Chapter 43The Metatarsal Region
The metatarsal region, like most of the distal hindlimb, has received little attention in previous lameness textbooks. However, it is a common source of lameness problems and should not be overlooked, especially in view of the high incidence of suspensory desmitis in sports horses.
Anatomy
The metatarsal region is bordered by the tarsometatarsal joint proximally and the metatarsophalangeal joint distally. The large third metatarsal bone (MtIII) provides all structural support and weight bearing and articulates predominantly with the third tarsal bone proximally and the proximal phalanx and proximal sesamoid bones (PSBs) distally. A prominent nutrient foramen in the MtIII should not be mistaken for a fracture and is usually located slightly higher than that of the third metacarpal bone (McIII).1
The second metatarsal bone (MtII) and fourth metatarsal bone (MtIV) are commonly referred to as the medial and lateral splint bones, respectively. The MtII articulates with the combined first and second tarsal bones proximally and ends distally with an enlarged “bell.” The MtIV articulates with the fourth tarsal bone proximally but transmits less load than the MtII. The dorsal metatarsal artery runs obliquely, in a distoplantar direction, in the proximal lateral aspect of the metatarsal region and then parallel and close to the dorsal aspect of the MtIV as it courses distally in the midmetatarsal region. The dorsal metatarsal artery then courses deep to the MtIV and must be avoided during distal splint ostectomy. I examined one horse in which the dorsal metatarsal artery coursed through a bony and fibrous ringlike foramen in the distal aspect of the MtIV and was inadvertently severed during ostectomy of the MtIV. Because the dorsal metatarsal artery is superficial, it can be lacerated from wounds in the lateral metatarsal region. Bleeding can be profound, and the ends of a lacerated dorsal metatarsal artery should be ligated unless anastomosis is performed with the horse under general anesthesia. Collateral circulation develops if ligation is necessary. The long plantar ligament attaches to the proximal aspect of the MtIV.
The orientation of the metatarsal bones is clinically important. The proximal aspect of the MtIV is large and is located in a more plantar location than its counterpart, the fourth metacarpal bone (McIV). This orientation makes it impossible to palpate the normal proximal and midbody portions of the suspensory ligament (SL). Therefore unless it is grossly enlarged, the SL cannot be palpated, and conditions such as mild-to-moderate suspensory desmitis can easily be missed, particularly if lameness is chronic and signs of acute inflammation are not present.
Dense metatarsal fascia attaches to the abaxial margins of the MtII and the MtIV and encircles the SL, deep digital flexor tendon (DDFT), and superficial digital flexor tendon (SDFT). A thinner fascia, the suspensory laminar fascia, lies superficial to the SL, deep to the DDFT. The metatarsal and laminar fascial layers appear confluent at the attachment on the MtII. Swelling of the SL within these fascial compartments can cause pain by compression of the adjacent metatarsal nerves.2 The SL has a broad origin on the proximal, plantar surface of the MtIII and a small attachment to the distal tarsal bones. The hind SL is slightly longer and thinner than the front SL, and muscle content may be higher in hindlimbs compared with forelimbs, which can complicate ultrasonographic examination.3 It has been suggested that the higher incidence of suspensory desmitis in Standardbreds (STBs) than in Thoroughbreds (TBs) is related to higher muscle content, but this is unproven.3
The plantar surface of the MtIII and the origin of the SL are oblique and not parallel to the dorsal surface of MtIII. During ultrasonographic examination, care should be taken to account for obliquity and to position the transducer perpendicular to SL fibers (see Chapter 72). The SL is bordered by the MtII and the MtIV and is thus trapped within a bony and dense soft tissue encasement. In the midmetatarsal region the body of the SL can be palpated as it emerges from this bony encasement and courses distally to divide into the medial and lateral branches that attach to the abaxial border of each PSB. The accessory ligament of the DDFT (ALDDFT) is usually present and is a variably sized structure ranging from thin to thick and occasionally has two or three parts; in a small proportion of horses (10 of 165, or 6.1%) there was no identifiable ALDDFT.4 Although the ALDDFT is anatomically present in most horses, injury is rare (see Chapter 71). Desmotomy to manage flexural deformity is rarely performed and generally would be ineffective because of the small size of the ALDDFT. I examined an aged Quarter Horse gelding with enlarged ALDDFTs with unusual flexural deformity characterized by intermittent, dynamic heel elevation; during walking the heels would land flat, but during standing the heels elevated bilaterally (see Chapter 71). I severed the ALDDFT in each hindlimb, and although improvement was seen temporarily, flexural deformity recurred. The DDFT is located plantar to the SL for most of the metatarsal region, but in the proximal metatarsal region it is positioned plantaromedially. The SDFT is located plantar to both the SL and DDFT. Because the tarsal sheath ends in the proximal metatarsal region, distention can sometimes be palpated (see Chapter 76). The digital flexor tendon sheath (DFTS) begins in the plantar, distal third of the metatarsal region and encompasses the DDFT and SDFT (see Chapter 74).
In the proximal third of the metatarsal region the lateral digital extensor tendon joins with the long digital extensor tendon, and the combined tendons course distally. The fibularis tertius and cranialis tibialis attach to the proximal, dorsal, and medial aspects of the MtIII. Osseous proliferation and fracture can occur at these locations.
