Chapter 17 Breathing and circulation
Introduction
The care of people with problems affecting their breathing and/or circulation takes place in diverse settings, from the home to the acute hospital, and includes people of all ages, from the neonate to older adults. Immense change has occurred over the past decade, through technological advances, the development of new drugs and, possibly more importantly, through the shift in focus from the health professional as expert to the concept of the ‘expert patient’ involved in self-management and decision-making. These have consequently led to change in the care delivered by nurses, some of which is discussed in this chapter.
Assessment of the patient is an important first step in their nursing management and treatment and so, following a brief review of the structure and function of the heart, circulation, blood and respiratory system, the chapter outlines some of the important nursing observations that may be undertaken as part of a holistic assessment. The chapter also outlines some of the more common disorders and investigations used in their diagnosis.
This chapter describes the ways in which the nurse can contribute towards the health of the person with disorders of breathing or circulation, reduce the effects of illness and maximize quality of life for both the patient and their family. Because disorders of breathing and circulation may at times require emergency treatment, some first aid measures are included. The health promoting activities that help to prevent problems with breathing and/or circulation are also explored.
An overview of breathing and circulation
This section provides an outline of the anatomy and physiology of breathing and the circulation. Readers should consult their own anatomy and physiology book for more detail. In addition, an outline of common conditions, basic life support, holistic assessment of the breathing and circulation and investigations are provided.
Life depends on an adequate and continuous supply of oxygen (O2) and nutrients to the cells and the removal of the waste products of metabolism. Without this, cells will become starved of oxygen and die. The accumulation of waste products such as carbon dioxide (CO2) also disrupts cell function and eventually contributes to cell death.
Breathing and circulation are therefore fundamental to life and the cardiovascular system (CVS), blood and respiratory system must work together to supply O2 to the cells and remove waste CO2. This requires an adequate intake of air and a good blood supply to the lungs in order for gaseous exchange to take place. Oxygenated blood carries O2 to the cells and deoxygenated blood, containing CO2, leaves the cells and is transported to the lungs. The CVS is responsible for circulating the blood around the body, and to and from the lungs.
Cardiovascular system – outline of anatomy and physiology
The CVS comprises the heart which pumps blood around the body and to the lungs and the circulatory system of arteries, capillaries and veins through which the blood travels.
The heart
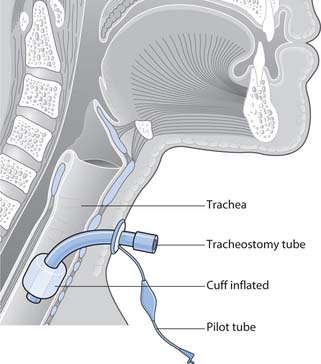
The heart is situated in the thorax, within the mediastinum (the space between the two lungs) with its base inclined to the left (Fig. 17.1). It is protected from injury by the bones forming the thoracic cage, the sternum (breastbone) in front, the ribs and the vertebral column behind.
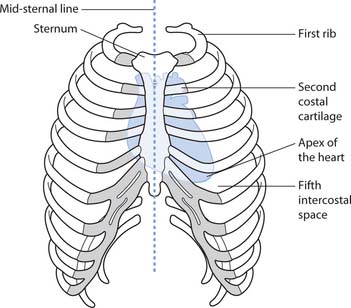
Fig. 17.1 Position of the heart in the thorax
(reproduced with permission from Brooker & Nicol 2006)
The wall of the heart has three layers (Fig. 17.2), as follows:
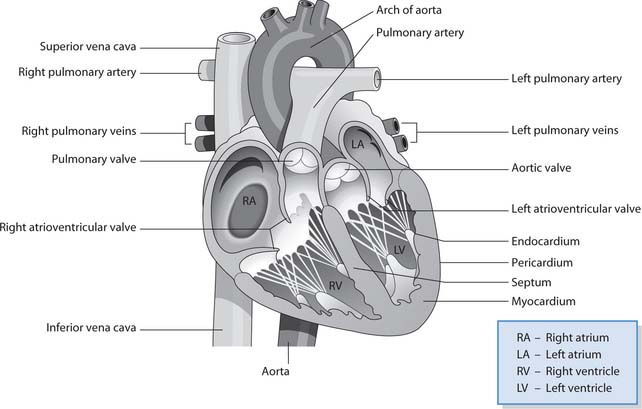
Fig. 17.2 Heart showing the chambers, valves and blood vessels
(reproduced with permission from Waugh & Grant 2001)
The heart is divided into four chambers (see Fig. 17.2). The two upper chambers or atria are the receiving chambers that pump blood into the ventricles. The two lower chambers are thick-walled ventricles that pump blood to the lungs (pulmonary circulation) and to the tissues and cells (systemic circulation). The right and left sides of the heart are divided by the septum.
Valves situated at the entrance or exit of the chambers ensure that the blood flows in one direction. The two semilunar valves are the pulmonary valve at the junction of the right ventricle and pulmonary artery and the aortic valve at the junction of the left ventricle and the aorta. The atrioventricular (AV) valves between the atria and ventricles prevent any backflow of blood from the ventricles to the atria as the ventricles contract. The right AV valve (tricuspid valve) lies between the right atrium and ventricle and the left AV valve (bicuspid or mitral valve) lies between the left atrium and ventricle.
Coronary circulation
Three major arteries supply the myocardium with oxygen: the right coronary, the left anterior descending and the circumflex. They branch to form a dense network of arterioles and capillaries that extend throughout the myocardium and ensure that it is supplied with oxygen and metabolic waste products are removed. Once the myocardium has been supplied with oxygen, blood returns to the right atrium via the coronary veins and is transported to the lungs for carbon dioxide removal and reoxygenation. The coronary arteries primarily fill with blood during diastole when the heart muscle is relaxed.
Conduction
The electrical conduction system of the heart has four main structures (Fig. 17.3):
The sinus node is known as the ‘pacemaker’ of the heart because it initiates each heartbeat. It normally fires at a rate between 60 and 100 beats per minute (bpm). From the sinus node, the impulse passes to the AV node causing the atria to contract (atrial systole). From the AV node the impulse passes down the AV bundle in the septum to the right and left bundle branches and the Purkinje fibres. This causes the ventricles to contract (ventricular systole) and eject blood into the aorta and pulmonary artery.
Cardiac cycle
The cardiac cycle is the rhythmic contraction (systole) and relaxation (diastole) of the heart as it fills with blood and pumps it around the body and to the lungs. It comprises a series of stages that occur during a single heartbeat. Normally the whole cycle is completed in less than 1 second. Once one cycle is completed, the next cycle commences to maintain a continuous flow of blood.
The function of the cardiac cycle is to provide an adequate output of blood from the heart. The amount of blood that is ejected with each heartbeat is referred to as the stroke volume (SV), whereas the term cardiac output (CO) refers to the amount of blood ejected from the heart in 1 minute. Hence the equation:
Cardiac Output (CO) 5 Heart Rate (HR) 3 Stroke Volume (SV).
Sinus rhythm
Sinus rhythm is the normal rhythm of the heart. It produces a typical waveform comprising five deflections known universally as P-QRS-T (Fig. 17.4). The deflections depicted on an electrocardiogram (ECG) represent the electrical activity in the heart and correspond to the events of conduction and the stages of the cardiac cycle:
At rest the adult heart normally beats in response to the sinus node activity at approximately 70bpm. Sinus rhythm describes any heart rhythm where the complexes described above can be seen and that occurs at a rate between 60 and 100bpm. In adults, a HR rate <60bpm is referred to as sinus bradycardia, while a HR >100bpm is sinus tachycardia.
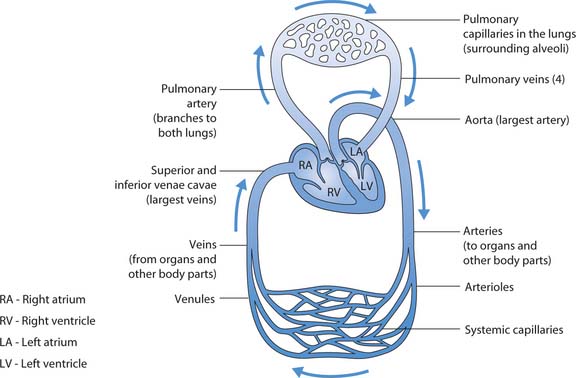
Systemic and pulmonary circulation
The systemic circulation is the circulation of oxygenated blood from the left ventricle into the aorta, to cells/tissues and deoxygenated blood back to the right atrium of the heart. The pulmonary circulation is the circulation of deoxygenated blood from the right ventricle to the pulmonary artery, to the lungs and oxygenated blood back to the left atrium of the heart.
Thus oxygenated blood returning from the lungs enters the left atrium and passes through the left AV valve into the left ventricle (see Fig. 17.2, p. 465). The left ventricle pumps blood into the systemic circulation through the aorta (large artery) and from there to numerous smaller arteries, arterioles and capillaries, which take blood to the rest of the body (Fig. 17.5). The coronary arteries supplying the myocardium are the first to branch from the aorta. The arterial blood supplies cells with oxygen and nutrients and returns, carrying carbon dioxide and other waste, to the right side of the heart via small veins (venules) and increasingly larger veins. Deoxygenated venous blood returns to the right atrium in two large veins – the superior and inferior venae cavae – and passes through the right AV valve into the right ventricle.
The right ventricle pumps blood into the pulmonary circulation through the pulmonary artery (see Fig. 17.5). The pulmonary artery divides to send a branch to each lung where further subdivisions occur and the blood moves through smaller and smaller arteries and arte-rioles until they reach the pulmonary capillaries. Gas exchange occurs between the blood in the capillaries and the air in the alveoli of the lungs (see p. 470); carbon dioxide moves from blood to the alveoli and oxygen from the alveoli to the blood.
The oxygenated blood is returned to the left atrium of the heart through venules and larger and larger veins that form four pulmonary veins (two from each lung).
An efficient pulmonary and systemic circulation ensures that the body tissues and organs are perfused with oxygenated blood and waste products are removed.
Blood – outline of anatomy and physiology
Blood is a viscous fluid circulating in the blood vessels. It is a connective tissue and forms the main transport system of the body. The colour depends upon the amount of oxygen it is carrying; well-oxygenated arterial blood is bright red, whereas oxygen-poor (deoxygenated) venous blood is darker in colour.
Blood comprises a fluid part called plasma which forms approximately 55%, and the blood cells which form the remaining 45%. Blood is slightly alkaline with a normal pH range of 7.35–7.45.
Blood volume varies according to body size and age. Adult blood volume forms approximately 7–8% of body weight. An adult male weighing 70 kg has around 5.6L of blood. Females have a smaller proportion than males; however, during pregnancy, the volume increases by between 20 and 40% in order to maintain blood flow through the enlarged uterus and placenta to supply oxygen and nutrients to the fetus and to remove fetal waste products. Infants and children have a greater proportion, which gradually decreases until adult proportions are reached. At birth the circulating blood volume varies, but is usually around 85 mL/kg. Thus a newborn weighing 4 kg has approximately 340 mL of blood.
The functions of the blood include the following:
Plasma
Plasma is the straw-coloured fluid found when blood separates. In the vascular system, plasma provides a medium to carry blood cells. Plasma is between 90 and 92% water and dissolved nutrients, gases, electrolytes, hormones, drugs, waste products and proteins such as albumin, globulins and fibrinogen.
Blood cells
There are three types of blood cell: erythrocytes (red cells), leucocytes (white cells) and thrombocytes (platelets).
Erythrocytes (red blood cells)
Erythrocytes are the most numerous of the blood cells. They are formed in the red bone marrow and their main function is to carry oxygen. They are biconcave discs that are small enough to pass through small capillaries where the exchange of oxygen, nutrients, carbon dioxide and other waste takes place. Erythrocytes contain haemoglobin (an iron-containing pigment/protein molecule), which is responsible for carrying most of the oxygen transported in the blood. Iron and some B complex vitamins (e.g. folic acid and vitamin B12) are essential for the formation of haemoglobin (Box 17.1).
