Conditions That Produce Fluid and Electrolyte Imbalance
http://evolve.elsevier.com/wong/ncic
The Child with Cardiovascular Dysfunction, Ch. 34
The Child with Gastrointestinal Dysfunction, Ch. 33
Diaper Dermatitis, Ch. 13
Disorders Affecting the Skin, Ch. 18
Family-Centered Care of the Child During Illness and Hospitalization, Ch. 26
Family-Centered Care of the Child with Chronic Illness or Disability, Ch. 22
Family-Centered Home Care, Ch. 25
Injury Prevention: Infant, Ch. 12; Toddler, Ch. 14; School-Age Child, Ch. 17
Intestinal Parasitic Diseases, Ch. 16
Pain Assessment and Pain Management, Ch. 7
Gastrointestinal Disorders
Diarrhea is a symptom that results from disorders involving digestive, absorptive, and secretory functions. Diarrhea is caused by abnormal intestinal water and electrolyte transport. Worldwide, there are an estimated 1.3 billion episodes of diarrhea each year. Approximately 24% of all deaths in children living in developing countries are related to diarrhea and dehydration. Most children living in developed countries have mild forms of gastroenteritis. However, in the United States, approximately 200,000 children younger than age 5 are hospitalized and approximately 200 children younger than 5 years die of diarrhea and dehydration each year (Malek, Curns, Holman, et al, 2006; Staat, 2006).
Diarrhea is caused by abnormal intestinal water and electrolyte transport. The transport of fluid and electrolytes in the developing gastrointestinal (GI) tract is related to the child’s age. The intestinal mucosa of the young infant is more permeable to water than that of an older child. Therefore in young infants with increased intestinal luminal osmolality caused by diarrhea, more fluid and electrolytes are lost than in older children (Box 29-1). Diarrhea results from several pathophysiologic processes.
Types of Diarrhea
![]() Diarrheal disturbances involve the stomach and intestines (gastroenteritis), the small intestine (enteritis), the colon (colitis), or the colon and intestines (enterocolitis). Diarrhea is classified as acute or chronic.
Diarrheal disturbances involve the stomach and intestines (gastroenteritis), the small intestine (enteritis), the colon (colitis), or the colon and intestines (enterocolitis). Diarrhea is classified as acute or chronic.
![]() Case Study—Acute Diarrhea (Gastroenteritis)
Case Study—Acute Diarrhea (Gastroenteritis)
Acute diarrhea, a leading cause of illness in children younger than 5 years of age, is defined as a sudden increase in frequency and a change in consistency of stools, often caused by an infectious agent in the GI tract (Box 29-2). It may be associated with upper respiratory or urinary tract infections, antibiotic therapy, or laxative use. Acute diarrhea is usually self-limited (<14 days’ duration) and subsides without specific treatment if dehydration does not occur. Acute infectious diarrhea (infectious gastroenteritis) is caused by a variety of viral, bacterial, and parasitic pathogens (Table 29-1).
TABLE 29-1
INFECTIOUS CAUSES OF ACUTE DIARRHEA
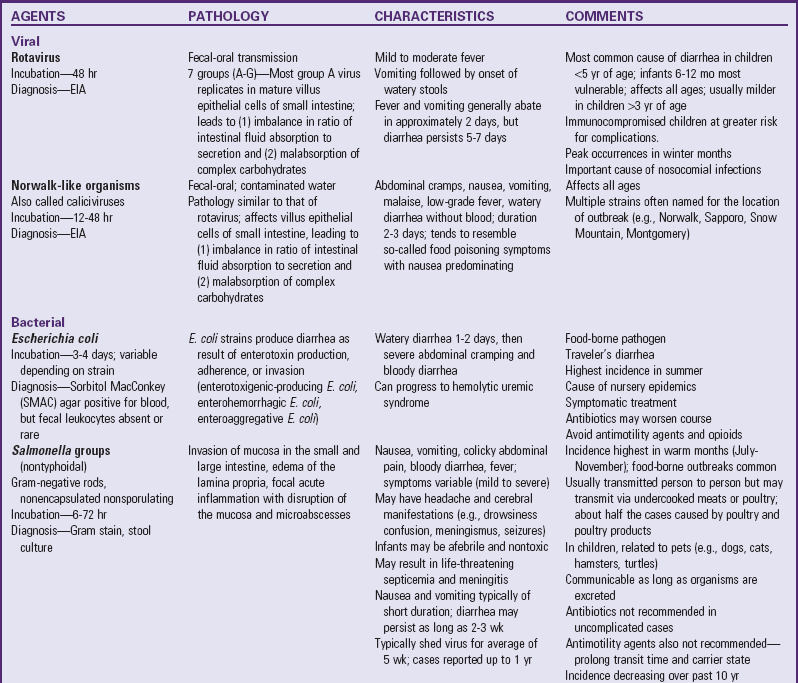
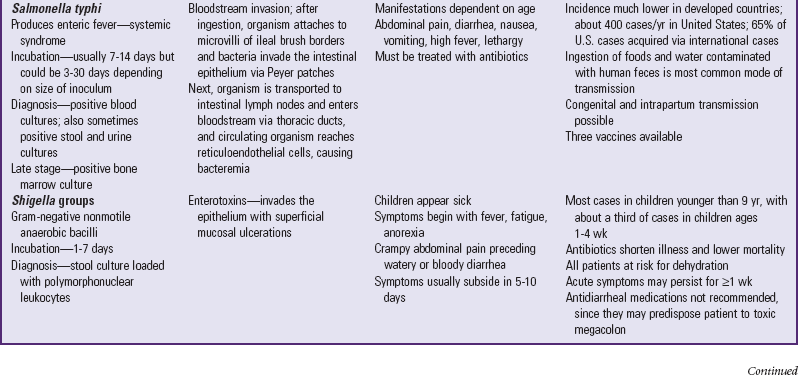
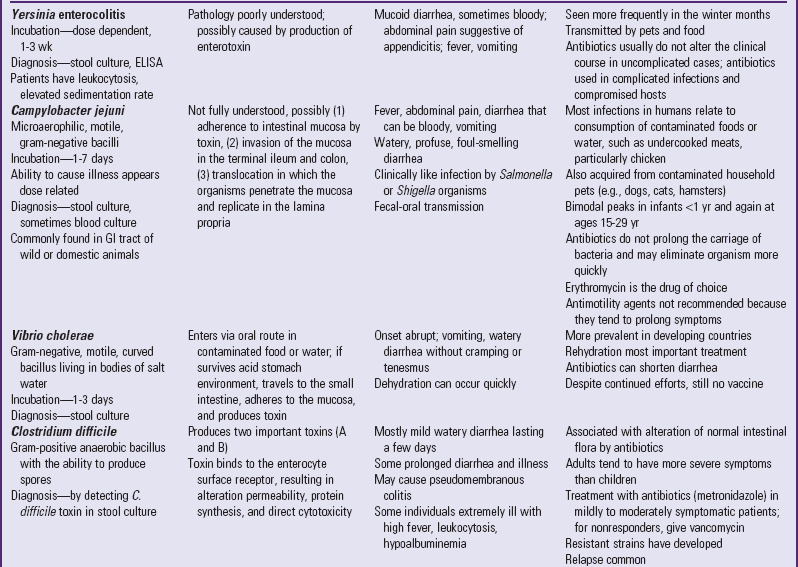
CNS, Central nervous system; EIA, enzyme immunoassay; ELISA, enzyme-linked immunosorbent assay; GI, gastrointestinal.
Chronic diarrhea is an increase in stool frequency and increased water content with a duration of more than 14 days. It is often caused by chronic conditions such as malabsorption syndromes, inflammatory bowel disease (IBD), immunodeficiency, food allergy, lactose intolerance, or chronic nonspecific diarrhea, or as a result of inadequate management of acute diarrhea.
Intractable diarrhea of infancy is a syndrome that occurs in the first few months of life, persists for longer than 2 weeks with no recognized pathogens, and is refractory to treatment. The most common cause is acute infectious diarrhea that was not managed adequately.
Chronic nonspecific diarrhea (CNSD), also known as irritable colon of childhood and toddlers’ diarrhea, is a common cause of chronic diarrhea in children 6 to 54 months of age. These children have loose stools, often with undigested food particles, and diarrhea greater than 2 weeks’ duration. Children with CNSD grow normally and have no evidence of malnutrition, no blood in their stool, and no enteric infection. Research has linked poor dietary habits and food sensitivities to chronic diarrhea. The excessive intake of juices and artificial sweeteners such as sorbitol, a substance found in many commercially prepared beverages and foods, may be a factor. Box 29-3 lists other factors that predispose patients to chronic diarrhea.
Etiology
Most pathogens that cause diarrhea are spread by the fecal-oral route through contaminated food or water or are spread from person to person where there is close contact (e.g., daycare centers). Lack of clean water, crowding, poor hygiene, nutritional deficiency, and poor sanitation are major risk factors, especially for bacterial or parasitic pathogens. Infants are often more susceptible to frequent and severe bouts of diarrhea because their immune system has not been exposed to many pathogens and has not acquired protective antibodies (Box 29-4). Worldwide, the most common causes of acute gastroenteritis are infectious agents, viruses, bacteria, and parasites. In developed nations, viruses, primarily rotavirus, cause 70% to 80% of infectious diarrhea.
Rotavirus is the most important cause of serious gastroenteritis among children and a significant nosocomial (hospital-acquired) pathogen, accounting for 55,000 to 70,000 hospitalizations annually (Committee on Infectious Diseases, 2007; Centers for Disease Control and Prevention, 2008; Staat, 2006). Rotavirus disease is most severe in children 3 to 24 months of age. Children younger than 3 months of age have some protection from the disease because of maternally acquired antibodies. Approximately 25% of severe cases of rotavirus occur in older children (Coffin, 2001).
Salmonella, Shigella, and Campylobacter organisms are the most frequently isolated bacterial pathogens. Salmonella infection has the highest occurrence in infants; Giardia and Shigella infections have the highest incidence among toddlers. Shigella infection is uncommon in the United States, accounting for less than 5% of diarrheal illnesses in infants and toddlers. Campylobacter infection has a bimodal presentation (highest in children less than 12 months of age with a second rise in incidence at ages 15 to 19 years). Giardia and Cryptosporidium organisms are parasites. Giardia infection represents 15% of nondysenteric illness in the United States; Cryptosporidium infection is often associated with outbreaks in young children in daycare centers. Plesiomonas and Yersinia are also parasites that are frequently responsible for causing diarrhea that lasts more than 10 days in a previously healthy adolescent. (See also Intestinal Parasitic Diseases, Chapter 16.)
Antibiotic administration is frequently associated with diarrhea because antibiotics alter the normal intestinal flora, resulting in an overgrowth of other bacteria such as Clostridium difficile. Antibiotic-associated diarrhea can also be caused by Salmonella organisms, Clostridium porringers type A, and Staphylococcus aureus pathogens (Jabbar and Wright, 2003).
Pathophysiology
Invasion of the GI tract by pathogens results in increased intestinal secretion as a result of enterotoxins, cytotoxic mediators, or decreased intestinal absorption secondary to intestinal damage or inflammation. Enteric pathogens attach to the mucosal cells and form a cuplike pedestal on which the bacteria rest. The pathogenesis of the diarrhea depends on whether the organism remains attached to the cell surface, resulting in a secretory toxin (noninvasive, toxin-producing, noninflammatory type diarrhea), or penetrates the mucosa (systemic diarrhea). Noninflammatory diarrhea is the most common diarrheal illness, resulting from the action of enterotoxin that is released after attachment to the mucosa. The most serious and immediate physiologic disturbances associated with severe diarrheal disease are (1) dehydration, (2) acid-base imbalance with acidosis, and (3) shock that occurs when dehydration progresses to the point that circulatory status is seriously impaired.
Diagnostic Evaluation
![]() Evaluation of the child with acute gastroenteritis begins with a careful history that seeks to discover the possible cause of diarrhea, to assess the severity of symptoms and the risk of complications, and to elicit information about current symptoms indicating other treatable illnesses that could be causing the diarrhea. The history should include questions about recent travel, exposure to untreated drinking or washing water sources, contact with animals or birds, daycare center attendance, recent treatment with antibiotics, or recent diet changes. History questions should also explore the presence of other symptoms such as fever and vomiting, frequency and character of stools (e.g., watery, bloody), urinary output, dietary habits, and recent food intake.
Evaluation of the child with acute gastroenteritis begins with a careful history that seeks to discover the possible cause of diarrhea, to assess the severity of symptoms and the risk of complications, and to elicit information about current symptoms indicating other treatable illnesses that could be causing the diarrhea. The history should include questions about recent travel, exposure to untreated drinking or washing water sources, contact with animals or birds, daycare center attendance, recent treatment with antibiotics, or recent diet changes. History questions should also explore the presence of other symptoms such as fever and vomiting, frequency and character of stools (e.g., watery, bloody), urinary output, dietary habits, and recent food intake.
![]() Case Study—Dehydration and Diarrhea
Case Study—Dehydration and Diarrhea
Extensive laboratory evaluation is not indicated in children who have uncomplicated diarrhea and no evidence of dehydration, since most diarrheal illnesses are self-limiting. Laboratory tests are indicated for children who are severely dehydrated and receiving intravenous (IV) therapy. Watery, explosive stools suggest glucose intolerance; foul-smelling, greasy, bulky stools suggest fat malabsorption. Diarrhea that develops after the introduction of cow’s milk, fruits, or cereal may be related to enzyme deficiency or protein intolerance. Neutrophils or red blood cells in the stool indicate bacterial gastroenteritis or IBD. The presence of eosinophils suggests protein intolerance or parasitic infection. Perform stool cultures only when blood, mucus, or polymorphonuclear leukocytes are present in the stool, when symptoms are severe, when there is a history of travel to a developing country, and when a specific pathogen is suspected. Gross blood or occult blood may indicate pathogens such as Shigella, Campylobacter, or hemorrhagic Escherichia coli strains. Providers may use an enzyme-linked immunosorbent assay (ELISA) to confirm the presence of rotavirus or Giardia organisms. If there is a history of recent antibiotic use, test the stool for C. difficile toxin. When bacterial and viral cultures are negative and when diarrhea persists for more than a few days, examine stools for ova and parasites. A stool specimen with a pH of less than 6 and the presence of reducing substances may indicate carbohydrate malabsorption or secondary lactase deficiency. Stool electrolyte measurements may help identify children with secretory diarrhea.
Determine urine specific gravity if dehydration is suspected. Obtain a complete blood count, serum electrolytes, creatinine, and blood urea nitrogen (BUN) in the child who requires hospitalization. The hemoglobin, hematocrit, creatinine, and BUN levels are usually elevated in acute diarrhea and should normalize with rehydration.
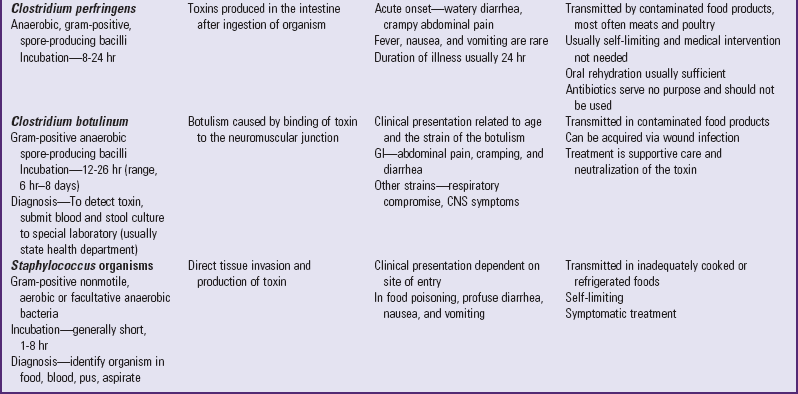
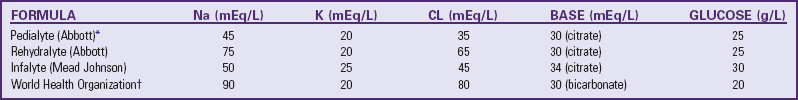
Therapeutic Management
The major goals in the management of acute diarrhea include (1) assessment of fluid and electrolyte imbalance, (2) rehydration, (3) maintenance fluid therapy, and (4) reintroduction of an adequate diet. Treat infants and children with acute diarrhea and dehydration first with oral rehydration therapy (ORT). ORT is one of the major worldwide health care advances. It is more effective, safer, less painful, and less costly than IV rehydration. The American Academy of Pediatrics, World Health Organization, and Centers for Disease Control and Prevention all recommend ORT as the treatment of choice for most cases of dehydration caused by diarrhea (Centers for Disease Control and Prevention, 2003) (Box 29-5). Oral rehydration solutions (ORSs) enhance and promote the reabsorption of sodium and water. These solutions greatly reduce vomiting, volume loss from diarrhea, and the duration of the illness. ORSs, including reduced osmolarity ORS, are available in the United States as commercially prepared solutions and are successful in treating the majority of infants with dehydration (Table 29-2). Guidelines for rehydration recommended by the American Academy of Pediatrics are given in Table 29-3.
TABLE 29-2
COMPOSITION OF SOME ORAL REHYDRATION SOLUTIONS
Cl, Chloride; K, potassium; Na, sodium.
*Note that many generic products are available with compositions identical to Pedialyte.
TABLE 29-3
ORS, Oral rehydration solution.
*If no signs of dehydration are present, rehydration therapy is not necessary. Proceed with maintenance therapy and replacement of stool losses.
After rehydration, ORS may be used during maintenance fluid therapy by alternating the solution with a low-sodium fluid such as water, breast milk, lactose-free formula, or half-strength lactose-containing formula. In older children ORS can be given and a regular diet continued. Ongoing stool losses should be replaced on a 1 : 1 basis with ORS. If the stool volume is not known, approximately 10 ml/kg (4 to 8 oz) of ORS should be given for each diarrheal stool.
Solutions for oral hydration are useful in most cases of dehydration, and vomiting is not a contraindication. Give a child who is vomiting an ORS at frequent intervals and in small amounts. For young children the caregiver may give the fluid with a spoon or small syringe in 5- to 10-ml increments every 1 to 5 minutes. An ORS may also be given via nasogastric or gastrostomy tube infusion. Infants without clinical signs of dehydration do not need ORT. They should, however, receive the same fluids recommended for infants with signs of dehydration in the maintenance phase and for ongoing stool losses. The use of probiotics reduces the risk of antibiotic-associated diarrhea in children by 56% (Szajewska, Ruszcynski, and Radzikowski, 2006).
Early reintroduction of nutrients is desirable and is gaining more widespread acceptance. Continued feeding or early reintroduction of a normal diet has no adverse effects and actually lessens the severity and duration of the illness and improves weight gain when compared with the gradual reintroduction of foods (Zangwill, 2006). Infants who are breast-feeding should continue to do so, and ORS should be used to replace ongoing losses in these infants. Formula-fed infants should resume their formula; if it is not tolerated, a lactose-free formula may be used for a few days. In older children a regular diet, including milk, can generally be offered after rehydration has been achieved. In toddlers there is no contraindication to continuing soft or pureed foods. A diet of easily digestible foods such as cereals, cooked vegetables, and meats is adequate for the older child.
In cases of severe dehydration and shock, IV fluids are initiated whenever the child is unable to ingest sufficient amounts of fluid and electrolytes to (1) meet ongoing daily physiologic losses, (2) replace previous deficits, and (3) replace ongoing abnormal losses. Patients who usually require IV fluids are those with severe dehydration, those with uncontrollable vomiting, those who are unable to drink for any reason (e.g., extreme fatigue, coma), and those with severe gastric distention.
Select the IV solution on the basis of what is known regarding the probable type and cause of the dehydration. The type of fluid normally used is a saline solution containing 5% dextrose in water. Sodium bicarbonate may be added, since acidosis is usually associated with severe dehydration. Although the initial phase of fluid replacement is rapid in both isotonic and hypotonic dehydration, rapid replacement is contraindicated in hypertonic dehydration because of the risk of water intoxication, especially in the brain cells.
