Alharbi, M, Pinto, G, Finidori, G, et al. Pamidronate treatment of children with moderate-to severe osteogenesis imperfect: a note of caution. Horm Res. 2009;71(1):38–44.
American Academy of Orthopaedic Surgeons, Keep injured high school athletes out of the game. Your Orthopaedic Connection 2007. available at http://orthoinfo.aaos.org/topic.cfm?topic=A00048 [(accessed August 1, 2009)].
American Academy of Pediatrics, Committee on Nutrition. Pediatric nutrition handbook, ed 6. Elk Grove Village, Ill: The Academy; 2009.
American Academy of Pediatrics. Use of performance-enhancing substances. Pediatrics. 2005;115(4):1103–1106.
American Academy of Pediatrics, Committee on Sports Medicine and Fitness. Climatic heat stress and the exercising child and adolescent. Pediatrics. 2000;106(1):158–159.
American Academy of Pediatrics, Committee on Sports Medicine and Fitness. Medical concerns in the female athlete. Pediatrics. 2000;106(3):610–613.
American Academy of Pediatrics, Section on Rheumatology and Section on Ophthalmology. Guidelines for ophthalmologic examinations in children with juvenile rheumatoid arthritis. Pediatrics. 1993;92(2):295–296.
Bachrach, LK, Ward, LM. Clinical review 1: bisphosphonate use in childhood osteoporosis. J Clin Endocrinol Metab. 2009;94(2):400–409.
Benseler, SM, Silverman, ED. Neuropsychiatric involvement in pediatric systemic lupus erythematosus. Lupus. 2007;16(3):564–571.
Bloom, BJ, Owens, JA, McGuinn, M, et al. Sleep and its relationship to pain, dysfunction and disease activity in juvenile rheumatoid arthritis. J Rheumatol. 2002;29(1):169–173.
Borse, NN, Gilchrist, J, Dellinger, AM, et al. CDC childhood injury report: patterns of unintentional injuries among 0-19 year olds in the United States, 2000-2006. Atlanta: Centers for Disease Control and Prevention; 2008.
Boyd, AS, Benjamin, HJ, Asplund, C. Principles of casting and splinting. Am Fam Physician. 2009;79(1):16–22. [23-24].
Brenner, JS, Council on Sports Medicine and Fitness. Overuse injuries, overtraining, and burnout in child and adolescent athletes. Pediatrics. 2007;119(6):1242–1245.
Brown, JC, Klein, EJ, Lewis, CW, et al. Emergency department analgesia for fracture pain. Ann Emerg Med. 2003;42(2):197–205.
Bullock, DP, Koval, KJ, Moen, KY, et al. Hospitalized cases of child abuse in America: who, what, when, and where. J Pediatr Orthop. 2009;29(3):231–237.
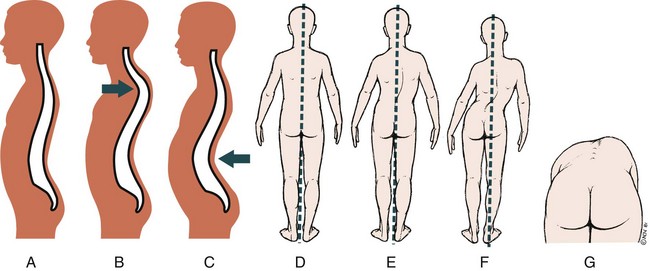
Bunnell, WP. Selective screening for scoliosis. Clin Orthop Relat Res. 2005;434:40–45.
Burmester, GR, Mease, PJ, Dijkmans, BA, et al. Adalimumab safety and mortality rates from global clinical trials of six immune-mediated inflammatory diseases. Ann Rheum Dis. 2009;68(12):1863–1869.
Calfee, R, Fadale, P. Popular erogenic drugs and supplements in young athletes. Pediatrics. 2006;117(3):e577–e589.
Cassidy, J, Kivlin, J, Lindsley, C, et al. Ophthalmologic Examinations in Children with juvenile rheumatoid arthritis. Pediatrics. 2006;117(5):1843–1845.
