling and lameness develop acutely or a trauma is observed. TB racehorses may lug (bear) in, lug out, or fail to change leads. A Standardbred (STB) racehorse may be on a line. Horses may be racing poorly, particularly those with bilaterally symmetrical lameness. In racehorses with right forelimb carpal lameness, signs may be worse on the turns. Although most STBs are on the ipsilateral line, rarely a horse with right forelimb carpal lameness will be on the left line, presumably because the horse is bearing away from medially located pain or has a shortened stride in the right forelimb. Nonracehorses may have poor performance, fail to change leads, and hit or refuse fences. They may be uncomfortable when studs are placed in or removed from the shoes. Ponies with antebrachiocarpal joint pain may start to stumble.
Degree of lameness varies with the type and severity of carpal injury. Horses with early or mild chronic OA have mild lameness, whereas those with acute osteochondral fragments, slab fractures, or other more serious injuries have more severe lameness. Horses with infectious arthritis and comminuted carpal or other severe fractures may not bear weight at the walk. Dynamic angular deformity, carpus valgus or varus, may be seen in horses attempting to bear weight with comminuted fractures and loss of joint integrity. Lameness may be intermittent in horses with early and incomplete osteochondral fragments and may be apparent only after training or racing. Racehorses with bilaterally symmetrical lameness may not show overt lameness but have a wide, short gait bilaterally. Advancing and placing the affected limb wide while walking or trotting (pacing) is typical of carpal lameness (see Chapter 7). ![]() Horses with severe OA and natural carpal ankylosis or surgical arthrodesis swing (abduct) the limb because the carpus cannot flex. Advancement and placement of the limb in a lateral (abducted) position is not pathognomonic for carpal lameness, and horses with proximal palmar metacarpal pain or those with pain originating laterally in the digit may manifest similar signs. However, carpal tenosynovitis does not result in this typical carpal gait. Horses with carpal lameness have a shortened cranial phase of the stride. Lameness can be worse with the limb on the inside or outside of the circle depending on whether the location of pain is medial or lateral, but, in general, lameness in most horses with carpal lameness is worse with the limb on the outside of the circle.
Horses with severe OA and natural carpal ankylosis or surgical arthrodesis swing (abduct) the limb because the carpus cannot flex. Advancement and placement of the limb in a lateral (abducted) position is not pathognomonic for carpal lameness, and horses with proximal palmar metacarpal pain or those with pain originating laterally in the digit may manifest similar signs. However, carpal tenosynovitis does not result in this typical carpal gait. Horses with carpal lameness have a shortened cranial phase of the stride. Lameness can be worse with the limb on the inside or outside of the circle depending on whether the location of pain is medial or lateral, but, in general, lameness in most horses with carpal lameness is worse with the limb on the outside of the circle.
Increased temperature (heat) over the dorsal surface of the carpus is a reliable indicator of carpal disease, but false positive and negative findings occur. If horses have been clipped for painting or blistering, or effects of topical counterirritation are still present, the area can be warm and sensitive without carpal lameness. The dorsal surface of each carpus should be evaluated and compared, but differences are difficult to detect if lameness is bilateral. Effusion is usually a reliable indicator for carpal synovitis, but it is not pathognomonic for carpal lameness. Horses with subchondral bone injury without overlying cartilage damage or incomplete osteochondral fragments often have carpal lameness without effusion. Effusion is suppressed in horses that have recently had corticosteroid injections. Effusion occurs commonly in young horses with early carpitis and in horses with advanced cartilage damage, osteochondral fragments, and infectious arthritis. Swelling associated with distention of the antebrachiocarpal or middle carpal joints is orientated horizontally on the dorsal aspect of the carpus, whereas effusion in a tendon sheath results in a longitudinally orientated swelling, compressed at intervals by horizontally orientated retinacular bands. With the horse’s limb in a weight-bearing position, the clinician’s fingers are used to ballot fluid within a distended carpal joint capsule. Capsular swellings are located between extensor tendons and medial to the tendon of the extensor carpi radialis. Older horses with chronic carpal changes often have mild or moderate effusion but can perform satisfactorily. In some horses there may be focal dorsal herniation of the antebrachiocarpal or middle carpal joint capsules.
Horses with acute carpal lameness, especially those with synovitis, often show a marked response to static flexion of the carpus. Horses with carpal tenosynovitis or other palmar carpal lameness also respond. Horses with pain from the proximal aspect of the limb, such as myositis in the proximal aspect of the antebrachium or elbow region pain, respond to carpal flexion (false-positive response). Static and dynamic flexion can be negative in horses with carpal lameness, especially in those with subchondral bone pain. Degree of flexion is usually decreased in horses with chronic OA because of joint capsule fibrosis. Careful palpation of all bony and soft tissue structures of the carpal region should be performed with the limb in standing and flexed positions, and responses should be compared with the contralateral limb. Swellings are best felt with the horse’s limb in a standing position. Swellings of nearby sheaths should be differentiated from authentic carpal effusion by location and ballottement. Horses with chronic OA often have firm, fibrous thickening at joint capsule attachments. Dorsomedial bony swelling of the radial and third carpal bones is observed and palpated in horses with chronic severe OA. The proximal aspect of the McII and the McIV should be palpated for bony and soft tissue swelling associated with fracture or exostoses. The proximal palmar metacarpal region should be palpated with the horse in the standing and flexed positions to differentiate pain in this region from carpal pain. The superficial digital flexor tendon should be carefully palpated to detect enlargement and pain, because horses with proximal superficial digital flexor tendonitis often manifest a positive response to carpal flexion. However, swelling of the superficial digital flexor tendon is easily overlooked because of compression by the extensive palmar retinaculum.
In my experience, the carpal flexion test is the most specific of any flexion test used, and if the test result is positive, carpal region pain is highly probable. A positive test result does not always incriminate the carpal joints, and the surrounding soft tissue structures must be kept in mind. A negative test result does not rule out carpal pain. Horses with subchondral bone pain, usually young racehorses with sclerosis of the third carpal bone, often have a negative or equivocal response to flexion. Horses with palmar metacarpal or elbow pain can respond positively.
Diagnostic Analgesia
In many horses, clinical signs and characteristic gait may allow a tentative diagnosis of carpal lameness, but in most horses diagnostic analgesia should be performed. Analgesia of the middle carpal and antebrachiocarpal joints should be performed independently and sequentially. Dorsal intraarticular techniques are most common, but in horses with scurf from previous counterirritant application or dorsal wounds, the palmarolateral pouches are used. Careful selective perineural and intraarticular analgesic techniques should be performed to differentiate between proximal palmar metacarpal pain and authentic carpal pain (see Chapter 10). Intraarticular analgesic techniques are highly specific, but false-negative results may occur.12 False-positive results may also result because of abolition of carpal sheath pain or proximal palmar metacarpal region pain. Subchondral bone pain may not always be eliminated by intrasynovial deposition of local anesthetic solution, because nerve fibers may be located in bone or travel to the site by another extrasynovial route. The median and ulnar nerve block, although lacking specificity, is useful in horses with suspected carpal region pain that is not abolished by intraarticular techniques.
Laboratory analysis of synovial fluid is reserved for horses in which acute inflammation or infectious arthritis is suspected, but color and viscosity should be evaluated, and abnormalities may help to convince an owner or trainer of a carpal problem. In a normal flexed carpus, fluid does not readily drain from a small-gauge needle, and compression of the joint capsule at a distant site is usually necessary. Horses with effusion have thin synovial fluid that drips spontaneously without compression of the nearby capsule. Horses with true serosanguineous fluid (as opposed to contamination by penetration of capsular or synovial vessels) likely have cartilage damage with exposed subchondral bone or an osteochondral fragment. Hemarthrosis can be caused by trauma or bleeding from a torn intercarpal ligament.
Imaging
Radiography
A minimum of six well-exposed and positioned radiographic images are necessary for comprehensive examination of the carpus, including the dorsopalmar (DPa), lateromedial (LM), dorsal 45° lateral-palmaromedial oblique (DL-PaMO), dorsal 45° medial-palmarolateral oblique (DM-PaLO), and flexed LM images and the dorsoproximal-dorsodistal (tangential, skyline) image of the distal row of carpal bones. The skyline image is most important for assessing subtle radiological changes of the third carpal bone, but well-positioned images are often difficult to obtain. Evaluation of the radial fossa requires flexion of the limb in the sagittal plane with the metacarpal region beneath the antebrachium (Figure 38-1). Lateral positioning of the distal part of the limb results in overlap of the radial fossa of the third carpal bone and the radial carpal bone. The skyline image underestimates the amount of increased radiopacity of the third carpal bone and magnifies normal anatomy and lesions approximately twofold.13 The skyline image is not a true proximal-to-distal view of the second, third, and fourth carpal bones, and therefore lesions located palmar to the dorsal edge of the radial carpal bone cannot be seen. The skyline image cannot be used to evaluate fracture lines located more than 8 to 10 mm from the dorsal edge of the third carpal bone or to differentiate large osteochondral fragments from frontal slab fractures of the third carpal bone. Additional images, such as the tangential image of the proximal row of carpal bones (used to identify osteochondral fragments and unusually located frontal or sagittal slab fractures), flexed oblique images (e.g., DL-PaMO view with the limb held in flexion for evaluation of the articular surfaces of the third and radial carpal bones), and weight-bearing, oblique images of different obliquity (e.g., off DPa views, used to identify sagittal slab fractures of the third carpal bone) are sometimes useful. Considerable confusion arises in description of oblique images, with the use of terms lateral and medial oblique instead of naming the images according to the direction of the x-ray beam. To most clinicians, the lateral oblique is equivalent to a DL-PaMO image, but to others it is just the opposite. Follow-up radiographic examination is recommended in 10 to 14 days if fracture is suspected but initial radiological findings are negative or equivocal.
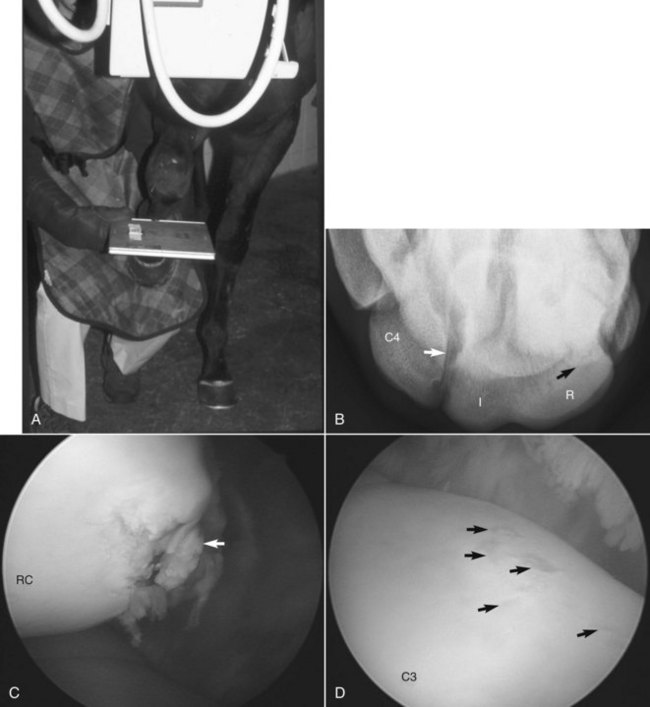
Fig. 38-1 A, A well-positioned dorsoproximal-dorsodistal (skyline) radiographic image of the distal row of carpal bones requires that the third metacarpal bone be aligned directly under the radius. This makes the radial fossa visible. B, Resulting digital radiographic image shows radial (R) and intermediate (I) fossae of the third carpal bone (C3) (medial is to the right and palmar is uppermost). There is dense increased radiopacity of the radial fossa. Sometimes overlap of the normal articulation between the third and fourth (C4) carpal bones appears as a linear radiolucent defect (white arrow) in the lateral aspect of C3, a finding confused with sagittal fracture of that bone. Often when digital radiographic techniques are used, fracture lines not visible on conventional radiographs can be seen, such as in this 3-year-old Thoroughbred colt with a small osteochondral fragment of the radial carpal bone (black arrow). The fracture fragment is superimposed on C3 but can readily be seen. C, Intraoperative arthroscopic photograph showing the chip fracture (arrow) and surrounding cartilage damage on the radial carpal bone (RC) in this horse. D, Intraoperative arthroscopic photograph showing thin articular cartilage and partial-thickness cartilaginous defects on C3 (arrows) that accompany sclerotic subchondral bone.