Distal continuation of the superficial fibular and saphenous nerves provides dorsal skin sensation. The tibial nerve divides to form the medial and lateral plantar nerves in the plantar tarsal region. The lateral plantar nerve, which courses plantar to the origin of the SL, gives off a deep branch that innervates the proximal aspect of the SL and gives off branches, which continue distally as the lateral and medial plantar metatarsal nerves that course on the axial aspects of each respective splint bone (see Figure 10-22; Figure 43-1). Neurectomy of the deep branch of the lateral plantar nerve provides analgesia of the origin of the SL and the plantar cortex of the MtIII and partial analgesia of sites more distal to the level of and including the metatarsophalangeal joint. Accurate interpretation of diagnostic analgesia is critical when planning this surgical procedure. Neurectomy has received considerable attention recently as a surgical approach for management of proximal suspensory desmitis (PSD; see later).5,6 Histological changes consistent with nerve compression have been identified in horses undergoing neurectomy of the deep branch of the lateral plantar nerve, and nerve compression was proposed as a possible cause of residual pain in horses even after desmitis resolved.6 In that study, 62% of horses returned to soundness after neurectomy,6 whereas in a different study 19 of 20 horses treated by neurectomy and laminar fasciotomy returned to the previous level of performance.5 The deep branch of the lateral plantar nerve that was examined histologically6 lies within the dense metatarsal but outside the laminar fascial planes. Recognition of neuritis in this segment indicates that compression of the deep branch may be occurring within this fascial compartment. The lateral plantar nerve and its counterpart, the medial plantar nerve, continue distally between the SL and DDFT.
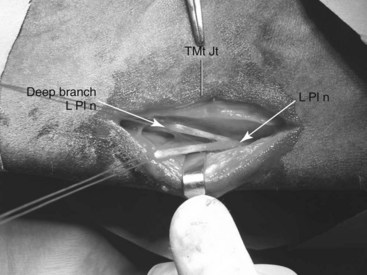
Fig. 43-1 Intraoperative photograph of a Warmblood gelding with chronic, recurrent proximal suspensory desmitis of the left hindlimb after a surgical approach to sever the deep branch of the lateral plantar nerve (L Pl n). The horse is in right lateral recumbency (proximal is to the right and dorsal is uppermost), the Kelly forceps is positioned at the level of the tarsometatarsal joint (TMt Jt), and the Senn retractors are positioned deep to the metatarsal fascia and superficial digital flexor tendon, both of which are retracted in a plantar direction. The parent lateral plantar nerve (L Pl n) coursing distally originates from the tibial nerve proximal to the tarsus and divides into a deep branch, a segment of which is removed during neurectomy, and then continues distally as the lateral plantar nerve. The deep branch further divides within the suspensory ligament and proximal metatarsal region to innervate the proximal aspect of the suspensory ligament and the plantar cortex of the third metatarsal bone; it then divides into lateral and medial plantar metatarsal nerves, which continue distally to innervate the fetlock joint (not shown, deep to the suspensory ligament).
Conformation
Sickle-hock and more important straight hindlimb conformation predispose to metatarsal region lameness (see Chapter 4).
Clinical Characteristics and Diagnosis of Lameness in the Metatarsal Region
There are no pathognomonic historical findings related to metatarsal region pain causing lameness. Palpation of the metatarsal region should be done with the horse in standing and non–weight-bearing positions. The metatarsal region cannot be adequately palpated when the horse is standing, because soft tissue structures in the proximal metatarsal region are not readily palpable in this position. Careful palpation for signs of inflammation and bony swelling should be performed with the limb in both positions. Even when the limb is flexed, it is still difficult to define the SL and DDFT proximally. However, it is possible to apply pressure over the proximal aspect of the SL to check for a painful response. In some horses with PSD, edema may be present or the area may feel full or slightly thickened, but dense fascia covering the SL and DDFT prevents expansion, and swelling may go undetected. A painful response to deep palpation over the proximal aspect of the medial splint bone and distal aspect of the tarsus, referred to as the Churchill test, may indicate the presence of referred pain and primary distal hock joint lameness, but in my experience this is a nonspecific test. Many horses with hindlimb lameness originating from sites other than the distal hock joints manifest a positive response to compression of both the medial and lateral splint bones and distal, medial aspect of the tarsus. Palpation of the dorsal cortex of the MtIII may reveal pain in trotters or other horses that interfere and may be an important finding, but palpation may not necessarily localize the primary source of pain that is causing lameness. Careful palpation of the abaxial and axial aspects of both splint bones is necessary to uncover hidden splint exostoses. Even subtle enlargement of the SL body, as it emerges from the bony encasement of the splint bones, that is accompanied by a painful response can indicate early suspensory desmitis. Both branches of the SL and attachments to the PSBs should be carefully palpated. Horses with a history of curb may develop progressive SDF tendonitis in the proximal metatarsal region, but this can easily be overlooked unless the area is carefully palpated (see Chapters 6, 69, and 78).