Chorley, JN. Ankle sprain discharge instructions from the emergency department. Pediatr Emerg Care. 2005;21(8):498–501.
Cimpello, LB, Khine, H, Avner, JR. Practice patterns of pediatric versus general emergency physicians for pain management of fractures in pediatric patients. Pediatr Emerg Care. 2004;20(4):228–232.
Clark, E, Plint, AC, Correll, R, et al. A randomized, controlled trial of acetaminophen, ibuprofen, and codeine for acute pain relief in children with musculoskeletal trauma. Pediatrics. 2007;119(3):460–467.
Cornwall, R. Upper limb. In Kliegman RM, Behrman RE, Jenson HB, et al, eds.: Nelson textbook of pediatrics, ed 18, Philadelphia: Saunders, 2007.
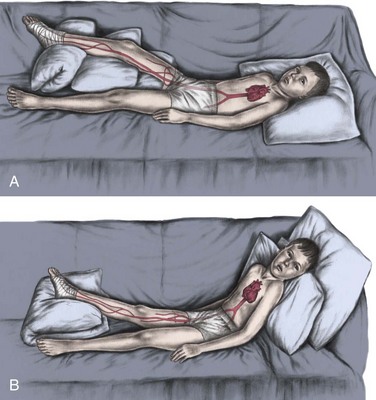
Curley, MA, Razmus, IS, Roberts, KE, et al. Predicting pressure ulcer risk in pediatric patients: the Braden Q Scale. Nurs Res. 2003;52(1):22–33.
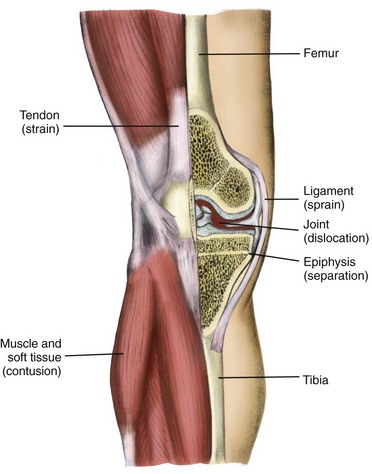
DiFazio, R, Atkinson, CC. Extremity fractures in children: when is it an emergency? J Pediatr Nurs. 2005;20(4):298–304.
Doyle, GS, Taillac, PP. Tourniquets: a review of current use with proposals for expanded prehospital use. Prehosp Emerg Care. 2008;12(2):241–256.
Drendel, AL, Lyon, R, Bergholte, J, et al. Outpatient pediatric pain management practices for fractures. Pediatr Emerg Care. 2006;22(2):94–99.
Drezner, JA, Chun, JS, Harmon, KG, et al. Survival trends in the United States following exercise-related cardiac arrest in the youth, 2000-2006. Heart Rhythm. 2008;5(6):794–799.
Drezner, JA, Courson, RW, Roberts, WO, et al. Inter Association Task Force recommendations on emergency preparedness and management of sudden cardiac arrest in high school and college athletic programs: a consensus statement. Prehosp Emerg Care. 2007;11(3):253–271.
Drezner, JA, Rao, AL, Heistand, J, et al. Effectiveness of emergency response planning for sudden cardiac arrest in United States high schools with automated external defibrillators. Circulation. 2009;120(6):518–525.
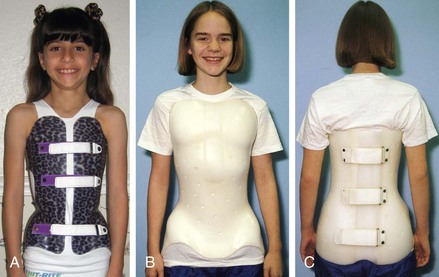
Fisher, TJ, Williams, SL, Levine, AM. Spinal orthosis. In Browner BD, Jupiter JB, Levine AM, et al, eds.: Skeletal trauma: basic science, management, and reconstruction, ed 4, Philadelphia: Saunders, 2008.