Normal radiological anatomy of the carpus is difficult because carpal bones overlap considerably, bones shift during flexion, and normal radiolucent defects and aberrant carpal bones can be difficult to interpret. In the skyline image of the distal row, the normal articulation between the third and fourth carpal bones can be superimposed on the lateral aspect of the third carpal bone and confused with a sagittal fracture (see Figure 38-1, B). On a DM-PaLO image the normal articulation between the second and third carpal bones should not be confused with a sagittal slab fracture, but this image is essential to diagnose sagittal fracture of the third carpal bone correctly, which runs parallel to this articulation. Radiolucent defects or osseous cystlike lesions are often seen in the ulnar carpal bone and are considered incidental findings, but when they appear in other bones, they can cause lameness regardless of whether communication with a joint exists. In LM and oblique images, the first and fifth carpal bones can be confused with osteochondral fragments. Radiolucent defects in the McII and the McIV often occur in the presence of the first (see Figure 37-7) and fifth (Figure 38-2) carpal bones but are normal. In a flexed LM image the radial carpal bone moves distally relative to the intermediate carpal bone. This normal finding is quite useful in determining the exact positioning of osteochondral fragments or other lesions on the proximal or distal surfaces of the radial and intermediate carpal bones. The flexed LM image is also highly useful for evaluation of the distal dorsal articular surface and subchondral bone of the radial carpal bone. Xeroradiography has largely been discontinued, but computed radiography and digital radiography are available at most institutions and many private practices and yield images superior to those obtained by conventional radiography, but positioning and exposure must still be optimized. Subtle radiological changes can be readily seen in most digital radiographic images, as can fragments, radiolucent defects, and other changes not previously visible on conventional images (see Figure 38-1). Care must be taken not to confuse normal articulations for fractures.

Fig. 38-2 Dorsal 45° lateral-palmaromedial oblique radiographic image of a left carpus in a 2-year-old Standardbred colt. A fifth carpal bone is present (arrow). Note the lucent area in the proximal aspect of the fourth metacarpal bone. Fifth and first carpal bones should not be confused with osteochondral fragments.
Computed tomography (CT) is available at some institutions and private referral hospitals and can be of value to determine fracture configuration and the presence of comminution, such as that demonstrated in a recent report of an Arabian filly with carpal instability, in which comminution that was not seen when digital radiography was used was confirmed with CT.14 Magnetic resonance imaging (MRI) has potential to be useful in the diagnosis of carpal region soft tissue and bony injuries but may have limited value because it is currently difficult to position a horse within some magnets to comprehensively evaluate the entire carpal region. Through use of ex vivo MRI, minor cartilage lesions and sclerotic subchondral bone have readily been seen in intact cadaveric specimens.15 Magnetic resonance (MR) contrast arthrography has been compared with arthroscopy and gross necropsy examination to evaluate and define the lateral palmar outpouching of the middle carpal joint.16 All structures of the palmarolateral outpouching including portions of the lateral collateral and lateral palmar intercarpal ligaments were visible in MR images, and information obtained compared favorably with arthroscopic examination performed after synovectomy using a motorized intraarticular blade.16 Ultrasonographic examination of the carpus can be useful to determine the extent of soft tissue damage, to determine if wounds or fistulous tracts communicate with carpal joints, and to diagnose extensor and digital flexor tendon injury, carpal tenosynovitis, and desmitis. Using ultrasonographic examination, the body and division into medial and lateral branches of the medial palmar intercarpal ligament could be seen from a dorsal approach, and the technique may be useful to image horses suspected of having injury of the ligament.17
Scintigraphy
Scintigraphy is especially useful to diagnose early stress-related subchondral bone injury and differentiate carpal lesions from those of the proximal metacarpal region (see Figure 19-19). A common finding in young racehorses is carpal lameness localized by clinical signs and diagnostic analgesia with negative or equivocal radiological abnormalities. Focal areas of increased radiopharmaceutical uptake (IRU) are often found unilaterally or bilaterally, most commonly in the third carpal bone (see Figure 19-16). Scintigraphy can be used to verify or refute the importance of sclerosis in the third carpal bone. Scintigraphy is useful in diagnosing unusual fractures of the palmar aspect of the third carpal bone, corner fractures or table surface collapse of the third carpal bone or other carpal bones, and lesions that are not apparent or are located in obscure areas not depicted radiologically. Focal areas of IRU occur with many carpal injuries, and although sensitivity is high, the specificity of scintigraphic images is low and differentiation of specific types of injuries is difficult. Scintigraphy is most useful in localizing the site of injury, based on which additional radiographic images are obtained, or rest is recommended, followed by repeated radiographic examination.
In general, scintigraphic examination is used when lameness is localized but a specific diagnosis cannot be made. In racehorses referred for evaluation of poor performance and obscure high-speed lameness, comprehensive scintigraphic examination of all limbs often reveals focal areas of IRU in the carpus, even when evidence of overt lameness is lacking. Areas of IRU are in locations typical for horses to develop osteochondral fragments and signs of OA. Whether these areas of IRU represent sources of pain causing high-speed or subtle lameness is unknown, but often radiological evidence of bone modeling (increased radiopacity, marginal osteophytes) or incomplete osteochondral fragments exists. Treadmill exercise of previously untrained horses has resulted in a significant IRU,18 a finding indicating scintigraphy can be useful to monitor skeletal response to exercise in normal horses. Mild IRU is seen as an adaptive response to bone modeling associated with exercise. In contrast, earlier work in normal horses showed exercise significantly increased subchondral bone density and uptake of radiopharmaceutical in the McIII condyles, but neither parameter increased significantly in carpal bones.19 More recently, in horses undergoing exercise after experimentally induced OA of the middle carpal joint, scintigraphic changes (IRU) were significantly correlated with lameness and increased beyond the normal adaptive response seen in association with exercise.20
Diagnostic Arthroscopy
Specific diagnosis is usually made before surgery, and in most racehorses arthroscopy is interventional rather than diagnostic. When results of thorough clinical, radiographic, and scintigraphic examinations are combined, a specific site of injury is usually identified. In racehorses, lameness of the carpus without scintigraphic or radiological abnormalities is unusual. Lack of subchondral bone involvement leads the veterinarian to suspect soft tissue diseases such as synovitis and intercarpal ligament tearing. In these horses, careful examination of the proximal palmar metacarpal region and carpal canal should be performed to avoid inadvertent misdiagnosis. Arthroscopic examination then is used to eliminate primary cartilage damage or intercarpal ligament tearing, but often arthroscopic findings can be unrewarding. Without overt cartilage damage the prognosis is favorable, so information gained by arthroscopic examination is useful, even if a primary diagnosis cannot be made. In sports horses the frequency of carpal joint injury is less than in racehorses but arthroscopy has proved invaluable for identification of focal full-thickness cartilage defects in the middle carpal joint and palmar intercarpal ligament injury. Recently, arthroscopic approaches to the palmarolateral and palmaromedial outpouchings of the antebrachiocarpal and middle carpal joints were refined, and it was proposed that approaches to these pouches would be useful to remove fracture fragments and to evaluate palmar intercarpal ligaments.21 I have used approaches to these joints to remove fragments from both the antebrachiocarpal and middle carpal joints, the results of which are discussed subsequently.
In horses with scintigraphic evidence of IRU and those with OA but without radiological confirmation of osteochondral fragmentation, arthroscopic examination usually reveals cartilage damage, the extent of which can be graded. Prognosis is inversely related to degree of cartilage damage (see Figures 23-7 and 38-1). Occult osteochondral fragments, most commonly involving the third and radial carpal bones, and intercarpal ligament tearing are found frequently in these horses (see Figure 23-4).
Specific Conditions of the Carpus
Osteoarthritis
OA is the most common carpal problem, but clear differentiation of OA from osteochondral fragmentation is difficult, because both problems are intertwined. Horses with osteochondral fragments often develop OA, and horses with early OA, and some with chronic OA, develop osteochondral fragments. Pathogenesis of OA and osteochondral fragmentation appears similar if not identical in some horses, but OA of the equine carpus has two forms. The most common form is seen in racehorses or ex-racehorses that initially develop stress-related subchondral bone injury of the middle carpal and antebrachiocarpal joints that leads to, or accompanies, overlying cartilage damage and osteochondral fragmentation (see Figure 38-1). A second form of OA develops in nonracehorses and is less common. Horses are usually middle aged or older, but occasionally it occurs in younger horses. Typical clinical and radiological evidence of OA exists, but osteochondral fragments are unusual (see Chapters 61 and 84).
OA in racehorses develops from a continuum of stress-related subchondral bone injury and cartilage damage, resulting from impact loading of the carpal bones during training and racing. This process has been studied most thoroughly in the third carpal bone but also occurs in other bones of the middle carpal and antebrachiocarpal joints. Sclerosis of the dorsal aspect of the third carpal bone is an adaptive response in racehorses.23,24 With continued loading the third carpal bone becomes densely sclerotic, and in this stage the response becomes maladaptive or nonadaptive and pathological. Subchondral changes precede those in overlying cartilage, a finding seen experimentally25 and clinically during arthroscopic examination in horses with primary stress-related subchondral bone injury (see Figure 38-1). Sclerotic subchondral bone may induce overlying cartilage damage from abnormal shear forces existing between normal and sclerotic areas.26 In most horses sclerosis leads to areas of resorption and necrosis, which then lead to osteochondral fragmentation and eventually to more advanced OA.6,23,27,28 A possible explanation for bone failure is the lack of support of overlying sclerotic subchondral bone by structurally weakened underlying trabecular bone.29 When carpal bone morphology and metabolism were studied in TB racehorses and unraced controls, racehorses were found to have a net increase in bone formation, leading to stiffer, sclerotic subchondral bone; but in addition, they had increased bone collagen synthesis and remodeling in adjacent trabecular bone that may have been structurally weakened.29 Because many of the changes in early OA in racehorses are mechanically induced, factors such as faulty conformation, intense exercise programs, and differences between racing breeds alter the rate of development and severity of OA. The pathological process continues, and some horses develop OA without osteochondral fragments, whereas others develop osteochondral fragments initially and then OA secondarily.
In many racehorses extensive OA and osteochondral fragmentation lead to retirement, but some are able to compete in other sporting events. Progressive OA can then develop later in life. In middle-aged to old nonracehorses, primary OA develops without stress-related subchondral bone injury, high-impact loading, or development of osteochondral fragmentation. This condition can be seen in Western performance horses, other sports horses, or even in horses and ponies used for pleasure riding. Often severe radiological evidence of OA is seen on initial examination when lameness is subtle (Figure 38-3). In fact, it has been proposed that the threshold of pain in riding horses with severe OA of the antebrachiocarpal joint may be higher than in those with similar conditions of the middle carpal joint, because observation of lameness by owners of these horses was a late event.30 Faulty conformation such as carpus valgus, back at the knee, or bench knee is seen in some horses, but in others neither mechanical nor training-related factors are present. OA in these horses can involve the antebrachiocarpal and middle carpal joints together or separately, but when disease involves the carpometacarpal joint, chronic and severe lameness develops (see Figure 3-2).

Fig. 38-3 Lateromedial digital radiographic image of the right carpus of an aged Quarter Horse gelding with advanced osteoarthritis of the antebrachiocarpal joint. Extensive marginal osteophyte formation in both the dorsal (large arrow) and palmar (small arrows) aspects of the joint can be seen. It is often difficult to determine if osteophytes represent osteoarthritic change or are actually small osteochondral fragments, but the close interrelationship of the most common causes of carpal lameness can be seen.