After the severe effects of dehydration are under control, begin specific diagnostic and therapeutic measures to detect and treat the cause of the diarrhea. Because of the self-limiting nature of vomiting and its tendency to improve when dehydration is corrected, the use of antiemetic agents is not recommended. The use of antibiotic therapy in children with acute gastroenteritis is controversial. Antibiotics may shorten the course of some diarrheal illnesses (e.g., those caused by Shigella organisms). However, most bacterial diarrheas are self-limiting, and the diarrhea often resolves before the causative organism can be determined. Antibiotics may prolong the carrier period for bacteria such as Salmonella. Antibiotics may be considered, however, in patients with immunosuppression, severe symptoms, or persistent disease or in patients who have had transplantation (Jabbar and Wright, 2003). (See Intestinal Parasitic Diseases, Chapter 16.)
Nursing Care Management
![]() The management of most cases of acute diarrhea takes place in the home with education of the caregiver. Teach caregivers to monitor for signs of dehydration (especially the number of wet diapers or voidings) and the amount of fluids taken by mouth, and to assess the frequency and amount of stool losses (see Nursing Care Plan). Education relating to ORT, including the administration of maintenance fluids and replacement of ongoing losses, is important (see Critical Thinking Exercise). ORS should be administered in small quantities at frequent intervals. Vomiting is not a contraindication to ORT unless it is severe. Information concerning the introduction of a normal diet is essential. Parents need to know that a slightly higher stool output initially occurs with continuation of a normal diet and with ongoing replacement of stool losses. The benefits of a better nutritional outcome with fewer complications and a shorter duration of illness outweigh the potential increase in stool frequency. Address parents’ concerns to ensure adherence to the treatment plan.
The management of most cases of acute diarrhea takes place in the home with education of the caregiver. Teach caregivers to monitor for signs of dehydration (especially the number of wet diapers or voidings) and the amount of fluids taken by mouth, and to assess the frequency and amount of stool losses (see Nursing Care Plan). Education relating to ORT, including the administration of maintenance fluids and replacement of ongoing losses, is important (see Critical Thinking Exercise). ORS should be administered in small quantities at frequent intervals. Vomiting is not a contraindication to ORT unless it is severe. Information concerning the introduction of a normal diet is essential. Parents need to know that a slightly higher stool output initially occurs with continuation of a normal diet and with ongoing replacement of stool losses. The benefits of a better nutritional outcome with fewer complications and a shorter duration of illness outweigh the potential increase in stool frequency. Address parents’ concerns to ensure adherence to the treatment plan.
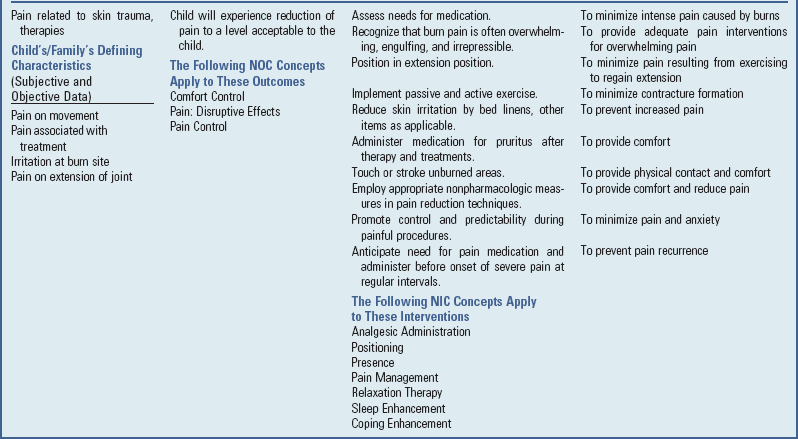
![]() Nursing Care Plan—The Child with Acute Diarrhea
Nursing Care Plan—The Child with Acute Diarrhea
If the child with acute diarrhea and dehydration is hospitalized, the nurse must obtain an accurate weight and carefully monitor intake and output. The child may be placed on parenteral fluid therapy with nothing by mouth for 12 to 48 hours. Monitoring the IV infusion is an important nursing function. The nurse must ensure that the correct fluid and electrolyte concentration is infused, that the flow rate is adjusted to deliver the desired volume in a given time, and that the IV site is maintained.
Accurate measurement of output is essential to determine whether renal blood flow is sufficient to permit the addition of potassium to the IV fluids. The nurse is responsible for examination of stools and collection of specimens for laboratory examination. (See Collection of Specimens, Chapter 27.) Take care when obtaining and transporting stools to prevent possible spread of infection. Use a clean tongue depressor to obtain specimens for laboratory examination or as an applicator for transfer to a culture medium. Transport stool specimens to the laboratory in appropriate containers and media according to hospital policy.
Diarrheal stools are highly irritating to the skin, and extra care is necessary to protect the skin of the diaper region from excoriation. (See Diaper Dermatitis, Chapter 13.) Avoid taking temperatures rectally because they stimulate the bowel, increasing passage of stool.
Support for the child and family involves the same care and consideration given all hospitalized children. (See Chapter 26.) Keep parents informed of the child’s progress and instruct them in the use of frequent and proper hand washing and the disposal of soiled diapers, clothes, and bed linen. Everyone caring for the child must be aware of “clean” areas and “dirty” areas, especially in the hospital, where the sink in the child’s room is used for many purposes. Discard soiled diapers and linen in receptacles close to the bedside. To remind caregivers to keep diapers and other soiled articles away from clean areas, place signs identifying “clean” (e.g., bed table) and “dirty” (e.g., sink, bathroom) areas. List the articles that may be stored in each area on these signs.
Prevention: The best intervention for diarrhea is prevention. The fecal-oral route spreads most infections, and parents need information about preventive measures such as personal hygiene, protection of the water supply from contamination, and careful food preparation.
Meticulous attention to perianal hygiene, disposal of soiled diapers, proper hand washing, and isolation of infected persons also minimizes the transmission of infection. (See Infection Control, Chapter 27.)
Parents need information about preventing diarrhea while traveling. Caution them against giving their children adult medications that are used to prevent traveler’s diarrhea. Until vaccines or other prophylactic measures are safe for children, the best measure during travel to areas where water may be contaminated is to allow children to drink only bottled water and carbonated beverages (from the container through a straw supplied from home). Children should also avoid tap water, ice, unpasteurized dairy products, raw vegetables, unpeeled fruits, meats, and seafood.
Vomiting
Vomiting is the forceful ejection of gastric contents through the mouth. It is a well-defined, complex, coordinated process that is under central nervous system control and is usually accompanied by nausea and retching. In contrast, regurgitation is a simpler, more passive, and effortless phenomenon. Vomiting has many causes, including acute infectious diseases, increased intracranial pressure (ICP), toxic ingestions, food intolerances and allergies, mechanical obstruction of the GI tract, metabolic disorders, and psychogenic problems (Acker, 2002). Vomiting is common in childhood, is usually self-limiting, and requires no specific treatment. However, complications can occur in children, including dehydration and electrolyte disturbances, malnutrition, aspiration, and Mallory-Weiss syndrome (small tears in the distal esophageal mucosa).
Etiology
The child’s age, pattern of vomiting, and duration of symptoms help determine the cause. For example, chronic and intermittent episodes of vomiting may indicate malrotation, whereas vomiting on a specific day at the same time before school is not likely to be a result of organic disease. The color and consistency of the emesis vary according to the cause. Green, bilious vomiting suggests bowel obstruction. Curdled stomach contents, mucus, or fatty foods that are vomited several hours after ingestion suggest poor gastric emptying or high intestinal obstruction. Gastric irritation by certain medicines, foods, or toxic substances may cause vomiting.
Associated symptoms also help identify the cause. Fever and diarrhea accompanying vomiting suggest an infection. Constipation associated with vomiting suggests an anatomic or functional obstruction. Localized abdominal pain and vomiting often occur with appendicitis, pancreatitis, or peptic ulcer disease. A change in the level of consciousness or a headache associated with vomiting indicates a central nervous system or metabolic disorder. Forceful vomiting is associated with pyloric stenosis.
Pathophysiology
The act of vomiting, including nausea and retching, is under control of the central nervous system. Two areas of the medulla are involved as the vomiting center. The medullary center is also activated by impulses from a second center, the chemoreceptor trigger zone, which is located in the floor of the fourth ventricle (Box 29-6). Nausea is a sensation that may be induced by visceral, labyrinthine (inner ear), or emotional stimuli. It is characterized by the desire to vomit, with discomfort felt in the throat or abdomen. Nausea is often associated with autonomic symptoms such as salivation, pallor, sweating, and tachycardia. Retching may occur with or without vomiting. Retching involves a series of spasmodic movements during inspiration, creating a negative intrathoracic pressure, and contraction of the abdominal muscles. Projectile vomiting is preceded and accompanied by vigorous peristaltic waves.
Vomiting is a well-recognized response to psychologic stress. During stress, adrenaline levels rise and may stimulate the chemoreceptor trigger zone. Nausea and vomiting are likely a protective mechanism to remove toxins from the system. Vomiting may follow GI infection or toxic ingestion, or it can be a learned behavioral response.
Cyclic vomiting syndrome is a rare disorder characterized by bouts of vomiting that can last from hours to several days (McRonald and Fleisher, 2005). The cause of this syndrome is unknown (Bullard and Page, 2005).
Diagnostic Evaluation
The diagnostic evaluation includes a thorough history and physical examination. The description of the vomitus; relationship to meals or specific foods; behavior; and presence of pain, constipation, diarrhea, or jaundice are important components of the history. Physical examination should include an assessment of the hydration status and an abdominal examination.
Further evaluation may include analysis of urine for protein or blood, serum electrolytes, and radiographic studies. A plain radiograph of the chest or abdomen or ultrasonography may reveal anatomic abnormalities. Brain scans are used to detect tumors. Endoscopy of the upper GI tract may be a valuable diagnostic procedure if the provider suspects esophagitis. A psychiatric evaluation may be indicated if cyclic vomiting, anorexia nervosa, bulimia, or self-poisoning is present. Self-induced vomiting and rumination may be a self-stimulation or gratification activity.
Therapeutic Management
Direct the management of vomiting toward detection and treatment of the cause of the vomiting and prevention of complications such as dehydration and malnutrition. Vomiting is often a symptom of a common infectious illness that is self-limiting and resolves with no specific treatment. Further investigation is indicated if there is dehydration, progressively severe vomiting, or persistent vomiting for more than 24 hours, or if the history and physical examination fail to suggest a diagnosis. If vomiting leads to dehydration, oral rehydration or parenteral fluids may be required.
Antiemetic drugs may be indicated when the vomiting can be anticipated, is of limited duration, and has a known cause. Limited adverse effects are rare with antiemetic use for vomiting in children (Li, DiGiuseppe, and Christakis, 2003). Antiemetic drugs may block the receptors in the chemoreceptor trigger zone (ondansetron [Zofran] or trimethobenzamide [Tigan]), enhance gastroduodenal peristalsis (metoclopramide [Reglan]), or compete for H1-receptor sites (promethazine [Phenergan]). For children who are prone to motion sickness, it is often helpful to administer an appropriate dose of dimenhydrinate (Dramamine) before a trip (see Evidence-Based Practice box).
Nursing Care Management
The major emphasis of nursing care of the vomiting infant or child is on observation and reporting of vomiting behavior and associated symptoms and on the implementation of measures to reduce the vomiting. Accurate assessment of the type of vomiting, appearance of the vomitus, and the child’s behavior in association with the vomiting greatly aids in establishing a diagnosis of disorders that have vomiting as a clinical feature.
The cause of the vomiting determines the nursing intervention. When the vomiting is a manifestation of improper feeding methods, establishing proper techniques through teaching and example ordinarily corrects the situation. If the vomiting is a probable sign of GI obstruction, the nurse usually withholds food or implements special feeding techniques. When vomiting is related to concurrent infection, dietary indiscretion, or emotional factors, direct efforts toward maintaining hydration or preventing dehydration.
The thirst mechanism is the most sensitive guide to fluid needs, and ad libitum administration of a glucose-electrolyte solution to an alert child restores water and electrolytes satisfactorily. It is important to include carbohydrates to spare body protein and to avoid ketosis resulting from exhaustion of glycogen stores. Small, frequent feedings of fluids or foods are preferable and more effective. Once vomiting has abated, offer more liberal amounts of fluids, followed by gradual resumption of the regular diet.
Position the infant or child who is vomiting to prevent aspiration and observe him or her for evidence of dehydration. It is important to emphasize the need for the child to brush the teeth or rinse the mouth after vomiting to dilute the hydrochloric acid that comes in contact with the teeth. Carefully monitor fluid and electrolyte status to avoid the possibility of electrolyte imbalance.
Shock States
![]() Shock, or circulatory failure, is a complex clinical syndrome characterized by tissue perfusion that is inadequate to meet the metabolic demands of the body, which results in cellular dysfunction and eventual organ failure. Although the causes are different, the physiologic consequences are the same: hypotension, tissue hypoxia, and metabolic acidosis.
Shock, or circulatory failure, is a complex clinical syndrome characterized by tissue perfusion that is inadequate to meet the metabolic demands of the body, which results in cellular dysfunction and eventual organ failure. Although the causes are different, the physiologic consequences are the same: hypotension, tissue hypoxia, and metabolic acidosis.
![]() Critical Thinking Exercise—Shock
Critical Thinking Exercise—Shock
Etiology
The most common type of circulatory failure in children is hypovolemic shock, which follows a reduction in circulating blood volume related to blood loss (e.g., trauma, major bleeding), plasma losses (e.g., burns, peritonitis), or extracellular fluid losses (e.g., diarrhea, dehydration) beyond the child’s physiologic ability to compensate. Cardiogenic shock results from impaired cardiac muscle function that leads to decreased cardiac output. It is uncommon in children but may be seen after cardiac surgery and in children with acute dysrhythmias, congestive heart failure, or cardiomyopathy. Distributive shock, or vasogenic shock, results from a vascular abnormality that produces maldistribution of blood supply throughout the body. This term includes (1) neurogenic shock, characterized by massive vasodilation resulting from the loss of sympathetic nervous system tone, which can occur with spinal cord injuries; (2) anaphylactic shock, which is characterized by a hypersensitivity reaction that causes massive vasodilation and capillary leak and may occur with drug or latex allergy, insect stings, or blood transfusion; and (3) septic shock, characterized by a decreased cardiac output and derangements in the peripheral circulation in response to a severe, overwhelming infection. Obstructive shock may resemble hypovolemic shock but is caused by cardiac tamponade, tension pneumothorax, ductal-dependent congenital heart lesions, or massive pulmonary embolism. The types of shock are described in Box 29-7 (Ralston, Hazinski, Zaritsky, et al, 2006).
Pathophysiology
The circulatory system of the healthy child is able to transport oxygen and nutrients to meet the essential needs of body tissues and can respond to increased demands resulting from an elevated metabolic rate. The cardiac output and distribution to the various body tissues can change rapidly in response to intrinsic (myocardial and intravascular) or extrinsic (neuronal) control mechanisms. In shock states these mechanisms are altered or challenged.
Reduced blood flow, as in hypovolemic shock, causes diminished venous return to the heart, low central venous pressure (CVP), low cardiac output, and hypotension. The reduced intravascular volume triggers a chain of compensatory mechanisms. Fluid is mobilized from the extracellular compartment. Vasomotor centers in the medulla are signaled, causing depressed vagal activity and increased sympathetic activity, which increase the force and rate of cardiac contraction and constrict the arterioles and veins, thereby increasing peripheral vascular resistance.
Simultaneously the lowered blood volume also leads to the release of large amounts of catecholamines, antidiuretic hormone, adrenocorticosteroids, and aldosterone in an effort to conserve body fluids. The catecholamines augment the vasomotor activity to produce vasoconstriction and reduce blood flow to the skin, kidneys, muscles, and splanchnic viscera in order to shunt the available blood to the brain and heart. Consequently, the skin feels cold and clammy, there is poor capillary filling, and glomerular filtration and urinary output are significantly reduced.
Impaired perfusion to the peripheral tissues also produces metabolic alterations. Oxygen depletion causes the cells to revert to anaerobic glycolytic metabolism, forming pyruvic acid; pyruvic acid is then converted to lactic acid, producing lactic acidosis. The acidosis places an extra burden on the lungs as they attempt to compensate for the metabolic acidosis by increasing the respiratory rate. Impaired cellular uptake and metabolism of glucose create an early, transient hyperglycemia. When plasma fluid is lost, hemoconcentration and diminished blood flow increase the viscosity of the blood and further impair perfusion.
Prolonged vasoconstriction results in fatigue, and the release of vasodilator substances such as histamine leads to vasodilation. Venules, which are less sensitive to vasodilator substances, remain constricted for a time. This causes massive pooling in the capillary and venular beds and transudation of plasma fluid into the tissues, which further depletes blood volume.
Complications of shock create further hazards. Central nervous system hypoperfusion may eventually lead to cerebral edema, cortical infarction, or intraventricular hemorrhage. Renal hypoperfusion causes renal ischemia with possible tubular or glomerular necrosis and renal vein thrombosis. Reduced blood flow to the lungs can interfere with surfactant secretion and result in shock lung or acute respiratory distress syndrome (ARDS). ARDS is characterized by sudden pulmonary congestion and atelectasis with formation of a hyaline membrane. (See Chapter 32.) GI tract bleeding and perforation are always a possibility following splanchnic ischemia and necrosis of intestinal mucosa. Metabolic complications of shock may include hypoglycemia, hypocalcemia, and other electrolyte disturbances.
Shock syndromes characterized by vascular abnormalities (distributive shock) have a somewhat different pathophysiologic pattern of hemodynamic collapse. In neurogenic shock, the sympathetic nervous system mechanisms that maintain vascular tone are interrupted, causing reduced vascular resistance and peripheral pooling of blood; with this increased vascular capacity there is loss of effective circulating blood volume. Septic shock produces a hyperdynamic state in which there is often an elevated plasma volume and reduced peripheral resistance that lead to widespread vasodilation. In many cases there is a high cardiac output caused by the vasodilation in infected tissues and elsewhere, plus a high metabolic rate resulting from the elevated body temperature. Degenerating tissues cause aggregation of red blood cells and sludging of the blood. Development of disseminated intravascular coagulation, triggered by either the degenerating tissue or bacterial toxins, consumes the clotting factors and produces widespread hemorrhages. (See Chapter 35.)
Clinical Manifestations
Shock can be regarded as a form of compensation for circulatory failure and, because of its progressive nature, can be divided into three stages or phases: compensated, decompensated, and irreversible. At all stages the principal differentiating signs are the (1) degree of tachycardia and perfusion to extremities, (2) level of consciousness, and (3) blood pressure (BP). Additional signs or modifications of these more universal signs may be present depending on the type and cause of the shock.
Compensated Shock: When vital organ function is maintained by intrinsic mechanisms and the child’s ability to compensate is effective, cardiac output and systemic arterial BP are usually normal or increased. However, blood flow is generally uneven or maldistributed in the microcirculation. Early clinical signs are subtle and include apprehension, irritability, normal BP, narrowing pulse pressure, thirst, pallor, and diminished urinary output.
Decompensated Shock: As shock progresses, perfusion in the microcirculation becomes marginal despite compensatory adjustments, and the signs are more obvious and indicate early decompensation. These signs are tachypnea; moderate metabolic acidosis; oliguria; and cool, pale extremities with decreased skin turgor and poor capillary filling. The outcomes of circulatory failure that progress beyond the limits of compensation are tissue hypoxia, metabolic acidosis, and eventual dysfunction of all organ systems.
Irreversible Shock: Irreversible, or terminal, shock implies damage to vital organs (e.g., the heart or brain) of such magnitude that the entire system is disrupted regardless of therapeutic intervention. There is pronounced systemic vasoconstriction and hypoxia of visceral and cutaneous circulations with hypotension, acidosis, lethargy or coma, and oliguria or anuria. The child is totally obtunded. A thready and weak pulse, hypotension, periodic breathing or apnea, anuria, and stupor or coma are signs of impending cardiopulmonary arrest. Death occurs even if cardiovascular measurements return to normal levels with therapy.
Diagnostic Evaluation
The nurse can discern the cause of shock from the history and physical examination. The extent of the shock is determined by measurement of vital signs, including CVP and capillary filling. Laboratory tests that assist in assessment are blood gas measurements, pH, and sometimes liver function tests. Coagulation status (prothrombin time, partial thromboplastin time, platelet count, fibrinogen, fibrin) is evaluated when there is evidence of bleeding, such as oozing from a venipuncture site, bleeding from any orifice, petechiae, or purpura. Cultures of blood and other sites are indicated when there is a high suspicion of sepsis. Perform renal function tests when impaired renal function is evident.
