Chapter 108The North American Standardbred
Description of the Sport
The Standardbred (STB) was developed as a racing breed by registering any horse that could trot or pace 1 mile in a set time, called the standard. An early standard was 2:30 (2 minutes, 30 seconds, 0 fifths). Early STBs were diverse because they were different types with a large genetic pool. Crossing many types resulted in a strong, rugged breed that lacked refinement of the head, ears, and bone structure. Trotters were large and coarse, whereas pacers were smaller and more refined. The breed has progressed rapidly by selective breeding in the past 4 decades. Although trotters and pacers now are bred separately, the physical appearance has become more alike, and both lines have a racy appearance similar to Thoroughbreds (TBs). Early trotters were farm or buggy horses, selected for good disposition and durability, traits that are still characteristic. Early STBs were raced several 1-mile races in the same day, called heats, a part of the sport demanding stamina and gameness.
A TB stallion, Messenger, imported from England in 1788, was prominent in the formative period of the STB. Many of his offspring had a natural inclination to trot. In 1849, a descendent of Messenger sired Hambletonian 10, the foundation sire of the STB breed. The breed developed in the northeastern United States, where it was influenced by the Hackney and Morgan breeds and local mixed-breed horses.
The STB races at two different gaits: the trot, a diagonal two-beat gait in which the left forelimb (LF) and right hindlimb (RH) move together, and the pace, a lateral two-beat gait in which the LF and left hindlimb (LH) move together. High knee action and a lateral (left to right) nodding of the head are typical of a trotter (Figure 108-1, A). A trotter travels straight ahead (see Figure 108-1, A) (Figures 108-2, A, and 108-3), but a pacer sways from side to side while moving forward (see Figure 108-1, B).

Fig. 108-1 A, Muscle Hill, a champion 3-year-old trotting colt of 2009, is seen here with driver Brian Sears. This talented young trotter equaled the all-age trotting world record of 150.1 in his overwhelming victory in the Hambletonian, raced at the Meadowlands racetrack outside of New York City. B, Paul MacDonell guides Somebeachsomewhere, a champion 3-year-old pacing colt in 2008. Somebeachsomewhere equaled the all-age pacing world record with his 146.4 performance at the Red Mile in Lexington, KY.
(Courtesy United States Trotting Association, Columbus, Ohio, United States.)
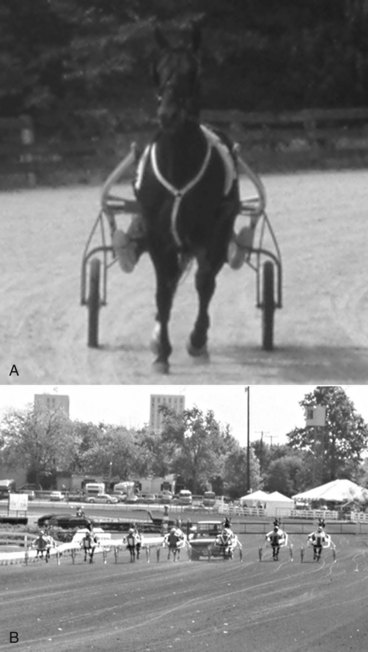
Fig. 108-2 A, A young trotter is on the left shaft coming out of a turn on a small farm track. On this track a horse has to negotiate four turns to train 1 mile. B, Horses approach the start of a race at the Red Mile, Lexington, Kentucky, a track that is 1 mile long. Compared with the turn in A, the turn on this track is substantially larger, and horses must negotiate only two turns for a 1-mile race.

Fig. 108-3 This trotter is on the left line and the right shaft in the straightaway. The horse’s head is turned to the left because the driver (Rich Ringler) has to pull harder on the left rein to keep the horse going straight. The horse’s hindquarters are closer to the right shaft. This combination of left line and right shaft would be consistent with left hindlimb lameness.
Fifty years ago trainers had to spend several months determining at which gait a STB was more talented; some could not handle speed at either gait. As late as the 1970s and 1980s, it was not unusual for a horse to race one season at one gait and the next season at the other. A few horses raced at different gaits weekly, but today most STBs race at only one gait. Many foals pace or trot naturally. Although trotters trot while racing, they occasionally break into a pace when they are lame. Pacers often jog—the term used for trotters and pacers when trotting the slow or wrong way (clockwise) of the track at the trot—but train and race at the pace. The pace is faster than the trot. The current (2009) world record for the pace during a parimutuel race is 1 : 46.4 (all-age, any size track) and that for the trot is 1 : 49.3 on a track longer than 1 mile and 1 : 50.1 on a 1-mile or smaller racetrack. Many purists in the sport do not consider a world record on a racetrack longer than 1 mile to be equivalent to that obtained on a smaller racetrack because there is only one turn compared with two or more on smaller racetracks. Many pacers race near record time, but trotters do not. Trotters and pacers do not race against each other in parimutuel races. A STB racehorse must qualify for racing, meaning the horse must better or match a minimal speed before being entered into a parimutuel race. Another form of speed test is called a time trial. At certain 1-mile-long racetracks, horses compete against a prompter, usually a TB in harness, and go as fast as possible, but the prompter cannot pass the STB. The world record for the time trial is 1 : 46.1 set by a pacer. Mean race times of STBs are decreasing constantly (the horses are becoming faster) because of selective breeding, changes in track surfaces and banking, popularity of 1-mile racetracks (racing is faster because horses only negotiate two turns), refinement in race bikes (sulky), and advances in veterinary care.
Early trotters were raced under saddle and then with carts and wagons, with a time under 3 minutes being noteworthy. Sulkies appeared regularly in races in the 1840s, and the 2:30 barrier fell in 1845, becoming a time standard for the era. Race times fell steadily, and in 1897 a stallion named Star Pointer paced a mile in under 2 minutes. The first horse to trot the 2-minute mile was Lou Dillon in 1903.
North American STBs start a race behind a moveable starting gate, a vehicle carrying a barrier to keep the horses in line until the gate pulls away, at which time the horses accelerate to start the race evenly. In some countries, horses start from a standing start, a staggered standing start, or a moving start without a gait. In Europe, races are only for trotters, and top 3-year-old and older North American trotters often are sold to European buyers.
STBs in North America are divided into four classes. The first is the International trotter that races in the top competitions in North America and Europe. The second is the Grand Circuit or stakes horse that travels from track to track, racing against the top 2- and 3-year-old horses. These horses may earn more than 1 million dollars a year. The third class includes the greatest number of horses stabled at or near a parimutuel track. These horses race repeatedly at one or two different tracks and are referred to as overnight horses. Overnight horses are raced in condition races, grouping similar quality horses by earnings, age, or sex, or in claiming races, where horses are grouped by price. The fourth class, county fair racehorses, popular mostly in the northeast and midwest United States, race for small purses at county fairgrounds, often under adverse track conditions, but they provide thrills for fans and owners beyond those of races with richer purses.
Amateur STB driving and racing under saddle are hobby-type events that are increasing in popularity. STBs compete at horse shows in the roadster classes, hitched to a bike or wagon, and also as road horses under saddle. Former STB racehorses are not only popular in the Amish community, but they also can be found performing diverse sporting activities such as low-level dressage and jumping. The Standardbred Retirement Foundation (http://www.adoptahorse.org) helps to find homes for former racehorses; the Harness Racing Museum and Hall of Fame (http://www.harnessmuseum.com) and the United States Trotting Association (http://www.ustrotting.com) are worthy causes and valuable sources of information about the North American STB.
Training
A classically trained STB has about 9 months of schooling and training before its first race. Most horses start training in the fall at  years of age and begin racing the next summer. Many states have racing programs for 2-, 3-, and 4-year-old horses and require a horse to be nominated early in life. Eligibility then is maintained by periodic payments, called stake payments, creating a large pool of money divided among the winners of elimination and final events. Although some stake races receive track or corporate purse assistance, owners who put up their own money support most races. Stake races are limited by age and sex. For example, 2-year-old trotting fillies race together. Stake payments must be made early in the spring, before talent and speed of individual horses can be confirmed, and owners, trainers, and veterinarians must decide which horses to stake. Emphasis on racing young STBs and the money necessary to maintain stakes eligibility place extreme pressure on trainers to race horses at 2 and 3 years of age. Horses often are pushed farther and faster than is reasonable, placing them at risk of stress-related bone injury, usually of subchondral bone. Many owners do not realize the difficulty of having a horse compete based on a calendar of scheduled events, expecting the horse to peak for the biggest purses, rather than on the horse’s training and fitness level. The process of nominating and planning for stakes races is an art and science, and often a staking service is hired to organize periodic stake payments. Stake payments are a considerable expense, and some owners spend several hundred thousand dollars a year. Horses not nominated, those dropped from stakes programs because of injury or lack of talent, or those in which payments were missed are still eligible for overnight racing. More and more late closer and entry-only stakes are becoming available for nonstaked horses.
years of age and begin racing the next summer. Many states have racing programs for 2-, 3-, and 4-year-old horses and require a horse to be nominated early in life. Eligibility then is maintained by periodic payments, called stake payments, creating a large pool of money divided among the winners of elimination and final events. Although some stake races receive track or corporate purse assistance, owners who put up their own money support most races. Stake races are limited by age and sex. For example, 2-year-old trotting fillies race together. Stake payments must be made early in the spring, before talent and speed of individual horses can be confirmed, and owners, trainers, and veterinarians must decide which horses to stake. Emphasis on racing young STBs and the money necessary to maintain stakes eligibility place extreme pressure on trainers to race horses at 2 and 3 years of age. Horses often are pushed farther and faster than is reasonable, placing them at risk of stress-related bone injury, usually of subchondral bone. Many owners do not realize the difficulty of having a horse compete based on a calendar of scheduled events, expecting the horse to peak for the biggest purses, rather than on the horse’s training and fitness level. The process of nominating and planning for stakes races is an art and science, and often a staking service is hired to organize periodic stake payments. Stake payments are a considerable expense, and some owners spend several hundred thousand dollars a year. Horses not nominated, those dropped from stakes programs because of injury or lack of talent, or those in which payments were missed are still eligible for overnight racing. More and more late closer and entry-only stakes are becoming available for nonstaked horses.
A STB is trained in a jog cart that is stronger, longer, and about three times as heavy as the 14-kg sulky or race bike. A young pacer is soon equipped with hobbles, which are leather or plastic straps encircling the ipsilateral forelimbs and hindlimbs, to keep legs moving in unison (see Figure 108-1, B). A horse capable of sustaining a pace without hobbles is called a free-legged pacer, but few race without hobbles. Hobbles can cause areas of hair loss on the cranial aspect of the forearm and the caudal aspect of the crus called hobble burns, which are typical marks of a pacer. Trotting hobbles, which are straps encircling both forelimbs that run through a pulley underneath the horse, have become popular and are being used on more and more trotters in recent years, even those competing in top stakes races. Trotting hobbles may stabilize the trotting gait at speed. Some in the industry frown on the use of these equipment additives, claiming they may give an unfair advantage and historically have not been used.
Equipment is important in understanding gait and lameness. Head poles, boots, brace bandages, gaiting straps, and gaiting poles are used to improve gait and performance, as well as to assist in steering the horse at racing speed. A head pole keeps the horse from turning the head and neck to the opposite side. A horse with right forelimb (RF) lameness usually bears left, called bearing in or on the right line, because the driver pulls on the right line, causing the horse to turn the head to the right. This horse would wear a left head pole. Gaiting straps and poles run alongside the horse and attach to the cart beside the driver’s seat and are used to keep the horse straight. Horses with unilateral hindlimb lameness often carry the hindquarters near the contralateral shaft, called being on the shaft. A horse with RH lameness goes on the left shaft and requires a left gaiting pole or strap. Boots are applied to minimize interference injury. Some horses chronically interfere, whereas interference in others is accidental. Soft brace bandages are used for protection and to widen the hindlimb gait.
Training the Young Standardbred
Yearling STBs are introduced to the harness and bridle in the stall and then are line driven at a walk for several days before being hitched and jogged on the track. Once the horses can go to the track with a single driver, trainer, or groom, they are jogged 1 to 2 miles each morning, usually in a clockwise direction (wrong way) first. Young STBs are encouraged to jog at the intended gait as soon as possible. STBs are usually jogged 6 days a week at slow speed. This is usually natural for trotters, but many pacers need hobbles or special shoeing. Weight usually is added to hind shoes of pacers, especially to the outside web, whereas the front feet may be left unshod. In trotters, weight is added to the front shoes. Shoeing and equipment changes begin early to produce the best gait possible.
Jogging is increased 1 mile every few weeks, up to 4 to 5 miles daily. Horses are taught to jog both ways of the track. Most young horses are jogged in groups, so horses overcome fear of traveling in close proximity. In large stables, horses are trained in sets of three to five to teach passing and racing in tight quarters and to simulate racing. In addition to jogging, horses are trained fast every 3 to 4 days initially, but later twice weekly, going counterclockwise (the race or right way on the track). Horses are trained 2 and sometimes 3 fast miles on training days but usually go back to the barn for a breather (to blow out) between fast miles (trips). STBs develop tremendous stamina compared with TBs, but fatigue and strain cycles predispose them to stress-related injury of the subchondral bone, not commonly of cortical bone unlike TBs. When the fastest miles approach racing speed, young horses are ready for baby or schooling races to learn how to leave the starting gait. It is interesting that most STBs are trained, schooled, and qualified in the morning daylight and then make the first parimutuel start at night under the lights.
Retraining a Racehorse
The classic retraining approach involves jogging 2 to 5 miles a day and additional training one to two times a week. A fast workout usually consists of two to three fast trips, which are simulated race miles taken at increasing speed. Horses usually are allowed to blow out between trips. Some are given double headers, which are two 1-mile workouts without returning to the barn, but they walk or jog slowly between trips. A break is when a horse leaves the expected gait and breaks into a gallop. Many training miles are given to obtain maximum physical fitness and to condition the horse to travel at speed without breaking. Many training miles are considered necessary to evaluate and adjust equipment and shoeing. Diagnostic analgesia can be performed between trips.