Clinical Signs and Diagnosis
Clinical signs of OA vary depending on age and use of horse, but they are similar to those of other carpal diseases. Classic signs of OA, such as obvious lameness, typical carpal gait, effusion, and a painful response to static and dynamic flexion, may be present, particularly in horses with advanced OA and in old horses with severe changes, but clinical signs can be subtle in young racehorses. In racehorses with early OA, historical information such as lugging in or out, being on a line, or poor performance may be present. Effusion varies, and absence of this clinical sign does not preclude the carpus as the source of pain. Carpal lameness was common in young STB racehorses, occurring in 28% of horses in training, and was attributed to subchondral bone pain and early sclerosis, because in most horses there was little to no effusion of the middle carpal joint.31 Overall, carpal lameness was the most common cause for more than 1 month of rest (wastage) and was thought to be accentuated by speed training and poor forelimb conformation.31 Racehorses in early training are prone to develop effusion primarily of the middle carpal joint, but the antebrachiocarpal joint can also be involved. Effusion may be most evident after work, but lameness usually is not present. Effusion usually results from strain of soft tissues, such as intercarpal ligaments or the joint capsule, but in horses with more advanced OA, effusion represents inflammation caused by continued cartilage damage. Clinical signs resolve after a brief period of rest or reduction in training. Most commonly, racehorses with early OA manifest clinical signs later in training as a 2-year-old or when racing begins.
Diagnosis should be confirmed using diagnostic analgesia of the involved joint(s). In horses with severe OA, complete resolution of lameness may not occur until median and ulnar blocks are performed. After pain in the primary limb has been abolished, lameness may be seen in the contralateral limb, indicating bilateral carpal lameness.
Radiological evidence of OA in young horses is often lacking, but increased radiopacity of the third carpal bone may be seen in a skyline image (see discussion of small osteochondral fragmentation). Early radiological changes include mild enthesophyte formation, most common on the radial carpal bone, and subtle marginal osteophytes on the carpal bones and distal radius. In horses with advanced OA, marginal osteophytes and enthesophytes become numerous and large, sometimes causing obvious visible bony swelling (see Figure 38-3). Loss of joint space occurs late in OA, but it is not an obvious radiological sign. Osteochondral fragments may be present, can be numerous, and may have occurred earlier during a racing career or can develop when marginal osteophytes break. Radiological evaluation of the contralateral carpus should be performed.
Scintigraphic examination is an excellent tool for diagnosis of early OA in racehorses, but IRU must be differentiated from mild normal adaptive increased uptake of radiopharmaceutical.18-20,31 Initially, focal areas of IRU are located on one side of a joint, such as in the third carpal bone, but later, subchondral IRU can be seen diffusely in one or more joints. Arthroscopic examination may be useful to establish prognosis and to evaluate possible soft tissue injury, such as intercarpal ligament tearing, and may be useful therapeutically.
Management
Management of OA is discussed in Chapter 84. Because pathogenesis involves stress-related subchondral bone injury, an important part of management of OA in racehorses involves stress relief by enforced rest or a reduction in training or racing intensity. Racehorses (STBs) without obvious radiological changes are given 2 to 3 weeks of hand walking or walking in the jog cart, nonsteroidal antiinflammatory drugs (NSAIDs), and local therapy such as cold water hosing or icing. Topical counterirritation is still a popular management technique administered to young racehorses early in training. Intraarticular administration of hyaluronan, with or without a short-acting corticosteroid, may help in horses with synovitis, but it is of limited value if the primary source of pain is subchondral bone with intact overlying cartilage. In racehorses with advanced sclerosis of the third carpal bone and early enthesophyte and marginal osteophyte formation, extended rest of 3 to 4 months is recommended. However, economic factors may dictate that these horses remain in training; thus work intensity often is decreased and horses receive a single or a series of intraarticular injections with hyaluronan or polysulfated glycosaminoglycans (PSGAGs). Horses with radiologically apparent osteochondral fragments are surgical candidates, but postoperative progression of OA and recurrence of fragmentation are common. As OA progresses in horses with or without osteochondral fragments, numerous intraarticular injections, often including methylprednisolone acetate, may be necessary to reduce inflammation, but if training and racing continue, OA progresses in an accelerated fashion. Bisphosphonate administration in combination with a modification in exercise or rest may have a beneficial effect, but more clinical study is necessary.
A syndrome has been recognized in ponies with OA of the antebrachiocarpal joint. These ponies are presented for examination because of repetitive stumbling when ridden. There is generally resentment of carpal flexion and restricted flexion, although no obvious lameness. Although the response to intraarticular analgesia may be disappointing, the response to intraarticular medication is often good. Although historically sclerosis of the third carpal bone has been considered a disease of the racehorse, it has also been recognized as a cause of intermittent lameness in both endurance horses and event horses. Focal areas of full thickness cartilage loss in the medial aspect of the middle carpal joint have been identified arthroscopically in a small number of show jumpers that had no localizing clinical signs, lameness that was improved by intraarticular analgesia, and no detectable radiological abnormality. Some sports horses with carpal OA show lameness only when ridden and not under other circumstances. In ex-racehorses or nonracehorse sports horses with primary OA, radiological changes may be advanced when lameness is first recognized, because OA is chronic and well tolerated. Conservative management is recommended and includes rest, NSAID therapy, and intraarticular injections. Horses with radiological evidence of large intact or broken osteophytes or old osteochondral fragments may be considered candidates for arthroscopic surgery, but although arthroscopic examination may be important to establish prognosis, surgical removal of osteophytes and old osteochondral fragments does not often result in long-term clinical improvement and may accelerate progression of OA (see Figure 38-3). Involvement of the carpometacarpal joint warrants a guarded prognosis.
Prognosis depends on the number of joints and limbs affected, rate of progression of clinical signs, severity of cartilage damage, presence of osteochondral fragments, and level of competition. Most racehorses with early OA and even those with radiological evidence of osteophytes and enthesophytes can race at some level, if the horses raced before diagnosis. Horses with advanced changes before racing begins, particularly those with faulty conformation, are unlikely to race but can be sound enough to perform other sporting activities. Valuable horses with severe OA, such as broodmares or breeding stallions, may be candidates for partial (intercarpal) or pancarpal arthrodesis.
Trauma to the craniodistal aspect of the radius and dorsal aspect of the carpus may result in the rapid development of periarticular new bone on the distocranial aspect of the radius and the dorsal aspect of the intermediate carpal bone. There is often associated diffuse soft tissue swelling. Lameness may be absent or mild, but there is marked resentment of carpal flexion, and flexion may induce moderate-to-severe lameness. I speculate that this occurs because of pressure mediated by the extensor tendons on this new bone.
Osteoarthritis of the Carpometacarpal Joint
Primary osteoarthritis of the carpometacarpal joint is unusual to rare but occurs primarily in old horses, especially Arabians,32 and is insidious and progressive (see Figure 3-2 and Chapter 37).
Osteochondral Fragmentation
Small Fragments
Osteochondral fragmentation is a disease primarily of racehorses or ex-racehorses, and pathogenesis is identical to that described for OA. I prefer to use the terms carpal osteochondral fragments (osteochondral fragments) and osteochondral fragmentation instead of carpal chip fractures to emphasize the importance of pathogenesis. The term chip fracture implies a single event traumatic injury. Although trauma plays a role, osteochondral fragments are not single-event injuries but are the end result of stress-related subchondral bone injury caused by repetitive loading, initially an adaptive response but later becoming nonadaptive remodeling and pathological.23,25,27,28 Sites located dorsally are prone to develop osteochondral fragments. Osteochondral fragments differ in size and number of joints affected. Small osteochondral fragments are those that involve one joint surface, such as either the middle carpal or the antebrachiocarpal joints. Large osteochondral fragments that involve two joint surfaces are called slab fractures. Often, advanced changes occur in subchondral bone, such as sclerosis of the third carpal bone or other evidence of modeling or remodeling that preceded development of lameness and osteochondral fragments, findings that support the concept that osteochondral fragments are not single-event injuries. The antebrachiocarpal joint is more susceptible to injury from supraphysiological loads or acute overload injury,6 particularly in fatigued horses, but fractures still occur associated with pathological conditions of the bone. Palmar carpal osteochondral fragments, such as those involving the accessory carpal bone or other bones of the antebrachiocarpal joint, occur as single event injuries such as falls, carpal hyperextension, or recovery from general anesthesia. Palmar carpal fragments in the middle carpal joint are often seen in combination with other dorsally located small or large osteochondral fragments (see later).22
In my experience, faulty conformation such as back at the knee predisposes TB and STB racehorses to develop osteochondral fragments, and trotters are more at risk than pacers. However, in a study attempting to evaluate the role of back-at-the-knee conformation in the development of osteochondral fragments in 21 horses, no differences in carpal angle were found compared with 10 horses without osteochondral fragments.33 No association between back-at-the-knee conformation and the development of carpal lameness was found in recent studies in TBs and Quarter Horses (QHs), but elite horses were studied, and those with faulty conformation may have been excluded.34,35 Somewhat surprising, mild carpus valgus conformation was proposed to be protective against carpal lameness, and an association between increased humeral length and carpal lameness was found (see Chapter 4).30
Carpal osteochondral fragments occur in defined locations in all racehorses, but distribution varies depending on the type of racehorse. In the STB, osteochondral fragments occur almost exclusively in the medial aspect of the middle carpal joint and rarely in the antebrachiocarpal joint.36 Although rare, osteochondral fragments in the STB antebrachiocarpal joint are most common in trotters and usually involve the distal aspect of the radius. In the middle carpal joint we found a nearly equal distribution of osteochondral fragments between the radial and third carpal bones, but in another study those of the third carpal bone outnumbered osteochondral fragments of the radial carpal bone by 2 : 1.36,37 The preponderance of osteochondral fragments in the medial aspect of the middle carpal joint in the STB is interesting, because training involves clockwise and counterclockwise exercise, whereas racing is counterclockwise. The assumption is that counterclockwise direction of training and racing places asymmetrical and uneven load distribution on each forelimb and may predispose the lateral aspect of the left forelimb and medial aspect of the right forelimb to compression injury. In two STB studies a nearly equal distribution of osteochondral fragments was noted between left and right middle carpal joints,36,37 but in another study osteochondral fragments of the third carpal bone occurred more commonly in the right carpus.28 Trotters were more likely to have right osteochondral fragments and had significantly more osteochondral fragments of the third carpal bone than the radial carpal bone compared with pacers.28
In TBs in North America, third carpal bone fractures occur more commonly in the right carpus, but considering all small osteochondral fragments, the distribution between left and right is similar.27,28,37 Palmar osteochondral fragments were more common in the right carpus, reflecting the preponderance of TB racehorses in that study and the fact that most fragments originated from co-existent dorsally located small or large osteochondral fragments.22 In TB and QH racehorses, osteochondral fragments are commonly seen in the middle carpal and antebrachiocarpal joints.37-39 These breeds in North America have a predilection for development of osteochondral fragments in the lateral aspect of the left antebrachiocarpal joint and the medial aspect of the right middle carpal joint, a distribution supporting the concept that osteochondral fragments develop on the compression side during counterclockwise training and racing. Overall, in TB and QH racehorses the most common sites for osteochondral fragments are the proximal aspect of the third and distal aspect of the radial carpal bones,22,37,39 followed by the proximal aspect of the intermediate carpal bone and the distal lateral aspect of the radius. Osteochondral fragments often develop on apposing surfaces, supporting the concept that certain sites are biomechanically at risk. This may be evident radiologically, but in some horses apposing fragmentation is identified only at arthroscopic surgery, and both limbs should be examined radiographically routinely, even if clinical signs are absent. Osteochondral fragments can be found at numerous sites in one or both carpi. Differences between racing breeds in distribution of osteochondral fragments may be explained by gait and sites predisposed to stress-related subchondral bone injury. Almost all STB osteochondral fragments occur medially, equally in both middle carpal joints. Most forelimb scintigraphic changes in STBs occur medially, indicating that the medial aspect in both forelimbs is at risk for stress-related subchondral bone injury. Classic training programs include many miles each day of jogging (trotting or pacing) clockwise (the wrong way of the track), and training one to two times each week counterclockwise (the right way). Although all speed is performed in one direction, STBs jog many more miles in the other direction, and the number of loading cycles may be more important than speed. Direction of training and racing is not the only factor influencing fracture location because QHs and TBs have a similar distribution yet race differently. The two-beat trot and pace and a more caudal center of balance with a cart and driver result in reduced carpal loads in STBs at speed compared with galloping racing breeds. The low occurrence of osteochondral fragments in the antebrachiocarpal joint of STBs may reflect absence of supraphysiological loads. Racing speeds in the STB are lower than in the TB and substantially lower than in the QH. Fatigue rather than speed of racing may be a factor.
