Chapter 6 Gastrointestinal disease
Introduction
The gastrointestinal tract has many functions such as digestion, absorption and excretion as well as the synthesis of an array of hormones, growth factors and cytokines. In addition, a complex enteric nervous system has evolved to control its function and communicate with the central and peripheral nervous systems. Finally, as the gastrointestinal tract contains the largest sources of foreign antigens to which the body is exposed, it houses well-developed arms of both the innate and acquired immune system.
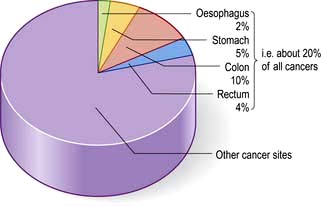
In developed countries gastrointestinal symptoms are a common reason for attendance to primary care clinics and to hospital outpatients. Approximately 75% of these consultations are for non-organic symptoms. The clinician’s main task is therefore to recognize when organic disease must be sought or excluded, remembering that 20% of all cancers occur in the gastrointestinal tract (Fig. 6.1). In developing countries, malnutrition and poor hygiene make infection a more probable diagnosis. The clinician needs to recognize and treat these infections promptly and also help with prevention by encouraging good hygiene.
Gastrointestinal symptoms and signs
Stomatitis and ‘burning mouth’ sensation
Stomatitis is inflammation in the mouth from any cause, such as ill-fitting dentures. Angular stomatitis is inflammation of the corners of the mouth.
The ‘burning mouth syndrome’ consists of a burning sensation with a clinically normal oral mucosa. It occurs more commonly in middle-aged and elderly females. It is probably psychogenic in origin. Halitosis (bad breath) is a common symptom and is due to poor oral hygiene, anxiety (often when halitosis is more apparent to the patient than real) and rarer causes, e.g. oesophageal stricture and pulmonary sepsis.
Dyspepsia and indigestion
‘Indigestion’ is common: 80% of the population will suffer from this symptom at some time. Dyspepsia is an inexact term used to describe a number of upper abdominal symptoms such as heartburn, acidity, pain or discomfort, nausea, wind, fullness or belching. Patients, when using the term ‘indigestion’, may also be describing lower GI symptoms such as constipation or the presence of undigested vegetable material in the stool, so obtaining a precise history is necessary.
Features of dyspepsia suggestive of serious diseases such as cancer are known as ‘Alarm’ symptoms.
Patients with these features have a higher possibility of significant gastrointestinal pathology and should be investigated, although the benefits are small.
Vomiting
Many gastrointestinal (and non-gastrointestinal) conditions are associated with vomiting (Table 6.1). This is controlled by a complex reflex involving central neural control centres located in the lateral reticular formation of the medulla which are stimulated by the chemoreceptor trigger zones (CTZs) in the floor of the fourth ventricle, and also by vagal afferents from the gut. The central zones are directly stimulated by toxins, drugs, motion sickness and metabolic disturbances. Raised intracranial pressure has a direct effect on the vomiting centre leading to vomiting. Luminal toxins, inflammation and mechanical obstruction are local GI causes of vomiting.
Table 6.1 Causes of vomiting: some examples
Nausea is a feeling of wanting to vomit, often associated with autonomic effects including salivation, pallor and sweating. It often precedes actual vomiting. Retching is a strong involuntary unproductive effort to vomit associated with abdominal muscle contraction but without expulsion of gastric contents through the mouth.
Faeculent vomit suggests low intestinal obstruction or the presence of a gastrocolic fistula.
Haematemesis is vomiting fresh or altered blood (‘coffee-grounds’) (see p. 254).
Early-morning nausea and vomiting is seen in pregnancy, alcohol dependence and some metabolic disorders (e.g. uraemia).
Persistent nausea alone is often stress-related and is not due to gastrointestinal disease.
Flatulence
This term describes excessive wind. It is used to indicate belching, abdominal distension, gurgling and the passage of flatus per rectum. Swallowing air (aerophagia) is described on page 296. Some of the swallowed air passes into the intestine where most of it is absorbed, but some remains to be passed rectally. Colonic bacterial breakdown of non-absorbed carbohydrate also produces gas. Rectal flatus thus consists of nitrogen, carbon dioxide, hydrogen and methane. It is normal to pass rectal flatus up to 20 times/day. Causes of increased gas production and intake include high-fibre diet and carbonated drinks.
Diarrhoea and constipation
These are common complaints and in the community are not usually due to serious disease. They are described in detail on pages 291 and 282, respectively. Some general rules concerning the aetiology and investigation of diarrhoea are shown in Box 6.1.
![]() Box 6.1
Box 6.1
Simple rules in diarrhoea
Patients often consider themselves constipated if their bowels are not open on most days, though normal stool frequency is very variable, from 3 times daily to 3 times a week. The difficult passage of hard stool is also regarded as constipation, irrespective of stool frequency. Constipation with hard stools is rarely due to organic colonic disease.
Abdominal pain
Pain is stimulated mainly by the stretching of smooth muscle or organ capsules. Severe acute abdominal pain can be due to a large number of gastrointestinal conditions, and normally presents as an emergency (see p. 298). An apparent ‘acute abdomen’ can occasionally be due to referred pain from the chest, as in pneumonia or to metabolic causes, such as diabetic ketoacidosis or porphyria.
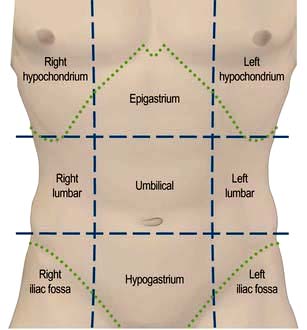
 Site (Fig. 6.2), intensity, character, duration and frequency of the pain
Site (Fig. 6.2), intensity, character, duration and frequency of the pain
 Aggravating and relieving factors
Aggravating and relieving factors
 Associated symptoms, including non-gastrointestinal symptoms.
Associated symptoms, including non-gastrointestinal symptoms.
Upper abdominal pain
Epigastric pain is very common and is often related to food intake. Although functional dyspepsia is the commonest diagnosis, the symptoms of peptic ulcer disease can be identical. Heartburn (a burning pain behind the sternum) is a common symptom of gastro-oesophageal reflux.
Right hypochondrial pain may originate from the gall bladder or biliary tract. Biliary pain can also be epigastric. Biliary pain is typically intermittent and severe, lasts a few hours and remits spontaneously to recur weeks or months later. Hepatic congestion (e.g. in hepatitis or cardiac failure) and sometimes peptic ulcer disease can present with pain in the right hypochondrium. Chronic, persistent or constant pain in the right (or left) hypochondrium in a well-looking patient is a frequent functional symptom; this chronic pain is not due to gall bladder disease (see p. 353).
Lower abdominal pain
Pain in the left iliac fossa may be colonic in origin (e.g. acute diverticulitis) but chronic pain is most commonly associated with functional bowel disorders.
Lower abdominal pain in women occurs in a number of gynaecological disorders and the differentiation from GI disease may be difficult.
Pain in the right iliac fossa may be due to acute appendicitis or ileocaecal disease, but may also commonly be functional.
Proctalgia fugax is a severe pain deep in the rectum that comes on suddenly but lasts only for a short time. It is not due to organic disease.
Abdominal wall pain
Persistent abdominal pain with localized tenderness, which is not relieved by tensing the abdominal muscles, is probably from the abdominal wall itself. Causes are thought to include nerve entrapment, external hernias, and entrapment of internal viscera (commonly omentum) within traumatic or surgical alterations of abdominal wall musculature.
Anorexia and weight loss
Anorexia describes reduced appetite. It is common in systemic disease and may be seen in psychiatric disorders. Anorexia often accompanies cancer but is usually a late symptom and not of diagnostic help. Weight loss is almost always due to reduced food intake and is a frequent accompaniment of gastrointestinal diseases. Weight loss in malabsorption disorders is primarily due to anorexia. Weight loss with a normal or increased dietary intake only occurs with hyperthyroidism and other catabolic states. Weight loss should always be assessed objectively as patients’ impressions are unreliable.
Examination of the abdomen
Inspection
Look for abdominal distension. Common causes (the five Fs) are: flatus, fat, fetus, fluid and faeces. Intermittent distension is most commonly a feature of functional bowel disorders.
Palpation
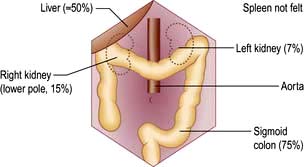
Look for palpable masses or abdominal tenderness. All abdominal quadrants should be palpated in turn followed by deeper palpations; remember to watch the patient’s face for signs of pain or discomfort. Evaluate any palpable mass and note its size, shape and consistency and whether it moves with respiration, to decide which organ is involved. Some abdominal organs may be just palpable normally, usually in thin people (Fig. 6.3). Reidel’s lobe is an anatomical variant consisting of a palpable enlargement of the lateral portion of the right lobe of the liver. The hernial orifices should be examined if intestinal obstruction is suspected.
Percussion
Abdominal percussion detects the areas of dullness caused by the liver and spleen, ascites or over masses. It can also detect a full bladder. Ascites is a term for excess fluid in the peritoneal cavity. It is detected clinically by central abdominal resonance due to gas within small bowel loops with dullness in the flanks which shifts when the patient lies on their side. This ‘shifting dullness’ is a reliable physical sign, if 1–2 L of fluid are present.
Auscultation
Auscultation is not of great value in abdominal disease, except for evaluation of bowel sounds in the acute abdomen (see p. 299). Abdominal bruits are often present in normal subjects and are rarely clinically significant.
A succussion splash suggests gastric outlet obstruction if the patient has not drunk for 2–3 hours. The splash of fluid in the stomach can be heard with a stethoscope laid on the abdomen when the patient is moved.
Examination of the rectum and sigmoid colon
A digital examination of the rectum should be performed in all patients with a change in bowel habit, rectal bleeding and prior to proctoscopy or sigmoidoscopy.
 Proctoscopy (see Practical Box 6.1) is performed in all patients with a history of bright red rectal bleeding to look for anorectal pathology such as haemorrhoids; a rigid sigmoidoscope is too narrow and long to enable adequate examination of the anal canal.
Proctoscopy (see Practical Box 6.1) is performed in all patients with a history of bright red rectal bleeding to look for anorectal pathology such as haemorrhoids; a rigid sigmoidoscope is too narrow and long to enable adequate examination of the anal canal.
 Sigmoidoscopy is part of the routine hospital examination in cases of diarrhoea and in patients with lower abdominal symptoms such as a change in bowel habit or rectal bleeding. The rigid sigmoidoscope allows inspection of a maximum of 20–25 cm of distal colon.
Sigmoidoscopy is part of the routine hospital examination in cases of diarrhoea and in patients with lower abdominal symptoms such as a change in bowel habit or rectal bleeding. The rigid sigmoidoscope allows inspection of a maximum of 20–25 cm of distal colon.
 Flexible sigmoidoscopy (FS) (60 cm) can reach up to the splenic flexure, and can be performed in the outpatient department or endoscopy unit after evacuation of the distal colon using an enema or suppository. FS can be used in patients with increased stool frequency or looseness or rectal bleeding to diagnose colitis or polyps. Most rectal bleeding is due to benign anorectal disease (haemorrhoids or fissure-in-ano) and an otherwise normal FS can be reassuring to avoid over-investigation. Up to 60% of colonic neoplasms occur within the range of FS (see Fig. 6.45) and it has therefore been proposed as screening test for colorectal cancer in asymptomatic individuals.
Flexible sigmoidoscopy (FS) (60 cm) can reach up to the splenic flexure, and can be performed in the outpatient department or endoscopy unit after evacuation of the distal colon using an enema or suppository. FS can be used in patients with increased stool frequency or looseness or rectal bleeding to diagnose colitis or polyps. Most rectal bleeding is due to benign anorectal disease (haemorrhoids or fissure-in-ano) and an otherwise normal FS can be reassuring to avoid over-investigation. Up to 60% of colonic neoplasms occur within the range of FS (see Fig. 6.45) and it has therefore been proposed as screening test for colorectal cancer in asymptomatic individuals.
![]() Practical Box 6.1
Practical Box 6.1
Sigmoidoscopy and proctoscopy
Sigmoidoscopy
 The technique using a 25 cm rigid sigmoidoscope is easy to learn, provides valuable information and is safe in competent hands.
The technique using a 25 cm rigid sigmoidoscope is easy to learn, provides valuable information and is safe in competent hands.
 No bowel preparation is required.
No bowel preparation is required.
 Explain to the patient the nature of the procedure and obtain consent.
Explain to the patient the nature of the procedure and obtain consent.
 The technique is relatively painless. In the irritable bowel syndrome, the patient’s pain is often reproduced by air insufflation:
The technique is relatively painless. In the irritable bowel syndrome, the patient’s pain is often reproduced by air insufflation:
Proctoscopy
1. The proctoscope is passed into the anus and the obturator is removed.
2. The patient strains down as the proctoscope is removed.
3. Haemorrhoids are seen as purplish veins in the left lateral, right posterior or right anterior positions.
4. Fissures may also be seen, but pain often prevents the procedure from being performed.
Stool examination
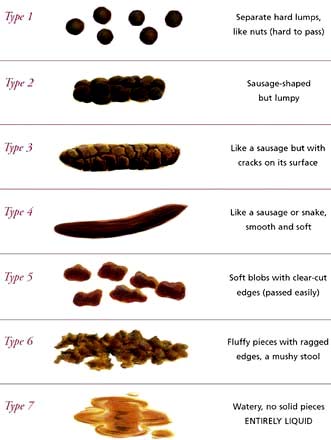
It is useful to confirm a patient’s account (e.g. passing of blood or steatorrhoea). The shape and size may be helpful (e.g. ‘rabbit dropping’ or ribbon-like stools in the irritable bowel syndrome). Stool charts for recording consistency and frequency of defecation are useful in inpatients to follow the progress of diarrhoea, particularly in the management of severe colitis. The Bristol Stool Chart is commonly used in the UK (Fig. 6.4).
Investigations
Routine haematology and biochemistry, followed by endoscopy and radiology, are the principal investigations. The investigation of small bowel disease is discussed in more detail on page 267. Manometry is mainly used in oesophageal disease (see p. 237) and anorectal disorders (see p. 286).
Endoscopy
Video endoscopes have replaced fibreoptic instruments and relay colour images to a high definition television monitor. The tip of the endoscope can be angulated in all directions. Channels in the instrument are used for air insufflation, water injection, suction, and for the passage of accessories such as biopsy forceps or brushes for obtaining tissue, snares for polypectomy and needles for injection therapies. Permanent photographic or video records of the procedure can be obtained.
 Oesophagogastroduodenoscopy (OGD, ‘gastroscopy’) is the investigation of choice for upper GI disorders with the possibility of therapy and mucosal biopsy. Findings include reflux oesophagitis, gastritis, ulcers and cancer. Therapeutic OGD is used to treat upper GI haemorrhage and both benign and malignant obstruction. Relative contraindications include severe chronic obstructive pulmonary disease, a recent myocardial infarction, or severe instability of the atlantoaxial joints. The mortality for diagnostic endoscopy is 0.001% with significant complications in 1 : 10 000, usually when performed as an emergency (e.g. GI haemorrhage).
Oesophagogastroduodenoscopy (OGD, ‘gastroscopy’) is the investigation of choice for upper GI disorders with the possibility of therapy and mucosal biopsy. Findings include reflux oesophagitis, gastritis, ulcers and cancer. Therapeutic OGD is used to treat upper GI haemorrhage and both benign and malignant obstruction. Relative contraindications include severe chronic obstructive pulmonary disease, a recent myocardial infarction, or severe instability of the atlantoaxial joints. The mortality for diagnostic endoscopy is 0.001% with significant complications in 1 : 10 000, usually when performed as an emergency (e.g. GI haemorrhage).
 Colonoscopy allows good visualization of the whole colon and terminal ileum. Biopsies can be obtained and polyps removed. Benign strictures can be dilated and malignant strictures stented. The success rate for reaching the caecum should be at least 90% after training. Cancer, polyps and diverticular disease are the commonest significant findings. Perforation occurs in 1 : 1000 examinations but this is higher (up to 2%) after polypectomy (see Practical Box 6.2).
Colonoscopy allows good visualization of the whole colon and terminal ileum. Biopsies can be obtained and polyps removed. Benign strictures can be dilated and malignant strictures stented. The success rate for reaching the caecum should be at least 90% after training. Cancer, polyps and diverticular disease are the commonest significant findings. Perforation occurs in 1 : 1000 examinations but this is higher (up to 2%) after polypectomy (see Practical Box 6.2).
 Balloon enteroscopy, either double or single balloon, can examine the small bowel from the duodenum to the ileum using specialized enteroscopes in expert centres.
Balloon enteroscopy, either double or single balloon, can examine the small bowel from the duodenum to the ileum using specialized enteroscopes in expert centres.
 Capsule endoscopy is used for the evaluation of obscure GI bleeding (after negative gastroscopy and colonoscopy) and for the detection of small bowel tumours and occult inflammatory bowel disease. It should be avoided if strictures are suspected.
Capsule endoscopy is used for the evaluation of obscure GI bleeding (after negative gastroscopy and colonoscopy) and for the detection of small bowel tumours and occult inflammatory bowel disease. It should be avoided if strictures are suspected.
![]() Practical Box 6.2
Practical Box 6.2
Gastroscopy and colonoscopy
Gastroscopy
1. Patient should be fasted for at least 4 hours.
2. Give oxygen and monitor oxygen saturation with an oximeter.
3. Give lidocaine throat spray or sedation (midazolam ± opiate if required).
4. Pass the gastroscope to the duodenum under direct vision.
5. Examine during insertion and withdrawal.
6. Gastroscopy takes 5–15 min, depending on the indication and findings.
7. Withhold fluid and food until LA/sedation wears off.
8. Complications are rare: beware of over-sedation, perforation and aspiration.
Colonoscopy
1. Stop oral iron a week before the procedure.
2. Restrict diet to low residue foods for 48 hours; clear fluids only for 24 hours.
3. Use local bowel cleansing regime, usually starting 24 hours beforehand (e.g. two sachets of sodium picosulfate with magnesium citrate and 2–4 bisacodyl tablets, or macrogols 2–4 L, or local alternative; more if constipated).
4. Give oxygen and monitor O2 levels.
5. Give sedation (midazolam ± opiate) if required by patient.
6. Pass the colonoscope to the caecum or ileum under direct vision.
7. Examine in detail during withdrawal.
8. Colonoscopy takes 15–30 min, depending on the colon anatomy, indication and findings.
9. Withhold fluid and food until sedation wears off.
10. Observe patient for at least an hour after sedation given.
11. Complications are rare: beware of over-sedation, perforation and aspiration.
Imaging
Full clinical information must be provided before the examination, and ideally, the images obtained should be reviewed with the radiologist to aid interpretation. The optimal technique to be used will depend on local expertise.
Plain X-rays of the chest and abdomen are chiefly used in the investigation of an acute abdomen. Interpretation depends on analysis of gas shadows inside and outside the bowel. Plain films are particularly useful where obstruction or perforation is suspected, to exclude toxic megacolon in colitis and to assess faecal loading in constipation. Calcification may be seen with gall bladder stones and in chronic pancreatitis, though CT is more sensitive for both.