Alternative training methods produce good results and are customized to the disposition and physical condition of the horse. Trainers now use interval training, straight tracks, inclines and hills, swimming, towing behind a vehicle, and mechanical walkers or joggers. With relocation of European trainers to North America, more alternative techniques have been introduced, including riding trotters between races.
Once racing, work is customized to each horse’s needs. Hard training using the classic training method consists of one race and two training trips per week, but in this system horses are under considerable stress. Now that the breed is refined and heat races are fewer, racing horses are given much less training between races, and fast work may not be given at all. Reducing exercise intensity between races is important in managing STBs with chronic lameness.
Lameness and Poor Racing Performance
Lameness is the leading cause of poor performance and a major cause of STBs making breaks. Some overnight and stakes horses are chronically lame but race weekly, although lame horses race slower, and horses drop in class as lameness progresses. The major effect of lameness is seen during the last quarter of the race, called the last quarter time. Lower-class horses usually have a fast opening quarter but slow last quarter time, whereas open and stakes horses have fast quarter times anytime during the race. Evaluation of last quarter time is useful to determine cause and severity of poor race performance. Lameness often costs a horse 1 to 2 seconds in last quarter race time, equating to 5 to 10 horse lengths. For example, a horse that normally paces the last quarter in 27.1 seconds but for the last few starts has been coming home in 28.4 to 29.2 seconds is probably lame, although concomitant respiratory and metabolic problems cannot be overlooked.
Track Surface and Lameness
STBs usually race around an oval track,  to 1 mile in circumference; a 1-mile track is most common. Races are usually 1 mile, but a few are
to 1 mile in circumference; a 1-mile track is most common. Races are usually 1 mile, but a few are  -mile sprints to 2-mile races. The track surface is a crushed rock base, covered with a packed, sandy soil and a thin sand or stone dust surface. STB racing requires a much firmer track surface than galloping horses. Sulky tires are more efficient if rolling over a firm smooth surface, and the STB gaits require a firmer and smoother surface than does the gallop. Track surfaces have become firmer because year-round racing requires a surface suitable for racing in rain and subfreezing temperatures. Hard tracks with loose surfaces require horses to wear shoes with added grabs and welded-on spots of borium to avoid slipping. Excessive slipping or overzealous use of shoes with additives predisposes horses to lameness. A soft or deep surface can predispose horses to tendonitis and suspensory desmitis. Hard tracks with a covering of loose stone dust are slippery and may predispose horses to carpal synovitis, bruised soles, and muscle soreness. Racetracks get soft and sticky with small amounts of rain and hard and unyielding with heavy rainfall that may wash the top surface into the infield. Recently, a three-dimensional dynamometric horseshoe was used to measure acceleration and other forces on the front hoof of French trotters performing at high speed on two different track surfaces, all-weather waxed and crushed sand track surfaces.1,2 Hoof deceleration was significantly less, and there was a 50% attenuation of shock when horses performed on the waxed surface, suggesting this surface had better shock-absorbing qualities compared with a crushed sand surface.1 The amplitude of the maximal longitudinal braking force was significantly lower and occurred 6% later in the stance phase. The magnitude of the ground reaction force at impact was lower on the waxed track compared with the crushed sand track surface.2 The attenuation of loading rate, amplitude of horizontal braking, and shock at impact on waxed surfaces suggested that there is likely a reduction in stress in the distal aspect of the forelimb, results that may be important in training normal horses or rehabilitating STBs with infirmities.2
-mile sprints to 2-mile races. The track surface is a crushed rock base, covered with a packed, sandy soil and a thin sand or stone dust surface. STB racing requires a much firmer track surface than galloping horses. Sulky tires are more efficient if rolling over a firm smooth surface, and the STB gaits require a firmer and smoother surface than does the gallop. Track surfaces have become firmer because year-round racing requires a surface suitable for racing in rain and subfreezing temperatures. Hard tracks with loose surfaces require horses to wear shoes with added grabs and welded-on spots of borium to avoid slipping. Excessive slipping or overzealous use of shoes with additives predisposes horses to lameness. A soft or deep surface can predispose horses to tendonitis and suspensory desmitis. Hard tracks with a covering of loose stone dust are slippery and may predispose horses to carpal synovitis, bruised soles, and muscle soreness. Racetracks get soft and sticky with small amounts of rain and hard and unyielding with heavy rainfall that may wash the top surface into the infield. Recently, a three-dimensional dynamometric horseshoe was used to measure acceleration and other forces on the front hoof of French trotters performing at high speed on two different track surfaces, all-weather waxed and crushed sand track surfaces.1,2 Hoof deceleration was significantly less, and there was a 50% attenuation of shock when horses performed on the waxed surface, suggesting this surface had better shock-absorbing qualities compared with a crushed sand surface.1 The amplitude of the maximal longitudinal braking force was significantly lower and occurred 6% later in the stance phase. The magnitude of the ground reaction force at impact was lower on the waxed track compared with the crushed sand track surface.2 The attenuation of loading rate, amplitude of horizontal braking, and shock at impact on waxed surfaces suggested that there is likely a reduction in stress in the distal aspect of the forelimb, results that may be important in training normal horses or rehabilitating STBs with infirmities.2
Track Size and Lameness
Track size has substantial implications in the development and expression of lameness. Tracks are 1 mile,  mile,
mile,  mile, and
mile, and  mile, and in general race times are lower (faster) on large tracks. Because most STB races are 1 mile, track size determines the number of turns during the race. During a race on a
mile, and in general race times are lower (faster) on large tracks. Because most STB races are 1 mile, track size determines the number of turns during the race. During a race on a  -mile track, a STB must negotiate four turns. Turns on smaller racetracks are much tighter than those on larger tracks (see Figure 108-2). There is a single racetrack larger than a 1-mile oval, Colonial Downs in Virginia, at which a short race meet is held each year; on this track, races involve negotiating a single turn. Horses racing with mild chronic lameness are less likely to sustain speeds necessary to be competitive on larger tracks, so they may race on smaller tracks; however, if lameness is worse in the turns, the horse may be less competitive on small tracks and better suited for a 1-mile track. If lameness is worse in the straightaway, the horse may be best suited for a small track. This is particularly important when lameness worsens as the race goes on because large tracks have a long straightaway at the end.
-mile track, a STB must negotiate four turns. Turns on smaller racetracks are much tighter than those on larger tracks (see Figure 108-2). There is a single racetrack larger than a 1-mile oval, Colonial Downs in Virginia, at which a short race meet is held each year; on this track, races involve negotiating a single turn. Horses racing with mild chronic lameness are less likely to sustain speeds necessary to be competitive on larger tracks, so they may race on smaller tracks; however, if lameness is worse in the turns, the horse may be less competitive on small tracks and better suited for a 1-mile track. If lameness is worse in the straightaway, the horse may be best suited for a small track. This is particularly important when lameness worsens as the race goes on because large tracks have a long straightaway at the end.
During counterclockwise racing, right-sided lameness conditions exert more influence, even though the LF and LH are on the inside. Horses with left-sided lameness can race successfully on small tracks and apparently negotiate turns well. However, those with right-sided lameness cannot trot or pace the turns well, most likely from the effect of centripetal and compressive forces. Ideally, all racehorses should be sound, but many horses can race successfully with mild infirmity. Horses with substantial lameness should be treated or rested until the condition improves.
Conformation
Forelimb and hindlimb faults lead to lameness and interference. Severity often depends on gait. A trotter should be as long from front to back as it is tall. Trotters are passing gaited if hind feet land outside the front feet, and in-line gaited if hind feet land in plane with the front feet. Wide hindlimb gait is advantageous because it allows a passing gait. Trotters can be mildly to moderately toed out in front without substantial interference problems, but they should not be toed in because winging out leads to interference and lateral suspensory branch desmitis. Pacers can be wide and mildly toed in but not toed out because this fault predisposes the horse to hitting the knees. A club foot is less well tolerated by a STB than a TB and usually results in foot lameness. Low, underslung heels and long toes are acquired by attempts to increase stride length or to decrease interference. Back at the knee is undesirable and leads directly to carpal lameness in a trotter, but it is better tolerated by a pacer. Offset (bench) knee is a major fault, and although horses may race successfully, lameness of the carpus and metacarpal region often develops. Mild carpus valgus is tolerated by pacers but can lead to lameness of the carpus and metacarpal region. Pacers that are tied in behind the knee are at risk of developing superficial digital flexor tendonitis, but surprisingly trotters are not. Short, straight pasterns and short backs are undesirable.
A serious hindlimb fault leading directly to moderate to severe lameness is sickle-hocked conformation (see Chapters 4 and 78). Mild sickle-hocked conformation typified many early pacers and is desired by some trainers. Sickle-hocked trotters are fast but develop curb and osteoarthritis (OA) of the distal hock joints, particularly severe in the dorsal aspect, and are chronically unsound. Sickle-hocked conformation predisposes all STBs to the development of slab fractures of the third and central tarsal bones. Straight hindlimb conformation is unusual but is a severe fault, leading to metatarsophalangeal and stifle joint lameness and suspensory desmitis. In horses with straight hindlimb conformation, excessive extension of the metatarsophalangeal joint occurs. Long, sloping pasterns also predispose horses to fetlock hyperextension, but a primary metatarsophalangeal joint weakness is seen in some trotters with normal pastern lengths, in which the base of the proximal sesamoid bones (PSBs) is level with the middle of the proximal phalanx. Abnormal elasticity or loss of support from the suspensory apparatus predisposes horses to run-down injury and suspensory desmitis. Run-down injury is more commonly seen in the hindlimbs. Cow-hocked conformation is prevalent in trotters but is not problematic unless severe. In-at-the-hock conformation predisposes horses to OA of the distal hock joints, curb, and medial splint bone disease. Base-wide and base-narrow conformational faults, if severe, can lead directly to interference and lameness.
Distribution of Lameness
STB racehorses have a higher percentage of hindlimb lameness than TBs. The STB trains and races using a two-beat gait: two limbs bear weight simultaneously. Load is shared almost equally between forelimbs and hindlimbs. The caudal location of the cart and driver (load) and the addition of the overcheck apparatus shift the center of balance caudally, increasing hindlimb lameness (see Figure 2-2Figure 2-3). The distribution of forelimb to hindlimb lameness is approximately 55% to 45%.
Lameness in the Young Standardbred
The top 10 list (see page 1024) contains those conditions seen in STB racehorses of all ages when grouped together, but unraced 2- and early 3-year-olds develop a subset of lameness conditions. Osteochondrosis (see Chapters 54 and 56), splint exostoses (splints), and curbs are common. Forelimb splints are usually medial but can occur laterally. Hindlimb splints are almost always medial and are more common in trotters. Splints can cause primary lameness or be secondary to carpal lameness, especially if the exostosis is proximal. Forelimb splints develop when the limb is carried or lands abnormally. Young horses develop splints from difficulty learning the racing gait and by making breaks. While breaking, pacers often hit themselves because galloping in hobbles is difficult. Curb is common in young pacers and may be recognized while horses are jogging, before training begins (see Chapter 78).
Carpal lameness is common in young horses. The middle carpal joint is the most common site, but synovitis can occur in the antebrachiocarpal joint. Carpal lameness is caused by early subchondral stress-related bone injury of the third carpal bone and is particularly common in trotters. Paddock turn out for 30 days is recommended. Middle carpal joint lameness must be differentiated from proximal suspensory desmitis (PSD). The thought once was that the distal radial physis was a source of occult carpal region lameness, but diagnosis was never confirmed. Physeal pain is a rare diagnosis today, but some veterinarians believe such pain is a possible source of so-called colt soreness.
Bucked shins are rare but do occur in 2-year-old pacers in July and August. Most bucked shins occur in the forelimbs. Genuine bucked shins rarely occur in trotters, but interference trauma of the dorsal cortex of the third metatarsal bone (MtIII) is common.
Distal hock joint pain is a common cause of acute unilateral lameness, but if pain is bilateral, overt lameness may not be present. Horses appear stiff and sore when starting out and warm out of lameness. Gait abnormalities and repeated breaking may cause distal hock joint pain. Lameness may be difficult to abolish completely with intraarticular analgesia because pain is multifactorial, arising from periarticular soft tissues and secondary gluteal myositis and trochanteric bursitis. Horses should be rested for 1 week and given nonsteroidal antiinflammatory drugs (NSAIDs) such as phenylbutazone (2.2 to 4.4 mg/kg orally [PO] twice daily). Intraarticular injections are avoided if possible, but treatment of the tarsometatarsal (TMT) joint with hyaluronan alone, or in combination with corticosteroids, often resolves residual lameness. Using a less aggressive training schedule for 20 to 30 days is recommended. Shoeing should be evaluated, and grabs and calks should be removed or minimized.
Interference injuries are common and plague many STBs throughout the racing career. Trotters interfere primarily by striking the toe of the ipsilateral front foot to the shin, pastern, or coronary band regions of the hindlimb (see Chapter 7 and Figure 7-2). Interference from a front foot striking the medial aspect of the contralateral forelimb (cross-firing) occurs occasionally in trotters but is a major form of interference injury in pacers. Injury to second (McII) and third metacarpal (McIII) bones, PSBs, carpus, heel, and hoof wall causes bruising and hematoma formation. Contusions can lead to soreness or frank lameness and can cause an altered gait. A trotter attempting to avoid striking the LH shin shortens the cranial phase of the stride, causing what appears to be a pelvic hike, mimicking LH lameness. Deliberate hiking can alter load distribution, causing compensatory lameness in the RH and RF. Local trauma is treated, and changes in equipment and shoeing, such as applying brace bandages and boots, are performed. A brief (5 to 7 days) reduction in exercise intensity is useful to allow a young horse to gain confidence in the corrected gait.