[Resources Food Standards Agency – http://www.eatwell.gov.uk/healthydiet/nutritionessentials/vitaminsandminerals/iron; www.eatwell.gov.uk/healthydiet/vegaveg Available July 2006]
Iron-rich foods
A balanced diet that supplies sufficient iron is needed for the body to produce haemoglobin. Foods rich in iron include:
Leucocytes (white blood cells)
Leucocytes are divided into different groups. These include:
All leucocytes have a role in defending the body against microorganisms and other foreign particles. Some leucocytes remove foreign particles such as a bacterium or an abnormal cell by phagocytosis, which involves engulfing and digesting the particle; other leucocytes are part of the immune response through the production of antibodies or destruction of abnormal body cells.
Haemostasis
Normally blood flows freely within the vascular system but when there is significant bleeding from a damaged blood vessel, the process of haemostasis normally prevents major blood loss.
Haemostasis involves four overlapping stages:
Blood groups
There are two major blood group classifications: the ABO system and the rhesus system.
The ABO system has four main blood groups – A, B, AB and O – which are defined by the presence of antigens (specific proteins) on the surface of the erythrocyte. People with antigen A are blood group A, those with antigen B are group B. People who have both A and B antigens are blood group AB and those without either antigen are group O.
Someone with blood group A will have anti-B antibodies in their plasma, someone with blood group B will have anti-A antibodies, people with blood group O will have both anti-A and B antibodies while someone with blood group AB will have no antibodies. These antibodies will bind to a foreign antigen and initiate a reaction that destroys the cell such as occurs if incompatible blood is transfused (Bywater & Rawlings 2003) (see p. 498).
It is important to be aware of the different blood groups in order to ensure that when blood is transfused, blood from the correct group is given to the correct person. Table 17.1 outlines the ABO blood group compatibility.
The rhesus group is determined by a further set of antigens on the erythrocyte. People who have the antigens are rhesus positive (Rh[D]-positive) and those without are rhesus negative (Rh[D]-negative). Unlike the ABO system there are no preformed anti-rhesus (anti-D) antibodies. However, if a rhesus negative person receives rhesus positive blood they will develop anti-D. Although this will not cause a transfusion reaction at the time, any future transfusion will initiate a reaction and the donor erythrocytes will be attacked.
During pregnancy a rhesus negative woman who has a rhesus positive fetus may become sensitized and develop anti-D antibodies. During a subsequent pregnancy with a rhesus positive fetus the anti-D antibodies can cross the placenta and cause haemolysis (breakdown) of the fetal erythrocytes. This is a serious condition and can lead to fetal death or the baby may suffer brain damage or die after birth. Women are tested for rhesus group during antenatal care. Anti-D is given to rhesus negative women to prevent the sensitization of the immune system. It is given by injection following events that may lead to sensitization such as bleeding during pregnancy, miscarriage, termination and labour.
Respiratory system – outline of anatomy and physiology
The respiratory tract provides oxygen for cellular function and excretes waste carbon dioxide. This is achieved by breathing, where air moves in (inspiration) and out (expiration) of the lungs and by gas exchange in the lungs and at the cells.
Respiratory structures
The respiratory structures (Fig. 17.6) include:
Nose
The first part of the nasal cavity is lined with skin containing hairs that trap large particles from the inspired air. The internal part of the nasal cavity is lined with respiratory mucosa comprising ciliated columnar epithelium containing many mucus-secreting goblet cells. The inspired air is humidified by the moist mucosa and warmed by plentiful blood vessels supplying the respiratory mucosa. The sticky mucus traps dust, bacteria and other foreign particles in the inspired air and the cilia then waft these particles towards the pharynx where they are swallowed and so do not enter the lungs.
Pharynx
The pharynx is a funnel-shaped passage with three parts: nasopharynx, oropharynx and laryngopharynx. The process of warming, humidifying and filtering inspired air normally continues in the nasopharynx, which is lined with respiratory mucosa (Box 17.2). The nasopharynx is exclusively respiratory, but the oropharynx and laryngopharynx provide a passage for food and fluids in addition to air. The oropharynx and laryngopharynx are lined with tougher stratified squamous epithelium, which is continuous with that of the oesophagus.
Mouth breathing, as may occur in patients with nasal obstruction or dyspnoea (difficult breathing), bypasses the normal processes in the nose and nasopharynx that warm, humidify and filter air and leads to an exacerbation of the breathing problems. The respiratory mucosa will be damaged, the cilia cease to function effectively and mucus secretions become dry, crusty and difficult to expectorate (cough up).
Angina
Myocardial infarction
Recognition
May progress to unconsciousness, or the casualty may stop breathing and the heart stop beating (see ‘Basic life support’, pp. 474–477).
Treatment
Note: Patients should be encouraged to seek help at the earliest possible opportunity. It is important that the public are aware of the symptoms of a myocardial infarction and understand that seeking medical help is vital.
[Reference: Mayor S 2004 Pass the salt: cutting down on salt to reduce blood pressure. British Journal of Primary Care Nursing 1(4):160–162; Resource: Food Standards Agency – www.salt.gov.uk Available July 2006]
Salt intake
A diet containing high levels of salt (sodium chloride) is associated with an increase in blood pressure. High blood pressure (hypertension) is a risk factor for coronary heart disease (CHD) and for strokes.
The salt content of unprocessed foods is comparatively low, but added salt is present in many prepared or processed foods, e.g. home cooked meals, cheese, snack foods, ready meals, breakfast cereals, etc. Food products with more than 1.25 g salt/100 g (0.5 g sodium/100 g) are considered high in salt (Mayor 2004).
Adults should be encouraged to keep their salt intake within the recommended daily intake. Parents and carers should be aware that the recommended intake for infants and children is much lower than in adults and depends on age. An even lower salt intake may be advised for people who are hypertensive and for those with chronic heart failure. This is because excess salt intake leads to water retention, which increases the blood pressure and leads to the formation of oedema (swelling due to fluid collecting in the tissues, see p. 479).
[Resource: Asthma UK Personal asthma action plan – www.asthma.org.uk/all_about_asthma/publications/be_in_control.html Available July 2006]
Self-management in asthma
All people with asthma should have a written self-management plan outlining the daily actions they should take to monitor their condition and identify any deterioration. It should suggest alterations to daily management when their condition deteriorates and indicate when professional help is needed.
A personal asthma action plan is available from Asthma UK, which, if used, should be completed by the patient and their doctor or practice nurse.
Any management plan should include the following:
Student activities
[Reference: Cancer Research UK – www.cancerresearch.org.uk Resources: Action on Smoking and Health (ASH) – www.ash.org.uk; British Heart Foundation – www.bhf.org.uk/smoking; NHS – www.givingupsmoking.co.uk All available July 2006]
Smoking cessation
Smoking is a major cause of death and disability. It causes:
Tobacco was responsible for 6.3 million deaths in the UK between 1950 and 2000 (Cancer Research UK 2005). Smoking is the single most preventable cause of premature death. Helping people to stop smoking and acting to prevent people starting to smoke is a vital role for all nurses.
The pharynx also contains lymphoid tissue – the nasopharyngeal tonsils in the nasopharynx and the palatine tonsils in the oropharynx – which form part of the body’s defences against invading microorganisms.
Larynx
The larynx (voice box) is formed from cartilage, ligaments and membranes. Inspired air moving through the larynx is warmed, humidified and filtered as it passes from the pharynx to the trachea. The vocal cords, which extend from the front to the back of the larynx, are concerned with sound production. Inspired air must pass through the opening between the vocal cords – the glottis – to enter the trachea.
During swallowing, various reflex mechanisms prevent food or fluids from entering the lower respiratory tract. These include:
In addition, if food or fluid does enter the larynx, the cough reflex is normally stimulated (see below and p. 484).
Trachea
The trachea (windpipe) is a continuation of the larynx and is between 12 and 15 cm in length in an adult. It divides (bifurcates) to become the right and left main bronchi, with one bronchus going to each lung. The trachea is formed from C-shaped rings of cartilage, which are incomplete at the back. This gives the trachea some flexibility while the cartilage ensures that the airway remains open. The trachea is also lined with respiratory mucosa and continues to warm, humidify and filter air, although warming and humidification is practically complete when air enters the trachea. The mucus continues to trap foreign particles and, in a synchronized process called the mucociliary escalator, the cilia move the mucus with particles upward to the larynx from where it is either expectorated by coughing or swallowed.
Irritation such as that caused by excess mucus or foreign material (food, fluid, etc.) in the larynx, trachea or bronchi stimulates the cough reflex in which a forced expiration expels the mucus and/or foreign material. For further coverage of the cough reflex and the first aid for choking, see pages 484–485.
Bronchi, bronchioles and alveoli
The processes of humidification and warming in the upper respiratory tract are complete, air is saturated with water and warmed to 37°C and most foreign particles have been removed before it enters the bronchi.
Once the right and left main bronchi enter the lungs they divide into smaller and smaller bronchi, bronchioles and finally the tiny alveolar ducts that lead into the alveoli. The larger bronchi are lined with respiratory mucosa and the walls are supported by rings of cartilage and so remain open throughout the respiratory cycle (inspiration and expiration). As the bronchi become smaller they lose the cartilage and the lining gradually changes to non-ciliated epithelium. Further changes occur as the walls become thinner until a single layer of simple epithelium remains in the alveolar ducts and alveoli. This structural adaptation facilitates gaseous exchange.
The alveoli are very small air sacs clustered together and surrounded by a network of pulmonary capillaries. Special cells in the walls of the alveoli secrete surfactant (phospholipid fluid) which ensures a moist membrane needed for gaseous exchange. Surfactant also reduces surface tension and prevents alveolar collapse between breaths. Surfactant starts to be secreted by about 22 weeks’ gestation and there is a rapid increase around 35 weeks’ gestation (MacGregor 2000). Hence in the preterm infant, surfactant production may be insufficient to maintain patency of the alveoli and lead to respiratory distress (see p. 483).
Oxygen diffuses from the alveolar air, across the very thin layer of cells, the respiratory and capillary membranes into capillary blood (Fig. 17.7). Carbon dioxide leaves the blood and diffuses across the two membranes into the alveoli. The carbon dioxide is excreted during expiration.
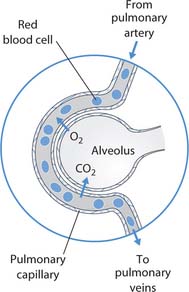
Fig. 17.7 Gas exchange between alveolus and pulmonary capillary
(reproduced with permission from Brooker and Nicol 2003)
For efficient gaseous exchange to occur there must be both adequate ventilation of the lungs and good perfusion with blood. In other words, if the lungs expand and fill with air, this will only lead to effective breathing; there also needs to be good supply of blood to the alveoli for the exchange of oxygen and carbon dioxide.
Lungs
The two lungs are situated within the thoracic cavity, either side of the heart and are protected from injury by the ribs (see Fig. 17.1, p. 464). The right lung is divided into three lobes whereas the left lung is smaller and has only two lobes. Its smaller size is due to the position of the heart in the mediastinum.
A double serous membrane called the pleura lines the thoracic cavity (parietal layer) and covers the outside of each lung (visceral layer). The pleura secretes serous fluid that lubricates the lungs, thus enabling them to move easily as they inflate and deflate. The intact pleura also keeps the lungs inflated.
Breathing (ventilation)
Breathing is the mechanical process by which air moves in and out of the lungs. There are two processes: inspiration, which requires energy and is active, and expiration, which is passive. Expiration is followed by a short pause before the next inspiration. In a normal respiratory cycle (at rest), the amount of air inhaled and exhaled is normally around 500 mL in an adult. This is known as the tidal volume (TV).