Therapeutic Management
![]() Treatment of shock consists of three major thrusts: (1) ventilation, (2) fluid administration, and (3) improvement of the pumping action of the heart (vasopressor support). The first priority is to establish an airway and administer oxygen. Once the airway is ensured, circulatory stabilization is the major concern. Placement of one or more multilumen central lines, preferably above the diaphragm (to deliver drugs closer to the heart and limit tissue injury from caustic medications), is a priority in shock (Jindal, Hollenberg, and Dellinger, 2000). These lines are needed for rapid volume replacement, administration of vasoactive drugs, and hemodynamic monitoring. An alternative is rapid surgical cutdown cannulation of the saphenous vein. The vein is anatomically accessible, can accommodate the volumes of fluid needed, and is situated where it does not interfere with any necessary resuscitation procedures. Another effective emergency method is intraosseous administration of fluids. (See Chapter 28.)
Treatment of shock consists of three major thrusts: (1) ventilation, (2) fluid administration, and (3) improvement of the pumping action of the heart (vasopressor support). The first priority is to establish an airway and administer oxygen. Once the airway is ensured, circulatory stabilization is the major concern. Placement of one or more multilumen central lines, preferably above the diaphragm (to deliver drugs closer to the heart and limit tissue injury from caustic medications), is a priority in shock (Jindal, Hollenberg, and Dellinger, 2000). These lines are needed for rapid volume replacement, administration of vasoactive drugs, and hemodynamic monitoring. An alternative is rapid surgical cutdown cannulation of the saphenous vein. The vein is anatomically accessible, can accommodate the volumes of fluid needed, and is situated where it does not interfere with any necessary resuscitation procedures. Another effective emergency method is intraosseous administration of fluids. (See Chapter 28.)
![]() Nursing Care Plan—The Child in Shock (Cardiovascular Failure)
Nursing Care Plan—The Child in Shock (Cardiovascular Failure)
Ventilatory Support: The lung is the organ most sensitive to shock. The decrease in or redistribution of blood flow to respiratory muscles plus the increased work of breathing can rapidly lead to respiratory failure. Critically ill patients are unable to maintain an adequate airway. To place the lung at rest and improve ventilation, endotracheal intubation is initiated early with positive-pressure ventilation and supplemental oxygen. Blood gases, oxygen saturation (using pulse oximetry), and pH are monitored frequently.
Increased extravascular lung water caused by edema—both hydrostatic and permeable—contributes to the development of respiratory complications. Hydrostatic edema occurs from the elevation of pulmonary microvascular pressure as a result of left ventricular dysfunction; permeable edema occurs when damage to alveolar cell and pulmonary capillary epithelium causes fluid to leak into the interstitial space, resulting in ARDS. (See Chapter 32.) Direct therapy toward maintaining normal arterial blood gas measurements, normal acid-base balance, and circulation. Make efforts to remove fluid and prevent its accumulation by increasing oncotic pressure and decreasing microvascular hydrostatic pressure. Promote elevated oncotic pressure by diuresis with furosemide or mannitol, colloid administration, or both.
Cardiac Support: In many cases rapid restoration of blood volume is the main therapy needed in the resuscitation of the child in shock. An isotonic crystalloid solution (normal saline or lactated Ringer’s solution) is usually the first choice for fluid replacement. Crystalloid is given in IV boluses of 10 to 20 ml/kg over 10 to 15 minutes and repeated as necessary. The child’s response is assessed after each bolus. An increase in BP and a decrease in heart rate indicate successful resuscitation. An increased cardiac output results in improved capillary circulation and skin color. Colloids (protein-containing fluids) are often administered to children in shock; albumin is the most common. Because albumin is a protein solution, it remains in the vascular space much longer than crystalloid fluids. A smaller volume of albumin can be given to increase intravascular volume and support cardiac output; with crystalloid fluids, a larger volume is needed to achieve the same effect. In general, because of the infectious risks, blood is administered only in situations of known blood loss, active bleeding, or markedly decreased hematocrit. Fresh-frozen plasma is used to correct coagulopathies, not as volume replacement.
For the critically ill child with shock and multisystem organ dysfunction, more aggressive monitoring is necessary. Central venous measurements of right atrial pressure or pulmonary wedge pressure help guide fluid therapy. In children with persistent shock, place a Swan-Ganz catheter for more accurate monitoring. Determination of arterial blood gases, hematocrit, serum electrolytes, glucose, and calcium concentrations provides additional information concerning composition of circulating blood. Correction of acidosis, hypoxemia, and any metabolic derangements is mandatory.
Vasopressor Support: Temporary pharmacologic support may be required to enhance myocardial contractility, reverse metabolic or respiratory acidosis, and maintain arterial pressure. The principal agents used to improve cardiac output and circulation are the exogenous catecholamines, administered by constant infusion pump. Dopamine is the preferred drug in most situations because it also improves renal perfusion. Other agents (e.g., dobutamine, isoproterenol, epinephrine) may be used to improve cardiac output, depending on the situation.
Metabolic acidosis is usually corrected with adequate tissue perfusion and improved renal function. This is accomplished with adequate ventilatory support, including oxygen, and restoration of blood volume and peripheral circulation. Sodium bicarbonate may also be administered to correct acidosis resulting from shock. It should be given in small boluses that are diluted to avoid acute changes in osmolality. The major complications of bicarbonate administration are sodium overload and hyperosmolality.
Calcium chloride may be administered to improve cardiac function and to offset the reduced ionized calcium associated with large amounts of albumin, whole blood, or fresh-frozen plasma. Diuretics, such as furosemide (Lasix), cause a reduction in ventricular filling pressures without changing cardiac output or heart rate and promote sodium and water excretion by the kidney in cases in which pulmonary congestion is a problem.
Other Therapies: Peritoneal dialysis may be necessary if hyperkalemia, acidosis, hypervolemia, or altered mental status occurs. Nutritional support is provided by both enteral and parenteral routes. Prevention of infection is a primary concern because host resistance is depressed in patients in shock. Other complicating disorders, such as disseminated intravascular coagulation and GI problems (e.g., paralytic ileus, stress ulceration), are managed appropriately. The intraaortic balloon pump may be used for a child with low cardiac output who is refractory to conventional medical management. Extracorporeal membrane oxygenation, where available, is used occasionally as a last resort.
Nursing Care Management
The child in shock requires observation and care, preferably in an intensive care environment. The initial action in caring for the child in shock is ensuring adequate tissue oxygenation (see Emergency Treatment box). The nurse should be prepared to administer oxygen by the appropriate route and to assist with any indicated intubation and ventilation procedures. Other procedures and activities that require immediate attention are establishing an IV line, estimating body weight (for calculating drug dosages), obtaining baseline vital signs, placing an indwelling urinary catheter, obtaining blood gas and other measurements, and administering medications as indicated.
The child is best positioned flat with the legs elevated. Hypotensive patients show no benefit from the traditional Trendelenburg position. Head-down positioning tends to increase ICP, decrease diaphragmatic excursion and lung volume, and decrease venous return to the heart because of the altered thoracic pressure. Elevating the lower extremities decreases pooling in the extremities, thereby returning blood supply to the heart.
The nurse’s responsibilities are to monitor vital signs (BP in particular); monitor intake and output; and perform a general assessment of the level of consciousness, circulatory perfusion, and parenteral infusion sites. The nurse titrates IV medications according to patient responses and obtains vital signs every 15 minutes during the critical periods and thereafter as needed. Measure urinary output hourly, and monitor blood gases, hematocrit, pH, and electrolytes frequently to assess the child’s status and the efficacy of therapy. Apnea and cardiac monitors are attached and monitored continuously. Oxygen saturation monitors provide continuous measurement of oxygenation. In the initial stages of acute shock, care of the child often requires more than one nurse because of all the activities that must be carried out simultaneously.
Family Support: Throughout the intense activity, do not overlook the parents. A member of the staff, such as a nurse, social worker, or clergy, may be called to provide comfort and support. If the family is not at the hospital, someone should contact them at frequent intervals to inform them about what is being done and whether there is any improvement. Ideally, someone should remain with the parents to serve as a liaison between them and the intensive care team. However, this is not always feasible in such a critical situation. As soon as possible, the parents should be allowed to see the child.
Septic Shock
Sepsis and septic shock are caused by an infectious organism (Maar, 2004). Normally an infection triggers an inflammatory response in a local area, which results in vasodilation, increased capillary permeability, and eventually elimination of the infectious agent. The widespread activation and systemic release of inflammatory mediators is called the systemic inflammatory response syndrome (SIRS) (Goldstein, Giroir, and Randolf, 2005). Box 29-8 provides the exact definitions for SIRS, infection, sepsis, and severe sepsis. SIRS can occur in response to both infectious and noninfectious (e.g., trauma, burns) causes. When caused by infection, it is called sepsis. Septic shock is sepsis with organ dysfunction and hypotension. Most of the physiologic effects of shock occur because the exaggerated immune response triggers more than 30 different mediators, which results in diffuse vasodilation, increased capillary permeability, and maldistribution of blood flow. This impairs oxygen and nutrient delivery to the cells, resulting in cellular dysfunction. If the process continues, multiple organ dysfunction occurs and may result in death. Table 29-4 includes the age-specific vital signs and laboratory values reflective of septic shock in children.
TABLE 29-4
AGE-SPECIFIC VITAL SIGNS AND LABORATORY VARIABLES IN SEPTIC SHOCK*
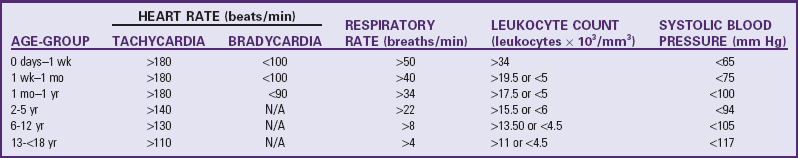
*Lower values for heart rate, leukocyte count, and systolic blood pressure are for 5th percentile, and upper values for heart rate, respiratory rate, or leukocyte count are for 95th percentile.
From Goldstein B, Giroir B, Randolph A: International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics, Pediatr Crit Care Med 6(1):2-8, 2005; used with permission.
The incidence of septic shock is increasing in adults and children (Arnal and Stein, 2003), possibly as a result of greater numbers of immunosuppressed patients, more widespread use of invasive devices in the seriously ill, increased awareness of the diagnosis, and a growing number of resistant microorganisms.
Three stages have been identified in septic shock. In early septic shock the patient has chills, fever, and vasodilation with increased cardiac output, which results in warm, flushed skin that reflects vascular tone abnormalities and hyperdynamic, warm, or hyperdynamic-compensated responses. BP and urinary output are normal. The patient has the best chance for survival in this stage. The second stage—the normodynamic, cool, or hyperdynamic-decompensated stage—lasts only a few hours. The skin is cool, but pulses and BP are still normal. Urinary output diminishes, and the mental state becomes depressed. With advancing disease, certain signs of circulatory decompensation that deteriorate to signs of circulatory collapse are indistinguishable from late shock of any cause. In the hypodynamic, or cold, stage of shock, cardiovascular function progressively deteriorates, even with aggressive therapy. The patient has hypothermia, cold extremities, weak pulses, hypotension, and oliguria or anuria. Patients are severely lethargic or comatose. Multiorgan failure is common. This is the most dangerous stage of shock.
Management of septic shock involves measures to provide hemodynamic stability and adequate oxygenation to the tissues and the use of antimicrobials to treat the infectious organism (Brierley, Choong, Cornell, et al, 2008; Dellinger, Levy, Carlet, et al, 2008). As with other forms of shock, hemodynamic stability is achieved with fluid volume resuscitation and inotropic agents as needed (Table 29-5). Providing adequate oxygenation often requires intubation and mechanical ventilation, supplemental oxygen, sedation, and paralysis to decrease the work of breathing. Septic shock involves activation of complement proteins that promote clumping of the granulocytes in the lung. The granulocytes can release chemicals that can cause direct lung injury to the pulmonary capillary endothelium. This causes a fluid leak into the alveoli, which causes stiff, noncompliant lungs. Disseminated intravascular coagulation and multiorgan dysfunction may also occur and require prompt assessment and management.
TABLE 29-5
PEDIATRIC SEPTIC SHOCK GOAL-DIRECTED THERAPY
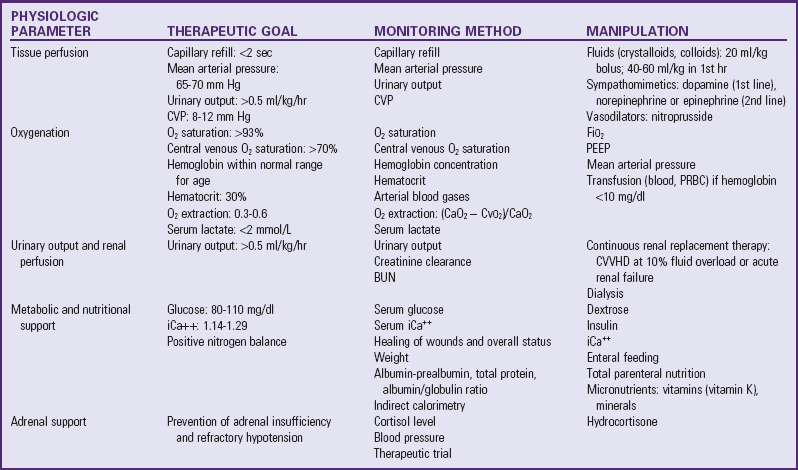
BUN, Blood urea nitrogen; CVP, central venous pressure; CVVHD, continuous venovenous hemofiltration/dialysis; iCa++, serum ionized calcium; PEEP, positive end-expiratory pressure; PRBC, packed red blood cells.
From Arnal LE, Stein F: Pediatric septic shock, Semin Pediatr Infect Dis 14(2):165-172, 2003; used with permission.
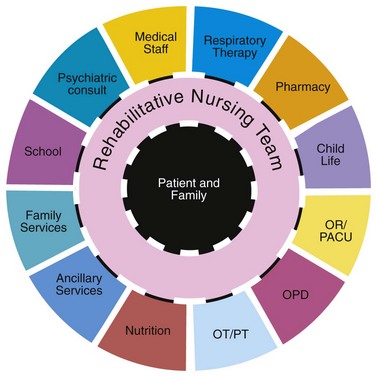
Nursing Care Management
Early identification of the symptoms of septic shock is critical to patient survival. A high index of suspicion is required in all critically ill patients who are at greater risk for sepsis because of multiple invasive lines and devices, poor nutrition, and impaired immune function. Subtle alterations in tissue perfusion and unexplained tachypnea and tachycardia often are early warning signs. Identification of the infectious agent and prompt treatment are also critical to patient survival. Patients should receive broad-spectrum antibiotics, and the nurse should remove the site of infection if possible (e.g., drain abscesses, remove indwelling lines). Manage patients in an intensive care unit, in which continuous monitoring and sophisticated cardiac and respiratory support are available. Multidisciplinary collaboration is essential in managing these critically ill patients.
Anaphylaxis
Anaphylaxis is the acute clinical syndrome resulting from the interaction of an allergen and a patient who is hypersensitive. This antigen-antibody (immunoglobulin E [IgE]) reaction stimulates the release of chemical substances, primarily histamine, from mast cells (Bohlke, Davis, DeStefano, et al, 2004). Histamine release causes vasodilation and increases capillary permeability, allowing fluid to leak into the interstitial space. Severe reactions are immediate; are often life threatening; and often involve multiple systems, primarily the cardiovascular, respiratory, GI, and integumentary systems. Exposure to the antigen can be through ingestion, inhalation, skin contact, or injection (Bohlke, Davis, DeStefano, et al, 2004). The most common allergens are listed in Box 29-9.
Prevention of a reaction is the primary goal. Preventing exposure is more easily accomplished in children known to be at risk, including those with (1) a history of a previous allergic reaction to a specific antigen, (2) a history of allergy (atopy), (3) a history of severe reactions in immediate family members, and (4) a reaction to a skin test (although skin tests are not available for all allergens).
Pathophysiology
An anaphylactic reaction occurs as a result of an interaction between an allergen and preexisting specific IgE. When the antigen enters the circulatory system, a generalized reaction rapidly occurs. Vasoactive amines (principally histamine or histamine-like substances) are released from mast cells and cause vasodilation, bronchoconstriction, and increased capillary permeability. Consequently, there is increased venous capacity and pooling, reduced arterial pressure, and rapid loss of fluid into interstitial spaces, causing a marked decrease in venous return to the heart.
Clinical Manifestations
The onset of clinical symptoms usually occurs within seconds or minutes of exposure to the antigen. The rapidity of the reaction is directly related to its intensity—the sooner the onset, the more severe the reaction. However, the onset may be delayed for as long as 2 hours. Typically the reaction is preceded by one or more prodromal signs and symptoms, including vague complaints of uneasiness or impending doom, restlessness, irritability, severe anxiety, headache, dizziness, paresthesia, and disorientation. The patient may lose consciousness. Cutaneous signs are the most common initial sign, and the child may complain of feeling warm. Angioedema is most noticeable in the eyelids, lips, tongue, hands, feet, and genitalia. As outlined in Box 29-10, any or all of several reactions may affect one or more organ systems.
Bronchiolar constriction often follows cutaneous manifestations. Bronchiolar constriction causes a narrowing of the airway, dilated pulmonary circulation produces pulmonary edema and hemorrhages, and there is often life-threatening laryngeal edema. Shock occurs as a result of mediator-induced vasodilation and sudden inadequacy of the circulation. Hypovolemia is further enhanced by increased capillary permeability and loss of intravascular fluid into the interstitial space. Laryngeal edema, with its acute upper airway obstruction and related hypovolemic shock, carries a more ominous prognosis.
Therapeutic Management
Successful outcome of anaphylactic reactions depends on rapid recognition of their severity and prompt treatment (Liberman and Teach, 2008). The goals of treatment are providing ventilation, restoring adequate circulation, and preventing further exposure by identifying and removing the cause when possible.
Observe the child for at least 6 hours because late deterioration may occur. Other routes of epinephrine administration are intramuscular and via an airway, either nebulized or by injection through an endotracheal tube. Strongly consider additional interventions such as fluid resuscitation, beta-agonists, antihistamines, and corticosteroids.
Position and monitor the child in the same way as for any shock patient. If this is the initial anaphylactic reaction, it is especially important to identify the allergen and implement measures to prevent any future reaction. The patient should carry medical identification at all times. Desensitization may be recommended in certain cases.
The nurse can manage a mild cutaneous reaction with no evidence of respiratory distress or cardiovascular compromise with antihistamines, such as diphenhydramine (Benadryl) and epinephrine. Moderate or severe distress presents a life-threatening emergency and requires immediate intervention. Severely unresponsive patients are transferred to hospital intensive care units when possible.
Nursing Care Management
The major nursing responsibility in anaphylaxis is anticipating which children are likely to develop a reaction, recognizing the early signs, and intervening appropriately. When an anaphylactic reaction is suspected, nursing responsibilities include immediate intervention and preparation for medical therapy. The nurse will need help and should notify the practitioner, but must not leave the patient. The child is placed in a head-elevated position (unless contraindicated by hypotension) to facilitate breathing, and oxygen is administered. If the child is not breathing, cardiopulmonary resuscitation is initiated.
If the cause can be determined, implement measures to slow the spread of the offending substance. For example, discontinue an IV medication or dye infusion. If an IV infusion line is not in place, establish one immediately, and monitor the flow rate carefully. Monitor vital signs every 15 minutes, and measure urinary output at regular intervals. Administer medications as prescribed, with regular assessment to monitor their effectiveness and to detect side effects of the medication and fluid overload.
To prevent an anaphylactic reaction, parents are always asked about possible allergic responses to foods, medications, products such as latex, and environmental conditions. (See Nursing Care Guidelines box, p. 408) These are displayed prominently on the patient’s chart. Note the specific allergen and the type and severity of the reaction. Parents are excellent historians, especially when the child has displayed a dramatic reaction to a substance. Drugs, including related drugs (e.g., penicillin and nafcillin), that have produced a previous reaction are never given.