Young horses with poor gait should be examined carefully for neurological disease. Equine protozoal myelitis (EPM) is endemic in STBs and can be a real cause of gait deficits or a catchall diagnosis (see Chapter 11).
Clinical History
Clinical history is critical for lameness diagnosis and to put lameness into context with other causes of poor racing performance. The attending veterinarian with an established relationship with the horse may know the horse’s history. A trainer often refers to mild lameness by saying, “The horse is just sore, Doc,” or “The horse is off when jogging, but throws it away when going the right way.” STBs have unusual resiliency and race rather well with chronic lameness, but lameness does not resolve with speed. Owners do not understand this concept. Signs of lameness become less visually apparent when horses go fast. Because STBs often race with numerous compensatory lameness problems, one must be open to the possibility that current lameness is not worsening of an existing problem but is an entirely new one.
A good starting place is to determine the chief complaint from the person(s) closest to the horse, usually the groom and trainer. What differs now from the horse’s normal activity, gait, or performance? Has a change in training or racing schedule occurred? Has there been a change in track surface? A horse noticed to be stiff and sore up front when walking to the track may be foot sore the day after the horse raced on a hard track. Have any equipment or shoeing changes been made? Additions of head poles, gaiting straps, and boots point to high-speed lameness and gait abnormalities. Shoeing changes, such as adding or removing bar shoes, are important because horses used to wearing bar shoes may have sore feet if bars are removed. Metacarpophalangeal joint lameness may be worse if bars are added. Stress-related bone injury of the metatarsophalangeal joint is seen soon after aluminum shoes with toe grabs are applied. Is the horse receiving any current medication, and when was the horse last examined? What treatments, if any, were given? Although an acute injury or worsening of chronic OA can cause acute synovitis, inflammatory and infectious arthritis can develop days to weeks after intraarticular injections, particularly if corticosteroids were used, because these drugs can suppress signs of inflammation and infection for weeks. Infectious arthritis is common 14 to 21 days after intraarticular injection, but often owners and trainers are incredulous because recent injections were not performed. What have the trainer and groom done recently to solve or treat the problem? Topical therapy may reduce or worsen inflammation and mask or augment clinical signs. Skin soreness after application of paints and blisters can cause a false-positive response to deep palpation.
Is the horse a trotter or a pacer? This information is critical. The usual distribution of pacers to trotters is about 3 : 1. Interference problems are different between gaits. Trotters often develop contralateral or diagonal compensatory lameness, whereas pacers most often develop ipsilateral compensatory lameness. A pacer with a left carpal lameness often develops LH compensatory lameness, but a trotter is more likely to develop compensatory lameness in the RH. Although this distribution of compensatory lameness is common when examining horses trotting in hand, load distribution and interference issues may complicate and change visual appearance of where primary lameness originates when a STB is pulling a cart on the track and on which gait the horse is performing. The distribution of lameness differs between gaits. Fractures of the proximal phalanx and the McIII and the MtIII and superficial digital flexor tendonitis are less common in trotters. Trotters with stifle lameness, specifically OA of the medial femorotibial joint, can cope better than pacers. Race times are different. Prognosis for certain problems such as osteochondral fragments of third carpal and radial carpal bones is worse in trotters. Pacers are more likely than trotters to start a race and to have five starts before and after surgical removal of osteochondral fragments of the carpus.3 Osteochondrosis is common in certain bloodlines of trotters and pacers.
Is the condition worse at the trot or pace? Trotters and many pacers trot while jogging the wrong way but assume the intended gait when turned the right way. Most forelimb lameness conditions are less obvious at the pace, but hindlimb lameness differs. In general, STBs with stifle lameness are worse at the pace than the trot. If trainers comment that the horse is worse at the pace than at the trot, the veterinarian should suspect stifle lameness until proved otherwise. Pacers wear hobbles, but trotting hobbles are often used in trotters making breaks.
Is lameness different depending on what direction the horse moves? Problems on the right side are worse going the right way of the track (counterclockwise). Horses with medial foot and carpal lameness may show signs in the turns, especially entering the turning radius going the right way, but not when jogging.
What is the horse’s last quarter time? Although high-speed lameness can cause a 1- to 2-second decrease in last quarter time, horses with mechanical upper airway disease and rhabdomyolysis have a 2- to 4-second reduction, and those with severe lameness or atrial fibrillation have a 5- to 10-second reduction in last quarter time.
Is the horse on a line? This is one of the most important pieces of information to obtain. Trainers sometimes dismiss young horses being mildly on the line because nervous and inexperienced horses may change directions suddenly, but in reality most of these abnormal movements are caused by lameness. During counterclockwise racing of a horse on the right line, the driver has to increase the tension (pull harder) on the right rein to keep the horse straight and prevent it from bearing toward the infield. Just the opposite occurs when horses are on the left line (see Figure 108-3). Because of bit pressure, when a horse is on the left line, it turns or cocks the head to the left, toward the inside rail, and vice versa. If history is unclear, the veterinarian should watch the horse on the track and observe head position. Because most horses bear away from pain, a horse on the right line is most often lame on the right side, but exceptions occur. A common finding is metacarpophalangeal effusion and a positive response to lower limb flexion. The trainer states, “The horse was on the left line when finishing the mile, but is usually on the right line especially in the turns.” Primary lameness may be in the right carpus, but chronic RF lameness has caused compensatory overloading and lameness of the left metacarpophalangeal joint, and both areas should be evaluated and potentially treated. Most horses on a line from forelimb lameness have foot or carpal lameness. However, problems located medially, such as medial sole bruising, quarter cracks, or carpal lameness, paradoxically can cause a horse to be on the contralateral line. Horses may lose power in the affected limbs and drift at speed toward the lame side. Therefore a horse with a medial LF quarter crack could be on the right line, whereas those with a right carpal lameness could be on the left line. All limbs should be examined because not all horses read the book. “If a horse is on the left line, think right hind,” one old saying goes, and rarely a horse with RH bruised or cracked heels will be on the left line.4
Horses on a line without overt signs of lameness are among the most difficult lameness mysteries to solve. Because compensatory lameness problems may be numerous in a horse in which primary lameness cannot be ascribed, deciding on which limb to begin diagnostic analgesia is a dilemma. Most horses need to be examined at speed after blocking, a time-consuming and frustrating process. In many horses on a line, obscure sources of pain such as subchondral bone can be difficult to identify, and horses often are referred for scintigraphic examination. Most horses chronically on a line have had many intraarticular or other injections, and trainers will state, “We’ve done his knees, hocks, stifles, and feet and nothing helped.” Often forgotten are the metatarsophalangeal joints. In many horses numerous sites of pain must be managed simultaneously rather than sequentially. Recommending numerous intraarticular and regional injections, a shoeing change, and a change in exercise intensity in a horse that is on a line is not unusual.
Is the horse on a shaft? A horse with RH lameness drifts to the left (see Figure 108-2) and positions the hindquarters closer to the left shaft of the sulky and is thus on the left shaft; the reverse is true with LH lameness (see Figure 108-3). Not all hindlimb lameness problems cause horses to be on a shaft. Horses with OA of the medial femorotibial joint may not be on a shaft, but those with distal hock joint pain will be. A horse may be falsely on a shaft if it is hard on a line and the driver pulls hard to keep the horse straight, compelling the horse to twist its entire body, positioning the hindquarters close to one shaft to maintain balance.
Is the horse worse in the turns or on the straightaway? Although nothing is pathognomonic, a few findings are consistent. Horses with front foot lameness, splints, and curbs get worse as the mile progresses and so appear worse on the final straightaway. Horses with distal hock joint pain appear to be worse when going into or coming out of a turn but usually can pace and trot the turns successfully. Horses with carpal, metatarsophalangeal, and stifle joint lameness are worse in the turns. If a horse gets rough in the first turn just after leaving the gate, a medial RF problem such as a splint or carpal lameness should be suspected.
On what size track does the horse race? The relationship of track size to expression of lameness and the differences between left- and right-sided lameness problems were discussed (see page 1017).
Is the horse making breaks? Unsound trotters often break stride and gallop but occasionally break into a pace. Lame trotters may pace when trotted in hand. Because high-speed lameness often causes pacers to gallop and trotters to pace or gallop, it seems that the gallop may be the easiest gait that a lame horse can maintain at speed. The most difficult gait to maintain at speed is the trot, followed by the pace, and lastly the gallop (MWR). Interference injury causes breaks, and current shoeing or recent changes should be evaluated. A different way to hang up a horse, meaning how to shoe and equip it, may be all that is needed.
The veterinarian must be current on all medication rules in the racing jurisdiction because changes, such as recent (2009) modifications of allowable blood levels of corticosteroids, may impact management strategy.
Lameness Examination
The lameness examination can be divided into three stages: palpation, observation while moving on a lead shank, and observation under harness. The veterinarian should avoid narrowing the examination to the area suspected by the groom and trainer but should first stand back and observe the horse and watch the horse moving around and coming out of the stall. Subtle neurological signs may be apparent. Asymmetry, such as muscle atrophy, may point toward chronic lameness or neurological disease.
Palpation
Careful palpation is the art of diagnosis in the racehorse but often is sacrificed because palpation is time consuming. Palpation is critical in STBs because of numerous compensatory lameness problems. The veterinarian needs to be able to “read” the horse to make a diagnosis. A successful lameness detective respects what the horse is trying to say. The veterinarian should move over the entire horse with a light touch to see whether a withdrawal response is elicited. A light touch along the neck and gluteal regions may elicit pain from secondary muscle soreness or painful previous intramuscular injection sites. Horses often exhibit a withdrawal response when a limb is first picked up, indicating a problem even before the specific region is manipulated. Horses may exhibit false-positive responses in areas that have been recently painted, blistered, or freeze fired. Once horses have been freeze fired for splints and curbs, many trainers assume the problem has been solved and are incredulous if the veterinarian suggests the area is still the source of pain. Cryotherapy is not a panacea and may have to be repeated, or another form of management may be needed (see Chapters 78 and 89).
Palpation should be done in a quiet place, before the horse is trotted in hand, so that all potential lameness problems are detected. Careful and detailed examination of the front feet should be performed. Hoof tester examination is critical, but most horses show a painful response for 1 to 2 days after racing, particularly if the track was hard. Effusion of the distal interphalangeal (DIP) joint capsule often accompanies early OA and sore feet. Shoes on the front and back feet should be evaluated critically for wear, type, weight, and the presence of additives. The proximal, dorsal aspect of the proximal phalanx should be palpated for pain associated with midsagittal fractures of the proximal phalanx. Palpation findings in the metacarpophalangeal and metatarsophalangeal joints often do not correlate well with degree of lameness, response to diagnostic analgesia, and results of scintigraphic examination. The presence of mild warmth (heat) on palpation, a subtle clinical finding, is an important observation for detection of subchondral bone pain in the distal aspect of the McIII or the MtIII. Pain on palpation of the PSBs may indicate sesamoiditis. Normally a horse responds little to compression of the suspensory ligament (SL), deep digital flexor tendon (DDFT), and superficial digital flexor tendon (SDFT). Pain is often the first sign of desmitis or tendonitis. Chronic enlargement of the SL and SDFT is common in lower-class horses, and although a horse may not react to palpation, it may have associated high-speed lameness. Splint exostoses are most painful after training or racing but may be nonpainful several days later. Standing and flexed subcarpal palpation may reveal pain associated with PSD, longitudinal and avulsion fractures of the McIII, proximal superficial digital flexor tendonitis, and a dorsal medial articular fracture of the McIII.
No palpable abnormalities may be associated with carpal lameness. The veterinarian should carefully assess for warmth and compare the limb with the contralateral limb. If the horse has been clipped for the application of a paint or blister, the affected area will feel warm compared with the surrounding unclipped skin. Effusion occurs in 2-year-old horses early in training, but it often is minimal in horses with subchondral bone pain. The antebrachiocarpal joint is rarely a site of carpal lameness in older racehorses, but in young horses, especially trotters, effusion may occur. The medial aspect of the carpus and the distal aspect of the antebrachium are common sites for interference injury. Carpal tenosynovitis is unusual to rare, but occasionally hyperextension injury and hemorrhage occur. Rarely, almost always in trotters, desmitis of the accessory ligament of the SDFT occurs, associated with carpal tenosynovitis. Pacers develop hobble burns and cellulitis in the proximal aspect of the antebrachium. Elbow and shoulder joint lameness is rare, but horses may exhibit pain when the biceps brachii, intertubercular bursa, and other muscles are palpated or the shoulder joint is flexed, from muscle soreness secondary to primary carpal lameness. The neck, back, and rump regions should be palpated for symmetry and muscle soreness. Young horses will occasionally manifest sore withers from an improperly fitted harness. Because intramuscular injections of counterirritant and antiinflammatory solutions are common in STBs, careful palpation is necessary to discover deep abscesses causing pain, lameness, and fever. Disease of the thoracic dorsal spinous processes is rare. In a 16-year period, only one of nearly 2400 STBs undergoing scintigraphic examination had increased radiopharmaceutical uptake (IRU) in the dorsal spinous processes or the intervertebral synovial joints, and no bony abnormalities were found in the pelvis.5
Secondary muscle soreness of the gluteal region is a common problem, and the diagnosis of trochanteric bursitis often is made based on a painful response to compression. Trochanteric bursitis (whorl bone disease) may be overdiagnosed and difficult to authenticate, but injections often improve hindlimb gait and performance (see Chapter 47). Rhabdomyolysis also can cause pain on palpation of the rump region. Young horses with loose stifles often knuckle behind, but palpation is often negative. Pain associated with the medial aspect of the stifle may be present, but abnormalities when manipulating the patella are absent. Femoropatellar effusion in young horses can signal osteochondrosis. The medial femorotibial joint capsule should be palpated because OA is the most important cause of lameness of the stifle. The crus is a rare site of pain. Hobble burns on the caudal aspect can cause soreness in young pacers.