During inspiration the capacity of the thoracic cavity is increased as the diaphragm (muscle between the thorax and the abdomen) and intercostal muscles (between the ribs) contract. The lungs are stretched, the pressure within the lungs falls and air moves into the lungs in order to equalize the atmospheric and alveolar air pressures.
During expiration, the relaxation of the diaphragm and intercostal muscles leads to an inward and downward movement of the thoracic cage and elastic recoil of the lungs. The pressure in the lungs is greater than atmospheric air and air moves out.
Normal, unlaboured breathing depends on several factors. These include:
Common conditions affecting breathing and circulation
Disorders of the heart and blood vessels, blood and respiratory tract can lead to difficulties with breathing and to circulatory problems. Unfortunately, these are common; for example, coronary heart disease (CHD), a disease that affects both breathing and circulation, accounted for 114000 deaths in 2003 in the UK (British Heart Foundation 2005) and is a major cause of premature death. Disorders of the lungs are also common and appear to be on the increase. In 1999 lung diseases led to 153000 deaths in the UK (British Thoracic Society 2001).
Diseases that affect breathing and circulation may be acute or chronic and affect all age groups. Some of the morecommon conditions are outlined in Tables 17.2-17.4. Readers requiring more information should consult the Further reading suggestions (e.g. Brooker & Nicol 2003, Chs 18–20).
Table 17.2 Common cardiovascular conditions
| Angina pectoris | See Coronary heart disease below |
| Cardiac arrhythmia | Abnormal heart rhythm. Arrhythmias include: |
| • Atrial fibrillation (AF) (see p. 480) | |
| • Supraventricular tachycardia (SVT) | |
| • Premature ventricular contraction (PVC) | |
| • Ventricular tachycardia (VT) (see p. 474) | |
| • Ventricular fibrillation (VF) (see p. 474) | |
| Coronary heart disease (CHD) | Common condition caused by narrowing of the coronary arteries by atherosclerosis. This is atheroma (fatty plaques on the lining layer) accompanied by damage to the lining of the artery, hardening and eventually a partial obstruction to the flow of blood through the vessel |
| Can manifest itself as angina or myocardial infarction and eventually leads to chronic heart failure | |
| Atherosclerosis may be caused by a diet high in saturated fats, hypertension and smoking and exacerbated by obesity and lack of physical exercise (see Boxes 17.5, p. 474; 17.7, p. 475) | |
| Narrowing of the coronary arteries by atheroma is the usual cause of angina but can be due to coronary artery spasm | |
| Narrowing leads to a reduction in the blood supply to the myocardium and transient chest pain, which may radiate to the arms (especially the left), abdomen, jaw, neck and throat | |
| Pain is often induced by exertion, cold weather and wind, emotional stress and sometimes following a large meal | |
| Rest promptly relieves the pain (see Box 17.3, p. 472) | |
| Angina affects just under 2 million people in the UK (British Heart Foundation 2005) | |
| Occurs when blood flow in the coronary arteries is blocked by atheroma and oxygen does not reach all of the myocardium | |
| The coronary artery is occluded and unless the artery is reopened, using thrombolytic drugs that dissolve clots or an invasive procedure such angioplasty, the myocardium supplied by that vessel will be damaged (infarcted) | |
| MI is a common cause of death in Western countries and, of the 300000 that occur each year in the UK, about 30% will be fatal (British Heart Foundation 2005) (see Box 17.4, p. 474) | |
| Congenital heart disease | Disorder that develops as the heart is formed and present at birth |
| Common congenital abnormalities include septal defects (hole in the heart) and patent ductus arteriosus (a fetal blood vessel between the left pulmonary artery and the aorta to bypass the lungs) | |
| Some may be caused by genetic or chromosomal abnormalities such as septal defects in infants with Usually treated surgically | |
| Heart failure | The heart fails to pump effectively and is unable to deliver adequate oxygen and nutrients to the cells and tissues It may occur in one side or both right and left |
| Heart failure is usually a chronic condition but it can occur acutely | |
| Chronic heart failure is commonly caused by CHD, cardiomyopathy (disease of the myocardium), valvular disease, arrhythmias, hypertension, chronic respiratory disease, etc. (see Box 17.5, p. 474) | |
| Hypertension | Blood pressure that is persistently higher than 140/90mmHg in adults |
| In children there is no precise definition for hypertension; however, it is generally agreed to be a blood pressure greater than 130/85mmHg on three consecutive readings | |
| In the vast majority of cases, no cause is found and it is termed ‘essential | |
| Secondary hypertension may result from a variety of conditions that include heart and blood vessel disease; kidney disease; endocrine diseases; drugs, e.g. corticosteroids, oral contraceptives, non-steroidal anti-inflammatory drugs (NSAIDs); pre-eclampsia associated with pregnancy (see Box 17.5, p. 474) | |
| Myocardial infarction (MI) – ‘heart attack’ | See Coronary heart disease above |
| Rheumatic heart disease | Chronic inflammation and scarring of the myocardium and valve cusps |
| Usually leads to valvular heart disease | |
| Valvular heart disease | Usually affects the mitral or aortic valves but the tricuspid and pulmonary valves can be affected |
| The valve may be either stenosed or regurgitant |
Table 17.3 Common blood (haematological) conditions
| Anaemia | Anaemia occurs when there is a reduced oxygen carrying capacity of the blood and the haemoglobin level falls below 9g/dL |
| There are several causes including: | |
| • Lack of iron and/or vitamin B12 or folate (see Box 17.1, p. 467) | |
| • Excessive blood loss – acute or chronic | |
| • Abnormal haemoglobin – see Haemoglobinopathies (below) | |
| • Excessive destruction of erythrocytes – haemolytic anaemia | |
| • Bone marrow suppression – aplastic anaemia | |
| Deep vein thrombosis (DVT) | A DVT is a clot that forms in a vein, usually a large vein of the leg or pelvis, but it can occur in the arm |
| Predisposing factors are venous stasis (slow bloodflow), increased blood stickiness and vein damage | |
| The risk factors for DVT therefore include prolonged immobility (see Ch. 18), increasing age (<40 years), poor peripheral blood flow, dehydration (see Ch. 19) or clotting disorders | |
| Identification of those at risk and prevention is vital (see Ch. 24) | |
| See Pulmonary embolus (below) | |
| Haemoglobinopathies | |
| 1. Sickle cell disease | An inherited condition which is due to abnormal haemoglobin, known as HbS |
| Seen in individuals from areas where falciparum malaria is common (equatorial Africa, parts of India and parts of the Eastern Mediterranean) and their descendants in Europe, West Indies and the USA | |
| The erythrocytes become sickle-shaped under certain conditions, e.g. hypoxia (reduced oxygen level in the tissues) or dehydration, which leads to reduced oxygen carriage, vessel blockage with pain and infarction and chronic haemolytic anaemia as the abnormal erythrocytes are destroyed in the spleen | |
| At-risk populations should be screened for the abnormal HbS | |
| 2. Thalassaemia | A group of inherited haemoglobinopathies |
| Thalassaemia can occur in people of all racial groups but is commonly found in people with Mediterranean ancestry | |
| The synthesis of globin chains, essential for haemoglobin production, is reduced because of a faulty gene, leading to fragile erythrocytes with impaired oxygen-carrying capacities, which are more rapidly destroyed by the spleen | |
| In thalassaemia major (two faulty genes inherited) there is severe anaemia, jaundice and enlarged liver and spleen | |
| Those with thalassaemia trait (one faulty gene inherited) may have mild anaemia or be asymptomatic | |
| Leukaemia | A group of malignant diseases affecting the tissues that produce blood cells |
| Leukaemia leads to an overproduction of immature leucocytes in the bone marrow that are released into the blood, suppressing normal production of erythrocytes and platelets, which leads to anaemia and risk of bleeding | |
| The lack of mature leucocytes increases the risk of infection | |
| There are several types of leukaemia affecting different leucocytes | |
| Leukaemia may be either acute or chronic. |
Table 17.4 Common respiratory conditions
| Asthma | A chronic condition where inflammation causes spasm of the smooth muscle of the bronchi (bronchospasm), leading to bronchoconstriction and narrowing |
| There is paroxysmal dyspnoea with wheezing and difficulty breathing out, a dry cough and tightness in the chest | |
| The emphasis is on self-management by patients or carers (see Box 17.6, p. 475) | |
| An attack of acute, severe asthma is a life-threatening medical emergency | |
| Bronchiectasis | The bronchi and bronchioles are abnormally dilated and contain copious amounts of foul-smelling purulent (containing pus) sputum |
| It may be localized or more generalized, when it may be associated with cystic fibrosis | |
| Bronchiolitis | Inflammation of the bronchioles, usually caused by a viral infection |
| Occurs mainly during winter months and usually affects infants under 12 months of age | |
| Chronic bronchitis | Inflammation of the bronchi, defined as a cough with sputum for at least 3 consecutive months in 2 consecutive years |
| There is an increase in mucus-secreting goblet cells and loss of cilia caused by tobacco smoke and air pollution | |
| A form of chronic obstructive pulmonary disease (see Box 17.7, p. 475). | |
| Chronic obstructive pulmonary disease (COPD) | A group of progressive obstructive lung diseases where airway resistance is increased with reduced airflow, e.g. emphysema, chronic bronchitis or severe asthma (see Box 17.7, p. 475) |
| Croup | An acute viral infection that causes swelling and/or spasm leading to narrowing of the larynx in children |
| The child will have harsh-sounding (stridulous) ‘croupy’ breathing | |
| Narrowing of the airway gives rise to the typical crowing inspiration | |
| Cystic fibrosis (CF) | A genetic disorder affecting the exocrine glands |
| A screening blood test is available for neonates | |
| High levels of sodium in sweat may confirm the diagnosis | |
| The affected glands produce viscous mucus, which leads to blocked bronchi or ducts, stasis of secretions, infection and fibrosis | |
| The lungs and pancreas are primarily affected, giving rise to repeated chest infections, respiratory problems, digestive problems and heart failure | |
| Emphysema (pulmonary) | Overdistension of the alveoli leading to rupture and a reduction in gas exchange in the lungs |
| Associated with tobacco smoking (see Box 17.7, p. 475) | |
| A form of chronic obstructive pulmonary disease (see Box 17.7, p. 475) | |
| Lung cancer | A primary malignant tumour in the lung or bronchi |
| Smoking is the most important factor in its development but exposure to tobacco smoke, asbestos and environmental pollution are also implicated (see Box 17.7, p. 475) | |
| Other cancers, e.g. breast, colorectal, often metastasize (spread) to the lung to form secondary cancers | |
| Pneumonia | An acute infection of the lung It may be hospital-or community-acquired, or associated with impaired immune responses |
| Pulmonary embolism (PE) | A clot that forms in a vein breaks away and travels in the circulation and through the heart to lodge in a pulmonary blood vessel in the lungs (see Deep vein thrombosis, above) |
| Leads to infarction of lung tissue in areas deprived of blood | |
| Tuberculosis (TB) | A notifiable infectious disease caused by the bacterium Mycobacterium tuberculosis |
| The BCG (bacillus Calmette–Guérin) vaccine is used to protect those at high risk of contracting TB, e.g. infants born in high-risk areas with 40 cases of TB per 100000 population or higher |
Basic life support – airway maintenance and cardiopulmonary resuscitation
Basic life support (BLS) comprises the first aid measures for maintenance of a clear airway, artificial respiration (e.g. rescue breaths) and chest compressions (external heart massage) in people who have suffered a cardiac arrest (also known as cardiopulmonary arrest), or artificial respiration alone if only breathing has stopped. BLS aims to provide an intake of oxygen and maintain the circulation of blood. Cardiac arrest is defined as the sudden cessation of effective output of blood from the heart. The failure of output from the heart means that the circulation is not maintained. There are several forms of cardiac arrest, including:
The causes of cardiac arrest include CHD, other heart diseases, hypovolaemia, e.g. severe haemorrhage, electric shock, electrolyte imbalances (see Ch. 19) and severe respiratory problems.