The child and the parents need as much reassurance as can be provided without giving false hope. Keep them informed of the child’s progress, the reasons for the therapies, and what they can reasonably expect. This is a frightening experience and one that the family will remember and make every effort to prevent from recurring. The use of a convenient and visible method of conveying medical information, such as a bracelet or necklace, is encouraged. For the child who is allergic to insect venom, prescribe the family an emergency kit to be kept with the child at all times (e.g., EpiPen or EpiPen Jr Auto-Injector). Teach both the family and the child, if the child is old enough and is likely to be away from the family (e.g., at school), how to use the equipment. (See Chapter 27.)
Toxic Shock Syndrome
Toxic shock syndrome (TSS) is a relatively rare condition caused by the toxins produced by the Staphylococcus bacteria. First described in 1978, TSS can cause acute multisystem organ failure and a clinical picture that resembles septic shock. TSS became well known in 1980 because of the striking relationship between the disease and tampon use (Nakase, 2000). An aggressive health education campaign about the dangers of prolonged tampon use and a change in the chemical composition of tampons have markedly reduced the incidence of TSS in menstruating women. Cases of TSS have also been reported in men, older women, and children.
Pathophysiology
Evidence from several sources suggests that TSS occurs secondary to infection with phage group 1 S. aureus (Chuang, Huang, and Lin, 2005). The organism is believed to produce an epidermal toxin, but the precise mode of transmission is not known.
In approximately half the cases, TSS is seen in menstruating women and is usually associated with tampon use. The tampon may carry the organism from the fingers or vulva into the vagina during insertion, may traumatize the vaginal wall, or may provide a favorable environment for growth of the organism. TSS has also been associated with other bacterial infections, such as sinusitis or pneumonia, catheter site infections, skin infections, postoperative wound infections, and infection related to foreign bodies such as nasal packing or contraceptive diaphragms (Chuang, Huang, and Lin, 2005).
Clinical Manifestations
The sudden development of high fever, vomiting and diarrhea, profound hypotension, shock, oliguria, and an erythematous macular rash with subsequent desquamation are characteristic manifestations of TSS. Other manifestations include headache, blurred vision, purulent conjunctivitis, abdominal guarding, and purulent vaginal discharge.
Complications of TSS include respiratory distress, cardiac dysfunction, hematologic changes (particularly disseminated intravascular coagulation), and abnormal liver function. Impaired perfusion to the extremities may become severe, with eventual necrosis and loss of extremities.
Diagnostic Evaluation
The diagnosis is established on the basis of criteria in the TSS case definition of the Centers for Disease Control and Prevention (Box 29-11). A history of tampon use contributes to the diagnosis. Laboratory tests may include cultures from blood, vagina, cervix, and discharge from any suspected source of infection. Other laboratory tests are those that facilitate the management of shock.
Therapeutic Management
The management of TSS is the same as management of shock of any cause. Because the disease is highly varied in intensity, direct therapy toward supportive care in mild cases to hospitalization and intensive care in severe cases. Appropriate parenteral antibiotics are usually administered after cultures are obtained. Preventing complications of impaired circulation demands constant observation and immediate therapeutic intervention for hypotension, pulmonary dysfunction, acidosis, hematologic changes, and renal impairment.
Nursing Care Management
Nursing care and observation of the acutely ill patient are the same as those described for shock of any cause. Because the disease is relatively rare, direct the major nursing efforts toward prevention. The association between TSS and the use of tampons provides some direction for education. Teach adolescent girls who use tampons general hygiene measures, such as hand washing before insertion of the tampon and not using a tampon that has been dropped or otherwise soiled. Insert tampons carefully to avoid vaginal abrasion. Also it is wise to modify their use. For example, use tampons intermittently during the menstrual cycle, alternating with sanitary napkins—perhaps using napkins at the night, when at home during the day, and when flow is light. Advise young girls not to use superabsorbent tampons and not to leave any tampon in the body for more than 4 to 6 hours.
Burns
![]() Burn injuries are usually attributed to extreme heat sources but may also result from exposure to cold, chemicals, electricity, or radiation. Most burns are relatively minor and do not require definitive medical treatment. However, burns involving a large body surface area, critical body parts, or the geriatric or pediatric population often benefit from treatment in specialized burn centers. The American Burn Association (2006) has established criteria to guide decisions regarding the severity of injury and the need for transfer for specialized care.
Burn injuries are usually attributed to extreme heat sources but may also result from exposure to cold, chemicals, electricity, or radiation. Most burns are relatively minor and do not require definitive medical treatment. However, burns involving a large body surface area, critical body parts, or the geriatric or pediatric population often benefit from treatment in specialized burn centers. The American Burn Association (2006) has established criteria to guide decisions regarding the severity of injury and the need for transfer for specialized care.
Epidemiology and Etiology
Burn injuries represent one of the most severe traumas a body can sustain. Ongoing efforts toward education, burn prevention, safer home and work environments, and new methods of firefighting have significantly decreased burn injuries. The death rate from fire and flame injury among children 14 years of age and under declined by 68% from 1987 to 2005. Fire and burns are the fourth leading cause of unintentional injury–related death among children 14 years of age and under. Children, particularly those 5 years of age and under, are at greatest risk from home fire death and injury, having a death rate of nearly twice the national average (Safe Kids Worldwide, 2008, 2009).
Another source of burn injury is nonaccidental injury due to maltreatment. Such injuries most commonly occur to children 3 years of age and younger. Maltreated children are most likely to live in poverty-level households headed by a young, single parent who has two or more children. Thirty percent of children suffering recurrent burn injury are eventually mortally injured (Robert, Blakeney, and Herndon, 2007). Scald burns are the most common injury, followed by contact burns. Suspect abuse if there is a burn distribution inconsistent with the reported incident, a delay in seeking treatment, and a history of family instability and inability to deal with stress in crisis situations. Laws now exist in all states requiring health care workers to report suspected child abuse.
The use of alternative heating devices such as kerosene heaters and wood-burning stoves has increased the risk of contact burns in all age-groups. Most contact burns result from the lack of shielding to prevent contact with hot surfaces. Flame burns involving flammable liquids such as gasoline account for approximately 30% of injuries seen in the pediatric population, especially in children over 8 years of age. The ignition of clothing is the second leading cause of burn injury. In the past, girls were more susceptible, but the incidence has decreased significantly and clothing ignition deaths have decreased as clothing styles have changed; such injuries are now rare among children, with little overall gender difference. From 1975, when it was mandated for sleep wear in sizes from 0 to 6x to successfully pass a standard flame test, until 1999 when that law was repealed, the percentage of clothing burns caused by sleep wear in children ages 0 to 12 decreased from 55% to 27%. Sleep wear–related burns are being closely monitored to assess the effect of deregulation of sleep wear garments on related burns (Pruitt, Wolf, and Mason, 2007).
Children playing with matches or other ignition devices account for 1 in 10 residential fire deaths. Boys 2 to 5 years of age have the highest rate of nonfatal burns, and children younger than 9 years old cause fire-related death and injury due to child play fires (Pruitt, Wolf, and Mason, 2007). Careless smoking is associated with the majority of fatal house fires and is the most common cause of residential fire deaths. The use of alternative heating sources is another common cause of house fires. The source of ignition is often a combustible material stored near the device, the buildup of creosote in the chimney, spillage of fuel, or use of the wrong fuel. Many of these fires result in multiple deaths and injuries, especially in rural areas. The majority of fatal house fires occur during the cold winter months, most commonly in the Eastern part of the United States from December through February. The single most important element in the decrease in fire-related deaths seen since 1978 is the use of smoke detectors.
The majority of burns result from contact with thermal agents such as a flame, hot surfaces, or hot liquids. Electrical injuries caused by household current have the greatest incidence in young children, who insert conductive objects into electrical outlets or bite or suck on connected electrical cords in sockets (Pruitt, Wolf, and Mason, 2007). They occur most commonly during the spring and summer months and are also associated with risk-taking behaviors in young boys. Direct contact with high-or low-voltage current and lightning strikes are the most frequent mechanism of injury. The resistance of the tissue and the path of the electric current are responsible for the damage incurred. Electric current travels through the body on the path of least resistance—tissue, fluid, blood vessels, and nerves. A more localized burn is produced if skin resistance is high at the area of contact, whereas a more systemic pattern of injury is produced if the skin resistance is low. Often compared to a crush injury, serious electrical trauma results from current passing through vital organs, muscle compartments, and nerve or vascular pathways. Loss of limbs, cardiac fibrillation, respiratory collapse, and burns are common after exposure to electrical energy.
Chemical burns can cause extensive injury. The severity of injury is related to the chemical agent (acid, alkali, or organic compound) and the duration of contact. The mechanism of injury differs from that in other burns in that there is a chemical disruption and alteration of the physical properties of the exposed body area. Noxious agents exist in many cleaning products commonly found in the home. In addition to concern for localized damage, the potential for systemic toxicity must also be addressed. Of particular concern are the exposure of the eyes to chemical agents and the ingestion of caustic substances.
Although radiation injuries are rare, the most common sources in pediatrics are related to radiation exposure from medical therapies and ultraviolet light.
The causative agent in all burns has important implications for the treatment and prognosis of the pediatric patient. The nurse uses knowledge of the pathophysiologic processes of each type of injury in assessing the trauma and in planning, implementing, and evaluating care. Psychosocial issues are also important considerations in planning for the optimum long-term outcome.
Burn Wound Characteristics
The child’s physiologic responses, therapy, prognosis, and physical disposition are directly related to the amount of tissue destroyed; therefore the severity of the burn injury is assessed on the basis of the percentage of body surface area burned and the depth of the burn. Also important in determining the seriousness of injury are the location of the wounds, the child’s age and general health, the causative agent, respiratory involvement, and concomitant injuries.
Extent of Injury
The extent of the burn is expressed as a percentage of total body surface area (TBSA) injured. The child has different body proportions than the adult, resulting in inaccurate estimation of injury if the standard adult rule of nines is used. The proportions of the child’s trunk and arms are roughly the same as those of the adult. However, the infant’s head and neck make up 18% of the TBSA, and each lower extremity accounts for 14% of the TBSA. A modified rule of nines for the pediatric population proposes that for each year of life after age 2 years, 1% is deducted from the head and 0.5% is added to each leg (Helvig, 1993). It is generally more efficient to use any of a variety of charts designed to assign body proportions to children of different ages (Fig. 29-1).
Depth of Injury
A thermal injury is a three-dimensional wound and is also assessed in relation to the depth of injury. Traditionally the terms first, second, third, and fourth degree have been used to describe the depth of tissue injury. However, with the current emphasis on wound healing, this traditional terminology is being replaced by more descriptive terms related to the extent of destruction to the epithelializing elements of the skin. In general, first-degree burns are classified as superficial, and second-degree burns as partial-thickness. Third- and fourth-degree wounds are classified as full-thickness wounds. Partial-thickness wounds are further classified as superficial or deep in relation to the time required for healing to occur and the functional and cosmetic results anticipated. Because both terminologies are often used interchangeably, they are both presented in Fig. 29-2, which describes the characteristics of burn wounds.
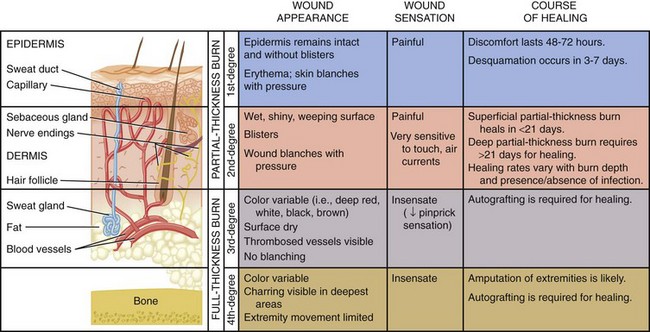
Fig. 29-2 Classification of burn depth according to depth of injury. (From Black JM: Medical-surgical nursing: clinical management for positive outcomes, ed 8, Philadelphia, 2008, Saunders.)
Superficial (first-degree) burns are usually of minor significance. There is often a latent period followed by erythema due to vasodilation. Tissue damage is minimum, the protective functions of the skin remain intact, and systemic effects are rare. Pain is the predominant symptom, and blisters do not form. The dead epidermis sloughs and is replaced by regenerating keratinocytes within 3 or 4 days without scarring (Pham, Gibran, and Heimbach, 2007). The burning sensation and pain usually resolve in 48 to 72 hours, and in 3 to 6 days the damaged epithelium peels off in small scales or sheets (Carrougher, 1998). A mild sunburn is an example of a superficial first-degree burn.
Partial-thickness (second-degree) injuries involve the epidermis and varying degrees of the dermis. These wounds are painful, moist, red, and blistered. Superficial partial-thickness burns involve the epidermis and part of the dermis. Dermal elements are intact, and the wound should heal in approximately 14 days with variable amounts of scarring. The wound is extremely sensitive to temperature changes, exposure to air, and light touch. Although classified as second-degree or partial-thickness burns, deep dermal burns resemble full-thickness injuries in many respects. Sweat glands and hair follicles remain intact. The burn may appear mottled, with pink, red, or waxy white areas exhibiting blisters and edema formation (Fig. 29-3). Systemic effects are similar to those encountered with full-thickness burns. Although these wounds heal spontaneously in approximately 21 days, they do so with extensive scarring.
Full-thickness (third-degree) burns are serious injuries that involve the entire epidermis and dermis and extend into subcutaneous tissue. Thrombosed vessels can be seen beneath the surface of the wound, and nerve endings, sweat glands, and hair follicles are destroyed. The burn varies in color from red to tan, waxy white, brown, or black and is distinguished by a dry, leathery appearance (Fig. 29-4). Normally, full-thickness burns lack sensation in the area of injury because of the destruction of nerve endings. However, most full-thickness burns have superficial and partial-thickness burned areas at the periphery of the burn, where nerve endings are intact and exposed. Also, excised eschar and donor sites cause exposed nerve fibers. Finally, as peripheral fibers regenerate, painful sensation returns. Consequently, children often experience severe pain related to the size and depth of the burn. Full-thickness wounds are not capable of reepithelialization and require surgical excision and grafting to close the wound.
Fourth-degree burns are also full-thickness injuries and involve underlying structures such as muscle, fascia, and bone. The wound appears dull and dry, and ligaments, tendons, and bone may be exposed.
Severity of Injury
Burns are classified as major, moderate, or minor, which is useful in determining the patient’s disposition for treatment. Burn patients can usually be distinguished as (1) those with a major burn injury, who require the services and facilities of a specialized burn center; (2) those with a moderate burn, who may be treated in a hospital with expertise in burn care; and (3) those with minor injuries, who can be treated on an outpatient basis (Table 29-6). The severity of the injury depends on the extent and depth of the burn, the causative agent, the body area involved, the patient’s age, and concomitant injuries and illnesses.
TABLE 29-6
SEVERITY GRADING SYSTEM ADOPTED BY AMERICAN BURN ASSOCIATION
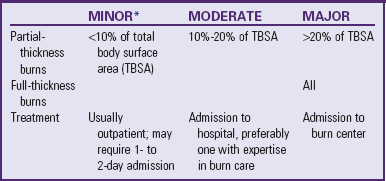
*Minor burns exclude any burn involving the face, hands, feet, perineum, or crossing joints; electrical burns; any injury complicated by inhalation injury or concomitant trauma; and children with psychosocial factors affecting the injury.
From Vaccaro P, Trofino RB: Care of the patient with minor to moderate burns. In Trofino RB, editor: Nursing care of the burn-injured patient, Philadelphia, 1991, FA Davis.
The nurse makes initial assessment of the extent of skin damage by observation and simple diagnostic techniques. The extent of body surface area involvement is readily calculated, and the appearance of the wound provides clues as to whether the injury involves the full thickness of the skin or only a portion of the skin layers. Touching injured surfaces to test for blanching and capillary refill indicates whether circulation to the area is intact.
It is important to consider the cause of injury and the duration of contact with the burning agent. In general, the more intense the heat source and the longer the contact, the deeper the resulting injury. Hot liquids may result in partial-thickness burns, whereas full-thickness injuries are associated with flame burns. This may vary with the child’s age. Very young children are likely to sustain deeper injuries because of the thin nature of infant skin. This makes estimation of burn depth difficult in young children, especially after scald injuries. Inflicted injuries tend to be more severe than accidental burns because contact with the burning agent is prolonged. Electrical injuries may also be difficult to assess initially. Visible tissue destruction may appear minimum, and damage to underlying structures may not be evident. The circumstances of the burn may also suggest the presence of associated injuries.
Certain areas of the body carry a higher risk of complications and therefore require specialized care. Burns of the hands and feet and across joints may not necessarily involve a large body surface area, but injury and scar formation may interfere with normal growth and development. Specialized care is required to preserve maximum function. Burns to the face and neck, along with a history of the injury occurring in an enclosed space, raise a high index of suspicion of inhalation injury. In addition, airway compromise and hypoxia may result from edema formation and pulmonary injury. Damage to the delicate cartilage of the nose and ears results in facial deformities. Facial burns may involve the eyes and have long-term consequences for vision. Perineal burns are prone to infection and maceration in all patients, especially in young children who are not toilet trained. Scar bands and contractures in the perineal area may interfere with hygiene and mobility.
Children younger than 2 years of age have a significantly higher mortality rate than older children with burns of a similar magnitude. The infant has minimum protein stores, which are rapidly depleted during burn shock; an immature immune response, which increases the risk of infection and sepsis; and a greater amount of body water in proportion to size that is intolerant of rapid fluid shifts. In addition, the child has not achieved mature renal function. This negatively affects the ability to retain sodium and water. These considerations, combined with the previously discussed fragility of the skin in the very young, increase the severity of injury.
Many patients sustaining thermal injuries may also suffer associated trauma. The circumstances of the accident may offer clues to related trauma. Children involved in house fires may have jumped from a window, sustaining fractures. Motor vehicle accidents and electrical injuries often result in concomitant injuries. Any suspicion of child abuse should alert the health care team to rule out other injuries.
Pathophysiology
![]() A burn injury represents a catastrophic insult that involves all organ systems. Understanding the pathophysiology underlying thermal trauma is essential to provide appropriate nursing care to the pediatric burn victim.
A burn injury represents a catastrophic insult that involves all organ systems. Understanding the pathophysiology underlying thermal trauma is essential to provide appropriate nursing care to the pediatric burn victim.
Local Response
Damage to human skin by heat results in two types of injury: an immediate direct cellular response and a delayed response caused by dermal ischemia. Irreversible cellular damage from protein denaturation occurs at temperatures exceeding 45° C (113° F). Three zones of injury demonstrate the evolution of local tissue damage (Fig. 29-5). The unstable area of injured cells, which may survive under ideal conditions, is designated the zone of stasis. Progressive injury caused by dermal ischemia may occur in this zone (Box 29-12).
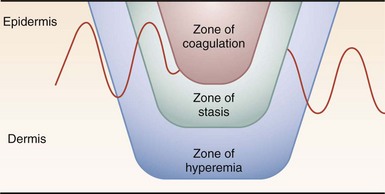
Fig. 29-5 Zones of injury in burn. (From Townsend CM: Sabiston textbook of surgery, ed 18, Philadelphia, 2007, Saunders.)
Edema Formation: Thermal injury to the vessels in the two outer zones results in increased capillary permeability. At the same time, vasodilation causes an increase in hydrostatic pressure within the capillaries. The increased hydrostatic pressure, combined with the increased capillary permeability, causes loss of water, protein, and electrolytes from the circulating volume into the interstitial spaces.
To understand the physiologic mechanism of the formation of burn edema, an understanding of the microvascular fluid balance is necessary. Burn injury not only causes edema at the site, but extravasated and sequestered fluid and protein also enters nonburned tissue. The directly injured cells have a damaged cell membrane that leads to an increase in sodium and potassium shift, resulting in cell swelling. Intracellular water and sodium increase. This process not only occurs in injured cells, but also with those that are not directly heat injured. Edema develops when the rate of fluid being filtered from the microvessels exceeds that of the lymph flow. The amount of edema depends on the type and extent of burn injury (Kramer, Lund, and Beckman, 2007).
Fluid Loss: Fluid transport across the microcirculatory wall in normal and pathologic states is quantitatively described by the Landis-Starling equation. This equation describes the physical forces and physiologic mechanisms that govern fluid transfer between vascular and extravascular compartments. Normal capillary barriers that separate the intravascular and interstitial compartments are disrupted, which results in severe depletion of plasma volume and an increase in extracellular fluid. Clinically this is manifested as hypovolemia (Warden, 2007).