The tarsocrural joint is the most common site for osteochondrosis, and effusion in young horses should prompt radiographic examination. Periarticular pain in the distal aspect of the tarsus and proximal metatarsal region often accompanies distal hock joint pain. The Churchill test is done routinely, but in addition to those with distal hock joint pain, STBs often respond positively with other common distal limb lameness. Bony enlargement (bone spavin) is rare. Plantar soft tissue swelling and pain associated with curb is a common cause of lameness (see Chapter 78). The plantar metatarsal region commonly is overlooked, but it should be palpated carefully for the presence of suspensory desmitis. Signs of inflammation may be difficult to detect because the SL is enclosed within the bony confines of the metatarsal bones. The first evidence of suspensory desmitis is mild enlargement and pain of the suspensory body in the midmetatarsal region. Compression of the splint bones puts indirect pressure on the SL and explains why the Churchill test is nonspecific. The dorsal aspect of the MtIII is a common site for interference injury in trotters. Palpation of the fetlock region is critical because the region is an important source of lameness, but often no localizing clinical signs are apparent. Mild warmth may signal the presence of subchondral bone injury. Pain from interference injury should be differentiated from that associated with midsagittal and dorsal plane fracture of the proximal phalanx. The hind foot is an unusual source of lameness, but fractures of the distal phalanx, bruising, navicular disease, and OA of the DIP joint are diagnosed occasionally. STBs normally respond positively to hoof testers placed across the heel.
Movement
The horse should be examined at a walk and trot in hand. The pace is a forgiving gait, and head and neck nod and pelvic hike can be difficult to see. Evaluating lameness in pacers is easier while they are trotting, but correlation between lameness seen in hand and during pacing at high speed is questionable. Forelimb lameness is less obvious at the pace. Degree of pelvic hike is comparable at the pace and trot. Baseline lameness should be determined before the harness is applied because horses that are fracture lame should not be taken to the track, and a good correlation exists between lameness seen in hand and in harness in horses with obvious lameness. The ability to trot horses in hand at the racetrack may be limited because of too much activity, lack of room, and often poor or slippery surfaces. Flexion tests are performed but lack specificity. The carpal flexion test is the most reliable and specific of all flexion tests. Direct compression of a painful splint, the proximal aspect of a SL, and a curb followed by trotting is useful. Subtle hindlimb lameness is best evaluated in harness because little correlation may exist with lameness seen in hand. Pulling a cart and different surface likely explain this observation. Subtle (less than grade 1 of 5) hindlimb lameness at the trot in hand should be taken with a grain of salt. Observation on the track puts lameness into perspective and allows evaluation of compensatory lameness. Although there may be a lack of correlation between lameness seen in hand and that observed on the track or at speed, any lameness condition may be an important contributor to poor performance. Lameness is most pronounced when horses are jogged slowly and is much less obvious with speed. High-speed lameness is evaluated by communication with the trainer and by resolving signs such as being on a line by using diagnostic analgesia.
Diagnostic Analgesia
Diagnostic analgesia is essential to pinpoint lameness, but trainers and owners often prefer treatment of a suspected area rather than lengthy investigation. With weekly racing, no time may be available for blocking because levels of local anesthetic solution will be detectable. Diagnosis often is made based on response to treatment. Many common lameness conditions involve subchondral stress-related bone injury, and often horses can be blocked sound but do not improve with intraarticular treatment. Perineural analgesia is more effective than intraarticular analgesia for diagnosing subchondral bone pain.
Controlling as many variables as possible is important when observing STBs in harness. The same gait, equipment, driver, approximate speed, and track direction should be used. Sometimes horses exhibit lameness when driven by the groom but not the trainer because trainers expect a higher level of performance and often carry a whip. A false-positive response occurs when a horse exhibits lameness at the pace but after diagnostic analgesia returns to the track without hobbles equipment and trots soundly. The diagnostic analgesia procedure should be the only variable. STBs often warm out of lameness and should be evaluated immediately when starting out after each block. Overzealous use of a twitch and rough handling may compromise evaluation, and administration of drugs can add another variable. If horses are observed in harness after diagnostic analgesia, the person driving the horse should be instructed to return the horse to the stable as soon as improvement is recognized because training a horse after blocking risks further injury.
Complete description of blocking techniques is found in Chapter 10. A few points about diagnostic analgesia in the STB must be kept in mind. Palmar or plantar digital analgesia desensitizes most of the foot. Horses with metacarpophalangeal or metatarsophalangeal joint lameness can be sound after palmar or plantar digital analgesia, particularly those with midsagittal fracture of the proximal phalanx.6 Palmar nerve blocks at the level of the PSBs are avoided because inadvertent analgesia of fetlock pain can be misinterpreted as lameness of the foot or pastern. Individual carpal joints should be blocked separately, and differentiation between carpal and proximal metacarpal region lameness is necessary. The median and ulnar nerve block is underused.
A low plantar block must be done routinely, or many lameness conditions will be diagnosed erroneously as high up. The fetlock region is a major source of hindlimb lameness. Although subchondral bone pain of the distal aspect of the MtIII (McIII) can be abolished using intraarticular analgesia of the fetlock joint, most consistently pain is abolished using perineural analgesia. A modification of the low plantar technique, blocking only the lateral plantar metatarsal nerve, can be completed and the horse evaluated. If lameness abates, then pain associated with the lateral aspect of the fetlock joint is diagnosed; however, if no response is seen sequentially, the medial plantar metatarsal nerve, then the medial and lateral plantar nerves must be blocked. The high plantar block is often overlooked, but PSD cannot be substantiated without it. The centrodistal (CD) joint is difficult to enter but should be blocked separately from the tarsometatarsal (TMT) joint because communication occurs in only 8% to 39% of horses. The medial femorotibial joint should be blocked separately from the femoropatellar joint, even though they communicate in a high percentage of horses.
Imaging Considerations
Radiography
Routine radiographic examination of STBs does not differ from that of other sports horses. However, a few specific images should be kept in mind. Down-angled oblique (dorsal 60° proximal 45° lateral-palmarodistal medial oblique and dorsal 60° proximal 45° medial-palmarodistal lateral oblique) and horizontal oblique (dorsolateral-palmaromedial oblique [DL-PaMO] and dorsomedial-palmarolateral oblique) images should be obtained to evaluate the DIP joint and palmar processes of the distal phalanx. The tangential (palmaroproximal-palmarodistal oblique) image of the navicular bone is less valuable in the STB than in other older sports horses. To evaluate the distal aspect of the McIII (or MtIII) for subchondral stress-related bone injury and the space between the proximal palmar (or plantar) aspect of the proximal phalanx and the base of the PSBs for the presence of fragments, down-angled oblique (dorsal 30° proximal 45° lateral-palmarodistal medial oblique and dorsal 30° proximal 45° medial-palmarodistal lateral oblique) images should be obtained (see Chapter 42). The most important images of the carpus are the DL-PaMO image and the tangential (skyline) image of the distal row of carpal bones. In STBs it is essential to have a well-exposed and well-positioned skyline image to evaluate the third carpal bone for increased radiopacity, radiolucency, and osteochondral fragments (see Chapter 38). Radiological changes of OA of the CD and TMT joints and slab fractures of the third tarsal bone are seen best on the lateromedial and dorsomedial-plantarolateral oblique (DM-PlLO) images. A common misconception is that changes associated with bone spavin occur medially but not in young STBs. The DM-PlLO image is essential in evaluating the tarsocrural joint for osteochondrosis fragments because two common locations—the cranial aspect of the intermediate ridge of the tibia and the lateral trochlear ridge of the talus—are evaluated best using this image. The caudocranial image is essential when evaluating the medial femorotibial joint for narrowing, osteophytes, and subchondral bone cysts. Inadequate exposure and positioning often result in images that cannot be interpreted.
Digital and computed radiography are useful in evaluating stress-related bone injury of subchondral bone and incomplete fractures. Computed tomography is useful to evaluate subchondral bone and fracture configuration. Magnetic resonance imaging is useful to evaluate subchondral bone and soft tissues of the distal aspect of the limb, but scintigraphic examination is still used routinely for investigation of high-speed lameness and poor performance and continues to have great value in lameness diagnosis in STBs.
Ultrasonographic Examination
Suspensory desmitis, superficial digital flexor tendonitis, curb, and desmitis of the distal sesamoidean ligaments are common in the STB, and ultrasonographic examination is essential for diagnosis and assessing prognosis (see Chapter 16).
Scintigraphic Examination
Referral for scintigraphic examination is common, and horses with poor performance often have numerous areas of IRU, indicating high-speed lameness is a part of the problem. Common areas of IRU include the distal phalanx, metacarpophalangeal joint (medial condyle of the McIII and PSBs), proximal aspect of the McIII, carpus, especially the third and radial carpal bones, metatarsophalangeal joint (proximal aspect of the proximal phalanx and distal plantarolateral aspect of the MtIII and PSBs), the proximal plantar aspect of the MtIII, subchondral bone of the TMT and CD joints and the medial femorotibial joint (see Chapter 19).
Proceeding Without a Diagnosis
Proper identification of lameness as the cause of poor performance and localizing the site(s) of pain can be challenging and relies heavily on experience. It is particularly important to differentiate lameness from interference because interference can cause signs that mimic lameness, lameness can result from interference, and lameness can cause interference. Horses on a line without obvious lameness and a negative response to diagnostic analgesia can be frustrating. Horses can become stubborn and react to equipment and twist and bend the head and neck, causing signs similar to being on a line. Occasionally, horses with tooth-related pain get on a line. An ocular problem is a rare cause of a horse being on a line. Trainers may use bridles with partial blinds or vision-restricting cups to control a horse on a line.
Simultaneous RF and RH or LF and LH lameness, or even primary hindlimb lameness, can be difficult because hindlimb lameness can cause a head nod mimicking ipsilateral forelimb lameness. Diagnostic analgesia should start in the hindlimb. In trotters with foot and carpal lameness the caudal phase of the lame forelimb is longer, and to avoid interference, the cranial phase of the ipsilateral hindlimb is shortened (hiking), mimicking hindlimb lameness. Pelvic hike abates when the source of forelimb lameness is localized. If the lameness problem is complex and frustrating, it is possible that a fresh perspective from a colleague or advanced imaging may help.
To differentiate lameness from interference gait abnormalities, phenylbutazone (4.4 mg/kg twice daily for 5 to 10 days) is administered (the bute test). Horses with pain should improve, whereas those with pure interference gait abnormalities should not. However, not all horses with musculoskeletal pain respond to NSAIDs, particularly those with chronic lameness or numerous compensatory problems. Alternatively, the veterinarian should medicate the suspected area and see whether performance improves because mimicking the maximal exertion of racing is difficult. A trotter on a line only going into the first turn may be helped by injection of corticosteroids around a mildly painful medial splint or into the middle carpal joint. Sometimes treating a different area between several races may allow a fortuitous discovery, but this requires good record keeping, and it may be expensive. Occasionally, horses with subtle or nondescript lameness or a rough gait are managed using a shotgun approach, and numerous intraarticular treatments are given simultaneously. This approach should be reserved for horses in which normal management procedures have failed and an important race is rapidly approaching. Sometimes a positive response to intraarticular corticosteroid injections results from systemic absorption and effect on a distant, rather than the intended, site.
A brief turnout period of 7 to 10 days is sometimes useful. In 2-year-olds, a decision often is made to stop training and give 3 to 4 months of turnout rather than risk compensatory lameness or fracture. The decision to stop training a horse should not be taken lightly. Getting an older horse back to the same level of racing is often difficult, even with a planned turnout period, and jogging the horse three to four times a week to maintain condition and range of joint motion may be best. The older the horse is, the more difficult it is to return the horse to racing. Older horses with chronic lameness do not thrive with rigorous training and often come out of a solo training mile lamer than after schooling or qualifying races. Older horses often are raced into fitness rather than trained rigorously. A common mistake is to train or race these horses too often.
A complete neurological examination should be performed in any horse with gait deficits and even some with overt lameness, if neurological signs are noticed concomitantly. EPM is frequently diagnosed, but positive identification of the source of neurological signs is difficult to make because serum and cerebrospinal fluid analyses are not accurate (see Chapter 11). The immunofluorescent antibody test (University of California, Davis, California, United States) ascribes a numerical value (titer) to the levels of antibodies to the organisms causing EPM and appears to be more accurate than the Western blot technique, and results of this test have correlated better with clinical signs in STBs suspected of having EPM. A common method to manage horses when all else fails is to treat for EPM and observe the results. Some horses improve despite having no overt neurological signs.
Shoeing and Lameness
Shoeing to obtain ideal high-speed gait is an art, especially in trotters that are difficult to balance. The farrier must be a part of the lameness team. Veterinarians have to take a back seat to the trainer and farrier and cannot be overtly critical of the shoeing approach. Sore front feet are common, and many approaches are used. Sometimes a simple shoeing change redistributes load away from a sore area, and a common approach in trotters is a switch from a half-round to a flip-flop shoe (see Figure 109-5). Classically, trotters are shod with more weight up front, whereas pacers are shod with more weight behind. Recently the tendency has been to lighten shoe weight in trotters and pacers in front and behind. The typical hind shoe of a pacer (a half-round, half-swedge) has been replaced by an aluminum shoe with a low toe grab. Aluminum shoes are used commonly in front in pacers. In trotters, heavy front shoes may predispose to interference injury and carpal lameness, and now aluminum shoes often are used behind, allowing a lighter shoe to be used in front. Light aluminum shoes with grabs allow maximal track purchase and increase speed, but they may worsen existing OA of many distal joints behind and in front. A STB can jog and train abnormally with a sprung shoe or a broken bar shoe. Special attention should be given to the medial half of the front feet because interference bruising is substantial.