The BLS procedures for cardiopulmonary resuscitation (CPR) outlined below are put in place until the emergency services or hospital cardiac arrest team can start advanced life support (see also Ch. 16). The BLS techniques are different for adults, children and infants. BLS is described using adult procedures and the differences in technique for children and infants are provided in Box 17.8 (p. 478).
Box 17.8 BLS – differences in techniques for children and infants
[Resources: Resuscitation Council (UK) (2005); St John Ambulance – www.sja.org.uk/firstaid/info]
Adult basic life support
An adult is defined as a person who has reached puberty for the purpose of providing BLS. If the casualty is outside hospital an emergency ambulance must be summoned by dialling 999 (see below). If the cardiopulmonary arrest has occurred in hospital the nurse should know the internal ‘crash call’ telephone number for summoning the cardiac arrest team. The National Patient Safety Agency (NPSA) (2004) advised all NHS Trusts in England and Wales to standardize the internal crash call telephone number to 2222. At the time of writing the vast majority of acute Trusts now use 2222 but until all Trusts have converted, individual hospitals may have a different number and all staff should be aware of it.
When initially faced with an adult whom you suspect has experienced a cardiopulmonary arrest, the following procedure should be started immediately:
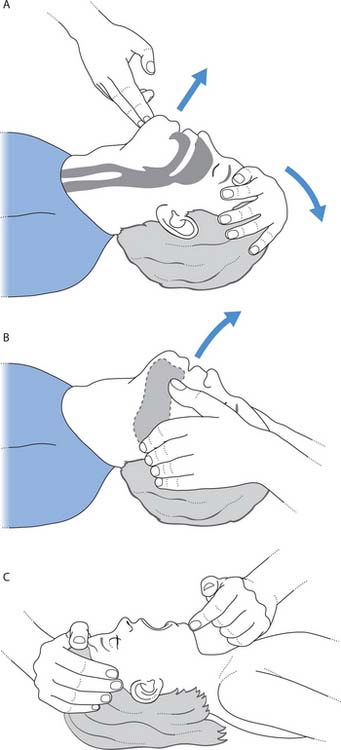
Fig. 17.8 Opening the airway: A. Head tilt/chin lift – adult. B. Jaw thrust – adult. C. Head tilt/chin lift – child
(reproduced from Mallik et al 1998 and Huband & Trigg 2000)
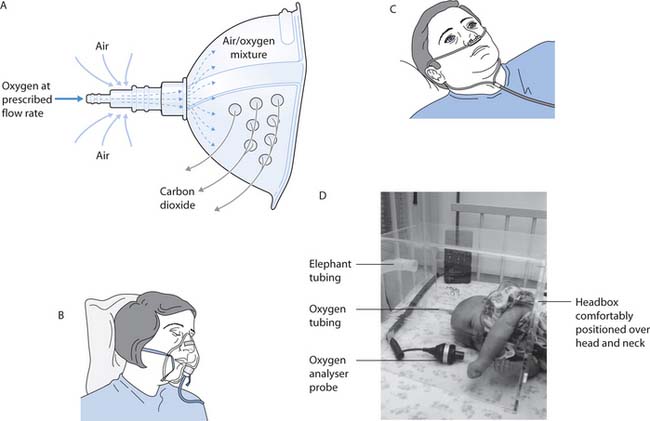
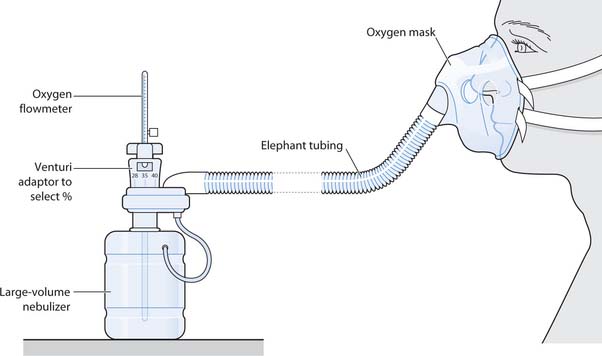
Fig. 17.17 Oxygen delivery systems: A. Fixed performance, high-flow Venturi system mask. B. Variable flow – Hudson-type mask. C. Nasal cannulae/prongs. D. Delivery of humidified oxygen via a head box
(reproduced with permission from Brooker & Nicol 2003; Nicol et al 2004; Huband & Trigg 2000)
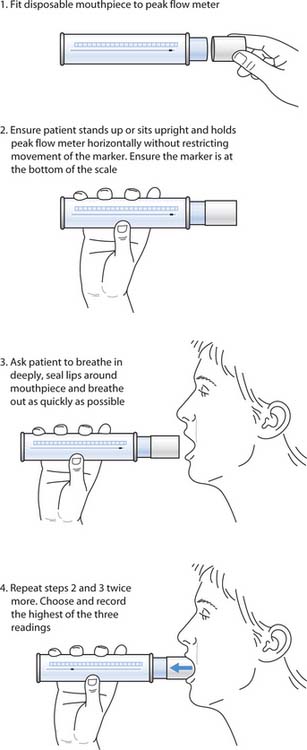
Fig. 17.11 Recording peak expiratory flow rate
(reproduced with permission from Brooker & Nicol 2003)
Basic life support for infants and children
A child is defined as a person aged 1 year and up to the age of puberty and an infant as being less than 12 months old for the provision of BLS. The differences between BLS for children and infants and that for adults (see above) are outlined in Box 17.8 (p. 478).
Assessment and observation – circulation and breathing
Assessment and observation form the basis for nursing management and treatment and are therefore key skills to learn. However, observations do not have to be complex, nor require sophisticated equipment. Some of the best skills for assessment and observation are those that involve looking, listening, touching and smelling.
This section will look at important areas for the assessment of breathing and circulation and include assessment of the skin, the heart rate, blood pressure and respiration.
Although assessment is useful, it only becomes a valuable tool if nurses know what to do with the findings. All data should be recorded in the patient’s notes and/or on observation charts (see Ch. 14). Where nurses suspect that the data are abnormal, then the person in charge should be notified as soon as possible.
Skin – general assessment
Assessment of the skin is quick and easy yet provides useful information about both breathing and circulation. Nurses should take every opportunity to assess a person’s skin, e.g. while helping them with personal hygiene. More information about skin condition and assessment is provided in Chapters 16 and 25.
In health the skin should be warm, dry, intact and normal colour for racial group. However, with normal ageing the skin becomes drier and loses its natural elasticity. In people with either very pale or dark skin it may be difficult to notice abnormalities such as pallor or a bluish hue (cyanosis). This explains why it is important to also look at the mucosae, e.g. inside the mouth or the conjunctiva inside the lower eyelid, which in health should be pink and moist.
Changes in skin colour
The colour of the skin including the nail beds and the lips and the mucosae can provide valuable information:
Skin turgor and oedema
Assessment of the skin should include turgor and the presence of oedema. Turgor indicates the elasticity of the skin and although this decreases with age, skin turgor may be useful in a holistic assessment of hydration status. Reduced turgor may be an early sign of dehydration (see Ch. 19).
To assess skin turgor, a fold of skin, usually on the back of the hand, is lifted. Once released, it should quickly return to its original position. However, because skin loses its elasticity with age it will not return to its original position so quickly in older people.
Oedema is an abnormal accumulation of tissue fluid between the cells (see Ch. 19). It usually collects in dependent regions such as the legs, ankles/feet or sacral area. For example, if someone spends much of the day sitting in a chair, fluid will collect in the sacral area and ankles. This is partly due to immobility and lack of normal contraction of the calf muscles. Normally muscle contraction squeezes the veins and helps to maintain the return of venous blood to the heart (see Ch. 25). However, dependent oedema is also compounded by gravity, which allows fluid to collect in these areas. Oedema may be seen in people with the following conditions:
However, swollen ankles with some oedema may be found when standing still in hot weather or during pregnancy and are not necessarily a sign of ill health.
The term ‘pitting’ is used to describe oedema that remains indented or pitted when lightly pressed. This is frequently a sign of more severe oedema.
Oedema is not usually visible until the body has retained at least 4L of fluid, which is equivalent to approximately 4 kg of weight gain. An accurate way to record fluid balance is through daily weighing and people with heart failure who are prone to fluid retention, for example, are frequently asked to record their weight daily.
Capillary refill time
Capillary refill time is useful for assessing skin perfusion (amount of blood passing through the skin) and cardiac output. Although peripheral areas such as the nail bed may be used, central areas such as the sternum are more useful in people with a poor cardiac output and poor peripheral circulation. To test capillary refill time, two fingers are lightly pressed into the area for a period of 5 seconds. On release, the skin colour should return to normal within 2 seconds. If it takes longer for the skin colour to return, capillary refill time is prolonged and it is likely that the person has a low cardiac output.
Heart/pulse rate
When blood is pumped from the heart there is rhythmic expansion and recoil of the arteries in the vascular system. Wherever an artery is near the skin surface this ejection of blood will cause a pulse, which can be felt when the artery is gently pressed against a bony prominence. In adults and older children this is commonly felt at the wrist where the radial artery crosses the forearm bone, the radius (see Ch. 14). In babies aged less than 6 months HR is determined by using a stethoscope to count the apex beat of the heart (see Ch. 14).
The pulse rate should be easily palpated and is a useful measure of the function of the cardiovascular system. The pulse should reflect the HR and varies with age. It is normally between 60 and 80bpm in adolescents and adults at rest, although up to 100bpm is considered normal. In the neonate the HR is faster and is usually between 120 and 160bpm depending on whether the baby is active, crying, resting or asleep. The HR slows during infancy and childhood to reach adult levels during adolescence (see Ch. 14).
Box 17.9 outlines some situations and disorders in which HR is faster or slower than normal.
Box 17.9 Causes of tachycardia and bradycardia
A heart rate greater than 100bpm in an adolescent or adult may normally occur in the following situations:
Disorders of breathing and circulation that cause tachycardia include:
A heart rate of less than 60bpm in an adolescent or adult may occur in the following situations:
Disorders affecting breathing and circulation that cause bradycardia include:
A weak and thready pulse is frequently faster than normal and is found in dehydration (see Ch. 19), hypovolaemia or heart failure. A pulse that feels strong and bounding is also frequently fast and may indicate pyrexia, anxiety or hypervolaemia (high blood volume).
When a pulse is noted to be irregular, it should be reported and documented in the nursing notes and on the appropriate charts. Many heart diseases, such as atrial fibrillation (AF), cause an irregular pulse rate and commonly occur in older people. Further investigations should be undertaken an apex–radial pulse should be recorded and an ECG performed.
Apex and radial
Sometimes the radial pulse rate is not the same as the HR (pulse deficit). This can happen if the heart rhythm is abnormal. A disturbance in heart rhythm is called an arrhythmia, e.g. AF where the atria beat very rapidly but only some of the beats lead to a pulse. In these situations the pulse is likely to be irregular and a simultaneous recording of the apex beat and the radial pulse rate is useful (Box 17.10).
Recording apex–radial pulse (adult)
Note: To record an apex–radial pulse, two members of staff are needed.
Procedure
If there is a large difference between the two values, it can be concluded that the radial pulse rate does not accurately reflect the heart rate, i.e. there is a pulse deficit. A heart arrhythmia should be suspected and an ECG performed if this is a new sign (Riley 2003).