Circulatory Status: Significant circulatory alterations take place in the zone of stasis located around the dead coagulated tissue. Heated red blood cells become spherical. These heat-damaged cells, together with hemoconcentration from fluid shifts, depressed cardiac output, and tissue edema, reduce the blood flow in the burned area, resulting in capillary stasis. Thrombi develop, which further impedes circulation and produces tissue ischemia and necrosis. Hyperviscosity and impaired blood flow are attributed to the release of substances such as thromboplastin and clot-activating factors from damaged cells. These substances cause the production of microemboli, platelet adhesion and aggregation, and increased pain and edema. Circulation in the area around partial-thickness wounds ceases immediately after injury but is usually restored within 24 to 48 hours. In full-thickness burns, however, the vascular supply is completely occluded, and no appreciable circulation is reestablished until granulation takes place at the interface between burned and unburned skin.
Tissue Repair: With reasonable care, superficial partial-thickness injuries heal spontaneously and uneventfully through the generative capacity of the stratum germinativum and epithelial cells of the lining of skin appendages. The wound should heal in approximately 14 days with minimum scarring.
Deep partial-thickness burns heal more slowly by regeneration from the epithelial lining of skin appendages, sweat glands, and hair follicles. A thin epithelial covering develops in 25 to 35 days, but this type of burn may require several months to heal. Scarring is common. Infection, trauma, or severe hypothermia easily converts a partial-thickness wound to a full-thickness injury, especially in the normally thinner skin of young children. Fluid loss and metabolic consequences may be considerable.
Cell destruction by coagulation necrosis occurs in full-thickness burns. Dead tissue and exudate convert to a thick, leathery eschar in 48 to 72 hours; the eschar liquefies and begins to separate in 12 to 21 days if not surgically excised. This process is a result of autolysis, leukocyte digestion, and disintegration of collagen fibers. The dead avascular tissue provides an ideal environment for bacterial growth. If tissue is not grafted, new granulation tissue forms on the wound bed. The wound heals slowly by proliferation from the edges, with a high risk of infection and severe scarring. Full-thickness burns result in severe edema with fluid and electrolyte shifts and extensive metabolic changes.
Systemic Responses
![]() Cardiovascular System:
Cardiovascular System: ![]() Animation—Capillary Leak
Animation—Capillary Leak
The immediate postburn period is marked by dramatic alterations in circulation, known as burn shock. A precipitous drop in cardiac output precedes any change in circulating blood or plasma volumes. This initial decrease in cardiac output (approximately 50% of normal resting values) is attributed to a circulating myocardial depressant factor that is associated with severe burn injury and directly affects the contractility of the heart muscle. As a result of fluid losses through denuded skin, increased capillary permeability, and vasodilation, the circulating volume decreases rapidly; cardiac output is reduced even further, usually leveling off at approximately 20% of normal resting values. After adequate fluid resuscitation, cardiac output spontaneously returns to normal in 24 to 36 hours. If fluid is not replaced, cardiac output continues to decrease, resulting in inadequate perfusion, organ dysfunction, and ultimately death.
Capillary permeability with leakage of fluid takes place both in uninjured areas and in the burn wound. Together with the shrinkage of drying eschar, severe edema caused by the rapid fluid shift to the interstitial spaces may produce a tourniquet effect, resulting in compartment syndrome. Compartments are composed of groups of muscles in the extremities and are surrounded by fibrous tissue. The inability of the fascia to expand in the presence of massive edema increases the pressure in the compartment, compromising circulation and entrapping nerves. Treatment is required during the acute phase and consists of surgical incision of the burned tissue (escharotomy) to restore distal circulation. If the escharotomy is not sufficient, an incision of the muscle sheath (fasciotomy) is performed (Fig. 29-6).
Edema fluid accumulates rapidly in the first 18 hours after injury and reaches a maximum in approximately 48 hours. Capillary permeability returns to normal, and fluid is reabsorbed, chiefly by way of the lymphatics. Reabsorption usually proceeds at the rate of fluid accumulation, although it may persist longer. Redistribution of fluid is often complex and unpredictable and is marked by diuresis.
In most children the cardiovascular system is able to withstand the demands placed on it, although shock is a prominent feature of large thermal injuries. Some children are prone to congestive heart failure and pulmonary edema. In addition, peripheral circulation in infants is less efficient and more labile, which complicates the burn response and therapy in this age-group.
Renal System: Children younger than 2 years of age lack the ability to concentrate urine because of the immaturity of their renal system and are therefore at an increased risk for dehydration. In addition, the child has a relatively larger TBSA in relation to weight than an adult. These issues, combined with limited physiologic reserves, increase the fluid requirements for children during burn shock resuscitation and in compensating for evaporative water losses (Warden, 1992). Loss of fluid from the intravascular compartment causes renal vasoconstriction that in turn leads to reduced renal plasma flow and depressed glomerular filtration. When adequate fluids are provided, the glomerular filtration rate returns to normal, and by the third or fourth postburn day, urinary output increases as edema fluid is mobilized and eliminated. In the first few days oliguria is more commonly the result of inadequate fluid replacement than of acute renal failure. If the child does not respond to treatment or if there is inadequate fluid resuscitation, acute renal failure may develop, with significant kidney damage.
BUN and creatinine levels are elevated as a result of tissue breakdown, decreased circulating volume, and oliguria. Hematuria may also be evident from the hemolysis of red blood cells, and oliguria may develop as a consequence of the increased pigment load. Myoglobinuria is especially common after extensive electrical injury. Cell destruction releases large amounts of myoglobin, which occludes the kidney tubules and places the victim of electrical trauma at high risk for renal failure.
Gastrointestinal System: The GI system has been recognized as a target of systemic shock. After a burn injury, blood flow decreases to the GI system by one third even though cardiac output is maintained by resuscitation fluids. Ischemia results and can produce ulcer formation, enterocolitis (severe enough to cause full-thickness necrosis), and even intestinal perforation. Poor perfusion to the kidney and the liver can ensue, resulting in organ dysfunction. The GI tract functions as a barrier to contain GI bacteria within it. Disruption of the GI mucosal integrity is possibly a focus for sepsis in the burn patient. The exact mechanism by which bacteria and their products pass through the GI barrier is not clear. Both intracellular and transcellular processes may be involved. These consequences can be profound, and translocating whole bacteria can be a direct source of sepsis (Sheridan and Tompkins, 2007b).
With the placement of a nasogastric tube, gastric decompression empties the stomach to control aspiration of gastric contents until motility is reestablished. Take care to observe for signs of aspiration of gastric contents into the lung as a result of incompetence of the gastroesophageal junction. With GI function intact, enteral feedings with a nasogastric tube are begun immediately after acute resuscitation (Andrews, 1994).
Metabolism: The greatly accelerated metabolic rate in burn patients is supported by protein and lipid catabolism. The child has limited glycogen stores to provide energy, which therefore accelerates the protein and lipid breakdown. No other disease state produces as great a hypermetabolism as the burn injury. Therefore the child is vulnerable to prolonged starvation (Lee and Herndon, 2007). When the burn injury is extensive (>50% of TBSA), energy needs may approach twice the predicted basal requirements.
The stress of injury places high demands on the body. Stress-invoked glycogen breakdown depletes the energy stores in 12 to 24 hours, after which the body resorts to glyconeogenesis for high-energy needs. Blood glucose levels may be elevated as a result of insulin resistance. Rapid protein breakdown and muscle wasting occur if sufficient protein replacement is not provided.
Body temperature reflects the net balance between heat production and heat loss. As a result of the accelerated metabolism, children with burn injuries typically exhibit an elevated body temperature, even in the absence of infection. The thermoregulatory response is activated and results in an elevation of core body temperature. Burn injured patients strive for a core body temperature of about 38° C (100.4° F). Low or “normal” temperature may indicate overwhelming sepsis, or a fatigued physiologic capability to maintain temperature, and should be viewed with concern. Routine methods of heat conservation after a major burn injury are inadequate because of excessive heat loss through evaporation and convection (Saffle and Graves, 2007). Heat is lost as a result of the energy-consuming process of water evaporation from the damaged skin surface. The body tries to raise the core and skin temperature to offset heat losses secondary to evaporation through the burn eschar (Norbury and Herndon, 2007). Infants and young children are especially vulnerable because of the large surface area relative to metabolically active tissue. Burning destroys a lipid layer and converts skin that is normally impermeable to water to a state that transmits water vapor at least four times as rapidly as unburned skin. In partial-thickness burns this loss is greatest on the day of injury; in full-thickness burns it rises slowly at first and rapidly increases to reach a peak approximately the fourth day after the burn. Evaporative losses continue until partial-thickness wounds are healed and full-thickness burns are grafted. Therefore body stores of energy are rapidly depleted unless sufficient replacement is provided or losses are reduced.
Medications that affect metabolic rate may be used to prevent loss of body protein stores, thus protecting immunity, wound healing, muscle integrity, and organ function. Oxandrolone is an anabolic steroid that works to maintain and restore muscle mass, increase weight gain, and promote wound healing. Supplements of essential amino acids such as glutamine and arginine provide an anticatabolic effect, support wound healing, indirectly preserve lean body mass, improve immune function, and provide an antioxidant quality (Demling, 2005).
Neuroendocrine System: As a response to stress of any origin, the hypothalamic-hypophyseal mechanism restores equilibrium by secreting trophic hormones, which stimulate various target organs of the neuroendocrine system. Adrenal activity is markedly increased. The medulla responds by secreting additional amounts of the catecholamines epinephrine and norepinephrine. Adrenocortical hormones reach a peak immediately after injury and remain elevated for some time. Aldosterone secretion and a release of antidiuretic hormone are sustained at a high level throughout hospitalization. Despite this increased adrenal activity, adrenal insufficiency is a rare complication.
Anemia and Metabolic Acidosis: The hematocrit is initially elevated because of hemoconcentration resulting from fluid shifts to the interstitial spaces and red blood cell destruction. In addition, a reduced red blood cell half-life results from increased cell fragility. A significant loss of circulating red blood cell mass is predominantly associated with major burns.
Most burn patients exhibit some degree of metabolic acidosis as a result of the disruption of the body’s buffering action because of the fluid shift to the extravascular spaces and the altered concentrations of potassium, sodium, chloride, and bicarbonate ions. Reduced blood volume and cardiac output result in diminished perfusion and tissue hypoxia, with a shift to anaerobic metabolism. The resultant formation of metabolic acids is usually sufficiently compensated by respiratory mechanisms. Renal compensatory activities are impaired by the decreased blood flow.
Complications
Thermally injured children are subject to a number of serious complications, both from the wound and from systemic alterations resulting from the injury. The immediate threat to life is related to airway compromise and profound shock. During healing, infection—both local and systemic sepsis—is the primary complication. Mortality associated with thermal trauma in children increases with the severity of injury and decreases as age advances. In children older than 3 years, the mortality rate is similar to that of adults. Below this age, the rate of survival from the burn and its associated complications lessens considerably.
Pulmonary System: The impact of thermal injury on pulmonary function includes a full range of respiratory dysfunctions, including inhalation injury, aspiration of gastric contents, bacterial pneumonia, pulmonary edema and insufficiency, and emboli. In every age and burn size category, pneumonia is one of the most common infections in burn patients and is associated with high risk of mortality (Murphey, Sherwood, and Toliver-Kinsky, 2007).
Inhalation injuries result from trauma to the tracheobronchial tree after inhalation of the heated gases and toxic chemicals produced during combustion. Although direct thermal injury to the upper airway may occur, heat damage below the vocal cords is rare. Inspired heated air is cooled in the upper airway before reaching the trachea. Reflex closure of the cords and laryngeal spasm prevent full inhalation. Evidence of direct thermal injury to the upper airway includes burns of the face and lips, singed nasal hairs, and laryngeal edema. Clinical manifestation may be delayed as long as 24 to 48 hours. Wheezing, increasing secretions, hoarseness, wet rales, and carbonaceous secretions are signs of respiratory tract involvement. Upper airway obstruction is often associated with burn shock and fluid resuscitation. In such situations endotracheal intubation may be necessary to preserve a patent airway.
Suspect inhalation of carbon monoxide when the injury has occurred in an enclosed space. (See Smoke Inhalation Injury, Chapter 32, for a discussion of carbon monoxide inhalation.) Inhalation of other products of combustion, such as smoke and toxic chemicals, can produce varying degrees of pulmonary damage. Smoke from burning wood is extremely irritating; burning plastic materials, especially polyvinyl chloride, release smoke with gases containing chlorine, sulfuric acid, and cyanide. Respiratory injury is manifested by mucosal erythema and edema followed by sloughing of the mucosa. A mucopurulent membrane replaces the mucosal lining and seriously compromises respiration and ventilation.
A common etiologic factor in respiratory failure in the pediatric population is bacterial pneumonia, which may be secondary to airway injury or contamination from intubation or may be acquired through hematogenous spread of bacteria. Early in the postburn period the largest percentage of pulmonary infections result from nosocomial exposure, immobility, and abdominal distention. The hematogenous variety occurs later and is related to the septic burn wound or other foci, such as phlebitis at the site of an invasive IV line. A less common complication is pulmonary edema resulting from fluid overload or ARDS in association with gram-negative sepsis. (See Chapter 32.) This syndrome results from pulmonary capillary damage and leakage of fluid into the interstitial spaces of the lung. A loss of compliance and interference with oxygenation are the consequences of pulmonary insufficiency in conjunction with systemic sepsis.
Deep burns, especially those circling the thorax, may cause restriction of chest excursion as a result of edema and inelastic eschar formation. Young children are particularly at risk because of the pliability of the skeletal structure. Hypoxia is relieved by an escharotomy of longitudinal incisions along the anterior axillary lines combined with a transverse incision at the costal level. This procedure allows expansion of the chest wall to facilitate ventilation.
Wound Sepsis: Sepsis is a critical problem in the treatment of burns and is an ever-present threat after the shock phase. Initially, burn wounds are relatively pathogen free unless contaminated with potentially infectious material such as dirt or polluted water. However, dead tissue and exudate provide a fertile field for bacterial growth. On approximately the third postburn day, early colonization of the wound surface by a preponderance of gram-positive organisms (primarily staphylococci) changes to predominantly gram-negative opportunistic organisms, particularly Pseudomonas aeruginosa. By the fifth postburn day, bacterial invasion is well underway beneath the surface of the burn wound.
Characteristics of the burn wound contribute to the proliferation of pathogenic organisms. Vascular supply to full-thickness burns is occluded immediately, and no appreciable blood is supplied to the area for approximately 3 weeks after the injury. In partial-thickness wounds the circulation to the injured area is suspended for 24 to 48 hours; circulation is then restored unless infection supervenes. Thrombosis from bacterial invasion will impair circulation sufficiently to convert partial-thickness wounds to full-thickness injuries. These large amounts of nonviable tissue also provide an excellent medium for the growth of microorganisms.
Occlusion of the local blood supply impairs the delivery of both humoral and cellular defense mechanisms to the burned area. Initially there is a decrease in inflammatory and phagocytic cells to the wound, but the number of phagocytes gradually increases until they are present in abundance by the third postburn week, when granulation tissue is forming. Granulation tissue, with its rich blood supply, affords increasing resistance to infection. Organisms are normally a part of skin flora; therefore cultures with an organism concentration of 105/g of tissue have been arbitrarily chosen as the level of burn wound invasion.
The microflora present at any institution are influenced by the treatment modalities and choice of antibiotics. During the past 30 years there has been a reduction in the percentage of specific bacteria and fungi recovered from burn wounds. This reduction reflects improvements in patient management, nutritional support, aggressive excision and grafting of wounds, and topical antimicrobial therapy. Sepsis, in burn injury, is a major complication and a significant factor in morbidity and mortality (Sherwood and Traber, 2007).
Gastrointestinal System: GI dysfunction is common after burn injury as evidenced by feeding intolerance; mucosa ulceration; and bleeding, particularly in the stomach and duodenum. Within 72 hours of a major burn injury a significant number of patients may develop mucosal changes. This may progress to ulceration with septic episodes and hypoxemia. Potential causes of stress ulcers in burn patients are (1) mucosal ischemia, (2) increased acid production, (3) increased acid back-diffusion, (4) energy depletion, (5) bile reflux, and (6) direct mucosal injury with placement of intraluminal tubes.
Enteral feeding is one of the most important means of providing nutrition and has led to a decrease in mortality. Early enteral feeding often prevents some of these potential complications. Aggressive fluid resuscitation aids in maintaining adequate mucosal blood flow. Antacid and H2 receptor antagonist therapy can effectively prevent ulceration of the stomach and duodenum.
Ileus is also a common complication after a burn injury. Sepsis, electrolyte imbalance, narcotics, and renal failure are common causes. Patients experience abdominal distention and pain. Early enteral feeding again can assist in avoiding intestinal complications (Beierle and Chung, 2007).
Central Nervous System: Burn encephalopathy, as characterized by lethargy, withdrawal, or coma, occurs in children. Symptoms such as delirium and transient psychosis occur rarely among children under the age of 10 years. In such cases, electroencephalograms typically reveal diffuse, nonspecific, slow waves. In most cases burn encephalopathy can be attributed to hypoxemia, hyponatremia, hypovolemia, septicemia, and drug administration. Hallucinations are uncommon, but when they do occur, stress is the most likely cause, followed by pain and various medications. These symptoms, though short lived, are upsetting to the family and treatment team.
Proper treatment must first address organic causes of delirium or encephalopathy. The nurse must stabilize vital signs and normalize blood chemistries, glucose, and oxygenation. Sepsis must be ruled out and pain addressed. Then psychotropic medications may be administered (Thomas, Meyer, and Blakeney, 2007). There is usually full neurologic recovery, even with prolonged and serious manifestations.
Therapeutic Management
The initial management of the burn patient begins at the scene of injury. The first priority is to stop the burning process. The child should then be transported immediately to the nearest medical facility for definitive treatment and evaluation for transfer to a burn center. The child and the family will be extremely frightened and anxious; sensitivity to their emotional state provides reassurance during the transport process.
Stop the Burning Process: The chief aim of rescue in flame burns is to smother the fire, not fan it. Children tend to panic and run, which serves only to spread the flames and make assistance more difficult. Place the injured child in a horizontal position and rolled in a blanket, rug, or similar article, taking care to not cover the head and face because of the danger of inhaling toxic fumes. If nothing is available, the victim should lie down, cover the mouth with the hands, and roll over slowly to extinguish the flames. Remaining in the vertical position may cause the hair to ignite or may lead to the inhalation of flames, heat, or smoke.
Major burns with large amounts of denuded skin should briefly be cooled with a single application of tepid water. Heat is rapidly lost from burned areas, and additional cooling leads to a drop in core body temperature and potential circulatory collapse. Continuous wet dressings or the application of ice promotes vasoconstriction because of cooling, resulting in impaired circulation to the burned area and increased tissue damage. Chemical burns present special circumstances and require flushing with copious amounts of water during transport to a medical facility. The use of neutralizing agents on the skin is contraindicated because a chemical reaction is initiated and further injury may result. If the chemical is in powder form, the addition of water may spread the caustic agent. The powder should be brushed off if possible. If the chemical burn produces a blister, it is advisable to open the blister with a sterile object to remove any chemical present.
Remove burned clothing to prevent further damage from smoldering fabric and hot beads of melted synthetic materials. Also remove jewelry to eliminate the transfer of heat from the metal and constriction from edema formation. These steps also provide better access to the wound and preclude more painful removal later on.
Assess the Victim’s Condition: As soon as the flames are extinguished, assess the victim’s condition. Airway, breathing, and circulation are the priority concerns. Cardiopulmonary and cerebral emergencies are always a consideration after trauma. Cardiopulmonary complications may result from exposure to electric current, inhalation of toxic fumes and smoke, hypovolemia, and shock. Institute emergency measures as appropriate.
Cover the Burn: Cover the burn wound with a clean dry cloth to prevent contamination and alleviate pain by eliminating air contact. Cover the child who has extensive burns to prevent hypothermia. No attempt should be made to treat the burn. The application of topical ointments, oils, or other home remedies is contraindicated.