Ultrasound involves no radiation and is the first-line investigation for abdominal distension, e.g. ascites, mass or suspected inflammatory conditions. It can show dilated fluid-filled loops of bowel in obstruction, and thickening of the bowel wall. It can be used to guide biopsies or percutaneous drainage. In an acute abdomen, ultrasound can diagnose cholecystitis, appendicitis, enlarged mesenteric glands and other inflammatory conditions.
 Endoscopic ultrasound (EUS) is performed with a gastroscope incorporating an ultrasound probe at the tip. It is used diagnostically for lesions in the oesophageal or gastric wall, including the detailed TNM staging (see p. 245) of oesophageal/gastric cancer and for the detection and biopsy of pancreatic tumours and cysts.
Endoscopic ultrasound (EUS) is performed with a gastroscope incorporating an ultrasound probe at the tip. It is used diagnostically for lesions in the oesophageal or gastric wall, including the detailed TNM staging (see p. 245) of oesophageal/gastric cancer and for the detection and biopsy of pancreatic tumours and cysts.
 Endoanal and endorectal ultrasonography are performed to define the anatomy of the anal sphincters (see p. 285), to detect perianal disease and to stage superficial rectal tumours.
Endoanal and endorectal ultrasonography are performed to define the anatomy of the anal sphincters (see p. 285), to detect perianal disease and to stage superficial rectal tumours.
Computed tomography involves a significant dose of radiation (approximately 10 millisieverts). Modern multislice fast scanners and techniques involving intraluminal and intravenous contrast enhance diagnostic capability. Intraluminal contrast may be positive (Gastrografin or Omnipaque) or negative (usually water). The bowel wall and mesentery are well seen after intravenous contrast especially with negative intraluminal contrast. Clinically unsuspected diseases of other abdominal organs are quite often also revealed (Fig. 6.5a).
 CT is widely used as a first-line investigation for the acute abdomen. CT is sensitive for small volumes of gas from a perforated viscus as well as leakage of contrast from the gut lumen.
CT is widely used as a first-line investigation for the acute abdomen. CT is sensitive for small volumes of gas from a perforated viscus as well as leakage of contrast from the gut lumen.
 Inflammatory conditions such as abscesses, appendicitis, diverticulitis, Crohn’s disease and its complications are well demonstrated. In high-grade bowel obstruction, CT is usually diagnostic of both the presence and the cause of the obstruction.
Inflammatory conditions such as abscesses, appendicitis, diverticulitis, Crohn’s disease and its complications are well demonstrated. In high-grade bowel obstruction, CT is usually diagnostic of both the presence and the cause of the obstruction.
 CT is widely used in cancer staging and as guidance for biopsy of tumour or lymph nodes.
CT is widely used in cancer staging and as guidance for biopsy of tumour or lymph nodes.
 CT pneumocolon/CT colonography (virtual colonoscopy) after CO2 insufflation into a previously cleansed colon provides an alternative to colonoscopy for diagnosis of colon mass lesions (Fig. 6.5b). It is being evaluated as a screening test for colon pathology with sensitivities of over 90% for >10 mm polyps.
CT pneumocolon/CT colonography (virtual colonoscopy) after CO2 insufflation into a previously cleansed colon provides an alternative to colonoscopy for diagnosis of colon mass lesions (Fig. 6.5b). It is being evaluated as a screening test for colon pathology with sensitivities of over 90% for >10 mm polyps.
 Unprepared CT is a good test for colon cancer in the frail (often elderly) patient who would have problems with bowel preparation.
Unprepared CT is a good test for colon cancer in the frail (often elderly) patient who would have problems with bowel preparation.
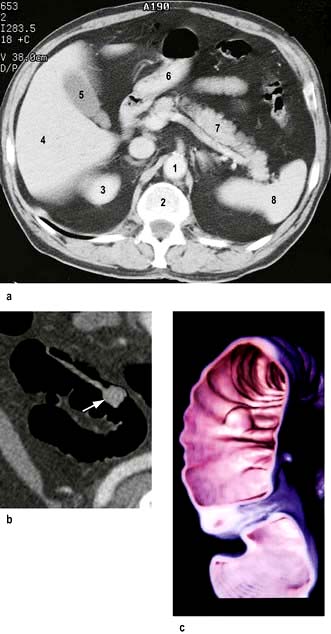
Figure 6.5 (a) CT scan of the normal abdomen at the level of T12. (1) Aorta; (2) spine; (3) top of right kidney; (4) liver; (5) gall bladder; (6) stomach (containing air); (7) pancreas; (8) spleen. (b) CT cross-sectional (2-dimensional) image of a colonic polyp on a long stalk. The colon has been emptied as for visual colonoscopy. The pedunculated polyp and its stalk show enhancement after intravenous contrast. (c) 3D reconstruction of part of the colon (false colour) generated by a computer program from multiple axial CT images. A sessile polypoid lesion is shown.
(b and c: Courtesy of Dr Paul Jenkins.)
Magnetic resonance imaging. MRI uses no radiation and is particularly useful in the evaluation of rectal cancers and abscesses and fistulae in the perianal region. It is also useful in small bowel disease and in hepatobiliary and pancreatic disease.
Positron emission tomography (PET) relies on detection of the metabolism of fluorodeoxyglucose. It is used for staging oesophageal, gastric and colorectal cancer and in the detection of metastatic and recurrent disease. PET/CT adds additional anatomical information.
Contrast studies
 Barium swallow examines the oesophagus and proximal stomach. Its main use is for investigating dysphagia.
Barium swallow examines the oesophagus and proximal stomach. Its main use is for investigating dysphagia.
 Double-contrast barium meal examines the oesophagus, stomach and duodenum. Barium is given to produce mucosal coating and effervescent granules producing carbon dioxide in the stomach create a double contrast between gas and barium. This test has a high accuracy for the detection of significant pathology – ulcers and cancer – but requires good technique. Gastroscopy is a more sensitive test and enables biopsy of suspicious areas.
Double-contrast barium meal examines the oesophagus, stomach and duodenum. Barium is given to produce mucosal coating and effervescent granules producing carbon dioxide in the stomach create a double contrast between gas and barium. This test has a high accuracy for the detection of significant pathology – ulcers and cancer – but requires good technique. Gastroscopy is a more sensitive test and enables biopsy of suspicious areas.
 Small bowel meal or follow-through specifically examines the small bowel. Ingested barium passes through the small bowel into the right colon. The fold pattern and calibre of the small bowel are assessed. Specific views of the terminal ileum can be obtained and are used to identify early changes in patients with suspected Crohn’s disease.
Small bowel meal or follow-through specifically examines the small bowel. Ingested barium passes through the small bowel into the right colon. The fold pattern and calibre of the small bowel are assessed. Specific views of the terminal ileum can be obtained and are used to identify early changes in patients with suspected Crohn’s disease.
 Small bowel enema (enteroclysis) is an alternative specific technique for small bowel examination. A tube is passed into the duodenum and a large volume of dilute barium is introduced. It is particularly used to demonstrate strictures or adhesions when there is suspicion of intermittent obstruction. Generally, this has been replaced by MR enteroclysis.
Small bowel enema (enteroclysis) is an alternative specific technique for small bowel examination. A tube is passed into the duodenum and a large volume of dilute barium is introduced. It is particularly used to demonstrate strictures or adhesions when there is suspicion of intermittent obstruction. Generally, this has been replaced by MR enteroclysis.
 Barium enema examines the colon and is used for altered bowel habit. Colonoscopy and CT colonography have largely replaced this examination for rectal bleeding, polyps and inflammatory bowel disease.
Barium enema examines the colon and is used for altered bowel habit. Colonoscopy and CT colonography have largely replaced this examination for rectal bleeding, polyps and inflammatory bowel disease.
 Absorbable water-soluble (Gastrografin or Omnipaque) contrast agents should be used in preference to barium when perforation is suspected anywhere in the gut.
Absorbable water-soluble (Gastrografin or Omnipaque) contrast agents should be used in preference to barium when perforation is suspected anywhere in the gut.
Radioisotopes
Radionuclides are used to a varying degree depending on availability and expertise. Some more common indications and techniques:
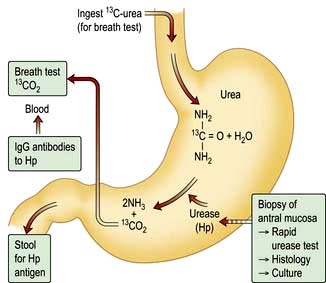
 Detect urease activity of Helicobacter pylori – 13C urea breath test (see p. 249)
Detect urease activity of Helicobacter pylori – 13C urea breath test (see p. 249)
 Assess oesophageal reflux – gamma camera scan after oral [99mTc]technetium-sulphur colloid
Assess oesophageal reflux – gamma camera scan after oral [99mTc]technetium-sulphur colloid
 Measure rate of gastric emptying – sequential gamma camera scans after oral [99mTc]technetium-sulphur colloid or 111In-DTPA (indium-labelled diethylene triamine penta-acetic acid)
Measure rate of gastric emptying – sequential gamma camera scans after oral [99mTc]technetium-sulphur colloid or 111In-DTPA (indium-labelled diethylene triamine penta-acetic acid)
 Demonstrate a Meckel’s diverticulum – gamma camera scan after i.v. [99mTc]pertechnetate, which has affinity for gastric mucosa
Demonstrate a Meckel’s diverticulum – gamma camera scan after i.v. [99mTc]pertechnetate, which has affinity for gastric mucosa
 Assess extent of inflammation and presence of inflammatory collections in inflammatory bowel disease – gamma camera scan after i.v. 99mTc-HMPAO (hexamethylpropylene amine oxime) labelled white cells
Assess extent of inflammation and presence of inflammatory collections in inflammatory bowel disease – gamma camera scan after i.v. 99mTc-HMPAO (hexamethylpropylene amine oxime) labelled white cells
 Evaluate neuroendocrine tumours and their metastases – gamma camera scan after i.v. radiolabelled octreotide or MIBG (meta-iodobenzylguanidine)
Evaluate neuroendocrine tumours and their metastases – gamma camera scan after i.v. radiolabelled octreotide or MIBG (meta-iodobenzylguanidine)
 Assess obscure gastrointestinal bleeding – gamma camera abdominal scan after i.v. injection of red cells labelled with 99mTc (only useful if the bleeding is >2 mL/min)
Assess obscure gastrointestinal bleeding – gamma camera abdominal scan after i.v. injection of red cells labelled with 99mTc (only useful if the bleeding is >2 mL/min)
 Measure albumin loss in the stools (in protein-losing enteropathy) – following albumin labelled in vivo with i.v. 51CrCl3. This test has been replaced by the measurement of the intestinal clearance of α1 antitrypsin
Measure albumin loss in the stools (in protein-losing enteropathy) – following albumin labelled in vivo with i.v. 51CrCl3. This test has been replaced by the measurement of the intestinal clearance of α1 antitrypsin
 Assess bile salt malabsorption (in patients with unexplained diarrhoea) – gamma camera scan to measure both isotope retention and faecal loss of orally administered 75selenium-homocholic acid taurine (SeHCAT) (see p. 293)
Assess bile salt malabsorption (in patients with unexplained diarrhoea) – gamma camera scan to measure both isotope retention and faecal loss of orally administered 75selenium-homocholic acid taurine (SeHCAT) (see p. 293)
 Detect bacterial overgrowth in the small bowel – measure 14CO2 in breath following oral 14C glycocholic acid.
Detect bacterial overgrowth in the small bowel – measure 14CO2 in breath following oral 14C glycocholic acid.
The mouth
The oral cavity extends from the lips to the pharynx and contains the tongue, teeth and gums. Its primary functions are mastication, swallowing and speech. Problems in the mouth are extremely common and, although they may be trivial, they can produce severe symptoms. Poor dental hygiene is often a factor.
Recurrent aphthous ulceration
Idiopathic aphthous ulceration is common and affects up to 25% of the population. Recurrent painful round or ovoid mouth ulcers are seen with inflammatory halos. They are commoner in females and non-smokers, usually appear first in childhood and tend to reduce in number and frequency before age 40. Other family members may be affected. There is no sign of systemic disease.
 Minor aphthous ulcers are the most common, are <10 mm diameter, have a grey/white centre with a thin erythematous halo and heal within 14 days without scarring. They rarely affect the dorsum of the tongue or hard palate.
Minor aphthous ulcers are the most common, are <10 mm diameter, have a grey/white centre with a thin erythematous halo and heal within 14 days without scarring. They rarely affect the dorsum of the tongue or hard palate.
 Major aphthous ulcers (>10 mm diameter) often persist for weeks or months and heal with scarring.
Major aphthous ulcers (>10 mm diameter) often persist for weeks or months and heal with scarring.
The cause is not known. Deficiencies of iron, folic acid or vitamin B12 (with or without gastrointestinal disorders) are sometimes found but are not causally linked. Secondary causes, e.g. Crohn’s disease, should be excluded.
There are no specific effective therapies. Sufferers should avoid oral trauma and acidic foods or drinks which cause pain. Topical (1% triamcinolone) or systemic corticosteroids may lessen the duration and severity of the attacks. Chlorhexidine gluconate or tetracycline mouthwash, dapsone, colchicine, thalidomide and azathioprine have all been used with variable effect.
Other causes
See Table 6.2.
Table 6.2 Causes of mouth ulcers
Neoplasia (squamous cell carcinoma)
Malignant tumours of the mouth account for 1% of all malignant tumours in the UK. The majority develop on the floor of the mouth or lateral borders of the tongue. Early lesions may be painless, but advanced tumours are easily recognizable as hard indurated ulcers with raised and rolled edges. Aetiological agents include tobacco, heavy alcohol consumption and the areca nut. Human papillomavirus 16 causes some oral cancers. Premalignant lesions include leucoplakia (single adherent white patch), lichen planus, submucous fibrosis and erythroplakia (a red patch).
Treatment is by surgical excision which may require extensive neck dissection to remove involved lymph nodes and/or radiotherapy. Ablative treatment with photodynamic therapy is being pioneered for early lesions.
Oral white patches
Transient white patches are either due to Candida infection or are very occasionally seen in systemic lupus erythematosus. Local causes include mechanical, irritative or chemical trauma from drugs (e.g. ill fitting dentures or aspirin). Oral candidiasis in adults is seen following therapy with broad-spectrum antibiotics or inhaled steroids and in people with diabetes, patients who are seriously ill or immunocompromised.
Persistent white patches can be due to leucoplakia, which is associated with alcohol and (particularly) smoking, and is premalignant. A biopsy should always be taken; histology shows alteration in the keratinization and dysplasia of the epithelium. Treatment is unsatisfactory. Isotretinoin possibly reduces disease progression. Oral lichen planus presents as white striae, which can rarely extend into the oesophagus.
Oral pigmented lesions
Non-neoplastic lesions
Racial pigmentation is scattered and symmetrically distributed. Amalgam tattoo is the most common form of localized oral pigmentation and consists of blue-black macules involving the gingivae and results from dental amalgam sequestering into the tissues. Diseases causing pigmentation include Peutz–Jeghers syndrome and Addison’s disease. Heavy metals, such as lead, bismuth and mercury, and drugs (e.g. phenothiazines and antimalarials) all cause pigmentation of the gums.
The tongue
The tongue may be affected by inflammatory or malignant processes with similar lesions to those described above.
 Glossitis is a red, smooth, sore tongue associated with B12, folate or iron deficiency. It is also seen in infections due to Candida and in riboflavin and nicotinic acid deficiency.
Glossitis is a red, smooth, sore tongue associated with B12, folate or iron deficiency. It is also seen in infections due to Candida and in riboflavin and nicotinic acid deficiency.
 A black hairy tongue is due to a proliferation of chromogenic microorganisms causing brown staining of elongated filiform papillae. The causes are unknown, but heavy smoking and the use of antiseptic mouthwashes have been implicated.
A black hairy tongue is due to a proliferation of chromogenic microorganisms causing brown staining of elongated filiform papillae. The causes are unknown, but heavy smoking and the use of antiseptic mouthwashes have been implicated.
 A geographic tongue is an idiopathic condition occurring in 1–2% of the population and may be familial. There are erythematous areas surrounded by well-defined, slightly raised irregular margins. The lesions are usually painless and the patient should be reassured.
A geographic tongue is an idiopathic condition occurring in 1–2% of the population and may be familial. There are erythematous areas surrounded by well-defined, slightly raised irregular margins. The lesions are usually painless and the patient should be reassured.
The gums
The gums (gingivae) are the mucous membranes covering the alveolar processes of the mandible and the maxilla.
 Chronic gingivitis follows the accumulation of bacterial plaque. It resolves when the plaque is removed. It is the most common cause of bleeding gums.
Chronic gingivitis follows the accumulation of bacterial plaque. It resolves when the plaque is removed. It is the most common cause of bleeding gums.
 Acute (necrotizing) ulcerative gingivitis (‘Vincent’s angina’) is characterized by the proliferation of spirochaete and fusiform bacteria associated with poor oral hygiene and smoking. Treatment is with oral metronidazole 200 mg three times daily for 3 days, improved oral hygiene and chlorhexidine gluconate mouthwash.
Acute (necrotizing) ulcerative gingivitis (‘Vincent’s angina’) is characterized by the proliferation of spirochaete and fusiform bacteria associated with poor oral hygiene and smoking. Treatment is with oral metronidazole 200 mg three times daily for 3 days, improved oral hygiene and chlorhexidine gluconate mouthwash.
 Desquamative gingivitis is a clinical description of smooth, red atrophic gingivae caused by lichen planus or mucous membrane pemphigoid. The diagnosis is confirmed by biopsy.
Desquamative gingivitis is a clinical description of smooth, red atrophic gingivae caused by lichen planus or mucous membrane pemphigoid. The diagnosis is confirmed by biopsy.
 Gingival swelling may be due to inflammation or fibrous hyperplasia. The latter may be hereditary (gingival fibromatosis) or associated with drugs (e.g. phenytoin, ciclosporin, nifedipine). Inflammatory swellings are seen in pregnancy, gingivitis and scurvy. Swelling due to infiltration is seen in acute leukaemia and Wegener’s granulomatosis.
Gingival swelling may be due to inflammation or fibrous hyperplasia. The latter may be hereditary (gingival fibromatosis) or associated with drugs (e.g. phenytoin, ciclosporin, nifedipine). Inflammatory swellings are seen in pregnancy, gingivitis and scurvy. Swelling due to infiltration is seen in acute leukaemia and Wegener’s granulomatosis.
The teeth
Dental caries occur as a result of bacterial damage to tooth structures leading to tooth decay and ‘cavities’. The main cause in man is Streptococcus mutans, which is cariogenic only in the presence of dietary sugar. Dental caries can progress to pulpitis and pulp necrosis, and spreading infection can cause dentoalveolar abscesses. If there is soft tissue swelling, antibiotics (e.g. amoxicillin or metronidazole) should be prescribed prior to dental intervention.
Erosion of the teeth can result from exposure to acid (e.g. in bulimia nervosa) or, very occasionally, in patients with gastro-oesophageal reflux disease.
Oral manifestations of HIV infection
HIV-infected patients often have characteristic oral lesions. Lesions strongly associated with HIV infection include candidiasis (with erythema and/or white exudates), erythematous candidiasis, oral hairy leucoplakia, Kaposi’s sarcoma, non-Hodgkin’s lymphoma, necrotizing ulcerative gingivitis and necrotizing ulcerative periodontitis and are described elsewhere.