A low-heel, underslung foot is not common in modern day STBs, although low-heel, long-toe conformation was previously favored in the erroneous assumption that it would increase stride length. When combined with heavy shoes, long toes prolong breakover, increase stress on the dorsal aspect of the forelimb, and predispose the horse to lameness. Using a shorter toe and more upright front foot is a major improvement in trimming trotters.
Quarter cracks and other hoof wall defects are common. Acrylic and composite repair of hoof defects have aided many sore-footed STBs. Acrylic often is applied to augment the hoof wall. In horses with thin walls, shoes are difficult to maintain, especially when shoes may be changed every 2 to 3 weeks. Overzealous application of acrylic can weaken a normal hoof wall.
Specific Lameness Conditions of the Standardbred Racehorse
Front Foot Lameness
Front foot lameness is the most common lameness condition. Palmar foot pain abolished using palmar digital analgesia is a common finding, but the veterinarian should keep in mind that palmar digital analgesia also abolishes most of the pain associated with the DIP joint and toe and lower pastern regions. Occasionally, palmar digital analgesia can abolish pain associated with the fetlock joint. Palmar foot pain can be caused by a bruised heel, corns, sheared heel, hoof cracks, contracted heel, wall separations and gravel, stress remodeling and stress fractures, traumatic fractures, OA, or various combinations of these conditions.
Bruises, Corns, and Abscesses
Bruised feet can be caused by faulty conformation such as that seen in a large, flat-footed horse that develops bruising of the heel and bars. Small, narrow-footed horses are prone to quarter and heel cracks and a sore heel. Young STB feet are trimmed and pared and subjected to daily concussion on a firm and unforgiving surface. Aggressive paring can predispose to palmar sole bruising. Overt lameness may not be seen. Horses are often sore when starting from the barn and warm out of lameness after jogging a short distance. Because early carpal lameness can produce similar signs, careful hoof tester examination is necessary and often reveals profound sensitivity across the heel.
Base-wide, toed-out conformation causes overload of the medial heel bulb and quarter, and long, sloping pasterns cause overload of the palmar aspect of the foot. Shoes that are too narrow or those with short branches can cause sole bruising and corns. Horses that interfere (cross-firing or forging) are often shod with the inside branch of the shoe turned in to prevent grabbing and pulling of the shoe, and this can cause corns. Shoeing to correct interference is important but so is management of lameness that may lead to interference. Tubbing and soaking may compound the problem, creating a softer, more easily bruised sole. Poulticing may reduce inflammation initially, but continuous poulticing has the same undesirable result. The sole should be hardened with daily applications of an iodine-based paint, such as Rites paint, an iodine-ether preparation. Attention should be given to the stall bedding because an overly dry stall may lead to dry, cracking hoof walls. Digging out a bruise prolongs lameness and predisposes the hoof to abscessation. A wide web, concave inner surface steel bar shoe is applied if the horse can tolerate this much weight. A trainer may prefer a lighter aluminum bar or egg bar shoe. Full pads may afford protection for an upcoming race, but bruises cannot be reassessed, and sole paint cannot be applied. In trotters the flip-flop shoe is advantageous because the pad can be lifted and the sole painted, and without shoe branches the heel can spread. Deep-seated bruises can become corns; corns can fissure and crack; and bacterial invasion can cause infection. With abscessation, judicious paring to establish drainage is necessary, but the more sole that is removed, the longer it takes to heal. Soaking in warm water with Epsom salts (magnesium sulfate) and then wrapping with ichthammol (an iodine-based drawing salve) promotes drainage.
Sheared Heel
Quarter and heel cracks, wall separations, and a contracted heel can result from a sheared heel. Improper and asymmetrical rasping over time results initially in lowering of one heel bulb and later to vertical heel walls, a contracted heel, and flaring of the wall on the side of the lower heel bulb. With medial-to-lateral hoof imbalance, the vertical heel strikes the ground first, and uneven impact causes structural breakdown between the bulbs of the heel. The heel bulbs are painful, and little resistance is offered to digital displacement of the bulbs in opposite directions. Corrective shoeing involves shoeing the steep side full and floating the quarter. The flared wall is shod tight and rasped off over several trimmings. For a horse with a long-toe and underrun heel predisposed to sheared heel, the toe should be shortened and the heel maintained. Recurrent quarter and heel cracks are common sequelae.
Hoof Cracks
Hoof cracks, depending on location, are known as heel or quarter cracks. Cracks may begin at the coronary band or at the bearing edge of the hoof wall. If the quarter crack extends to the sensitive laminae, local tenderness and variable lameness result. Horses with dry, shelly feet or vertical walls are predisposed to quarter cracks. Untreated chronic inflammation, inappropriate rasping of the periople, and application of excessive acrylic predispose horses to dry feet because exposure of horn tubules results in loss of moisture. Indiscriminate cutting of bars predisposes horses to a contracted heel and results in vertical walls. A vertical wall is more likely to crack than a normal one. Quarter cracks can develop if horses are shod with the web of the shoe set in. To manage quarter cracks, weight bearing is prevented by floating, and artificial support to the weakened and cracked wall is applied using a full or egg bar shoe. Extensive, deep, or painful cracks are repaired and stabilized. Acrylic patches are now preferred, but the crack must be prepared by paring and drying with iodine paint or gentian violet; otherwise, infection may develop.
Contracted Heel
A contracted heel can result from palmar foot pain rather than cause it. Dry, brittle feet cannot expand normally and may contract, as does a foot that has a long toe and low heel. When faced with a choice, farriers too often pick a shoe that fits tight (narrow), rather than full (wide), when the horse really needs a size in between. The wall inevitably grows to the small shoe and contracts. The indiscriminate use of acrylic results in heel contraction because the material restricts expansion. Acrylic should be placed on the weight-bearing wall surface only to repair broken or brittle walls for nail placement or for rebuilding low heels. The last shoe nail should be placed at the bend in the foot quarter, rather than in a more palmar location, to prevent restriction of heel movement. Other causes of palmar foot pain reduce weight bearing at the heel, leading to contraction. To manage a contracted heel, the quarter is softened, the toe is shortened, and an extended bar shoe that fits full (wide) is applied. Lowering the heel to achieve frog pressure is contraindicated.
Wall Separation and Gravel
Gravel is caused by separation of the white line at the quarter and heel and bacterial invasion. Lameness, insidious at first, progresses to nearly non–weight bearing. Digital pulse amplitude is increased, and the horse responds intensely to hoof tester pressure over the affected area. The coronary band or heel bulb becomes sensitive just before infection breaks out. Local therapy such as soaking and poulticing may hasten coalescence and proximal migration of exudate. If pastern cellulitis occurs, broad-spectrum antimicrobial agents should be given. The horse is generally sound within 24 hours after drainage, but a full pad may be necessary to avoid repeat infection during wall healing. Wall separations and gravel are common complications to sheared heels and dry, brittle feet. Seedy toe is an infected wall separation at the toe.
Sidebone
Ossification of the cartilages of the foot (sidebone) is a rare cause of lameness. Ossification may be hastened in horses with poor hoof conformation, particularly in those with chronic medial to lateral hoof imbalance or in those in which interference injury occurs. Sidebone is found more often radiologically in aged horses with large, round, flat feet, but it may be seen incidentally in yearlings. If sidebone is painful to digital palpation, a bar shoe with heel clips and local subcutaneous injection of corticosteroids and Sarapin (High Chemical Company, Levittown, Pennsylvania, United States) may provide temporary relief. Interference injury may cause fracture and infection of a cartilage of the foot.
Fractures of the Distal Phalanx
Fractures of the distal phalanx occur most commonly in the LF lateral and RF medial palmar processes and are usually articular (Figure 108-4).7 Clockwise training and racing may account for asymmetrical location of fractures. Nonarticular palmar process and midsagittal fractures are rare. Predisposing factors include hard racing surfaces (most fractures occur during a race, more often in winter months), foot imbalance, impact on an uneven surface, and overloading. Fractures of the distal phalanx are unlikely single-event injuries and are the sequelae to maladaptive or nonadaptive remodeling of the distal phalanx that results from stress-related bone injury. IRU often is seen in the lateral aspect of the LF and medial aspect of the RF distal phalanx in horses with lameness abolished by palmar digital analgesia but in which radiographs are negative (Figure 108-5).8 Most fractures of the distal phalanx occur in aged horses. Treatment includes application of a wide web, concave inner surface steel straight or egg bar shoe with two side clips on each side. Horses are given 3 months of stall rest and then 3 months of turnout in a small paddock. Most fractures are complete but nondisplaced; mild displacement results in a step in the articular surface. Fractures take months to heal, and some appear to develop chronic nonunions, although many horses return to racing soundness even with a radiologically apparent nonunion. Distal phalangeal fractures in the hind feet are unusual to rare but generally involve the medial plantar process and are articular in location.5 OA of the DIP joint often occurs, particularly in horses with displacement or nonunion, but unless severe, prognosis for racing is good. Osteochondral fragments of the extensor process of the distal phalanx are unusual, but arthroscopic removal of small fragments and repair of large ones are indicated. Prognosis is fair, but OA of the DIP joint can affect prognosis negatively.
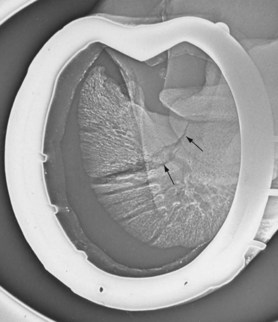
Fig. 108-4 Dorsomedial proximal-palmarolateral distal oblique xeroradiographic image of the right front foot of a Standardbred racehorse. There is a typical articular fracture of the medial palmar process (arrows) of the distal phalanx. The horse is shod with a bar shoe with clips.
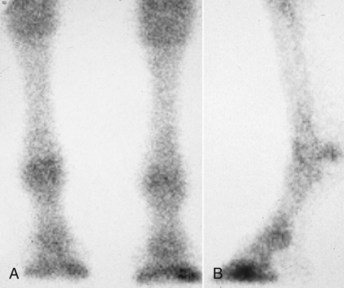
Fig. 108-5 A, Dorsal delayed (bone phase) scintigraphic image showing a typical distribution of increased radiopharmaceutical uptake of the Standardbred front feet. The left forelimb is on the right. B, Lateral delayed (bone) phase scintigraphic image of the left forelimb. This Standardbred was lame in the left forelimb, and lameness was localized to the lateral aspect of the distal phalanx. In the left forelimb, stress remodeling of subchondral bone of the distal phalanx was diagnosed. Increased radiopharmaceutical uptake involving the lateral aspect of the left forelimb and medial aspect of the right forelimb distal phalanx is thought to be caused by counterclockwise training and racing, and stress-related bone injury can lead to fracture in these locations.
Osteoarthritis of the Distal Interphalangeal Joint
The earliest sign of primary OA of the DIP joint is effusion. Effusion is also common in horses with nondescript foot soreness. Intraarticular injections of hyaluronan and corticosteroids are often performed into the DIP joint. Progressive OA can cause severe lameness, chronic fibrosis, and thickening of the DIP joint capsule, radiological evidence of proliferative changes on the dorsal aspect of the middle phalanx and extensor process of the distal phalanx, and narrowing of the DIP joint space.
Other Foot Lameness
Navicular disease is a rare cause of palmar foot pain. In 2-year-olds and early 3-year-olds, IRU in the navicular bone is seen in delayed (bone) phase scintigraphic images, indicating abnormal bone modeling, but rarely do radiographs show substantial changes, except for mild medullary increased radiopacity. Navicular bone fracture, cysts, and acute separation of bipartite navicular bone are diagnosed rarely in forelimbs and hindlimbs. Horses with bipartite bones or fractures have a poor prognosis, and palmar digital neurectomy is recommended. Keratomas in young racehorses are not seen, but they can occur rarely in broodmares or older STBs being used for alternative sporting activities.
Undiagnosed foot lameness—sore feet—is common. Horses have sensitivity to hoof testers and likely have soft tissue trauma, but a definitive diagnosis cannot be made. Treatment of the DIP joint with corticosteroids and hyaluronan, perineural injection of antiinflammatory agents, and shoeing changes are recommended.