Transport the Child to Medical Aid: Do not give the child with an extensive burn anything by mouth to avoid aspiration in the presence of paralytic ileus and upper airway edema and to prevent water intoxication. The child is transported to the nearest medical facility. If this cannot be accomplished within a relatively short time, establish IV access if possible with a large-bore catheter. Oxygen, if available, is administered at 100%. Give a report of the initial assessment and any interventions implemented to the medical facility assuming responsibility for the child’s care.
Management of Minor Burns
Treatment of burns classified as minor can usually be managed adequately on an outpatient basis when the caregiver is reliable and able to carry out instructions for care and observation. Patients with less than optimum circumstances may require close follow-up to ensure compliance with the treatment program.
Cleanse the wound with mild soap and tepid water. Débridement of the wound includes removal of any embedded debris, chemicals, and devitalized tissue. Removal of intact blisters remains controversial. Some authorities argue that blisters provide a barrier against infection; others maintain that blister fluid is an effective medium for the growth of microorganisms (Smith, 2000). Most practitioners favor covering the wound with an antimicrobial ointment to reduce the risk of infection and provide some pain relief. The dressing consists of a fine-mesh gauze placed over the ointment and a light wrap of gauze dressing that avoids interference with movement. This helps keep the wound clean and protect it from trauma. Instruct the caregiver to wash the wound, reapply the dressing, and return the child to the office or clinic as directed for wound observation. The frequency of dressing changes can vary from every other day to twice a day.
Other practitioners prefer an occlusive dressing, such as a hydrocolloid, which is placed over the wound after cleansing. This method eliminates the discomfort associated with frequent dressing changes but impairs visualization of the wound surface.
If there is a high probability of infection or other complications or if there is doubt about the ability to carry out instructions, direct the parents to return daily for dressing changes and inspection, or a nurse may be assigned to make a home visit for that purpose. Frequent removal of the dressing is an effective mode of débridement. Soaking the dressing in tepid water before removal helps loosen the dressing and debris and reduces discomfort. Burns of the face and ears are usually treated by an open method (Carrougher, 1998). The wound is washed and débrided in the same manner, and a thin film of antimicrobial ointment is applied twice a day.
Obtain a tetanus history on admission. Tetanus prophylaxis is administered if there is no history of immunization or if more than 5 years have passed since the last immunization. Administration of antibiotics for minor burns is controversial. A mild analgesic such as acetaminophen is usually sufficient to relieve discomfort; the antipyretic effect of the drug also alleviates the sensation of heat.
Most minor burns heal without difficulty, but hospitalization is indicated if the wound margin becomes erythematous, gross purulence is noted, or the child develops evidence of systemic reaction (e.g., fever or tachycardia). Evaluate the child for functional impairment, and instruct the caregiver in the exercise and ambulation program. After wound healing, an evaluation of scar maturation and range of motion will indicate any need for further therapy.
Management of Major Burns
When a child with extensive burns is admitted to the hospital for treatment, a variety of assessments are conducted and therapies initiated. Of these, the priority concerns include the establishment and maintenance of an adequate airway, initiation of fluid administration, and evaluation and treatment of the wound. Although the order of implementation may vary from institution to institution, a number of procedures and activities are generally initiated on admission. Some are carried out simultaneously (Box 29-13).
Other therapies, including nutritional support, positioning and splinting to prevent contractures, treatment of anemia and hypoproteinemia, psychosocial support, and rehabilitative aspects of burn management, are initiated as appropriate throughout the course of treatment.
Establishment of an Adequate Airway: The first priority of care is airway maintenance. Thermal injuries to the face, nares, and upper torso; a history of injury in an enclosed space; an examination of the oral and nasal membranes that reveals edema, hyperemia, and blisters; and evidence of trauma to the upper respiratory passages all suggest inhalation of noxious agents or respiratory burns. If there is evidence of respiratory involvement, administer 100% oxygen and determine blood gas values, including carbon monoxide levels.
If the child exhibits changes in sensorium, air hunger, or other signs of respiratory distress, insert an endotracheal tube to maintain the airway. When severe edema of the face and neck is anticipated, perform intubation before swelling makes it difficult or impossible. A controlled intubation is preferred to an emergency procedure. Intubation allows for the delivery of humidified oxygen, the removal of secretions from respiratory passages, and the provision of ventilatory support.
Treatment may include bronchodilators (e.g., albuterol) to reduce bronchospasm. Bronchopulmonary hygiene to prevent atelectasis and pooling of secretions reduces the risk of pneumonia. Therapies include percussion and postural drainage, frequent position changes, and suctioning to remove secretions. Placing the child in a semi-Fowler position with high-flow oxygen and maximum humidity is often sufficient to relieve bronchospasm produced by trauma to the bronchial mucosa.
When full-thickness burns encircle the chest, constricting eschar may limit chest wall excursion. The child becomes increasingly difficult to ventilate. Escharotomy of the chest relieves this pressure and improves ventilation.
Fluid Replacement Therapy: The objectives of fluid therapy are compensation for water and sodium losses to the traumatized area and the interstitial spaces, replenishment of sodium deficits, restoration of circulating volume, provision of adequate perfusion, correction of acidosis, and improvement of renal function. Initiate treatment for burn shock in children with burns in excess of 15% to 20% of TBSA.
Types of fluid and electrolyte therapy in the first 24 hours after injury remain controversial. Lactated Ringer solution appears to be the most common resuscitation fluid currently used. Proponents of crystalloids alone for resuscitation report that other solutions, specifically colloids, are no better and certainly more expensive than crystalloids for maintaining intravascular volume after burn injury. The most common reason for not using colloids is that even large proteins leak from the capillary after burn injury (Warden, 2007).
The composition of the fluid administered varies with the philosophy of the individual practitioner and may consist of an isotonic saline solution, a near-isotonic solution, or even a hypertonic saline solution. Children’s decreased tolerance to hypertonic solutions may result in hypernatremia, hyperosmolality, and intracellular dehydration. Many formulas have been proposed as guidelines for fluid administration after burn injury. Perhaps the most commonly employed regimen is the Parkland formula. It is important to remember that any formula used during resuscitation serves only as a guideline; individual adjustments must be made based on the patient’s response to therapy. Fluid replacement is maintained at a rate that provides an hourly urinary output of 30 ml in older children and 1 to 2 ml/kg in children weighing less than 30 kg (66 lb). Other parameters monitored during fluid resuscitation include vital signs, capillary refill, and sensorium.
Some common reasons for patients to require fluids well in excess of the calculated volume include underestimation of burn size (particularly in pediatric patients), pulmonary injury that sequesters resuscitation fluid in the lung, electrical injury with greater tissue destruction than is visible, and delay in the initiation of fluid resuscitation (Smith, 2000). Irreversible burn shock that persists despite aggressive fluid resuscitation remains a significant cause of death in the immediate postburn period. Exchange transfusion consisting of the replacement of circulating volume by banked whole blood provides a therapeutic modality that may benefit the patient who fails to respond to conventional resuscitation. Inflammatory response factors, thought to be important in burn shock, are removed, thus lowering the concentration present in the body, restoring capillary integrity, and substantially reducing fluid requirements.
After the initial 24 to 48 hours, the capillary seal is restored. Fluid requirements decrease to a constant that persists until wound coverage is achieved. Colloid solutions such as albumin or plasma are useful to maintain plasma volume. Fluid balance may continue to be a problem throughout the course of treatment; especially during periods of increased evaporative loss from the burn wound. Approximately 48 to 72 hours after injury, interstitial fluid returns to the vascular compartment and diuresis occurs to eliminate excess fluids. During this phase, increasing intake to match urinary output can result in circulatory overload.
Nutrition: For 2 or 3 days immediately after injury, burn patients experience a hypometabolic phase when their metabolic rate and cardiac output decrease. Following this phase patients experience a hypermetabolic phase. This hypermetabolism is characterized by a hyperdynamic circulatory response with increased body temperature, oxygen and glucose consumption, carbon dioxide production, glycogenolysis, proteolysis, and lipolysis. This response begins on the fifth postburn day and continues up to 9 months after the burn, causing erosion of lean body mass, muscle weakness, immunodepression, and poor wound healing (Norbury and Herndon, 2007). This hypermetabolism is thought to slow wound healing, prolong generalized weakness, lead to loss of lean body mass, and increase morbidity (Lee and Herndon, 2007). Nutritional support, particularly through enteral feedings, recently has become more aggressive. The continuity of these feedings is important.
Some burn patients are able to eat. Encourage a high-protein, high-calorie diet as soon as possible after resolution of paralytic ileus. However, many have poor appetites and are unable to meet energy requirements solely by oral feeding. Most children with burns in excess of 25% TBSA require supplementation with tube feeding. An absence of bowel sounds does not preclude enteral nutrition. Because the small bowel maintains motility and absorptive capabilities, the placement of a small-bore feeding tube into the duodenum allows for the safe delivery of enteral nutrition during periods of paralytic ileus associated with trauma, sepsis, and anesthesia. A nasogastric tube that decompresses the stomach protects the patient from aspiration.
Use of total parenteral nutrition (TPN) has now been essentially replaced by enteral nutrition for both theoretical and practical reasons. Enteral nutrition directly nourishes the bowel mucosa with nutrients (e.g., glutamine). Small amounts of these nutrients within the bowel lumen stimulate the function of intestinal cells and normal mucosa function. This may help preserve normal blood supply to the intestines. Maintaining intestinal integrity may reduce bacterial translocation and sepsis, as well as preserve immune function. Along with the hazards of central venous access, TPN appears to be associated with increased secretion of tumor necrosis factor and other proinflammatory mediators (Saffle and Graves, 2007).
Specific guidelines for vitamin and micronutrient supplementation for the burn patient have not been established. Limited research has been done on the homeostasis of vitamins and trace elements after burn injury (Klein, Przkora, and Herndon, 2007).
Medication: Antibiotics are usually not administered prophylactically. The administration of systemic antibiotics to control wound colonization is not indicated, since decreased circulation to the injured area prevents delivery of the medication to areas of deepest injury. Surveillance cultures and monitoring of the clinical course provide the most reliable indicators of developing infection. Appropriate antibiotics can then be instituted to treat the identified organism. Group B streptococci cultured from the throat or wounds are particularly destructive to grafted tissue. Do not overlook otitis media as a source of fever in the pediatric population.
Some form of sedation and analgesia is required in the care of burned children (Henry and Foster, 2000). During the initial resuscitation period, IV administration of narcotics, along with anxiolytics, is required for baseline and procedural pain management. Morphine, fentanyl (Sublimaze), and midazolam (Versed) are the most commonly used agents (Kahana, 2003). (See Pain Management, Chapter 7.)
Anesthetic agents such as nitrous oxide, propofol, and ketamine also are used to control procedural pain. A major drawback with nitrous oxide is that staff is exposed to the gas because it is self-administered by the patient. Propofol is a nonbarbiturate hypnotic agent without analgesic activity. It also causes depressed respiratory drive, loss of airway reflexes, and hypertension. Propofol must be given in doses large enough to cause loss of consciousness to prevent response to painful procedures. Ketamine may preserve airway reflex; however, side effects may be noted such as production of copious upper airway secretions, tachycardia, and hypertension. Ketamine can produce postadministration hallucinations, particularly in adolescent boys. Repeated use may produce tolerance, so increased doses are required over time. To avoid volatile anesthetics, a combination of midazolam and fentanyl can be given intravenously (Meyer, Patterson, Jaco, et al, 2007).
Management of the Burn Wound
After the initial period of shock and restoration of fluid balance, the primary concern is the burn wound. The primary goal for burn wound management is to close the wound as soon as possible (Gordon and Marvin, 2007). The objectives of wound management include prevention of infection, removal of devitalized tissue, and closure of the wound. The application of dressings and topical antimicrobial therapy reduce pain by minimizing air exposure.
Primary Excision: In children with large, full-thickness burn wounds, excision is performed as soon as the patient is hemodynamically stable after initial resuscitation. Because the burn wound is precipitating the exaggerated physiologic response, many associated complications do not resolve until the eschar is excised and the wound is closed. One of the most effective therapies for decreasing mortality from major burn injuries is the early excision of the burn wound and its coverage by various techniques (Barrow and Herndon, 2007).
Wound Hygiene: Hydrotherapy is used to cleanse the wound and assist with separating eschar. There are variances from institution to institution on the particular method, but the common approach is to cleanse and débride once or twice a day. Hydrotherapy helps cleanse not only the wound but the entire body and also aids in maintenance of range of motion. Partial-thickness wounds require débridement of devitalized tissue to promote healing. Débridement is very painful and requires some type of analgesia before the procedure. The water acts to loosen and remove sloughing tissue, exudate, and topical medications. Mesh gauze entraps the exudative slough and is readily removed during hydrotherapy (Fig. 29-7). Any loose tissue is carefully trimmed away before the wound is redressed (Fig. 29-8).
Wound Dressings: Daily dressing changes of the burn wound are recommended to allow for inspection and cleansing of the wound. Dressing changes offer an opportunity to meticulously observe the burn for infection. The volume of draining and the physical condition of the dressing also dictate frequency of dressing change. Often wound dressings become saturated, soiled, or disheveled, indicating that additional dressing changes may be required (Hartford and Kealey, 2007).
Topical Antimicrobial Agents: Several methods are used for covering the burn wound (Box 29-14 and Fig. 29-9). All meet the objective of preparation for permanent wound coverage, and all use some type of topical agent. Before the development of effective topical agents for reducing the incidence of invasive organisms, wound sepsis was the major cause of mortality from burn injury. The goal is to minimize wound colonization. A variety of specific agents are available, including silver sulfadiazine (Thermazene), mafenide acetate (Sulfamylon), and bacitracin. Topical agents do not eliminate organisms from the wound but can effectively inhibit bacterial growth. To be effective, a topical application must be nontoxic, capable of diffusing through eschar, harmless to viable tissue, inexpensive, and easy to apply. It should not encourage the development of resistant strains of bacteria and should produce minimum electrolyte derangement.

Fig. 29-9 Burn wound covered with gauze dressings and secured with tubular elastic netting. (Courtesy CR Boeckman Regional Burn Center, Akron, Ohio.)
Some topical agents are packaged and prepared on a fine-mesh gauze, which allows ease of application (Fig. 29-10). The gauze provides necessary protection for the wound, maximizes patient comfort, increases the rate of healing, reduces the necessity for frequent dressing changes, and is cost-effective. Examples include a nanocrystalline film of pure silver (Acticoat and Silverlon) and a hydrofiber with ionic silver (Aquacel Ag). Most often these gauzes are used on superficial second-degree burns, on donor sites, and for graft care, except for Acticoat, which can also be used for full-thickness wounds (Bessey, 2007).
Temporary Skin Substitute: Permanent coverage of extensive burns is a prolonged process that requires repeated operations for débridement and grafting. Temporary skin substitutes provide transient physiologic wound closure, thereby helping control pain, absorb wound exudates, and prevent wound desiccation (Sheridan and Tompkins, 2007a). Temporary skin substitutes markedly reduce pain and facilitate movement of joints to retain range of motion.
Allograft (homograft) skin comes from human cadavers and is processed by commercial skin banks (Box 29-15). These skin banks screen donors for communicable diseases and track the skin much like blood transfusions. Allograft skin is particularly useful in the coverage of surgically excised, deep partial-thickness and full-thickness wounds in extensive burns when available donor sites are limited. Severe immunosuppression occurs in massively burned children, and the allograft becomes adherent (Fig. 29-11). The allograft can remain in place until suitable donor sites become available. Typically rejection occurs approximately 14 days after application. The use of an allograft is limited by the availability of tissue banks and the supply of suitable donors.
Although various animal skins have been used for many years to provide temporary coverage of wounds, only porcine xenograft is widely used today. Porcine xenograft does not vascularize, but it will adhere to a clean superficial burn and provide excellent pain control while the burn heals (Sheridan and Tompkins, 2007a). Pigskin dressings are replaced daily or every 2 or 3 days. They are particularly effective in children with partial-thickness scald burns of the hands and face because they allow relatively pain-free movement, which reduces contracture formation and has the added benefit of improving appetite and morale (Fig. 29-12).

Fig. 29-12 Porcine xenograft applied to partial-thickness burn. (Courtesy CR Boeckman Regional Burn Center, Akron, Ohio.)
When applied early to a superficial partial-thickness injury, biologic dressings appear to accelerate wound healing. They create an environment at the wound surface that is conducive to epithelial growth; this is in contrast to topical antimicrobial agents, which may slow epithelialization. Biologic dressings must be applied to clean wounds. If the dressing covers areas of heavy microbial contamination, infection occurs beneath the dressing. In the case of partial-thickness burns, such an infection may convert the wound to a full-thickness injury. It is important to observe the wound daily for any signs of an infectious process.
Synthetic Skin Coverings: A number of satisfactory skin substitutes are available for the management of partial-thickness burn wounds. Ideally, the dressing should provide many of the properties of human skin: adherence, elasticity, durability, and hemostasis. Synthetic skin substitutes are readily available, have varied shelf lives, and are relatively expensive.
Synthetic dressings are composed of a variety of materials and can be used successfully in the management of superficial partial-thickness burns and donor sites. These dressings do not contain antimicrobial properties. Examples include a pertrolatum dressing (Xeroform), synthetic silicone meshed products (Biobrane), a hydrocolloid dressing (DuoDERM), and transparent adhesive films (OpSite and Tegaderm) (Bessey, 2007). As with biologic dressings, it is important that the wound be free of debris before applying the dressing. Body temperature elevation or evidence of purulence, erythema, or cellulitis around the wound edges may indicate that the wound has become infected beneath the dressing. Prompt discontinuance of the synthetic dressing is indicated. All synthetic dressings are reputed to hasten wound healing and reduce discomfort.
Artificial Skin: Integra, a biologic two-layer product that allows the dermis to regenerate, has significantly improved burn wound healing and decreased scar formation. It is applied to partial- and full-thickness burns. The inner layer is porous woven fiber made of a pure form of collagen (a fibrous protein taken from animal tendons and cartilage) and other materials designed to induce better regeneration of the patient’s normal tissue. The outer layer is a soft silicone membrane that holds moisture for 2 to 3 weeks. The silicone layer is peeled off after the dermis is formed. The application of artificial skin does not replace the grafting procedure, but it prepares the burn wound to accept an ultrathin autograft. Advantages include faster healing of the burn wound when integrity of the dermis is restored, faster healing of donor sites with the use of ultrathin grafts, and restoration of sweat glands and hair follicles. A disadvantage is its high cost.
Permanent Skin Coverings: Permanent coverage of deep partial- and full-thickness burns is usually accomplished with a split-thickness skin graft. This graft consists of the epidermis and a portion of the dermis removed from an intact area of skin by a special instrument: the dermatome (Fig. 29-13). If all the wounds cannot be grafted at once, there are priority areas for coverage: the face, hands, joint surfaces, and neck. These preferential sites are chosen to hasten healing, establish function, and improve the patient’s sense of well-being.
With extensive burns it is often difficult to find enough viable skin to cover the wounds; therefore available donor sites are used to the best advantage by special techniques. Box 29-15 describes the various types of split-thickness skin grafts. Sheet grafts (Fig. 29-14) are used in areas where cosmetic results are most visible; mesh grafts (Fig. 29-15) result in a less desirable cosmetic and functional outcome. Requirements for the successful vascularization of any graft are listed in Box 29-16.
Until blood supply to the grafted skin is established, it is nourished by osmotic interchange with the recipient bed. Wound healing occurs as the area releases fibrin, which attaches the graft to the bed. The fibrin is infiltrated by leukocytes, fibroblasts, and the capillary buds of the granulation tissue. This process begins within hours of grafting, and vascularization is established after 3 days. Within 2 weeks the graft is attached to the recipient bed by connective tissue.
The donor site is dressed with synthetic wound coverings or fine-mesh gauze until the dressing separates at 10 to 14 days, when the wound is healed. Dressings are not changed on donor sites to avoid damage to newly healed, delicate epithelium. Healed donor sites are available for reharvesting in patients with extensive burns and limited undamaged skin (Fig. 29-16). The quality of skin from donor sites is decreased when multiple grafts are taken.
Cultured Epithelium: For more than 20 years it has been possible to culture vast numbers of epithelial cells from a small skin biopsy, and this has led to the widespread use of cultured epithelial grafts to cover burns. Colonies of epithelial cells expand into broad sheets of undifferentiated epithelial cells. The resulting sheets are attached to a petrolatum gauze carrier to ease handling. Many of the imperfections associated with epithelial cell wound closure may be attributed to the lack of dermis. Despite scattered cases, application of cultured epithelial grafts onto artificial skin has not been proven effective (Sheridan and Tompkins, 2007a). High cost is a disadvantage of using both applications.