Foeldvari, I, Wierk, A. Methotrexate is an effective treatment for chronic uveitis associated with juvenile idiopathic arthritis. J Rheumatol. 2005;33(2):362–365.
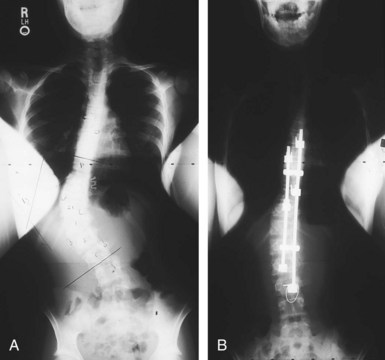
Freeman, BL, III. Scoliosis and kyphosis. In Canale ST, Beaty JH, eds.: Campbell’s operative orthopaedics, ed 11, Philadelphia: Mosby, 2007.
Friday, JH, Kanegaye, JT, McCaslin, I, et al. Ibuprofen provides analgesia equivalent to acetaminophen-codeine in the treatment of acute pain in children with extremity injuries: A randomized clinical trial. Acad Emerg Med. 2009;16(8):711–716.
Graham, JM, Gomez, M, Halberg, A, et al. Management of deformational plagiocephaly: repositioning versus orthotic therapy. J Pediatr. 2005;146(2):258–262.
Green, NE, Swiontkowski, MF. Skeletal trauma in children, ed 4. Philadelphia: Mosby/Elsevier; 2008.
Gregory, AJM, Fitch, RW. Sports medicine: performance-enhancing drugs. Pediatr Clin North Am. 2007;54(4):797–806.
Gutierrez, K. Bone and joint infections in children. Pediatr Clin North Am. 2005;52(3):779–794.
Hart, ES, Grottkau, BE, Albright, MB. Slipped capital femoral epiphysis: don’t miss this pediatric hip disorder. Nurs Pract. 2007;32(3):14. [16-18, 21].
Hayata, AL, Borba, EF, Bonfa, E, et al. The frequency of high/moderate lipoprotein risk factor for coronary artery disease is significant in juvenile-onset systemic lupus erythematosus. Lupus. 2005;14(8):613–617.
Hazinski, MF, Markenson, D, Neish, S, et al. Response to cardiac arrest and selected life-threatening medical emergencies: the medical emergency response plan for schools: a statement for healthcare providers, policymakers, school administrators, and community leaders. Pediatrics. 2004;113(1):155–168.
Holmes, SB, Brown, SJ, Pin Site Care Expert Panel. Skeletal pin site care: National Association of Orthopaedic Nurses guidelines for orthopaedic nursing. Orthop Nurs. 2005;24(2):99–107.
Hosalkar, HS, Horn, D, Friedman, J, et al. The hip. In Kliegman RM, Behrman RE, Jenson HB, et al, eds.: Nelson textbook of pediatrics, ed 18, Philadelphia: Saunders, 2007.
Houghton, KM, Tucker, LB, Potts, JE, et al. Fitness, fatigue, disease activity, and quality of life in pediatric lupus. Arthritis Rheum. 2008;59(4):537–545.
Ilowite, NT. Update on biologics in juvenile idiopathic arthritis. Curr Opin Rheumatol. 2008;20(5):613–618.
Ivins, D. Acute ankle sprain: an update. Am Fam Physician. 2006;74(10):1714–1720. [1723-1724, 1725-1726].
Jarvis, J, Garbedian, S, Swamy, G. Juvenile idiopathic scoliosis: the effectiveness of part-time bracing. Spine (Phila 1976). 2008;33(10):1074–1078.
Joy, EA, Van Hala, S, Cooper, L. Health-related concerns of the female athlete: a lifespan approach. Am Fam Physician. 2009;79(6):489–495.
Kennedy, RM, Luhmann, JD, Luhmann, SJ. Emergency department management of pain and anxiety related to orthopedic fracture care: a guide to analgesic techniques and procedural sedation in children. Pediatr Drugs. 2004;6(1):11–31.
Kerkhoffs GM, Struijs PA, Assendelft WJ, et al: Different functional treatment strategies for acute lateral ankle ligament injuries in adults, Cochrane Database Syst Rev (3):CD002938, 2002.