All oral lesions are much less common since the introduction of HAART (in Chapter 4).
The salivary glands
Excessive salivation (ptyalism) may occur prior to vomiting or be secondary to other intraoral pathology. It can be psychogenic.
Dry mouth (xerostomia) can result from a variety of causes:
 Drugs (e.g. antimuscarinic, antiparkinsonian, antihistamines, lithium, monoamine oxidase inhibitors, tricyclic and related antidepressants, and clonidine)
Drugs (e.g. antimuscarinic, antiparkinsonian, antihistamines, lithium, monoamine oxidase inhibitors, tricyclic and related antidepressants, and clonidine)
The principles of management are to preserve what flow remains, stimulate flow and replace saliva (glycerine and lemon mouthwash and artificial saliva).
Sialadenitis
Acute sialadenitis is viral (mumps, p. 110) or bacterial. Bacterial sialadenitis is a painful ascending infection with Staphylococcus aureus, Streptococcus pyogenes and Strep. pneumoniae, usually secondary to secretory failure. Pus can be expressed from the affected duct.
Salivary duct obstruction due to calculus
Obstruction to salivary flow is usually due to a calculus. There is a painful swelling of the submandibular gland after eating and stones can sometimes be felt in the floor of the mouth. Plain X-ray films and sialography will show the calculus; removal of the obstruction by sialoendoscopy gives complete relief.
Sarcoidosis (see also p. 845)
Sarcoidosis can involve the major salivary glands as part of Heerfordt’s syndrome (uveoparotid fever).
Neoplasms
Salivary gland neoplasms account for 3% of all tumours worldwide. The majority occur in the parotid gland. The pleomorphic adenoma is the most common and 15% of these undergo malignant transformation. Malignant tumours classically result in lower motor neurone 7th cranial nerve signs. Recurrence following surgical excision is common.
The pharynx and oesophagus
Structure and physiology
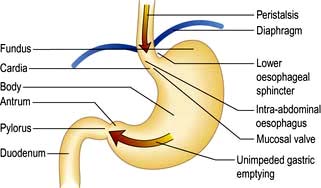
The oesophagus is a muscular tube approximately 20 cm long that connects the pharynx to the stomach just below the diaphragm. Its only function is to transport food from the mouth to the stomach. In the upper portion of the oesophagus, both the outer longitudinal layer and inner circular muscle layers are striated. In the lower two-thirds of the oesophagus, including the thoracic and abdominal parts containing the lower oesophageal sphincter, both layers are composed of smooth muscle.
The oesophagus is lined by stratified squamous epithelium, which extends distally to the squamocolumnar junction where the oesophagus joins the stomach, recognized endoscopically by a zig-zag (‘Z’) line, just above the most proximal gastric folds.
The oesophagus is separated from the pharynx by the upper oesophageal sphincter (UOS), which is normally closed due to tonic activity of the nerves supplying the cricopharyngeus. The lower oesophageal sphincter (LOS) consists of a 2–4 cm zone in the distal end of the oesophagus that has a high resting tone and, assisted by the diaphragmatic sphincter, is largely responsible for the prevention of gastric reflux.
Swallowing
During swallowing, the bolus of food is voluntarily moved from the mouth to the pharynx. This process is mediated by a complex reflex involving a swallowing centre in the dorsal motor nucleus of the vagus in the brainstem. Once activated, the swallowing centre neurones send pre-programmed discharges of inhibition followed by excitation to the motor nuclei of the cranial nerves. This results in initial relaxation, followed by distally progressive activation of neurones to the oesophageal smooth muscle and LOS. Pharyngeal and oesophageal peristalsis mediated by this swallowing reflex causes primary peristalsis. Secondary peristalsis arises as a result of stimulation by a food bolus in the lumen, mediated by a local intra-oesophageal reflex. Tertiary contractions indicate pathological non-propulsive contractions resulting from aberrant activation of local reflexes within the myenteric plexus.
The smooth muscle of the thoracic oesophagus and lower oesophageal sphincter is supplied by vagal autonomic motor nerves consisting of extrinsic preganglionic fibres and intramural postganglionic neurones in the myenteric plexus (Fig. 6.6). There are parallel excitatory and inhibitory pathways.
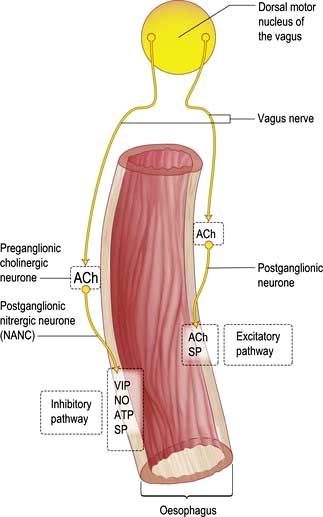
Figure 6.6 Innervation of the oesophagus. The excitatory pathway consists of vagal preganglionic neurones releasing acetylcholine (ACh), connecting to postganglionic neurones that release ACh and substance P. The inhibitory pathway consists of vagal preganglionic neurones releasing ACh, connecting to postganglionic neurones that release nitric oxide (NO), vasoactive intestinal peptide (VIP), adenosine triphosphate (ATP) and substance P (SP).
Symptoms of oesophageal disorders
Major oesophageal symptoms are:
 Dysphagia, or difficulty in swallowing, is defined as a sensation of obstruction during the passage of liquid or solid through the pharynx or oesophagus, i.e. within 15 s of food leaving the mouth. The characteristics of the progression of dysphagia to solids can be helpful, e.g. intermittent slow progression with a history of heartburn suggests a benign peptic stricture; relentless progression over a few weeks suggests a malignant stricture. The slow onset of dysphagia for solids and liquids at the same time suggests a motility disorder, e.g. achalasia (see p. 237). The causes are shown in Table 6.3.
Dysphagia, or difficulty in swallowing, is defined as a sensation of obstruction during the passage of liquid or solid through the pharynx or oesophagus, i.e. within 15 s of food leaving the mouth. The characteristics of the progression of dysphagia to solids can be helpful, e.g. intermittent slow progression with a history of heartburn suggests a benign peptic stricture; relentless progression over a few weeks suggests a malignant stricture. The slow onset of dysphagia for solids and liquids at the same time suggests a motility disorder, e.g. achalasia (see p. 237). The causes are shown in Table 6.3.
 Odynophagia is pain during the act of swallowing and is suggestive of oesophagitis. Causes include reflux, infection, chemical oesophagitis due to drugs such as bisphosphonates or slow-release potassium or associated with oesophageal stenosis.
Odynophagia is pain during the act of swallowing and is suggestive of oesophagitis. Causes include reflux, infection, chemical oesophagitis due to drugs such as bisphosphonates or slow-release potassium or associated with oesophageal stenosis.
 Substernal discomfort, heartburn. This is a common symptom of reflux of gastric contents into the oesophagus. It is usually a retrosternal burning pain that can spread to the neck, across the chest, and when severe can be difficult to distinguish from the pain of ischaemic heart disease. It is often worst lying down at night when gravity promotes reflux or on bending or stooping.
Substernal discomfort, heartburn. This is a common symptom of reflux of gastric contents into the oesophagus. It is usually a retrosternal burning pain that can spread to the neck, across the chest, and when severe can be difficult to distinguish from the pain of ischaemic heart disease. It is often worst lying down at night when gravity promotes reflux or on bending or stooping.
 Regurgitation is the effortless reflux of oesophageal contents into the mouth and pharynx. Uncommon in normal subjects, it occurs frequently in patients with gastro-oesophageal reflux disease or organic stenosis.
Regurgitation is the effortless reflux of oesophageal contents into the mouth and pharynx. Uncommon in normal subjects, it occurs frequently in patients with gastro-oesophageal reflux disease or organic stenosis.
Signs of oesophageal disorders
The main sign of oesophageal disease is weight loss due to reduced food intake. Cervical lymphadenopathy with cancer is uncommon. Rarely a pharyngeal pouch may be seen to swell the neck during drinking.
Investigations available for oesophageal disorders
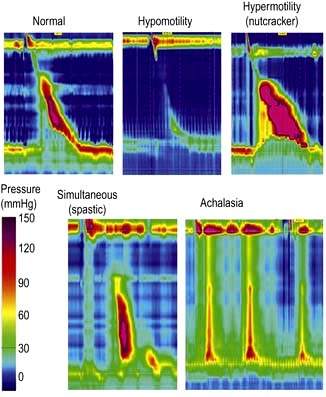
 Manometry (Fig. 6.7) is performed by passing a catheter through the nose into the oesophagus and measuring the pressures generated within the oesophagus. It is used to assess oesophageal motor activity. It is not a primary investigation and should be performed only when the diagnosis has not been achieved by history, barium radiology or endoscopy. Recordings are usually made over a short time period, or much more rarely for up to 24 h. High resolution manometry has superseded conventional manometry and the greater concentration of pressure sensors enables the identification of a wider range of abnormalities of oesophageal function with a greater diagnostic accuracy.
Manometry (Fig. 6.7) is performed by passing a catheter through the nose into the oesophagus and measuring the pressures generated within the oesophagus. It is used to assess oesophageal motor activity. It is not a primary investigation and should be performed only when the diagnosis has not been achieved by history, barium radiology or endoscopy. Recordings are usually made over a short time period, or much more rarely for up to 24 h. High resolution manometry has superseded conventional manometry and the greater concentration of pressure sensors enables the identification of a wider range of abnormalities of oesophageal function with a greater diagnostic accuracy.
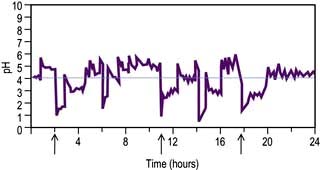
 pH monitoring – 24-hour ambulatory monitoring uses a pH-sensitive probe positioned in the lower oesophagus and is used to identify acid reflux episodes (pH <4). Catheter and implantable sensors are available; both are insensitive to alkali. Although only 5–10% of recorded acid reflux episodes are perceived by the patient, pH is a valuable means of correlating episodes of acid reflux with patient’s symptoms.
pH monitoring – 24-hour ambulatory monitoring uses a pH-sensitive probe positioned in the lower oesophagus and is used to identify acid reflux episodes (pH <4). Catheter and implantable sensors are available; both are insensitive to alkali. Although only 5–10% of recorded acid reflux episodes are perceived by the patient, pH is a valuable means of correlating episodes of acid reflux with patient’s symptoms.
 Impedance uses a catheter to measure the resistance to flow of ‘alternating current’ in the contents of the oesophagus. Combined with pH it allows assessment of acid, weakly acid, alkaline and gaseous reflux, which is helpful in understanding the symptoms that are produced by a non-acid reflux. Treatment is, however, still difficult in these conditions.
Impedance uses a catheter to measure the resistance to flow of ‘alternating current’ in the contents of the oesophagus. Combined with pH it allows assessment of acid, weakly acid, alkaline and gaseous reflux, which is helpful in understanding the symptoms that are produced by a non-acid reflux. Treatment is, however, still difficult in these conditions.
Gastro-oesophageal reflux disease (GORD)
Pathophysiology
Between swallows, the muscles of the oesophagus are relaxed except for those of the sphincters. The LOS remains closed due to the unique property of the muscle and relaxes when swallowing is initiated. Transient Lower Oesophageal Sphincter Relaxations (TLESRs) are part of normal physiology, but occur more frequently in GORD patients (Fig. 6.8).
Small amounts of gastro-oesophageal reflux are normal. The lower oesophageal sphincter (LOS) in the distal oesophagus is in a state of tonic contraction and relaxes transiently to allow the passage of a food bolus (see p. 229). Sphincter pressure also increases in response to rises in intra-abdominal and intragastric pressures.
Other antireflux mechanisms involve the intra-abdominal segment of the oesophagus which acts as a flap valve. In addition, the mucosal rosette formed by folds of the gastric mucosa and the contraction of the crural diaphragm at the LOS acting like a pinchcock, prevent acid reflux. A large hiatus hernia can impair this mechanism. The oesophagus is also normally rapidly ‘cleared’ of refluxate by secondary peristalsis, gravity and salivary bicarbonate.
The clinical features of reflux occur when the antireflux mechanisms fail, allowing acidic gastric contents to make prolonged contact with the lower oesophageal mucosa. The sphincter relaxes transiently independently of a swallow after meals and this is the cause of almost all reflux in normals and about two-thirds in GORD patients.
Oesophageal mucosal defence mechanisms
 Surface. Mucus and the unstirred water layer trap bicarbonate. This mechanism is a weak buffering mechanism compared to that in the stomach and duodenum.
Surface. Mucus and the unstirred water layer trap bicarbonate. This mechanism is a weak buffering mechanism compared to that in the stomach and duodenum.
 Epithelium. The apical cell membranes and the junctional complexes between cells act to limit diffusion of H+ into the cells. In oesophagitis, the junctional complexes are damaged leading to increased H+ diffusion and cellular damage.
Epithelium. The apical cell membranes and the junctional complexes between cells act to limit diffusion of H+ into the cells. In oesophagitis, the junctional complexes are damaged leading to increased H+ diffusion and cellular damage.
 Postepithelium. Bicarbonate normally buffers acid in the cells and intracellular spaces. Hydrogen ions impair the growth and replication of damaged cells.
Postepithelium. Bicarbonate normally buffers acid in the cells and intracellular spaces. Hydrogen ions impair the growth and replication of damaged cells.
 Sensory mechanisms. Acid stimulates primary sensory neurones in the oesophagus by activating the vanilloid receptor-1 (VR1). This can initiate inflammation and release of pro-inflammatory substances from the tissue and produce pain. Pain can also be due to contraction of longitudinal oesophageal muscle.
Sensory mechanisms. Acid stimulates primary sensory neurones in the oesophagus by activating the vanilloid receptor-1 (VR1). This can initiate inflammation and release of pro-inflammatory substances from the tissue and produce pain. Pain can also be due to contraction of longitudinal oesophageal muscle.
Clinical features
Heartburn is the major feature. Factors associated with GORD are shown in Table 6.4.
Table 6.4 Factors associated with gastro-oesophageal reflux
The burning is aggravated by bending, stooping or lying down which promote acid exposure, and may be relieved by oral antacids. The patient complains of pain on drinking hot liquids or alcohol.
The correlation between heartburn and oesophagitis is poor. Some patients have mild oesophagitis but severe heartburn; others have severe oesophagitis without symptoms, and may present with a haematemesis or iron deficiency anaemia from chronic blood loss. Psychosocial factors are often determinants of symptom severity. Many patients erroneously ascribe their symptoms to their hiatus hernia (Box 6.2) but the symptoms are due to reflux.
![]() Box 6.2
Box 6.2
Hiatus hernia
Differentiation of cardiac and oesophageal pain can be difficult; 20% of cases admitted to a coronary care unit have GORD (Box 6.3). In addition to the clinical features, a trial of a proton pump inhibitor (PPI) is always worthwhile and if symptoms persist, ambulatory pH and impedance monitoring should be performed.
![]() Box 6.3
Box 6.3
Features of the pain of gastro-oesophageal reflux and cardiac ischaemia
Regurgitation of food and acid into the mouth occurs, particularly on bending or lying flat. Aspiration pneumonia is unusual without an accompanying stricture, but cough and asthma can occur and respond slowly (1–4 months) to a PPI.
Diagnosis and investigations
The clinical diagnosis can usually be made without investigation. Unless there are alarm signs, especially dysphagia (see p. 229), patients under the age of 45 years can safely be treated initially without investigations. If investigation is required, there are two aims:
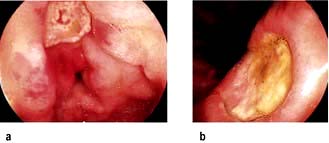
 Assess oesophagitis and hiatal hernia by endoscopy. If there is oesophagitis (Fig. 6.9) or Barrett’s oesophagus (see p. 241), reflux is confirmed.
Assess oesophagitis and hiatal hernia by endoscopy. If there is oesophagitis (Fig. 6.9) or Barrett’s oesophagus (see p. 241), reflux is confirmed.
 Document reflux by intraluminal monitoring (Fig. 6.10). 24-hour intraluminal pH monitoring or impedance combined with manometry is helpful if there is no response to PPI and should always be performed to confirm reflux before surgery. Excessive reflux is defined as a pH <4 for >4% of the time. There should also be a good correlation between reflux (pH <4.0) and symptoms. It is also helpful to assess oesophageal dysmotility as a potential cause of the symptoms.
Document reflux by intraluminal monitoring (Fig. 6.10). 24-hour intraluminal pH monitoring or impedance combined with manometry is helpful if there is no response to PPI and should always be performed to confirm reflux before surgery. Excessive reflux is defined as a pH <4 for >4% of the time. There should also be a good correlation between reflux (pH <4.0) and symptoms. It is also helpful to assess oesophageal dysmotility as a potential cause of the symptoms.
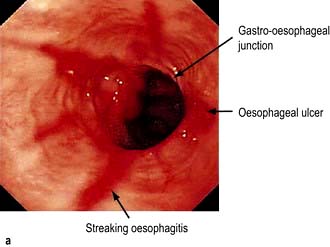
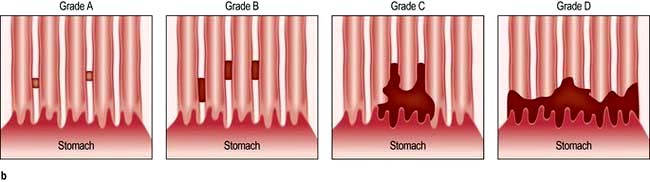
Figure 6.9 (a) Oesophagitis seen on endoscopy. (b) Los Angeles Classification of oesophagitis. Grade A = mucosal breaks confined to the mucosal folds, each no longer than 5 mm. Grade B = at least one mucosal break longer than 5 mm confined to the mucosal fold but not continuous between two folds. Grade C = mucosal breaks that are continuous between the tops of mucosal folds but not circumferential. Grade D = extensive mucosal breaks engaging at least 75% of the oesophageal circumference.
Treatment
Approximately half of patients with reflux symptoms in primary care can be treated successfully with simple antacids, loss of weight and raising the head of the bed at night. Precipitating factors should be avoided, with dietary measures, reduction in alcohol and caffeine consumption and cessation of smoking. These measures are simple to say but difficult to carry out, though they are useful in mild disease in compliant patients.
Drugs
Alginate-containing antacids (10 mL three times daily) are the most frequently used ‘over the counter’ agents for GORD. They form a gel or ‘foam raft’ with gastric contents to reduce reflux. Magnesium-containing antacids tend to cause diarrhoea while aluminium-containing compounds may cause constipation.
The dopamine antagonist prokinetic agents metoclopramide and domperidone are occasionally helpful as they enhance peristalsis and speed gastric emptying, but there is little data to substantiate this.
H2-receptor antagonists (e.g. cimetidine, ranitidine, famotidine and nizatidine) are frequently used for acid suppression if antacids fail as they can often be obtained over the counter.