Carpal Lameness
The carpus is the most common articular location for lameness and conformational faults. In 2-year-olds, carpal synovitis is common. High prevalence of carpal lameness is caused in part by racing young, immature STBs around tight turns on firm surfaces. The medial aspect of the middle carpal joint and the right carpus are predisposed to injury. Lateral injury of the carpus is unusual. Heat, effusion, and pain on careful palpation of the dorsal surfaces are common. Heat (the perception of warmth) on the dorsal aspect of the carpus is the earliest clinical sign of subchondral bone injury of the dorsomedial aspect of the middle carpal joint. Lameness varies with severity of injury, and horses carry the limb in an abducted position during advancement (see Chapter 38). Response to flexion varies, and diagnosis should be confirmed using intraarticular or median and ulnar analgesia. Secondary shoulder muscle soreness often develops. Horses warm out of lameness, and weeks to months may pass before consistent lameness is seen. Radiographs are usually negative or equivocal initially, but increased radiopacity of the third carpal bone and mild marginal osteophyte production can predispose the horse to small osteochondral fragments or slab fractures of the third carpal bone. The mere presence of increased radiopacity of the third carpal bone, however, is not diagnostic for subchondral bone pain because mild sclerosis is an adaptive response to race training (Figure 108-6). Diagnosis of subchondral bone pain as a result of maladaptive or nonadaptive remodeling is made using a combination of abnormal clinical and imaging findings. In a radiological study evaluating degree of increased radiopacity of the third carpal bone, exercised horses had significantly more increased radiopacity than nonexercised control horses, and lameness referrable to the middle carpal joint developed more commonly in STBs with higher degrees of third carpal bone increased radiopacity.9 Thirty percent of STBs in the study developed lameness of the middle carpal joint.9 In a separate study the same investigators determined the importance of middle carpal joint pain in STBs and found carpal lameness to be present in 28% of STBs overall and in 56% of those with forelimb lameness.10 Carpal lameness was the most common reason for more than 1 month of rest in STBs in race training. Few clinical signs such as effusion were present. Risk factors were faulty conformation and intense speed training.10 Diagnostic analgesia remains a most important aspect of clinical diagnosis, given the lack of early clinical signs associated with subchondral bone injury. Scintigraphic examination often reveals focal areas of IRU, usually involving the third carpal bone or the subchondral bone of the dorsomedial aspect of the middle carpal joint collectively; bilateral lesions are common (see Figure 19-16). Stress-related bone injury results in a continuum of subchondral and overlying cartilage damage, eventually leading to OA or osteochondral fragments. Rest is the best form of management but is usually unacceptable to trainers and owners. Topical counterirritation with iodine paints is still popular and is used with apparent success because blistering usually is accompanied by a reduction in exercise intensity. The administration of NSAIDs for 3 to 5 days and a brief period of reduced exercise (2 weeks) may be an acceptable compromise between the veterinarian and the trainer, but keep in mind that although a reduction in training intensity is helpful, bone cannot heal in 2 weeks, and pain may not subside. Intraarticular injections of hyaluronan or polysulfated glycosaminoglycans (PSGAGs) may reduce inflammation and theoretically may be useful in cartilage healing, but these often are used in a palliative rather than therapeutic manner, given a lack of synovitis in most horses. Injections may be of little benefit when pain originates from subchondral bone. Ten 2-year-old STBs with mild carpitis were treated with three to five weekly intraarticular injections with PSGAGs (Adequan, Luitpold Pharmaceuticals, Inc., Shirley, New York, United States) and were compared with a control group receiving NSAIDs and topical counterirritation.11 The treated group had substantially less carpal lameness during the ensuing racing season. All horses raced, but horses in the control group required intraarticular injections to maintain soundness. Early aggressive intraarticular therapy may forestall development of progressive OA in young STBs. Extracorporeal shock wave therapy has gained popularity as an adjunctive therapy in the management of STBs with subchondral bone injury and OA. With the exception of a palliative analgesic effect, the role of this modality in potentiating healing remains unknown. The possibility exists that as a result of the analgesic effect horses could be continued in training well past the ability of injured bone to adapt.

Fig. 108-6 Dorsoproximal-dorsodistal digital radiographic image of the right distal row of carpal bones in a 2-year-old Standardbred filly that was sound and racing successfully at the time of this radiological study conducted as part of an examination before purchase (medial is to the right). Mild-to-moderate increased radiopacity of the radial fossa (between arrows) is seen as an adaptive response to training and racing. This filly continued to race successfully for the remainder of the 2- and 3-year-old racing years.
Palmar foot pain may play a role in the development of carpal lameness in young STBs. Early carpal lameness is easier to treat if palmar foot pain is recognized early and managed aggressively. In horses with bruised bars and poor medial-to-lateral hoof balance, the application of wide web bar shoes reduces inflammation and signs of carpal lameness. In all ages of trotters, the flip-flop shoe appears to be effective in reducing clinical signs of carpal lameness. Small osteochondral fragments of the carpus are the most common fractures and involve the third and radial carpal bones and rarely other bones in the middle carpal and antebrachiocarpal joints. Arthroscopic surgical removal and PSGAG therapy after surgery are recommended. Frontal (dorsal) and sagittal slab fractures occur commonly, and repair using screws placed in lag fashion is recommended. Small, frontal slab fracture fragments can be removed. Although rest is an option in horses with nondisplaced fractures, internal fixation may shorten recovery period and reduce risk of recurrence (see Chapter 38).
Metatarsophalangeal Joint Lameness
The metatarsophalangeal joint is a common source of pain causing lameness in STBs, and diagnostic analgesia is usually essential for diagnosis.
Stress and Maladaptive or Nonadaptive Remodeling
Stress and maladaptive or nonadaptive remodeling of the metatarsophalangeal joint most often involves the distal, plantarolateral aspect of the MtIII, PSBs, and the proximal aspect of the proximal phalanx (see Chapters 19 and 42).6,12 Initially the horse has a variable, subtle, high-speed lameness, most commonly manifested around turns or by the horse making breaks. Later, grade 1 to 2 of 5 hindlimb lameness is seen at the trot in hand. Lameness can be localized to the metatarsophalangeal joint, but it does not improve with intraarticular treatment. Palpation findings are negative or equivocal. Horses show variable responses to flexion and have negative radiological findings but positive responses to diagnostic analgesia. The low plantar or lateral plantar metatarsal block is most effective, but horses may respond partially to intraarticular analgesia (and may require 12 mL of local anesthetic solution). Later, increased radiopacity and radiolucent changes of the plantarolateral aspect of the MtIII are seen on down-angled radiographic images. Ultrasonographic evaluation may reveal a defect in articular cartilage late in the disease process. Scintigraphic examination is the best way to establish a diagnosis and shows focal IRU involving the distal aspect of the MtIII (see Figure 19-6Figure 19-20Figure 42-1Figure 42-2Figure 42-3Figure 42-6Figure 42-7Figure 42-8Figure 42-9). The disease can affect both hindlimbs. The distal aspect of the MtIII appears at risk to develop stress-related bone injury before other sites in the metatarsophalangeal joint, possibly from anatomical variations or uneven loading during the full extension and landing phases of the stride. Shoe additives such as calks or grabs may play an adverse mechanical role. The metatarsophalangeal joint is a high-motion joint and subject to high-strain cyclic fatigue (repetitive loading) that is encountered during intense exercise around turns and on hard surfaces. This continuum of stress-related bone injury can lead to OA and fracture (see Chapter 42).
Exercise intensity is reduced for 1 to 3 weeks. If lameness is prominent, a 3- to 4-month rest period is necessary. Exercise reduction allows the modeling and remodeling processes to equilibrate and microdamage to heal. A flat shoe is applied or the horse is left bare footed. Cold water therapy and the administration of NSAIDs (phenylbutazone or acetylsalicylic acid) appear helpful initially. Intraarticular injections of hyaluronan and PSGAGs may help, but early in disease, overlying cartilage damage and synovitis are not prominent, and response to intraarticular injections is minimal. When radiolucent changes and synovitis develop, response to intraarticular injections is better, but prognosis is worsened. Extracorporeal shock wave and radial pressure wave therapy may be useful in providing partial analgesia and may prolong training and racing. Bisphosphonate therapy is currently used for many conditions, including subchondral bone pain, OA, and other bone-related problems, but efficacy is unknown (see Chapter 42, page 490). In TBs there is a higher risk of catastrophic breakdown than in STBs, although the wisdom of training and racing a STB with chronic pain is certainly debatable. Whenever possible, frank advice must be given to trainers and owners about the long-term sequelae of continued training and racing a STB with a condition that may lead to OA.
Fractures
Acute, severe lameness is seen most commonly in STBs with fractures of the metatarsophalangeal joint, but some horses can race with incomplete fractures. Horses shorten the cranial phase of the stride, land on the toe, and rapidly compensate with other limbs. Often no effusion or pain on flexion is apparent unless a fracture is displaced. Diagnostic analgesia and examination in harness are avoided if a fracture is suspected because comminution or displacement can occur. Radiographs, including flexed dorsoplantar or 125° dorsoplantar and flexed lateromedial images, should be obtained.
Midsagittal fractures of the proximal phalanx are most common, causing severe intermittent or severe unrelenting lameness, depending on fracture length and configuration. Fractures can be short, incomplete with mild periosteal proliferation on the dorsal aspect of the proximal phalanx (Figure 108-7) or long, incomplete or complete midsagittal fractures, fractures that break out of the lateral cortex, and comminuted fractures (see Figure 36-10). Horses with short, midsagittal fractures often race or train because lameness is intermittent and often abates after several days. Clinical signs precede radiological evidence of fracture for 7 to 21 days, and scintigraphic examination reveals focal IRU in the proximal aspect of the proximal phalanx (see Figure 19-20, C). Horses with short, midsagittal fractures can be rested or have internal fixation and have a good prognosis with either treatment.13 Long incomplete, complete, displaced, or comminuted fractures should be repaired. Prognosis depends on degree of comminution and displacement and whether a strut of bone is intact to which to attach fragments. Horses with comminuted fractures rarely race again and are at risk of infection, fracture displacement, and OA of the metatarsophalangeal and proximal interphalangeal joints and contralateral limb laminitis (see Chapter 35).

Fig. 108-7 Dorsoplantar (A) and flexed lateromedial (B) xeroradiographic images showing a short, incomplete, midsagittal fracture of the proximal phalanx (arrow). There is slight periosteal new bone on the proximodorsal aspect of the proximal phalanx seen in the flexed lateromedial image (white arrow). Radiological changes often lag behind clinical signs, and follow-up radiological and scintigraphic examinations often are needed to establish a diagnosis.
Dorsal plane (frontal) fractures of the proximal phalanx can be unilateral or bilateral, are most common in the RH, and occur in trotters and pacers (see Figure 42-11 and accompanying text). Fractures of the PSBs are common and most often involve the lateral PSB. Small medial abaxial fragments can be difficult to identify. Apical PSB fractures are most common, but abaxial, midbody, and rarely basilar fractures occur, and the combination of suspensory desmitis, and splint bone and PSB fractures is not uncommon. Horses show acute lameness after training or racing, with grade 3 to 4 of 5 lameness, and prefer to bear weight only on the toe. Effusion and a positive response to flexion are usually present, and the diagnosis is confirmed radiologically. Ultrasonographic examination of the SL should be performed to establish baseline information and assess prognosis. Surgical removal of apical, abaxial, and basilar fragments and surgical repair of displaced midbody fractures using bone screws or wiring techniques are recommended. Prognosis is guarded in trotters and fair in pacers that have raced before fracture. Horses in which fractures occur early in training appear to have a poor prognosis. Of 43 STBs with apical PSB fractures no difference in prognosis was found between pacers and trotters; 86% of fractures involved the hindlimbs. Prognosis was better in STBs with hindlimb PSB fractures than with forelimb injuries. Eighty-eight percent of horses that raced before injury raced after injury, whereas only 56% of those previously unraced raced after injury. Neither fracture fragment dimensions nor associated suspensory desmitis negatively affected outcome.14 These latter two findings are surprising given our experience.
Condylar fractures of the McIII or the MtIII occur, and fractures of the lateral condyles are more common than those of the medial condyles. Medial condylar fractures of the MtIII outnumber those occurring in the McIII. Clinical signs are similar to those caused by midsagittal fracture of the proximal phalanx, but diagnosis can be difficult unless good-quality radiographs with appropriate views are obtained. A flexed dorsoplantar or 125° dorsoplantar image should be obtained. Medial condylar fractures often spiral proximally and should be repaired, although even with repair there is a risk of catastrophic failure of the bone. In general, lateral condylar fractures of the McIII or the MtIII are best managed using surgical fixation, although STBs with short, incomplete fractures can be successfully managed conservatively. Regardless of management method, prognosis is favorable; 12 of 13 STBs with incomplete condylar fractures of the MtIII and 7 of 9 with incomplete condylar fractures of the McIII raced after injury.15 Four of six surviving horses with medial spiral fractures of the MtIII raced after injury.15 In that study, TBs were overrepresented and STBs were underrepresented when compared with the hospital population; TBs had significantly more lateral condylar fractures and forelimb condylar fractures than did STBs.15
Osteochondrosis
The metatarsophalangeal joint is a major site for osteochondrosis, and the most common manifestation is plantar fragmentation. A complete discussion of axial, articular fragments and abaxial, nonarticular fragments and other forms of osteochondrosis can be found in Chapter 42. Some debate exists over the management of STBs with axial, articular fragments and abaxial, nonarticular fragments and other fragments. Horses with axial, articular fragments and dorsal fragments respond well to arthroscopic removal and postoperative intraarticular injections of PSGAGs or hyaluronan. We believe that surgical removal prolongs racing careers and decreases metatarsophalangeal joint lameness. Some horses, particularly pacers, race successfully without surgery.
Proliferative synovitis, radiolucent defects of the PSBs, traumatic small osteochondral fragments of the proximal phalanx, and OA are discussed in Chapter 42.
Distal Hock Joint Pain and Other Tarsal Lameness
The hock joint is under considerable stress and strain, especially going into turns and with quick acceleration. Distal hock joint pain and progressive OA of the TMT and CD joints are common. However, distal hock joint pain should not be a default diagnosis, and careful lameness examination, including diagnostic analgesia, should always be performed. Injection of the “knees and hocks” is commonplace in the STB sport, despite our experience highlighting the importance of the metatarsophalangeal joint as a cause of hindlimb pain. Horses with distal hock joint pain warm out of lameness, often dramatically, because they may come out of the barn or paddock on the toe and eventually be able to train or race successfully. Horses show a mildly shortened cranial phase of the stride and a stabbing type of gait, with medial deviation of the limb during protraction and landing first on the outside toe (stabbing laterally), but this gait is not pathognomonic for distal hock joint pain. Palpation in a flexed position often reveals pain of periarticular soft tissue structures, and the Churchill test is often positive. Upper limb flexion is positive, but diagnostic analgesia is essential for diagnosis. Radiographs may show evidence of OA in older horses, but radiographs are negative or equivocal in most 2- and 3-year-olds. Changes are seen most often in the DM-PlLO image, but dorsoplantar, lateromedial, and slightly off dorsoplantar images can be helpful. Scintigraphic examination confirms that OA of the TMT joint is most common, and changes are lateral and dorsolateral (Figure 108-8). Focal IRU is sometimes seen involving only the CD joint in horses that failed to respond to intraarticular analgesia of the TMT joint, emphasizing the need to block and treat each joint separately.