Diagnostic Analgesia
The high plantar perineural block (see Chapter 10) should be used to localize pain to the metatarsal region. Medial and lateral plantar nerves and medial and lateral plantar metatarsal nerves are blocked just distal (approximately 1.5 cm) to the tarsometatarsal joint (see Chapter 10). Variations of this block are often used, but it is important to recognize that subtarsal analgesic techniques targeting the lateral plantar nerve, or its deep branch, will not block the medial plantar nerve, and false-negative results could be obtained. More important, false-positive results incriminating the proximal aspect of the SL as a source of pain can occur. Subtarsal analgesia should be performed only after results of low plantar analgesia are observed, because most injection techniques in the subtarsal region are likely to desensitize the plantar metatarsal nerves, important contributors to innervation of the metatarsophalangeal joint. An injection technique was recently described for the diagnosis of PSD; the lateral plantar nerve is blocked approximately 15 mm distal to the head of the MtIV, just axial to the MtIV, at a depth of 25 mm.7 Although in theory this block is done in close proximity to the deep branch of the lateral plantar nerve, it is within the same fascial compartment as the parent branch, leading to the possibility of blocking this important contributor to distal limb innervation. If completed as a stand-alone technique without first performing low plantar analgesia, subtarsal analgesia may lead the clinician to the erroneous impression that pain is emanating from the proximal aspect of the SL. Management of horses with PSD by desmoplasty and fasciotomy was recently described, but criteria for inclusion of cases suggested that pain was localized to the proximal metacarpal or metatarsal region by use of only subcarpal or subtarsal analgesia without first blocking the distal aspect of the limb.8
In the forelimb, distal palmar outpouchings of the carpometacarpal joint complicate interpretation of diagnostic analgesic techniques. In the hindlimb, distal plantar outpouchings of the tarsometatarsal joint can potentially be penetrated when high plantar analgesic techniques are performed, but outpouchings of the joint were not seen in magnetic resonance images of cadaver specimens in a study comparing imaging modalities in the plantar metatarsal region.9 In an in vivo radiographic contrast study in only 5% of limbs was the tarsometatarsal joint inadvertently penetrated when injection mimicking high plantar analgesia was performed at a level of 1.5 cm distal to the tarsometatarsal joint, although in the same study inadvertent penetration of the tarsal sheath occurred in 40% of limbs.10 Care must be taken when interpreting diagnostic analgesia.
Imaging Considerations
Routine radiographic examination includes the dorsoplantar (DPl), lateromedial (LM), dorsolateral-plantaromedial oblique (DL-PlMO), and dorsomedial-plantarolateral oblique (DM-PlLO) images. In a DPl image of the proximal aspect of the MtIII, there is a normal area of mild increased radiopacity that should not be interpreted as modeling that is associated with stress reaction of the origin of the SL (Figure 43-2). Accurate assessment of the proximal aspect of the MtIII for the presence of increased radiopacity or avulsion fracture requires that radiographic views be centered at this level.

Fig. 43-2 Dorsoplantar radiographic image showing the normal coarse trabecular pattern (arrows) seen in the proximal aspect of the third metatarsal bone, which can be mistaken for increased radiopacity associated with the suspensory attachment. This Standardbred racehorse had a sagittal fracture of the talus. Note the radiolucency of the talus (open arrow).
Pool and delayed (bone) phase scintigraphic examination is quite useful to differentiate bone from soft tissue injury in horses with proximal plantar metatarsal pain and osteoarthritis. It is also useful to differentiate other conditions of the tarsometatarsal joint from those involving the proximal aspect of the MtIII. Focal increased radiopharmaceutical uptake (IRU) seen in delayed (bone) phase images involving the proximal plantar aspect of the MtIII is the most important scintigraphic finding in the metatarsal region. In TB and STB racehorses there is normally mild to mild-moderate IRU of the dorsal cortex of the MtIII, from the most proximal aspect to the mid-to-distal diaphysis. This finding was originally proposed to be age dependent because the dorsal cortex of the McIII could be “seen” scintigraphically as a normal finding in young but not older TB racehorses.11 In a population of predominantly sports horses and few racehorses the dorsal cortex was evident visually and with use of profile analysis in all horses regardless of age.12 When normal plantar scintigraphic images of the proximal metatarsal region are evaluated, there is usually asymmetrical radiopharmaceutical uptake (RU), with greater RU of the lateral aspect involving the lateral aspect of the MtIII and the MtIV. A central area of increased radiopacity seen radiologically (see Figure 43-2) does not appear to be active scintigraphically in normal horses. Asymmetrical RU was confirmed in a recent scintigraphic study of the proximal metacarpal and metatarsal regions in normal horses.13 Using region of interest analysis there was significantly higher RU in the lateral aspect of the metatarsal region compared with the medial aspect in plantar images, and significantly higher RU in the right proximal metatarsal region compared with the left. In lateral images there was maximum RU in the central and plantar aspect of the proximal metatarsal region. There was no effect of age on RU.13 In horses with PSD, visual appraisal and profile analysis of scintigraphic images failed to reveal abnormalities in most of 126 horses with forelimb or hindlimb lameness, but quantitative analysis using region of interest analysis revealed greater RU ratios in plantar images of lame limbs compared with nonlame limbs.14 Given that PSD is primarily a soft tissue injury, the lack of scintigraphic findings is easily understood; that many horses have chronic or recurrent hindlimb PSD could explain mild scintigraphic abnormalities found in plantar metatarsal images.