Clinical Signs
Lameness in horses with small osteochondral fragments varies from subtle to severe. In most horses, prominent-to-severe lameness is seen immediately after the fracture occurs, but subtle prodromal clinical signs are often present. Historically, horses may have been treated for suspected carpal lameness, may be on a line (STB), may lug in or out, or may fail to take a lead or change leads. Degree of lameness depends on location and number of osteochondral fragments and whether osteochondral fragments are present bilaterally. Horses with third carpal bone osteochondral fragments, and in particular incomplete fractures, show more pronounced lameness than those with osteochondral fragments elsewhere. Lameness is increased when the affected limb is on the outside of the circle in horses with osteochondral fragments in the middle carpal joint, but this response varies in those with osteochondral fragments in the antebrachiocarpal joint. TB and QH racehorses with osteochondral fragments of the distal, lateral aspect of the radius or proximal aspect of the intermediate carpal bone may show only mild signs of lameness. I have always thought the antebrachiocarpal joint was more “forgiving” than the middle carpal joint, with horses able to endure more substantial injury or larger osteochondral fragments, without showing overt signs of lameness, an observation shared by others.30 Horses with bilateral osteochondral fragments may show minimal overt lameness. Horses with lameness inappropriately severe for the location, number, or size of fragment(s) present may have substantial cartilage damage.
There is generally effusion and heat over the carpus, but in horses with incomplete fractures, clinical signs can be subtle. Palpation may reveal a focal painful response over the site of fragmentation, and occasionally fragments can be palpated directly. Degree of flexion varies, but usually the response to a carpal flexion test is positive. Signs of OA including joint capsule fibrosis and enthesophyte production are common, particularly in horses with chronic lameness. Arthrocentesis usually reveals serosanguineous fluid, particularly if lameness is acute. Intraarticular analgesia usually, but not always, abolishes signs of pain.
Radiographic examination is usually diagnostic, and all views should be obtained. In STBs abnormalities are usually only detected in DL-PaMO and LM images and a skyline image of the distal row of carpal bones. All common osteochondral fragment locations should be carefully evaluated. Fragments involving the distal aspect of the radial carpal bone are most visible on a DL-PaMO image and can vary in size, can be displaced or nondisplaced, and may extend to the level of the joint capsule attachment (Figure 38-4). Osteochondral fragments involving the third carpal bone most commonly affect the radial fossa and can be seen on the DL-PaMO, LM, and skyline images (Figure 38-5). Small osteochondral fragments involve only the middle carpal joint surface and usually break out dorsally, near the joint capsule attachment on the third carpal bone. It is important to differentiate small osteochondral fragments from frontal or sagittal slab fractures. Third carpal bone osteochondral fragments can be singular or numerous, involve only the radial or intermediate (rare) fossa or both, can be complete or incomplete, or can involve the medial (most common) or lateral corners of the bone. Medial corner fragments of the third carpal bone may resemble subchondral lucency and sagittal slab fracture, so other views must be carefully interpreted. Authentic sagittal slab fractures must be confirmed using a DM-PaLO image. Osteochondral fragments of the distal, lateral aspect of the radius are the largest of the small osteochondral fragments and are often bipartite. The large dorsal fragment is separated from the parent radius by a small separate fragment in the interposed trough (Figure 38-6). The large dorsal fragment can extend proximal to the joint capsule attachment on the distal lateral aspect of the radius. Concomitant osteochondral fragments frequently involve the proximal medial aspect of the intermediate carpal bone. Osteochondral fragments of the proximal aspect of the intermediate carpal bone may occur alone or in combination with osteochondral fragments of the distal lateral aspect of the radius (Figure 38-7). Other, less common osteochondral fragments do occur alone but usually in combination with other osteochondral fragments. Evidence of OA such as enthesophytes and marginal osteophytes may be present (see Figure 38-4). Sclerosis of the third carpal bone is common in horses with osteochondral fragments of the third and radial carpal bones. Mild sclerosis is a normal adaptive response to training, and the presence of sclerosis as a solitary finding is not diagnostic of carpal lameness. Degree of sclerotic change is important, because in my experience a positive correlation exists between the degree of the third carpal bone sclerosis and the extent of cartilage damage on the third and radial carpal bones. However, a radiological study showed no significant relationship between degree of increased radiopacity and prognosis,40 and although there was a continuous increase in the density of the third carpal bone in STB trotters in race training, increased radiopacity was of limited value in predicting carpal lameness.41 More recently, however, carpal lameness was more likely in STBs with higher grades of third carpal bone increased radiopacity.42

Fig. 38-4 Dorsal 45° lateral-palmaromedial oblique radiographic image of a Thoroughbred racehorse with a typical small, displaced, distal radial carpal osteochondral fragment (large arrow), the most common small osteochondral fragment. The presence of entheseous new bone formation (small arrows) at the joint capsule attachment indicates that damage of the radial carpal bone is chronic.
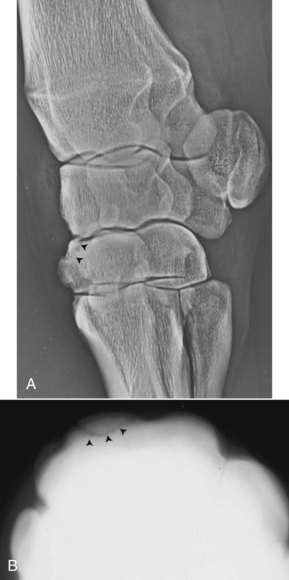
Fig. 38-5 Dorsolateral-palmaromedial oblique xeroradiographic (A) and skyline radiographic (B) images of a horse with a third carpal bone small osteochondral fragment. The osteochondral fragment (arrowheads) breaks out of the dorsal aspect of the third carpal bone in the dorsolateral-palmaromedial oblique image, confirmation that it does not span both articular surfaces of the third carpal bone.
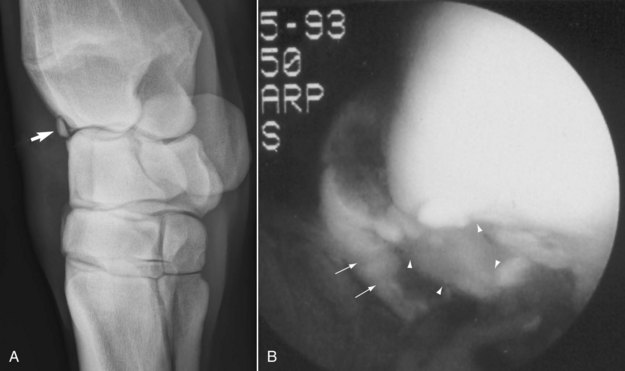
Fig. 38-6 A, Dorsal 45° medial-palmarolateral oblique radiographic image of a right carpus showing typical distal lateral radius small osteochondral fragment (arrow) in a Thoroughbred. B, Intraoperative photograph (dorsal is to the left; proximal is up) shows large dorsal fragment (arrows) separated from the parent radius by a small, interposed wedge-shaped fragment (arrowheads).
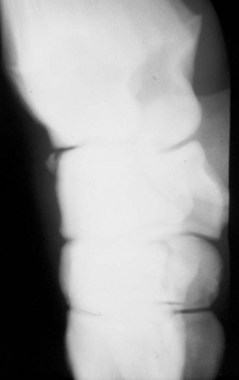
Fig. 38-7 Dorsomedial-palmarolateral oblique radiographic image of a typical osteochondral fragment of the proximal aspect of the intermediate carpal bone. These fragments often appear in combination with osteochondral fragments of the distal lateral aspect of the radius and vary in size, but they generally occur slightly more medially than those of the distal, lateral aspect of the radius.
Scintigraphic examination is an excellent method to diagnose incomplete or occult osteochondral fragments and to evaluate other sites of stress-related subchondral bone injury in the involved or contralateral carpus. Focal IRU on one side of a joint seen in several scintigraphic images, including a flexed dorsal image, can help pinpoint exact location of osteochondral fragments.
Management
The ideal treatment is surgical removal of osteochondral fragments, because unstable surfaces and fragment movement predispose to additional synovitis and development of osteoarthritis (see Figure 23-7). Fragments left in place to heal in displaced fashion cause uneven joint surfaces and are prone to refracture. Arthroscopic examination also allows evaluation and grading of cartilage damage and intercarpal ligament integrity and identification of occult fragments. However, factors such as economic value, racing class, and time of year relative to upcoming races and location of osteochondral fragments are relevant. Horses not worthy of arthroscopic surgery are managed with short-term rest and intraarticular injections of hyaluronan and corticosteroids, or they are given 3 to 6 months of rest. When conservative management procedures are used, fractures develop fibrous unions and become stable, but they are usually displaced and may resemble marginal osteophytes when healed. Many horses that are managed conservatively, especially those with fractures in the antebrachiocarpal joint, return to racing successfully, but recurrence of osteochondral fragments and development of OA are likely. It is difficult to convince owners and trainers to give horses long-term (>6 months) rest. However, rest, with or without arthroscopic surgery, is critical, not only for healing of incomplete fractures or, if osteochondral fragments have been removed, the fracture site, but also for healing of the surrounding cartilage and subchondral bone. Horses with incomplete osteochondral fragments are candidates for conservative management, but if horses are not given adequate time for fracture healing, recurrence is likely (Figure 38-8). Alternatively, I have recommended arthroscopic surgery and fragment removal in horses with incomplete fractures if I know the client will not opt for long-term rest without surgical intervention. Although carpal lameness may recur, at least the original osteochondral fragment will not refracture. During arthroscopic surgery, cartilage damage is graded as mild, moderate, severe, or global, and prognosis is inversely proportional to the extent of damage—a clinical finding substantiated in studies in STB, TB, and QH racehorses36,39 (see Figures 23-4 and 23-7, and Figure 38-1). During arthroscopic surgery, the osteochondral fragment(s) are removed and the surrounding cartilage and bone are curetted, depending on the amount of damage seen. If partial thickness cartilage damage is seen and damage does not extend into subchondral bone past the zone of calcified cartilage, then microfracture can be performed (see Chapter 23). Damage on apposing surfaces is common, and occult osteochondral fragments are often found there or at distant locations. Bilateral carpal arthroscopic surgery is commonly performed in all racing breeds, and in the TB and QH it may be necessary to evaluate all major joints.
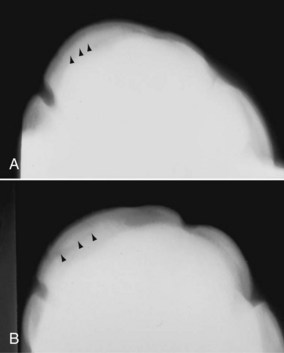
Fig. 38-8 A, Dorsoproximal-dorsodistal (skyline) radiographic image of the distal row of carpal bones of a 2-year-old Standardbred colt with an incomplete osteochondral fragment of the third carpal bone. In this image there is predominantly dense increased radiopacity of the radial fossa, and the faint fracture is difficult to identify (arrowheads). B, Seven months later, when the horse was 3 years old, lameness and fracture recurred. The horse had been given inadequate rest to allow the fracture to heal completely.
After arthroscopic surgery horses are given a progressively increasing exercise program, the length of which depends on severity of damage and location of osteochondral fragments. For instance, in TB racehorses with osteochondral fragments of the distal, lateral aspect of the radius and the proximal aspect of the intermediate carpal bone, I recommend 2 weeks of stall rest, followed by 4 weeks of stall rest with hand walking (or walking in a caged walker), followed by 2 to 4 weeks of turnout or swimming physiotherapy. Lameness is less pronounced initially, and horses appear able to return to work earlier when osteochondral fragments involve the antebrachiocarpal joint rather than the middle carpal joint. In horses with routine distal radial carpal bone and proximal third carpal bone fragments, I recommend 4 weeks of stall rest, followed by 4 weeks of stall rest with hand walking, followed by 8 weeks of turnout or swimming physiotherapy. In horses with numerous fragments and severe or global cartilage damage, I recommend 4 to 6 months of total rest.