Klein-Gitelman, MS, Pachman, LM. Intravenous corticosteroids: adverse reactions are more variable than expected in children. J Rheumatol. 1998;25(10):1995–2002.
Klepper, SE. Exercise in pediatric rheumatic diseases. Curr Opin Rheumatol. 2008;20(5):619–624.
Koller, DM, Myers, AB, Lorenz, D, et al. Effectiveness of oxycodone, ibuprofen, or the combination in the initial management of orthopedic injury-related pain in children. Pediatr Emerg Care. 2007;23(9):627–633.
Lampe, RM. Osteomyelitis and suppurative arthritis. In Kliegman RM, Behrman RE, Jenson HB, et al, eds.: Nelson textbook of pediatrics, ed 18, Philadelphia: Saunders, 2007.
Land, C, Rauch, F, Travers, R, et al. Osteogenesis imperfecta type VI in childhood and adolescence: effects of cyclical intravenous pamidronate treatment. Bone. 2007;40(3):638–644.
Laskowski-Jones, L. Responding to an out-of-hospital emergency. Nursing 2002. 2002;32(9):36–42.
Lee, C, Porter, KM, Hodgetts, TJ. Tourniquet use in the civilian prehospital setting. Emerg Med J. 2007;24(8):584–587.
Loder, RT. Controversies in slipped capital femoral epiphysis. Orthop Clin North Am. 2006;37(2):211–221.
Loder, RT, Feinberg, JR. Orthopaedic injuries in children with nonaccidental trauma: demographics and incidence from the 2000 kids’ inpatient database. J Pediatr Orthop. 2007;27(4):421–426.
Lonner, BS. Emerging minimally invasive technologies for the management of scoliosis. Orthop Clin North Am. 2007;38(3):431–440.
Lovell, DJ, Giannini, EH, Reiff, A, et al. Long-term efficacy and safety of etanercept in children with polyarticular juvenile rheumatoid arthritis: interim results from an ongoing multicenter, open-label, extended-treatment trial. Arthritis Rheum. 2003;48(1):218–226.
Lovell, DJ, Reiff, A, Ilowite, NT, et al. Safety and efficacy of up to 8 years of continuous etanercept therapy in patients with juvenile rheumatoid arthritis. Arthritis Rheum. 2008;58(5):1496–1503.
Lovell, DJ, Ruperto, N, Goodman, S, et al. Adalimumab with or without methotrexate in juvenile rheumatoid arthritis. N Engl J Med. 2008;359(8):810–820.
Lucas, B, Davis, PS. Why restricting movement is important. In Kneale JD, Davis PS, eds.: Orthopaedic and trauma nursing,, ed 2, London: Elsevier, 2005.
Lupus Foundation of America, About lupus: what is lupus?. Washington, DC: The Foundation; 2009. accessed April 25, 2010, at www.lupus.org/webmodules/webarticlesnet/templates/new_learnunderstanding.aspx?articleid=2232&zoneid=523
Manzi, S, Meilahn, EN, Rairie, JE, et al. Age-specific incidence rates of myocardial infarction and angina in women with systemic lupus erythematosus: comparison with the Framingham study. Am J Epidemiol. 1997;145(5):408–414.
Marini, JC. Osteogenesis imperfect. In Kliegman RM, Behrman RE, Jenson HB, et al, eds.: Nelson textbook of pediatrics, ed 18, Philadelphia: Saunders, 2007.
Maron, BJ. Medical progress: sudden death in young athletes. N Engl J Med. 2003;349(11):1064–1075.
Maron, BJ, Doerer, JJ, Haas, TS, et al. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980-2006. Circulation. 2009;119(8):1085–1092.
Maron, BJ, Gohman, TE, Aeppli, D. Prevalence of sudden cardiac death during competitive sports activities in Minnesota high school athletes. J Am Coll Cardiol. 1998;32(7):1881–1884.
Meredith, JR, O’Keefe, KP, Galwankar, S. Pediatric procedural sedation and analgesia. J Emerg Trauma Shock. 2008;1(2):88–96.