Peripheral pulses
Pulses are found wherever a blood vessel lies close to the skin surface. The radial pulse has been described above (see p. 479). Other peripheral pulses (see Fig. 14.10, p. 378) are assessed in a variety of specific situations. Peripheral pulses indicate the flow of blood to the peripheries and how well the heart is functioning. Additionally, they provide information on the state of the individual blood vessels, e.g. checking for the presence of the pedal pulse (dorsalis pedis) in the foot when a person has a sus-pected blockage in the arteries supplying the leg, or following surgery to clear a blockage (see Ch. 14 for further information).
The electrocardiogram
The ECG waveform depicts the electrical activity of the heart (see p. 466 and Fig. 17.4). It is used to detect arrhythmias and heart diseases such as myocardial infarction. Readers requiring more information about ECG should consult Further reading suggestions.
Blood pressure
Blood pressure (BP) is the pressure exerted upon the wall of the arteries by the circulating blood. It is a useful, non-invasive measurement, widely used in patient assessment (see Ch. 14). BP is usually measured indirectly using a sphygmomanometer (usually aneroid) or an electronic device. Mercury sphygmomanometers are being replaced as a safety measure because of the toxicity of mercury. BP is a routine aspect of health assessment in adults and at prescribed intervals for monitoring condition, e.g. after surgery or for hypertension. BP is less frequently recorded as part of assessment in children; however, in some cases BP can indicate the presence of congenital heart disease or kidney disease.
BP has two measurements and is measured in millimetres of mercury pressure (mmHg). The two measurements reflect different stages of the cardiac cycle (see p. 465): the upper reading, the systolic pressure, when the heart contracts (systole) and the lower reading, the diastolic pressure, when the heart is relaxed (diastole). As the heart contracts, blood is pumped from the left ventricle into the aorta and systemic arteries and this is recorded as the systolic BP. Following ventricular ejection, blood moves along the arteries, and the elastic vessel walls start to recoil. This is then recorded as the diastolic BP (see Ch. 14 for details of measuring BP).
The normal BP range varies with age: in adults the optimum BP is <120 systolic and <80 diastolic, and a normal BP is described as <130/,85 mmHg (Williams et al 2004). In the neonate, BP is normally between 60 and 85 systolic/20 and 60 diastolic mmHg (see Ch. 14).
In addition, there are many factors that normally influence BP throughout a 24-hour period (see Ch. 14). These include:
A sustained increase in BP is termed hypertension and in adults this is defined as a BP over 140/90 mmHg. For example, Grade 1 (mild) hypertension is systolic pressure between 140 and 159 mmHg and diastolic pressure between 90 and 99 mmHg (Williams et al 2004). BP tends to increase with age in developed countries. Lifestyle factors contributing to hypertension are outlined in Box 17.11.
[Resource: National Institute for Health and Clinical Excellence 2004 Hypertension (persistently high blood pressure) in adults. Understanding NICE guidance – a guide for people with hypertension, their families and carers, and the public. Online: www.nice.org.uk/pdf/CG018publicinfo.pdf Available July 2006]
Lifestyle and hypertension
Several lifestyle factors contribute to hypertension (Williams et al 2004). These include:
Hypertension is a serious condition and leads to many problems, e.g. CHD, heart failure, strokes, kidney damage and retinal changes. The BP is recorded on three separate occasions before treatment is commenced for hypertension. This is because there are several factors that may lead to inaccuracies in blood pressure readings in addition to ‘white coat’ hypertension where the anticipation of having BP recorded causes it to increase. Box 17.12 outlines some interventions to ensure the accuracy of BP measurement and recording.
[Reference: National Institute for Health and Clinical Excellence 2004 Hypertension (persistently high blood pressure) in adults. Understanding NICE guidance – a guide for people with hypertension, their families and carers, and the public. Online: www.nice.org.uk/pdf/CG018publicinfo.pdf Available July 2006]
Maximizing the accuracy of blood pressure measurement*
Measures that help to ensure accuracy include the following:
A low blood pressure that is insufficient to maintain tissue blood flow and oxygenation is termed hypotension. It may be caused by:
[Resources: Mohun et al (2002); St John Ambulance, First aid advice online – www.sja.org.uk/firstaid/info/bleeding.asp Available July 2006]
Dealing with minor bleeding and cuts and grazes
You and the community nurse are visiting Rodney who lives in sheltered accommodation when the carer mentions that he cut himself the other week. The cut was only small but it bled for a few minutes and no one was sure what they should do. The community nurse asks you to gather some information about dealing with minor cuts and grazes ready for your next visit to the client.
Hypotension may lead to feelings of dizziness or even fainting (syncope) because insufficient blood and hence oxygen reaches the brain. Fainting can also be caused by other factors. These include:
The first aid for fainting is outlined in Box 17.14.
Fainting
Treatment
Note: If the person does not start to regain consciousness quickly, open their airway and check breathing and circulation (see pp. 475–476, 478). Put the person into the recovery position (see Ch. 16) and call for medical assistance. If necessary, commence BLS (see pp. 473–478).
Central venous pressure
Central venous pressure (CVP) records the pressure in the central venous system or the right atrium of the heart and is a useful measurement to assess fluid status. A catheter is inserted into a large central vein, usually the internal jugular or subclavian vein, and attached to a monitoring device. Frequently a pressure transducer monitors and records the pressure in mm of mercury (mmHg). Occasionally a water column is used, in which case the measurement is recorded in centimetres of water (cmH2O). Central venous pressure is measured in the acutely ill and as such is frequently seen in intensive care or high dependency units. However, central venous pressures may also be measured in the patient on the general ward and so it is useful to have some idea of the importance of this measurement.
Breathing – general assessment
The assessment of breathing includes respiratory rate, depth and rhythm and assessment of the function of the lungs. Normal breathing at rest is silent, even and regular and is the unconscious active inspiration of air followed by passive expiration. However, both inspiration and expiration may become active with the person forcing air in or out of the lungs. Active breathing usually uses accessory muscles of breathing, the abdominal muscles and the muscles of the neck and shoulders. The use of the accessory muscles occurs in normal deep breathing and is also frequently seen in a person with breathing difficulties (see p. 483).
Respiratory rate
The respiratory rate should be recorded as one of the first observations in all general assessments and is referred to in greater depth in Chapter 14. In addition, the respiratory rate should be recorded as part of ongoing monitoring of vital signs, as ‘respiratory rate is a significant predictor of critical illness’ (Butler-Williams et al 2005, p. 35). When counting the respiratory rate, breathing should be observed for a 60-second period, with the person at rest. It is also a useful idea to count the respiratory rate without the person being aware and inadvertently altering their breathing rate.
The normal respiratory rate varies with age. The normal adult respiratory rate at rest is usually between 12 and 15 breaths per minute, while it is normal for a neonate to breathe at 30–60 breaths per minute (see Ch. 14).
A respiratory rate that is faster than that expected for age (tachypnoea) is normal when caused by:
Disorders of breathing and circulation that cause tachypnoea may include:
A respiratory rate that is slower then expected for age (bradypnoea) is normal when the person is sleeping; however, it is abnormal when caused by:
Breathing patterns – depth and rhythm
The breathing pattern should be assessed while counting the respiratory rate. When assessing breathing patterns the nurse should observe features that include:
[See Tables 17.2-17.4 (pp. 471–473) for further information about some conditions that affect breathing and circulation.]
Abnormal breath sounds
Normal breathing is silent. Any noise that occurs during breathing is therefore abnormal. The noise may occur either during inspiration or expiration. Abnormal sounds include:
[Resources: BBC – www.bbc.co.uk/health/first_aid_action/action_file_menu.shtml (Select asthma from Breathing difficulties); Interactive test – www.bbc.co.uk/health/first_aid_action/hs_child/hs_asthma.shtml All available July 2006]
Asthma attack
Cough and sputum
In health, regular deep breathing and ciliary action remove normal secretions and inhaled foreign particles. Secretions are generally swallowed but may be coughed up (expectorated). However, when these mechanisms are ineffective or there is an increase in mucus secretion or foreign particles, the cough becomes essential (Jones & Moffat 2002). A cough is the sudden and rapid expulsion of air from the lungs. Coughing may be voluntary or it may be an involuntary cough reflex. The cough reflex is part of the protective mechanisms that protect the airway from foreign bodies that either irritate or may obstruct the airway. The cough reflex occurs, for example, when food or fluid goes the ‘wrong way’.
Choking occurs when there is a partial blockage to the upper airway. The person will be anxious, have difficulty breathing and may start coughing. This may dislodge the foreign body but, if not, urgent treatment may be necessary to prevent asphyxia. This is characterized by severe hypoxia leading to hypoxaemia (reduced oxygen content in arterial blood) and hypercapnia (increased carbon dioxide in arterial blood). Unconsciousness occurs and eventually death without effective treatment. Choking has a number of causes but usually occurs when a foreign body, e.g. food such as peanuts, small toys or pieces of toys, loose tooth, pen top, etc., is inhaled.
The first aid treatment for an adult who is choking is outlined in Box 17.17. The first aid procedures for choking in infants and children differ from those in adults and readers are advised to consult Further reading (e.g. Mohun et al 2002). Obviously it is preferable to prevent choking in the first place by identifying the risks and excluding them whenever possible, such as by choosing toys suitable for a child’s age (Box 17.18).
Choking in adults
Treatment
[Resources: Child Accident Prevention Trust – www.capt.org.uk/FAQ/default.htm; Royal Society for the Prevention of Accidents (RoSPA) – www.rospa.com/homesafety/advice/child/accidents.htm Available July 2006]
Preventing choking in babies and small children
A friend who has a new baby and a toddler aged 18 months tells you that she and her partner are worried about the risk of choking, as they have heard how easily this can happen in babies and small children. She asks you about how they might reduce the risk as much as possible.
A cough may be described as dry or productive. Coughing may be associated with pain in some chest conditions and following chest or abdominal surgery (see Ch. 24). Prolonged coughing can cause muscle pain and may deter patients from coughing. The nurse should assess levels of pain and ensure that effective pain relief is provided (see Ch. 23).
A dry cough is one that develops without the presence of excess secretions. The cough could result from an irritant in the upper airway such as smoke or cold air and sometimes develops into a ‘tickly’ cough. Some forms of medication cause a dry cough, e.g. some heart medication such as angiotensin-converting enzyme (ACE) inhibitors. A constant dry cough is frequently a nuisance to the person and may result in them stopping their medication if they think this is the likely cause. For this reason it is important to listen to the patient’s complaints and inform the prescriber so that medication can be reviewed.
A productive cough is one where excess mucus or sputum (‘phlegm’) is present in the respiratory tract. When the airways are inflamed, as occurs during an infection, there is an excessive secretion of mucus, which then accumulates in the airways. The mucus is usually expectorated by coughing. A productive cough may also be found where ciliary action is ineffective. Smoking is known to damage the cilia, and is responsible for the so called ‘smokers cough’.
The nurse should observe the colour, consistency, quantity and odour of any sputum produced during coughing and record this information in the nursing notes and charts (Box 17.19). Any changes should be reported to the person in charge.
Box 17.19 Characteristics of sputum – colour, consistency, quantity and odour
A specimen of sputum will be sent to the laboratory for microscopy, culture and sensitivity if infection is suspected (see Ch. 15). Box 17.20 (p. 486) outlines the safe and effective collection of a sputum specimen. If the patient is unable to expectorate a specimen may be obtained during nasopharyngeal/tracheal suctioning (see pp. 490–491) by using a sputum trap.
Collection of a sputum specimen
Preparation
Procedure
Peak expiratory flow rate
The peak expiratory flow rate (PEFR) is the greatest rate of airflow out of the lungs and is measured in litres per minute (L/min) during a forced expiration. The normal range for PEFR depends on age, height and gender. It is an important measure of lung function and is frequently used as a guide to monitor the progress of a condition such as asthma or the person’s response to their medication. A Wright or mini-Wright peak flow meter is used to measure PEFR (Box 17.21).