Ultrasonographic evaluation should be performed to evaluate the plantar soft tissue structures, the most important of which is the SL (see Chapters 16, 72, and 78). Computed tomography (CT) can be useful to evaluate complex fractures in the metatarsal region, the plantar cortex of the MtIII, and bony exostoses of the metatarsal bones (see Chapter 20). CT was useful in imaging new bone formation on the proximal plantar aspect of the MtIII in three horses with PSD that were successfully treated by ostectomy and osteostixis of the MtIII.15 Magnetic resonance imaging (MRI) is quite valuable in the diagnosis of PSD and for identifying adhesions between the MtII or the MtIV and the SL (see Chapters 21 and 37). In a study comparing the results of ultrasonography, MRI, and histology of the SL in the forelimb and hindlimb, the heterogeneity of the SL including the presence of muscular and adipose tissue, artifacts, and variable size were thought to be limitations of ultrasonographic examination.9 In the hindlimb the SL had a single large area of origin on the MtIII with a few fibers originating from the distal row of tarsal bones, was mildly bilobed in appearance, and was located slightly more laterally on the MtIII than at the corresponding position in the forelimb; significantly more muscular tissue was found laterally and similar sizes of the lateral and medial lobes were found.8 There was good correlation in morphology between MRI and histology, but cross-sectional area measurements were significantly higher with MRI than with either ultrasonography or histology, and histological cross-sectional area measurements were significantly higher than those obtained with ultrasonography.9 At the origin of the SL in the hindlimb, ultrasonographically determined cross-sectional area measurements were less than half of those determined using histology and MRI. Although relative measurements between limbs obtained using ultrasonography may be comparable, measurements between horses must be interpreted with caution.9 Measurement of plantar-to-dorsal thickness, however, was similar using all three modalities and may be the most useful measurement with which to compare sizes within and between horses.9 Ultrasonographic examination of the proximal aspect of the SL will likely underestimate cross-sectional area, and heterogeneity must be interpreted carefully. MRI was useful in characterizing injury and formulating management options in the proximal metacarpal and metatarsal regions of 45 horses, of which 13 horses had hindlimb PSD.16
Specific Conditions of the Metatarsal Region
Bucked and Sore Shins: Dorsal Cortical Fractures of the Third Metatarsal Bone
Modeling and remodeling of the dorsal cortex of the MtIII occur similarly to that of the McIII, but differences in load distribution between forelimbs and hindlimbs account for the relative lack of clinical signs associated with this process in the hindlimbs. Scintigraphic examination often reveals mild, diffuse IRU in the dorsal cortex of the MtIII in TB racehorses (see earlier discussion), but clinical signs of bucked shins are rare. In trotters common findings are pain on palpation, wounds and abrasions, and in some horses bony swelling that is associated with interference injury in the dorsal or dorsal medial metatarsal region. Although these areas are painful to palpation, most sites are a sign rather than the cause of a high-speed gait deficit. Finding evidence of interference injury, however, is quite important, because interference is often a sign of ipsilateral forelimb lameness and can be a cause of horses making breaks (going off stride). Dorsal cortical fractures are rare but can occur in TB and STB racehorses.
Medial and Lateral Condylar and Spiral Fractures of the Third Metatarsal Bone
Medial and lateral condylar and spiral fractures of the MtIII are discussed in Chapter 42.
Midshaft, Simple, or Comminuted Fractures of the Third Metatarsal Bone
Diaphyseal fractures of the MtIII can result from propagation and displacement of medial condylar fractures. Direct trauma is the most common cause, often from kicks by other horses. Complete fracture of the MtIII occurs in foals and adult horses. Critical prognostic factors are degree of comminution; proximity of the fracture to the metatarsophalangeal joint and tarsometatarsal joints; integrity of the vascular supply; whether the fracture is open or closed; degree of contamination if open; and the horse’s age, value, performance level, and intended use. Prognosis for adult horses with open, comminuted fractures of the MtIII is poor, but in those with closed, mildly comminuted or oblique fractures, repair is possible and prognosis is guarded to fair. Often, financial considerations are paramount in determining success with fractures of the metatarsal region in adult horses, because even if fractures are open and comminuted, advanced methods of repair and use of techniques such as intravenous regional limb perfusion may improve prognosis. The locking compression plate, designed with locking screws to provide a fixed-angle construct not dependent on the plate-bone interface being in compression, is ideal to use in horses with comminuted fractures and can be thought of as an internal-external fixator. This advanced system was successfully used in two horses recently and would be my choice if internal fixation was to be used in repair of a MtIII fracture.17 Horses with open fractures with gross contamination have a grave prognosis, regardless of age and degree of comminution, but those with small areas of skin loss and minor contamination can be successfully managed. Repair in horses with comminuted fractures involving the tarsometatarsal joint is difficult, but transfixation pin casts using the distal tibia and distal aspect of the MtIII could be considered. In foals, vascular supply of the limb distal to a fracture is a concern and should be assessed clinically or by using angiography or Doppler ultrasonography. Prognosis in foals with simple or mildly comminuted midshaft MtIII fractures repaired using one or two dynamic compression plates is fair to good (Figure 43-3). In foals, external coaptation often causes profound flexor tendon laxity and should be avoided. External skeletal fixation by using pins and sidebars of casting material or acrylic is possible in a foal. In adult horses, methods of stabilization and repair include internal fixation using two bone plates, locking compression plates or a combination of limited-contact dynamic and locking compression plates, transfixation pin casts in combination with internal fixation, and casts alone.

Fig. 43-3 This open (mildly contaminated) midshaft fracture of the third metatarsal bone in a 4-month-old Thoroughbred colt was successfully managed using two dynamic compression plates and a half-limb bandage. A, The preoperative and B, postoperative appearance of the third metatarsal bone are shown. The plates were removed 4 months later.
Of 25 horses with MtIII or McIII fractures that were managed with internal fixation, external coaptation, or both, age, sex, weight, and the limb affected were not related to outcome, but affected horses were younger than the general hospital population. Seventeen horses had open fractures, and infection was the most common complication after surgery.17 Nonunion in an infected fracture was the most common reason for failure (seven horses). Of 24 horses in which outcome was determined, 16 (67%) had healed fractures and 12 (50%) horses were sound for the intended use.17 Intended use was not defined; therefore prognosis in foals for future racing could not be determined. Of 37 horses and foals undergoing transfixation pin casting for management of difficult fractures, 10 of 15 horses (67%) in which fractures involved the McIII or the MtIII survived, a prognosis level similar to that seen with internal fixation.18,19 Five of six horses, including both foals, managed with transfixation pin casting of the MtIII fractures survived.19 Transfixation pin casting is often chosen when fractures are difficult or open, when there is gross contamination, and when financial constraints preclude use of expensive implants such as the locking compression plates and screws.