After arthroscopic surgery I recommend the use of intraarticular injections of hyaluronan at 14 and 28 days in horses with mild or moderate cartilage damage, and a series of intraarticular PSGAG injections at 3, 5, and 7 weeks after surgery. I recommend intramuscular administration of PSGAGs once weekly for 8 weeks, beginning 14 days after surgery. Little concrete evidence shows that any form or combination of intraarticular therapy is of long-term benefit for cartilage healing after surgery, although antiinflammatory effects are likely mildly beneficial. Short-term benefit of several intraarticular or parenterally administered products evaluated in an osteochondral fragment model has been shown (see Chapter 84).
Cartilage resurfacing techniques have been used experimentally and in a limited number of horses with osteochondral fragments and OA (see Chapters 23, 63, and 84). Cell-based techniques such as injection of cloned chondrocytes in autogenous fibrin loaded with growth factors appear promising. Microfracture of calcified cartilage appears promising in experimental trials, but seeing horses with partial-thickness cartilage damage is unusual. Subchondral bone is usually already exposed, obviating the need to use this.
Prognosis depends on several factors, including type and age of horse, racing class, limb(s) affected, number and location of osteochondral fragment(s), and amount of cartilage damage. Intuitively, a better prognosis would be expected in the STB than the TB and QH, because load is better shared by the hindlimbs and gait allows compensation by a lateral or diagonal limb. However, in STBs osteochondral fragments often develop later in the nonadaptive remodeling process, when OA is already well beyond that in TBs with comparable lesions. In most racehorses any damage of the third carpal bone is a major limiting factor in prognosis, and because osteochondral fragments of the third carpal bone are common in STBs, overall prognosis for STBs might be expected to be less favorable than for TBs and QHs. The prognosis for horses with lesions in the antebrachiocarpal joint is better than for those in the middle carpal joint, and because osteochondral fragments occur with similar frequency in both joints in TBs and QHs, the overall prognosis is better. The prognosis for return to racing is good to excellent, but the likelihood of racing at the preinjury level is inversely proportional to the degree of cartilage damage. Seventy-four percent of STBs with osteochondral fragments returned to racing after arthroscopic surgery, but only 61% raced at or above the preinjury level. Pacers were more likely than trotters to start a race and to have five starts before and after injury.36 Kinematic studies show that the pace may slow forelimb fatigue and reduce forelimb load.43 Median earnings per start decreased significantly after injury and arthroscopic surgery, but horses went significantly faster after surgery.36
Of 445 TB and QH racehorses, 303 (68%) raced at a level equal to or better than the preinjury level, but when grouped according to cartilage damage, only 53% of horses with the most severe cartilage damage raced at these levels. Eleven percent of horses had decreased performance and had carpal lameness, 6% developed additional osteochondral fragments, and 2% developed collapsing slab fractures while racing.36 Prognosis was worse for horses with osteochondral fragments of the third carpal bone.
Palmar Carpal Osteochondral Fragments
Osteochondral fragments can occur in the palmar aspect of the carpus and can result from a single-event injury or can be associated with other osteochondral fragments in the dorsal aspect of the carpal joints. Trauma may result from falling, hitting a fence, or landing with subsequent hyperextension of the carpus or falling when the carpus is flexed (hyperflexion). Palmar carpal injury is one of the more common catastrophic injuries occurring in horses during recovery from general anesthesia (Figure 38-9, A). Palmar carpal injury after general anesthesia can be career-limiting or career-ending and often leads to severe OA of the involved carpal joints. In horses that sustain palmar carpal fragments as a result of a traumatic event, osteochondral fragments usually involve the palmar aspect of the radial and intermediate carpal bones and the articular surface of the accessory carpal bone but can involve any of the carpal bones, can be singular or numerous, and occur medially and laterally. Articular osteochondral fragments of the accessory carpal bone are usually comminuted and involve at least two or three pieces.

Fig. 38-9 A, Dorsal 45° medial-palmarolateral digital radiographic image of the left carpus of a horse sustaining a comminuted palmar carpal fracture of the radial carpal bone (arrows) and intermediate carpal bones during recovery from general anesthesia. Because of severe lameness this horse was euthanized. B, Lateromedial digital radiographic image of a racehorse with palmar carpal osteochondral fragments (large arrow) located in the palmarolateral pouch of the middle carpal joint. Fragments have migrated from a primary site of osteochondral fragmentation, the distal dorsal aspect of the radial carpal bone (small arrow).
(A courtesy David Levine and Eric Parente, Kennett Square, Pennsylvania, United States. B courtesy of Liberty Getman, Kennett Square, Pennsylvania, United States.)
In horses with known chronic osteochondral fragments in the dorsal aspect of the carpus and those with OA, radiographs occasionally reveal what appear to be small fragments or mineralization in the palmarolateral or palmaromedial aspects of the middle carpal joint (see Figure 38-9, B). It was once thought that radiopacities in the palmar aspect of the middle carpal joint were areas of dystrophic mineralization after corticosteroid injections, but it is now known these are most likely small fragments that migrate from the dorsal to the palmar aspect of the joint and occur when training and racing continues in horses with existing osteochondral fragments, which then become macerated. When the condition is observed, cartilage damage is usually extensive, and prognosis is guarded. In a study of 31 racehorses with palmar carpal osteochondral fragments, only 48% of horses returned to racing and earned money, and only 32% had five or more race starts after injury.22 Horses with numerous fragments had significantly lower earnings and lower performance indices after surgery than those with one fragment, and those with fragments smaller than 3 mm diameter were significantly less likely to return to racing than those with larger fragments.22 Palmar carpal fragments were most commonly seen in the palmarolateral pouch of the middle carpal joint and in 24 horses were associated with coexistent osteochondral fragmentation in the dorsal aspect of the joint.22 Seven horses had palmar carpal fragments without associated dorsal fragmentation, and in six of these seven horses fragments involved the palmar aspect of the antebrachiocarpal joint (all involved the proximal aspect of the radial carpal bone).22 It has been suggested that fragment migration from the dorsal to the palmar aspect of the middle carpal joint occurs because of medial palmar intercarpal ligament injury, an association that I have not found true. No association was found between palmar carpal fragment size or number and medial palmar intercarpal ligament injury.22
Lameness is acute in onset, with effusion of the middle carpal or antebrachiocarpal joints. Often the response to static flexion of the carpus is profound. Careful interpretation of radiographs is necessary to confirm the presence of osteochondral fragments, locate precisely the parent bone from which the osteochondral fragment arose, and determine the number of fragments. The clinician should recognize that osteochondral fragments in the palmar aspect of the carpus may represent only one aspect of more global damage to the joint(s). Any evidence of fragmentation dorsally, or active OA if trauma occurred at least 10 to 14 days before radiographic examination, is a poor prognostic indicator, because this reflects substantial subchondral bone and cartilage injury dorsally. OA and chronic lameness are inevitable, particularly in horses with palmar carpal injury sustained while jumping or during recovery from general anesthesia. Palmar osteochondral fragments can be removed using arthroscopic surgery or arthrotomy,44 but access can be difficult. Recent studies have refined the surgical approaches and anatomy of the palmar pouches of the carpal joints and the value of arthroscopic examination.16,21,22 The palmarolateral pouch of the antebrachiocarpal joint is large, and osteochondral fragments involving the accessory and intermediate carpal bones can be removed from this approach. When removing osteochondral fragments from the palmaromedial or the palmarolateral aspect of the middle carpal joint, both portals must be made within a small joint pouch, making triangulation difficult. Prognosis for future soundness is guarded to fair for racehorses (see earlier). In nonracehorses, prognosis for horses with single fragments without substantial OA is fair, but it is guarded to poor in those with substantial instability or bone and cartilage damage at more distant sites.
Large Osteochondral Fragments: Slab Fractures
Slab fractures are defined as fractures that involve a proximal and distal articular surface and thus traverse the entire depth (proximal-distal direction) of the bone. Size and involvement of two articular surfaces differentiate these fractures from small osteochondral fragments. Slab fractures of the third carpal bone are by far the most common form of large osteochondral fragments in the carpus, but slab fractures of the radial, fourth, and intermediate carpal bones occasionally occur. A combination of radial and third carpal bone slab fractures occurs in TB racehorses and may lead to instability and carpal collapse. In most instances, slab fractures develop as a terminal event in the cascade of maladaptive or nonadaptive remodeling changes leading to sclerosis, biomechanical weakness, and subsequent fracture. When slab fractures occur in unusual locations, the possibility of single-event injury must be considered. Slab fractures occur almost exclusively in racehorses.
Frontal (Dorsal) Slab Fractures of the Third Carpal Bone
The most common large osteochondral fragment in the carpus is a slab fracture of the third carpal bone in the frontal (dorsal) plane. A frontal slab fracture of the third carpal bone usually involves the radial fossa, but fractures of the intermediate fossa alone or in combination with fracture of the radial fossa do occur (Figures 38-10 and 38-11). Frontal slab fractures of the third carpal bone involving the radial fossa vary in size and can involve the entire medial-to-lateral width of the fossa, or any portion of it, and range from the common size of 8 to 10 mm in the dorsal-to-palmar direction up to 20 to 25 mm. These latter, large fragments cannot be seen on a skyline radiographic image, extend across the entire medial-to-lateral width of the third carpal bone involving both fossae, and are L shaped (Figure 38-12).
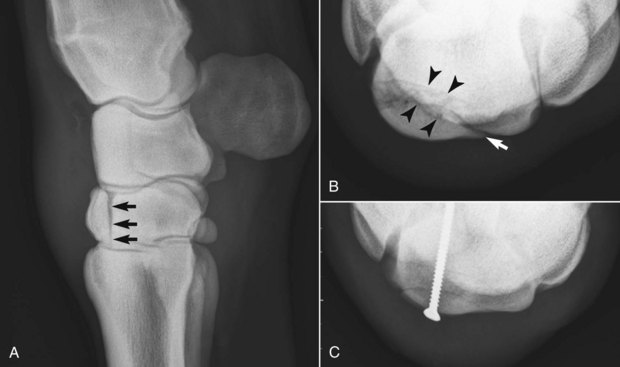
Fig. 38-10 A, Standing lateromedial digital radiographic image (dorsal is to the left) showing a complete, mildly displaced frontal slab fracture of the radial fossa of the third carpal bone (arrows) in a 3-year-old Thoroughbred racehorse. The fracture line traverses the entire depth of the third carpal bone involving the middle carpal and carpometacarpal joints. Displacement is best seen in this radiographic image. B, Dorsoproximal-dorsodistal (skyline) digital radiographic image of the distal row of carpal bones showing the frontal slab fracture of the radial fossa of the third carpal bone (medial is left and palmar is uppermost). The slab fracture traverses the entire radial fossa (arrow). Interposed between the fracture line and the parent third carpal bone is a wedge-shaped osteochondral fragment (arrowheads) that is generally removed before repair. C, The frontal slab fracture has been repaired using a single 3.5-mm bone screw placed in lag fashion in the center of the fracture fragment using arthroscopic guidance. The wedge-shaped fragment seen in the preoperative view (B) has been removed, and there is good anatomical alignment of the repair.
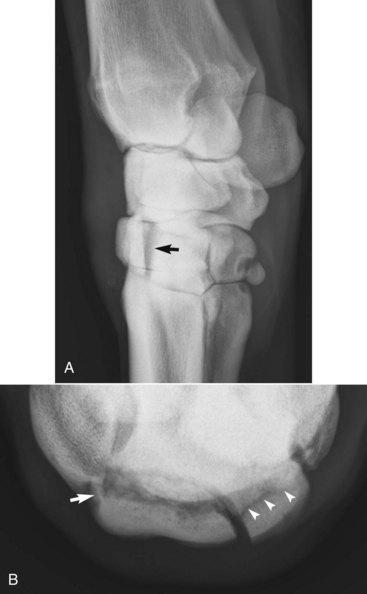
Fig. 38-11 A, Dorsal 45° medial-palmarolateral oblique digital radiographic image showing a displaced frontal slab fracture of the intermediate fossa of the third carpal bone (arrow). B, Dorsoproximal-dorsodistal digital radiographic image of the distal row of carpal bones (medial is to the left and palmar is uppermost) showing a comminuted frontal slab fracture of the third carpal bone involving the radial (large arrow at fracture line) and intermediate (arrowheads at fracture line) fossae.