[Further reading: Higgins D 2005 Measuring PEFR. Nursing Times 101(10): 32–33]
Measuring peak expiratory flow rate (Fig. 17.11)
Preparation
Procedure
Pulse oximetry
Pulse oximetry is used to measure the percentage of saturated haemoglobin in the arterial blood and gives a useful indication of the amount of oxygen in the peripheral blood. Oxygen saturation monitoring is frequently undertaken, either continuously or as a periodic measurement. The normal oxygen saturation range is 94–98%.
The measurement is performed with a non-invasive pulse oximeter, a device comprising a probe connected to a monitor (Fig. 17.12). The probe should be placed where it is in close contact with the blood such as the nail bed or ear lobe. The pulse oximeter measures and displays the peripheral capillary saturation of haemoglobin (SpO2) (Allen 2004). Pulse oximetry has limitations and results must be interpreted carefully (Box 17.22).
[Further reading: Higgins D 2005 Pulse oximetry. Nursing Times 101(6):34–35]
Mr Jones
Arterial blood gas analysis, an invasive procedure, may be used in critically ill people to directly measure the amount of oxygen and carbon dioxide in the blood and other parameters that include blood pH (see Ch. 19).
Pain associated with breathing or circulation problems
Pain is abnormal and, if present, may indicate circulatory or breathing problems. It can be caused by a variety of conditions and may be either cardiac or non-cardiac in origin. As with any pain, it is important for the care team to identify the cause so that appropriate pain relief and management can be planned (see Ch. 23).
The following points should be considered when assessing the person with pain associated with breathing or circulation problems:
It is important, however, to remember that it is not always easy to ascertain answers to questions about levels and sites of pain. People with a learning difficulty or speech problems can find it difficult to describe pain or its location, while a child’s response to pain is linked to their developmental stage (see Ch. 23).
Common investigations – breathing and circulation
There are many different investigations used to identify disorders affecting breathing and circulation and some of these are outlined in Box 17.23. Box 17.24 provides an opportunity to find out what a cardiac investigation can involve.
Box 17.23 Common investigations – breathing and circulation
[Resources: BBC – www.bbc.co.uk/health/talking/tests Available July 2006]
The following investigations may be used to diagnose or evaluate treatment for disorders affecting breathing and circulation.
A simple explanation of some of these investigations accessed on the BBC website will help you provide patients with information; more detailed nursing explanation can be found in Riley (2003).
Care of the person with breathing and/or circulation problems
Breathing and circulation problems may affect people of all ages and causes range from respiratory problems such as poor oxygenation, cardiac causes when the heart is unable to pump oxygenated blood around the body or blood disorders when there is insufficient oxygen delivered to the body tissues and organs due to a low haemoglobin level (see Tables 17.2-17.4, pp. 471–473). Problems associated with breathing and circulation such as dyspnoea (see Box 17.15, p. 483) or profound fatigue may impact upon all aspects of life: physical functioning and daily activities, and psychological and social aspects.
This section of the chapter outlines the basic, but essential, aspects of care needed by patients who have breathing and circulation problems, helping with expectoration, inhaled medication, oxygen therapy, respiratory support, blood transfusion and rehabilitation.
Communication and relief of anxiety
Breathlessness is extremely frightening and may increase anxiety, which in turn makes the patient more breathless (Prigmore 2005). Communication is both important yet difficult. Communication is a two-way process and this is difficult for the person who is struggling for breath, has a breathing tube, e.g. tracheostomy (opening in the trachea), requires continuous oxygen therapy or who is too breathless to form words (Box 17.25). The nurse must maintain a calm appearance, use gentle touch and appropriate eye contact to provide reassurance. Additionally, alternative communication strategies should be employed such as a pen and pad or a word or picture board. Giving the patient time to express their feelings is clearly important and the nurse should use both verbal and non-verbal cues to ensure that they do not feel rushed. When talking is very difficult, the use of closed questions that do not require long answers may also be useful (see Ch. 9).
Positioning to relieve breathlessness
Patients feeling breathless should be supported by pillows in an upright position, either in bed or in a chair. This will increase their lung expansion, which assists gaseous exchange in the alveoli. Breathing may also be easier if they lean forward slightly on pillows placed on a bedside table (Fig. 17.13).
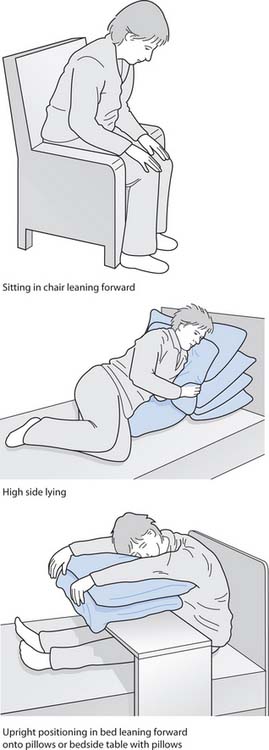
Fig. 17.13 Position for relieving breathlessness
(reproduced with permission from Brooker & Nicol 2003)
The breathless person is likely to feel anxious if laid flat. However, if they are comfortable lying down, they should lie with their back straight, again to assist with chest expansion. Opening a window may also help someone who is struggling to breathe.
Personal hygiene and skin care
Patients may need help with personal cleansing and dressing depending on how breathless they are and the degree of fatigue caused by poor oxygenation and the constant struggle to breathe (see Ch. 16). They may need extra time to wash and also the opportunity to rest during personal hygiene. Additionally, if mouth breathing (see Box 17.2, p. 469), they will have a dry mouth and require oral hygiene, mouth washes and ice to suck.
Patients with breathing difficulties are likely to have poor oxygenation and consequently some degree of tissue hypoxia. This, combined with factors such as underlying disease, reduced mobility, sliding down from the upright position and poor nutrition, will make them susceptible to pressure ulcers. It should therefore be assumed that any person with a breathing problem is at risk of developing a pressure ulcer and scoring using a pressure ulcer risk tool should be used so that appropriate measures to prevent their occurrence can be implemented. Regular repositioning, mobilization and the use of pressure-relieving devices should be considered (see Ch. 25).
Nutrition and hydration
The breathless patient frequently finds it difficult to eat because of a dry mouth and may also feel nauseated, particularly if they are swallowing secretions. The provision of small, frequent meals helps the breathless person maintain an adequate dietary intake (see Ch. 19). Adequate nutrition to cope with the increased work of breathing is essential in the person with a chronic breathing problem who may also require a high protein diet. The dietitian should be approached for advice.
Mouth breathing makes their mouth dry and uncomfortable. Additionally, the patient may have an increased respiratory rate or pyrexia (see Ch. 14) that will increase fluid loss from the body. Attention to adequate hydration in the breathless patient is essential, not only for their overall fluid balance, but also for their comfort. A dry mouth rapidly leads to cracked lips and discomfort (see Ch. 16) and dehydration (see Ch. 19) and will lead to viscous secretions. Plugging of the airways may result.
Helping the person with expectoration
Increased and/or viscous secretions make breathing more difficult and the nurse should work with the physiotherapist to assist expectoration and maximize breathing effort.
Breathing exercises and coughing
Secretions can be moved and expectorated by deep breathing exercises and coughing. The patient should be encouraged to increase their fluid intake so that they can more easily expectorate the secretions. It is important to provide the patient with clean sputum cartons with lids as required and mouth washes/teeth cleaning facilities after expectoration. A specimen of sputum may be requested (see Box 17.20, p. 486). The nurse should advise the patient to avoid swallowing secretions, as this can lead to nausea.
Patients with chest infections or those who are susceptible to an infection, e.g. postoperatively or with rib fractures, should be encouraged to breathe deeply at intervals. The nurse must ensure that effective analgesics are administered to allow this without pain. Deep breathing with expansion of both lung bases is easiest with the spine straight. This is either in the upright sitting position or with the back straight when lying flat. This will expand the lung bases and facilitate gaseous exchange and clearance of basal secretions.
Breathlessness is extremely frightening and breathing exercises may control and help the person restore their normal breathing pattern during an attack of breathlessness or following a bout of coughing. Usually the patient will find these exercises easier if they are in a half side-lying position. They should be encouraged to breathe out gently while relaxing their shoulders and upper chest. When breathing in, this should also be gentle, and they should feel their lower ribs and upper abdomen expand. They should be encouraged to breathe gently, with minimal effort. Patients prone to panic attacks and attacks of breathlessness should be encouraged to practise this technique.
‘Huffing’ and coughing are useful techniques to help expectorate secretions. Huffing is thought to be less tiring than coughing and so it is useful to teach this to someone with chronic respiratory disease (Box 17.26).
Box 17.26 Huffing and coughing
Postural drainage
Sometimes postural drainage is needed to remove secretions, particularly in patients with chronic respiratory disease. In these circumstances the person lies in bed with the foot of the bed elevated. Gravity then assists the movement of secretions from areas of the lungs. Alternatively, the patient can lie on their side with pillows placed under their waist to gently tip their head down. The physiotherapist will modify the patient’s position to drain secretions from particular lobes or lung segments.
In small children with bronchiectasis or cystic fibrosis, a parent or carer may perform postural drainage.
Suctioning
In some circumstances it may be necessary to use suction to remove secretions from the airway. This is more likely when there is an artificial airway such as an endotracheal tube (a plastic tube introduced through the mouth or nose into the trachea to secure or maintain the airway) or tracheostomy tube (Fig. 17.14 and Box 17.27), the person is sedated or unconscious, when there is a poor cough reflex as may occur following a stroke or head injury, or when the patient is too weak to expectorate.
A tracheostomy is a surgical opening into the trachea through the front of the neck. The tracheostomy is kept open with a tracheostomy tube (see Fig. 17.14). It facilitates breathing, oxygen therapy or clearance of secretions and may be short or long term.
Common reasons for a tracheostomy include:
[Further reading: Harkin H, Russell C 2001 Tracheostomy patient care. Nursing Times 97(25):34–36; Russell C 2005 Providing the nurse with a guide to tracheostomy care and management. British Journal of Nursing 14(8):428–433]
Suctioning should only be undertaken by someone who is competent to do so. The nurse should therefore have been taught how to undertake the procedure and observed in order to confirm competence. Patients and parents can also be taught how to perform suctioning when long-term assistance with clearing of secretions is required, e.g. a child or adult discharged home on home ventilation (see pp. 495–496).
Suctioning should be performed as a clean procedure. The nurse should wash their hands and protect themselves from infection by wearing a clean (not necessarily sterile) glove on both hands, plastic apron and eye protection if necessary.
Readers can find more information about suctioning in Further reading suggestions (e.g. Nicol et al 2004, Higgins 2005).
Inhaled medication
Inhaled medication is frequently used in the management of respiratory diseases such as asthma or COPD because the drug acts more quickly when it is administered directly to the site of action. Drugs administered in this way include bronchodilators (e.g. ipratropium bromide), antibiotics or corticosteroids (see Ch. 22).
There are various ways to administer inhaled medication, including:
Nebulizers (Fig. 17.15A, p. 492)
A nebulizer can be used to administer medication or to liquefy secretions with 0.9% saline solution. The drug is inhaled and is rapidly absorbed through the alveolar blood supply. It therefore acts quickly and side-effects associated with oral intake are avoided. Most nebulizers require a flow of gas and will be administered either with compressed air or oxygen. The nebulizer breaks up the solution so that it is inhaled as small droplets suspended in a gas. The use of a nebulizer is outlined in Box 17.28 (p. 492).
(reproduced with permission from Nicol et al 2004). B. Metered-dose inhaler. C. Inhaler with spacer attached
Use of a nebulizer
Procedure
Note: When more than one medication is prescribed for the nebulizer; they should not be mixed and should be administered one after the other, with the bronchodilator (if prescribed) given first. This will open the airways and facilitate more effective treatment with the second drug. Each nebulizer should be labelled according to the medication use.