Physeal Fractures of the Distal Aspect of the Third Metatarsal Bone
The most common fracture of the distal MtIII physis is a Salter-Harris type II fracture, but various other fractures can occur. These fractures are usually quite stable, but perfect reduction is difficult to achieve. Fracture reduction and external coaptation are usually successful, but insertion of one or two 3.5- or 4.5-mm bone screws in the metaphyseal component may help stabilize the fracture and reduce the time necessary for external coaptation. Even short periods of cast immobilization in foals can cause rapid onset of flexor tendon laxity. Cast-bandage and bandage-splint combinations are preferred in young foals that are only several weeks old.
Incomplete Longitudinal Fractures of the Plantar Aspect of the Third Metatarsal Bone and Stress Reactions
Incomplete longitudinal fractures of the plantar cortex of the MtIII occur considerably less frequently than those of the McIII. Stress reactions of the MtIII, defined as focal areas of IRU without radiological confirmation of fracture, occur as part of a continuum of stress-related bone injury at the origin of the SL. Combined MtIII injury and PSD worsens prognosis, and it is important to establish whether injury involves bone, soft tissue, or both (see Chapters 37 and 72).
Transverse Stress Fractures of the Distal Aspect of the Third Metatarsal Bone
Transverse stress fractures of the distal aspect of the McIII are described in Chapter 37. I have not recognized this specific fracture type in the MtIII.
Avulsion Fractures of the Third Metatarsal Bone Associated with the Origin of the Suspensory Ligament
Avulsion fractures of the MtIII that are associated with the origin of the SL are frequently seen and can be solitary injuries or associated with PSD. Horses can have acute-onset or chronic mild-to-moderate hindlimb lameness, depending on size and duration of fracture. Fractures occur most commonly in dressage horses, jumpers, and STB racehorses. Local signs of swelling are usually absent, and diagnostic analgesia is essential for localization of pain. Focal areas of IRU are seen that are roughly triangular and involve the proximal plantar aspect of the MtIII (Figure 43-4). It is important to differentiate IRU from that seen in the tarsometatarsal joint, but concomitant IRU in both areas is not unusual. A well-defined fracture is often not detectable radiologically, and usually only suspicious areas of radiolucency and increased radiopacity are seen. Bilateral avulsion fractures or stress reactions occur. Conservative management using a progressive increase in exercise without turnout is usually successful. Recurrence is common and most likely in horses that have associated PSD (see Chapter 72).
Articular Fracture of the Dorsoproximolateral Aspect of the Third Metatarsal Bone
Articular fracture of the dorsoproximolateral aspect of the MtIII occurs primarily in STB and TB racehorses.20,21 Acute onset of lameness is common, but a history of either chronic, undiagnosed hindlimb lameness or lameness referable to the distal hock joints is usually uncovered. This fracture occurs most commonly in horses with sickle-hock conformation, a conformational abnormality that predisposes to dorsal and plantar tarsal and proximal metatarsal injury, and may worsen prognosis. This fracture occurs most frequently in horses in the later stages of training, but often before racing, a clinical characteristic that may worsen prognosis. Acute soft tissue swelling is rare. A small bony enlargement is often palpable but is easy to miss. Horses exhibit a positive response to upper limb flexion and to focal, deep pressure over the dorsolateral aspect of the MtIII. Lameness partially resolves after intraarticular analgesia of the tarsometatarsal joint or perineural analgesia of the fibular and tibial nerves. Initial radiological examination reveals the presence of bony proliferation, indicating that bone modeling preceded acute fracture (Figure 43-5). Incomplete fractures are most common, but complete and mildly displaced fractures also occur. Scintigraphic examination is useful in differentiating this fracture from other conditions involving the tarsometatarsal joint and those involving the proximal plantar aspect of the MtIII. Radiographs and scintigraphic images of the contralateral hindlimb often reveal similar but less pronounced changes.

Fig. 43-5 Dorsomedial-plantarolateral xeroradiographic image of the hock and proximal metatarsal region of a Standardbred racehorse. There is an articular fracture of the dorsoproximolateral aspect of the third metatarsal bone (MtIII) (arrows). Note the bone modeling of the proximal aspects of the MtIII that preceded the fracture.
Because proliferative changes precede fracture, it is presumed that the cause involves chronic fatigue and stress-related bone injury. Attachment of the tendons of the fibularis tertius and cranialis tibialis muscles likely contributes substantially to bone stress and may play a role. Concomitant radiological evidence of osteoarthritis involving the dorsal aspect of the tarsometatarsal and centrodistal joints and dorsoproximolateral fracture of the MtIII is common.
Conservative management is advised in horses with incomplete fractures, but in those with displaced fractures, internal fixation using one or two 3.5-mm bone screws placed in lag fashion is advised. If horses raced before fracture, the prognosis for future racing is good but only fair to guarded for returning to or sustaining racing in the same class. Horses that develop this fracture before actual racing begins have a poor prognosis. When horses return to training or racing, progressive osteoarthritis of the tarsometatarsal and centrodistal joints appears to be a limiting factor even when the fracture heals and proliferative changes on the MtIII smooth.