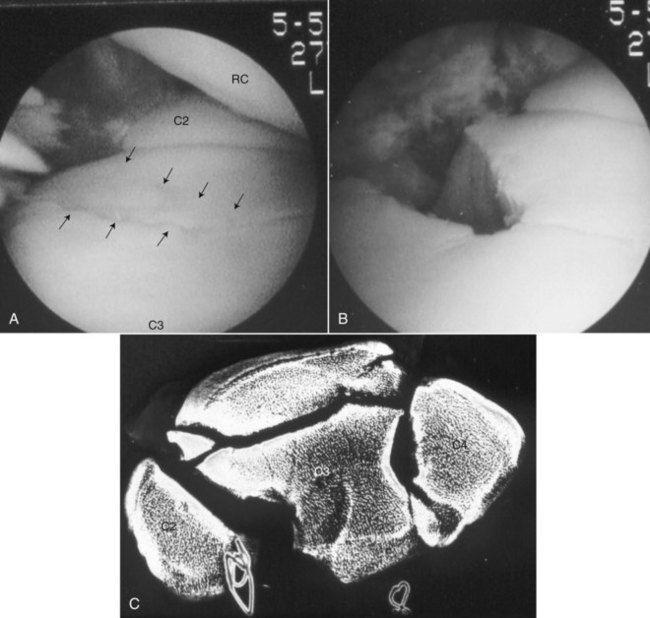
Fig. 38-12 This pacer had an L-shaped fracture of the third carpal bone that involved a sagittal and frontal component. A, The initial intraoperative photograph shows the sagittal component (arrows) and crushed medial aspect of the third carpal bone. B, This area was debrided, and the fracture healed without internal fixation. The sagittal component of the fracture appears palmar to the defect. C, True proximal-to-distal radiographic image of a trotter obtained at necropsy shows that the large slab fracture of the third carpal bone has frontal and sagittal components. C2, Second carpal bone; C3, third carpal bone; C4, fourth carpal bone; RC, radial carpal bone.
Lameness in horses with a frontal slab fracture is acute and severe and is generally worse than in those with small osteochondral fragments, but chronic, subtle prodromal lameness may have been present. A previous history of small osteochondral fragments and arthroscopic surgery is common. Lameness may be less than expected in horses recently injected with corticosteroids and in those with bilateral frontal slab fractures of the third carpal bone. Clinical signs such as heat, effusion, and response to static and dynamic flexion are pronounced, and horses are usually lame at the walk. Horses with non–weight-bearing lameness may have unstable carpi and should be evaluated carefully for collapse from comminuted fractures. The contralateral carpus should always be evaluated and palpation should be complete to uncover compensatory lameness problems. In TB racehorses in North America the right third carpal bone is affected more commonly than the left,45 but in STBs the distribution between right and left is similar.46
Frontal slab fractures of the third carpal bone are usually obvious radiologically. If they involve the radial fossa, fractures are best seen on the LM, flexed LM, and DL-PaMO images and a skyline image. Because frontal slab fractures of the third carpal bone by definition involve the middle carpal and carpometacarpal joint surfaces, if a fracture line breaks out dorsally before reaching the carpometacarpal joint, the fragment is not a true slab fracture. This is important when determining a management plan. A frontal slab fracture of the third carpal bone can be incomplete, complete but nondisplaced, or complete and displaced and may be associated with other small osteochondral fragments. Degree of displacement is worse on a standing LM image, but when the carpus is flexed, the fracture returns to near normal alignment. Flexion is a useful maneuver during reduction. In most instances a triangular, wedge-shaped fragment appears in the trough between the slab fracture fragment and the parent bone, and this accounts for the appearance of many fracture lines in a skyline view (see Figure 38-10, B). Careful examination of the overlying radial carpal bone is required in TB racehorses, because concomitant slab fracture of the radial carpal bone can accompany a frontal slab fracture of the third carpal bone.
Management depends on several factors, including the horse’s value, age, racing class, presence of other lameness problems, and specifically whether the frontal slab fracture of the third carpal bone is incomplete, displaced, or comminuted. Long-term rest (6 months) is successful in horses with incomplete or complete nondisplaced fractures. However, surgical fixation can help preserve articular surfaces by preventing displacement. Frontal slab fracture fragments that are thin (<5 mm in the dorsal-to-palmar direction) can be removed using arthroscopic surgery or conventional arthrotomy techniques or, if the articular surface is intact, can be repaired. Arthroscopic techniques are preferred when possible, and the technique remains largely unchanged since originally described.47 Surgical removal of small frontal slab fractures of the third carpal bone can be difficult using arthroscopic techniques and can leave a large defect radiologically but is successful. Horses with large frontal slab fragments that are displaced are usually managed with arthroscopic surgery and internal fixation, using one or two cortex screws placed in lag fashion. Either 3.5- or 4.5-mm screws can be used, but I prefer using one or two 3.5-mm screws because the screw heads are smaller and countersinking in the dorsal aspect of the third carpal bone is not necessary. Horses with large frontal fractures of the radial fossa, those with comminuted fractures involving both the radial and intermediate fossae (see Figure 38-11), and those in which fracture fragments cannot be adequately reduced should be repaired with 4.5-mm screws, because 3.5-mm screws can sometimes break. Use of needles and intraoperative radiographs to position and guide screw insertion accurately is preferred.45 A single bone screw provides adequate fixation in horses with most frontal slab fractures of the third carpal bone involving only the radial fossa, because capsular attachments maintain rotational stability. The fracture line is debrided, often before screw placement, and the wedge-shaped trough fragment is removed, leaving a gap at the fracture line. Loose cartilage is curetted, cartilage damage is graded, and other small osteochondral fragments are removed if present. Alternatively the proximal articular surface of the fragment may be removed, with repair of the distal aspect, leaving the portion of the fragment with capsular attachments intact. Occasionally, additional slab fractures of the third or radial carpal bones are found and repaired. In horses with more than one slab fracture, a Robert Jones bandage or cast is used for recovery from general anesthesia. In TB racehorses with a frontal slab fracture of the third carpal bone, an ominous defect in the articular cartilage of the radial carpal bone is often seen, caused by the incongruent apposing surface of the third carpal bone, but in most horses subchondral bone fracture is not present. Horses are typically given stall rest for 4 weeks, followed by stall rest with hand walking for 8 weeks, followed by turnout in a small paddock for 2 to 3 months before beginning race training. Recommendations for intraarticular therapy are similar to those in horses with small osteochondral fragments.
In a large retrospective study of TB and STB racehorses with a frontal slab fracture of the third carpal bone, the radial fossa was involved in 87% of horses, and females of both breeds were less likely to race after injury and surgery, but treatment and fracture characteristics had no effect on outcome.46 Fracture characteristics such as size and degree of displacement did influence treatment selection, so thin frontal slab fractures of the third carpal bone were removed, displaced fractures were repaired, and horses with incomplete or nondisplaced frontal slab fracture of the third carpal bone were managed conservatively.46 All STBs that had raced before surgery also raced after surgery, and overall 77% raced after surgery. Sixty-five percent of TBs with frontal slab fractures of the third carpal bone raced after surgery, and although earnings per start decreased in both breeds, the decrease was more pronounced in TBs.46 In another study, 67% of TBs with a frontal slab fracture of the third carpal bone raced at least once after surgery, but the mean claiming value in horses decreased significantly.45 In a study in which lag screw fixation was used in horses with incomplete frontal plane fractures of the radial facet of the third carpal bone, 69% of horses were considered to have successful outcomes, and there was no difference in racing longevity or ability after surgery between principles and age-, sex-, and sire-matched controls.48
Sagittal Slab Fractures of the Third Carpal Bone
Sagittal slab fractures of the third carpal bone are much less common than frontal slab fractures, usually involve the medial aspect of the radial fossa (see Figures 38-12 and 38-13), and occur in a direction parallel to the articulation between the second and third carpal bones. However, sagittal slab fractures of the third carpal bone can occur in the intermediate fossa, and fractures can be bilateral. Authentic sagittal slab fractures of the third carpal bone involve both articular surfaces of the bone and can be best seen radiologically in skyline and DM-PaLO images. Sagittal slab fractures of the third carpal bone must be differentiated from corner fractures, subchondral lucency, and other crushing-type injuries that occur in the radial fossa. Clinical signs associated with sagittal slab fractures of the third carpal bone are similar to those of other osteochondral fragments but are usually less severe than a frontal slab fracture of the bone. Lameness is usually prominent, but in horses with bilateral fracture or substantial OA or osteochondral fragments in the contralateral carpus, diagnostic analgesia may be required. Often horses have a prominent history of chronic carpal lameness before acute lameness develops. Of 32 racehorses with sagittal slab fracture of the third carpal bone, 19 were TBs, 11 were STBs, and 2 were Arabian racehorses, and fractures were found in the right forelimb (19), left forelimb (12), and bilaterally in one horse.49 Overall, 22 (69%) horses raced after treatment, all seven horses treated with interfragmentary compression raced, and horses that underwent interfragmentary compression had significantly higher earnings per start than those treated without surgery.49 Eight of nine horses managed with arthroscopic debridement raced, but only 7 of 16 horses managed conservatively raced.49

Fig. 38-13 Initial (A) and 8-month follow-up (B) skyline radiographic images of the third carpal bone showing a sagittal slab fracture (arrows) that failed to heal and became a nonunion (B). This Standardbred trained and raced with the nonunion fracture but dropped substantially in class. Results such as this have prompted me to manage sagittal slab fractures of the third carpal bone surgically.
Conservative management was recommended, but only 7 of 12 horses with a sagittal slab fracture of the third carpal bone managed conservatively raced.50 Fracture healing takes extensive time, and a chronic nonunion often develops (see Figure 38-13, B). Horses can be sound enough to race with chronic nonunion fractures, but this is undesirable. I have seen one STB and one TB racehorse with bilateral lateral, nonunion sagittal slab fractures of the third carpal bone racing successfully, but with conservative management comes a risk of chronic high-speed lameness, worse if fracture involves the right forelimb, and horses drop substantially in racing class. If any doubt exists about the nature of a lesion affecting the medial aspect of the third carpal bone, arthroscopic examination can be performed to formulate a surgical plan. If an authentic sagittal slab fracture of the third carpal bone does not exist, but medial corner osteochondral fragments, necrotic subchondral bone, or other crush-type injuries are found, a combination of fragment removal and curettage is performed. I currently recommend surgical management for most horses with sagittal slab fractures of the third carpal bone. To repair a fracture, I prefer a direct view provided by arthrotomy, because positioning a screw perpendicular to the fracture line using arthroscopic surgery and stereotactic techniques is difficult and because the fracture is closely associated with the second carpal bone. A single 3.5-mm screw is placed in lag fashion. Alternatively, arthroscopic evaluation and debridement result in a better outcome than does conservative management.49 Evaluating the joint arthroscopically and then formulating a management plan is a reasonable approach, but certainly surgical management is preferred over rest alone. Management after surgery is similar to that described for horses with frontal slab fractures of the third carpal bone.
Slab Fractures of Other Carpal Bones
Slab fractures of carpal bones other than the third are unusual. Whenever slab fractures of the radial carpal bone or other unusual slab fractures are discovered, all radiographic images should be evaluated carefully. CT was shown to be valuable in identifying fracture lines and comminution not seen using radiography.14 Slab fractures of the radial carpal bone can occur independent of or in combination with frontal slab fracture of the third carpal bone. When frontal slab fractures of the radial and third carpal bones occur simultaneously and carpal instability results, the fracture is called a comminuted carpal fracture. Repairing both bones by placing numerous screws using arthroscopic surgery may be possible. A sleeve or full-limb fiberglass cast is placed, and an assisted recovery from general anesthesia is recommended.