Dry powder inhalers
A dry powder inhaler releases medication as the person breathes in. The patient places their mouth around the device and breathes in. The flow generated by their breath releases the medication into particles that can be inhaled. These inhalers are easy to carry around and are therefore convenient to use at work, at home, in the car or at school.
The nurse should ensure that patients are able to use their inhaler effectively. Inhaler technique should always be checked by the practice nurse or general practitioner or before hospital discharge and on a regular basis in clinic.
Metered-dose inhalers (Fig. 17.15B, p. 492)
These are also available for inhaled medication and are frequently used by people with asthma. The inhaler is designed to deliver a dry powder and the medication, which is forced into the lungs.
Before use the inhaler is shaken to distribute the powder evenly within the gas. The cap is removed and the inhaler is held upright. To be effective, the patient should breathe out gently and then place their mouth around the mouthpiece of the inhaler. As they start to breathe in, the canister top should be pressed to release the medication. The breath should be slow and deep, and held for approximately 10 seconds. Usually the prescribed dose is for more than one ‘puff’ in which case the subsequent doses should be taken after approximately 30 seconds.
Using the inhaler requires a degree of coordination and may therefore not be suitable for children, some people with learning disabilities, some older people or those with poor dexterity (Box 17.29, p. 493). Spacer devices are available which are easier to use (Fig. 17.15C, p. 492). They comprise a large and, usually, cone-shaped device, onto which the inhaler is fitted and are thought to be effective when used with regular breathing.
[Further reading: Huband & Trigg, Ch. 16, pp. 144–149 (2000)]
Rosie
4-year-old Rosie needs to have inhaled medication to control her asthma symptoms.
Oxygen therapy
Oxygen is a drug and should always be prescribed, except in an emergency situation such as cardiopulmonary arrest. The prescription should indicate the oxygen concentration, e.g. 24%, and flow rate in L/min. This includes oxygen delivered by any method, e.g. by mask (face or tracheostomy), nasal cannulae or an incubator, etc. Oxygen is given, usually in the short term, to relieve hypoxia while the underlying cause of the problem is urgently sought.
Oxygen is a potentially hazardous substance. It supports combustion and therefore requires certain precautions:
Additionally, the administration of high levels of oxygen can be dangerous and may lead to:
Problems associated with oxygen therapy
There are various physical, psychological and social problems associated with oxygen therapy, many of which are similar to those experienced by patients who are breath-less (see pp. 488–490) (Box 17.30). The problems include:
Pete
15-year-old Pete has required continuous oxygen therapy for the past 2 days. The bridge of his nose is sore and he does not want to wear the facemask any longer. His mouth is dry, he has no appetite and is reluctant to drink. Pete is very quiet and does not want to see visitors.
Oxygen administration systems
Oxygen is supplied via a piped system in hospitals or in standard colour-coded cylinders (black with a white top) in the community and occasionally in hospital (Fig. 17.16, p. 494).
Oxygen can be administered in a variety of ways (Fig. 17.17, p. 494), including:
The administration method chosen will depend upon age, the reason for administration, whether it is short or long term and where possible the patient’s preferences. For example, a young child or baby may not tolerate an oxygen mask and so a headbox or incubator may be used.
Oxygen may be given as a short-term treatment, e.g. postoperatively. However, long-term oxygen therapy (LTOT) may be needed for a patient with COPD, and arrangements must be made for oxygen therapy to be supplied at home (Box 17.31, p. 494).
Box 17.31 Long-term oxygen therapy
[Reference: NICE 2004 Chronic obstructive pulmonary disease. Quick reference guide. Online: www.nice.org.uk/pdf/CG012quickrefguide.pdf Available July 2006]
LTOT is supplied at home for patients with COPD who meet certain criteria; for example, ‘Patients should breathe supplemental oxygen for at least 15 hours/day’ (NICE 2004, p. 9).
‘Oxygen converters should be used to provide the fixed supply at home for LTOT’ (NICE 2004, p. 9). Oxygen converters remove nitrogen from room air to provide a high concentration of oxygen for the patient.
In addition, ambulatory oxygen is supplied to patients having LTOT who want to continue with treatment outside their home.
Fixed performance Venturi systems (high-flow)
Fixed performance facemasks deliver a high flow of gas achieved by entraining atmospheric air to give a fixed and accurate oxygen concentration (Higgins 2005) (see Fig. 17.17A). Masks are available that provide oxygen at various concentrations (24%, 28%, 35%) and the oxygen flow rate is set between 4 and 8L/min according to the manufacturer’s instructions. Specific high-flow masks are available for use with tracheostomy tubes. Humidification should be used with high-flow masks.
Variable performance systems
These systems use a low-flow mask, e.g. a Hudson mask, and are frequently used either in the emergency situation or for a person recovering from an anaesthetic (see Fig. 17.17B). With an oxygen flow rate of between 6 and 10L/min, a concentration of up to 60–70% can be given.
Nasal cannulae/nasal prongs
Nasal cannulae/prongs are small plastic tubes, which are inserted into each nostril to administer oxygen (see Fig. 17.17C). The cannulae are secured by tubing over the ears. Oxygen flow rates of approximately 2L/min are used. Higher flow rates may cause discomfort and drying of the nasal mucosa, which will damage the delicate mucosal lining.
The system enables the patient to also breathe room air and so does not require an elaborate humidification system. Their use also enables the patient requiring oxygen to eat, drink or talk and is therefore useful alongside a standard oxygen facemask for short-term use. Nasal cannulae are available in small sizes for infants and young children.
Headbox, body/trunk box
A headbox is frequently used for infants up to about 8 months of age, requiring oxygen, as it is unlikely that they will tolerate a facemask. Boxes, which are integral to a baby chair, e.g. Manchester chair, are available for older infants (Huband & Trigg 2000). This system allows the infant to be nursed in a more upright position.
The clear plastic headbox is placed around the infant’s head and neck. Humidified oxygen is delivered into the box and the infant breathes air with a higher oxygen concentration (see Fig. 17.17D). The oxygen flow rate should be sufficient to prevent the accumulation of carbon dioxide in the head box. An oxygen analyser probe is used within the box to ensure that the infant receives the correct oxygen concentration. The clear nature of the headbox means that the infant can see out while also being observed for signs of deterioration such as increased respiratory rate.
Oxygen tent
Oxygen tents are predominantly used when infants or young children will not tolerate an oxygen mask. The oxygen is supplied to an oxygen tent placed over the bed. The child is free to move in the bed, while still breathing a higher oxygen concentration than room air. However, they are infrequently used today due to their several disadvantages. There is a high concentration of oxygen within the oxygen tent and the risk of fire is increased, observation of the child is limited and oxygen concentration falls every time the tent is opened for monitoring, care or treatment.
Incubator
An incubator is useful for the preterm or sick baby where the percentage of oxygen in inspired air can be easily controlled while also providing a stable temperature. These are frequently used for the very ill or preterm neonate.
Continuous positive airway pressure (CPAP)
CPAP is increasingly used to correct hypoxaemia. A tight-fitting mask is placed around the mouth and nose and positive pressure is applied throughout both inspiration and expiration in a spontaneously breathing patient. CPAP is useful to improve oxygen saturations. Not all patients, however, are able to tolerate CPAP and air swallowing can lead to gastric distension with vomiting and aspiration. Careful monitoring of the patient is important with checks made on respiratory rate and effort, oxygen saturations, blood pressure and heart rate.
Because the mask needs to fit securely the skin condition should also be checked. The bridge of the nose is liable to pressure from the tight-fitting mask. A small piece of DuoDERM® or protective material placed over this area may increase patient comfort. Additionally, it is important to ensure that there is no air leak around the eyes, as the high-flow oxygen can dry and irritate the eyes and cause conjunctivitis.
Humidification
Water vapour is present in atmospheric air to a greater or lesser extent and so when breathing atmospheric air humidification is dependent upon the environmental humidity. Normal air humidity is between 40 and 60% and depends on temperature. Further water vapour is normally added to inspired air as it passes through the upper airways (see pp. 468–469). However, humidification of inspired air is impaired in situations that include:
Various hot- and cold-water devices are available for the humidification of inspired air and one such device is shown in Figure 17.18 (p. 496).
Respiratory support – artificial ventilation
This term refers to the process whereby a mechanical device (a ventilator) ventilates the lungs with gases. It is usually delivered through an endotracheal or tracheostomy tube, which is attached to a ventilator that pushes oxygen into the lungs. They are frequently used in the intensive care unit or operating theatre when the person is unable to breathe adequately. This process is referred to as intermittent positive pressure ventilation (IPPV). Readers requiring more information should consult Further reading (e.g. Woodrow 2000).
Non-invasive intermittent positive pressure ventilation
Artificial ventilation can also be delivered using non-invasive intermittent positive pressure ventilation (NIPPV), also known as non-invasive ventilation (NIV). A mask is used to avoid the need for an endotracheal tube or tracheostomy.
A mask covers the mouth and/or nose and is attached to a mechanical ventilator that pushes oxygen into the lungs. It is useful in nocturnal hypoventilation, a syndrome related to sleep apnoea (see Ch. 10). It is also used in severe muscle fatigue, neuromuscular weakness, COPD and in severe heart failure. NIPPV may be used almost continuously or on a sporadic basis for someone who only requires support at night. It is therefore increasingly used at home for both adults and children who require longer-term assistance with breathing while living at home. However, if this is to be effective it is essential that not only do the family receive accurate information beforehand, but they also receive adequate support. People on home ventilation understandably worry that they may suffer equipment failure and back-up systems and emergency plans should be decided upon in advance.
Although NIPPV can enable the person to live at home, travel and stay with friends, the device is heavy and awkward to move. It is frequently noisy to use and this may be a significant problem when cohabiting couples share a bed.
Care of patients requiring a blood transfusion
Blood transfusions can be life saving but they are expensive and can be hazardous. The risks associated with a blood transfusion using donor blood include transfusion reactions, fluid overload and also the risk of acquiring variant Creutzfeldt–Jakob disease (vCJD).
A blood transfusion may be required for a variety of reasons, including:
For the person with anaemia, or awaiting major surgery where blood loss is expected, every attempt should be made to improve haemoglobin levels through measures including oral iron supplements and a diet rich in available iron (see Box 17.1, p. 467).
In the UK, transfused blood is usually obtained from a healthy volunteer donor. Donors are asked a series of health questions and have a check on their haemoglobin level to ensure that the donation will be safe for both donor and patient. All donated blood is screened for hepatitis B and C, human immunodeficiency virus (HIV) and syphilis. In addition, other tests may be performed, e.g. if the donor has recently returned from certain countries. The blood is stored in a blood bank at around 4°C and labelled with the blood group and type.
Whole blood is transfused but various blood components, e.g. platelets, may be used in specific situations (Box 17.32).
Box 17.32 Blood and blood products
Prior to transfusing blood, the recipient’s blood should be cross-matched in the laboratory to ensure ABO blood group and rhesus factor compatibility with that of the donor (see Table 17.1, p. 468). This is done to prevent a transfusion reaction where the donor erythrocytes clump together (agglutinate) and block small blood vessels.
Monitoring during blood transfusion
Prior to commencing a blood transfusion it is important to obtain baseline recordings of temperature, pulse rate, blood pressure and respiration rate. These should then be repeated according to local policy during the transfusion, e.g. recorded every 15 minutes for the first hour and thereafter recorded hourly if the person is well and shows no adverse effects until the unit of blood is transfused. However, when more than one unit of blood is given, the observations should be recommenced at 15 minute intervals with each new unit of blood. The early signs of a transfusion reaction, including fever and rigors, should be observed. If a severe reaction occurs, BLS (see pp. 473–478) may be required.