Proton pump inhibitors (PPIs: omeprazole, rabeprazole, lansoprazole, pantoprazole, esomeprazole) inhibit gastric hydrogen/potassium-ATPase. PPIs reduce gastric acid secretion by up to 90% and are the drugs of choice for all but mild cases. Most patients with GORD will respond well, but this is only 20–30% of patients presenting with heartburn. Patients with severe symptoms may need twice-daily PPIs and prolonged treatment, often for years. Once oesophageal sensitivity has normalized, a lower dose, e.g. omeprazole 10 mg, may be sufficient for maintenance. The patients who do not respond to a PPI are sometimes described as having non-erosive reflux disease (NERD) (Fig. 6.11), when the endoscopy is normal. These patients are usually female and often the symptoms are functional, although a small group have a hypersensitive oesophagus, giving discomfort with only slight changes in pH. Isomers of some of the original PPIs (e.g. dexlansoprazole) have the benefit of more effective gastric acid inhibition over a longer time period as their metabolism to the active metabolite is slower.
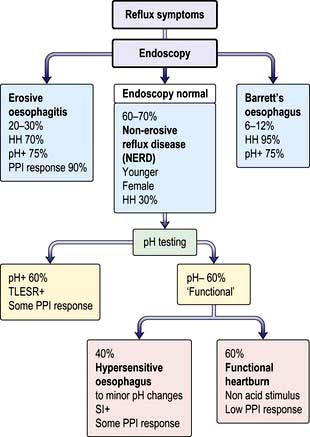
Figure 6.11 Outcome of patients with reflux symptoms. pH+, meets standard criteria for excessive acid reflux on intraluminal testing; pH−, does not meet standard criteria for excessive acid reflux; SI+, symptom index; TLESR, transient lower (o)esophageal sphincter relaxation; HH, hiatus hernia; PPI, proton pump inhibitor.
Endoluminal gastroplication
In this endoscopic procedure, multiple plications or pleats are made below the gastro-oesophageal junction. Randomized controlled trials have shown benefit with reduction in heartburn, acid reflux episodes and PPI usage.
Surgery
Surgery should never be performed for a hiatus hernia alone. The best predictors of a good surgical result are typical reflux symptoms with documented acid reflux, which correlates with symptoms and response to a PPI. With such highly selected cases in experienced hands, the laparoscopic Nissen fundoplication has over a 90% satisfaction rate at 5 years, and available 10-year data show satisfaction rates remain high at 88%. Current surgical techniques return the oesophagogastric junction to the abdominal cavity, mobilize the gastric fundus, close the diaphragmatic crura snugly and involve a short tension-free fundoplication.
Indications for operation are not clear cut but include intolerance to medication, the desire for freedom from medication, the expense of therapy and the concern of long-term side-effects. The most common cause of mechanical fundoplication failure is recurrent hiatus hernia.
Patients with oesophageal dysmotility unrelated to acid reflux, patients with no response to PPIs and those with underlying functional bowel disease should not have surgery.
Complications
Peptic stricture
Since the advent of PPIs peptic strictures have become far less common. They usually occur in patients over the age of 60 and present with intermittent dysphagia for solids which worsens gradually over a long period. Mild cases may respond to PPI alone. More severe cases need endoscopic dilatation and long-term PPI therapy. Surgery is required if medical treatment fails.
Barrett’s oesophagus

Barrett’s oesophagus. (a) Endoscopic picture of Barrett’s oesophagus. (b). Endoscopic narrow band imaging of Barrett’s mucosa. (c) Alcian blue staining of Barrett’s mucosa highlighting the blue-staining goblet cells. (d) H&E staining of the Barrett’s columnar mucosa.
Barrett’s oesophagus is a condition in which part of the normal oesophageal squamous epithelium is replaced by metaplastic columnar mucosa to form a segment of ‘columnar-lined oesophagus’ (CLO). It is a complication of gastro-oesophageal reflux disease and there is almost always a hiatus hernia present.
Diagnosis and classification. The diagnosis is made by endoscopy showing proximal displacement of the squamocolumnar mucosal junction and biopsies demonstrating columnar lining above the proximal gastric folds; intestinal metaplasia is no longer a requirement of the British Society of Gastroenterology definition, but is central to the American College of Gastroenterology guidelines. Barrett’s oesophagus may be seen as a continual circumferential sheet, or finger-like projections extending upwards from the squamocolumnar junction or as islands of columnar mucosa interspersed in areas of residual squamous mucosa. The Prague Classification (Fig. 6.12) is used for recording the endoscopic distribution, stating both the length of circumferential CLO (C measurement) as well as the maximum length (M measurement), the distance from the top of the gastric folds to the most proximal tongue of the columnar mucosa.
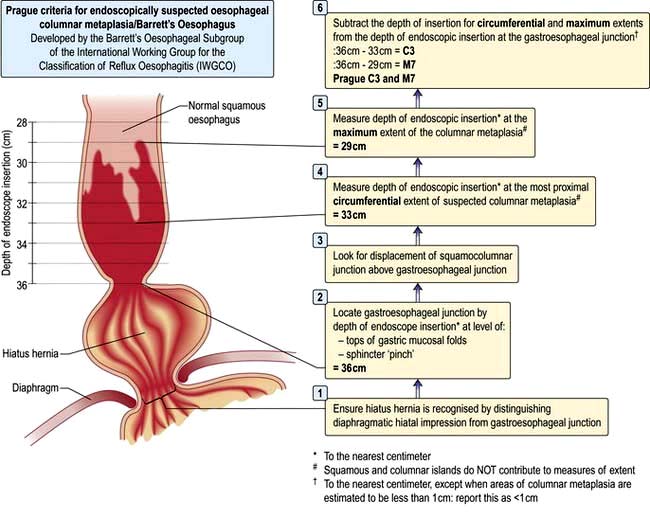
Figure 6.12 The Prague Criteria for endoscopically suspected oesophageal columnar metaplasia/Barrett’s oesophagus.
Central obesity increases the risk of Barrett’s by 4.3 times. Long segment (>3 cm) and short segment (<3 cm) Barrett’s is found respectively in 5% and 15% of patients undergoing endoscopy for reflux symptoms. It is also often found incidentally in endoscoped patients without reflux symptoms. Barrett’s is commonest in middle-aged obese men. The major concern is that approximately 0.12–0.5% of Barrett’s patients develop oesophageal adenocarcinoma per year, the majority, probably, through a gradual transformation from intestinal metaplasia to low-grade then high-grade dysplasia, before invasive adenocarcinoma. Barrett’s increases the chance of developing oesophageal adenocarcinoma 30- to 50-fold in early studies but a recent study showed the risk to be much lower.
In the absence of high quality trial evidence, 2-yearly gastroscopies are recommended by some, at which time biopsies from all four quadrants (every 1–2 cm) of the CLO are taken, as well as biopsies from macroscopically abnormal areas. High-grade dysplasia (HGD) is usually associated with endoscopically visible nodules or ulceration which are optimally visualized with a high definition endoscope. Chromo-endoscopy (the topical application of stains or pigments via the endoscope), narrow band and autofluorescence imaging may aid the diagnosis of dysplasia and carcinoma.
Endoscopic screening and surveillance in Barrett’s oesophagus. Because of the poor correlation between Barrett’s oesophagus and symptoms screening ‘at risk’ populations has not been shown to reduce the risk of oesophageal adenocarcinoma and is not recommended. As yet, there is no good evidence base for endoscopic surveillance of patients with established Barrett’s oesophagus; however, a randomized control trial is currently underway. The global consensus currently favours 2-yearly screening (in the absence of dysplastic change) with endoscopic technology improving the detection of premalignant lesions and enabling their removal with either endoscopic mucosal resection (EMR) or endoscopic submucosal dissection, therefore preventing surgical oesophagectomy. However, recent data, which have shown a reduction in the incidence of Barrett’s oesophagus, have cast doubt on this approach.
If low-grade dysplasia is found on endoscopic surveillance, a repeat endoscopy with quadrantic biopsies every 1 cm is usually performed within 6 months, while on high-dose proton pump inhibition. Long-term surveillance in this group is controversial.
If high-grade dysplasia is found, this is usually in the context of an endoscopically visible lesion which, if nodular, is removed by endoscopic mucosal resection for more accurate histological staging. If high-grade dysplasia is detected in the absence of any endoscopically visible lesion high-dose proton pump inhibition is started and repeat biopsies taken within 3 months. Endoscopic ultrasound is frequently used to more accurately stage this patient group to exclude cancer and associated significant lymphadenopathy.
Radiofrequency ablation (RFA) has superseded photodynamic therapy as the technique of choice for endoscopic treatment of dysplasia within Barrett’s segments following removal of any nodular lesions, returning the oesophagus to squamous lining. The benefit of RFA in low-grade dysplasia is currently under evaluation.
FURTHER READING
Galmiche J-P, Hatlebakk J, Attwood S et al., for the LOTUS Trial Collaborators. Laparoscopic antireflux surgery vs esomeprazole treatment for chronic GERD: The LOTUS Randomized Clinical Trial. JAMA 2011; 305:1969–1977.
Kahrilas PJ. Clinical practice. Gastrooesophageal reflux disease. N Engl J Med 2008; 359:1700–1707.
Kahrilas PJ, Shaheen NJ, Vaezi MF; American Gastroenterological Association Institute; Clinical Practice and Quality Management Committee. American Gastroenterological Association Institute technical review on the management of gastroesophageal reflux disease. Gastroenterology 2008; 135:1392–1413.
Kandulski A, Malfertheiner P. GERD in 2010: diagnosis, novel mechanisms of disease and promising agents. Nat Rev Gastroenterol Hepatol 2011; 8:73–74.
Massey BT. Physiology of oral cavity, pharynx and upper esophageal sphincter. In: Goyal R, Shaker R (eds). GI Motility. Also online: www.nature.com/gimo/contents/pt1/full/gimo2.html
Motility disorders
Achalasia
Achalasia is characterized by oesophageal aperistalsis and impaired relaxation of the lower oesophageal sphincter.
Clinical features
Achalasia incidence is 1 : 100 000 equally in males and females. It occurs at all ages but is rare in childhood. Patients usually have a long history of intermittent dysphagia, characteristically for both liquids and solids from the onset. Regurgitation of food from the dilated oesophagus occurs, particularly at night, and aspiration pneumonia is a complication. Spontaneous chest pain occurs, said to be due to oesophageal ‘spasm’. Dysphagia may be mild and accepted by the patient as normal. The pain may be misdiagnosed as cardiac. Weight loss is usually not marked.
Pathogenesis
The aetiology is unknown. Autoimmune, neurodegenerative and viral aetiologies have been implicated. A similar clinical picture is seen in chronic Chagas’ disease (American try-panosomiasis, p. 148) where there is damage to the neural plexus of the gut.
Histopathology shows inflammation of the myenteric plexus of the oesophagus with reduction of ganglion cell numbers. Cholinergic innervation appears to be preserved. Reduction in nitric oxide synthase-containing neurones has been shown by immunohistochemical staining. Pharmacological studies in patients with achalasia support the selective loss of inhibitory, nitrergic neurones. The differential diagnosis of achalasia worldwide includes genetic syndromes, infectious diseases, neoplasms and chronic inflammatory conditions.
Investigations
 Chest X-ray shows a dilated oesophagus, sometimes with a fluid level seen behind the heart. The fundal gas shadow is absent.
Chest X-ray shows a dilated oesophagus, sometimes with a fluid level seen behind the heart. The fundal gas shadow is absent.
 Barium swallow shows lack of peristalsis and often synchronous contractions in the body of the oesophagus, sometimes with dilatation. The lower end shows a ‘bird’s beak’ due to failure of the sphincter to relax (Fig. 6.13).
Barium swallow shows lack of peristalsis and often synchronous contractions in the body of the oesophagus, sometimes with dilatation. The lower end shows a ‘bird’s beak’ due to failure of the sphincter to relax (Fig. 6.13).
 Oesophagoscopy is performed to exclude a carcinoma at the lower end of the oesophagus, which can produce a similar X-ray appearance. When there is marked dilatation, a 24-hour liquid-only diet and a washout prior to endoscopy is useful to remove food debris. In true achalasia the endoscope passes through the lower oesophageal sphincter with little resistance.
Oesophagoscopy is performed to exclude a carcinoma at the lower end of the oesophagus, which can produce a similar X-ray appearance. When there is marked dilatation, a 24-hour liquid-only diet and a washout prior to endoscopy is useful to remove food debris. In true achalasia the endoscope passes through the lower oesophageal sphincter with little resistance.
 CT scan excludes distal oesophageal cancer.
CT scan excludes distal oesophageal cancer.
 Manometry shows aperistalsis of the oesophagus and failure of relaxation of the lower oesophageal sphincter (Fig. 6.7).
Manometry shows aperistalsis of the oesophagus and failure of relaxation of the lower oesophageal sphincter (Fig. 6.7).
Treatment
All current forms of treatment for achalasia are palliative. Drug therapy rarely produces satisfactory or durable relief; nifedipine (20 mg sublingually) or sildenafil can be tried initially.
Endoscopic and surgical therapies are equally effective. Endoscopic dilatation of the LOS using a hydrostatic balloon under X-ray control weakens the sphincter and is successful initially in 80% of cases. About 50% of patients require a second or third dilatation in the first 5 years. There is a low but significant risk of perforation. Intrasphincteric injection of botulinum toxin A produces satisfactory initial results but the effects wear off within months. Further injections can be given. It is safer and simpler than dilatation, so may be valuable in patients at risk of death if a perforation occurs. Neither pneumatic dilatation nor botulinum toxin works as well in younger patients.
Surgical division of the LOS, Heller’s operation, usually performed laparoscopically is the surgical treatment of choice. This can now be performed endoscopically.
Reflux oesophagitis complicates all procedures and the aperistalsis of the oesophagus remains.
FURTHER READING
Boeckxstaens GE, Annese V, des Varannes SB et al., for the European Achalasia Trial Investigators. Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med 2011; 364:1807–1816.
Richter JE, Boeckxstaens GE. Management of achalasia: surgery or pneumatic dilation. Gut 2011; 60:869–876.
Systemic sclerosis
The oesophagus is involved in almost all patients with this disease. Diminished peristalsis and oesophageal clearance, detected manometrically (Fig. 6.7) or by barium swallow, is due to replacement of the smooth muscle by fibrous tissue. LOS pressure is decreased, allowing reflux with consequent mucosal damage. Strictures may develop. Initially there are no symptoms, but dysphagia and heartburn occur as the oesophagus becomes more severely involved. Similar motility abnormalities may be found in other autoimmune rheumatic disorders, particularly if Raynaud’s phenomenon is present. Treatment is as for reflux (see p. 240) and benign stricture.
Diffuse oesophageal spasm
This is a severe form of oesophageal dysmotility that can sometimes produce retrosternal chest pain and dysphagia. It can accompany GORD. Swallowing is accompanied by bizarre and marked contractions of the oesophagus without normal peristalsis (Fig. 6.7). On barium swallow the appearance may be that of a ‘corkscrew’ oesophagus. However, asymptomatic oesophageal ‘dysmotility’ is not infrequent, particularly in patients over the age of 60 years.
A variant of diffuse oesophageal spasm is the ‘nutcracker’ oesophagus, which is characterized by very high-amplitude peristalsis (pressures >200 mmHg) within the oesophagus. Chest pain is commoner than dysphagia.
Treatment
True oesophageal spasm producing severe symptoms is uncommon and treatment is often difficult. PPIs may be successful if reflux is a factor. Antispasmodics, nitrates, calcium-channel blockers and more recently GABA receptor agonists (e.g. baclofen) are used. Occasionally, balloon dilatation or even longitudinal oesophageal myotomy is necessary.
Other oesophageal disorders
Oesophageal diverticulum
 Immediately above the upper oesophageal sphincter (pharyngeal pouch – Zenker’s diverticulum) (see p. 1054).
Immediately above the upper oesophageal sphincter (pharyngeal pouch – Zenker’s diverticulum) (see p. 1054).
 Near the middle of the oesophagus (traction diverticulum due to inflammation, or associated with diffuse oesophageal spasm or mediastinal fibrosis)
Near the middle of the oesophagus (traction diverticulum due to inflammation, or associated with diffuse oesophageal spasm or mediastinal fibrosis)
 Just above the lower oesophageal sphincter (epiphrenic diverticulum – associated with achalasia).
Just above the lower oesophageal sphincter (epiphrenic diverticulum – associated with achalasia).
Usually detected incidentally on a barium swallow performed for other reasons, these are often asymptomatic. Dysphagia and regurgitation can occur with a pharyngeal pouch (see p. 1054).
Rings and webs
An oesophageal web is a thin, membranous tissue flap covered with squamous epithelium. Most acquired webs are located anteriorly in the postcricoid region of the cervical oesophagus and are well seen on barium swallow. They may produce dysphagia. In the Plummer–Vinson syndrome (or Paterson–Brown–Kelly syndrome), a web is associated with chronic iron deficiency anaemia, glossitis and angular stomatitis. This rare syndrome affects mainly women and its aetiology is not understood. The web may be difficult to see at endoscopy and may be ruptured unintentionally by the passage of the endoscope. Dilatation of the web is rarely necessary. Iron is given for the iron deficiency.
Lower oesophageal rings
Lower oesophageal rings are of two types:
1. Mucosal (Schatzki’s ring, also called B ring) located at the squamocolumnar mucosal junction; it is common, and is associated with characteristic history of intermittent bolus obstruction. Barium swallow with a distended oesophagus shows the abnormality which may be difficult to see at endoscopy.
2. Muscular (A ring) located proximal to the mucosal ring and uncommon. It is covered by squamous epithelium and may cause dysphagia.
Treatment for these rings is usually with reassurance and dietary advice, but dilatation is occasionally necessary. After a single dilatation, 68% of patients with Schatzki’s rings are symptom free at 1 year, 35% remain symptom free after 2 years, but only 11% are symptom free at 3 years. Many also respond to oral PPI, either alone or with dilatation.
Benign oesophageal stricture
Peptic stricture secondary to reflux is the most common cause of benign strictures (for treatment, see p. 241). They also occur after the ingestion of corrosives, after radiotherapy, after sclerosis of varices, and following prolonged nasogastric intubation. Dysphagia is usually treated by endoscopic dilatation. Surgery is sometimes required.
Oesophageal infections
Infection is a cause of painful swallowing and is seen particularly in immunosuppressed (e.g. on chemotherapy) and debilitated patients and patients with AIDS. Infection can occur with:
It is occasionally difficult to distinguish between these disorders either on barium swallow or oesophagoscopy, as only widespread ulceration is seen. In candidiasis, the characteristic white plaques are frequently found; oral candidiasis is not always present. The diagnosis of Candida infection can be confirmed by examining a direct smear taken at endoscopy, but often infections are mixed and cultures and biopsies must be performed. TB causes deep ulceration with associated mediastinal lymphadenopathy.
Eosinophilic oesophagitis
Eosinophils can be seen in the oesophageal mucosa (which is usually devoid of eosinophils microscopically) due to a variety of causes such as eosinophilic (or allergic) oesophagitis and GORD.
Eosinophilic oesophagitis is being increasingly recognized but its pathogenesis is unknown. There may be a personal or family history of allergic disorders such as food allergy.
Patients present with a long history of dysphagia, food impaction, ‘heartburn’ and oesophageal pain. Usually the patient is male, white, and with an average age at diagnosis of 35, but it also occurs in children.
Typical endoscopic abnormalities include mucosal furrowing, loss of vascular pattern due to a thickened mucosa, plaques of eosinophilic surface exudate and prominent circular folds, but the oesophagus may appear macroscopically normal. Reflux oesophagitis and Schatzki’s rings may co-exist. Endoscopic forceps biopsies (× 6) should be taken from upper, mid and lower oesophagus for histology with eosinophil counts.