Slab fractures of the intermediate, fourth, and ulnar carpal bones occur rarely. In five horses with intermediate and fourth carpal bone slab fractures, outcome was poor because of delay in diagnosis, and four horses were only pasture sound.51 Surgical repair should proceed as early as possible, but prognosis is limited by cartilage damage and other osteochondral fragments.
Subchondral Lucency of the Third Carpal Bone
Subchondral lucency of the third carpal bone52 is an unusual condition occurring most commonly in STB racehorses, although it is occasionally seen in the TB racehorse, and is seen radiologically as single or multiple central areas of bone loss in the radial fossa of the third carpal bone (Figure 38-14). Overall, I am seeing fewer STB racehorses with this lesion. Earlier recognition and intervention may be credited. Lesions can be seen in a DL-PaMO image in horses with advanced subchondral lucency of the third carpal bone. Mild-to-severe sclerosis may surround radiolucent defects,52 but in one study no relationship was found between radiolucency of the third carpal bone and increased radiopacity.40 The lesion was more common in the right carpus, and, although pacers predominated, distribution was similar to the racing population in the United States.52 Pathogenesis is identical to that described for OA, osteochondral fragments, and slab fractures of the third carpal bone, but in horses with subchondral lucency of the third carpal bone, necrosis of subchondral bone causes table surface collapse rather than osteochondral fragments or slab fractures involving the dorsal margin. Subchondral lucency of the third carpal bone is not a disease of young racehorses, because the mean age in STBs was 4.1 years (range, 3 to 7 years) and chronic stress-related subchondral bone injury is required.
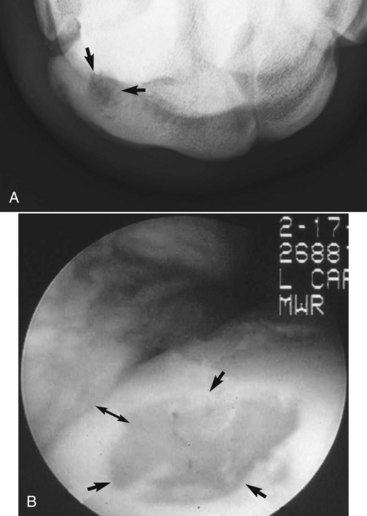
Fig. 38-14 A, Dorsoproximal-dorsodistal (skyline) digital radiographic image of the left carpus of a Thoroughbred racehorse with subchondral lucency (arrows) of the radial fossa of the left third carpal bone (medial is to the left and palmar is uppermost). Subchondral lucency of the third carpal bone should be differentiated from other sagittal plane injury, such as sagittal slab fracture. This horse underwent arthroscopic debridement successfully. B, Intraoperative arthroscopic photograph of the left third carpal bone of a Standardbred racehorse that underwent successful debridement of subchondral lucency of the third carpal bone (dorsal is to the left and proximal is uppermost). Full-thickness cartilage damage and soft, crumbly subchondral bone were debrided (arrows), and the dorsal aspect (rim) of the third carpal bone was left intact (double-headed arrow).
(A courtesy Dean Richardson, Kennett Square, Pennsylvania, United States.)
There are prodromal clinical signs of mild carpal lameness and usually a history of the administration of numerous intraarticular injections before onset of acute lameness, usually graded from 2 to 4 on a 5-point scale. Heat, effusion, and a positive response to flexion may be absent, and diagnostic analgesia is usually required to confirm diagnosis. The results of initial radiological evaluation may be equivocal, and follow-up radiographic and scintigraphic examinations can help pinpoint subchondral lucency of the third carpal bone. Focal areas of IRU in the radial fossa of the third carpal bone similar to that seen with frontal or sagittal slab fracture are seen.
Surgical debridement is the treatment of choice (see Figure 38-14, B). During arthroscopic examination, soft crumbly necrotic subchondral bone and damaged overlying cartilage are found. In some horses only a small full-thickness cartilage defect can be probed, but deep extensive subchondral bone softening is later found, whereas in others, fibrin-filled, full-thickness defects resembling subchondral bone collapse or table surface fracture are found. The damaged tissue is curetted, and if the resulting lesion is smaller than 5 mm palmar to the dorsal margin of the third carpal bone, this rim is removed, creating a defect that resembles removal of an osteochondral fragment. If subchondral lucency of the third carpal bone lesions is deep within the third carpal bone, the dorsal margin is not removed. Cartilage resurfacing could be considered, but it is not necessary for a successful outcome.
Prognosis is excellent for return to racing, particularly in pacers, but horses drop in racing class. Prognosis for return to racing the next year is guarded in 3- or 4-year-old trotters, but some make useful older racehorses. Of nine horses, eight returned to racing, but only six raced at the previous level.52
Comminuted Fractures
Comminuted fractures are unusual, but they occur occasionally in TB and QH racehorses and other horses that sustain injury while turned out in a field. Comminuted in this sense refers to numerous fractures in more than one carpal bone. In STB racehorses, large, comminuted fractures of the third carpal bone can occur, but I have not seen a STB with a large osteochondral fracture involving more than one bone. The most common combination of fractures in TB and QH racehorses involves the third carpal bone and either the radial or intermediate carpal bone, or both. Carpal instability, most commonly carpus varus, is usually readily apparent if horses bear weight, but they are usually non–weight bearing. These injuries occur almost exclusively in racehorses, and often horses have chronic carpal lameness before injury, but fracture can occur in other types of horses without previous lameness during turnout exercise. Effusion and edema of surrounding soft tissues occurs. Diagnosis of comminuted fracture and instability is confirmed radiologically (Figure 38-15). If fractures involve only the distal row of carpal bones, instability is minimal and prognosis is better than if the middle carpal and antebrachiocarpal joints are involved. Consideration should be given for euthanasia if the horse is a gelding or intact male with limited breeding potential. Conservative management using sleeve or full-limb casts, or a combination of splints with a Robert Jones bandage, may give support and provide comfort, but usually instability is pronounced, horses develop extensive cast sores, and they are at profound risk to develop laminitis in the contralateral limb. Severe OA, collapse, and angular limb deformity generally result in an unacceptable outcome in horses managed conservatively. Surgical management using carpal arthrodesis is the treatment of choice.

Fig. 38-15 A, Non–weight-bearing dorsopalmar computed radiographic image obtained before surgery of the left carpus (lateral is to the right and proximal is uppermost) in an aged gelding riding horse that sustained a comminuted carpal fracture while turned out. Notice marked carpus valgus limb deformity caused by collapse of the lateral aspect of the middle carpal joint. There were comminuted fractures of the third and fourth carpal bones. B, Dorsopalmar digital radiographic image obtained 3 years after successful panarthrodesis of the carpus, showing complete fusion of the antebrachiocarpal, middle carpal, and carpometacarpal joints. Two broad dynamic compression plates and interfragmentary compression of the third carpal bone were used. Today, locking compression plates would likely be used, but successful arthrodesis was achieved with this fixation in conjunction with external coaptation with a fiberglass sleeve cast.
Carpal Arthrodesis
Arthrodesis is indicated when horses have comminuted carpal fractures and instability, when they have severe lameness and OA of one or more carpal joints, or when OA is severe with collapse and angular deformity of the carpus. Partial (intercarpal) carpal arthrodesis involves fusing the middle carpal and carpometacarpal joints using bone plates applied to the proximal row of carpal bones and the McIII. Pancarpal arthrodesis involves bridging the entire carpus with bone plates applied to the distal radius, both rows of carpal bones, and the McIII, fusing all three joints. Two plates, either dynamic compression plates or, more recently, locking compression plates,53,54 are used for either technique, and in one study allografts were used to provide axial support in some horses with collapsed carpi undergoing pancarpal arthrodesis. In one horse, I successfully used acrylic to create an artificial fourth carpal bone to maintain axial stability, in addition to two dynamic compression plates and interfragmentary repair of fractures (see Figure 38-15). Overall, prognosis for salvage is good, but complications included infection and contralateral laminitis. Of 36 horses undergoing carpal arthrodesis, 30 (83%) survived 3 months, and 24 (67%) survived at least 9 months after surgery.55 Prognosis was similar between horses undergoing pancarpal and partial carpal arthrodesis.55,56
Accessory Carpal Bone Fractures
Fracture of the accessory carpal bone results from trauma, such as a fall while jumping, a hyperextension injury when landing, or an accident while turned out. Acute, severe lameness and swelling involve the palmar aspect of the carpus. Horses have severe pain during carpal flexion. Carpal tenosynovitis may occur acutely, but it is difficult to differentiate from diffuse swelling. Pronounced lameness lasts for several days, but horses are rarely non–weight bearing, and swelling resolves in 2 to 3 weeks. Horses with a chronic fracture may have little to no swelling, and diagnosis may be difficult unless carpal tenosynovitis is present, because the lameness is not typical of carpal pain.
The most common fracture of the accessory carpal bone is a vertical slab fracture that involves the palmar aspect of the bone in the frontal (dorsal) plane (Figure 38-16). Most fragments are simple, but small fragments at the proximal aspect of the fracture may occur. Fractures can be incomplete, but most are complete with mild displacement. Gross displacement and large comminuted fragments are unusual. Articular fractures were discussed previously (see page 439).

Fig. 38-16 A lateromedial radiographic image of a horse with a failed attempt at surgical management of a frontal slab fracture of the accessory carpal bone. These fractures are best managed conservatively without attempting repairs such as this one.
Conservative management of horses with nonarticular fractures of the accessory carpal bone is recommended. The forces on the accessory carpal bone are substantial and result in failure of screw fixation, chronic instability, implant loosening, and osteitis (see Figure 38-16). Surgical fixation using the tension band principle may be successful, but I have not attempted repair because prognosis is favorable with conservative management. Horses are given NSAIDs, and a heavy full-limb cotton bandage is applied. Horses are given stall rest for 8 weeks, followed by stall rest with hand walking for 8 weeks, followed by walking with a rider up for 8 weeks. Radiographs most often reveal bony proliferative changes and fibrous rather than bony union of the fracture. Even with fibrous union, horses are usually serviceably sound. Prognosis for TB racehorses appears to be worse than for field hunters, jumpers, and other horses that may be able to perform with a mild gait restriction from chronic fibrosis. Carpal canal syndrome and carpal tenosynovitis may result (see Chapter 75).
Osteochondrosis
Osteochondrosis of the carpus is rare. In a radiological study of yearling TBs, 0.4% had either radiological changes associated with osteochondritis dissecans (OCD) or a subchondral bone cyst, other than that seen involving the distal aspect of the ulnar carpal bone (see later).57 In experimental studies extensive cartilage lesions histologically similar to those in naturally occurring OCD have been produced. Rarely, radiographs of yearlings before or after public sales reveal rounded osteochondral fragments, usually involving the distal medial aspect of the radius or the distal medial aspect of the radial carpal bone or proximal aspect of the third carpal bone. These fragments appear as solitary osteochondral fragments and do not have associated marginal osteophytes or enthesophytes, unlike osteochondral fragments caused by trauma at a young age. At the time of surgery these unusual fragments appear intercalated in dense joint capsule attachments, are rounded, and often have a smooth defect in the distal aspect of the radius or third carpal bone, apparently the origin of the fragment. Whether these fragments represent a form of OCD or old trauma is not known, but they appear similar to forms of OCD found elsewhere.