Nursing Care Management
![]() Nursing care of the pediatric burn patient represents a challenge to the nurse’s knowledge of anatomy and physiology, the behavioral sciences, and pathophysiology. Patient outcome after thermal injury is the result of the collaboration of a professional multidisciplinary team using a family-centered care approach. In addition to providing nursing care, the nurse coordinates the efforts of a multidisciplinary burn team (Henry and Foster, 2000).
Nursing care of the pediatric burn patient represents a challenge to the nurse’s knowledge of anatomy and physiology, the behavioral sciences, and pathophysiology. Patient outcome after thermal injury is the result of the collaboration of a professional multidisciplinary team using a family-centered care approach. In addition to providing nursing care, the nurse coordinates the efforts of a multidisciplinary burn team (Henry and Foster, 2000).
![]() Nursing Care Plan—The Child with Burns
Nursing Care Plan—The Child with Burns
Because the care of burned children encompasses such a broad range of skills and foci, it has been divided into segments that correspond with the major phases of burn treatment. The acute phase, also referred to as the emergent or resuscitative phase, involves the first 24 to 48 hours. The management phase extends from the completion of adequate resuscitation through wound coverage. The rehabilitative phase begins once the majority of the wounds have healed and rehabilitation becomes the predominant focus of the care plan. This phase continues until all reconstructive procedures and corrective measures have been accomplished and often extends over a period of months or years.
Acute Phase
The primary emphasis during the emergent phase is the treatment of burn shock and management of pulmonary status. Monitoring vital signs, output, fluid infusion, and respiratory parameters are ongoing activities in the hours immediately after injury. IV infusion begins immediately and is regulated to maintain a urinary output of at least 1 to 2 ml/kg in children weighing less than 30 kg (66 lb). Expect an output of 30 to 50 ml/hr in children weighing more than 30 kg. Urinary output and specific gravity, vital signs, laboratory data, and objective signs of adequate hydration guide the rate of fluid administration.
The nurse observes patients for changes in all parameters. They require constant observation and assessment, with special attention given to signs of respiratory, cardiac, and renal complications. Alterations in electrolyte balance can produce clinical symptoms of confusion, weakness, cardiac irregularities, and seizures. Changes in respiratory function and gas exchange are reflected clinically by restlessness, irritability, increased work of breathing, and alterations in blood gas values. The loss of the skin’s protective function exposes burned children to an increased risk of hypothermia.
Care of the burn wound is secondary to the more critical problems of respiratory and cardiac failure. When transfer to a special burn care facility is anticipated, it is important to cover the wounds with clean sheets and wrap the child in blankets to maintain body temperature during transfer. The burn wound can be evaluated and dressed after arrival at the burn center. If no burn unit is available, the wound is cleansed and dressed in the emergency department. Many burn units maintain a pictorial record of the wound to record progress and for legal purposes, especially in cases of suspected child maltreatment. The burn wound is treated according to the protocol of the specific burn facility. The burn team implements infection control procedures and ensures that staff and visitors comply with established protocols to prevent cross-contamination in the burn unit.
Throughout the acute phase of care, do not overlook the psychosocial needs of the children and their families. The child is frightened, uncomfortable, and often confused. Children may be isolated from familiar persons and surroundings, and the often overwhelming physical needs at this time are the primary focus of the staff and parents. In addition to feeling concern for their child, the parents experience guilt, which is related to the fact they did not or could not protect their child. Consistency in the information presented and the attitude of the staff creates a sense of familiarity and stability during the emergent phase.
Management and Rehabilitative Phases
After the patient’s condition is stabilized, the management phase begins. The multidisciplinary team concentrates on preventing wound infections, closing the wound as quickly as possible, and managing the numerous complications that may occur. Although the rehabilitative phase begins when permanent wound closure has been achieved, rehabilitation issues are identified on admission and are included in the care plan throughout the hospital course (see Nursing Care Plan).
The management phase of burn care involves intensive nursing care, which is often difficult for the patient, family, and nursing staff. Except for minor burn injuries, care should take place in a burn unit and involve a variety of disciplines, such as physical therapy, nutrition, social services, and respiratory care.
Comfort Management: The severe pain of the wound and resultant therapies, the anxiety generated by these experiences, sleep deprivation, itching related to wound healing, and the conscious and unconscious interpretations of traumatic events contribute to the psychologic reactions and behaviors commonly observed in children with burns. It is important to assess the individual experiences and needs of the burn-injured child. A common myth in pediatrics is that children do not feel pain as intensely as adults do. What may be more accurate is that children do not always express their pain in the same way as adults. Children may display pain through behaviors of fear, anxiety, agitation, anger, aggression, tantrums, depression, withdrawal, and regression.
How the child’s experience of pain from the burn injury and anxiety from the hospitalization are managed has lasting psychologic effects. A careful nursing history that includes the child’s past experiences with pain and ways that caregivers successfully handled those events may provide clues to the control of current pain. Caregiver involvement is especially important for a child (Lee and Herndon, 2007). Interventions may include medications (including IV morphine and short-term anesthetics such as propofol or ketamine), relaxation techniques, distraction therapy, cutaneous stimulation by touching, and family participation. Nonpharmacologic therapies may be used as adjuncts in the treatment of pain. In young children, distraction and imagery work well (Kahana, 2003; Henry and Foster, 2000).
To reduce the anxiety associated with an unfamiliar environment and frightening treatments, it is important to offer thorough, age-appropriate explanations to the child before procedures. Compounding the pain is the child’s interpretation of it and of the procedure; this is closely related to the child’s developmental level. Children often feel anger, guilt, and depression; as in all illnesses, they may also exhibit regressive behavior. When children appear to accept pain with little or no response, psychologic consultation is in order.
Care of the Burn Wound: The nurse has a major responsibility for cleansing, débriding, and applying topical medications and dressings to the burn wound. Because dressing removal is a painful procedure, children should receive adequate analgesia before the scheduled dressing change. The nurse should administer medication so that the drug’s peak effect coincides with the procedure. Children who have an understanding of the procedure to be performed and some perceived control demonstrate less maladaptive behavior. Children respond well to participating in decisions and the actual procedure as their condition allows.
With some children, nonpharmacologic interventions are effective means of coping with pain. Distraction therapy, deep breathing, and relaxation techniques may facilitate the procedure. Most children also benefit from parental participation. Medical play is often effective in helping the younger child gain some mastery over the procedure. Incorporate those techniques that work best for the individual patient into the care plan and consistently implement them during the dressing change procedure.
Outer dressings are removed; any dressings that have adhered to the wound are easier to remove by applying tepid water. Loose or easily detached tissue is also débrided during the cleansing process. Encourage children to participate in dressing removal. Giving them something constructive to do helps them focus on something other than the procedure. In dressing the wound, it is important that all areas be clean, that medication be amply applied, and that no two burned surfaces touch each other (e.g., fingers or toes, or ears touching the side of the head). If touching, the burned surfaces will heal together, causing deformity or dysfunction.
Topical medications are applied directly to the wound with a clean gloved hand or impregnated into fine-mesh gauze before application. Then apply dressings to assist in exudate absorption, wound débridement, and increased patient comfort. All dressings applied circumferentially should be wrapped in a distal-to-proximal manner. Apply the dressing with sufficient tension to remain in place without impairing circulation or limiting motion. A stable dressing is especially important when the child is ambulatory.
Burns that involve the eyelids require special care to prevent corneal ulceration. No solution other than saline should come in contact with the eyes during the cleansing process. Avoid vigorous débridement in this area of thin, delicate tissue. Assess the patient throughout the healing process for the ability to close the eyes. Inability to close the eyes because of contracture formation, administration of paralytic agents, or corneal burns requires instilling ophthalmic ointment and covering the eyes with a patch to prevent further corneal damage (Achauer and Adair, 2000).
Universal Precautions, including the use of protective garb and barrier techniques, should be followed when caring for all patients with thermal injuries. Frequent hand and forearm washing is the single most important element of the infection control program. Implement strict policies for cleaning the environment and patient care equipment to minimize the risk of cross-contamination. All visitors and members of other departments should be oriented to the infection control policies, including the importance of hand and forearm washing and use of protective garb. Screen all visitors for infection and contagious diseases before patient contact.
Nutrition: Oral feedings are common unless the child is intubated or paralytic ileus persists. Because children often lack an appetite, the nursing staff must provide a great deal of encouragement, help, and patience. Consultation between the parents and dietitian helps determine food preferences. Include children who are old enough to participate in meal planning.
Nourishing snacks are provided between scheduled meals. Painful procedures should not be scheduled around meals; most children are too physically exhausted and emotionally upset to eat at this time. Many children eat better in an atmosphere more nearly like what they are accustomed to at home. When their condition allows, children enjoy sitting at a table for meals and interacting with other children.
Children who require enteral supplementation by tube feeding must be monitored on an ongoing basis for intolerance and tube malposition. The nurse should monitor and record any indications of abdominal distention, diarrhea, or electrolyte and metabolic derangement. Accurate documentation of oral, parenteral, and enteral nutritional intake is essential to evaluate the adequacy of nutritional support.
Prevention of Complications: Acute Care: The maintenance of body temperature is important to the child with burns. Reduction of heat loss is imperative to decrease energy demands and evaporative water loss. Ambient temperatures and humidity should be maintained at 28° to 33° C (82.4° to 91.4° F) and 80%, respectively, to control heat loss (Lee and Herndon, 2007). Large areas of the body should not be exposed simultaneously during dressing changes. Warmed solutions, linens, occlusive dressings, heat shields, a radiant warmer, and warming blankets assist in preventing hypothermia. The optimum environment for the child with burns can be uncomfortable for persons attending the child.
The chief danger during acute care is infection—wound infection, generalized sepsis, or bacterial pneumonia. The burn wound should be assessed for changes indicative of wound infection, which include conversion of a partial-thickness to a full-thickness burn injury, early eschar separation, subeschar hemorrhage, degeneration of granulation tissue, discoloration of unburned skin at the wound margins, or green discoloration of subcutaneous fat (indicative of Pseudomonas and other gram-negative organisms). In addition to the signs of developing wound infection, the child with systemic sepsis may have a core temperature of more than 38.5° C (101.3° F) or less than 36° C (96.8° F), tachycardia, tachypnea, and leukocytosis or leukopenia. Tachycardia and tachypnea are common presenting symptoms in many pediatric diseases. Children with septic shock often maintain a normal BP until they are severely ill. Shock may occur long before hypotension in children. It is a sign of late and decompensated shock. Meticulous assessment should include signs of decreased perfusion (including decreased peripheral pulses), altered alertness, prolonged capillary refill (2 seconds), mottled or cool extremities, or decreased urinary output (Goldstein, Giroir, and Randolph, 2005).
Children are reluctant to move when doing so causes pain, and they are likely to assume a position of comfort. Unfortunately, the most comfortable position is often one that encourages the formation of contractures and loss of function. Ongoing efforts to prevent contractures include the positioning and splinting of involved extremities in extension, active and passive physical therapy, and the encouragement of spontaneous movement when feasible. In addition to maintenance of proper body alignment, frequent position changes are important to improve bronchopulmonary hygiene and capillary perfusion to common pressure areas. Low–air loss beds are beneficial for the morbidly obese or for children with posterior grafts. Areas of particular concern for pressure area development in the pediatric population are the posterior scalp, heels, and areas exposed to mechanical irritation from splints and dressings.
Prevention of Complications: Long-Term Care: The rehabilitative phase of care begins once wound coverage has been achieved. Scar formation becomes a major problem as burn wounds heal (Fig. 29-17). The scar tissue is metabolically active and highly vascular; collagen is deposited in an undefined pattern. Contractile properties of the scar tissue can result in disabling contractures, deformity, and disfigurement. As long as the scar is raised, red, and firm, it is considered active (Fig. 29-18). Hypertrophic scarring typically reaches a peak approximately 4 to 6 months after wound healing, and most scars mature or become inactive in 1 to 2 years. The mature scar is characterized by pigmented color, flattening, and increased suppleness of the tissue (Fig. 29-19).

Fig. 29-17 Extensive scars from flame burn. (Courtesy CR Boeckman Regional Burn Center, Akron, Ohio.)
Uniform pressure applied to the scar decreases the blood supply and forces the collagen into a more normal alignment. When pressure is removed, blood supply to the scar is immediately increased; therefore periods without pressure should be brief to avoid nourishment of the hypertrophic tissue. Continuous pressure to areas of scarring can be achieved by elastic bandages or commercially available pressure garments. Because these custom-made garments are often worn for months, revision may be required as the child grows. It is much easier to prevent scarring and contracture of the wound than to resolve an existing problem. Splints and appliances may also be necessary until wound maturation occurs (Fig. 29-20). Part of outpatient and home care often includes the continuation of regular physical therapy (Fig. 29-21).

Fig. 29-21 Daily physical therapy to prevent contracture deformity is continued at home or in an outpatient setting. Note how nurse encourages child to imitate her facial action. (Courtesy CR Boeckman Regional Burn Center, Akron, Ohio.)
Scar tissue has certain significant properties, particularly for growing children. Intense itching occurs in healing burn wounds and scar tissue until the scar is no longer active. Itching is usually treated with hydroxyzine (Atarax) or diphenhydramine and frequent applications of a moisturizer, such as Eucerin, cocoa butter, or Nivea. Massage therapy during the application of moisturizers is also beneficial to stretch scar tissue and help prevent contracture. Scar tissue has no sweat glands, and children with extensive scarring may experience difficulty during hot weather. Alert caregivers to this possibility and make sure they are prepared to institute alternate methods of cooling when necessary.
Scar tissue does not grow and expand like normal tissue, which may create difficulties, especially in functional areas such as the hands and over joints. Additional surgery is sometimes required to allow independent functioning in daily activities, to improve cosmetic appearance, or to restore anatomic integrity. Reconstructive surgery employs various techniques, including local or distant flaps, full- or partial-thickness grafts, tissue expanders, or pedicle flaps.
The nursing activities in the rehabilitative phase of treatment focus on the child’s and family’s adaptation to the burn injury and their ability to reintegrate into the community. The multidisciplinary team approach remains the model for support of the child and family (Fig. 29-22).
The psychologic pain and impact of severe burn injury are as intense as the physical trauma. The impact of severe burns taxes the capabilities at all ages. Very young children, who suffer acutely from separation anxiety, and adolescents, who are developing an identity, are probably the most affected psychologically. Toddlers cannot understand why the parents they love and who have protected them can leave them in such a frightening and unfamiliar place. Adolescents, in the process of achieving independence from the family, find themselves in a dependent role with a damaged body. Being different from others at a time when conformity with peers is so important is difficult to accept.
Anticipation of the return to school can be overwhelming and frightening. It is essential that health care professionals recognize the importance of preparing teachers and classmates for the child’s return. Provide teachers with information to assist the child and family and to promote the child’s optimum adjustment. Hospital-sponsored school reentry programs use a variety of methods to provide education and information about the implications of the injury, the garments and appliances, and the need for support and acceptance. Telephone calls, videotapes, information packets, and visits by members of the health care team offer opportunities to help with reintegration into the school environment—a focal point of the child’s life.
Psychosocial Support of the Child: Children should begin early to do as much for themselves as possible and to be active participants in their care. Loss of control and perceived helplessness may result in acting-out behaviors. Nurses should be sensitive to these feelings and allow the child the opportunity for choices and decision making as the condition allows. At the same time, it is important to set boundaries and establish a daily schedule to provide a sense of predictability, security, and control. During illness, children regress to a previous developmental level that allows them to deal with stress. As children begin to participate in their care, they gain in confidence and self-esteem. Fears and anxieties diminish with accomplishment and self-confidence. If the child demonstrates nonadherence in the rehabilitative phase, initiate a behavior modification program to promote or reward the child’s accomplishment in care.
Select and encourage activities on the basis of each child’s developmental level and interest. Quiet activities such as reading, coloring, and games are always appropriate. Critically ill children enjoy tapes and stories, even though they may not be able to actively participate in play. Television is a satisfactory diversion but should not replace contact with others. Play that encourages the expression of anger, frustration, and guilt is especially therapeutic. Medical play is a valuable tool to teach children what to expect and their role in the treatment process. School-age children benefit by continuing study activities as they are able.
Children need to feel they look nice. The burns, dressings, and medical equipment do little to foster a positive self-image. Small things, such as careful hair combing, a bright ribbon or pajamas, a pretty blanket, or colorful stickers will help them feel better about themselves and feel worthwhile to others.
Children need to know that their injury and the treatments are not punishment for real or imagined transgressions and that the nurse understands their fear, anger, and discomfort. They also need body contact. This is often difficult to arrange for the child with massive burns; stroking areas of unburned skin is comforting. Even older children enjoy sitting on the nurse’s or parent’s lap and being cuddled and hugged. This can be a reward or a comfort in times of stress, but most of all it is a natural part of childhood.
Psychosocial Support of the Family: There is a growing recognition that trauma affects not only the victim but also those closest to the child. Severe trauma challenges the belief that the world is safe and predictable. Parents and other family members are concerned about the child’s survival, recovery, and future potential. Recognizing and respecting each family’s strengths, differences, and methods of coping allows the nurse to respond to their unique needs by implementing a family-centered approach to care. It is the family, particularly the parents, who are the most significant persons in the child’s life.
As in any emergency situation, all attention is focused on the child, and the parents feel powerless and ineffectual. Most parents feel overwhelming guilt, whether or not the guilt is justified. They feel responsible for the injury. These feelings may have a negative effect on the child’s rehabilitation. For example, parents may indulge the child and allow poor behavior that affects physical and emotional recovery.
Nurses have the opportunity to assist parents in coping with the stresses of the child’s illness and with their own feelings of guilt and helplessness. The parents need to be informed of the child’s progress and assisted in coping with their feelings while providing support to their child. The nurse can help them understand that it is not selfish to look after themselves and their own needs to better meet the needs of their child. Definitive professional help may be needed for parents whose response to the injury is severe or whose response to stress is manifested in destructive behavior.
The parents are members of the multidisciplinary team and participate in the development of the care plan. It is important to address their input to consider all aspects of the physical, emotional, social, and cultural factors affecting the child and family and to establish a realistic home therapy program. The family’s willingness to assume responsibility for care and their ability to implement the therapeutic regimen are assessed. Explore home, school, and other environmental factors with the family, as well as financial concerns and available community resources. The nurse can then develop a specific care plan, with an anticipated follow-up program.
Caring for the Caregiver: Burn care is a complex and demanding specialty. Nurses who choose this field reap many rewards and endure many stresses. Ongoing support from peers, the multidisciplinary team, and nursing management is important to assist burn nurses in caring for themselves so they can continue to render high-quality care to their patients.
Prevention of Burn Injury
Burn prevention is the responsibility of all members of the community. Nurses have an obligation to participate in educational efforts directed at parents, children, and others regarding the prevention of burn injuries and fire-related deaths. The best cure is prevention.
Infants and toddlers are most commonly injured by hot liquids in the kitchen and bathroom. These injuries often occur as a result of inadequate supervision of this curious and energetic age-group. Target prevention efforts at parents and other caregivers; education includes the importance of adequate supervision and the establishment of safe play areas in the home. Hot liquids should be kept out of reach; tablecloths and dangling appliance cords are often pulled by toddlers, spilling hot grease and liquids on them. Electrical cords and outlets represent a potential risk to small children, who may chew on accessible cords and insert objects into outlets.
Since 1974, the Consumer Product Safety Commission has recommended a reduction of hot water heater thermostats to a maximum of 49° C (120° F). This recommendation has been supported by utility companies, burn treatment centers, medical personnel, and others interested in public safety. However, many hot water heaters remain set at levels well above the safe level. Small children are especially at risk for scald injuries from hot tap water because of their decreased reaction time and agility, their curiosity, and the thermal sensitivity of their skin (Fig. 29-23). Educate caregivers about never leaving a child in a bath without adult supervision. Caregiver should also test the water before placing a child in the tub or shower.