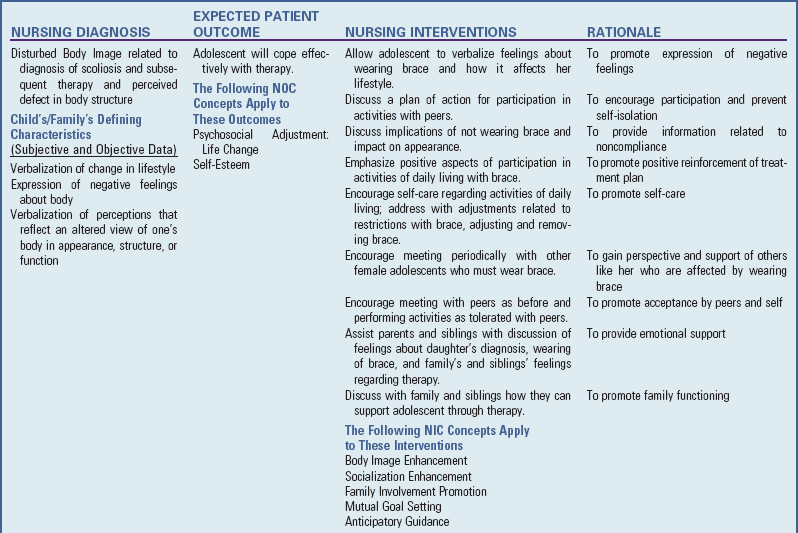
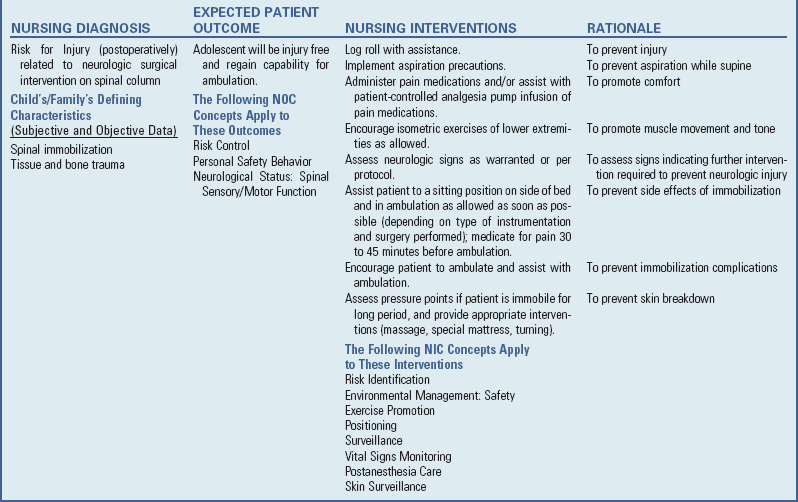
Napierkowski, DB. Scoliosis: a case study in an adolescent boy. Orthop Nurs. 2007;26(3):147–153.
Nelson, AJ, Collins, CL, Yard, EE, et al. Ankle injuries among United States high school sports athletes, 2005-2006. J Athl Train. 2007;42(3):381–387.
Newton, PO, Wenger, DR. Idiopathic and congenital scoliosis. In: Morrissy RT, Weinstein SL, eds. Lovell and Winter’s pediatric orthopaedics. Philadelphia: Williams & Wilkins, 2001.
Nwobi, O, Abitbol, CL, Chandar, J, et al. Rituximab therapy for juvenile-onset systemic lupus erythematosus. Pediatr Nephrol. 2008;23(3):413–419.
Paredes, A. Can mycophenolate mofetil substitute cyclophosphamide treatment of pediatric lupus? Pediatr Nephrol. 2007;22(8):1077–1082.
Persing, J, James, H, Swanson, J, et al. Prevention and management of positional skull deformities in infants. Pediatrics. 2003;112(1):199–202.
Petty, RE, Southwood, TR, Baum, J, et al. Revision of the proposed classification criteria for juvenile idiopathic arthritis: Durban, 1997. J Rheumatol. 1998;25(10):1991–1994.