Fig. 108-8 A, Plantar delayed (bone) phase scintigraphic image of the hocks. There is focal, nucleate (right) and intense (left) increased radiopharmaceutical uptake in the dorsolateral aspect of both tarsometatarsal joints (left hindlimb is on the left) in this 2-year-old Standardbred filly. B, Dorsomedial-plantarolateral oblique xeroradiographic image of the left hindlimb showing minimal changes (arrow). Lameness and scintigraphic evidence of distal tarsitis precede radiological changes by many months.
Treatment comprises intraarticular injections, NSAIDs, shoeing changes, and rest. Early, intraarticular hyaluronan is useful to decrease inflammation, and concomitant use of NSAIDs such as phenylbutazone (4.4 mg/kg PO daily for 5 days and 2.2 mg/kg PO daily for 5 days) is recommended initially. Later, as OA progresses, methylprednisolone acetate (80 mg/joint every 6 to 8 weeks) is most effective to manage inflammation. A series of intraarticular and intramuscular injections of PSGAGs also can be given. In horses with severe OA, 4 to 6 months of rest is successful, but recurrent lameness often mandates a limited racing schedule (10 to 15 starts/year). The toe is shortened, and a flat aluminum or steel squared-toe shoe is applied to allow easy breakover. All shoe additives are removed to decrease shear stress.11
Slab fractures of the third tarsal bone and fractures of the proximal, dorsomedial aspect of the MtIII result from stress-related bone injury or from pathological fractures in horses with OA (see Chapter 44). Third tarsal bone fractures are the most common and are best seen on a DM-PlLO image. Fractures of the central tarsal bone are usually oblique, involve the dorsal aspect of the bone, occur without concomitant OA, and are best seen in lateromedial images. Conservative management is recommended in horses with nondisplaced fractures, but displaced fractures should be repaired. Ninety-two percent of horses with slab fractures of the third tarsal bone and 88% with slab fractures of the central tarsal bone raced after conservative management.16
The tarsocrural joint is often injected, but tarsocrural joint lameness is uncommon, except in young horses with osteochondrosis. Trainers often request injection of the upper and lower hock joints (tarsocrural and TMT joints), but lameness most likely is caused by pain associated with the distal hock joints. Bog spavin occurs most commonly in weanlings and yearlings, and radiological identification of osteochondrosis fragments prompts surgical removal. Most yearlings begin training without fragments. Although debate exists about the importance of tarsocrural osteochondrosis and lameness, we recommend surgical removal to resolve current inflammation, if present, and to prevent future lameness. However, osteochondrosis fragments are seen in some older racehorses in which neither lameness nor effusion is present. Tarsocrural lameness may occur without effusion, and diagnostic analgesia is necessary to differentiate the site of hock pain. Good-quality radiographs are essential to discover occult osteochondrosis fragments and fractures. The DM-PlLO image is best for evaluating the cranial aspect of the intermediate ridge of the tibia and a slightly oblique dorsoplantar image (dorsal 5° to 7° lateral-plantaromedial oblique) is best to evaluate the medial malleolus. The most common sites for osteochondrosis are the cranial aspect of the intermediate ridge of the tibia, lateral trochlear ridge of the talus, medial malleolus of the tibia, medial trochlear ridge of the talus, and lateral malleolus of the tibia. Medial malleolar fragments appear to be increasing in importance, particularly in trotters, although a heightened awareness and improved imaging may be uncovering fragments in this location that may have previously been missed. Osteochondrosis fragments can be large, numerous, loose, and free floating, and cartilage damage can be prominent even in yearlings; however, prognosis is good with removal. If distention of the tarsocrural joint is unexplained, osteochondrosis of the medial malleolus of the tibia should be suspected, and diagnostic arthroscopy is recommended. Small osteochondrosis fragments (dewdrop lesions) of the distal aspect of the medial trochlear ridge of the talus may be incidental but can cause lameness if displaced or if impinging on the central tarsal bone. Surgical removal is recommended.
Tarsocrural OA occurs in older horses (usually >5 years) and may be associated with osteochondrosis because fragments often are seen concomitantly. OA causes progressive lameness and effusion, but intraarticular analgesia should be performed to validate the source of pain. Large volumes of local anesthetic solution (30 to 50 mL) are necessary because pain is severe; false-negative responses occur if 10 to 15 mL is used. Radiographs may reveal prominent increased radiopacity and narrowing of the tarsocrural joint space, but end-stage OA can be present with only subtle radiological abnormalities (Figure 108-9, A). Scintigraphic evaluation reveals diffuse IRU on both sides of the tarsocrural joint and is useful to differentiate OA from sagittal fracture of the talus (Figure 108-9, B) or subchondral injury of the distal aspect of the tibia. Prognosis is grave.

Fig. 108-9 A, In this dorsomedial-plantarolateral oblique xeroradiographic image, the tarsocrural joint space is narrow, indicating end-stage OA of the tarsocrural joint, but this radiological sign is difficult to recognize because proliferative changes are minimal. B, Flexed lateral delayed (bone) phase scintigraphic image of a different Standardbred with a sagittal fracture of the talus. With flexion, the area of moderate to intense increased radiopharmaceutical uptake moves with the talus and can be differentiated clearly from end-stage osteoarthritis (OA) or distal tibial subchondral trauma.
Sagittal fracture of the talus is unusual. Acute, grade 3 to 4 of 5 lameness is localized to the tarsocrural joint by diagnostic analgesia, but often subtle tarsal lameness precedes fracture. Focal IRU is seen involving the talus (see Figure 108-9, B), and slightly oblique dorsoplantar images reveal subchondral lucency or fracture. Eight of 11 horses with sagittal fracture of the talus were STBs, and 7 raced after being managed conservatively.17
Enthesitis of the long, lateral collateral ligament of the tarsocrural joint, on the lateral aspect of the calcaneus, results in mild to moderate lameness and mild tarsocrural effusion (Figure 108-10). Soft tissue swelling is easy to miss initially, and radiological changes lag behind clinical signs for at least 14 to 21 days; however, lameness abates or is improved considerably with tarsocrural analgesia. Scintigraphic examination reveals focal IRU in the lateral aspect of the calcaneus. Local injections and radiation therapy may allow continued racing, but rest to allow enthesitis to subside is often necessary.

Fig. 108-10 A, Lateral delayed (bone) phase scintigraphic image of a hock showing focal, moderate to intense increased radiopharmaceutical uptake in the calcaneus. B, Dorsoplantar xeroradiographic image showing proliferative changes associated with the collateral ligament attachment on the lateral aspect of the calcaneus (arrows).
Injury of the fibularis tertius tendon anywhere from the midcrus to the distal tarsus can occur but is rare, and injury usually occurs at the insertion on the MtIII and the third tarsal bone. Soft tissue swelling is present, and the hock can be pushed forward without concomitant extension of the stifle with the limb in standing position. Horses require 4 to 6 months of rest.
Inflammatory synovitis or infection of the tarsocrural joint is not uncommon. Prognosis depends on the extent of existing cartilage damage and the financial ability of owners to manage infection aggressively (see Chapter 65).
Suspensory Desmitis
Suspensory desmitis is the most common soft tissue injury and can be classified as unilateral branch desmitis, bilateral branch desmitis, body desmitis, and PSD. Suspensory desmitis is often an overload compensatory lameness condition because fatigue and improper landing occur in lame horses. Suspensory desmitis is seldom a single-event injury but is caused by accumulated damage over weeks to months (see Chapter 72). Diagnosis is made by careful palpation from the origin to the insertion of the SL with the limb in standing and flexed positions. The splint bones and PSBs are examined for associated injuries. One of us (JBM) has found that horses with core lesions are lamer, but exhibit fewer outward signs of inflammation, than those with peripheral lesions. Horses with suspensory branch desmitis are common and heal quicker (6 to 8 weeks) with lower recurrence than do those with body desmitis and PSD (4 to 6 months). Core lesions recur frequently. Because suspensory desmitis is often a compensatory injury, the primary lameness needs to be resolved. For example, OA and osteochondral fragments of the left carpus frequently cause suspensory desmitis of the RF in horses of both gaits, RH suspensory desmitis in trotters, and LH suspensory desmitis in pacers.
Ultrasonographic examination is critical in assessing the SL, and its entire length should be examined systematically. In hindlimbs, enlargement of the origin and body is more common than core lesions, and cross-sectional area measurements of the affected and contralateral limb are mandatory. Branches are evaluated for change in shape, loss of margin definition, central or marginal hypoechoic lesions, subcutaneous hemorrhage and edema, fibrosis and calcification, irregular contour (step line defects), and avulsion fragments of the PSBs. The intersesamoidean ligament rarely is involved.
Forelimb unilateral branch desmitis results from toed-in or toed-out conformation, hoof imbalance, and uneven landing. To correct interference injury with knee knocking resulting from toed-out conformation, the hoof is commonly lowered on the inside, causing uneven loading and medial unilateral branch desmitis, whereas in horses with toed-in conformation, lateral unilateral branch desmitis occurs. Improper impact can occur from fatigue or if a horse is stopped suddenly. Lameness varies with severity of injury and presence of associated splint and PSB disorders.
Forelimb bilateral branch desmitis is caused by acute or chronic hyperextension of the metacarpophalangeal joint. Prognosis depends on the degree of fetlock drop seen when the contralateral limb is held in flexion. Concomitant PSB fractures can occur. Dorsal subluxation (flexion) of the proximal interphalangeal joint is seen in horses with bilateral branch desmitis and body desmitis, whereas palmar subluxation (extension) is seen in horses with distal sesamoidean desmitis and loss of palmar support. If the axis of the proximal interphalangeal joint is altered, the prognosis for racing is poor.
Forelimb body desmitis often begins just proximal to the bifurcation of the SL, and careful palpation reveals pain and mild enlargement. The first sign may be mild swelling, without lameness, and training and racing are often continued, leading to further suspensory desmitis. Horses often race successfully with chronic suspensory branch desmitis, but if desmitis progresses into the body, lameness becomes pronounced. There is a considerable difference in the potential for catastrophic breakdown injury with branch desmitis between TBs and STBs. Rarely, a STB develops catastrophic injury of the suspensory apparatus as a result of chronic suspensory desmitis, whereas continued racing with any suspensory branch desmitis is dangerous in TBs. Chronic enlargement and thickening of the SL often cause bowing of the splint bones, and concussion leads to fracture. Horses with recalcitrant swelling of the SL should be examined with ultrasonography because exuberant exostosis from fractures may encroach on the SL and cause swelling and pain.
Proximal palmar metacarpal pain is common and often called a check ligament problem, although genuine desmitis of the accessory ligament of the DDFT is rare. Palmar metacarpal pain can be caused by avulsion or longitudinal fracture of the McIII and stress reaction/stress fracture of the McIII, but PSD is most common. STBs often have pain on palpation of the proximal palmar metacarpal region and may have compensatory PSD, with primary lameness elsewhere. Lameness is noticed in the first half of the support phase of stride. An exaggerated head nod is often noted (JSM). A carpal type of gait may be seen. Lameness is most prominent when the affected limb is on the outside of a circle. Local analgesia and ultrasonographic examination should be performed. Radiographs are necessary to identify bone injury. Scintigraphic examination is useful to differentiate proximal metacarpal pain from carpal pain.
In hindlimbs, unilateral branch desmitis, bilateral branch desmitis, body desmitis, and PSD occur but less frequently than in forelimbs. Degree of lameness varies, and similar concerns exist about the MtIII, a splint bone, and a PSB involvement. Horses often land on the toe and are reluctant to put the heel down, especially if a concurrent pathological condition of the PSB exists. Suspensory branch desmitis often occurs first and can be managed successfully with continued work in some horses, but proximal progression toward the bifurcation and body causes substantial increase in lameness and may involve the splint bones, and often horses lose support of the metatarsophalangeal joint. Racing can no longer continue. Hindlimb suspensory desmitis is particularly important in young trotters. Many top 2- and 3-year-old trotters have been retired because of hindlimb suspensory desmitis. Second to carpal lameness, hindlimb suspensory desmitis is the most dangerous, career-limiting cause of lameness in trotters.
Early PSD can go unrecognized because of lack of obvious swelling. Local analgesia is critical for diagnosis. Once desmitis involves the body, swelling may be recognized, but damage is now extensive.
Inflammation can be suppressed, but rest is essential for healing. Rest is not well received by owners and trainers, who often exert pressure to keep a horse in work. Cryotherapy is used to manage horses with suspensory branch desmitis and distal body desmitis. Horses with marginal lesions respond well but not those with core lesions. Cryotherapy decreases pain and seems to promote more or better-organized scar tissue. Periligamentous injections of sclerosing agents such as sodium oleate promote fibrosis and can be used to cause a swollen SL to “set up.” Periligamentous injections of corticosteroid mixtures reduce inflammation and lameness, but if training and racing continue, further damage occurs. Many naive owners lack understanding that the latest popular injection does not promote healing but simply masks inflammatory signs. Although horses may continue to race a few more starts, further damage inevitably occurs. Horses with PSD often can be managed using injections of corticosteroids, internal blisters, and, if available, radiation therapy, and if lameness is mild and support is not lost, racing may continue. Shock wave therapy has gained prominence and shows promise.
Rest is the best approach, and there is no substitute. Between 3 to 6 months of rest may be necessary to allow healing. A combination of stall rest, handwalking, walking in the jog cart, and swimming is recommended. We do not recommend turnout, but many horses are blistered and turned out, although this has been shown to be detrimental to healing. Healing progress is assessed by ultrasonography. Surgical management using a modified Asheim approach (ligament splitting, or desmoplasty) and ostectomy of fractured splint bones and PSB fragments is recommended. Desmoplasty and injection of fresh liquid bone marrow have been used successfully (MWR). Other intraligamentous injections with products such as platelet-rich plasma and stem cells have shown modest success. One of us (MWR) has performed bone marrow injection and fasciotomy on a limited number of top trotters with hindlimb PSD and body desmitis with modest success.