The eosinophilic infiltration of the oesophagus due to reflux disease can be excluded by rebiopsy after a 6-week course of full-dose PPI, when the eosinophil count will have fallen to below 15 per high power field
Treatment is topical, swallowing inhaled steroid preparations such as fluticasone, budesonide syrup, systemic steroids or elimination diets (more beneficial in children). Mepolizumab, a humanized monoclonal antibody against IL-5, has shown some benefit in small trials. Dilatation is sometimes necessary, with a risk of perforation of 2%.
Oesophageal perforation or rupture
Oesophageal perforation most commonly occurs at the time of endoscopic dilatation and, rarely, following insertion of a nasogastric tube, gastroscope or transoesophageal echoprobe. Patients with malignant, corrosive or post-radiotherapy strictures are more likely to suffer perforation than those with a benign peptic stricture.
Management usually involves placement of an expanding covered oesophageal stent (see p. 246), which usually seals the hole. A water-soluble contrast X-ray is performed after 2–3 days to check the perforation has sealed.
‘Spontaneous’ oesophageal rupture occurs with violent vomiting (Boerhaave’s syndrome), producing severe chest pain and collapse in typical cases. Diagnosis can be difficult because classic symptoms are absent in about a third of cases and delays in presentation for medical care are common. It may follow alcohol ingestion. A chest X-ray shows a hydropneumothorax. The diagnosis is made with a water-soluble contrast swallow or on CT. The mortality rate is approximately 35%, making it the most lethal perforation of the GI tract. The best outcomes are associated with early diagnosis and definitive surgical management within 12 hours of rupture. If intervention is delayed longer than 24 hours, the mortality rate (even after surgery) rises to above 50% and to nearly 90% after 48 hours.
Oesophageal tumours
Cancer of the oesophagus
This is the sixth most common cancer worldwide. Squamous cancers occurring in the middle third account for 40% of tumours, and in the upper third, 15%. Adenocarcinomas occur in the lower third of the oesophagus and at the cardia and represent approximately 45% of tumours. Primary small cell cancer is extremely rare.
Epidemiology and aetiological factors
Squamous cell carcinoma (SCC)
The geographic variation in incidence is greater than for any other carcinoma – often in regions very close to one another. It is common in Ethiopia, China, South and east Africa and in the Caspian regions of Iran. By contrast, north, middle and west Africa have low rates.
In the UK, the incidence is 5–10 per 100 000 and represents 2.2% of all malignant disease. The incidence of SCC is decreasing, in contrast to adenocarcinoma. SCC of the oesophagus is more common in men (2 : 1). Risk factors are shown in Table 6.5.
Table 6.5 Risk factors for cancer of the oesophagus
| Squamous cell carcinoma | Adenocarcinoma |
|---|---|
Tobacco smoking |
Longstanding, heartburn |
High alcohol intake |
Barrett’s oesophagus |
Plummer–Vinson syndrome |
Tobacco smoking |
Achalasia |
Obesity |
Corrosive stricturesCoeliac diseaseBreast cancer treated with radiotherapy |
Breast cancer treated with radiotherapy |
Older age |
|
|
|
Tylosisa |
|
a Tylosis is a rare autosomal dominant condition with hyperkeratosis of the palms and soles.
High levels of alcohol consumption increase the risk of squamous cell cancer of the oesophagus, while tobacco use is associated with an increased incidence of both squamous cell and adenocarcinomas of the oesophagus. Smoking, obesity and low fruit and vegetable consumption are implicated in approximately 9 in 10 squamous cell cancers of the oesophagus.
Diets rich in fibre, carotenoids, folate, vitamin C and non-starchy vegetables probably decrease the risk of oesophageal cancer whereas diets high in saturated fat and cholesterol and refined cereals have been associated with an increased risk. Red and processed meat intake has been associated with an increased risk of both oesophageal SCC and adenocarcinoma. Conversely, fish and white meat consumption have been inversely associated with risk of oesophageal SCC in case–control studies from Italy, Switzerland and Uruguay.
Adenocarcinoma
These tumours primarily arise in columnar-lined epithelium in the lower oesophagus (see also Barrett’s oesophagus, p. 241). The incidence of this tumour is increasing in western industrialized countries). A study of the cancer registry in the USA estimated that incidence in white males rose four-fold from 1979 to 2004. Extension of an adenocarcinoma of the gastric cardia into the oesophagus can present with the same symptoms. Previous reflux symptoms increase the risk up to eight-fold and the risk is proportional to their severity.
Clinical features
Carcinoma of the oesophagus occurs mainly in those aged 60–70 years. Dysphagia is progressive and unrelenting. Initially, there is difficulty in swallowing solids, but typically dysphagia for liquids follows within weeks. Impaction of food causes pain, but more persistent pain implies infiltration of adjacent structures.
The lesion may be ulcerative, proliferative or scirrhous, extending variably around the wall of the oesophagus to produce a stricture. Direct invasion of the surrounding structures and metastases to lymph nodes are commoner than disseminated metastases. Weight loss, due to the dysphagia as well as to anorexia, is frequent. Oesophageal obstruction eventually causes difficulty in swallowing saliva, and coughing and aspiration into the lungs is common.
Weight loss, anorexia and lymphadenopathy are the commonest physical signs.
Investigation
Diagnostic
 Endoscopy provides histological and or cytological proof of the carcinoma (Fig. 6.14a).
Endoscopy provides histological and or cytological proof of the carcinoma (Fig. 6.14a).
 Barium swallow can be useful where the differential diagnosis of dysphagia includes a motility disorder such as achalasia (Fig. 6.14b).
Barium swallow can be useful where the differential diagnosis of dysphagia includes a motility disorder such as achalasia (Fig. 6.14b).
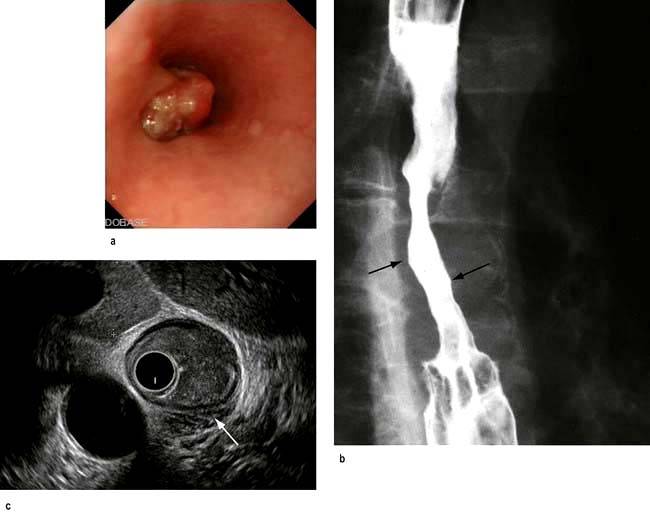
Figure 6.14 Carcinoma of the oesophagus. (a) Endoscopic image. (b) Barium swallow, showing an irregular narrowed area (arrows) at the lower end of the oesophagus. (c) Endoscopic ultrasound. The central concentric circles are the probe. The arrow points to a break in the muscle layer and the soft tissue mass of the carcinoma.
Staging
The TNM staging system is used (see p. 253), similar to the one used for gastric cancer. Tumour invasion of the wall of the oesophagus (T), presence of tumour in lymph nodes (N) or metastases (M) are combined into stage categories. Tumours arising in the cervical, thoracic and oesophagus, or abdominal oesophagus, including those that arise from within 5 cm from the gastro-oesophageal junction, share the same TNM staging criteria, but recent reclassification has differentiated between squamous and oesophageal cancers.
 CT scan of the thorax and upper abdomen shows the volume of the tumour, local invasion, peritumoral and coeliac lymph node involvement and metastases in the lung and elsewhere.
CT scan of the thorax and upper abdomen shows the volume of the tumour, local invasion, peritumoral and coeliac lymph node involvement and metastases in the lung and elsewhere.
 MRI is equivalent to CT in local staging but not as good for pulmonary metastases.
MRI is equivalent to CT in local staging but not as good for pulmonary metastases.
 Endoscopic ultrasound has an accuracy rate of nearly 90% for assessing depth of tumour and infiltration and 80% for staging lymph node involvement. It is useful if CT does not show a lesion already too advanced for surgery. A fine-needle aspiration (FNA) of lymph nodes improves staging accuracy, particularly of the coeliac nodes. Accurate T staging is necessary as cancers confined to the superficial mucosa can be removed endoscopically (Fig. 6.14c).
Endoscopic ultrasound has an accuracy rate of nearly 90% for assessing depth of tumour and infiltration and 80% for staging lymph node involvement. It is useful if CT does not show a lesion already too advanced for surgery. A fine-needle aspiration (FNA) of lymph nodes improves staging accuracy, particularly of the coeliac nodes. Accurate T staging is necessary as cancers confined to the superficial mucosa can be removed endoscopically (Fig. 6.14c).
 Laparoscopy is useful if the tumour is at the cardia, to look for peritoneal and node metastases.
Laparoscopy is useful if the tumour is at the cardia, to look for peritoneal and node metastases.
 Positron emission tomography (PET) after fluorodeoxyglucose is used principally to confirm distant metastases suspected on CT.
Positron emission tomography (PET) after fluorodeoxyglucose is used principally to confirm distant metastases suspected on CT.
Treatment
Although oesophageal SCC and adenocarcinomas are undoubtedly two different disease processes with independent tumour biology, the majority of trial data does not discriminate the two. Before 2010, they shared identical TNM staging system. How histology should influence treatment is therefore unclear and varies around the globe.
Treatment is dependent on the age and performance status of the patient and the stage of the disease. Five-year survival with stage 1 is 80% (T1/T2, N0, M0), stage 2 is 30%, stage 3 is 18% and stage 4 is 4%. Some 70% of patients present with stage 3 or greater disease, so that overall survival is 27% at 1 year and around 10% at 5 years. Management should be undertaken by multidisciplinary teams.
 Surgery provides the best chance of a cure but should only be used only when imaging (see above) has shown that the tumour has not infiltrated outside the oesophageal wall. Less than 40% of patients will have potentially resectable disease at the time of presentation. Patients must be carefully evaluated preoperatively, particularly with regard to performance status (see p. 253), and surgery undertaken in designated units. Poor outcome data from surgery alone has challenged its role as monotherapy and it is more often used in conjunction with neo-adjuvant (preoperative) and adjuvant (postoperative) treatment.
Surgery provides the best chance of a cure but should only be used only when imaging (see above) has shown that the tumour has not infiltrated outside the oesophageal wall. Less than 40% of patients will have potentially resectable disease at the time of presentation. Patients must be carefully evaluated preoperatively, particularly with regard to performance status (see p. 253), and surgery undertaken in designated units. Poor outcome data from surgery alone has challenged its role as monotherapy and it is more often used in conjunction with neo-adjuvant (preoperative) and adjuvant (postoperative) treatment.
 Chemoradiation. Preoperative (‘neo-adjuvant’) chemoradiation therapy may benefit patients with stage 2b and 3 disease. Prolongation of survival has been shown in some studies. In the USA neo-adjuvant chemoradiotherapy is preferred to the neo-adjuvant chemotherapy that is typically used in the UK.
Chemoradiation. Preoperative (‘neo-adjuvant’) chemoradiation therapy may benefit patients with stage 2b and 3 disease. Prolongation of survival has been shown in some studies. In the USA neo-adjuvant chemoradiotherapy is preferred to the neo-adjuvant chemotherapy that is typically used in the UK.
 Palliative therapy is often the only realistic possibility. Dilatation is only of short-term benefit and the perforation risk is higher than for benign strictures. Combination of endoscopic dilatation with laser or brachytherapy (see p. 447) prolongs luminal patency and gives as good if not better functional results than stenting. Insertion of an expanding metal stent allows liquids and soft foods to be eaten.
Palliative therapy is often the only realistic possibility. Dilatation is only of short-term benefit and the perforation risk is higher than for benign strictures. Combination of endoscopic dilatation with laser or brachytherapy (see p. 447) prolongs luminal patency and gives as good if not better functional results than stenting. Insertion of an expanding metal stent allows liquids and soft foods to be eaten.
 Photodynamic therapy (PDT) can be useful in more superficial cancers.
Photodynamic therapy (PDT) can be useful in more superficial cancers.
 Chemoradiation alone is sometimes given, but evidence of benefit is poor except in early stage SCC.
Chemoradiation alone is sometimes given, but evidence of benefit is poor except in early stage SCC.
 Nutritional support, as well as support for the patient and their family, is vital in this distressing condition.
Nutritional support, as well as support for the patient and their family, is vital in this distressing condition.
Other oesophageal tumours
Most other tumours are rare. Gastrointestinal stromal tumours (see p. 253) and leiomyomas (both submucosal tumours) are found usually by chance; 10% cause dysphagia or bleeding. Surgical removal is performed for symptomatic lesions or those over 3 cm, which are more likely to harbour malignancy. Small benign tumours are relatively common and often do not require treatment.
Kaposi’s sarcoma is found in the oesophagus as well as the mouth (see p. 193) and hypopharynx in patients with AIDS.
FURTHER READING
Cunningham D, Allum WH, Stenning SP et al., MAGIC Trial Participants. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med 2006; 355:11–20.
Okines A, Sharma B, Cunningham D. Perioperative management of esophageal cancer. Nat Rev Clin Oncol 2010; 7:231–238.
The stomach and duodenum
Structure
The stomach occupies a small area immediately distal to the oesophagus (the cardia), the upper region (the fundus, under the left diaphragm), the mid-region or body and the antrum, which extends to the pylorus (Fig. 6.8). It serves as a reservoir where food can be retained and broken up before being actively expelled in to the proximal small intestine.
The smooth muscle of the wall of the stomach has three layers: outer longitudinal, inner circular and innermost oblique layers. There are two sphincters, the gastro-oesophageal sphincter and the pyloric sphincter. The latter is largely made up of a thickening of the circular muscle layer and controls the exit of gastric contents into the duodenum.
The duodenum has outer longitudinal and inner smooth muscle layers. It is C-shaped and the pancreas sits in the concavity. It terminates at the duodenojejunal flexure where it joins the jejunum.
 The mucosal lining of the stomach can stretch in size with feeding. The greater curvature of the undistended stomach has thick folds or rugae. The mucosa of the upper two-thirds of the stomach contains parietal cells that secrete hydrochloric acid, and chief cells that secrete pepsinogen (which initiates proteolysis). There is often a colour change at the junction between the body and the antrum of the stomach that can be seen macroscopically, and confirmed by measuring surface pH.
The mucosal lining of the stomach can stretch in size with feeding. The greater curvature of the undistended stomach has thick folds or rugae. The mucosa of the upper two-thirds of the stomach contains parietal cells that secrete hydrochloric acid, and chief cells that secrete pepsinogen (which initiates proteolysis). There is often a colour change at the junction between the body and the antrum of the stomach that can be seen macroscopically, and confirmed by measuring surface pH.
 The antral mucosa secretes bicarbonate and contains mucus-secreting cells and G cells, which secrete gastrin, stimulating acid production. There are two major forms of gastrin, G17 and G34, depending on the number of amino-acid residues. G17 is the major form found in the antrum. Somatostatin, a suppressant of acid secretion, is also produced by specialized antral cells (D cells).
The antral mucosa secretes bicarbonate and contains mucus-secreting cells and G cells, which secrete gastrin, stimulating acid production. There are two major forms of gastrin, G17 and G34, depending on the number of amino-acid residues. G17 is the major form found in the antrum. Somatostatin, a suppressant of acid secretion, is also produced by specialized antral cells (D cells).
 Mucus-secreting cells are present throughout the stomach and secrete mucus and bicarbonate. The mucus is made of glycoproteins called mucins.
Mucus-secreting cells are present throughout the stomach and secrete mucus and bicarbonate. The mucus is made of glycoproteins called mucins.
 The ‘mucosal barrier’, made up of the plasma membranes of mucosal cells and the mucus layer, protects the gastric epithelium from damage by acid and, for example, alcohol, aspirin, NSAIDs and bile salts. Prostaglandins stimulate secretion of mucus, and their synthesis is inhibited by aspirin and NSAIDs, which inhibit cyclo-oxygenase (see Fig. 15.30).
The ‘mucosal barrier’, made up of the plasma membranes of mucosal cells and the mucus layer, protects the gastric epithelium from damage by acid and, for example, alcohol, aspirin, NSAIDs and bile salts. Prostaglandins stimulate secretion of mucus, and their synthesis is inhibited by aspirin and NSAIDs, which inhibit cyclo-oxygenase (see Fig. 15.30).
 The duodenal mucosa has villi like the rest of the small bowel, and also contains Brunner’s glands that secrete alkaline mucus. This, along with the pancreatic and biliary secretions, helps to neutralize the acid secretion from the stomach when it reaches the duodenum.
The duodenal mucosa has villi like the rest of the small bowel, and also contains Brunner’s glands that secrete alkaline mucus. This, along with the pancreatic and biliary secretions, helps to neutralize the acid secretion from the stomach when it reaches the duodenum.
Physiology
Acid secretion is central to the functionality of the stomach; factors controlling acid secretion are shown in Figure 6.15. Acid is not essential for digestion but does prevent some food-borne infections. It is under neural and hormonal control and both stimulate acid secretion through the direct action of histamine on the parietal cell. Acetylcholine and gastrin also release histamine via the enterochromaffin cells. Somatostatin inhibits both histamine and gastrin release and therefore acid secretion.
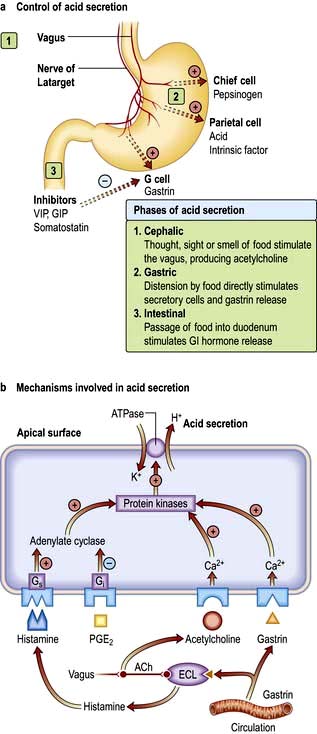
Figure 6.15 (a) Control of acid secretion. (b) Mechanisms involved in acid secretion: Histamine stimulates Gs via the H2 receptors and acts via cyclic AMP; prostaglandin E2 activates the Gi protein and inhibits acid secretion; acetylcholine (ACh) acts via the vagus M3 receptors; ACh also acts via the ECL cell; gastrin acts via the gastrin receptor, increasing the intracellular free calcium, and also via the ECL cell stimulating histamine. Gs and Gi, stimulating and inhibiting G-proteins; ECL, enterochromaffin cells.
Other major gastric functions are:
Gastric emptying depends on many factors. There are osmoreceptors in the duodenal mucosa that control gastric emptying by local reflexes and the release of gut hormones. In particular, intraduodenal fat delays gastric emptying by negative feedback through duodenal receptors.