Petty, RE, Southwood, TR, Manners, P, et al. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol. 2004;31(2):390–392.
Plint, AC, Perry, JJ, Correll, R, et al. A randomized, controlled trial of removable splinting versus casting for wrist buckle fractures in children. Pediatrics. 2006;117(3):691–697.
Prahalad, S, Glass, DN, A comprehensive review of the genetics of juvenile idiopathic arthritis. Pediatr Rheumatol 2008;11(6). available at www.ped-rheum.com/content/6/1/11 [(accessed April 24, 2009)].
Priori, R, Medda, E, Conti, F, et al. Familial autoimmunity as a risk factor for systemic lupus erythematosus and vice versa: a case-control study. Lupus. 2003;12(10):735–740.
Rauch, F, Munns, CF, Land, C, et al. Risedronate in the treatment of mild pediatric osteogenesis imperfecta: a randomized placebo-controlled study. J Bone Miner Res. 2009;24(7):1282–1289.
Ravelli, A, Ruperto, N, Martini, A. Outcome in juvenile onset lupus erythematosus. Curr Opin Rheumatol. 2005;17(5):568–573.
Rechel, JA, Yard, EE, Comstock, RD. An epidemiologic comparison of high school sports injuries sustained in practice and competition. J Athl Train. 2008;43(2):197–204.
Rice, SG, Council on Sports Medicine and Fitness. Medical conditions affecting sports participation. Pediatrics. 2008;121(4):841–848.
Richards, BS, Vitale, MG. Screening for idiopathic scoliosis in adolescents: an information statement. J Bone Joint Surg. 2008;90(1):195–198.
Rodriguez, NR, DiMarco, NM, Langley, S, et al. Position of the American Dietetic Association, Dietitians of Canada, and the American College of Sports Medicine: nutrition and athletic performance. J Am Diet Assoc. 2009;109(3):509–527.
Sandborg, C, Ardoin, SP, Schanberg, L. Therapy insight: cardiovascular disease in pediatric systemic lupus erythematosus. Nat Clin Pract Rheumatol. 2008;4(5):258–265.
Slote, RJ. Psychological effects of caring for the adolescent undergoing spinal fusion for scoliosis. Orthop Nurs. 2002;21(6):19–28.
Spiegel, DA, Hosalkar, HS, Dormans, JP, et al. The neck. In Kliegman RM, Behrman RE, Jenson HB, et al, eds.: Nelson textbook of pediatrics, ed 18, Philadelphia: Saunders, 2007.
Spiegel, DA, Hosalkar, HS, Dormans, JP. Bone and joint disorders: the spine. In Kliegman RM, Behrman RE, Jenson HB, et al, eds.: Nelson textbook of pediatrics, ed 18, Philadelphia: Saunders, 2007.
Tsao, BP, Wu, H. Genetics of human lupus. In Wallace DJ, Hahn BH, eds.: Dubois’ Lupus Erythematosus, ed 7, Philadelphia: Lippincott Williams & Wilkins, 2007.
Tucker, LB. Making the diagnosis of systemic lupus erythematosus in children and adolescents. Lupus. 2007;12(8):546–549.
Venables, MC, Shaw, L, Jeukendrup, AE, et al. Erosive effect of a new sports drink on dental enamel during exercise. Med Sci Sports Exerc. 2005;37(1):39–44.
Waldrop, J. Early identification and interventions for female athlete triad. J Pediatr Health Care. 2005;19(4):213–220.
Warren, RW, Perez, MD, Curry, MR, et al. Juvenile idiopathic arthritis (juvenile rheumatoid arthritis. In: Koopman WJ, ed. Arthritis and allied conditions. Philadelphia: Lippincott Williams & Wilkins, 2001.
Wipke-Tevis, DD, Rich, K. Vascular disorders. In Lewis SL, Heitkemper MM, Dirksen S, et al, eds.: Medical-surgical nursing: assessment and management of clinical problems, ed 7, St Louis: Mosby, 2007.