Osseous Cystlike Lesions
Osseous cystlike lesions do occur in the carpus. Those of the ulnar carpal bone are common, appear to be incidental radiological findings, are usually nonarticular, and have sclerotic borders. Often, small bony fragments can be seen within the radiolucent defect and can be misinterpreted as acute fractures, sometimes called avulsion injury of the lateral palmar intercarpal ligament (see later). Ulnar carpal bone radiolucent defects were the most common radiological abnormality found in a large study of TB yearlings.57 Abnormalities of the distal aspect of the ulnar carpal bone were found in 20% of yearlings and were exclusively unilateral, and no negative association between this radiological change and racing performance was found.57,58 Incidental osseous cystlike lesions may also be seen in the second carpal bone, often in the presence of the first carpal bone, and also in the base (head) of the McII. Osseous cystlike lesions of the radial carpal bone and distal aspect of the radius can cause lameness.59 Effusion, heat, and a positive response to flexion are inconsistent, and diagnostic analgesia is usually necessary. Radiological signs may be obvious, but in some horses they are subtle, and scintigraphic examination is useful to pinpoint the area of modeling. In horses with an osseous cystlike lesion that communicates with an articular surface, I have performed debridement and curettage, but results have been unfavorable to fair at best. Alternatively, I have had good success using a combination of rest (4 to 6 months) and serial intraarticular injections (two or three) of hyaluronan and corticosteroids (40 mg methylprednisolone acetate) when cysts appear radiologically to communicate with a carpal joint (see Figure 39-4).
Osteochondromatosis
Osteochondromatosis is rare but has been seen in the carpometacarpal joint.60 Progressive enlargement of the carpometacarpal joint and numerous unusual radiopacities were seen radiologically.60 Arthroscopic examination of the carpometacarpal joint was possible, and osteochondral fragments were removed60 (see Chapter 67).
Other Fractures Involving the Carpus
Avulsion Fracture of the Third Metacarpal Bone Associated with the Origin of the Suspensory Ligament
See Chapter 37 for a discussion of avulsion fracture of the McIII associated with the origin of the SL (page 417).
Incomplete, Longitudinal Fracture of the Proximal Palmar Cortex of the Third Metacarpal Bone
See Chapter 37 for a discussion of incomplete, longitudinal fracture of the proximal palmar cortex of the McIII (page 413).
Dorsomedial Articular Fracture of the Proximal Aspect of the Third Metacarpal Bone
See Chapter 37 for a discussion of dorsomedial articular fracture of the proximal aspect of the McIII (page 416).
Fracture of the Proximal Aspect of the Second and Fourth Metacarpal Bones
See Chapter 37 for a discussion of the proximal aspect of the McII and the McIV (page 421).
Articular Fracture of the Distal Aspect of the Radius
Fractures of the distal aspect of the radius rarely involve the antebrachiocarpal joint. Complete or incomplete, displaced or nondisplaced fractures of the radius in the sagittal plane and resembling condylar fractures of the McIII or the third metatarsal bone can occur.61 Horses should be managed conservatively using full-limb bandages, NSAIDs, and absolute stall rest if fractures are nondisplaced. Some consideration should be given to cross-tying the horse for 3 to 6 weeks. Comminuted fractures of the radius, or those involving the distal radial physis and epiphysis that involve the antebrachiocarpal joint, should be repaired.
Soft Tissue Injuries of the Carpus and Carpal Region
Medial Palmar Intercarpal Ligament
Various degrees of tearing of the medial palmar intercarpal ligament have been observed during arthroscopic examination of horses with osteochondral fragments or OA and in some horses with occult carpal lameness (see Figure 23-4). The medial palmar intercarpal ligament has recently been the source of considerable study and supposition, but whether tearing of this ligament observed in horses with carpal disease is causative or simply results from other pathological conditions is not yet known. The anatomy of the medial palmar intercarpal ligament and the relationship between osteochondral fragments and the dorsomedial intercarpal ligament were previously discussed (see page 427).
Because tearing of the medial palmar intercarpal ligament is an observation during arthroscopic examination of the middle carpal joint and a diagnosis impossible currently to make before surgery, specific clinical signs cannot be described. Once MRI becomes more widely available, diagnosis in horses with occult carpal lameness suspected to originate from the medial palmar intercarpal ligament may be possible before arthroscopic examination. Tearing of the medial palmar intercarpal ligament was observed in 27 joints in 20 horses with carpal lameness.5 No correlation was found between tearing and severity of clinical signs. Joints with more medial palmar intercarpal ligament tearing had significantly less cartilage and subchondral bone damage, and an inverse relationship existed between the size and number of osteochondral fragments and ligament damage.5 Therefore, although tearing of the medial palmar intercarpal ligament occurred commonly in horses with middle carpal joint damage, tearing was not seen with severe subchondral bone damage, and what role damage plays in the development of joint disease remains questionable.
In my experience, tearing of the medial palmar intercarpal ligament is unusual without at least mild cartilage damage or osteochondral fragmentation, but I have seen a small number of horses in which the only identifiable lesion was tearing and hemorrhage of the frayed ends, resulting in hemarthrosis. Complete tearing of the medial palmar intercarpal ligament occurs more frequently in TB racehorses compared with STBs; partial tearing (fraying) of the medial palmar intercarpal ligament is quite common in STBs. In horses with a complete tear of the ligament, examining the palmar aspect of the middle carpal joint from the routine dorsal approach was possible. Rupture of the medial palmar intercarpal ligament has been seen in a small number of nonracehorse competition horses with pain localized to the middle carpal joint.62 No other lesion was identified during arthroscopic examination. I suspect tearing of the medial palmar intercarpal ligament in horses with confirmed carpal lameness, but in which scintigraphic and radiological findings are negative or equivocal, and in those with unexplained hemarthrosis of the middle carpal joint. Because horses that fall into this category are rare, prognosis is difficult to estimate.
Lateral Palmar Intercarpal Ligament
Avulsion injury at the origin of the lateral palmar intercarpal ligament on the ulnar carpal bone has been described and characterized, but I remain skeptical of this lesion as an authentic cause of lameness.63,64 Differentiation between genuine avulsion injury and the common radiological abnormalities such as radiolucent defects and fragments that occur commonly at the distal aspect of the ulnar carpal bone is difficult. I have not been able to document IRU on scintigraphic examination of horses with radiological evidence of fracture, radiolucent defects, or radiolucent defects with fragmentation, in this location (Figure 38-17). Fragments removed from this location histologically were consistent with fracture, and the authors differentiated fracture from the common cystic lesions that occur in this location by the presence of actual fragments and the position of the fragments at the palmar transition zone at the confluence of the lateral palmar intercarpal ligament.63 In the clinical report 26 of 37 horses underwent arthroscopic surgery to remove fragments and 20 returned to work, whereas five of nine horses managed conservatively returned to work.64 Scintigraphic examination was not performed, and complete clinical examination including diagnostic analgesia was not included for all horses.64 Careful clinical examination and advanced imaging may be necessary to differentiate horses with radiological abnormalities of the distal aspect of the ulnar carpal bone. It is possible that the presence of radiolucent defects, fragments, or a combination of radiological abnormalities in young untrained horses could be associated with the future development of other carpal lameness such as OA and osteochondral fragmentation, but to establish an association would require a large prospective clinical study.
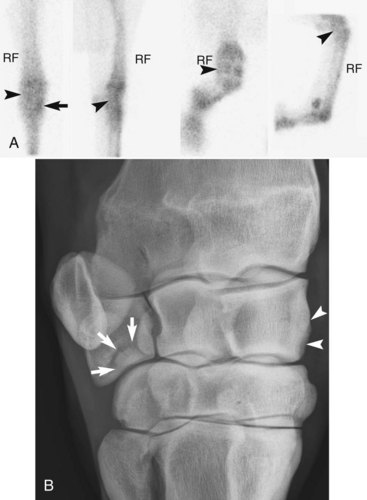
Fig. 38-17 A, Delayed-phase scintigraphic images of a 3-year-old Thoroughbred colt with mild increased radiopharmaceutical uptake (IRU) in the medial aspect of the right radial carpal bone (arrow). There is normal radiopharmaceutical uptake in the region of the ulnar carpal bone (arrowheads). B, Dorsal 45° lateral-palmaromedial oblique digital radiographic image of the right carpus showing mild enthesophyte and marginal osteophyte formation of the dorsomedial aspect of the radial carpal bone (arrowheads). Note also a bony fragment at the distal aspect of the ulnar carpal bone (arrows). This fragment is likely an incidental finding because IRU was not seen.
Collateral Ligament
Injury of the dense collateral ligaments of the carpus is rare (see Chapter 67). Usually fracture of the distal aspect of the radius, the carpal bones, or the proximal aspect of the McII and the McIV occurs instead of collateral ligament damage. In foals, collateral ligament laxity is seen commonly and is self-limiting but can contribute to the development of angular limb deformity. Three horses with collateral desmopathy remained lame despite prolonged rest, and ultrasonographic examination was useful to characterize the injury.65
Carpal Tenosynovitis and Flexor Tendonitis
See Chapters 69 and 75 for a discussion of carpal tenosynovitis and flexor tendonitis.
Exostoses of the Distal Caudal Aspect of the Radius
An unusual clustering of horses with carpal region pain as a result of carpal tenosynovitis from impingement of small exostoses of the caudal perimeter of the radial physis on structures of the carpal canal has been reported.66 I have seen three horses with carpal tenosynovitis as a result of irritation of deep surface of the deep digital flexor tendon by exostoses from the distal, caudal aspect of the radius and acute-onset lameness as a result of hemorrhage and inflammation of the carpal sheath. Signs resolved after tenoscopy and ostectomy. Radiological evidence of small exostoses of the distal, caudal radius is common, and careful clinical examination including diagnostic analgesia should be performed to ensure a correct diagnosis. See Chapters 70 and 75 for more information.
Carpal Hygroma
Hygroma refers to a sac, bursa, or cavity filled with fluid. Carpal hygroma usually results from direct and blunt trauma to the dorsal aspect of the joint, including the capsule and overlying extensor tendons and sheaths. Carpal hygroma is an occasional complication after arthroscopic surgery or arthrotomy of the carpus. During arthrotomy, a distinct subcutaneous space over the dorsal aspect of the carpus is encountered, but in most instances this is a potential rather than a real space. When traumatized, this space fills with fluid, resulting in a large sac. Initially, diffuse edema may be present, and horses may be lame, particularly after flexion, but lameness soon abates. A large, fluid filled, nonpainful swelling results that must be differentiated from extensor tenosynovitis (longitudinal swellings) and herniation of the middle carpal and antebrachiocarpal joint capsules (horizontal swellings). Lameness is usually not observed in horses with chronic hygroma unless a large swelling prohibits carpal flexion. Communication with an extensor sheath or joint capsule is rare, unless previous arthroscopic surgery has been performed and a portal inadvertently was made through a tendon sheath. In naturally occurring carpal hygroma a secretory lining is present, but it must develop from cell differentiation because communication with a source of synovial cells is lacking. Diagnosis is based on clinical signs. Positive contrast radiography and ultrasonographic examination are used to determine extent and communication with nearby structures.
The swelling is usually persistent, but it often does not compromise gait, although swelling does result in a cosmetic blemish. I have heard of resolution after injection with oxytetracycline, atropine, or contrast material. Drainage, with or without corticosteroid injection, and chronic bandaging are usually unsuccessful in permanently resolving swelling. Surgical management in the form of en bloc resection is the treatment of choice for cosmetic results. Simply draining the cavity and inserting through-and-through or closed-suction drains may temporarily resolve swelling, but recurrence is likely. I attempt resection en bloc without entering the hygroma cavity, but invariably the lining is penetrated. The lining is dissected from all overlying subcutaneous tissues and underlying capsule and tendon sheaths. Once the lining is removed, Penrose drains are placed, a light sterile bandage is applied, and horses recover with a sleeve cast-bandage that is left in place a minimum of 7 to 10 days. Drains are removed in 7 to 10 days when cast material is cut, and then the cast material can be used as a splint over a heavy padded bandage. Horses are given absolute stall confinement for 3 weeks. This treatment is successful but expensive.
Neoplasia
A rare cause of carpal region lameness is neoplasia. Lameness and progressive swelling were seen in a 20-year-old horse with chondrosarcoma of the distal aspect of the radius that caused bony proliferation and swelling of the antebrachiocarpal joint.67 I have seen an undifferentiated sarcoma of the distal aspect of the antebrachium causing progressive swelling, mild lameness, and a reduction in carpal flexion in a TB broodmare.
Hypertrophic Osteopathy
Lameness associated with hypertrophic osteopathy (see Chapters 15 and 37) is usually mild, and the condition does not directly affect the carpus, but fibrous and bony swelling of the distal aspect of the radius may cause enlargement of the antebrachiocarpal joint region, prompting radiographic examination.