Gastritis and gastropathy
Gastritis
‘Gastritis’ indicates inflammation associated with mucosal injury (although the term is often used loosely by endoscopists to describe ‘redness’), and ‘gastropathy’ indicates epithelial cell damage and regeneration without inflammation. Several classifications of gastritis (e.g. Sydney classification) have been proposed but are controversial due to lack of correlation, for example between endoscopic and histological findings. H. pylori infection is the commonest cause of gastritis (80%). Autoimmune gastritis is seen in 5%, while the remaining causes include viruses (e.g. cytomegalovirus and herpes simplex), duodenogastric reflux and specific causes, e.g. Crohn’s, more common in children than adults.
Autoimmune gastritis
This affects the fundus and body of the stomach (pangastritis), leading to atrophic gastritis and loss of parietal cells with achlorhydria and intrinsic factor deficiency causing the clinical syndrome of ‘pernicious anaemia’. Metaplasia, usually of the intestinal type, is almost always in the context of atrophic gastritis. Serum autoantibodies to gastric parietal cells are common and nonspecific: antibodies to intrinsic factor are rarer and more significant (see p. 382).
Gastropathy
Gastropathy is usually caused by irritants (drugs, NSAIDs and alcohol), bile reflux, hypovolaemia and chronic congestion. Acute erosive/haemorrhagic gastropathy can also be seen after severe stress (stress ulcers) and secondary to burns (Curling ulcers), trauma, shock, renal failure or in portal hypertension (called portal gastropathy). The underlying mechanism for these ulcers is unknown but may be related to an alteration in mucosal blood flow.
Ménétrier’s disease
This is a rare condition with characteristic giant gastric folds, mainly in the fundus and the body of the stomach. Histologically, there is hyperplasia of the gastric pits, atrophy of glands and an overall increase of mucosal thickness. Hyperchlorhydria is usually present. The patient may complain of epigastric pain. Peripheral oedema may occur because of hypoalbuminaemia due to protein loss through the gastric mucosa. It is probably premalignant but the rarity of the condition makes this uncertain. Treatment is unclear; some patients have responded to Helicobacter eradication and some improve spontaneously. Anti-secretory drugs are usually given. A few patients will require surgery.
Helicobacter pylori infection
H. pylori is a slow-growing spiral Gram-negative flagellate urease-producing bacterium (Fig. 6.16) which plays a major role in gastritis and peptic ulcer disease. It colonizes the mucous layer in the gastric antrum, but is also found in the duodenum in areas of gastric metaplasia. H. pylori is found in greatest numbers under the mucous layer in gastric pits, where it adheres specifically to gastric epithelial cells. It is protected from gastric acid by the juxtamucosal mucous layer which traps bicarbonate secreted by antral cells, and ammonia produced by bacterial urease.
Figure 6.16 Helicobacter pylori. (a) Organisms (arrowed) are shown on the gastric mucosa (cresyl fast violet (modified Giemsa) stain).
(Courtesy of Dr Alan Phillips, Department of Paediatric Gastroenterology, Royal Free Hospital.)

Epidemiology
The prevalence of H. pylori is high in developing countries (80–90% of the population), and much lower (20–50%) in developed countries. Infection rates are highest in lower income groups. Infection is usually acquired in childhood; although the exact route is uncertain, it may be faecal–oral or oral–oral. The incidence increases with age, probably due to acquisition in childhood when hygiene was poorer (cohort effect) rather than infection in adult life, which is probably far less than 1% per year in developed countries.
Pathogenesis
The pathogenetic mechanisms are not fully understood, with the majority of the colonized population remaining asymptomatic throughout their life. H. pylori is highly adapted to the stomach environment, exclusively colonizing gastric epithelium and inhabiting the mucous layer, or just beneath. It adheres by a number of adhesion molecules including BabA, which binds to the Lewis antigen expressed on the surface of gastric mucosal cells and causes gastritis in all infected subjects. Damage to the gastric epithelial cell is caused by the release of enzymes and the induction of apoptosis through binding to class II MHC molecules. The production of urease enables the conversion of urea to ammonium and chloride, which are directly cytotoxic. Ulcers are commonest when the infecting strain expresses CagA (cytotoxic-associated protein) and VacA (vacuolating toxin) genes secondary to a more pronounced inflammatory and immune response. Expression of CagA and VacA is associated with greater induction of IL-8, a potent mediator of gastric inflammation. Genetic variations in the host are also thought to be involved; for example, polymorphisms leading to increased levels of IL-1β are associated with atrophic gastritis and cancer.
Results of infection
Antral gastritis is the usual effect of H. pylori infection. It is usually asymptomatic, although patients without ulcers do sometimes experience relief of dyspeptic symptoms after Helicobacter eradication. Chronic antral gastritis causes hypergastrinaemia due to gastrin release from antral G cells. The subsequent increase in acid output is usually asymptomatic, but can lead to duodenal ulceration
Duodenal ulcer (DU) (see Fig. 6.18a). The prevalence of H. pylori infection in patients with duodenal ulceration is falling and in the developed world is now between 50% and 75%, whereas duodenal ulceration was once rare in the absence of H. pylori infection. This has been attributed to a decrease in prevalence of the bacteria and an increase in NSAID use. Eradication of the infection improves ulcer healing and decreases the incidence of recurrence.
The precise mechanism of duodenal ulceration is unclear, as only 15% of patients infected with H. pylori (50–60% of the adult population worldwide) develop duodenal ulcers. Factors that have been implicated include: increased gastrin secretion, smoking, bacterial virulence and genetic susceptibility.
Gastric ulcer (GU) (see Fig. 6.18b). Gastric ulcers are associated with a gastritis affecting the body as well as the antrum of the stomach (pangastritis) causing parietal cell loss and reduced acid production. The ulcers are thought to occur because of reduction of gastric mucosal resistance due to cytokine production by the infection or perhaps to alterations in gastric mucus.
Peptic ulcer disease
A peptic ulcer consists of a break in the superficial epithelial cells penetrating down to the muscularis mucosa of either the stomach or the duodenum; there is a fibrous base and an increase in inflammatory cells. Erosions, by contrast, are superficial breaks in the mucosa alone. Most DUs are found in the duodenal cap; the surrounding mucosa appears inflamed, haemorrhagic or friable (duodenitis). GUs are most commonly seen on the lesser curve near the incisura, but can be found in any part of the stomach.
Epidemiology of peptic ulcer disease
Duodenal ulcers affect approximately 10% of the adult population and are two to three times more common than gastric ulcers.
Ulcer rates are declining rapidly for younger men and increasing for older individuals, particularly women. Both DUs and GUs are common in the elderly. There is considerable geographical variation, with peptic ulcer disease being more prevalent in developing countries related to the high H. pylori infection. In the developed world the percentage of NSAID-induced peptic ulcers is increasing, as the prevalence of H. pylori declines.
Clinical features of peptic ulcer disease
The characteristic feature of peptic ulcer is recurrent, burning epigastric pain. It has been shown that if a patient points with a single finger to the epigastrium as the site of the pain this is strongly suggestive of peptic ulcer disease. The relationship of the pain to food is variable and on the whole not helpful in diagnosis. The pain of a DU classically occurs at night (as well as during the day) and is worse when the patient is hungry, but this is not reliable. The pain of both gastric and duodenal ulcers may be relieved by antacids.
Nausea may accompany the pain; vomiting is infrequent but can relieve the pain. Anorexia and weight loss may occur, particularly with GUs. Persistent and severe pain suggests complications such as penetration into other organs. Back pain suggests a penetrating posterior ulcer. Severe ulceration can occasionally be symptomless, as many who present with acute ulcer bleeding or perforation have no preceding ulcer symptoms.
Untreated, the symptoms of a DU relapse and remit spontaneously. The natural history is for the disease to remit over many years due to the onset of atrophic gastritis and a decrease in acid secretion.
Examination is usually unhelpful; epigastric tenderness is common in non-ulcer dyspepsia.
Diagnosis of Helicobacter pylori infection
Diagnosis of H. pylori is necessary if the clinician plans to treat a positive result. This is usually in the context of active peptic ulcer disease, previous peptic ulcer disease or MALT lymphoma, or to ‘test and treat’ patients with dyspepsia under the age of 55 with no alarm symptoms (i.e. weight loss, anaemia, dysphagia, vomiting, or family history of gastrointestinal cancer).
Non-invasive methods
 Serological tests detect IgG antibodies and are reasonably sensitive (90%) and specific (83%). They have been used in diagnosis and in epidemiological studies. IgG titres may take up to 1 year to fall by 50% after eradication therapy and therefore are not useful for confirming eradication or the presence of a current infection. Antibodies can also be found in the saliva, but tests are not as sensitive or specific as serology.
Serological tests detect IgG antibodies and are reasonably sensitive (90%) and specific (83%). They have been used in diagnosis and in epidemiological studies. IgG titres may take up to 1 year to fall by 50% after eradication therapy and therefore are not useful for confirming eradication or the presence of a current infection. Antibodies can also be found in the saliva, but tests are not as sensitive or specific as serology.
 13C-Urea breath test (Fig. 6.17). This is a quick and reliable test for H. pylori and can be used as a screening test. The measurement of 13CO2 in the breath after ingestion of 13C urea requires a mass spectrometer. The test is sensitive (90%) and specific (96%), but the sensitivity can be improved by insuring the patient has not taken antibiotics in the 4 weeks prior and proton pump inhibitors in the 2 weeks before the test.
13C-Urea breath test (Fig. 6.17). This is a quick and reliable test for H. pylori and can be used as a screening test. The measurement of 13CO2 in the breath after ingestion of 13C urea requires a mass spectrometer. The test is sensitive (90%) and specific (96%), but the sensitivity can be improved by insuring the patient has not taken antibiotics in the 4 weeks prior and proton pump inhibitors in the 2 weeks before the test.
 Stool antigen test. This is beginning to supersede breath testing as the method with which to determine H. pylori status. A specific immunoassay using monoclonal antibodies for the qualitative detection of H. pylori antigen is now widely available. The overall sensitivity is 97.6% with a specificity of 96%. It is useful in the diagnosis of H. pylori infection and for monitoring efficacy of eradication therapy. Patients should be off PPIs for 2 weeks but can continue with H2 blockers. Newer stool antigen tests are being developed that can be performed in the clinic setting, although at present the sensitivity and specificity are not as good as those performed in the laboratory.
Stool antigen test. This is beginning to supersede breath testing as the method with which to determine H. pylori status. A specific immunoassay using monoclonal antibodies for the qualitative detection of H. pylori antigen is now widely available. The overall sensitivity is 97.6% with a specificity of 96%. It is useful in the diagnosis of H. pylori infection and for monitoring efficacy of eradication therapy. Patients should be off PPIs for 2 weeks but can continue with H2 blockers. Newer stool antigen tests are being developed that can be performed in the clinic setting, although at present the sensitivity and specificity are not as good as those performed in the laboratory.
Invasive (endoscopy)
 Biopsy urease test. Gastric biopsies, usually antral unless additional material is needed to exclude proximal migration, are added to a substrate containing urea and phenol red. If H. pylori are present, the urease enzyme that they produce splits the urea to release ammonia which raises the pH of the solution and causes a rapid colour change (yellow to red). This enables a patient’s H. pylori status to be determined before they leave the endoscopy suite. The test may be falsely negative if patients are taking PPIs or antibiotics at the time.
Biopsy urease test. Gastric biopsies, usually antral unless additional material is needed to exclude proximal migration, are added to a substrate containing urea and phenol red. If H. pylori are present, the urease enzyme that they produce splits the urea to release ammonia which raises the pH of the solution and causes a rapid colour change (yellow to red). This enables a patient’s H. pylori status to be determined before they leave the endoscopy suite. The test may be falsely negative if patients are taking PPIs or antibiotics at the time.
 Histology. H. pylori can be detected histologically on routine (Giemsa) stained sections of gastric mucosa obtained at endoscopy. The sensitivity is reduced if a patient is on PPIs, but less so than with the urease test. This can be improved with immunohistochemical staining using an anti H. pylori antibody.
Histology. H. pylori can be detected histologically on routine (Giemsa) stained sections of gastric mucosa obtained at endoscopy. The sensitivity is reduced if a patient is on PPIs, but less so than with the urease test. This can be improved with immunohistochemical staining using an anti H. pylori antibody.
 Culture. Biopsies obtained can be cultured on a special medium, and in vitro sensitivities to antibiotics can be tested. This technique is typically used for patients with refractory H. pylori infection to identify the appropriate antibiotic regimen and routine culture is rare.
Culture. Biopsies obtained can be cultured on a special medium, and in vitro sensitivities to antibiotics can be tested. This technique is typically used for patients with refractory H. pylori infection to identify the appropriate antibiotic regimen and routine culture is rare.
Investigation of suspected peptic ulcer disease
 Patients under 55 years of age with typical symptoms of peptic ulcer disease who test positive for H. pylori can start eradication therapy without further investigation.
Patients under 55 years of age with typical symptoms of peptic ulcer disease who test positive for H. pylori can start eradication therapy without further investigation.
 Endoscopic diagnosis and exclusion of cancer is required in older patients (Fig. 6.18). All gastric ulcers must be biopsied to exclude an underlying malignancy and should be followed up endoscopically until healing has taken place.
Endoscopic diagnosis and exclusion of cancer is required in older patients (Fig. 6.18). All gastric ulcers must be biopsied to exclude an underlying malignancy and should be followed up endoscopically until healing has taken place.
 Endoscopy is required in all patients with ‘alarm symptoms’ (see p. 229).
Endoscopy is required in all patients with ‘alarm symptoms’ (see p. 229).
Eradication therapy
Current recommendations are that all patients with duodenal and gastric ulcers should have H. pylori eradication therapy if the bacteria is present. Many patients have incidental H. pylori infection with no gastric or duodenal ulcer. Whether all such patients should have eradication therapy is controversial (see Functional dyspepsia, p. 296).
The increase in the prevalence of GORD and adenocarcinoma of the lower oesophagus in the last few years is currently unexplained, but has been postulated to be linked to eradication of H. pylori. This seems unlikely but is not disproven.
Depending on local antibacterial resistance patterns standard eradication therapies in the developed world are successful in approximately 90% of patients.
Reinfection is very uncommon (1%) in developed countries. In developing countries reinfection is more common, compliance with treatment may be poor and metronidazole resistance is high (>50%) (as it is frequently used for parasitic infections), so failure of eradication is common.
There are many regimens for eradication, but all must take into account that:
 There is a high incidence of resistance to metronidazole and clarithromycin, particularly in some populations
There is a high incidence of resistance to metronidazole and clarithromycin, particularly in some populations
Metronidazole, clarithromycin, amoxicillin, tetracycline and bismuth are the most widely used agents. Resistance to amoxicillin (1–2%) and tetracycline (<1%) is low except in countries where they are available without prescription where resistance may exceed 50%. Quinolones such as ciprofloxacin, furazolidone and rifabutin are also used when standard regimens have failed (‘rescue therapy’). None of these drugs is effective alone; eradication regimens therefore usually comprise two antibiotics given with powerful acid suppression in the form of a PPI. Recent evidence has advocated bismuth-containing quadruple therapy as first-line because of increasing clarithromycin resistance.
FURTHER READING
Gisbert JP, Calvet X, O’Connor JP et al. The sequential therapy regimen for Helicobacter pylori eradication. Expert Opin Pharmacother 2010; 11:905–918.
Malfertheiner P, Bazzoli F, Delchier JC et al.; Pylera Study Group. Helicobacter pylori eradication with a capsule containing bismuth subcitrate potassium, metronidazole, and tetracycline given with omeprazole versus clarithromycin-based triple therapy: a randomised, open-label, non-inferiority, phase 3 trial. Lancet 2011; 377:905–913.
Example regimens are
 Omeprazole 20 mg + clarithromycin 500 mg and amoxicillin 1 g all twice daily
Omeprazole 20 mg + clarithromycin 500 mg and amoxicillin 1 g all twice daily
 Omeprazole 20 mg + metronidazole 400 mg and clarithromycin 500 mg – all twice daily.
Omeprazole 20 mg + metronidazole 400 mg and clarithromycin 500 mg – all twice daily.
These should be given for 7 or 14 days. Two-week treatments increase the eradication rates but increased side-effects may reduce compliance. Bismuth chelate is not usually given in initial regimens because of the more complex dosing regimen and side-effects. However, a single capsule is now available.
In eradication failures, bismuth chelate (120 mg 4× daily); metronidazole (400 mg 3× daily); tetracycline (500 mg 4× daily) and a PPI (20–40 mg 2× daily) for 14 days, is used. Sequential courses of therapy are being used in areas where resistance is high. With the increase in clarithromycin resistance, many are using this quadruple therapy for initial treatment.
Prolonged therapy with a PPI after a course of PPI-based 7-day triple therapy is not necessary for ulcer healing in most H. pylori-infected patients. The effectiveness of treatment for uncomplicated duodenal ulcer should be assessed symptomatically. If symptoms persist, breath or stool testing should be performed to check eradication.
Patients with a risk of bleeding or those with complications, i.e. haemorrhage or perforation, should always have a 13C urea breath test or stool test for H. pylori 6 weeks after the end of treatment to be sure eradication is successful. Long-term PPIs may be necessary if a rebleed would be likely to be fatal.
General measures
Stopping smoking should be strongly encouraged, as smoking slows mucosal healing.
Patients with gastric ulcers should be routinely re-endoscoped at 6 weeks to exclude a malignant tumour by confirming healing with biopsy if necessary.
Complications of peptic ulcer
Perforation (Box 6.4; see also p. 299)
The frequency of perforation of peptic ulceration is decreasing, partly attributable to medical therapy. DUs perforate more commonly than GUs, usually into the peritoneal cavity; perforation into the lesser sac also occurs. Detailed management of perforation is described on page 301. Laparoscopic surgery is usually performed to close the perforation and drain the abdomen. Conservative management using nasogastric suction, intravenous fluids and antibiotics is occasionally used in elderly and very sick patients.
Gastric outlet obstruction
The obstruction may be prepyloric, pyloric or duodenal. The obstruction occurs either because of an active ulcer with surrounding oedema or because the healing of an ulcer has been followed by scarring. However, obstruction due to peptic ulcer disease and gastric malignancy are now uncommon; Crohn’s disease or external compression from a pancreatic carcinoma are more common causes. Adult hypertrophic pyloric stenosis is a very rare cause.
After gastric outlet obstruction the stomach becomes full of gastric juice and ingested fluid and food, giving rise to the main symptom of vomiting, usually without pain as the characteristic ulcer pain has abated owing to healing.
Vomiting is infrequent, projectile, large in volume, and the vomitus contains particles of previous meals. On examination of the abdomen there may be a succussion splash. The diagnosis is made by endoscopy but can be suspected by the nature of the vomiting; by contrast, psychogenic vomiting is frequent, small volume and usually noisy.
Severe or persistent vomiting causes loss of acid from the stomach and a metabolic alkalosis (see p. 666). Vomiting will often settle with intravenous fluid and electrolyte replacement, gastric drainage via a nasogastric tube and potent acid suppression therapy. Endoscopic dilatation of the pyloric region is useful, as is luminal stenting, and overall, 70% of patients can be managed without surgery.
Surgical treatment and its long-term consequences
Once the mainstay of treatment, surgery is now used in peptic ulcer disease only for complications including:
No other procedure, such as gastrectomy or vagotomy, is required.
In the past, two types of operation were performed:
 Vagotomy. Initially this was a truncal vagotomy and required a gastric drainage procedure such as pyloroplasty or gastro-jejunostomy. In later years, this was usually highly selective vagotomy or proximal gastric vagotomy, in which only the nerves supplying the parietal cells were transected, and therefore no drainage of the stomach was required.