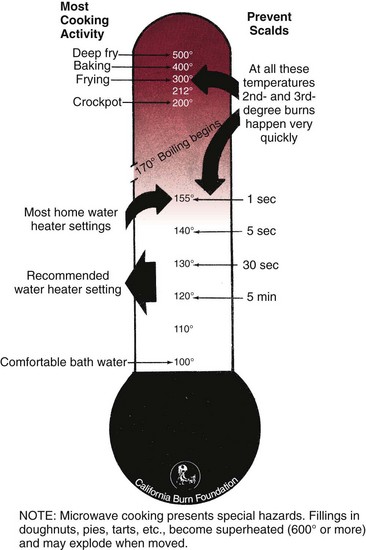
Fig. 29-23 Temperatures associated with common burn injuries in the home. All temperatures given in Fahrenheit. note: Most authorities recommend that water heaters be kept at the lowest safe setting of 120° F (49° C). (Courtesy California Burn Foundation, Canoga Park, Calif.)
Microwave ovens, although perceived by many as safer than conventional ovens and stoves, heat foods and liquids to high temperatures that can result in burns from spills, splashes, and the release of steam (Box 29-17).
As children mature, risk-taking behaviors increase. Matches and lighters are dangerous in the hands of the young. In 2006 alone, an estimated 14,500 structural fires were reported to U.S. fire departments as a result of children playing with fire (National Fire Protection Association, 2009). Adults must remember to keep potentially hazardous items out of the reach of children; a lighter, like a match, is a tool for adult use.
Education related to fire safety and survival should begin with the very young. They can practice “stop, drop, and roll” to extinguish a fire and the fire escape route, including a safe meeting place away from the home in case of fire. Materials such as coloring books are available from many fire departments and burn foundations. Community burn prevention programs also provide opportunities to educate children and parents about fire, burn hazards, and prevention behaviors.
Community activities are helpful in the effort to support burn survivors and prevent burns. The Aluminum Cans for Burned Children (ACBC) is an exemplary effort based in the Paul and Carol David Foundation Burn Institute, Akron, Ohio. Activities funded by ACBC include Burn Survivors Support Group, Burn Camp, and meetings of Juvenile Firestoppers (for children with fire-setting behavior). Adult weekend retreats and school and family education sessions are a part of this program. Burn center staff and fire department staff present the programs.
Additional information on burn care and prevention can be obtained from the American Burn Association* and the National Safety Council.† The Alisa Ann Ruch Burn Foundation provides assistance to burn victims and burn centers. The Shriners Burn Institutes‡ are staffed to treat pediatric patients after acute burn injuries and those requiring rehabilitative and reconstructive services as a result of scarring and functional impairment. Nurses can also obtain information from local Shrine Temples and Clubs, from Shriners Hospitals, or from the Shriners International Headquarters.§ The Alisa Ann Ruch Burn Foundation and Shriners Hospitals for Crippled Children support research to improve burn care and treatment and promote public education in burn prevention.
Future Research Needs
Many advances in burn prevention have reduced the occurrence of burn injury. Early excision and grafting of the burn wound, with control of infection, have improved survival rates for burn injury. Areas for future research include the rate of wound healing, characteristics of the healed wound, support techniques for inhalation injury, the effect of hypothermia immediately after burn injury, nursing interventions that promote healing of donor sites and skin grafts, and the most effective wound-cleansing protocol. Evidence for improvement of burn nursing care is best organized with research findings (Carrougher, 1998). Evidence-based practice integrates nurse’s clinical expertise with the best methods. It helps structure how to make accurate and timely decisions for care of the patient (Gordon and Marvin, 2007).
Key Points
• GI disorders of childhood that commonly cause fluid depletion and electrolyte disturbance are diarrhea and vomiting.
• The four general mechanisms of diarrhea are secretory, cytotoxic, osmotic, and dysenteric diarrhea.
• The treatment for acute diarrhea consists primarily of oral rehydration and provision of an adequate diet.
• Burns are caused by thermal, electrical, chemical, or radioactive agents.
• The severity of burn injury is assessed on the basis of the percentage of TBSA burned, depth, location, age, etiologic agent, concomitant injuries, and general health.
• Emergency measures for severe burns include stopping the burning process; assessing for airway, breathing, and circulation; covering the burn; transporting the child to the hospital; and providing reassurance to the child and family.
• Management of minor burns consists of facilitating wound healing, relieving pain and discomfort, and preventing complications.
• Management of major burn injuries involves facilitating wound healing, relieving pain and discomfort, replacing destroyed skin, preventing or treating complications, and providing rehabilitation.
• Active participation by the child and family is important in the care of the child with burn trauma.
Answers to Critical Thinking Exercise
1. Yes, there are sufficient data for the nurse practitioner to arrive at some conclusions.
2. a. See Table 28-3, p. 1059, Evaluating Extent of Dehydration, and note the criteria for mild dehydration.
b Infants and children with mild dehydration are managed with oral rehydration therapy and early reintroduction of an adequate diet. In cases of severe dehydration, or when infants and children have uncontrollable vomiting, intravenous fluids are used in the management of acute diarrhea.
c Breast-feeding generally can be continued in mild dehydration.
d Antidiarrheal medications are not recommended for the treatment of acute infectious diarrhea. These medications have adverse effects such as slowed motility and can prolong the illness.
3. At present, Mary meets all the criteria for mild dehydration. It is highly probable that she has acute infectious diarrhea because her mother noted that she has had a “cold” for several days and she is vomiting, has diarrhea, and has an elevated temperature. The priority for nursing care at this time is to provide rehydration via an oral rehydration solution (ORS). ORS is an effective, safe, and cost-effective way to treat mild dehydration. The nurse practitioner should instruct the mother to give Mary ORS at frequent intervals and in small amounts. The mother should also be instructed to continue with breast-feeding and normal feedings. Early reintroduction of normal nutrients is desirable in cases of mild dehydration; delayed introduction of food may be harmful and can prolong the illness. Mary’s mother should also be told to avoid the use of antidiarrheal medications.
4. Yes, the evidence supports this initial plan of management.
References
Achauer, BM, Adair, SR. Acute and reconstructive management of the burned eyelid. Clin Plast Surg. 2000;27(1):87–96.
Acker, ME. Vomiting in children. Adv Nurse Pract. 2002;10(1):51–56. [68].
American Burn Association, Guidelines for the operation of burn centers. Chicago: The Association; 2006. available at www.ameriburn.org/Chapter14.pdf [accessed March 11, 2010].
Andrews, DA. Management of the burned child. Prob Gen Surg. 1994;11(4):662–665.
Arnal, LE, Stein, F. Pediatric septic shock: why has mortality decreased? The utility of goal-directed therapy. Semin Pediatr Infect Dis. 2003;14(2):165–172.
Barrow, RE, Herndon, DN. History of the treatment of burns. In: Herndon DN, ed. Total burn care. Philadelphia: Saunders, 2007.
Beierle, EA, Chung, DH. Surgical management of complications of burn injury. In: Herndon DN, ed. Total burn care. Philadelphia: Saunders, 2007.
Bessey, PQ. Wound care. In: Herndon DN, ed. Total burn care. Philadelphia: Saunders, 2007.
Bohlke, K, Davis, RL, DeStefano, F, et al. Epidemiology of anaphylaxis among children and adolescents enrolled in a health maintenance organization. J Allergy Clin Immunol. 2004;113(3):536–542.
Brierley, J, Choong, K, Cornell, T, et al. 2007 American College of Critical Care Medicine clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock. Crit Care Med. Nov 28, 2008. [(Epub)].
Bullard, J, Page, NE. Cyclic vomiting syndrome: a disease in disguise. Pediatr Nurs. 2005;31(1):27–29.
Carrougher, G. Burn care and therapy. St Louis: Mosby; 1998.
Centers for Disease Control and Prevention. Delayed onset and diminished magnitude of rotavirus activity—United States, November 2007–May 2008. MMWR. 2008;57(25):697–700.
Centers for Disease Control and Prevention. Managing acute gastroenteritis among children: oral rehydration, maintenance, and nutritional therapy. MMWR. 2003;52(RR-16):1–16.
Chuang, YY, Huang, YC, Lin, TY. Toxic shock syndrome in children: epidemiology, pathogenesis, and management (review). Paediatr Drugs. 2005;7(1):11–25.
Coffin, SE. Future vaccines: recent advances and future prospects. Primary Care. 2001;28(4):869–887.
Committee on Infectious Diseases. Prevention of rotavirus disease: guidelines for use of rotavirus vaccine. Pediatrics. 2007;119(1):171–182.
Dellinger, RP, Levy, MM, Carlet, JM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36(1):296–327.
Demling, RH. The role of anabolic hormones for wound healing in catabolic states. J Burns Wounds. 2005;4:e2.
Goldstein, B, Giroir, B, Randolph, A. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005;6(1):2–8.
Gordon, M, Marvin, J. Burn nursing. In: Herndon DN, ed. Total burn care. Philadelphia: Saunders, 2007.
Hartford, CE, Kealey, GP. Care of outpatient burns. In: Herndon DN, ed. Total burn care. Philadelphia: Saunders, 2007.
Helvig, E. Pediatric burn injuries. AACN Clin Issues. 1993;4(2):433–442.
Henry, DB, Foster, RL. Burn pain management in children. Pediatr Clin North Am. 2000;47(3):681–698.
Jabbar, A, Wright, RA. Gastroenteritis and antibiotic-associated diarrhea. Primary Care. 2003;30(1):63–80.
Jindal, N, Hollenberg, SM, Dellinger, RP. Pharmacologic issues in the management of septic shock. Crit Care Clin. 2000;16(2):233–249.
Kahana, MD. Burn pain management: avoiding the “private nightmare.”. In: Schechter N, Berde C, Yaster M, eds. Pain in infants, children, and adolescents. Baltimore: Williams & Wilkins, 2003.
Klein, GL, Przkora, R, Herndon, DN. Vitamin and trace element homeostasis following severe burn injury. In: Herndon DN, ed. Total burn care. Philadelphia: Saunders, 2007.
Kramer, GC, Lund, T, Beckman, OK. Pathophysiology of burn shock and burn edema. In: Herndon DN, ed. Total burn care. Philadelphia: Saunders, 2007.
Lee, JO, Herndon, DN. The pediatric burned patient. In: Herndon DN, ed. Total burn care. Philadelphia: Saunders, 2007.
Li, ST, DiGiuseppe, DL, Christakis, DA. Antiemetic use for acute gastroenteritis in children. Arch Pediatr Adolesc Med. 2003;157(5):475–479.
Liberman, DB, Teach, SJ. Management of anaphylaxis in children. Pediatr Emerg Care. 2008;24(12):867–869.
Maar, SP. Emergency care in pediatric septic shock. Pediatr Emerg Care. 2004;20(9):617–624.
Malek, MA, Curns, AT, Holman, RC, et al. Diarrhea- and rotavirus-associated hospitalizations among children less than 5 years of age: United States, 1997 and 2000. Pediatrics. 2006;117(6):1887–1892.
McRonald, FE, Fleisher, DR. Anticipatory nausea in cyclical vomiting. BMC Pediatr. 2005;5(1):3.
Meyer, WJ, Patterson, DR, Jaco, M, et al. Management of pain and other discomforts in burned patients. In: Herndon DN, ed. Total burn care. Philadelphia: Saunders, 2007.
Murphey, ED, Sherwood, ER, Toliver-Kinsky, T. The immunological response and strategies for intervention. In: Herndon DN, ed. Total burn care. Philadelphia: Saunders, 2007.
Nakase, J. Update on emerging infections from the Centers for Disease Control and Prevention. Ann Emerg Med. 2000;36(3):268–270.
National Fire Protection Association. Children playing with fire. available at www.nfpa.org/categoryList.asp?categoryID=281&URL=Research%20&%Reports/Fact%20sheets/Children%20and%20fire, 2009. [(accessed March 11, 2010)].
Norbury, WB, Herndon, DN. Modulation of the hypermetabolic response after burn. In: Herndon DN, ed. Total burn care. Philadelphia: Saunders, 2007.
Pham, TN, Gibran, NS, Heimbach, DM. Evaluation of the burn wound: management decisions. In: Herndon DN, ed. Total burn care. Philadelphia: Saunders, 2007.
Pruitt, BA, Wolf, SE, Mason, AD. Epidemiological, demographic, and outcome characteristics of burn injury. In: Herndon DN, ed. Total burn care. Philadelphia: Saunders, 2007.
Ralston M, Hazinski MF, Zaritsky AL, et al, eds. Pediatric life support. Dallas: American Heart Association, 2006.
Robert, R, Blakeney, P, Herndon, DN. Maltreatment by burning. In: Herndon DN, ed. Total burn care. Philadelphia: Saunders, 2007.
Safe Kids Worldwide, Fire safety. Washington, DC: The Company; 2009. available at www.usa.safekids.org [accessed March 11, 2010].
Safe Kids Worldwide. Report to the nation: trends in unintentional childhood injury mortality and parental views on child safety. Washington DC: National Safe Kids Campaign; 2008.
Saffle, JR, Graves, C. Nutritional support of the burned patient. In: Herndon DN, ed. Total burn care. Philadelphia: Saunders, 2007.
Selbst, SM. Sedation and analgesia in the ER department. In: Schechter N, Berde C, Yaster M, eds. Pain in infants, children, and adolescents. Baltimore: Williams & Wilkins, 2003.
Sheridan, RL, Tompkins, RG. Alternative wound coverings. In: Herndon DN, ed. Total burn care. Philadelphia: Saunders, 2007.
Sheridan, RL, Tompkins, RG. Etiology and prevention of multisystem organ failure. In: Herndon DN, ed. Total burn care. Philadelphia: Saunders, 2007.
Sherwood, ER, Traber, DL. The systemic inflammatory response syndrome. In: Herndon DN, ed. Total burn care. Philadelphia: Saunders, 2007.
Smith, ML. Pediatric burns: management of thermal, electrical, and chemical burns and burn-like dermatologic conditions. Pediatr Ann. 2000;29(6):367–378.
Staat, MA. What is the disease burden associated with rotavirus? In: The management and prevention of rotavirus. Thorofare, NJ: Vindico Medical Education; 2006.
Suman, OE, Przkora, R, Blakeney, P, et al. Mitigation of the burn-induced hypermetabolic response during convalescence. In: Herndon DN, ed. Total burn care. Philadelphia: Saunders, 2007.
Szajewska, H, Ruszcynski, M, Radzikowski, A. Probiotics in the prevention of antibiotic-associated diarrhea in children: a meta-analysis of randomized controlled trials. J Pediatr. 2006;149(3):367–372.
Thomas, CR, Meyer, WJ, Blakeney, PE. Psychiatric disorders associated with burn injury. In: Herndon DN, ed. Total burn care. Philadelphia: Saunders, 2007.
Warden, GD. Fluid resuscitation and early management. In: Herndon DN, ed. Total burn care. Philadelphia: Saunders, 2007.
Warden, GD. Burn shock resuscitation. World J Surg. 1992;1(1):16–32.
Zangwill, KM. Protecting against rotavirus disease and its complications. In: The management and prevention of rotavirus. Thorofare, NJ: Vindico Medical Education; 2006.
*625 North Michigan Ave., Suite 2550, Chicago, IL 60611; 312-642-9260; fax: 312-642-9130; e-mail: info@ameriburn.org; www.ameriburn.org.
†1121 Spring Lake Drive, Itasca, IL 60143-3201; 630-285-1121, e-mail: info@nsc.org; www.nsc.org.
‡2501 W. Burbank Blvd., Suite 201, Burbank, CA 91505; 800-242-BURN; www.aarbf.org.
§2900 Rocky Point Drive, Tampa, FL 33607; Shriners International Headquarters website: www.shrinershq.org; Shriners Hospitals for Children website: www.shriners.com/Hospitals/_Hospitals_for_Children.
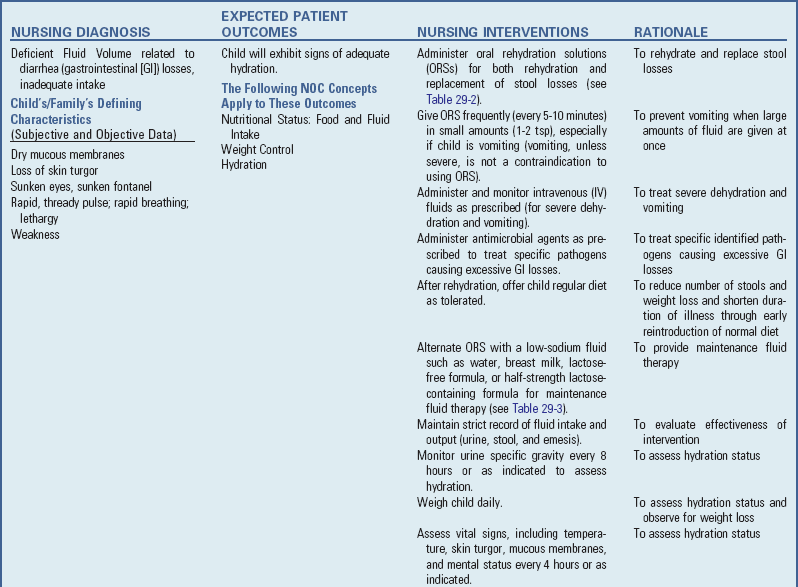
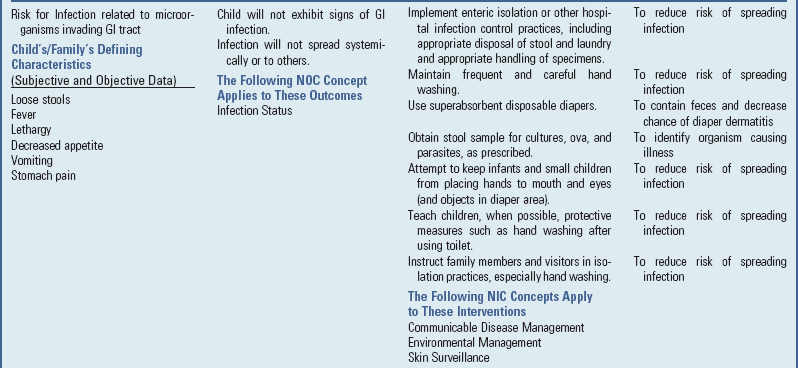
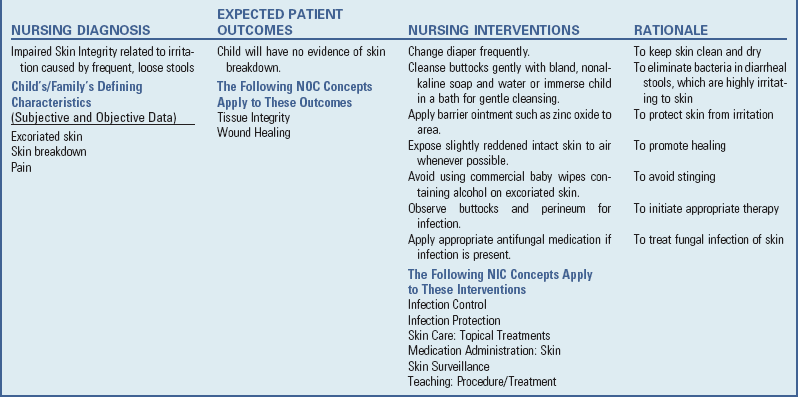
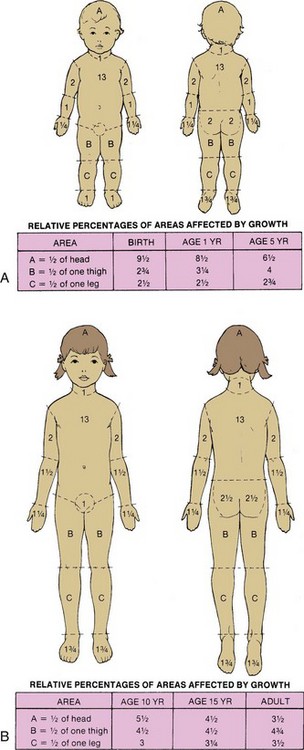




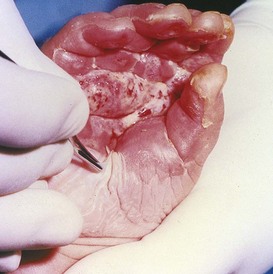

 to 9 times the area of the sheet graft (see
to 9 times the area of the sheet graft (see