Prognosis depends on level of injury, gait (trotters worse than pacers), severity of injury (poor prognosis with fetlock drop), and associated bony pathological conditions. Unless the SL is totally disrupted, prognosis for racing is good, but racing class is an important consideration because few STBs return to the same or improved race class after sustaining suspensory desmitis (Figure 108-11).

Fig. 108-11 Images of a 3-year-old Standardbred colt pacer in May after being trained and qualified for racing; the colt had won divisional honors the previous year but developed substantial (3 of 5) left hindlimb lameness as a result of complex injury in the proximal plantar metatarsal region. A, Delayed phase lateral (left) and plantar scintigraphic images showing focal, intense increased radiopharmaceutical uptake in the proximal, plantar aspect of the third metatarsal bone (MtIII) indicative of bony injury at the origin of the suspensory ligament (double-headed arrow). B, Dorsoplantar digital radiograph (lateral is to the left) of the left proximal metatarsal region showing increased radiopacity (arrow) and mild radiolucency (arrowhead) of the MtIII; neither avulsion nor longitudinal fracture was seen, but changes of this magnitude in bone indicate the lesion is chronic. C, Transverse (left) and longitudinal ultrasonographic images acquired with the transducer medial to the plantar midline showing enlargement (double-headed arrow) of the proximal aspect of the suspensory ligament (cross-section area measured 2.4 cm2) and a large hypoechogenic region (arrowheads). This colt was retired from racing.
Metacarpophalangeal Joint Lameness
Fatigue from underconditioning and other factors causing overload may lead to hyperextension of the metacarpophalangeal joint. Hyperextension leads to injury of the dorsal aspect of the joint, such as small osteochondral fragments of the proximal phalanx and proliferative synovitis, and to injury of the palmar aspect of the joint, such as fractures of the PSBs and suspensory branch insertional injury. Traumatic disruption of the suspensory apparatus is rare but usually involves rupture of the SL. Stress-related bone injury of subchondral bone leading to OA and fracture occurs in the metacarpophalangeal joint, as described for the metatarsophalangeal joint. In a STB with normal conformation, metacarpophalangeal effusion should be a red flag (a barometer), often a sign of compensatory lameness. Young horses often have bilateral metacarpophalangeal synovitis secondary to palmar foot pain because toe-first landing overloads the joint. Corrective trimming and shoeing often helps. In older horses unilateral carpal lameness often causes contralateral metacarpophalangeal synovitis. Primary lameness of the metacarpophalangeal can begin when horses break stride, stumble, or stop quickly.
OA and stress-related bone injury are the most common problems of the metacarpophalangeal joint. Early radiographs are usually negative, but radiolucency and increased radiopacity of the distal medial aspect of the McIII develop later. Scintigraphic evidence of IRU is more prominent medially, unlike in the metatarsophalangeal joint, in which IRU is more common laterally. In older horses (about 4 years of age) with progressive severe OA, narrowing of the medial joint space indicates severe cartilage damage. Owners are incredulous that the horse has end-stage OA because lameness can be acute and severe, and fracture often is suspected.
Early OA is treated using intraarticular injection of hyaluronan alone or a combination of hyaluronan and PSGAGs. The latter is preferred, and three to four weekly injections are combined with a reduction in exercise. Horses that do not respond may have proliferative synovitis, usually seen in older horses with chronic OA. Injecting the joint in the dorsal pouch may be difficult, and little synovial fluid may be present. Surgical resection of synovial pads and postoperative intraarticular injections of PSGAGs are recommended.
Fractures and osteochondritis dissecans occur, but palmar fragments are rare (see Chapter 36).
Splint Bone Disease
Exostoses and Fractures of the Second and Fourth Metacarpal Bones (Splints)
Splints are a common problem in 2- and 3-year-olds (see page 1018). Poor conformation and hard track surfaces predispose horses to splints. Whether tearing of the interosseous ligaments occurs is unknown. Medial splints are most common. Yearlings can begin training with dormant, so-called field splints that become active as training advances. Splints rarely cause severe head nodding lameness, but put a horse on a line and signs become worse as work progresses. Splints on the abaxial surfaces of the McII and McIV are visible and can be palpated readily, but those on the axial surfaces require the limb to be lifted to relax the SL. Axially-located splints cause more obvious lameness than do abaxially-located splints.
Management includes reducing inflammation and limiting callus. Cold-water therapy and poultice should be applied, and horses are given NSAIDs. Blistering and external heat therapy may be contraindicated if reduction in the size of the callus is desirable. Ionophoresis with corticosteroids is successful. Perilesional injection of corticosteroids and cryotherapy are used successfully. Cryotherapy is a common therapeutic option often performed in STBs, but after the procedure local pain and inflammation persist, complicating palpation during reexamination. In these STBs, resolution of signs of lameness or other horse-related factors, such as a reduction or cessation of being on a line, is often used as evidence of clinical improvement. Cryotherapy may need to be repeated, and if necessary additional local therapy can be given once cutaneous sores from the procedure heal. If signs fail to abate, a fracture may be present. Improper toe-heel impact and medial-to-lateral hoof imbalance predispose horses to splints. Chronic splint disease in older horses is almost always related to palmar foot pain. Aggressive therapy for palmar foot pain and restoring normal hoof strike is critical. Direct trauma from interference and breaking must be prevented.
Fractures of the McII and the McIV can be caused by direct trauma. Interference injury can cause fracture of the McII, and accidents involving carts and other equipment predispose horses to fractures of the McIV. If fractures are located proximally and displacement exists, surgical fixation using small plates and screws is best. McIV fractures can heal functionally without fixation. Most distal splint bone fractures are secondary to suspensory desmitis. Exuberant callus can impinge on the SL. Fracture callus and fragments should be removed.
Exostoses and Fractures of the Second and Fourth Metatarsal Bones
Exostoses most commonly involve the MtII, but chronic painful splint exostoses are not as common as in the forelimb. Perilesional corticosteroid therapy is recommended (80 mg of methylprednisolone and 8 mL of Sarapin, (High Chemical Company). Fractures of the MtII and the MtIV occur occasionally and usually result from direct trauma, but distal splint fractures can be secondary to suspensory branch desmitis. Fracture fragments should be removed.
Stifle Joint Lameness
The stifle joint often is incriminated as a source of pain, but diagnostic analgesia identifies a problem in the more distal part of the limb. OA of the medial femorotibial joint is the most important stifle lameness, but osteochondrosis should be considered in young horses. OA is a progressive disease beginning in late 2-year-olds, and degree of lameness varies from grade 1 to 4 of 5. Distention of the medial femorotibial joint capsule is an important finding, but in some STBs this is a subtle finding. The limb may be carried forward slightly lateral or outward during the cranial phase of the stride. The cranial phase is shortened, and lameness is worse in the turns. Radiographs are usually negative or equivocal in 2-year-olds, and arthroscopic evaluation reveals generalized cartilage thinning and fissure formation. Later, in caudocranial radiographic images, narrowing of the medial femorotibial joint space and mild osteophyte formation on the proximal medial aspect of the tibia and distal medial aspect of the femur are visible (Figure 108-12, A). Scintigraphic examination can confirm extensive OA. Diffuse IRU involves both sides of the medial femorotibial joint and is best seen in a caudal image, although if extensive IRU can be seen in a lateral image as well. Arthroscopic evaluation at this time reveals exposed subchondral bone and severe synovitis, but therapeutic value of arthroscopy is negligible. If the diagnosis of OA is made in a 2-year-old, a period of 3 to 4 months of rest is recommended. The stifle joint often is injected in horses without stifle lameness, and few untoward effects are seen. Treatment of STBs with OA of the medial femorotibial joint with methylprednisolone acetate is contraindicated early in the course of the disease. Although the drug is effective and allows continued racing, OA can progress rapidly, resulting in severe lameness. Hyaluronan (40 mg) and isoflupredone acetate (4 to 6 mg) or triamcinolone acetonide (4 mg), interleukin-1 receptor antagonist protein, or PSGAGs (750 to 1000 mg) are preferred, and although they are less effective than methylprednisolone acetate, they decrease inflammation and prolong the racing career. Systemic administration of PSGAGs or hyaluronan is helpful. Methylprednisolone acetate is necessary for older horses with advanced OA, but if no improvement is seen, the racing career is usually over (see Figure 108-12, B). Once severe lameness occurs, rest may improve comfort slightly, but horses will not tolerate training again. Trotters can tolerate racing with more advanced OA than can pacers.
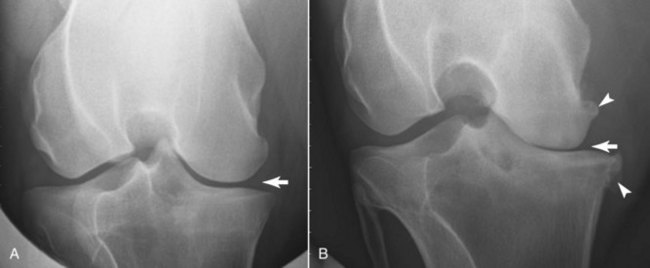
Fig. 108-12 A, Caudocranial digital radiographic image of the left stifle of a 4-year-old Standardbred (STB) trotter with marked narrowing of the medial femorotibial joint (MFTJ, arrow). Radiological evidence of narrowing on a well-positioned caudocranial image is the earliest sign of osteoarthritis (OA) of the MFTJ. B, Advanced OA of the MFTJ is seen in this caudocranial image of a 9-year-old STB pacer. Absence of an obvious MFTJ space (arrow), marginal osteophyte formation (arrowheads) of the distal, medial aspect of the femur and proximal medial aspect of the tibia, and radiolucency of the distal aspect of the medial femoral condyle can be seen. This horse was 4 of 5 lame in the left hindlimb, and the prognosis for racing is grave.
In young horses osteochondrosis can cause lameness and effusion in early training, prompting radiographic examination, but signs of osteochondrosis often are seen in weanlings and yearlings, and surgery is performed before training begins. Osteochondritis dissecans of the lateral trochlear ridge of the femur is most common; it causes considerable effusion of the femoropatellar joint and if bilateral may cause a bunny-hopping gait. Surgical treatment, 4 to 6 months of rest, and intraarticular therapy are recommended. Prognosis for racing is good unless lesions are severe or cartilage damage of the patella is advanced. Subchondral bone cysts most commonly involve the medial femoral condyle but can occur in the proximal aspect of the tibia. Lameness is often progressive, with horses first being on a line. Surgical debridement of the cyst is recommended, although injection of corticosteroids beneath the lining of the cyst and into the cyst cavity under arthroscopic guidance can be used. After debridement, lameness persists for several months, but this approach may be a better long-term solution. Horses need a minimum of 6 to 8 months of rest to allow healing and for lameness to abate. Prognosis is fair (70%) for successful racing.
Rhabdomyolysis and Muscle Soreness
We divide muscle lameness into metabolic disease (recurrent exertional rhabdomyolysis [RER]) and nonmetabolic disease (muscle soreness). Signs vary, but horses appear stiff and hindlimbs are not fully engaged in the stride unilaterally or bilaterally. Palpation often reveals muscle pain but must be done carefully because aggressive, sudden, and deep palpation elicits false-positive responses.
RER occurs more commonly in females and can cause swollen muscles. Overt clinical signs of tying up after racing and training can be seen, but subclinical RER can be a cause of poor performance. Myoglobinuria and elevation of serum creatine kinase (CK) and aspartate transaminase (AST) levels are diagnostic. Horses are managed initially with intravenous fluids, NSAIDs, tranquilization, and methocarbamol (22 mg/kg intravenously [IV] or 33 mg/kg PO twice daily). Care must be taken when using acetylpromazine and methocarbamol simultaneously because effects may be additive, and horses may act severely tranquilized (JSM). Walking is recommended in horses with mild RER but is contraindicated in those with severe RER. Dantrolene sodium (2 mg/kg IV or via nasogastric tube) and intravenous dimethyl sulfoxide solution are recommended in horses with severe RER. Large quantities of intravenous or oral fluids should be administered. After an acute episode, signs may recur or subclinical myositis may persist, reflected by elevations in CK and AST concentrations. Enzyme levels should return to baseline before intense training or racing resumes.
In horses with subclinical RER or those with recurrent acute episodes, we recommend a management protocol that includes a reduction in carbohydrate intake, especially before exercise, a high-fat diet, vitamin E and selenium supplementation, supplementation with oral potassium, and a regular 7-day exercise program combining jogging, brief periods of intensive training, and paddock exercise, if feasible. Chronic administration of dantrolene sodium (2 mg/kg) or phenytoin (8 to 10 mg/kg PO twice daily) is recommended, but racing jurisdiction rules must be followed.
Nonmetabolic myositis is common, and gait is similar to that described for stifle lameness. Signs are similar to RER, but serum CK and AST levels are usually within or just above normal limits. The middle gluteal muscle and associated tendons commonly are affected unilaterally or bilaterally. Myositis may be a secondary problem or a primary source of pain after traumatic injuries such as accidents during transport, paddock injuries, slipping while racing on muddy or other undesirable surfaces, or by making a break. Horses are managed initially with muscle relaxants, NSAIDs, and rest (5 to 7 days). Horses with chronic soreness are treated with an internal counterirritant or corticosteroids injected strategically in the sore areas (see Chapter 88).
Curb and Superficial Digital Flexor Tendonitis
Other soft tissue injuries such as curb and superficial digital flexor tendonitis occur commonly. Curb in the STB is discussed in detail in Chapter 78. Superficial digital flexor tendonitis is discussed in detail in Chapter 69. Surgical management using desmotomy of the accessory ligament of the superficial digital flexor muscle (superior check desmotomy) and annular desmotomy if tendonitis involves the distal metacarpal region are recommended.