Fluid balance is monitored and recorded and this includes recording the volume of blood transfused. It is generally assumed that a unit of whole blood is 500 mL and a unit of packed red cells is 300 mL. For more accurate recording of fluid volume, the unit of blood should be weighed. Grams of weight approximate to millilitres of volume, i.e. a unit of blood weighing 490 g is recorded as 490 mL.
When monitoring fluid balance (see Ch. 19) it is also important to record urine output. If a transfusion reaction occurs the donor erythrocytes agglutinate and can cause kidney damage. If the patient complains of loin or back pain, a sample of urine should be observed and tested for haematuria (blood in the urine).
Fluid balance is of particular importance in older people, the very young or those with cardiac or respiratory failure, when circulatory overload may lead to hypertension and pulmonary oedema. This is characterized by increasing respiratory rate, dyspnoea and agitation.
Documentation is important. All observations should be clearly recorded. In addition, the start and finish times of each unit of blood should be documented.
Ensuring transfusion safety
Due to the danger associated with the transfusion of incorrect or incompatible blood and other complications, hospitals and community settings have their own strict blood transfusion policy that must be observed. Although blood should be administered at room temperature it should be removed from the blood bank fridge no more than 30 min/1 hour before transfusion, and, preferably, only 15 minutes prior. The local policy regarding the checking procedure on removal from the blood bank and prior to commencing the transfusion, including patient identification, must be undertaken and a qualified nurse should always take responsibility for this procedure.
The safe disposal of equipment is essential. Gloves should be worn when handling blood or intravenous administration sets to protect staff from blood-borne diseases (see Ch. 15).
When completed, the transfused blood packs should be returned to the laboratory if a transfusion reaction is suspected. Otherwise, the disposal of blood bags should be in accordance with the local policy. Due to concerns over vCJD, any blood products or blood waste must be incinerated.
Transfusion complications
Complications associated with blood transfusion include:
Box 17.33 Blood incompatibility
Transfusion of the wrong or incompatible blood is extremely serious and can lead to life-threatening complications, e.g. kidney failure. It may occur because a mistake has been made with blood samples or the vital bedside checks have not been followed.
When a transfusion reaction is suspected the registered nurse should immediately stop the transfusion and obtain urgent medical assistance. The intravenous access should be kept patent with 0.9% saline. The haematologist should be contacted and any remaining blood returned to the laboratory for investigation.
Readers requiring more information about complications should consult Further reading (e.g. Bywater & Rawlings 2003).
Alternatives to donated blood transfusion
Apart from blood conservation through minimizing loss, the alternatives to the transfusion of donor blood include:
Rehabilitation for conditions affecting breathing or circulation
Rehabilitation for people with conditions affecting breathing and/or circulation aims to restore someone to as normal a situation as possible (see Ch. 11); for example, for the breathless person, the ability to function in normal activities of daily living such as washing, dressing, cooking and shopping and return to work if possible. This will include issues such as managing their symptoms, advice to prevent worsening of their condition, increasing exercise tolerance and improving psychosocial coping.
Rehabilitation programmes are provided for people after a heart attack and for those with COPD. Programmes should use a holistic approach to focus on the needs of each individual but are likely to involve education, exercise, and counselling and support. For example, a programme for a breathless person will include:
| BBC | www.bbc.co.uk/health |
| Available July 2006 | |
| British Committee for Standards in Haematology – Guidelines | www.bcshguidelines.com |
| Available July 2006 | |
| British Heart Foundation | www.bhf.org.uk |
| Available July 2006 | |
| British Thoracic Society | www.brit-thoracic.org.uk |
| Available July 2006 |
Allen K. Principles and limitations of pulse oximetry in patient monitoring. Nursing Times. 2004;100(41):34-37.
British Heart Foundation. 2005 Coronary heart disease statistics. Online: www.heartstats.org.
British Thoracic Society. The burden of lung disease. London: British Thoracic Society, 2001.
Brooker C, Nicol M, editors. Nursing adults. The practice of caring. Edinburgh: Mosby, 2003.
Butler-Williams C, Cantrill N, Maton S. Increasing staff awareness of respiratory rate significance. Nursing Times. 2005;101(27):35-37.
Bywater L, Rawlings E. Nursing patients with blood disorders. In: Brooker C, Nicol M, editors. Nursing adults. The practice of caring. Edinburgh: Mosby, 2003.
Higgins D. Oxygen therapy. Nursing Times. 2005;101(4):30-31.
Huband S, Trigg E. Practices in children’s nursing. Edinburgh: Churchill Livingstone, 2000.
Jones M, Moffat F. Cardiopulmonary physiotherapy. Guildford: BIOS Scientific, 2002.
Mallik M, Hall C, Howard D. Nursing knowledge and practice. London: Baillière Tindall, 1998.
MacGregor J. Introduction to the anatomy and physiology of children. London: Routledge, 2000.
Margereson C, Riley J. Cardiothoracic surgical nursing: current trends in adult care. Oxford: Blackwell Publishing, 2003.
National Patient Safety Agency (NPSA). 2004 Patient safety alert 02. Establishing a standard crash call telephone number in hospitals. Online: www.npsa.nhs.uk.
Nicol M, Bavin C, Bedford-Turner S, Cronin P, Rawlings-Anderson K. Essential nursing skills, 2nd edn. Edinburgh: Mosby, 2004.
Prigmore S. Assessment and nursing care of the patient with dyspnoea. Nursing Times. 2005;101(14):50-53.
Resuscitation Council (UK). 2005 Adult basic life support. Online: www.resus.org.uk/pages/bls.pdf.
Riley J. Nursing patients with cardiovascular disorders. In: Brooker C, Nicol M, editors. Nursing adults. The practice of caring. Edinburgh: Mosby, 2003.
Waugh A, Grant A. Ross and Wilson’s anatomy and physiology, 9th edn. Edinburgh: Churchill Livingstone, 2001.
Williams B, Poulter NR, Brown MJ, et al. British Hypertension Society Guidelines. Guidelines for the management of hypertension: report of the fourth working party of British Hypertension Society, 2004 – BHS IV. Journal of Human Hypertension. 2004;18:139-185.
Brooker C, Nicol M, editors. Nursing adults. The practice of caring. Edinburgh: Mosby, 2003. Chs 18–21
Bywater L, Rawlings E. Nursing patients with blood disorders. In: Brooker C, Nicol M, editors. Nursing adults. The practice of caring. Edinburgh: Mosby, 2003.
Higgins D. Tracheal suction. Nursing Times. 2005;101(8):36-37.
Mohun J, John K, Lee T, editors. First aid manual. Editorized manual of St John Ambulance, St Andrew’s Ambulance Association and The British Red Cross, 8th edn, London: Dorling Kindersley, 2002.
Moore T. Suctioning techniques for the removal of respiratory secretions. Nursing Standard 18(9):47–53, Quiz 54–55. Erratum 2003, Nursing Standard. 2003;18(13):31.
Moore T, Woodrow P. High dependency nursing care. London: Routledge, 2004.
Nicol M, Bavin C, Bedford-Turner S, Cronin P, Rawlings-Anderson K. Essential nursing skills, 2nd edn. Edinburgh: Mosby, 2004.
Sheppard M, Wright M. Principles and practice of high dependency nursing, 2nd edn. Edinburgh: Baillière Tindall, 2006.
Waugh A, Grant A. Ross and Wilson’s anatomy and physiology, 10th edn. Edinburgh: Churchill Livingstone, 2006.
Woodrow P. Intensive care nursing: a framework for practice. London: Routledge, 2000.
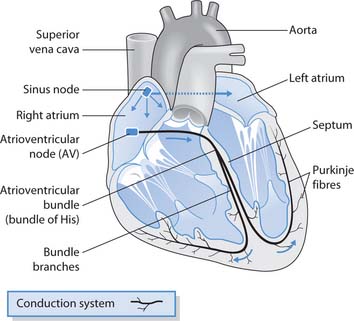
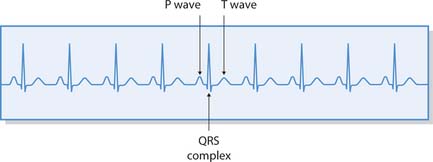
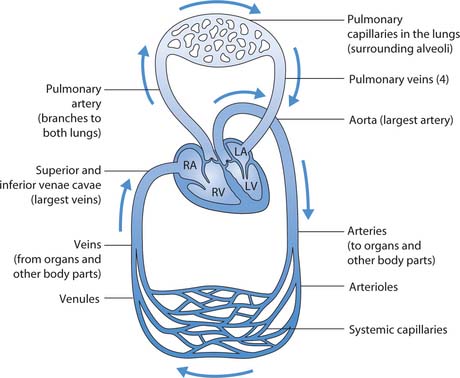
 HEALTH PROMOTION
HEALTH PROMOTION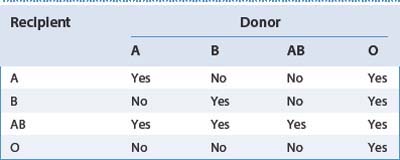
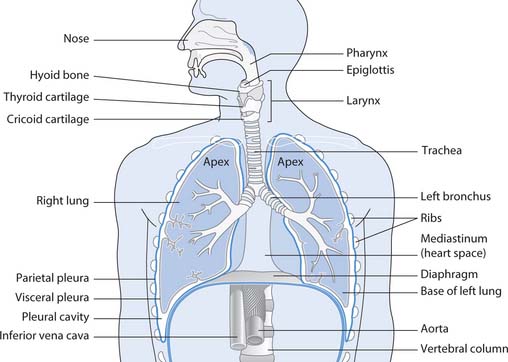
 FIRST AID
FIRST AID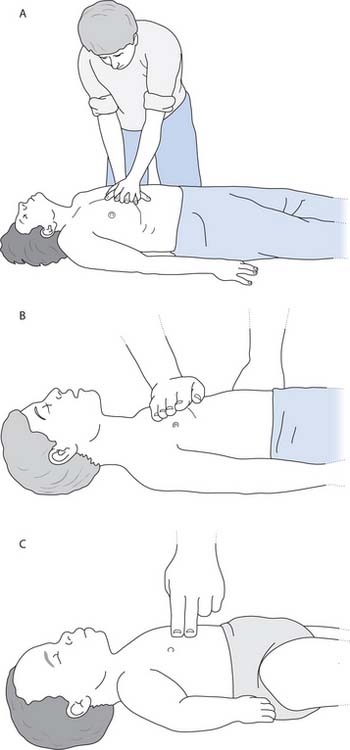
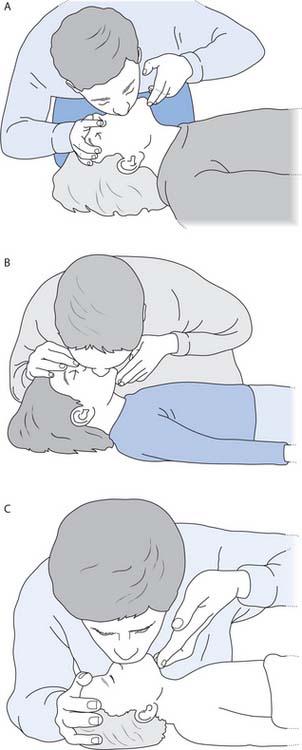
 NURSING SKILLS
NURSING SKILLS REFLECTIVE PRACTICE
REFLECTIVE PRACTICE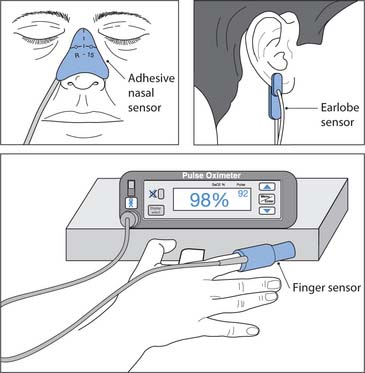
 CRITICAL THINKING
CRITICAL THINKING