Exostoses of the Second, Third, and Fourth Metatarsal Bones
Exostoses of the metatarsal bones (splint exostoses, splints) occur considerably less commonly than those involving the metacarpal bones, but they can cause lameness, or in racehorses, high-speed soreness. However, it is common to find large exostoses involving the proximal lateral aspect of the MtIII or MtIV as an incidental finding that is usually not associated with lameness, although the lesion is scintigraphically active. Splint exostoses can be caused by direct trauma or instability between the metatarsal bones. There is a common misconception that splints arise from tearing of the interosseous ligaments between the MtII or MtIV and the MtIII, but many splints do not involve the space between bones, and it is difficult to believe that instability and primary desmitis adequately explain the cause of splints. Many splints in the hindlimb involve the MtIII alone (and not the MtII or the MtIV), although the MtII and the MtIV can be affected. Axially located exostoses (blind splints) do occur and are most important proximally, where bony proliferation could crowd or impinge on the proximal aspect of the SL and lateral and medial plantar metatarsal nerves. Adhesions may occur between the axial aspect of the exostosis and the SL and other nearby soft tissue structures, but lameness from adhesions and encroachment into the region of the SL appears to involve the McII or McIV most commonly. Direct trauma from interference injury is the most likely cause of most medially located splints. Faulty conformation does not appear to play a prominent role. Mature distal splint exostoses may predispose the MtII and MtIV to fracture in horses with progressive enlargement of the SL.
Lameness associated with splint exostoses is usually mild (grade 1 to  of 5). Direct palpation elicits a painful withdrawal response, and lameness is exacerbated. Infiltration of local anesthetic solution alleviates pain and a majority of observed lameness, but perineural analgesia of the lateral plantar metatarsal and lateral plantar nerves, or medial plantar metatarsal and medial plantar nerves proximal to exostoses involving the MtIV and the MtII, respectively, may be required. Radiographs should be obtained when a fracture is suspected but otherwise yield little useful information unless there is drainage associated with bony proliferation.
of 5). Direct palpation elicits a painful withdrawal response, and lameness is exacerbated. Infiltration of local anesthetic solution alleviates pain and a majority of observed lameness, but perineural analgesia of the lateral plantar metatarsal and lateral plantar nerves, or medial plantar metatarsal and medial plantar nerves proximal to exostoses involving the MtIV and the MtII, respectively, may be required. Radiographs should be obtained when a fracture is suspected but otherwise yield little useful information unless there is drainage associated with bony proliferation.
Management of horses with splint exostoses includes local cold therapy, including cold water hosing and icing, the application of a poultice and bandaging, and the administration of nonsteroidal antiinflammatory drugs (NSAIDs). Injections of methylprednisolone acetate (80 mg) and Sarapin, an extract of the pitcher plant (6 mL), subcutaneously and axially if needed for each exostosis reduce inflammation and pain. Repeat injections are often necessary. Cryotherapy is popular in racehorses, but clinicians should be aware that superficial skin pain persists for several weeks afterward, which leaves few ways to monitor improvement other than to monitor performance. Surgical removal of persistently painful exostoses by periostectomy, ostectomy of exostoses without removing the parent MtII or MtIV, adhesiolysis, and fasciotomy can be performed if exostoses involve the axial aspects and encroach on or are adhered to the SL. Surgery is usually not required for abaxially located splint exostoses.
Fractures of the Second and Fourth Metatarsal Bones
Fractures of the MtII and MtIV occur primarily as a result of direct trauma from either a kick from another horse or kicking into or through a stationary object. The MtIV is injured most commonly. Simple, comminuted, and displaced fractures occur, and often wounds extend directly into the fracture site. The MtIV bears little load and appears to have remarkable recuperative ability. Diagnosis is usually straightforward, particularly if a wound is involved, but in some horses the presence of chronic lameness or drainage several weeks after injury prompts later radiographic examination, and only then is fracture diagnosed. Radiographs often reveal extensive comminution, but in many horses, basic axial alignment of fragments is maintained. When fractures of either the MtIV or MtII involve the tarsometatarsal joint, and particularly if fractures are open, infectious arthritis and osteoarthritis are possible but may be amenable to treatment.
The majority of MtIV fractures heal with conservative management, despite comminution and infectious osteitis, with appropriate antimicrobial administration and wound care. Loose subcutaneously located fragments can be removed with ease and deep tissue samples should be collected for bacterial culture and antimicrobial susceptibility testing. Although internal fixation,22 total ostectomy of the MtIV,23 and segmental ostectomy24 have been described, I have rarely found it necessary to contemplate surgery, with the exception of removing loose bone fragments from wounds or persistently draining tracts (Figure 43-6). Comminuted fractures with an intact column of bone will heal satisfactorily in most horses, although delayed unions or nonunions requiring surgical intervention occur infrequently. Horses may need 4 to 6 months of rest, and long-term antimicrobial therapy (4 to 8 weeks) may be necessary in horses with open or infected fractures. Impingement on the SL function by callus from fracture healing is a possible complication but is unusual. Fractures of the mid and distal aspects of the MtII and MtIV are caused by chronic suspensory desmitis involving the body or branches. Suspensory desmitis is primary and MtII and MtIV fractures are secondary, resulting from a bowstring effect of the enlarging SL. Occasionally, axially located callus from an old splint bone fracture may cause mild lameness from local irritation of the nearby SL. Local injections of antiinflammatory agents resolve pain in most instances, but occasionally exostoses and the distal aspect of the splint bone are removed.
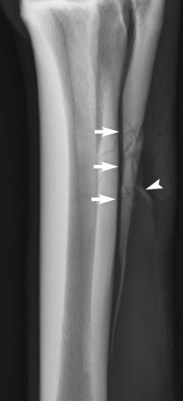
Fig. 43-6 Dorsal 45° lateral-plantaromedial oblique digital radiographic image of a horse with an open, comminuted fracture of the fourth metatarsal bone (MtIV) (arrows). As long as an intact column of bone is present, fractures of the MtIV will often heal without major surgical intervention except for removal of loose fragments (arrowhead) through the original wound. Long-term management with antimicrobial agents and rest is necessary.