Vagotomy. Initially this was a truncal vagotomy and required a gastric drainage procedure such as pyloroplasty or gastro-jejunostomy. In later years, this was usually highly selective vagotomy or proximal gastric vagotomy, in which only the nerves supplying the parietal cells were transected, and therefore no drainage of the stomach was required.
Long-term complications of surgery which are still seen occasionally include:
 Recurrent ulcer. If this occurs, check for H. pylori; rule out Zollinger–Ellison syndrome (see p. 370). Malignancy needs to be excluded in all cases.
Recurrent ulcer. If this occurs, check for H. pylori; rule out Zollinger–Ellison syndrome (see p. 370). Malignancy needs to be excluded in all cases.
 Dumping. This term describes a number of upper abdominal symptoms (e.g. nausea and distension associated with sweating, faintness and palpitations) that occur in patients following gastrectomy or gastroenterostomy. It is due to ‘dumping’ of food into the jejunum, causing rapid fluid shifts from plasma to dilute the high osmotic load with reduction of blood volume. The symptoms are usually mild and patients adapt to them. It is rare for it to be a long-term problem, and if so, the symptoms usually have a functional element. Hypoglycaemia can also occur.
Dumping. This term describes a number of upper abdominal symptoms (e.g. nausea and distension associated with sweating, faintness and palpitations) that occur in patients following gastrectomy or gastroenterostomy. It is due to ‘dumping’ of food into the jejunum, causing rapid fluid shifts from plasma to dilute the high osmotic load with reduction of blood volume. The symptoms are usually mild and patients adapt to them. It is rare for it to be a long-term problem, and if so, the symptoms usually have a functional element. Hypoglycaemia can also occur.
 Diarrhoea was chiefly seen after vagotomy. Recurrent severe episodes occurred in about 1% of patients. Antidiarrhoeals are the usual treatment.
Diarrhoea was chiefly seen after vagotomy. Recurrent severe episodes occurred in about 1% of patients. Antidiarrhoeals are the usual treatment.
 Nutritional complications: in the long term almost any gastric surgery, but particularly gastrectomy, may be followed by:
Nutritional complications: in the long term almost any gastric surgery, but particularly gastrectomy, may be followed by:
Other H. pylori-associated diseases
 Gastric adenocarcinoma. The incidence of distal (but not proximal) gastric cancer parallels that of H. pylori infection in countries with a high incidence of gastric cancer. Serological studies show that people infected with H. pylori have a higher incidence of distal gastric carcinoma (see p. 252).
Gastric adenocarcinoma. The incidence of distal (but not proximal) gastric cancer parallels that of H. pylori infection in countries with a high incidence of gastric cancer. Serological studies show that people infected with H. pylori have a higher incidence of distal gastric carcinoma (see p. 252).
 Gastric B cell lymphoma. Over 70% of patients with gastric B cell lymphomas (mucosal-associated lymphoid tissue – MALT) have H. pylori. H. pylori gastritis has been shown to contain the clonal B cell that eventually gives rise to the MALT lymphoma (see pp. 467 and 468).
Gastric B cell lymphoma. Over 70% of patients with gastric B cell lymphomas (mucosal-associated lymphoid tissue – MALT) have H. pylori. H. pylori gastritis has been shown to contain the clonal B cell that eventually gives rise to the MALT lymphoma (see pp. 467 and 468).
NSAIDs, Helicobacter and ulcers
Aspirin and other NSAIDs deplete mucosal prostaglandins by inhibiting the cyclo-oxygenase (COX) pathway, which leads to mucosal damage. Cyclo-oxygenase occurs in two main forms: COX-1, the constitutive enzyme, and COX-2, inducible by cytokine stimulation in areas of inflammation. COX-2 specific inhibitors have less effect on the COX-1 enzyme in the gastric mucosa, but still produce gastric mucosal damage but less than with other conventional NSAIDs. Their use is limited by concern regarding cardiovascular side-effects.
Some 50% of patients taking regular NSAIDs will develop gastric mucosal damage and approximately 30% will have ulcers on endoscopy. Only a small proportion of patients have symptoms (about 5%) and only 1–2% have a major problem, i.e. GI bleed. Because of the large number of patients on NSAIDs including low-dose aspirin for vascular prophylaxis, this is a significant problem, particularly in the elderly.
H. pylori and NSAIDs are independent and synergistic risk factors for the development of ulcers. In a meta-analysis, the odds ratio (OR) for the incidence of peptic ulcer was 61.1 in patients infected with H. pylori and also taking NSAIDs, compared with uninfected controls not taking NSAIDs.
Treatment
In many people with severe arthritis, stopping NSAIDs may not be possible. Therefore use:
 An NSAID with low GI side-effects at lowest dose possible (see p. 511) or if there is no cardiovascular risk, a COX-2 NSAID can be used (see p. 511).
An NSAID with low GI side-effects at lowest dose possible (see p. 511) or if there is no cardiovascular risk, a COX-2 NSAID can be used (see p. 511).
 Prophylactic cytoprotective therapy, e.g. PPI or misoprostol (a synthetic analogue of prostaglandin E1 800 µg/day) for all high-risk patients, i.e. over 65 years; those with a peptic ulcer history, particularly with complications, and patients on therapy with corticosteroids or anticoagulants. PPIs reduce the risk of endoscopic duodenal and gastric ulcers and are better tolerated than misoprostol, which causes diarrhoea.
Prophylactic cytoprotective therapy, e.g. PPI or misoprostol (a synthetic analogue of prostaglandin E1 800 µg/day) for all high-risk patients, i.e. over 65 years; those with a peptic ulcer history, particularly with complications, and patients on therapy with corticosteroids or anticoagulants. PPIs reduce the risk of endoscopic duodenal and gastric ulcers and are better tolerated than misoprostol, which causes diarrhoea.
Gastric tumours
Adenocarcinoma
Gastric cancer is currently the fourth most common cancer found worldwide and the second leading cause of cancer-related mortality. The incidence increases with age (peak incidence 50–70 years), and it is rare under the age of 30 years. The highest incidences of the disease are found in Eastern Asia, Eastern Europe and South America. The incidence in men is twice that in women and varies throughout the world, being high in Japan (M: 53/100 000, F: 21.3/100 000) and Chile and relatively low in the USA (M: 7/100 000, F: 2.9/100 000). In the UK carcinoma of the stomach (see Fig. 6.1) is the eighth most common cancer (M: 16/100 000, F 9/100 000). Although the overall worldwide incidence of gastric carcinoma is falling, even in Japan, probably due to reductions in incidence of Helicobacter and before this, improvements in food storage, proximal gastric cancers are increasing in the West and have very similar demographic and pathological features as Barrett’s associated oesophageal adenocarcinoma.
Epidemiology and pathogenesis
 There is a strong link between H. pylori infection and distal gastric cancer. H. pylori is recognized by the International Agency for Research in Cancer (IARC) as a Group 1 (definite) gastric carcinogen. H. pylori infection causes chronic gastritis which eventually leads to atrophic gastritis and premalignant intestinal metaplasia (Fig. 6.19). Much of the earlier epidemiological data (i.e. the increase of cancer in lower socioeconomic groups) can be explained by the intrafamilial spread of H. pylori. Epstein–Barr virus is detected in 2–16% of gastric cancers worldwide, but its role in aetiology is not well understood.
There is a strong link between H. pylori infection and distal gastric cancer. H. pylori is recognized by the International Agency for Research in Cancer (IARC) as a Group 1 (definite) gastric carcinogen. H. pylori infection causes chronic gastritis which eventually leads to atrophic gastritis and premalignant intestinal metaplasia (Fig. 6.19). Much of the earlier epidemiological data (i.e. the increase of cancer in lower socioeconomic groups) can be explained by the intrafamilial spread of H. pylori. Epstein–Barr virus is detected in 2–16% of gastric cancers worldwide, but its role in aetiology is not well understood.
 Dietary factors may also be involved (as both initiators and promoters) and have separate roles in carcinogenesis. Diets high in salt probably increase the risk. Dietary nitrates can be converted into nitrosamines by bacteria at neutral pH, and nitrosamines are known to be carcinogenic in animals but the evidence in human carcinogenesis is limited. Nitrosamines are also present in the stomach of patients with achlorhydria, who have an increased cancer risk.
Dietary factors may also be involved (as both initiators and promoters) and have separate roles in carcinogenesis. Diets high in salt probably increase the risk. Dietary nitrates can be converted into nitrosamines by bacteria at neutral pH, and nitrosamines are known to be carcinogenic in animals but the evidence in human carcinogenesis is limited. Nitrosamines are also present in the stomach of patients with achlorhydria, who have an increased cancer risk.
 Smoking tobacco is associated with an increased incidence of stomach cancer.
Smoking tobacco is associated with an increased incidence of stomach cancer.
 Genetic abnormality. The commonest is a loss of heterozygosity (LOH) of tumour suppressor genes such as p53 (in 50% of cancers as well as in pre-cancerous states) and the APC gene (in over one-third of gastric cancers). These abnormalities are similar to those found in colorectal cancers. Some rare families with diffuse gastric cancer have been shown to have mutations in the E-cadherin gene (CDH-1). There is a higher incidence of gastric cancer in blood group A patients.
Genetic abnormality. The commonest is a loss of heterozygosity (LOH) of tumour suppressor genes such as p53 (in 50% of cancers as well as in pre-cancerous states) and the APC gene (in over one-third of gastric cancers). These abnormalities are similar to those found in colorectal cancers. Some rare families with diffuse gastric cancer have been shown to have mutations in the E-cadherin gene (CDH-1). There is a higher incidence of gastric cancer in blood group A patients.
 First-degree relatives of patients with gastric cancer have two- to three-fold increased relative risk of developing the disease, but this may be environmental rather than inherited.
First-degree relatives of patients with gastric cancer have two- to three-fold increased relative risk of developing the disease, but this may be environmental rather than inherited.
 Pernicious anaemia carries a small increased risk of gastric carcinoma due to the accompanying atrophic gastritis.
Pernicious anaemia carries a small increased risk of gastric carcinoma due to the accompanying atrophic gastritis.
 There is an increased risk of gastric cancer after a partial gastrectomy (postoperative stomach) whether performed for a gastric or a duodenal ulcer, probably due to untreated H. pylori infection.
There is an increased risk of gastric cancer after a partial gastrectomy (postoperative stomach) whether performed for a gastric or a duodenal ulcer, probably due to untreated H. pylori infection.
Screening
Earlier diagnosis has been advocated in an attempt to improve the poor prognosis of gastric cancer. (Screening is discussed on p. 435.) Although the incidence of gastric cancer is falling in Japan where aggressive screening by barium meal and endoscopy is pursued, there is no evidence that screening has had an effect on overall mortality. Similarly, early investigation of dyspepsia has had little effect on mortality, possibly because of the relatively low incidence of cancer.
Early gastric cancer
Early gastric cancer is defined as a carcinoma that is confined to the mucosa or submucosa, regardless of the presence of lymph node metastases. It is associated with 5-year survival rates of approximately 90%, but many of these patients would have survived 5 years without treatment. In Japan, mass screening with mobile X-ray units has increased the proportion of early gastric cancers (EGC) diagnosed. In a large series of patients with gastric cancer from the UK, only 0.7% were identified as having EGC. They are usually detected by chance as although EGC exists in western populations, endoscopists do not readily recognize it at present.
Pathology
There are two major types of gastric cancer:
 Intestinal (type 1): with well-formed glandular structures (differentiated). The tumours are polypoid or ulcerating lesions with heaped-up, rolled edges. Intestinal metaplasia is seen in the surrounding mucosa, often with H. pylori. This type is more likely to involve the distal stomach and occur in patients with atrophic gastritis. It has a strong environmental association.
Intestinal (type 1): with well-formed glandular structures (differentiated). The tumours are polypoid or ulcerating lesions with heaped-up, rolled edges. Intestinal metaplasia is seen in the surrounding mucosa, often with H. pylori. This type is more likely to involve the distal stomach and occur in patients with atrophic gastritis. It has a strong environmental association.
 Diffuse (type 2): with poorly cohesive cells (undifferentiated) that tend to infiltrate the gastric wall, may involve any part of the stomach, especially the cardia, and have a worse prognosis than the intestinal type. Loss of expression of the cell adhesion molecule E-cadherin is the key event in the carcinogenesis of diffuse gastric cancers. Unlike type 1 gastric cancers, type 2 cancers have similar frequencies in all geographic areas and occur in a younger population.
Diffuse (type 2): with poorly cohesive cells (undifferentiated) that tend to infiltrate the gastric wall, may involve any part of the stomach, especially the cardia, and have a worse prognosis than the intestinal type. Loss of expression of the cell adhesion molecule E-cadherin is the key event in the carcinogenesis of diffuse gastric cancers. Unlike type 1 gastric cancers, type 2 cancers have similar frequencies in all geographic areas and occur in a younger population.
Some 50% of gastric cancers in western countries occur in the proximal stomach.
Clinical features
Symptoms
Of patients with EGC discovered at screening, 50% have no symptoms. Most patients with carcinoma of the stomach have advanced disease at the time of presentation. The most common symptom of advanced disease is epigastric pain, indistinguishable from the pain of peptic ulcer disease; it may be relieved by food and antacids. The pain can vary in intensity, but may be constant and severe, and there may also be nausea, anorexia and weight loss. Vomiting is frequent and can be severe if the tumour encroaches on the pylorus. Dysphagia can occur with tumours involving the fundus. Gross haematemesis is unusual, but anaemia from occult blood loss is frequent. No pattern of symptoms is suggestive of early gastric cancer.
Widely spreading submucosal gastric cancer causes diffuse thickening and rigidity of the stomach wall and is called ‘linitis plastica’.
Patients can present at a late stage with malignant ascites or jaundice due to liver involvement. Metastases also occur in bone, brain and lung, producing appropriate symptoms.
Signs
Weight loss is often the dominant feature. Nearly 50% of patients have a palpable epigastric mass with abdominal tenderness. A palpable lymph node is sometimes found in the supraclavicular fossa (Virchow’s node, usually on the left side) and metastases are present in up to one-third of patients at presentation. This cancer is the most frequently associated with dermatomyositis (see p. 540) and acanthosis nigricans.
Diagnosis
 Gastroscopy (Fig. 6.20). Gastroscopy is performed so that biopsies can be taken for histological assessment. Positive biopsies can be obtained in almost all cases of obvious carcinoma, but a negative biopsy does not necessarily rule out the diagnosis. For this reason, 8–10 biopsies should be taken from suspicious lesions. Superficial brushings for cytology further improve the diagnostic rate.
Gastroscopy (Fig. 6.20). Gastroscopy is performed so that biopsies can be taken for histological assessment. Positive biopsies can be obtained in almost all cases of obvious carcinoma, but a negative biopsy does not necessarily rule out the diagnosis. For this reason, 8–10 biopsies should be taken from suspicious lesions. Superficial brushings for cytology further improve the diagnostic rate.
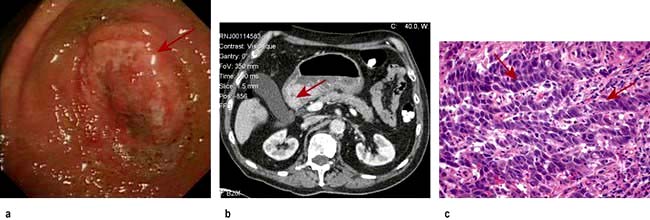
Figure 6.20 Carcinoma of the stomach. (a) Endoscopic picture showing a large irregular ulcer with rolled edges (arrow). (b) Axial CT scan (ulcer arrowed). (c) Histopathology showing an adenocarcinoma (arrows).
Staging
 CT scan of the chest and abdomen: CT with a gastric water load can demonstrate gastric wall thickening, lymphadenopathy and lung and liver secondaries, but has limited ability to determine the depth of local tumour invasion.
CT scan of the chest and abdomen: CT with a gastric water load can demonstrate gastric wall thickening, lymphadenopathy and lung and liver secondaries, but has limited ability to determine the depth of local tumour invasion.
 Transabdominal ultrasound can demonstrate masses, gastric wall thickening, lymphadenopathy and liver secondaries.
Transabdominal ultrasound can demonstrate masses, gastric wall thickening, lymphadenopathy and liver secondaries.
 Endoscopic ultrasound is useful for local staging to demonstrate the depth of penetration of the cancer through the gastric wall and extension into local lymph nodes. It complements CT and ultrasound but is most relevant to confirm a cancer is confined to the superficial mucosa, before endoscopic resection.
Endoscopic ultrasound is useful for local staging to demonstrate the depth of penetration of the cancer through the gastric wall and extension into local lymph nodes. It complements CT and ultrasound but is most relevant to confirm a cancer is confined to the superficial mucosa, before endoscopic resection.
 Laparoscopy is useful in patients being considered for surgery to exclude serosal disease.
Laparoscopy is useful in patients being considered for surgery to exclude serosal disease.
 PET and CT/PET can be helpful in further delineation of the cancer.
PET and CT/PET can be helpful in further delineation of the cancer.
The TNM classification is used. The tumour grade (T) indicates depth of tumour invasion, N denotes the presence or absence of lymph nodes, M indicates presence or absence of metastases. TNM classification is then combined into stage categories 0–4. At presentation, two-thirds of patients are at stage 3 or 4, i.e. advanced disease (Table 6.6). The histological grade of the tumour also determines survival.
Table 6.6 Gastric cancer – staging and 5-year survival rates
| Stage | TNM stage | 5-year survival (%) |
|---|---|---|
1 |
T1N0M0, T1N1M0 or T2N0M0 |
88 |
2 |
T1N2M0, T2N1M0 or T3N0M0 |
65 |
3a |
T2N2M0, T3N1M0 or T4N0M0 |
35 |
3b |
T3N2M0 |
35 |
4 |
T4N1–3M0, TxN3M0 or TxNxM1a |
5 |
T, tumour; N, nodes; M, metastases. aTx indicates any T stage; Nx, any N stage.
Treatment
As with all cancers, treatment is discussed with a multidisciplinary team. Early non-ulcerated mucosal lesions can be removed endoscopically by either endoscopic mucosal resection or endoscopic submucosal desection.
Surgery remains the most effective form of treatment if the patient is an operative candidate. Careful selection has reduced the numbers undergoing surgery and has improved the overall surgical 5-year survival rates to around 30%. Five-year survival rates in ‘curative’ operations are as high as 50%. Surgery and combined chemoradiotherapy and treatment of advanced disease is described on page 477. The multinational MAGIC trial demonstrated the benefits of perioperative chemotherapy with epirubicin, cisplatin and infusional 5-fluorouracil (ECF) (see Table 9.10), where 5-year survival in operable gastric and lower oesophageal adenocarcinomas increased from 23% to 36%. An alternative regimen is oral epirubicin, oxaliplatin and capecitabine. Despite the improved results, the overall survival rate for a patient with gastric carcinoma has not dramatically improved, with a maximum 10% 5-year survival rate overall. Palliative care with relief of pain and counselling are usually required.
Gastrointestinal stromal tumours (GIST)
GI stromal tumours (GISTs) are a subset of GI mesenchymal tumours of varying differentiation. They are usually asymptomatic and found by chance but they can occasionally ulcerate and bleed. There are 200–900 new cases each year in the UK. GISTs mostly affect people between 55 and 65.
These tumours used to be classified as GI leiomyomas, leiomyosarcomas, leiomyoblastomas or Schwannomas. Truly benign leiomyomas do occur, mainly in the oesophagus. GISTs are now recognized as a distinct group of mesenchymal tumours and comprise about 80% of GI mesenchymal tumours. They are of stromal origin, thought to share a common ancestry with the interstitial cells of Cajal. They have varying differentiation. Mutations occur in the cellular proto-oncogene KIT (which leads to activation and cell-surface expression of the tyrosine kinase KIT (CD 117)) in 80% and also in platelet-derived growth factor receptor-α (PDGFRA) in up to 10% of patients.
Treatment is surgical as far as possible. These tumours generally grow slowly but may be malignant. Imatinib, a tyrosine kinase inhibitor (p. 446), is used for unresectable or metastatic disease, and more recently as adjunctive therapy after surgical removal of the primary in the absence of metastatic disease. Some patients are resistant to this: sunitinib can be used as an alternative agent within a narrow time period.
Primary gastric lymphoma
Mucosa-associated lymphatic tissue lymphomas are indolent B cell marginal zone lymphomas primarily involving sites other than lymph nodes (gastrointestinal tract, thyroid, breast or skin). They constitute about 10% of all types of non-Hodgkin’s lymphoma (NHL).
Presentation
Most patients are diagnosed in their 60s with stage I or stage II disease outside the lymph nodes. Patients have stomach pain, ulcers or other localized symptoms, but rarely have systemic complaints such as fatigue or fever.
Causes
About 90% of cases are due to H. pylori infection. Chromosome abnormalities t(1;14)(p22; q32) and t(11;18)(q21; q21) have also been noted in this form of NHL.
Treatment
Eradication of H. pylori infection may resolve cases of local gastric involvement. After standard eradication regimens, 50% of patients show resolution at 3 months. Other patients may resolve after 12–18 months of observation. Stage III or IV disease is treated with surgery or CHOP chemotherapy with or without radiation. The prognosis is good, with an estimated 90% 5-year survival.
Gastric polyps
Gastric polyps are found in about 1% of endoscopies, usually by chance. They rarely produce symptoms.
Endoscopic biopsy is the usual approach to diagnosis with possible polypectomy based on histological finding for treatment. Occasional large or multiple polyps may require surgery.
Hyperplastic polyps are by far the most common. Most are <2 cm. The polyps are rarely premalignant, but may be accompanied by premalignant atrophic gastritis.
Adenomatous polyps are usually solitary lesions in the antrum. Approximately 3% progress to gastric cancer, especially if >2 cm in diameter, but they are not a common cause of gastric cancer (cf. colorectal cancer).
Cystic gland polyps contain microcysts that are lined by fundic-type parietal and chief cells. They are located in the fundus and body of the stomach. They are found in otherwise normal subjects, but are especially common in familial polyposis syndromes and have no malignant potential, although low-grade dysplasia is seen in the absence of FAP and high grade exclusively in its presence.
Inflammatory fibroid polyps are benign spindle cell tumours infiltrated by eosinophils. Excision of these polyps is indicated because of their propensity to enlarge and cause obstruction.
Acute and chronic gastrointestinal bleeding
This section should be read in conjunction with the descriptions of the specific conditions mentioned.
Acute upper gastrointestinal bleeding
The cardinal features are haematemesis (the vomiting of blood) and melaena (the passage of black tarry stools; the black colour due to blood altered by passage through the gut). Melaena can occur with bleeding from any lesion proximal to the right colon. Following a bleed from the upper GI tract, unaltered blood can appear per rectum, but the bleeding must be massive and is almost always accompanied by shock. The passage of dark blood and clots without shock is always due to lower GI bleeding.
Aetiology (Fig. 6.21)

Endoscopic view of GAVE (gastric antral vascular ectasia). Argon plasma coagulation catheter at 6 o’clock.
Peptic ulceration is the commonest cause of serious and life-threatening gastrointestinal bleeding. The relative incidence of causes depends on the patient population; overall the incidence has fallen. In the developing world haemorrhagic viral infections (see Table 4.20) can cause significant gastrointestinal bleeding.
Drugs. Aspirin (even 75 mg/day) and other NSAIDs can produce ulcers and erosions. These agents are also responsible for GI haemorrhage from both duodenal and gastric ulcers, particularly in the elderly. They are available over the counter in the UK and patients may not be aware they are taking aspirin or an NSAID. Corticosteroids in the usual therapeutic doses have no influence on GI haemorrhage. Anticoagulants do not cause acute GI haemorrhage per se but bleeding from any cause is greater if the patient is anticoagulated.
Clinical approach to the patient
All cases with a recent (i.e. within 48 hours) significant GI bleed should be seen in hospital. In many, no immediate treatment is required as there has been only a small amount of blood loss. Approximately 85% of patients stop bleeding spontaneously within 48 hours.
Scoring systems have been developed to assess the risk of rebleeding or death.
Table 6.7 shows the Rockall score, which is based on clinical and endoscopy findings. The Blatchford score uses the level of plasma urea, haemoglobin and clinical markers but not endoscopic findings to determine the need for intervention such as blood transfusion or endoscopy in GI bleeding.
The following factors affect the risk of rebleeding and death:
 Evidence of co-morbidity, e.g. cardiac failure, ischaemic heart disease, chronic kidney disease and malignant disease
Evidence of co-morbidity, e.g. cardiac failure, ischaemic heart disease, chronic kidney disease and malignant disease
 Presence of the classical clinical features of shock (pallor, cold peripheries, tachycardia and low blood pressure)
Presence of the classical clinical features of shock (pallor, cold peripheries, tachycardia and low blood pressure)
 Endoscopic diagnosis, e.g. Mallory–Weiss tear, peptic ulceration
Endoscopic diagnosis, e.g. Mallory–Weiss tear, peptic ulceration
 Endoscopic stigmata of recent bleeding, e.g. adherent blood clot, spurting vessel
Endoscopic stigmata of recent bleeding, e.g. adherent blood clot, spurting vessel
Bleeding associated with liver disease is often severe and recurrent if it is from varices. Liver failure can develop.
FURTHER READING
Banerjee S, Cash BD, Dominitz JA et al.; ASGE Standards of Practice Committee. The role of endoscopy in the management of patients with peptic ulcer disease. Gastrointest Endosc 2010; 71:663–668.
Gralnek IM, Baskin AN, Bardon M. Management of acute bleeding from a peptic ulcer. N Engl J Med 2008; 359:928–937.
Scottish Intercollegiate Guidelines Network (SIGN). Management of acute upper and lower gastrointestinal bleeding. Guideline No. 105, September 2008: www.sign.ac.uk/guidelines/fulltext/105/index.html
Immediate management
This is shown in Emergency Box 6.1. In addition, stop NSAIDs, aspirin, clopidogrel and warfarin if patients are taking them. Stopping antiplatelets can be dangerous and produce thrombosis: discuss urgently with a cardiologist.
![]() Emergency Box 6.1
Emergency Box 6.1
Management of acute gastrointestinal bleeding
 History and examination. Note co-morbidity
History and examination. Note co-morbidity
 Monitor the pulse and blood pressure half-hourly
Monitor the pulse and blood pressure half-hourly
 Take blood for haemoglobin, urea, electrolytes, liver biochemistry, coagulation screen, group and cross-matching (2 units initially)
Take blood for haemoglobin, urea, electrolytes, liver biochemistry, coagulation screen, group and cross-matching (2 units initially)
 Establish intravenous access – 2 large bore i.v. cannulae
Establish intravenous access – 2 large bore i.v. cannulae
 Give blood transfusion/colloid if necessary. Indications for blood transfusion are:
Give blood transfusion/colloid if necessary. Indications for blood transfusion are:
 Urgent endoscopy in shocked patients/liver disease
Urgent endoscopy in shocked patients/liver disease
 Continue to monitor pulse and BP
Continue to monitor pulse and BP
Many hospitals have multidisciplinary specialist teams with agreed protocols and these should be followed carefully. Patients should be managed in high-dependency beds. Oxygen should be given by facemask and the patient should be kept nil by mouth until endoscopy has been performed.
Patients with large bleeds and clinical signs of shock require urgent resuscitation. Details of the management of shock are given in Figure 16.25.
Blood volume
The major principle is to rapidly restore the blood volume to normal. This can be best achieved by transfusion of red cell concentrates via one or more large-bore intravenous cannulae; plasma expanders or 0.9% saline are given until the blood becomes available (see p. 887).
Transfusion must be monitored to avoid overload leading to heart failure, particularly in the elderly. The pulse rate and venous pressure are the best guides to adequacy of transfusion. A central venous pressure line is inserted for patients with organ failure who require blood transfusion, and in those most at risk of developing heart failure.
Haemoglobin levels are generally a poor indicator of the need to transfuse because anaemia does not develop immediately as haemodilution has not taken place. However, if the Hb is <100 g/L and the patient has either bled recently or is actively bleeding, transfusion is usually necessary. In most patients, the bleeding stops, albeit temporarily, so that further assessment can be made.
Endoscopy
Endoscopy will usually make a diagnosis, risk stratify and enable therapy to be performed if needed. Endoscopy should be performed as soon as possible after the patient has been resuscitated. Patients with Rockall scores of 0 or 1 pre-endoscopy may be candidates for immediate (see over) discharge and outpatient endoscopy the following day, depending on local policy.
Endoscopy can detect the cause of the haemorrhage in 80% or more of cases. In patients with a peptic ulcer, if the stigmata of a recent bleed are seen (i.e. a spurting vessel, active oozing, fresh or organized blood clot or black spots) the patient is more likely to rebleed. Calculation of the post-endoscopy Rockall score gives an indication of the risk of rebleeding and death.
 Varices should be treated, usually with banding. Stenting for varices is a recent innovation, not yet widely available – see page 333, for management of varices and is an alternative to a Sengstaken tube in the control of bleeding oesophageal varices.
Varices should be treated, usually with banding. Stenting for varices is a recent innovation, not yet widely available – see page 333, for management of varices and is an alternative to a Sengstaken tube in the control of bleeding oesophageal varices.
 Bleeding ulcers and those with stigmata of recent bleeding should be treated with two or three haemostatic methods, usually injection with epinephrine (adrenaline) and thermal coagulation (with heater probe, bipolar probe, laser or argon plasma coagulation) or endoscopic clipping because dual and triple therapy is more effective than monotherapy in reducing rebleeding.
Bleeding ulcers and those with stigmata of recent bleeding should be treated with two or three haemostatic methods, usually injection with epinephrine (adrenaline) and thermal coagulation (with heater probe, bipolar probe, laser or argon plasma coagulation) or endoscopic clipping because dual and triple therapy is more effective than monotherapy in reducing rebleeding.
 Antral biopsies should be taken to look for H. pylori. A positive biopsy urease test is valid, but a negative test is not reliable. If the urease test is negative, gastric histology should always be performed.
Antral biopsies should be taken to look for H. pylori. A positive biopsy urease test is valid, but a negative test is not reliable. If the urease test is negative, gastric histology should always be performed.
Drug therapy
After diagnosis at endoscopy, intravenous omeprazole 80 mg followed by infusion 8 mg/h for 72 hours should be given to all patients with actively bleeding ulcers or ulcers with a visible vessel, as it reduces rebleeding rates and the need for surgery. The majority of the landmark studies in this field have taken place in Hong Kong. H2-receptor antagonists are of no value.
Uncontrolled or repeat bleeding
Endoscopy should be repeated to assess the bleeding site and to treat, if possible. Surgery is necessary if bleeding is persistent and/or uncontrollable and should aim primarily to control the haemorrhage.
Discharge policy
The patient’s age, diagnosis on endoscopy, co-morbidity and the presence or absence of shock and the availability of support in the community should be taken into consideration. In general, all patients who are haemodynamically stable and have no stigmata of recent haemorrhage on endoscopy (Rockall Score pre-endoscopy 0, post-endoscopy <1) can be discharged from hospital within 24 hours. All shocked patients and patients with co-morbidity need longer inpatient observation.
Specific conditions
Oesophageal varices. These are discussed on page 924.
Mallory–Weiss tear. This is a linear mucosal tear occurring at the oesophagogastric junction and produced by a sudden increase in intra-abdominal pressure. It often occurs after a bout of coughing or retching and is classically seen after alcoholic ‘dry heaves’. There may, however, be no antecedent history of retching. Most bleeds are minor and discharge is usual within 24 hours. The haemorrhage may be large but most patients stop spontaneously. Early endoscopy confirms diagnosis and allows therapy if necessary. Surgery with oversewing of the tear is rarely needed.
Chronic peptic ulcer. Eradication of H. pylori is started as soon as possible (see p. 249). A PPI is continued for 4 weeks to ensure ulcer healing. Eradication of H. pylori should always be checked in a patient who has bled and long-term acid suppression given if HP eradication is not achieved. If bleeding is not controlled the patient should either undergo angiography and embolization or be referred directly for surgery.
Gastric carcinoma. Most of these patients do not have large bleeds but surgery is occasionally necessary for uncontrolled or repeat bleeding. Usually, surgery can be delayed until the patient has been fully evaluated (see p. 253). Oozing from gastric cancer is very difficult to control endoscopically. Radiotherapy can occasionally be successful.
Bleeding after percutaneous coronary intervention (PCI). In the era of ever more aggressive percutaneous coronary intervention the list of anti thrombotic medication grows longer: glycoprotein IIb/IIIa inhibitors, unfractionated heparin, low molecular weight heparin, fundoparinux, platelet inhibitors (e.g. clopidogrel, prasugrel). These, in addition to the oral anticoagulants that this group of patients are often taking, give rise to a GI bleeding rate of approximately 2% of patients undergoing PCI (who are on antiplatelet therapy, e.g. clopidogrel), and has a high mortality of 5–10%. It has become increasingly evident in this patient group that gastroscopy should be performed on an urgent basis and not deferred for days or weeks. A bolus of i.v. PPI is administered followed by an infusion; platelet infusion is given to counter the effect of clopidogrel. Management is difficult as cessation of antiplatelet therapy has a high risk of acute stent thrombosis and also an associated high mortality. Using a risk assessment score (e.g. Rockall, Table 6.7), a reasonable approach is to stop all antiplatelet therapy in high-risk patients but continue in low-risk ones. Co-prescribed proton pump inhibition does not decrease the antiplatelet effect of clopidogrel as was first thought. These patients should be under the combined care of a cardiologist and a gastroenterologist.
Acute lower gastrointestinal bleeding
Massive bleeding from the lower GI tract is rare and usually due to diverticular disease or ischaemic colitis. Common causes of small bleeds are haemorrhoids and anal fissures. The causes of lower GI bleeding are shown in Figure 6.22.
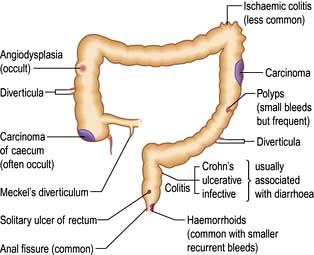
Figure 6.22 Causes of lower gastrointestinal bleeding. The sites shown are illustrative – many of the lesions can be seen in other parts of the colon.
Management
Most acute lower GI bleeds start and stop spontaneously. The few patients who continue bleeding and are haemodynamically unstable need resuscitation using the same principles as for upper GI bleeding (see p. 255). Surgery is rarely required.
A diagnosis is made using the history, examination including rectal examination and the following investigations as appropriate:
 Proctoscopy (e.g. anorectal disease, particularly haemorrhoids)
Proctoscopy (e.g. anorectal disease, particularly haemorrhoids)
 Flexible sigmoidoscopy or colonoscopy (e.g. inflammatory bowel disease, cancer, ischaemic colitis, diverticular disease, angiodysplasia)
Flexible sigmoidoscopy or colonoscopy (e.g. inflammatory bowel disease, cancer, ischaemic colitis, diverticular disease, angiodysplasia)
 Angiography – vascular abnormality (e.g. angiodysplasia). The yield of angiography is low, so it is a test of last resort.
Angiography – vascular abnormality (e.g. angiodysplasia). The yield of angiography is low, so it is a test of last resort.
Isolated episodes of rectal bleeding in the young (<45 years) usually only require rectal examination and flexible sigmoidoscopy because the probability of a significant proximal lesion is very low unless there is a strong family history of colorectal cancer at a young age. Individual lesions are treated as appropriate.
Chronic gastrointestinal bleeding
Patients with chronic bleeding usually present with iron-deficiency anaemia (see Ch. 8).
Chronic blood loss producing iron deficiency anaemia in all men, and all women after the menopause, is always due to bleeding from the GI tract. The primary concern is to exclude cancer, particularly of the stomach or right colon, and coeliac disease. Occult blood tests are unhelpful (Box 6.5). Iron deficiency anaemia can be due to poor iron intake (rare) or absorption as well as chronic blood loss.
![]() Box 6.5
Box 6.5
Measurement of faecal occult blood
This is frequently performed unnecessarily. It is only of value in:
 Premenopausal women – if a history of menorrhagia is uncertain and the cause of iron deficiency is unclear
Premenopausal women – if a history of menorrhagia is uncertain and the cause of iron deficiency is unclear
Advantages: cheap and easy to perform
Disadvantages: high false-positive rate, leading to unnecessary investigations
Diagnosis
Chronic blood loss can occur with any lesion of the GI tract that produces acute bleeding (Figs 6.21, 6.22). However, oesophageal varices usually bleed obviously and rarely present as chronic blood loss. Although uncommon in developed countries, hookworm is the most common worldwide cause of chronic GI blood loss.
History and examination may indicate the most likely site of the bleeding, but if no clue is available it is usual to investigate both the upper and lower GI tract endoscopically at the same session (‘top and tail’):
 Upper gastrointestinal endoscopy is usually performed first. Duodenal biopsies should always be taken to exclude coeliac disease, which is a recognized cause of iron deficiency.
Upper gastrointestinal endoscopy is usually performed first. Duodenal biopsies should always be taken to exclude coeliac disease, which is a recognized cause of iron deficiency.
 Colonoscopy follows and any lesion should be biopsied or removed, though it is not safe to assume that colonic polyps are the cause of chronic blood loss.
Colonoscopy follows and any lesion should be biopsied or removed, though it is not safe to assume that colonic polyps are the cause of chronic blood loss.
 Unprepared CT scanning is a reasonable test to look for colon cancer in frail patients.
Unprepared CT scanning is a reasonable test to look for colon cancer in frail patients.
 CT colonography can be used as an alternative to colonoscopy.
CT colonography can be used as an alternative to colonoscopy.
If gastroscopy, colonoscopy and duodenal biopsy have not revealed the cause, investigation of the small bowel is necessary. Capsule endoscopy is the diagnostic investigation of choice, but currently has no therapeutic ability. Positive diagnostic yield varies from 60% to 85% depending on series. Bleeding lesions can be identified and later treated with balloon-assisted enteroscopy.
Occasionally, intravenous technetium-labelled colloid may be used to demonstrate a potential bleeding site in a Meckel’s diverticulum.
Treatment
The cause of the bleeding should be treated, if found. Oral iron is given to treat anaemia (see p. 380), although intravenous infusions are occasionally required. Some patients will require maintenance with regular transfusion as a last resort.