Ostectomy of distal fragments of the MtII and MtIV can be performed in combination with SL splitting and, in some horses, with ostectomy of apical or abaxial fracture fragments of the PSBs. A triad of clinical problems involving the SL, splint bone, and PSBs (called the three Ss) is often seen, and all three structures should be evaluated before management and prognostic recommendations are made.
Enostosis-like Lesions of the Third Metatarsal Bone
During scintigraphic examination, single or multifocal areas of IRU within the medullary cavity of the MtIII are occasionally seen, and intensity can range from mild to intense. Subsequent radiological examination reveals one or more round to irregularly shaped radiopacities within the medullary cavity. Lameness in horses with enostosis-like lesions of the MtIII is unusual, particularly if there are small, focal areas of IRU involving only the area around the nutrient foramen. Of 17 enostosis-like lesions (in 10 horses), four lesions were identified in the MtIII, but in only one horse was lameness localized to the metatarsal region.25 Lameness, if present, should abate with a high plantar block and resolves with rest and the administration of NSAIDs.
Suspensory Desmitis
Suspensory desmitis, including PSD, suspensory body desmitis, and suspensory branch desmitis and associated bony injury, is the most important cause of lameness in the metatarsal region (see Chapter 72).
Hindlimb proximal and proximal and body desmitis are career-threatening injuries and horses should be managed aggressively. Managing horses with hindlimb suspensory desmitis is exceedingly more challenging than managing those with similar forelimb injuries—the proverbial apples and oranges comparison. One of the Editors (SJD) has written extensively on the subject and aptly points out that the prognosis in horses with acute forelimb PSD approaches 90%, whereas prognosis in those with acute hindlimb desmitis managed conservatively is 14%.26 I have managed 23 horses, 13 nonracehorses (dressage horses, jumpers, event horses) and 10 STB trotters, with confirmed proximal and body suspensory desmitis by using autogenous bone marrow injection27 and proximal metatarsal fasciotomy. Horses are placed under general anesthesia, and a medial approach is used to gain access to the proximal aspect of the SL (Figure 43-7). A large volume, 30 to 60 mL, of liquid bone marrow is harvested from the sternum and injected directly into the proximal aspect of the SL and body as determined by ultrasonographic evaluation. The dense, overlying medial metatarsal fascia is transected from the level of just proximal to the tarsometatarsal joint to the midbody region. Although no attempt was made to separately incise the laminar suspensory fascia, this fascial layer is confluent with the overlying metatarsal fascia along the axial aspect of the MtII. The subcutaneous tissues and skin are closed. Horses should be given 4 to 6 months of progressive increase in exercise, including 4 weeks of stall rest, followed by 4 weeks of stall rest with handwalking, 4 weeks of walking with a rider up or in the jog cart, and then 4 weeks of walking and light trotting. Turnout exercise is forbidden. Of 13 nonracehorses, eight (62%) returned to full work, three of these to elite competition; one horse returned to a lower level of competition, but lameness persisted or recurred in four horses. Of 10 trotters, eight raced but only two raced more than five starts without recurrence of desmitis. Hindlimb suspensory desmitis in the trotter is a substantial cause of lameness and is career-limiting. Whether improvement in some horses may result from reparative processes accelerated by the transfer of stem cells, the injection of growth factor–rich substrate into damaged SLs (see Chapters 72 and 73), fasciotomy and relief of compartment syndrome, or a combination of factors is unknown. In an experimental study, acellular bone marrow was significantly better than platelet-rich plasma and growth factors in stimulating cartilage oligomeric matrix protein production in an in vitro study using cultured SL fibroblasts.28 See Chapters 72 and 73 for a complete discussion regarding alternative approaches to healing, reparative and regenerative healing, and other aspects of management of suspensory desmitis. Numerous other management options are available including stem cell therapy (see Chapter 73), a combination of desmoplasty (splitting) and fasciotomy,8 fasciotomy and neurectomy of the deep branch of the lateral plantar nerve,4 and radial pressure wave therapy.29 Realistically, prognosis is only guarded to fair for return to the same level of competition, particularly in elite horses and STB trotters, and to date, a method of management suitable for all horses is not available. Accurate diagnosis and imaging must be performed to authenticate location and source of pain. Prognosis is particularly guarded in older Warmblood horses with desmitis extending into the body of the SL with palpably thickened metatarsal regions, in those with straight hindlimb conformation and with hyperextension of the metatarsophalangeal joints (dropped fetlock joints), and in those in which desmitis is chronic and recurrent. A particularly severe form of suspensory desmitis is seen in some Warmblood horses, and may possibly be associated with pathological accumulation of proteoglycans in connective tissues, and resembles the degenerative suspensory disorder known to occur in the Peruvian Paso and related breeds.30,31 Horses can have severe unilateral or bilateral desmitis with severe lameness and hyperextension of the hock and fetlock joints and are most often refractory to treatment.

Fig. 43-7 An anatomy specimen (A) and a cadaver specimen (B) showing the location and approach (dotted line) for bone marrow injection and fasciotomy used in management of horses with proximal suspensory and body desmitis. Dense metatarsal fascia is being retracted using Allis tissue forceps, exposing the origin of the suspensory ligament (curved Kelly forceps is positioned plantar to the suspensory ligament).
Tenosynovitis of the Digital Flexor Tendon Sheath
Tenosynovitis of the DFTS is discussed in Chapter 74.
Desmopathy of the Accessory Ligament of the Deep Digital Flexor Tendon
Desmitis of the ALDDFT is discussed in Chapter 71.
Deep Digital Flexor Tendonitis
Deep digital flexor tendonitis is discussed in Chapters 70, 76, and 78.
Superficial Digital Flexor Tendonitis
Tendonitis of the superficial digital flexor (SDF) is an unusual-to-rare cause of lameness, but it occurs in racehorses with chronic, progressive curb and in any type of sports horse as a result of direct trauma (see Chapter 78). SDF tendonitis may be obvious clinically or may be more subtle and requires careful palpation and ultrasonographic examination for confirmation of diagnosis. STB and TB racehorses with spontaneous SDF tendonitis invariably have sickle-hock conformation. The points of the hock should be compared, because in some horses loss of support accompanies SDF tendonitis and is a negative prognostic sign. Long-term rest has been successful in pacers, but trotters and TB racehorses have a poor prognosis for returning to racing. Most horses, regardless of breed or gait, drop in race class.
Undiagnosed Metatarsal Region Lameness
In a small proportion of horses, lameness can be localized to the metatarsal region by high plantar analgesia, but comprehensive imaging fails to identify a source of pain. I believe most of these horses have PSD and pain from subtle swelling of the SL. Measurement of the cross-sectional area and comparison with the contralateral limb are useful. Horses with lameness inappropriate for the degree of injury confirmed using radiographic and ultrasonographic examinations should be referred for scintigraphic examination and are likely candidates for MRI or CT examination. Pain associated with the distal tarsal joints and tarsal sheath occasionally can be abolished using high plantar analgesic techniques, a fact that must be kept in mind in horses in which a diagnosis in the metatarsal region cannot be made.
Wounds of the Metatarsal Region
Wounds involving the metatarsal region are common and can be simple and involve the skin and subcutaneous tissues, but they are often complex and involve bone and deep soft tissue structures. Lacerations often involve the extensor and digital flexor tendons (see Chapter 81), and those involving the digital flexor tendons have serious implications for future performance and salvage. Laceration of the long digital extensor tendon often delays healing of overlying wounds because movement of tendon ends exacerbates granulation tissue formation and delays wound contraction and epithelialization. Horses with long digital extensor tendon lacerations knuckle initially, but functional healing of the tendon most often results. A common wound is a distal-based flap wound that exposes the dorsal cortex of the MtIII and often is associated with extensor tendon lacerations. Because the skin base is distal, much of the proximal, triangular section of skin becomes necrotic. The skin should not be removed prematurely. Osteitis of the MtIII from direct trauma, drying from exposure, superficial infection, and loss of blood supply may prolong healing. Occasionally, large areas of the dorsal cortex of the MtIII have radiological characteristics of sequestra, but in many horses surgical removal or curettage is not required. In my experience, many horses have received unnecessary surgery to remove damaged areas of the MtIII cortex that if left in place would likely have healed uneventfully. However, horses that develop extensive proliferative changes of the MtIII usually have adhesions to the long digital extensor tendon and often have chronic lameness.
Small puncture wounds may result in localized osteitis of the MtII or MtIV. Removal and curettage should be reserved for those with purulent drainage refractory to management with antimicrobial therapy. Horses without drainage but with radiological evidence of fragmentation within a radiolucent defect can be managed conservatively unless expedient resolution of the problem is mandatory. Horses with wounds and evidence of MtIII cortical crushing or obvious fractures should be managed with caution because catastrophic fracture could develop. Of substantial risk are those with acute, cortical fractures that resemble true saucer fractures. If horses are placed under general anesthesia to remove what is misinterpreted as devitalized pieces of cortex, there is a risk for catastrophic fracture during recovery from general anesthesia.
Acquired or secondary stringhalt is an unusual complication from metatarsal region wounds involving the long digital extensor tendon and sometimes the lateral digital extensor tendon. Horses at risk are those with extensive proliferation of the MtIII and adhesion formation with the overlying long digital extensor tendon. Mechanisms to account for the development of stringhalt include adhesion formation and interruption of the normal myotactic reflex.32 Of 10 horses that developed stringhalt after dorsal metatarsal trauma, six horses developed stringhalt within 3 months, three developed stringhalt after 3 months, and in one horse time of injury to development of stringhalt was undetermined.32 Of four horses managed with rest and progressive exercise, stringhalt resolved in one, improved in two, and remained the same in one horse.32 Of five horses that received surgical management using lateral digital extensor myotenectomy, stringhalt resolved in two, improved in two, and remained the same in one horse.31 In my limited experience with this condition, prognosis is guarded to poor for complete resolution of the gait deficit.
Diffuse Swelling in the Metatarsal Region
Diffuse swelling in the metacarpal region is discussed in Chapter 37, and this also applies to the metatarsal region.
Severe Cellulitis of the Metatarsal Region
Cellulitis of the hindlimb occurs frequently from kick wounds or other trauma. In many horses obvious signs of trauma are lacking, but severe lameness and signs of infection in the metatarsal region occur. A severe form of cellulitis occurs primarily in TB racehorses in which severe lameness, swelling, and fever develop, apparently from a very small skin wound or excoriation, because an obvious wound is most difficult to find. This condition is similar to focal, peritarsal cellulitis (see Chapters 44 and 107). Initially it is difficult to differentiate cellulitis from infection of the tarsal sheath, SDFT, DDFT, and the DFTS, because swelling is diffuse and horses are severely lame. Within 48 to 72 hours, skin necrosis and sloughing can occur, which exposes an underlying and sometimes infected SDFT. Staphylococcus and occasionally Streptococcus species are cultured. Laminitis in the contralateral limb is a risk initially. Skin sloughing can be pronounced and requires weeks to months of wound care and, in some horses, grafting. Involvement of the underlying SDFT and other soft tissue structures is a poor prognostic sign.
